Abstract
Introduction
Major depression is a common and potentially lethal condition. Early data suggest that the population-level burden of depression has been exacerbated by the COVID-19 pandemic. Prepandemic estimates of depression prevalence are required to quantify and comprehensively address the pandemic's impact on mental health in the U.S.
Methods
Data were drawn from the 2015–2020 National Survey on Drug Use and Health, a nationally representative study of U.S. individuals aged ≥12 years. The prevalence of past-year depression and help seeking for depression were estimated from 2015 to 2019, and time trends were tested with Poisson regression with robust SEs. Point estimates were calculated for 2020 and not included in statistical trend analyses because of differences in data collection procedures.
Results
In 2020, 9.2% (SE=0.31) of Americans aged ≥12 years experienced a past-year major depressive episode. Depression was more common among young adults aged 18–25 years (17.2%, SE=0.78), followed closely by adolescents aged 12–17 years (16.9%, SE=0.84). Depression increased most rapidly among adolescents and young adults and increased among nearly all sex, racial/ethnic, income, and education groups. Depression prevalence did not change among adults aged ≥35 years, and the prevalence of help seeking remained consistently low across the study period.
Conclusions
From 2015 to 2019, there were widespread increases in depression without commensurate increases in treatment, and in 2020, past 12‒month depression was prevalent among nearly 1 in 10 Americans and almost 1 in 5 adolescents and young adults. Decisive action involving a multipronged public health campaign that includes evidence-based prevention and intervention to address this ongoing mental health crisis is urgently needed.
INTRODUCTION
Major depression is the most common mental disorder in the U.S.1 and is the strongest risk factor for suicide behavior.2, 3, 4 Previous findings show increases in depression in the U.S. population from 6.6% in 2005 to 7.3% in 2015,5 consistent with other data.6 The most rapid increases from 2005 to 2015 were observed among adolescents and those at the highest and lowest income levels. For race/ethnicity and sex, trends were generally equivalent with increases across all groups.6 Early reports in 2020 and forward suggest that the coronavirus 2019 (COVID-19) pandemic has contributed to a worsening mental health crisis in the U.S.,7, 8, 9, 10 especially among adolescents and young adults.4 Obtaining accurate prepandemic national estimates is critical to eventually quantifying and adequately addressing the mental health impact of the pandemic.
Most individuals with depression remain untreated or undertreated.11, 12, 13 Although substantial progress has been made in evidence-supported pharmacologic and psychotherapeutic treatments for depression over the past several decades,13 , 14 commensurate and comprehensive implementation of and access to affordable high-quality mental health care has not occurred.
Moreover, substantive sociodemographic differences in help seeking and receipt of treatment for depression persist. For instance, individuals with higher SES and/or insurance coverage (versus those with lower SES and/or without insurance) are more likely to access and receive depression treatment, more likely to engage more extensively in treatment, and less likely to discontinue medication treatment for depression.15, 16, 17, 18 Over the past 2 decades, policy changes (e.g., the 2008 Mental Health Parity and Addiction Equity Act) that increased coverage of mental health and addiction treatment services and efforts to reduce the stigma associated with mental disorders (e.g., celebrity disclosures19 , 20) should theoretically have resulted in increases in help seeking and receipt of treatment.
This study estimated the prevalence of past 12‒month major depression among U.S. individuals aged ≥12 years in each year from 2015 to 2020. The study then estimated changes in the prevalence of depression from 2015 to 2019 overall and by sociodemographic characteristics. Finally, the study investigated the prevalence of help seeking, including receipt of pharmacologic treatment for depression, among individuals with past-year depression from 2015 to 2019 and in 2020, overall and by sociodemographic characteristics.
METHODS
Study Sample
Data were drawn from the National Survey on Drug Use and Health (NSDUH). The NSDUH provides annual cross-sectional national data on substance use and mental health in the U.S. and is described elsewhere.21 A multistage area probability sample for each of the 50 states and the District of Columbia was conducted to represent the male and female civilian non-institutionalized population of the U.S. aged ≥12 years. Datasets from each year included in this analysis (2015–2019) were pooled, adding a variable for the survey year. Estimates for 2020 were added but not in the statistical analysis of trends because methods used in 2020 differed because of the COVID-19 pandemic, making these incomparable statistically with previous estimates. Person-level analysis sampling weights were computed to control for individual-level nonresponse and were adjusted to ensure consistency with population estimates obtained from the U.S. Census Bureau. A new weight was created by dividing the original weight by the number of data sets combined. For this study, analyses were restricted to those who responded to questions about past-year depression at the time of the interview (98.4%), resulting in a total analytic sample of N=278,176 (mean per survey year=55,635; range=55,132–56,292) from 2015 to 2019 and n=32,893 for 2020. The study was exempt from IRB review.
Measures
Questions to assess major depressive episodes (MDEs) were based on DSM-IV criteria, and separate depression modules were administrated to adults versus youth aged 12–17 years. Depression modules were adapted from the National Comorbidity Survey-Replication22 for adult respondents (aged ≥18 years) and from the National Comorbidity Survey-Adolescent23 for adolescent respondents (aged 12–17 years). Both adult and adolescent respondents were classified as having had a lifetime MDE on the basis of reporting ≥5 of 9 symptoms for MDE, including either depressed mood or loss of interest or pleasure in daily activities, during the same 2-week period in their lifetime. Respondents with lifetime MDE were further classified as having past-year MDE if they met the criteria for a lifetime MDE and reported feeling depressed or having lost interest or pleasure in daily activities as well as other symptoms for at least 2 weeks during the past 12 months. The past-year MDE variable for this study was created by combining the adolescent and adult variables.
Past-year help seeking for depression was assessed by 2 questions. Respondents were asked whether they had seen or talked to a medical doctor (MD) or other professional about their MDE symptoms in the past 12 months and whether they had received prescription medication for their MDE symptoms in the past 12 months.
Statistical Analysis
First, the prevalence of past-year depression and associated SEs for each survey year were calculated. Time trends in the prevalence of past-year depression from 2015 to 2019 were tested using Poisson regression, with continuous year as the predictor for the linear time trend. These analyses were conducted twice: first with no covariates (unadjusted) and then while adjusting for age, race/ethnicity, sex, marital status, income, and education.
Second, the prevalence of past-year depression and associated SEs for each survey year and sociodemographic subgroup were calculated. Time trends from 2015 to 2019 in the prevalence of past-year depression by sociodemographic subgroup were tested using Poisson regression, with continuous year as the predictor for the linear time trend. These analyses were conducted twice: first with no covariates (unadjusted) and then while adjusting for the sociodemographic characteristics other than the stratified variable.
Third, the sample was restricted to those meeting the criteria for past-year MDE, and the prevalence of help seeking and associated SEs were calculated for each survey year. Time trends from 2015 to 2019 in the prevalence of speaking with an MD or other professional about MDE symptoms and receiving a prescription medication for MDE symptoms in the past 12 months were tested in separate Poisson regression models, with continuous year as the predictor for the linear time trend. These analyses were conducted twice: first with no covariates (unadjusted) and then while adjusting for age, race/ethnicity, sex, marital status, income, and education. These analyses were also repeated stratifying by the same sociodemogrpahic variables.
All analyses were conducted in 2021–2022 with SAS (version 9.4) and used appropriate sample weights to correct for differences in the probability of selection and were adjusted for survey design effects to obtain accurate SEs. RRs with robust SEs were calculated for the effects within each model.
RESULTS
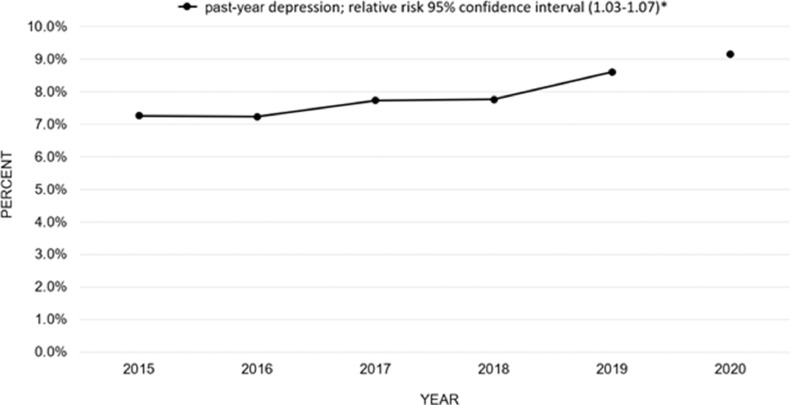
The prevalence of past-year depression increased from 7.3% (SE=0.15) in 2015 to 8.6% (SE=0.18) in 2019 (Figure 1 ), and this monotonic increase from 2015 to 2019 remained after adjusting for sociodemographic characteristics. The prevalence of past-year depression in 2020 was 9.2% (SE=0.31).
Figure 1.
Prevalence of past-year depression in the U.S., 2015 to 2020.
*Statistical significance at p<0.05.
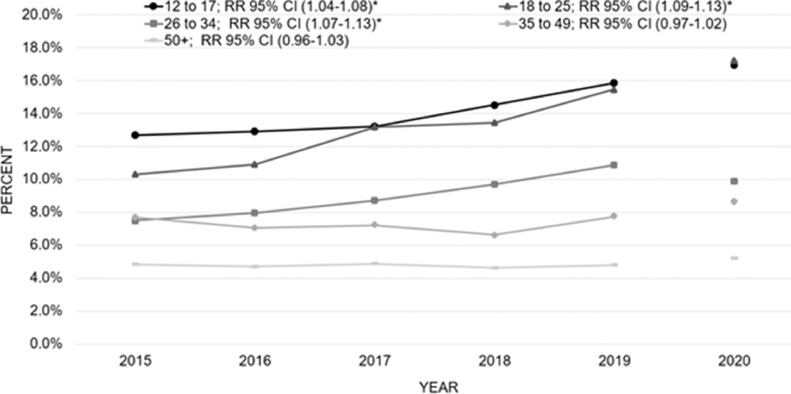
Stratifying the population by age, the highest prevalences of depression across time were found among adolescents (aged 12–17 years) and young adults (aged 18–25 years). Increases in depression from 2015 to 2019 were observed among those aged 12–17 years (2015: 12.7% [SE=0.40] to 2019: 15.8% [SE=0.34] and 2020: 16.9% [SE=0.84]), 18–25 years (2015: 10.3% [SE=0.31] to 2019: 15.5% [SE=0.41] and 2020: 17.2% [SE=0.78]), and 26–34 years (2015: 7.5% [SE=0.31] to 2019: 10.9% [SE=0.52] and 2020: 9.9% [SE=0.65]) (Figure 2 ). These trends remained relatively unchanged after adjusting for sociodemographic characteristics. No increases in depression were observed among those aged 35–49 years or aged ≥50 years in unadjusted models.
Figure 2.
Prevalence of past-year depression in the U.S., 2015 to 2020, by age group.
*Statistical significance at p<0.05.
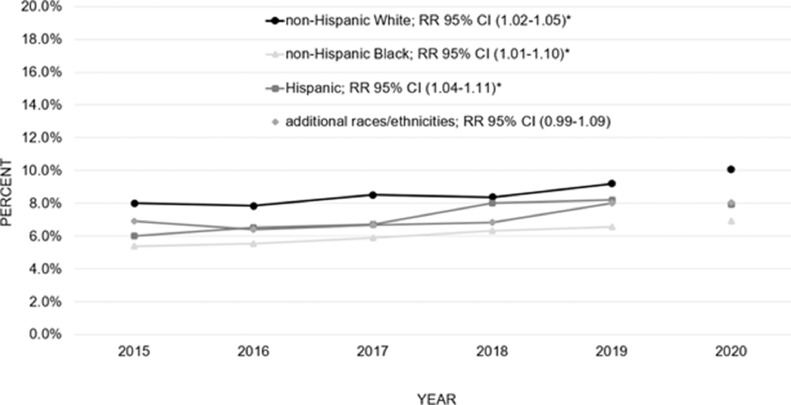
Stratifying the population by race/ethnicity, the prevalence of depression among non-Hispanic White individuals exceeded that among all other racial/ethnic groups. An increase in depression from 2015 to 2019 was observed among those in each racial/ethnic subgroup (2015: 8.0% [SE=0.18] to 2019: 9.2% [SE=0.24] and 2020: 10.1% [SE=0.40] for non-Hispanic White; 2015: 5.4% [SE=0.34] to 2019: 6.6% [SE=0.40] and 2020: 6.9% [SE=0.83] for non-Hispanic Black; 2015: 6.0% [SE=0.31] to 2019: 8.22% [SE=0.44] and 2020: 7.9% [SE=0.59] for Hispanic; and 2015: 6.9% [SE=0.60] to 2019: 8.0% [SE=0.57] and 2020: 8.1% [SE=0.59] for additional races/ethnicities) (Figure 3 ). Increases remained after adjusting for sociodemographic characteristics.
Figure 3.
Prevalence of past-year depression in the U.S., 2015 to 2020, by race/ethnicity.
*Statistical significance at p<0.05.
The prevalence of depression was consistently higher for women than for men. Depression increased from 2015 to 2019 among both men (2015: 4.7% [SE=0.16] to 2019: 6.3% [SE=0.21] and 2020: 6.4% [SE=0.32]) and women (2015: 9.7% [SE=0.24] to 2019: 10.8% [SE=0.26] and 2020: 11.8% [SE=0.44]) (Appendix Figure 1, available online). Increases remained after adjusting for sociodemographic characteristics.
Stratifying by marital status, the prevalence of depression was highest among adults who were not currently nor previously married. In unadjusted models there was an increase in depression from 2015 to 2019 for those who had not been married (2015: 10.1% [SE=0.23] to 2019: 13.7% [SE=0.34] and 2020: 14.2% [SE=0.51) (Appendix Figure 2, available online]). This finding remained after adjusting for other sociodemographic characteristics. No increases in depression were found among married individuals or those who were widowed, divorced, or separated in unadjusted or adjusted models.
Considering income, the highest prevalence of depression was evident among those with the lowest household income, whereas those with the highest household income exhibited the lowest prevalence of depression. There was an increase in depression from 2015 to 2019 for those in each income group (2015: 10.1% [SE=0.37] to 2019: 12.1% [SE=0.54] and 2020: 11.6% [SE=0.73] for <$20,000; 2015: 7.2% [SE=0.29] to 2019: 9.1% [SE=0.35] and 2020: 10.2% [SE=0.67] for $20,000 to $49,999; 2015: 7.5% [SE=0.42] to 2019: 8.7% [SE=0.43] and 2020: 9.3% [SE=0.80] for $50,000–$74,999; and 2015: 5.8% [SE=0.24] to 2019: 6.9% [SE=0.21] and 2020: 7.5% [SE=0.43] for ≥$75,000) (Appendix Figure 3, available online]). These associations remained after adjusting for sociodemographic characteristics.
Considering education, the prevalence of depression was higher among those with some college education than among all other education subgroups. The prevalence of depression increased from 2015 to 2019 among those who were high-school graduates (2015: 6.2% [SE=0.28] to 2019: 7.1% [SE=0.35] and 2020: 7.5% [SE=0.60]), those with some college education (2015: 8.9% [SE=0.37] to 2019: 10.4% [SE=0.35] and 2020: 7.6% [SE=0.48]), and those with a college or graduate degree (2015: 5.6% [SE=0.28] to 2019: 6.9% [SE=0.33] and 2020: 7.6% [SE=0.47]) (Appendix Figure 4 , available online]). These associations remained after adjusting for sociodemographic characteristics. There was no change in the prevalence of depression from 2015 to 2019 among those without a high-school diploma in unadjusted or adjusted analyses.
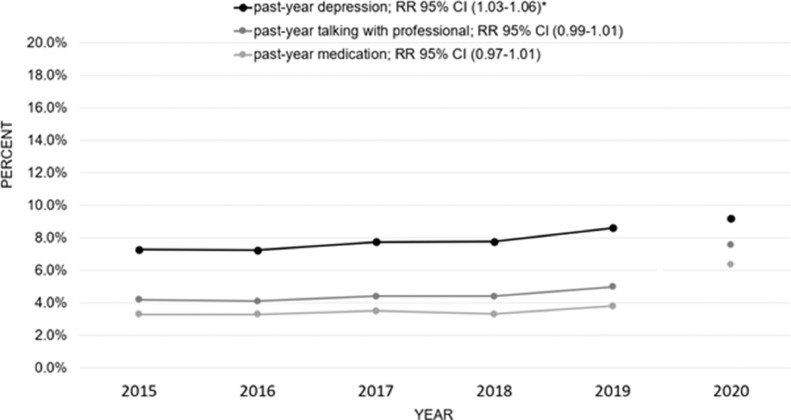
Overall, the prevalence of (1) seeing or talking to an MD or other professional about symptoms of MDE and (2) receiving a prescription medication for MDE symptoms did not change from 2015 to 2019 among those with past-year depression (Figure 4).
Figure 4.
Prevalence of past-year depression and talking with a medical professional and medication prescription among those with past-year depression in the U.S. from 2015 to 2020.
*Statistical significance at p<0.05.
Stratifying the population by age, modest increases in both talking to an MD or other professional (2015: 42.4% [SE=1.47] to 2019: 47.4% [SE=1.28] and 2020: 51.7% [SE=1.94]) and receiving a prescription medication for symptoms of depression (2015: 30.0% [SE=1.45] to 2019: 31.8% [SE=1.08] and 2020: 38.7% [SE=1.64]) were observed only among young adults aged 18 to 25 years (Appendix Figures 5 and 6, available online). These results were evident in both unadjusted and adjusted models. Among adolescents ages 12 to 17 years, there was no change in the prevalence of receiving prescription medication in either unadjusted or adjusted models, but in the model adjusted for other sociodemographic variables, an increase in talking to an MD or other professional was observed between 2015 and 2019 (2015: 36.0% [SE=1.29] to 2019: 39.7% [SE=1.55] and 2020: 40.1% [SE=2.48]). This increase was also modest, and most adolescents with depression neither told a healthcare professional about depression symptoms nor received pharmacologic treatment from 2015 through 2020. No change in the prevalence of help seeking was found in the age groups of ≥26 years.
Stratifying the population by sex, modest increases in help seeking and receiving a prescription medication for symptoms of depression from 2015 to 2019 were observed among females (2015: 60.2% [SE=1.12] to 2019: 62.4% [SE=1.21] and 2020: 61.2% [SE=1.95] for talking to an MD or other professional; 2015: 47.9% [SE=1.46] to 2019: 48.9% [SE=1.11] and 2020: 48.0% [SE=2.20] for receiving a prescription medication) but only within the adjusted models and were not observed among males either in unadjusted or adjusted models (Appendix Figure 7, available online). Stratifying by race/ethnicity, marital status, education, and income did not reveal subgroup differences in talking to an MD/other professional or receiving prescription medication for depression.
DISCUSSION
This study updates the depression prevalence estimates for the U.S. general population through the year 2020 and confirms increases in depression from 2015 to 2019, reflecting an escalating public health crisis in the U.S. even before the onset of the pandemic. Depression increased among those aged younger than 35 years, among those who never married (after adjusting for age), and among those with at least a high-school diploma. Across sex, income, and racial/ethnic subgroups, increases were generally equivalent. It should also be noted that the prevalence of depression did not decline in any sociodemographic subgroup during this period. In 2020, past-year depression was common among nearly 1 of 10 Americans overall, and the depression prevalence approached 20% among adolescents and young adults.
The percentage of those with depression in the overall population who reported speaking with a medical professional about or receiving medication for depression did not change appreciably from 2015 to 2019 and remained low, below 6%. Depression prevalence from 2015 to 2019 increased most rapidly among young adults aged 18–25 years (consistent with recent evidence on anxiety24), and in 2020, the depression prevalence was approximately 17% among adolescents aged 12–17 years, although fewer than half of those with depression spoke with a health professional or received prescription medication. This gap in treatment is consistent with and extends findings from earlier studies.25 , 26 Help seeking did not increase for any group by race/ethnicity, income, marital status, or education. The net effect of these trends suggests an escalating public health crisis and that parity and public-service announcement efforts have been unsuccessful in achieving equity in depression treatment. The elevated level and concentration of untreated depression among adolescents and young adults are especially problematic because untreated depression early in life is predictive of a more intractable course and increased risk of subsequent additional mental health problems.27 , 28 The short- and long-term impact of the pandemic on depression are not yet clear, but these estimates are a start toward quantifying the consequences.
Although the NSDUH does not provide information about specific depression treatments received, in the context of extant evidence about mental health care in the U.S., these results suggest that undertreatment of depression may be widespread even among the proportion who sought help. Severe shortages of psychiatrists—particularly child and adolescent psychiatrists—exist in many U.S. states and are concentrated in lower SES and racial/ethnic minority communities. For instance, reports indicate that there are 30 psychiatrists per 100,000 people in Massachusetts versus 5.3 per 100,000 in Idaho.29 Psychiatrists are more likely to practice in counties with higher average income and a proportion of adults with extensive formal education.29 Therefore, although cost-effective, evidence-supported treatments for depression exist, they may still be difficult to access in community healthcare settings and, as such, remain inaccessible for most Americans who could benefit from them.26 Greater investment in testing the effectiveness of evidence-based treatments in the community and making them as widely available and affordable as possible through trained healthcare professionals is needed. Pediatricians and primary care providers are a potential key to addressing the treatment gap because they are more likely to be involved in the delivery of mental health care than specialists. Unfortunately, with few exceptions, such as the work of REACH,30 which offers a training program in patient-centered mental health in pediatric primary care to increase clinician comfort with addressing pediatric mental health problems, there is very little training for pediatricians or primary care physicians in the diagnosis or treatment of common mental health conditions. Collaborative care and integrated care models have also shown promise and could be implemented more widely.31, 32, 33 Beyond lack of training for physicians, a purely clinical approach is not likely feasible because of inadequate number of providers, inadequate access, and ongoing stigma associated with help seeking. Community- and school-based programs that educate gatekeepers are another low-cost, evidence-based approach that could be expanded.34, 35, 36
Limitations
Limitations of this study must be considered. Observed increases in the prevalence of depression may be because of greater reporting. Yet, it is not immediately clear why reporting would increase more dramatically in certain groups than in others. Furthermore, there were no available data on the depth of engagement when talking with a health care professional about depressive symptoms or the suitability of specific pharmacologic treatments. It is also possible that help seeking for other mental health problems such as anxiety, which is highly overlapping with depression in terms of concurrent diagnoses and treatments, could impact estimates of depression prevalence and/or treatment. In addition, combining racial/ethnic categories to conduct the analyses with adequate sample sizes may have obscured the differences in depression prevalence and depression treatment between groups.15 , 37
CONCLUSIONS
These U.S. national data reveal a clear increase in depression and, critically, in untreated depression. Depression is the strongest risk factor for suicide behavior, and these patterns demand immediate action, especially for adolescents and young adults, at both the clinical and public health levels. Expanding evidence-based campaigns that promote early intervention, prevention, and education about depression are needed now.
Acknowledgments
ACKNOWLEDGMENTS
No financial disclosures were reported by the authors of this paper.
CRediT AUTHOR STATEMENT
Renee D. Goodwin: Conceptualization, Investigation, Methodology, Project administration, Writing – original draft. Lisa C. Dierker: Data curation, Formal analysis, Investigation, Methodology, Software, Visualization. Sandro Galea: Investigation, Methodology, Visualization. Christina W. Hoven: Investigation, Writing – review and editing. Melody Wu: Investigation, Visualization, Writing – review and editing. Andrea H. Weinberger: Investigation, Writing – review and editing.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2022.05.014.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang SS, Stuckler D, Yip P, Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. 2013;347:f5239. doi: 10.1136/bmj.f5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Depression. Geneva, Switzerland: World Health Organization. http://www.who.int/mediacentre/factsheets/fs369/en/. Published 2016. Accessed June 1, 2021.
- 5.Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018;48(8):1308–1315. doi: 10.1017/S0033291717002781. [DOI] [PubMed] [Google Scholar]
- 6.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. 2019;128(3):185–199. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- 7.Hou WK, Li TW, Liang L, et al. Trends of depression and anxiety during massive civil unrest and COVID-19 in Hong Kong, 2019–2020. J Psychiatr Res. 2021;145:77–84. doi: 10.1016/j.jpsychires.2021.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ettman CK, Cohen GH, Abdalla SM, et al. Persistent depressive symptoms during COVID-19: a national, population-representative, longitudinal study of U.S. adults. Lancet Reg Health Am. 2022;5:100091. 10.1016/j.lana.2021.100091. [DOI] [PMC free article] [PubMed]
- 9.Lorenzoni G, Azzolina D, Maresio E, et al. Impact of the COVID-19 lockdown on psychological health and nutritional habits in Italy: results from the #PRESTOinsieme study. BMJ Open. 2022;12(4) doi: 10.1136/bmjopen-2021-048916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murthy V. Office of the Surgeon General, HHS; Washington, DC: U.S.: 2021. Protecting youth mental health: the U.S. Surgeon General’s advisory.https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf Accessed September 1, 2022. [Google Scholar]
- 11.Whiteford HA, Harris MG, McKeon G, et al. Estimating remission from untreated major depression: a systematic review and meta-analysis. Psychol Med. 2013;43(8):1569–1585. doi: 10.1017/S0033291712001717. [DOI] [PubMed] [Google Scholar]
- 12.Riolo SA, Nguyen TA, Greden JF, King CA. Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. Am J Public Health. 2005;95(6):998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shim RS, Baltrus P, Ye J, Rust G. Prevalence, treatment, and control of depressive symptoms in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. J Am Board Fam Med. 2011;24(1):33–38. doi: 10.3122/jabfm.2011.01.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357–1366. doi: 10.1016/S0140-6736(17)32802-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: too little for too few. Arch Gen Psychiatry. 2010;67(1):37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shao Z, Richie WD, Bailey RK. Racial and ethnic disparity in major depressive disorder. J Racial Ethn Health Disparities. 2016;3(4):692–705. doi: 10.1007/s40615-015-0188-6. [DOI] [PubMed] [Google Scholar]
- 17.Olfson M, Marcus SC, Tedeschi M, Wan GJ. Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry. 2006;163(1):101–108. doi: 10.1176/appi.ajp.163.1.101. [DOI] [PubMed] [Google Scholar]
- 18.Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatr Serv. 2004;55(12):1379–1385. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- 19.Brusie C. A mind of her own: 7 famous women helping to #endthestigma of mental illness. Healthline.September 9, 2018. https://www.healthline.com/health/mental-illness-celebrities. Accessed April 21, 2022.
- 20.Cooper A. A conversation Starater. Bring Change to Mind. May 23, 2021. https://bringchange2mind.org/conversations. Accessed April 22, 2022.
- 21.Substance Abuse and Mental Health Services Administration . Substance Abuse and Mental Health Services Administration, HHS; Rockville, MD: 2020. 2019 National Survey on Drug Use and Health Codebook. [Google Scholar]
- 22.Hedden S, Gfroerer J, Barker P, et al. CBHSQ Data Review. Substance Abuse and Mental Health Services Administration (U.S.); Rockville, MD: February 2012. Comparison of NSDUH mental health data and methods with other data sources.https://www.ncbi.nlm.nih.gov/books/NBK390286/ Accessed September 1, 2022. [PubMed] [Google Scholar]
- 23.Merikangas KR, Avenevoli S, Costello EJ, Koretz D, Kessler RC. National Comorbidity Survey Replication Adolescent supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48(4):367–379. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodwin RD, Weinberger AH, Kim JH, Wu M, Galea S. Trends in anxiety among adults in the United States, 2008–2018: rapid increases among young adults. J Psychiatr Res. 2020;130:441–446. doi: 10.1016/j.jpsychires.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mojtabai R, Olfson M. National trends in mental health care for U.S. adolescents. JAMA Psychiatry. 2020;77(7):703–714. doi: 10.1001/jamapsychiatry.2020.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6) doi: 10.1542/peds.2016-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59(3):225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 28.Glied S, Pine DS. Consequences and correlates of adolescent depression. Arch Pediatr Adolesc Med. 2002;156(10):1009–1014. doi: 10.1001/archpedi.156.10.1009. [DOI] [PubMed] [Google Scholar]
- 29.McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, Yu H. Growth and distribution of child psychiatrists in the United States: 2007–2016. Pediatrics. 2019;144(6) doi: 10.1542/peds.2019-1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patient-centered mental health in pediatric primary care. The REACH Institute.https://www.thereachinstitute.org/services/for-primary-care-practitioners/primary-pediatric-psychopharmacology-1. Accessed June 6, 2021.
- 31.Leung LB, Benitez CT, Dorsey C, et al. Integrating mental health in safety-net primary care: a five-year observational study on visits in a county health system. Med Care. 2021;59(11):975–979. doi: 10.1097/MLR.0000000000001637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coleman KJ, Dreskin M, Hackett DL, et al. A roadmap for institutionalizing collaborative care for depression in a large integrated healthcare system. J Gen Intern Med. 2020;35(suppl 2):839–848. doi: 10.1007/s11606-020-06102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.White K, Stetson L, Hussain K. Integrated behavioral health role in helping pediatricians find long term mental health interventions with the use of assessments. Pediatr Clin North Am. 2021;68(3):685–705. doi: 10.1016/j.pcl.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 35.Ghoncheh R, Gould MS, Twisk JW, Kerkhof AJ, Koot HM. Efficacy of adolescent suicide prevention e-learning modules for gatekeepers: a randomized controlled trial. JMIR Ment Health. 2016;3(1):e8. doi: 10.2196/mental.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. Public health action for the prevention of suicide: a framework. Geneva, Switzerland: World Health Organization. https://apps.who.int/iris/rest/bitstreams/104057/retrieve. Published 2012. Accessed September 1, 2022.
- 37.González HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res. 2010;44(15):1043–1051. doi: 10.1016/j.jpsychires.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.