Abstract
Cancer has become a major challenge in the global disease burden. Artificial sweeteners are a class of chemical compounds that are used as food and beverage addition agent to replace sugar. However, the health effects of consuming artificial sweeteners are still unclear. This meta-analysis was performed to evaluate the role of artificial sweeteners on cancer. The databases PubMed, Cochrane Library, MEDLINE, Web of Science and EMBASE were searched up until July 2022. A Newcastle–Ottawa scale (NOS) was used to estimate the study quality. A total of 25 observational studies were included with a total of 3,739,775 subjects. The intake of artificial sweeteners had no apparent association with overall cancer incidence and mortality. However, in Europe, artificial sweeteners’ intake could increase the risk of cancer incidence (HR/RR = 1.07, 95% CI = [1.02, 1.12], I2 = 25.8%, P = 0.223), which appears to be related to a shift in nutritional behaviors in the countries. Significant results were also observed in subgroups with aspartame and a mixed intake of artificial sweeteners. Moreover, higher risk was observed for artificial sweeteners intake in all-cause mortality (HR/RR =1.13, 95% CI = [1.03, 1.25], I2 = 79.7%, p < 0.001) and a J-shaped association between them was found. More data from well-conducted studies and clinical trials are required.
Keywords: artificial sweeteners, cancer, incidence, mortality, meta-analysis
1. Introduction
Cancer has become a major challenge in the global disease burden. A global estimate of 23.6 million new cancer cases and 10.0 million cancer deaths occurred in 2019, which represented a 26.3% and 20.9% increase in new cases and deaths, respectively [1]. It is estimated that the burden of cancer will continue to increase over the next two decades at least [1]. The existing evidence suggests that obesity and cardiovascular disease (CVD) are directly or indirectly promoted by a high-sugar diet [2]. The similar effects of a high-sugar diet are also observed in the rates of cancer [3,4,5,6]. Therefore, as a substitute for sugar in foods and beverages, sweeteners have become more prevalent over the past few decades [7]. High-intensity sweeteners approved by the Food and Drug Administration (FDA) include six artificial sweeteners (saccharin, aspartame, acesulfame potassium (Ace-K), sucralose, neotame and aspartame) and two natural sweeteners (stevia (steviol glycosides) and Monk fruit) [8]. Since natural sweeteners are still in the developing stage in terms of sensory attributes, dominance duration and extraction technology, artificial sweeteners are still widely used [9]. Some of the metabolic and hormonal changes caused by high-calorie sugars either do not occur or are reduced after consuming artificial sweeteners [10]. Studies have indicated that the release of various hormones and markers of postprandial glucose homeostasis, such as insulin and glucagon-like peptide-1 (GLP-1), were not significantly altered when artificial sweeteners are delivered directly to the stomach or intestine. Artificial sweeteners alone do not stimulate insulin or incretin release [11,12,13]. In fact, the health and metabolic effects of consuming artificial sweeteners are unclear, and the debate about whether artificial sweeteners themselves increase cancer risk is still not solved. As early as 1970, based on the results of animal experiments, the FDA have suspected that cyclamate (sodium cyclohexyl sulfamate) could induce cancer, thus banning its use in all dietary foods and fruits in the United States [7].
Nowadays, according to the latest report, there is at least a third of adults and children who consume artificial sweeteners regularly in the United States, Europe and Australia [14]. It is due to the increasing availability of new artificial sweeteners and the rising obesity epidemic, thus more “low-calorie” products, especially beverages, are being used [15,16]. Therefore, artificial sweeteners have again been linked to cancer. Although the effect of consumption of artificial sweeteners on gastrointestinal cancers and the intake of soft drinks on the mortality of cancer have been examined via meta-analysis, it is unclear whether artificial sweeteners cause cancer in any form [17,18]. Our study aimed to evaluate the role of artificial sweeteners on the risk of cancer incidence and mortality and all-cause mortality based on the data from all of the current prospective cohort studies.
2. Materials and Methods
2.1. Sources and Methods of Data Retrieval
The PubMed, Web of Science, MEDLINE, Cochrane Library and EMBASE databases were searched up to July 2022, and the used keywords included artificial sweetener, aspartame, artificially sweetened beverage (ASBs), cancer and tumor, to screen and identify published literatures. The search had no restriction on publication date or language. The detailed search strategy of PubMed that was performed is shown in Table S1.
2.2. Inclusion Criteria
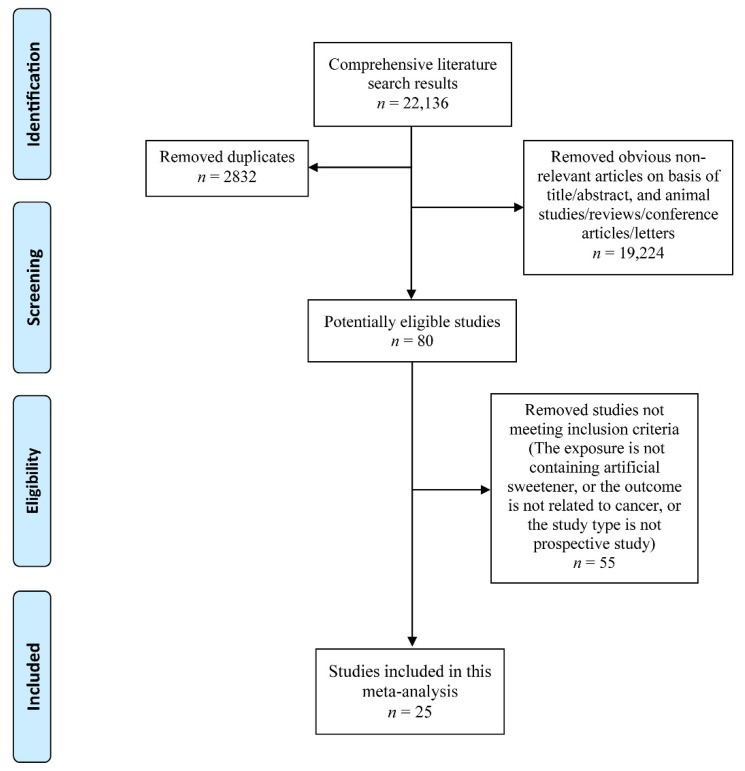
The inclusion criteria were as follows: (1) exposure: using artificial sweeteners in food, drinks and packets; (2) overall or site-specific cancer incidence or mortality, or all-cause mortality as a consequence; (3) hazard ratio (HR) or risk ratio (RR) with 95% confidence interval (CI) for the association between artificial sweetener and any type of cancer incidence and mortality was estimated; (4) animal studies, in vitro studies, duplicates, reviews, or conference papers were excluded. Two researchers independently assessed all of the included studies, resolved disagreements via discussion and collected final eligible literatures (Figure 1).
Figure 1.
Flow diagram of the literature search and selection.
2.3. Data Extraction and Risk of Bias within Individual Studies
A literature review was conducted to extract the following data: publication year, first author, region, cancer type, usage of artificial sweeteners (including type and dose) and outcome of studies. Based on the Newcastle–Ottawa scale (NOS), the bias risk for the included study was estimated [19].
2.4. Statistical Analysis
Statistical analysis was carried out with the software Stata12.0. Statistics heterogeneity was evaluated using the I2 statistic and p < 0.05 was considered significant. In our study, random effects models were used in all of the analyses based on the level of heterogeneity. Egger’s test was employed to gauge publication bias, while the trim-and-fill approach was used to correct results and analyze the influence of bias on them [20,21]. Subgroup analyses were performed based on the region (Europe, Americas and Oceania), cancer type (obesity-related cancers and non-obesity-related cancers), type of artificial sweetener intake (ASBs alone or mixed intake (including drinks, packet and other methods)) and role of aspartame intake alone. Specially, all of the malignancies that include obesity as one of the risk factors or protective variables in their genesis are considered to be obesity-related cancers including colorectal cancer, gastric cancer, breast cancer, liver cancer, etc. Moreover, meta-regression was also conducted to confirm the source of heterogeneity.
3. Results
A total of 25 studies met our inclusion criteria, which contained 3,739,775 subjects (Table 1) [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]. Among them, the relationship between artificial sweeteners and cancer incidence was analyzed in 14 studies, and the risk of artificial sweeteners intake for cancer or all-cause mortality was assessed in the rest of the papers. The average score of NOS in all of the included studies was 8.52 (range 7–9).
Table 1.
Details of included studies.
| Author | Year | Region | Sample Size | NOS | Cancer Type | Type of Artificial Sweetener Intake | Aspartame Intake Only | Follow-Up Time | Dose of Artificial Sweetener | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Heath A. K. et al [26]. | 2021 | Europe | 281,483 | 8 | Kidney Cancer | ASBs alone | No | Incidence (15 years); Mortality (16 years) | per 100 g/day increment | Incidence/Cancer Mortality |
| Romanos-Nanclares A. et al [22]. | 2021 | US | 175,798 | 9 | Breast Cancer | ASBs alone | No | 36 years | ≥1/day | Incidence |
| Debras C. et al [25]. | 2022 | France | 102,865 | 9 | Cancer (unclassified) | Mixed intake | Yes | 7.8 years | >17.44 mg/day in men and >19.00 mg/day in women | Incidence |
| Chazelas E. et al [24]. (1). | 2019 | France | 101,257 | 9 | Breast Cancer | ASBs alone | No | 5.1 years | >7.9 mL/day in men and >11.6 mL/day in women | Incidence |
| Chazelas E. et al [24]. (2). | Colorectal Cancer | |||||||||
| Chazelas E. et al [24]. (3). | Prostate Cancer | |||||||||
| Navarrete-Munoz E. M. et al [32]. | 2016 | Europe | 477,199 | 9 | Pancreatic Cancer | ASBs alone | No | 11.60 years | >92.2 g/day | Incidence |
| Schernhammer E. S. et al [33]. | 2012 | US | 125,028 | 9 | Hematopoietic Malignancy | Mixed intake | Yes | 22 years | † | Incidence |
| Hodge A. M. et al [27]. (1). | 2018 | Australia | 35,593 | 9 | Prostate Cancer | ASBs alone | No | 9–17 years | ≥1/day | Incidence |
| Hodge A. M. et al [27]. (2). | Ovary Cancer | |||||||||
| Hodge A. M. et al [27]. (3). | Kidney Cancer | |||||||||
| Hodge A. M. et al [27]. (4). | Colorectal Cancer | |||||||||
| Hodge A. M. et al [27]. (5). | Breast Cancer | |||||||||
| Hodge A. M. et al [27]. (6). | Endometrium Cancer | |||||||||
| Hodge A. M. et al [27]. (7). | Gastric Cancer | |||||||||
| Hur J. et al [28]. | 2021 | US | 95,464 | 8 | Colorectal Cancer | ASBs alone | No | 24 years | ≥2 servings/day | Incidence |
| Bassett J. K. et al [23]. | 2019 | Australia | 35,109 | 9 | Cancers not related to obesity | ASBs alone | No | 19 years | >1/day | Incidence |
| Stepien M. et al [34]. | 2016 | Europe | 477,206 | 7 | Liver Cancer | ASBs alone | No | 11.4 years | per 1 serving/day increment | Incidence |
| McCullough M. L. et al [31]. | 2014 | US | 100,442 | 9 | Hematopoietic Malignancy | Mixed intake | Yes | 10 years | ≥1 can/day | Incidence |
| Lim U. et al [30]. (1). | 2006 | US | 473,984 | 8 | Hematopoietic Malignancy | Mixed intake | Yes | 5 years | ≥600 mg/d | Incidence |
| Lim U. et al [30]. (2). | Gliomas | |||||||||
| Inoue-Choi M. et al [29]. | 2013 | US | 23,039 | 8 | Endometrial Cancer | ASBs alone | No | 24 years | 2.8–64.1 servings/week | Incidence |
| Zamora-Ros R. et al [42]. | 2022 | Europe | 450,064 | 8 | Thyroid cancer | ASBs alone | No | 14 years | 43.0–3389.5 mL/d | Incidence |
| Guercio B. J. et al [36]. | 2018 | US | 1018 | 8 | Colorectal Cancer | ASBs alone | No | 10 months | ≥2 servings/day | Cancer Mortality |
| Farvid M. S. et al [35]. | 2021 | US | 8863 | 8 | Breast Cancer | ASBs alone | No | 11.5 years | >3 servings/week | Cancer Mortality |
| Zhang Y. B. et al [39]. | 2020 | US | 31,402 | 8 | Cancer (unclassified) | ASBs alone | No | 7.9 years | ≥2 servings/day | Cancer/All-Cause Mortality |
| Zoltick E. S. et al [40]. | 2021 | US | 1463 | 9 | Colorectal Cancer | ASBs alone | No | 8.0 years | per 1 serving/day increment | Cancer Mortality |
| Mullee A. et al [38]. (1). | 2019 | Europe | 252,357 | 9 | Colorectal Cancer | ASBs alone | No | 16.4 years | ≥1 servings/day | Cancer/All-Cause Mortality |
| Mullee A. et al [38]. (2). | Breast Cancer | |||||||||
| Mullee A. et al [38]. (3). | Prostate Cancer | |||||||||
| Malik V. S. et al [37]. (1). | 2019 | US | 85,030 | 9 | Lung Cancer | ASBs alone | No | 34 years | ≥2 servings/day | Cancer/All-Cause Mortality |
| Malik V. S. et al [37]. (2). | Colorectal Cancer | |||||||||
| Malik V. S. et al [37]. (3). | Breast Cancer | |||||||||
| Malik V. S. et al [37]. (4). | Prostate Cancer | |||||||||
| Liu D. et al [41]. | 2022 | Europe | 51,874 | 9 | Cancer (unclassified) | ASBs alone | No | 7.0 years | >4.5 servings /day | Cancer/All-Cause Mortality |
| Vyas A. et al [44]. | 2014 | Columbia | 59,614 | 9 | - | ASBs alone | No | 8.7 years | ≥2/day | All-Cause Mortality |
| Anderson J. J. et al [45]. | 2020 | Europe | 198,285 | 9 | - | ASBs alone | No | 7 years | >2/day | All-Cause Mortality |
| Paganini-Hill A. et al [46]. | 2007 | US | 13,624 | 8 | - | ASBs alone | No | 23 years | >1 can/week | All-Cause Mortality |
| Mossavar-Rahmani Y. et al [43]. | 2019 | US | 81,714 | 8 | - | ASBs alone | No | 11.9 years | ≥2/day | All-Cause Mortality |
ASBs: artificially sweetened beverages; NOS: Newcastle–Ottawa scale. †: Aspartame intake was divided into 5 categories by quantiles, but specific values for each category were not provided.
3.1. Risk of Cancer Incidence
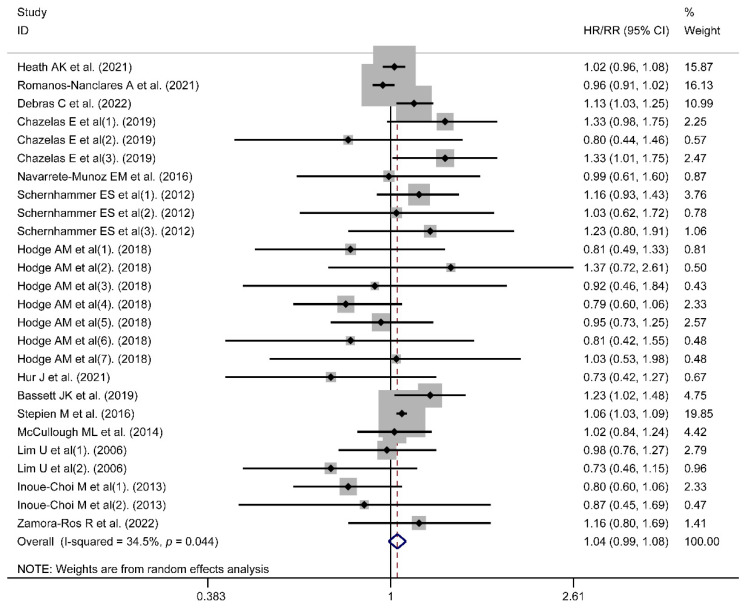
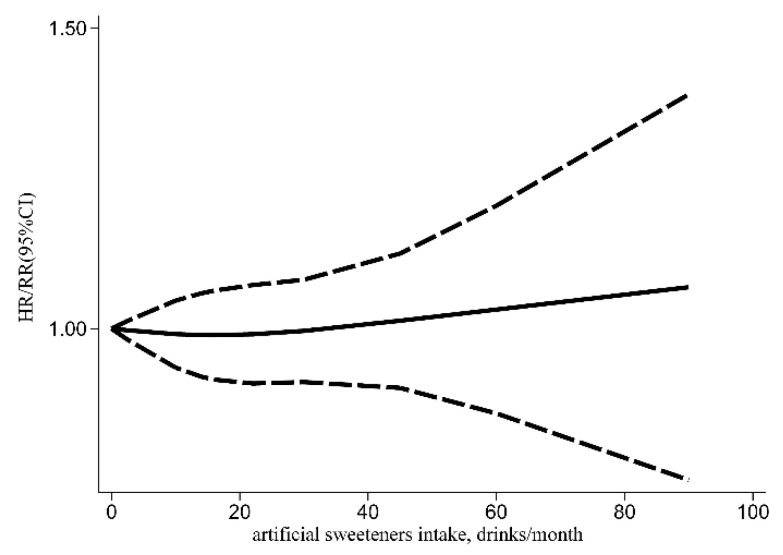
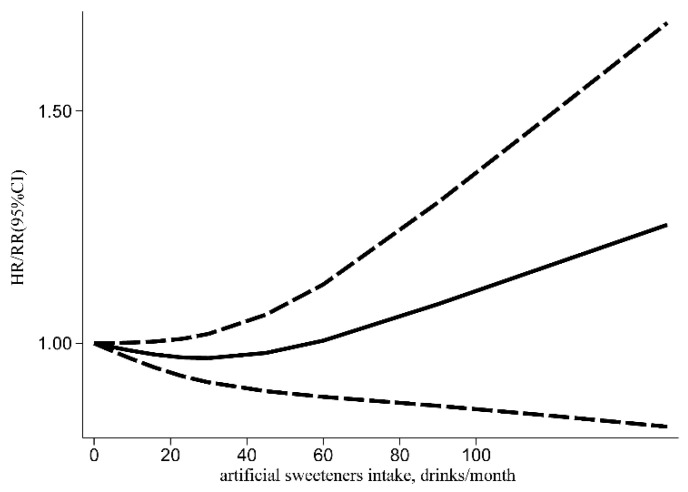
A meta-analysis was performed in 14 included studies to evaluate the link between artificial sweeteners intake and cancer incidence. The results indicated that no association existed (HR/RR = 1.04, 95% CI = [0.99, 1.08], I2 = 34.5%, p = 0.044; Figure 2). Simultaneously, publication bias was not found in the results of cancer incidence (Egger’s test: coefficient = −0.234, t = −0.77, p = 0.450). According to the subgroup analysis of region, artificial sweeteners’ intake could increase the risk of cancer incidence in the European group (HR/RR = 1.07, 95% CI = [1.02, 1.12], I2 = 25.8%, p = 0.223). Meanwhile, artificial sweeteners’ mixed intake could increase the risk of cancer incidence (HR/RR = 1.09, 95% CI = [1.01, 1.18], I2 = 0.0%, p = 0.513). Moreover, significant differences were also observed with aspartame (HR/RR = 1.10, 95% CI = [1.01, 1.19], I2 = 0.0%, p = 0.467) (Table 2). The outcomes of the meta-regression showed that the regional factor could influence the total heterogeneity and effect size (p < 0.05) (Table 3). As a result, the regional factor may be the primary source of heterogeneity, as indicated by the results of the meta-regression and subgroup analyses. The dose–response relationship between artificial sweeteners intake and cancer incidence is shown in Figure 3.
Figure 2.
Meta-analysis results of artificial sweeteners intake for cancer incidence (HR: hazard ratio; RR: relative risk; CI: Confidence Interval) [22,23,24,25,26,27,28,29,30,31,32,33,34,42].
Table 2.
Subgroup analyses were performed for cancer incidence and mortality.
| Outcome | Sub-grouped by | No. of Studies | HR/RR | 95% CI | Heterogeneity I2 (%), p |
|---|---|---|---|---|---|
| Incidence | Region | ||||
| Europe | 6 | 1.07 | (1.02, 1.12) | 25.8%, 0.223 | |
| Americas | 6 | 0.97 | (0.92, 1.02) | 0.0%, 0.476 | |
| Oceania | 2 | 0.99 | (0.85, 1.16) | 25.8%, 0.223 | |
| Cancer type | |||||
| Obesity-related cancers | 7 | 1.01 | (0.94, 1.09) | 51.7%, 0.011 | |
| Cancers not related to obesity | 8 | 1.04 | (0.99, 1.09) | 0.0%, 0.617 | |
| Type of artificial sweetener intake | |||||
| ASBs alone | 10 | 1.02 | (0.97, 1.08) | 42.3%, 0.027 | |
| Mixed intake | 4 | 1.09 | (1.01, 1.18) | 0.0%, 0.513 | |
| Aspartame intake only | |||||
| Yes | 4 | 1.10 | (1.01, 1.19) | 0.0%, 0.467 | |
| No | 10 | 1.02 | (0.97, 1.08) | 42.3%, 0.027 | |
| mortality | Region | ||||
| Europe | 3 | 1.05 | (0.99, 1.13) | 0.0%, 0.502 | |
| Americas | 5 | 0.91 | (0.78, 1.06) | 55.7%, 0.027 | |
| Cancer type | |||||
| Obesity-related cancers | 5 | 0.97 | (0.84, 1.13) | 46.7%, 0.059 | |
| Cancers not related to obesity | 2 | 1.01 | (0.89, 1.15) | 54.4%, 0.139 |
ASBs: artificially sweetened beverages; HR: hazard ratio; RR: relative risk; CI: Confidence Interval.
Table 3.
Meta-regression for cancer incidence.
| Variables | I2 (%) | Adj R2 | Exp (b) | Std. Err. | t | p | 95% CI |
|---|---|---|---|---|---|---|---|
| Region (Europe) | 16.22 | 35.98 | 1.11 | 0.06 | 2.09 | 0.048 | (1.01, 1.23) |
| Region (Oceania) | 1.04 | 0.08 | 0.55 | 0.588 | (0.89, 1.22) | ||
| Cancer type | 35.32 | −46.15 | 0.96 | 0.05 | −0.72 | 0.476 | (0.86, 1.08) |
| Type of artificial sweetener intake | 34.14 | 14.61 | 0.95 | 0.05 | −0.93 | 0.360 | (0.84, 1.07) |
| Aspartame intake only | 34.82 | 16.88 | 1.06 | 0.06 | 0.97 | 0.341 | (0.94, 1.20) |
CI: Confidence Interval.
Figure 3.
Dose–response relationship of artificial sweeteners intake with cancer incidence (HR: hazard ratio; RR: relative risk; CI: Confidence Interval).
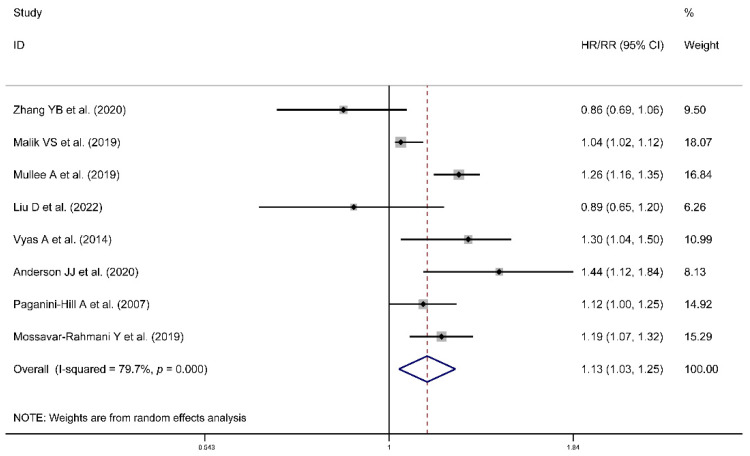
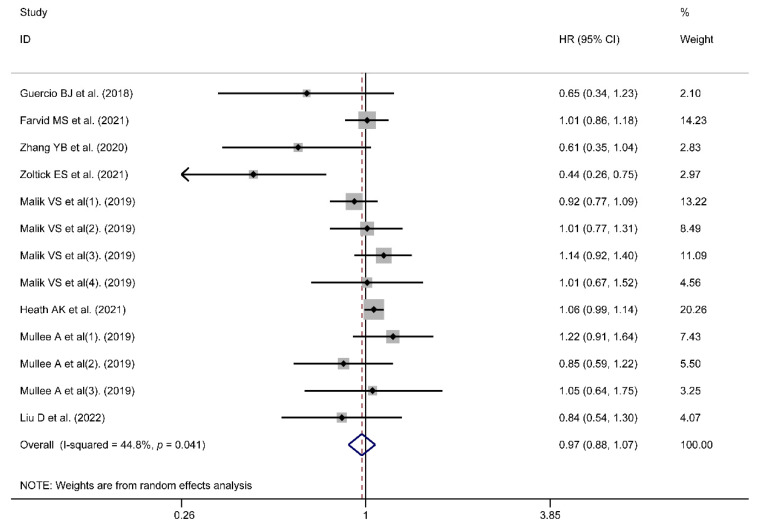
3.2. Risk of All-Cause or Cancer Mortality
Higher risk was observed for artificial sweeteners’ intake in all-cause mortality (HR/RR = 1.13, 95% CI = [1.03, 1.25], I2 = 79.7%, p < 0.001; Figure 4) and a J-shaped association between them was observed (Figure 5). However, the association could not be found in cancer mortality (HR = 0.97, 95% CI = [0.88, 1.07], I2 = 44.8%, p = 0.041; Figure 6). Publication biases were observed in the cancer mortality (Egger’s test: coefficient = −1.224, t = −2.44, p = 0.033). However, no trimming was performed and the data were unchanged after using the trim-and-fill method. As a result, the impact of publication bias was considered minimal and the results were consistent.
Figure 4.
Meta-analysis results of artificial sweeteners intake for all-cause mortality (HR: hazard ratio; RR: relative risk; CI: Confidence Interval) [37,38,39,41,43,44,45,46].
Figure 5.
Dose–response relationship of artificial sweeteners intake with all-cause mortality (HR: hazard ratio; RR: relative risk; CI: Confidence Interval).
Figure 6.
Meta-analysis results of artificial sweeteners intake for cancer mortality (HR: hazard ratio; CI: Confidence Interval) [26,35,36,37,38,39,40,41].
4. Discussion
The idea behind artificial sweeteners was originally to replace the sugar so that using these products would reduce caloric intake, result in weight loss and reduce diabetes mellitus’ incidence [16]. However, existing research has shown that instead of reducing the risk of certain chronic diseases such as obesity, insulin resistance, or coronary artery disease, the use of artificial sweeteners even increases the likelihood of these diseases [47,48,49]. The results of our research demonstrated that artificial sweeteners’ intake seemed not to increase the risk of overall cancer incidence and mortality. However, in Europe, the consumption of artificial sweeteners could increase cancer incidence. This may be related to the fact that European countries are shifting towards a nutritional approach that adopts healthier eating behaviors. Over the past 30 years, dietary consumption patterns in European countries have changed significantly, with the average intake of sugar decreasing and people opting for its alternatives instead [50].
Our meta-analysis found a J-shaped association between artificial sweeteners intakes and all-cause mortality, which was also observed in some original studies and other similar meta-analysis [41,51]. Many previous studies have suggested that a reverse causation was existed [37,45,46]. The participants with the highest intake of artificial sweeteners were more likely to be obese, hypertensive and experience hypercholesterolemia, leading these people to switch to non-caloric sweeteners. Correspondingly, those people consuming artificial sweeteners in small quantities are more likely to have healthier lifestyles and dietary habits. However, almost all of the original studies adjusted for energy metabolism such as BMI and found that the association was attenuated but still significant, suggesting that the association cannot simply be explained by reverse causality. Interestingly, one study mentions that the result may reflect a cognitive process in which artificial sweeteners considered “healthy” allow an excessive consumption of other “unhealthy” foods [46]. Meanwhile, residual confounding could be an alternative explanation. In particular, we did not observe a clear association between artificial sweetener intake and cancer mortality. However, some of the original studies of our meta-analysis observed the association [40]. Although it did not provide a plausible explanation for the corresponding results, other studies have suggested that this may be related to sugar-sweetened foods that may lead to more severe clinical outcomes for patients with colon cancer [36].
Existing evidence indicated that the artificial sweeteners’ intake could indirectly cause a reduction in sugar-sweetened beverages or foods, thus leading to a decrease in the cancer incidence rate related to them [18]. Although most of the literature included in our study regarded artificial sweeteners and sugar-sweetened beverages as control variables mutually, the direct link between artificial sweeteners and cancer could be masked. Meanwhile, our study did not found the difference in the impact of artificial sweeteners on obesity-related cancer and other cancers. The results of the Melbourne Collaborative Cohort Study indicated that an association between artificial sweeteners and obesity-related cancers was not observed [27]. However, the association was found in a recent study [25]. As mentioned above, although the purpose of artificial sweeteners was to reduce obesity by substituting them for sugar, existing evidence suggests that artificial sweeteners could induce metabolic syndrome and the development of obesity by altering the host microbiome and reducing body satiety [16]. Therefore, one explanation for the existence of this association may be driven by overweight-related metabolic disturbances, although BMI and weight gain were adjusted throughout the study [25]. In essence, despite great interest in the potential of low-calorie sweeteners to prevent obesity and its complications, we found little evidence to support their health benefits. It also appears to have limited effects on blood glucose and lipids [52].
In subgroup analyses, we evaluated the effect of artificially sweetened beverages or aspartame intake alone. Aspartame, a well-known artificial sweetener, is now used as a sweetener and flavor enhancer in six thousand food products worldwide [33]. Notably, although aspartame is one of the most studied food additives, its safety remains controversial [31]. Formaldehyde, a metabolic byproduct of aspartame, is an established carcinogen that can cause DNA damage, chromosomal aberrations and mitotic errors [53,54]. Soffritti et al. found that it plays a major role in aspartame-induced carcinogenesis in the liver and lungs in mice [55]. Our meta-analysis also found a specific effect of aspartame intake on cancer. However, although aspartame exposure proved to increase incidence of lymphoma and leukemia in rats with a dose–response relationship in an Italian study, the European Food Safety Authority dismissed the findings due to the high rates of infection and inflammation in these animals, as well as the uncertainty of diagnosis [56,57]. In addition, recent studies have suggested that the measurements of ASBs might not be sufficient to accurately describe the overall dietary exposure to artificial sweeteners [25]. Through subgroup analysis, we found that although the effects of artificial sweeteners on cancer incidence were different based on the different intake type, a mixed intake of artificial sweeteners could increase the risk of cancer incidence, which seems to confirm the above view. Of course, given that there are fewer studies on aspartame or a mixed intake of artificial sweeteners, we hope to have more data in the future to clarify their relationship with cancer.
Some limitations existed in our study. Although almost all of the original literature included are large-scale, prospective studies with long-term follow-up, the reliability of causal conclusions may not be as robust because they are all observational studies. Although possible confounding factors were adjusted in the original studies, the findings should be cautiously interpreted given the existence of residual confounding. Meanwhile, more data are also required to evaluate the effects of other artificial sweeteners on cancer.
5. Conclusions
Our meta-analysis indicated that artificial sweeteners’ intake could increase the risk of all-cause mortality, but the relationship was not observed in the risk of overall cancer incidence and mortality. However, in Europe, the consumption of artificial sweeteners could increase cancer incidence. More data from well-conducted studies and clinical trials are required to confirm the association.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14183742/s1, Table S1: Search strategy (PubMed).
Author Contributions
Conceptualization, S.Y. and W.C.; Data curation, S.Y.; Formal analysis, S.Y. and F.Y.; Funding acquisition, S.L.; Methodology, W.C.; Project administration, S.L.; Software, S.Y.; Supervision, B.L., S.L. and W.C.; Visualization, S.Y. and L.L.; Writing—original draft, S.Y.; Writing—review and editing, S.Y., F.Y., L.L. and W.C. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kocarnik J.M., Compton K., Dean F.E., Fu W., Gaw B.L., Harvey J.D., Henrikson H.J., Lu D., Pennini A., Xu R., et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022;8:420–444. doi: 10.1001/jamaoncol.2021.6987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stanhope K.L. Sugar consumption, metabolic disease and obesity: The state of the controversy. Crit. Rev. Clin. Lab. Sci. 2016;53:52–67. doi: 10.3109/10408363.2015.1084990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kushi L.H., Doyle C., McCullough M., Rock C.L., Demark-Wahnefried W., Bandera E.V., Gapstur S., Patel A.V., Andrews K., Gansler T. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: Reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Clin. 2012;62:30–67. doi: 10.3322/caac.20140. [DOI] [PubMed] [Google Scholar]
- 4.Qin B., Moorman P.G., Alberg A.J., Barnholtz-Sloan J.S., Bondy M., Cote M.L., Funkhouser E., Peters E.S., Schwartz A.G., Terry P., et al. Dietary carbohydrate intake, glycaemic load, glycaemic index and ovarian cancer risk in African-American women. Br. J. Nutr. 2016;115:694–702. doi: 10.1017/S0007114515004882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romieu I., Ferrari P., Rinaldi S., Slimani N., Jenab M., Olsen A., Tjonneland A., Overvad K., Boutron-Ruault M.C., Lajous M., et al. Dietary glycemic index and glycemic load and breast cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) Am. J. Clin. Nutr. 2012;96:345–355. doi: 10.3945/ajcn.111.026724. [DOI] [PubMed] [Google Scholar]
- 6.Sieri S., Krogh V., Agnoli C., Ricceri F., Palli D., Masala G., Panico S., Mattiello A., Tumino R., Giurdanella M.C., et al. Dietary glycemic index and glycemic load and risk of colorectal cancer: Results from the EPIC-Italy study. Int. J. Cancer. 2015;136:2923–2931. doi: 10.1002/ijc.29341. [DOI] [PubMed] [Google Scholar]
- 7.Weihrauch M.R., Diehl V. Artificial sweeteners—Do they bear a carcinogenic risk? Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2004;15:1460–1465. doi: 10.1093/annonc/mdh256. [DOI] [PubMed] [Google Scholar]
- 8.Muenprasitivej N., Tao R., Nardone S.J., Cho S. The Effect of Steviol Glycosides on Sensory Properties and Acceptability of Ice Cream. Foods. 2022;11:1745. doi: 10.3390/foods11121745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chadha D., Hamid N., Kantono K., Marsan M. Changes in temporal sensory profile, liking, satiety, and postconsumption attributes of yogurt with natural sweeteners. J. Food Sci. 2022;87:3190–3206. doi: 10.1111/1750-3841.16224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swithers S.E. Artificial sweeteners produce the counterintuitive effect of inducing metabolic derangements. Trends Endocrinol. Metab. TEM. 2013;24:431–441. doi: 10.1016/j.tem.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma J., Bellon M., Wishart J.M., Young R., Blackshaw L.A., Jones K.L., Horowitz M., Rayner C.K. Effect of the artificial sweetener, sucralose, on gastric emptying and incretin hormone release in healthy subjects. Am. J. Physiol. Gastrointest. Liver Physiol. 2009;296:G735–G739. doi: 10.1152/ajpgi.90708.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma J., Chang J., Checklin H.L., Young R.L., Jones K.L., Horowitz M., Rayner C.K. Effect of the artificial sweetener, sucralose, on small intestinal glucose absorption in healthy human subjects. Br. J. Nutr. 2010;104:803–806. doi: 10.1017/S0007114510001327. [DOI] [PubMed] [Google Scholar]
- 13.Steinert R.E., Frey F., Töpfer A., Drewe J., Beglinger C. Effects of carbohydrate sugars and artificial sweeteners on appetite and the secretion of gastrointestinal satiety peptides. Br. J. Nutr. 2011;105:1320–1328. doi: 10.1017/S000711451000512X. [DOI] [PubMed] [Google Scholar]
- 14.Sylvetsky A.C., Rother K.I. Trends in the consumption of low-calorie sweeteners. Physiol. Behav. 2016;164 Pt B:446–450. doi: 10.1016/j.physbeh.2016.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson R.K., Lichtenstein A.H., Anderson C.A.M., Carson J.A., Després J.P., Hu F.B., Kris-Etherton P.M., Otten J.J., Towfighi A., Wylie-Rosett J. Low-Calorie Sweetened Beverages and Cardiometabolic Health: A Science Advisory From the American Heart Association. Circulation. 2018;138:e126–e140. doi: 10.1161/CIR.0000000000000569. [DOI] [PubMed] [Google Scholar]
- 16.Pearlman M., Obert J., Casey L. The Association Between Artificial Sweeteners and Obesity. Curr. Gastroenterol. Rep. 2017;19:64. doi: 10.1007/s11894-017-0602-9. [DOI] [PubMed] [Google Scholar]
- 17.Pan B., Ge L., Lai H., Wang Q., Wang Q., Zhang Q., Yin M., Li S., Tian J., Yang K., et al. Association of soft drink and 100% fruit juice consumption with all-cause mortality, cardiovascular diseases mortality, and cancer mortality: A systematic review and dose-response meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 2021:1–12. doi: 10.1080/10408398.2021.1937040. [DOI] [PubMed] [Google Scholar]
- 18.Tepler A., Hoffman G., Jindal S., Narula N., Shah S.C. Intake of artificial sweeteners among adults is associated with reduced odds of gastrointestinal luminal cancers: A meta-analysis of cohort and case-control studies. Nutr. Res. 2021;93:87–98. doi: 10.1016/j.nutres.2021.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wells G.A.S.B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. [(accessed on 5 August 2022)]. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 20.Egger M. Bias in meta-analysis detected by a simple, graphical test. BMJ Br. Med. J. 1997;315:629. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duval S., Tweedie R. A Nonparametric “Trim and Fill” Method of Accounting for Publication Bias in Meta-Analysis. J. Am. Stat. Assoc. 2000;95:89–98. [Google Scholar]
- 22.Andrea R.N., Collins L.C., Hu F.B., Willett W.C., Rosner B.A., Estefania T., Heather E.A. Sugar-Sweetened Beverages, Artificially Sweetened Beverages, and Breast Cancer Risk: Results From 2 Prospective US Cohorts. J. Nutr. 2021;151:2768–2779. doi: 10.1093/jn/nxab172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bassett J.K., Milne R.L., English D.R., Giles G.G., Hodge A.M. Consumption of sugar-sweetened and artificially sweetened soft drinks and risk of cancers not related to obesity. Int. J. Cancer. 2020;146:3329–3334. doi: 10.1002/ijc.32772. [DOI] [PubMed] [Google Scholar]
- 24.Chazelas E., Srour B., Desmetz E., Kesse-Guyot E., Julia C., Deschamps V., Druesne-Pecollo N., Galan P., Hercberg S., Latino-Martel P., et al. Sugary drink consumption and risk of cancer: Results from NutriNet-Santé prospective cohort. BMJ. 2019;366:l2408. doi: 10.1136/bmj.l2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Debras C., Chazelas E., Srour B., Druesne-Pecollo N., Esseddik Y., Szabo de Edelenyi F., Agaësse C., De Sa A., Lutchia R., Gigandet S., et al. Artificial sweeteners and cancer risk: Results from the NutriNet-Santé population-based cohort study. PLoS Med. 2022;19:e1003950. doi: 10.1371/journal.pmed.1003950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heath A.K., Clasen J.L., Jayanth N.P., Jenab M., Tjønneland A., Petersen K.E.N., Overvad K., Srour B., Katzke V., Bergmann M.M., et al. Soft Drink and Juice Consumption and Renal Cell Carcinoma Incidence and Mortality in the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol. Biomark. Prev. 2021;30:1270–1274. doi: 10.1158/1055-9965.EPI-20-1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hodge A.M., Bassett J.K., Milne R.L., English D.R., Giles G.G. Consumption of sugar-sweetened and artificially sweetened soft drinks and risk of obesity-related cancers. Public Health Nutr. 2018;21:1618–1626. doi: 10.1017/S1368980017002555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hur J., Otegbeye E., Joh H.-K., Nimptsch K., Ng K., Ogino S., Meyerhardt J.A., Chan A.T., Willett W.C., Wu K., et al. Sugar-sweetened beverage intake in adulthood and adolescence and risk of early-onset colorectal cancer among women. Gut. 2021;70:2222–2223. doi: 10.1136/gutjnl-2020-323450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Inoue-Choi M., Robien K., Mariani A., Cerhan J.R., Anderson K.E. Sugar-sweetened beverage intake and the risk of type I and type II endometrial cancer among postmenopausal women. Cancer Epidemiol. Biomark. Prev. 2013;22:2384–2394. doi: 10.1158/1055-9965.EPI-13-0636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lim U., Subar A.F., Mouw T., Hartge P., Morton L.M., Stolzenberg-Solomon R., Campbell D., Hollenbeck A.R., Schatzkin A. Consumption of aspartame-containing beverages and incidence of hematopoietic and brain malignancies. Cancer Epidemiol. Biomark. Prev. 2006;15:1654–1659. doi: 10.1158/1055-9965.EPI-06-0203. [DOI] [PubMed] [Google Scholar]
- 31.McCullough M.L., Teras L.R., Shah R., Diver W.R., Gaudet M.M., Gapstur S.M. Artificially and sugar-sweetened carbonated beverage consumption is not associated with risk of lymphoid neoplasms in older men and women. J. Nutr. 2014;144:2041–2049. doi: 10.3945/jn.114.197475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Navarrete-Muñoz E.M., Wark P.A., Romaguera D., Bhoo-Pathy N., Michaud D., Molina-Montes E., Tjønneland A., Olsen A., Overvad K., Boutron-Ruault M.C., et al. Sweet-beverage consumption and risk of pancreatic cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) Am. J. Clin. Nutr. 2016;104:760–768. doi: 10.3945/ajcn.116.130963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schernhammer E.S., Bertrand K.A., Birmann B.M., Sampson L., Willett W.C., Feskanich D. Consumption of artificial sweetener- and sugar-containing soda and risk of lymphoma and leukemia in men and women. Am. J. Clin. Nutr. 2012;96:1419–1428. doi: 10.3945/ajcn.111.030833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stepien M., Duarte-Salles T., Fedirko V., Trichopoulou A., Lagiou P., Bamia C., Overvad K., Tjønneland A., Hansen L., Boutron-Ruault M.C., et al. Consumption of soft drinks and juices and risk of liver and biliary tract cancers in a European cohort. Eur. J. Nutr. 2016;55:7–20. doi: 10.1007/s00394-014-0818-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farvid M.S., Spence N.D., Rosner B.A., Chen W.Y., Eliassen A.H., Willett W.C., Holmes M.D. Consumption of sugar-sweetened and artificially sweetened beverages and breast cancer survival. Cancer. 2021;127:2762–2773. doi: 10.1002/cncr.33461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guercio B.J., Zhang S., Niedzwiecki D., Li Y., Babic A., Morales-Oyarvide V., Saltz L.B., Mayer R.J., Mowat R.B., Whittom R., et al. Associations of artificially sweetened beverage intake with disease recurrence and mortality in stage III colon cancer: Results from CALGB 89803 (Alliance) PLoS ONE. 2018;13:e0199244. doi: 10.1371/journal.pone.0199244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malik V.S., Li Y., Pan A., De Koning L., Schernhammer E., Willett W.C., Hu F.B. Long-Term Consumption of Sugar-Sweetened and Artificially Sweetened Beverages and Risk of Mortality in US Adults. Circulation. 2019;139:2113–2125. doi: 10.1161/CIRCULATIONAHA.118.037401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mullee A., Romaguera D., Pearson-Stuttard J., Viallon V., Stepien M., Freisling H., Fagherazzi G., Mancini F.R., Boutron-Ruault M.C., Kühn T., et al. Association Between Soft Drink Consumption and Mortality in 10 European Countries. JAMA Intern. Med. 2019;179:1479–1490. doi: 10.1001/jamainternmed.2019.2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y.-B., Chen J.-X., Jiang Y.-W., Xia P.-F., Pan A. Association of sugar-sweetened beverage and artificially sweetened beverage intakes with mortality: An analysis of US National Health and Nutrition Examination Survey. Eur. J. Nutr. 2021;60:1945–1955. doi: 10.1007/s00394-020-02387-x. [DOI] [PubMed] [Google Scholar]
- 40.Zoltick E.S., Smith-Warner S.A., Yuan C., Wang M., Fuchs C.S., Meyerhardt J.A., Chan A.T., Ng K., Ogino S., Stampfer M.J., et al. Sugar-sweetened beverage, artificially sweetened beverage and sugar intake and colorectal cancer survival. Br. J. Cancer. 2021;125:1016–1024. doi: 10.1038/s41416-021-01487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu D., Li Z.-H., Shen D., Zhang P.-D., Song W.-Q., Zhang W.-T., Huang Q.-M., Chen P.-L., Zhang X.-R., Mao C. Association of Sugar-Sweetened, Artificially Sweetened, and Unsweetened Coffee Consumption with All-Cause and Cause-Specific Mortality. Ann. Intern. Med. 2022;175:909–917. doi: 10.7326/M21-2977. [DOI] [PubMed] [Google Scholar]
- 42.Zamora-Ros R., Cayssials V., Clèries R., Torrents M., Byrnes G., Weiderpass E., Sandstrm M., Almquist M., Boutron-Ruault M.C., Tjnneland A. Sweetened beverages are associated with a higher risk of differentiated thyroid cancer in the EPIC cohort: A dietary pattern approach. Eur. J. Nutr. 2022:1–10. doi: 10.1007/s00394-022-02953-5. [DOI] [PubMed] [Google Scholar]
- 43.Mossavar-Rahmani Y., Kamensky V., Manson J.E., Silver B., Rapp S.R., Haring B., Beresford S.A.A., Snetselaar L., Wassertheil-Smoller S. Artificially Sweetened Beverages and Stroke, Coronary Heart Disease, and All-Cause Mortality in the Women’s Health Initiative. Stroke. 2019;50:555–562. doi: 10.1161/STROKEAHA.118.023100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vyas A., Rubenstein L., Robinson J., Seguin R.A., Vitolins M.Z., Kazlauskaite R., Shikany J.M., Johnson K.C., Snetselaar L., Wallace R. Diet drink consumption and the risk of cardiovascular events: A report from the Women’s Health Initiative. J. Gen. Intern. Med. 2015;30:462–468. doi: 10.1007/s11606-014-3098-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anderson J.J., Gray S.R., Welsh P., Mackay D.F., Celis-Morales C.A., Lyall D.M., Forbes J., Sattar N., Gill J.M.R., Pell J.P. The associations of sugar-sweetened, artificially sweetened and naturally sweet juices with all-cause mortality in 198,285 UK Biobank participants: A prospective cohort study. BMC Med. 2020;18:97. doi: 10.1186/s12916-020-01554-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paganini-Hill A., Kawas C.H., Corrada M.M. Non-alcoholic beverage and caffeine consumption and mortality: The Leisure World Cohort Study. Prev. Med. 2007;44:305–310. doi: 10.1016/j.ypmed.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fowler S.P., Williams K., Resendez R.G., Hunt K.J., Hazuda H.P., Stern M.P. Fueling the obesity epidemic? Artificially sweetened beverage use and long-term weight gain. Obesity. 2008;16:1894–1900. doi: 10.1038/oby.2008.284. [DOI] [PubMed] [Google Scholar]
- 48.O’Connor L., Imamura F., Lentjes M.A., Khaw K.T., Wareham N.J., Forouhi N.G. Prospective associations and population impact of sweet beverage intake and type 2 diabetes, and effects of substitutions with alternative beverages. Diabetologia. 2015;58:1474–1483. doi: 10.1007/s00125-015-3572-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fung T.T., Malik V., Rexrode K.M., Manson J.E., Willett W.C., Hu F.B. Sweetened beverage consumption and risk of coronary heart disease in women. Am. J. Clin. Nutr. 2009;89:1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dokova K.G., Pancheva R.Z., Usheva N.V., Haralanova G.A., Nikolova S.P., Kostadinova T.I., Egea Rodrigues C., Singh J., Illner A.K., Aleksandrova K. Nutrition Transition in Europe: East-West Dimensions in the Last 30 Years—A Narrative Review. Front. Nutr. 2022;9:919112. doi: 10.3389/fnut.2022.919112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang Y.B., Jiang Y.W., Chen J.X., Xia P.F., Pan A. Association of Consumption of Sugar-Sweetened Beverages or Artificially Sweetened Beverages with Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2021;12:374–383. doi: 10.1093/advances/nmaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wiebe N., Padwal R., Field C., Marks S., Jacobs R., Tonelli M. A systematic review on the effect of sweeteners on glycemic response and clinically relevant outcomes. BMC Med. 2011;9:123. doi: 10.1186/1741-7015-9-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rycerz K., Jaworska-Adamu J.E. Effects of aspartame metabolites on astrocytes and neurons. Folia Neuropathol. 2013;51:10–17. doi: 10.5114/fn.2013.34191. [DOI] [PubMed] [Google Scholar]
- 54.Ylmaz S., Uar A. A review of the genotoxic and carcinogenic effects of aspartame: Does it safe or not? Cytotechnology. 2014;66:875–881. doi: 10.1007/s10616-013-9681-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Soffritti M., Belpoggi F., Manservigi M., Tibaldi E., Lauriola M., Falcioni L., Bua L. Aspartame administered in feed, beginning prenatally through life span, induces cancers of the liver and lung in male Swiss mice. Am. J. Ind. Med. 2010;53:1197–1206. doi: 10.1002/ajim.20896. [DOI] [PubMed] [Google Scholar]
- 56.Soffritti M., Belpoggi F., Degli Esposti D., Lambertini L., Tibaldi E., Rigano A. First experimental demonstration of the multipotential carcinogenic effects of aspartame administered in the feed to Sprague-Dawley rats. Environ. Health Perspect. 2006;114:379–385. doi: 10.1289/ehp.8711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS) Scientific Opinion on the re-evaluation of aspartame (E 951) as a food additive. Efsa J. 2013;11:3496. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.