Abstract
Objective
To conduct an overview of meta-analyses evaluating the impact of exercise interventions on improving health outcomes in patients with chronic kidney disease (CKD).
Design
An umbrella review of systematic review and meta-analyses of intervention trials was performed.
Data sources
PubMed, Web of Science, Embase and the Cochrane Database of Systematic Reviews were searched from inception to 9 March 2021 for relevant articles.
Eligibility criteria for selecting studies
Eligible meta-analyses compared the effects of usual care with and without exercise in patients with CKD. Health outcomes included those related to cardiovascular risk factors, physical fitness, dialysis-related symptoms, dialysis adequacy and health-related quality of life. Systematic reviews and meta-analyses that included fewer than 3 RCTs or fewer than 100 participants were excluded from the analysis.
Results
A total of 31 eligible systematic reviews and meta-analyses were included that assessed 120 outcomes. For physical fitness, there was a moderate effect size for cardiorespiratory fitness, muscle strength and body composition and small effect size for muscle endurance. The effect sizes for cardiovascular risk factors, dialysis-related symptoms and health-related quality of life outcomes were small. According to the Grading of Recommendations Assessment, Development and Evaluation framework, most outcomes were low or very low quality.
Conclusion
Exercise appears to be a safe way to affect concomitant cardiovascular risk factors, such as blood pressure, improve physical fitness and health-related quality of life and reduce dialysis-related symptoms in patients with CKD.
PROSPERO registration number
CRD42020223591.
Keywords: nephrology, rehabilitation medicine, chronic renal failure
Strengths and limitations of this study.
A strength of this study is to comprehensively summarise the systematic review and meta-analysis of exercise interventions on the spectrum of chronic kidney disease.
Methodological quality of the included reviews was assessed using standardised measures.
The limitation of this overview is that language bias may exist in this review because the search strategy was limited to English.
Another limitation was that most studies were based on haemodialysis-dependent chronic kidney disease.
Introduction
Chronic kidney disease (CKD) is a long-term condition characterised by the gradual loss of renal function over time.1 In the past 30 years, the mortality attributed to CKD increased by 41.5%, a percentage rate that exceeds several cancers and cardiovascular diseases.2 With the increasing incidence of hypertension, diabetes and obesity, this number will continue to rise.3 4 Patients with CKD experience a high symptom burden with progressively impaired physical performance, leading to decreased kidney function, lower health-related quality of life (HRQOL), increased risk of cardiovascular events and increased all-cause mortality.5 6
With an increasing number of patients with CKD living longer, the effectiveness and accessibility of their health services have never been more critical. Renal rehabilitation is a multifaceted intervention programme. Rehabilitation consists of exercise interventions, diet control, fluid management and psychological support to alleviate physical/mental deficiencies caused by kidney disease and renal replacement therapy to improve disease prognosis and prolong life expectancy.7 Since exercise is the core of renal rehabilitation, there is an increasing number of systematic reviews and meta-analyses investigating the influence of exercise on health outcomes in patients with CKD.8
Data from large cohort studies show that mortality risk was lower for regular (equal to or more than once/week) versus non-regular (less than once/week) exercisers (adjusted HR=0.73, 95% CI: 0.69 to 0.78), and mortality risk tended to decrease as exercise frequency increased (HR for participants who exercised once/week=0.82, 95% CI: 0.73 to 0.91; HR for those who exercised 6–7 times/week=0.69, 95% CI: 0.63 to 0.76) and patients who exercised daily had lower mortality risk (HR=0.84, 95% CI: 0.74 to 0.96) than patients exercising once/week.9 Based on data from 41 randomised controlled trials (RCT), Heiwe et al reported practical improvements in aerobic capacity, muscular function and walking capacity in patients with CKD after exercise,10 indicators that are the core of frailty.11 In other words, exercise is an essential non-pharmacological strategy to improve frailty symptoms in patients with CKD, the latter being a significant cause of sedentary behaviour in such population.12 Because of this, some researchers and guidelines recommend that healthcare providers prescribe exercise for patients with CKD.13–16 However, the results of meta-analyses of exercise in patients with CKD are inconsistent.
This umbrella review aims to assess the therapeutic effects of exercise on cardiovascular risk factors, physical fitness, dialysis-related symptoms, dialysis adequacy and HRQOL in patients with CKD, summarised in systematic reviews and meta-analyses.
Methods and analysis
This umbrella review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17 The review was prospectively registered (PROSPERO: CRD42020223591), and the protocol for this review was published.18
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Literature search
A comprehensive search strategy was performed to identify systematic reviews and meta-analyses of patients with CKD that compared usual care procedures with and without exercise interventions. PubMed, Embase, the Cochrane Database of Systematic Reviews and the Web of Science were searched for systematic reviews and meta-analyses from inception to 9 March 2021. The detailed search strategy is summarised in online supplemental table S1. The references of existing systematic reviews were also screened. Any reviews considered potentially relevant by authors were retrieved for further consideration.
bmjopen-2021-054887supp002.pdf (218.4KB, pdf)
Eligibility criteria
Eligible systematic reviews and meta-analyses included those (1) where patients were diagnosed with CKD at various stages of treatment; (2) that compared exercise interventions with sham/no exercise or usual/standard care; (3) that reported outcomes on at least one of the following: cardiovascular risk factors (blood pressure), physical fitness, dialysis-related symptoms, dialysis adequacy and HRQOL. The methods to assess each outcome are shown in online supplemental figure S1 (4) systematic reviews with meta-analysis of intervention trials (RCTs and quasi-experimental studies). A meta-analysis that included fewer than 3 studies or fewer than 100 participants was excluded. For duplicate literature, the article with the most comprehensive data was selected. The language was restricted to English. Letters to the editor, trial protocols and conference abstracts were excluded.
bmjopen-2021-054887supp001.pdf (363.9KB, pdf)
Study selection
Two independent authors screened all titles and abstracts compiled from the search results. Each paper was examined for appropriate eligibility criteria, and a third author resolved disagreements.
Data extraction
Requisite data were extracted independently by two independent authors into a standardised format that included: (1) study, (2) stage of CKD, (3) the number of included studies and participants, (4) exercise type, (5) exercise mode (intradialytic or interdialytic), (6) standardised mean difference (SMD) or mean difference (MD) with corresponding 95% CI for each outcome, (7) p values, (8) I2 values and (9) exercise-related adverse events.
Risk of bias assessment
A Measurement Tool to Assess Systematic Reviews-2 (AMSTAR-2) was used to assess the risk of bias among the included systematic reviews.19 This checklist contains 16 items, and each item was answered with a ‘yes’ (1 point), ‘partial yes’ (0.5 points) or ‘no’ (0 points). The percentage score for each study was calculated using the total score as the numerator and the highest score of 16 points as the denominator. A meta-analysis scoring ≥80% was classified as high quality, 40%–79% as medium quality and those scoring <40% as low quality.20 Two authors performed the risk of bias assessment independently, and discussions resolved the disagreement.
Data analysis
The summary effect size from each meta-analysis was analysed qualitatively based on the SMD and its 95% CI for each outcome. If they were not presented as SMD in the original meta-analysis, Review Manager V.5.3 was used to convert SMD outcomes. If data could not be converted into SMD, we contacted the authors of the meta-analysis for the data. Effects were considered small (SMD <0.50), moderate (SMD from 0.50 to 0.79) and large (SMD ≥0.80).21 I2 values were interpreted as follows: ≤25% indicate low heterogeneity, 25%<I2≤50% indicate mild heterogeneity, 50%<I2≤75% indicate moderate heterogeneity and >75% indicate high heterogeneity.22
The level of evidence for each meta-analysis was evaluated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system.23 The quality of evidence was assessed using five domains: risk of bias, inconsistency, indirectness, imprecision and publication bias. Beginning with an initial score of 4 points, the score for each of these five domains was reduced accordingly: ‘not reported (−1)’, ‘serious (−1)’, ‘very serious (−2)’ or ‘neutral (0)’. Studies were rated as high (4 points), moderate (3 points), low (2 points) or very low (≤1 point) using the GRADE system. The GRADE assessment was conducted independently by two authors. Any differences were resolved by discussion or adjudication by a third author. The incidence of adverse events was based on the number of reported divided by the patients in the exercise group.
Results
Characteristics of the meta-analyses
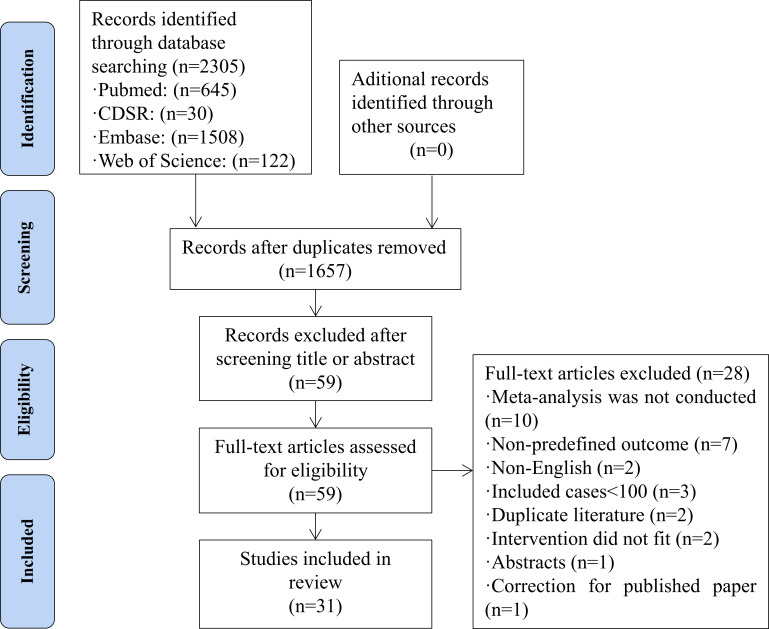
The search identified 2305 potential articles, of which 648 were duplicates. After reading the title and abstract, 1598 papers were excluded and 28 were excluded after full-text review resulting in 31 final studies.10 24–53 The PRISMA flow chart of study inclusion is illustrated in figure 1. The reasons for excluded articles are listed in online supplemental table S2.
Figure 1.
Flow chart of literature screening. CDSR, Cochrane Database of Systemic Review.
The 31 included systematic reviews and meta-analyses were published from September 2011 through March 2021. The number of included studies assessed in the articles ranged from 3 to 24, with a mean of 8 studies. The study sample sizes ranged from 106 to 874 participants, with a mean of 304. The characteristics of the included meta-analyses are shown in online supplemental table S3. SMD data from four papers could not be obtained from the authors, and the data of their effect size were presented as MD.29 30 40 46
Scores based on AMSTAR-2 ranged from 34.4% to 100.0%, with an average score of 68.0%. Seven (22.6%) systematic reviews were rated high quality, while 23 (74.2%) were rated medium quality, and just one (0.3%) was rated low quality (online supplemental table S4).
Of the GRADE evidence quality of the 120 outcomes, 1.7% (2/120) reported evidence of high quality, 17.5% (21/120) reported evidence of moderate quality, 20.0% (24/120) reported evidence of low quality and 60.8% (73/120) reported evidence of very low quality (online supplemental table S5).
Blood pressure
There were 25 meta-analyses (reported in 13 articles) investigating the effect of exercise on cardiovascular risk factors (systolic and diastolic blood pressure) in patients with CKD.10 27 30 33 34 40 41 43 46–49 52 Of which, the number of studies ranged from 3 to 12 with a mean of 314 participants (range from 198 to 514) were included in each meta-analysis (table 1).
Table 1.
Summary of the effect of exercise on cardiovascular risk factor in patients with CKD
| Study | Design | Stage of CKD | k (n)* | Exercise type | Mode | SMD or MD (95% CI) | Effect size | P value | I 2 | GRADE |
| SBP | ||||||||||
| Pei et al40 | RCT/Quasi-RCT | Mixed | 12 (514) | AE | – | MD: −2.91 (−6.68 to 0.87) | – | 0.13 | 40.0% | ⨁⨁◯◯ |
| Wu et al48 | RCT/Quasi-RCT | Predialysis | 3 (204) | AE+RT | – | SMD: −0.19 (-0.46 to 0.08) | Small | 0.16 | 50.0% | ⨁◯◯◯ |
| Chen et al27 | RCT | KTRs | 5 (198) | Mixed | – | SMD: 0.18 (-0.10 to 0.46) | Small | 0.21 | 0.0% | ⨁◯◯◯ |
| Pu et al41 | RCT | HD | 7 (287) | Mixed | Intradialytic | SMD: −0.28 (−0.52 to 0.05) | Small | 0.02 | 0.0% | ⨁◯◯◯ |
| Yamamoto et al49 | RCT | Predialysis | 10 (392) | AE | – | SMD: −0.75 (−1.24 to 0.26) | Moderate | 0.003 | 80.3% | ⨁◯◯◯ |
| Thompson et al46 | RCT | Predialysis | 10 (335) | Mixed | – | MD: −4.30 (-9.00 to 0.40) | – | N.P. | 50.4% | ⨁◯◯◯ |
| Zhang et al52 | RCT | Predialysis | 14 (463) | Mixed | – | SMD: −0.41 (−0.70 to 0.11) | Small | 0.007 | 55.0% | ⨁⨁⨁◯ |
| Huang et al34 | RCT | HD | 7 (260) | Mixed | Mixed | SMD: −0.17 (-0.41 to 0.08) | Small | 0.18 | 8.0% | ⨁⨁◯◯ |
| Heiwe et al33 | RCT/Quasi-RCT | Mixed | 9 (347) | Mixed | – | SMD: 0.25 (0.04 to 0.47) | Small | 0.02 | 0.0% | ⨁◯◯◯ |
| Heiwe and Jacobson10 | RCT | HD | 10 (312) | Mixed | – | SMD: 0.04 (-0.34 to 0.41) | Small | 0.8 | 58.0% | ⨁⸋◯ |
| Sheng et al43 | RCT | HD | 7 (296) | Mixed | Intradialytic | SMD: −0.27 (−0.50 to 0.04) | Small | 0.02 | 0.0% | ⨁◯◯◯ |
| Ferrari et al30 | RCT | HD | 10 (332) | AE | Intradialytic | MD: −10.07 (16.35 to 3.78) | – | 0.002 | 44.0% | ⨁◯◯◯ |
| Vanden Wyngaert et al47 | RCT | Predialysis | 8 (269) | AE | – | SMD: 0.08 (-0.58 to 0.74) | Small | 0.81 | 84% | ⨁◯◯◯ |
| DBP | ||||||||||
| Pei et al40 | RCT/Quasi-RCT | Mixed | 12 (514) | AE | – | MD: −1.11 (−3.41 to 1.20) | – | 0.35 | 0.0% | ⨁⨁◯◯ |
| Wu et al48 | RCT/Quasi-RCT | Predialysis | 4 (194) | AE+RT | – | SMD: −0.47 (-1.10 to 0.15) | Small | 0.14 | 70.0% | ⨁◯◯◯ |
| Chen et al27 | RCT | KTRs | 5 (198) | Mixed | – | SMD: 0.04 (-0.45 to 0.52) | Small | 0.89 | 59.0% | ⨁◯◯◯ |
| Pu et al41 | RCT | HD | 7 (287) | Mixed | Intradialytic | SMD: −0.32 (−0.55 to 0.08) | Small | 0.008 | 42.0% | ⨁◯◯◯ |
| Thompson et al46 | RCT | Predialysis | 8 (303) | Mixed | – | MD: −1.18 (-4.76 to 2.40) | – | N.P. | 60.5% | ⨁◯◯◯ |
| Zhang et al52 | RCT | Predialysis | 12 (399) | Mixed | – | SMD: −0.31 (-0.71 to 0.08) | Small | 0.12 | 70.0% | ⨁⨁◯◯ |
| Huang et al34 | RCT | HD | 7 (260) | Mixed | Mixed | SMD: −0.23 (-0.69 to 0.24) | Small | 0.34 | 68.0% | ⨁◯◯◯ |
| Heiwe et al33 | RCT/Quasi-RCT | Mixed | 11 (419) | Mixed | – | SMD: 0.16 (-0.04 to 0.36) | Small | 0.11 | 40.0% | ⨁◯◯◯ |
| Heiwe and Jacobson10 | RCT | HD | 10 (212) | Mixed | Mixed | SMD: 0.17 (-0.16 to 0.49) | Small | 0.3 | 45.0% | ⨁⨁◯◯ |
| Sheng et al43 | RCT | HD | 7 (296) | Mixed | Intradialytic | SMD: −0.24 (−0.47 to 0.01) | Small | 0.04 | 52.1% | ⨁◯◯◯ |
| Ferrari et al30 | RCT | HD | 10 (334) | AE | Intradialytic | MD: −2.96 (-7.71 to 1.78) | – | 0.22 | 0.0% | ⨁◯◯◯ |
| Vanden Wyngaert et al47 | RCT | Predialysis | 7 (237) | AE | – | SMD: −0.09 (-0.78 to 0.59) | Small | 0.79 | 83% | ⨁◯◯◯ |
Mixed means aerobic exercise combined with resistance training.
*Number of included studies and corresponding sample size.
AE, aerobic exercise; CKD, chronic kidney disease; DBP, diastolic blood pressure; GRADE, Grading of Recommendations Assessment, Development and Evaluation; HD, haemodialysis; KTRs, kidney transplant recipients; MD, mean difference; N.P., no report; RCT, randomised controlled trial; RT, resistance training; SBP, systolic blood pressure; SMD, standardised mean difference.
The effect of exercise on systolic blood pressure was investigated in 13 meta-analyses with a mild heterogeneity (average I2=36.1%),10 27 30 33 34 40 41 43 46–49 52 and 6 reported a positive statistically significant outcome.30 33 41 43 49 52 Of the 13 meta-analyses, 9 reported a small effect size10 27 33 34 41 43 47 48 52 and 1 reported moderate.49 GRADE assessment of quality indicated the overall evidence as being very low (10 meta-analyses10 27 30 33 41 43 46–49), low (2 meta-analyses34 40) and moderate (1 meta-analysis52).
The effect of exercise on diastolic blood pressure was investigated in 12 meta-analyses with a mild heterogeneity (average I2=49.1%),10 27 30 33 34 40 41 43 46–48 52 and 2 reported a positive statistically significant outcome.41 43 Of the 12 meta-analyses, 9 reported small effect sizes10 27 33 34 41 43 47 48 52 and all were graded as low or very low quality of evidence.
Cardiorespiratory fitness
There were 34 meta-analyses (reported in 21 articles) that investigated the effects of exercise on cardiorespiratory fitness in patients with CKD using a peak oxygen uptake (18 of 34), a 6 min walk test (14 of 34) or aerobic capacity (2 of 34). The meta-analyses included a mean of 9 studies (ranging from 5 to 20) and a mean of 330 participants (ranging from 179 to 504) (table 2).
Table 2.
Summary of the effect of exercise on cardiopulmonary fitness in patients with CKD
| Study | Design | Stage of CKD | k (n)* | Exercise type | Mode | SMD or MD (95% CI) | Effect size | P value | I 2 | GRADE |
| VO2 peak | ||||||||||
| Pei et al40 | RCT/Quasi-RCT | Mixed | 17 (464) | AE | – | MD: 2.08 (1.10 to 3.05) | – | <0.001 | 25.0% | ⨁⨁◯◯ |
| Nakamura et al38 | RCT/Cross-over | Predialysis | 10 (401) | Mixed | – | SMD: 0.88 (0.53 to 1.23) | Large | <0.001 | 56.0% | ⨁⨁◯◯ |
| Chen et al27 | RCT | KTRs | 6 (202) | Mixed | – | SMD: 0.33 (-0.02 to 0.69) | Small | 0.06 | 27.0% | ⨁◯◯◯ |
| Andrade et al24 | RCT | HD | 5 (201) | AE+RT | Intradialytic | SMD: 1.01 (0.71 to 1.30) | Large | <0.001 | 0.0% | ⨁⨁◯◯ |
| Chung et al28 | RCT | HD | 6 (238) | Mixed | Intradialytic | SMD: 0.55 (0.18 to 0.92) | Moderate | 0.003 | 52.9% | ⨁◯◯◯ |
| Pu et al41 | RCT | HD | 10 (400) | Mixed | Intradialytic | SMD: 0.57 (0.23 to 0.90) | Moderate | <0.001 | 59.0% | ⨁⨁◯◯ |
| Yamamoto et al49 | RCT | Predialysis | 10 (365) | AE | – | SMD: 0.54 (0.29 to 0.78) | Moderate | <0.001 | 24.6% | ⨁◯◯◯ |
| Yang et al50 | RCT | Mixed | 5 (179) | Mixed | – | SMD: 0.33 (0.03 to 0.63) | Small | 0.003 | 47.0% | ⨁⨁◯◯ |
| Huang et al34 | RCT | HD | 10 (371) | Mixed | Mixed | SMD: 0.73 (0.52 to 0.95) | Moderate | <0.001 | 71.0% | ⨁⨁◯◯ |
| Matsuzawa et al37 | RCT | HD | 18 (582) | Mixed | Mixed | SMD: 0.62 (0.38 to 0.87) | Moderate | <0.001 | 49.0% | ⨁⨁⨁⨁ |
| Smart et al44 | RCT | HD | 8 (365) | Mixed | Mixed | SMD: 0.75 (0.39 to 1.11) | Moderate | <0.001 | 60.0% | ⨁⨁◯◯ |
| Bogataj et al25 | RCT | HD | 20 (504) | Mixed | Mixed | SMD: 0.58 (0.32 to 0.85) | Moderate | <0.001 | 57.4% | ⨁◯◯◯ |
| Sheng et al43 | RCT | HD | 7 (310) | Mixed | Intradialytic | SMD: 0.53 (0.30 to 0.76) | Moderate | <0.001 | 36.0% | ⨁◯◯◯ |
| Neto et al32 | RCT | HD | 10 (394) | Mixed | Intradialytic | SMD: 0.60 (0.15 to 1.04) | Moderate | 0.008 | 76.0% | ⨁◯◯◯ |
| Ferrari et al30 | RCT | HD | 5 (201) | AE+RT | Intradialytic | MD: 5.41 (4.03 to 6.79) | – | <0.001 | 0.0% | ⨁◯◯◯ |
| Ferrari et al30 | RCT | HD | 7 (248) | AE | Intradialytic | MD: 2.07 (0.42 to 3.72) | – | <0.001 | 0.0% | ⨁◯◯◯ |
| Vanden Wyngaert et al47 | RCT | Predialysis | 11 (325) | AE | – | SMD: 0.99 (0.49 to 1.48) | Large | <0.001 | 74.0% | ⨁◯◯◯ |
| Oguchi et al39 | RCT | KTRs | 4 (182) | Mixed | – | SMD: 0.38 (-0.06 to 0.82) | Small | 0.09 | 45.0% | ⨁⨁◯◯ |
| 6MWT | ||||||||||
| Pei et al40 | RCT/Quasi-RCT | Mixed | 8 (496) | AE | – | MD: 0.04 (−0.52 to 0.59) | – | 0.90 | 86.0% | ⨁◯◯◯ |
| Nakamura et al38 | RCT/Cross-over | Predialysis | 5 (392) | Mixed | – | SMD: 1.04 (0.17 to 1.90) | Large | 0.02 | 92.0% | ⨁◯◯◯ |
| Lu et al36 | RCT | Dialysis | 11 (300) | Mixed | Mixed | SMD: 0.52 (0.31 to 0.72) | Moderate | <0.001 | 39.0% | ⨁⨁⨁◯ |
| Chung et al28 | RCT | HD | 4 (127) | Mixed | Intradialytic | SMD: 0.44 (0.09 to 0.80) | Small | 0.015 | 0.0% | ⨁⨁◯◯ |
| Zhang et al51 | RCT | HD | 8 (299) | RT | Intradialytic | SMD: 0.52 (0.28 to 0.75) | Moderate | <0.001 | 18.7% | ⨁⨁◯◯ |
| Pu et al41 | RCT | HD | 7 (219) | Mixed | Intradialytic | SMD: 0.57 (0.30 to 0.84) | Moderate | <0.001 | 0.0% | ⨁⨁◯◯ |
| Clarkson et al29 | RCT | Dialysis | 18 (744) | Mixed | – | MD: 33.64 (23.74 to 43.54) | – | <0.001 | 0.0% | ⨁⨁⨁◯ |
| Huang et al34 | RCT | HD | 7 (205) | Mixed | Mixed | SMD: 1.01 (0.26 to 1.76) | Large | 0.008 | 83.0% | ⨁◯◯◯ |
| Matsuzawa et al37 | RCT | HD | 10 (326) | Mixed | Mixed | SMD: 0.58 (0.24 to 0.93) | Moderate | <0.001 | 53.0% | ⨁⨁◯◯ |
| Bogataj et al25 | RCT | HD | 19 | Mixed | Mixed | SMD: 0.44 (0.21 to 0.67) | Small | <0.001 | 49.6% | ⨁◯◯◯ |
| Sheng et al43 | RCT | HD | 4 (146) | Mixed | Intradialytic | SMD: 0.58 (0.23 to 0.93) | Moderate | <0.001 | 89.7% | ⨁◯◯◯ |
| Neto et al32 | RCT | HD | 6 (158) | Mixed | Intradialytic | SMD: 0.96 (0.11 to 1.80) | Large | 0.03 | 82.0% | ⨁◯◯◯ |
| Ferrari et al30 | RCT | HD | 6 (211) | RT | Intradialytic | MD: 68.5 (29.05 to 107.96) | – | <0.001 | 36.0% | ⨁◯◯◯ |
| Ferrari et al30 | RCT | HD | 6 (188) | AE | Intradialytic | MD: 64.98 (43.86 to 86.11) | – | <0.001 | 0.0% | ⨁◯◯◯ |
| Aerobic capacity | ||||||||||
| Heiwe et al33 | RCT/Quasi-RCT | Mixed | 24 (847) | Mixed | – | SMD: −0.56 (−0.70 to 0.42) | Moderate | <0.001 | 12.0% | ⨁◯◯◯ |
| Heiwe and Jacobson10 | RCT | HD | 21 (374) | Mixed | Mixed | SMD: −0.80 (−1.02 to 0.58) | Large | <0.001 | 0.0% | ⨁⨁◯◯ |
Mixed means aerobic exercise combined with resistance training.
*Number of included studies and corresponding sample size.
AE, aerobic exercise; CKD, chronic kidney disease; GRADE, Grading of Recommendations Assessment, Development and Evaluation; HD, haemodialysis; KTRs, kidney transplant recipients; MD, mean difference; 6MWT, 6 min walk test; RCT, randomised controlled trial; RT, resistance training; SMD, standardised mean difference; VO2 peak, peak oxygen uptake.
The effect of exercise on peak oxygen consumption was investigated in 18 meta-analyses (reported in 17 articles) with a mild heterogeneity (average I2=42.2%),24 25 27 28 30 32 34 37 38 40 41 43 44 49 50 54 and 16 reported positive statistically significant outcomes.24 25 28 30 32 34 37 38 40 41 43 44 47 49 50 Of the 18 meta-analyses, 3 reported a low effect size,27 39 50 9 reported a moderate effect size25 28 32 34 37 41 43 44 49 and 3 reported a large effect size.24 38 47 GRADE assessment of quality indicated the overall evidence as being very low (nine meta-analyses25 27 28 30 32 37 43 47 49), low (eight meta-analyses24 34 38–41 44 50) and high (one meta-analysis37). A meta-analysis that included kidney transplant recipients found no statistically significant difference in the SMD of the exercise group (0.38; 95% CI: −0.06 to 0.82; p=0.09).39
The effect of exercise on the 6 min walk test was investigated in 14 meta-analyses (reported in 13 articles) with a mild heterogeneity (average I2=44.9%),25 28–30 32 34 36–38 40 41 43 51 and 13 reported positive statistically significant outcomes.25 28–30 32 34 36–38 41 43 51 Of the 14 meta-analyses, 2 reported a small effect size,25 28 5 reported a moderate effect size36 37 41 43 51 and 3 reported a large effect size.32 34 38 GRADE assessment of quality indicated the overall evidence as being very low (eight meta-analyses25 30 32 34 38 40 43), low (four meta-analyses28 37 41 51) and moderate (two meta-analyses29 36). In addition, the meta-analysis by Heiwe and Jacobson10 showed that regular exercise had significant beneficial effects on aerobic capacity.10 33
Muscle strength
Ten meta-analyses (reported in nine articles) investigated the effects of exercise on muscle strength in patients with CKD with a low heterogeneity (average I2=19.1%).10 26 32 33 35–38 51 The meta-analyses included a mean of 7 studies (ranging from 3 to 12) and a mean of 252 participants (ranging from 115 to 385) (table 3).
Table 3.
Summary of the effect of exercise on muscle strength in patients with CKD
| Study | Design | Stage of CKD | k (n)* | Exercise type | Mode | SMD or MD (95% CI) | Effect size | P value | I 2 | GRADE |
| Cheema et al26 | RCT | Predialysis | 7 (249) | RT | – | SMD: 1.15 (0.80 to 1.49) | Large | 0.161 | 35.0% | ⨁⨁◯◯ |
| Nakamura et al38 | RCT/Cross-over | Predialysis | 4 (119) | Mixed | – | SMD: 0.35 (-0.03 to 0.73) | Small | 0.07 | 7.0% | ⨁◯◯◯ |
| Lu et al36 | RCT | Dialysis | 5 (234) | Mixed | Mixed | SMD: 0.59 (0.20 to 0.98) | Moderate | 0.003 | 52.0% | ⨁⨁◯◯ |
| Lu et al36 | RCT | Dialysis | 7 (224) | Mixed | Mixed | SMD: 0.47 (0.20 to 0.74) | Small | <0.001 | 0.0% | ⨁⨁◯◯ |
| Zhang et al51 | RCT | HD | 6 (300) | RT | Intradialytic | SMD: 0.35 (0.12 to 0.58) | Small | 0.003 | 41.6% | ⨁⨁◯◯ |
| Heiwe et al33 | RCT/Quasi-RCT | Mixed | 9 (358) | Mixed | – | SMD: −0.52 (−0.73 to 0.31) | Moderate | <0.001 | 0.0% | ⨁◯◯◯ |
| Heiwe and Jacobson10 | RCT | HD | 12 (385) | Mixed | Mixed | SMD: −0.56 (−0.77 to 0.35) | Moderate | <0.001 | 0.0% | ⨁◯◯◯ |
| Matsuzawa et al37 | RCT | HD | 9 (281) | Mixed | Mixed | SMD: 0.94 (0.67 to 1.21) | Large | <0.001 | 10.0% | ⨁◯◯◯ |
| Neto et al32 | RCT | HD | 9 (250) | Mixed | Intradialytic | SMD: 0.61 (0.39 to 0.83) | Moderate | <0.001 | 58.9% | ⨁◯◯◯ |
| Ju et al35 | RCT | Mixed | 3 (115) | Mixed | – | SMD: 0.52 (0.14 to 0.89) | Moderate | 0.007 | 0.0% | ⨁◯◯◯ |
Mixed means aerobic exercise combined with resistance training.
*Number of included studies and corresponding sample size.
CKD, chronic kidney disease; GRADE, Grading of Recommendations Assessment, Development and Evaluation; HD, haemodialysis; MD, mean difference; RCT, randomised controlled trial; RT, resistance training; SMD, standardised mean difference.
Muscle strength was measured using handgrip strength and lower limb muscle strength. For patients in 8 of 10 meta-analyses, exercise resulted in statistically significant improvements in muscle strength.10 32 33 35–37 51 Of the 10 meta-analyses, 3 reported a small effect size,36 38 51 5 reported a moderate effect size10 32 33 35 36 and 2 reported a large effect size.26 37 GRADE assessment of quality indicated the overall evidence as being very low (six meta-analyses10 32 33 35 37 38) and low (four meta-analyses26 36 51).
Muscle endurance
Nine meta-analyses (reported in eight articles) investigated the effects of exercise on muscle endurance with a mild heterogeneity (average I2=29.4%).10 25 33 36 38 40 43 51 An average of 238 participants (ranging from 106 to 461) from 5 studies (ranging from 3 to 7) were included in the meta-analysis (table 4).
Table 4.
Summary of the effect of exercise on muscle endurance in patients with CKD
| Study | Design | Stage of CKD | k (n)* | Exercise type | Mode | Outcome | SMD or MD (95% CI) | Effect size | P value | I 2 | GRADE |
| Lu et al36 | RCT | Dialysis | 3 (193) | Mixed | Mixed | STS 10 | MD: −4.69 (−9.01 to 0.38) | – | 0.028 | 72.2% | ⨁◯◯◯ |
| Bogataj et al25 | RCT | HD | 5 (461) | Mixed | – | STS 10 | SMD: −0.55 (−1.00 to 0.09) | Moderate | 0.019 | 71.6% | ⨁◯◯◯ |
| Lu et al36 | RCT | Dialysis | 6 (240) | Mixed | Mixed | STS 30 | SMD: 0.43 (0.17 to 0.69) | Small | 0.001 | 2.0% | ⨁⨁◯◯ |
| Zhang et al51 | RCT | HD | 5 (164) | RT | Intradialytic | STS 30 | SMD: 0.42 (0.11,0.74) | Small | 0.008 | 0.0% | ⨁◯◯◯ |
| Sheng et al43 | RCT | HD | 3 (106) | Mixed | Intradialytic | STS 60 | SMD: 0.71 (0.31,1.12) | Moderate | <0.001 | 0.0% | ⨁◯◯◯ |
| Pei et al40 | RCT/Quasi-RCT | Mixed | 5 (445) | AE | – | STS 60 | MD: 2.08 (1.1,3.05) | – | 0.98 | 82.0% | ⨁◯◯◯ |
| Nakamura et al38 | RCT/Cross-over | Predialysis | 3 (170) | Mixed | – | TUGT | SMD: −0.42 (−0.73 to 0.11) | Small | 0.007 | 0.0% | ⨁◯◯◯ |
| Heiwe et al33 | RCT/Quasi-RCT | Mixed | 7 (191) | Mixed | – | Walking capacity | SMD: −0.48 (−0.79 to 0.17) | Small | 0.003 | 2.0% | ⨁◯◯◯ |
| Heiwe and Jacobson10 | RCT | HD | 7 (174) | Mixed | Mixed | Walking capacity | SMD: −0.33 (-0.67,0.01) | Small | 0.06 | 16.0% | ⨁⨁⨁◯ |
Mixed means aerobic exercise combined with resistance training.
*Number of included studies and corresponding sample size.
AE, aerobic exercise; CKD, chronic kidney disease; GRADE, Grading of Recommendations Assessment, Development and Evaluation; HD, haemodialysis; MD, mean difference; RCT, randomised controlled trial; RT, resistance training; SMD, standardised mean difference; STS 10, sit-to-stand 10 test; STS 30, sit-to-stand 30 test; STS 60, sit-to-stand 60 test; TUGT, timed up and go test.
Muscle endurance was measured using a sit-to-stand test, timed up and go test and walking capacity exercise. Pooled effect estimates from all nine meta-analyses suggested a beneficial effect of exercise on muscle endurance in patients with CKD. Seven of the nine meta-analyses reported power to detect a statistically significant effect.25 33 36 38 43 51 Two meta-analyses reported moderate effect size and five reported small effect size. GRADE assessment of quality indicated the overall evidence as being very low (seven meta-analyses25 33 36 38 40 43 51), low (one meta-analyses36) and moderate (one meta-analyses10).
Body composition
Four meta-analyses consisting of 9 studies (ranging from 4 to 13) and a mean of 335 participants (ranging from 166 to 466) included body mass index as an outcome.27 47 49 52 There was a low heterogeneity (average I2=12.0%) among the study outcomes (table 5).
Table 5.
Summary of the effect of exercise on body composition in patients with CKD
| Study | Design | Stage of CKD | k (n)* | Exercise type | Mode | SMD (95% CI) | Effect size | P value | I 2 | GRADE |
| Chen et al27 | RCT | KTRs | 4 (166) | Mixed | – | SMD: 0.02 (−0.28 to 0.33) | Small | 0.89 | 0.0% | ⨁◯◯◯ |
| Yamamoto et al49 | RCT | Predialysis | 10 (414) | AE | – | SMD: −0.19 (−0.38 to 0.00) | Small | 0.026 | 0.0% | ⨁⨁◯◯ |
| Zhang et al52 | RCT | Predialysis | 13 (466) | Mixed | – | SMD: −0.21 (−0.39 to 0.03) | Small | 0.02 | 0.0% | ⨁⨁⨁◯ |
| Vanden Wyngaert et al47 | RCT | Predialysis | 9 (294) | AE | – | SMD: −0.36 (−0.60 to 0.13) | Small | 0.002 | 48.0% | ⨁⨁◯◯ |
Mixed means aerobic exercise combined with resistance training.
*Number of included studies and corresponding sample size.
AE, aerobic exercise; CKD, chronic kidney disease; GRADE, Grading of Recommendations Assessment, Development and Evaluation; KTRs, kidney transplant recipients; RCT, randomised controlled trial; SMD, standardised mean difference.
Three of the four meta-analyses showed a positive statistically significant impact on body mass index using exercise interventions in patients with CKD.47 49 52 Small effect size was reported in all meta-analyses. GRADE assessment of quality indicated the overall evidence as being very low (one meta-analysis), low (two meta-analyses47 49) and moderate (one meta-analysis52).
Dialysis-related symptoms
Nine meta-analyses (reported in seven articles) investigated the effect of exercise on dialysis-related symptoms in patients with CKD.30 31 34 41 43 45 53 Each meta-analysis included a mean of 7 studies (ranging from 3 to 12 studies) and a mean of 239 participants (ranging from 139 to 370) (table 6).
Table 6.
Summary of the effect of exercise on dialysis-related symptoms in patients with CKD
| Study | Design | Stage of CKD | k (n)* | Exercise type | Mode | Outcomes | SMD or MD (95% CI) | Effect size | P value | I 2 | GRADE |
| Ferreira et al31 | RCT/Quasi-RCT | HD | 10 (346) | AE | Intradialytic | Kt/V† | SMD: 2.21 (1.17 to 3.25) | Large | <0.001 | 92.0% | ⨁◯◯◯ |
| Pu et al41 | RCT | HD | 10 (301) | Mixed | Intradialytic | Kt/V | SMD: 0.29 (0.06 to 0.52) | Small | 0.01 | 0.0% | ⨁◯◯◯ |
| Huang et al34 | RCT | HD | 8 (257) | Mixed | Mixed | Kt/V | SMD: 0.19 (-0.06 to 0.43) | Small | 0.14 | 0.0% | ⨁◯◯◯ |
| Sheng et al43 | RCT | HD | 7 (233) | Mixed | Intradialytic | Kt/V | SMD: 0.27 (0.01 to 0.53) | Small | 0.04 | 0.0% | ⨁◯◯◯ |
| Ferrari et al30 | RCT | HD | 12 (370) | AE | Intradialytic | Kt/V | MD: 0.08 (0.0 to 0.15) | – | 0.04 | 56.0% | ⨁◯◯◯ |
| Ferrari et al31 | RCT | HD | 6 (220) | RT | Intradialytic | Kt/V | MD: 0.10 (0.0 to 0.2) | – | 0.06 | 6.0% | ⨁◯◯◯ |
| Song et al45 | RCT | HD | 4 (141) | Mixed | Mixed | RLS | SMD: −1.79 (−2.21 to 1.37) | Large | <0.001 | 87.0% | ⨁◯◯◯ |
| Song et al45 | RCT | HD | 3 (139) | Mixed | Mixed | Fatigue | SMD: −0.85 (−1.20 to 0.50) | Large | <0.001 | 0.0% | ⨁◯◯◯ |
| Zhao et al53 | RCT | Dialysis | 3 (141) | Mixed | – | Fatigue | SMD: −0.97 (−1.32 to 0.62) | Large | <0.001 | 47.0% | ⨁⨁◯◯ |
Mixed means aerobic exercise combined with resistance training.
*Number of included studies and corresponding sample size.
†An indicator to assess dialysis adequacy
AE, aerobic exercise; CKD, chronic kidney disease; GRADE, Grading of Recommendations Assessment, Development and Evaluation; HD, haemodialysis; KTRs, kidney transplant recipients; MD, mean difference; RCT, randomised controlled trial; RLS, restless legs syndrome; RT, resistance training; SMD, standardised mean difference.
Fatigue was measured using the Rhoten Fatigue Scale, Visual Analogue Scale and Haemodialysis Patients Fatigue Scale. The effect of exercise on fatigue was investigated in two meta-analyses with a low heterogeneity (average I2=23.5%).45 53 The two meta-analyses revealed a statistically significant effect of exercise on fatigue. Although the meta-analyses reported large effect size, the quality of evidence was low45 or very low53 according to GRADE criteria.
Just one meta-analysis investigated the effects of exercise on restless legs syndrome in patients with CKD.45 The results showed that pooled effect estimated for restless legs syndrome with statistically significant but considerable average heterogeneity (I2=87.0%). According to GRADE criteria, the overall evidence for this outcome was very low.
Dialysis adequacy
Dialysis adequacy was measured using the value of Kt/V. Six meta-analyses (reported in five articles) investigated the effects of exercise on Kt/V in patients with CKD with a mild heterogeneity (average I2=25.7%).30 31 34 41 43 Comprehensive effect estimates from all the six meta-analyses with Kt/V outcomes showed that exercise had a beneficial effect. In three of the six meta-analyses, three reported a small effect size34 41 43 and one reported large effect size.31 According to GRADE criteria, all meta-analyses were rated as very low-quality evidence (table 6).
Health-related quality of life
Twenty-nine meta-analyses (reported in 13 articles) investigated the effect of exercise on HRQOL in patients with CKD.26 28 32 34 35 37 39–43 51 53 Among them, nine meta-analyses assessed the physical and mental subscale of the Short-Form Health Survey-36.28 32 34 37 41–43 51 53 Each meta-analysis included an average of 6 studies (ranging from 3 to 10) and 311 participants (ranging from 167 to 562). The included meta-analyses had moderate heterogeneity (average I2=51.0%) (table 7).
Table 7.
Summary of the effect of exercise on health-related quality of life in patients with CKD
| Study | Design | Stage of CKD | k (n)* | Exercise type | Mode | Outcomes | SMD or MD (95% CI) | Effect size | P value | I 2 | GRADE |
| Salhab et al42 | RCT | HD | 5 (282) | AE | Intradialytic | PCS | SMD: 1.82 (-0.92 to 4.55) | Large | 0.19 | 98.0% | ⨁◯◯◯ |
| Chung et al28 | RCT | HD | 6 (229) | Mixed | Intradialytic | PCS | SMD: 0.46 (0.20 to 0.73) | Small | <0.001 | 1.90% | ⨁⨁◯◯ |
| Zhang et al51 | RCT | HD | 7 (297) | RT | Intradialytic | PCS | SMD: 0.23 (-0.00 to 0.46) | Small | 0.055 | 0.0% | ⨁⨁◯◯ |
| Pu et al41 | RCT | HD | 10 (320) | Mixed | Intradialytic | PCS | SMD: 0.57 (0.14 to 1.01) | Moderate | 0.01 | 70.0% | ⨁◯◯◯ |
| Zhao et al53 | RCT | Dialysis | 5 (186) | Mixed | – | PCS | SMD: 0.31 (0.02 to 0.61) | Small | 0.04 | 46.0% | ⨁⨁◯◯ |
| Huang et al34 | RCT | HD | 7 (263) | Mixed | Mixed | PCS | SMD: 0.34 (0.09 to 0.59) | Small | 0.007 | 27.0% | ⨁⨁◯◯ |
| Matsuzawa et al37 | RCT | HD | 9 (264) | Mixed | Mixed | PCS | SMD: 0.53 (0.52 to 0.82) | Moderate | <0.001 | 19.0% | ⨁◯◯◯ |
| Sheng et al43 | RCT | HD | 7 (256) | Mixed | Intradialytic | PCS | SMD: 0.30 (0.05 to 0.55) | Small | 0.02 | 39.5% | ⨁◯◯◯ |
| Neto et al32 | RCT | HD | 7 (187) | Mixed | Intradialytic | PCS | SMD: 0.50 (-0.19 to 1.18) | Moderate | 0.16 | 62.0% | ⨁◯◯◯ |
| Salhab et al42 | RCT | HD | 5 (282) | AE | Intradialytic | MCS | SMD: 1.02 (0.31 to 1.73) | Large | 0.005 | 75.0% | ⨁◯◯◯ |
| Chung et al28 | RCT | HD | 5 (193) | Mixed | Intradialytic | MCS | SMD: 0.23 (-0.05 to 0.52) | Small | 0.109 | 0.0% | ⨁⨁◯◯ |
| Zhang et al51 | RCT | HD | 7 (297) | RT | Intradialytic | MCS | SMD: 0.13 (-0.10 to 0.36) | Small | 0.082 | 46.5% | ⨁⨁◯◯ |
| Pu et al41 | RCT | HD | 8 (219) | Mixed | Intradialytic | MCS | SMD: 0.19 (-0.09 to 0.46) | Small | 0.18 | 30.0% | ⨁⨁◯◯ |
| Zhao et al53 | RCT | Dialysis | 5 (186) | Mixed | – | MCS | SMD: 0.30 (-0.20 to 0.80) | Small | 0.24 | 64.0% | ⨁◯◯◯ |
| Huang et al34 | RCT | HD | 7 (263) | Mixed | Mixed | MCS | SMD: 0.27 (0.02 to 0.51) | Small | 0.03 | 0.0% | ⨁⨁◯◯ |
| Matsuzawa et al37 | RCT | HD | 8 (228) | Mixed | Mixed | MCS | SMD: 0.14 (-0.15 to 0.42) | Small | 0.34 | 10.0% | ⨁◯◯◯ |
| Sheng et al43 | RCT | HD | 5 (167) | Mixed | Intradialytic | MCS | SMD: 0.14 (-0.16 to 0.43) | Small | 0.37 | 14.8% | ⨁◯◯◯ |
| Neto et al32 | RCT | HD | 7 (185) | Mixed | Intradialytic | MCS | SMD: 0.39 (-0.19 to 0.98) | Small | 0.19 | 50.0% | ⨁◯◯◯ |
| Pei et al40 | RCT/Quasi-RCT | Mixed | 6 (522) | AE | – | Physical function (SF-36) | MD: 8.36 (-1.24 to 17.95) | – | 0.09 | 76.0% | ⨁◯◯◯ |
| Pei et al40 | RCT/Quasi-RCT | Mixed | 7 (562) | AE | – | Physical role (SF-36) | MD: 14.65 (1.47 to 27.84) | – | 0.03 | 78.0% | ⨁◯◯◯ |
| Pei et al40 | RCT/Quasi-RCT | Mixed | 6 (447) | AE | – | Social function (SF-36) | MD: 8.24 (-1.09 to 17.58) | – | 0.08 | 85.0% | ⨁◯◯◯ |
| Pei et al40 | RCT/Quasi-RCT | Mixed | 6 (513) | AE | – | Pain (SF-36) | MD: 5.94 (1.65 to 10.23) | – | 0.007 | 49.0% | ⨁◯◯◯ |
| Pei et al40 | RCT/Quasi-RCT | Mixed | 7 (562) | AE | – | General health (SF-36) | MD: 8.90 (2.48 to 15.32) | – | 0.007 | 71.0% | ⨁◯◯◯ |
| Pei et al40 | RCT/Quasi-RCT | Mixed | 6 (542) | AE | – | Mental health (SF-36) | MD: 7.30 (-0.94 to 15.54) | – | 0.08 | 84.0% | ⨁◯◯◯ |
| Cheema et al26 | RCT | Predialysis | 6 (223) | RT | – | HRQOL | SMD: 0.83 (0.51 to 1.16) | Large | 0.226 | 27.8% | ⨁⨁◯◯ |
| Oguchi et al39 | RCT | KTRs | 4 (179) | Mixed | – | HRQOL | SMD: 0.54 (0.02 to 1.07) | Moderate | 0.04 | 58.0% | ⨁◯◯◯ |
| Ju et al35 | RCT | Mixed | 3 (387) | Mixed | – | Symptom/Problem (KDQOL) | SMD: 1.92 (-1.06 to 4.90) | Large | 0.21 | 99.0% | ⨁◯◯◯ |
| Ju et al35 | RCT | Mixed | 3 (387) | Mixed | – | Effects of kidney disease (KDQOL) | SMD: −3.69 (-8.56 to 1.19) | Large | 0.14 | 99.0% | ⨁◯◯◯ |
| Ju et al35 | RCT | Mixed | 3 (387) | Mixed | – | Burden of kidney disease (KDQOL) | SMD: 1.04 (-0.75 to 2.82) | Large | 0.26 | 98.0% | ⨁◯◯◯ |
Mixed means aerobic exercise combined with resistance training.
*Number of included studies and corresponding sample size.
AE, aerobic exercise; CKD, chronic kidney disease; COM, combine; GRADE, Grading of Recommendations Assessment, Development and Evaluation; HD, haemodialysis; HRQOL, health-related quality of life; KDQOL, kidney disease quality of life; KTRs, kidney transplant recipients; MCS, mental component summary; MD, mean difference; PCS, physical component summary; RCT, randomised controlled trial; RT, resistance training; SF-36, Short Form Health Survey-36; SMD, standardised mean difference.
Of the 29 meta-analyses, a comprehensive effect estimate of the 28 meta-analyses shows that exercise is beneficial to the HRQOL of patients with CKD, but only 12 of 29 meta-analyses reported a statistically significant outcome.28 34 37 39 41–43 53 There were 13 of 29 meta-analyses reporting a small effect size,28 32 34 37 41 43 51 53 4 were moderate32 37 39 41 and 6 were large.26 35 42 According to GRADE criteria, the overall of evidence for HRQOL was rated as very low (20 meta-analyses32 35 37 39–43 53) or low (9 meta-analyses26 28 34 41 51 53).
Adverse events
Six meta-analyses reported exercise-related adverse events.26 28 38 41 43 44 Of the adverse effects, the most commonly reported were hypotension and cramping. Overall, the incidence of adverse events was approximately 0.3%.
Discussion
Summary of main results
Several meta-analyses have been published on exercise interventions in patients with CKD.55 The findings of these meta-analyses should be assessed to determine if the evidence is consistent among the studies. This umbrella review included 31 eligible articles involving 120 separate meta-analyses investigating the effect of exercise on the health outcomes in patients with CKD. There was low-quality or very low-quality evidence for moderate beneficial effects of exercise on cardiorespiratory fitness, muscle strength and body composition. In addition, there was very low-quality evidence for minor beneficial effects of exercise on muscle endurance, cardiovascular risk factors, dialysis-related symptoms and HRQOL. Few adverse events related to exercise indicate that exercise is safe for patients with CKD.
Interpretation of study effects
Cardiovascular disease is a frequent complication of CKD and is the leading cause of death in patients with CKD.56 Hypertension is an important modifiable risk factor for cardiovascular diseases and progressive renal dysfunction in patients with CKD.57 The present overview showed that exercise has a small to moderate effect on blood pressure (SMD: −0.75 to 0.04 for systolic blood pressure and SMD: −0.47 to 0.04 for diastolic blood pressure); it is an appealing strategy for blood pressure control in patients with CKD. However, the dose effects of exercise in the context of the cardiovascular health of patients with CKD should be considered. A recent cohort study found that 7.5–15 metabolic equivalent hours per week (MET-h/week) was associated with the lowest risk of cardiovascular events.58 Regrettably, the benefit of exercise on cardiovascular risk factors cannot be determined because there are an insufficient number of conclusive studies that assess exercise effects on overall cardiovascular health. In a systematic review by Heiwe et al, a meta-analysis including two trials found that exercise improved cardiovascular function in patients with CKD, as reflected in the SD of all normal RR intervals and left ventricular mass index.10 Furthermore, a recent randomised controlled trial published by Graham-Brown et al indicated that intradialytic exercise could reduce left ventricular mass and is safe, deliverable and well-tolerated.59 Although the GRADE evidence was low, exercise should be recommended for patients with CKD, particularly those comorbid with cardiovascular disease. Future randomised controlled exercise trials need to focus more on the role of exercise in cardiovascular events in patients with CKD.
Physical fitness is necessary for participation in activities of daily living. The exercise provided the best results in improving cardiorespiratory fitness and muscle strength in patients with CKD, with more than half of the meta-analyses reporting moderate or large effect sizes, regardless of the quality of evidence. Cardiorespiratory fitness is considered a significant independent predictor of mortality, and muscle strength is an essential indicator of physical performance in patients with CKD.60 It is well known that aerobic exercise is the ‘gold standard’ for cardiorespiratory rehabilitation61 and resistance training for muscle strength improvement.62 However, a combination of aerobic and resistance exercises may have a more profound effect on patients with CKD based on the current review. Meta-analyses by Andrade et al showed that combined training benefits cardiorespiratory fitness in patients with CKD.24
Both sarcopenia and obesity have increased mortality risk and progression to end-stage renal disease in patients with CKD.63 Unlike patients receiving dialysis, treatment requirements for patients with predialysis CKD are based on maintaining a ‘healthy weight’ and preventing or attenuating obesity.14 In this overview, the effectiveness of exercise for body mass index was supported by four analyses with small effect sizes and moderate quality of evidence. Based on the results, exercise may contribute to lower body mass index in patients with CKD. However, additional studies are needed to confirm the benefits of exercise programmes for reducing sarcopenia and weight.
CKD population experience multiple symptoms that affect the patient’s prognosis and HRQOL.64 Patients who received dialysis treatment commonly reported restless legs syndrome, fatigue and inadequate dialysis due to kidney function deterioration and dialysis-related side effects.65 66 These symptoms affect sleep and daily activities and impose considerable psychological distress and economic burden.67 An increasing number of researchers have investigated the role of exercise as an important non-pharmacological strategy for preventing and/or treating symptoms.68 69 The results of a small number of meta-analyses suggested the beneficial effect of exercise on dialysis adequacy (SMD: 0.19 to 2.21) and improving restless legs syndrome (SMD: −1.79) and fatigue symptoms (SMD: −0.97 to −0.85). Nevertheless, the efficacy of exercise in patients with CKD for preventing dialysis-related symptoms awaits new clinical evidence.
With similar results obtained in another overview that included chronic disease,70 results from this overview demonstrated minor beneficial effects of exercise on HRQOL, irrespective of the evidence level in patients with CKD. Improved HRQOL is vital because most of the population reported poor health and well-being due to diet restriction, weakness and dialysis treatment.71 The consistent health benefits of exercise in this overview demonstrated that exercise could be a strategy to improve the poor long-term prognosis in patients with CKD.
Several meta-analyses reported exercise-related adverse events. Based on the reported adverse events, we calculate that only three adverse events occurred per 1000 patients with CKD. The low incidence of adverse events indicated that the benefits of exercise in patients with CKD outweigh its potential risks and most reflected typical response to exercise (eg, muscle soreness). However, most meta-analyses only included intradialytic exercise for haemodialysis patients in their assessments. Exercises during haemodialysis are usually performed under the supervision of a healthcare worker to ensure safety.72 It has been reported that all patients with CKD are at risk for cardiovascular events (eg, arrhythmias, myocardial ischaemia) during exercise. Therefore, medical screening should be performed before exercise to determine which patients may be at increased risk for cardiovascular accidents.73 In addition, special attention should be paid to dry weight and blood pressure in patients with haemodialysis-dependent CKD to avoid excessive volume loading or dehydration, which may increase the risk associated with exercise.60
Implications for clinical
Taken together, there is good reason to recommend exercise for improving prognosis in patients with CKD. Evidence from most randomised controlled trials increased confidence in the findings of this umbrella review. Because most of the meta-analyses assessed in this study did not detail the exercises instituted, it is difficult to make recommendations about the type of exercise that would be the most beneficial for patients with CKD. Although exercise’s effect sizes on improving health prognosis of patients with CKD were generally moderate, these effects may bring some clinical benefit to patients experiencing impaired function or symptom distress. Despite numerous meta-analyses providing only low-quality or very low-quality evidence, similar beneficial effects of exercise were reported by meta-analyses of randomised controlled trials with different grades of evidence. Remarkably, a recently published trial found that a 6-month intradialytic exercise programme effectively reduces healthcare costs.74 Overall, exercise should be integrated into the care of CKD, but the overall benefit of exercise to CKD is still debatable.
Limitations
This overview has several limitations. First, most meta-analyses included in this review involve haemodialysis patients, limiting the results’ extrapolation to other CKD stages. Second, improvement of flexibility in patients with CKD was not investigated. Flexibility is an important component of physical fitness that impacts muscular injury.75 The evidence for the efficacy of exercise on flexibility improvement is insufficient for a systematic review or meta-analysis. Third, since the search strategy was limited to English, this review may have language bias. It is unknown whether meta-analyses published in other languages would affect the results of our study. Fourth, the results may have been influenced by an overlap in the original studies. Fifth, the accuracy of the MD data cannot be guaranteed. Sixth, subgroup analyses of different types of exercise were not performed as described in the published protocol because most of the included meta-analyses did not detail the exercises. Seventh, both body composition and cardiovascular risk factors are common terms. However, the inclusion of studies was limited, so this review focused only on body mass index and blood pressure, and more evidence is still needed for the effects of other assessment metrics.
Conclusion
In patients with CKD, exercise improves muscle strength, endurance, body composition and HRQOL. At the same time, exercise decreases blood pressure and dialysis-related symptoms in patients with CKD. However, the quality of the evidence was considered low or very low for all outcomes indicating that we have low certainty evidence to support the findings above. More rigorous study is still needed in the future. Nevertheless, given the health benefits of physical activity, exercise should be integrated into renal care for a patient with any stage of CKD.
Supplementary Material
Footnotes
Contributors: FZ and LH conceived and designed the review. YB and XZ searched databases, extracted the data and conducted the statistical analysis. WZ revised the manuscript. WW and HZ provided technical support. All authors had read and approved the final manuscript and agreed on its submission. FZ was the guarantor of this work.
Funding: This study was supported by Longhua Hospital Shanghai University of Traditional Chinese Medicine (grant number: Y21026), and Longhua Hospital Shanghai University of Traditional Chinese Medicine (YW.006.035)
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Zoccali C, Vanholder R, Massy ZA, et al. The systemic nature of CKD. Nat Rev Nephrol 2017;13:344–58. 10.1038/nrneph.2017.52 [DOI] [PubMed] [Google Scholar]
- 2.GBD Chronic Kidney Disease Collaboration . Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet 2020;395:709–33. 10.1016/S0140-6736(20)30045-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang C, Gao B, Zhao X, et al. Executive summary for China kidney disease network (CK-NET) 2016 annual data report. Kidney Int 2020;98:1419–23. 10.1016/j.kint.2020.09.003 [DOI] [PubMed] [Google Scholar]
- 4.Cheng H-T, Xu X, Lim PS, et al. Worldwide epidemiology of diabetes-related end-stage renal disease, 2000-2015. Diabetes Care 2021;44:89-97. 10.2337/dc20-1913 [DOI] [PubMed] [Google Scholar]
- 5.Roshanravan B, Robinson-Cohen C, Patel KV, et al. Association between physical performance and all-cause mortality in CKD. J Am Soc Nephrol 2013;24:822–30. 10.1681/ASN.2012070702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang XH, Mitch WE. Mechanisms of muscle wasting in chronic kidney disease. Nat Rev Nephrol 2014;10:504–16. 10.1038/nrneph.2014.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoshino J. Renal rehabilitation: exercise intervention and nutritional support in dialysis patients. Nutrients 2021;13:1444. 10.3390/nu13051444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilund KR, Viana JL, Perez LM. A critical review of exercise training in hemodialysis patients: personalized activity prescriptions are needed. Exerc Sport Sci Rev 2020;48:28–39. 10.1249/JES.0000000000000209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tentori F, Elder SJ, Thumma J, et al. Physical exercise among participants in the dialysis outcomes and practice patterns study (DOPPS): correlates and associated outcomes. Nephrol Dial Transplant 2010;25:3050–62. 10.1093/ndt/gfq138 [DOI] [PubMed] [Google Scholar]
- 10.Heiwe S, Jacobson SH. Exercise training in adults with CKD: a systematic review and meta-analysis. Am J Kidney Dis 2014;64:383–93. 10.1053/j.ajkd.2014.03.020 [DOI] [PubMed] [Google Scholar]
- 11.Wong L, Duque G, McMahon LP. Sarcopenia and frailty: challenges in mainstream nephrology practice. Kidney Int Rep 2021;6:2554–64. 10.1016/j.ekir.2021.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rampersad C, Darcel J, Harasemiw O, et al. Change in physical activity and function in patients with baseline advanced Nondialysis CKD. Clin J Am Soc Nephrol 2021;16:1805–12. 10.2215/CJN.07050521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.March DS, Graham-Brown MP, Young HM, et al. 'There is nothing more deceptive than an obvious fact': more evidence for the prescription of exercise during haemodialysis (intradialytic exercise) is still required. Br J Sports Med 2017;51:1379. 10.1136/bjsports-2017-097542 [DOI] [PubMed] [Google Scholar]
- 14.Clinical Practice Guideline . Exercise and lifestyle in chronic kidney disease. Available: https://renal.org/sites/renal.org/files/Exercise%20and%20Lifestyle%20in%20CKD%20clinical%20practice%20guideline33_v4_FINAL_0.pdf [DOI] [PMC free article] [PubMed]
- 15.Yamagata K, Hoshino J, Sugiyama H, et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Renal Replacement Therapy 2019;5. 10.1186/s41100-019-0209-8 [DOI] [Google Scholar]
- 16.Deschamps T. Let's programme exercise during haemodialysis (intradialytic exercise) into the care plan for patients, regardless of age. Br J Sports Med 2016;50:1357–8. 10.1136/bjsports-2016-096356 [DOI] [PubMed] [Google Scholar]
- 17.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 18.Zhang F, Wang H, Huang L, et al. Therapeutic effects of exercise interventions for patients with chronic kidney disease: protocol for an overview of systematic reviews and meta-analyses of clinical trials. BMJ Open 2021;11:e043011. 10.1136/bmjopen-2020-043011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grgic J, Grgic I, Pickering C, et al. Wake up and smell the coffee: caffeine supplementation and exercise performance-an umbrella review of 21 published meta-analyses. Br J Sports Med 2020;54:681–8. 10.1136/bjsports-2018-100278 [DOI] [PubMed] [Google Scholar]
- 21.Cohen J. Quantitative methods in psychology: a power primer. Psychological Bulletin 1992;112:115–59. 10.1037//0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrade FP, Rezende PdeS, Ferreira TdeS, et al. Effects of intradialytic exercise on cardiopulmonary capacity in chronic kidney disease: systematic review and meta-analysis of randomized clinical trials. Sci Rep 2019;9:18470. 10.1038/s41598-019-54953-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bogataj Š, Pajek M, Pajek J, et al. Exercise-Based interventions in hemodialysis patients: a systematic review with a meta-analysis of randomized controlled trials. J Clin Med 2019;9. 10.3390/jcm9010043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheema BS, Chan D, Fahey P, et al. Effect of progressive resistance training on measures of skeletal muscle hypertrophy, muscular strength and health-related quality of life in patients with chronic kidney disease: a systematic review and meta-analysis. Sports Med 2014;44:1125–38. 10.1007/s40279-014-0176-8 [DOI] [PubMed] [Google Scholar]
- 27.Chen G, Gao L, Li X. Effects of exercise training on cardiovascular risk factors in kidney transplant recipients: a systematic review and meta-analysis. Ren Fail 2019;41:408–18. 10.1080/0886022X.2019.1611602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chung Y-C, Yeh M-L, Liu Y-M. Effects of intradialytic exercise on the physical function, depression and quality of life for haemodialysis patients: a systematic review and meta-analysis of randomised controlled trials. J Clin Nurs 2017;26:1801–13. 10.1111/jocn.13514 [DOI] [PubMed] [Google Scholar]
- 29.Clarkson MJ, Bennett PN, Fraser SF, et al. Exercise interventions for improving objective physical function in patients with end-stage kidney disease on dialysis: a systematic review and meta-analysis. Am J Physiol Renal Physiol 2019;316:F856–72. 10.1152/ajprenal.00317.2018 [DOI] [PubMed] [Google Scholar]
- 30.Ferrari F, Helal L, Dipp T, et al. Intradialytic training in patients with end-stage renal disease: a systematic review and meta-analysis of randomized clinical trials assessing the effects of five different training interventions. J Nephrol 2020;33:251–66. 10.1007/s40620-019-00687-y [DOI] [PubMed] [Google Scholar]
- 31.Ferreira GD, Bohlke M, Correa CM, et al. Does Intradialytic exercise improve removal of solutes by hemodialysis? A systematic review and meta-analysis. Arch Phys Med Rehabil 2019;100:2371–80. 10.1016/j.apmr.2019.02.009 [DOI] [PubMed] [Google Scholar]
- 32.Gomes Neto M, de Lacerda FFR, Lopes AA, et al. Intradialytic exercise training modalities on physical functioning and health-related quality of life in patients undergoing maintenance hemodialysis: systematic review and meta-analysis. Clin Rehabil 2018;32:1189–202. 10.1177/0269215518760380 [DOI] [PubMed] [Google Scholar]
- 33.Heiwe S, Jacobson SH, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev 2011;10:Cd003236. 10.1002/14651858.CD003236.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang M, Lv A, Wang J, et al. Exercise training and outcomes in hemodialysis patients: systematic review and meta-analysis. Am J Nephrol 2019;50:240–54. 10.1159/000502447 [DOI] [PubMed] [Google Scholar]
- 35.Ju H, Chen H, Mi C, et al. The impact of home-based exercise program on physical function of chronic kidney disease patients: a meta-analysis of randomized controlled trials. Physikalische Medizin, Rehabilitationsmedizin, Kurortmedizin 2020;30:108–14. 10.1055/a-1079-3714 [DOI] [Google Scholar]
- 36.Lu Y, Wang Y, Lu Q. Effects of exercise on muscle fitness in dialysis patients: a systematic review and meta-analysis. Am J Nephrol 2019;50:291–302. 10.1159/000502635 [DOI] [PubMed] [Google Scholar]
- 37.Matsuzawa R, Hoshi K, Yoneki K, et al. Exercise training in elderly people undergoing hemodialysis: a systematic review and meta-analysis. Kidney Int Rep 2017;2:1096–110. 10.1016/j.ekir.2017.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakamura K, Sasaki T, Yamamoto S, et al. Effects of exercise on kidney and physical function in patients with non-dialysis chronic kidney disease: a systematic review and meta-analysis. Sci Rep 2020;10:18195. 10.1038/s41598-020-75405-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oguchi H, Tsujita M, Yazawa M, et al. The efficacy of exercise training in kidney transplant recipients: a meta-analysis and systematic review. Clin Exp Nephrol 2019;23:275–84. 10.1007/s10157-018-1633-8 [DOI] [PubMed] [Google Scholar]
- 40.Pei G, Tang Y, Tan L, et al. Aerobic exercise in adults with chronic kidney disease (CKD): a meta-analysis. Int Urol Nephrol 2019;51:1787–95. 10.1007/s11255-019-02234-x [DOI] [PubMed] [Google Scholar]
- 41.Pu J, Jiang Z, Wu W, et al. Efficacy and safety of intradialytic exercise in haemodialysis patients: a systematic review and meta-analysis. BMJ Open 2019;9:e020633. 10.1136/bmjopen-2017-020633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salhab N, Karavetian M, Kooman J, et al. Effects of intradialytic aerobic exercise on hemodialysis patients: a systematic review and meta-analysis. J Nephrol 2019;32:549–66. 10.1007/s40620-018-00565-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sheng K, Zhang P, Chen L, et al. Intradialytic exercise in hemodialysis patients: a systematic review and meta-analysis. Am J Nephrol 2014;40:478–90. 10.1159/000368722 [DOI] [PubMed] [Google Scholar]
- 44.Smart N, Steele M, Steele M. Exercise training in haemodialysis patients: a systematic review and meta-analysis. Nephrology 2011;16:626–32. 10.1111/j.1440-1797.2011.01471.x [DOI] [PubMed] [Google Scholar]
- 45.Song Y-Y, Hu R-J, Diao Y-S, et al. Effects of exercise training on restless legs syndrome, depression, sleep quality, and fatigue among hemodialysis patients: a systematic review and meta-analysis. J Pain Symptom Manage 2018;55:1184–95. 10.1016/j.jpainsymman.2017.12.472 [DOI] [PubMed] [Google Scholar]
- 46.Thompson S, Wiebe N, Padwal RS, et al. The effect of exercise on blood pressure in chronic kidney disease: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2019;14:e0211032. 10.1371/journal.pone.0211032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vanden Wyngaert K, Van Craenenbroeck AH, Van Biesen W, et al. The effects of aerobic exercise on eGFR, blood pressure and VO2peak in patients with chronic kidney disease stages 3-4: a systematic review and meta-analysis. PLoS One 2018;13:e0203662. 10.1371/journal.pone.0203662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu X, Yang L, Wang Y, et al. Effects of combined aerobic and resistance exercise on renal function in adult patients with chronic kidney disease: a systematic review and meta-analysis. Clin Rehabil 2020;34:851–65. 10.1177/0269215520924459 [DOI] [PubMed] [Google Scholar]
- 49.Yamamoto R, Ito T, Nagasawa Y, et al. Efficacy of aerobic exercise on the cardiometabolic and renal outcomes in patients with chronic kidney disease: a systematic review of randomized controlled trials. J Nephrol 2021;34:155–64. 10.1007/s40620-020-00865-3 [DOI] [PubMed] [Google Scholar]
- 50.Yang H, Wu X, Wang M. Exercise affects cardiopulmonary function in patients with chronic kidney disease: a meta-analysis. Biomed Res Int 2017;2017:1–9. 10.1155/2017/6405797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang F, Zhou W, Sun Q, et al. Effects of intradialytic resistance exercises on physical performance, nutrient intake and quality of life among haemodialysis people: a systematic review and meta-analysis. Nurs Open 2021;8:529–38. 10.1002/nop2.274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang L, Wang Y, Xiong L, et al. Exercise therapy improves eGFR, and reduces blood pressure and BMI in non-dialysis CKD patients: evidence from a meta-analysis. BMC Nephrol 2019;20:398. 10.1186/s12882-019-1586-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhao Q-G, Zhang H-R, Wen X, et al. Exercise interventions on patients with end-stage renal disease: a systematic review. Clin Rehabil 2019;33:147–56. 10.1177/0269215518817083 [DOI] [PubMed] [Google Scholar]
- 54.Invalid citation.
- 55.Clyne N, Anding-Rost K. Exercise training in chronic kidney disease-effects, expectations and adherence. Clin Kidney J 2021;14:ii3–14. 10.1093/ckj/sfab012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Webster AC, Nagler EV, Morton RL, et al. Chronic kidney disease. Lancet 2017;389:1238–52. 10.1016/S0140-6736(16)32064-5 [DOI] [PubMed] [Google Scholar]
- 57.Cheung AK, Chang TI, Cushman WC, et al. Blood pressure in chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int 2019;95:1027–36. 10.1016/j.kint.2018.12.025 [DOI] [PubMed] [Google Scholar]
- 58.Kuo CP, Tsai MT, Lee KH, et al. Dose-Response effects of physical activity on all-cause mortality and major cardiorenal outcomes in chronic kidney disease. Eur J Prev Cardiol 2021. 10.1093/eurjpc/zwaa162 [DOI] [PubMed] [Google Scholar]
- 59.Graham-Brown MPM, March DS, Young R, et al. A randomized controlled trial to investigate the effects of intra-dialytic cycling on left ventricular mass. Kidney Int 2021;99:1478–86. 10.1016/j.kint.2021.02.027 [DOI] [PubMed] [Google Scholar]
- 60.Zelle DM, Klaassen G, van Adrichem E, et al. Physical inactivity: a risk factor and target for intervention in renal care. Nat Rev Nephrol 2017;13:152–68. 10.1038/nrneph.2016.187 [DOI] [PubMed] [Google Scholar]
- 61.Mezzani A, Hamm LF, Jones AM, et al. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: a joint position statement of the European association for cardiovascular prevention and rehabilitation, the American association of cardiovascular and pulmonary rehabilitation and the Canadian association of cardiac rehabilitation. Eur J Prev Cardiol 2013;20:442–67. 10.1177/2047487312460484 [DOI] [PubMed] [Google Scholar]
- 62.Chan D, Cheema BS. Progressive resistance training in end-stage renal disease: systematic review. Am J Nephrol 2016;44:32–45. 10.1159/000446847 [DOI] [PubMed] [Google Scholar]
- 63.Androga L, Sharma D, Amodu A, et al. Sarcopenia, obesity, and mortality in US adults with and without chronic kidney disease. Kidney Int Rep 2017;2:201–11. 10.1016/j.ekir.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Weisbord SD, Fried LF, Arnold RM, et al. Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol 2005;16:2487–94. 10.1681/ASN.2005020157 [DOI] [PubMed] [Google Scholar]
- 65.Flythe JE, Hilliard T, Castillo G, et al. Symptom prioritization among adults receiving In-Center hemodialysis: a mixed methods study. Clin J Am Soc Nephrol 2018;13:735–45. 10.2215/CJN.10850917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gregg LP, Bossola M, Ostrosky-Frid M, et al. Fatigue in CKD: epidemiology, pathophysiology, and treatment. Clin J Am Soc Nephrol 2021;16:1445-1455. 10.2215/CJN.19891220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Flythe JE, Dorough A, Narendra JH, et al. Perspectives on symptom experiences and symptom reporting among individuals on hemodialysis. Nephrol Dial Transplant 2018;33:1842–52. 10.1093/ndt/gfy069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Metzger M, Abdel-Rahman EM, Boykin H, et al. A narrative review of management strategies for common symptoms in advanced CKD. Kidney Int Rep 2021;6:894–904. 10.1016/j.ekir.2021.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Johansen KL. The promise and challenge of aerobic exercise in people undergoing long-term hemodialysis. Clin J Am Soc Nephrol 2021;16:505–7. 10.2215/CJN.01960221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fuller JT, Hartland MC, Maloney LT, et al. Therapeutic effects of aerobic and resistance exercises for cancer survivors: a systematic review of meta-analyses of clinical trials. Br J Sports Med 2018;52:1311. 10.1136/bjsports-2017-098285 [DOI] [PubMed] [Google Scholar]
- 71.Amir N, Tong A, McCarthy H, et al. Trajectories of quality of life in chronic kidney disease: a novel perspective of disease progression. Nephrol Dial Transplant 2021;36:1563–5. 10.1093/ndt/gfab006 [DOI] [PubMed] [Google Scholar]
- 72.Parker K. Intradialytic exercise is medicine for hemodialysis patients. Curr Sports Med Rep 2016;15:269–75. 10.1249/JSR.0000000000000280 [DOI] [PubMed] [Google Scholar]
- 73.Smart NA, Williams AD, Levinger I, et al. Exercise & Sports Science Australia (ESSA) position statement on exercise and chronic kidney disease. J Sci Med Sport 2013;16:406–11. 10.1016/j.jsams.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 74.March DS, Hurt AW, Grantham CE, et al. A cost-effective analysis of the CYCLE-HD randomized controlled trial. Kidney Int Rep 2021;6:1548–57. 10.1016/j.ekir.2021.02.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fuhrmann I, Krause R. Principles of exercising in patients with chronic kidney disease, on dialysis and for kidney transplant recipients. Clin Nephrol 2004;61 Suppl 1:S14–25. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-054887supp002.pdf (218.4KB, pdf)
bmjopen-2021-054887supp001.pdf (363.9KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.