Abstract
It has long been observed that the development of asthma, allergic rhinitis and food allergy are frequently preceded by atopic dermatitis, a phenomenon known as the “atopic march”. Clinical, genetic and experimental studies have supported the fact that atopic dermatitis could be the initial step of the atopic march, leading to the subsequent development of other atopic diseases. This brief review will focus on the current evidence showing that epidermal barrier dysfunction and the keratinocyte-derived cytokine thymic stromal lymphopoietin play critical roles in the onset of the atopic march.
Introduction
Atopic diseases, including atopic dermatitis (known also as eczema) [1], asthma [2], allergic rhinitis and food allergy, are closely related inflammatory diseases involving different sites of the body, i.e. the skin, airways and digestive tract, with common features including the production of specific IgE to allergens (so called “atopy”) and T-helper (Th)2 inflammation. The term “atopic march” refers to the natural history of atopic manifestations, showing that atopic dermatitis precedes the development of other atopic diseases, and that the severity of atopic dermatitis appears to influence the course of respiratory allergy [3–6]. A better understanding of the mechanism of the atopic march is crucially required in order to develop strategies for the efficient prevention and treatment of atopic diseases.
Atopic dermatitis is characterised by pruritic, eczematoid skin lesions, frequently starting in early infancy and peaking in the first year of life [1, 4]. Atopic dermatitis has been recognised as a major risk factor for the development of asthma. Several longitudinal studies have reported an increased odds ratio for asthma in children with atopic dermatitis compared with children without atopic dermatitis. More than 50% of children with atopic dermatitis develop asthma and/or allergic rhinitis at a later stage (typically starting from 3 years of age) [7]. Moreover, an early onset of atopic dermatitis is associated with an increased risk of sensitisation to allergens [8], and the severity of atopic dermatitis correlates with the degree of sensitisation [9, 10]. These clinical studies have suggested that allergen sensitisation that frequently develops during atopic dermatitis could be a critical step in the onset of the atopic march [11]. This review highlights recent evidence from genetic and experimental studies suggesting that epidermal barrier dysfunction and skin-derived cytokine thymic stromal lymphopoietin (TSLP) play crucial roles in driving allergen sensitisation and the atopic march.
Epidermal barrier dysfunction and the atopic march
The epidermis functions as a primary defence and biosensor to the external environment. Defective epidermal barrier function has been recognised as a critical factor in the initiation and exacerbation of atopic dermatitis, as well as in the progression from atopic dermatitis to asthma. Epidermal barrier dysfunction could be due to multiple abnormalities in the stratum corneum barrier involving desquamation, stratum corneum structural proteins, lipid metabolism or the tight junction barrier [12, 13]. This review will focus on recent progress from human genetic studies and experimental animal models in recognising the stratum corneum barrier dysfunction, either due to genetic mutations or environmental stimuli, in developing allergen sensitisation and the atopic march.
Genetic mutations associated with epidermal barrier dysfunction and the atopic march
Human genetic studies have identified that gene mutations of several major factors in epidermal barrier function are responsible for diseases associated with atopic dermatitis and other atopy manifestations (asthma, allergic rhinitis and food allergy). These include SPINK5, CDSN and FLG.
The SPINK5 gene encodes a serine peptidase inhibitor that critically regulates the protease network controlling the desquamation process. Human genetic studies have identified loss-of-function mutations in SPINK5 (chromosome 5q32) leading to Netherton syndrome [14]. Netherton syndrome is a severe, autosomal recessive ichthyosis characterised by severe atopic dermatitis-like skin inflammation with ultrastructual analyses showing a marked increase in corneodesmosome cleavage and stratum corneum detachment, resulting in the loss of the stratum corneum barrier, which is accompanied by constant atopic manifestations. Other genetic studies have found coding polymorphisms in the SPINK5 gene in association with atopic dermatitis and asthma [15–17], food allergy [18] and serum IgE levels [19], suggesting that this barrier defect could predispose subjects to sensitisation to environmental allergens and development of the atopic march.
The CDSN gene (chromosome 6p21) codes corneodesmosin, a structural protein of cordeodesmosomes, which mediate intercorneocyte adhesion in the stratum corneum. Mutations in the CDSN gene have recently been identified for peeling skin syndrome type B [20, 21], in which the whole stratum corneum is easily detached from the underlying living layers. The patients exhibit chronic dermatitis associated with asthma, allergic rhinitis, food allergy, elevated levels of serum IgE and eosinophilia, providing further evidence that stratum corneum barrier dysfunction precedes the onset of atopic diseases.
Filaggrin is a key epidermal protein that regulates several critical functions for the structure and composition of the stratum corneum [22, 23]. Filaggrin monomers with keratin-binding activities are thought to contribute to the cell compaction observed in the lower stratum corneum and are further degraded into “natural moisturising factors”, which maintain hydration of the upper stratum corneum. Loss-of-function mutations in the FLG gene (chromosome 1q21) were initially identified as the cause of ichthyosis vulgaris [24], the most common disorder of keratinisation, and later reported to also be a major predisposing factor for atopic dermatitis [25]. Subsequent investigations have suggested that FLG-null mutations could be a risk factor for developing allergic sensitisation [26] as well as for the atopic march, as they have been reported in a subgroup of asthma in association with atopic dermatitis [27–30], allergic rhinitis [28, 31] and peanut allergy [32].
To date, evidence from these gene mutations has suggested that compromised barrier function is associated with skin inflammation and atopy. As mentioned previously, epidermal barrier dysfunction could be a result of multiple abnormalities [12, 13]; therefore, it is not surprising that more candidates have been identified (e.g. desmoglein 1 [33] and fatty acid transport protein 4 [34]), or may be found in the future, in the category of diseases sharing atopic dermatitis and atopic features. Interestingly, as gene redundancy or compensation mechanisms might exist in the skin [35, 36], one may link this with the clinical observation that some atopic dermatitis patients experience an improvement in their dermatological disease over time, although the allergic sensitisation that occurred during the atopic dermatitis period may well predispose them to other atopic diseases.
It should be noted that despite the association of the gene mutations with atopic dermatitis or atopic dermatitis-related skin disorders and other atopic features in humans, how the gene mutations are involved in generating allergen sensitisation through barrier-defective skin and in triggering the atopic march remain to be explored. To this end, mice with ablation of gene selectively in mouse skin [37, 38], combined with an experimental protocol to induce atopic march (see below), should provide useful tools for further investigation.
Experimental mouse models based on epicutaneous sensitisation through barrier-disrupted skin
Initial studies from a number of groups [39–44] have shown that epicutaneous treatment with a protein allergen (e.g. ovalbumin (OVA)) on barrier-disrupted skin elicits a local and systemic, Th2-predominant response in mice. Recently, Leyva-Castillo et al. [45] modified and established an experimental atopic march mouse model, in which sensitisation was achieved through topical application of OVA on barrier-impaired skin, followed by allergen challenge in the airway. In this model, barrier impairment via tape stripping induces the production of TSLP in keratinocytes (see below), and epicutaneous OVA treatment leads to allergic skin inflammation represented by eosinophils, basophils and CD4+ T-cell infiltration, as well as an induced Th2, but not Th1 or Th17, immune response. The OVA-treated mice developed allergen sensitisation evidenced by systemic immune responses, including the production of OVA-specific immunoglobulins (indicating an allergen-specific B-cell response), and cytokine production of splenocyte cells following in vitro OVA stimulation (indicating an allergen-specific T-cell response). Upon intranasal challenge, these epicutaneous OVA-sensitised mice exhibited an asthmatic phenotype, showing: pulmonary infiltration of cells, including eosinophils and basophils: hyperplasia of mucus-secreting goblet cells; upregulated expression of Th2 cytokines and chemokines; and enhanced airway hyperresponsiveness. Therefore, this study established and characterised an experimental atopic march mouse model for studying how allergen sensitisation through barrier-defective skin may initiate and trigger the atopic march.
Keratinocyte-produced TSLP and the atopic march
The past years have seen great progress in recognising TSLP, a type I cytokine, as a key player in the pathogenesis of atopic disorders [46]. An initial link between TSLP and atopic dermatitis was established by Soumelis et al. [47], showing that TSLP was induced in keratinocytes from the suprabasal layers of the epidermis of lesioned skin from acute and chronic atopic dermatitis patients. Although data from large cohorts are still lacking, serum TSLP levels in children with atopic dermatitis were reported to be elevated compared with healthy controls in two studies [48, 49]. Another report showed that adult atopic dermatitis patients exhibited an increase in TSLP mRNA (in skin) and protein (in serum) compared with healthy controls [50]. Moreover, patients with Netherton syndrome, who exhibit a severe atopic dermatitis-like phenotype with itchy skin, elevated serum IgE levels and sensitisation to common allergens and other atopic disorders, presented with elevated TSLP expression in the skin [51].
In vivo studies in mice have provided strong evidence that overproduction of TSLP, either due to gene ablation in skin [52], transgenic overexpression [52, 53] or induced TSLP expression in keratinocytes following MC903 skin topical treatment [54], drives the atopic dermatitis pathogenesis. Further studies proposed that TSLP is an important molecule linking atopic dermatitis to asthma. Evidence from a recent study revealed that increased expression of TSLP in skin keratinocytes, either by ablation of retinoid X receptor in adult mouse keratinocytes or MC903 skin topical treatment, triggered an aggravation of asthmatic lung inflammation when mice were concomitantly subjected to OVA intraperitoneal sensitisation and intranasal challenge [55]. Another study from Demehri et al. [56] showed that induced TSLP production in skin by ablation of keratinocytic, RBPj-aggravated, OVA-induced airway inflammation. Moreover, Zhang et al. [55] found that the increased production of TSLP in keratinocytes during only the intraperitoneal sensitisation phase was able to aggravate asthma; thus, raising the hypothesis that TSLP produced by skin keratinocytes contributes to the progression from atopic dermatitis to asthma by enhancing allergen sensitisation.
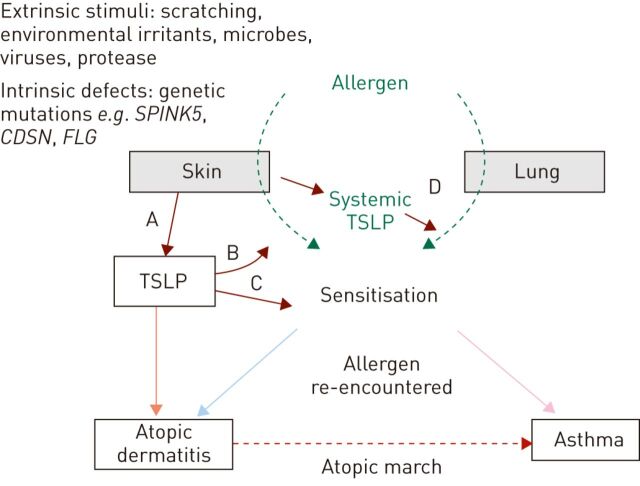
Despite these advances, the clinical relevance of the studies remains to be demonstrated. First, because atopic dermatitis driven by TSLP overexpression does not reflect the defective epidermal barrier and allergen sensitisation in human atopic dermatitis, and secondly, because the experimental allergen sensitisation-based asthma mouse model induced by intraperitoneal injection of OVA complexed with exogenous adjuvant (aluminium hydroxide) scarcely mimics the “natural” sensitisation that occurs in epithelia, such as the skin and airways [57, 58]. Most recently, the role of TSLP in atopic dermatitis, allergen sensitisation and the atopic march were extensively explored using the experimental mouse model of atopic march, providing strong evidence that skin-derived TSLP is a key trigger of the atopic march (fig. 1).
Figure 1.
Schematic representation of evidence from experimental mouse model studies showing how skin-derived cytokine thymic stromal lymphopoietin (TSLP) may contribute to the pathogenesis of atopic dermatitis, and the progression from atopic dermatitis to asthma: the so-called “atopic march”. Epicutaneous sensitisation to allergen may occur in skin that has epidermal barrier defects, due to either intrinsic genetic mutations of barrier genes (e.g. serine peptidase inhibitor, kazal type 5 (SPINK5), corneodesmosin (CDSN) and filaggrin (FLG)) and/or extrinsic stimuli. The cytokine TSLP, which is produced by skin keratinocytes (A), is crucially required for generating allergic skin inflammation and developing epicutaneous sensitisation to allergens (B). Furthermore, the overproduced TSLP, which can be induced and amplified by a variety of factors, boosts epicutaneous sensitisation (C), thereby promoting the atopic march. In addition, the skin-derived TSLP enters the circulation and can enhance the airway sensitisation to aeroallergens, such as house dust mites (D), thus aggravating the allergic asthma.
Increased keratinocytic TSLP in barrier-impaired skin
It has been shown that barrier impairment by tape stripping promotes TSLP production in the skin of mice [45, 59]. The induction of TSLP protein was demonstrated in epidermal keratinocytes [45]. In agreement with these data from mice, impairment of the stratum corneum in human skin by tape stripping or application of detergent (sodium lauryl sulfate) induced TSLP production in the epidermis [60].
Keratinocytic TSLP is essential for allergen sensitisation and for subsequent asthmatic inflammation
By subjecting the mice in which TSLP is selectively and inducibly ablated in epidermal keratinocytes [61] to the atopic march model, it has recently been demonstrated that an essential role of keratinocytic TSLP is generating skin allergic inflammation (e.g. infiltrate of CD4+ T-cells, eosinophils and basophils) and inducing allergen-induced Th2 response [45]. It is also essential for developing allergen sensitisation (shown by allergen-specific IgE and IgG1, and Th2 cytokine production by splenocytes upon allergen stimulation) and, furthermore, for triggering allergic asthma phenotypes upon airway challenge of the allergen. Thus, this study suggests that TSLP produced by keratinocytes exerts a “Th2 adjuvant” that is critical in promoting allergen sensitisation through barrier-impaired skin, eventually leading to asthma [45].
Skin TSLP levels correlate with skin sensitisation strength and asthma severity
Interestingly, by employing a mouse model in which overexpression of TSLP in keratinocytes could be induced in a dose-dependent manner, a recent study showed that skin TSLP levels were correlated with skin sensitisation strength and asthma severity, suggesting that skin TSLP could promote allergic asthma in a quantity-dependent manner [45].
Skin TSLP enhances airway sensitisation triggering the atopic march
Besides the effect of TSLP on skin sensitisation, whether TSLP produced by skin could impact airway sensitisation was also investigated. Using an experimental asthma model involving airway sensitisation and challenge to house dust mites, another study showed that, in addition to being a crucial factor in allergen sensitisation through the skin, TSLP produced by epidermal keratinocytes promoted sensitisation to aeroallergens through the airway, and triggered the development of allergic asthma [62]. Of particular interest, skin TSLP promotes sensitisation to a very low “non-asthmatic” dose of house dust mites. Given that house dust mites are the most clinically relevant aeroallergen for allergic asthma and that their levels in the environment have been correlated with the prevalence of asthma [63], this study suggests that when exposed to a common environment, individuals with atopic dermatitis showing increased skin TSLP expression may have a higher risk of developing sensitisation to inhalant common allergens through airways, thus contributing to the onset of the “atopic march”.
Conclusion
In summary, these recent studies provide new experimental proof that skin TSLP plays a critical role during the allergen sensitisation phase in the onset of the atopic march leading to allergic asthma (fig. 1). Recently, Noti et al. [64] reported that the interaction of TSLP with its receptor is necessary and sufficient for the development of experimental eosinophilic oesophagitis-like syndrome in mice. The same group also showed that skin TSLP promoted the development of intestinal food allergy in mice [65]. These data support a similar role of skin TSLP in linking atopic dermatitis to gastrointestinal tract allergy.
Despite this progress, it remains still to be explored whether serum (as well as tissue) levels of TSLP in patients with atopic dermatitis, particularly in infants with early-onset atopic dermatitis (in which sensitisation often develops at early stage), correlate with sensitisation to environmental allergens in these patients and the development of other atopy. Nevertheless, these recent studies suggest that the treatment or prevention strategy of asthma in targeting only airways may not be sufficient. Blocking TSLP production in the skin could be therapeutically helpful in preventing or limiting both skin and airway sensitisation; thus, halting the progress of the atopic march.
In conclusion, the recent advances in the pathogenesis of atopic diseases have provided further evidence that atopic dermatitis is an initial step in the “atopic march” onset leading to the subsequent development of other atopic diseases. In addition, these advances have highlighted that identification and therapy for the repair and amelioration of the epidermal barrier in infants, in combination with targeting critical cytokine mediators such as TSLP, may help to prevent or halt the atopic march.
Acknowledgments
I would like to thank the current and past current members of the laboratory for their contribution, particularly Pierre Chambon and Daniel Metzger (Institut de Génétique et de Biologie Moléculaire et Cellulaire, Illkirch, France) for their discussions and help.
Footnotes
For editorial comments see page 275.
Support statement: Funding support was received from l’Agence Nationale de la Recherche (ANR JCJC-1106-01 and ANR-13-BSV1-0024-01), Fondation Simone et Cino del Duca - Institut de France, Société Française d’Allergologie and the Association pour la Recherche à l’ Institut de Génétique et de Biologie Moléculaire et Cellulaire. Support was also received from the Centre National de la Recherche Scientifique, the Institut National de la Santé et de la Recherche Médicale (INSERM) and the Université de Strasbourg, Strasbourg, France.
Conflict of interest: None declared.
Provenance: Submitted article, peer reviewed.
References
- 1.Bieber T. Atopic dermatitis. N Engl J Med 2008; 358: 1483–1494. [DOI] [PubMed] [Google Scholar]
- 2.Ober C, Yao T-C. The genetics of asthma and allergic disease: a 21st century perspective. Immunol Rev 2011; 242: 10–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hahn EL, Bacharier LB. The atopic march: the pattern of allergic disease development in childhood. Immunol Allergy Clin North Am 2005; 25: 231–246. [DOI] [PubMed] [Google Scholar]
- 4.Leung DY, Boguniewicz M, Howell MD, et al. New insights into atopic dermatitis. J Clin Invest 2004; 113: 651–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spergel JM. From atopic dermatitis to asthma: the atopic march. Ann Allergy Asthma Immunol 2010; 105: 99–106. [DOI] [PubMed] [Google Scholar]
- 6.Spergel JM, Paller AS. Atopic dermatitis and the atopic march. J Allergy Clin Immunol 2003; 112: Suppl. 6, S118–S127. [DOI] [PubMed] [Google Scholar]
- 7.Boguniewicz M, Leung DY. Atopic dermatitis: a disease of altered skin barrier and immune dysregulation. Immunol Rev 2011; 242: 233–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gustafsson D, Sjoberg O, Foucard T. Development of allergies and asthma in infants and young children with atopic dermatitis – a prospective follow-up to 7 years of age. Allergy 2000; 55: 240–245. [DOI] [PubMed] [Google Scholar]
- 9.Schafer T, Heinrich J, Wjst M, et al. Association between severity of atopic eczema and degree of sensitization to aeroallergens in schoolchildren. J Allergy Clin Immunol 1999; 104: 1280–1284. [DOI] [PubMed] [Google Scholar]
- 10.Oettgen HC, Geha RS. IgE regulation and roles in asthma pathogenesis. J Allergy Clin Immunol 2001; 107: 429–440. [DOI] [PubMed] [Google Scholar]
- 11.Bieber T. Atopic dermatitis 2.0: from the clinical phenotype to the molecular taxonomy and stratified medicine. Allergy 2012; 67: 1475–1482. [DOI] [PubMed] [Google Scholar]
- 12.Benedetto AD, Kubo A, Beck LA. Skin barrier disruption: a requirement for allergen sensitization? J Invest Dermatol 2012; 132: 949–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kubo A, Nagao K, Amagai M. Epidermal barrier dysfunction and cutaneous sensitization in atopic diseases. J Clin Invest 2012; 122: 440–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chavanas S, Bodemer C, Rochat A, et al. Mutations in SPINK5, encoding a serine protease inhibitor, cause Netherton syndrome. Nat Genet 2000; 25: 141–142. [DOI] [PubMed] [Google Scholar]
- 15.Kato A, Fukai K, Oiso N, et al. Association of SPINK5 gene polymorphisms with atopic dermatitis in the Japanese population. Br J Dermatol 2003; 148: 665–669. [DOI] [PubMed] [Google Scholar]
- 16.Nishio Y, Noguchi E, Shibasaki M, et al. Association between polymorphisms in the SPINK5 gene and atopic dermatitis in the Japanese. Genes Immun 2003; 4: 515–517. [DOI] [PubMed] [Google Scholar]
- 17.Walley AJ, Chavanas S, Moffatt MF, et al. Gene polymorphism in Netherton and common atopic disease. Nat Genet 2001; 29: 175–148. [DOI] [PubMed] [Google Scholar]
- 18.Kusunoki T, Okafuji I, Yoshioka T, et al. SPINK5 polymorphism is associated with disease severity and food allergy in children with atopic dermatitis. J Allergy Clin Immunol 2005; 115: 636–638. [DOI] [PubMed] [Google Scholar]
- 19.Hubiche T, Ged C, Benard A, et al. Analysis of SPINK 5, KLK7 and FLG genotypes in a French atopic dermatitis cohort. Acta Derm Venereol 2007; 87: 499–505. [DOI] [PubMed] [Google Scholar]
- 20.Israeli S, Zamir H, Sarig O, et al. Inflammatory peeling skin syndrome caused by a mutation in CDSN encoding corneodesmosin. J Invest Dermatol 2011; 131: 779–781. [DOI] [PubMed] [Google Scholar]
- 21.Oji V, Eckl K-M, Aufenvenne K, et al. Loss of corneodesmosin leads to severe skin barrier defect, pruritus, and atopy: unraveling the peeling skin disease. Am J Hum Genet 2010; 87: 274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kezic S, Kemperman PM, Koster ES, et al. Loss-of-function mutations in the filaggrin gene lead to reduced level of natural moisturizing factor in the stratum corneum. J Invest Dermatol 2008; 128: 2117–2119. [DOI] [PubMed] [Google Scholar]
- 23.O’Regan GM, Sandilands A, McLean WH, et al. Filaggrin in atopic dermatitis. J Allergy Clin Immunol 2008; 122: 689–693. [DOI] [PubMed] [Google Scholar]
- 24.Smith FJD, Irvine AD, Terron-Kwiatkowski A, et al. Loss-of-function mutations in the gene encoding filaggrin cause ichthyosis vulgaris. Nat Genet 2006; 38: 337–342. [DOI] [PubMed] [Google Scholar]
- 25.Palmer CN, Irvine AD, Terron-Kwiatkowski A, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet 2006; 38: 441–446. [DOI] [PubMed] [Google Scholar]
- 26.van den Oord RA, Sheikh A. Filaggrin gene defects and risk of developing allergic sensitisation and allergic disorders: systematic review and meta-analysis. BMJ 2009; 339: b2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henderson J, Northstone K, Lee SP, et al. The burden of disease associated with filaggrin mutations: a population-based, longitudinal birth cohort study. J Allergy Clin Immunol 2008; 121: 872–877. [DOI] [PubMed] [Google Scholar]
- 28.Weidinger S, O’Sullivan M, Illig T, et al. Filaggrin mutations, atopic eczema, hay fever, and asthma in children. J Allergy Clin Immunol 2008; 121: 1203–1209. [DOI] [PubMed] [Google Scholar]
- 29.Marenholz I, Bauerfeind A, Esparza-Gordillo J, et al. The eczema risk variant on chromosome 11q13 (rs7927894) in the population-based ALSPAC cohort: a novel susceptibility factor for asthma and hay fever. Hum Mol Genet 2011; 20: 2443–2449. [DOI] [PubMed] [Google Scholar]
- 30.Brown SJ, Relton CL, Liao H, et al. Filaggrin null mutations and childhood atopic eczema: a population-based case-control study. J Allergy Clin Immunol 2008; 121: 940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schuttelaar ML, Kerkhof M, Jonkman MF, et al. Filaggrin mutations in the onset of eczema, sensitization, asthma, hay fever and the interaction with cat exposure. Allergy 2009; 64: 1758–1765. [DOI] [PubMed] [Google Scholar]
- 32.Brown SJ, Asai Y, Cordell HJ, et al. Loss-of-function variants in the filaggrin gene are a significant risk factor for peanut allergy. J Allergy Clin Immunol 2011; 127: 661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Samuelov L, Sarig O, Harmon RM, et al. Desmoglein 1 deficiency results in severe dermatitis, multiple allergies and metabolic wasting. Nat Genet 2013; 45: 1244–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klar J, Schweiger M, Zimmerman R, et al. Mutations in the fatty acid transport protein 4 gene cause the ichthyosis prematurity syndrome. Am J Hum Genet 2009; 85: 248–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sevilla LM, Nachat R, Groot KR, et al. Mice deficient in involucrin, envoplakin, and periplakin have a defective epidermal barrier. J Cell Biol 2007; 179: 1599–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Segre JA. Epidermal barrier formation and recovery in skin disorders. J Clin Invest 2006; 116: 1150–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li M, Indra AK, Warot X, et al. Skin abnormalities generated by temporally controlled RXRα mutations in mouse epidermis. Nature 2000; 407: 633–636. [DOI] [PubMed] [Google Scholar]
- 38.Metzger D, Li M, Chambon P. Targeted somatic mutagenesis in the mouse epidermis. Methods Mol Biol 2005; 289: 329–340. [DOI] [PubMed] [Google Scholar]
- 39.Herrick CA, MacLeod H, Glusac E, et al. Th2 responses induced by epicutaneous or inhalational protein exposure are differentially dependent on IL-4. J Clin Invest 2000; 105: 765–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kondo H, Ichikawa Y, Imokawa G. Percutaneous sensitization with allergens through barrier-disrupted skin elicits a Th2-dominant cytokine response. Eur J Immunol 1998; 28: 769–779. [DOI] [PubMed] [Google Scholar]
- 41.Oyoshi MK, Murphy GF, Geha RS. Filaggrin-deficient mice exhibit TH17-dominated skin inflammation and permissiveness to epicutaneous sensitization with protein antigen. J Allergy Clin Immunol 2009; 124: 485–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spergel JM, Mizoguchi E, Brewer JP, et al. Epicutaneous sensitization with protein antigen induces localized allergic dermatitis and hyperresponsiveness to methacholine after single exposure to aerosolized antigen in mice. J Clin Invest 1998; 101: 1614–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Strid J, Hourihane J, Kimber I, et al. Disruption of the stratum corneum allows potent epicutaneous immunization with protein antigens resulting in a dominant systemic Th2 response. Eur J Immunol 2004; 34: 2100–2109. [DOI] [PubMed] [Google Scholar]
- 44.Wang G, Savinko T, Wolff H, et al. Repeated epicutaneous exposures to ovalbumin progressively induce atopic dermatitis-like skin lesions in mice. Clin Exp Allergy 2007; 37: 151–161. [DOI] [PubMed] [Google Scholar]
- 45.Leyva-Castillo JM, Hener P, Jiang H, et al. TSLP produced by keratinocytes promotes allergen sensitization through skin and thereby triggers atopic march in mice. J Invest Dermatol 2013; 133: 154–163. [DOI] [PubMed] [Google Scholar]
- 46.Ziegler SF. Thymic stromal lymphopoietin and allergic disease. J Allergy Clin Immunol 2012; 130: 845–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Soumelis V, Reche PA, Kanzler H, et al. Human epithelial cells trigger dendritic cell mediated allergic inflammation by producing TSLP. Nat Immunol 2002; 3: 673–680. [DOI] [PubMed] [Google Scholar]
- 48.Lee EB, Kim KW, Hong JY, et al. Increased serum thymic stromal lymphopoietin in children with atopic dermatitis. Pediatr Allergy Immunol 2010; 21: e457–e460. [DOI] [PubMed] [Google Scholar]
- 49.Yao W, Zhang Y, Jabeen R, et al. Interleukin-9 is required for allergic airway inflammation mediated by the cytokine TSLP. Immunity 2013; 38: 360–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alysandratos KD, Angelidou A, Vasiadi M, et al. Increased affected skin gene expression and serum levels of thymic stromal lymphopoietin in atopic dermatitis. Ann Allergy Asthma Immunol 2010; 105: 403–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hovnanian A. Netherton syndrome: skin inflammation and allergy by loss of protease inhibition. Cell Tissue Res 2013; 351: 289–300. [DOI] [PubMed] [Google Scholar]
- 52.Li M, Messaddeq N, Teletin M, et al. Retinoid X receptor ablation in adult mouse keratinocytes generates an atopic dermatitis triggered by thymic stromal lymphopoietin. Proc Natl Acad Sci USA 2005; 102: 14795–14800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yoo J, Omori M, Gyarmati D, et al. Spontaneous atopic dermatitis in mice expressing an inducible thymic stromal lymphopoietin transgene specifically in the skin. J Exp Med 2005; 202: 541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li M, Hener P, Zhang Z, et al. Topical vitamin D3 and low-calcemic analogs induce thymic stromal lymphopoietin in mouse keratinocytes and trigger an atopic dermatitis. Proc Natl Acad Sci USA 2006; 103: 11736–11741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang Z, Hener P, Frossard N, et al. Thymic stromal lymphopoietin overproduced by keratinocytes in mouse skin aggravates experimental asthma. Proc Natl Acad Sci USA 2009; 106: 1536–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Demehri S, Morimoto M, Holtzman MJ, et al. Skin-derived TSLP triggers progression from epidermal-barrier defects to asthma. PLoS Biol 2009; 7: e1000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Takeda K, Gelfand EW. Mouse models of allergic diseases. Curr Opin Immunol 2009; 21: 660–665. [DOI] [PubMed] [Google Scholar]
- 58.Holgate S. Perspective: a human touch. Nature 2011; 479: S22. [Google Scholar]
- 59.Oyoshi MK, Larson RP, Ziegler SF, et al. Mechanical injury polarizes skin dendritic cells to elicit a Th2 response by inducing cutaneous thymic stromal lymphopoietin expression. J Allergy Clin Immunol 2010; 126: 976–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Angelova-Fischer I, Fernandez IM, Donnadieu M-H, et al. Injury to the stratum corneum induces in vivo expression of human thymic stromal lymphopoietin in the epidermis. J Invest Dermatol 2010; 130: 2505–2507. [DOI] [PubMed] [Google Scholar]
- 61.Li M, Hener P, Zhang Z, et al. Induction of thymic stromal lymphopoietin expression in keratinocytes is necessary for generating an atopic dermatitis upon application of the active vitamin D3 analogue MC903 on mouse skin. J Invest Dermatol 2009; 129: 498–502. [DOI] [PubMed] [Google Scholar]
- 62.Jiang H, Hener P, Li J, et al. Skin thymic stromal lymphopoietin promotes airway sensitization to inhalant house dust mites leading to allergic asthma in mice. Allergy 2012; 67: 1078–1082. [DOI] [PubMed] [Google Scholar]
- 63.Platts-Mills TA, de Weck AL. Dust mite allergens and asthma – a worldwide problem. J Allergy Clin Immunol 1989; 83: 416–427. [DOI] [PubMed] [Google Scholar]
- 64.Noti M, Wojno EDT, Kim BS, et al. Thymic stromal lymphopoietin-elicited basophil responses promote eosinophilic esophagitis. Nature Med 2013; 19: 1005–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Noti M, Kim BS, Siracusa MC, et al. Exposure to food allergens through inflamed skin promotes intestinal food allergy through the thymic stromal lymphopoietin-basophil axis. J Allergy Clin Immunol 2014; 133: 1390–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]