Abstract
Background and Aims
Endoscopic therapies in the treatment of refractory GERD have largely been regarded as inferior as surgical intervention. Procedures such as the transoral endoscopic incisionless fundoplication (TIF), Stretta, and antireflux mucosectomy (ARMS) are less invasive but produce outcomes that are middling to lackluster, with many patients having to continue proton pump therapy without resolution of symptoms. Antireflux band mucosectomy (ARBM), in which the cardia is banded, may provide more effective relief. We present 4 patients with refractory GERD who did not opt for surgical intervention and were successfully treated with the ARBM procedure.
Methods
Four patients with GERD refractory to medical therapy underwent ARBM. Three patients had nonerosive esophagitis and 1 patient had erosive esophagitis. Two patients had hiatal hernias ≤2 cm. All underwent preprocedure and postprocedure pH bravo testing as well as follow-up EGD.
Results
All cases were completed successfully. All patients underwent a decrease in DeMeester score and acid exposure time. Procedure time ranged from 6 to 15 minutes. There were no adverse events. All patients were taken off proton pump inhibitor (PPI) therapy by 4 weeks postprocedure.
Conclusions
Four patients with refractory GERD who declined surgery underwent the ARBM procedure with technical success. All experienced significant decrease to complete resolution of symptoms. All patients were weaned off PPIs by 4 weeks postprocedure.
Abbreviations: ARBM, antireflux band mucosectomy; ARMS, antireflux mucosectomy; EGJ, esophagogastric junction; LES, lower esophageal sphincter; PPI, proton pump inhibitor; TIF, transoral endoscopic incisionless fundoplication
Video
Antireflux band mucosectomy procedure.
Introduction
GERD is one of the most prevalent digestive diseases, involving approximately 1 in 5 within the United States.1 Medical therapy and lifestyle modifications are highly effective for most patients with GERD. Despite this, refractory GERD affects 30% to 45% of patients. This subset of the patient population may require endoscopic or surgical approaches to achieve clinical resolution of symptoms.2,3 Endoscopic procedures tend to be less invasive and include transoral endoscopic incisionless fundoplication (TIF), Stretta, and antireflux mucosectomy (ARMS). Antireflux surgical techniques include Nissen’s fundoplication, which yields impressive clinical improvement. However, it is highly invasive and carries additional risks. Here, we showcase the antireflux band-assisted mucosectomy (ARBM) for the successful treatment of refractory GERD.
Case Description
Patient 1 is a 58-year-old man with a history of GERD who presented with acid regurgitation and nausea. No dysphagia was reported. He completed a barium esophagram confirming normal motility and found a small hiatal hernia. Preprocedure EGD visualized mucosal damage consistent with nonerosive esophagitis, hill grade 2 valve, and a small hiatal hernia <1 cm (Fig. 1). The pH bravo test off proton pump inhibitors (PPIs) was positive for reflux (DeMeester score 28.8, acid exposure time 7.4), and he had partial symptom improvement on maximal dose PPI twice daily. The patient was presented with both surgical and endoscopic options and declined surgical intervention. Multiple endoscopic therapies were offered, including TIF, ARMS, and ARBM. We also discussed that we believed the ARBM procedure would be safe owing to no active resection. The risk and benefits of all the procedures were discussed, and the patient decided to proceed with ARBM.
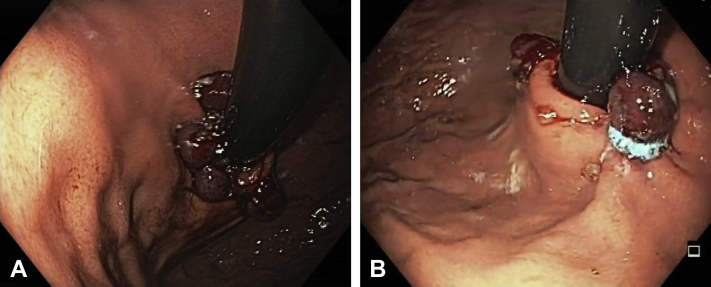
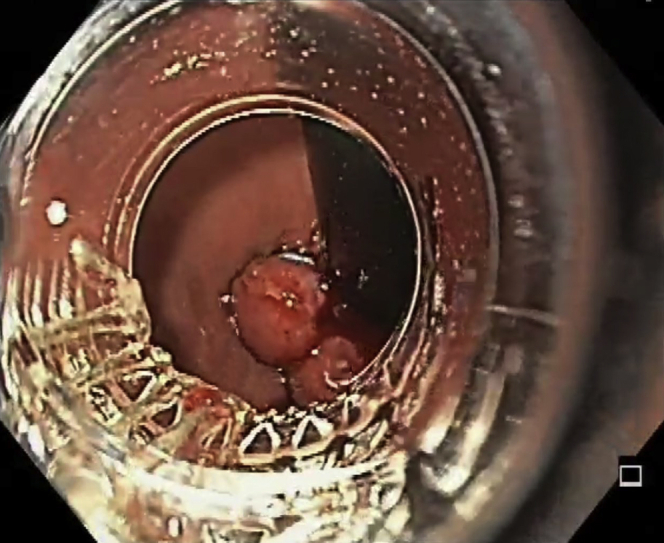
Figure 1.
A forward-viewing gastroscope was advanced to the esophagogastric junction, visualizing nonerosive esophagitis.
Procedure
An adult gastroscope was advanced to the lower esophageal sphincter (LES) and into the stomach. Next, the gastroscope was retroflexed to view the cardia and fundus. Then, band ligation with suction was applied parallel to the angle of His (Fig. 2). A total of 4 bands were positioned around the esophagogastric junction (EGJ) (Fig. 3). Once band application was complete, constriction of the EGJ was clearly displayed (Fig. 4A and B). There were no adverse events during and after the completion of the procedure (Video 1, available online at www.giejournal.org). The patient was discharged on the same day. He was weaned off his PPI 2 weeks after the procedure. At 3 months follow-up, the patient reported complete resolution of his symptoms. The repeat EGD with pH test was done at 3 months, demonstrating complete acid control postprocedure (DeMeester score 1.5, acid exposure time 0.4) (Fig. 5).
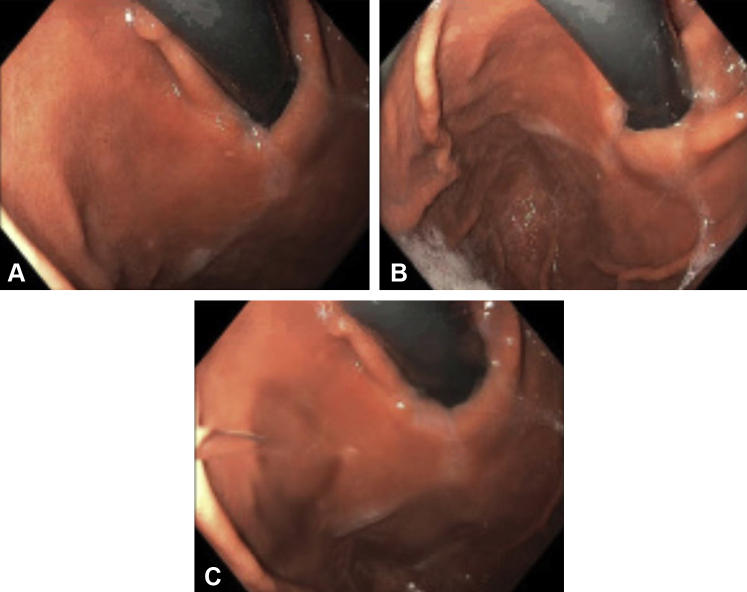
Figure 2.
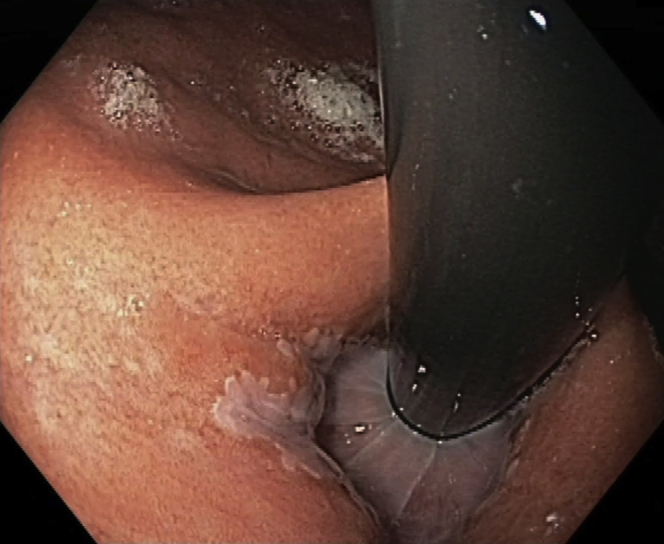
Band ligation by using suction occurred parallel to the angle of His.
Figure 3.
A total of 4 bands were placed around the esophagogastric junction.
Figure 4.
Narrowing of the esophagogastric junction was clearly demonstrated after the application of band ligation. A, View 1. B, View 2.
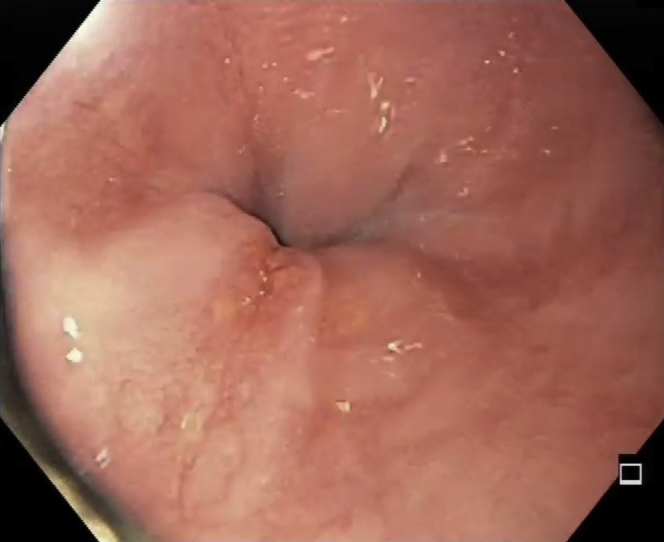
Figure 5.
Three-month follow-up with complete resolution of symptoms. A-C, Repeat EGD with pH bravo test found a significant reduction in reflux events.
Outcomes
The ARBM procedure was performed in a total of 4 patients. All procedures were technically successful. All patients had a significant decrease in their DeMeester scores and acid exposure time. No adverse events occurred before, during, or after the procedure. All patients were able to stop PPIs by 4 weeks postprocedure. Demographic and clinical data for all patients are presented in Table 1.
Table 1.
Clinical and demographic data of the 4 patients who underwent the antireflux band mucosectomy procedure
|
Pre-ARBM | |||||||
|---|---|---|---|---|---|---|---|
| Patient | Age/sex | Esophagitis (Y or N) | Esophagitis grade (A, B, C, D) | Hiatal hernia (Y or N) | Hiatal hernia size (cm) | DeMeester score | % Time pH < 4 |
| 1 | 58/M | N | NA | Y | <1 | 28 | 7.4 |
| 2 | 70/F | N | NA | N | 0 | 33 | 25 |
| 3 | 65/F | N | NA | N | 0 | 26 | 33 |
| 4 | 48/M | Y | A | Y | 2 | 45 | 55 |
| Post-ARBM | |||||||
| Patient | Age/sex | Esophagitis (Y or N) | Esophagitis grade (A, B, C, D) | Hiatal hernia (Y or N) | Hiatal hernia size (cm) | DeMeester score | % Time pH < 4 |
| 1 | 58/M | N | NA | Y | <1 | 1.5 | 0.4 |
| 2 | 70/F | N | NA | N | 0 | 10 | 3 |
| 3 | 65/F | N | NA | N | 0 | 8 | 5 |
| 4 | 48/M | Y | A | Y | 2 | 11 | 9 |
| ARBM procedure | |||||||
| Patient | Age/sex | Procedure technical success (Y or N) | Number of bands deployed | Procedure time (minutes) | Periprocedural AEs | Immediate AEs (0-24 hours) | Delayed AEs (24+ hours) |
| 1 | 58/M | Y | 4 | 6 | No | No | No |
| 2 | 70/F | Y | 6 | 12 | No | No | No |
| 3 | 65/F | Y | 6 | 14 | No | No | No |
| 4 | 48/M | Y | 6 | 15 | No | No | No |
AEs, Adverse events; ARBM, antireflux band mucosectomy; F, female; M, male; N, no; NA, not applicable; Y, yes.
Discussion
Refractory GERD can significantly impair the quality of life.4,5 While Nissen’s fundoplication is an excellent option for these patients, it is an invasive procedure with side effects and can significantly impair the venting of swallowed air.6 Endoscopic therapies such as TIF have relatively few side effects, but their effectiveness can be inconsistent. One study reported that only 39% of patients could discontinue PPI use post-TIF.7 The Stretta procedure is thought to increase the LES tone through radiofrequency ablation to induce scarring and fibrosis. Still, a recent metanalysis of 4 randomized controlled trials determined there was no meaningful change in LES pressure. No statistical improvement in stopping PPIs and GERD symptom scores was found.6,8 ARMS uses piecemeal mucosectomy with or without band ligation to cause scarring and fibrosis, narrowing the EGJ. However, average procedure times can be lengthy, ranging from 35 to 76 minutes.9 Our proposed technique avoids the active resection portion of the procedure in favor of circumferential band placement around the EGJ. The band placement narrows the EGJ through the constriction of the mucosa by using the exact mechanisms as ARMS. Furthermore, both ARMS and ARBM resect/band the cardia. The cardia naturally retroflexes with the valve, which facilitates banding along the valve and cardia. After each band is placed, we evaluate for valve tightening; if it is observed, we cease band placement. We only band 280 to 300 degrees along the cardia. Based on earlier ARMS data, complete circumferential banding may lead to high-grade strictures. The risk of stricture is thought to be increased when resection takes place in the esophagus.10 The lack of active resection in ARBM is speculated to increase its safety profile with a reduced risk of bleeding and perforation. Additionally, this procedure was completed in 6 minutes, showcasing its technical simplicity. The ARBM procedure should be considered in patients who decline surgery and have a hiatal hernia <2 cm, a hill grade ≤2, and an abnormal pH study with symptomatic reflux. The efficacy, safety, and speed of the ARBM will need to be evaluated in future studies.
ARBM is a novel minimally invasive endoscopic intervention that only uses band ligation and therefore has the potential to be a safer, faster, and less technically challenging alternative compared with other endoscopic and surgical interventions.
Disclosure
Dr Nieto is a consultant for Boston Scientific. All other authors disclosed no financial relationships.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Nieto at drjnieto@yahoo.com.
Supplementary data
Antireflux band mucosectomy procedure.
References
- 1.Peery A.F., Crockett S.D., Barritt A.S., et al. Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology. 2015;149:1731–1741.e3. doi: 10.1053/j.gastro.2015.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fass R. Therapeutic options for refractory gastroesophageal reflux disease. J Gastroenterol Hepatol. 2012;27:3–7. doi: 10.1111/j.1440-1746.2012.07064.x. [DOI] [PubMed] [Google Scholar]
- 3.Delshad S.D., Almario C.V., Chey W.D., et al. Prevalence of gastroesophageal reflux disease and proton pump inhibitor-refractory symptoms. Gastroenterology. 2020;158:1250–1261.e2. doi: 10.1053/j.gastro.2019.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang X.J., Jiang H.M., Hou X.H., et al. Anxiety and depression in patients with gastroesophageal reflux disease and their effect on quality of life. World J Gastroenterol. 2015;21:4302–4309. doi: 10.3748/wjg.v21.i14.4302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mizuki A., Tatemichi M., Sakakibara T., et al. A multicenter, randomized, open-label trial: efficacy of once-daily versus twice-daily double-dose rabeprazole on refractory gastroesophageal reflux disease-related symptoms and quality of life. Curr Ther Res Clin Exp. 2016;79:1–7. doi: 10.1016/j.curtheres.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganz R.A. A review of new surgical and endoscopic therapies for gastroesophageal reflux disease. Gastroenterol Hepatol (N Y) 2016;12:424–431. [PMC free article] [PubMed] [Google Scholar]
- 7.Witteman B.P.L., Conchillo J.M., Rinsma N.F., et al. Randomized controlled trial of transoral incisionless fundoplication vs. proton pump inhibitors for treatment of gastroesophageal reflux disease. Am J Gastroenterol. 2015;110:531–542. doi: 10.1038/ajg.2015.28. [DOI] [PubMed] [Google Scholar]
- 8.Lipka S., Kumar A., Richter J.E. No evidence for efficacy of radiofrequency ablation for treatment of gastroesophageal reflux disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2015;13:1058–1067.e1. doi: 10.1016/j.cgh.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Monino L., Gonzalez J.M., Vitton V., et al. Anti-reflux mucosectomy with band ligation in the treatment of refractory gastroesophageal reflux disease. Endoscopy. 2019;51:E215–E216. doi: 10.1055/a-0875-3479. [DOI] [PubMed] [Google Scholar]
- 10.Inoue H., Ito H., Ikeda H., et al. Anti-reflux mucosectomy for gastroesophageal reflux disease in the absence of hiatus hernia: a pilot study. Ann Gastroenterol. 2014;27:346–351. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Antireflux band mucosectomy procedure.
Antireflux band mucosectomy procedure.