Abstract
The median nerve can be compressed due to a tumor along the course of the median nerve, causing typical compression symptoms or even persistence or recurrence after an operation. The aim of this review is to provide a comprehensive overview of rare tumors described in recent publications that cause median nerve compression and to evaluate treatment options.
The PubMed, Embase, and Web of Science databases were searched for studies describing median nerve compression due to a tumor in adults, published from the year 2000 and written in English. From 94 studies, information of approximately 100 patients have been obtained.
Results The rare tumors causing compression were in 32 patients located at the carpal tunnel, in 21 cases in the palm of the hand, and 28 proximal from the carpal tunnel. In the other cases the compression site extended over a longer trajectory. There were 37 different histological types of lesions. Complete resection of the tumor was possible in 58 cases. A total of 8 patients presented for the second time after receiving initial therapy. During follow-up, three cases of recurrence were reported with a mean follow-up period of 11 months.
The most common published cause of median nerve compression is the lipofibromatous hamartoma. Besides the typical sensory and motor symptoms of median nerve compression, a thorough physical examination of the complete upper extremity is necessary to find any swelling or triggering that might raise suspicion of the presence of a tumor.
Keywords: median neuropathy, neoplasms, rare diseases
Introduction
Median nerve compression occurs mostly at sites of fibro-osseous or fibromuscular tunnels. The most common site is at the carpal tunnel, causing carpal tunnel syndrome (CTS). However, proximal compression of the median nerve such as pronator syndrome and Lacertus syndrome should not be overlooked.
The etiology of CTS is mostly an idiopathic cause. Chronic trauma, rheumatoid arthritis, menopause, pregnancy, hypothyroidism, diabetes mellitus, acromegaly, and amyloidosis are also associated with the development of CTS. 1 2
Median nerve compression due to a benign or malign tumor is rare. A lipofibromatous hamartoma (LFH) is the most common histological type of tumor, but also lipomas, ganglion cysts, and fibromas are rarely found in the trajectory of the median nerve. These tumors can be incidental findings during diagnostics or routine carpal tunnel surgery. Unfortunately, they can have an uncommon presentation of symptoms which makes it hard to diagnose or distinguish from an idiopathic cause, with the possible consequence of a prolonged duration of the diagnostic process or even multiple surgical procedures. If missed or neglected, irreversible damage to the median nerve may occur. 3 This narrative review presents a list of uncommon tumors which can cause median nerve compression and may help to avoid diagnostic delay and unnecessary surgery.
The objective of this review is to provide a comprehensive overview of tumors described in recent publications that cause median nerve compression and to evaluate treatment options.
Materials and Methods
Search Strategy
PubMed, Embase, and Web of Science were searched for studies which described unique or rare cases of median nerve compression due to tumors. The first search was performed on May 11, 2020, and the last update of the search was performed on May 25, 2020.
Due to the lack of a valid bias analysis for narrative reviews, specific criteria for article selection and inclusion and exclusion were developed. The following criteria have been used to include a study to this review: papers describing a case, cause or etiology of median nerve compression, tumors, year of publication from 2000, age of patients 18 years or older, and written in English.
Excluded studies involved cadavers, animals, and cases of other causes of median nerve compression (including idiopathic CTS, pregnancy, edema, rheumatoid arthritis, gout, diabetes mellitus, hypothyroidism, tenosynovitis, acromegaly, repetitive tasks, anatomic anomalies, traumatic neuropathy, and infectious causes). A detailed electronic search strategy is described in Supplementary Appendix A (available in the online version).
Data Extraction
Data of patient characteristics, side of compression, uni- or bilateral compression, cause of compression, symptoms at presentation, duration of symptoms at presentation, physical examination, diagnostics, treatments, location of tumor, results of treatment, complications, follow-up, and recurrence were extracted and analyzed by two reviewers with the use of EndNote X8.2 (Clarivate Analytics, Philadelphia, PA).
Disagreements were resolved by discussion or by the third reviewer. All outcomes were processed in SPSS (IBM SPSS statistics version 26). If any data was missing studies were excluded from that particular part of statistical analysis.
Data Analysis
All included studies were analyzed together for the general characteristics. In addition, three categories were formed: neural, nonneural, and combined. The neural category includes tumors consisting of neural elements. The nonneural category includes tumors arising from the surrounding tissue. In case of the presence of multiple tumors from both categories, the case was listed in the combined category. Furthermore, cases of proximal median nerve compression were analyzed separately from compression at carpal tunnel.
All papers were evaluated and analyzed in a systematic way to reduce bias. Studies with a limited case description are still included to reduce reporting bias and to include all available information.
Results
Study Selection
The initial search revealed 2,024 studies. After removing duplicate studies ( n = 534), abstracts from 1,490 studies were evaluated and 1,396 studies were excluded based on the title and abstract. Furthermore, 15 studies were excluded on the base of full-text analysis leaving a total of 79 papers for full-text review. Also, there were 15 additional studies found in the reference lists. Supplementary Appendix B (available in the online version) presents the study selection process.
Case Characteristics
Eventually, 94 studies with a description of 100 cases of median nerve compression due to a tumor have been reviewed. There were 45 (46%) male patients and 54 (56%) female patients with a mean age of 45.14 (ranging from 18 to 86) years. In 39 cases the left side was affected, in 56 cases the right side. Only two bilateral cases were described. In 8 cases (8%) the patient presented for the second time, after failing of initial therapy (6 carpal tunnel releases and 2 nonsurgical treatments). Table 1 describes the general characteristics of the reviewed cases.
Table 1. Characteristics of cases.
| Frequency ( n ) | Percent (%) | ||
|---|---|---|---|
| Gender a | Male | 45 | 46 |
| Female | 54 | 56 | |
| Side b | Left | 39 | 40 |
| Right | 56 | 58 | |
| Bilateral | 2 | 2.1 | |
| Sensory symptoms | 82 | 82 | |
| Motor symptoms | 27 | 27 | |
| Pain | 53 | 53 | |
| Swelling | 40 | 40 | |
| Triggering | 6 | 6 | |
| Preoperative imaging c | 81 | 87 | |
| Treatment d | Carpal tunnel release | 52 | 55 |
| Complete resection mass | 58 | 62 | |
| Partial resection mass | 4 | 4.3 | |
| Only biopsy | 7 | 7.4 | |
| Treatment outcome | Recovery | 43 | 43 |
| Improvement | 28 | 28 | |
| Not described/unknown | 29 | 29 | |
| Recurrence | Yes | 3 | 3 |
| No | 47 | 47 | |
| Not described/unknown | 50 | 50 | |
For 1 case missing data.
For 3 cases missing data.
For 7 cases missing data.
For 6 cases missing data.
Symptoms
Most patients ( n = 82) experience sensory symptoms at first presentation, 53 patients reported pain and only 27 patients had motor dysfunction. In 40 cases swelling was reported. Triggering of the wrist was presented in six cases. In the neural category, 22 patients experienced sensory symptoms (63%), 15 reported pain (43%), 6 had motor dysfunction (17%), 20 swelling (57%), and 1 triggering (3%). In the nonneural category, 58 patients had sensory symptoms (92%), 36 patients experienced pain (57%), 20 had motor dysfunction (32), 20 swelling (32%), and in 5 patients the lesion caused triggering of the wrist (7.9%).
The tumor was located in the proximal (fore)arm in 28 cases. A total of 15 out of these 28 patients experienced pain (54%).
Treatment
In 58 cases the mass was completely resected and in only 4 patients a partial resection was possible due to a strong adherence of some areas of the tumor to the median nerve and due to the inability to distinguish the tumor from the surrounding tissue.
The most performed procedure was an open median nerve release (52 patients) whether or not combined with resection of the mass causing compression. In one case an endoscopic carpal tunnel release was performed. In three cases the patient rejected a surgical approach. Treatment in case of neural masses: 22 open median nerve releases (69%), complete resection in 15 cases (47%), 1 partial resection (3.1%), and 3 resection biopsies (9.4%) have been performed. Treatment for nonneural masses consisted of 28 performed open median nerve releases (47%), 41 complete resections (68%), 3 partial resections (5%), and 4 resection biopsies (6.7%).
Outcome of Treatment
The mean follow-up period was 11 months. Not all studies described the outcome of treatment and eventual recurrence. Information about the recovery of 43 out 71 patients was reported in the studies of which 28 out of 71 patients reported an improvement. In 47 out of 50 patients no signs of recurrence were present at follow-up. In 50 cases the recurrence rate was not reported.
Causes of Median Nerve Compression
Table 2 shows all 35 different histological types of 100 lesions that can cause median nerve compression. There are three main categories of tumors causing median nerve compression: neural origin ( n = 35), nonneural origin ( n = 63), and a combination of causes ( n = 2). The most common cause of neural origin is the LFH (19 patients, 19%). Lipomas are the most common cause in the nonneural origin category (16 patients, 16%). In two patients, a combination of causes was present. A total of nine tumors were malignant. The pie chart in Fig. 1 provides a quick overview of all causes.
Table 2. Tumors causing median nerve compression.
| Tumor | Frequency ( n ) | Percent of total (%) | Percent of category (%) | |
|---|---|---|---|---|
| Neural origin ( n = 35) |
Lipofibromatous hamartoma | 19 | 19 | 54 |
| Schwannoma | 8 | 8 | 23 | |
| Intraneural lipoma | 2 | 2 | 5.7 | |
| Intraneural perineurioma | 3 | 3 | 5.7 | |
| Neurothekeoma | 2 | 2 | 5.7 | |
| Plexiform neurofibroma | 1 | 1 | 2.9 | |
| Nonneural origin ( n = 63) |
Lipoma | 16 | 16 | 26 |
| Ganglion | 6 | 6 | 9.5 | |
| Fibroma | 6 | 6 | 9.5 | |
| Tenosynovial giant cell tumor | 5 | 5 | 3.2 | |
| Deep leiomyoma | 2 | 2 | 3.2 | |
| Heterotrophic ossification | 2 | 2 | 3.2 | |
| Myoepithelioma | 2 | 2 | 3.2 | |
| Myxofibrosarcoma a | 2 | 2 | 3.2 | |
| Osteochondroma | 2 | 2 | 3.2 | |
| Solitary calcified nodule | 2 | 2 | 3.2 | |
| Synovial sarcoma a | 2 | 2 | 3.2 | |
| Calcifying aponeurotic fibrolipoma | 1 | 1 | 1.6 | |
| Epithelioid sarcoma a | 1 | 1 | 1.6 | |
| Extraskeletal chondroma | 1 | 1 | 1.6 | |
| Glomus tumor | 1 | 1 | 1.6 | |
| Hamartoma | 1 | 1 | 1.6 | |
| Hibernoma | 1 | 1 | 1.6 | |
| Macrodystrophia lipomatosa | 1 | 1 | 1.6 | |
| Malignant tenosynovial giant cell tumor a | 1 | 1 | 3.2 | |
| Melorheostosis | 1 | 1 | 1.6 | |
| Metaplastic synovial cyst | 1 | 1 | 1.6 | |
| Metastasis of breast cancer a | 1 | 1 | 1.6 | |
| Neuroleukemiosis a | 1 | 1 | 1.6 | |
| Non-Hodgkin lymphoma a | 1 | 1 | 1.6 | |
| Osteophyte trapezium | 1 | 1 | 1.6 | |
| Synovial hemangioma | 1 | 1 | 1.6 | |
| Synovial osteochondromatosis | 1 | 1 | 1.6 | |
| Combined | Intraneural lipoma and AVM | 1 | 1 | 50 |
| Lipofibromatous hamartoma and osteochondroma | 1 | 1 | 50 |
Abbreviation: AVM, arteriovenous malformation.
Malignant tumors.
Fig. 1.
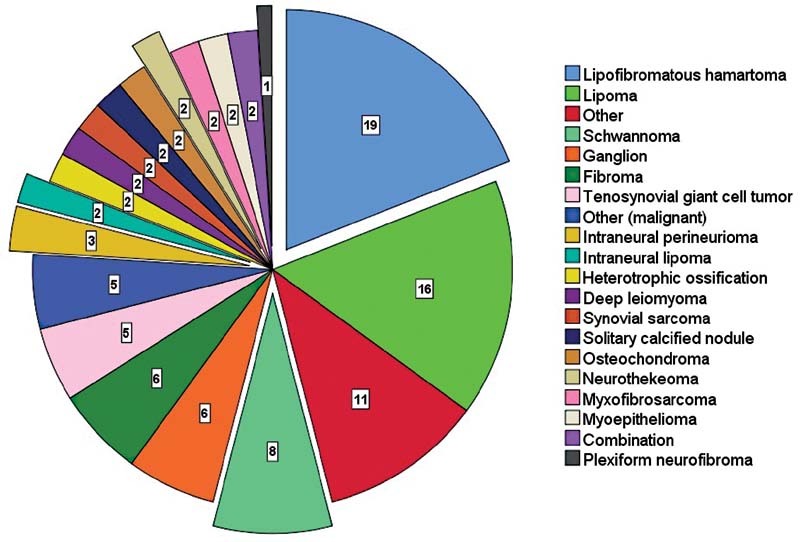
Pie chart of tumors causing median nerve compression. The exploded slices show neural causes. Causes in the group “other” occurred only once and contains: hamartoma, glomus tumor, extraskeletal chondroma, synovial osteochondromatosis, synovial hemangioma, osteophyte trapezium, metaplastic synovial cyst, melorheostosis, macrodystrophia lipomatosa, hibernoma, and calcifying aponeurotic fibrolipoma. Causes in the group “other (malignant)” occurred only once and contains: epithelioid sarcoma, non-Hodgkin lymphoma, neuroleukemiosis, and metastasis of breast cancer.
Location of Compression
Tumors causing the compression of the median nerve can occur at every point of the trajectory. Fig. 2 shows the results of the found locations of the tumors. Compression due to a tumor occurs most often in the carpal tunnel ( n = 32), 21 lesions were found in the palm of the hand and 13 lesions were located in the distal forearm. The other sites of compression ranged from biceps to the proximal phalanx of the index finger. In a few cases, the lesion was so extensive that it took up more than one location, among others a lesion in the distal forearm reaching to the palm of the hand.
Fig. 2.
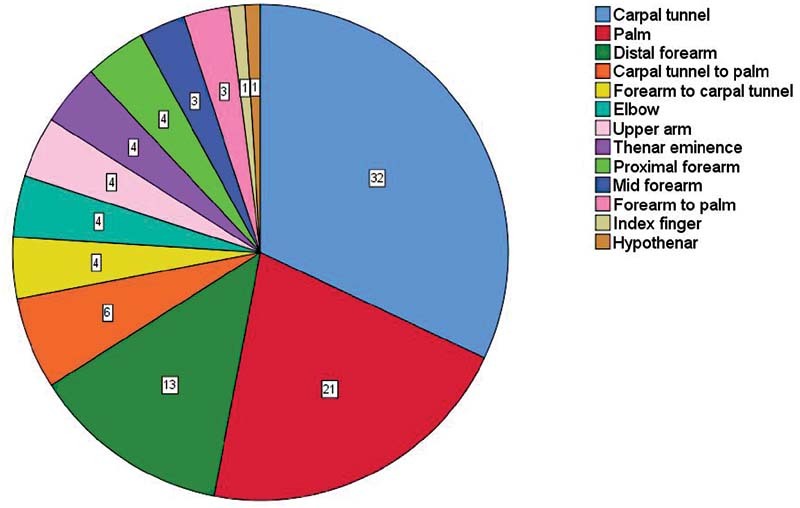
Pie chart of the anatomic locations of median nerve compression due to a tumor.
Discussion
Overview of Tumors Causing Carpal Tunnel Syndrome
Neural ( n = 35)
Lipofibromatous Hamartoma
The most common cause of median nerve compression of neural origin in this review is the LFH (19 cases). The LFH is a benign and slow growing peripheral nerve tumor. It has predilection for the median nerve and it is associated with macrodactyly (more than one-third). 4 5 This type of tumor is mostly reported in young patients.
Fibrofatty tissue infiltrates the nerve which separates and compresses the nerve, so complete excision is not possible without damaging the nerve. In case of CTS, decompression surgery has shown to be effective. Different surgical approaches are advocated, among which microsurgical intraneural dissection and excision with nerve grafting. If excision is not possible, a biopsy can confirm the diagnosis. 6
Schwannoma
Schwannomas also called neurilemmomas, are benign, slow growing neural tumors originating from Schwann cells of a peripheral nerve. The incidence in adults is only 5%. 7 Typical finding at physical examination is a mass which is mobile in longitudinal plane but not in transversal plane. 7 The nerve fascicles are pushed aside while the tumor grows. Therefore, complete enucleation is in most cases possible. 8 Recurrence is rarely reported, even in incomplete excision. 7
Intraneural Perineurioma
In three patients an intraneural perineurioma caused median nerve compression. This is a slow growing benign tumor. The presentation is in most cases as a slow progressive mononeuropathy causing hypoesthesia and motor weakness. 9 No consensus about therapy exists, varying from conservative management 10 to resection with interposing nerve graft. 11 12 Uerschels et al promotes interfascicular neurolysis in combination with decompression surgery.
Intraneural Lipoma
An intraneural lipoma is encapsulated but does not contain neural elements. Therefore, a complete excision is possible without damaging the nerve. In only two cases an intraneural lipoma caused median nerve compression.
Neurothekeoma
A neurothekeoma is a benign, small, and slow growing tumor which originates from the endoneurium of peripheral nerves. It mostly occurs before 30 years of age with a preference for the female gender. It has a high tendency of local recurrence (11%). 13 14 Complete surgical excision is the treatment of first choice.
Plexiform Neurofibroma
Neurofibromas are benign nerve sheath tumors occurring in patients between 20 and 30 years. Tumor mass and nerve fascicles are intertwined and therefore complete excision may sacrifice the nerve. With microdissection of the neurofibroma, nerve fascicles can be spared. Plexiform neurofibromas are associated with neurofibromatosis-1 and surgical removal is often impossible due to their serpiginous growth, significant vascularization, and multiple nerve fiber involvement. In previous publications, a recurrence rate of 50% is reported. 15
In this review, all neural causes were benign. Malignant peripheral nerve sheath tumors were not described in the reviewed articles, but must also be considered in the differential diagnosis. Other benign neural causes, not described in this review, are neuroma and osteoid osteoma.
Nonneural ( n = 63)
Benign lesions are often easily resected with minimal nerve morbidity and with a very good outcome. 16
Soft Tissue
Lipoma
In 16 cases a lipoma was found as a cause of median nerve compression. Lipomas are soft encapsulated masses, easily separated from surrounding tissue. Chen et al found three lipomas in 23 space occupying lesions and Cavit et al reported 20 out of 402 hand tumors to be lipomas (4.9%). 17
Ganglion Cyst
Ganglion cysts can communicate with tendon (sheats), nerves, or joints and can arise from joint synovial tissue. Cavit et al published a review in which ganglion cysts were the most common soft tissue tumors (125 out of 402, 31%). In this review, ganglion cysts caused median nerve compression in 6 out of 63 nonneural tumors. Recurrence rate in case of aspiration is higher compared with a surgical excision. 18 19 20
Fibroma
A fibroma is a well-circumscribed, lobulated, and sometimes encapsulated benign mass, which is generally attached to tendon sheaths. Fibromas are easily excised. Evangelisti and Nojiri describe a 24% recurrence rate in case of inadequate excision. 22 30
Tenosynovial Giant Cell Tumor
Also called pigmented villonodular synovitis, caused by a benign, but invasive synovial proliferation. Treatment requires extensive synovectomy and in some cases adjuvant radiotherapy depending on the extensiveness of the lesion. Despite aggressive therapy, a high recurrence is reported (8–56%). 21
Other uncommon causes found in this review were a deep leiomyoma ( n = 2), myoepithelioma ( n = 2), solitary calcified nodule ( n = 2), glomus tumor ( n = 1), hamartoma ( n = 1), hibernoma ( n = 1), metaplastic synovial cyst ( n = 1), synovial hemangioma ( n = 1), and calcified aponeurotic fibrolipoma ( n = 1).
Bone and Cartilage
A total of eight bony and cartilage tumors were found in this review. All of these tumors were benign in nature. The following histological bony and cartilage tumors were found as a cause of median nerve compression: osteochondroma ( n = 2), heterotopic ossification ( n = 2), osteophyte ( n = 1), extraskeletal chondroma ( n = 1), melorheostosis ( n = 1), and synovial osteochondromatosis ( n = 1).
Malignant
Merely 9 out of 100 reviewed lesions causing median nerve compression were malignant, involving epithelioid sarcoma, non-Hodgkin lymphoma, neuroleukemiosis, and a metastasis of breast cancer. There were only nonneural malignant masses. Especially, fast growing tumor or a tumor with more than 5 cm in diameter has to be suspected for malignancy. 23
Combined ( n = 2)
In two patients a combined cause of median nerve compression was found.
The first case described treatment of proximal median nerve compression with full release of median nerve in the forearm and epineurotomy.
During the operation, a lipomatous tumor was found and left undisturbed. Postoperative imaging showed a LFH and an osteochondroma.
Due to recurrent symptoms and diagnosed osteochondroma, a second operation consisting of excision of the osteochondroma was performed. The median nerve was pushed anteriorly by the osteochondroma and internal compression took place due to the LFH.
The second patient was diagnosed with an intraneural lipoma combined with an arteriovenous malformation during preoperative imaging. Both lesions were totally excised in combination with a carpal tunnel decompression. The patient had full recovery and there were no signs of tumor recurrence during follow-up. The authors recommend preoperative imaging in case of unilateral CTS and palpable tumors.
Both papers make no statement about incidence or coincidence of finding both tumors in one patient.
The most described cause of median nerve compression due to a mass lesion in previous publications is a LFH. The second and third most common published cause is a lipoma and a ganglion cyst, respectively. In this review, 8 patients already received treatment for median nerve compression but experienced persistent or recurrent symptoms. In all 8 cases unilateral symptoms were present and initial treatment through carpal tunnel release or lidocaine/corticosteroid injection was performed without preoperative imaging. Therefore, a tumor causing CTS was initially missed and after a period of persistence of symptoms after initial treatment, the tumor was found on imaging. Owing to the high incidence of idiopathic CTS, tumors are often missed. In all cases of diagnosing the tumor preoperatively, no recurrence of symptoms was reported, except for tenosynovial giant cell tumors. For these tumors, a high recurrence rate was already reported. 21
After analysis of all cases included in this review, we conclude imaging could be helpful for correct diagnosis and preoperative planning, especially in cases of unilateral median nerve compression to prevent multiple operations.
This review consists of case reports and case series published in the English literature, which are unfortunately known for a low level of evidence. However, these cases provide useful information for clinical practice. This study is limited by publication bias. Case reports will only be published in case of an interesting or rare topic, such as rare causes of median nerve compression. For actual incidence rates of common causes of median nerve compression, other research articles must be consulted.
The carpal tunnel is a preferred location for median nerve compression, but compression can occur along the complete trajectory of the median nerve. It can be difficult to distinguish a tumor as a cause of median nerve compression from the idiopathic cause of CTS, which is more common. However, a palpable swelling was found in 40 patients, suggesting a lesion as the cause of the complaints. Besides, in 6 cases, triggering of the wrist was a symptom at first presentation which is an indication of a lesion. These findings are essential not only for diagnostic process, but also for adequate preoperative planning of patients. A total of 53 out of 100 patients experienced pain as a symptom. From the 28 cases of proximal median nerve compression due to a tumor, 15 patients experienced pain (54%).
In case of the presence of swelling or wrist triggering combined with symptoms of median nerve compression, a tumor must be suspected and therefore imaging is recommended.
Landi et al provided a thorough and clear overview of rare causes of CTS. However, they used studies up to 1998 and only wrote about median nerve compression at the site of the carpal tunnel. In our review, we analyzed studies about median nerve compression due to tumors, from 2000 till present, without restriction of a compression site. 31
The causes were divided into three groups (neural, nonneural, and combination of causes), to provide a clear overview. However, the treatment cannot be grouped and should always be conducted according to the corresponding guidelines per country and/or hospital.
Malignant tumors causing median nerve compression are uncommon. However, leukemia, lymphomas, and even metastases can cause median nerve compression if located in the arm. 24 25 26 27 28
Conclusion
Rare tumors causing median nerve compression can be divided into three groups: neural, nonneural, and a combined origin. The most common cause of compression in our review is due to LFH, a neural tumor. Complete excision of LFH is not possible without damaging the nerve but decompression surgery can relief symptoms. 6 Lipomas form the most frequent cause of uncommon median nerve compression in the nonneural category. In general, complete excision of a lipoma is possible.
A thorough physical examination of the complete upper extremity must be performed and documented to find any swelling along the course of the median nerve. Based on the data found in this review, in case of swelling or triggering, a lesion must be suspected and therefore early imaging diagnostics are recommended.
To choose the adequate treatment, it is essential to have a preoperative diagnosis before the operation. Complete excision of neural masses is often more difficult in comparison to nonneural masses. 29 Malignant tumors as a cause of median nerve compression is extremely rare. Therefore, treatment should be adapted to the national guidelines and with multidisciplinary consultation.
Conflict of Interest None of the authors is an Editorial Board member. No other potential conflicts of interest relevant to this article were reported.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors. For this type of study informed consent is not required.
Authors' Contributions
All the authors have approved the final contents of the submission, been actively involved in the planning and enactment of the study, and have also assisted with the preparation of the submitted article.
Supplementary Material
References
- 1.Cheng T F, Chen C Y, Liu P T, Yang S W. Solitary calcified nodules as the cause of carpal tunnel syndrome: two case reports and literature reviews. Front Neurol. 2019;10:224. doi: 10.3389/fneur.2019.00224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mascitelli J R, Halpern C H, Dolinskas C A, Zager E L, Welch W C. Carpal tunnel syndrome secondary to an osteophyte of the trapezium. J Clin Neurosci. 2011;18(11):1558–1559. doi: 10.1016/j.jocn.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Gillig J D, White S D, Rachel J N. Acute carpal tunnel syndrome: a review of current literature. Orthop Clin North Am. 2016;47(03):599–607. doi: 10.1016/j.ocl.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Amadio P C, Reiman H M, Dobyns J H. Lipofibromatous hamartoma of nerve. J Hand Surg Am. 1988;13(01):67–75. doi: 10.1016/0363-5023(88)90203-1. [DOI] [PubMed] [Google Scholar]
- 5.Silverman T A, Enzinger F M. Fibrolipomatous hamartoma of nerve. A clinicopathologic analysis of 26 cases. Am J Surg Pathol. 1985;9(01):7–14. doi: 10.1097/00000478-198501000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Nanno M, Sawaizumi T, Takai S. Case of fibrolipomatous hamartoma of the digital nerve without macrodactyly. J Nippon Med Sch. 2011;78(06):388–392. doi: 10.1272/jnms.78.388. [DOI] [PubMed] [Google Scholar]
- 7.Forthman C L, Blazar P E.Nerve tumors of the hand and upper extremity Hand Clin 20042003233–242, v.v. [DOI] [PubMed] [Google Scholar]
- 8.Kang H J, Shin S J, Kang E S. Schwannomas of the upper extremity. J Hand Surg [Br] 2000;25(06):604–607. doi: 10.1054/jhsb.2000.0472. [DOI] [PubMed] [Google Scholar]
- 9.Uerschels A-K, Krogias C, Junker A, Sure U, Wrede K H, Gembruch O. Modern treatment of perineuriomas: a case-series and systematic review. BMC Neurol. 2020;20(01):55. doi: 10.1186/s12883-020-01637-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jazayeri M A, Robinson J H, Legolvan D P. Intraneural perineurioma involving the median nerve. Plast Reconstr Surg. 2000;105(06):2089–2091. doi: 10.1097/00006534-200005000-00026. [DOI] [PubMed] [Google Scholar]
- 11.Gruen J P, Mitchell W, Kline D G. Resection and graft repair for localized hypertrophic neuropathy. Neurosurgery. 1998;43(01):78–83. doi: 10.1097/00006123-199807000-00051. [DOI] [PubMed] [Google Scholar]
- 12.Sachanandani N S, Brown J M, Zaidman C, Brown S S, Mackinnon S E. Intraneural perineurioma of the median nerve: case report and literature review. Hand (N Y) 2010;5(03):286–293. doi: 10.1007/s11552-009-9228-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fetsch J F, Laskin W B, Hallman J R, Lupton G P, Miettinen M. Neurothekeoma: an analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information. Am J Surg Pathol. 2007;31(07):1103–1114. doi: 10.1097/PAS.0b013e31802d96af. [DOI] [PubMed] [Google Scholar]
- 14.Sharma A, Kamble P C, Singh V. A rare case of intraneural neurothekeoma of median nerve mimicking carpal tunnel syndrome. J Orthop Case Rep. 2017;7(06):73–75. doi: 10.13107/jocr.2250-0685.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen R, Ibrahim C, Friedrich R E, Westphal M, Schuhmann M, Mautner V F. Growth behavior of plexiform neurofibromas after surgery. Genet Med. 2013;15(09):691–697. doi: 10.1038/gim.2013.30. [DOI] [PubMed] [Google Scholar]
- 16.Sughrue M E, Levine J, Barbaro N M. Pain as a symptom of peripheral nerve sheath tumors: clinical significance and future therapeutic directions. J Brachial Plex Peripher Nerve Inj. 2008;3:6. doi: 10.1186/1749-7221-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cavit A, Özcanli H, Sançmiş M, Ayşe G Ocak, İnanç E Gürer. Tumorous conditions of the hand: a retrospective review of 402 cases. Turk Patoloji Derg. 2018;34(01):66–72. doi: 10.5146/tjpath.2017.01413. [DOI] [PubMed] [Google Scholar]
- 18.Wright T W, Cooney W P, Ilstrup D M. Anterior wrist ganglion. J Hand Surg Am. 1994;19(06):954–958. doi: 10.1016/0363-5023(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 19.Okada K, Miyake J, Kataoka T, Moritomo H, Murase T, Yoshikawa H. Median nerve neuropathy in the forearm due to recurrence of anterior wrist ganglion that originates from the scaphotrapezial joint: case report. J Brachial Plex Peripher Nerve Inj. 2012;7(01):1. doi: 10.1186/1749-7221-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Head L, Gencarelli J R, Allen M, Boyd K U. Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg Am. 2015;40(03):546–5.3E9. doi: 10.1016/j.jhsa.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 21.Nassar W A, Bassiony A A, Elghazaly H A. Treatment of diffuse pigmented villonodular synovitis of the knee with combined surgical and radiosynovectomy. HSS J. 2009;5(01):19–23. doi: 10.1007/s11420-008-9104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nojiri H, Ogawa S, Takayanagi N, Watanabe A, Kaneko K, Kurosawa H. Fibroma of the tendon sheath that expanded into the radiocarpal joint with bony involvement. Scand J Plast Reconstr Surg Hand Surg. 2006;40(06):357–361. doi: 10.1080/02844310500296370. [DOI] [PubMed] [Google Scholar]
- 23.Yildiran G, Akdag O, Karamese M. Giant lipomas of the hand. Hand Microsurg. 2015;4(01):8–11. [Google Scholar]
- 24.Leclère F M, Vogt P, Casoli V, Pelissier P, Choughri H. Double crush syndrome of the median nerve revealing a primary non-Hodgkin's lymphoma of the flexor digitorum superficialis muscle. Chir Main. 2015;34(05):256–259. doi: 10.1016/j.main.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Wang T, Miao Y, Meng Y, Li A. Isolated leukemic infiltration of peripheral nervous system. Muscle Nerve. 2015;51(02):290–293. doi: 10.1002/mus.24435. [DOI] [PubMed] [Google Scholar]
- 26.Theunissen C I, Bras J, Lienden K P, Obdeijn M C. Malignant giant cell tumor in the carpal tunnel: a case report and review of literature. J Wrist Surg. 2013;2(03):271–275. doi: 10.1055/s-0033-1350087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harish S, Saifuddin A, Fajinmi M. Epithelioid sarcoma of the median nerve mimicking a peripheral nerve sheath tumour. Australas Radiol. 2007;51(01):71–74. doi: 10.1111/j.1440-1673.2006.01662.x. [DOI] [PubMed] [Google Scholar]
- 28.Almusarhed M, Eldeeb H. Solitary biceps muscle metastasis from breast cancer. BMJ Case Rep. 2017;2017:bcr-2017-220597. doi: 10.1136/bcr-2017-220597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Afshar A. Carpal tunnel syndrome due to lipofibromatous hamartoma of the median nerve. Arch Iran Med. 2010;13(01):45–47. [PubMed] [Google Scholar]
- 30.Evangelisti S, Reale F V. Fibroma of tendon sheath as a cause of carpal tunnel syndrome. J Hand Surg Am. 1992;17(06):1026–1027. doi: 10.1016/s0363-5023(09)91052-8. [DOI] [PubMed] [Google Scholar]
- 31.Landi A, Acciaro L A, Rosa D N, Pellacani A.Carpal Tunnel Syndrome: Rare CausesSpringer:Berlin, Heidelberg: 200795–101. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


