Abstract
Pulmonary alveolar microlithiasis (PAM) is a rare disease characterised by the widespread intra-alveolar accumulation of minute calculi called microliths. It is caused by mutation of the SLC34A2 gene encoding the type IIb sodium phosphate cotransporter in alveolar type II cells. The present study explores the epidemiological, familial, genetic, clinical, diagnostic, radiological and therapeutic aspects with the aim of contributing to a better understanding of this uncommon disease.
We searched articles on PAM published up to December 2014 and 544 papers were found, accounting for 1022 cases.
PAM is present in all continents and in many nations, in particular in Turkey, China, Japan, India, Italy and the USA. Familiality is frequent. The clinical course is not uniform and the causes of this clinical variability seem to be largely nongenetic. The optimal diagnostic procedure is the association of chest high-resolution computed tomography (HRCT) with bronchoalveolar lavage, but a chest radiograph may suffice in families in which a case has already been diagnosed. Moreover, chest radiography and HRCT allow the classification of the evolutionary phase of the disease and its severity. At present lung transplantation is the only effective therapy. However, better knowledge of the gene responsible offers hope for new therapies.
Short abstract
Familial, genetic, clinical, radiological and therapeutic aspects of pulmonary alveolar microlithiasis epidemiology http://ow.ly/St3Mw
Introduction
Pulmonary alveolar microlithiasis (PAM) (OMIM 265100) is a rare autosomal recessive disease with a high penetrance characterised by widespread intra-alveolar accumulation of innumerable minute calculi called microliths. It is caused by inactivating mutations in the gene “solute carrier family 34 member 2”, encoding a sodium-dependent phosphate cotransporter (SLC34A2, Npt2b, NaPi-2b). SLC34A2 is expressed primarily in alveolar epithelial type II cells and is responsible for the uptake of phosphate released from phospholipids in outdated surfactant. The formation of calcium phosphate microliths in PAM could be explained by the inability to clear phosphate from the alveolar space [1–3].
An Italian scientist, Malpighi, was the first to give a concise and detailed macroscopic description of the disease in 1686: “In vesciculis pulmonum innumeri lapilli sunt”. Centuries later, in 1918, the Norwegian Harbitz provided an accurate autoptic and radiological description of a second case. The third case was reported in 1932 in Germany by Schildknecht and in 1933 the disease was named PAM by the Hungarian pathologist Puhr. In 1947 Mariani et al. highlighted the first clinical, functional and radiological features in Italian patients, and in 1954 Mikhailov[4] described the first multiple cases in one family in Bulgaria. Subsequently, there were numerous reports of individual, small series and familial case histories. In 1957, the radiologist Sosman et al. [5] published the first world review of 45 cases. World cases were then extended by various authors: Perosa and Ramunni [6] described 74 cases in 1959; Mariani et al. 136 cases in 1967, 18 of which were Italian; Burguet and Reginster 107 cases in 1967, 48 familial and 59 isolated; and Susini et al. 171 cases in 1970, 25 of which were Italian. Finally, two exhaustive reviews of world case series have been published, by Castellana and Lamorgese [7], who reported 424 cases up to 2001, and by Mariotta et al. [8], who documented 576 cases up to January 2003 (further references are given in the online supplementary material).
The present study was conducted with the aim of investigating the current world epidemiology and disease characteristics of PAM, paying particular attention to the familial, genetic, clinical, diagnostic, radiological and therapeutic aspects in order to contribute to a better understanding of this rare disease.
Methods
Search strategy
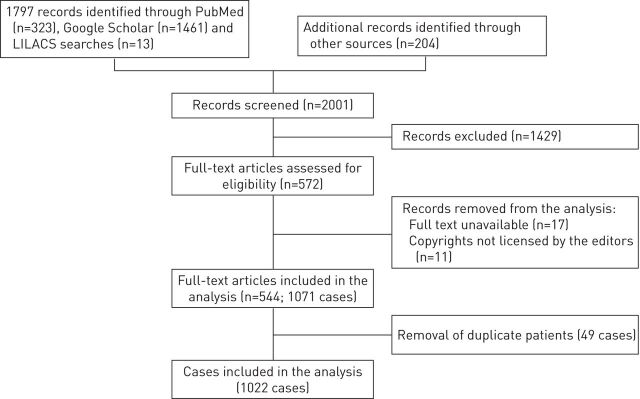
PubMed, Google Scholar and LILACS (Literatura Latino Americana em Ciências da Saúde) searches were performed in June 2014 and then updated in December 2014 including the following keywords (“pulmonary alveolar microlithiasis” [All Fields]). In addition, all references that were cited in these studies and papers published in nonindexed journals were searched, with no language restrictions. The latter articles were found in Italian libraries or were directly requested from national libraries and publishing houses. We identified 2001 papers (fig. 1).
FIGURE 1.
Flow diagram of the study.
Study selection
One team consisting of two reviewers (G. Castellana and G. Castellana) screened, independently and in duplicate, titles and abstracts of identified citations. Papers not addressing PAM in humans and duplicate papers were excluded. Citations flagged by either reviewer as potentially eligible were reviewed in full text. Articles with full text unavailable were excluded.
Data extraction and removal of duplicate patients
Two investigators (G. Castellana and G. Castellana) entered data into a database using a dedicated entry screen; for those papers published in languages other than Italian and English, the help of a native language translator was requested. The following data were extracted from each study: nationality, sex, age at diagnosis, family traits, genetic analysis, symptoms, clinical course, duration of the disease, comorbidities, diagnostic procedures, radiological findings, extrapulmonary calcifications, misdiagnosis of tuberculosis and unsuccessful antitubercular therapy, and therapeutic approach for PAM. Cases with nationality missing were classified under the country of the main author's affiliation. Duplicate patients were identified on the basis of the author's declaration and/or analysing the available information. Discrepancies were solved by discussion.
Statistical analysis
All data were analysed using Excel 2010 (Microsoft, Redmond, WA, USA).
Results and discussion
World cases
For this literature review, a total of 544 publications were read in the original language. Up to 1960, 110 cases were described, 299 by 1970, 389 by 1980, 541 by 1990 and 669 by 2000. Up to December 2014 a total of 1022 PAM cases were described in the literature in 65 nations. The nationality of origin was reported in all cases, the sex in 934, the age at diagnosis in 904 and negative family history in 641. 66 cases were not documented individually but were cited by the authors in national case series [9, 10].
PAM is present in all continents, but not uniformly, the majority of cases being in Asia (576 cases; 56.3%) and in Europe (285 cases; 27.8%). The nation with the highest number of recorded cases is Turkey (139 cases; 13.6%), followed by China (133 cases; 13.0%), Japan (119 cases; 11.6%), India (80 cases; 7.8%), Italy (65 cases; 6.3%) and the USA (50 cases; 4.9%) (table 1). Turkey, China, Japan, India and Italy account for 52.4% of the world cases. The ratio between the number of cases reported by December 2014 per million of population is 1.85 for Turkey, 1.08 for Italy, 0.92 for Japan, 0.15 for USA, 0.10 for China and 0.06 for India. Two particular local clusters were found: one in the South of Bari (Italy) with 14 cases reported [11], and a smaller one in the village of Diyarbakir (Turkey) consisting of eight patients, five of whom were detected during microfilm screening of 279 residents [12].
TABLE 1.
World cases of pulmonary alveolar microlithiasis subdivided by continent, nation of birth and sex
| Continent | Nation of birth | Total | Male | Female | Sex not specified |
| Africa | Morocco | 14 | 6 | 8 | 0 |
| Algeria | 7 | 0 | 1 | 6 | |
| Egypt | 5 | 4 | 1 | 0 | |
| Libya | 4 | 4 | 0 | 0 | |
| Tunisia | 3 | 3 | 0 | 0 | |
| Nigeria | 3 | 1 | 2 | 0 | |
| South Africa | 1 | 1 | 0 | 0 | |
| Tanzania | 1 | 1 | 0 | 0 | |
| Total | 38 | 20 | 12 | 6 | |
| Asia | Turkey | 139 | 92 | 46 | 1 |
| China | 133 | 78 | 55 | 0 | |
| Japan | 119 | 27 | 34 | 58 | |
| India | 80 | 43 | 36 | 1 | |
| Iran | 26 | 12 | 5 | 9 | |
| Thailand | 15 | 10 | 5 | 0 | |
| Iraq | 10 | 8 | 2 | 0 | |
| Lebanon | 9 | 6 | 3 | 0 | |
| Saudi Arabia | 9 | 5 | 4 | 0 | |
| Kuwait | 8 | 6 | 2 | 0 | |
| Pakistan | 8 | 6 | 2 | 0 | |
| Israel | 4 | 2 | 2 | 0 | |
| Sri Lanka | 4 | 2 | 2 | 0 | |
| Jordan | 3 | 2 | 1 | 0 | |
| Bangladesh | 2 | 0 | 2 | 0 | |
| Malaysia | 2 | 1 | 1 | 0 | |
| Armenia | 1 | 1 | 0 | 0 | |
| Nepal | 1 | 1 | 0 | 0 | |
| Singapore | 1 | 1 | 0 | 0 | |
| South Korea | 1 | 1 | 0 | 0 | |
| United Arab Emirates | 1 | 1 | 0 | 0 | |
| Total | 576 | 305 | 202 | 69 | |
| North America | USA | 50 | 24 | 26 | 0 |
| Mexico | 13 | 6 | 7 | 0 | |
| Canada | 1 | 0 | 1 | 0 | |
| Total | 64 | 30 | 34 | 0 | |
| Central America | Cuba | 1 | 1 | 0 | 0 |
| Honduras | 2 | 2 | 0 | 0 | |
| Guatemala | 1 | 0 | 1 | 0 | |
| Jamaica | 1 | 1 | 0 | 0 | |
| Total | 5 | 4 | 1 | 0 | |
| South America | Brazil | 19 | 8 | 11 | 0 |
| Peru | 10 | 4 | 6 | 0 | |
| Venezuela | 9 | 6 | 3 | 0 | |
| Columbia | 5 | 1 | 4 | 0 | |
| Argentina | 4 | 3 | 1 | 0 | |
| Uruguay | 2 | 0 | 2 | 0 | |
| Bolivia | 1 | 1 | 0 | 0 | |
| Total | 50 | 23 | 27 | 0 | |
| Europe | Italy | 65 | 26 | 39 | 0 |
| Spain | 38 | 12 | 25 | 1 | |
| Germany | 30 | 20 | 10 | 0 | |
| France | 29 | 11 | 18 | 0 | |
| Russia | 21 | 4 | 12 | 5 | |
| UK | 21 | 14 | 7 | 0 | |
| Bulgaria | 17 | 11 | 6 | 0 | |
| Ex-Yugoslavia | 12 | 4 | 7 | 1 | |
| Greece | 9 | 3 | 6 | 0 | |
| Hungary | 8 | 3 | 2 | 3 | |
| Switzerland | 7 | 6 | 1 | 0 | |
| Belgium | 6 | 3 | 3 | 0 | |
| Poland | 5 | 1 | 2 | 2 | |
| Finland | 4 | 3 | 1 | 0 | |
| Austria | 4 | 2 | 2 | 0 | |
| Czechoslovakia | 2 | 1 | 1 | 0 | |
| Denmark | 2 | 2 | 0 | 0 | |
| Norway | 2 | 1 | 1 | 0 | |
| Romania | 2 | 0 | 1 | 1 | |
| Ireland | 1 | 1 | 0 | 0 | |
| Total | 285 | 128 | 144 | 13 | |
| Oceania | New Zealand | 3 | 2 | 1 | 0 |
| Australia | 1 | 1 | 0 | 0 | |
| Total | 4 | 3 | 1 | 0 |
Data are presented as n. Cases with missing nationality were classified under the country of origin of the main author's affiliation.
The disease affects both sexes, with a slight predominance among males worldwide: 513 males (50.2%) and 421 females (41.2%) were identified, while in the remaining 88 cases (8.6%) the sex was not specified. A larger male predominance was found in Turkey, China and India, where 66.7%, 58.6% and 54.4% of cases were male, respectively. By contrast, among Italian, Spanish and French cases a female predominance was reported (table 1).
Although cases of PAM are described at all ages, the second and third decade were found to be more frequently involved, showing a progressive decline thereafter and very few cases in the elderly. The youngest reported cases were premature monochorionic twins, who died after 12 h of life [13], two newborns [14], an 8-month-old infant [15] and an 18-month-old infant [16]. The most elderly cases at diagnosis were an 84-year-old female [17], an 82-year-old female [18] and an 80-year-old male [19]. Sex appears to be equally distributed in all age groups, except the one ranging between 11 and 30 years, which shows a prevalence of the male sex (male:female ratio 3:2) (online supplementary fig. E1).
In relation to familiality, 641 out of 1022 cases were classified as sporadic (62.7%); among these, the sex was reported in 591 cases, of which 341 were male (57.7%) and 250 female (42.3%). The higher male incidence in sporadic cases could probably be ascribed to more frequent radiographic examinations performed in males for civic (military service) and/or health purposes (a higher frequency of diseases with respiratory involvement).
Finally, two pairs of monozygotic twins were diagnosed as adults [20, 21].
Familiality
Since 1957, several authors have pointed out the trend to a familial occurrence of PAM, with a frequency ranging between 32% and 61% [5]. It should be underlined that the larger frequencies of familial cases have been reported only in smaller reviews. Moreover, before the identification of the gene, two historical reports supporting the hereditary hypothesis were published, describing two large family groups with affected relatives in several generations, one in Italy [22], and the other in Turkey [23]. Owing to this presence of familial cases, PAM has been classified as a genetic disease.
In our review, a family history was present in 381 of 1022 patients (37.2%), belonging to 163 families; 182 were male and 161 female, while for 38 cases the sex was not specified. The most numerous groups were two families with six affected relatives [6, 23], followed by two families with five patients [6, 24] and five families with four cases [5, 16, 25–27]. In accordance with the autosomal recessive inheritance, in almost all familial cases transmission was horizontal (online supplementary table E1). When vertical transmission was reported, consanguinity was always present: in 36 out of 163 families the parents were first cousins and in six of these families vertical transmission occurred [4, 22, 23, 28–30]. First cousins are third-degree relatives, sharing 1/8 of their genes and with a 1/16 chance of homozygosity by descent. It should be noted that in two cases the parents were first cousins, with a generation leap [22, 29]. The female sex seems to be predominant in familial cases: when three or more horizontal siblings were affected, they were usually females. Other than chance, it is difficult to explain these data (see other references in the online supplementary material).
Genetic characteristics
As stated earlier, the heterogeneous geographical distribution and the familial occurrence of PAM disease clearly suggests a genetic aetiology, with a pattern of autosomal recessive inheritance.
In 2006 a PAM locus was first mapped at 4p15 and then, by a candidate-gene approach, SLC34A2 was identified as the gene responsible for the disease [1]. The SLC34A2 gene consists of 13 exons, the first of which is noncoding, and the remaining exons code for a 690-amino acid protein, a type 2 phosphate transporter, expressed in several human tissues of epithelial origin. SLC34A2 mutations causes a defective sodium phosphate-IIb transporter protein, and consequently, alveolar epithelial type II cells are no longer able to clear phosphorus ions, and calcium phosphate deposits (microliths) form in the extracellular fluid [31].
Corut et al. [1] first identified six homozygous mutations in the SLC34A2 gene in six out of six unrelated patients and one family affected by PAM. Since 2006 to date, 18 patients and five families affected by PAM have been analysed, and 16 different mutations reported in the literature (table 2) [1, 2, 26, 27, 32–38].
TABLE 2.
SLC34A2 mutations described in pulmonary alveolar microlithiasis patients and literature references
| Location | Mutation | Protein | First author, year [ref.] | Patient number in the paper |
| Promoter exon 1 | c.[-6773_-6588del] | Not synthesised | Corut, 2006 [1] | 1 |
| Exon 2 | insT (not specified) | Truncation | Dogan, 2010 [34] | 1 |
| Exon 2–6 | 5.5 Kb deletion | Truncation | Hishihara, 2008 [33] | 1 |
| Exon 3 | c.114delA | Truncation | Corut, 2006 [1] | 3, 5 |
| Exon 3 | c.226C→T | Truncation | Corut, 2006 [1] | 7 |
| Exon 4 | c.316G→C (p. G106R) | Substitution | Corut, 2006 [1] Özbudak, 2012 [36] | 6 1 |
| Exon 6 | c.575C>A (p.T192K) | Substitution | Ma, 2014 [26] | 1–3 |
| Exon 7 | insdel857-871 | Truncation | Huqun, 2007 [2] | 3, 5 |
| Exon 8 | C.910A>T | Truncation | Zhong, 2009 [32] Yin, 2013 [37] Wang, 2014 [27] | 1 1–4 1 |
| Exon 8 | IVS8+1G>A | Truncation by splicing failure | Huqun, 2007 [2] | 1, 2, 4, 6 |
| Exon 11 | c.1328delT | Truncation | Corut, 2006 [1] | 2 |
| Exon 12 | c.1342delG | Truncation | Corut, 2006 [1] | 4 |
| Exon 12 | c.1363T>C (p. Y455H) | Substitution | Wang, 2014 [27] | 1 |
| Exon 12 | c.1393-1404delACC | Aberrant (threonine deletion) | Jönsson, 2012 [35] | 1 |
| Exon 12 | c.1402-1404delACC | Aberrant (threonine deletion) | Jönsson, 2012 [35] | 2 |
| Exon 12 | c.1456C>T | Truncation | Proesmans, 2012 [38] | 1 |
Despite the paucity of PAM patients with a molecular characterisation, some conclusions can be drawn. Firstly, SLC34A2 seems to be the only gene involved, with full penetrance in all families analysed. The detection rate of SLC34A2 molecular analysis is very high: mutations have been identified in almost all patients tested. The only exceptions are the cases reported by Yang et al. [39], and Olauson et al. [40]. As regards the PAM patient reported by Yang et al. it should be noted that, even if a SLC34A2 mutation was not identified, the authors were able to demonstrate aberrant SLC34A2 gene expression in alveolar cells [39]. The clinical features of the case described by Olauson et al. were very unusual, as clearly discussed by the authors, indicating the possible contribution of other genetic factors [40].
With the exception of the patient reported by Wang et al. [27], the mutations were always in a homozygous state, highlighting the rarity of PAM. Huqun et al. [2] calculated that the frequency of a mutant allele in the general population is <0.008. Regarding mutations, exon 8 and exon 12 are more commonly involved. In particular the c. 910A>T exon 8 mutation seems to be common and might be the screening target for Chinese patients [27, 32, 37]. Apart from these cases, no other recurrent mutations have been identified, indicating that the high prevalence of PAM disease in some populations (e.g. Turks and Italians) is not attributable to a founder effect, but, more consistently, to identity by descent in the presence of a high proportion of consanguineous marriages.
Most of the mutations result in loss of function or premature termination, with a possible decreased activity of the protein (exon 12). The only exceptions are the mutations in exon 12 identified in two unrelated Danish patients by Jönsson et al. [35] and in one patient described by Wang et al. [27], and the homozygous mutation in exon 6 reported by Ma et al. [26]. In the Danish cases, the authors hypothesised that mutations resulted in the deletion of one of the four sequential threonine codons, altering protein structure and, presumably, function [35]. In the case described by Wang et al. [27], computational prediction of three-dimensional structures of the mutants revealed that the c.1363T>C (p. Y455H) mutation resulted in the formation of irregular coils in the transmembrane domain. Finally, the exon 6 mutation reported by Ma et al. [26] was considered the pathological factor on the basis of phenotype–genotype cosegregation in the family.
It has been noted that, even if microliths appear early, lung deterioration progresses at different speeds in PAM patients. As suggested by several authors, the cause for an early onset and/or a worse disease course could probably be found in environmental factors (i.e. smoking, inflammation and cold temperature) accelerating the turnover of the alveolar epithelial cells [26, 35]. Therefore, even if more cases are needed to reach a final conclusion, we may affirm that the data in the literature do not support any genotype–phenotype correlation, the disease variability being almost exclusively linked to nongenetic factors.
Clinical presentation and course
Most of the cases described in the literature were presented as case reports, illustrated to highlight some peculiarities of the disease. Serial monitoring from diagnosis over the years was rarely reported: 20 and 15 patients were followed-up for 10–19 and 20–29 years, respectively; 17 patients were followed-up for 30 years or more.
In six cases, it was possible to establish the date of onset of the disease, thanks to the availability of previous chest radiographs showing an entirely normal picture; in particular, in two cases the chest radiograph had been taken only 2 years previously. This suggests that the disease can be acquired during life.
The clinical traits are heterogeneous, ranging from totally asymptomatic to respiratory failure. No significant differences were found, compared to previous reviews [8].
Nevertheless, it is worth highlighting the fact that finger clubbing was observed in 72 patients in the advanced stages of the disease, as expected for chronic lung diseases, and PAM was complicated by pneumothorax in 16 cases.
As regards the clinical course, in few patients did the disease remain stationary in terms of both symptoms and of the radiological and functional findings, while in the majority it progressed at different speeds, leading to cor pulmonale and respiratory failure (online supplementary table E2). The longest living clinical case, with an absolutely stationary clinical, functional and radiographic picture, is still alive, 58 years after the diagnosis [41]. By contrast, the case of Biressi and Casassa [42] was particularly interesting in view of the rapid onset and evolution: the patient had a normal chest radiograph at a medical visit prior to employment at a factory, but only 11 months later, during which he had been symptom-free at work, a periodic visit demonstrated the picture of PAM. The patient was followed-up for 7 years, during which his symptoms gradually worsened and he finally died (see other references in the online supplementary material).
Comorbidities
The main comorbidity was tuberculosis, which was found to be concomitant in five cases. It could be explained by the epidemiology of this infectious disease, which affects more than a third of the world population. Other reported associated diseases include milk alkali syndrome, pericardial cyst, lymphocytic interstitial pneumonitis, diaphyseal aclasia, autosomal recessive Waardenburg-anophthalmia syndrome, hypertrophic pulmonary osteoarthropathy, pectus excavatum, rheumatoid arthritis, psoriasis, osteopetrosis, non-Hodgkin lymphoma, antiphospholipid syndrome and discoid lupus after Varicella zoster infection and Sjögren's syndrome.
One case of PAM was described in a renal transplant recipient and six cases in females during pregnancy (see additional references in the online supplementary material).
Microliths and calcifications in extrapulmonary sites
The SLC34A2 gene is also expressed in the mammary glands, small intestine, kidneys, pancreas, ovaries, liver, testes, placenta and prostate [3]; this can explain the systemic phenotype described in the patients reported below.
In six cases, minute calcifications like pulmonary microliths were seen in the male genital apparatus. Coetzee [43] described a 24-year-old male referred to the hospital for recurrent attacks of acute abdominal pain with no satisfactory explanation: PAM with extrapulmonary microliths in the testicles were revealed by computed tomography and in sympathetic ganglia by laparotomy. Sandhyamani et al. [44] reported a 27-year-old male with PAM referred to the hospital for infertility: bilateral testicular atrophy correlated with the microliths present in the seminal vesicles was found. Arslan et al. [45] described a 26-year-old male with PAM complaining of haematuria, in whom multiple microliths were found in the seminal vesicles, as documented by ultrasound scan and computed tomography. Qublan et al. [46] reported a 30-year-old male with PAM, testicular microlithiasis and azoospermia, revealed by ultrasonography and by semen analyses, respectively. Kanat et al. [47] reported a 37-year-old male with PAM and microliths in the head of the epididymides and in the periurethral tissue, causing obstructive azoospermia. Finally, Castellana et al. [48] described a 32-year-old male with recurrent haematuria caused by microliths in the seminal vesicles associated with PAM. Moreover, Chatterji et al. [49] described a 40-year-old male with PAM and associated azoospermia, but no imaging was performed on the genital apparatus.
This peculiar observation warrants further investigation and suggests that in all male cases of PAM close attention should also be paid to the genital tract. Microlithiasis of the male genital apparatus could be another clinical phenotype of PAM and a possible cause of male infertility [49]. Moreover, PAM should be included in the list of chronic pulmonary diseases associated with sterility, such as immotile cilia syndrome and cystic fibrosis.
Gross calcifications, unlike microliths, have been described in organs other than the lungs: medullary nephrocalcinosis, pericardial calcification, gallstones, kidney stones and prostatic calcification (see other references in the online supplementary material).
Diagnostic procedures
Diagnostic procedures can be classified into two main groups: imaging and anatomopathological. The former include chest radiography, chest computed tomography and high-resolution computed tomography (HRCT); the latter, listed in increasing order of invasiveness, bronchoalveolar lavage (BAL), transbronchial biopsy, open lung biopsy and autopsy.
The first cases of PAM were reported in the 1950s and 1960s in patients with respiratory failure; they were most often diagnosed by autopsy. The most complete description was provided by Pollice and Pirrelli [50]; another notable case was the autopsy described by Terada [51] featuring a marked reduction of the pulmonary artery vascular bed. The maximum lung weight was 4880 g [52], followed by 4500 and 4400 g; normal weight being ∼1300 g.
Later, PAM was frequently described incidentally in subjects undergoing chest radiography for other reasons: a preliminary check-up for military service or for employment; in employment monitoring; to exclude tuberculosis; or as work-up for other organ disease.
As expected, according to the introduction of new technologies, we found two different periods for the diagnosis of PAM. Before 1980, in 252 out of 398 cases (63.3%), chest radiography alone was sufficient, while in 92 (23.1%) and 54 (13.6%) cases, open lung biopsy and autopsy were required, respectively. After 1980, 192 out of 624 cases (30.7%) were diagnosed by chest radiography alone, while the remaining patients required computed tomography or HRCT (n=78; 12.5%), BAL and/or transbronchial biopsy (n=175; 28.0%), open lung biopsy (n=159; 25.4%) or autopsy (n=20; 3.2%).
BAL and biopsy show the characteristic calciospherocitis (microliths) in the alveoli
Histologically, the microliths are periodic acid–Schiff-positive and consist of calcareous concentric lamellae around a central nucleus with an amorphous or granular aspect. This appearance is distinct from those of metastatic and dystrophic calcifications, which are located in the interstitial or vascular compartments [3].
The microliths usually range from 50 to 1000 μm in diameter, although microliths up to 5000 μm in size have been reported, and are mainly composed of calcium and phosphorus (phosphorus:calcium ratio of 1:2), with varying amounts of iron, magnesium, potassium and copper [3].
Biopsy also shows variable degrees of fibrosis in the lung interstitium
To date, the best diagnostic schedule for PAM is the association of BAL and chest HRCT, as the former investigation can document the diagnosis while the latter provides further information about the degree of inflammation and/or fibrosis or calcification of the interstitium. This association makes it possible to avoid performing transbronchial and open lung biopsy, burdened by higher complication rates [11]. Identification of the SLC34A2 gene mutation could clinch the diagnosis.
Radiological aspects
PAM has been amply described as regards imaging. With the advent of computed tomography and HRCT, it became possible to study these aspects in greater detail [53, 54]. The variable radiological aspects (chest radiographs and chest HRCTs) of the disease and its evolution in individual cases have enabled a radiological classification of different degrees of severity to be drawn up and subdivided into four evolutionary phases [55].
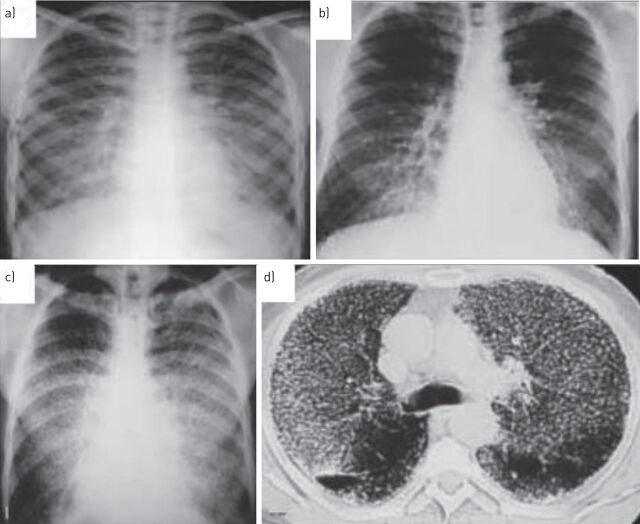
The first phase, known as precalcific, delineates the early disease stage. The radiological pattern is not yet typical due to the small number and lesser calcification of the microliths (fig. 2a). Such radiographic findings have only ever been reported by three authors. This PAM model may not be recognised, because it is occasionally observed in asymptomatic children.
FIGURE 2.
Evolutionary radiological phases of pulmonary alveolar microlithiasis. a) Chest radiograph of the first, “precalcific” phase: diffuse noncalcific micronodules. b) Chest radiograph of the second phase: diffuse, scattered, calcific micronodules with a greater concentration in the medial and inferior regions, the outlines of the heart and diaphragm are still clearly visible. c) Chest radiograph of the second phase (variant): micronodules show a larger diameter (∼2–4 mm), uniformly distributed. d) High-resolution computed tomography scan of fig. 2c: diffuse endoalveolar micronodules with thickening of the interstitial picture.
The second phase already shows the typical radiological picture: the lungs appear “sandy”, featuring diffuse, scattered calcific micronodules with a diameter of <1 mm (fig. 2b). The microliths are typically clearly outlined and bright, with a uniform size and distribution throughout the lungs, although there tends to be a greater concentration in the medial and inferior regions. The overall appearance resembles that of sandpaper, but the outlines of the heart and diaphragm are still clearly visible. In some cases, the single micronodules show a larger diameter, ∼2–4 mm, and resemble berries rather than a fine sandstorm (fig. 2c, d). This second calcification model is generally present in cases discovered in childhood or adolescence.
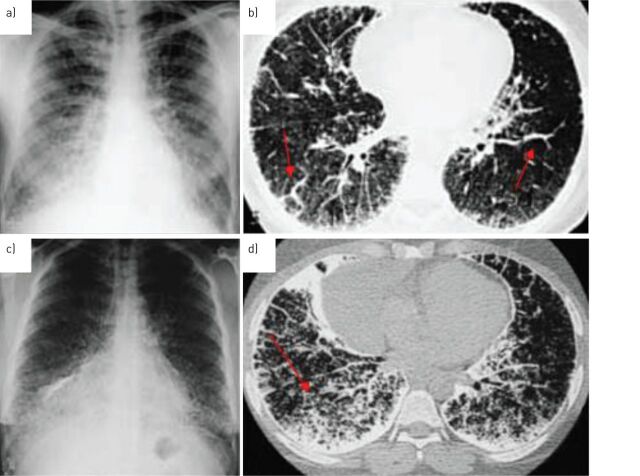
In the third phase the number and volume of the opacifications increase. The picture becomes more granular, nodular and confused due to the initial thickening of the interstitial weave, which partly masks the micronodules. In the medial and inferior fields, superimposition of the opacifications hides the outlines of the heart and diaphragm (fig. 3a, b). This third radiological model is more often seen in young adults.
FIGURE 3.
Evolutionary radiological phases of pulmonary alveolar microlithiasis. a) Chest radiograph of the third phase: extremely dense, uniform distribution of radio-opaque bright punctiform elements, with sandstorm appearance. It is not possible to distinguish heart and diaphragm borders in the medial and inferior fields. b) Chest high-resolution computed tomography (HRCT) scan of the third phase: initial calcification of the pleural lining and interlobular septa (arrows), which partly masks the micronodules. c) Chest radiograph of the fourth phase: diffuse microliths with some calcific agglomerates. d) HRCT of the fourth phase: microliths are increased in number, forming calcific agglomerates in some areas, together with intense involvement of the pleural lining and interlobular septa.
By the fourth phase, the number and size of the calcific deposits have grown even more, and there is intense calcification of the interstitium and sometimes the pleural serosa, which makes the lungs appear almost entirely opaque. They thus have the overall aspect of “white lungs” due to the diffuse presence of calcification, although the apical regions may be partially spared, as reported by other authors (fig. 3c, d). In this phase, apart from interstitial calcific fibrosis, there may be paraseptal emphysema, large bubbles or air cysts in the upper lobes, as well as pneumothorax and areas of ossification. This fourth radiological model is generally seen in older adults, or in any case in advanced cases.
A “crazy paving” pattern on chest HRCT with calcifications along the interlobular septa may be considered diagnostic, even pathognomonic, of the third and the fourth phases of PAM [56]. The extent and severity of PAM generally depend on the patient's age and the speed of progression of the disease (see other references in the online supplementary material).
Differential diagnosis
The radiographic picture of PAM is highly characteristic and thus constitutes an extremely important diagnostic element. Superficial assessment of the radiological findings in patients with PAM can cause confusion with other diseases associated with miliary dissemination such as tuberculosis, mycosis, sarcoidosis, haemosiderosis, pneumoconiosis and amyloidosis, which can all present with diffuse opacifications, although the symptoms are more severe in these diseases. Moreover, due to the intense calcifications present in PAM, X-ray exposure needs to be three to five times stronger in order to obtain good radiographs demonstrating the typical picture of the disease. In short, the aphorism of the radiologist, Sosman, that “we see only what we look for; we recognise only what we know” holds good for PAM, too.
As already described, PAM seems to occur more frequently in countries where tuberculosis is common, such as Turkey, China and India. Physicians understandably tend to suspect tuberculosis more readily, due to the lack of knowledge of PAM and the similar imaging features, despite different clinical manifestations. In ≥72 cases, PAM was wrongly diagnosed as miliary tuberculosis and useless therapy was administered (see other references in the online supplementary material).
In contrast, PAM can also be a cause of misdiagnosis: Weinstein et al. [57] reported a case with diffuse micronodular calcification, later found to be sarcoidosis.
Therapy and lung transplantation
Currently, there is no medical or gene therapy capable of reducing disease progression. Systemic corticosteroids, calcium-chelating agents and serial bronchopulmonary lavage have been shown to be ineffective and are used as palliative treatments [37, 58, 59]. The use of diphosphonates has also been proposed to reduce calcium phosphate precipitation in PAM. However, this therapy remains controversial given the limited number of reports in the literature [38, 39, 60–62].
In 1988, the Toronto Lung Transplantation Group reported a successful double lung transplantation in humans. The first bilateral lung transplant in a patient with PAM was described in 1992 in France [63], followed by a second one in 1993 in Germany [64] and two others in 1997 in the USA [65]. Single transplants were reported in 1996 in Saudi Arabia [66], in 2001 in Canada [67], in 2009 in Iran [68] and in 2014 in Italy [69]. Four other bilateral transplants were performed in France in 2009 [70], in Brazil in 2010 [71], in the USA in 2010 [72] and 2011 [73] and five in Vienna between 1989 and 2013 (one of these was also published by Güçyetmez et al. [74, 75]). The longest-living trasplanted patient is a 63-year-old female [72]. The longest survival for PAM treated by transplantation is 15 years without recurrence (table 3) [67].
TABLE 3.
Lung transplantation in 17 cases of pulmonary alveolar microlithiasis
| First author, year [ref.] | Nation | Sex | Age years | Transplant type | Survival and follow-up |
| Bonnette, 1992 [63] | France | F | 46 | Bilateral | Followed-up for 20 months, died of bronchiolitis obliterans |
| Stamatis, 1993 [64] | Germany | M | 32 | Bilateral | Followed-up for 18 months |
| Raffa, 1996 [66] | Saudi Arabia | F | 48 | Single | Followed-up for 12 months |
| Edelman, 1997 [65] | USA | M | 56 | Bilateral | Died postoperatively because of multi-organ failure |
| Edelman, 1997 [65] | USA | F | 35 | Bilateral | Followed-up for 5 years, died of bronchiolitis obliterans |
| Jackson, 2001 [67] | Canada | F | 53 | Single | Followed-up for 15 years |
| Shadmehr, 2009 [68] | Iran | M | 32 | Single | Died postoperatively from haemodynamic instability |
| Coulibaly, 2009 [70] | France | F | 49 | Bilateral | Died after 3 months from sepsis |
| Shigemura, 2010 [72] | USA | F | 63 | Bilateral | Followed-up for 16 months |
| Samano et al. 2010 [71] | Brazil | M | 47 | Bilateral | Followed-up for 12 months |
| Siddiqui, 2011 [73] | USA | M | 48 | Bilateral | No information |
| Klikovits, 2013 [74] | Austria | 3F 1M | 46# | Bilateral | 1 died postoperatively from sepsis |
| Güçyetmez, 2014 [75] | Turkey (surgery performed in Vienna, Austria) | F | 52 | Bilateral | Followed-up for 12 months |
| Borrelli, 2014 [69] | Italy | F | 64 | Single | Followed-up for 5 years |
Data are presented as n, unless otherwise stated. F: female; M: male. #: mean value.
Based on these experiences, lung transplantation remains the only possible treatment for end-stage disease. Nonetheless, guidelines for the decision as to when transplantation should be undertaken are not available due to the lack of well-defined prognostic indices and the insidious nature of PAM [65]. When either right heart failure or severe respiratory failure requiring oxygen are present, transplantation should be considered. In order to maximise the chances of a successful outcome, patients should be referred before the development of severe right ventricular dysfunction.
Bilateral lung replacement is preferred to the unilateral, because the replacement of only one lung might result in persistent shunting of blood through the native lung, filling of the alveolar spaces and the consequent creation of large areas of intrapulmonary shunt [63]. However, two patients underwent single lung transplantation with acceptable results, and thus far have shown no evidence of recurrence in the transplanted lung [64, 67]. Furthermore, even after bilateral transplantation it is not known whether PAM can recur. To date, no recurrence after transplantation has been reported, confirming that PAM is caused by a local alteration in the alveolar metabolism. Finally, the normalisation of the right ventricular ejection fraction and the regression of right ventricular hypertrophy strongly suggest that surgery can be an effective treatment option for end-stage PAM patients [71].
Strengths and limits of the review
We identified 544 articles corresponding to 1022 cases. The main strength of our review is the systematic search of references and non-peer-reviewed journals which allowed us to find 204 of the 544 papers not indexed in PubMed, Google Scholar and LILACS. We also searched for duplicates, using available information even for those papers without a specific declaration by the author/s.
Our review has several limitations. PAM is a rare disease and defining the real number of world cases is diffcult. Two main elements contribute to this problem: differential diagnosis with other common diseases (in particular tuberculosis) means that cases could have been missed; and missing a local journal report, in view of the significant number of papers in languages other than English. Moreover, 28 articles were requested from national libraries but could not be analysed due to the unavailability of the article or copyrights not licensed by the editor.
Conclusion
The characterisation of PAM remains challenging because of its rarity worldwide. The present study aimed to contribute to the current knowledge of this disease.
The important goal of the discovery of the implicated gene and underlying disease mechanism has now been attained: PAM is a rare genetic lung disease with an autosomal recessive trait caused by mutations of the SLC34A2 gene. From an epidemiological point of view, Turkey, China, Japan, India, Italy and USA are the nations with the largest case series. A familial occurrence is very frequent among PAM patients and consanguinity of their unaffected parents is common. The clinical course is not uniform and may be rapid or slow; the reasons for this variability are not yet known. Involvement of the male genital apparatus may be more common than is currently known, and a further contribution to the knowledge of PAM may derive from future systematic investigations of the genital tract in males with PAM and, vice versa, from lung investigations in infertile males.
The best diagnostic work-up consists of chest radiography followed by the combination of chest HRCT with BAL, but a chest radiography may suffice in family members of a patient already diagnosed with PAM. Moreover, chest radiography and HRCT make it possible to classify the evolutionary stage of the disease and its severity. Genetic counselling of families of individuals affected by PAM could be important to gain a better knowledge, but available data do not support genotype–phenotype correlation.
PAM is an “orphan” disease and lung transplantation is currently the only effective therapy. However, since the demonstration of the gene responsible for PAM, it is hoped that in the future new therapies may become available, that can reduce the phosphate ions in the alveolar spaces and so arrest or delay the formation of microliths and the progression to interstitial disease. Future evaluations are needed to investigate patient survival rates and the risk of PAM recurrence after lung transplantation.
Supplementary Material
Acknowledgements
We thank Myroslava Ovachuc (G.D’Annunzio University of Chieti, Chieti, Italy), for translation of the papers published in Russian, and Mary Victoria Pragnell (Aldo Moro University of Bari, Bari, Italy), for revision of the language editing. We also thank Marco Castellana (Aldo Moro University of Bari) for his contribution to the study design and the critical revision of the manuscript.
Footnotes
This article has supplementary material available from err.ersjournals.com
Conflict of interest: None declared.
Provenance: Submitted article, peer reviewed.
References
- 1.Corut A, Senyiğit A, Ugur SA, et al. Mutations in SLC34A2 cause pulmonary alveolar microlithiasis and are possibly associated with testicular microlithiasis. Am J Hum Genet 2006; 79: 650–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huqun, Izumi S, Miyazawa H, et al. Mutations in the SLC34A2 gene are associated with pulmonary alveolar microlithiasis. Am J Respir Crit Care Med 2007; 175: 263–268. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira Francisco FA, Pereira e Silva JL, Hochhegger B, et al. Pulmonary alveolar microlithiasis. State-of-the-art review. Respir Med 2013; 107: 1–9. [DOI] [PubMed] [Google Scholar]
- 4.Mikhailov V. Pulmolithiasis endalveolaris et interstitialis diffusa. [Pulmonary alveolar microlithiasis]. Klin Med (Moskau) 1954; 32: 31–36. [PubMed] [Google Scholar]
- 5.Sosman MC, Dodd GD, Jones WD, et al. The familial occurrence of pulmonary alveolar microlithiasis. Am J Roentgenol Ther Nucl Med 1957; 77: 947–1012. [PubMed] [Google Scholar]
- 6.Perosa L, Ramunni M. La microlitiasi endoalveolare del polmone. Rec Progr Med 1959; 26: 353–429. [Google Scholar]
- 7.Castellana G, Lamorgese V. Pulmonary alveolar microlithiasis. World cases and review of the literature. Respiration 2003; 70: 549–555. [DOI] [PubMed] [Google Scholar]
- 8.Mariotta S, Ricci A, Papale M, et al. Pulmonary alveolar microlithiasis: report on 576 cases published in the literature. Sarcoidosis Vasc Diffuse Lung Dis 2004; 21: 173–181. [PubMed] [Google Scholar]
- 9.Ye F, Xie J, Zhang N, et al. Pulmonary alveolar microlithiasis: report of three cases and literature review. Int J Respir 2011; 31: 1394–1398. [Google Scholar]
- 10.Hagiwara K, Johkob T, Tachibana T. Pulmonary alveolar microlithiasis. In: McCormack FX, Trapnell BC, Panos RJ, eds. Molecular Basis of Pulmonary Disease: Insights from Rare Lung Disorders. New York, Springer Science+ Business Media, 2010; pp. 325–338. [Google Scholar]
- 11.Castellana G, Lamorgese V, Lombardi P, et al. Microlitiasi alveolare polmonare: proposta di iter diagnostico ottimale. La casistica della Puglia. Rass Pat App Respir 2004; 19: 323–328. [Google Scholar]
- 12.Tanrikuku AÇ, Dağli EC, Şenyiğit A, et al. Pulmoner alveoler mikrolithiazis: Türkiye’ de sekiz olgunun radyolojik bulgulari. [Pulmonary alveolar microlithiasis: radiological findings of eight cases in Turkey]. Turkiye Klinikleri J Med Sci 2010; 30: 713–720. [Google Scholar]
- 13.Caffrey PR, Altman RS. Pulmonary alveolar microlithiasis occurring in premature twins. J Pediatr 1965; 66: 758–763. [DOI] [PubMed] [Google Scholar]
- 14.Stefani M. La microlitiasi alveolare polmonare. Anat Patol Oncol 1968; 34: 485–526. [Google Scholar]
- 15.Dahabreh M, Najada A. Pulmonary alveolar microlithiasis in an 8-month-old infant. Ann Trop Paediatr 2009; 29: 55–59. [DOI] [PubMed] [Google Scholar]
- 16.Yalin T, Arslan A, Selçuk M, et al. Pulmoner alveoler mikrolitiazis: altı olgu bildirisi. OMÜ Tip Dergisi 1993; 10: 47–50. [Google Scholar]
- 17.Krishnakurup J, Abdelsayed G. The calcareous lung. Mayo Clin Proc 2011; 86: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takahashi H, Chiba H, Shiratori M, et al. Elevated serum surfactant protein A and D in pulmonary alveolar microlithiasis. Respirology 2006; 11: 330–333. [DOI] [PubMed] [Google Scholar]
- 19.Sears MR, Chang AR, Taylor AJ. Pulmonary alveolar microlithiasis. Thorax 1971; 26: 704–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaber KA, Najem SA, Twair A, et al. Pulmonary alveolar microlithiasis in living adult monozygotic twin; CT scan versus CXR family screening results. Am J Respir Crit Care Med 2012; 185: A5427. [Google Scholar]
- 21.da Silva Figueiredo S, Vilela Ribeiro LH, da Nóbrega BB, et al. Microlitíase alveolar pulmonar em gemeos univitelinos – relato de dois casos. Radiol Bras 2002; 35: 239–242. [Google Scholar]
- 22.Castellana G, Lamorgese V. La micro litiasi endoalveolare polmonare. Caso clinico a sostegno dell'ipotesi ereditaria. Rass Pat App Respir 1997; 12: 247–251. [Google Scholar]
- 23.Senyiğit A, Yaramiş A, Gϋrkan F, et al. Pulmonary alveolar microlithiasis: a rare familial inheritance with report of six cases in a family. Respiration 2001; 68: 204–209. [DOI] [PubMed] [Google Scholar]
- 24.Kiatboonsri S, Charoenpan P, Vathesatogkit P, et al. Pulmonary alveolar microlithiasis: report of five cases and literature review. J Med Assoc Thai 1985; 68: 672–677. [PubMed] [Google Scholar]
- 25.Esguerra-Gómez G, Lichtemberger E, Santamaría A, et al. Familial pulmonary alveolar microlithiasis: four cases from Colombia. Radiology 1959; 72: 550–561. [DOI] [PubMed] [Google Scholar]
- 26.Ma T, Ren J, Yin J. A pedigree with pulmonary alveolar microlithiasis: a clinical case report and literature review. Cell Biochem Biophys 2014; 70: 565–572. [DOI] [PubMed] [Google Scholar]
- 27.Wang H, Yin X, Wu D, et al. SLC34A2 gene compound heterozygous mutation identification in a patient with pulmonary alveolar microlithiasis and computational 3D protein structure prediction. Meta Gene 2014; 2: 557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thiruvengadam KV, Arunachalam K, Murali MR, et al. Pulmonary alveolar microlithiasis in a family. J Assoc Physicians India 1972; 7: 707–712. [PubMed] [Google Scholar]
- 29.Kanra G, Tanyol E, Göçmen A. Pulmonary alveolar microlithiasis (a case report). Turkish J Pediatr 1988; 30: 61–67. [PubMed] [Google Scholar]
- 30.Monabati A, Ghayumi AM, Kumar PV. Familial pulmonary alveolar microlithiasis diagnosed by bronchoalveolar lavage. A case report. Acta Cytol 2007; 51: 80–82. [DOI] [PubMed] [Google Scholar]
- 31.Poelma DL, Ju MR, Bakker SC, et al. A common pathway for the uptake of surfactant lipids by alveolar cells. Am J Respir Cell Mol Biol 2004; 30: 751–758. [DOI] [PubMed] [Google Scholar]
- 32.Zhong YQ, Hu CP, Cai XD, et al. [A novel mutation of the SLC34A2 gene in a Chinese pedigree with pulmonary alveolar microlithiasis]. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2009; 26: 365–368. [PubMed] [Google Scholar]
- 33.Hishihara Y, Hagiwara K, Zen K, et al. A case of pulmonary alveolar microlithiasis with an intragenetic deletion in SLC34A2 detected by a genome-wide SNP study. Thorax 2009; 64: 365–367. [DOI] [PubMed] [Google Scholar]
- 34.Dogan OT, Ozsahin SL, Gul E, et al. A frame-shift mutation in the SLC34A2 gene in three patients with pulmonary alveolar microlithiasis in an inbred family. Intern Med 2010; 49: 45–49. [DOI] [PubMed] [Google Scholar]
- 35.Jönsson ÅL, Hilberg O, Bendstrup EM, et al. SLC34A2 gene mutation may explain comorbidity of pulmonary alveolar microlithiasis and aortic valve sclerosis. Am J Respir Crit Care Med 2012; 185: 464. [DOI] [PubMed] [Google Scholar]
- 36.Özbudak IH, Başsorgun CI, Ozbılım G, et al. Pulmonary alveolar microlithiasis with homozygous c.316G > C (p.G106R) mutation: a case report. Turk Patoloji Derg 2012; 28: 282–285. [DOI] [PubMed] [Google Scholar]
- 37.Yin X, Wang H, Wu D, et al. SLC34A2 gene mutation of pulmonary alveolar microlithiasis: report of four cases and review of literatures. Respir Med 2013; 107: 217–222. [DOI] [PubMed] [Google Scholar]
- 38.Proesmans M, Boon M, Verbeken E, et al. Pulmonary alveolar microlithiasis: a case report and review of the literature. Eur J Pediatr 2012; 171: 1069–1072. [DOI] [PubMed] [Google Scholar]
- 39.Yang Y, Qiao JH, An JH, et al. [Detection of SLC34A2 in patients with pulmonary alveolar microlithiasis and the effect of SLC34A2 on transportation of calcium and phosphate in human alveolar epithelial cells]. Zhonghua Jie He He Hu Xi Za Zhi 2008; 31: 908–911. [PubMed] [Google Scholar]
- 40.Olauson H, Brandenburg V, Larsson TE. Mutation analysis and serum FGF23 level in a patient with pulmonary alveolar microlithiasis. Endocrine 2010; 37: 244–248. [DOI] [PubMed] [Google Scholar]
- 41.Castellana G, Fanelli C, Napoli D, et al. La microlitiasi alveolare polmonare: decorso clinico, terapia e rivisitazione di un singolare caso lungo vivente. Quad Pat Tor D Cotugno 1998; 7: 26–29. [Google Scholar]
- 42.Biressi PC, Casassa PM. La microlitiasi polmonare endoalveolare. Min Med 1956; 47: 930–939. [PubMed] [Google Scholar]
- 43.Coetzee T. Pulmonary alveolar microlithiasis with involvement of the sympathetic nervous system and gonads. Thorax 1970; 25: 637–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sandhyamani S, Verma K, Sharma SK, et al. Pulmonary alveolar microlithiasis. Indian J Chest Dis Allied Sci 1982; 24: 33–35. [PubMed] [Google Scholar]
- 45.Arslan A, Yalin T, Akan H, et al. Pulmonary alveolar microlithiasis associated with calcifications in the seminal vesicles. J Belge Radiol 1996; 79: 118–119. [PubMed] [Google Scholar]
- 46.Qublan HS, Athamneh I, Al-Kaisi NS. Azoospermia associated with testicular and pulmonary microlithiasis. J Diagn Med Sonogr 2003; 19: 192–194. [Google Scholar]
- 47.Kanat F, Teke T, Imecik O. Pulmonary alveolar microlithiasis with epididymal and periurethral calcifications causing obstructive azospermia. Int J Tuberc Lung Dis 2004; 8: 1274–1276. [PubMed] [Google Scholar]
- 48.Castellana G, Castellana R, Carone D, et al. Microlitiasi alveolare polmonare associata a microlitiasi delle vescichette seminali. Rass Pat App Respir 2010; 25: 206–210. [Google Scholar]
- 49.Chatterji R, Gaude GS, Patil PV. Pulmonary alveolar microlithiasis: diagnosed by sputum examination and transbronchial biopsy. Indian J Chest Dis Allied Sci 1997; 39: 263–267. [PubMed] [Google Scholar]
- 50.Pollice L, Pirrelli A. La microlitiasi endoalveolare del polmone. Rec Progr Med 1970; 48: 63–96. [PubMed] [Google Scholar]
- 51.Terada T. Pulmonary alveolar microlithiasis with cor pulmonale: an autopsy case demonstrating a marked decrease in pulmonary vascular beds. Respir Med 2009; 103: 1768–1771. [DOI] [PubMed] [Google Scholar]
- 52.Harbitz F. Extensive calcification of the lungs as a distinct disease. Arch Intern Med 1918; 21: 139–146. [Google Scholar]
- 53.Marchiori E, Gonçalves CM, Escuissato DL, et al. Pulmonary alveolar microlithiasis: high-resolution computed tomography findings in 10 patients. J Bras Pneumol 2007; 33: 552–557. [DOI] [PubMed] [Google Scholar]
- 54.Sumikawa H, Johkoh T, Tomiyama N, et al. Pulmonary alveolar microlithiasis: CT and pathologic findings in 10 patients. Monaldi Arch Chest Dis 2005; 63: 59–64. [DOI] [PubMed] [Google Scholar]
- 55.Castellana G, Castellana R, Fanelli C, et al. La microlitiasi alveolare polmonare: decorso clinico e radiologico, convenzionale e HRCT, in tre casi. Ipotesi di classificazione radiologica della malattia. Radiol Med 2003; 106: 160–168.14612837 [Google Scholar]
- 56.Gasparetto EL, Tazoniero P, Escuissato DL, et al. Pulmonary alveolar microlithiasis presenting with crazy-paving pattern on high resolution CT. Br J Radiol 2004; 77: 974–976. [DOI] [PubMed] [Google Scholar]
- 57.Weinstein DS. Pulmonary sarcoidosis: calcified micronodular pattern simulating pulmonary alveolar microlithiasis. J Thorac Imaging 1999; 14: 218–220. [PubMed] [Google Scholar]
- 58.Palombini BC, da Silva Porto N, Wallau CU, et al. Bronchopulmonary lavage in alveolar microlithiasis. Chest 1981; 80: 242–243. [DOI] [PubMed] [Google Scholar]
- 59.Caputi M, Guarino C, Cautiero V, et al. Ruolo diagnostico del BAL nella microlitiasi alveolare polmonare. [Diagnostic role of BAL in pulmonary alveolar microlithiasis]. Arch Monaldi Mal Torace 1990; 45: 353–364. [PubMed] [Google Scholar]
- 60.Mariotta S, Guidi L, Mattia P, et al. Pulmonary microlithiasis. Report of two cases. Respiration 1997; 64: 165–169. [DOI] [PubMed] [Google Scholar]
- 61.Ozcelik U, Yalcin E, Ariyurek M, et al. Long-term results of disodium etidronate treatment in pulmonary alveolar microlithiasis. Pediatr Pulmonol 2010; 45: 514–517. [DOI] [PubMed] [Google Scholar]
- 62.Azim S, Azim W, Hayat F, et al. Treatment of pulmonary alveolar microlithiasis with allendronate sodium. Biomedica 2004; 20: 32–35. [Google Scholar]
- 63.Bonnette P, Bisson A, el Kadi NB, et al. Bilateral single lung transplantation. Complications and results in 14 patients. Eur J Cardiothorac Surg 1992; 6: 550–554. [DOI] [PubMed] [Google Scholar]
- 64.Stamatis G, Zerkowski HR, Doetsch N, et al. Sequential bilateral lung transplantation for pulmonary alveolar microlithiasis. Ann Thorac Surg 1993; 56: 972–975. [DOI] [PubMed] [Google Scholar]
- 65.Edelman JD, Bavaria J, Kaiser LR, et al. Bilateral sequential lung transplantation for pulmonary alveolar microlithiasis. Chest 1997; 112: 1140–1144. [DOI] [PubMed] [Google Scholar]
- 66.Raffa H, El-Dakhaknny M, Al-Ibrahim K, et al. Single lung transplantation for alveolar microlithiasis: the first clinical report. Saudi J Kidney Dis Transpl 1996; 7: 189–193. [PubMed] [Google Scholar]
- 67.Jackson KB, Modry DL, Halenar J, et al. Single lung transplantation for pulmonary alveolar microlithiasis. J Heart Lung Transplant 2001; 20: 226. [DOI] [PubMed] [Google Scholar]
- 68.Shadmehr MB, Arab M, Pejhan S, et al. Eight years of lung transplantation: experience of the National Research Institute of Tuberculosis and Lung Diseases. Transplant Proc 2009; 41: 2887–2889. [DOI] [PubMed] [Google Scholar]
- 69.Borrelli R, Fossi A, Volterrani L, et al. Right single-lung transplantation for pulmonary alveolar microlithiasis. Eur J Cardiothorac Surg 2014; 45: e40. [DOI] [PubMed] [Google Scholar]
- 70.Coulibaly B, Fernandez C, Reynaud-Gaubert M, et al. Microlithiase alvéolaire avec fibrose leading to lung sévère conduisant à la greffe. Ann Pathol 2009; 29: 241–244. [DOI] [PubMed] [Google Scholar]
- 71.Samano MN, Waisberg DR, Canzian M, et al. Lung transplantation for pulmonary alveolar microlithiasis: a case report. Clinics (Sao Paolo) 2010; 6: 233–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shigemura N, Bermudez C, Hattler BG, et al. Lung transplantation for pulmonary alveolar microlithiasis. J Thorac Cardiovasc Surg 2010; 139: e50–e52. [DOI] [PubMed] [Google Scholar]
- 73.Siddiqui NA, Fuhrman CR. Best cases from the AFIP: pulmonary alveolar microlithiasis. Radiographics 2011; 31: 585–590. [DOI] [PubMed] [Google Scholar]
- 74.Klikovits T, Jaksch P, Hoda M, et al. A seldom indication for lung transplantation: pulmonary alveolar microlithiasis – the Vienna experience. Joint Annual Congress of the German, Austrian and Swiss Society of Thoracic Surgery, Basel, Switzerland, October 24–26, 2013. [DOI] [PubMed]
- 75.Güçyetmez B, Ogan A, Ayyildiz AC, et al. Lung transplantation in an intensive care patient with pulmonary alveolar microlithiasis – a case report. F1000Res 2014; 3: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.