Abstract
Objective
We investigated prolonged COVID-19 symptom duration, defined as lasting 28 days or longer, among people with systemic autoimmune rheumatic diseases (SARDs).
Methods
We analysed data from the COVID-19 Global Rheumatology Alliance Vaccine Survey (2 April 2021–15 October 2021) to identify people with SARDs reporting test-confirmed COVID-19. Participants reported COVID-19 severity and symptom duration, sociodemographics and clinical characteristics. We reported the proportion experiencing prolonged symptom duration and investigated associations with baseline characteristics using logistic regression.
Results
We identified 441 respondents with SARDs and COVID-19 (mean age 48.2 years, 83.7% female, 39.5% rheumatoid arthritis). The median COVID-19 symptom duration was 15 days (IQR 7, 25). Overall, 107 (24.2%) respondents had prolonged symptom duration (≥28 days); 42/429 (9.8%) reported symptoms lasting ≥90 days. Factors associated with higher odds of prolonged symptom duration included: hospitalisation for COVID-19 vs not hospitalised and mild acute symptoms (age-adjusted OR (aOR) 6.49, 95% CI 3.03 to 14.1), comorbidity count (aOR 1.11 per comorbidity, 95% CI 1.02 to 1.21) and osteoarthritis (aOR 2.11, 95% CI 1.01 to 4.27). COVID-19 onset in 2021 vs June 2020 or earlier was associated with lower odds of prolonged symptom duration (aOR 0.42, 95% CI 0.21 to 0.81).
Conclusion
Most people with SARDs had complete symptom resolution by day 15 after COVID-19 onset. However, about 1 in 4 experienced COVID-19 symptom duration 28 days or longer; 1 in 10 experienced symptoms 90 days or longer. Future studies are needed to investigate the possible relationships between immunomodulating medications, SARD type/flare, vaccine doses and novel viral variants with prolonged COVID-19 symptoms and other postacute sequelae of COVID-19 among people with SARDs.
Keywords: COVID-19, patient reported outcome measures, inflammation, vaccination
WHAT IS ALREADY KNOWN ON THIS TOPIC
While prolonged viral shedding during COVID-19 has been described in immunosuppressed patients, few studies have focused on symptom duration among people with systemic autoimmune rheumatic diseases (SARDs).
The US Centers for Disease Control and Prevention (CDC) defines prolonged COVID-19 symptoms as lasting 28 days or more; WHO defines it as lasting 90 days or more.
WHAT THIS STUDY ADDS
The median duration of COVID-19 symptoms among people with SARDs was 15 days.
Overall, 24.2% of respondents with SARDs and self-report of test-confirmed COVID-19 met the US CDC definition for prolonged symptom duration of 28+ days; 9.8% met the WHO definition of 90+ days.
Baseline factors associated with increased odds of prolonged symptom duration included more severe acute COVID-19, number of comorbidities and osteoarthritis, while disease onset in 2021 (vs June 2020 or earlier) was associated with lower odds.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These findings may help clinicians counsel people with SARDs on the expected duration of symptoms in COVID-19.
Future studies should focus on the subset of people with SARDs who experience prolonged COVID-19 symptoms to describe in further detail their experiences and investigate potential management strategies.
Introduction
The COVID-19 pandemic has had extensive impacts on health and society. People with systemic autoimmune rheumatic diseases (SARDs) have been particularly affected and may have an increased risk for both acquiring COVID-19 infection and developing severe acute outcomes, such as hospitalisation, mechanical ventilation and mortality.1 2 However, less research has focused on the postacute sequelae of COVID-19 (PASC), broadly composed of prolonged, persistent or evolving symptoms, sequelae and medical complications among survivors after the resolution of the acute COVID-19 phases.3 4 The US Centers for Disease Control and Prevention (CDC) defines prolonged COVID-19 symptom duration (colloquially referred to as ‘long COVID’) as lasting 28 days or longer after being infected with SARS-CoV-2.5 Alternatively, WHO defines prolonged COVID-19 symptom duration as lasting 90 days or longer.6
People with SARDs may be susceptible to prolonged COVID-19 symptoms for several reasons. These include potentially longer duration of viral infection, altered immunity, the use of immunosuppressive medications or potential overlap of SARD flare and COVID-19 symptoms.7 Although some immunosuppressed patients have been shown to have prolonged viral shedding, the symptom duration of COVID-19 among people with SARDs is less clear.8 9 A single-centre study of 174 COVID-19 survivors with SARDs found that 45% of people met the CDC definition of prolonged symptom duration, and many had underlying SARD flares and disruption of immunosuppressive medication.10 Larger, more diverse studies are needed to determine the incidence and baseline characteristics associated with prolonged COVID-19 symptom duration among people with SARDs.
We used the COVID-19 Global Rheumatology Alliance (GRA) Vaccine Survey to investigate symptom duration of COVID-19 among people with SARDs. First, we estimated the distribution of symptom duration after COVID-19 onset. Second, we reported the proportion of people recovered from COVID-19 with pre-existing SARDs experiencing prolonged symptom duration. Third, we investigated baseline factors associated with prolonged COVID-19 symptom duration.
Methods
Study design and population
We analysed data from the COVID-19 GRA Vaccine Survey to investigate symptom duration among people with SARDs who reported test-confirmed COVID-19. The survey was disseminated to people with SARDs and has been described elsewhere in detail.11 12 Briefly, the survey was iteratively developed in collaboration with rheumatologists, investigators, stakeholders and patient partners and disseminated online broadly via social media, email lists of the GRA and patient/physician organisations. The survey was launched globally in English on 2 April 2021, and subsequently translated into 11 other languages (Italian, Hebrew, French, Punjabi, Russian, Spanish, Arabic, Traditional Chinese (Mandarin), Simplified Chinese, Turkish and Hindi). We analysed data up to 15 October 2021, but nearly all responded prior to 1 July 2021. Participants provided consent at the initiation of the survey and confirmed SARD status and age of 18 years or older.
Systemic autoimmune rheumatic diseases
Respondents were asked, “Has a doctor ever told you that you had any of the following rheumatologic diseases?” For this analysis, respondents with only osteoarthritis and/or fibromyalgia were excluded.
Confirmed COVID-19 infection, severity and date of onset
Respondents were asked, “Have you been diagnosed with, or thought you had, COVID-19 (Coronavirus) infection?” Those who answered ‘yes’ were asked how COVID-19 was diagnosed. Possible answers were: (1) “I diagnosed myself based on symptoms”, (2) “My doctor diagnosed me based only on symptoms”, (3) “I was diagnosed based on positive test results for COVID-19 or SARS-CoV-2 (such as PCR or antibodies)”, (4) ‘not sure’ and (5) ‘other (please specify)’. For this analysis, we only analysed those who reported a positive test for COVID-19 (option 3). A study physician (JSp) reviewed all free-text responses to identify additional confirmed cases (typically rapid antigen tests). Respondents also specified the severity of the acute COVID-19 course: not hospitalised and no difficulties performing daily activities (reference group); not hospitalised but had difficulties performing daily activities; hospitalised or hospitalised and required intensive care unit (ICU) admission.
Respondents provided the month and year that they developed COVID-19. We a priori divided the calendar time into three time blocks related to major developments in the treatment and prevention of COVID-19: (1) the ‘early pandemic era’ of December 2019 to June 2020 (reference group); (2) the widespread use of dexamethasone to treat hospitalised COVID-19 from July 2020 to December 202013 and (3) the availability of COVID-19 vaccines from January 2021 onwards. While we collected data on vaccination, the timing related to infection was not collected.
COVID-19 symptom duration and definition of prolonged duration
People with COVID-19 were asked “Has your COVID-19 infection resolved at the time of this survey (meaning you no longer have symptoms related to COVID-19)?”. For those who answered ‘yes’, they were asked how many days their symptoms took to resolve. For those who answered ‘no’ or ‘not sure’, they were asked how long their symptoms have been ongoing. Since this study was focused on symptom duration, we did not analyse people with missing responses (n=4) for symptom duration.
A prespecified aim of the study was to investigate the proportion of SARDs that experience prolonged symptom duration and identify its baseline predictors. For the primary analysis, we excluded people with SARDs who had unresolved COVID-19 symptoms at time of survey completion and were <28 days from the onset of the infection, as we would be unable to determine whether or not they would go on to develop prolonged symptom duration. However, we included them in a sensitivity analysis investigating the observed symptom duration of all COVID-19 survivors with SARDs. For those reporting ongoing COVID-19 symptoms after day 28, we retained them in the analysis since we were able to determine they had met the CDC definition for prolonged symptom duration.
We also analysed the more stringent WHO definition of prolonged COVID-19 symptom duration of 90 days or longer as a secondary analysis, due to fewer outcomes, using similar methods.
Characteristics
The survey collected data on demographics, rheumatic medications and comorbidities. Demographics included age, sex and race/ethnicity (Asian, black, Hispanic/Latinx/Latin American, Middle Eastern or North African, American Indian/Alaska Native/Aboriginal/Indigenous/First Nations, white or other), WHO geographic region of residence (Americas, European, African, South-East Asian, Western Pacific or Eastern Mediterranean) and education (high school or less, some college, graduated college or graduate/professional degree).
Statistical analysis
We constructed a Kaplan-Meier survival curve to describe the primary outcome of time to symptom resolution. Time 0 was the date of COVID-19 onset provided by the respondent in relation to duration of COVID-19 symptoms at resolution or at the date of survey if still unresolved. For people with unresolved COVID-19, they were censored at the date of survey. We reported the days of symptom duration at the 25th, 50th, 75th, 95th and 99th percentiles.
We summarised characteristics that were collected at time of survey using descriptive statistics. We then stratified the sample by two groups (presence or absence (ie, resolved prior to day 28) of prolonged symptom duration) as the binary outcome variable. We performed age-adjusted models using multivariable logistic regression to obtain ORs and 95% CIs. We adjusted for age as a continuous variable since this may be a confounder between exposure variables such as COVID-19 severity and comorbidities and the outcome variable of prolonged COVID-19 symptom duration.
We reported characteristics separately for those who were excluded from the primary analysis due to having unresolved COVID-19 of <28 days duration. We performed a sensitivity analysis including them in the Kaplan-Meier curve analysis in case this influenced results. As in the primary analysis, those with unresolved COVID-19 symptoms were censored at the date of survey completion in the sensitivity analysis. We also performed similar analyses for the alternative WHO definition of prolonged symptom duration (90 days or longer).
The primary analysis only included those with test-confirmed COVID-19 to enhance the likelihood that a true infection was experienced. Since testing may have been limited or inaccessible to some, we performed sensitivity analyses also considering those with possible COVID-19. These people reported having COVID-19 but did not have test confirmation (possible responses included “I diagnosed myself based on symptoms”, “My doctor diagnosed me based only on symptoms”, “not sure” and ‘other’ and free-text response without test-confirmed COVID-19). Similar to the primary analysis, we did not analyse people with missing symptom duration data and who had unresolved COVID-19 symptom duration <28 days. We repeated the primary analyses (Kaplan-Meier curves and stratifying the sample by presence or absence of the US CDC definition of prolonged COVID-19 symptom duration) among those with possible COVID-19. Finally, we repeated the analyses among the entire combined sample of test-confirmed and possible COVID-19.
We considered a two-sided p value of <0.05 as statistically significant. We did not adjust for multiple comparisons. All analyses were performed using R software.
Results
Analysed study sample
As of 15 October 2021, 11 415 people from 102 countries completed the GRA Vaccine Survey. Figure 1 shows the flow diagram of the analysed study sample. Overall, there were 497 people with SARDs who reported test-confirmed COVID-19 and symptom duration. There were 56 people excluded from the primary analysis due to ongoing symptoms of <28 days duration. Thus, the primary study sample consisted of 441 people.
Figure 1.
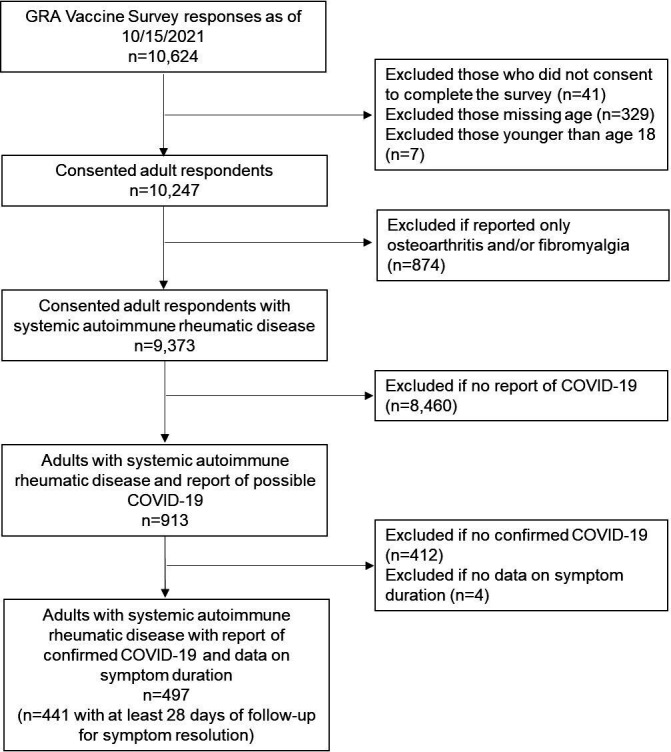
Flow diagram illustrating analysed study sample. GRA, Global Rheumatology Alliance.
Study sample characteristics
Table 1 shows the COVID-19 characteristics and demographics of the primary study sample, also stratified by presence or absence of prolonged symptom duration (ie, lasting 28 days or longer). Mean age was 48.2 years (SD 12.6), and 83.7% were female. Most respondents were located in either the Americas (63.2%) or Europe (30.5%).
Table 1.
COVID-19 and demographic characteristics of people with systemic autoimmune rheumatic diseases with confirmed COVID-19, overall and stratified by resolved or prolonged symptom duration by US Centers for Disease Control and Prevention definition of 28 days or longer (n=441)
| Overall N=441 |
Symptoms resolved in <28 days N=334 | Prolonged symptom duration 28 days or longer (active or resolved) N=107 | |
| Median COVID-19 symptom duration (or as of survey if ongoing), days (IQR) | 15 (7, 25) | 10 (7, 16) | 60 (30, 130) |
| COVID-19 symptom resolution | |||
| Yes | 398 (90.2) | 334 (100.0) | 64 (59.8) |
| No | 32 (7.3) | 0 (0.0) | 32 (29.9) |
| Not sure | 11 (2.5) | 0 (0.0) | 11 (10.3) |
| Date of COVID-19 onset | |||
| December 2019 to June 2020 | 108 (24.5) | 79 (23.7) | 29 (27.1) |
| July 2020 to December 2020 | 208 (47.2) | 148 (44.3) | 60 (56.1) |
| January 2021 to July 2021 | 125 (28.3) | 107 (32.0) | 18 (16.8) |
| Acute COVID-19 severity | |||
| Not hospitalised and no difficulties performing daily activities | 175 (39.7) | 157 (47.0) | 18 (16.8) |
| Not hospitalised but had difficulties performing daily activities | 211 (47.8) | 146 (43.7) | 65 (60.7) |
| Hospitalised | 46 (10.4) | 26 (7.8) | 20 (18.7) |
| Hospitalised and required ICU care | 9 (2) | 5 (1.5) | 4 (3.7) |
| Age (years), mean (SD) | 48.2 (12.6) | 47.3 (12.7) | 50.8 (12.0) |
| Age categories, years | |||
| 18–29 | 37 (8.4) | 30 (9.0) | 7 (6.5) |
| 30–49 | 197 (44.7) | 159 (47.6) | 38 (35.5) |
| 50–69 | 191 (43.3) | 134 (40.1) | 57 (53.3) |
| 70+ | 16 (3.6) | 11 (3.3) | 5 (4.7) |
| Female sex | 369 (83.7) | 276 (82.6) | 93 (86.9) |
| Race/Ethnicity | |||
| Asian (South, East Asian) | 11 (2.5) | 7 (2.1) | 4 (3.7) |
| Black | 13 (2.9) | 8 (2.4) | 5 (4.7) |
| Hispanic, Latinx or Latin American | 84 (19.0) | 72 (21.6) | 12 (11.2) |
| Middle Eastern or North African | 11 (2.5) | 10 (3) | 1 (0.9) |
| American Indian/Alaska Native/Aboriginal/Indigenous/First Nations | 1 (0.2) | 1 (0.3) | 0 (0.0) |
| White | 268 (60.8) | 194 (58.1) | 74 (69.2) |
| Other | 49 (11.1) | 38 (11.4) | 11 (10.3) |
| WHO region | |||
| Americas | 277 (62.8) | 211 (63.2) | 66 (61.7) |
| European | 140 (31.7) | 102 (30.5) | 38 (35.5) |
| Eastern Mediterranean | 10 (2.3) | 8 (2.4) | 2 (1.9) |
| South-East Asian | 8 (1.8) | 7 (2.1) | 1 (0.9) |
| African | 1 (0.2) | 1 (0.3) | 0 (0) |
| Western Pacific | 1 (0.2) | 1 (0.3) | 0 (0) |
| Education | |||
| High school (secondary level/GED) or less | 70 (15.9) | 55 (16.5) | 15 (14) |
| Some college | 103 (23.4) | 82 (24.6) | 21 (19.6) |
| Bachelor degree (graduated college) | 110 (24.9) | 82 (24.6) | 28 (26.2) |
| Graduate or professional degree | 154 (34.9) | 111 (33.2) | 43 (40.2) |
N (%) are presented unless otherwise specified.
GED, general equivalency degree; ICU, intensive care unit;
Table 2 shows the baseline clinical characteristics of the primary study sample. Rheumatoid arthritis (39.5%) was the most common SARD, followed by systemic lupus (15.6%), inflammatory myositis (11.6%) and Sjögren’s syndrome (11.6%). Most (274/411, 82.0%) were on at least one disease-modifying antirheumatic drug (DMARD) at time of survey. The most common DMARDs were methotrexate (26.5%), antimalarials (26.1%) and tumour necrosis factor inhibitors (15.0%); 27.4% reported glucocorticoid use. The most common comorbidities were hypertension (26.5%), obesity (23.1%) and lung disease (18.1%).
Table 2.
Baseline clinical characteristics of people with systemic autoimmune rheumatic diseases with confirmed COVID-19, overall and stratified by resolved or prolonged symptom duration by US Centers for Disease Control and Prevention definition of 28 days or longer (n=441)
| Overall N=441 |
Symptoms resolved in <28 days N=334 | Prolonged symptom duration 28 days or longer (active or resolved) N=107 | |
| SARD type | |||
| Rheumatoid arthritis | 174 (39.5) | 139 (41.6) | 35 (32.7) |
| Systemic lupus erythematosus | 69 (15.6) | 55 (16.5) | 14 (13.1) |
| Myositis | 51 (11.6) | 38 (11.4) | 13 (12.1) |
| Sjögren’s syndrome | 51 (11.6) | 36 (10.8) | 15 (14) |
| Spondyloarthritis, other than psoriatic arthritis | 50 (11.3) | 33 (9.9) | 17 (15.9) |
| Systemic vasculitis | 32 (7.3) | 24 (7.2) | 8 (7.5) |
| Psoriatic arthritis | 31 (7.0) | 26 (7.8) | 5 (4.7) |
| Systemic sclerosis | 18 (4.1) | 16 (4.8) | 2 (1.9) |
| Other connective tissue disease* | 15 (3.4) | 11 (3.3) | 4 (3.7) |
| Antiphospholipid syndrome | 11 (2.5) | 7 (2.1) | 4 (3.7) |
| Autoinflammatory disease | 4 (0.9) | 3 (0.9) | 1 (0.9) |
| Sarcoidosis | 2 (0.5) | 2 (0.6) | 0 (0) |
| Comorbidity count, mean (SD) | 4.5 (2.5) | 4.3 (2.5) | 5.0 (2.4) |
| Individual comorbidities | |||
| Hypertension | 117 (26.5) | 79 (23.7) | 38 (35.5) |
| Obesity | 102 (23.1) | 71 (21.3) | 31 (29.0) |
| Lung disease† | 80 (18.1) | 55 (16.5) | 25 (23.4) |
| Fibromyalgia | 51 (11.6) | 35 (10.5) | 16 (15.0) |
| Osteoarthritis | 35 (7.9) | 21 (6.3) | 14 (13.1) |
| Diabetes | 28 (6.3) | 20 (6.0) | 8 (7.5) |
| Cardiovascular disease | 17 (3.9) | 10 (3.0) | 7 (6.5) |
| No comorbidity | 145 (32.9) | 120 (35.9) | 25 (23.4) |
N (%) are presented.
*Other connective tissue disease includes mixed connective tissue disease and undifferentiated connective tissue disease.
†Lung disease includes asthma, emphysema, chronic bronchitis, chronic obstructive pulmonary disease, pulmonary hypertension, interstitial lung disease, idiopathic pulmonary fibrosis and other lung diseases.
SARD, systemic autoimmune rheumatic disease.
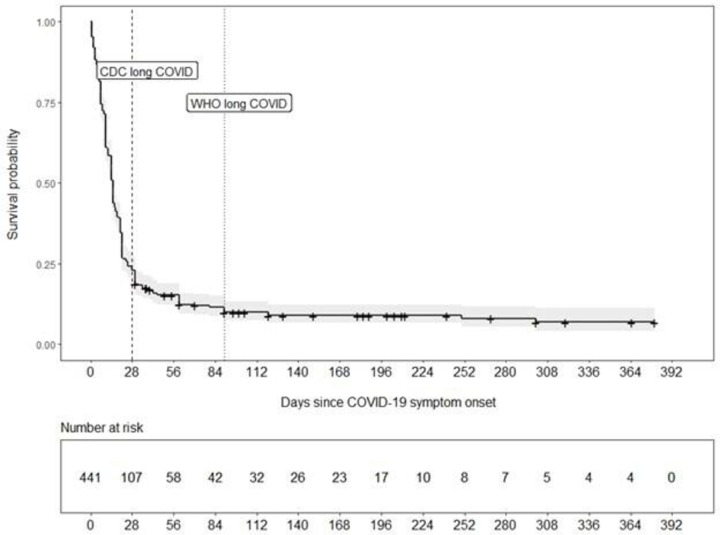
COVID-19 symptom duration
Figure 2 shows the Kaplan-Meier curve describing symptom resolution. Twenty-five percent of patients had symptom resolution 7 days after the infection, 50% after 15 days, 75% after 25 days and 95% after 180 days. By 312 days, 99% of people had symptom resolution.
Figure 2.
Kaplan-Meier survival curve for outcome of symptom resolution among people with systemic autoimmune rheumatic diseases with report of test-confirmed COVID-19 (n=441). The censoring event was ongoing symptom duration at time of survey (either unresolved or unsure if resolved). The vertical lines at days 28 and 90 indicate prolonged symptom duration, as defined by the US Centers for Disease Control and Prevention (CDC) and WHO, respectively. The symptom durations at the 25th, 50th, 75th, 95th and 99th percentiles were 7, 15, 25, 180 and 312 days, respectively.
Proportion with prolonged symptom duration by CDC definition (28+ days) and associations
A total of 107 (24.2%) people met the CDC definition for prolonged symptom duration lasting 28 days or more. Most (90.2%) had resolved COVID-19 symptoms at time of survey. Among all respondents, 54/411 (13.1%) were hospitalised for COVID-19, and 5/411 (1.5%) required ICU care.
Compared with those without prolonged symptom duration, those with prolonged symptom duration more often had COVID-19 managed as outpatient but with difficulties performing daily activities (age-adjusted OR (aOR) 4.02, 95% CI 2.31 to 7.31, table 3). Hospitalisation for COVID-19 was also associated with prolonged symptom duration as a PASC (aOR 6.49, 95% CI 3.03 to 14.1). Those with COVID-19 onset in January to July 2021 vs June 2020 or earlier had lower odds of prolonged symptom duration (aOR 0.42, 95% CI 0.21 to 0.81).
Table 3.
ORs for prolonged symptom duration by age, acute COVID-19 severity, date of COVID-19 onset and comorbidities
| OR (95% CI) for prolonged symptom duration 28 days or longer (CDC definition) | OR (95% CI) for prolonged symptom duration 90 days or longer (WHO definition) | |
| Age (per 10 years) | 1.25 (1.05 to 1.50) | 1.29 (1.00 to 1.68) |
| Age categories, years | ||
| 18–29 | 1.0 (ref) | 1.0 (ref) |
| 30–49 | 1.02 (0.44 to 2.69) | 1.55 (0.41 to 10.1) |
| 50–69 | 1.82 (0.80 to 4.73) | 2.16 (0.50 to 13.9) |
| 70+ | 1.95 (0.49 to 7.47) | 4.04 (0.61 to 33.4) |
| Age-adjusted OR (95% CI) | Age-adjusted OR (95% CI) | |
| Acute COVID-19 severity | ||
| Not hospitalised and no difficulties performing daily activities | 1.0 (ref) | 1.0 (ref) |
| Not hospitalised but had difficulties performing daily activities | 4.02 (2.31 to 7.31) | 2.84 (1.34 to 6.60) |
| Hospitalised | 6.49 (3.03 to 14.1) | 2.93 (0.92 to 8.72) |
| Hospitalised and required ICU care | 7.28 (1.66 to 30.4) | * |
| Date of COVID-19 onset | ||
| December 2019 to June 2020 | 1.0 (ref) | 1.0 (ref) |
| July 2020 to December 2020 | 1.05 (0.63 to 1.80) | 1.30 (0.61 to 2.95) |
| January 2021 to July 2021 | 0.42 (0.21 to 0.81) | 0.46 (0.15 to 1.28) |
| Comorbidity count (per comorbidity) | 1.11 (1.02 to 1.21) | 1.16 (1.02 to 1.33) |
| Individual comorbidities | ||
| Hypertension (vs not) | 1.55 (0.96 to 2.48) | 2.23 (1.14 to 4.33) |
| Lung disease† (vs not) | 1.52 (0.89 to 2.55) | 0.87 (0.34 to 1.94) |
| Obesity (vs not) | 1.46 (0.89 to 2.36) | 1.33 (0.63 to 2.63) |
| Diabetes (vs not) | 1.10 (0.45 to 2.43) | 0.62 (0.10 to 2.19) |
| Cardiovascular disease (vs not) | 1.87 (0.68 to 4.74) | 3.62 (1.11 to 10.1) |
| Osteoarthritis (vs not) | 2.11 (1.01 to 4.27) | 1.96 (0.69 to 4.80) |
| Fibromyalgia (vs not) | 1.51 (0.79 to 2.79) | 2.33 (1.01 to 5.02) |
| No comorbidity (vs any) | 0.60 (0.36 to 0.98) | 0.34 (0.13 to 0.78) |
*Model did not converge due to few outcomes.
†Lung disease includes asthma, emphysema, chronic bronchitis, chronic obstructive pulmonary disease, pulmonary hypertension, interstitial lung disease, idiopathic pulmonary fibrosis and other lung diseases.
CDC, Centers for Disease Control and Prevention; ICU, intensive care unit; ref, reference.
Other factors associated with prolonged symptom duration included older age (mean 50.8 years (SD 12.0) for those with prolonged symptom duration vs 47.3 years (SD 12.7) for those with symptom resolution by day 28, OR 1.25 per 10 years, 95% CI 1.05 to 1.50), comorbidity count (aOR 1.11 per comorbidity, 95% CI 1.02 to 1.21) and osteoarthritis (aOR 2.11, 95% CI 1.01 to 4.27). Those reporting no comorbidities (aOR 0.60, 95% CI 0.36 to 0.98) had lower odds of prolonged symptom duration. There were no statistical associations of SARD types with prolonged symptom duration.
WHO definition of prolonged symptom duration (90+ days)
The analysis investigating the more stringent WHO definition of prolonged symptom duration included 429 participants with sufficient follow-up to analyse (online supplemental table 1). Of these, 42 (9.8%) reported COVID-19 symptom duration of 90 days or longer and met this definition. Overall, the associations of baseline characteristics with prolonged symptom duration were similar but some no longer had statistical significance likely due to fewer outcomes. For example, hospitalised COVID-19 vs not hospitalised and mild symptoms (aOR 2.93, 95% CI 0.92 to 8.72), comorbidity count (aOR 1.16 per comorbidity, 95% CI 1.02 to 1.33) and COVID-19 onset in January to July 2021 vs June 2020 or earlier (aOR 0.46, 95% CI 0.15 to 1.28). In this analysis, fibromyalgia was associated with prolonged COVID-19 symptoms (aOR 2.33, 95% CI 1.01 to 5.02).
rmdopen-2022-002587supp001.pdf (208.5KB, pdf)
Sensitivity analyses
Online supplemental table 2 details the 56 people with unresolved COVID-19 at time of survey lasting <28 days. When these people were also included in the Kaplan-Meier curve (online supplemental figure 1), the 25th, 50th, 75th, 95th and 99th percentiles were 7, 14, 21, 150 and 301 days, respectively, overall similar to the primary analysis.
Results of the sensitivity analysis considering those with possible COVID-19 (n=381 after excluding n=16 with missing symptom duration and n=15 with unresolved COVID-19 of <28 days duration) are shown in online supplemental table 3 and the Kaplan-Meier curve in online supplemental figure 2. People with possible COVID-19 had median COVID-19 symptom duration of 20 days (IQR 10, 42). Among those with possible COVID-19, 152/381 (39.9%) met the CDC definition of prolonged COVID-19 symptom duration. When combining those with possible and test-confirmed COVID-19 (n=822, online supplemental table 4 and figure 3), median COVID-19 symptom duration was 15 days (IQR 8, 30) and 259/822 (31.5%) had COVID-19 symptoms for 28 days or longer.
Discussion
In this international survey-based study of people with SARDs reporting test-confirmed COVID-19, we found that the median COVID-19 symptom duration was 15 days. However, over one-quarter of people with SARDs and COVID-19 reported symptoms lasting for 28 days or longer; 1 in 10 had symptoms lasting for 90 days. We identified several baseline characteristics associated with prolonged symptom duration, which included acute COVID-19 severity, older age, comorbidities and osteoarthritis. Of note, those who had COVID-19 in 2021 (vs June 2020 or earlier) were less likely to have prolonged symptom duration, suggesting that the availability of vaccines or improvements in acute COVID-19 management may alter the risk for prolonged symptom duration. Further research is also needed regarding the minority of people with SARDs that experience prolonged symptom duration to define the natural history, optimal management and impact on the SARD course.
In the general population, estimates of median symptom duration of COVID-19 range between 7 and 12 days depending on factors such as methods of measurement, distribution of acute severity and viral epidemiology.14–16 Other studies also suggest that other immunosuppressed patients may have slightly longer median symptom duration than the general population. Some with cancer and organ transplant had very lengthy symptom duration and viral shedding.17–22 A study investigated persistent COVID-19 symptoms after hospital discharge for COVID-19 among 1969 people, of which 31 had pre-existing rheumatic or musculoskeletal disease (RMD).23 They found no association of RMD with long-term post-COVID-19 symptoms, but they may have been underpowered to detect a statistical association (OR 1.46, 95% CI 0.89 to 2.40, p=0.15) and RMD may have included non-systemic conditions.23 Overall, our results also suggest that many people with SARDs who develop COVID-19 may have symptom duration similar to the general population. However, there were a minority of people with SARDs who experienced lengthy symptom duration. Future studies with larger sample size control groups from the general population and people with SARDs without COVID-19 or after other infections are needed.
Other studies have also investigated prolonged COVID-19 symptom duration among people with SARDs. A recent study performed in Boston, Massachusetts, USA surveyed 174 people with SARDs who survived confirmed COVID-19 (82% as outpatient) and reported a median symptom duration of 25 days.10 That study found that a higher proportion of patients (45%) met the CDC definition for prolonged symptom duration than our current study (26.0%). Unlike the present study, they had data on specific post-COVID-19 symptoms; fatigue, pain, dyspnoea, dysgeusia and anosmia were common.10 That study also found a high proportion of DMARD disruption and SARD flares after COVID-19, emphasising that COVID-19 may also impact the underlying SARD activity. Another study found that SARD status was not associated with risk for ‘long-haul’ COVID-19 (defined in that study as 3 months or longer) compared with people without SARDs seen in a New York City academic rheumatology practice.24 However, it was composed of only 152 people with SARDs, so it may have been underpowered to detect a difference.24 They found that the presence of several symptoms during acute COVID-19 was associated with long-hauler status. They also showed that long-haulers were more likely to have higher PROMIS-29 scores indicating more anxiety, depression, fatigue and pain than those whose COVID-19 symptoms resolved within 1 month. Another study performed in Spain surveyed 105 rheumatology clinic patients (classified as SARDs or non-SARDs) who were hospitalised for COVID-19.25 They found that 69% of these posthospitalisation survivors were still experiencing fatigue, pain or dyspnoea about 2 months after COVID-19 onset.25 These findings emphasise the need for further research to define how COVID-19 may impact SARDs, particularly as prevention, treatment and virus properties evolve throughout the pandemic.
Similar to studies on the general population, we found that severity of acute COVID-19, older age and comorbidities were associated with prolonged symptom duration.3 26 27 Notably, we found that people who developed COVID-19 more recently (since January 2021 vs earlier) were less likely to develop prolonged COVID-19 symptoms. Several reasons for this observation of calendar time with risk of prolonged COVID-19 symptom duration could be considered. First, this period coincided with the wide availability of highly effective vaccines and treatment options (eg, monoclonal antibodies in the outpatient setting), suggesting that vaccination against COVID-19 or outpatient treatment may shorten the duration of viral shedding and reduce the likelihood of developing prolonged symptoms, as reported for the general population.28–32 Second, it is possible that specific circulating variants may impact symptom duration.33 Third, differential recall bias, where people with more recent onset of COVID-19 more accurately reported the end of symptoms, may have affected reporting. Fourth, patients who reported COVID-19 more recently may actually have been experiencing re-infection, which may have a different disease course.34 Fifth, people with unresolved COVID-19 cases at the time of survey may have been more likely to have been infected recently, and some of these may have later developed prolonged symptoms. Even after adjustment for age, osteoarthritis was associated with the US CDC definition of prolonged COVID-19 severity but not the WHO definition. Future studies are needed to replicate this finding and investigate potential mechanisms that include predisposition to prolonged COVID-19 symptom duration due to frailty or secondary osteoarthritis as a marker of SARD severity. Studies should also investigate whether vaccination, immunomodulating medications and SARD flares may impact risk for prolonged symptom duration for people with SARDs experiencing breakthrough infection while accounting for possible differential follow-up related to timing of infection onset and measurement of post-COVID-19 symptoms.
Strengths of our study include the relatively large sample size of contemporaneous survey data from people with SARDs and test-confirmed COVID-19 as well as the international nature of the study with multiple languages. However, there are also limitations to consider. First, the primary aim of the survey was to gather information about COVID-19 vaccine experience and perceptions. It is possible this may have selected for healthier people. However, survey dissemination did not select for people still experiencing COVID-19 symptoms, which may be a relative strength, as it may be more representative of people with SARDs who had COVID-19. Second, the results relied on self-report that may be inaccurate or subject to recall bias, particularly in those whose infection occurred remotely relative to survey response and in those with high SARD activity, features of which may overlap with COVID-19 symptoms. Third, selection bias related to illness severity (people who were severely affected with COVID-19 may have been less likely to respond) or location (most respondents were from the Americas and Europe) may affect generalisability. The survey was conducted in early 2021 and only 501/10 247 (4.9)% had test-confirmed COVID-19. Respondents may have been more likely to be previously uninfected and interested in COVID-19 prevention. When also including possible COVID-19 cases, the proportion that experienced COVID-19 was 913/10 247 (8.9%). However, the results may not be generalisable to contemporaneous populations with higher prevalence of COVID-19. Fourth, we did not gather data on specific symptoms that patients were experiencing; it is possible these were manifestations of their underlying SARD or unrelated to COVID-19. Fifth, we did not have comparator groups such as the general population with COVID-19 or people with SARDs who did not have COVID-19 to quantify the background rate of overlapping symptoms of SARDs such as fatigue, pain and dyspnoea. Our primary analysis only analysed test-confirmed cases, but some may have experienced COVID-19 without testing. These people with possible COVID-19 had slightly longer reported COVID-19 symptom duration and a higher proportion met the CDC criteria for prolonged symptom duration than those with test-confirmed COVID-19. This emphasises the need for future research on prolonged symptoms after infections. Finally, we only had cross-sectional data at time of survey without temporal data on relationships. For example, we were unable to examine associations of vaccination with persistent symptoms since it was not clear whether vaccine administration occurred before or after infection. People experiencing prolonged COVID-19 symptoms may have been more likely to pursue vaccination due to some reports that this could ameliorate symptoms.35–37
In conclusion, our study suggests that the majority of people with SARDs and COVID-19 may have symptom resolution by 15 days of onset. However, a subset may experience prolonged symptom duration and experience lengthy duration of symptoms. We found that the severity of acute COVID-19, older age and comorbidities may be associated with prolonged symptom duration. Conversely, those experiencing COVID-19 more recently appeared less likely to experience prolonged COVID-19 duration. Prospective studies are needed to investigate symptom duration after breakthrough infection, among those on specific immunosuppressive therapies and in contemporaneous settings, related to treatment and viral variants. Retrospective studies are also needed to investigate other health-related outcomes, such as clinical events, after acute COVID-19 among people with SARDs that could be performed using population-based and administrative datasets.
Acknowledgments
We wish to thank all patients who participated in the COVID-19 Global Rheumatology Alliance Vaccine Survey.
Footnotes
Twitter: @ebrheum, @SattuiSEMD, @pedrommcmachado, @philipcrobinson, @InitaBulina, @drdavidliew, @mugartegil
JH, JSi and JSp contributed equally.
Contributors: MD, KK, JL, MSP, ES, SES, JH, JSi and JSp contributed to data collection, data quality control, data analysis and interpretation. They drafted and revised the manuscript critically for important intellectual content and gave final approval of the version published. TTM, CH, MLa, MLe, GF, L-AT and LGR contributed to planning and data collection, reviewed the manuscript and provided important intellectual content. SB, WC, RG, PMM, PCR, PS, ZW and JY contributed to the acquisition, analysis and interpretation of the data. They drafted and revised the manuscript critically for important intellectual content and gave final approval of the version published. JSp, JSi and JH directed the work, designed the data collection methods and contributed to the analysis and interpretation of the data. They drafted and revised the manuscript critically for important intellectual content and gave final approval of the version to be published. MD, KK, JSi and JSp had full access to the data and verify the credibility of the underlying data. All authors have read, revised and approved this manuscript and final responsibility for the decision to submit for publication. JSp accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish.
Disclaimer: The views expressed here are those of the authors and participating members of the COVID-19 Global Rheumatology Alliance and do not necessarily represent the views of the American College of Rheumatology (ACR), the European Alliance of Associations for Rheumatology (EULAR), the UK National Health Service (NHS), the National Institute for Health Research (NIHR), the UK Department of Health, or any other organisation. The funders had no role in the decision to publish or preparation of this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard University, its affiliated academic health care centers, or the National Institutes of Health.
Competing interests: MP reports grants from AbbVie—SELECT-GCA Participating Center and AstraZeneca—MANDARA Participating Center; and consulting fees from Novartis, outside the submitted work. ES is a board member of the Canadian Arthritis Patient Alliance, a patient run, volunteer-based organisation whose activities are primarily supported by independent grants from pharmaceutical companies. SES reports research funding related to clinical trials from AstraZeneca (MANDARA) and is supported by the Vasculitis Clinical Research Consortium and Vasculitis Foundation, outside the submitted work. CH is a stockholder for Aurinia Pharmaceuticals; an Advisory Board member for Aurinia Pharmaceuticals, AstraZeneca Pharmaceuticals and UCB Pharmaceuticals; and reports consulting fees from AstraZeneca, UCB, Antidote and Aurinia Pharmaceuticals, outside the submitted work. MJL reports grants from American College of Rheumatology, during the conduct of the study and consulting fees from AbbVie, Amgen, Actelion, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Gilead, Johnson & Johnson, Mallinckrodt, Novartis, Pfizer, Roche, Sandoz, Sanofi, Sobi and Union Chimique Belge, outside the submitted work. SB reports non-branded consulting fees from AbbVie, Amgen, Horizon Pharma, Novartis and Pfizer outside the submitted work, and is a Pfizer employee as of September 2021. RG reports speaker honoraria from AbbVie New Zealand, Cornerstones and Janssen New Zealand; speaker honoraria and non-financial support Pfizer Australia; non-financial support from Janssen Australia and personal fees from Novartis (all <$A10 000) outside the submitted work. PMM reports consulting fees from AbbVie, Eli Lilly, Janssen, Novartis, Pfizer and Union Chimique Belge; and grants and consulting fees from Orphazyme, outside the submitted work. PCR reports personal fees from AbbVie, Gilead, Eli Lilly and Roche; grants and personal fees from Novartis, Union Chimique Belge, Janssen and Pfizer and non-financial support from Bristol Myers Squibb, outside the submitted work. ZSW reports grants from NIH, Bristol Myers Squibb and Principia/Sanofi; and personal fees from Viela Bio and MedPace, outside the submitted work. JY reports grants from NIH/NIAMS K24 during the conduct of the study and outside the submitted work, reports research grants from Gilead, BMS Foundation and AstraZeneca; consulting fees from Pfizer, AstraZeneca and Aurinia. MG-M reports consulting fees for BMS, BI, JNJ and Aurinia (all <$A10 000), outside the submitted work. RH reports grants from AbbVie, Amgen, Boehringer Ingleheim, Johnson & Johnson, Eli Lilly, Novartis, Pfizer and Union Chimique Belge, all paid to Spondylitis Association of America, and consultant fees from GlaxoSmithKline and Novartis, outside the submitted work. RH also owns stocks (<20 shares and representing <4% of personal investments) in AbbVie, Amgen, Bristol Myers Squibb, GlaxoSmithKline, Johnson & Johnson, Eli Lilly, Merck, Novartis, Pfizer, Teva and Union Chimique Belge. DA-R is a scientific advisor for and reports personal fees from GlaxoSmithKilne Mexico unrelated to this work. RC reports speaker fees from Janssen, Roche, Sanofi and AbbVie, outside the submitted work. AD-G reports grants from the Centers for Disease Control and Prevention, Rheumatology Research Foundation and Mayo Clinic, outside the submitted work. JAS has received consultant fees from Schipher, Crealta/Horizon, Medisys, Fidia, PK Med, Two Labs, Adept Field Solutions, Clinical Care options, Clearview healthcare partners, Putnam associates, Focus forward, Navigant consulting, Spherix, MedIQ, Jupiter Life Science, UBM, Trio Health, Medscape, WebMD and Practice Point communications; and the National Institutes of Health and the American College of Rheumatology. JAS has received institutional research support from Zimmer Biomet Holdings. JAS received food and beverage payments from Intuitive Surgical/Philips Electronics North America. JAS owns stock options in TPT Global Tech, Vaxart Pharmaceuticals, Atyu Biopharma, Adaptimmune Therapeutics, GeoVax Labs, Pieris Pharmaceuticals, Enzolytics, Seres Therapeutics, Tonix Pharmaceuticals Holding and Charlotte’s Web Holdings. JAS previously owned stock options in Amarin, Viking and Moderna pharmaceuticals. JAS is on the speaker’s bureau of Simply Speaking. JAS is a member of the executive of Outcomes Measures in Rheumatology (OMERACT), an organisation that develops outcome measures in rheumatology and receives arms-length funding from eight companies. JAS serves on the FDA Arthritis Advisory Committee. JAS is the chair of the Veterans Affairs Rheumatology Field Advisory Board (FAB). JAS is the editor and the Director of the University of Alabama at Birmingham (UAB) Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis. JAS previously served as a member of the following committees: member, the American College of Rheumatology's (ACR) Annual Meeting Planning Committee (AMPC) and Quality of Care Committees, the Chair of the ACR Meet-the-Professor, Workshop and Study Group Subcommittee and the co-chair of the ACR Criteria and Response Criteria subcommittee. MFU-G reports research grants from Pfizer and Janssen, unrelated to this work. JSH reports grants from and Rheumatology Research Alliance; consulting fees from Novartis, Pfizer and Biogen; and is a member of the Childhood Arthritis and Rheumatology Research Alliance (CARRA). JFS received research grant funding from the National Institutes of Health unrelated to this work (NIAMS R01 AR077103 and NIAID R01 AI154533). JSp is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grant numbers R01 AR077607, P30 AR070253 and P30 AR072577), the R. Bruce and Joan M. Mickey Research Scholar Fund, the Llura Gund Award for Rheumatoid Arthritis Research and Care and Bristol Myers Squibb; and personal fees for AbbVie, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum and Pfizer, unrelated to this work.
Patient and public involvement statement: Patient partners were involved in the development of the COVID-19 Global Rheumatology Alliance Vaccine Survey and this analysis.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Researchers interested in performing additional analyses from survey data are invited to submit proposals through the COVID-19 Global Rheumatology Alliance at rheum-covid.org. For approved projects, we will be able to provide summary tables and data analyses as requested. We do not currently have institutional review board approval to make the raw data available to other researchers.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by Boston Children’s Hospital: IRB-P00035062. Participants gave informed consent to participate in the study before taking part.
References
- 1.Conway R, Grimshaw AA, Konig MF, et al. SARS-CoV-2 infection and COVID-19 outcomes in rheumatic diseases: a systematic literature review and meta-analysis. Arthritis Rheumatol 2022;74:766–75. 10.1002/art.42030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hausmann JS, Kennedy K, Simard JF, et al. Immediate effect of the COVID-19 pandemic on patient health, health-care use, and behaviours: results from an international survey of people with rheumatic diseases. Lancet Rheumatol 2021;3:e707–14. 10.1016/S2665-9913(21)00175-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep 2021;11:16144. 10.1038/s41598-021-95565-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Proal AD, VanElzakker MB. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front Microbiol 2021;12:698169. 10.3389/fmicb.2021.698169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) . Long COVID or Post-COVID conditions, 2022. Available: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
- 6.Soriano JB, Murthy S, Marshall JC, et al. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis 2022;22:e102–7. 10.1016/S1473-3099(21)00703-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grainger R, Kim AHJ, Conway R, et al. COVID-19 in people with rheumatic diseases: risks, outcomes, treatment considerations. Nat Rev Rheumatol 2022;18:191–204. 10.1038/s41584-022-00755-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi B, Choudhary MC, Regan J, et al. Persistence and evolution of SARS-CoV-2 in an immunocompromised host. N Engl J Med 2020;383:2291–3. 10.1056/NEJMc2031364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choudhary MC, Crain CR, Qiu X, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) sequence characteristics of coronavirus disease 2019 (COVID-19) persistence and reinfection. Clin Infect Dis 2022;74:237–45. 10.1093/cid/ciab380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Iorio M, Cook CE, Vanni KMM, et al. DMARD disruption, rheumatic disease flare, and prolonged COVID-19 symptom duration after acute COVID-19 among patients with rheumatic disease: a prospective study. Semin Arthritis Rheum 2022;55:152025. 10.1016/j.semarthrit.2022.152025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sattui SE, Liew JW, Kennedy K, et al. Early experience of COVID-19 vaccination in adults with systemic rheumatic diseases: results from the COVID-19 global rheumatology alliance vaccine survey. RMD Open 2021;7:e001814. 10.1136/rmdopen-2021-001814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Putman M, Kennedy K, Sirotich E, et al. COVID-19 vaccine perceptions and uptake: results from the COVID-19 global rheumatology alliance vaccine survey. Lancet Rheumatol 2022;4:e237–40. 10.1016/S2665-9913(22)00001-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021;384:693–704. 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santos REA, da Silva MG, do Monte Silva MCB, et al. Onset and duration of symptoms of loss of smell/taste in patients with COVID-19: a systematic review. Am J Otolaryngol 2021;42:102889. 10.1016/j.amjoto.2020.102889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiss A, Jellingsø M, Sommer MOA. Spatial and temporal dynamics of SARS-CoV-2 in COVID-19 patients: a systematic review and meta-analysis. EBioMedicine 2020;58:102916. 10.1016/j.ebiom.2020.102916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niavarani A, Poustchi H, Shayanrad A, et al. Dynamics of the COVID-19 clinical findings and the serologic response. Front Microbiol 2021;12:743048. 10.3389/fmicb.2021.743048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lafarge A, Mabrouki A, Yvin E, et al. Coronavirus disease 2019 in immunocompromised patients: a comprehensive review of coronavirus disease 2019 in hematopoietic stem cell recipients. Curr Opin Crit Care 2022;28:83–9. 10.1097/MCC.0000000000000907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Purpura LJ, Chang M, Annavajhala MK, et al. Prolonged severe acute respiratory syndrome coronavirus 2 persistence, attenuated immunologic response, and viral evolution in a solid organ transplant patient. Am J Transplant 2022;22:649–53. 10.1111/ajt.16837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kute VB, Ray DS, Yadav DK, et al. A multicenter cohort study from India of 75 kidney transplants in recipients recovered after COVID-19. Transplantation 2021;105:1423–32. 10.1097/TP.0000000000003740 [DOI] [PubMed] [Google Scholar]
- 20.Chaudhry B, Didenko L, Chaudhry M, et al. Longest reported case of symptomatic COVID-19 reporting positive for over 230 days in an immunocompromised patient in the United States. SAGE Open Med Case Rep 2021;9:2050313X211040028:2050313X2110400. 10.1177/2050313X211040028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niyonkuru M, Pedersen RM, Assing K, et al. Prolonged viral shedding of SARS-CoV-2 in two immunocompromised patients, a case report. BMC Infect Dis 2021;21:743. 10.1186/s12879-021-06429-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang B, Fan J, Huang J, et al. Clinical and molecular characteristics of COVID-19 patients with persistent SARS-CoV-2 infection. Nat Commun 2021;12:3501. 10.1038/s41467-021-23621-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fernández-de-Las-Peñas C, Martín-Guerrero JD, Navarro-Pardo E, et al. The presence of rheumatological conditions is not a risk factor of long-term post-COVID symptoms after SARS-CoV-2 infection: a multicenter study. Clin Rheumatol 2022;41:585–6. 10.1007/s10067-021-05935-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barbhaiya M, Jannat-Khah D, Levine J. Risk factors for “Long Haul” COVID-19 in rheumatology outpatients in New York City [abstract]. Arthritis Rheumatol 2021;73. [Google Scholar]
- 25.Leon L, Perez-Sancristobal I, Madrid A, et al. Persistent post-discharge symptoms after COVID-19 in rheumatic and musculoskeletal diseases. Rheumatol Adv Pract 2022;6:rkac008. 10.1093/rap/rkac008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maglietta G, Diodati F, Puntoni M, et al. Prognostic factors for post-COVID-19 syndrome: a systematic review and meta-analysis. J Clin Med 2022;11. 10.3390/jcm11061541. [Epub ahead of print: 11 03 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Michelen M, Manoharan L, Elkheir N, et al. Characterising long COVID: a living systematic review. BMJ Glob Health 2021;6:e005427. 10.1136/bmjgh-2021-005427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kissler SM, Fauver JR, Mack C, et al. Viral dynamics of SARS-CoV-2 variants in vaccinated and unvaccinated persons. N Engl J Med 2021;385:2489–91. 10.1056/NEJMc2102507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prathipati KK, Mishra M, Rathod B, et al. Symptomatology and relationship between symptoms and duration among COVID-19 patients in a COVID-19 care hospital in central India. Cureus 2022;14:e21541. 10.7759/cureus.21541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Porru S, Spiteri G, Monaco MGL, et al. Post-vaccination SARS-CoV-2 infections among health workers at the university hospital of Verona, Italy: a retrospective cohort survey. Vaccines 2022;10. 10.3390/vaccines10020272. [Epub ahead of print: 10 02 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amanatidou E, Gkiouliava A, Pella E, et al. Breakthrough infections after COVID-19 vaccination: insights, perspectives and challenges. Metabol Open 2022;14:100180. 10.1016/j.metop.2022.100180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bergwerk M, Gonen T, Lustig Y, et al. Covid-19 breakthrough infections in vaccinated health care workers. N Engl J Med 2021;385:1474–84. 10.1056/NEJMoa2109072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takahashi K, Ishikane M, Ujiie M, et al. Duration of infectious virus shedding by SARS-CoV-2 omicron variant-Infected vaccinees. Emerg Infect Dis 2022;28:998–1001. 10.3201/eid2805.220197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dhillon RA, Qamar MA, Gilani JA, et al. The mystery of COVID-19 reinfections: a global systematic review and meta-analysis. Ann Med Surg 2021;72:103130. 10.1016/j.amsu.2021.103130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scherlinger M, Pijnenburg L, Chatelus E, et al. Effect of SARS-CoV-2 vaccination on symptoms from post-acute sequelae of COVID-19: results from the nationwide VAXILONG study. Vaccines 2021;10. 10.3390/vaccines10010046. [Epub ahead of print: 30 12 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wisnivesky JP, Govindarajulu U, Bagiella E, et al. Association of vaccination with the persistence of post-COVID symptoms. J Gen Intern Med 2022;37:1748–53. 10.1007/s11606-022-07465-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Massey D, Berrent D, Akrami A. Change in s ymptoms and immune response in people with post-acute sequelae of SARS-Cov-2 Infection (PASC) After SARS-Cov-2 Vaccination. medRxiv 2021:2021.07.21.21260391. 10.1101/2021.07.21.21260391 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2022-002587supp001.pdf (208.5KB, pdf)
Data Availability Statement
Data are available on reasonable request. Researchers interested in performing additional analyses from survey data are invited to submit proposals through the COVID-19 Global Rheumatology Alliance at rheum-covid.org. For approved projects, we will be able to provide summary tables and data analyses as requested. We do not currently have institutional review board approval to make the raw data available to other researchers.