ABSTRACT
Background
Patients with cervicogenic dizziness (CGD) present with dizziness, cervical spine dysfunctions, and postural imbalance, symptoms that can significantly impact their daily functioning.
Objectives
To provide evidence-based recommendations for the management of patients with CGD.
Methods
Three databases were searched for randomized controlled trials (RCTs) (last search 15 May 2021). Outcome measures included dizziness, cervical spine, and balance parameters. Cochrane standard methodological procedures were used and included the RoB 2.0 and GRADE. Where possible, RCTs were pooled for meta-analysis.
Results
Thirteen RCTs (n = 898 patients) of high (two RCTs), moderate (five RCTs), and low (six RCTs) methodological quality were analyzed. Six RCTs were included in the meta-analysis. Only three RCTs specified the cause of CGD. They showed inconsistent findings for the effectiveness of exercise therapy in patients with traumatic CGD. Manual therapy and manual therapy combined with exercise therapy may reduce CGD, cervical spine, and balance dysfunctions.
Conclusion
There is moderate quality of evidence that manual therapy reduces CGD, cervical spine, and balance symptoms. When manual therapy is combined with exercise therapy, the positive effect on CGD, cervical spine, and balance symptoms is even stronger. However, the quality of the evidence here is very low.
KEYWORDS: Dizziness, cervical vertebrae, exercise therapy, musculoskeletal manipulations
Introduction
Dizziness is a frequently occurring symptom with a lifetime prevalence between 15% and 35% in the general population [1–6]. There are many different causes of dizziness, including vestibular, cardiorespiratory, neurological, mental/psychiatric, and cervical [7]. Cervical-related dizziness can be divided further into dizziness caused by altered blood flow in the cervical arterial blood vessels, either by compression (e.g. vertebrobasilar insufficiency) or disruption (e.g. sympathetic plexus induced vasoconstriction) [8,9], and dizziness caused by altered functioning of the cervical proprioceptors [10,11]. The latter is called cervicogenic dizziness (CGD) and is the scope of this review.
The cervical proprioceptors are very densely concentrated in the cervical zygapophyseal joints of C1 to C3 and the deep segmental upper cervical muscles [12,13]. They can become dysfunctional due to trauma [14], muscle fatigue [15], degenerative changes [10] and/or inflammation. In addition, due to the altered cervical proprioceptive information to the central nervous system, head and body posture control may be impaired, and dizziness may occur due to a sensory mismatch with the information from the vestibular and visual systems [11,16].
Dizziness, cervical spine, and balance complaints can significantly impact patients’ daily functioning [17,18]. Therefore, it is essential to find adequate therapeutic methods for patients with CGD. Across studies, multiple interventions have been described. A frequently discussed therapeutic method is manual therapy. Manual therapy (both mobilization and manipulation techniques) targeting the upper cervical spine has been shown to not only reduce muscle spasms and restore zygapophyseal joint mobility and joint play, but also to promote the flow of afferent information, including proprioceptive input, toward the central nervous system [19–21]. This theoretical effectiveness of upper cervical manual therapy for CGD has been confirmed in clinical studies [22–24]. Furthermore, there is a theoretical framework for the use of vestibular rehabilitation for CGD as well. It has been postulated that vestibular exercises can stimulate the vestibulo-cerebellar system to compensate for the altered cervical afferent input [22,25].
It remains, however, unclear what the effectiveness is compared to other therapeutic approaches in reducing CGD. In addition, no summary is available showing which therapeutic strategies are effective for cervical spine and balance complaints in patients with CGD.
Central sensitization or nociplastic pain (i.e. increased responsiveness of the central neurons to noxious input) is a common feature in patients with (whiplash) neck trauma [26–28]. Furthermore, this cervical sensory hypersensitivity has been linked to prolongation of postural balance complaints [29,30] and can therefore complicate therapy. To ascertain whether patients with and without traumatic CGD should require a different therapeutic approach, the results in this study are discussed separately for these two subgroups of patients.
This review aims to evaluate the average intervention effect of different therapeutic methods on dizziness, and secondarily on the cervical spine and balance symptoms in patients with CGD of both traumatic and non-traumatic origin.
Methods
This systematic review has been drafted according to the recommendations of The Cochrane Handbook for Systematic Reviews of Interventions [31] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [32]. A protocol of this study was submitted prospectively (PROSPERO – registration number CRD42020140301).
Information sources and search strategy
Electronic databases of PubMed, Embase and Web of Science were searched up to 15 May 2021. The search strategies (APPENDIX A), formulated in agreement with three subject matter experts (C.D.V., S.R., W.D.H.), included both terms (and synonyms) for CGD and for therapeutic methods. In addition, nonspecific terms were used for therapeutic methods to allow a broad search in the literature. Additional terms were added to include only randomized controlled trials (RCTs).
Article selection
The study inclusion criteria were: (1) patients (≥ 18 years old) who presented with both dizziness and a cervical spine dysfunction, either reported as such or implied by mentioning cervical spine symptoms or cervical spine triggers for dizziness; (2) evaluation of the effectiveness of therapeutic methods on CGD (primary outcome measure), cervical spine and balance symptoms (secondary outcome measures); (3) RCT design; and (4) written in English or Dutch. RCTs that included patients suffering from strong sensations of spinning vertigo or whose dizziness could be explained by another disorder, were excluded. RCTs which discussed only preliminary findings were excluded as well.
All collected articles and predefined study selection criteria were imported into an excel template (available from: http://processbook.kce.fgov.be) by first author C.D.V. and provided to all reviewers (J.L. and W.D.H.). After each reviewer screened all articles separately, the findings were compared to form a consensus. The reference lists were checked manually for additional relevant RCTs of all RCTs included through consensus.
Data collection process
The following data were extracted from the included RCTs: (1) study characteristics (authors, year of publication, and sample size); (2) patient characteristics (age, gender, and criteria for CGD); (3) therapeutic characteristics (type, intensity, and duration); and (4) therapeutic effect on CGD and, if mentioned, on the cervical spine and balance symptoms. In case of unclear or missing data, the corresponding authors were contacted.
Data extraction was performed independently using a pre-formatted excel spreadsheet by C.D.V. and J.L. Results were compared afterward, and any discrepancies were discussed to reach a final consensus. If needed, a third reviewer (W.D.H.) provided additional feedback.
To facilitate insight into the study results, the collected data were discussed separately depending on the cause of CGD mentioned (traumatic versus non-traumatic) and the type of therapy investigated (e.g. physiotherapeutic techniques, medication).
Risk of bias assessment
For the risk of bias (RoB) assessment, the RoB 2.0 tool was used [33,34]. Each RCT was screened for bias in five domains: the randomization procedure, the intervention, handling missing outcome data, the measurement of the outcome, and the reported results. The RoB assessment was performed individually by the reviewers (C.D.V. and J.L.) in the manner described in the RoB 2.0 guidelines. The individual assessments of C.D.V. and J.L. were compared, and where they disagreed, a third reviewer (W.D.H.) made the final decision.
Statistical analysis
For each of the included RCTs, the within-group differences (i.e. the differences between baseline and post-therapy results) were first calculated for both the intervention and control groups separately. Then, these within-group differences in the outcome parameter were compared between intervention and control groups to measure the magnitude of the therapeutic effects. Means and standard deviations were extracted from the RCTs. Non-reported standard deviations were calculated based on the reported confidence intervals (CI), standard errors, or p-values. Other calculations performed were merging of data results of similar experimental interventions within the same RCT, merging of data results related to the same plane of movement (e.g. rotation left and right), and conversion of outcome results into the units of the most commonly used instrument if needed [35]. Along with the difference in means (MD), the equivalent 95% CI was also computed.
A meta-analysis, using the random-effects method [36], was performed provided that a minimum of three RCTs had comparable patient and therapeutic characteristics. Heterogeneity among these RCTs was measured with the Cochran Q test. Significant heterogeneity was present if Chi2 < 0.10. The Higgins I2 test expressed the amount of heterogeneity. The I2 ranges between 0 and 100%, whereby a higher value means more heterogeneity across studies [37]. Results were graphically displayed through forest plots.
Significance was set at a p-value of less than 0.05. Statistical analyses were performed using the software package Review Manager 5.3 [31].
Minimal clinically important difference
Information on the minimal clinically important difference (MCID) is available in the literature for the Dizziness Handicap Inventory questionnaire (DHI 0–100 points = 18 points) [38], neck pain visual analogue scale (VAS 0–100 mm = varied between 4.6 to 21.4 mm) [39], and cervical range of motion (CROM flexion-extension = 4–6°; CROM rotation = 5–10°) [40].
GRADE assessment
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to rate the quality of the retrieved evidence. The following five domains were assessed: within-study risk of bias, inconsistency, indirectness, imprecision, and publication bias [41]. Information on the interpretation of the quality of evidence score is provided in Table 1. The GRADE was performed by C.D.V. and J.L. separately. Their findings were compared. In case of disagreements, a third reviewer (W.D.H.) made the final decision.
Table 1.
Interpretation of the quality of evidence (the GRADE method) a, b.
| Quality |
Explanation |
| High | There is high confidence that the true effect lies close to that of the estimate of the effect. |
| Moderate | There is moderate confidence in the effect estimate. The true effect is likely to be close to the estimate of the effect but there is a possibility that is it substantially different. |
| Low | There is limited confidence in the effect estimate. The true effect may be substantially different from the estimate of the effect. |
| Very low | There is little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of the effect. |
aAbbreviations: GRADE = Grading of Recommendations, Assessment, Development and Evaluations
bGuyatt, G.H., et al., GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. British Medical Journal, 2008. 336(7650): p. 924–6.
Results
The search yielded 2658 articles. Manual search resulted in one additional article [42]. Of those, thirty-six articles were screened on full text resulting in 13 RCTs representing 11 unique studies (n = 898), meeting all eligibility criteria [42–54]. Flowchart of study selection and characteristics of excluded articles are available in Figure 1 and APPENDIX B, respectively.
Figure 1.
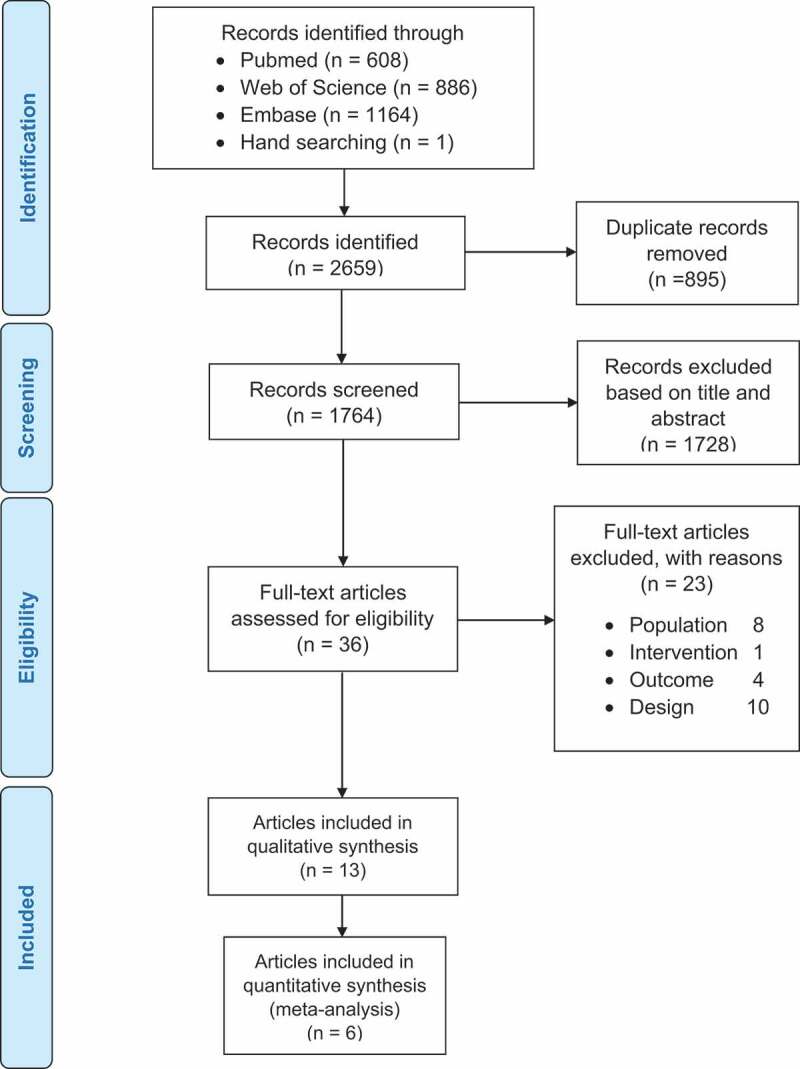
PRISMA flow diagram.
Characteristics of the included RCTs
Characteristics of the included RCTs are presented in APPENDIX B.
The main criteria for a CGD diagnosis were non-rotatory dizziness and neck pain [45–54]. Only three RCTs (n = 169) specified the cause of CGD, all of which were of traumatic origin (i.e. whiplash-associated disorder) [42–44].
Twelve of the 13 RCTs discussed physiotherapeutic techniques [42–53]. Six RCTs focused on manual therapy and investigated traction-manipulations [46] and sustained natural apophyseal glides (SNAGs) of the upper cervical segments in the dizziness provoking movement directions [48,50], or a combination of SNAGs and mobilizations [51–53]. Three RCTs that did specify the cause of CGD, focused on exercise therapy and investigated vestibular rehabilitation [42,43] and cervical spine exercises (including motor relearning, stabilization, and endurance training) with or without behavioral approach [44]. In three RCTs, exercise therapy was combined with dry needling (trapezius and sternocleidomastoid muscles) [45], or manual therapy. The manual therapy consisted of DennerollTM cervical spine traction [49], or soft tissue and passive mobilization techniques [47]. The exercise therapy included cervical spine stretching, strengthening and stabilization exercises, relaxation techniques, and trunk stabilization exercises. One RCT discussed an alternative therapy, Shi-style cervical spine mobilizations [54].
Control interventions were usually sham or no therapy [42,43,46–48,50–53]. Yet, the control intervention was physiotherapeutic techniques in three RCTs (i.e. general physical activity [44], cervical spine exercises [45] or a multimodal cervical program [49]), or traditional massage in one RCT [54].
Dizziness outcome measures were intensity, frequency, and impact on quality of life. Cervical spine outcome measures were reported in ten RCTs [42,44,46–53] and included cervical spine pain, mobility, repositioning accuracy, trigger points, sagittal alignment, and impact on quality of life. Static and dynamic balance outcome measures were reported in nine RCTs [42,44–48,50,52,53].
Follow-up periods ranged from 48 hours to 1 year. In addition, six RCTs, which did not specify the cause of CGD and discussed manual therapy, provided data for meta-analyses [46,48,50–53].
Risk of bias of the individual RCTs
Risk of bias was high or unclear for the randomization procedure (5 RCTs) [42,45,47,50,51], the intervention (7 RCTs) [42–45,47,49,54], handling missing outcome data (4 RCTs) [43,46,48,54], the measurement of the outcome (3 RCTs) [44,45,47], and the reported results (8 RCTs) [42,43,45,47,50–52,54]. The overall RoB was low in 2 RCTs [49,53], moderate in 5 RCTs [46,48,50–52] and high in 6 RCTs [42–45,47,54] (Table 2 and Table 3).
Table 2.
Risk of bias summary: review authors’ judgments about each risk of bias item for each included RCT a.
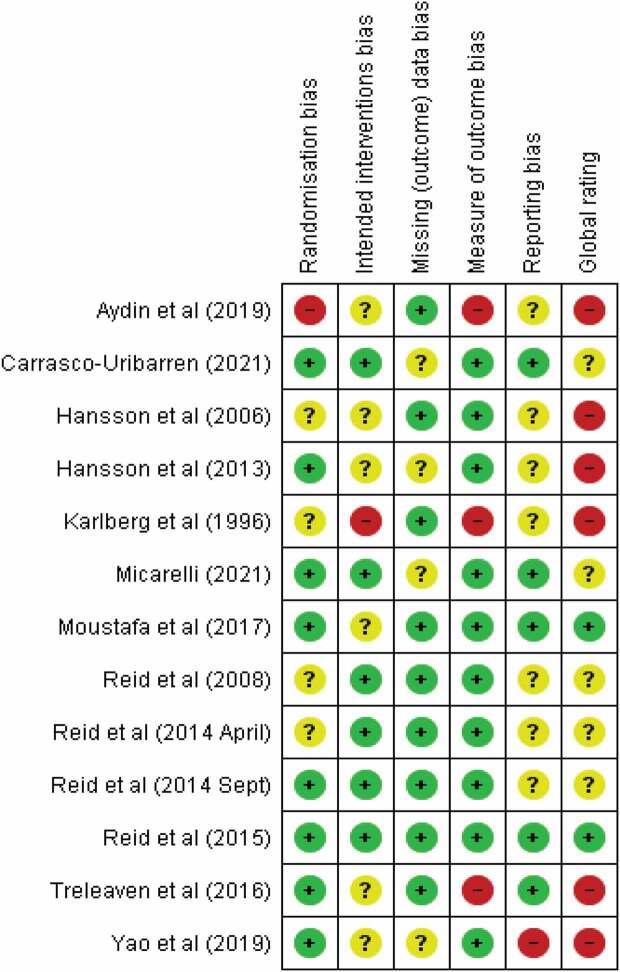 |
aInterpretation:  = Low risk of bias;
= Low risk of bias;  = Moderate risk of bias;
= Moderate risk of bias;  = High risk of bias
= High risk of bias
Table 3.
Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included RCTs a.
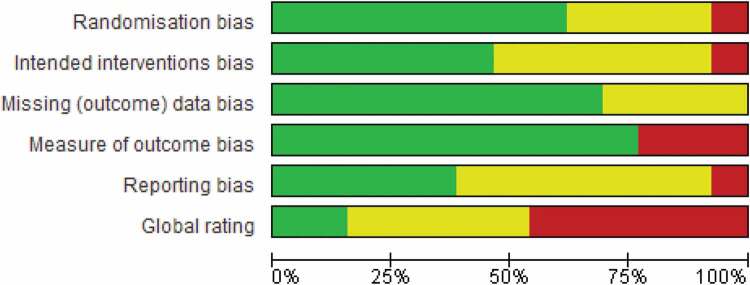 |
aInterpretation:  = Low risk of bias;
= Low risk of bias;  = Moderate risk of bias;
= Moderate risk of bias;  = High risk of bias
= High risk of bias
Results of the individual RCTs and syntheses
The results are available in APPENDIX C. The GRADE assessment is provided in APPENDIX D (Table D1-3).
RCTs specifying the cause of CGD (traumatic origin in all cases)
Dizziness. There is only a very low quality of evidence (GRADE) for the effectiveness of exercise therapy in reducing CGD. In comparison with controls, cervical spine exercises with or without behavioral therapy may reduce dizziness intensity (10 cm visual analogue scale (VAS); at rest: MD −6.46 [−10.93; −1.99] 95% CI, p < 0.005; during activity: MD −6.93 [−12.79; −1.07] 95% CI, p = 0.02) and impact on quality of life (University of California Los Angeles dizziness questionnaire; MD −2.65 [−4.82; −0.48] 95% CI, p = 0.02) up to 1-year follow-up [44]. Vestibular rehabilitation may not affect CGD [42,43].
Cervical spine. There is only very low quality of evidence (GRADE) for the effectiveness of exercise therapy in reducing cervical spine symptoms. In comparison with controls, cervical spine exercises with or without behavioral therapy may improve head repositioning accuracy toward rotation (MD −1.53 [−2.71; −0.35] 95% CI, p = 0.01) and reduce Neck Disability Index score (MD −2.26 [−4.04; −0.48] 95% CI, p = 0.01) up to 1-year follow-up. However, cervical spine exercises with or without behavioral therapy may have no effect on neck pain (10 cm VAS; MD at 1-year follow-up: −4.73 [−10.77; 1.31] 95% CI, p = 0.13) although the MD exceeds the MCID [44]. Vestibular rehabilitation may not affect cervical spine symptoms [42,43].
Balance. Based on a very low level of evidence (GRADE), exercise therapy may have no effect on static or dynamic balance compared with the control intervention [42–44].
RCTs not specifying the cause of CGD
Dizziness. Based on moderate level of evidence (GRADE) and in comparison with controls, manual therapy likely reduces CGD (i.e. intensity [46,50,51,53], frequency [51,53], and impact on quality of life [46,48,50,51,53]) up to 1-year follow-up. Meta-analyses confirm the overall beneficial effect of manual therapy in reducing dizziness intensity (10 cm VAS, MD at 4–6 weeks follow-up: −22.56 [−28.11; −17.01] 95% CI; p < 0.001; I2 = 0%; Figure 2) [46,50,51,53], and the impact of dizziness on quality of life (Dizziness Handicap Inventory scale (DHI), MD at 4–6 weeks follow-up: −10.04 [−16.36; −3.73] 95% CI; p = 0.002; I2 = 79%; Figure 3) even though the MD does not exceed the MCID in this case [46,50,51,53,55]. Furthermore, based on very low level of evidence (GRADE) and in comparison with controls, combined exercise therapy and manual therapy may reduce CGD (i.e. intensity [47,49], frequency [49], and impact on quality of life [49]), and combined exercise and dry needling therapy may reduce the impact of CGD on quality of life [45] up to 1-year follow-up. Shi-style cervical mobilizations probably do not reduce CGD compared to the control intervention, which is based on a moderate level of evidence (GRADE) [54].
Figure 2.
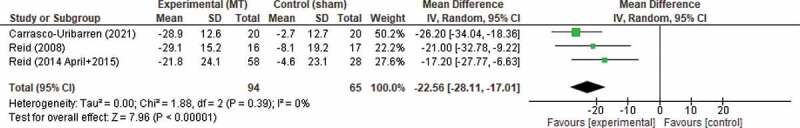
Forest plot demonstrating the effectiveness of manual therapy on Dizziness intensity at 4–6 weeks post-therapy a, b.
(1) Carrasco-Uribarren (2021) = traction-manipulation(2) Reid (2008) = sustained natural apophyseal glides(3) Reid (2014 April+2015) = sustained natural apophyseal glides and cervical mobilizationsa Dizziness intensity: 0–100 mm VAS; the higher the VAS, the higher the dizziness intensityb Abbreviations: CI = confidence interval; df = degrees of freedom; IV = inverse variance; MT = manual therapy; SD = standard deviation
Figure 3.
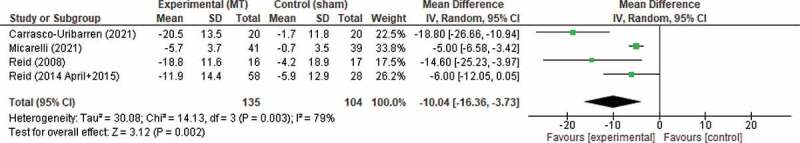
Forest plot demonstrating the effectiveness of manual therapy on Dizziness Handicap Inventory (DHI) at 4–6 weeks post-therapy a, b.
(1) Carrasco-Uribarren (2021) = traction-manipulation(2) Micarelli (2021) = sustained natural apophyseal glides(3) Reid (2008) = sustained natural apophyseal glides(4) Reid (2014 April+2015) = sustained natural apophyseal glides and cervical mobilizationsa DHI: 0–100 points; the higher the DHI score, the higher the impact of dizziness on quality of lifeb Abbreviations: CI = confidence interval; df = degrees of freedom; DHI = Dizziness Handicap Inventory; IV = inverse variance; MT = manual therapy; SD = standard deviation
Cervical spine. Based on moderate level of evidence (GRADE) and in comparison with controls, manual therapy likely improves cervical spine symptoms (i.e. pain [46,48,50], mobility [46,48,50], and impact on quality of life [48]) up to 1-year follow-up. Meta-analyses confirm the overall beneficial effect of manual therapy in improving mobility (MD at 4–6 weeks follow-up for CROM flexion-extension: 7.18 [3.65; 10.70] 95% CI, p < 0.0001, I2 = 65%; MD for CROM rotation 3.88 [0.18; 7.59] 95% CI, p = 0.04, I2 = 73%; Figure 4) [46,48,50,52,53] and pain intensity (10 cm VAS, MD at 4–6 weeks follow-up: −14.01 [−22.77; −5.26] 95% CI, p = 0.002, I2 = 81%; Figure 5) [46,48,50,51,53]. Here, the MDs for CROM flexion-extension and cervical spine pain intensity exceed their respective MCIDs. Furthermore, based on very low level of evidence (GRADE) and in comparison with controls, combined exercise and manual therapy may improve cervical spine pain [47,49], head repositioning accuracy [49], and sagittal alignment [49], and combined exercise and dry needling therapy may improve cervical spine pain, pressure pain threshold and head repositioning accuracy [45] up to 1-year follow-up. No information is available on the effectiveness of Shi-style cervical mobilizations in improving neck symptoms [54].
Figure 4.
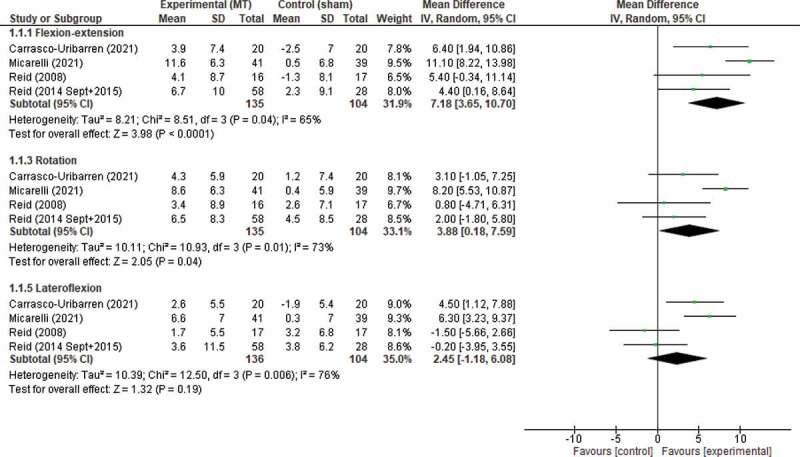
Forest plot demonstrating the effectiveness of manual therapy on cervical range of motion (CROM) at 4–6 weeks post-therapy a, b.
(1) Carrasco-Uribarren (2021) = traction-manipulation(2) Micarelli (2021) = sustained natural apophyseal glides(3) Reid (2008) = sustained natural apophyseal glides(4) Reid (2014 Sept+2015) = sustained natural apophyseal glides and cervical mobilizationsa CROM: degrees; the higher the CROM, the higher the cervical mobilityb Abbreviations: CI = confidence interval; CROM = cervical range of motion; df = degrees of freedom; IV = inverse variance; MT = manual therapy; SD = standard deviation
Figure 5.
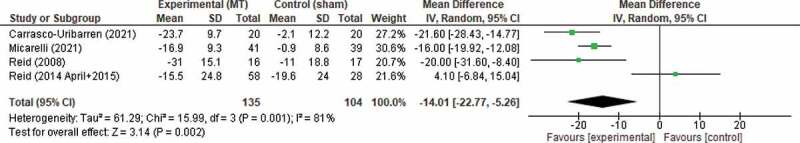
Forest plot demonstrating the effectiveness of manual therapy on neck pain intensity at 4–6 weeks post-therapy a, b.
(1) Carrasco-Uribarren (2021) = traction-manipulation(2) Micarelli (2021) = sustained natural apophyseal glides(3) Reid (2008) = sustained natural apophyseal glides(4) Reid (2014 April+2015) = sustained natural apophyseal glides and cervical mobilizationsa Neck pain intensity: 0–100 mm VAS; the higher the VAS score, the higher the neck pain intensityb Abbreviations: CI = confidence interval; df = degrees of freedom; IV = inverse variance; MT = manual therapy; SD = standard deviation; VAS = visual analogue scale
Balance. Based on a moderate level of evidence (GRADE) and in comparison with controls, manual therapy likely improves balance (i.e. static [48,50,52,53] and dynamic balance [46,52,53]) up to 1-year follow-up. Compared with controls, combined exercise and manual therapy may improve static balance [47], and combined exercise and dry needling therapy may improve fall index [45]). However, the level of evidence for this finding is very low (GRADE). No information is available on the effectiveness of Shi-style cervical mobilizations on balance [54].
DISCUSSION
Thirteen RCTs with a total of 898 patients were included in this systematic review [42–54]. However, the cause of CGD was specified in only three RCTs, all of which investigated exercise therapy [42–44].
Summary of main results
The effectiveness of manual therapy (aimed at the upper cervical segments in the dizziness-provoking directions) was investigated in six RCTs [46,48,50–53]. We found a moderate quality of evidence supporting the use of upper cervical manual therapy in reducing CGD, which is consistent with the literature [23,24]. What has not been previously synthesized is that there is also moderate evidence for the effectiveness of upper cervical manual therapy in reducing cervical spine and balance symptoms in patients with CGD. Based on the MCIDs, this includes a clinically significant improvement of symptoms for cervical spine pain and ROM from the patients’ perspective. The literature confirms cervical spine dysfunction, such as reduced range of motion [56–58], and postural imbalance [59–61] in patients with CGD, especially those with a whiplash-associated disorder. Theoretical background to support the positive effect on cervical spine symptoms is that manual therapy induces a chain of neurophysiological effects (e.g. decreasing muscle spasm, reducing inflammatory mediators) in the cervical spine [62,63]. In addition, manual therapy also affects direct and indirect neural pathways between the cervical spine and the central nervous system (including the vestibular and visual systems), which may explain the positive effects of manual therapy on balance function [63].
Results of the only three RCTs investigating the effectiveness of exercise therapy in patients with whiplash-related CGD were of very low quality of evidence and provided conflicting results [42–44]: cervical spine exercises, preferably with a behavioral approach, may be effective in reducing CGD and cervical spine symptoms, including a clinically relevant reduction of neck pain as reported by the patient based on its MCID. However, vestibular rehabilitation would have no positive effects at all in patients with whiplash-related CGD. In the literature, the evidence for the use of (cervical spine) exercises to improve cervical spine symptoms in chronic whiplash-associated disorder is modest [64,65], and study results on the added value of behavioral therapy are unclear [66,67]. A possible explanation for the uncertainty about the effectiveness of behavioral therapy may be that studies include both patients with and without central sensitization in their intervention group. It could be that patients with central sensitization benefit most from behavioral therapy [68]. Another possible explanation may be that behavioral therapy should be given before exercise therapy [68]. Vestibular rehabilitation is an effective therapy for many vestibular disorders [69]. However, research on the effectiveness of vestibular rehabilitation in patients with neck pain or CGD is very limited. Only two RCTs could be included, of very low methodological quality [42,43]. Given that there is a rationale for the effectiveness of vestibular rehabilitation in CGD [22], further high-quality research is indicated.
Thus far, upper cervical manual therapy seems to be the most promising therapy in patients with CGD. However, this review identified that a combination of manual therapy and exercise therapy is more effective than manual therapy alone in reducing CGD and both cervical spine and balance symptoms. The effectiveness of combined manual and exercise therapy has only been summarized in the context of patients with neck pain without dizziness [70–72].
Not all objectives of this review could be addressed thoroughly. It is still not clear whether therapy should be different depending on the cause of CGD. This is because only three of the included RCTs specified the cause of CGD [42–44]. Further complicating this issue is the heterogeneity in the diagnostic criteria used for CGD.
Evidence quality of the review
Several factors reduced confidence in the review’s effect estimates because of limitations in the included RCTs, such as: (1) moderate to high RoB in most RCTs, (2) multicomponent interventions, which increase the indirectness of the evidence (i.e. it is not clear to what extent the individual therapeutic components contribute to the overall therapeutic effect), (3) wide confidence intervals in the RCTs with a small sample size or large variability in the standard deviation of measurements between individuals, and (4) heterogeneity of diagnostic criteria for CGD, outcome measures and control interventions.
Potential biases in the review process
Even though the methodological procedures (Cochrane) and reporting guidelines (PRISMA) were rigorously adhered to, bias cannot be excluded. First, bias may have been introduced by the predefined restrictions on study eligibility (i.e. language and study design). Additionally, although the methods for the meta-analysis were discussed with a statistics expert from Antwerp University, a professional librarian with expertise in systematic review methodology was not involved.
Recommendations for future research
Further research into the optimal therapy methods in patients with CGD is needed. It is important that all studies use the same diagnostic criteria for CGD. In addition, a distinction should be made between patients with traumatic and non-traumatic origin for CGD. Furthermore, it is important that the studies correctly follow the methodological study procedures to guarantee that the measured therapy effect is reliable.
Conclusions
Based on the moderate quality of evidence, manual therapy effectively reduces CGD, neck, and balance symptoms. Combined manual and exercise therapy maybe even more effective in reducing CGD, cervical spine, and balance symptoms, but the quality of evidence for this is currently very low. Further research of high methodological quality is needed, including evaluating whether the cause for CGD should be considered.
Supplementary Material
Biographies
Charlotte De Vestel is Researcher at the Department of Rehabilitation Sciences and Physiotherapy of the University of Antwerp. Her research interests include the assessment and treatment of patients with an acute, episodic, and chronic vestibular syndrome, and patients with cervicogenic dizziness.
Luc Vereeck is Professor at the Department of Rehabilitation Sciences and Physiotherapy of the University of Antwerp. His clinical and research interests include the assessment and treatment of patients with peripheral, functional, and central vestibular disorders, and patients with multiple sensory deficits.
Susan A. Reid is a Senior Lecturer at the Physiotherapy Department of the Australian Catholic University. Her research interests include the treatment of patients with cervical spine dysfunction, headaches, temporomandibular pain, concussion, and dizziness.
Vincent Van Rompaey is Professor at the Department of Otorhinolaryngology and the Department of Translational Neurosciences of the University of Antwerp, and Consultant at the Maastricht University Medical Centre. His research interests include hearing implants, ear surgery, skull base surgery, tinnitus, balance disorders, and DFNA9.
Joris Lemmens is teaching assistant at the Department of Rehabilitation Sciences and Physiotherapy of the University of Antwerp, and is musculoskeletal physical therapist. His clinical and research interests include migraine, back and neck pain, and patient education on injury prevention, pain and movement.
Willem De Hertogh is Associate Professor at the Department of Rehabilitation Sciences and Physiotherapy of the University of Antwerp, and is musculoskeletal physical therapist with over 20 years of clinical expertise. His research interests include head and neck complaints, headaches (cervicogenic headache, tension-type headache, migraine), tinnitus, and dizziness.
Funding Statement
This work was supported by the University of Antwerp (Faculty of Medicine and Health Sciences), Wilrijk 2610, Antwerp, Belgium;
Author contributions
All authors contributed to: (1) the outline of the research goals; (2) the analysis/interpretation of data or editing of the manuscript; and (3) the final reviewing and approval of the manuscript. This research is an original work for which the authors assume public responsibility.
Disclosure statement
No potential conflict of interest was reported by the authors.
Trial registration
PROSPERO – CRD42020140301.
Data availability statement
All data relevant to the study are included in the article or are available as supplementary files.
Supplementary material
Supplemental data for this article can be accessed here
References
- [1].Yardley L, Owen N, Nazareth I, et al. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract. 1998;48(429):1131–1135. [PMC free article] [PubMed] [Google Scholar]
- [2].Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch of Int Med. 1993;153(21):2474-80. [PubMed] [Google Scholar]
- [3].Hannaford PC, Simpson JA, Bisset AF, et al. The prevalence of ear, nose and throat problems in the community: results from a national cross-sectional postal survey in Scotland. Fam Pract. 2005;22(3):227–233. [DOI] [PubMed] [Google Scholar]
- [4].Gopinath B, McMahon CM, Rochtchina E, et al. Dizziness and vertigo in an older population: the blue mountains prospective cross-sectional study. Clin Otolaryngol. 2009;34(6):552–556. [DOI] [PubMed] [Google Scholar]
- [5].Wiltink J, Tschan R, Michal M, et al. Dizziness: anxiety, health care utilization and health behavior–results from a representative German community survey. J Psychosom Res. 2009;66(5):417–424. [DOI] [PubMed] [Google Scholar]
- [6].Mendel B, Bergenius J, Langius-Eklof A.. Dizziness: a common, troublesome symptom but often treatable. J Vestib Res. 2010;20(5):391–398. [DOI] [PubMed] [Google Scholar]
- [7].Post RE, Dickerson LM. Dizziness: a diagnostic approach. Am Fam Physician. 2010;82(4):361–368. [PubMed] [Google Scholar]
- [8].Knapstad MK. Clinical characteristics in patients with cervicogenic dizziness: a systematic review. Health Sci Rep. 2019;2(9):e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yacovino DA, Hain TC. Clinical characteristics of cervicogenic-related dizziness and vertigo. Semin Neurol. 2013;33(3):244–255. [DOI] [PubMed] [Google Scholar]
- [10].Yang L, Yang C, Pang X, et al. Mechanoreceptors in diseased cervical intervertebral disc and vertigo. spine (Phila Pa 1976. Spine. 2017;42(8):540–546. [DOI] [PubMed] [Google Scholar]
- [11].Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39(5):364–377. [DOI] [PubMed] [Google Scholar]
- [12].Hulse M. Disequilibrium, caused by a functional disturbance of the upper cervical spine. Clinical aspects and differential diagnosis. Manual Med. 1983;1(1):18–23. [Google Scholar]
- [13].Sterling M, Jull G, Vicenzino B, et al. Development of motor system dysfunction following whiplash injury. Pain. 2003;103(1):65–73. [DOI] [PubMed] [Google Scholar]
- [14].Treleaven J, Jull G, Sterling M. Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med. 2003;35(1):36–43. [DOI] [PubMed] [Google Scholar]
- [15].Abdelkader NA, Mahmoud AY, Fayaz NA, et al. Decreased neck proprioception and postural stability after induced cervical flexor muscles fatigue. J of Musculoskeletal & Neuronal Interact. 2020;20(3):421–428. [PMC free article] [PubMed] [Google Scholar]
- [16].Wrisley DM, Sparto PJ, Whitney SL, et al. Cervicogenic dizziness: a review of diagnosis and treatment. J Orthop Sports Phys Ther. 2000;30(12):755–766. [DOI] [PubMed] [Google Scholar]
- [17].Dros J, Maarsingh OR, Beem L, et al. Impact of dizziness on everyday life in older primary care patients: a cross-sectional study. Health Qual Life Outcomes. 2011;9(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rogers RG. The effects of spinal manipulation on cervical kinesthesia in patients with chronic neck pain: a pilot study. J Manipulative Physiol Ther. 1997;20(2):80–85. [PubMed] [Google Scholar]
- [20].Sterling M, Jull G, Wright A. Cervical mobilisation: concurrent effects on pain, sympathetic nervous system activity and motor activity. Man Ther. 2001;6(2):72–81. [DOI] [PubMed] [Google Scholar]
- [21].Pickar JG. Neurophysiological effects of spinal manipulation. Spine J. 2002;2(5):357–371. [DOI] [PubMed] [Google Scholar]
- [22].Lystad RP, Bell G, Bonnevie-Svendsen M, et al. Manual therapy with and without vestibular rehabilitation for cervicogenic dizziness: a systematic review. Chiropr Man Therap. 2011;19(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Yaseen K, Hendrick P, Ismail A, et al. The effectiveness of manual therapy in treating cervicogenic dizziness: a systematic review. J Phys Ther Sci. 2018;30(1):96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Man Ther. 2005;10(1):4–13. [DOI] [PubMed] [Google Scholar]
- [25].Hansson EE. Vestibular rehabilitation – for whom and how? A systematic review. Adv Physiother. 2009;9(3):106–116. [Google Scholar]
- [26].Malfliet A, Kregel J, Cagnie B, et al. Lack of evidence for central sensitization in idiopathic, non-traumatic neck pain: a systematic review. Pain Physician. 2015;18(3):223–236. [PubMed] [Google Scholar]
- [27].Van Oosterwijck J, Nijs J, Meeus M, et al. Evidence for central sensitization in chronic whiplash: a systematic literature review. Eur J Pain. 2013;17(3):299–312. [DOI] [PubMed] [Google Scholar]
- [28].Chimenti RL, Frey-Law LA, Sluka KA. A mechanism-based approach to physical therapist management of pain. Phys Ther. 2018;98(5):302–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Treleaven J, Jull G, Grip H. Head eye co-ordination and gaze stability in subjects with persistent whiplash associated disorders. Manual ther. 2011;16(3):252–257. [DOI] [PubMed] [Google Scholar]
- [30].Huntley AH, Srbely JZ, Zettel JL. Experimentally induced central sensitization in the cervical spine evokes postural stiffening strategies in healthy young adults. Gait Posture. 2015;41(2):652–657. [DOI] [PubMed] [Google Scholar]
- [31].Higgins JPT TJ, Chandler J, Cumpston M, et al. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2022). Cochrane Database Syst Rev. 2021. Available from www.training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Ma LL, Wang YY, Yang ZH, et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- [35].Johnston BC, Patrick DL, Thorlund K, et al. Patient-reported outcomes in meta-analyses-part 2: methods for improving interpretability for decision-makers. Health Qual Life Outcomes. 2013;11(1):211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. Controlled Clinical Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- [37].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Jacobson GP, Newman CW. The development of the dizziness handicap inventory. arch otolaryngol head neck surg. Arch of Otolaryngology--head & Neck Surg. 1990;116(4):424–427. [DOI] [PubMed] [Google Scholar]
- [39].MacDowall A, Skeppholm M, Robinson Y, et al. Validation of the visual analog scale in the cervical spine. J Neurosurg Spine. 2018;28(3):227–235. [DOI] [PubMed] [Google Scholar]
- [40].Jorgensen R, Ris I, Juhl C, et al. Responsiveness of clinical tests for people with neck pain. BMC Musculoskelet Disord. 2017;18(1):548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336(7650):924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Ekvall Hansson E, Mansson NO, Ringsberg KA, et al. Dizziness among patients with whiplash-associated disorder: a randomized controlled trial. J Rehabil Med. 2006;38(6):387–390. [DOI] [PubMed] [Google Scholar]
- [43].Hansson EE, Persson L, Malmstrom EM. Influence of vestibular rehabilitation on neck pain and cervical range of motion among patients with whiplash-associated disorder: a randomized controlled trial. J Rehabil Med. 2013;45(9):906–910. [DOI] [PubMed] [Google Scholar]
- [44].Treleaven J, Peterson G, Ludvigsson ML, et al. Balance, dizziness and proprioception in patients with chronic whiplash associated disorders complaining of dizziness: a prospective randomized study comparing three exercise programs. Man Ther. 2016;22:122–130. [DOI] [PubMed] [Google Scholar]
- [45].Aydin T, Dernek B, Ege TS, et al. The effectiveness of dry needling and exercise therapy in patients with dizziness caused by cervical myofascial pain syndrome; prospective randomized clinical study. Pain Med. 2019;20(1):153–160. [DOI] [PubMed] [Google Scholar]
- [46].Carrasco-Uribarren A, Rodriguez-Sanz J, López-de-Celis C, et al. Short-term effects of the traction-manipulation protocol in dizziness intensity and disability in cervicogenic dizziness: a randomized controlled trial. Disabil Rehabil. 2021:1–9. [DOI] [PubMed] [Google Scholar]
- [47].Karlberg M, Magnusson M, Malmstrom EM, et al. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil. 1996;77(9):874–882. [DOI] [PubMed] [Google Scholar]
- [48].Micarelli A, Viziano A, Granito I, et al. Postural and clinical outcomes of sustained natural apophyseal glides treatment in cervicogenic dizziness patients: a randomised controlled trial. Clin Rehabil. 2021;35(11):1566-1576. [DOI] [PubMed] [Google Scholar]
- [49].Moustafa IM, Diab AA, Harrison DE. The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: a 1-year randomized controlled study. Eur J Phys Rehabil Med. 2017;53(1):57–71. [DOI] [PubMed] [Google Scholar]
- [50].Reid SA, Rivett DA, Katekar MG, et al. Sustained natural apophyseal glides (SNAGs) are an effective treatment for cervicogenic dizziness. Man Ther. 2008;13(4):357–366. [DOI] [PubMed] [Google Scholar]
- [51].Reid SA, Rivett DA, Katekar MG, et al. Comparison of mulligan sustained natural apophyseal glides and maitland mobilizations for treatment of cervicogenic dizziness: a randomized controlled trial. Phys Ther. 2014;94(4):466–476. [DOI] [PubMed] [Google Scholar]
- [52].Reid SA, Callister R, Katekar MG, et al. Effects of cervical spine manual therapy on range of motion, head repositioning, and balance in participants with cervicogenic dizziness: a randomized controlled trial. Arch Phys Med Rehabil. 2014;95(9):1603–1612. [DOI] [PubMed] [Google Scholar]
- [53].Reid SA, Callister R, Snodgrass SJ, et al. Manual therapy for cervicogenic dizziness: long-term outcomes of a randomised trial. Man Ther. 2015;20(1):148–156. [DOI] [PubMed] [Google Scholar]
- [54].Yao M, Tang ZY, Cui XJ, et al. Shi-style cervical mobilizations versus massage for cervical vertigo: a multicenter, randomized, controlled clinical trial. J Altern Complement Med. 2019;26(1):58–66. [DOI] [PubMed] [Google Scholar]
- [55].Micarelli A, Viziano A, Micarelli B, et al. Usefulness of postural sway spectral analysis in the diagnostic route and clinical integration of cervicogenic and vestibular sources of dizziness: a cross-sectional preliminary study. J vestibul res equilib orientat. 2021;31(5):353–364. [DOI] [PubMed] [Google Scholar]
- [56].Sjolander P, Michaelson P, Jaric S, et al. Sensorimotor disturbances in chronic neck pain–range of motion, peak velocity, smoothness of movement, and repositioning acuity. Man Ther. 2008;13(2):122–131. [DOI] [PubMed] [Google Scholar]
- [57].Rudolfsson T, Bjorklund M, Djupsjobacka M. Range of motion in the upper and lower cervical spine in people with chronic neck pain. Man Ther. 2012;17(1):53–59. [DOI] [PubMed] [Google Scholar]
- [58].Vogt L, Segieth C, Banzer W, et al. Movement behaviour in patients with chronic neck pain. Physiother Res Int. 2007;12(4):206–212. [DOI] [PubMed] [Google Scholar]
- [59].Treleaven J. Dizziness, unsteadiness, visual disturbances, and sensorimotor control in traumatic neck pain. J Orthop Sports Phys Ther. 2017;47(7):492–502. [DOI] [PubMed] [Google Scholar]
- [60].Treleaven J, Jull G, LowChoy N. The relationship of cervical joint position error to balance and eye movement disturbances in persistent whiplash. Man Ther. 2006;11(2):99–106. [DOI] [PubMed] [Google Scholar]
- [61].Saadat M, Salehi R, Negahban H, et al. Postural stability in patients with non-specific chronic neck pain: a comparative study with healthy people. Med J Islam Repub Iran. 2018;32(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Bialosky JE, Bishop MD, Price DD, et al. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Bishop MD, Torres-Cueco R, Gay CW, et al. What effect can manual therapy have on a patient’s pain experience? Pain Manag. 2015;5(6):455–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Southerst D, Nordin MC, Cote P, et al. Is exercise effective for the management of neck pain and associated disorders or whiplash-associated disorders? A systematic review by the ontario protocol for traffic injury management (optima) collaboration. Spine J. 2016;16(12):1503–1523. [DOI] [PubMed] [Google Scholar]
- [65].Michaleff ZA, Maher CG, Lin C-WC, et al. Comprehensive physiotherapy exercise programme or advice for chronic whiplash (PROMISE): a pragmatic randomised controlled trial. Lancet. 2014;384(9938):133–141. [DOI] [PubMed] [Google Scholar]
- [66].Söderlund A, Lindberg P. Cognitive behavioural components in physiotherapy management of chronic whiplash associated disorders (WAD)–a randomised group study. G Ital Med Lav Ergon. 2007;29(1 Suppl A):A5–11. [PubMed] [Google Scholar]
- [67].Ludvigsson ML, Peterson G, O'Leary S, et al. The effect of neck-specific exercise with, or without a behavioral approach, on pain, disability, and self-efficacy in chronic whiplash-associated disorders: a randomized clinical trial. Clin J Pain. 2015;31(4):294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Nijs J, Ickmans K. Chronic whiplash-associated disorders: to exercise or not? Lancet. 2014;384(9938):109–111. [DOI] [PubMed] [Google Scholar]
- [69].Han BI, Song HS, Kim JS. Vestibular rehabilitation therapy: review of indications, mechanisms, and key exercises. J Clin Neurol. 2011;7(4):184–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Akhter S, Khan M, Ali SS, et al. Role of manual therapy with exercise regime versus exercise regime alone in the management of non-specific chronic neck pain. Pak J Pharm Sci. 2014;27(6 Suppl):2125–2128. [PubMed] [Google Scholar]
- [71].Miller J, Gross A, D'Sylva J, et al. Manual therapy and exercise for neck pain: a systematic review. Manual ther. 2010;15(4):334–354. [PubMed] [Google Scholar]
- [72].Hidalgo B, Hall T, Bossert J, et al. The efficacy of manual therapy and exercise for treating non-specific neck pain: a systematic review. J Back Musculoskelet Rehabil. 2017;30(6):1149–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or are available as supplementary files.


