Abstract
Purpose:
Antibiotics are seldom necessary to treat acute conjunctivitis. We assessed how frequently patients who are newly diagnosed with acute conjunctivitis fill prescriptions for topical antibiotics and factors associated with antibiotic prescription fills.
Design:
Retrospective observational cohort study.
Participants:
340372 enrollees in a large nationwide US managed care network who were newly diagnosed with acute conjunctivitis during 2001–2014.
Methods:
We identified all enrollees diagnosed with acute conjunctivitis (International Classification of Diseases, 9th Revision codes 372.00, 372.30, or 077.3). We calculated the proportion of enrollees with newly diagnosed acute conjunctivitis who filled ≥1 topical antibiotic prescription within 14 days of initial diagnosis. Multivariable logistic regression assessed sociodemographic, medical, and other factors associated with antibiotic prescription fills for acute conjunctivitis. Geographic variation in prescription fills was also studied.
Main Outcome Measures:
Odds ratios (ORs) with 95% confidence intervals (CIs) for filling an antibiotic prescription for acute conjunctivitis.
Results:
Among 340372 enrollees with acute conjunctivitis, 198462 (58%) filled ≥1 topical antibiotic prescription and 38774 filled prescriptions for antibiotic-corticosteroid combination products. Compared to whites, blacks (OR:0.89, CI:0.86–0.92) and Latinos (OR:0.83, CI:0.81–0.86) had lower odds of filling antibiotic prescriptions. More affluent and educated enrollees had higher odds of filling antibiotic prescriptions compared to those with lesser affluence and education (p<0.05 for all). Compared to persons initially diagnosed with acute conjunctivitis by ophthalmologists, enrollees had considerably higher odds of antibiotic prescription fills if first diagnosed by optometrists (OR:1.26, CI:1.21–1.31), urgent care physicians (OR:3.29, CI:3.17–3.41), internists (OR:2.79, CI:2.69–2.90), pediatricians (OR:2.27, CI:2.13–2.43), or family practitioners (OR:2.46, CI:2.37–2.55). Antibiotic prescription fills did not differ for persons with risk factors for developing serious infections, such as contact lens wearers (p=0.21) or those with HIV/AIDS (p=0.60) relative to others without these conditions.
Conclusion:
Nearly 60% of enrollees in this managed care network filled antibiotic prescriptions for acute conjunctivitis, and 1 of every 5 antibiotic users filled prescriptions for antibiotic-corticosteroids which are contraindicated for acute conjunctivitis. These potentially harmful practices may prolong infection duration, promote antibiotic resistance, and increase costs. Antibiotic fills appear to be driven more by sociodemographic factors and type of provider diagnosing the enrollee than medical indication.
Precis
Nearly 60% of privately insured US patients with newly diagnosed acute conjunctivitis filled topical antibiotic prescriptions soon after diagnosis. Antibiotic use was associated more with demographics, geography, and healthcare provider type than with medical indications.
INTRODUCTION
Acute conjunctivitis is one of the most common ocular conditions encountered in general medical practice, affecting 6 million persons in the United States each year.1 Approximately one half of all eye-related diagnoses seen in primary care offices2 and nearly one third of all emergency department visits for ocular problems are for conjunctivitis.3 Unlike other common ocular conditions such as refractive error or cataract, most cases of acute conjunctivitis are diagnosed and managed by non-eye care providers rather than ophthalmologists and optometrists.
Accurate differentiation between viral, bacterial, allergic, and other causes of acute conjunctivitis can be challenging because all these etiologies can present with similar clinical features. However, since acute conjunctivitis is often self-limiting, the majority of patients with this condition do not require topical antibiotic therapy.3 It is estimated that over 60% of patients with acute conjunctivitis have adenovirus or other viral infections4,5 which do not respond to antibiotics.3 Allergic conjunctivitis is also quite common and does not respond to antibiotics. Bacterial infections comprise a much smaller proportion of acute conjunctivitis cases. These cases are usually mild and self-limiting, often resolving within 7–14 days without antibiotic therapy.6 Although topical antibiotics may hasten resolution of symptoms among persons with bacterial conjunctivitis,6 this benefit must be weighed against the risk of ocular surface toxicity,3 antibiotic resistance,7,8 and the cost associated with their use.1 Topical corticosteroids are contraindicated in most cases of acute conjunctivitis because they can prolong adenoviral infections, worsen underlying ocular herpes simplex virus infections, and if taken for prolonged periods of time can increase the risk of cataract and glaucoma.3
In the US, researchers have determined that nearly one-third of outpatient antibiotic prescriptions for common viral or mild bacterial conditions such as sinusitis, influenza, and pharyngitis are unnecessary or inappropriate, representing an opportunity to improve patient safety and conserve health care resources.9 Like these other conditions, acute conjunctivitis is also very common and seldom requires antibiotics. In 2013, as part of the nationwide “Choosing Wisely” initiative to reduce wasteful or unnecessary medical testing and treatment, the American Academy of Ophthalmology recommended avoiding antibiotic prescriptions for viral conjunctivitis and deferring immediate antibiotic therapy when the etiology of conjunctivitis is unknown.10 To our knowledge, no prior study has assessed antibiotic use for acute conjunctivitis among a large, diverse segment of the US population. We assessed topical antibiotic prescription fills for acute conjunctivitis among enrollees in a large US managed care network, identified factors associated with antibiotic prescription fills for this condition, and explored how this practice varies among communities throughout the country.
METHODS
Data Source
The Clinformatics DataMart database (OptumInsight, Eden Prairie, MN) contains de-identified records of all beneficiaries in a large nationwide managed care network. We had access to data for all enrollees with any form of eye care from January 1, 2001 to December 31, 2014. This subset comprises enrollees who had ≥1 International Classification of Diseases (ICD-9-CM) codes for any eye-related diagnosis (360–379.9) and Current Procedural Terminology (CPT-4®) codes for any eye-related visits, and diagnostic or therapeutic procedures (65091–68899 or 92002–92499) during their time in the plan. We had access to enrollees’ medical claims including ICD-9-CM codes for all ocular and non-ocular conditions. The Clinformatics Data Mart database also contains sociodemographic information (age, sex, race, annual income, education level) of each enrollee. For every clinical encounter, the type of health care provider who cared for the enrollee was also captured. In addition, the database contains details about all outpatient medication prescriptions filled including the date of the prescription fill and the type and quantity of medication filled. All enrollees were fully enrolled in the pharmacy plan during their entire medical plan enrollment. This database has been used to study patients with other ocular diseases.11,12 The University of Michigan Institutional Review Board approved this study which uses de-identified data.
Eligibility criteria
Eligible enrollees were those who had been diagnosed with acute conjunctivitis based on the following ICD-9-CM codes: 372.00, 372.30, or 077.3. We also required all eligible persons to be continuously enrolled in the managed care plan for at least 4 years preceding and 90 days following their initial acute conjunctivitis diagnosis. Since appropriate management of first-time episodes of acute conjunctivitis often differs markedly from management of recurrent, chronic, non-infectious, hospital-associated, or postoperative conjunctivitis, we excluded enrollees with any prior diagnosis of chronic conjunctivitis (ICD-9-CM code 372.1), inpatient hospitalization at the time of the initial acute conjunctivitis diagnosis, or records of intraocular surgery within 90 days of the initial acute conjunctivitis diagnosis. We also excluded enrollees with any previous diagnosis of acute conjunctivitis in the 4 years preceding their initial acute conjunctivitis diagnosis to help exclude persons with recurrent or chronic conjunctivitis.
Outcomes
The primary outcome of interest was the proportion of persons with newly diagnosed acute conjunctivitis who filled prescriptions for topical antibiotics within 14 days of their initial diagnosis. We did not consider oral, intravenous, or other routes of antibiotic administration, since these routes of administration are rarely used to treat conjunctivitis and are likely capturing antibiotic use for other infections. We examined all major classes of topical ophthalmic antibiotics including fluoroquinolones, macrolides, aminoglycosides, sulfonamides, bacitracin, and polymyxins (Table 1). We also examined prescription fills for antibiotic-corticosteroid combination products. Some enrollees filled prescriptions for multiple antibiotic classes during the 14 day period of interest. In addition, we calculated the proportion of enrollees filling prescriptions for any of these classes of antibiotics stratified by the type of health care provider who made the initial conjunctivitis diagnosis: ophthalmologist, optometrist, internal medicine physician, family practice physician, pediatrician, urgent care physician, or unspecified health care provider.
Table 1.
Topical Antibiotic Classes
| Antibiotic | Number and % of patients* |
|---|---|
|
| |
| Fluoroquinolones | 65994 (33%) |
| Besifloxacin | |
| Ciprofloxacin | |
| Gatifloxacin | |
| Levofloxacin | |
| Moxifloxacin | |
| Ofloxacin | |
|
| |
| Aminoglycosides | 22651 (11%) |
| Gentamycin | |
| Tobramycin | |
|
| |
| Polymyxins | 31070 (16%) |
| Polymyxin/Bacitracin | |
| Polymycin/Bacitracin/Neomycin | |
| Polymyxin/Neomycin/Gramicidin | |
| Polymyxin/Trimethoprim | |
|
| |
| Sulfonamides | 14463 (7%) |
| Sulfacetamide | |
|
| |
| Macrolides | 34815 (18%) |
| Erythromycin | |
| Azithromycin | |
|
| |
| Bacitracin | 606 (0.3%) |
| Bacitracin | |
|
| |
| Antibiotic-corticosteroid combinations | 38774 (20%) |
| Polymycin/Neomycin/Bacitracin/Hydrocortisone | |
| Polymyxin/Neomycin/Dexamethasone | |
| Polymyxin/Neomycin/Hydrocortisone | |
| Sulfacetamide/Prednisolone | |
| Tobramycin/Dexamethasone | |
| Tobramycin/Loprednol | |
Percentage of patients with newly diagnosed acute conjunctivitis who filled >1 prescriptions for topical antibiotics belonging to each antibiotic category within 14 days of initial diagnosis. Some patients may have filled prescriptions for more than one agent in a given class or agents from more than 1 class during the 14 day period so the total number of prescriptions filled does not equal the total number of patients who filled prescriptions.
Statistical analysis
Data analyses were performed using SAS software version 9.4 (SAS, Inc., Cary, NC). Characteristics of the study population were summarized using means and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. Differences in continuous variables were assessed using the two-sample t-test. Differences in categorical variables were assessed using the chi square test. Results with p<0.05 were considered statistically significant.
Factors Associated with Filling Prescriptions for Antibiotics for Acute Conjunctivitis
Multivariable logistic regression was used to assess factors associated with filling ≥1 prescription for topical antibiotics for acute conjunctivitis. In the model, the dependent variable was ≥1 antibiotic prescription fill within 14 days of the enrollee’s initial acute conjunctivitis diagnosis. Covariates of interest included age at the time of acute conjunctivitis diagnosis, sex, race/ethnicity, annual income, education level, presence of comorbid diabetes mellitus (DM), human immunodeficiency virus (HIV) or acquired immune deficiency syndrome (AIDS), contact lens use, calendar year of initial acute conjunctivitis diagnosis, and the type of health care provider who first diagnosed the enrollee with acute conjunctivitis. Enrollees were categorized as not having DM, having DM without any record of end-organ damage from this condition, or having DM with evidence of end-organ damage such as diabetic nephropathy, neuropathy, or retinopathy.
Geographic Variation in Prescription Fills of Topical Antibiotics for Acute Conjunctivitis
To evaluate geographic variation in topical antibiotic prescription fills for acute conjunctivitis, we divided the United States into 306 hospital referral regions (HRRs) according to established methods developed by investigators at Dartmouth University.13 Briefly, HRRs represent regional health care markets for tertiary medical care14 and have been used extensively to study geographic variation in medical service utilization.15 Each enrollee was assigned a given HRR based on his or her current zip code of residence. For all HRRs that had 20 or more enrollees with acute conjunctivitis, we calculated the proportion of persons with newly diagnosed acute conjunctivitis who filled a prescription for a topical antibiotic within 14 days of initial diagnosis. Proportions were divided into quintiles and plotted on a map of the United States using ArcGIS software (Esri, Inc., Redlands, CA).
RESULTS
A total of 340372 enrollees with newly-diagnosed acute conjunctivitis met the study eligibility criteria. The mean ± SD age of the study sample at the time of initial conjunctivitis diagnosis was 38 ± 22 years old. The study sample consisted of 197926 (58%) females and the racial/ethnic composition included 250891 (78%) whites, 28574 (9%) blacks, 31471 (10%) Latinos, and 12102 (4%) Asians. Eligible enrollees were continuously enrolled in the plan for a mean ± SD of 8.8 ± 2.7 years. Among the 340372 persons with newly diagnosed acute conjunctivitis, 198462 enrollees (58%) filled ≥1 prescriptions for topical antibiotics within 14 days of their initial diagnosis. Antibiotic fills in a given calendar year ranged from a low of 51% in 2013–2014 to a high of 62% in 2007–2008, with no clear trend across the study period. Compared to enrollees who did not fill prescriptions, those who filled antibiotic prescriptions were younger (35 ± 20 years for those filling prescriptions versus 43 ± 25 years for those who did not), had higher incomes, and were more educated (p<0.001 for all comparisons). Risk factors for more serious bacterial infections were either similar between the two groups or more prevalent among enrollees not filling antibiotic prescriptions. Prevalence of contact lens wear (p=0.48) and HIV/AIDS (p=0.33) were similar between the two groups, while enrollees not filling antibiotic prescriptions had a higher prevalence of DM than enrollees filling prescriptions (10.9% versus 8.6% for DM without end-organ damage, 6.6% versus 2.9% for DM with end-organ damage, p<0.001). (Table 2)
Table 2.
Characteristics of Enrollees with Newly Diagnosed Acute Conjunctivitis Who Did and Did Not Fill Antibiotic Prescriptions
| Antibiotic prescription fill within 14 days of initial acute conjunctivitis diagnosis | |||||||
|---|---|---|---|---|---|---|---|
| No | Yes | Total | P-value* | ||||
| N | % | N | % | N | % | ||
| Total | 141910 | 41.7 | 198462 | 58.3 | 340372 | 100% | |
| Age at conjunctivitis diagnosis | <0.0001 | ||||||
| 0–4 years | 1724 | 1.2 | 2840 | 1.4 | 4564 | 1.3 | |
| 5–12 years | 21685 | 15.3 | 34046 | 17.2 | 55731 | 16.4 | |
| 13–18 years | 13015 | 9.2 | 21849 | 11.0 | 34864 | 10.2 | |
| 19–35 years | 20592 | 14.5 | 37589 | 18.9 | 58181 | 17.1 | |
| 36–65 years | 56392 | 39.7 | 95190 | 48.0 | 151582 | 44.5 | |
| ≥ 66 years | 28502 | 20.1 | 6948 | 3.5 | 35450 | 10.4 | |
| Year of conjunctivitis diagnosis | <0.0001 | ||||||
| 2005–2006 | 23887 | 16.8 | 36340 | 18.3 | 60227 | 17.7 | |
| 2007–2008 | 22838 | 16.1 | 38368 | 19.3 | 61206 | 18.0 | |
| 2009–2010 | 27432 | 19.3 | 40456 | 20.4 | 67888 | 19.9 | |
| 2011–2012 | 35152 | 24.8 | 49178 | 24.8 | 84330 | 24.8 | |
| 2013–2014 | 32601 | 23.0 | 34120 | 17.2 | 66721 | 19.6 | |
| Sex | 0.04 | ||||||
| Male | 59102 | 41.6 | 83344 | 42.0 | 142446 | 41.9 | |
| Female | 82808 | 58.4 | 115118 | 58.0 | 197926 | 58.1 | |
| Race | <0.0001 | ||||||
| White | 101868 | 75.8 | 149023 | 79.0 | 250891 | 77.7 | |
| Black | 12634 | 9.4 | 15940 | 8.5 | 28574 | 8.8 | |
| Latino | 14247 | 10.6 | 17224 | 9.1 | 31471 | 9.7 | |
| Asian | 5663 | 4.2 | 6439 | 3.4 | 12102 | 3.7 | |
| Education level | <0.0001 | ||||||
| Less than high school | 785 | 0.6 | 659 | 0.3 | 1444 | 0.4 | |
| High school diploma | 32699 | 2.3 | 42246 | 21.5 | 74945 | 22.3 | |
| Some college | 74638 | 53.3 | 107129 | 54.5 | 181767 | 54.0 | |
| Bachelor’s degree or more | 31958 | 22.8 | 46502 | 23.7 | 78460 | 23.3 | |
| Annual income (USD) | <0.0001 | ||||||
| <$40,000 | 18258 | 16.3 | 13210 | 8.4 | 31468 | 11.7 | |
| $40,000 to <$60,000 | 14302 | 12.7 | 16990 | 10.9 | 31292 | 11.6 | |
| $60,000 to <$100,000 | 27002 | 24.0 | 39672 | 25.4 | 66674 | 24.8 | |
| ≥$100,000 | 52737 | 47.0 | 86461 | 55.3 | 139198 | 51.8 | |
| Contact lens wear | 1499 | 1.1 | 2047 | 1.0 | 3546 | 1.0 | 0.48 |
| Diabetes mellitus † | <0.0001 | ||||||
| None | 117058 | 82.5 | 175695 | 88.5 | 292753 | 86.0 | |
| Uncomplicated | 15456 | 10.9 | 17048 | 8.6 | 32504 | 9.5 | |
| Complicated | 9396 | 6.6 | 5719 | 2.9 | 15115 | 4.4 | |
| HIV/AIDS | 465 | 0.3 | 689 | 0.3 | 1154 | 0.3 | 0.33 |
| Diagnosing health care provider | <0.0001 | ||||||
| Ophthalmologist | 18897 | 13.3 | 10660 | 5.4 | 29557 | 8.7 | |
| Optometrist | 15556 | 11.0 | 12246 | 6.2 | 27802 | 8.2 | |
| Pediatrician | 2972 | 2.1 | 4227 | 2.1 | 7199 | 2.1 | |
| Family practice physician | 19642 | 13.8 | 24306 | 12.2 | 43948 | 12.9 | |
| Internist | 18031 | 12.7 | 24923 | 12.6 | 42954 | 12.6 | |
| Urgent care physician | 14006 | 9.9 | 29441 | 14.8 | 43447 | 12.8 | |
| Other provider | 52806 | 37.2 | 92659 | 46.7 | 145465 | 42.7 | |
All values presented as N (column %) unless otherwise specified.
P values calculated using the chi square test.
Race missing for 17334 enrollees, education level missing for 3756 enrollees, annual income variable missing for 71740 enrollees.
Diabetes mellitus status: None; Uncomplicated (diabetes mellitus without end-organ damage); Complicated (diabetes mellitus with end-organ damage such as neuropathy, nephropathy, or retinopathy)
HIV/AIDS: Human immunodeficiency virus / Acquired immune deficiency syndrome.
USD: United States dollars.
Among the 198462 persons who filled ≥1 prescriptions for topical antibiotics, 194534 individuals (98%) filled prescriptions within 3 days of the initial diagnosis. The most commonly filled prescriptions included fluoroquinolones (N=65994; 33%), macrolides (N=34815; 18%), polymyxins (N=31070; 16%), aminoglycosides (N=22651; 11%), sulfonamides (N=14463; 7%), and bacitracin (N=606; 0.3%). Among persons who filled antibiotic prescriptions, 20% (N=38774) filled prescriptions for antibiotic-corticosteroid combination agents. (Table 1)
Eighty-three percent of the enrollees were first diagnosed with acute conjunctivitis by other health care providers besides ophthalmologists or optometrists. Antibiotic fills varied substantially for persons diagnosed by different health care providers (p<0.001). Persons first diagnosed with acute conjunctivitis by ophthalmologists had the lowest percentage of antibiotic fills (36%), with higher proportions of antibiotic fills among persons first diagnosed by optometrists (44%), family practice physicians (55%), internal medicine physicians (58%), pediatricians (59%), urgent care physicians (68%), or other health care providers (64%) (Figure 1). The proportion of patients initially diagnosed with conjunctivitis by ophthalmologists, optometrists, and all other healthcare providers who received combination antibiotic corticosteroid products during the 14 days after initial diagnosis was 23%, 30%, and 8%, respectively.
Figure 1.
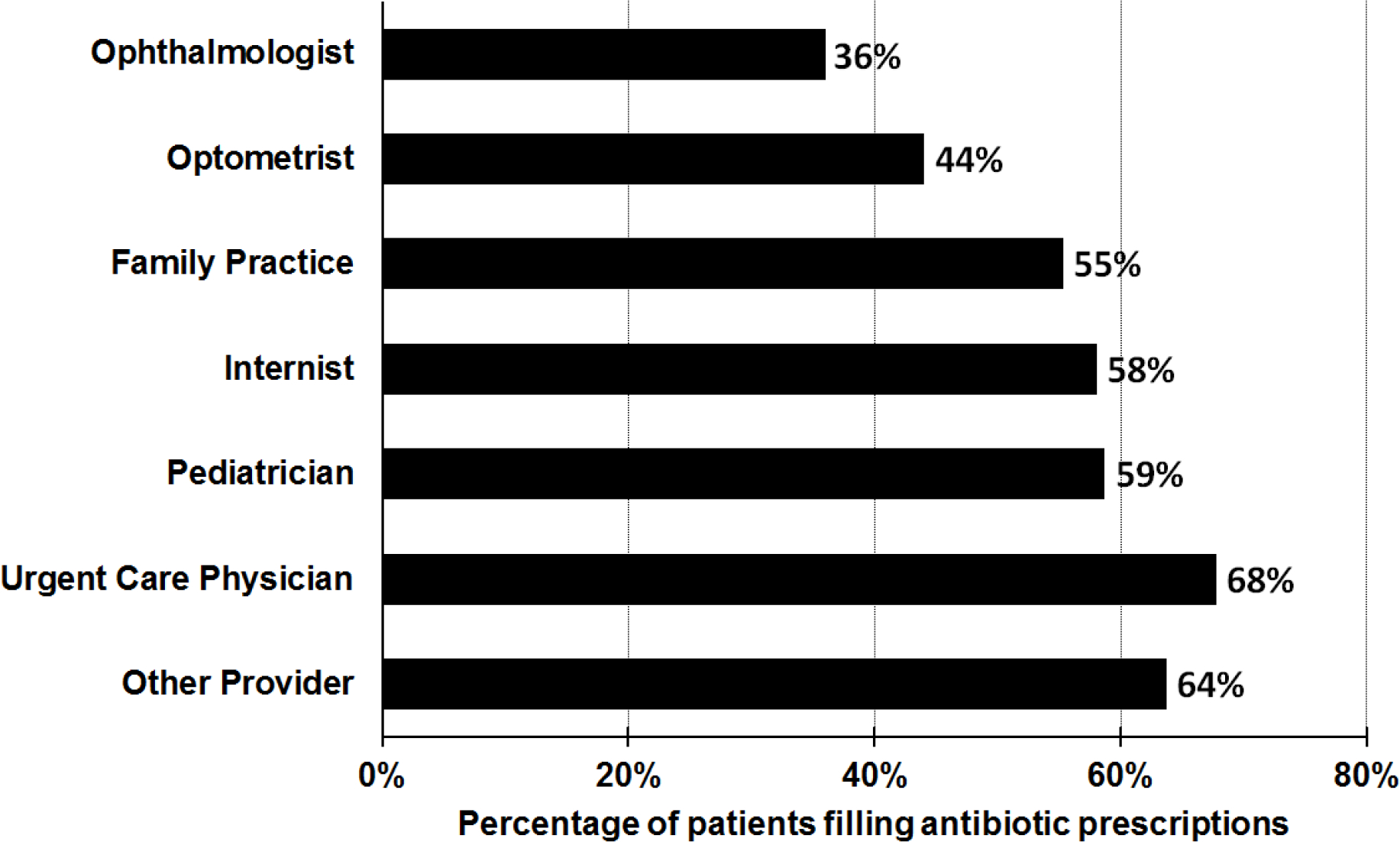
Proportion of Enrollees Filling Topical Antibiotic Prescriptions for Newly-Diagnosed Acute Conjunctivitis, by Type of Health Care Provider Who First Diagnosed the Condition
After adjustment for potential confounding factors, the multivariable model showed that enrollees age 19–35 years old at time of diagnosis had higher odds of filling prescriptions for antibiotics compared to younger enrollees (p<0.001 for all comparisons). Enrollees eligible for Medicare Advantage plans (age ≥66) were substantially less likely to fill prescriptions for topical antibiotics (OR:0.16, CI:0.16–0.17) compared to persons age 19–35 years old. Compared to whites, blacks had 11% lower odds (OR 0.89, CI:0.86–0.92), Latinos had 17% lower odds (OR:0.83, CI:0.81–0.86), and Asians had 27% lower odds (OR :0.73, CI:0.70–0.76) of filling prescriptions for acute conjunctivitis. College educated enrollees were 16% more likely to fill an antibiotic prescription relative to others who had not completed high school (OR:1.16, CI:1.01–1.35). Persons earning ≥$100,000 United States dollars (USD) per year were 35% more likely to fill an antibiotic prescription than those earning <$40,000/year (OR:1.35, CI:1.31–1.39). Contact lens wearers (p=0.21) and enrollees with HIV/AIDS (p=0.60) were no more likely to fill antibiotic prescriptions compared to persons without these conditions. Compared to enrollees without DM, those with DM without end-organ damage were no more likely to fill prescriptions for antibiotics (OR:0.99, CI:0.96–1.02), while enrollees with end-organ damage from DM were 20% less likely to fill a prescription for antibiotics (OR:0.80, CI: 0.77–0.84). Compared to enrollees first diagnosed with acute conjunctivitis by an ophthalmologist, those diagnosed by an optometrist had 26% increased odds of filling an antibiotic prescription (OR:1.26, CI:1.21–1.31). Moreover, compared to enrollees diagnosed with acute conjunctivitis by an ophthalmologist, enrollees had two- to three-fold higher odds of filling prescriptions for topical antibiotics if they were initially diagnosed by urgent care physicians (OR:3.29, CI:3.17–3.41), internists (OR:2.79, CI:2.69–2.90), pediatricians (OR:2.27, CI:2.13–2.43), or family practitioners (OR:2.46, CI:2.37–2.55) (Table 3).
Table 3.
Adjusted Odds Ratios for Filling an Antibiotic Prescription for Acute Conjunctivitis Within 14 Days of an Initial Diagnosis
| Value | OR (95% CI)a | p value |
|---|---|---|
| Age at conjunctivitis diagnosis | ||
| 0–4 years | 0.77 (0.71, 0.83) | < 0.0001 |
| 5–12 years | 0.76 (0.74, 0.78) | < 0.0001 |
| 13–18 years | 0.87 (0.84, 0.90) | < 0.0001 |
| 19–35 years | REF | |
| 36–65 years | 0.98 (0.96, 1.01) | 0.18 |
| ≥ 66 years | 0.16 (0.16, 0.17) | < 0.0001 |
| Year of conjunctivitis diagnosis | 0.95 (0.95, 0.96) | < 0.0001 |
| Sex | ||
| Male | REF | |
| Female | 1.02 (1.01, 1.04) | 0.01 |
| Race | ||
| White | REF | |
| Black | 0.89 (0.86, 0.92) | < 0.0001 |
| Latino | 0.83 (0.81, 0.86) | < 0.0001 |
| Asian | 0.73 (0.70, 0.76) | < 0.0001 |
| Education level | ||
| Less than high school | REF | |
| High school diploma | 1.24 (1.08, 1.44) | 0.003 |
| Some college | 1.22 (1.05, 1.41) | 0.007 |
| Bachelor’s degree or more | 1.16 (1.01, 1.35) | 0.04 |
| Annual income (USD) | ||
| <$40,000 | REF | |
| $40,000 to <$60,000 | 1.21 (1.17, 1.26) | < 0.0001 |
| $60,000 to <$100,000 | 1.32 (1.27, 1.36) | < 0.0001 |
| ≥$100,000 | 1.35 (1.31, 1.39) | < 0.0001 |
| Contact lens wear | 1.06 (0.97, 1.15) | 0.21 |
| Diabetes mellitus status † | ||
| None | REF | |
| Uncomplicated | 0.99 (0.96, 1.02) | 0.53 |
| Complicated | 0.80 (0.77, 0.84) | < 0.0001 |
| HIV/AIDS | 0.96 (0.84, 1.11) | 0.60 |
| Diagnosing health care provider | ||
| Ophthalmologist | REF | |
| Optometrist | 1.26 (1.21, 1.31) | < 0.0001 |
| Pediatrician | 2.27 (2.13, 2.43) | < 0.0001 |
| Family practice physician | 2.46 (2.37, 2.55) | < 0.0001 |
| Internist | 2.79 (2.69, 2.90) | < 0.0001 |
| Urgent care physician | 3.29 (3.17, 3.41) | < 0.0001 |
| Other provider | 2.79 (2.70, 2.88) | < 0.0001 |
Odds ratio (OR) and 95% confidence interval (CI) calculated using multivariable logistic regression model adjusting for age at conjunctivitis diagnosis, year of conjunctivitis diagnosis, sex, race, education level, annual income, contact lens wear, diabetes mellitus status, HIV/AIDS status, and type of diagnosing health care provider.
Diabetes mellitus status: None; Uncomplicated (diabetes mellitus without end-organ damage); Complicated (diabetes mellitus with end-organ damage such as neuropathy, nephropathy, or retinopathy)
HIV/AIDS: Human immunodeficiency virus / Acquired immune deficiency syndrome.
USD: United States dollars
Figure 2 shows the proportion of enrollees filling antibiotic prescriptions for acute conjunctivitis in 302 communities across the United States. Antibiotic fills varied widely from a low of 22% in Modesto, CA to as high as 80% in Traverse City, MI (Table 4). As reflected in Figure 2, there was considerable nationwide variation in antibiotic use, often across adjacent HRRs, but no obvious preponderance of antibiotic fills by larger geographic regions (Northeast, Midwest, Southeast, etc.), though communities near the West coast tended to have lower proportions. In some cases, there was considerable variation in geographically adjacent communities. For example, Saginaw, MI and Traverse City, MI had a 35% difference in antibiotic prescription fills.
Figure 2. Geographic Variation in Antibiotic Prescription Fills for Persons with Newly Diagnosed Acute Conjunctivitis.
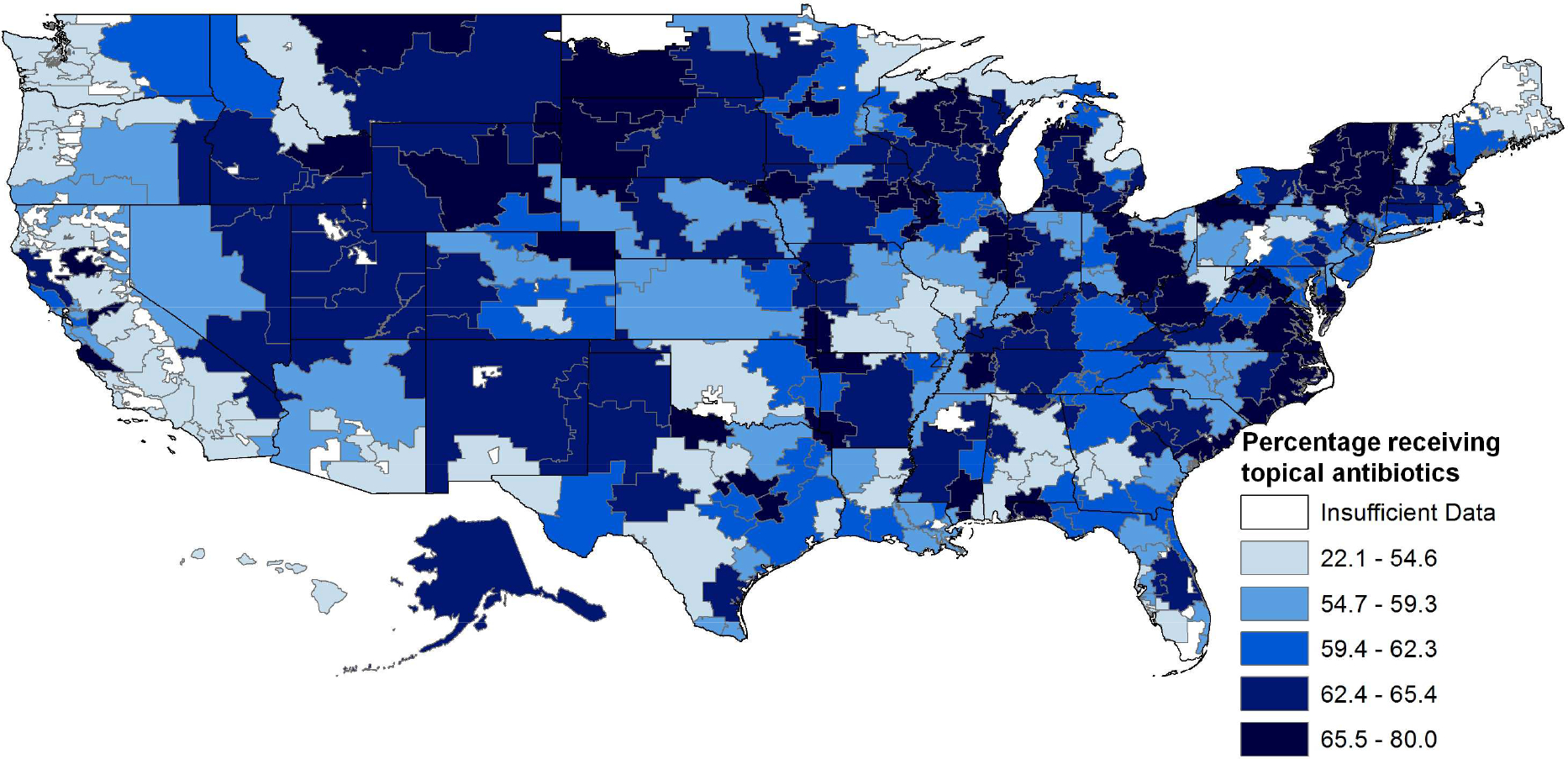
Proportion of enrollees with newly diagnosed acute conjunctivitis who filled ≥1 antibiotic prescription was calculated for 302 of 306 hospital referral regions (HRRs) with at least 20 eligible patients. Four of 306 HRRs with less than 20 eligible patients were excluded.
Table 4.
Hospital Referral Regions with Highest and Lowest Proportions of Enrollees Filling Prescriptions for Antibiotics for Acute Conjunctivitis
| Highest antibiotic prescription fills | Lowest antibiotic prescription fills | ||||
|---|---|---|---|---|---|
| Hospital referral region | Enrollees (N) | Antibiotic fills (%) | Hospital referral region | Enrollees (N) | Antibiotic fills (%) |
| Traverse City, MI | 20 | 80.0 | Modesto, CA | 398 | 22.1 |
| Wichita Falls, TX | 38 | 79.0 | Santa Barbara, CA | 188 | 23.9 |
| Gulfport, MS | 37 | 78.4 | Palm Springs/Rancho Mira, CA | 158 | 26.0 |
| Chico, CA | 44 | 77.3 | Mobile, AL | 560 | 28.0 |
| Burlington, VT | 61 | 75.4 | San Diego, CA | 2286 | 29.4 |
| Wausau, WI | 85 | 75.3 | San Luis Obispo, CA | 91 | 33.0 |
| Rapid City, SD | 56 | 75.0 | San Bernardino, CA | 1084 | 38.8 |
| Terre Haute, IN | 54 | 74.1 | Everett, WA | 312 | 38.8 |
| Sioux City, IA | 127 | 74.0 | Ventura, CA | 491 | 39.5 |
| Dearborn, MI | 109 | 73.4 | Honolulu, HI | 186 | 39.8 |
DISCUSSION
Using health care claims data from enrollees in a large nationwide US managed care network, we found that nearly 60% of persons who were newly diagnosed with acute conjunctivitis filled topical antibiotic prescriptions within a few days of their initial diagnosis. One-fifth of those who filled prescriptions for topical antibiotics received antibiotic-corticosteroid combinations, which are contraindicated in acute cases of conjunctivitis. We also noted considerable geographic variation in the percentage of patients filling antibiotic prescriptions for this condition. Sociodemographic factors such as white race, higher income, and higher educational level were associated with increased odds of filling antibiotic prescriptions, while risk factors that may predispose a patient to a more serious infection or superinfection, such as DM, HIV/AIDS, and contact lens wear were not associated with an increase in odds of filling antibiotic prescriptions for acute conjunctivitis.
Possible Reasons for Antibiotic Use
Reasons why so many persons diagnosed with acute conjunctivitis are receiving antibiotics are likely multifactorial. Health care providers may struggle to distinguish viral and allergic conjunctivitis cases from bacterial cases and some health care providers may lack education regarding appropriate management of acute conjunctivitis. Distinguishing between bacterial, viral, and allergic etiologies of acute conjunctivitis remains a challenge even for eye care providers because all three conditions may present with overlapping clinical features such as conjunctival injection, thin discharge, ocular surface irritation, foreign body sensation, and mild photophobia.3 A survey of primary care providers in the United Kingdom revealed that only 36% felt they could accurately differentiate bacterial and viral conjunctivitis.16
The odds of filling a prescription for topical antibiotics for acute conjunctivitis appear to be associated with the type of health care provider making the initial diagnosis. Compared to enrollees first diagnosed by eye care providers, those who had been diagnosed by non-eye care providers such as pediatricians, family practice physicians, internists, and urgent care physicians had two- to three-fold higher odds of filling prescriptions for topical antibiotics. These findings are consistent with previous studies which have demonstrated substantial antibiotic over-prescription for acute infectious conjunctivitis in the primary care setting in the United Kingdom16 and the Netherlands, with the latter study showing that 80% of patients received antibiotic prescriptions despite national guidelines recommending initial conservative management.17 Since acute conjunctivitis is primarily managed in the ambulatory and urgent care settings2, including the present study where 83% of persons diagnosed with acute conjunctivitis had been diagnosed by non-eye care providers, these findings indicate a pressing need to better educate all health care providers about the fact that most cases of acute conjunctivitis do well with conservative management and do not require immediate antibiotic therapy.
An interesting finding from these analyses is that the odds of filling prescriptions for acute conjunctivitis appear to be more associated with sociodemographic characteristics such as age, race, income, and education and less related to the presence of medical comorbidities that may predispose an enrollee to more serious infections. For example, a white, college-educated person earning over $100,000/year had 85% higher odds of antibiotic prescription fill compared to a black enrollee with the same health insurance who had not graduated from high school and was earning less than $40,000/year (data not shown). It may be easier for wealthier and more educated patients to pay the out of pocket costs for these medications. Likewise, more affluent and well-educated enrollees may be more inclined to pressure health care providers to prescribe these agents rather than use more conservative options. As with viral upper respiratory infections,18,19 some patients with acute conjunctivitis may be demanding antibiotics due to a desire for faster resolution of symptoms,20 perceived reduction in infectivity with antibiotic therapy,20 lack of awareness of the condition’s self-limited nature,21 or a belief that the infection is likely to worsen without treatment with antibiotics.21
Societal demand for antibiotics, particularly due to work and school policies, may also be driving antibiotic prescription fills.20,22 In a survey of 43 state health departments, 20 states had policies either encouraging or requiring children to receive antibiotics for acute conjunctivitis before permitting them to return to school. Only 4 states’ policies differentiated between viral and bacterial conjunctivitis.22 Working-age adults often face similar requirements for antibiotics before being permitted to return to work, although the extent of this practice is unknown. Such policies may be contributing to the high percentages of antibiotic prescription fills we are observing and warrant further scrutiny.
Among the 302 communities we studied, 7 of the 10 communities with the lowest antibiotic fill rates for acute conjunctivitis were in the state of California. These communities included Modesto, Santa Barbara, Palm Springs, San Diego, San Luis Obispo, San Bernardino, and Ventura, CA. It is unclear why these communities have much lower fill rates relative to others throughout the country. California is a state that does not have any requirements mandating children take antibiotics before they can return to school. Perhaps many employers in the state follow similar policies for the adults they employ. It is also possible that clinicians practicing in these communities receive better training about the importance of judicious use of antibiotics. Additional research is needed to better identify the factors that are contributing to lower fill rates in these communities with the hope that communities with much higher rates can learn from them.
Consequences of Antibiotic Overuse
The antibiotic prescription fill patterns identified in this study have public health and financial implications. Acute conjunctivitis costs the US health care system hundreds of millions of dollars in lost wages, clinical evaluation, and treatment every year.1 Given how prevalent acute conjunctivitis is, the societal costs associated with unnecessary treatment are likely quite high. For example, antibiotic prescriptions for conjunctivitis cost the United Kingdom National Health Service approximately $8.7 million in 1998.23 Topical fluoroquinolones were the most commonly filled antibiotic class in our study and can cost up to $200 per bottle.
As with antibiotic overuse for upper respiratory infections,18,19 the patterns of potential overuse identified here may be contributing to the growing problem of antibiotic resistance among ocular surface flora. As few as only 4 doses of antibiotic eye drops are associated with significant changes to the ocular flora24 and increased presence of multidrug-resistant strains.8 Fluoroquinolones, the most commonly filled antibiotic class in this study, are strongly associated with fluoroquinolone resistance as well as increased incidence of methicillin-resistant Staphylococcus aureus (MRSA) isolates on the ocular surface.25,26 The prevalence of ocular MRSA has increased from 30% in 2000 to 42% in 2005 while the incidence of MRSA endophthalmitis has also increased in the past several years.26,27 Nationwide surveillance studies have shown that antibiotic resistance among ocular surface isolates closely parallels resistance rates for systemic infections.7,25
Nearly one-fifth of the enrollees who received antibiotics for acute conjunctivitis filled prescriptions for antibiotic-corticosteroid combination therapy even though corticosteroids are known to increase adenoviral shedding, prolong duration of viral infections, and reactivate latent ocular herpes simplex virus infections.3 It is curious that persons who had been diagnosed by ophthalmologists or optometrists had much higher percentage of prescription fills for antibiotic-corticosteroid therapy (23% and 30% of all acute conjunctivitis cases, respectively) compared to persons diagnosed by non-eye care providers (8% of all cases). Eye care providers may feel more confident in their ability to distinguish bacterial or allergic conjunctivitis from viral conditions compared to other health care providers or may simply be more aware of the availability of antibiotic-corticosteroid combination therapies than non-eye care providers, leading to an increased tendency to prescribe such products.
Potential solutions for reducing antibiotic overuse should target patients, health care providers, and policymakers. Educating patients about acute conjunctivitis’ often benign, self-limited course may help dispel misconceptions about the condition and reduce reflexive demands for immediate antibiotic use.21 Use of a rapid, point-of-care test for adenovirus1 may reduce health care providers’ diagnostic uncertainty and increase their comfort with deferring antibiotic therapy. One study estimates as many as 1.1 million cases of treatment can be avoided, resulting in a savings of $400 million in the US alone, with the use of this test.1 Health care providers are much less likely to prescribe unnecessary antibiotics if they are presented with alternative treatment plans in the electronic health record, asked to justify their rationale for prescribing antibiotics in the electronic health record,28 encouraged to commit to reducing unnecessary antibiotic use in front of a group of peer health care providers,29 or shown their own antibiotic prescribing rates in comparison to those of other health care providers.28 Educational efforts must also target policymakers who set the policies that many schools, day care centers, workplaces, and health departments are required to follow, since current policies are likely contributing to the high rates of antibiotic prescription fills we are observing.
Limitations
This study has limitations. Although our data source contained information on diagnoses of acute conjunctivitis made by health care providers, we lacked access to the actual medical records required for determining appropriateness of antibiotic prescriptions for specific enrollees. No doubt some of the enrollees who had been diagnosed with “acute conjunctivitis” would have been appropriate candidates for antibiotic therapy. For example, neonatal and adult gonococcal conjunctivitis cases warrant immediate and aggressive antibiotic therapy.3 However, given that the overwhelming majority of acute conjunctivitis cases are likely to be viral4,5 or allergic,3 it is unlikely that so many of the enrollees in our study sample had severe or unremitting bacterial infections that warranted immediate antibiotic therapy. Second, results from this sample of enrollees with commercial health insurance may not capture patterns of care for patients with other forms of health insurance or persons who are uninsured. Third, this study used prescription fill data as a surrogate measure of antibiotic use but could not capture free medication samples that are frequently dispensed to patients in clinics. Thus, the proportion of patients with acute conjunctivitis actually receiving antibiotics may be even higher than the numbers we are reporting. Finally, the study excluded inpatient and hospital-acquired cases of acute conjunctivitis, which are known to affect many patients and incur substantial costs.1
CONCLUSION
Nearly 60% of enrollees who were newly diagnosed with acute conjunctivitis in this managed care network filled prescriptions for topical antibiotic medications shortly after initial diagnosis. Geographic variation in antibiotic fills was substantial, varying from as low as 20–30% in some communities to as high as 75% or higher in others. Patterns of antibiotic use for acute conjunctivitis appear to be driven more by sociodemographic factors and the type of health care provider who diagnosed the condition than by medical indications. These findings highlight the need to better educate patients, clinicians, and health policymakers about acute conjunctivitis and search for ways to reduce unnecessary use of antibiotics for this condition.
Grant Support:
W.K. Kellogg Foundation, East Grand Rapids, MI; National Eye Institute, Bethesda, MD, 1R01EY026641–01A1 (JDS); American Ophthalmological Society Travel Grant, San Francisco, CA (NSS).
Footnotes
This paper has been presented in part at the following meetings:
American Ophthalmological Society 152nd Annual Meeting, Colorado Springs, CO, May 20, 2016.
Association for Research in Vision and Ophthalmology 2016 Annual Meeting, Seattle, WA, May 4, 2016.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES:
- 1.Udeh BL, Schneider JE, Ohsfeldt RL. Cost effectiveness of a point-of-care test for adenoviral conjunctivitis. Am J Med Sci. 2008;336:254–264. [DOI] [PubMed] [Google Scholar]
- 2.Shields T, Sloane PD. A Comparison of eye problems in primary care and ophthalmology practices. Fam Med. 1991;23:544–546. [PubMed] [Google Scholar]
- 3.American Academy of Ophthalmology Cornea/External Disease Panel. Preferred Practice Pattern® Guidelines. Conjunctivitis. San Francisco, CA: American Academy of Ophthalmology; 2013. Available at: https://www.aao.org/preferred-practice-pattern/conjunctivitis-ppp--2013. Accessed April 17, 2017. [Google Scholar]
- 4.Sambursky RP, Fram N, Cohen EJ. The prevalence of adenoviral conjunctivitis at the Wills Eye Hospital Emergency Room. Optometry. 2007;78:236–239. [DOI] [PubMed] [Google Scholar]
- 5.Woodland RM, Darougar S, Thaker U, et al. Causes of conjunctivitis and keratoconjunctivitis in Karachi, Pakistan. Trans R Soc Trop Med Hyg. 1992;86:317–320. [DOI] [PubMed] [Google Scholar]
- 6.Sheikh A, Hurwitz B, van Schayck CP, et al. Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2012;(9):CD001211. [DOI] [PubMed] [Google Scholar]
- 7.Haas W, Pillar CM, Torres M, et al. Monitoring antibiotic resistance in ocular microorganisms: results from the Antibiotic Resistance Monitoring in Ocular micRorganisms (ARMOR) 2009 Surveillance Study. Am J Ophthalmol. 2011;152:567–574. [DOI] [PubMed] [Google Scholar]
- 8.Dave SB, Toma HS, Kim SJ. Ophthalmic antibiotic use and multidrug-resistant staphylococcus epidermidis: a controlled, longitudinal study. Ophthalmology. 2011;118:2035–2040. [DOI] [PubMed] [Google Scholar]
- 9.Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among us ambulatory care visits, 2010–2011. JAMA. 2016;315:1864–1873. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Ophthalmology. Choosing wisely: five things physicians and patients should question. http://www.choosingwisely.org/societies/american-academy-of-ophthalmology; 2013. Accessed March 25, 2017.
- 11.Kauh CY, Blachley TS, Lichter PR, et al. Geographic variation in the rate and timing of cataract surgery among US communities. JAMA Ophthalmol. 2016;134:267–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stein JD, Shekhawat N, Talwar N, Balkrishnan R. Impact of the introduction of generic latanoprost on glaucoma medication adherence. Ophthalmology. 2015;122:738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wennberg JE, Cooper MM. The Dartmouth Atlas of Health Care. Chicago: American Hospital Publishing;1996. [PubMed] [Google Scholar]
- 14.Wennberg J, Gittelsohn A. Small area variations in health care delivery. Science. 1973;182:1102–1108. [DOI] [PubMed] [Google Scholar]
- 15.Fisher ES, Wennberg JE. Health care quality, geographic variations, and the challenge of supply-sensitive care. Perspect Biol Med. 2003;46:69–79. [DOI] [PubMed] [Google Scholar]
- 16.Everitt H, Little P. How do GPs diagnose and manage acute infective conjunctivitis? A GP survey. Fam Pract. 2002;19:658–660. [DOI] [PubMed] [Google Scholar]
- 17.Rietveld RP, Ter Riet G, Bindels PJ, et al. Do general practitioners adhere to the guideline on infectious conjunctivitis? Results of the Second Dutch National Survey of General Practice. BMC Fam Pract. 2007;8:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnett ML, Linder JA. Antibiotic prescribing to adults with sore throat in the United States, 1997–2010. JAMA Intern Med. 2014;174:138–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dooling KL, Shapiro DJ, Van Beneden C, et al. Overprescribing and inappropriate antibiotic selection for children with pharyngitis in the United States, 1997–2010. JAMA Pediatr. 2014;168:1073–1074. [DOI] [PubMed] [Google Scholar]
- 20.Rose PW, Ziebland S, Harnden A, et al. Why do general practitioners prescribe antibiotics for acute infective conjunctivitis in children? Qualitative interviews with GPs and a questionnaire survey of parents and teachers. Fam Pract. 2006;23:226–232. [DOI] [PubMed] [Google Scholar]
- 21.Everitt H, Kumar S, Little P. A qualitative study of patients’ perceptions of acute infective conjunctivitis. Br J Gen Pract. 2003;53:36–41. [PMC free article] [PubMed] [Google Scholar]
- 22.Ohnsman CM. Exclusion of students with conjunctivitis from school: policies of state departments of health. J Pediatr Ophthalmol Strabismus. 2007;44:101–105. [DOI] [PubMed] [Google Scholar]
- 23.Department of Health. Prescription cost analysis data. http://webarchive.nationalarchives.gov.uk/20120503222906/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4021787.pdf; 1998. Accessed April 20, 2017.
- 24.Dave SB, Toma HS, Kim SJ. Changes in ocular flora in eyes exposed to ophthalmic antibiotics. Ophthalmology. 2013;120:937–941. [DOI] [PubMed] [Google Scholar]
- 25.McDonald M, Blondeau JM. Emerging antibiotic resistance in ocular infections and the role of fluoroquinolones. J Cataract Refract Surg. 2010;36:1588–1598. [DOI] [PubMed] [Google Scholar]
- 26.Asbell PA, Sanfilippo CM, Pillar CM, et al. Antibiotic resistance among ocular pathogens in the United States: five-year results from the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) Surveillance Study. JAMA Ophthalmol. 2015;133:1445–1454. [DOI] [PubMed] [Google Scholar]
- 27.Sadaka A, Durand ML, Sisk R, Gilmore MS. Staphylococcus aureus and its bearing on ophthalmic disease. Ocul Immunol Inflamm. 2015;25:111–121. [DOI] [PubMed] [Google Scholar]
- 28.Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA. 2016;315:562–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meeker D, Knight TK, Friedberg MW, et al. Nudging guideline-concordant antibiotic prescribing: a randomized clinical trial. JAMA Intern Med. 2014;174:425–431. [DOI] [PMC free article] [PubMed] [Google Scholar]


