Abstract
Background
Coronavirus disease-2019 (COVID-19) has had negative physical and mental impacts on people globally. The current study examined general psychiatric symptoms (fear, anxiety, depression, and insomnia) and loneliness, and their interrelationships and correlates among Bangladeshi individuals approximately 1 year after the onset of the COVID-19 outbreak.
Methods
An internet-based cross-sectional survey was conducted among 1004 Bangladeshi people (51.8% male; mean age: 25.41 ± 7.80; age range: 18–60 years). Data were collected using a semi-structured e-questionnaire including informed consent, socio-demographics, lifestyle measures, and psychometric tools assessing loneliness, anxiety, depression, insomnia, and fear of COVID-19.
Results
Sizeable participants screened positive for loneliness (63.5%), anxiety (26.3%), depression (46.4%), and insomnia (50.7%). Considerable numbers of respondents also reported fear of COVID-19. In hierarchical regression analyses, loneliness, anxiety, depression, insomnia, and fear of COVID-19 were associated with socio-demographic and lifestyle factors. Loneliness, anxiety, depression, insomnia, and fear of COVID-19 were positively correlated with each other (p < 0.001). In exploratory path analyses, anxiety, depression, and insomnia mediated the relationship between loneliness and fear of COVID-19.
Conclusions
The findings indicate that many people in Bangladesh have experienced psychiatric concerns approximately 1 year after the onset of the COVID-19 outbreak. Investigation into empirically supported interventions and their implementation is needed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-022-04232-3.
Keywords: COVID-19, Loneliness, Anxiety, Depression, Insomnia, Fear, Bangladesh
Introduction
Worldwide, the outbreak of coronavirus disease-2019 (COVID-19) is a significant public health concern [1]. COVID-19 originated in Wuhan, Hubei Province, China in December 2019 [2, 3]. The COVID-19 pandemic represents a huge disease burden, infecting over 556 million people around the globe as of July 15, 2022 [4]. Symptoms range from asymptomatic infection to severe respiratory infection and mortality [5]. In addition to the physical health consequences, public health authorities globally have expressed concerns over an international mental health crisis due to quarantine, social isolation, financial strain, and the threat of infection [6, 7]. Experts remain uncertain regarding the differential trajectories of the COVID-19 pandemic across jurisdictions, projected numbers of cases and deaths, and to what extent restrictive measures may disrupt daily life [8]. The unpredictability and ambiguity surrounding COVID-19 may trigger numerous psychiatric and related phenomena, including loneliness, anxiety, depression, sleep concerns such as insomnia, and fear [8–15], in varying forms and to different degrees [16].
Major epidemics and pandemic outbreaks can have profound and wide-ranging psychological impacts on people [17]. Even people not directly affected by the disease may have considerable psychological problems stemming from the pandemic, as people may experience uncertainty and fear of falling sick or dying, feelings of helplessness, and stigma [18]. These experiences may impact their overall mental health, sometimes throughout their lives [19]. In the setting of physical separation, which mandates reducing in-person social interactions, rates of loneliness may rise, potentially increasing the prevalence of mood disorders, self-harm, and suicide, as well as exacerbating pre-existing mental health conditions [12]. The extent to which loneliness may operate to worsen mental health that may then impact abilities or tendencies to adapt to stressors like the COVID-19 pandemic warrants consideration.
Bangladesh has been facing tremendous challenges since the first verified COVID-19 outbreak on March 8, 2020 [20] with a total of over 1.9 million transmissions with a 14% infection rate as of July 15, 2022 [21]. To deal with this challenge, the government has imposed numerous pandemic-related limitations (e.g., lockdown, quarantine, and social isolation) to address this pandemic [22]. In this environment, individuals may feel isolated, potentially compromising their psychological well-being [11, 15, 22]. A prior study early in the pandemic reported that 33.7% of Bangladeshi adults suffered from anxiety, with 57.9%, and 59.7% experiencing depressive symptoms and stress, respectively [15]. Another Bangladeshi study found that 27.8% of participants were depressed, and depression was associated with COVID-19-related fear [23]. Sleep concerns were also prominent among Bangladeshi residents early during the COVID-19 pandemic, with about 2.8% of participants reporting severe forms of insomnia [14]. Recent publications in Bangladesh suggest factors such as age, gender, socioeconomic status, education level, occupation, and perceptions of COVID-19 relate to psychiatric disorders [15, 24]. Furthermore, fear of infection, financial uncertainty, inadequate food supply, and physical inactivity were related to anxiety and depression [25].
While prior studies of specific psychiatric concerns in Bangladesh have been reported during the initial period of the outbreak of COVID-19 [11, 15, 24, 26], little is known about the longer-term mental health impacts due to this ongoing pandemic. Bangladesh has been encountering a surge in COVID-19 infections, with nearly 50% more deaths every day than during the previous peak in June 2020 [27]. Given these circumstances, it is crucial to understand the current psychiatric concerns of Bangladeshi people as the pandemic progresses. The objective of this study was to investigate the prevalence and associated factors of psychiatric symptoms among Bangladeshi people approximately 1 year after the first COVID-19 diagnosis. Additionally, exploratory path analyses were conducted to examine the extent to which loneliness may operate through psychiatric symptoms (anxiety, depression, and insomnia) to impact fear of COVID-19.
Methods
Study design and setting
The study employed a cross-sectional design. Data were collected from January to March 2021, nearly 1 year after the COVID-19 outbreak in Bangladesh [20]. Bangladesh has a population of around 169 million with an area of 56,977 sq. miles, or 147,570 sq. km [28]. Islam is the most popular religion, with 90% of the population being Muslim. The population density of the country is 1140 per sq. km., and per capita income is 2824 USD (2021–2022). The main economic activity is agriculture [29].
Sample size calculation
The sample size was calculated using the following Eq. (1):
| 1 |
Here,
n = number of samples
z = 1.96 (95% confidence level)
p = prevalence estimate (37.3% or 0.373)
q = (1-p)
d = precision limit or proportion of sampling error (0.05)
As a previous study reported 37.3% anxiety among Bangladeshi people early in the outbreak [24], a sample size of 503 participants was estimated assuming a 40% non-response rate. However, the present study’s sample size exceeded this estimate.
Study procedure
Participants were recruited through an online survey using a convenience sampling technique. A semi-structured self-reported questionnaire (see Supplementary file) written in Bangla (the native language of participants) was designed and incorporated into the Google survey tool (Google Forms) for data collection. The link generated from the tool was shared across different social media platforms (e.g., Facebook, WhatsApp, etc.) and other online platforms (e.g., email, blogs, etc.) as an advertisement for participation in the survey. The questionnaire was pre-tested with 50 individuals before starting the final data collection for acceptability and clarity. Informed consent from each participant was obtained before starting the survey by asking, “Are you willing to participate in this survey voluntarily?” with “yes” or “no” responses. Those who responded positively were allowed to participate in this survey by giving access to the full questionnaire; otherwise, a blank survey form was submitted automatically. A total of 1033 participants completed the online survey form. Of these, 1004 participants were selected following quality control and manual check procedures to exclude incomplete and invalid surveys and were included in the final analysis. The inclusion criteria were i) being a Bangladeshi resident, ii) being aged ≥18 years, iii) good internet access, and iv) voluntary participation. The study protocol was reviewed and approved by the Biosafety, Biosecurity, and Ethical review board of the Jahangirnagar University, Savar, Dhaka-1342, Bangladesh [BBEC, JU/M 2020/COVID-19/(11)2]. The study was conducted following the Checklist for Reporting Results of Internet ESurveys (CHERRIES) guidelines [30].
Measures
Socio-demographic measures
Participants’ socio-demographic information, including age, gender, marital status, education (below university/university), monthly family income, and residence (rural/urban), were collected during the survey. The respondents’ levels of education were primary (grades 1–5), secondary (grades 6–10), intermediate (grades 11–12), bachelor, master, and above, which were then further recoded into below university and university. Monthly family income was divided into four categories: less than 20,000 Bangladeshi Taka (BDT), 20,000–30,000 BDT, 30,000–40,000 BDT, and more than 40,000 BDT.
Lifestyle-related measures during COVID-19
Lifestyle-related measures were collected by asking questions about participants’ chronic health conditions (e.g., diabetes, high blood pressure, asthma/respiratory problems, heart disease, kidney problems, cancer, and any other conditions) (yes/no), self-rated health status (SRH) [31] (good/poor), worries due to COVID-19 (yes/no), experiencing prolonged home quarantine (yes/no), decreased household income due to COVID-19 (yes/no), unemployment of family members due to COVID-19 (yes/no), food scarcity (yes/no), sleep duration (< 7 hours/7–9 hours/> 9 hours), engaging in physical exercise (yes/no), average hours of browsing the internet, social media use (e.g., Facebook, WhatsApp) (not at all/rarely/sometimes/often/always), COVID-19 related news exposure (yes/no), tobacco smoking (yes/no), alcohol consumption (yes/no), and self-reported quality of life (SQL) [31] (good/poor). In terms of SRH and SQL, participants were asked, “In general, how would you rate your overall health?” and “In general, how would you rate your overall quality of life?”, respectively [31]. The responses were based on a five-point Likert scale with response options: “excellent”, “very good”, “good”, “fair”, and “poor”. In the present study, the responses for both SRH and SQL were recoded as good (excellent/very good/good) and poor (poor/fair). Average internet browsing hours were categorized as “< 2 hours”, “2–4 hours”, “4–6 hours”, and “> 6 hours”.
University of California, Los Angeles (UCLA) loneliness scale [32]
Participants’ loneliness was measured using the three-item translated Bangla version of the UCLA loneliness scale. Participants’ responses were based on a three-point Likert scale ranging from 1 (hardly ever) to 3 (often). The sum of the total scores ranged from 3 to 9, with higher scores indicating higher levels of loneliness. A score of ≥6 indicated loneliness, as in earlier research [12, 32–34]. The reliability or internal consistency of the measure was very good in the current sample (Cronbach’s α = 0.85).
Generalized anxiety disorder (GAD-7) [35]
The Bangla version of the seven-item GAD-7 was used for assessing the anxiety of the participants [36]. Participants’ responses were recorded using a four-point Likert scale ranging from 0 (Not at all) to 3 (Nearly every day). Total scores ranged from 0 to 21, with higher scores reflecting greater anxiety. A score of ≥10 indicated moderate to severe anxiety, as previously [12, 37, 38]. In the present study, the GAD-7 scale had excellent reliability (Cronbach’s alpha: α = 0.90).
Patient Health Questionnaire (PHQ-9) [39]
Participants’ depressive symptoms were measured using the Bangla version of the PHQ-9 [40]. Symptoms of depression during the past 2 weeks were recorded. Participant responses were recorded on a four-point Likert scale ranging from 0 (Not at all) to 3 (Nearly every day). Total scores ranged from 0 to 27, with higher scores reflecting greater depression [41, 42]. A score of ≥10 indicated depression, as previously [43, 44]. The internal consistency of the PHQ-9 scale in the present sample was very good (Cronbach’s α = 0.87).
Insomnia Severity Index (ISI) [45]
Participants’ insomnia was measured using the seven-item Bangla version of the ISI [46]. Each item is rated on a five-point Likert scale (e.g., 0 “Not at all” to 4 “Extremely”). Total scores ranged from 0 to 28, with higher scores reflecting greater insomnia severity. A final score ranging from 0 to 7 indicated no insomnia; a score of 8–14 indicated sub-threshold insomnia; a score of 15–21 indicated moderate insomnia; and a score of 22–28 indicated severe insomnia [14, 47]. A predetermined cutoff (ISI ≥ 10) was used to diagnose insomnia [47]. The Cronbach’s alpha was 0.91 in the present study.
Fear of COVID-19 Scale (FCV-19S) [48]
Participants’ COVID-19-related fear was measured using the seven-item Bangla version of the FCV-19S [49]. Participants’ responses were recorded using a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Cumulative scores ranged from 7 to 35, with higher scores reflecting more COVID-19-related fear. The reliability or the internal consistency of the scale in the present study was very good (Cronbach’s α = 0.86).
Statistical analysis
All statistical analyses were performed using two software packages (Microsoft Excel 2019 and SPSS version 25). Data cleaning, sorting, and coding were first performed using Microsoft Excel. Using SPSS, descriptive statistics (i.e., frequencies, percentages, means, and standard deviations) were computed. Inferential statistics involve conducting t-tests or one-way analyses of variance (ANOVAs) to determine the mean differences among variable groups. Bivariate Pearson correlation analyses were used for continuous variables. Variables that showed group differences/bivariate in initial analyses were included in hierarchical regression analyses. In each hierarchical regression model, socio-demographics were included in Block 1; Block 2 included lifestyle factors; and Block 3 included psychiatric symptoms. A p-value < 0.05 was considered significant for all statistical analyses. Exploratory analyses assessing whether insomnia, anxiety, and depression statistically mediated the relationship between loneliness and fear of COVID-19 were conducted with SPSS PROCESS and 5000 bootstrap resamples [50]. Loneliness was included as the independent variable, fear of COVID-19 as the dependent variable, and the severity of insomnia, anxiety, and depression as potential mediators. Associations, indirect effects, and bootstrapped confidence intervals (CIs) were calculated. Significant indirect effects were determined by CIs that did not include zero.
Results
General profile of participants
A total of 1004 individuals (mean age of 25.41 (SD = 7.80) years) comprised the study sample. Most participants were male (51.8%), unmarried (72.8%), had university educations (82.1%), and resided in urban areas (75.3%); many had monthly incomes between 30,000–40,000 BDT [319–426 US$] (27.5%) [1 US$ ≈ 93.91 BDT] (Table 1). Most denied chronic health conditions (81.6%) and reported good health status (60.6%). The distributions of continuous variables are presented in Table 2.
Table 1.
Distributions of categorical variables by general psychiatric symptoms
| Variables | Overall | Loneliness | Anxiety | Depression | Insomnia | Fear of COVID-19 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Mean (SD) | t | Mean (SD) | t | Mean (SD) | t | Mean (SD) | t | Mean (SD) | t | |
| Gender | |||||||||||
| Male | 520 (51.8) | 5.61 (1.78) | 10.46** | 6.99 (4.59) | 2.52 | 9.91 (5.12) | 1.66 | 9.43 (6.66) | 0.75 | 17.5 (5.74) | 3.83 |
| Female | 484 (48.2) | 5.99 (1.86) | 7.45 (4.63) | 10.33 (5.23) | 9.8 (6.72) | 18.21 (5.63) | |||||
| Marital status | |||||||||||
| Unmarried | 731 (72.8) | 5.85 (1.85) | 7.29** | 6.97 (4.57) | 4.00* | 9.87 (5.1) | 8.33*** | 9.34 (6.64) | 2.19 | 17.33 (5.39) | 13.04*** |
| Married | 208 (20.7) | 5.42 (1.7) | 7.74 (4.67) | 10.17 (4.96) | 10.37 (7.18) | 19.58 (5.83) | |||||
| In a relationship | 65 (6.5) | 6.31 (1.78) | 8.25 (4.75) | 12.58 (6.07) | 10.2 (5.28) | 18.11 (7.31) | |||||
| Education | |||||||||||
| Below university | 180 (17.9) | 5.87 (1.76) | 0.36 | 7.84 (4.38) | 4.07* | 11.17 (4.5) | 9.31** | 9.53 (6.47) | 0.03 | 18.26 (5.94) | 1.15 |
| University | 824 (82.1) | 5.78 (1.84) | 7.07 (4.66) | 9.88 (5.29) | 9.63 (6.74) | 17.75 (5.64) | |||||
| Monthly household income (BDT) | |||||||||||
| < 20,000 | 216 (21.5) | 5.73 (1.97) | 1.63 | 7.16 (5.02) | 0.31 | 10.26 (5.21) | 0.18 | 7.86 (6.18) | 7.18*** | 17.18 (5.57) | 3.59* |
| 20,000–30,000 | 274 (27.3) | 5.7 (1.74) | 7.01 (4.18) | 9.93 (4.82) | 9.61 (6.8) | 18.58 (5.94) | |||||
| 30,000–40,000 | 276 (27.5) | 5.73 (1.72) | 7.34 (4.41) | 10.14 (4.95) | 10.22 (6.58) | 18.13 (5.55) | |||||
| > 40,000 | 238 (23.7) | 6.02 (1.91) | 7.33 (4.95) | 10.14 (5.78) | 10.49 (6.85) | 17.26 (5.59) | |||||
| Residence | |||||||||||
| Urban | 756 (75.3) | 5.77 (1.82) | 0.33 | 7.13 (4.66) | 1.05 | 9.98 (5.23) | 1.95 | 9.81 (6.67) | 2.80 | 17.88 (5.56) | 0.10 |
| Rural | 248 (24.7) | 5.85 (1.87) | 7.47 (4.47) | 10.51 (4.98) | 8.99 (6.71) | 17.74 (6.09) | |||||
| Chronic health conditions | |||||||||||
| Yes | 185 (18.4) | 6.25 (1.72) | 14.60*** | 8.66 (4.61) | 23.00*** | 11.52 (5.05) | 17.06*** | 12.25 (6.33) | 36.66*** | 18.5 (5.73) | 3.00 |
| No | 819 (81.6) | 5.69 (1.84) | 6.88 (4.56) | 9.79 (5.15) | 9.01 (6.62) | 17.69 (5.68) | |||||
| Self-reported health status | |||||||||||
| Good | 608 (60.6) | 5.53 (1.78) | 32.06*** | 6.6 (4.37) | 27.88*** | 9.71 (5.08) | 9.21** | 8.8 (6.41) | 23.22*** | 17.61 (5.58) | 2.61 |
| Poor | 396 (39.4) | 6.19 (1.83) | 8.15 (4.82) | 10.72 (5.26) | 10.85 (6.92) | 18.2 (5.85) | |||||
| Worried due to COVID-19 | |||||||||||
| Yes | 697 (69.4) | 5.85 (1.68) | 1.86 | 7.56 (4.42) | 13.26*** | 10.18 (4.8) | 0.39 | 10.36 (6.55) | 29.36*** | 19.05 (5.44) | 113.48*** |
| No | 307 (30.6) | 5.67 (2.13) | 6.42 (4.95) | 9.96 (5.94) | 7.91 (6.68) | 15.11 (5.3) | |||||
| Experienced prolonged home quarantine | |||||||||||
| Yes | 801 (79.8) | 5.74 (1.87) | 3.43 | 7.2 (4.71) | 0.02 | 10.12 (5.18) | 0.02 | 9.21 (6.77) | 14.31*** | 17.84 (5.64) | < 0.01 |
| No | 203 (20.2) | 6 (1.64) | 7.26 (4.21) | 10.07 (5.19) | 11.18 (6.11) | 17.85 (5.91) | |||||
| Decreased household income due to COVID-19 | |||||||||||
| Yes | 644 (64.1) | 5.83 (1.84) | 0.84 | 7.5 (4.59) | 7.07** | 10.44 (5.08) | 7.37** | 9.78 (6.82) | 1.23 | 18.15 (5.68) | 5.22* |
| No | 360 (35.9) | 5.72 (1.81) | 6.69 (4.62) | 9.52 (5.31) | 9.29 (6.44) | 17.29 (5.69) | |||||
| Unemployment of family members due to COVID-19 | |||||||||||
| Yes | 366 (36.5) | 5.87 (1.74) | 0.99 | 8.01 (4.42) | 17.34*** | 10.81 (5.06) | 10.50** | 10.88 (7.07) | 21.28*** | 18.48 (5.93) | 7.16** |
| No | 638 (63.5) | 5.75 (1.88) | 6.76 (4.66) | 9.71 (5.2) | 8.88 (6.34) | 17.48 (5.53) | |||||
| Food scarcity | |||||||||||
| Yes | 387 (38.5) | 5.85 (1.74) | .62 | 7.98 (4.35) | 17.74*** | 10.54 (4.93) | 4.30* | 11 (7.02) | 28.06*** | 19.1 (5.87) | 31.55*** |
| No | 617 (61.5) | 5.76 (1.88) | 6.73 (4.71) | 9.84 (5.31) | 8.73 (6.31) | 17.06 (5.44) | |||||
| Average sleep duration | |||||||||||
| < 7 hours | 304 (30.3) | 5.66 (1.91) | 1.98 | 7.38 (5.12) | 0.30 | 9.49 (5.68) | 3.19* | 10.86 (7.12) | 7.75*** | 18.19 (5.69) | 3.41* |
| 7–9 hours | 532 (53.0) | 5.8 (1.7) | 7.12 (4.4) | 10.41 (4.79) | 9.04 (6.11) | 17.97 (5.64) | |||||
| > 9 hours | 168 (16.7) | 6.01 (2.06) | 7.2 (4.33) | 10.28 (5.34) | 9.13 (7.32) | 16.82 (5.8) | |||||
| Physical exercise | |||||||||||
| Yes | 424 (42.2) | 5.49 (1.87) | 20.74*** | 6.85 (4.79) | 4.42* | 9.8 (5.23) | 2.62 | 8.95 (6.96) | 7.13** | 17.64 (5.39) | 0.89 |
| No | 580 (57.8) | 6.02 (1.77) | 7.47 (4.47) | 10.34 (5.13) | 10.09 (6.44) | 17.99 (5.91) | |||||
| Internet browsing hours | |||||||||||
| < 2 hours | 123 (12.3) | 5.02 (1.75) | 14.85*** | 6.64 (4.68) | 1.74 | 9.33 (4.89) | 3.08* | 7.47 (6.88) | 7.95*** | 18.36 (5.55) | 2.98* |
| 2–4 hours | 258 (25.7) | 5.5 (1.65) | 6.88 (4.47) | 9.58 (4.76) | 8.92 (6.02) | 18.04 (5.48) | |||||
| 4–6 hours | 318 (31.7) | 6.11 (1.68) | 7.53 (4.51) | 10.6 (4.88) | 10.59 (6.31) | 18.25 (5.9) | |||||
| > 6 hours | 305 (30.4) | 6.02 (2.03) | 7.39 (4.8) | 10.36 (5.83) | 10.03 (7.27) | 17.05 (5.65) | |||||
| Social media use | |||||||||||
| Not at all | 55 (5.5) | 5.09 (1.92) | 6.83*** | 8.45 (4.8) | 5.15*** | 10.64 (4.63) | 1.51 | 8.11 (7.7) | 3.94** | 18.96 (6.27) | 2.61* |
| Rarely | 86 (8.6) | 5.8 (1.51) | 8.1 (4.71) | 10.57 (5.6) | 10.19 (6.48) | 18.81 (5.43) | |||||
| Sometime | 285 (28.4) | 5.58 (1.65) | 6.62 (4.21) | 9.53 (4.58) | 9.57 (5.96) | 18.25 (5.63) | |||||
| Often | 374 (37.3) | 5.79 (1.8) | 6.84 (4.51) | 10.17 (5.1) | 8.97 (6.23) | 17.54 (5.4) | |||||
| Always | 204 (20.3) | 6.28 (2.1) | 8 (5.05) | 10.49 (5.96) | 10.99 (7.94) | 17.12 (6.14) | |||||
| COVID-19-related news exposure | |||||||||||
| Yes | 641 (63.8) | 5.74 (1.81) | 1.69 | 7.26 (4.64) | 0.23 | 9.93 (5.01) | 2.09 | 9.39 (6.75) | 1.83 | 18.41 (5.61) | 18.02*** |
| No | 363 (36.2) | 5.89 (1.86) | 7.12 (4.57) | 10.42 (5.44) | 9.99 (6.56) | 16.84 (5.72) | |||||
| Tobacco smoking | |||||||||||
| Yes | 186 (18.5) | 5.89 (1.82) | 0.61 | 7.67 (4.42) | 2.28 | 10.38 (5.56) | 0.60 | 10.72 (6.7) | 6.36* | 17.68 (5.6) | 0.18 |
| No | 818 (81.5) | 5.77 (1.83) | 7.11 (4.65) | 10.05 (5.08) | 9.35 (6.66) | 17.88 (5.72) | |||||
| Alcohol consumption | |||||||||||
| Yes | 73 (7.3) | 6.49 (1.93) | 11.65** | 7.4 (4.66) | 0.13 | 10.29 (5.96) | 0.09 | 12.53 (7.25) | 15.30*** | 17.41 (6.68) | 0.45 |
| No | 931 (92.7) | 5.74 (1.81) | 7.2 (4.61) | 10.1 (5.11) | 9.38 (6.59) | 17.88 (5.61) | |||||
| Self-reported quality of life | |||||||||||
| Good | 653 (65.0) | 5.53 (1.75) | 39.59*** | 6.74 (4.39) | 20.26*** | 9.87 (5.12) | 4.11* | 9.01 (6.31) | 15.18*** | 17.66 (5.58) | 1.99 |
| Poor | 351 (35.0) | 6.28 (1.88) | 8.1 (4.89) | 10.56 (5.25) | 10.72 (7.21) | 18.19 (5.89) | |||||
SD Standard deviation, BDT Bangladeshi Taka
*p < 0.05, **p < 0.01, ***p < 0.001
Table 2.
Distributions of all continuous variables including general psychiatric symptoms
| Variables | α | Mean (SD) | Range | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|---|
| 1. Age (years) | — | 25.41 (7.80) | (18–60) | — | ||||
| 2. Loneliness | 0.85 | 5.79 (1.83) | (3–9) | −0.04 | — | |||
| 3. Fear of COVID-19 | 0.86 | 17.84 (5.69) | (7–35) | 0.19** | 0.11* | — | ||
| 4. Anxiety | 0.90 | 7.21 (4.62) | (0–21) | 0.13** | 0.42** | 0.31** | — | |
| 5. Depression | 0.87 | 10.11 (5.18) | (0–27) | 0.05 | 0.32** | 0.23** | 0.62** | — |
| 6. Insomnia | 0.91 | 9.61 (6.69) | (0–24) | 0.10* | 0.39** | 0.26** | 0.40** | 0.27** |
α Cronbach alpha, SD Standard deviation
*p < 0.01**p < 0.001
Lifestyle during the COVID-19 pandemic
Most respondents reported worries due to COVID-19 infection (69.4%) and were in prolonged home quarantine (79.8%) (Table 1). Substantial proportions reported decreased household incomes (64.1%), joblessness of family members (36.5%), and food scarcity (38.5%) due to the pandemic. More than half (53.0%) reported they slept in a normal range (7–9 hours/day), and 57.8% reported not engaging in physical exercise during the COVID-19 pandemic. Participants reported considerable online behaviors during the COVID-19 pandemic, including internet use (> 6 hours/day: 30.4%) and social media use (e.g., Facebook, WhatsApp; most of the time: 20.3%). A sizeable minority reported smoking cigarettes (18.5%) and drinking alcohol (7.3%) during the pandemic. Most (63.8%) participants were exposed to regular COVID-19-related news. Finally, 35% reported a poor quality of life during the pandemic.
Loneliness
The prevalence estimate of loneliness was 63.5%. Loneliness was positively associated with female gender, physical inactivity, frequent internet, and Facebook use, alcohol consumption, poor quality of life, anxiety, depression, and insomnia (Table 3). The regression model predicted 30% of the variance in loneliness [F(13,990) = 33.36; p < .001].
Table 3.
Hierarchical regression analysis predicting loneliness
| Variables | Model 1 | Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | t | B | SE | β | t | B | SE | β | t | ΔR2 | R2Adj | |
| Block 1 – Socio-demographics (F(4,999) = 14.00; p < 0.001) | 0.05 | 0.05 | ||||||||||||
| Gendera | 0.36 | 0.11 | 0.10 | 3.17** | 0.33 | 0.11 | 0.09 | 3.02** | 0.28 | 0.10 | 0.08 | 2.83** | ||
| Marital statusb | −0.06 | 0.10 | −0.02 | − 0.66 | − 0.02 | 0.09 | − 0.01 | − 0.21 | − 0.13 | 0.08 | − 0.04 | −1.57 | ||
| Chronic health conditionsc | − 0.55 | 0.15 | − 0.12 | −3.73*** | − 0.66 | 0.15 | − 0.14 | −4.48*** | − 0.24 | 0.14 | − 0.05 | −1.77 | ||
| Self-reported health statusd | 0.62 | 0.12 | 0.17 | 5.36*** | 0.22 | 0.13 | 0.06 | 1.72 | 0.04 | 0.12 | 0.01 | 0.33 | ||
| Block 2 – Lifestyle factors (F(9,994) = 17.57; p < 0.001) | 0.08 | 0.13 | ||||||||||||
| Physical exercisec | 0.52 | 0.11 | 0.14 | 4.70*** | 0.40 | 0.10 | 0.11 | 3.96*** | ||||||
| Internet browsing hoursd | 0.27 | 0.07 | 0.15 | 4.04*** | 0.15 | 0.06 | 0.08 | 2.51* | ||||||
| Social media usee | 0.15 | 0.06 | 0.09 | 2.42* | 0.15 | 0.06 | 0.09 | 2.64** | ||||||
| Alcohol consumptionc | −0.75 | 0.21 | −0.11 | −3.49** | −0.65 | 0.19 | −0.09 | −3.32** | ||||||
| Self-reported quality of lifef | 0.59 | 0.13 | 0.15 | 4.46*** | 0.44 | 0.12 | 0.12 | 3.70*** | ||||||
| Block 3 – Psychiatric symptoms (F(13,990) = 33.36; p < 0.001) | 0.17 | 0.30 | ||||||||||||
| Fear of COVID-19 | −0.01 | 0.01 | −0.04 | −1.32 | ||||||||||
| Anxiety | 0.10 | 0.01 | 0.25 | 6.96*** | ||||||||||
| Depression | 0.03 | 0.01 | 0.09 | 2.60* | ||||||||||
| Insomnia | 0.06 | 0.01 | 0.21 | 6.97*** | ||||||||||
B Unstandardized regression coefficient, SE Standard error, β Standardized regression coefficient; a1 = Male, 2 = Female; b1 = Unmarried, 2 = Married, 3 = In a relationship; c1 = Yes, 2 = No; d1 = < 2 hours, 2 = 2–4 hours, 3 = 4–6 hours, 4 = > 6 hours; e1 = Not at all, 2 = Rarely, 3 = Sometime, 4 = Often, 5 = Always; f1 = Good, 2 = Poor. *p < 0.05, **p < 0.01, ***p < 0.001
Anxiety
The prevalence estimate of moderate to severe anxiety was 26.3%. Anxiety was positively associated with older age, loneliness, depression, insomnia, and fear of COVID-19 (Table 4). Overall, the regression model predicted 49% of the variance in anxiety [F(16,987) = 61.52; p < 0.001].
Table 4.
Hierarchical regression analysis predicting anxiety
| Variables | Model 1 | Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | t | B | SE | β | t | B | SE | β | t | ΔR2 | R2Adj | |
| Block 1 - Socio-demographics (F(5,998) = 12.49; p < 0.001) | 0.06 | 0.05 | ||||||||||||
| Age | 0.05 | 0.02 | 0.08 | 2.25* | 0.03 | 0.02 | 0.05 | 1.23 | 0.04 | 0.02 | 0.07 | 2.38* | ||
| Marital statusa | 0.34 | 0.26 | 0.04 | 1.28 | 0.31 | 0.26 | 0.04 | 1.19 | −0.11 | 0.20 | −0.02 | − 0.58 | ||
| Educationb | −0.21 | 0.39 | −0.02 | − 0.54 | − 0.24 | 0.40 | − 0.02 | − 0.60 | 0.20 | 0.29 | 0.02 | 0.66 | ||
| Chronic health conditionsc | −1.50 | 0.37 | −0.13 | −4.04*** | − 1.63 | 0.38 | − 0.14 | −4.33*** | − 0.16 | 0.29 | − 0.01 | − 0.55 | ||
| Self-reported health statusd | 1.43 | 0.29 | 0.15 | 4.91*** | 0.91 | 0.34 | 0.10 | 2.70** | 0.37 | 0.25 | 0.04 | 1.45 | ||
| Block 2 – Lifestyle factors (F(12,991) = 7.53; p < 0.001) | 0.03 | 0.07 | ||||||||||||
| Worry due to COVID-19c | −0.80 | 0.32 | −0.08 | −2.50* | − 0.16 | 0.25 | − 0.02 | − 0.65 | ||||||
| Decreased household income due to COVID-19c | −0.18 | 0.33 | −0.02 | −0.55 | 0.06 | 0.25 | 0.01 | 0.25 | ||||||
| Unemployment of family members due to COVID-19c | −0.49 | 0.35 | −0.05 | −1.41 | − 0.10 | 0.26 | − 0.01 | −0.38 | ||||||
| Food scarcityc | −0.40 | 0.37 | −0.04 | −1.07 | − 0.18 | 0.28 | − 0.02 | −0.65 | ||||||
| Physical exercisec | 0.59 | 0.29 | 0.06 | 1.99* | −0.07 | 0.22 | − 0.01 | − 0.30 | ||||||
| Social media used | 0.27 | 0.14 | 0.06 | 1.87 | −0.09 | 0.11 | − 0.02 | −0.80 | ||||||
| Self-reported quality of lifee | 0.67 | 0.35 | 0.07 | 1.93 | 0.25 | 0.26 | 0.03 | 0.97 | ||||||
| Block 3 – Psychiatric symptoms (F(16,987) = 61.52; p < 0.001) | 0.42 | 0.49 | ||||||||||||
| Loneliness | 0.47 | 0.07 | 0.19 | 7.10*** | ||||||||||
| Fear of COVID-19 | 0.10 | 0.02 | 0.12 | 4.66*** | ||||||||||
| Depression | 0.44 | 0.02 | 0.49 | 19.55*** | ||||||||||
| Insomnia | 0.10 | 0.02 | 0.15 | 5.51*** | ||||||||||
B Unstandardized regression coefficient, SE Standard error, β Standardized regression coefficient; a1 = Unmarried, 2 = Married, 3 = In a relationship; b1 = Below university, 2 = University; c1 = Yes, 2 = No; d1 = Not at all, 2 = Rarely, 3 = Sometime, 4 = Often, 5 = Always; e1 = Good, 2 = Poor. *p < 0.05, **p < 0.01, ***p < 0.001
Depression
The prevalence estimate of moderate to severe depression was 46.4%. Depression was positively associated with decreased household income due to COVID-19, presence of food scarcity, more sleep, loneliness, and anxiety (Table 5). The regression model predicted 49% of the variance in depression [F(14,989) = 49.31; p < 0.001].
Table 5.
Hierarchical regression analysis predicting depression
| Variables | Model 1 | Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | t | B | SE | β | t | B | SE | β | t | ΔR2 | R2Adj | |
| Block 1 - Socio-demographics (F(4,999) = 9.99; p < 0.001) | 0.04 | 0.04 | ||||||||||||
| Marital statusa | 0.73 | 0.28 | 0.08 | 2.64** | 0.72 | 0.28 | 0.08 | 2.55* | 0.37 | 0.23 | 0.04 | 1.64 | ||
| Educationb | −0.89 | 0.43 | −0.07 | −2.06* | −0.92 | 0.43 | −0.07 | −2.13* | −0.64 | 0.34 | −0.05 | −1.86 | ||
| Chronic health conditionsc | −1.51 | 0.42 | −0.11 | −3.61*** | −1.66 | 0.42 | −0.12 | −3.96*** | − 0.41 | 0.34 | − 0.03 | − 1.19 | ||
| Self-reported health statusd | 0.93 | 0.33 | 0.09 | 2.83** | 0.67 | 0.38 | 0.06 | 1.76 | 0.00 | 0.31 | 0.00 | 0.00 | ||
| Block 2 – Lifestyle factors (F(10,993) = 6.39; p < 0.001) | 0.02 | 0.05 | ||||||||||||
| Decreased household income due to COVID-19c | − 0.76 | 0.38 | −0.07 | −2.01* | − 0.63 | 0.30 | − 0.06 | − 2.10* | ||||||
| Unemployment of family members due to COVID-19c | −0.59 | 0.39 | −0.06 | −1.52 | −0.24 | 0.31 | −0.02 | − 0.78 | ||||||
| Food scarcityc | 0.15 | 0.41 | 0.01 | 0.38 | 0.69 | 0.33 | 0.07 | 2.11* | ||||||
| Average sleep durationd | 0.25 | 0.24 | 0.03 | 1.06 | 0.47 | 0.19 | 0.06 | 2.40* | ||||||
| Internet browsing hourse | 0.59 | 0.16 | 0.11 | 3.60*** | 0.21 | 0.13 | 0.04 | 1.54 | ||||||
| Self-reported quality of lifef | 0.19 | 0.39 | 0.02 | 0.49 | −0.39 | 0.31 | −0.04 | −1.25 | ||||||
| Block 3 – Psychiatric symptoms (F(14,989) = 49.31; p < 0.001) | 0.35 | 0.40 | ||||||||||||
| Loneliness | 0.19 | 0.08 | 0.07 | 2.29* | ||||||||||
| Fear of COVID-19 | 0.04 | 0.02 | 0.05 | 1.74 | ||||||||||
| Anxiety | 0.64 | 0.03 | 0.57 | 19.48*** | ||||||||||
| Insomnia | 0.01 | 0.02 | 0.01 | 0.27 | ||||||||||
B Unstandardized regression coefficient, SE Standard error, β Standardized regression coefficient; a1 = Unmarried, 2 = Married, 3 = In a relationship; b1 = Below university, 2 = University; c1 = Yes, 2 = No; d1 = < 7 hours, 2 = 7–9 hours, 3 = > 9 hours; e1 = < 2 hours, 2 = 2–4 hours, 3 = 4–6 hours, 4 = > 6 hours; f1 = Good, 2 = Poor. *p < 0.05, **p < 0.01, ***p < 0.001
Insomnia
The prevalence estimate of insomnia was 50.7%. Among those with insomnia, estimates of subthreshold, moderate, and severe insomnia were 37.8, 17.1, and 4.7%, respectively. Insomnia was positively associated with higher monthly income, chronic health conditions, worries regarding COVID-19 infection, not having prolonged home quarantine, joblessness of family members due to COVID-19, food scarcity, less sleep, alcohol consumption, loneliness, anxiety, and fear of COVID-19 (Table 6). The regression model predicted 32% of the variance in insomnia [F(19,984) = 26.22; p < 0.001].
Table 6.
Hierarchical regression analysis predicting insomnia
| Variables | Model 1 | Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | t | B | SE | β | t | B | SE | β | t | ΔR2 | R2Adj | |
| Block 1 - Socio-demographics (F(4,999) = 21.45; p < 0.001) | 0.08 | 0.08 | ||||||||||||
| Age | 0.03 | 0.08 | 2.44* | 0.02 | 0.03 | 0.03 | 0.77 | 0.01 | 0.03 | 0.01 | 0.36 | |||
| Monthly household incomea | 0.19 | 0.14 | 4.61*** | 0.86 | 0.19 | 0.14 | 4.51*** | 0.80 | 0.17 | 0.13 | 4.60*** | |||
| Chronic health conditionsb | 0.53 | −0.17 | −5.42*** | −3.02 | 0.52 | −0.18 | −5.78*** | −1.94 | 0.48 | −0.11 | −4.02*** | |||
| Self-reported health statusc | 0.42 | 0.14 | 4.64*** | 0.92 | 0.46 | 0.07 | 2.00* | 0.44 | 0.42 | 0.03 | 1.05 | |||
| Block 2 – Lifestyle factors (F(15,988) = 16.52; p < 0.001) | 0.12 | 0.19 | ||||||||||||
| Worry due to COVID-19b | −2.07 | 0.44 | −0.14 | −4.69*** | −1.16 | 0.42 | −0.08 | −2.74** | ||||||
| Prolonged home quarantineb | 2.35 | 0.50 | 0.14 | 4.70*** | 1.98 | 0.46 | 0.12 | 4.32*** | ||||||
| Unemployment of family members due to COVID-19b | −1.44 | 0.47 | −0.10 | −3.05** | −1.19 | 0.43 | −0.09 | −2.75** | ||||||
| Food scarcityb | −1.49 | 0.48 | −0.11 | −3.11** | −1.17 | 0.44 | −0.09 | −2.69** | ||||||
| Average sleep durationc | −1.59 | 0.29 | −0.16 | −5.52*** | −1.44 | 0.27 | −0.15 | −5.44*** | ||||||
| Physical exerciseb | 1.31 | 0.40 | 0.10 | 3.31** | 0.66 | 0.37 | 0.05 | 1.81 | ||||||
| Internet browsing hoursd | 0.78 | 0.24 | 0.12 | 3.20** | 0.41 | 0.22 | 0.06 | 1.83 | ||||||
| Social media usee | 0.49 | 0.23 | 0.08 | 2.15* | 0.40 | 0.21 | 0.06 | 1.92 | ||||||
| Tobacco smokingb | 0.36 | 0.53 | 0.02 | 0.67 | 0.11 | 0.48 | 0.01 | 0.22 | ||||||
| Alcohol consumptionb | −1.99 | 0.81 | −0.08 | −2.46* | −1.59 | 0.74 | −0.06 | −2.14* | ||||||
| Self-reported quality of lifef | 1.30 | 0.47 | 0.09 | 2.75** | 0.53 | 0.44 | 0.04 | 1.21 | ||||||
| Block 3 – Psychiatric symptoms (F(19,984) = 26.22; p < 0.001) | 0.14 | 0.32 | ||||||||||||
| Loneliness | 0.79 | 0.11 | 0.22 | 7.11*** | ||||||||||
| Fear of COVID-19 | 0.13 | 0.03 | 0.11 | 3.85*** | ||||||||||
| Anxiety | 0.27 | 0.05 | 0.19 | 5.18*** | ||||||||||
| Depression | 0.03 | 0.04 | 0.02 | 0.70 | ||||||||||
B Unstandardized regression coefficient, SE Standard error, β Standardized regression coefficient; a1 = < 20,000, 2 = 20,000-30,000, 3 = 30,000-40,000, 4 = > 40,000; b1 = Yes, 2 = No; c1 = < 7 hours, 2 = 7–9 hours, 3 = > 9 hours; d1 = < 2 hours, 2 = 2–4 hours, 3 = 4–6 hours, 4 = > 6 hours; e1 = Not at all, 2 = Rarely, 3 = Sometime, 4 = Often, 5 = Always; f1 = Good, 2 = Poor. *p < 0.05, **p < 0.01, ***p < 0.001
Fear of COVID-19
The mean FCV-19S score was 17.84 (SD = 5.69). Fear of COVID-19 was positively associated with older age, COVID-19-related worries, and employment of family members, COVID-19 news exposure, anxiety, depression, and insomnia (Table 7). The regression model predicted 22% of the variance in fear of COVID-19 [F(15,988) = 20.12; p < 0.001].
Table 7.
Hierarchical regression analysis predicting fear of COVID-19
| Variables | Model 1 | Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | t | B | SE | β | t | B | SE | β | t | ΔR2 | R2Adj | |
| Block 1 - Socio-demographics (F(3,1000) = 13.01; p < 0.001) | 0.04 | 0.04 | ||||||||||||
| Age | 0.12 | 0.03 | 0.17 | 4.99*** | 0.08 | 0.03 | 0.11 | 3.25** | 0.07 | 0.02 | 0.09 | 2.66** | ||
| Marital statusa | 0.46 | 0.33 | 0.05 | 1.41 | 0.60 | 0.31 | 0.06 | 1.93 | 0.43 | 0.30 | 0.05 | 1.45 | ||
| Monthly household incomeb | 0.01 | 0.17 | 0.00 | 0.04 | −0.02 | 0.17 | 0.00 | −0.13 | −0.14 | 0.16 | −0.03 | −0.86 | ||
| Block 2 – Lifestyle factors (F(11,992) = 15.86; p < 0.001) | 0.12 | 0.14 | ||||||||||||
| Worry due to COVID-19c | −3.37 | 0.39 | −0.27 | −8.74*** | −3.04 | 0.37 | −0.25 | −8.22*** | ||||||
| Decreased household income due to COVID-19c | 0.21 | 0.40 | 0.02 | 0.53 | 0.27 | 0.38 | 0.02 | 0.72 | ||||||
| Unemployment of family members due to COVID-19c | 0.56 | 0.41 | 0.05 | 1.36 | 0.94 | 0.39 | 0.08 | 2.39* | ||||||
| Food scarcityc | −0.99 | 0.44 | −0.09 | −2.26* | −0.74 | 0.42 | −0.06 | −1.75 | ||||||
| Average sleep durationd | −0.64 | 0.25 | −0.08 | −2.53* | − 0.44 | 0.25 | − 0.05 | −1.80 | ||||||
| Internet browsing hourse | 0.13 | 0.21 | 0.02 | 0.61 | −0.11 | 0.20 | −0.02 | − 0.55 | ||||||
| Social media usef | −0.22 | 0.20 | −0.04 | −1.12 | − 0.20 | 0.19 | − 0.04 | − 1.07 | ||||||
| COVID-19 news exposurec | −1.46 | 0.36 | −0.12 | −4.05*** | −1.51 | 0.34 | −0.13 | −4.41*** | ||||||
| Block 3 – Psychiatric symptoms (F(15,988) = 20.12; p < 0.001) | 0.08 | 0.22 | ||||||||||||
| Loneliness | −0.09 | 0.10 | −0.03 | − 0.91 | ||||||||||
| Anxiety | 0.21 | 0.05 | 0.17 | 4.26*** | ||||||||||
| Depression | 0.11 | 0.04 | 0.10 | 2.73** | ||||||||||
| Insomnia | 0.11 | 0.03 | 0.13 | 4.00*** | ||||||||||
B Unstandardized regression coefficient, SE Standard error, β Standardized regression coefficient; a1 = Unmarried, 2 = Married, 3 = In a relationship; b1 = < 20,000, 2 = 20,000-30,000, 3 = 30,000-40,000, 4 = > 40,000; c1 = Yes, 2 = No; d1 = < 7 hours, 2 = 7–9 hours, 3 = > 9 hours; e1 = < 2 hours, 2 = 2–4 hours, 3 = 4–6 hours, 4 = > 6 hours; f1 = Not at all, 2 = Rarely, 3 = Sometime, 4 = Often, 5 = Always. *p < 0.05, **p < 0.01, ***p < 0.001
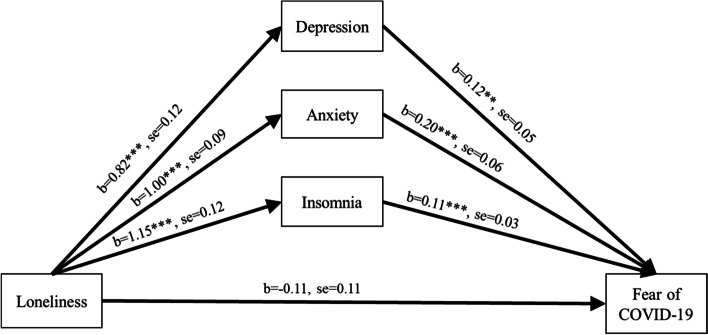
Figure 1 depicts the path coefficients of the indirect relationships between loneliness and fear of COVID-19 through insomnia, anxiety, and depression. The model variables accounted for significant variance in fear of COVID-19 [R2 = 0.25, F(25, 978) = 14.71, p < 0.001]. Loneliness was associated with greater levels of insomnia, anxiety, and depression (all p < 0.001), which in turn, were associated with greater fear of COVID-19 at the p < 0.001 level, except for depression (p = 0.01). Loneliness had significant indirect effects on fear of COVID-19 through insomnia (b = 0.13, se = 0.04, CI = 0.06–0.21), anxiety (b = 0.20, se = 0.05, CI = 0.09–0.31), and depression (b = 0.10, se = 0.04, CI = 0.03–0.18). Additionally, the association between loneliness and fear of COVID-19 (b = 0.32, se = 0.10, p < 0.001) reduced to non-significance upon adding mediating variables (b = − 0.11, se = 0.11, p = 0.30). Hence, insomnia, anxiety, and depression mediated the relationship between loneliness and fear of COVID-19.
Fig. 1.
Depression, anxiety, and insomnia mediate the relationship between loneliness and fear of COVID-19. Note: Results of mediation analysis depicting coefficients, standard error (se), and significance of associations. Mediation analysis controlled for socio-demographics and lifestyle factors. *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001. The significant relationship between loneliness and fear of COVID-19 was no longer significant in the mediation model outlined above, indicating that insomnia, anxiety and depression mediated the relationship between loneliness and fear of COVID-19
Discussion
The COVID-19 pandemic has been deemed by some as the world’s most disastrous crisis, and considerable psychological concerns have been reported among people of all ages [51–53]. Investigation into the psychological burdens due to this pandemic (with respect to psychiatric disorders and less severe manifestations) is important in considering interventions to promote mental health and well-being [54]. The present study investigated the prevalence of psychiatric symptomatology and associated factors among Bangladeshi individuals approximately 1 year following the COVID-19 outbreak. We observed high levels of loneliness, depression, anxiety, insomnia, and fear of COVID-19 that were interrelated and associated with specific health correlates.
The prevalence estimate of loneliness was 63.5% in the present study, which indicates a higher prevalence of loneliness among Bangladeshi general people, and this is consistent with a previous study that also found a higher prevalence of loneliness (71%) among Bangladeshi general people during this COVID-19 pandemic [55]. This is plausible due to the fact that social isolation during the COVID-19 pandemic is a risk factor for loneliness according to a previous study [56]. However, similar surveys during the COVID-19 pandemic among the citizens of Canada [57] and the United Kingdom [12] found prevalence estimates of loneliness of 34.8% and 27%, respectively. This discrepancy may be related to the methods used in assessing the loneliness symptoms. Loneliness was more prevalent in women than in men in the current study, consistent with findings from other countries during the COVID-19 pandemic [58, 59]. Women with fewer integrated, cohesive groups of friends have reported feeling more lonely than men [60], and gender-related factors promoting loneliness during the COVID-19 warrant more study. Loneliness associated with COVID-19 has previously been linked to higher levels of psychological distress and poorer quality of life [61], consistent with the present findings. Loneliness was also associated with frequent internet use, similar to findings among Italian adults [43]. Loneliness was also found to be linked to the high-frequency use of social media (e.g., Facebook) in the present study, similar to findings from other investigations [62]. Loneliness is also connected to psychiatric symptomatology including anxiety and depression. Increased loneliness resulting from spatial distancing efforts during the COVID-19 pandemic may constitute a serious concern that may contribute to increases in depression and anxiety [63, 64], and this possibility warrants additional investigation.
The prevalence of moderate to severe anxiety was 26.3%. Banna et al. found that the prevalence of anxiety symptoms among Bangladeshi adults during an earlier stage of the COVID-19 pandemic was 33.7% [15]. In the present study, anxiety symptoms were particularly prevalent among older individuals. Similar findings were found in prior COVID-19 research in Bangladesh [15, 24]. This finding may be attributed to anxiety regarding the higher COVID-19 death rate among older people [24]. However, other data suggest that older adults may be more resilient to anxiety, depression, and stress-related mental health disorders [65, 66]. Anxiety was also associated with loneliness in the current study. In line with previous findings, loneliness due to social distancing during the COVID-19 pandemic was the main factor linked to depression and anxiety [63]. The results underscore that loneliness during pandemic situations may have a notable psychiatric impact. Accordingly, policymakers and mental health practitioners should emphasize the importance of safe social interactions while remaining connected [67]. Moreover, anxiety was linked to insomnia, in line with previous studies [68, 69]. In Italy, anxiety related to COVID-19 was associated with disturbed sleep [70]. Moreover, a study conducted among Swedish general people that suggests a bidirectional relationship between anxiety (and depression) and insomnia [71].
The present study found slightly less than half of the participants (46.4%) were suffering from moderate to severe depression. A prior Bangladeshi study found a considerably higher percentage earlier in the pandemic [15]. Presently, depression is associated with decreased household income due to COVID-19. Lower levels of household income have been associated with psychological distress [72]. Consistent with the current findings, food insecurity during the COVID-19 pandemic has been linked to mental health issues such as anxiety and depression, and the impact of food insecurity has been estimated to be three times that of joblessness during the pandemic [73]. Excessive sleep during the COVID-19 pandemic was also associated with depression. This finding aligns with a prior Bangladeshi longitudinal study [36] and other findings [74] but appears to contrast with another prior Bangladeshi report [75] that observed no association between hours of sleep and depression. Loneliness was also significantly associated with depression. A recent review suggests loneliness has been elevated during the COVID-19 pandemic, with 43% of respondents scoring above validated thresholds, and has been strongly associated with depression and suicidal ideation [64].
In the current study, prevalence estimates of subthreshold, moderate, and severe insomnia were 37.8%, 17.1%, and 4.7%, respectively, which are similar to those from a prior Bangladeshi study [14]. Consistent with other studies, this study found that participants with chronic conditions had elevated odds of insomnia [14, 76]. Insomnia has been linked to worries about COVID-19 infection previously in Greek and French populations [77, 78], and sleep patterns and quality may also relate to worries about contamination and financial concerns [77]. Insomnia in this study was linked with not having prolonged home quarantine. The COVID-19 situation, in which people were often compelled to perform work or study at home, with accompanying concerns about health risks and social isolation, has been associated with disrupted sleep patterns [79]. According to the findings of this study, participants with family members who lost jobs during the pandemic had higher odds of insomnia. Because losing a job often generates a great deal of insecurity in terms of earning a living, insomnia may develop [80]. Alcohol consumption is also paired with insomnia in this study. Aoyama et al. [81] found that alcohol intake was associated with insomnia. Not surprisingly, reduced sleep duration was associated with insomnia. While the emergence of sleep disturbances in response to stressful life events is to be expected, contrary findings exist. Li et al. [82] found an increase in total sleep time and a decrease in overall sleep quality among people during the COVID-19 pandemic. Loneliness was linked to insomnia among the current participants. Loneliness may induce increased feelings of vulnerability, thereby increasing arousal, and generating insomnia [78].
This study’s mean FCV-19S score was 17.84, comparable to a Bangladeshi study conducted earlier during the COVID-19 pandemic, which revealed a mean score of 18.53 [83]. In the current study, older people were more likely to be fearful of COVID-19. This is unsurprising given that older people are more susceptible to mortality and disability as a result of COVID-19 [84]. Consequently, they may be more fearful of contracting the disease [85, 86]. Participants in this study who were more worried about COVID-19 infection were more likely to be fearful of COVID-19. A prior study reported a high level of worry as being associated with increased anxiety and fear of COVID-19 [87]. In the current study, participants with family members still working during the pandemic were more fearful of contracting the virus. Since the majority of people who continued working during COVID-19 were more likely to go outside of the house, they may have been considered more prone to becoming infected with COVID-19 and spreading it to family members [88]. Additionally, participants who had been exposed to COVID-19 news on a regular basis were more likely to report higher levels of fear of COVID-19. This finding may reflect information and possible misinformation about COVID-19 having been spread through various media outlets, possibly generating widespread fear among the public [89]. The present study also found that anxiety and depression were associated with fear of COVID-19. Similarly, an Israeli study found that anxiety, stress, and depression were associated with fear of COVID-19 [90]. It is also evident that the presence of fear is associated with the occurrence of sleep problems and as such, the fear related to COVID-19 appears to be the same [14]. Stress may lead to insomnia and other psychological problems [91].
In the present study, anxiety, depression, and insomnia also mediated the relationship between loneliness and fear of COVID-19. The relationship between loneliness and fear of COVID-19 is consistent with prior reports [92, 93]. The correlations between loneliness and anxiety/depression/insomnia, and between anxiety/depression/insomnia and fear of COVID-19 have also been documented separately [61, 63, 64, 78, 90, 91]. However, the relationship between loneliness and fear of COVID-19, as mediated by anxiety, depression, and insomnia, is novel and suggests possible etiological factors that may be targeted in interventions aimed at reducing fear of COVID-19. The extent to which such pathways may extend to fears of other illnesses warrants additional direct examination, as does the investigated pathway in longitudinal data.
Limitations
Study limitations warrant consideration. First, this study used a cross-sectional design; thus, causality cannot be established. Longitudinal studies would help in this regard. Second, responses were self-reported and may be subject to biases and tendencies to report socially desirable responses. Third, the use of online for surveying respondents is prone to selection bias due to the necessity of having internet access to participate. Finally, the sample was largely composed of single individuals with a high level of education and low medical comorbidity, so results might not generalize or represent an accurate reflection of the whole Bangladeshi population or groups from other jurisdictions.
Conclusions
In summary, our findings suggest that the COVID-19 pandemic may be having longer-term psychological impacts on Bangladeshi people. Loneliness, anxiety, depression, and insomnia were frequently acknowledged, and considerable levels of fear of COVID-19 were observed. Although these domains appear correlated, specific socio-demographic and lifestyle-related factors were observed to link to specific aspects of mental health. One year into the COVID-19 pandemic, special attention may be needed to protect the mental health of potentially vulnerable populations including older adults, women, people with frequent internet users, and those who are worried about COVID-19 infection. Since a pandemic like COVID-19 has the potential to exacerbate social disparities in psychological health in subtle ways, authorities and health systems should consider developing national guidelines for dealing with psychological distress during and after the COVID-19 pandemic. Better preparedness for infectious disease outbreaks, including investment in psychiatric interventions and the use of validated instruments to assist in the identification and helping of at-risk individuals, may foster resilience and enhance public safety during events like the COVID-19 pandemic.
Supplementary Information
Additional file 1. Questionnaire: General psychiatric symptoms among Bangladeshi people approximately 1 year after the onset of the COVID-19 pandemic.
Acknowledgments
The authors would like to express the most profound gratitude to all of the respondents who participated in this study voluntarily and spontaneously. Furthermore, the authors wish to express their sincere appreciation for the contributions and assistance of Liva Haque, Saida Mahmuda Rahman, Md. Al Amin, Nayma Ahmmed, Jannatul Mawa, Sangita Chakraborty, Ikram Hossen, Alvi Nitul, Naimur Rahman, Sharmin Akter Shathi, Sheikh Hafsa Boqul, Tashdika Mahdi, Shehab Uddin, Anisa Ibnat, Md. Zillur Rahman, Md. Tafazzal Hossain for their contribution to data collection.
Abbreviations
- COVID-19
Coronavirus disease-2019
- CHERRIES
Checklist for Reporting Results of Internet ESurveys
- BDT
Bangladeshi Taka
- SRH
Self-rated health status
- SQL
Self-reported quality of life
- UCLA
University of California, Los Angeles
- GAD-7
Generalized Anxiety Disorder
- PHQ-9
Patient Health Questionnaire
- ISI
Insomnia Severity Index
- FCV-19S
Fear of COVID-19 Scale
- SPSS
Statistical Package for the Social Sciences
- ANOVA
Analysis of variance
- CIs
Confidence intervals
- SD
Standard deviation
Authors’ contributions
RB: Conceptualization, Methodology, Investigation, Data curation, Results interpretation, Writing - original draft, Editing, Validation., MSI: Conceptualization, Methodology, Investigation, Data curation, Formal analysis, Results interpretation, Writing - original draft, Editing, Validation., MA: Writing - original draft, Validation., KNK: Editing, Validation., MM: Editing, Validation., MR: Investigation, Editing, Validation., ZWZ: Formal analysis, Writing - original draft, Editing, Validation., MTS: Supervision, Investigation, Editing, Validation., MNP: Writing - original draft, Editing, Validation. All authors have read and approved the manuscript.
Funding
The authors didn’t receive any grants or remunerations from either public or private organizations or other funding agencies.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Institutional Research Ethics guidelines and ethical guidelines involving human participation (i.e., Helsinki Declaration). Formal ethics approval was granted by the Biosafety, Biosecurity, and Ethical review board of the Jahangirnagar University, Savar, Dhaka-1342, Bangladesh [BBEC, JU/M 2020/COVID-19/(11)2]. All participants provided their informed consent to participate in the study after being informed about the purpose of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the publication of this research output. Dr. Potenza has consulted for and advised Opiant Pharmaceuticals, Idorsia Pharmaceuticals, AXA, Game Day Data, and the Addiction Policy Forum; has received research support from the Mohegan Sun Casino, Connecticut Council on Problem Gambling, and National Center for Responsible Gaming; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; has contributed to a patent application for gambling and gaming disorder treatment, and has consulted for law offices and gambling entities on issues related to impulse control or addictive disorders.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rajon Banik, Email: rajonbanik.phi.ju@gmail.com.
Md. Saiful Islam, Email: islam.msaiful@outlook.com.
Masruk Ahmed, Email: ahmedrudro9@gmail.com.
Kamrun Nahar Koly, Email: koly@icddrb.org.
Mahfuza Mubarak, Email: mahfuza@juniv.edu.
Mahmudur Rahman, Email: mahmudur.rahman@juniv.edu.
Zu Wei Zhai, Email: zuweizhai@gmail.com.
Md. Tajuddin Sikder, Email: sikder@juniv.edu.
Marc N. Potenza, Email: marc.potenza@yale.edu
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organization WH. WHO coronavirus (COVID-19) dashboard. 2021. [Google Scholar]
- 5.Wang L, Wang Y, Ye D, Liu Q. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int J Antimicrob Agents. 2020;55:105948. doi: 10.1016/j.ijantimicag.2020.105948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Organization WH . Mental health and psychosocial considerations during the COVID-19 outbreak. 2020. [Google Scholar]
- 7.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 8.Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatr. 2020;51:101990. doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho SC, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. [DOI] [PMC free article] [PubMed]
- 10.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mamun MA, Sakib N, Gozal D, Israfil AKM, Hossain S, Al F, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J Affect Disord. 2020;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Groarke JM, Berry E, Graham-wisener L, Mckenna- PE, Mcglinchey E, Armour C. Loneliness in the UK during the COVID-19 pandemic : cross-sectional results from the COVID-19 psychological wellbeing study. PLoS One. 2020;15:e0239698. doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mistry SK, Ali ARMM, Akther F, Yadav UN, Harris MF. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Glob Health. 2021;17:47. doi: 10.1186/s12992-021-00698-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mamun F, al, Gozal D, Hosen I, Mawa J, Mamun MA. Predictive factors of insomnia during the COVID-19 pandemic in Bangladesh: a GIS-based nationwide distribution. Sleep Med. 2022;91:219-25. [DOI] [PMC free article] [PubMed]
- 15.Al BMH, Sayeed A, Kundu S, Christopher E, Hasan MT, Begum MR, et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. Int J Environ Health Res. 2020:1–12. 10.1080/09603123.2020.1802409. [DOI] [PubMed]
- 16.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Person B, Sy F, Holton K, Govert B, Liang A. Team NC for IDCO. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. 2004;10:358–363. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orhan M, Korten N, Paans N, de Walle B, Kupka R, van Oppen P, et al. Psychiatric symptoms during the COVID-19 outbreak in older adults with bipolar disorder. Int J Geriatr Psychiatry. 2021;36:892-900. [DOI] [PubMed]
- 20.Banik R, Rahman M, Sikder MT, Gozal D. COVID-19 in Bangladesh: public awareness and insufficient health facilities remain key challenges. Public Health. 2020;183:50–51. doi: 10.1016/j.puhe.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization . WHO coronavirus (COVID-19) dashboard-Bangladesh situation. 2022. [Google Scholar]
- 22.Islam SMD-U, Bodrud-Doza M, Khan RM, Haque MA, Mamun MA. Exploring COVID-19 stress and its factors in Bangladesh: a perception-based study. Heliyon. 2020;6:e04399. doi: 10.1016/j.heliyon.2020.e04399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakib N, Akter T, Zohra F, Bhuiyan AKMI. Fear of COVID-19 and Depression : a comparative study among the general population and healthcare professionals during COVID-19 pandemic crisis in Bangladesh. Int J Ment Health Addict. 2021;36(6):892-900. [DOI] [PMC free article] [PubMed]
- 24.Islam MS, Ferdous MZ, Potenza MN. Panic and generalized anxiety during the COVID-19 pandemic among Bangladeshi people: an online pilot survey early in the outbreak. J Affect Disord. 2020;276:30–37. doi: 10.1016/j.jad.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. J Affect Disord. 2020;277:121–128. doi: 10.1016/j.jad.2020.07.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeasmin S, Banik R, Hossain S, Hossain MN, Mahumud R, Salma N, et al. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: a cross-sectional study. Child Youth Serv Rev. 2020;117:105277. doi: 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.New Age . South Asia new epicentre of COVID-19 pandemic: IFRC. 2021. [Google Scholar]
- 28.Bangladesh Bureau of Statistics (BBS) Bangladesh statistics 2019. 2019. [Google Scholar]
- 29.Ministry of Finance B . Bangladesh economic review 2022. 2022. [Google Scholar]
- 30.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J Med Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahmed MS, Sen L, Griffiths M. Association between self-rated health and quality of life with sleep quality among Bangladeshi university students. Soc Heal Behav. 2020;3:35–37. doi: 10.4103/SHB.SHB_15_20. [DOI] [Google Scholar]
- 32.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Debnath PR, Islam MS, Karmakar PK, Sarker R, Zhai ZW, Potenza MN. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a Large Tertiary Care Hospital in Bangladesh. Int J Ment Health Addict. 2021;1-21. [DOI] [PMC free article] [PubMed]
- 35.Spitzer RL, Kroenke K, Williams JBW, Lo B. A brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 36.Hossain S, Anjum A, Uddin ME, Rahman MA, Hossain MF. Impacts of socio-cultural environment and lifestyle factors on the psychological health of university students in Bangladesh: a longitudinal study. J Affect Disord. 2019;256:393–403. doi: 10.1016/j.jad.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 37.Rahman ME, Islam MS, Mamun MA, Moonajilin MS, Yi S. Prevalence and factors associated with suicidal ideation among university students in Bangladesh. Arch Suicide Res. 2020:1–10. 10.1080/13811118.2020.1833800. [DOI] [PubMed]
- 38.Islam MS, Rahman ME, Moonajilin MS, van Os J. Prevalence of depression, anxiety and associated factors among school going adolescents in Bangladesh: findings from a cross-sectional study. PLoS One. 2021;16:e0247898. doi: 10.1371/journal.pone.0247898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chowdhury A, Ghosh S, Sanyal D. Bengali adaptation of brief patient health questionnaire for screening depression at primary care. J Indian Med Assoc. 2004;102:544–547. [PubMed] [Google Scholar]
- 41.Islam MS, Rahman ME, Moonajilin MS, Griffiths MD. Validation and evaluation of the psychometric properties of Bangla nine-item internet disorder scale–short form. J Addict Dis. 2020;38:540–549. doi: 10.1080/10550887.2020.1799134. [DOI] [PubMed] [Google Scholar]
- 42.Moonajilin MS, Rahman ME, Islam MS. Relationship between overweight/obesity and mental health disorders among Bangladeshi adolescents: a cross-sectional survey. Obes Med. 2020;18:100216.
- 43.Boursier V, Gioia F, Musetti A, Schimmenti A. Facing loneliness and anxiety during the COVID-19 isolation : the role of excessive social media use in a sample of Italian adults. 2020. pp. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhuiyan AKMI, Hossain S, Abdullah AH, Sarker A, Rayhan I, Sikder T, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J Affect Disord. 2021;279:462-72. [DOI] [PMC free article] [PubMed]
- 45.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 46.Koly KN, Khanam MI, Islam MS, Mahmood SS, Hanifi SMA, Reidpath DD, et al. Anxiety and insomnia among urban slum dwellers in Bangladesh: the role of COVID-19 and its associated factors. Front Psych. 2021;12:769048. doi: 10.3389/fpsyt.2021.769048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2022;20:1537-45. [DOI] [PMC free article] [PubMed]
- 49.Sakib N, Bhuiyan AKMI, Hossain S, Al Mamun F, Hosen I, Abdullah AH, et al. Psychometric validation of the Bangla fear of COVID-19 scale: confirmatory factor analysis and Rasch analysis. Int J Ment Health Addict. 2020;1-12. [DOI] [PMC free article] [PubMed]
- 50.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford publications; 2017. [Google Scholar]
- 51.Alam MK, Bin AF, Banik R, Yasmin S, Salma N. Assessing the mental health condition of home-confined university level students of Bangladesh due to the COVID-19 pandemic. J Public Health. 2022;30:1685-92. [DOI] [PMC free article] [PubMed]
- 52.Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mamun MA, Sakib N, Gozal D, Israfil AKM, Hossain S, Al F, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh : a population-based nationwide study. J Affect Disord. 2021;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zixin L, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291:113267. doi: 10.1016/j.psychres.2020.113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Das R, Hasan MR, Daria S, Islam MR. Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open. 2021;11:e045727. doi: 10.1136/bmjopen-2020-045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dahlberg L. Loneliness during the COVID-19 pandemic. Aging Ment Health. 2021;25:1161–1164. doi: 10.1080/13607863.2021.1875195. [DOI] [PubMed] [Google Scholar]
- 57.Savage RD, Wu W, Li J, Lawson A, Bronskill SE, Chamberlain SA, et al. Loneliness among older adults in the community during COVID-19: a cross-sectional survey in Canada. BMJ Open. 2021;11:e044517. doi: 10.1136/bmjopen-2020-044517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bu F, Steptoe A, Fancourt D. Social Science & Medicine Loneliness during a strict lockdown : trajectories and predictors during the COVID-19 pandemic in 38 , 217 United Kingdom adults. Soc Sci Med. 2020;265:113521. doi: 10.1016/j.socscimed.2020.113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown ? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–34. doi: 10.1016/j.puhe.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stokes J, Levin I. Gender differences in predicting loneliness from social network characteristics. J Pers Soc Psychol. 1986;51:1069–1074. doi: 10.1037/0022-3514.51.5.1069. [DOI] [PubMed] [Google Scholar]
- 61.Horesh D, Lev-ari RK, Hasson-ohayon I. Risk factors for psychological distress during the COVID-19 pandemic in Israel: loneliness, age, gender, and health status play an important role. Br J Health Psychol. 2020;25:925–33. [DOI] [PMC free article] [PubMed]
- 62.Primack BA, Shensa A, Sidani JE, Whaite EO, Lin L, Rosen D, et al. Social media use and perceived social isolation among young adults in the U.S. Am J Prev Med. 2017;53:1–8. doi: 10.1016/j.amepre.2017.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hoffart A, Johnson SU, Ebrahimi OV. Loneliness and social distancing during the COVID-19 pandemic : risk factors and associations with psychopathology. Front Psych. 2020;11:589127. doi: 10.3389/fpsyt.2020.589127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Killgore WDS, Cloonen SA, Taylor EC, Dailey NS, Cloonen SA, Taylor EC. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290:113117. [DOI] [PMC free article] [PubMed]
- 65.Pearman A, Hughes ML, Smith EL, Neupert SD. Age differences in risk and resilience factors in COVID-19-related stress. J Gerontol B Psychol Sci Soc Sci. 2021;76:e38–e44. doi: 10.1093/geronb/gbaa120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Viewpoint T, Con- D. Older adults and the mental health effects of COVID-19. JAMA. 2020;324:2253–2254. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- 67.Jeste DV, Diego S, Diego S, Diego S, Lee EE, Diego S, et al. Battling the modern behavioral epidemic of loneliness suggestions for research and interventions. JAMA Psychiat. 2020;77:553–554. doi: 10.1001/jamapsychiatry.2020.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Monti JM, Monti D. Sleep disturbance in generalized anxiety disorder and its treatment. Sleep Med Rev. 2000;4:263–276. doi: 10.1053/smrv.1999.0096. [DOI] [PubMed] [Google Scholar]
- 69.Jansson M, Linton SJ. The role of anxiety and depression in the development of insomnia : cross- sectional and prospective analyses. Psychol Health. 2006;21:383–397. doi: 10.1080/14768320500129015. [DOI] [Google Scholar]
- 70.Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64:443–449. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 72.Id MN, Muto K, Yamamoto I. Impacts of anxiety and socioeconomic factors on mental health in the early phases of the COVID-19 pandemic in the general population in Japan : a web-based survey. PLoS One. 2021;16:e0247705. doi: 10.1371/journal.pone.0247705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fang D, Thomsen MR, Jr, RMN. The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health. 2021;21:607. doi: 10.1186/s12889-021-10631-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. 2014;18:521–529. doi: 10.1016/j.smrv.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 75.Islam MS, Akter R, Sikder MT, Griffiths MD. Weight-related status and associated predictors with psychological well-being among first-year university students in Bangladesh: a pilot study. Int J Ment Health Addict. 2022;20:1354–69.
- 76.Zhang W, Wang K, Zhao W, Xue Q. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89:242-50. [DOI] [PMC free article] [PubMed]
- 77.Kokou-Kpolou CK, Megalakak O, Laimoua D, Kousouri M. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, Holzinger B, et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I academy. J Sleep Res. 2020;29:e13052. doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 80.Ara T, Rahman MM, Hossain MA, Ahmed A. Identifying the associated risk factors of sleep disturbance during the COVID-19 lockdown in Bangladesh: a web-based survey. Front Psych. 2020;11:1–11. doi: 10.3389/fpsyt.2020.580268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Colrain LM, Nicholas CL, Baker FC. Alcohol and the sleeping brain. Handb Clin Neurol. 2014;125:415–431. doi: 10.1016/B978-0-444-62619-6.00024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li Y, Qin Q, Sun Q, Sanford LD, Vgontzas AN, Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med. 2020;16:1417–1418. doi: 10.5664/jcsm.8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hossain MA, Jahid MIK, Hossain KMA, Walton LM, Uddin Z, Haque MO, et al. Knowledge, attitudes, and fear of COVID-19 during the rapid rise period in Bangladesh. PLoS One. 2020;15:e0239646. doi: 10.1371/journal.pone.0239646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Organization WH. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020.
- 85.Parlapani E, Holeva V, Nikopoulou VA, Sereslis K, Athanasiadou M, Godosidis A, et al. Intolerance of uncertainty and loneliness in older adults during the COVID-19 pandemic. Front Psych. 2020;11:842. doi: 10.3389/fpsyt.2020.00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Powell T, Bellin E, Ehrlich AR. Older adults and Covid-19: the Most vulnerable, the hardest hit. Hastings Cent Rep. 2020;50:61–63. doi: 10.1002/hast.1136. [DOI] [PubMed] [Google Scholar]
- 87.Baiano C, Zappullo I, Conson M, Di Mauro G, Petra M, Piacenti M, et al. Tendency to worry and fear of mental health during Italy’s COVID-19 lockdown. Int J Environ Res Public Health. 2020;17:1–8. doi: 10.3390/ijerph17165928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nabe-Nielsen K, Nilsson CJ, Juul-Madsen M, Bredal C, Hansen LOP, Hansen AM. COVID-19 risk management at the workplace, fear of infection and fear of transmission of infection among frontline employees. Occup Environ Med. 2021;78:248–254. doi: 10.1136/oemed-2020-106831. [DOI] [PubMed] [Google Scholar]
- 89.Banerjee D. The COVID-19 outbreak: crucial role the psychiatrists can play. Asian J Psychiatr. 2020;50:102014. doi: 10.1016/j.ajp.2020.102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tzur Bitan D, Grossman-Giron A, Bloch Y, Mayer Y, Shiffman N, Mendlovic S. Fear of COVID-19 scale: psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020;289:113100. [DOI] [PMC free article] [PubMed]
- 91.Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kayis AR, Satici B, Deniz ME, Satici SA, Griffiths MD. Fear of COVID-19, loneliness, smartphone addiction, and mental wellbeing among the Turkish general population: a serial mediation model. Behav Inf Technol. 2021:1–13.
- 93.Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the first wave of COVID-19 outbreak. Int J Environ Res Public Health. 2021;18:2586. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Questionnaire: General psychiatric symptoms among Bangladeshi people approximately 1 year after the onset of the COVID-19 pandemic.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.