Abstract
The cerebral cortex forms early in development according to a series of heritable neurodevelopmental instructions. Despite deep evolutionary conservation of the cerebral cortex and its foundational six-layered architecture, significant variations in cortical size and folding can be found across mammals, including a disproportionate expansion of the prefrontal cortex in humans. Yet our mechanistic understanding of neurodevelopmental processes is derived overwhelmingly from rodent models, which fail to capture many human-enriched features of cortical development. With the advent of pluripotent stem cells and technologies for differentiating three-dimensional cultures of neural tissue in vitro, cerebral organoids have emerged as an experimental platform that recapitulates several hallmarks of human brain development. In this review, we discuss the merits and limitations of cerebral organoids as experimental models of the developing human brain. We highlight innovations in technology development that seek to increase its fidelity to brain development in vivo and discuss recent efforts to use cerebral organoids to study regeneration and brain evolution as well as to develop neurological and neuropsychiatric disease models.
Keywords: organoid
1. Pluripotent Stem Cells
Human tissues are frequently inaccessible to experimentation. In particular, long-term perturbational studies involving human cells resort to cell-based models. This is especially challenging for organs such as the brain, where limited or no stem cell populations can be robustly isolated and cultured in vitro. The isolation of mouse embryonic stem (ES) cells [1,2], the discovery of factors that enable propagation of undifferentiated stem cells in vitro [3], and the establishment of early protocols for neuronal differentiation [4] laid the scientific groundwork for utilizing stem cell-based models of nervous system development. Subsequent isolation of ES cell lines from human blastocysts [5], as well as the discovery of transcription factors that enable reprogramming of somatic cells to ‘induced’ pluripotent stem (iPS) cells [6,7], represent transformative advances that opened up immense opportunities for applying the approach to human cells (Figure 1a). Among early studies, optimized protocols for deriving human cortical cell lineage from embryonic stem cells using small molecules [8,9] and from induced pluripotent stem cells [10] have been instrumental in widespread adoption of the technology by the wider scientific community.
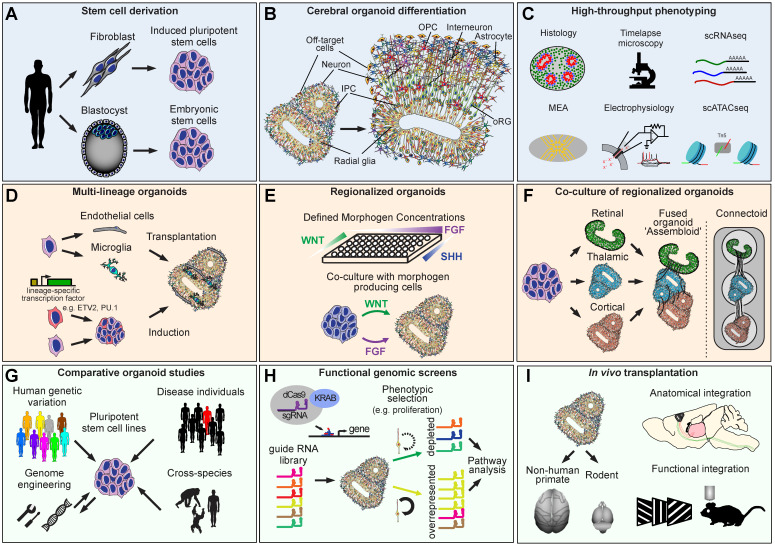
Figure 1.
Derivation, refinement, and applications of cerebral organoid technologies. (A) Pluripotent stem cells can be derived from embryonic material or somatic cells. (B) Cerebral organoids recapitulate key cell types of the developing brain. (C) Scalable organoid characterization technologies. (D) Multi-lineage organoids can be derived to recapitulate tissue cell type diversity more completely. (E) Improved regional specificity can be achieved by manipulating developmental signaling pathways according to the blueprint of normal developing tissue. (F) Interactions between brain regions can be modeled using co-cultured organoids. (G) Organoids derived from different sources of pluripotent stem cells can be used to compare developmental trajectories across individuals, species, or disease states. (H) Functional genomic screens can be used to map the genetic architecture of biological phenotypes relevant to neural development. (I) Combining organoids with animal models to advance future regenerative medicine applications.
2. Characterization
In parallel with the advances in stem cell differentiation into neuroectoderm in serum-free conditions using defined combinations of small molecules, a protocol for differentiating organoids as models of cortical development was introduced [11]. By culturing differentiating cells in three-dimensional aggregates, as opposed to two-dimensional cultures, neuroepithelial stem cells induced from pluripotent stem cells were allowed to self-organize and form clusters (rosettes), forming apical-like structures composed of tight and adherens junctions as well as apical cilia. These apical zone-like structures resemble the early developing cortical neuroepithelium with apico-basal polarity. Glutamatergic neurons emerging from these progenitors were capable of radial migration and formed axonal projections consistent with glutamatergic neuron identities after transplantation into immunocompromised mice [11].
The advent of human ES and iPS cells enabled the adoption of these three-dimensional culture protocols for human cells [12,13,14] (Figure 1b). In particular, the pioneering work of Lancaster et al. used a minimally guided differentiation strategy to generate cerebral organoid cultures that recapitulated many distinct brain regions, including dorsal cerebral cortex, ganglionic eminences (ventral cortex), midbrain, and hindbrain, within a single organoid [12]. In contrast to mouse ES cell-derived organoids [11], human stem cell-derived organoids developed a substantial population of outer radial glia (oRG) cells, which are a distinguishing feature of the mouse and human developing brains (discussed in the following section). In parallel, human ES cell differentiation using directed differentiation protocols demonstrated efficient induction of organoids containing only the dorsal cortical neural lineage [14].
Protocols for differentiating cortical organoids have been further refined, and cell types that emerge within brain organoids have been further characterized. For example, the emergence of cortical astrocytes has been demonstrated [13,15,16], as well as that of oligodendrocytes [17]. Neurons have been shown to develop functional synapses [13] and to organize into laminar patterns that resemble cortical layers [16].
More recently, by using multi-electrode arrays to measure spontaneous and evoked activity, organoids have been shown to be able to respond to light stimulation [18], and to develop complex oscillatory patterns of network behavior [19,20]. New engineering approaches are urgently needed to advance the capacity for performing longitudinal extracellular recordings from cultured organoids with minimal interference to their normal neurodevelopmental processes, and exciting solutions are currently being developed [21,22,23]. Integration of such systems with cloud-enabled infrastructure for data processing will be necessary to provide scalability of such methods and wide adoption by the scientific community [24].
Together, these studies have demonstrated a remarkable capacity of neural differentiations to self-organize, recapitulating many complex features of the developing brain, including cell type heterogeneity, cellular organization, and even cell-cell interactions necessary to enable complex patterns of neural activity to emerge (Figure 1b,c).
3. Benchmarking against Primary Tissue
Transcriptomic and epigenomic datasets generated from primary human tissue serve as an invaluable resource for benchmarking in vitro models. For example, brain organoids have been profiled using single cell transcriptomics and compared against microdissected bulk tissue transcriptomic data from developing human cerebral cortex, revealing that the molecular programs underlying human cortical neurogenesis are broadly expressed in cortical organoids [25]. This study also revealed that organoids contained primarily the dorsal telencephalic neural lineage with a small proportion of non-neural cells. Thanks to the generation of multiple single cell transcriptomic datasets from primary human tissue [26,27,28,29,30,31], it is now possible to compare cell types emerging in brain organoids to their primary counterparts in even greater detail. These studies have revealed that as development proceeds, cells from brain organoids fail to accurately recapitulate the full breadth of mature cell types and the associated diversity of specific patterns of gene expression found in primary tissue. Furthermore, organoid cells upregulate molecular signatures of cell stress [32,33]. Similar findings have been reported more broadly for in vitro cultured cells [31], including cultured human primary cells [33]. Recently developed bioinformatic approaches can be leveraged to regress stress signatures [34]. As new protocols and approaches are being developed to limit the effects of cell stress in culture conditions, single-cell transcriptomic studies will serve as an invaluable resource for comparing the fidelity and robustness of these protocols to the normal developing brain. Data sharing resources, such as the UCSC Cell Browser, have emerged to facilitate rapid data sharing and access, particularly for single cell RNA sequencing datasets whose processing steps have been largely standardized [35].
Similarly to transcriptomic analyses, epigenomic and epitranscriptomic (mRNA modifications) profiling have been applied to brain organoid and primary human tissue samples, which also revealed that broad neurodevelopmental trajectories and transitions are recapitulated in organoids sampled at different stages of differentiation [36,37,38,39]. Single cell epigenomic datasets from primary human tissue are only beginning to be generated [40,41]. Therefore systematic comparisons of epigenetic states between primary tissue and organoid cell types remain to be performed. Chromatin accessibility changes occurring during neurodevelopmental transitions have been shown to occur in brain organoids, and organoid-derived neural cells recapitulate a substantial fraction of the putative enhancers identified in developing human tissue [39,41].
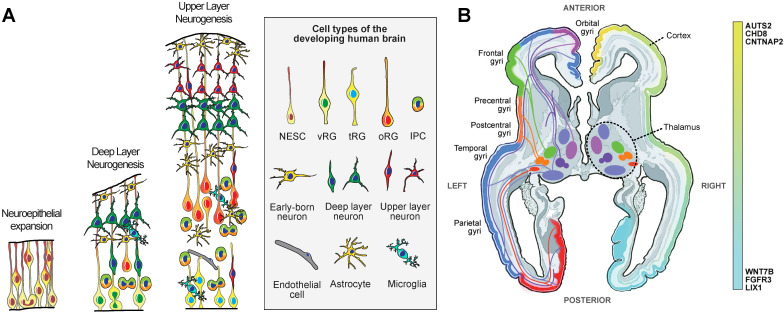
While transcriptomic and epigenomic data are tremendously valuable in that they enable genome-wide comparisons, they are unable to capture the dynamic neurodevelopmental processes that give rise to the complex cell types of the developing brain. Mechanistic studies of cortical development have been overwhelmingly conducted in mice. These studies have underscored the role of radial glia as the neural stem cells of the brain [42,43,44]. Radial glia are a specialized cell type that consists of a spindle-shaped cell body with bipolar morphology, including an apical fiber contacting the lateral ventricle and forming an apical junction, and a basal fiber extending to and contacting the pial surface [45] (Figure 2a). These cells have been shown to generate glutamatergic neurons directly [46,47] or indirectly via intermediate neural progenitor cells [48,49,50]. In the cerebral cortex, neurogenesis occurs within a specific time window [51] and in a temporally hierarchical order, with deep layer neurons generated before upper layer neurons [52]. During mouse cortical development, neurogenesis is followed by gliogenesis [44,48,53]. This series of neurodevelopmental events is often referenced as a template for cortical development across mammalian species.
Figure 2.
Development of the human brain. (A) Schematic representation of the key cellular populations during stages of peak neurogenesis and early gliogenesis in the human cerebral cortex. NESC—neuroepithelial stem cells, vRG—ventricular radial glia, tRG—truncated radial glia, oRG—outer radial glia, IPC-intermediate progenitor cells. (B) Development of the long-range connectivity between prospective subdivisions of the thalamus and cortical areas. The schematic shows a horizontal section through a developing human brain. The left half highlights major projection pathways between the emerging thalamic nuclei and cortical areas. The right half highlights differences in expression levels of specific genes with rostro-caudal expression gradients.
In many species outside mice, such as ferrets, macaques, and human developing cerebral cortex, radial glia extensively diversify into outer radial glia (‘oRG’, also referred to as ‘basal’ radial glia) in the outer subventricular zone (OSVZ) [54,55,56,57,58,59], and truncated radial glia [60,61] in the ventricular zone (VZ). At late stages of cortical development, the OSVZ harbors most of the proliferating cells in the developing cerebral cortex [54]. The discovery of molecular programs enriched in oRG cells [62,63] has identified mechanisms by which the development of these cell types can be promoted, and the hypothesis that LIF/STAT3 signaling can enhance oRG cell generation has been tested in organoids [64]. The role of this pathway was surprising, given the central role of this pathway in gliogenesis [65].
Importantly, oRG cells have been shown to give rise to oligodendrocyte progenitor cells (OPC) [66], although new studies suggest that other neural stem cell populations may generate OPCs at early developmental periods [67]. Astrocytes have been shown to be a major cellular output of oRG cells [68,69], but recent studies have revealed further complexity that exists within this cell class in both humans and mice [70,71,72,73], which underscores the need for further studies of their developmental cell lineage. Adding to this complexity, human glial progenitor cells have been shown to generate oligodendrocytes and astrocytes [74], and overlapping molecular signatures of the oligodendrocyte and astrocyte lineages have been identified in single cell studies [40,75,76].
Glutamatergic neurons of the cerebral cortex are generated by radial glia and IPCs during human development [54,55,56,57,58]. At late stages of cortical neurogenesis, oRG cells have been shown to generate neurons directly and indirectly [55]. Notably, periods of neurogenesis and gliogenesis in humans, as well as ferrets, overlap extensively [60,71], in contrast to mice [44,48,53]. Importantly, glutamatergic neurons that emerge in anatomically distinct areas of the cerebral cortex are molecularly divergent [27,30].
GABAergic neurons of the cerebral cortex originate in the ganglionic eminences [77,78,79,80,81]. However, a substantial fraction of progenitor cells and newly born neurons in the cerebral cortical wall at late stages of neurogenesis express markers of GABAergic lineage [28,82,83,84]. This presumed local production of cortical GABAergic neurons has been confirmed by a barcoded lineage tracing study of human cortical radial glia [79]. Notably, many studies utilizing cortical organoids have observed GABAergic neurons emerging at late stages of differentiation, but their origin and subtype identity remain unclear [32,85,86].
A deeper understanding of radial glia heterogeneity and differentiation trajectories in the human cerebral cortex will provide critical resources for benchmarking cerebral organoids as models of human neural development and may provide important insights into the cell of origin of brain tumors [87,88,89]. While many bioinformatic methods have been developed to reconstruct developmental trajectories from single cell transcriptomic data [90,91], they are limited in several important ways that may be important for our understanding of developmental processes [92]. Timelapse microscopy experiments in human and non-human primate tissue have provided critical insights into the complex patterns of progenitor cell behavior and differentiation trajectories in the developing brain [55,56,93,94]. These studies have revealed the neural stem cell potential of oRG cells [56], demonstrated evolutionary conservation of oRG cell behaviors [93], identified mechanisms underlying oRG cell generation [94], and revealed the remarkable neurogenic capacity of oRG cells, including their striking potential to give rise to neurons via direct neurogenesis in addition to their capacity to generate intermediate neural progenitors (‘indirect neurogenesis’) [55,62].
Timelapse microscopy studies conducted in cerebral organoids have demonstrated that the characteristic behaviors of radial glia subtypes are recapitulated in organoids [95,96], as well as their capacity to differentiate via direct and indirect neurogenesis [97]. In addition to timelapse microscopy, technologies that enable multiplexed tracking of cell lineage at high-throughput using single cell transcriptomics can be applied to cerebral organoids [98,99] and primary tissue [79,100,101]. Examining mechanisms underlying human brain development using brain organoids will critically depend on rigorous benchmarking of the differentiation trajectories of neural progenitor cells.
4. Protocol and Data Standards
Cerebral organoid protocols are being widely adopted to model human neurodevelopment, the consequences of genetic mutations, and in the context of evolutionary comparisons. In parallel, advanced methods are being developed to apply next-generation technologies to brain organoid culture. Publications describing detailed protocols as well as hands-on training workshops represent important steps towards developing protocol commons, as well as quality control standards that could be agreed upon by the scientific community to support the generation of interpretable data. One difference in experimental design that could lead to different experimental outcomes involves the choice of neural induction protocol. Some studies have relied on protocols that are more directed and involve dual smad inhibition [11,13,14], while other studies utilize minimally guided differentiations, which result in the generation of multiple lineages within the same organoid [12]. Depending on the nature of the assay (e.g., single cell transcriptomics or neural activity), the results of studies utilizing these divergent methods could require different interpretative frameworks.
Another important issue that is rarely discussed is the fact that lines from very few donors have thus far been utilized by most organoid studies. There is an unmet need to establish lines from donors that represent a more complete spectrum of human genetic diversity. Validation of their differentiation capacity using newly developed protocols that increase the reproducibility of cerebral organoid differentiations [85,102] will be key to advancing the field of organoid research. Equally important, datasets generated from cerebral organoids should ideally follow the principles of findability, accessibility, interoperability, and reusability (FAIR standards) [103]. Such datasets, together with platforms for data sharing, will be necessary to enable rigorous comparisons of experimental results from studies involving organoids. It is not unexpected that protocols and outcomes will vary depending on the research question being asked and the cell lines being used. However, benchmarking the data generated in cerebral organoid studies to both human primary tissue compendia and publically available cerebral organoid datasets, such as those in the UCSC Cell Browser, will go a long way towards establishing the relevance and utility of newly published cerebral organoid studies.
5. Reducing Stress
A pervasive cell culture-associated cell stress response has been identified as a potential confounding factor in organoid experiments [32,33]. Some of the potential consequences include genomic instability and the acquisition of somatic mutations in iPS derived models [104]. To overcome these limitations, algorithmic approaches have been developed to regress gene expression signatures related to cell stress [34]. While a variety of approaches are being examined, protocols that incorporate slicing of organoids or culture at the air-liquid interface [16,105] have shown a substantial reduction in the level of hypoxia within organoids. Moreover, incorporation of non-neuronal cells that do not emerge spontaneously in large numbers during neural differentiation may provide beneficial outcomes for organoid development. For example, microglia are the tissue-resident macrophages of the brain that arise in the yolk sac and are involved in innate immune and homeostatic functions [106]. Incorporation of microglia into organoids via transplantation or induction of the PU.1 transcription factor expression in a subset of organoid cells [107,108,109,110] (Figure 1d) has been shown to attenuate DNA damage responses in organoids and to promote the maturation of neuronal activity.
Similarly, most cell types that form the cerebrovasculature [111] do not arise from neural stem cells but can be introduced into organoids by co-culture [112,113,114] or by ectopic expression of the ETV2 transcription factor [115] (Figure 1d). Endothelial cells can self-organize to form tubular structures reminiscent of early developing vascular networks and can improve the viability of organoid cells and enhance functional maturation [115]. An important future direction involves developing vascular cell differentiation protocols that can more rapidly generate vascular cells at high purity [116], as well as those that more robustly resemble cerebrovascular endothelial cells as opposed to endothelial cells found in other organs [117].
Other cell types that are involved in cerebrovascular interactions, such as pericytes, smooth muscle cells, fibroblasts, fibromyocytes, or perivascular macrophages [111], remain to be explored. Incorporation of flow may be required to support successful vascularization of brain organoids and enable mechanistic studies of neurovascular interactions and disease modeling using organoids. Dysfunction of the cerebrovascular system is thought to be central to the pathophysiology of vascular malformations and neurodegeneration [118,119]. Therefore developing vascularized organoid models will be important for studies of these conditions using human cell-based models.
6. Multi-Brain Region Organoids
During development, neurons form local and long-range interactions with cells located in ontogenetically distinct regions (Figure 1e). While the initial differentiation protocols focused on accomplishing high efficiency differentiations for dorsal cortex organoids, protocols that enable other brain region specific differentiations have also emerged, including for ganglionic eminence [120,121,122], striatum [123], hippocampus [124], hypothalamus [86,125], pituitary gland [125,126], thalamus [127,128], midbrain [86,129,130,131], and cerebellum [132] organoids. Algorithms that enable data-driven alignment of organoids to a spatially resolved transcriptomic atlas of the developing brain can provide rapid validation of newly optimized differentiation protocols. Specifically, by leveraging spatially resolved gene expression data, such as the Allen Institute RNA in situ hybridization and laser capture microdissection microarray databases, the VoxHunt algorithm can annotate organoid single cell RNAseq data with brain regional identity information [133]. One limitation of this method is that the reference data currently available are not transcriptome-wide or single cell resolved. With the advent of brain region-resolved single cell or spatial datasets with single cell resolution, the accuracy of predicting regional identities of organoid cells will likely increase. Broader comparisons to not only brain tissue but also non-brain reference data will additionally enable fully agnostic, data-driven benchmarking of organoid cells against the blueprint of developing human tissue.
Physical co-culture of two or more brain region-specific organoids enables interactions between cells that emerge from different sets of progenitors to be studied in vitro. This approach is sometimes referred to as an ‘assembloid’ assay (Figure 1f), and allows for new neurodevelopmental processes to be assayed in vitro, such as the migration of GABAergic neurons from ventral telencephalic progenitors to the cortical plate [120,121,122]. Early developmental events involved in the formation of long-range neuronal tracts can also be examined, such as the cortico-striatal [123] or cortico-thalamic tracts [128]. In another exciting application, organoids co-cultured with non-neural tissue, such as muscle tissue [134,135], demonstrated the potential for organoid neurons to functionally innervate non-neural tissues, opening an exciting new frontier for regenerative medicine research (Figure 1g).
However, organoid fusions require parallel organoids to be differentiated into distinct regions, and in most cases, organoid fusion is not performed until these regional identities are fully acquired. As an alternative strategy, a growing number of studies are employing methodologies that deliver localized sources of developmental morphogens into parts of an organoid, such that they can mimic the effects of organizer regions that normally pattern the developing neuroepithelium. As a result, multiple brain regions can be simultaneously induced within the same organoid [136,137].
Another experimental approach that enables studies of neural interactions involves the separate induction of brain organoids that are cultured separately while allowing for neurons to form reciprocal axonal connections. These “connectoid” cultures have been shown to develop more complex neural activity profiles [138] than individually cultured organoids [20] (Figure 1f).
7. Specification of Cortical Neuron Subtypes
Cortical organoid differentiation protocols have been convincingly shown to generate cortical lineage neurons. However, the brain contains dozens of neuronal subtypes that ultimately give rise to its complex function. In this section, we will discuss broadly how the diversity of neurons in the mammalian forebrain is specified and how these are modeled using organoids.
Cortical neurons are specified along two major axes. First, their position in the six-layered cortical plate defines their morphology and connectivity. For example, “deep layer” neurons located in layers five and six send axons to subcortical areas, including the spinal cord and thalamus, respectively, whereas “upper layer” neurons of layers two, three, and four project to other cortical layers, to the contralateral hemisphere, or to the striatum [139]. The specification of cortical layer neurons follows a temporal, inside-out, order [52] and involves the induction of transcription factors that specify the major neuronal subtypes [140]. The sequential generation of deep and upper layer neurons is recapitulated in iPS derived cultures and cerebral organoids [8,10,141], although the stereotypical layering of cortical neurons has only been reported in a few studies [16].
The second axis follows the surface of the cerebral cortex, which can be divided into dozens of anatomically and functionally distinct areas, called aerial or regional identities. During early development, developmental morphogens secreted by organizer regions induce the expression of patterning transcription factors in radial glial cells, which subsequently give rise to glutamatergic neurons (reviewed by [142]). Different areas of the cerebral cortex have transcriptionally divergent glutamatergic neurons [27,30] (Figure 2b).
As an early application of the organoid technology, Sasai et al. demonstrated that cortical neuron differentiation can be further refined by harnessing lessons from developmental biology to increase regional specificity. In their experiments, inhibiting FGF signaling favored the specification of caudal cortical identities (NR2F2+ ve neurons), whereas activating Wnt and BMP signaling favored the specification of medial structures such as the cortical hem and choroid plexus [11]. Subsequently, these findings have been extended to form the basis for developing protocols for generating hippocampal organoids [86,124]. By modulating the duration of FGF signaling exposure during initial patterning, Studer et al. developed a protocol that promotes the specification of prefrontal cortical neurons [143].
Regulatory programs underlying cortical neuron specification and arealization have been extensively studied in mice [142]. Targeted knock-down of such master-regulatory transcription factors, such as GLI3, using CRISPR can be used to examine the effects of the manipulation on neuronal subtype specification [99] (Figure 1h), recapitulating the findings from mouse models [144].
Finally, epigenomic datasets generated from distinct areas of the cerebral cortex are beginning to emerge [41,145,146], and these studies have the potential to uncover regulatory programs underlying cortical arealization more comprehensively. For example, transcription factor motif enrichment analysis of prefrontal cortex enriched open chromatin regions identified retinoic acid receptor motif enrichment. Mechanistic studies of retinoic acid signaling have revealed a role for this pathway in the specification of the prefrontal cortex in the developing human brain and shown that modulation of retinoic acid signaling during organoid differentiation can regulate the differentiation of prefrontal and occipital cortical neurons in cerebral organoids [41,147]. Additional studies are needed to more comprehensively predict the regulatory grammar of cortical arealization which could be leveraged to derive next-generation protocols for generating area-specific cortical organoids.
8. Transplantation
One of the key applications of stem cell-based technologies is regenerative medicine. Pluripotent stem cell derived neurons have been successfully transplanted into neonatal immunocompromised mice and shown to develop projection patterns consistent with their molecular identities [11,148]. Moreover, transplanted human cells have been shown to integrate into mouse cortical circuits and develop evoked responses consistent with in situ neurons [149] (Figure 1i). The remarkable capacity of transplanted cells to integrate into the brain offers a promising outlook for future application of this approach in clinical settings. However, most transplantation paradigms are performed in the early postnatal period, when the majority of the mouse brain is still undergoing normal developmental processes. Transplantation into the adult brain is highly inefficient and rarely performed.
Several pioneering studies have successfully transplanted intact organoids into adult mouse brains [150,151,152,153]. These studies have shown that neurons within brain organoids continue to undergo normal developmental transitions, integrate into cortical tissue, and form functional synapses with mouse cells. Endogenous vascular cells of the mouse have been shown to progressively vascularize brain organoids.
In one study, organoids were transplanted into 3-year-old cynomolgus monkeys [152]. By 12 weeks post transplantation, axons of organoid neurons extended projections within the cortex, to the corpus callosum, and the striatum. No projections were found extending through the internal capsule, but this may be unsurprising given that the vast majority of neurons in the grafted organoids expressed SATB2, a marker of intratelencephalic neurons [154]. Future optimizations may be needed to develop protocols that could enhance the survival and integration of other neuronal subtypes into the monkey brain, including corticospinal and corticothalamic projection neurons.
While chimeric animal studies are necessary to understand the fidelity and function of in vitro derived human brain tissue and are a necessary first step for regenerative medicine approaches, they are not without controversy. Biomedical researchers, ethicists, and the public have questioned whether and when transplanting human neural tissue into experimental animals leads to human-like perception or cognition. Would chimeric animals modeling neuropsychiatric diseases potentially experience human disease symptoms in a distressing manner? The National Academies of Science, Engineering, and Medicine published a report on neural chimeric tissues in 2021 [155] that called out areas of concern with respect to this research, although it also stated that current regulation of stem cell and animal research was adequate. This issue continues to spur a lively debate in the research community that will only increase as brain organoids increase in their complexity and similarity to human brain tissue [156].
9. Disease Modeling
The discovery of reprogramming factors has allowed for the generation of pluripotent stem cells from patient cells, allowing for in vitro studies in a patient-specific genetic background. As a result, one of the most common applications of iPS technology today is disease modeling. Two early studies differentiated glutamatergic neurons from iPS lines derived from idiopathic schizophrenia [157] and Timothy Syndrome [158] patients. These studies heralded an era of disease modeling using human cell-based models [159]. The results of these studies have been extensively discussed in a number of recent reviews [160], and will not be further discussed in this review.
In addition to patient-derived cells, genome engineering technologies using CRISPR have also enabled the generation of ‘isogenic’ iPS lines where a putative disease-causing variant can be introduced into control iPS lines or corrected in a patient iPS line. This approach offers tremendous potential for screening large numbers of candidate mutations as well as for assessing the role of genetic background in specific disease-associated variants. However, rigorous validation of isogenic iPS lines will be necessary because non-specific ‘passenger’ mutations are frequently introduced during clonal selection of isogenic lines [161].
9.1. Neurological Disorders
Cerebral organoids generated from patient-derived iPS lines have also been applied to studies of disease mechanisms. For example, organoids derived from an iPS line derived from a patient with compound heterozygous truncating mutations in CDK5RAP2 have been shown to exhibit slower growth kinetics compared to control iPS lines [12]. This study also identified precocious differentiation and alterations in the cell division plane of radial glia that likely underlie the microcephaly phenotype. This study was, to the best of our knowledge, the first application of cerebral organoids to disease modeling.
The advent of new technologies, such as single cell barcoding and CRISPR perturbation screening, has enabled parallel and multiplexed perturbations of genes in cerebral organoids. Esk et al. applied this approach to study the effects of loss of function of 173 candidate microcephaly genes [98]. This study has revealed a novel role for genes involved in endoplasmic reticulum (ER) function as a point of vulnerability in microcephaly.
Mechanisms underlying microcephaly have been successfully studied using mouse models thanks to the conservation of many biochemical processes of cell division. By contrast, lissencephaly is a condition inherently difficult to model in mice due to the lissencephalic nature of the mouse cerebral cortex. LIS1 (encoded by PAFAH1B1) encodes one of the five genes implicated in primary lissencephaly in humans [162]. Studies in mice have found subtle neurodevelopmental phenotypes in transgenic mice with Lis1 loss of function, including neuronal migration and neurite extension deficits [163,164]. By contrast, introduction of LIS1 loss of function mutations into human ES cell lines using CRISPR, followed by differentiation into cerebral organoids, was sufficient to detect a striking difference in neuroepithelial stem cell and radial glia proliferation [165], suggesting that, in humans, LIS1 could play an important role beyond the control of neuronal migration that was discovered using a mouse model.
Miller-Dieker Syndrome is characterized by lissencephaly but also microcephaly, and organoids derived from patients with this condition show a number of distinct phenotypes impacting the survival of neuroepithelial cells, outer radial glia cell division, and neuronal migration [95]. Notably, Miller-Dieker Syndrome patients carry mutations in PAFAH1B1 in addition to other genes, highlighting the need for isogenic lines for dissecting the contribution of individual genes to distinct phenotypes.
Tuberous sclerosis is a rare condition that involves the formation of many non-cancerous tumors throughout the body. Tuberous sclerosis patients often develop epileptic seizures [166], and two high-confidence risk genes, TSC1 and TSC2, have been identified [167,168]. Both TSC1 and TSC2 act as negative regulators of the mammalian target of rapamycin gene (mTOR) in mammalian cells [169]. In the brain, mTOR signaling has been shown to be a major regulator of synaptic function, and its inhibition has been shown to rescue synaptic phenotypes in tuberous sclerosis [170]. However, mTOR signaling also plays a significant role in brain development. In humans, mTOR signaling is highly enriched in oRG cells [27] and regulates radial glia fiber maintenance [171]. By contrast, the radial glia of the developing mouse brain are less dependent on mTOR signaling [172] and do not develop tubers, arguing for the development of a human cell-based model of tuberous sclerosis. Organoids derived from human ES cell lines with TCS1 and TSC2 mutations have been shown to have precocious gliogenesis that can be rescued by rapamycin inhibition [173].
Another study used cerebral organoids to investigate neurodevelopmental phenotypes underlying periventricular heterotopia by generating mutations in DCHS1 and FAT4. Radial glia deficient for these proteins showed severe disorganization of radial morphology and neuronal migration defects, as well as possible defects in neuronal fate specification [174].
9.2. Psychiatric Conditions
Perhaps the most aspirational application of brain organoids is in studies of psychiatric disorders, where iPS-derived organoids allow researchers to study human neurodevelopmental processes in the human genetic background. This may be especially important in conditions such as schizophrenia or autism spectrum disorders (ASD), which involve the contribution of many genetic variants. Polygenic risk architecture may be difficult to capture in animal models.
Starting from syndromic disorders that include nervous system alterations, iPS cells derived from patients with Timothy syndrome have been used to identify neural deficits associated with the condition [158], including calcium signaling defects in progenitors and neurons. More recently, assembloids derived from cortical and ganglionic eminence organoids have been used to show that tangentially migrating interneurons exhibit abnormal patterns of neuronal migration in Timothy syndrome and can be rescued by inhibiting GABA-A receptor signaling [120,175].
Several studies utilized pluripotent stem cells derived from patients with DiGeorge syndrome, which is caused by a microdeletion at the 22q11.2 locus. Cortical differentiations of these lines have been shown to result in precocious gliogenesis [176] and a delayed switch of the GABA reversal potential [177]. In addition, mitochondrial defects have been identified [178]. Cortical organoids derived from 22q11.2 microdeletion patients have been shown to exhibit neuronal hyperexcitability that could be rescued by restoring the expression of DGCR8 [179], an enzyme critical to the synthesis of microRNAs [180].
MECP2 encodes a CpG binding protein and is mutated in patients with Rett syndrome [181,182]. Rett syndrome patient-derived iPS cells differentiated into cortical glutamatergic neurons have been shown to develop reduced synaptic arbors, a phenotype that could be rescued by overexpression of MECP2 as well as the addition of IGF1 based on findings from a mouse model [183,184]. Inhibition of ribosomal proofreading activity using gentimicin was also suggested to elevate MeCP2 expression, but the effect was highly sensitive to drug concentration [184]. A subsequent study using brain organoids further revealed neuronal network activity phenotypes that could be attenuated using Nefiracetam and PHA 543,613 [185]. Fused cortical and ganglion eminence organoids derived from stem cell lines carrying loss of function mutations in MECP2 have been shown to exhibit abnormal patterns of oscillatory network activity that can be partially rescued by Pifithrin-α, a TP53 inhibitor [186], consistent with studies in patient derived fibroblasts showing increased induction of P53 and senescence [187]. These studies illustrate the complexity of neurodevelopmental processes regulated by MeCP2 and suggest that MeCP2 loss of function consequences may be mediated by many biological processes and do not converge upon a small number of biochemical targets.
Studies of ASD pathobiology have attracted substantial interest in the scientific community due to the complex nature of this early-onset condition. Human genetics studies have implicated hundreds of genetic variants that might underlie ASD [188,189,190]. The genetic architecture of ASD involves rare as well as common variants and following the discovery of high-confidence ASD risk loci comes the challenge of understanding their function.
Copy number variants in the 16p11.2 locus are strongly associated with ASD diagnosis [191,192]. Studies investigating neurodevelopmental phenotypes using two-dimensional cultures of patient-derived cells identified several phenotypes associated with 16p11.2 microdeletion [193]. Neurons derived from cells with 16p11.2 deletion showed enlarged cell soma and deficits in synaptic morphology. In addition, a study of cortical organoids derived from 16p11.2 microdeletion patients revealed deficits in neuronal migration, and deficits in Wnt signaling pathway activation, and a reduced pool of neural progenitor cells [194]. Additionally, a recent study measuring gene expression in 16p11.2 microdeletion organoids derived from 13 donors implicates neural progenitor cells in early developmental changes and suggests transcriptional dysregulation through gene coexpression network analysis [195].
High-confidence ASD risk genes discovered through whole exome sequencing studies coalesce into several categories, including gene expression regulation and synaptic transmission. Understanding the points of convergence between them that might underlie the highly stereotypical nature of ASD symptoms remains challenging. However, early analyses have uncovered brain regions and developmental time points that are enriched for ASD risk gene expression. Specifically, by intersecting ASD candidate risk genes with gene expression information from the developing human brain [196], two studies identified enriched expression of ASD risk genes in prenatally developing human prefrontal cortex [197,198]. Intersection of these genes with single cell expression data from the human brain [27,29] has further shown that many ASD risk genes show enriched expression in glutamatergic and gabaergic neurons [188,190]. Classical annotations of protein function are often based on studies in cell lines and animal models. This can inaccurately capture the complex roles of these proteins across the wide spectrum of cells in the human brain. Moreover, assumptions that expression level correlates with functional significance can be misleading. For example, the vast majority of studies into the role of the ASD risk gene SynGAP1 have been focused on the role of this protein in synaptic transmission [199]. Indeed, in the developing human brain, SYNGAP1 mRNA is enriched in glutamatergic neurons, but its expression can also be detected in radial glia [27]. Emerging evidence from cerebral organoids suggests that SynGAP1 may also play a role in radial glia during early neurogenesis [200]. This finding highlights the need to systematically interrogate gene function across the range of cell types where risk genes are expressed.
In an effort to systematically screen high-confidence ASD risk genes for their function in neurodevelopment, several studies have begun to interrogate neurodevelopmental phenotypes for multiple genes in parallel, using iPS-derived neurons and cerebral organoids.
Cederquist et al. generated isogenic pluripotent stem cell lines carrying loss of function mutations for 27 high confidence ASD risk genes and differentiated the cells in a pooled assay to glutamatergic neurons of the prefrontal cortex [143]. Loss of function mutations in CUL3, KDM5B, ASH1L, ASXL3, ANKRD11, RELN, DEAF1, and KMT2C resulted in decreased neurogenesis. Mutations in KMT2A, SUV420H1, DYRK1A, GRIN2B, and CHD8 resulted in proportionately increased numbers of newborn neurons at the expense of progenitors.
Lalli et al. investigated progenitor cell proliferation and neuronal differentiation phenotypes across 13 high-confidence ASD risk genes using a pooled CRISPR screen approach in neural progenitor cells [201]. This study found that out of the 13 ASD risk genes investigated, knock-down of five genes (CHD2, ARID1B, ADNP, ASH1L, and DYRK1A) resulted in reduced proliferation, while knock-down of two genes (PTEN and CHD8) led to accelerated maturation and increased proliferation. Four genes (ASH1L, ADNP, ARID1B, and DYRK1A) resulted in reduced neurite extension, while one gene (PTEN) led to increased neurite extension in cortical neurons.
An organoid-based study investigated the neurodevelopmental consequences of SUV420H1 (also known as KMT5B), ARID1B, and CHD8 loss of function using comprehensive single cell RNA sequencing analysis. In this study, heterochrony of neuronal maturation and excessive production of GABAergic versus glutamatergic neurons were observed [202]. Transcriptional changes between mutant and control cells were found to be more consistent across cell types within candidate mutations (especially for ARID1B and CHD8) than across candidate genes. A parallel study using CHD8 isogenic mutant cerebral organoids reported alterations in the proliferative capacity of progenitor cells, with prolonged proliferation of mutant cells [203].
Together, these studies suggest that loss of function mutations of at least a subset of high-confidence ASD risk genes disrupt radial glia proliferation or neuronal differentiation. This is consistent with clinical reports suggesting that patients with ASD can have either increased or decreased head circumference relative to the general population [204]. However, while functional genomic information may support patient stratification, the results of these studies do not offer a simple answer to the question of phenotype convergence across diverse risk genes.
Complementing the studies of rare risk variants, organoids derived from idiopathic ASD patients have identified phenotypes of increased abundance of cortical interneurons [205,206] in addition to alterations of cortical progenitor cell proliferation. These findings appear to be consistent with the recent study in organoids with SUV420H1, ARID1B, and CHD8 mutations [202]. Follow-up studies are beginning to further investigate this question using iPS lines derived from idiopathic ASD individuals who were either normocephalic or macrocephalic [207]. Phenotypic differences in progenitor cell development, neurogenesis, and neuronal differentiation between donors stratified according to macrocephaly status may provide important insights into neurodevelopmental phenotypes underlying patient phenotypes.
Additional studies are needed to investigate the consequences of ASD risk gene mutations on additional neurodevelopmental phenotypes, including cell behavior, epigenetics, neurophysiology, synaptogenesis, cell dynamics, gliogenesis, and connectivity. Progress in addressing these questions will require advances in culture methods that promote neuronal maturation [208,209], scalable methods combining multiplexed perturbation strategies with increasingly complex phenotypes, such as pooled optical CRISPR screens [210], or perturb-ATAC [211]. Moreover, it will be important to apply these strategies across a wide range of cell types, not limited to a specific brain region or even just the neural lineage. The advent of quantitative frameworks that can take advantage of sparse datasets to learn latent representations of biological phenotypes will be critical to interpreting the results of such experiments [212,213].
One of the general themes that has emerged thus far from organoid-based modeling of neurodevelopmental phenotypes associated with psychiatric variants is that such mutations frequently lead to aberrant timing of neurodevelopmental events. Such heterochronicity could lead to disorganized development of neural circuits, likely leading to functional abnormalities. Given the inherent variability of cerebral organoid differentiations as well as the current inability to precisely control many neurodevelopmental processes, such as the positional identity of radial glia, insights gained from organoids should be carefully validated to determine their predictive value.
However, validating early neurodevelopmental phenotypes in human tissue can be challenging due to the limited availability of suitable research material. Still, insights gained from brain organoids can and should lead to predicted consequences in brain structure or function. Functional imaging studies that have been performed in patients with psychiatric conditions can serve as a point of reference [214]. Similarly, studies of postmortem tissue derived from patients with autism or schizophrenia have provided insights into molecular and cellular changes associated with these conditions [215,216,217,218,219]. Even though postmortem tissue likely involves additional changes related to co-morbidities and drug treatments, one would expect some degree of overlap between primary tissue and organoid models, especially where the comparison is performed between samples with the same mutation. Finally, comparisons to animal models can be extremely useful in identifying robust phenotypes and can serve as a guiding principle for the use of such models in preclinical studies [220,221].
9.3. Neurodegeneration
Another area of growing interest is the application of organoid technology to interrogate mechanisms underlying neurodegenerative phenotypes. Neurodegenerative disorders involve many genetic and non-genetic risk factors and are thought to involve dysfunction of homeostatic mechanisms involving not only neurons but also non-neuronal cells. Four major disease areas are being actively studied: Parkinson’s disease, Huntington’s disease, Alzheimer’s disease, and Down syndrome.
Multiple studies have leveraged patient derived iPS cells to recapitulate deficits in neuronal survival as well as abnormalities in biochemical processes relevant to these conditions [31,222,223,224,225,226]. For an in-depth review, see [227].
Cerebral organoids have also been applied to the study of neuronal phenotypes associated with neurodegeneration. Organoids derived from patients with familial Alzheimer’s disease as well as Down syndrome have been shown to recapitulate toxic accumulation of the Ab fragment of the amyloid precursor protein [228,229]. Disruption of nuclear architecture of progenitor cells has been observed [230]. The advent of CRISPR interference technology, which enables flexible targeting of genes upregulated in disease states [231,232,233], can be applied to target and limit abnormal activation of pathways discovered using in vitro models [234].
In an excellent demonstration of organoid technology for disease modeling, a recent study modeled neuronal phenotypes using iPS lines carrying MAPT mutations that underlie frontotemporal dementia [235]. Extensive biochemical, morphological, and transcriptomic characterization identified accelerated neuronal maturation and upregulation of synaptic genes as a key feature associated with MAPT mutations. ELAVL4, a splicing factor involved in neuronal maturation, was identified as a core master-regulatory gene upregulated in mutant cells, leading to transcriptome-wide changes in splicing and changes to synaptic recycling rates. This could be reversed by inhibition of PIKFYVE, a lipid kinase that regulates endolysosomal trafficking, consistent with findings in a mouse model of C9ORF72 hexanucleotide repeat expansion that underlies both frontotemporal dementia and amyotrophic lateral sclerosis [236].
10. Evolutionary Insights
The mammalian neocortex is a highly evolved structure, but even across mammals it shows substantial variation in size, cellular organization, and folding pattern [237]. Many hypotheses have been put forward about the developmental mechanisms that might underlie these differences across species [238,239,240,241,242,243,244]. Of particular interest are those changes that might underlie the remarkable adaptations of the human brain to higher cognition, but for practical reasons, many studies have thus far focused on the analysis of progenitor cell proliferation, which might underlie the disproportionate evolutionary expansion of the human cerebral cortex.
Three prominent hypotheses have been promoted to account for the expansion of the neocortex. One, changes to the proliferative expansion of the neuroepithelial stem cells, which serve as the founder population of cortical radial glia [245]. Two, a reduction in programmed apoptotic cell death of neuroepithelial or radial glial cells [246]. Three, the expansion of the secondary proliferative populations in the outer subventricular zone [54,238,247] is driven by changes in gene expression or activity-dependent processes [248].
Cerebral organoids have the potential to serve as an experimental platform for establishing causality between genetic changes between species and specific neuro-developmental or neurophysiological phenotypes. Two main approaches have emerged so far in the field.
The first approach has been to use organoids to study the function of genetic variants that have been identified as derived from the human lineage [249,250,251,252]. Two examples of variants include NOTCH2NL and NOVA1. NOTCH2NL has been shown to control the production and proliferation of radial glia cells [253,254]. The archaic allele of NOVA1 has been shown to increase progenitor cell apoptosis [255]. Both of these mechanisms are consistent with the prevailing hypotheses about human brain expansion.
The second approach has been to derive brain organoids from multiple species. Thanks to the discovery of somatic reprogramming factors, it is possible to derive brain organoids from many species, including great apes [256,257,258,259]. By comparing organoid differentiations from human and chimpanzee, Mora-Bermudez et al. identified differences in cell cycle kinetics between species [260] and identified candidate modern human-specific causative mutations [261]. Pollen et al. demonstrated that organoids derived from non-human primates recapitulate cross-species gene expression differences observed in primary tissue and identified changes in mTOR signaling pathway activation [32]. Benito-Kwiecinski reported differences in neuroepithelial stem cell proliferation [262]. In addition, Kanton et al. captured transcriptomic and epigenomic differences in developmental trajectories in human and chimpanzee organoids, including changes that overlap with human accelerated regions, and confirmed at least a subset of these molecular differences in primary human and non-human primate prefrontal cortex tissue [263].
Organoids derived from tetrapoid iPS cells generated by fusing cells from different species provide another avenue for interrogating cis- and trans-regulatory programs for transcriptional divergence between species [264]. As an example, cortical organoids derived from human-chimpanzee tetraploid iPS cells showed accelerated expression of gliogenic programs and increased expression of human somatostatin receptor 2. Differential expression of these pathways between humans and chimpanzees represents yet another candidate pathway that may have contributed to the evolutionary expansion of the human cerebral cortex.
11. Conclusions
In the last two decades, pluripotent stem cell-derived brain organoids have advanced from a novel finding to the premier research tool for studying human brain development and disease. These models are utilized by hundreds of researchers. Many challenges remain to improve the fidelity of organoids relative to in vivo tissues and to expand the features of brain development and function that can be effectively studied in these cell culture models. However, there is tremendous enthusiasm to tackle these issues, as outlined in the research reviewed here. In vitro differentiation of human pluripotent stem cells to cerebral organoids offers a tremendous opportunity to understand human neurodevelopment, identify the consequences of disease-relevant mutations, and begin to develop strategies to advance regenerative medicine applications.
Acknowledgments
The authors wish to thank Alex Pollen for critical feedback on the manuscript.
Author Contributions
Writing—S.R.S. and T.J.N. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by NIH awards R01MH120295, 1RM1HG011543, NSF 2134955 (to S.R.S.), R01NS123263, U01MH115747 and gift from the William K. Bowes Jr. Foundation (to T.J.N.) and Schmidt Futures Foundation SF857 (to S.R.S and T.J.N.).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Evans M.J., Kaufman M.H. Establishment in Culture of Pluripotential Cells from Mouse Embryos. Nature. 1981;292:154–156. doi: 10.1038/292154a0. [DOI] [PubMed] [Google Scholar]
- 2.Martin G.R. Isolation of a Pluripotent Cell Line from Early Mouse Embryos Cultured in Medium Conditioned by Teratocarcinoma Stem Cells. Proc. Natl. Acad. Sci. USA. 1981;78:7634–7638. doi: 10.1073/pnas.78.12.7634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith A.G., Heath J.K., Donaldson D.D., Wong G.G., Moreau J., Stahl M., Rogers D. Inhibition of Pluripotential Embryonic Stem Cell Differentiation by Purified Polypeptides. Nature. 1988;336:688–690. doi: 10.1038/336688a0. [DOI] [PubMed] [Google Scholar]
- 4.Jones-Villeneuve E.M., McBurney M.W., Rogers K.A., Kalnins V.I. Retinoic Acid Induces Embryonal Carcinoma Cells to Differentiate into Neurons and Glial Cells. J. Cell Biol. 1982;94:253–262. doi: 10.1083/jcb.94.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomson J.A., Itskovitz-Eldor J., Shapiro S.S., Waknitz M.A., Swiergiel J.J., Marshall V.S., Jones J.M. Embryonic Stem Cell Lines Derived from Human Blastocysts. Science. 1998;282:1145–1147. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 6.Takahashi K., Yamanaka S. Induction of Pluripotent Stem Cells from Mouse Embryonic and Adult Fibroblast Cultures by Defined Factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 7.Park I.-H., Zhao R., West J.A., Yabuuchi A., Huo H., Ince T.A., Lerou P.H., Lensch M.W., Daley G.Q. Reprogramming of Human Somatic Cells to Pluripotency with Defined Factors. Nature. 2008;451:141–146. doi: 10.1038/nature06534. [DOI] [PubMed] [Google Scholar]
- 8.Chambers S.M., Fasano C.A., Papapetrou E.P., Tomishima M., Sadelain M., Studer L. Highly Efficient Neural Conversion of Human ES and iPS Cells by Dual Inhibition of SMAD Signaling. Nat. Biotechnol. 2009;27:275–280. doi: 10.1038/nbt.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Watanabe K., Kamiya D., Nishiyama A., Katayama T., Nozaki S., Kawasaki H., Watanabe Y., Mizuseki K., Sasai Y. Directed Differentiation of Telencephalic Precursors from Embryonic Stem Cells. Nat. Neurosci. 2005;8:288–296. doi: 10.1038/nn1402. [DOI] [PubMed] [Google Scholar]
- 10.Shi Y., Kirwan P., Smith J., Robinson H.P.C., Livesey F.J. Human Cerebral Cortex Development from Pluripotent Stem Cells to Functional Excitatory Synapses. Nat. Neurosci. 2012;15:477–486, S1. doi: 10.1038/nn.3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eiraku M., Watanabe K., Matsuo-Takasaki M., Kawada M., Yonemura S., Matsumura M., Wataya T., Nishiyama A., Muguruma K., Sasai Y. Self-Organized Formation of Polarized Cortical Tissues from ESCs and Its Active Manipulation by Extrinsic Signals. Cell Stem Cell. 2008;3:519–532. doi: 10.1016/j.stem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Lancaster M.A., Renner M., Martin C.-A., Wenzel D., Bicknell L.S., Hurles M.E., Homfray T., Penninger J.M., Jackson A.P., Knoblich J.A. Cerebral Organoids Model Human Brain Development and Microcephaly. Nature. 2013;501:373–379. doi: 10.1038/nature12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paşca A.M., Sloan S.A., Clarke L.E., Tian Y., Makinson C.D., Huber N., Kim C.H., Park J.-Y., O’Rourke N.A., Nguyen K.D., et al. Functional Cortical Neurons and Astrocytes from Human Pluripotent Stem Cells in 3D Culture. Nat. Methods. 2015;12:671–678. doi: 10.1038/nmeth.3415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kadoshima T., Sakaguchi H., Nakano T., Soen M., Ando S., Eiraku M., Sasai Y. Self-Organization of Axial Polarity, inside-out Layer Pattern, and Species-Specific Progenitor Dynamics in Human ES Cell-Derived Neocortex. Proc. Natl. Acad. Sci. USA. 2013;110:20284–20289. doi: 10.1073/pnas.1315710110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sloan S.A., Darmanis S., Huber N., Khan T.A., Birey F., Caneda C., Reimer R., Quake S.R., Barres B.A., Paşca S.P. Human Astrocyte Maturation Captured in 3D Cerebral Cortical Spheroids Derived from Pluripotent Stem Cells. Neuron. 2017;95:779–790.e6. doi: 10.1016/j.neuron.2017.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qian X., Su Y., Adam C.D., Deutschmann A.U., Pather S.R., Goldberg E.M., Su K., Li S., Lu L., Jacob F., et al. Sliced Human Cortical Organoids for Modeling Distinct Cortical Layer Formation. Cell Stem Cell. 2020;26:766–781.e9. doi: 10.1016/j.stem.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marton R.M., Miura Y., Sloan S.A., Li Q., Revah O., Levy R.J., Huguenard J.R., Pașca S.P. Differentiation and Maturation of Oligodendrocytes in Human Three-Dimensional Neural Cultures. Nat. Neurosci. 2019;22:484–491. doi: 10.1038/s41593-018-0316-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quadrato G., Nguyen T., Macosko E.Z., Sherwood J.L., Min Yang S., Berger D.R., Maria N., Scholvin J., Goldman M., Kinney J.P., et al. Cell Diversity and Network Dynamics in Photosensitive Human Brain Organoids. Nature. 2017;545:48–53. doi: 10.1038/nature22047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharf T., van der Molen T., Glasauer S.M.K., Guzman E., Buccino A.P., Luna G., Cheng Z., Audouard M., Ranasinghe K.G., Kudo K., et al. Functional Neuronal Circuitry and Oscillatory Dynamics in Human Brain Organoids. Nat. Commun. 2022;13:4403. doi: 10.1038/s41467-022-32115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trujillo C.A., Gao R., Negraes P.D., Gu J., Buchanan J., Preissl S., Wang A., Wu W., Haddad G.G., Chaim I.A., et al. Complex Oscillatory Waves Emerging from Cortical Organoids Model Early Human Brain Network Development. Cell Stem Cell. 2019;25:558–569.e7. doi: 10.1016/j.stem.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park Y., Franz C.K., Ryu H., Luan H., Cotton K.Y., Kim J.U., Chung T.S., Zhao S., Vazquez-Guardado A., Yang D.S., et al. Three-Dimensional, Multifunctional Neural Interfaces for Cortical Spheroids and Engineered Assembloids. Sci. Adv. 2021;7:eabf9153. doi: 10.1126/sciadv.abf9153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Floch P., Li Q., Lin Z., Zhao S., Liu R., Tasnim K., Jiang H., Liu J. Stretchable Mesh Nanoelectronics for 3D Single-Cell Chronic Electrophysiology from Developing Brain Organoids. Adv. Mater. 2022;34:e2106829. doi: 10.1002/adma.202106829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonald M., Sebinger D., Brauns L., Gonzalez-Cano L., Menuchin-Lasowski Y., Mierzejewski M., Psathaki O.-E., Stumpf A., Wickham J., Rauen T., et al. A Mesh Microelectrode Array for Non-Invasive Electrophysiology within Neural Organoids. bioRxiv. 2021 doi: 10.1016/j.bios.2023.115223. bioRxiv:2020.09.02.279125. [DOI] [PubMed] [Google Scholar]
- 24.Voitiuk K., Geng J., Keefe M.G., Parks D.F., Sanso S.E., Hawthorne N., Freeman D.B., Currie R., Mostajo-Radji M.A., Pollen A.A., et al. Light-Weight Electrophysiology Hardware and Software Platform for Cloud-Based Neural Recording Experiments. J. Neural Eng. 2021;18:066004. doi: 10.1088/1741-2552/ac310a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Camp J.G., Badsha F., Florio M., Kanton S., Gerber T., Wilsch-Bräuninger M., Lewitus E., Sykes A., Hevers W., Lancaster M., et al. Human Cerebral Organoids Recapitulate Gene Expression Programs of Fetal Neocortex Development. Proc. Natl. Acad. Sci. USA. 2015;112:15672–15677. doi: 10.1073/pnas.1520760112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pollen A.A., Nowakowski T.J., Shuga J., Wang X., Leyrat A.A., Lui J.H., Li N., Szpankowski L., Fowler B., Chen P., et al. Low-Coverage Single-Cell mRNA Sequencing Reveals Cellular Heterogeneity and Activated Signaling Pathways in Developing Cerebral Cortex. Nat. Biotechnol. 2014;32:1053–1058. doi: 10.1038/nbt.2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nowakowski T.J., Bhaduri A., Pollen A.A., Alvarado B., Mostajo-Radji M.A., Di Lullo E., Haeussler M., Sandoval-Espinosa C., Liu S.J., Velmeshev D., et al. Spatiotemporal Gene Expression Trajectories Reveal Developmental Hierarchies of the Human Cortex. Science. 2017;358:1318–1323. doi: 10.1126/science.aap8809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhong S., Zhang S., Fan X., Wu Q., Yan L., Dong J., Zhang H., Li L., Sun L., Pan N., et al. A Single-Cell RNA-Seq Survey of the Developmental Landscape of the Human Prefrontal Cortex. Nature. 2018;555:524–528. doi: 10.1038/nature25980. [DOI] [PubMed] [Google Scholar]
- 29.Polioudakis D., de la Torre-Ubieta L., Langerman J., Elkins A.G., Shi X., Stein J.L., Vuong C.K., Nichterwitz S., Gevorgian M., Opland C.K., et al. A Single-Cell Transcriptomic Atlas of Human Neocortical Development during Mid-Gestation. Neuron. 2019;103:785–801.e8. doi: 10.1016/j.neuron.2019.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhaduri A., Sandoval-Espinosa C., Otero-Garcia M., Oh I., Yin R., Eze U.C., Nowakowski T.J., Kriegstein A.R. An Atlas of Cortical Arealization Identifies Dynamic Molecular Signatures. Nature. 2021;598:200–204. doi: 10.1038/s41586-021-03910-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.La Manno G., Gyllborg D., Codeluppi S., Nishimura K., Salto C., Zeisel A., Borm L.E., Stott S.R.W., Toledo E.M., Villaescusa J.C., et al. Molecular Diversity of Midbrain Development in Mouse, Human, and Stem Cells. Cell. 2016;167:566–580.e19. doi: 10.1016/j.cell.2016.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pollen A.A., Bhaduri A., Andrews M.G., Nowakowski T.J., Meyerson O.S., Mostajo-Radji M.A., Di Lullo E., Alvarado B., Bedolli M., Dougherty M.L., et al. Establishing Cerebral Organoids as Models of Human-Specific Brain Evolution. Cell. 2019;176:743–756.e17. doi: 10.1016/j.cell.2019.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhaduri A., Andrews M.G., Mancia Leon W., Jung D., Shin D., Allen D., Jung D., Schmunk G., Haeussler M., Salma J., et al. Cell Stress in Cortical Organoids Impairs Molecular Subtype Specification. Nature. 2020;578:142–148. doi: 10.1038/s41586-020-1962-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vértesy Á., Eichmüller O.L., Naas J., Novatchkova M., Esk C., Balmaña M., Ladstaetter S., Bock C., von Haeseler A., Knoblich J.A. Gruffi: An Algorithm for Computational Removal of Stressed Cells from Brain Organoid Transcriptomic Datasets. EMBO J. 2022:e111118. doi: 10.15252/embj.2022111118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Speir M.L., Bhaduri A., Markov N.S., Moreno P., Nowakowski T.J., Papatheodorou I., Pollen A.A., Raney B.J., Seninge L., Kent W.J., et al. UCSC Cell Browser: Visualize Your Single-Cell Data. Bioinformatics. 2021;37:4578–4580. doi: 10.1093/bioinformatics/btab503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gordon A., Yoon S.-J., Tran S.S., Makinson C.D., Park J.Y., Andersen J., Valencia A.M., Horvath S., Xiao X., Huguenard J.R., et al. Long-Term Maturation of Human Cortical Organoids Matches Key Early Postnatal Transitions. Nat. Neurosci. 2021;24:331–342. doi: 10.1038/s41593-021-00802-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luo C., Lancaster M.A., Castanon R., Nery J.R., Knoblich J.A., Ecker J.R. Cerebral Organoids Recapitulate Epigenomic Signatures of the Human Fetal Brain. Cell Rep. 2016;17:3369–3384. doi: 10.1016/j.celrep.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yoon K.-J., Ringeling F.R., Vissers C., Jacob F., Pokrass M., Jimenez-Cyrus D., Su Y., Kim N.-S., Zhu Y., Zheng L., et al. Temporal Control of Mammalian Cortical Neurogenesis by m6A Methylation. Cell. 2017;171:877–889.e17. doi: 10.1016/j.cell.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Amiri A., Coppola G., Scuderi S., Wu F., Roychowdhury T., Liu F., Pochareddy S., Shin Y., Safi A., Song L., et al. Transcriptome and Epigenome Landscape of Human Cortical Development Modeled in Organoids. Science. 2018;362:eaat6720. doi: 10.1126/science.aat6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trevino A.E., Müller F., Andersen J., Sundaram L., Kathiria A., Shcherbina A., Farh K., Chang H.Y., Pașca A.M., Kundaje A., et al. Chromatin and Gene-Regulatory Dynamics of the Developing Human Cerebral Cortex at Single-Cell Resolution. Cell. 2021;184:5053–5069.e23. doi: 10.1016/j.cell.2021.07.039. [DOI] [PubMed] [Google Scholar]
- 41.Ziffra R.S., Kim C.N., Ross J.M., Wilfert A., Turner T.N., Haeussler M., Casella A.M., Przytycki P.F., Keough K.C., Shin D., et al. Single-Cell Epigenomics Reveals Mechanisms of Human Cortical Development. Nature. 2021;598:205–213. doi: 10.1038/s41586-021-03209-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malatesta P., Hartfuss E., Götz M. Isolation of Radial Glial Cells by Fluorescent-Activated Cell Sorting Reveals a Neuronal Lineage. Development. 2000;127:5253–5263. doi: 10.1242/dev.127.24.5253. [DOI] [PubMed] [Google Scholar]
- 43.Hartfuss E., Galli R., Heins N., Götz M. Characterization of CNS Precursor Subtypes and Radial Glia. Dev. Biol. 2001;229:15–30. doi: 10.1006/dbio.2000.9962. [DOI] [PubMed] [Google Scholar]
- 44.Temple S. The Development of Neural Stem Cells. Nature. 2001;414:112–117. doi: 10.1038/35102174. [DOI] [PubMed] [Google Scholar]
- 45.Rakic P. Mode of Cell Migration to the Superficial Layers of Fetal Monkey Neocortex. J. Comp. Neurol. 1972;145:61–83. doi: 10.1002/cne.901450105. [DOI] [PubMed] [Google Scholar]
- 46.Noctor S.C., Flint A.C., Weissman T.A., Dammerman R.S., Kriegstein A.R. Neurons Derived from Radial Glial Cells Establish Radial Units in Neocortex. Nature. 2001;409:714–720. doi: 10.1038/35055553. [DOI] [PubMed] [Google Scholar]
- 47.Miyata T., Kawaguchi A., Okano H., Ogawa M. Asymmetric Inheritance of Radial Glial Fibers by Cortical Neurons. Neuron. 2001;31:727–741. doi: 10.1016/S0896-6273(01)00420-2. [DOI] [PubMed] [Google Scholar]
- 48.Haubensak W., Attardo A., Denk W., Huttner W.B. Neurons Arise in the Basal Neuroepithelium of the Early Mammalian Telencephalon: A Major Site of Neurogenesis. Proc. Natl. Acad. Sci. USA. 2004;101:3196–3201. doi: 10.1073/pnas.0308600100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Noctor S.C., Martínez-Cerdeño V., Ivic L., Kriegstein A.R. Cortical Neurons Arise in Symmetric and Asymmetric Division Zones and Migrate through Specific Phases. Nat. Neurosci. 2004;7:136–144. doi: 10.1038/nn1172. [DOI] [PubMed] [Google Scholar]
- 50.Englund C., Fink A., Lau C., Pham D., Daza R.A.M., Bulfone A., Kowalczyk T., Hevner R.F. Pax6, Tbr2, and Tbr1 Are Expressed Sequentially by Radial Glia, Intermediate Progenitor Cells, and Postmitotic Neurons in Developing Neocortex. J. Neurosci. 2005;25:247–251. doi: 10.1523/JNEUROSCI.2899-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Takahashi T., Nowakowski R.S., Caviness V.S., Jr. Cell Cycle Parameters and Patterns of Nuclear Movement in the Neocortical Proliferative Zone of the Fetal Mouse. J. Neurosci. 1993;13:820–833. doi: 10.1523/JNEUROSCI.13-02-00820.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Angevine J.B., Jr., Sidman R.L. Autoradiographic Study of Cell Migration during Histogenesis of Cerebral Cortex in the Mouse. Nature. 1961;192:766–768. doi: 10.1038/192766b0. [DOI] [PubMed] [Google Scholar]
- 53.Okano H., Temple S. Cell Types to Order: Temporal Specification of CNS Stem Cells. Curr. Opin. Neurobiol. 2009;19:112–119. doi: 10.1016/j.conb.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 54.Smart I.H.M., Dehay C., Giroud P., Berland M., Kennedy H. Unique Morphological Features of the Proliferative Zones and Postmitotic Compartments of the Neural Epithelium Giving Rise to Striate and Extrastriate Cortex in the Monkey. Cereb. Cortex. 2002;12:37–53. doi: 10.1093/cercor/12.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Betizeau M., Cortay V., Patti D., Pfister S., Gautier E., Bellemin-Ménard A., Afanassieff M., Huissoud C., Douglas R.J., Kennedy H., et al. Precursor Diversity and Complexity of Lineage Relationships in the Outer Subventricular Zone of the Primate. Neuron. 2013;80:442–457. doi: 10.1016/j.neuron.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 56.Hansen D.V., Lui J.H., Parker P.R.L., Kriegstein A.R. Neurogenic Radial Glia in the Outer Subventricular Zone of Human Neocortex. Nature. 2010;464:554–561. doi: 10.1038/nature08845. [DOI] [PubMed] [Google Scholar]
- 57.Kelava I., Reillo I., Murayama A.Y., Kalinka A.T., Stenzel D., Tomancak P., Matsuzaki F., Lebrand C., Sasaki E., Schwamborn J.C., et al. Abundant Occurrence of Basal Radial Glia in the Subventricular Zone of Embryonic Neocortex of a Lissencephalic Primate, the Common Marmoset Callithrix Jacchus. Cereb. Cortex. 2012;22:469–481. doi: 10.1093/cercor/bhr301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fietz S.A., Kelava I., Vogt J., Wilsch-Bräuninger M., Stenzel D., Fish J.L., Corbeil D., Riehn A., Distler W., Nitsch R., et al. OSVZ Progenitors of Human and Ferret Neocortex Are Epithelial-like and Expand by Integrin Signaling. Nat. Neurosci. 2010;13:690–699. doi: 10.1038/nn.2553. [DOI] [PubMed] [Google Scholar]
- 59.Reillo I., de Juan Romero C., García-Cabezas M.Á., Borrell V. A Role for Intermediate Radial Glia in the Tangential Expansion of the Mammalian Cerebral Cortex. Cereb. Cortex. 2011;21:1674–1694. doi: 10.1093/cercor/bhq238. [DOI] [PubMed] [Google Scholar]
- 60.Nowakowski T.J., Pollen A.A., Sandoval-Espinosa C., Kriegstein A.R. Transformation of the Radial Glia Scaffold Demarcates Two Stages of Human Cerebral Cortex Development. Neuron. 2016;91:1219–1227. doi: 10.1016/j.neuron.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bilgic M., Wu Q., Suetsugu T., Tsunekawa Y., Sitamukai A., Kadota M., Nishimura O., Kuraku S., Matsuzaki F. Single Cell Transcriptomics of Ferrets Reveal a Common Temporal Pattern of Progenitors in Brain Development of Gyrencephalic Mammals. bioRxiv. 2022 bioRxiv:2022.05.05.490846. [Google Scholar]
- 62.Pollen A.A., Nowakowski T.J., Chen J., Retallack H., Sandoval-Espinosa C., Nicholas C.R., Shuga J., Liu S.J., Oldham M.C., Diaz A., et al. Molecular Identity of Human Outer Radial Glia during Cortical Development. Cell. 2015;163:55–67. doi: 10.1016/j.cell.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thomsen E.R., Mich J.K., Yao Z., Hodge R.D., Doyle A.M., Jang S., Shehata S.I., Nelson A.M., Shapovalova N.V., Levi B.P., et al. Fixed Single-Cell Transcriptomic Characterization of Human Radial Glial Diversity. Nat. Methods. 2016;13:87–93. doi: 10.1038/nmeth.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Watanabe M., Buth J.E., Vishlaghi N., de la Torre-Ubieta L., Taxidis J., Khakh B.S., Coppola G., Pearson C.A., Yamauchi K., Gong D., et al. Self-Organized Cerebral Organoids with Human-Specific Features Predict Effective Drugs to Combat Zika Virus Infection. Cell Rep. 2017;21:517–532. doi: 10.1016/j.celrep.2017.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bonni A., Sun Y., Nadal-Vicens M., Bhatt A., Frank D.A., Rozovsky I., Stahl N., Yancopoulos G.D., Greenberg M.E. Regulation of Gliogenesis in the Central Nervous System by the JAK-STAT Signaling Pathway. Science. 1997;278:477–483. doi: 10.1126/science.278.5337.477. [DOI] [PubMed] [Google Scholar]
- 66.Huang W., Bhaduri A., Velmeshev D., Wang S., Wang L., Rottkamp C.A., Alvarez-Buylla A., Rowitch D.H., Kriegstein A.R. Origins and Proliferative States of Human Oligodendrocyte Precursor Cells. Cell. 2020;182:594–608.e11. doi: 10.1016/j.cell.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.van Bruggen D., Pohl F., Langseth C.M., Kukanja P., Lee H., Kabbe M., Meijer M., Hilscher M.M., Nilsson M., Sundström E., et al. Developmental Landscape of Human Forebrain at a Single-Cell Level Unveils Early Waves of Oligodendrogenesis. bioRxiv. 2021 doi: 10.1016/j.devcel.2022.04.016. bioRxiv:2021.07.22.453317. [DOI] [PubMed] [Google Scholar]
- 68.deAzevedo L.C., Fallet C., Moura-Neto V., Daumas-Duport C., Hedin-Pereira C., Lent R. Cortical Radial Glial Cells in Human Fetuses: Depth-Correlated Transformation into Astrocytes. J. Neurobiol. 2003;55:288–298. doi: 10.1002/neu.10205. [DOI] [PubMed] [Google Scholar]
- 69.Zhang Y., Sloan S.A., Clarke L.E., Caneda C., Plaza C.A., Blumenthal P.D., Vogel H., Steinberg G.K., Edwards M.S.B., Li G., et al. Purification and Characterization of Progenitor and Mature Human Astrocytes Reveals Transcriptional and Functional Differences with Mouse. Neuron. 2016;89:37–53. doi: 10.1016/j.neuron.2015.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bayraktar O.A., Bartels T., Holmqvist S., Kleshchevnikov V., Martirosyan A., Polioudakis D., Ben Haim L., Young A.M.H., Batiuk M.Y., Prakash K., et al. Astrocyte Layers in the Mammalian Cerebral Cortex Revealed by a Single-Cell in Situ Transcriptomic Map. Nat. Neurosci. 2020;23:500–509. doi: 10.1038/s41593-020-0602-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Allen D.E., Donohue K.C., Cadwell C.R., Shin D., Keefe M.G., Sohal V.S., Nowakowski T.J. Fate Mapping of Neural Stem Cell Niches Reveals Distinct Origins of Human Cortical Astrocytes. Science. 2022;376:eabm5224. doi: 10.1126/science.abm5224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Falcone C., McBride E.L., Hopkins W.D., Hof P.R., Manger P.R., Sherwood C.C., Noctor S.C., Martínez-Cerdeño V. Redefining Varicose Projection Astrocytes in Primates. Glia. 2022;70:145–154. doi: 10.1002/glia.24093. [DOI] [PubMed] [Google Scholar]
- 73.Falcone C., Penna E., Hong T., Tarantal A.F., Hof P.R., Hopkins W.D., Sherwood C.C., Noctor S.C., Martínez-Cerdeño V. Cortical Interlaminar Astrocytes Are Generated Prenatally, Mature Postnatally, and Express Unique Markers in Human and Nonhuman Primates. Cereb. Cortex. 2021;31:379–395. doi: 10.1093/cercor/bhaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kondo T., Raff M. Oligodendrocyte Precursor Cells Reprogrammed to Become Multipotential CNS Stem Cells. Science. 2000;289:1754–1757. doi: 10.1126/science.289.5485.1754. [DOI] [PubMed] [Google Scholar]
- 75.Yang L., Li Z., Liu G., Li X., Yang Z. Developmental Origins of Human Cortical Oligodendrocytes and Astrocytes. Neurosci. Bull. 2022;38:47–68. doi: 10.1007/s12264-021-00759-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fu Y., Yang M., Yu H., Wang Y., Wu X., Yong J., Mao Y., Cui Y., Fan X., Wen L., et al. Heterogeneity of Glial Progenitor Cells during the Neurogenesis-to-Gliogenesis Switch in the Developing Human Cerebral Cortex. Cell Rep. 2021;34:108788. doi: 10.1016/j.celrep.2021.108788. [DOI] [PubMed] [Google Scholar]
- 77.Hansen D.V., Lui J.H., Flandin P., Yoshikawa K., Rubenstein J.L., Alvarez-Buylla A., Kriegstein A.R. Non-Epithelial Stem Cells and Cortical Interneuron Production in the Human Ganglionic Eminences. Nat. Neurosci. 2013;16:1576–1587. doi: 10.1038/nn.3541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ma T., Wang C., Wang L., Zhou X., Tian M., Zhang Q., Zhang Y., Li J., Liu Z., Cai Y., et al. Subcortical Origins of Human and Monkey Neocortical Interneurons. Nat. Neurosci. 2013;16:1588–1597. doi: 10.1038/nn.3536. [DOI] [PubMed] [Google Scholar]
- 79.Delgado R.N., Allen D.E., Keefe M.G., Mancia Leon W.R., Ziffra R.S., Crouch E.E., Alvarez-Buylla A., Nowakowski T.J. Individual Human Cortical Progenitors Can Produce Excitatory and Inhibitory Neurons. Nature. 2022;601:397–403. doi: 10.1038/s41586-021-04230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Schmitz M.T., Sandoval K., Chen C.P., Mostajo-Radji M.A., Seeley W.W., Nowakowski T.J., Ye C.J., Paredes M.F., Pollen A.A. The Development and Evolution of Inhibitory Neurons in Primate Cerebrum. Nature. 2022;603:871–877. doi: 10.1038/s41586-022-04510-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mayer C., Jaglin X.H., Cobbs L.V., Bandler R.C., Streicher C., Cepko C.L., Hippenmeyer S., Fishell G. Clonally Related Forebrain Interneurons Disperse Broadly across Both Functional Areas and Structural Boundaries. Neuron. 2015;87:989–998. doi: 10.1016/j.neuron.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pebworth M.-P., Ross J., Andrews M., Bhaduri A., Kriegstein A.R. Human Intermediate Progenitor Diversity during Cortical Development. Proc. Natl. Acad. Sci. USA. 2021;118:e2019415118. doi: 10.1073/pnas.2019415118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Letinic K., Zoncu R., Rakic P. Origin of GABAergic Neurons in the Human Neocortex. Nature. 2002;417:645–649. doi: 10.1038/nature00779. [DOI] [PubMed] [Google Scholar]
- 84.Al-Jaberi N., Lindsay S., Sarma S., Bayatti N., Clowry G.J. The Early Fetal Development of Human Neocortical GABAergic Interneurons. Cereb. Cortex. 2015;25:631–645. doi: 10.1093/cercor/bht254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Velasco S., Kedaigle A.J., Simmons S.K., Nash A., Rocha M., Quadrato G., Paulsen B., Nguyen L., Adiconis X., Regev A., et al. Individual Brain Organoids Reproducibly Form Cell Diversity of the Human Cerebral Cortex. Nature. 2019;570:523–527. doi: 10.1038/s41586-019-1289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Qian X., Nguyen H.N., Song M.M., Hadiono C., Ogden S.C., Hammack C., Yao B., Hamersky G.R., Jacob F., Zhong C., et al. Brain-Region-Specific Organoids Using Mini-Bioreactors for Modeling ZIKV Exposure. Cell. 2016;165:1238–1254. doi: 10.1016/j.cell.2016.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang R., Sharma R., Shen X., Laughney A.M., Funato K., Clark P.J., Shpokayte M., Morgenstern P., Navare M., Xu Y., et al. Adult Human Glioblastomas Harbor Radial Glia-like Cells. Stem Cell Reports. 2020;14:338–350. doi: 10.1016/j.stemcr.2020.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tirosh I., Venteicher A.S., Hebert C., Escalante L.E., Patel A.P., Yizhak K., Fisher J.M., Rodman C., Mount C., Filbin M.G., et al. Single-Cell RNA-Seq Supports a Developmental Hierarchy in Human Oligodendroglioma. Nature. 2016;539:309–313. doi: 10.1038/nature20123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bhaduri A., Di Lullo E., Jung D., Müller S., Crouch E.E., Espinosa C.S., Ozawa T., Alvarado B., Spatazza J., Cadwell C.R., et al. Outer Radial Glia-like Cancer Stem Cells Contribute to Heterogeneity of Glioblastoma. Cell Stem Cell. 2020;26:48–63.e6. doi: 10.1016/j.stem.2019.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.La Manno G., Soldatov R., Zeisel A., Braun E., Hochgerner H., Petukhov V., Lidschreiber K., Kastriti M.E., Lönnerberg P., Furlan A., et al. RNA Velocity of Single Cells. Nature. 2018;560:494–498. doi: 10.1038/s41586-018-0414-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Trapnell C., Cacchiarelli D., Grimsby J., Pokharel P., Li S., Morse M., Lennon N.J., Livak K.J., Mikkelsen T.S., Rinn J.L. The Dynamics and Regulators of Cell Fate Decisions Are Revealed by Pseudotemporal Ordering of Single Cells. Nat. Biotechnol. 2014;32:381–386. doi: 10.1038/nbt.2859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wagner D.E., Klein A.M. Lineage Tracing Meets Single-Cell Omics: Opportunities and Challenges. Nat. Rev. Genet. 2020;21:410–427. doi: 10.1038/s41576-020-0223-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gertz C.C., Lui J.H., LaMonica B.E., Wang X., Kriegstein A.R. Diverse Behaviors of Outer Radial Glia in Developing Ferret and Human Cortex. J. Neurosci. 2014;34:2559–2570. doi: 10.1523/JNEUROSCI.2645-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.LaMonica B.E., Lui J.H., Hansen D.V., Kriegstein A.R. Mitotic Spindle Orientation Predicts Outer Radial Glial Cell Generation in Human Neocortex. Nat. Commun. 2013;4:1665. doi: 10.1038/ncomms2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bershteyn M., Nowakowski T.J., Pollen A.A., Di Lullo E., Nene A., Wynshaw-Boris A., Kriegstein A.R. Human iPSC-Derived Cerebral Organoids Model Cellular Features of Lissencephaly and Reveal Prolonged Mitosis of Outer Radial Glia. Cell Stem Cell. 2017;20:435–449.e4. doi: 10.1016/j.stem.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Subramanian L., Bershteyn M., Paredes M.F., Kriegstein A.R. Dynamic Behaviour of Human Neuroepithelial Cells in the Developing Forebrain. Nat. Commun. 2017;8:14167. doi: 10.1038/ncomms14167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Coquand L., Macé A.-S., Farcy S., Avalos C.B., Di Cicco A., Lampic M., Bessières B., Attie-Bitach T., Fraisier V., Guimiot F., et al. A Cell Fate Decision Map Reveals Abundant Direct Neurogenesis in the Human Developing Neocortex. bioRxiv. 2022 doi: 10.1038/s41556-024-01393-z. bioRxiv:2022.02.01.478661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Esk C., Lindenhofer D., Haendeler S., Wester R.A., Pflug F., Schroeder B., Bagley J.A., Elling U., Zuber J., von Haeseler A., et al. A Human Tissue Screen Identifies a Regulator of ER Secretion as a Brain-Size Determinant. Science. 2020;370:935–941. doi: 10.1126/science.abb5390. [DOI] [PubMed] [Google Scholar]
- 99.He Z., Maynard A., Jain A., Gerber T., Petri R., Lin H.-C., Santel M., Ly K., Dupré J.-S., Sidow L., et al. Lineage Recording in Human Cerebral Organoids. Nat. Methods. 2022;19:90–99. doi: 10.1038/s41592-021-01344-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bandler R.C., Vitali I., Delgado R.N., Ho M.C., Dvoretskova E., Ibarra Molinas J.S., Frazel P.W., Mohammadkhani M., Machold R., Maedler S., et al. Single-Cell Delineation of Lineage and Genetic Identity in the Mouse Brain. Nature. 2021;601:404–409. doi: 10.1038/s41586-021-04237-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ratz M., von Berlin L., Larsson L., Martin M., Westholm J.O., La Manno G., Lundeberg J., Frisén J. Clonal Relations in the Mouse Brain Revealed by Single-Cell and Spatial Transcriptomics. Nat. Neurosci. 2022;25:285–294. doi: 10.1038/s41593-022-01011-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yoon S.-J., Elahi L.S., Pașca A.M., Marton R.M., Gordon A., Revah O., Miura Y., Walczak E.M., Holdgate G.M., Fan H.C., et al. Reliability of Human Cortical Organoid Generation. Nat. Methods. 2019;16:75–78. doi: 10.1038/s41592-018-0255-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wilkinson M.D., Dumontier M., Aalbersberg I.J.J., Appleton G., Axton M., Baak A., Blomberg N., Boiten J.-W., da Silva Santos L.B., Bourne P.E., et al. The FAIR Guiding Principles for Scientific Data Management and Stewardship. Sci. Data. 2016;3:160018. doi: 10.1038/sdata.2016.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Puigdevall P., Jerber J., Danecek P., Castellano S., Kilpinen H. Effects of Somatic Mutations on Cellular Differentiation in iPSC Models of Neurodevelopment. bioRxiv. 2022 bioRxiv:2022.03.04.482992. [Google Scholar]
- 105.Giandomenico S.L., Sutcliffe M., Lancaster M.A. Generation and Long-Term Culture of Advanced Cerebral Organoids for Studying Later Stages of Neural Development. Nat. Protoc. 2021;16:579–602. doi: 10.1038/s41596-020-00433-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schafer D.P., Lehrman E.K., Kautzman A.G., Koyama R., Mardinly A.R., Yamasaki R., Ransohoff R.M., Greenberg M.E., Barres B.A., Stevens B. Microglia Sculpt Postnatal Neural Circuits in an Activity and Complement-Dependent Manner. Neuron. 2012;74:691–705. doi: 10.1016/j.neuron.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Popova G., Soliman S.S., Kim C.N., Keefe M.G., Hennick K.M., Jain S., Li T., Tejera D., Shin D., Chhun B.B., et al. Human Microglia States Are Conserved across Experimental Models and Regulate Neural Stem Cell Responses in Chimeric Organoids. Cell Stem Cell. 2021;28:2153–2166.e6. doi: 10.1016/j.stem.2021.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cakir B., Tanaka Y., Kiral F.R., Xiang Y., Dagliyan O., Wang J., Lee M., Greaney A.M., Yang W.S., duBoulay C., et al. Expression of the Transcription Factor PU.1 Induces the Generation of Microglia-like Cells in Human Cortical Organoids. Nat. Commun. 2022;13:430. doi: 10.1038/s41467-022-28043-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sabate-Soler S., Nickels S.L., Saraiva C., Berger E., Dubonyte U., Barmpa K., Lan Y.J., Kouno T., Jarazo J., Robertson G., et al. Microglia Integration into Human Midbrain Organoids Leads to Increased Neuronal Maturation and Functionality. Glia. 2022;70:1267–1288. doi: 10.1002/glia.24167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fagerlund I., Dougalis A., Shakirzyanova A., Gómez-Budia M., Pelkonen A., Konttinen H., Ohtonen S., Fazaludeen M.F., Koskuvi M., Kuusisto J., et al. Microglia-like Cells Promote Neuronal Functions in Cerebral Organoids. Cells. 2021;11:124. doi: 10.3390/cells11010124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ross J.M., Kim C., Allen D., Crouch E.E., Narsinh K., Cooke D.L., Abla A.A., Nowakowski T.J., Winkler E.A. The Expanding Cell Diversity of the Brain Vasculature. Front. Physiol. 2020;11:600767. doi: 10.3389/fphys.2020.600767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Shi Y., Sun L., Wang M., Liu J., Zhong S., Li R., Li P., Guo L., Fang A., Chen R., et al. Vascularized Human Cortical Organoids (vOrganoids) Model Cortical Development in Vivo. PLoS Biol. 2020;18:e3000705. doi: 10.1371/journal.pbio.3000705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sun X.-Y., Ju X.-C., Li Y., Zeng P.-M., Wu J., Zhou Y.-Y., Shen L.-B., Dong J., Chen Y.-J., Luo Z.-G. Generation of Vascularized Brain Organoids to Study Neurovascular Interactions. Elife. 2022;11:e76707. doi: 10.7554/eLife.76707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kook M.G., Lee S.-E., Shin N., Kong D., Kim D.-H., Kim M.-S., Kang H.K., Choi S.W., Kang K.-S. Generation of Cortical Brain Organoid with Vascularization by Assembling with Vascular Spheroid. Int J Stem Cells. 2022;15:85–94. doi: 10.15283/ijsc21157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Cakir B., Xiang Y., Tanaka Y., Kural M.H., Parent M., Kang Y.-J., Chapeton K., Patterson B., Yuan Y., He C.-S., et al. Engineering of Human Brain Organoids with a Functional Vascular-like System. Nat. Methods. 2019;16:1169–1175. doi: 10.1038/s41592-019-0586-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ang L.T., Nguyen A.T., Liu K.J., Chen A., Xiong X., Curtis M., Martin R.M., Raftry B.C., Ng C.Y., Vogel U., et al. Generating Human Artery and Vein Cells from Pluripotent Stem Cells Highlights the Arterial Tropism of Nipah and Hendra Viruses. Cell. 2022;185:2523–2541.e30. doi: 10.1016/j.cell.2022.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Nikolova M.T., He Z., Wimmer R.A., Seimiya M., Nikoloff J.M., Penninger J.M., Gray Camp J., Treutlein B. Fate and State Transitions during Human Blood Vessel Organoid Development. bioRxiv. 2022 bioRxiv:2022.03.23.485329. [Google Scholar]
- 118.Winkler E.A., Kim C.N., Ross J.M., Garcia J.H., Gil E., Oh I., Chen L.Q., Wu D., Catapano J.S., Raygor K., et al. A Single-Cell Atlas of the Normal and Malformed Human Brain Vasculature. Science. 2022;375:eabi7377. doi: 10.1126/science.abi7377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yang A.C., Vest R.T., Kern F., Lee D.P., Agam M., Maat C.A., Losada P.M., Chen M.B., Schaum N., Khoury N., et al. A Human Brain Vascular Atlas Reveals Diverse Mediators of Alzheimer’s Risk. Nature. 2022;603:885–892. doi: 10.1038/s41586-021-04369-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Birey F., Andersen J., Makinson C.D., Islam S., Wei W., Huber N., Fan H.C., Metzler K.R.C., Panagiotakos G., Thom N., et al. Assembly of Functionally Integrated Human Forebrain Spheroids. Nature. 2017;545:54–59. doi: 10.1038/nature22330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Xiang Y., Tanaka Y., Patterson B., Kang Y.-J., Govindaiah G., Roselaar N., Cakir B., Kim K.-Y., Lombroso A.P., Hwang S.-M., et al. Fusion of Regionally Specified hPSC-Derived Organoids Models Human Brain Development and Interneuron Migration. Cell Stem Cell. 2017;21:383–398.e7. doi: 10.1016/j.stem.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bagley J.A., Reumann D., Bian S., Lévi-Strauss J., Knoblich J.A. Fused Cerebral Organoids Model Interactions between Brain Regions. Nat. Methods. 2017;14:743–751. doi: 10.1038/nmeth.4304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Miura Y., Li M.-Y., Birey F., Ikeda K., Revah O., Thete M.V., Park J.-Y., Puno A., Lee S.H., Porteus M.H., et al. Generation of Human Striatal Organoids and Cortico-Striatal Assembloids from Human Pluripotent Stem Cells. Nat. Biotechnol. 2020;38:1421–1430. doi: 10.1038/s41587-020-00763-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sakaguchi H., Kadoshima T., Soen M., Narii N., Ishida Y., Ohgushi M., Takahashi J., Eiraku M., Sasai Y. Generation of Functional Hippocampal Neurons from Self-Organizing Human Embryonic Stem Cell-Derived Dorsomedial Telencephalic Tissue. Nat. Commun. 2015;6:8896. doi: 10.1038/ncomms9896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Suga H., Kadoshima T., Minaguchi M., Ohgushi M., Soen M., Nakano T., Takata N., Wataya T., Muguruma K., Miyoshi H., et al. Self-Formation of Functional Adenohypophysis in Three-Dimensional Culture. Nature. 2011;480:57–62. doi: 10.1038/nature10637. [DOI] [PubMed] [Google Scholar]
- 126.Ozone C., Suga H., Eiraku M., Kadoshima T., Yonemura S., Takata N., Oiso Y., Tsuji T., Sasai Y. Functional Anterior Pituitary Generated in Self-Organizing Culture of Human Embryonic Stem Cells. Nat. Commun. 2016;7:10351. doi: 10.1038/ncomms10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shiraishi A., Muguruma K., Sasai Y. Generation of Thalamic Neurons from Mouse Embryonic Stem Cells. Development. 2017;144:1211–1220. doi: 10.1242/dev.144071. [DOI] [PubMed] [Google Scholar]
- 128.Xiang Y., Tanaka Y., Cakir B., Patterson B., Kim K.-Y., Sun P., Kang Y.-J., Zhong M., Liu X., Patra P., et al. hESC-Derived Thalamic Organoids Form Reciprocal Projections When Fused with Cortical Organoids. Cell Stem Cell. 2019;24:487–497.e7. doi: 10.1016/j.stem.2018.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Jo J., Xiao Y., Sun A.X., Cukuroglu E., Tran H.-D., Göke J., Tan Z.Y., Saw T.Y., Tan C.-P., Lokman H., et al. Midbrain-like Organoids from Human Pluripotent Stem Cells Contain Functional Dopaminergic and Neuromelanin-Producing Neurons. Cell Stem Cell. 2016;19:248–257. doi: 10.1016/j.stem.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zagare A., Gobin M., Monzel A.S., Schwamborn J.C. A Robust Protocol for the Generation of Human Midbrain Organoids. STAR Protoc. 2021;2:100524. doi: 10.1016/j.xpro.2021.100524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fiorenzano A., Sozzi E., Birtele M., Kajtez J., Giacomoni J., Nilsson F., Bruzelius A., Sharma Y., Zhang Y., Mattsson B., et al. Single-Cell Transcriptomics Captures Features of Human Midbrain Development and Dopamine Neuron Diversity in Brain Organoids. Nat. Commun. 2021;12:7302. doi: 10.1038/s41467-021-27464-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Muguruma K., Nishiyama A., Kawakami H., Hashimoto K., Sasai Y. Self-Organization of Polarized Cerebellar Tissue in 3D Culture of Human Pluripotent Stem Cells. Cell Rep. 2015;10:537–550. doi: 10.1016/j.celrep.2014.12.051. [DOI] [PubMed] [Google Scholar]
- 133.Fleck J.S., Sanchís-Calleja F., He Z., Santel M., Boyle M.J., Camp J.G., Treutlein B. Resolving Organoid Brain Region Identities by Mapping Single-Cell Genomic Data to Reference Atlases. Cell Stem Cell. 2021;28:1148–1159.e8. doi: 10.1016/j.stem.2021.02.015. [DOI] [PubMed] [Google Scholar]
- 134.Andersen J., Revah O., Miura Y., Thom N., Amin N.D., Kelley K.W., Singh M., Chen X., Thete M.V., Walczak E.M., et al. Generation of Functional Human 3D Cortico-Motor Assembloids. Cell. 2020;183:1913–1929.e26. doi: 10.1016/j.cell.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Giandomenico S.L., Mierau S.B., Gibbons G.M., Wenger L.M.D., Masullo L., Sit T., Sutcliffe M., Boulanger J., Tripodi M., Derivery E., et al. Cerebral Organoids at the Air-Liquid Interface Generate Diverse Nerve Tracts with Functional Output. Nat. Neurosci. 2019;22:669–679. doi: 10.1038/s41593-019-0350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Takata N., Sakakura E., Eiraku M., Kasukawa T., Sasai Y. Self-Patterning of Rostral-Caudal Neuroectoderm Requires Dual Role of Fgf Signaling for Localized Wnt Antagonism. Nat. Commun. 2017;8:1339. doi: 10.1038/s41467-017-01105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Cederquist G.Y., Asciolla J.J., Tchieu J., Walsh R.M., Cornacchia D., Resh M.D., Studer L. Specification of Positional Identity in Forebrain Organoids. Nat. Biotechnol. 2019;37:436–444. doi: 10.1038/s41587-019-0085-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Osaki T., Ikeuchi Y. Advanced Complexity and Plasticity of Neural Activity in Reciprocally Connected Human Cerebral Organoids. bioRxiv. 2021 bioRxiv:2021.02.16.431387. [Google Scholar]
- 139.Molyneaux B.J., Arlotta P., Menezes J.R.L., Macklis J.D. Neuronal Subtype Specification in the Cerebral Cortex. Nat. Rev. Neurosci. 2007;8:427–437. doi: 10.1038/nrn2151. [DOI] [PubMed] [Google Scholar]
- 140.Greig L.C., Woodworth M.B., Galazo M.J., Padmanabhan H., Macklis J.D. Molecular Logic of Neocortical Projection Neuron Specification, Development and Diversity. Nat. Rev. Neurosci. 2013;14:755–769. doi: 10.1038/nrn3586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Anderson S., Vanderhaeghen P. Cortical Neurogenesis from Pluripotent Stem Cells: Complexity Emerging from Simplicity. Curr. Opin. Neurobiol. 2014;27:151–157. doi: 10.1016/j.conb.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Cadwell C.R., Bhaduri A., Mostajo-Radji M.A., Keefe M.G., Nowakowski T.J. Development and Arealization of the Cerebral Cortex. Neuron. 2019;103:980–1004. doi: 10.1016/j.neuron.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cederquist G.Y., Tchieu J., Callahan S.J., Ramnarine K., Ryan S., Zhang C., Rittenhouse C., Zeltner N., Chung S.Y., Zhou T., et al. A Multiplex Human Pluripotent Stem Cell Platform Defines Molecular and Functional Subclasses of Autism-Related Genes. Cell Stem Cell. 2020;27:35–49.e6. doi: 10.1016/j.stem.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hasenpusch-Theil K., Watson J.A., Theil T. Direct Interactions Between Gli3, Wnt8b, and Fgfs Underlie Patterning of the Dorsal Telencephalon. Cereb. Cortex. 2017;27:1137–1148. doi: 10.1093/cercor/bhv291. [DOI] [PubMed] [Google Scholar]
- 145.Ypsilanti A.R., Pattabiraman K., Catta-Preta R., Golonzhka O., Lindtner S., Tang K., Jones I.R., Abnousi A., Juric I., Hu M., et al. Transcriptional Network Orchestrating Regional Patterning of Cortical Progenitors. Proc. Natl. Acad. Sci. USA. 2021;118:e2024795118. doi: 10.1073/pnas.2024795118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Markenscoff-Papadimitriou E., Whalen S., Przytycki P., Thomas R., Binyameen F., Nowakowski T.J., Kriegstein A.R., Sanders S.J., State M.W., Pollard K.S., et al. A Chromatin Accessibility Atlas of the Developing Human Telencephalon. Cell. 2020;182:754–769.e18. doi: 10.1016/j.cell.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Shibata M., Pattabiraman K., Lorente-Galdos B., Andrijevic D., Kim S.-K., Kaur N., Muchnik S.K., Xing X., Santpere G., Sousa A.M.M., et al. Regulation of Prefrontal Patterning and Connectivity by Retinoic Acid. Nature. 2021;598:483–488. doi: 10.1038/s41586-021-03953-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Espuny-Camacho I., Michelsen K.A., Gall D., Linaro D., Hasche A., Bonnefont J., Bali C., Orduz D., Bilheu A., Herpoel A., et al. Pyramidal Neurons Derived from Human Pluripotent Stem Cells Integrate Efficiently into Mouse Brain Circuits in Vivo. Neuron. 2013;77:440–456. doi: 10.1016/j.neuron.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 149.Linaro D., Vermaercke B., Iwata R., Ramaswamy A., Libé-Philippot B., Boubakar L., Davis B.A., Wierda K., Davie K., Poovathingal S., et al. Xenotransplanted Human Cortical Neurons Reveal Species-Specific Development and Functional Integration into Mouse Visual Circuits. Neuron. 2019;104:972–986.e6. doi: 10.1016/j.neuron.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mansour A.A., Gonçalves J.T., Bloyd C.W., Li H., Fernandes S., Quang D., Johnston S., Parylak S.L., Jin X., Gage F.H. An in Vivo Model of Functional and Vascularized Human Brain Organoids. Nat. Biotechnol. 2018;36:432–441. doi: 10.1038/nbt.4127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Daviaud N., Friedel R.H., Zou H. Vascularization and Engraftment of Transplanted Human Cerebral Organoids in Mouse Cortex. eNeuro. 2018;5:ENEURO.0219-18.2018. doi: 10.1523/ENEURO.0219-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kitahara T., Sakaguchi H., Morizane A., Kikuchi T., Miyamoto S., Takahashi J. Axonal Extensions along Corticospinal Tracts from Transplanted Human Cerebral Organoids. Stem Cell Reports. 2020;15:467–481. doi: 10.1016/j.stemcr.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Chen H.I., Song H., Ming G.-L. Applications of Human Brain Organoids to Clinical Problems. Dev. Dyn. 2019;248:53–64. doi: 10.1002/dvdy.24662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Britanova O., de Juan Romero C., Cheung A., Kwan K.Y., Schwark M., Gyorgy A., Vogel T., Akopov S., Mitkovski M., Agoston D., et al. Satb2 Is a Postmitotic Determinant for Upper-Layer Neuron Specification in the Neocortex. Neuron. 2008;57:378–392. doi: 10.1016/j.neuron.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 155.National Academies of Sciences, Engineering, and Medicine. Policy and Global Affairs. Committee on Science, Technology, and Law. Committee on Ethical, Legal, and Regulatory Issues Associated with Neural Chimeras and Organoids . The Emerging Field of Human Neural Organoids, Transplants, and Chimeras: Science, Ethics, and Governance. National Academies Press (US); Washington, DC, USA: 2021. [PubMed] [Google Scholar]
- 156.Powell K. Hybrid Brains: The Ethics of Transplanting Human Neurons into Animals. Nature. 2022;608:22–25. doi: 10.1038/d41586-022-02073-4. [DOI] [PubMed] [Google Scholar]
- 157.Brennand K.J., Simone A., Jou J., Gelboin-Burkhart C., Tran N., Sangar S., Li Y., Mu Y., Chen G., Yu D., et al. Modelling Schizophrenia Using Human Induced Pluripotent Stem Cells. Nature. 2011;473:221–225. doi: 10.1038/nature09915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Paşca S.P., Portmann T., Voineagu I., Yazawa M., Shcheglovitov A., Paşca A.M., Cord B., Palmer T.D., Chikahisa S., Nishino S., et al. Using iPSC-Derived Neurons to Uncover Cellular Phenotypes Associated with Timothy Syndrome. Nat. Med. 2011;17:1657–1662. doi: 10.1038/nm.2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dolmetsch R., Geschwind D.H. The Human Brain in a Dish: The Promise of iPSC-Derived Neurons. Cell. 2011;145:831–834. doi: 10.1016/j.cell.2011.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Rowe R.G., Daley G.Q. Induced Pluripotent Stem Cells in Disease Modelling and Drug Discovery. Nat. Rev. Genet. 2019;20:377–388. doi: 10.1038/s41576-019-0100-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Panda A., Suvakov M., Mariani J., Drucker K.L., Park Y., Jang Y., Kollmeyer T.M., Sarkar G., Bae T., Kim J.J., et al. Clonally Selected Lines after CRISPR/Cas Editing Are Not Isogenic. bioRxiv. 2022 doi: 10.1089/crispr.2022.0050. bioRxiv:2022.05.17.492193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kato M., Dobyns W.B. Lissencephaly and the Molecular Basis of Neuronal Migration. Hum. Mol. Genet. 2003;12:R89–R96. doi: 10.1093/hmg/ddg086. [DOI] [PubMed] [Google Scholar]
- 163.Cahana A., Escamez T., Nowakowski R.S., Hayes N.L., Giacobini M., von Holst A., Shmueli O., Sapir T., McConnell S.K., Wurst W., et al. Targeted Mutagenesis of Lis1 Disrupts Cortical Development and LIS1 Homodimerization. Proc. Natl. Acad. Sci. USA. 2001;98:6429–6434. doi: 10.1073/pnas.101122598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Youn Y.H., Pramparo T., Hirotsune S., Wynshaw-Boris A. Distinct Dose-Dependent Cortical Neuronal Migration and Neurite Extension Defects in Lis1 and Ndel1 Mutant Mice. J. Neurosci. 2009;29:15520–15530. doi: 10.1523/JNEUROSCI.4630-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Karzbrun E., Kshirsagar A., Cohen S.R., Hanna J.H., Reiner O. Human Brain Organoids on a Chip Reveal the Physics of Folding. Nat. Phys. 2018;14:515–522. doi: 10.1038/s41567-018-0046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Thiele E.A. Managing and Understanding Epilepsy in Tuberous Sclerosis Complex. Epilepsia. 2010;51((Suppl. S1)):90–91. doi: 10.1111/j.1528-1167.2009.02458.x. [DOI] [PubMed] [Google Scholar]
- 167.European Chromosome 16 Tuberous Sclerosis Consortium Identification and Characterization of the Tuberous Sclerosis Gene on Chromosome 16. Cell. 1993;75:1305–1315. doi: 10.1016/0092-8674(93)90618-Z. [DOI] [PubMed] [Google Scholar]
- 168.van Slegtenhorst M., de Hoogt R., Hermans C., Nellist M., Janssen B., Verhoef S., Lindhout D., van den Ouweland A., Halley D., Young J., et al. Identification of the Tuberous Sclerosis Gene TSC1 on Chromosome 9q34. Science. 1997;277:805–808. doi: 10.1126/science.277.5327.805. [DOI] [PubMed] [Google Scholar]
- 169.Tee A.R., Fingar D.C., Manning B.D., Kwiatkowski D.J., Cantley L.C., Blenis J. Tuberous Sclerosis Complex-1 and -2 Gene Products Function Together to Inhibit Mammalian Target of Rapamycin (mTOR)-Mediated Downstream Signaling. Proc. Natl. Acad. Sci. USA. 2002;99:13571–13576. doi: 10.1073/pnas.202476899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Costa V., Aigner S., Vukcevic M., Sauter E., Behr K., Ebeling M., Dunkley T., Friedlein A., Zoffmann S., Meyer C.A., et al. mTORC1 Inhibition Corrects Neurodevelopmental and Synaptic Alterations in a Human Stem Cell Model of Tuberous Sclerosis. Cell Rep. 2016;15:86–95. doi: 10.1016/j.celrep.2016.02.090. [DOI] [PubMed] [Google Scholar]
- 171.Andrews M.G., Subramanian L., Kriegstein A.R. mTOR Signaling Regulates the Morphology and Migration of Outer Radial Glia in Developing Human Cortex. Elife. 2020;9:e58737. doi: 10.7554/eLife.58737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Onda H., Crino P.B., Zhang H., Murphey R.D., Rastelli L., Gould Rothberg B.E., Kwiatkowski D.J. Tsc2 Null Murine Neuroepithelial Cells Are a Model for Human Tuber Giant Cells, and Show Activation of an mTOR Pathway. Mol. Cell. Neurosci. 2002;21:561–574. doi: 10.1006/mcne.2002.1184. [DOI] [PubMed] [Google Scholar]
- 173.Blair J.D., Hockemeyer D., Bateup H.S. Genetically Engineered Human Cortical Spheroid Models of Tuberous Sclerosis. Nat. Med. 2018;24:1568–1578. doi: 10.1038/s41591-018-0139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Klaus J., Kanton S., Kyrousi C., Ayo-Martin A.C., Di Giaimo R., Riesenberg S., O’Neill A.C., Camp J.G., Tocco C., Santel M., et al. Altered Neuronal Migratory Trajectories in Human Cerebral Organoids Derived from Individuals with Neuronal Heterotopia. Nat. Med. 2019;25:561–568. doi: 10.1038/s41591-019-0371-0. [DOI] [PubMed] [Google Scholar]
- 175.Birey F., Li M.-Y., Gordon A., Thete M.V., Valencia A.M., Revah O., Paşca A.M., Geschwind D.H., Paşca S.P. Dissecting the Molecular Basis of Human Interneuron Migration in Forebrain Assembloids from Timothy Syndrome. Cell Stem Cell. 2022;29:248–264.e7. doi: 10.1016/j.stem.2021.11.011. [DOI] [PubMed] [Google Scholar]
- 176.Toyoshima M., Akamatsu W., Okada Y., Ohnishi T., Balan S., Hisano Y., Iwayama Y., Toyota T., Matsumoto T., Itasaka N., et al. Analysis of Induced Pluripotent Stem Cells Carrying 22q11.2 Deletion. Transl. Psychiatry. 2016;6:e934. doi: 10.1038/tp.2016.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Amin H., Marinaro F., De Pietri Tonelli D., Berdondini L. Developmental Excitatory-to-Inhibitory GABA-Polarity Switch Is Disrupted in 22q11.2 Deletion Syndrome: A Potential Target for Clinical Therapeutics. Sci. Rep. 2017;7:15752. doi: 10.1038/s41598-017-15793-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Li J., Ryan S.K., Deboer E., Cook K., Fitzgerald S., Lachman H.M., Wallace D.C., Goldberg E.M., Anderson S.A. Mitochondrial Deficits in Human iPSC-Derived Neurons from Patients with 22q11.2 Deletion Syndrome and Schizophrenia. Transl. Psychiatry. 2019;9:302. doi: 10.1038/s41398-019-0643-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Khan T.A., Revah O., Gordon A., Yoon S.-J., Krawisz A.K., Goold C., Sun Y., Kim C.H., Tian Y., Li M.-Y., et al. Neuronal Defects in a Human Cellular Model of 22q11.2 Deletion Syndrome. Nat. Med. 2020;26:1888–1898. doi: 10.1038/s41591-020-1043-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Landthaler M., Yalcin A., Tuschl T. The Human DiGeorge Syndrome Critical Region Gene 8 and Its D. Melanogaster Homolog Are Required for miRNA Biogenesis. Curr. Biol. 2004;14:2162–2167. doi: 10.1016/j.cub.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 181.Amir R.E., Van den Veyver I.B., Wan M., Tran C.Q., Francke U., Zoghbi H.Y. Rett Syndrome Is Caused by Mutations in X-Linked MECP2, Encoding Methyl-CpG-Binding Protein 2. Nat. Genet. 1999;23:185–188. doi: 10.1038/13810. [DOI] [PubMed] [Google Scholar]
- 182.Lewis J.D., Meehan R.R., Henzel W.J., Maurer-Fogy I., Jeppesen P., Klein F., Bird A. Purification, Sequence, and Cellular Localization of a Novel Chromosomal Protein That Binds to Methylated DNA. Cell. 1992;69:905–914. doi: 10.1016/0092-8674(92)90610-O. [DOI] [PubMed] [Google Scholar]
- 183.Tropea D., Giacometti E., Wilson N.R., Beard C., McCurry C., Fu D.D., Flannery R., Jaenisch R., Sur M. Partial Reversal of Rett Syndrome-like Symptoms in MeCP2 Mutant Mice. Proc. Natl. Acad. Sci. USA. 2009;106:2029–2034. doi: 10.1073/pnas.0812394106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Marchetto M.C.N., Carromeu C., Acab A., Yu D., Yeo G.W., Mu Y., Chen G., Gage F.H., Muotri A.R. A Model for Neural Development and Treatment of Rett Syndrome Using Human Induced Pluripotent Stem Cells. Cell. 2010;143:527–539. doi: 10.1016/j.cell.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Trujillo C.A., Adams J.W., Negraes P.D., Carromeu C., Tejwani L., Acab A., Tsuda B., Thomas C.A., Sodhi N., Fichter K.M., et al. Pharmacological Reversal of Synaptic and Network Pathology in Human MECP2-KO Neurons and Cortical Organoids. EMBO Mol. Med. 2021;13:e12523. doi: 10.15252/emmm.202012523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Samarasinghe R.A., Miranda O.A., Buth J.E., Mitchell S., Ferando I., Watanabe M., Allison T.F., Kurdian A., Fotion N.N., Gandal M.J., et al. Identification of Neural Oscillations and Epileptiform Changes in Human Brain Organoids. Nat. Neurosci. 2021;24:1488–1500. doi: 10.1038/s41593-021-00906-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ohashi M., Korsakova E., Allen D., Lee P., Fu K., Vargas B.S., Cinkornpumin J., Salas C., Park J.C., Germanguz I., et al. Loss of MECP2 Leads to Activation of P53 and Neuronal Senescence. Stem Cell Reports. 2018;10:1453–1463. doi: 10.1016/j.stemcr.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Satterstrom F.K., Kosmicki J.A., Wang J., Breen M.S., De Rubeis S., An J.-Y., Peng M., Collins R., Grove J., Klei L., et al. Large-Scale Exome Sequencing Study Implicates Both Developmental and Functional Changes in the Neurobiology of Autism. Cell. 2020;180:568–584.e23. doi: 10.1016/j.cell.2019.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Sanders S.J., He X., Willsey A.J., Ercan-Sencicek A.G., Samocha K.E., Cicek A.E., Murtha M.T., Bal V.H., Bishop S.L., Dong S., et al. Insights into Autism Spectrum Disorder Genomic Architecture and Biology from 71 Risk Loci. Neuron. 2015;87:1215–1233. doi: 10.1016/j.neuron.2015.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Wang T., Kim C., Bakken T.E., Gillentine M.A., Henning B., Mao Y., Gilissen C., The SPARK Consortium. Nowakowski T.J., Eichler E.E. Integrated Gene Analyses of de Novo Mutations from 46,612 Trios with Autism and Developmental Disorders. bioRxiv. 2021 doi: 10.1073/pnas.2203491119. bioRxiv:2021.09.15.460398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Willsey H.R., Willsey A.J., Wang B., State M.W. Genomics, Convergent Neuroscience and Progress in Understanding Autism Spectrum Disorder. Nat. Rev. Neurosci. 2022;23:323–341. doi: 10.1038/s41583-022-00576-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Weiss L.A., Shen Y., Korn J.M., Arking D.E., Miller D.T., Fossdal R., Saemundsen E., Stefansson H., Ferreira M.A.R., Green T., et al. Association between Microdeletion and Microduplication at 16p11.2 and Autism. N. Engl. J. Med. 2008;358:667–675. doi: 10.1056/NEJMoa075974. [DOI] [PubMed] [Google Scholar]
- 193.Deshpande A., Yadav S., Dao D.Q., Wu Z.-Y., Hokanson K.C., Cahill M.K., Wiita A.P., Jan Y.-N., Ullian E.M., Weiss L.A. Cellular Phenotypes in Human iPSC-Derived Neurons from a Genetic Model of Autism Spectrum Disorder. Cell Rep. 2017;21:2678–2687. doi: 10.1016/j.celrep.2017.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Urresti J., Zhang P., Moran-Losada P., Yu N.-K., Negraes P.D., Trujillo C.A., Antaki D., Amar M., Chau K., Pramod A.B., et al. Cortical Organoids Model Early Brain Development Disrupted by 16p11.2 Copy Number Variants in Autism. Mol. Psychiatry. 2021;26:7560–7580. doi: 10.1038/s41380-021-01243-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lim E.T., Chan Y., Dawes P., Guo X., Erdin S., Tai D.J.C., Liu S., Reichert J.M., Burns M.J., Chan Y.K., et al. Orgo-Seq Integrates Single-Cell and Bulk Transcriptomic Data to Identify Cell Type Specific-Driver Genes Associated with Autism Spectrum Disorder. Nat. Commun. 2022;13:3243. doi: 10.1038/s41467-022-30968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kang H.J., Kawasawa Y.I., Cheng F., Zhu Y., Xu X., Li M., Sousa A.M.M., Pletikos M., Meyer K.A., Sedmak G., et al. Spatio-Temporal Transcriptome of the Human Brain. Nature. 2011;478:483–489. doi: 10.1038/nature10523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Willsey A.J., Sanders S.J., Li M., Dong S., Tebbenkamp A.T., Muhle R.A., Reilly S.K., Lin L., Fertuzinhos S., Miller J.A., et al. Coexpression Networks Implicate Human Midfetal Deep Cortical Projection Neurons in the Pathogenesis of Autism. Cell. 2013;155:997–1007. doi: 10.1016/j.cell.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Parikshak N.N., Luo R., Zhang A., Won H., Lowe J.K., Chandran V., Horvath S., Geschwind D.H. Integrative Functional Genomic Analyses Implicate Specific Molecular Pathways and Circuits in Autism. Cell. 2013;155:1008–1021. doi: 10.1016/j.cell.2013.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gamache T.R., Araki Y., Huganir R.L. Twenty Years of SynGAP Research: From Synapses to Cognition. J. Neurosci. 2020;40:1596–1605. doi: 10.1523/JNEUROSCI.0420-19.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Birtele M., Del Dosso A., Xu T., Nguyen T., Wilkinson B., Urenda J.-P., Knight G., Moore R., Sharma R., Pirrotte P., et al. The Autism-Associated Gene SYNGAP1 Regulates Human Cortical Neurogenesis. bioRxiv. 2022 bioRxiv:2022.05.10.491244. [Google Scholar]
- 201.Lalli M.A., Avey D., Dougherty J.D., Milbrandt J., Mitra R.D. High-Throughput Single-Cell Functional Elucidation of Neurodevelopmental Disease-Associated Genes Reveals Convergent Mechanisms Altering Neuronal Differentiation. Genome Res. 2020;30:1317–1331. doi: 10.1101/gr.262295.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Paulsen B., Velasco S., Kedaigle A.J., Pigoni M., Quadrato G., Deo A.J., Adiconis X., Uzquiano A., Sartore R., Yang S.M., et al. Autism Genes Converge on Asynchronous Development of Shared Neuron Classes. Nature. 2022;602:268–273. doi: 10.1038/s41586-021-04358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Villa C.E., Cheroni C., Dotter C.P., López-Tóbon A., Oliveira B., Sacco R., Yahya A.Ç., Morandell J., Gabriele M., Tavakoli M.R., et al. CHD8 Haploinsufficiency Links Autism to Transient Alterations in Excitatory and Inhibitory Trajectories. Cell Rep. 2022;39:110615. doi: 10.1016/j.celrep.2022.110615. [DOI] [PubMed] [Google Scholar]
- 204.Crucitti J., Hyde C., Enticott P.G., Stokes M.A. Head Circumference Trends in Autism between 0 and 100 Months. Autism. 2020;24:1726–1739. doi: 10.1177/1362361320921037. [DOI] [PubMed] [Google Scholar]
- 205.Mariani J., Coppola G., Zhang P., Abyzov A., Provini L., Tomasini L., Amenduni M., Szekely A., Palejev D., Wilson M., et al. FOXG1-Dependent Dysregulation of GABA/Glutamate Neuron Differentiation in Autism Spectrum Disorders. Cell. 2015;162:375–390. doi: 10.1016/j.cell.2015.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Adhya D., Swarup V., Nagy R., Dutan L., Shum C., Valencia-Alarcón E.P., Jozwik K.M., Mendez M.A., Horder J., Loth E., et al. Atypical Neurogenesis in Induced Pluripotent Stem Cells from Autistic Individuals. Biol. Psychiatry. 2021;89:486–496. doi: 10.1016/j.biopsych.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Jourdon A., Wu F., Mariani J., Capauto D., Norton S., Tomasini L., Amiri A., Suvakov M., Schreiner J.D., Jang Y., et al. ASD Modelling in Organoids Reveals Imbalance of Excitatory Cortical Neuron Subtypes during Early Neurogenesis. bioRxiv. 2022 bioRxiv:2022.03.19.484988. [Google Scholar]
- 208.Hergenreder E., Zorina Y., Zhao Z., Munguba H., Calder E.L., Baggiolini A., Minotti A.P., Walsh R.M., Liston C., Levitz J., et al. Combined Small Molecule Treatment Accelerates Timing of Maturation in Human Pluripotent Stem Cell-Derived Neurons. bioRxiv. 2022 bioRxiv:2022.06.02.494616. [Google Scholar]
- 209.Ciceri G., Cho H., Kshirsagar M., Baggiolini A., Aromolaran K.A., Walsh R.M., Goldstein P.A., Koche R.P., Leslie C.S., Studer L. An Epigenetic Barrier Sets the Timing of Human Neuronal Maturation. bioRxiv. 2022 doi: 10.1038/s41586-023-06984-8. bioRxiv:2022.06.02.490114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Feldman D., Singh A., Schmid-Burgk J.L., Carlson R.J., Mezger A., Garrity A.J., Zhang F., Blainey P.C. Optical Pooled Screens in Human Cells. Cell. 2019;179:787–799.e17. doi: 10.1016/j.cell.2019.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Rubin A.J., Parker K.R., Satpathy A.T., Qi Y., Wu B., Ong A.J., Mumbach M.R., Ji A.L., Kim D.S., Cho S.W., et al. Coupled Single-Cell CRISPR Screening and Epigenomic Profiling Reveals Causal Gene Regulatory Networks. Cell. 2019;176:361–376.e17. doi: 10.1016/j.cell.2018.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Cleary B., Regev A. The Necessity and Power of Random, under-Sampled Experiments in Biology. arXiv. 20202012.12961 [Google Scholar]
- 213.Wu Z., Chhun B.B., Popova G., Guo S.-M., Kim C.N., Yeh L.-H., Nowakowski T., Zou J., Mehta S.B. DynaMorph: Self-Supervised Learning of Morphodynamic States of Live Cells. Mol. Biol. Cell. 2022;33:ar59. doi: 10.1091/mbc.E21-11-0561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Moreau C.A., Kumar K., Harvey A., Huguet G., Urchs S., Douard E.A., Schultz L.M., Sharmarke H., Jizi K., Martin C.-O., et al. Atlas of Functional Connectivity Relationships across Rare and Common Genetic Variants, Traits, and Psychiatric Conditions. bioRxiv. 2021 doi: 10.1101/2021.05.21.21257604. [DOI] [Google Scholar]
- 215.Velmeshev D., Schirmer L., Jung D., Haeussler M., Perez Y., Mayer S., Bhaduri A., Goyal N., Rowitch D.H., Kriegstein A.R. Single-Cell Genomics Identifies Cell Type-Specific Molecular Changes in Autism. Science. 2019;364:685–689. doi: 10.1126/science.aav8130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Ramaswami G., Won H., Gandal M.J., Haney J., Wang J.C., Wong C.C.Y., Sun W., Prabhakar S., Mill J., Geschwind D.H. Integrative Genomics Identifies a Convergent Molecular Subtype That Links Epigenomic with Transcriptomic Differences in Autism. Nat. Commun. 2020;11:4873. doi: 10.1038/s41467-020-18526-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.de la Torre-Ubieta L., Won H., Stein J.L., Geschwind D.H. Advancing the Understanding of Autism Disease Mechanisms through Genetics. Nat. Med. 2016;22:345–361. doi: 10.1038/nm.4071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Chen J.A., Peñagarikano O., Belgard T.G., Swarup V., Geschwind D.H. The Emerging Picture of Autism Spectrum Disorder: Genetics and Pathology. Annu. Rev. Pathol. 2015;10:111–144. doi: 10.1146/annurev-pathol-012414-040405. [DOI] [PubMed] [Google Scholar]
- 219.Ruzicka W.B., Mohammadi S., Davila-Velderrain J., Subburaju S., Tso D.R., Hourihan M., Kellis M. Single-Cell Dissection of Schizophrenia Reveals Neurodevelopmental-Synaptic Axis and Transcriptional Resilience. bioRxiv. 2020 doi: 10.1101/2020.11.06.20225342. [DOI] [Google Scholar]
- 220.Bhaduri A., Andrews M.G., Kriegstein A.R., Nowakowski T.J. Are Organoids Ready for Prime Time? Cell Stem Cell. 2020;27:361–365. doi: 10.1016/j.stem.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Willsey H.R., Exner C.R.T., Xu Y., Everitt A., Sun N., Wang B., Dea J., Schmunk G., Zaltsman Y., Teerikorpi N., et al. Parallel in Vivo Analysis of Large-Effect Autism Genes Implicates Cortical Neurogenesis and Estrogen in Risk and Resilience. Neuron. 2021;109:788–804.e8. doi: 10.1016/j.neuron.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Ortiz-Virumbrales M., Moreno C.L., Kruglikov I., Marazuela P., Sproul A., Jacob S., Zimmer M., Paull D., Zhang B., Schadt E.E., et al. CRISPR/Cas9-Correctable Mutation-Related Molecular and Physiological Phenotypes in iPSC-Derived Alzheimer’s PSEN2 N141I Neurons. Acta Neuropathol. Commun. 2017;5:77. doi: 10.1186/s40478-017-0475-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Cooper O., Seo H., Andrabi S., Guardia-Laguarta C., Graziotto J., Sundberg M., McLean J.R., Carrillo-Reid L., Xie Z., Osborn T., et al. Pharmacological Rescue of Mitochondrial Deficits in iPSC-Derived Neural Cells from Patients with Familial Parkinson’s Disease. Sci. Transl. Med. 2012;4:141ra90. doi: 10.1126/scitranslmed.3003985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Woodard C.M., Campos B.A., Kuo S.-H., Nirenberg M.J., Nestor M.W., Zimmer M., Mosharov E.V., Sulzer D., Zhou H., Paull D., et al. iPSC-Derived Dopamine Neurons Reveal Differences between Monozygotic Twins Discordant for Parkinson’s Disease. Cell Rep. 2014;9:1173–1182. doi: 10.1016/j.celrep.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Ochalek A., Mihalik B., Avci H.X., Chandrasekaran A., Téglási A., Bock I., Giudice M.L., Táncos Z., Molnár K., László L., et al. Neurons Derived from Sporadic Alzheimer’s Disease iPSCs Reveal Elevated TAU Hyperphosphorylation, Increased Amyloid Levels, and GSK3B Activation. Alzheimers. Res. Ther. 2017;9:90. doi: 10.1186/s13195-017-0317-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Choi S.H., Kim Y.H., Hebisch M., Sliwinski C., Lee S., D’Avanzo C., Chen H., Hooli B., Asselin C., Muffat J., et al. A Three-Dimensional Human Neural Cell Culture Model of Alzheimer’s Disease. Nature. 2014;515:274–278. doi: 10.1038/nature13800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Penney J., Ralvenius W.T., Tsai L.-H. Modeling Alzheimer’s Disease with iPSC-Derived Brain Cells. Mol. Psychiatry. 2020;25:148–167. doi: 10.1038/s41380-019-0468-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Alić I., Goh P.A., Murray A., Portelius E., Gkanatsiou E., Gough G., Mok K.Y., Koschut D., Brunmeir R., Yeap Y.J., et al. Correction: Patient-Specific Alzheimer-like Pathology in Trisomy 21 Cerebral Organoids Reveals BACE2 as a Gene Dose-Sensitive AD Suppressor in Human Brain. Mol. Psychiatry. 2021;26:5789. doi: 10.1038/s41380-021-01206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Gonzalez C., Armijo E., Bravo-Alegria J., Becerra-Calixto A., Mays C.E., Soto C. Modeling Amyloid Beta and Tau Pathology in Human Cerebral Organoids. Mol. Psychiatry. 2018;23:2363–2374. doi: 10.1038/s41380-018-0229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Meharena H.S., Marco A., Dileep V., Lockshin E.R., Akatsu G.Y., Mullahoo J., Watson L.A., Ko T., Guerin L.N., Abdurrob F., et al. Down-Syndrome-Induced Senescence Disrupts the Nuclear Architecture of Neural Progenitors. Cell Stem Cell. 2022;29:116–130.e7. doi: 10.1016/j.stem.2021.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Tian R., Abarientos A., Hong J., Hashemi S.H., Yan R., Dräger N., Leng K., Nalls M.A., Singleton A.B., Xu K., et al. Genome-Wide CRISPRi/a Screens in Human Neurons Link Lysosomal Failure to Ferroptosis. Nat. Neurosci. 2021;24:1020–1034. doi: 10.1038/s41593-021-00862-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Tian R., Gachechiladze M.A., Ludwig C.H., Laurie M.T., Hong J.Y., Nathaniel D., Prabhu A.V., Fernandopulle M.S., Patel R., Abshari M., et al. CRISPR Interference-Based Platform for Multimodal Genetic Screens in Human iPSC-Derived Neurons. Neuron. 2019;104:239–255.e12. doi: 10.1016/j.neuron.2019.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Dräger N.M., Sattler S.M., Huang C.T.-L., Teter O.M., Leng K., Hashemi S.H., Hong J., Aviles G., Clelland C.D., Zhan L., et al. A CRISPRi/a Platform in iPSC-Derived Microglia Uncovers Regulators of Disease States. bioRxiv. 2022 doi: 10.1038/s41593-022-01131-4. bioRxiv:2021.06.16.448639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Tang X.-Y., Xu L., Wang J., Hong Y., Wang Y., Zhu Q., Wang D., Zhang X.-Y., Liu C.-Y., Fang K.-H., et al. DSCAM/PAK1 Pathway Suppression Reverses Neurogenesis Deficits in iPSC-Derived Cerebral Organoids from Patients with Down Syndrome. J. Clin. Investig. 2021;131:e135763. doi: 10.1172/JCI135763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Bowles K.R., Silva M.C., Whitney K., Bertucci T., Berlind J.E., Lai J.D., Garza J.C., Boles N.C., Mahali S., Strang K.H., et al. ELAVL4, Splicing, and Glutamatergic Dysfunction Precede Neuron Loss in MAPT Mutation Cerebral Organoids. Cell. 2021;184:4547–4563.e17. doi: 10.1016/j.cell.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Staats K.A., Seah C., Sahimi A., Wang Y., Koutsodendris N., Lin S., Kim D., Chang W.-H., Gray K.A., Shi Y., et al. Small Molecule Inhibition of PIKFYVE Kinase Rescues Gain- and Loss-of-Function C9ORF72 ALS/FTD Disease Processes in Vivo. bioRxiv. 2019 bioRxiv:685800. [Google Scholar]
- 237.Elston G.N. Cortex, Cognition and the Cell: New Insights into the Pyramidal Neuron and Prefrontal Function. Cereb. Cortex. 2003;13:1124–1138. doi: 10.1093/cercor/bhg093. [DOI] [PubMed] [Google Scholar]
- 238.Kriegstein A., Noctor S., Martínez-Cerdeño V. Patterns of Neural Stem and Progenitor Cell Division May Underlie Evolutionary Cortical Expansion. Nat. Rev. Neurosci. 2006;7:883–890. doi: 10.1038/nrn2008. [DOI] [PubMed] [Google Scholar]
- 239.Borrell V., Reillo I. Emerging Roles of Neural Stem Cells in Cerebral Cortex Development and Evolution. Dev. Neurobiol. 2012;72:955–971. doi: 10.1002/dneu.22013. [DOI] [PubMed] [Google Scholar]
- 240.Borrell V., Calegari F. Mechanisms of Brain Evolution: Regulation of Neural Progenitor Cell Diversity and Cell Cycle Length. Neurosci. Res. 2014;86:14–24. doi: 10.1016/j.neures.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 241.Molnár Z., Métin C., Stoykova A., Tarabykin V., Price D.J., Francis F., Meyer G., Dehay C., Kennedy H. Comparative Aspects of Cerebral Cortical Development. Eur. J. Neurosci. 2006;23:921–934. doi: 10.1111/j.1460-9568.2006.04611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Rakic P. Evolution of the Neocortex: A Perspective from Developmental Biology. Nat. Rev. Neurosci. 2009;10:724–735. doi: 10.1038/nrn2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Rakic P. Developmental and Evolutionary Adaptations of Cortical Radial Glia. Cereb. Cortex. 2003;13:541–549. doi: 10.1093/cercor/13.6.541. [DOI] [PubMed] [Google Scholar]
- 244.Monuki E.S., Walsh C.A. Mechanisms of Cerebral Cortical Patterning in Mice and Humans. Nat. Neurosci. 2001;4:1199–1206. doi: 10.1038/nn752. [DOI] [PubMed] [Google Scholar]
- 245.Chenn A., Walsh C.A. Regulation of Cerebral Cortical Size by Control of Cell Cycle Exit in Neural Precursors. Science. 2002;297:365–369. doi: 10.1126/science.1074192. [DOI] [PubMed] [Google Scholar]
- 246.Kuida K., Haydar T.F., Kuan C.Y., Gu Y., Taya C., Karasuyama H., Su M.S., Rakic P., Flavell R.A. Reduced Apoptosis and Cytochrome c-Mediated Caspase Activation in Mice Lacking Caspase 9. Cell. 1998;94:325–337. doi: 10.1016/S0092-8674(00)81476-2. [DOI] [PubMed] [Google Scholar]
- 247.Lui J.H., Hansen D.V., Kriegstein A.R. Development and Evolution of the Human Neocortex. Cell. 2011;146:18–36. doi: 10.1016/j.cell.2011.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Dehay C., Giroud P., Berland M., Killackey H.P., Kennedy H. Phenotypic Characterisation of Respecified Visual Cortex Subsequent to Prenatal Enucleation in the Monkey: Development of Acetylcholinesterase and Cytochrome Oxidase Patterns. J. Comp. Neurol. 1996;376:386–402. doi: 10.1002/(SICI)1096-9861(19961216)376:3<386::AID-CNE3>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 249.Sulovari A., Li R., Audano P.A., Porubsky D., Vollger M.R., Logsdon G.A., Human Genome Structural Variation Consortium. Warren W.C., Pollen A.A., Chaisson M.J.P., et al. Human-Specific Tandem Repeat Expansion and Differential Gene Expression during Primate Evolution. Proc. Natl. Acad. Sci. USA. 2019;116:23243–23253. doi: 10.1073/pnas.1912175116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Dougherty M.L., Underwood J.G., Nelson B.J., Tseng E., Munson K.M., Penn O., Nowakowski T.J., Pollen A.A., Eichler E.E. Transcriptional Fates of Human-Specific Segmental Duplications in Brain. Genome Res. 2018;28:1566–1576. doi: 10.1101/gr.237610.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Kronenberg Z.N., Fiddes I.T., Gordon D., Murali S., Cantsilieris S., Meyerson O.S., Underwood J.G., Nelson B.J., Chaisson M.J.P., Dougherty M.L., et al. High-Resolution Comparative Analysis of Great Ape Genomes. Science. 2018;360:eaar6343. doi: 10.1126/science.aar6343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Pollard K.S., Salama S.R., Lambert N., Lambot M.-A., Coppens S., Pedersen J.S., Katzman S., King B., Onodera C., Siepel A., et al. An RNA Gene Expressed during Cortical Development Evolved Rapidly in Humans. Nature. 2006;443:167–172. doi: 10.1038/nature05113. [DOI] [PubMed] [Google Scholar]
- 253.Fiddes I.T., Lodewijk G.A., Mooring M., Bosworth C.M., Ewing A.D., Mantalas G.L., Novak A.M., van den Bout A., Bishara A., Rosenkrantz J.L., et al. Human-Specific NOTCH2NL Genes Affect Notch Signaling and Cortical Neurogenesis. Cell. 2018;173:1356–1369.e22. doi: 10.1016/j.cell.2018.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Suzuki I.K., Gacquer D., Van Heurck R., Kumar D., Wojno M., Bilheu A., Herpoel A., Lambert N., Cheron J., Polleux F., et al. Human-Specific NOTCH2NL Genes Expand Cortical Neurogenesis through Delta/Notch Regulation. Cell. 2018;173:1370–1384.e16. doi: 10.1016/j.cell.2018.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Trujillo C.A., Rice E.S., Schaefer N.K., Chaim I.A., Wheeler E.C., Madrigal A.A., Buchanan J., Preissl S., Wang A., Negraes P.D., et al. Reintroduction of the Archaic Variant of NOVA1 in Cortical Organoids Alters Neurodevelopment. Science. 2021;371:eaax2537. doi: 10.1126/science.aax2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Gallego Romero I., Pavlovic B.J., Hernando-Herraez I., Zhou X., Ward M.C., Banovich N.E., Kagan C.L., Burnett J.E., Huang C.H., Mitrano A., et al. A Panel of Induced Pluripotent Stem Cells from Chimpanzees: A Resource for Comparative Functional Genomics. Elife. 2015;4:e07103. doi: 10.7554/eLife.07103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Otani T., Marchetto M.C., Gage F.H., Simons B.D., Livesey F.J. 2D and 3D Stem Cell Models of Primate Cortical Development Identify Species-Specific Differences in Progenitor Behavior Contributing to Brain Size. Cell Stem Cell. 2016;18:467–480. doi: 10.1016/j.stem.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Marchetto M.C., Hrvoj-Mihic B., Kerman B.E., Yu D.X., Vadodaria K.C., Linker S.B., Narvaiza I., Santos R., Denli A.M., Mendes A.P., et al. Species-Specific Maturation Profiles of Human, Chimpanzee and Bonobo Neural Cells. Elife. 2019;8:e37527. doi: 10.7554/eLife.37527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Field A.R., Jacobs F.M.J., Fiddes I.T., Phillips A.P.R., Reyes-Ortiz A.M., LaMontagne E., Whitehead L., Meng V., Rosenkrantz J.L., Olsen M., et al. Structurally Conserved Primate LncRNAs Are Transiently Expressed during Human Cortical Differentiation and Influence Cell-Type-Specific Genes. Stem Cell Reports. 2019;12:245–257. doi: 10.1016/j.stemcr.2018.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Mora-Bermúdez F., Badsha F., Kanton S., Camp J.G., Vernot B., Köhler K., Voigt B., Okita K., Maricic T., He Z., et al. Differences and Similarities between Human and Chimpanzee Neural Progenitors during Cerebral Cortex Development. Elife. 2016;5:e18683. doi: 10.7554/eLife.18683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Mora-Bermúdez F., Kanis P., Macak D., Peters J., Naumann R., Xing L., Sarov M., Winkler S., Oegema C.E., Haffner C., et al. Longer Metaphase and Fewer Chromosome Segregation Errors in Modern Human than Neanderthal Brain Development. Sci. Adv. 2022;8:eabn7702. doi: 10.1126/sciadv.abn7702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Benito-Kwiecinski S., Giandomenico S.L., Sutcliffe M., Riis E.S., Freire-Pritchett P., Kelava I., Wunderlich S., Martin U., Wray G.A., McDole K., et al. An Early Cell Shape Transition Drives Evolutionary Expansion of the Human Forebrain. Cell. 2021;184:2084–2102.e19. doi: 10.1016/j.cell.2021.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Kanton S., Boyle M.J., He Z., Santel M., Weigert A., Sanchís-Calleja F., Guijarro P., Sidow L., Fleck J.S., Han D., et al. Organoid Single-Cell Genomic Atlas Uncovers Human-Specific Features of Brain Development. Nature. 2019;574:418–422. doi: 10.1038/s41586-019-1654-9. [DOI] [PubMed] [Google Scholar]
- 264.Agoglia R.M., Sun D., Birey F., Yoon S.-J., Miura Y., Sabatini K., Pașca S.P., Fraser H.B. Primate Cell Fusion Disentangles Gene Regulatory Divergence in Neurodevelopment. Nature. 2021;592:421–427. doi: 10.1038/s41586-021-03343-3. [DOI] [PMC free article] [PubMed] [Google Scholar]