Abstract
Introduction
The co-occurrence of health risk behaviours (HRBs, ie, tobacco smoking, at-risk alcohol use, insufficient physical activity and unhealthy diet) increases the risks of cancer, other chronic diseases and mortality more than additively; and applies to more than half of adult general populations. However, preventive measures that target all four HRBs and that reach the majority of the target populations, particularly those persons most in need and hard to reach are scarce. Electronic interventions may help to efficiently address multiple HRBs in healthcare patients. The aim is to investigate the acceptance of a proactive and brief electronic multiple behaviour change intervention among general hospital patients with regard to reach, retention, equity in reach and retention, satisfaction and changes in behaviour change motivation, HRBs and health.
Methods and analysis
A pre–post intervention study with four time points is conducted at a general hospital in Germany. All patients, aged 18–64 years, admitted to participating wards of five medical departments (internal medicine A and B, general surgery, trauma surgery, ear, nose and throat medicine) are systematically approached and invited to participate. Based on behaviour change theory and individual HRB profile, 175 participants receive individualised and motivation-enhancing computer-generated feedback at months 0, 1 and 3. Intervention reach and retention are determined by the proportion of participants among eligible patients and of participants who continue participation, respectively. Equity in reach and retention are measured with regard to school education and other sociodemographics. To investigate satisfaction with the intervention and subsequent changes, a 6-month follow-up is conducted. Descriptive statistics, multivariate regressions and latent growth modelling are applied.
Ethics and dissemination
The local ethics commission and data safety appointee approved the study procedures. Results will be disseminated via publication in international scientific journals and presentations on scientific conferences.
Trial registration number
Keywords: PREVENTIVE MEDICINE, Substance misuse, PUBLIC HEALTH, SOCIAL MEDICINE
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The behaviour change intervention to be tested targets on the great co-occurrence of health risk behaviours in general hospital patients.
The proactive computer-based intervention is designed to reach and retain the majority of patients.
The theory-based intervention provides highly individualised, motivation-enhancing feedback over multiple time points.
Established measures are used to assess health risk behaviours and motivational aspects.
The study is not designed to investigate the efficacy or effectiveness of the intervention.
Introduction
The co-occurrence of health risk behaviours (HRBs) such as tobacco smoking, at-risk alcohol use, insufficient physical activity and/ or unhealthy diet increases the risks of cancer, other chronic diseases and mortality more than additively.1 2 What is more, more than half of the adult population practise two or more of these HRBs.3–6 To reduce chronic diseases on the population level, individual prevention measures are recommended, particularly in healthcare settings.7–9
However, there are three major issues: First, the implementation of individual behaviour change interventions into routine healthcare is lacking. Lack of time, high work load and self-perceived lack of expertise in medical staff have been identified as barriers on the provider side.10 Second, behaviour change interventions often focus on single HRBs.11 Given that for example, 93% of the general hospital patients identified with at-risk alcohol use practice at least one other of the four HRBs,12 neglecting the co-occurrence of multiple HRBs in persons results in missed opportunities and cost-inefficiency. Third, the ‘reach’ dimension of the public health impact of interventions13 14 has been largely disregarded. That is, individual interventions often fail to reach the majority of the target population, and particularly those subgroups most in need and often hard to reach for preventive measures such as persons with low socioeconomic status.15 16 For example, persons with low level of school education do not only practice increased numbers of HRBs,17 18 but are also particularly hard to reach.16 The failure to reach this subgroup may further widen social inequity in health and mortality, a major and yet increasing issue in public health.19–21 Thus, in terms of the public health impact,14 the development of high-reach interventions that address multiple HRBs and that have a good chance to be adopted, implemented and maintained in healthcare are a major challenge for population-wide prevention of cancer and other chronic diseases.
In terms of adoption, implementation and maintenance of interventions in healthcare, digital behaviour change interventions may provide the means to relief healthcare personnel, and to store and recall intervention information reliably. In terms of reach, however, standalone applications such as web-based interventions fail to reach the majority of the target population. Although, potentially, accessible to everyone, they require the target population to seek for help, which does not apply to the vast majority of target populations, also due to little motivation to change HRBs.22 23 Interventions that aim to reach the whole target population with little selectivity need to be proactive and to provide helpful intervention strategies for the large part of persons with initially low motivation to change.24 25 Personalised cancer risk information derived from the number of HRBs, alone appears to be sufficient to change HRBs.26 The transtheoretical model of intentional behaviour change (TTM) provides a potential theoretical background on how to address behaviour change, particularly on how to enhance motivation in persons not yet ready to change certain behaviours.27 With regards to decreasing alcohol use, tobacco smoking and improving measures of health, TTM-based interventions targeting single behaviours have been found to produce desirable changes over 2 years in healthcare patients.28–31
General hospitals may provide an ideal setting to approach patients for the delivery of comprehensive lifestyle interventions for several reasons: First, two-thirds of general hospital patients report multiple of the four HRBs.12 Second, with participation rates of 80% and higher, general hospital patients have been found to be reached well for individual interventions targeting single behaviours.32 And third, within one single approach, a proactive automatised lifestyle intervention (PAL) could serve primary as well secondary prevention purposes among general hospital patients.
The purpose of this study protocol (30 May 2022; version 1) is to describe a study that intends to investigate the acceptance of a PAL among general hospital patients regardless of their current disease or injury. The intervention is designed (1) to address all four HRBs, (2) to reach the vast majority of the target population, also ‘most in need and hard to reach’ subgroups and (3) to produce long-term improvements concerning HRBs and health by applying psychological health behaviour change theory, by tailoring feedback to participant’s level of motivation to change and by providing multiple feedbacks. This protocol describes a study which aims to investigate (1) intervention reach (ie, the proportion of all eligible general hospital patients who participate), (2) intervention retention (ie, the proportion of all participants who continue participation after hospitalisation), (3) equity in reach and retention for example, with regards to socio-economic status, (4) satisfaction with the intervention and (5) trajectories of change with regards to motivation, HRBs and health-related measures over 6 months.
Methods and analysis
Study design
The single-group-intervention study, as summarised in table 1, is part of a broader research project ‘PAL for cancer prevention’ funded between 1 July 2020 and 31 December 2022. The project also included the preceding development of the intervention and the conduction of a survey among general hospital patients for purposes of intervention development (PAL-Survey). This current study (also: PAL-Pilot) includes three intervention timepoints at baseline, month 1, month 3 and a 6-month follow-up (figure 1). Recruitment and study procedure were tested on 3 days between 24 May 2022 and 27 May 2022. Enrolment of the first real participant started on 31 May 2022 and was completed with the last participant recruited on 5 July 2022.
Table 1.
Study information
| Data category | Information |
| Primary registry and trial identifying no | ClinicalTrials.gov NCT05365269; any important protocol modifications will be communicated here |
| Date of registration in primary registry | 5 May, 2022 |
| Secondary identifying numbers | D850000001 |
| Source(s) of monetary or material support | Deutsche Krebshilfe (German Cancer Aid) University Medicine Greifswald |
| Primary sponsor | University Medicine Greifswald |
| Secondary sponsor(s) | Deutsche Krebshilfe (German Cancer Aid) |
| Principal investigators | JF-A, Prof. Dr.—Design, preparation of protocol, publication of study reports, trial management UJ, Prof. Dr.—Design, preparation of protocol, publication of study reports |
| Data management team | AT, FK, KS— Maintenance of trial IT system and data entry, data verification, data cleansing, participant flow documentation, |
| Contact for public queries | JF-A, Prof. Dr. (see corresponding author information) AT (see CTN record) |
| Contact for scientific queries | JF-A, Prof. Dr. (see corresponding author information) |
| Public title | Proactive automatised lifestyle intervention for cancer prevention in general hospital patients |
| Scientific title | Proactive automatised lifestyle intervention to prevent cancer in general hospital patients |
| Country of recruitment | Germany |
| Health condition(s) or problem(s) studied | Hospitalisation at a general hospital, irrespective of reason for admission and health risk behaviour profile |
| Intervention(s) | Proactive automatised lifestyle intervention consisting of computer-generated, individually tailored feedback on health risk behaviours; 3 times over 3 months |
| Key inclusion and exclusion criteria | Ages eligible for study: 18–64 years Sexes eligible for study: both Accepts healthy volunteers: no Inclusion criteria: General hospital patients admitted to participating wards of five medical departments (internal medicine A and B, surgical medicine, trauma medicine, ear-nose-throat-medicine) Exclusion criteria: patient cognitively or physically incapable, patient with highly infectious disease, patient discharged or transferred within the first 24 hours, patient already asked for participation during previous hospital stay, patient with insufficient language skills, patient employed at the conducting research institute, patient with neither telephone nor email |
| Study type | Interventional Allocation: All patients receive intervention Intervention model: Single-group assignment Masking: non-blinded as participants are informed about the intervention prior to participation Primary purpose: prevention |
| Date of first enrolment | 31 May 2022 |
| Target sample size | 175 |
| Recruitment status | Completed: 5 July 2022 |
| Date of final data collection | Anticipated: 31 March 2023 |
| Primary outcome(s) | Intervention reach (time frame: month 0) Intervention retention (time frame: months 1, 3) |
| Key secondary outcomes | Satisfaction with intervention (time frame: month 6) Change in health risk behaviours, that is, physical activity, diet, alcohol use, tobacco smoking, sum of health risk behaviours (time frame: months 0, 1, 3, 6) Change in motivational measures, that is, stage of change, self-efficacy, decisional balance, processes of change (time frame: months 0, 1, 3, 6) Change in health-related measures, that is, body mass index, general health, mental health, number of sick days, non-communicable diseases, utilisation of healthcare (time frame: months 0, 6) |
Figure 1.
Study design PAL. PAL, proactive automatised lifestyle intervention.
Patient and public involvement
Patient involvement includes the assessment of patient satisfaction and discomfort with the intervention. However, beyond that, patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Recruitment
All consecutively admitted patients aged 18–64 years from participating wards of five medical departments (internal medicine A and B, surgical medicine, trauma medicine, ear, nose and throat) at the University Medicine Hospital Greifswald in northeastern Germany are eligible to participate. The hospital provides general hospital care for 600 000 people per annum. The catchment area includes the university town of Greifswald with 59000 inhabitants and surrounding communities within a radius of approximately 25 km; the extended catchment includes primarily rural communities within a radius of up to 65 km. On four weekdays each week (Tuesdays through Fridays), trained research assistants systematically approach each patient admitted on the previous day. Patients cognitively or physically incapable, with highly infectious diseases, discharged or transferred outside the study area within the first 24 hours, already asked to participate during a previous hospital stay, with insufficient language skills or employed at the conducting research institute are excluded.
A two-step recruitment procedure is used. All eligible patients are informed about the study procedure orally and in writing, and are first asked to participate in a survey on their lifestyle. Given oral and electronic consent, the participants complete the survey using tablet PCs. After survey completion, survey participants are asked by the research assistant to participate in the intervention study. Those providing informed written consent (including usage and storage of data, see online supplemental file) then receive the intervention over three time-points, and will be followed up 6 months after baseline using computer-assisted telephone interviews (CATIs). Patients with neither telephone nor email address are excluded.
bmjopen-2022-065136supp001.pdf (104.6KB, pdf)
Intervention
Intervention characteristics
Overall, the brief behaviour change intervention PAL is:
Proactive: All persons of the target population are approached personally and offered to participate.
Computer based: Feedback is generated by a computer-expert system software which generates letters that are handed out to participants (after baseline), sent to participants electronically and/or by ordinary mail in case of discharge and after months 1 and 3 (figure 2).
Multibehavioural: The participants receive feedback on their individual HRB profile, concerning physical inactivity, unhealthy diet, at-risk alcohol use and tobacco smoking. In addition, they receive motivation-enhancing feedback for up to two HRBs.
Figure 2.
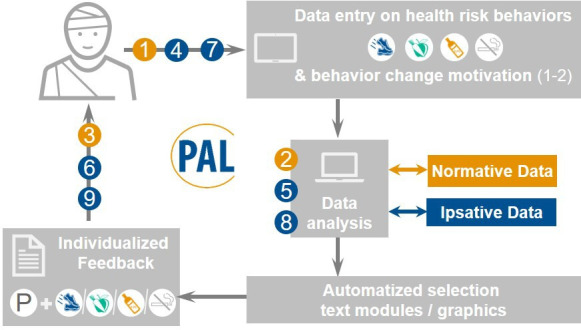
Computer-expert system PAL. Steps 1–3 baseline, steps 4–6 month 1, steps 7–9 month 3; p=Profile of individual health risk behaviours. PAL, proactive automatised lifestyle intervention.
In detail, the feedback itself is:
Individualised: A pool of more than 4500 text modules, graphics and allocation rules ensures that each information fits the participant’s data. Each feedback is unique, that is, no two participants receive the same feedback. For example, the smoking module alone allows the creation of 1040 to more than 442 000 unique feedbacks for smokers.33
Theory based: Based on psychological behaviour change theory, and to enhance motivation to change, the participants receive feedback for up to two HRBs tailored to their current motivational stage of change according to the TTM.27 While in the past, TTM-based interventions often missed the model’s multidimensional nature and failed to show convincing effects,34 35 interventions attending to the multiple dimensions of behaviour change theories, and of the TTM in particular, have been shown to be related to larger intervention effects,36 37 and to show over-time increasing intervention effects in healthcare populations.28–31 The intervention addresses all dimensions of the TTM, that is, stage of change, decisional balance, processes of change and self-efficacy.
Repetitive: Feedback is delivered three times, at baseline and 1 and 3 months later.
Ipsative: Participants receive feedback on changes in their HRB profile and on changes in behaviour and motivational aspects since the last intervention time point. To do so, each intervention contact first requires computer-based assessment of HRBs and motivational aspects. The current data are then compared with the participants’ previous data.
Normative: Participants receive feedback on how the participant’s responses compare to those of others of the same gender or in the same motivational stage. The normative data base is derived from previous studies conducted in the general population or in healthcare settings (eg, from PAL-Survey).
Intervention modules
PAL was developed by a multidisciplinary team of psychologists, a nutritional scientist and a software engineer. As a starting point two computer-based brief interventions addressing at-risk alcohol use and smoking cessation were used as prototypes. These interventions have been shown to successfully reduce the respective HRBs and to improve measures of health in healthcare patients over 2 years.28–31 These two interventions were slightly modified and integrated into the PAL intervention as two separate modules. PAL consists of five modules, that is, one HRB profile module and one module for each of the four HRBs:
Module ‘Profile’ is delivered to all participants first. It provides information on the participant’s individual HRB profile consisting of insufficient physical activity, insufficient vegetable and fruit intake as indicator of unbalanced diet, at-risk alcohol use and tobacco smoking. Based on guidelines by the WHO, insufficient physical activity is identified when less than 150 min of moderate or less than 75 min of vigorous physical activity or less than a respective combination of both is reported.38 Insufficient intake of vegetable and fruit is identified when less than five servings a day are reported.39 40 According to guidelines by the German Centre of Addiction Issues41 and the National Institute on Alcohol Abuse and Alcoholism,42 at-risk alcohol use is identified when women/men report on average more than 1 drink (12g of pure alcohol)/2 drinks (24 g) per day and/or more than 3 drinks/4 drinks per occasion. Any tobacco smoking is considered HRB.
Module ‘Inactivity’ is delivered to participants reporting insufficient physical activity. It contains (1) behaviour feedback on the participant’s physical activity in relation to guidelines38 and other women or men, and (2) motivation-enhancing feedback on increasing physical activity. Table 2 includes further details.
Module ‘Diet’ is delivered to participants reporting insufficient vegetable and fruit intake. It contains (1) behavioural feedback on the participant’s intake of fibre, fat, salt and sugar and on vegetable and fruit intake according to recommendations by the WHO and the World Cancer Research Fund,39 40 43–45 and (2) motivation-enhancing feedback on increasing vegetable and fruit intake.
Module ‘Alcohol’ is delivered to participants reporting at-risk alcohol use. It contains (1) behavioural feedback on the participant’s alcohol use in relation to guidelines41 46 and others, and (2) motivation-enhancing feedback on reducing alcohol use.
Module ‘Smoking’ is delivered to participants reporting to be tobacco smokers currently. It contains (1) behavioural feedback and (2) motivation-enhancing feedback on quitting smoking.
Table 2.
Content of PAL intervention modules
| Modules | Target | For whom | Behavioural feedback | Motivational feedback | |||||
| Recommendations | Behaviour | Normative | Ipsative | TTM constructs | Normative | Ipsative | |||
| Profile HRBs | Provide information on overall lifestyle | All | Listed below | Overview over individual HRBs | – | Month 1 Month 3 |
– | – | – |
| Physical inactivity | Increase physical activity | Participants with insufficient physical activity | ≥150 or ≥75 min of moderate or vigorous activity per week or an according combination of both38 | No of minutes per week | Baseline | Month 1 Month 3 |
Stage of change Processes Decisional balance Self-efficacy Plan to change |
Baseline | Month 1 Month 3 |
| Unbalanced diet | Increase vegetable/ fruit intake | Participants with low vegetable and fruit intake | 5 servings/day39 40 | Servings of vegetable and fruit per day | – | Month 1 Month 3 |
Stage of change Processes Decisional balance Self-efficacy Plan to change |
Baseline | Month 1 Month 3 |
| Increase fibre, decrease fat, salt, sugar intake* | Participants with none of the 4 HRBs | Fat <30% of total energy intake Fibre ≥30 g/ day Salt <5 g/ day Sugar <50 g/ day 39 40 43–45 |
Fibre intake, Salt intake, Fat intake, Sugar intake |
– | Month 1 Month 3 |
– | – | – | |
| At-risk alcohol use | Decrease alcohol use | Participants drinking alcohol at-risk | ≤7/14 drinks per week and <4/5 drinks per drinking occasion for women/men41 46 | Drinks per drinking day; Heavy drinking occasions; Risk of own drinking |
Baseline Month 1 Month 3 |
Month 1 Month 3 |
Stage of change Processes Decisional balance Self-efficacy Plan to change |
Baseline Month 1 Month 3 |
Month 1 Month 3 |
| Tobacco smoking | Quit smoking | Participants currently smoking | Non-smoking | No of cigarettes | Baseline | Month 1 Month 3 |
Stage of change Processes Decisional balance Self-efficacy |
Baseline | Month 1 Month 3 |
*The behavioural feedback on the intake of fibre, fat, salt and sugar is not only delivered to participants with insufficient vegetable and fruit intake but also to participants with none of the four HRBs (alcohol, smoking, insufficient vegetable and fruit intake, physical inactivity) in addition to the behavioural feedback provided by the module ‘Profile’.
HRBs, health risk behaviours; PAL, proactive automatised lifestyle intervention; TTM, transtheoretical model of intentional behaviour change.
Each module’s written feedback is supported by visualising elements. The profile module results in about an ½ A4 page; and the four HRB modules result in about 2–3 feedback pages each. To avoid overwhelming participants with multiple HRBs, a maximum of two HRB modules are selected per participant based on evidence-based decisions and participant’s preference (figure 3). In detail, participants with more than 2 HRBs receive at least one of the two modules for which efficacy has been established, that is, ‘alcohol’ or ‘smoking’, depending on the following decision rules: (1) If either at-risk alcohol use or tobacco smoking is present, the according module is selected by the system. The second module is determined by asking participants ‘What part of your lifestyle would you have to change to achieve the largest impact on your quality of life?’ with two response options (physical activity; diet). (2) If both at-risk alcohol use and tobacco smoking are present, participants are first asked to choose between alcohol use and tobacco smoking by using the above question, and are asked again to choose between the remaining two or three options. (3) There is one exception to both rules: In case of AUDIT-C scores ≥8, the system does not preselect the module ‘alcohol’ (rule 1) or tobacco smoking is preselected (rule 2) as the efficacy of the module ‘alcohol’ has not been established for at-risk users with AUDIT-scores ≥8.47
Figure 3.

Composition of PAL feedback modules based on co-occurrence of health risk behaviours and selection by system and participant preference. *Month 0 only. AUDIT-C, Alcohol Use Disorder Identification Test-consumption; PAL, proactive automatised lifestyle intervention.
Intervention development study PAL-Survey: The preceding developmental process included the conduction of a survey on HRBs and TTM measures among 256 general hospital patients (PAL-Survey): (1) to test the questionnaires and/ or German translations concerning the assessment of HRBs and TTM-based measures for the new modules ‘inactivity’ and ‘diet’; (2) to obtain normative data for the TTM-measures required for normative feedback as part of the modules ‘inactivity’ and ‘diet’; and (3) to obtain information on the participants preferences concerning feedback in case multiple HRBs occur.48
Intervention delivery
After baseline, participants receive the first part of the computer-generated feedback. One and 3 months later, participants are contacted by email to fill in intervention questionnaires. If contact attempts by email fail or if participants prefer to be phoned, they are contacted for CATIs by a research assistant to facilitate intervention retention. The 1-month and 3-month feedback letters are sent out accordingly, either online or by ordinary mail. Intervention delivery is discontinued when participants do not wish to participate any longer.
Follow-ups
Follow-ups are conducted 6 months after initial contact by self-administered online questionnaires or CATIs. Follow-up participation is enhanced by sending out prepaid incentives (ie, previously self-selected 10 Euro-vouchers) along with postal reminders. Paying monetary incentives is an evidence-based strategy to increase study participation, to reduce selectivity and thereby to increase the informative value of the study. Delivering monetary incentives before rather than after actual participation results in particularly high participation.49 50
Measures
Computer-assisted assessments described in more detail in table 3 are based on self-report. To increase the reliability of self-report, standardised and validated psychometrical measures are used if available. At baseline, assessments are self-administered. Patients are introduced into the handling of the questionnaire using tablet computers and if required, they may receive support by research assistants. Intervention assessments at months 1 and 3 may either be self-administered online or through CATIs. They primarily include assessments required for individualised feedback. Follow-ups after 6 months are conducted through CATIs if possible or self-administered online. It includes most of the baseline assessment plus assessments on satisfaction with the intervention. All research assistants involved in recruitment and data collection are trained and supervised on a weekly basis.
Table 3.
PAL self-report measures for each measurement time point
| Measure | Reference; modifications | No of items | Target group at month | |||
| 0 | 1 | 3 | 6 | |||
| Health risk behaviours | ||||||
| Physical inactivity (I) | ||||||
| European Health Interview Survey-Physical Activity Questionnaire | Item seven modified: active day instead of week53 | 8 | All | All | All | All |
| Physical effort | Own construction | 3 | All | All | All | All |
| Unbalanced diet | ||||||
| Vegetable, fruit (V) | Own construction, similar to, assesses servings of food containing fat, fibre, salt and/or sugar per day/week; complemented by descriptive examples55 | 2 | All | All | All | All |
| Fat, fibre, salt, sugar | 14 | All | All | All | All | |
| At-risk alcohol use (A) | ||||||
| Alcohol Use Disorder Identification Test- Consumption | Item three gender-specific: ≥4 women, ≥5 men56 57 | 3 | All | All | All | All |
| Time-Line-Follow-back past month | Based on60 | 3 | A | A | A | A |
| Exploration abstinence | Own construction | 2 | Abstainers | – | – | – |
| Tobacco smoking (S) | ||||||
| Smoking status | 53 61 | 1 | All | All | All | All |
| Cigarettes per day | 53 61 | 2 | S | S | S | S |
| Motivation modules (maximum of 2) | ||||||
| Module Inactivity | ||||||
| Staging algorithm | Adapted to physical activity from32 | 4 | I | I | I | I |
| Processes of change | Own translation62 | 18 | I * | I * | I * | I * |
| Decisional balance | Own translation62 | 9 | I * | I * | I * | I * |
| Self-efficacy | Own translation62 | 6 | I * | I * | I * | I * |
| Module diet (vegetable and fruit intake) | ||||||
| Staging algorithm | Own translation; modification based on63 64 | 1 | V | V | V | V |
| Processes of change | Own translation63 | 14 | V * | V * | V * | V * |
| Decisional balance | Own translation63 | 8 | V * | V * | V * | V * |
| Self-efficacy | Own translation63 | 6 | V * | V * | V * | V * |
| Module alcohol | ||||||
| Staging algorithm | Described in; developed according to refs 32 64 65 | 4 | A | A | A | A |
| Processes of change | 66 67 | 16 | A * | A * | A * | A * |
| Decisional balance | 68 69 | 10 | A * | A * | A * | A * |
| Self-efficacy | 68 70 | 8 | A * | A * | A * | A * |
| Module smoking | ||||||
| Staging algorithm | Modification based on refs 64 65 71 | 2 | S | S | S | S |
| Processes of change | 71 72 | 19/24 | S * | S * | S * | S * |
| Decisional balance | 71 | 8 | S * | S * | S * | S * |
| Self-efficacy | 71 | 9 | S * | S * | S * | S * |
| Intervention aspects | ||||||
| Module selection | ||||||
| Expected impact of change on life | Own construction | 2 | ≥3 HRBs | – | – | – |
| Acceptance and satisfaction | Based on refs 51 52 73 | 29 | – | – | – | All |
| Health | ||||||
| Body weight and height | 2 | All | – | – | All | |
| General health | 74 | 1 | All | – | – | All |
| Sick days past 6 months | Described in28 | 1 | All | – | – | All |
| Non-communicable diseases | Own construction, examples from53 | 4 | All | – | – | All |
| Mental health inventory | 75 76 | 5 | All | – | – | All |
| Utilisation medical care | Modified time frame: 6 instead of 12 months53 | 6 | All | – | – | All |
| Sociodemographics | ||||||
| Sex, age | 2 | All | All | All | All | |
| Family status, children | 3 | All | – | – | – | |
| School education, employment | 77 | 4 | All | – | – | – |
| Migrant background | 1 | All | – | – | – | |
*When health risk behaviour present and selected for intervention.
A, at risk alcohol use present; I, physical inactivity present; PAL, proactive automatised lifestyle intervention; S, tobacco smoking present; V, insufficient vegetable and fruit intake present.
Primary outcomes
Primary outcomes are intervention reach and retention. Reach is measured using observed numbers and proportions of participants reached among all eligible patients at baseline. Retention is measured using observed numbers and proportions of participants who continued participation at months 1 and 3. These indicators for intervention reach and retention are analysed for the total sample and subgroups of particular interests, such as participants with low school education.
Secondary outcomes
Secondary outcomes are based on self-report and include satisfaction with the intervention after 6 months, and changes in HRBs, health and motivation (table 1).
Satisfaction with intervention is assessed at month 6, using a 29-item measure based on.51 52 The modified and adapted measure, assesses satisfaction with intervention process (ie, intervention characteristic, dose and format, usage, overall) and intervention outcome (ie, discomfort, attribution of outcomes to treatment).
Physical activity is assessed using the European Health Interview Survey-Physical Activity Questionnaire53 54 plus three self-created items on physical effort. The questionnaire includes eight items on sitting, muscle strengthening activities and frequency and quantity of walking and cycling for transportation purpose and of sports activity in leisure time. As it does not differentiate between moderate and vigorous activity and this differentiation is required for feedback according to WHO recommendations (as reported above), three items with three response categories separately assess the effort used for walking, cycling and sports activity. To weigh minutes reported for walking and cycling, the item asks ‘When doing so, do you breathe or sweat more than normal or does your heart beat faster?’. The response category ‘No, usually not’ indicates that the minutes reported may not be counted as moderate physical activity according to WHO recommendations, and are excluded from the total minutes of physical activity. ‘Yes, frequently’ indicates that the number of minutes reported may in part be considered as moderate activity, and reported minutes are multiplied by 0.5. ‘Yes, almost always’ indicates that minutes reported may be considered as moderate activity, and minutes are calculated as reported. To weigh minutes reported for sports, the item asks ‘When doing so, how much stronger than normal do you breathe, sweat or does your heart beat?’. The response category ‘A little stronger’ indicates moderate activity, and minutes are calculated as reported. ‘Much stronger’ indicates vigorous activity and minutes reported are multiplied by 2.0. ‘Sometimes so and sometimes so’ indicates a combination of moderate and vigorous activity, and minutes are multiplied by 1.5. When summing up all three products, the total number of minutes of moderate activity per week is obtained.
Diet is assessed using a diet screener, a measure developed similar to the Mediterranean Diet screener.55 This 16-item diet screener was needed to provide a brief measure assessing the intake of fat, fibre, salt and sugar. Participants are required to report the number of servings of different foods per day or per week. Each item is supported by several examples of what one serving may include. The calculation of intake of fibre in gram is based on four items (vegetable, fruit, bread, other food rich in fibre), of fat in kilocalories on seven items (cheese, convenience food, salted snacks, eggs, fatty fish, red meat, processed meat, butter/ oil, milk), of salt in gram on six items (cheese, convenience food, salted snacks, red meat, processed meat, bread) and of sugar in gram on three items (sweets, added sugar, sweetened drinks). Vegetable and fruit intake of less than five servings a day is used as indicator of HRB.
Alcohol use is assessed using the Alcohol Use Disorder Identification Test-Consumption.56 Women with sum scores of 4 and higher and men with values of 5 and higher are considered HRB, that is, to drink alcohol at-risk.57
Tobacco smoking is assessed by smoking status and the number of cigarettes per day. Any occasional or daily smoking is considered HRB.
An overall HRB index, that is, the sum of the current HRBs is created. Insufficient physical inactivity, insufficient With each HRB counted as 1, the index ranges between 0 and 4.58 Test characteristics of this particular index are investigated as part of the project. Similar measures have been found to predict individuals’ risks of various cancer diseases in women and men for example,.59
Measures on health include body weight and height to calculate the body-mass-index, general health, mental health, number of sick days in previous 6 months, non-communicable diseases, utilisation of healthcare. These are assessed at baseline and at month 6.
Measures on motivation include packages of four TTM measures assessing motivational stage of behaviour change, decisional balance, processes of change and self-efficacy for each HRB (table 3). The assessment is required to generate motivation-enhancing feedback as part of the intervention. While stage of change is assessed among all participants reporting the according HRB, decisional balance, processes of change and self-efficacy are assessed among those participants assigned to the according intervention module. The TTM measures for the modules ‘alcohol’ and ‘smoking’ have been used previously30 31; those for the modules ‘inactivity’ and ‘diet’ were translated from English into German, tested and modified as part of the intervention development study PAL-Survey.
Data management, monitoring and safety
Assessment data are entered electronically, that is, either through tablet computers, online or CATIs. To enable the determination of the proportion of patients reached versus not reached for the intervention, a temporary contact list is used. When data collection is finished, the doctoral students will conduct data cleansing, including data plausibility checks, labelling of variables and values. A codebook is provided.
To ensure that all staff involved with collection, entry and management of data adhere to the protocol and to discuss upcoming issues, weekly meetings are conducted. Given little risks from behavioural interventions, a data monitoring committee is not needed, the study is not expected to be stopped prematurely, and no ancillary or post-trial care is planned.
The study procedures concerning usage, storage and delivery of data have been approved by the local data security appointee. Confidentiality before, during and after the trial is ensured through, for example, pseudonymisation, storage of informed consent forms with linking participant identifying information and participant ID in a steel locker with access limited to an independent trustee, separate storage of participant identifying information and research data, anonymised evaluation of data, non-release of participant identifying data outside the study, security of all databases by password-protected access systems.
The principal investigator will have full access to the complete final dataset and oversee the intrastudy data sharing process, with input from the data management team. Full access to participant identifying information is limited to an independent trustee. To ensure confidentiality, data dispersed to project team members are blinded of any identifying information.
Statistical analyses
Intervention reach and retention are determined by descriptive statistics, namely (1) the proportion of participants among eligible patients and (2) the proportion of participants who continue participation after hospitalisation among all initial trial participants. Equity in reach and retention are measured with regard to school education and other sociodemographics using multivariate regressions. Satisfaction with the intervention is determined by descriptive statistics. To analyse change in motivational measures, HRBs and health measures over four time points in 6 months, latent growth modelling is applied, allowing the inclusion of all initial participants regardless of missingness using maximum likelihood estimation.
Sample size determination
The longitudinal sample to be recruited is 175 participants irrespective of HRB profile and reason of hospital admission. The sample is expected to be large enough to investigate the acceptance of the PAL intervention in terms of reach, retention and satisfaction, to provide a sufficient number of cases for latent growth modelling, and to have sufficient power (80%, α=0.05, two tailed) to detect small-sized to medium-sized effects (Cohen’s d=0.38) in mean differences between two independent groups, for example, participants versus non-participants. Expecting 90% of the eligible patients participating in the survey, and 80% of these to participate in the intervention study as achieved in own previous studies,32 we expect to approach about 243 patients over 2 months.
Ethics and dissemination
Intervention participants provide written informed consent. The ethical commission of the University Medicine Greifswald and data safety appointee approved the study procedures described above (BB 024/17; BB 024/17a).
Results will be disseminated via publication in international scientific journals and presentations on scientific conferences. Substantive contributions to the design, conduct, interpretation and reporting of the trial are recognised through the granting of authorship on the final trial report. In terms of reproducible research, anonymised data and supporting information including the codebook and analytical code may be made available on reasonable request.
Supplementary Material
Acknowledgments
We very much appreciate our student assistants Sarah Habicht and Greta Otto who provided support in designing pictograms for the intervention.
Footnotes
Contributors: JF-A and UJ designed the study and acquired funding. JF-A, FK and AT initiate the study design, and KS and MS help with implementation. JF-A, FK, AT, KS, MS and KK integrated and designed new intervention modules for the purpose of this study. CG programmed the electronic assessment and intervention. JF-A wrote the first draft of the study protocol. All authors contributed to refinement of the study protocol and approved the final manuscript.
Funding: JF-A and UJ receive funding from the German Cancer Aid (grant no. 70113382, 70114206) to develop and test the PAL intervention among general hospital patients. We acknowledge support for the Article Processing Charge by the German Research Foundation and the Open Access Publication Fund of the University of Greifswald (grant no. N/A).
Disclaimer: The funders have no role in study design; collection, analysis and interpretation of data; writing the report; and the decision to submit the report for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; peer reviewed for ethical and funding approval prior to submission.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Khaw K-T, Wareham N, Bingham S, et al. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med 2008;5:e12. 10.1371/journal.pmed.0050012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen KEN, Johnsen NF, Olsen A, et al. The combined impact of adherence to five lifestyle factors on all-cause, cancer and cardiovascular mortality: a prospective cohort study among Danish men and women. Br J Nutr 2015;113:849–58. 10.1017/S0007114515000070 [DOI] [PubMed] [Google Scholar]
- 3.John U, Hanke M, Freyer-Adam J. Health risk behavior patterns in a national adult population survey. Int J Environ Res Public Health 2018;15:873. 10.3390/ijerph15050873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y, Croft JB, Wheaton AG, et al. Clustering of five health-related behaviors for chronic disease prevention among adults, United States, 2013. Prev Chronic Dis 2016;13:E70. 10.5888/pcd13.160054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poortinga W. The prevalence and clustering of four major lifestyle risk factors in an English adult population. Prev Med 2007;44:124–8. 10.1016/j.ypmed.2006.10.006 [DOI] [PubMed] [Google Scholar]
- 6.Schuit AJ, van Loon AJM, Tijhuis M, et al. Clustering of lifestyle risk factors in a general adult population. Prev Med 2002;35:219–24. 10.1006/pmed.2002.1064 [DOI] [PubMed] [Google Scholar]
- 7.American Heart Association . The American heart association diet and lifestyle recommendations, 2019. Available: https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/aha-diet-and-lifestyle-recommendations [Accessed 14 Jun 2019].
- 8.World Cancer Research Fund/American Institute for Cancer Research . Diet, nutrition, physical activity and cancer: a global perspective. continous update project expert report 2018. Washington: World Cancer Research Fund/American Institute for Cancer Research, 2018. [Google Scholar]
- 9.World Health Organization . Global status report on alcohol and health 2014. Geneva, Switzerland: WHO Press, 2014. [Google Scholar]
- 10.Johnson M, Jackson R, Guillaume L, et al. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health 2011;33:412–21. 10.1093/pubmed/fdq095 [DOI] [PubMed] [Google Scholar]
- 11.Prochaska JJ, Prochaska JO. A review of multiple health behavior change interventions for primary prevention. Am J Lifestyle Med 2011;5. 10.1177/1559827610391883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freyer-Adam J, Noetzel F, Baumann S, et al. Behavioral health risk factor profiles in general Hospital patients: identifying the need for screening and brief intervention. BMC Public Health 2019;19:1594. 10.1186/s12889-019-7931-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glasgow RE, Klesges LM, Dzewaltowski DA, et al. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med 2004;27:3–12. 10.1207/s15324796abm2701_2 [DOI] [PubMed] [Google Scholar]
- 14.Glasgow RE, Estabrooks PE. Pragmatic applications of RE-AIM for health care initiatives in community and clinical settings. Prev Chronic Dis 2018;15:E02. 10.5888/pcd15.170271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schneider F, Schulz DN, Pouwels LHL, et al. The use of a proactive dissemination strategy to optimize reach of an internet-delivered computer tailored lifestyle intervention. BMC Public Health 2013;13:721. 10.1186/1471-2458-13-721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bender AM, Jørgensen T, Helbech B, et al. Socioeconomic position and participation in baseline and follow-up visits: the Inter99 study. Eur J Prev Cardiol 2014;21:899–905. 10.1177/2047487312472076 [DOI] [PubMed] [Google Scholar]
- 17.Fine LJ, Philogene GS, Gramling R, et al. Prevalence of multiple chronic disease risk factors. 2001 National health interview survey. Am J Prev Med 2004;27:18–24. 10.1016/j.amepre.2004.04.017 [DOI] [PubMed] [Google Scholar]
- 18.Linardakis M, Smpokos E, Papadaki A, et al. Prevalence of multiple behavioral risk factors for chronic diseases in adults aged 50+, from eleven European countries - the SHARE study (2004). Prev Med 2013;57:168–72. 10.1016/j.ypmed.2013.05.008 [DOI] [PubMed] [Google Scholar]
- 19.Commission on Social Determinants of Health . Closing the gap in a generation: health equity through action on the social determinants of health. Geneva, Switzerland: World Health Organization, 2008. [DOI] [PubMed] [Google Scholar]
- 20.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001-2014. JAMA 2016;315:1750–66. 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackenbach JP, Kulhánová I, Menvielle G, et al. Trends in inequalities in premature mortality: a study of 3.2 million deaths in 13 European countries. J Epidemiol Community Health 2015;69:207–17. 10.1136/jech-2014-204319 [DOI] [PubMed] [Google Scholar]
- 22.Garrett NA, Alesci NL, Schultz MM, et al. The relationship of stage of change for smoking cessation to stage of change for fruit and vegetable consumption and physical activity in a health plan population. Am J Health Promot 2004;19:118–27. 10.4278/0890-1171-19.2.118 [DOI] [PubMed] [Google Scholar]
- 23.Rumpf HJ, Hapke U, Meyer C, et al. Motivation to change drinking behavior: comparison of alcohol-dependent individuals in a general Hospital and a general population sample. Gen Hosp Psychiatry 1999;21:348–53. 10.1016/s0163-8343(99)00032-8 [DOI] [PubMed] [Google Scholar]
- 24.Prochaska JO. Multiple health behavior research represents the future of preventive medicine. Prev Med 2008;46:281–5. 10.1016/j.ypmed.2008.01.015 [DOI] [PubMed] [Google Scholar]
- 25.Hannöver W, Thyrian JR, Hapke U, et al. The readiness to change questionnaire in subjects with hazardous alcohol consumption, alcohol misuse and dependence in a general population survey. Alcohol Alcohol 2002;37:362–9. 10.1093/alcalc/37.4.362 [DOI] [PubMed] [Google Scholar]
- 26.Masson G, Mills K, Griffin SJ, et al. A randomised controlled trial of the effect of providing online risk information and lifestyle advice for the most common preventable cancers. Prev Med 2020;138:106154. 10.1016/j.ypmed.2020.106154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12:38–48. 10.4278/0890-1171-12.1.38 [DOI] [PubMed] [Google Scholar]
- 28.Freyer-Adam J, Baumann S, Bischof G, et al. Sick days in general Hospital patients two years after brief alcohol intervention: secondary outcomes from a randomized controlled trial. Prev Med 2020;139:106106. 10.1016/j.ypmed.2020.106106 [DOI] [PubMed] [Google Scholar]
- 29.Freyer-Adam J, Baumann S, Haberecht K, et al. Can brief alcohol interventions in general Hospital inpatients improve mental and general health over 2 years? results from a randomized controlled trial. Psychol Med 2019;49:1722–30. 10.1017/S0033291718002453 [DOI] [PubMed] [Google Scholar]
- 30.Freyer-Adam J, Baumann S, Haberecht K, et al. In-person alcohol counseling versus computer-generated feedback: results from a randomized controlled trial. Health Psychol 2018;37:70–80. 10.1037/hea0000556 [DOI] [PubMed] [Google Scholar]
- 31.Meyer C, Ulbricht S, Baumeister SE, et al. Proactive interventions for smoking cessation in general medical practice: a quasi-randomized controlled trial to examine the efficacy of computer-tailored letters and physician-delivered brief advice. Addiction 2008;103:294–304. 10.1111/j.1360-0443.2007.02031.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freyer-Adam J, Baumann S, Haberecht K, et al. In-person and computer-based alcohol interventions at general hospitals: reach and retention. Eur J Public Health 2016;26:844–9. 10.1093/eurpub/ckv238 [DOI] [PubMed] [Google Scholar]
- 33.Schumann A, John U, Ulbricht S, et al. Variability of tailoring of a smoking cessation intervention based on the transtheoretical model. Addict Behav 2007;32:3083–7. 10.1016/j.addbeh.2007.06.004 [DOI] [PubMed] [Google Scholar]
- 34.Bridle C, Riemsma RP, Pattenden J, et al. Systematic review of the effectiveness of health behavior interventions based on the transtheoretical model. Psychol Health 2005;20:283–301. 10.1080/08870440512331333997 [DOI] [Google Scholar]
- 35.Hutchison AJ, Breckon JD, Johnston LH. Physical activity behavior change interventions based on the transtheoretical model: a systematic review. Health Educ Behav 2009;36:829–45. 10.1177/1090198108318491 [DOI] [PubMed] [Google Scholar]
- 36.Noar SM, Benac CN, Harris MS. Does tailoring matter? meta-analytic review of tailored print health behavior change interventions. Psychol Bull 2007;133:673–93. 10.1037/0033-2909.133.4.673 [DOI] [PubMed] [Google Scholar]
- 37.Webb TL, Joseph J, Yardley L, et al. Using the Internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010;12:e4. 10.2196/jmir.1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization . WHO guidelines on physical activity and sedentary behaviour, 2020. Available: file:///C:/Users/freyerj/AppData/Local/Temp/9789240015128-eng.pdf [PubMed]
- 39.World cancer research Fund/American Institute for cancer Research/American Institute for cancer research. continous update project expert report 2018. recommendations and public health and policy implications. Available: dietandcancerreport.org 2018
- 40.World Health Organization . Healthy diet online: who, 2020. Available: https://www.who.int/news-room/fact-sheets/detail/healthy-diet [Accessed 16 Mar 2022].
- 41.Seitz HK, Bühringer G, Mann K. [Limits for the consumption of alcoholic beverages: Guidelines of the scientific board of trustees of the DHS]. In: Yearbook addiction 2008. Geesthacht: Neuland, 2008: 205–9. [Google Scholar]
- 42.National Institute on Alcohol Abuse and Alcoholism . Underage drinking: a major public health challenge, 2003. Available: http://pubs.niaaa.nih.gov/publications/aa59.htm
- 43.World Health Organization . Guideline: sodium intake for adults and children. Geneva, Switzerland: WHO Press, 2012. [PubMed] [Google Scholar]
- 44.World Health Organization . Global status report on noncommunicable diseases 2014. Geneva, Switzerland: WHO Press, 2014. [Google Scholar]
- 45.World Health Organization . Guideline: sugar intake for adults and children. Geneva, Switzerland: WHO Press, 2015. [Google Scholar]
- 46.National Institute on Alcohol Abuse and Alcoholism . Rethinking drinking: alcohol and your health 2021. Available: https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Whats-the-harm/What-is-Alcohol-Misuse.aspx [Accessed 10 Aug 2022].
- 47.Baumann S, Gaertner B, Haberecht K, et al. How alcohol use problem severity affects the outcome of brief intervention delivered in-person versus through computer-generated feedback letters. Drug Alcohol Depend 2018;183:82–8. 10.1016/j.drugalcdep.2017.10.032 [DOI] [PubMed] [Google Scholar]
- 48.Spielmann M, Tiede A, Krolo F. Co-Occurring behavioral health risk factors and sick days prior to hospitalization in general Hospital patients. submitted 2022. [DOI] [PMC free article] [PubMed]
- 49.Edwards P, Cooper R, Roberts I, et al. Meta-Analysis of randomised trials of monetary incentives and response to Mailed questionnaires. J Epidemiol Community Health 2005;59:987–99. 10.1136/jech.2005.034397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Edwards P, Roberts I, Clarke M, et al. Increasing response rates to postal questionnaires: systematic review. BMJ 2002;324:1183. 10.1136/bmj.324.7347.1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sidani S, Epstein DR, Fox M. Psychometric evaluation of a multi-dimensional measure of satisfaction with behavioral interventions. Res Nurs Health 2017;40:459–69. 10.1002/nur.21808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krause K, Guertler D, Moehring A, et al. Feasibility and acceptability of an intervention providing computer-generated tailored feedback to target alcohol consumption and depressive symptoms in Proactively recruited health care patients and Reactively recruited media volunteers: results of a pilot study. Eur Addict Res 2019;25:119-131. 10.1159/000499040 [DOI] [PubMed] [Google Scholar]
- 53.Koch-Institut R. Fragebogen zur Studie "Gesundheit in Deutschland aktuell": GEDA 2014-2015-EHIS. J Health Monit 2017;2:105–35. [Google Scholar]
- 54.Baumeister SE, Ricci C, Kohler S, et al. Physical activity surveillance in the European Union: reliability and validity of the European health interview Survey-Physical activity questionnaire (EHIS-PAQ). Int J Behav Nutr Phys Act 2016;13:61. 10.1186/s12966-016-0386-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Martínez-González MA, García-Arellano A, Toledo E, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One 2012;7:e43134. 10.1371/journal.pone.0043134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bush K, Kivlahan DR, McDonell MB. The audit alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med 1998;158:1789–95. 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- 57.Reinert DF, Allen JP. The alcohol use disorders identification test: an update of research findings. Alcohol Clin Exp Res 2007;31:185–99. 10.1111/j.1530-0277.2006.00295.x [DOI] [PubMed] [Google Scholar]
- 58.Prochaska JJ, Velicer WF, Nigg CR, et al. Methods of quantifying change in multiple risk factor interventions. Prev Med 2008;46:260–5. 10.1016/j.ypmed.2007.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim DJ, Rockhill B, Colditz GA. Validation of the Harvard cancer risk index: a prediction tool for individual cancer risk. J Clin Epidemiol 2004;57:332–40. 10.1016/j.jclinepi.2003.08.013 [DOI] [PubMed] [Google Scholar]
- 60.Sobell LC, Agrawal S, Sobell MB, et al. Comparison of a quick drinking screen with the timeline Followback for individuals with alcohol problems. J Stud Alcohol 2003;64:858–61. 10.15288/jsa.2003.64.858 [DOI] [PubMed] [Google Scholar]
- 61.John U, Meyer C, Schumann A, et al. A short form of the Fagerström test for nicotine dependence and the Heaviness of smoking index in two adult population samples. Addict Behav 2004;29:1207–12. 10.1016/j.addbeh.2004.03.019 [DOI] [PubMed] [Google Scholar]
- 62.Geller KS, Nigg CR, Motl RW, et al. Transtheoretical model constructs for physical activity behavior are invariant across time among ethnically diverse adults in Hawaii. Psychol Sport Exerc 2012;13:606–13. 10.1016/j.psychsport.2012.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Horwath CC, Nigg CR, Motl RW, et al. Investigating fruit and vegetable consumption using the transtheoretical model. Am J Health Promot 2010;24:324–33. 10.4278/ajhp.071218138 [DOI] [PubMed] [Google Scholar]
- 64.Lippke S, Ziegelmann JP, Schwarzer R, et al. Validity of stage assessment in the adoption and maintenance of physical activity and fruit and vegetable consumption. Health Psychol 2009;28:183–93. 10.1037/a0012983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.DiClemente CC, Prochaska JO, Fairhurst SK, et al. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol 1991;59:295–304. 10.1037//0022-006x.59.2.295 [DOI] [PubMed] [Google Scholar]
- 66.DiClemente CC, Carbonari JP, Addy RC. Alternate short forms of a processes of change scale for alcoholism treatment. Fourth International Congress of Behavioral Medicine, Washington DC: The Society of Behavioral Medicine, 1996. [Google Scholar]
- 67.Freyer J, Bott K, Riedel J, et al. Psychometric properties of the 'Processes of Change' scale for alcohol misuse and its short form (POC-20). Addict Behav 2006;31:821–32. 10.1016/j.addbeh.2005.06.007 [DOI] [PubMed] [Google Scholar]
- 68.Baumann S, Gaertner B, Schnuerer I, et al. How well do TTM measures work among a sample of individuals with unhealthy alcohol use that is characterized by low readiness to change? Psychol Addict Behav 2013;27:573–83. 10.1037/a0029368 [DOI] [PubMed] [Google Scholar]
- 69.King TK, DiClemente CC. A decisional balance measure for assessing and predicting drinking behavior. Conference of the Association for the Advancement of Behavior Therapy, Atlanta GA, 1993. [Google Scholar]
- 70.DiClemente CC, Carbonari JP, Montgomery RP, et al. The alcohol abstinence self-efficacy scale. J Stud Alcohol 1994;55:141–8. 10.15288/jsa.1994.55.141 [DOI] [PubMed] [Google Scholar]
- 71.Tönjes B, Meyer C, Ulbricht S. Skalen Zur Erfassung Der Konstrukte des Transtheorischen Modells Zur Änderung des Rauchverhaltens: Psychometrische Eigenschaften in einer Stichprobe hausärztlicher Patienten. Zeitschrift für Gesundheitspsychologie 2007;15:67–77. [Google Scholar]
- 72.Etter JF, Bergman MM, Perneger TV. On quitting smoking: development of two scales measuring the use of self-change strategies in current and former smokers (SCS-CS and SCS-FS). Addict Behav 2000;25:523–38. 10.1016/s0306-4603(00)00068-x [DOI] [PubMed] [Google Scholar]
- 73.Freyer-Adam J, Baumann S, Schnuerer I. Alcohol screening and brief intervention among General Hospital inpatients: comparative efficacy of an in-person and a computer-based intervention. 13th International Conference on treatment of addictive behaviors. Denmark: Odense, 2015. [Google Scholar]
- 74.Idler EL, Benyamini Y. Self-Rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 1997;38:21–37. [PubMed] [Google Scholar]
- 75.Berwick DM, Murphy JM, Goldman PA, et al. Performance of a five-item mental health screening test. Med Care 1991;29:169–76. 10.1097/00005650-199102000-00008 [DOI] [PubMed] [Google Scholar]
- 76.Rumpf HJ, Meyer C, Hapke U, et al. Screening for mental health: validity of the MHI-5 using DSM-IV axis I psychiatric disorders as gold standard. Psychiatry Res 2001;105:243–53. 10.1016/s0165-1781(01)00329-8 [DOI] [PubMed] [Google Scholar]
- 77.Scheidt-Nave C, Kamtsiuris P, Gößwald A, et al. German health interview and examination survey for adults (DEGS) - design, objectives and implementation of the first data collection wave. BMC Public Health 2012;12:730. 10.1186/1471-2458-12-730 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065136supp001.pdf (104.6KB, pdf)



