Abstract
Testosterone is a hormone that plays a key role in carbohydrate, fat, and protein metabolism. Testosterone deficiency is associated with multiple comorbidities, e.g., metabolic syndrome and type 2 diabetes. Despite its importance in many metabolic pathways, the mechanisms by which it controls metabolism are not fully understood. The present study investigated the short-term metabolic changes of pharmacologically induced castration and, subsequently, testosterone supplementation in healthy young males. Thirty subjects were submitted to testosterone depletion (TD) followed by testosterone supplementation (TS). Plasma samples were collected three times corresponding to basal, low, and restored testosterone levels. An untargeted metabolomics study was performed by liquid chromatography–high resolution mass spectrometry (UHPLC–HRMS) to monitor the metabolic changes induced by the altered hormone levels. Our results demonstrated that TD was associated with major metabolic changes partially restored by TS. Carnitine and amino acid metabolism were the metabolic pathways most impacted by variations in testosterone. Furthermore, our results also indicated that LH and FSH might strongly alter the plasma levels of indoles and lipids, especially glycerophospholipids and sphingolipids. Our results demonstrated major metabolic changes induced by low testosterone that may be important for understanding the mechanisms behind the association of testosterone deficiency and its comorbidities.
Subject terms: Biochemistry, Endocrinology
Introduction
Testosterone is the main androgen in men and serve diverse and essential roles in the human body, not solely regarding reproduction but also in the modulation of carbohydrate, protein, and lipid metabolism1. Testosterone is associated with glucose uptake stimulation and insulin-regulated glucose transporter 4 (GLUT4) translocation in skeletal muscle cells, cardiomyocytes, and adipocytes2–4. Other effects include an increment in lipolysis and lipid oxidation, which impacts the regulation of glucose metabolism and insulin function5, and controlling the muscle mass to an anabolic state, increasing protein synthesis and decreasing protein breakdown6.
Low testosterone levels are associated with adverse metabolic profiles linked to hypogonadism, cardiovascular disease, metabolic syndrome, and diabetes7–10. Moreover, patients with reduced androgen production and/or bioavailability often have erectile dysfunction (ED), increased fat mass index, decreased muscle strength, cognitive impairment, and mood disorders11,12. Studies on testosterone replacement therapy (TRT) have demonstrated improved quality of life in men with hypogonadism, reduced symptoms such as ED and fat mass index, and increased lean body mass and sexual desire13,14. Furthermore, TRT improved insulin resistance and glycemic control in men with testosterone deficiency15,16.
Despite the multifaceted functions of testosterone in reproduction and metabolism and the diverse comorbidities associated with low testosterone, the molecular changes induced by testosterone deficiency have not yet been fully characterized. A better understanding of these events would enable the comprehension of the pathobiology and also the identification of new biomarkers, and improve diagnostic strategies and treatment monitoring.
In this context, metabolomics has been suggested to be a valuable strategy for investigation of disease and response to testosterone supplementation17. MS-based untargeted metabolomics is a powerful tool for metabolic and endocrine screening and has the potential to identify new biomarkers suitable for implementation in patient care18,19.
Our group previously designed a short-term human model, in which thirty healthy young males were submitted to testosterone depletion followed by testosterone supplementation. Blood samples corresponding to basal, low, and restored testosterone levels were collected20. Proteomic analysis of this controlled cohort revealed biological processes driven by gonadotropin and testosterone21 and indicated proteins and amino acids associated with testosterone fluctuations22,23. However, a deep metabolomic analysis associated with testosterone and gonadotropins changes was not performed.
This study aims to describe a deep plasma metabolic profile in healthy young men with pharmacologically induced alterations in testosterone and gonadotropins levels. Plasma samples from the human model were analyzed by MS-based untargeted metabolomics. Our results highlight for the first time the complex metabolic changes induced by androgen depletion in healthy men and the short-term effect of testosterone recovery. Several metabolites were impacted, especially those related to carnitine and amino acid metabolism. On the other hand, many metabolites associated with indoles and lipid metabolism appear to be affected by gonadotropin, i.e., LH and FSH, rather than testosterone levels.
Results
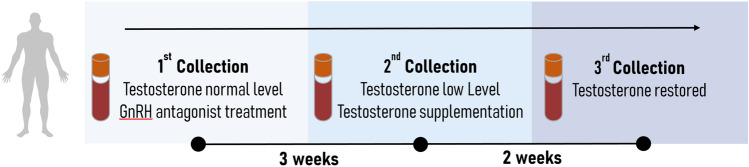
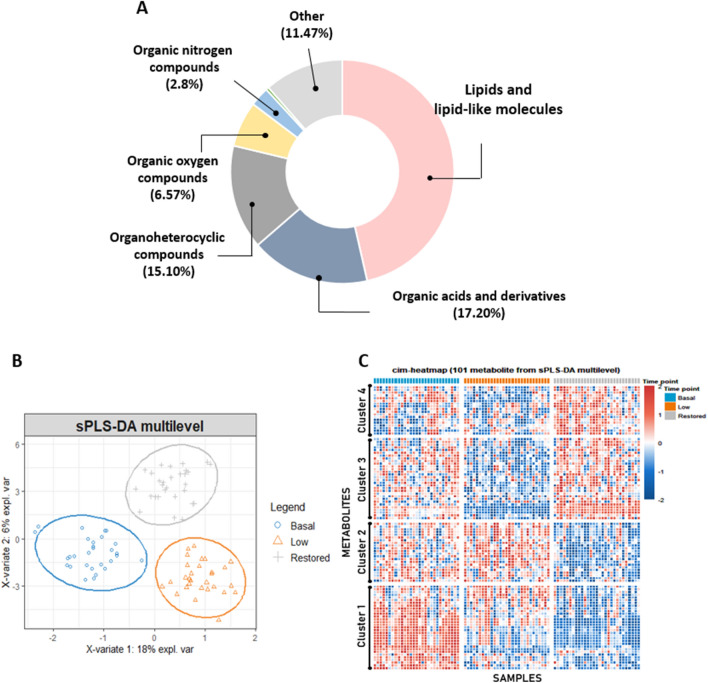
Our untargeted metabolomic analysis (UHPLC–HRMS) on plasma samples from thirty healthy young men submitted to gonadotropin and testosterone deficiency (TD) followed by testosterone supplementation (TS) identified 706 metabolites that were altered as a result of pharmacologically induced hormonal changes. The samples were classified into three groups: Basal, Low, and Restored testosterone levels (Fig. 1), and the metabolites were categorized according to their chemical class (Fig. 2A).
Figure 1.
Schematic representation of the designed human model. Blood samples were collected three times. The first collection was done before any pharmacological treatment and represents testosterone and gonadotropins at baseline levels. During the same visit, after blood collection, all subjects received a subcutaneous injection of gonadotropin-releasing hormone antagonist (GnRHa, 240 mg, Degarelix, Ferring Pharmaceuticals, Sweden). Three weeks later, subjects' blood samples were collected again, corresponding to low testosterone and gonadotropin levels. All participants then received an intramuscular injection of testosterone undecanoate (1000 mg, Nebido, Bayer Pharmaceuticals, Germany). After two weeks, the last blood samples were collected, corresponding to testosterone restored samples and low gonadotropin levels.
Figure 2.
Untargeted metabolomics analysis. (A) Chemical class of compounds identified by untargeted metabolomics approach based on UHPLC–HRMS. (B) Multilevel multivariate approach: sPLS-DA 2D score plot. The blue, orange, and gray regions represent the 95% confidence area of each group. The blue circles represent the Basal testosterone group, the orange triangles symbolize the Low testosterone group after chemical castration, and the gray crosses represent the Restored testosterone group after TS. (C) hierarchical clustering and heatmap based on sPLS-DA data. Four major metabolites clusters were revealed. Most compounds present in clusters 2, 3 and 4 seem to be driven by testosterone since they recovered or tended to recover their levels after TS. Conversely, many metabolites present in cluster 1 appear to be more influenced by LH and FSH expression since their levels did not normalize after TS.
A Sparse Partial Least Squares Discriminant Analysis (sPLS-DA) discriminated the samples according to the sample collection time points, i.e., different testosterone levels (Basal, Low, and Restored) (Fig. 2B), emphasizing the particular metabolic signature of each group. The hierarchical clustering analysis based on sPLS-DA data revealed four distinct clusters, highlighting some key metabolites (Fig. 2C). Table 1 shows the fifty known compounds present in the Human Metabolome Database (HMDB) and/or in the Kyoto Encyclopedia of Genes and Genomes (KEGG) that were responsible for the cluster separation, among them only six were non-significant (ANOVA paired analysis, q value > 0.05). Other molecules were not included. Additional information regarding the compounds identified by sPLS-DA, such as normalized average area value and Log2 fold-change, are present in the supplementary data (Table S1).
Table 1.
Metabolites identified by sPLS-DA analysis.
| Cluster | Compounds | Overall q value1 | VIP coef | Log2 Fold change | Trend | ||
|---|---|---|---|---|---|---|---|
| B versus L2 | L × R3 | B × R4 | |||||
| 1 | 5-Hydroxyindole-3-acetic acid | 4.70E−08 | 0.70 | 1.02* | 0.37 | 1.39* | NR |
| 1 | α-Methyl-DL-histidine | 1.00E−02 | 0.29 | 0.38 | 0.34 | 0.72* | NR |
| 1 | Indole-3-lactic acid | 1.48E−10 | 0.31 | 1.09* | 0.22 | 1.31* | NR |
| 1 | Bilirubin | 7.67E−07 | 0.81 | 0.70* | 0.31 | 1.01* | NR |
| 1 | Kynurenine | 3.17E−08 | 1.16 | 0.96* | 0.44* | 1.40* | NR |
| 1 | Phenylalanine | 6.44E−12 | 4.48 | 0.28 | 1.29* | 1.57* | NR |
| 1 | 1-(1Z-octadecenyl)-2-(4Z,7Z,10Z,13Z,16Z-docosapentaenoyl)-sn-glycero-3-phosphoethanolamine | 4.14E−03 | 0.20 | 0.45 | 0.36 | 0.81* | NR |
| 1 | PC(P-16:0/22:6(4Z,7Z,10Z,13Z,16Z,19Z)) | 3.05E−05 | 0.15 | 0.48* | 0.17 | 0.65* | NR |
| 1 | 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoethanolamine | 5.64E−04 | 0.56 | 0.42* | 0.33 | 0.75* | NR |
| 1 | 1-palmitoyl-2-[(9Z,12Z,15Z)-octadecatrienoyl]-sn-glycero-3-phosphocholine | 1.09E−02 | 0.40 | 0.30 | 0.41 | 0.72* | NR |
| 1 | PC(18:3(9Z,12Z,15Z)/18:2(9Z,12Z)) | 4.14E−03 | 1.03 | 0.21 | 0.49* | 0.70* | NR |
| 1 | 1-octadecanoyl-2-[(4Z,7Z,10Z,13Z,16Z)-docosapentaenoyl]-sn-glycero-3-phosphoethanolamine | 2.57E−03 | 0.57 | 0.39 | 0.39 | 0.78* | NR |
| 1 | 1-oleoyl-2-arachidonoyl-sn-glycerol-3-phosphoethanolamine | 7.35E−02 | 0.13 | 0.11 | 0.46 | 0.57* | NR |
| 1 | Androsterone | 5.37E−11 | 0.21 | 1.59* | − 0.97* | 0.62* | R |
| 1 | (2S,3R,4E)-2-(Dodecanoylamino)-3-hydroxy-4-octadecen-1-yl 2-(trimethylammonio)ethyl phosphate | 6.24E−03 | 1.54 | − 0.36 | 0.72* | 0.36 | R |
| 1 | L-alpha-lysophosphatidylcholine | 3.42E−03 | 1.81 | − 0.34 | 0.82* | 0.48 | R |
| 1 | (2R)-1-(Phosphonooxy)-3-(stearoyloxy)-2-propanyl (4Z,7Z,10Z,13Z,16Z)-4,7,10,13,16-docosapentaenoate | 8.76E−04 | 2.24 | − 0.54* | 0.95* | 0.41 | R |
| 2 | N-Acetylneuraminic acid | 5.35E−02 | 0.16 | 0.19 | 0.44 | 0.63* | NR |
| 2 | Propionylcarnitine | 6.73E−06 | 3.34 | − 0.44* | 1.01* | 0.57* | R |
| 2 | 4-Hydroxybenzaldehyde | 1.76E−03 | 1.60 | − 0.63* | 0.92* | 0.29 | R |
| 2 | Tryptophan | 1.04E−03 | 2.25 | − 0.40 | 0.85* | 0.45* | R |
| 2 | Nicotinamide | 1.34E−03 | 2.17 | − 0.28 | 0.89* | 0.61* | R |
| 2 | Tyrosine | 3.48E−06 | 3.65 | − 0.54* | 1.30* | 0.76* | R |
| 2 | 3-Hydroxy-3-[(3-methylbutanoyl)oxy]-4-(trimethylammonio)butanoate | 3.41E−04 | 1.97 | − 0.57* | 0.80* | 0.24 | R |
| 2 | 2,4,6-Octatriyn-1-ol | 2.10E−04 | 2.19 | − 0.69* | 1.05* | 0.36 | R |
| 2 | Pipecolic acid | 3.42E−03 | 1.63 | 0.01 | 0.54* | 0.54* | R |
| 2 | Carnitine | 2.95E−03 | 1.75 | − 0.03 | 0.56* | 0.52* | R |
| 3 | 2-linoleoyl-sn-glycero-3-phosphoethanolamine | 3.24E−03 | 1.81 | 0.23 | − 0.69* | − 0.46* | NR |
| 3 | 12,13-Epoxy-9-hydroxy-10-octadecenoate | 1.37E−01 | 0.06 | 0.10 | − 0.47 | − 0.37 | NR |
| 3 | L-alpha-Glycerylphosphorylcholine | 3.52E−03 | 1.87 | 0.09 | − 0.67* | − 0.58* | R |
| 3 | Homomethionine | 5.88E−04 | 1.05 | 0.8* | − 0.84* | − 0.04 | R |
| 3 | N6,N6,N6-Trimethyl-L-lysine | 2.99E−04 | 0.37 | 0.57* | − 0.46* | 0.11 | R |
| 3 | Z-Maleylacetic acid | 2.99E−03 | 1.78 | 0.42 | − 0.86* | − 0.44 | R |
| 3 | Testosterone | 1.15E−33 | 4.72 | 1.88* | − 2.14* | − 0.26* | R |
| 3 | Itaconic acid | 1.53E−02 | 1.32 | 0.33 | − 0.78* | − 0.45 | R |
| 3 | Aminolevulinic acid | 1.00E−02 | 0.85 | 0.54* | − 0.71* | − 0.17 | R |
| 3 | 4-[(3-Aminopropyl)amino]butanoic acid | 6.72E−05 | 1.74 | 0.37* | − 0.41* | − 0.04 | R |
| 3 | Testosterone sulfate | 3.42E−03 | 0.53 | 0.66* | − 0.62* | 0.04 | R |
| 3 | Androsterone sulfate | 6.24E−13 | 5.28 | 0.93* | − 1.56* | − 0.63* | R |
| 3 | N3,N4-Dimethyl-L-arginine | 2.52E−04 | 0.37 | 0.92* | − 0.74* | 0.18 | R |
| 3 | Hypoxanthine | 3.38E−02 | 0.45 | 0.40 | − 0.56* | − 0.16 | R |
| 3 | Proline | 6.90E−02 | 0.08 | 0.41 | − 0.56* | − 0.15 | R |
| 3 | Guanine | 1.03E−01 | 0.47 | 0.34 | − 0.69* | − 0.36 | R |
| 4 | Stachydrine | 2.56E−02 | 1.01 | 0.20 | − 0.52* | − 0.32 | NR |
| 4 | (S)-glyceryl 1,2-dilinoleate | 2.25E−02 | 1.05 | 0.23 | − 0.65* | − 0.42 | R |
| 4 | 1-oleoyl-2-linoleoyl-sn-glycerol | 1.17E−02 | 0.75 | 0.57* | − 0.74* | − 0.17 | R |
| 4 | Tetradecanoylcarnitine | 3.65E−02 | 0.10 | 0.56 | − 0.65* | − 0.09 | R |
| 4 | Oleoylcarnitine | 3.78E−07 | 1.65 | 1.18* | − 1.07* | 0.11 | R |
| 4 | Palmitoylcarnitine | 6.44E−05 | 0.41 | 1.11* | − 0.88* | 0.23 | R |
| 4 | Stearoylcarnitine | 7.90E−02 | 0.36 | − 0.06 | − 0.55 | − 0.62* | TR |
R = Recovery profile (p value < 0.05, Low versus Restored)/TR = Tendency to recovery (p value > 0.05, Low versus Restored))/ NR = Non-restored.
1Overall change by ANOVA paired analysis.2B versus L = Basal versus Low (Basal–Low) / 3L versus R = Low versus Restored (Low-Retored)/ 4B versus R = Basal versus Restored (Basal–Restored) / *p value < 0.05, Pairwise comparison (Turkey Posthoc). Log2Fold Change: negative values were linked to relatively high abundant metabolites and positive values to relatively low abundant metabolites.
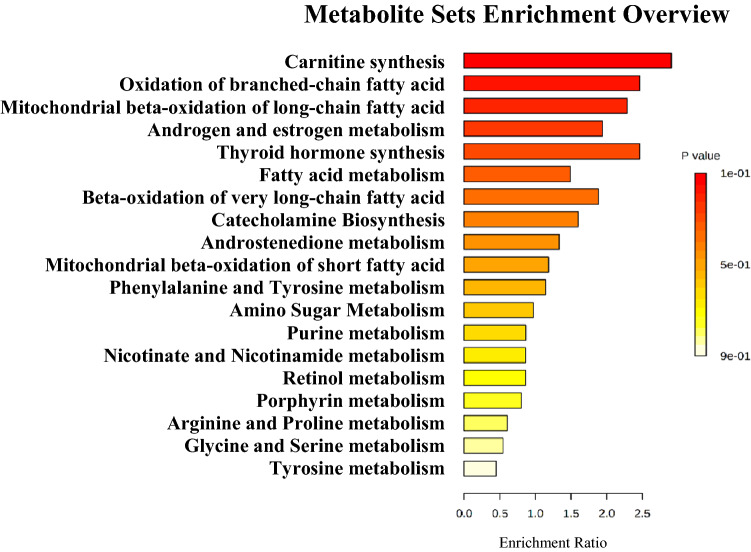
The hierarchical clustering analysis demonstrated that some metabolites reverted to basal levels or presented a tendency to recover after testosterone replacement, indicating that these compounds could potentially reflect the plasma testosterone level. In this respect, most of the compounds present in clusters 2, 3, and 4 seem to be driven by testosterone (Fig. 2C and Table 1), among them tyrosine, tryptophan, oleoylcarnitine, palmitoylcarnitine, and testosterone metabolites (ANOVA paired analysis, q value ≤ 0.05). Moreover, the biological roles connected with these metabolites present in clusters 2, 3, and 4 highlighted the importance of carnitine, beta-oxidation of fatty acids, and amino acid metabolism (p value > 0.05) as the top metabolic pathways altered by testosterone levels (Fig. 3). Moreover, other molecules (cluster 1) appear to be influenced by gonadotrophins, i.e., LH and FSH, since their levels did not restore after TS (Fig. 2C, Table 1). This pattern was also seen in indole compounds and different glycerophospholipids (ANOVA paired analysis, (q value ≤ 0.05).
Figure 3.
Pathway analysis of markers metabolites of testosterone levels identified by sPLS-DA analysis. Metabolic Set Enrichment Analysis (MSEA) results based on search in The Small Molecule Pathway Database (SMPDB) library. Bar graphs illustrating the enrichment overview of the top metabolic pathways of metabolites present in clusters 2, 3, and 4 with recovery or tendency to recover the respective abundance profiles. Color intensity (yellow to red) indicates their increasing statistical significance.
Additionally, we carried out an ANOVA paired analysis to deeply examine which compounds were most impacted by the different plasma testosterone levels. A total number of 368 compounds with a statistical difference (q value ≤ 0.05, ANOVA paired) were identified, among them 311 were altered by low levels of testosterone and gonadotropins (pairwise comparison, Basal versus Low), 83 molecules normalized after testosterone supplementation (p value ≤ 0.05, Low vs. Restored) and 98 demonstrated tendency to recovery based on their median values (not statistically significant, Low vs. Restored).
The metabolites present in the Human Metabolome Database (HMDB) that appear to be regulated by testosterone are listed in the Table 2 (recovery or tendency to recovery profile). Compounds that appear to be driven by gonadotropins (metabolites non-restored) are listed in Table 3. Information about the chemical class or subclass that suggests biological function of respective metabolites are included. Metabolites present in Table 1 are not included. All molecules, including non-significant compounds are present in the supplementary data (Tables S2 and S3).
Table 2.
Metabolites associated with testosterone level.
| Class or Subclass | Compound | Log2 Fold change | Trend | ||
|---|---|---|---|---|---|
| B versus L1 | L × R2 | B × R3 | |||
| Amino acids, peptides, and analogues | Arginine | 0.78* | − 0.34 | 0.43 | TR |
| Acetyl-L-methionine | 0.83* | − 0.32 | 0.51 | TR | |
| Serine | 0.8* | − 0.54* | 0.26 | R | |
| Pyroglutamic acid | 0.63* | − 0.46 | 0.17 | TR | |
| Creatinine | 0.89* | − 0.48* | 0.42 | R | |
| Leucine/Isoleucine | − 0.74* | 0.66* | − 0.08 | R | |
| Citrulline | 0.66* | − 0.46* | 0.2 | R | |
| N(5)-Acetyl-L-ornithine | 0.52* | − 0.19 | 0.32 | TR | |
| Glutamine | 0.74* | − 0.27 | 0.46 | TR | |
| N-Acetylvaline | 0.5* | − 0.51* | − 0.01 | R | |
| Myristoylglycine | − 1.56* | 0.37 | − 1.19* | TR | |
| Ornithine | 0.63* | − 0.55* | 0.08 | R | |
| Carboxylic acids and derivatives | Succinic acid | 0.88* | − 0.51 | 0.36 | TR |
| Fatty Acyls | (2E)-hexadecenoylcarnitine | 0.68* | − 0.6* | 0.07 | R |
| Palmitic Acid | − 1.19* | 0.27 | − 0.92* | TR | |
| Meglutol | 0.76* | − 0.44 | 0.32 | TR | |
| pentadecanoic acid | − 1.52* | 0.31 | − 1.21* | TR | |
| cis-5,8,11,14,17-Eicosapentaenoic acid | − 0.83* | 0.1 | − 0.73* | TR | |
| 8Z,11Z,14Z-Eicosatrienoic acid | − 0.91* | 0.04 | − 0.88* | TR | |
| 3-[(15Z,19Z)-11,12-Dihydroxy-15,19-dotriacontadien-1-yl]-5-methyl-2(5H)-furanone | 0.71* | − 0.31 | 0.4 | TR | |
| 2,4-dihydroxyheptadec-16-ynyl acetate | − 1.56* | 0.4 | − 1.17* | TR | |
| 3-[(19Z)-15,16-Dihydroxy-19-dotriaconten-1-yl]-5-methyl-2(5H)-furanone | − 1.03* | 0.52 | − 0.51 | TR | |
| 2-Hydroxy-3-(pentadecanoyloxy)propyl (6Z,9Z,12Z,15Z)-6,9,12,15-octadecatetraenoate | 0.64* | − 0.05 | 0.59* | TR | |
| Glycerophospholipids | (2R)-1-[(6Z,9Z,12Z,15Z)-6,9,12,15-Octadecatetraenoyloxy]-3-(phosphonooxy)-2-propanyl (15Z)-15-tetracosenoate | 1.35* | − 0.17 | 1.18* | TR |
| 1-Oleoyl-2-Stearoyl-sn-Glycero-3-Phosphocholine | 0.94* | − 0.09 | 0.85* | TR | |
| 1-[(11Z)-octadecenoyl]-sn-glycero-3-phosphocholine | 0.83* | − 0.61* | 0.22 | R | |
| (2R)-2-Acetoxy-3-[(9Z)-9-octadecen-1-yloxy]propyl 2-(trimethylammonio)ethyl phosphate | 0.67* | − 0.45 | 0.22 | TR | |
| (18R)-24-Amino-21-hydroxy-21-oxido-15-oxo-16,20,22-trioxa-21lambda ~ 5 ~ -phosphatetracosan-18-yl (6Z,9Z,12Z)-6,9,12-octadecatrienoate | − 0.57* | 0.57* | 0.004 | R | |
| 1-hexadecanoyl-sn-glycero-3-phosphoethanolamine | 1.05* | − 0.45 | 0.59* | TR | |
| Hydroxy acids and derivatives | 3-Hydroxy-cis-5-tetradecenoylcarnitine | 0.62* | − 0.47 | 0.15 | TR |
| 12-Hydroxydodecanoic acid | 1.49* | − 0.18 | 1.31* | TR | |
| Imidazopyrimidines | Uric acid | 0.98* | − 0.66* | 0.32 | R |
| Keto acids and derivatives | Acetonedicarboxylic Acid | 0.88* | − 0.38 | 0.5 | TR |
| Non-metal oxoanionic compounds | Phosphoric acid | − 1.68* | 0.44* | − 1.25* | R |
| Organic phosphoric acids and derivatives | Dimethylphosphate | − 1.69* | 0.48* | − 1.2* | R |
| Organonitrogen compounds | Anandamide | 1.04* | − 0.1 | 0.94* | TR |
| Carbohydrates and carbohydrate conjugates | beta-D-Mannopyranose | 1.1* | − 0.12 | 0.98* | TR |
| (2xi)-D-gluco-heptonic acid | 0.8* | − 0.01 | 0.79* | TR | |
| 2,3-Diketogulonic Acid | 1.05* | − 0.51* | 0.54* | R | |
| (2R)-DIMBOA glucoside | − 1.36* | 0.61* | − 0.75* | R | |
| Phenols | p-Cresol | − 1.55* | 0.51* | − 1.04* | R |
| Prenol lipids | 7-Isopropyl-4a-methyl-1-methylene-1,2,3,4,4a,9,10,10a-octahydrophenanthrene | 1.3* | − 0.62* | 0.69* | R |
| 5-Isopropyl-2-methyl-2-cyclohexen-1-one | 1.02* | − 0.37 | 0.65* | TR | |
| Coenzyme Q2 | 0.75* | − 0.4 | 0.34 | TR | |
| (3R,6'R)-3',4',5',18'-Tetradehydro-5',6'-dihydro-beta,beta-caroten-3-ol | 0.95* | − 0.12 | 0.83* | TR | |
| Sphingolipids | Ceramide (d18:1/24:0) | 0.67* | − 0.06 | 0.61* | TR |
Do not include putative metabolites present in Table 1. R = Recovery profile (p-value < 0.05, Low vs. Restored)/TR = Tendency to recovery (p value > 0.05, Low vs. Restored))/ NR = Non-restored. 2B versus L = Basal versus Low (Basal–Low) / 3L versus R = Low versus Restored (Low-Retored)/ 4B versus R = Basal versus Restored (Basal – Restored) / *p value < 0.05, Pairwise comparison (Turkey Posthoc). Log2Fold Change: negative values were linked to relatively high abundant metabolites and positive values to relatively low abundant metabolites.
Table 3.
Metabolites associated with gonadotropin level.
| Class or Subclass | Compound | Log2 Fold change1 | Trend | ||
|---|---|---|---|---|---|
| B versus L3 | L × R4 | B × R5 | |||
| Fatty Acyls | Methyl 10-undecenoate | 0.66* | 0.11 | 0.77* | NR |
| Oleic acid | − 0.61* | − 0.23 | − 0.85* | NR | |
| ricinelaidic acid | 0.81* | 0.14 | 0.95* | NR | |
| 9,10-Dihydroxystearic acid | 0.54* | 0.02 | 0.57* | NR | |
| Stearic acid | − 0.67* | − 0.18 | − 0.85* | NR | |
| all-cis-4,7,10,13,16-Docosapentaenoic acid | − 0.66* | − 0.08 | − 0.74* | NR | |
| Docosahexaenoic acid | 1.26* | − 0.05 | 1.21* | NR | |
| Adrenic acid | − 0.66* | − 0.11 | − 0.77* | NR | |
| 15,16-Dihydroxyoctadecanoic acid | 0.72* | − 0.05 | 0.67* | NR | |
| 5-[8,10-Dihydroxy-11-(hydroxymethyl)-4,7-dimethyltridecyl]-6-ethyl-4-hydroxy-4,5-dimethyl-2-cyclohexen-1-one | − 0.71* | 0.12 | − 0.59* | NR | |
| 2,4-dihydroxyheptadec-16-enyl acetate | − 0.88* | − 0.14 | − 1.01* | NR | |
| α-Eleostearic acid | − 0.74* | − 0.13 | − 0.87* | NR | |
| Linoelaidic acid | − 0.63* | − 0.26 | − 0.89* | NR | |
| (2S)-1-Hydroxy-3-(pentadecanoyloxy)-2-propanyl (9Z,12Z)-9,12-octadecadienoate | 0.66* | 0.06 | 0.72* | NR | |
| (2S)-3-Hydroxy-2-(pentadecanoyloxy)propyl (9Z,12Z)-9,12-octadecadienoate | 0.53* | 0.15 | 0.69* | NR | |
| Glycerolipids | 1-Stearoyl-2-arachidonoyl-sn-glycerol | − 1.26* | 0.08 | − 1.17* | NR |
| (2S)-2,3-Dihydroxypropyl pentadecanoate | 0.79* | 0.02 | 0.81* | NR | |
| Glycerophospholipids | (2-Hydroxy-2-oxido-1,3,2-dioxaphospholan-4-yl)methyl palmitate | − 1.08* | − 0.14 | − 1.21* | NR |
| 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine | 0.72* | − 0.06 | 0.66* | NR | |
| PC | 0.99* | − 0.24 | 0.75* | NR | |
| 1-oleoyl-2-linoleoyl-sn-glycero-3-phosphocholine | 0.71* | 0.2 | 0.92* | NR | |
| PC(18:2(9Z,12Z)/18:2(9Z,12Z)) | 0.74* | 0.07 | 0.81* | NR | |
| 1-hexadecyl-2-[(9Z,12Z)-octadecadienoyl]-sn-glycero-3-phosphocholine | 0.45* | 0.02 | 0.47* | NR | |
| 1-[(9Z)-hexadecenyl]-2-[(9Z)-hexadecenoyl]-sn-glycero-3-phosphocholine | 0.65* | 0.21 | 0.85* | NR | |
| Dioleoylphosphatidylethanolamine | 0.73* | − 0.02 | 0.71* | NR | |
| 1-stearoyl-2-oleoyl-sn-glycero-3-phosphoethanolamine zwitterion | 0.61* | 0.22 | 0.83* | NR | |
| (9Z,21R)-27-Amino-24-hydroxy-24-oxido-18-oxo-19,23,25-trioxa-24lambda ~ 5 ~ -phosphaheptacos-9-en-21-yl (5Z,8Z,11Z)-5,8,11-icosatrienoate | − 0.64* | 0.15 | − 0.49* | NR | |
| (2R)-3-{[(2-Aminoethoxy)(hydroxy)phosphoryl]oxy}-2-[(1Z,11Z)-1,11-octadecadien-1-yloxy]propyl (9Z)-9-octadecenoate | 0.72* | − 0.12 | 0.6* | NR | |
| 1,2-dioleoyl-sn-glycero-3-phospho-N,N-dimethylethanolamine | 0.61* | − 0.19 | 0.41 | NR | |
| 1-arachidonoyl-sn-glycero-3-phosphoethanolamine | − 0.68* | − 0.24 | − 0.92* | NR | |
| PG(a-13:0/i-24:0) | 0.79* | 0.14 | 0.94* | NR | |
| Hydroxy acids and derivatives | Malic acid | 0.69* | 0.1 | 0.79* | NR |
| Indoles and derivatives | Indole-3-acetic acid | 0.99* | 0.16 | 1.15* | NR |
| Methyl indole-3-acetate | 0.76* | − 0.07 | 0.69* | NR | |
| Organonitrogen compounds | EPEA | 1.07* | 0.01 | 1.07* | NR |
| Choline | − 1.22* | − 0.04 | − 1.25* | NR | |
| Prenol lipids | (1E)-5-Hydroxy-4,8,12-trimethyl-1-(2,6,6-trimethyl-1-cyclohexen-1-yl)-1-pentadecen-7-one | 0.81* | − 0.09 | 0.72* | NR |
| 3-Hydroxy-3'-oxo-beta,epsilon-carotene | 0.51* | 0.12 | 0.64* | NR | |
| Sphingolipids | Ceramide (d18:1/16:0) | 0.93* | − 0.1 | 0.83* | NR |
| Sphinganine 1-phosphate | 0.68* | 0.26 | 0.94* | NR | |
| Palmitoyl sphingomyelin | 0.59* | 0.19 | 0.79* | NR | |
| D-Erythro-sphingosine 1-phosphate | 0.7* | 0.19 | 0.89* | NR | |
| Steroids and steroid derivatives | Cortisone | 1.37* | − 0.23 | 1.14* | NR |
| Cortisol | 0.58* | 0.24 | 0.81* | NR | |
| Vitamin D and derivatives | Calcitriol | 0.9* | − 0.13 | 0.78* | NR |
Do not include putative metabolites present in Table 1. R = Recovery profile (p value < 0.05, Low vs. Restored)/TR = Tendency to recovery (p value > 0.05, Low vs. Restored))/ NR = Non-restored. 12B versus L = Basal versus Low (Basal–Low) / 3L versus R = Low versus Restored (Low-Retored)/ 4B versus R = Basal versus Restored (Basal–Restored) / *p value < 0.05, Pairwise comparison (Turkey Posthoc). Log2Fold Change: negative values were linked to relatively high abundant metabolites and positive values to relatively low abundant metabolites.
Markers compounds of testosterone and gonadotropin levels
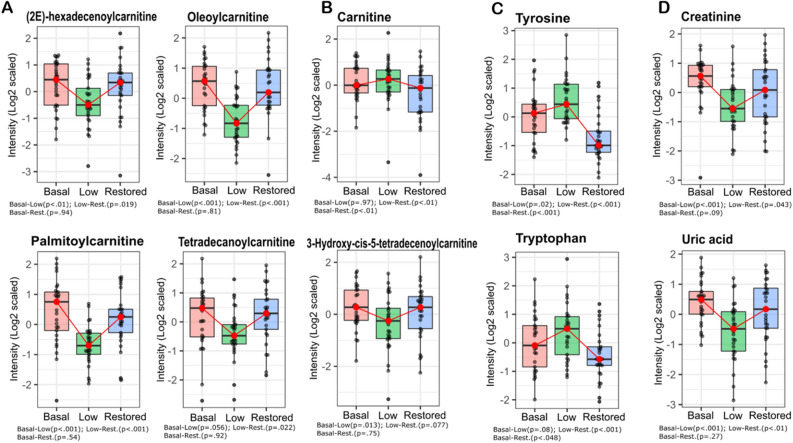
The untargeted metabolomic analysis revealed metabolites that vary in concentration in parallel with testosterone. Acylcarnitines, many intermediate compounds of arginine metabolism, and common biomarkers of renal function, i.e., creatinine and uric acid, decrease after TD and normalize after TS. On the other hand, aromatic amino acids, i.e., tryptophan and tyrosine, seem to be driven by testosterone in a converse manner, increasing in concentration after androgen depletion and reverting to basal levels with TS (Fig. 4 and Figure S2). In contrast, cortisol, a hydroxysteroid, did not recover after TS (Figure S1).
Figure 4.
Markers of testosterone levels. Levels of some metabolites after TD and TS. (A) Some acylcarnitines: (2E)-hexadecenoylcarnitine*,#, Oleoylcarnitine*,#, Palmitoylcarnitine*,#, 3-Hydroxy-cis-5-tetradecenoylcarnitine*, and Tetradecanoylcarnitine*,#. (B) Carnitine#,ǂ. (C) Aromatic amino acids: Tyrosine*,#,ǂ, and Tryptophan#,ǂ. (D) Biomarkers of kidney function: Creatinine*,#, and Uric acid*,#. Boxplot colors: Pink, Basal testosterone group; Green, Low testosterone group; Blue, Restored testosterone group. *p value ≤ 0.05, Basal versus Low, #p value ≤ 0.05, Low versus Restored, ǂp value ≤ 0.05, Basal vs. Restored.
In addition to the evaluation of short-term metabolic changes driven by testosterone, our study model may also allow for metabolite identification that reflect LH and FSH levels. The results indicate that low LH and FSH might alter the concentration of plasma lipids, e.g., glycerophospholipids and sphingolipids, compounds associated with tryptophan and indole metabolism, and calcitriol. Our results showed that these metabolites decreased in parallel with the gonadotropins (Table 3).
Discussion
To the best of our knowledge, this is the first study investigating the metabolomic changes in a cohort of young, healthy men with pharmacologically induced TD and subsequent TS. Testosterone deficiency has a complex association with hypogonadism, obesity, metabolic dysfunction, impaired glucose tolerance, type 2 diabetes mellitus, and sleep disorders24. The design of our study model enabled an evaluation of the early metabolic effects associated with variations in testosterone and gonadotropins levels without the influence of comorbidities and age. The pharmacological supplementation of testosterone to chemically castrated men results in metabolic changes similar to what is seen in individuals with low gonadotropins and normal testosterone. A comparison between the metabolic states before TD and after TS could therefore provide clues to identify pathways and metabolites that reflect testosterone fluctuations (with normal gonadotropin levels). These changes correspond to what was seen in the present human model, both amino acid and lipid metabolism were altered, and testosterone supplementation could restore 83 of 311 metabolites (additionally, 98 compounds demonstrate tendencies to recover), indicating that some of the metabolic changes may be driven by a decrease in gonadotropin rather than testosterone levels. Insulin-like growth factors, tyrosine catabolism and the level of many other amino acids, glucose metabolism (glycolysis/gluconeogenesis)21–23, as well as steroidal profile, mitochondrial metabolism, and renal biomarkers were impacted by testosterone or by its derivatives. Our findings demonstrate that testosterone might influence the levels and metabolism of acylcarnitines, amino acids, and renal markers. The amino acid and renal markers changes could indicate the role of testosterone in protein turnover. Furthermore, our results further suggest that LH and FSH strongly affect the levels of indoles and lipids, especially glycerophospholipids and sphingolipids.
Carnitine is a key metabolite in energy metabolism in most mammals, where it supports energy metabolism by transporting long-chain fatty acids into mitochondria for energy production. Our metabolomic analysis revealed that acylcarnitines levels change in a testosterone-sensitive direction, decreasing after TD and restoring upon TS (Table 2 and Fig. 4A). This is in agreement with Fanelli and coworkers who showed that male patients with hypogonadism present lower levels of acylcarnitines25, an alteration that was even more pronounced in patients with insulin resistance, which appeared to be involved with the metabolism of acetyl-CoA and production of precursor for gluconeogenesis26. Also, our previous study in rats showed that TS increases the acylcarnitine levels27.
Additionally, testosterone has been associated with the promotion of lipid oxidation28–30 Our results showed that the concentration of palmitoylcarnitine and palmitic acid, lipid oxidation-related molecules, were correlated with testosterone changes. Palmitoylcarnitine decreased upon testosterone decrease and increased after testosterone supplementation, whereas palmitic acid increased upon testosterone decrease and was partially restores after testosterone supplementation. Similar changes were seen in a previous study, in which palmitic acid oxidation increased in human myotubes after treatment with testosterone30. Altogether, these findings might reflect the role of testosterone in modulating lipid oxidation and, consequently, changing the acylcarnitines and fatty acids plasma levels. However, since carnitine and acylcarnitines are affected not only by mitochondrial metabolism but also by several diseases31, this must be taken into account when considering the influence of testosterone in various clinical scenarios.
Also, several studies have pointed out that testosterone could impair renal function, promoting tubular epithelial apoptosis in a dose-dependent way32 and reducing estimated glomerular filtration, which could elevate creatinine levels33. Our study also indicates that testosterone could promote higher levels of kidney function markers (i.e., creatinine and uric acid) since subjects with basal and restored testosterone levels showed an increased abundance of these metabolites (Table 2 and Fig. 4D). These findings are in agreement with a recent study where higher testosterone was associated with an increment in uric acid levels in adolescent boys34,35, and a case report of hypogonadism where renal function decreased after testosterone replacement therapy and creatinine levels increased36. However, considering that creatinine is also involved in muscle metabolism, the positive correlation between testosterone and creatinine might reflect the increase in muscle mass and not an impairment in renal function37. This is especially important, taking into account that creatinine has been reported as a biased biomarker of acute change in kidney function since its levels can vary widely due to hydration status, age, sex, muscle mass, and metabolism38. Similarly, increased uric acid levels might mirror mass muscle growth due to a rise in purines levels35. In a previous study on trans men who received TRT, uric acid and creatinine levels increased in a dose-dependent manner, which is at least partially attributed to an increment in muscle mass39. These findings emphasize that the respective classical renal-muscle mass biomarker could reflect testosterone levels and thus contribute valuable diagnostic information when monitoring patients under TRT.
Our results concerning amino acids and protein turnover are challeging. The hierarchical clustering analysis based on sPLS-DA data highlighted that the abundance of some amino acids (e.g. tryptophan and tyrosine) correlate negatively with testosterone, low levels of testosterone were associated with increased tryptophan and tyrosine levels, supporting the suppressive effect of testosterone on protein breakdown (Table 1 and Fig. 4C)40. This is in contrast to arginine and metabolites of the arginine biosynthesis pathway, especially citrulline and ornithine, that decrease in concentration after testosterone depletion and restored or tended to restore (based on median values) after testosterone supplementation. Considering that citrulline and arginine have been reported as functional nutrients able to enhance muscle protein synthesis41–43, these findings might reflect the muscle protein anabolism mediated by testosterone.
The results concerning lipid metabolism regulation revealed a complex metabolic picture. The ANOVA paired analysis and the sPLS-DA data highlighted that testosterone alteration and gonadotropins depletion are linked to lipid metabolism. While some of the lipid metabolites increase after androgen deprivation, others decrease. The different patterns may be due to the different effects of testosterone and gonadotropins, testosterone appears to suppress fatty acids synthesis44, whereas FSH promotes the biosynthesis of these metabolites by upregulation of genes involved in lipid biosynthesis45,46. In addition, most sphingolipids changed parallel with the gonadotropins, reduced levels after testosterone depletion and no normalization after testosterone supplementation, thus suggesting that FSH and/or LH are important for lipid metabolism (Tables 2 and 3). Interestingly, sphingolipids (e.g., ceramides, sphingomyelin, and sphingosine-1-phosphate) appear to influence steroidogenesis at different biological levels, including actions as second messengers in signaling cascades and regulation of gene and enzymes expression that controls steroidogenesis47,48.
The level of one of the fat soluble vitamins, calcitriol (i.e., bioactive vitamin D) showed a tendency to decrease upon testosterone depletion, and did not increase after testosterone supplementation, possibly indicating that gonadotropins are involved in vitamin D metabolism, also supported by the fact that low levels of vitamin D have been correlated with secondary hypogonadism21,49. Moreover, according to the The European Society of Endocrinology Clinical Guideline several hormonal alterations, among them testosterone deficiency, low values of LH/FSH ratios in men, and vitamin D deficiency50 often occur together, indicating that a functional relationship may exist.
Lastly, some metabolites of tryptophan and indoles turnover decreased after testosterone depletion and did not restore by testosterone. Some of these indoles represent microbial metabolites from tryptophan gut metabolism51 and the alteration may be the result of the altered steroid profile, several studies indicate that steroids influence the gut microbiome52,53.
In summary, our study demonstrates the importance of testosterone and gonadotropins for the plasma metabolome in young, healthy men. Major metabolic pathways were impacted by testosterone depletion, changes that only in some cases could be reverted by testosterone supplementation indicating that not only testosterone but also gonadotropins are important for metabolic regulation. These findings may contribute to a better understanding of the mechanisms behind the association of testosterone deficiency and its comorbidities.
Materials and methods
We performed an untargeted metabolomic analysis based on UHPLC–HRMS to evaluate the short-term metabolic changes associated with testosterone depletion and its subsequent restoration in a healthy young men cohort. The efficiency of chemical castration and testosterone replacement was previously verified by measuring the levels of gonadotropins and sex hormones (Table 4)20. Most subjects restored their testosterone levels or exhibited higher testosterone than at baseline after testosterone supplementation. As expected, LH and FSH were not restored after testosterone supplementation due to the GnRHa effect. The natural recovery of testosterone was not applied in this study to evaluate what happens in individuals with low gonadotropins and normal testosterone since this is a way to study the changes correlated with testosterone plasmatic alterations. Furthermore, since the testosterone axis recovery period varies significantly among males, this fluctuation might interfere with the last time point metabolic analysis.
Table 4.
Plasma concentration of gonadotropins and sex hormones in the three groups: Basal, Low and Restored testosterone levels.
| Biomarker | Mean ± SD | ||
|---|---|---|---|
| Basal | Low | Restored | |
| Testosterone (nmol/L)a,b,c | 19.97 ± 5.7 | 0.71 ± 0.3 | 37.39 ± 11.1 |
| Estradiol (pmol/L)a,b,c | 107.66 ± 18.4 | 91 ± 0 | 144.45 ± 49.6 |
| Luteinising hormone-LH (IU/L)a,c | 4.99 ± 1.6 | 0.14 ± 0.1 | 0.14 ± 0.1 |
| Follicle stimulating hormone—FSH (IU/L)a,c | 3.09 ± 1.7 | 0.15 ± 0.1 | 0.14 ± 0.1 |
This results were extracted from Sahlin et al22. Variables are expressed as mean ± standard deviation.
ap value < 0.05, Basal versus Low.
bp value < 0.05, Low versus Restored.
cp value < 0.05, Basal versus Restored.
Subjects and ethical considerations
Thirty healthy men of 23.9 years old (19–32 years) were recruited for this study. All subjects had a body mass index of 20–25 kg/m2 and were non-smokers or occasional smokers, without any chronic diseases, such as cancer, diabetes, liver, and heart disease. The selected participants did not use anabolic steroids or any regular medication20. All experimental procedures were approved by the Regional Ethical Review Board Lund (Approval number: DNR 2014/311) and performed in accordance with relevant guidelines and regulations. The study was registered at the NIH clinical trial registry (http://clinicaltrials.gov, Registration number: NCT03541395, date of registration 30/05/2018) and all participants signed informed consent.
Study design: testosterone depletion and replacement
Thirty subjects were submitted to a testosterone depletion by the use of gonadotropin-releasing hormone antagonist (GnRHa) (subcutaneous injection, 240 mg, Degarelix, Ferring Pharmaceuticals, Sweden) and, after three weeks, to an androgen supplementation by use of testosterone undecanoate (intramuscular injection, 1000 mg, Nebido, Bayer Pharmaceuticals, Germany)20.
Therefore, blood samples were collected three times: (i) before TD, corresponding to testosterone and gonadotropins' baseline levels (Basal group); (ii) before the androgen supplementation, relating to low testosterone and gonadotropins' levels (Low group); (iii) two weeks after TS, corresponding to Testosterone restored samples (Restored group) (Fig. 1).
The naturally recover of testosterone was not applied in this study in order to evaluate what happens in an individual with low gonadotropins and normal testosterone. We assumed that this is a way to study the changes correlated just with testosterone fluctuations. Furthermore, it is important to consider that the testosterone axis recovery period varies significantly among males. Therefore, we believe that this variance would interfere with the last time point metabolic analysis.
Sample preparation
Blood plasma samples from the thirty subjects, in fasting condition, submitted to testosterone depletion and replacement were collected in tubes with sodium citrate. For metabolomic experiments, plasma proteins were precipitated with ice-cold methanol enriched with an isotopic labeled internal standard (Testosterone-D3, 50 nM, LGC Standards; London, England). The samples were maintained at − 30 °C for 30 min, followed by centrifugation at 14000 g for 15 min at 40 °C. Supernatants were collected, dried, and reconstituted in 0.1% formic acid27. A pool of all samples was used as quality control (QC). The QC was prepared using 10 µL of each experimental sample and submitted for the same procedures as performed in the experimental samples. Blank samples (0.1% formic acid) were prepared following the same procedures and used to analyze possible contaminants and to determine background signals. Among the ninety samples, one was excluded from this study due to technical problems.
UHPLC–HRMS: untargeted metabolomics analysis
Samples were analyzed by ultra-high-performance liquid chromatography (Dionex Ultimate 3000 UHPLC, Thermo Scientific, USA) coupled to high-resolution mass spectrometry (Q-Exactive Plus, Thermo Scientific, USA). Chromatographic separation was carried out employing a C18 column (Zorbax, 50 × 2.1 mm, 1.8 μm, Agilent, USA) and a mobile phase constituted of aqueous solution A (0.1% formic acid and 5 mM ammonium formate) and organic solution B (methanol acidified with 0.1% formic acid). The column was held at 40 ºC. A gradient method (400 μL min-1) was applied over 20 min, as follows: 0–1 min, 5% B; 1–14 min, linear gradient from 5 to 100% B; 14–16 min, 100% B; 16–16.5 min, decreasing linearly from 100 to 5% B; 16.5–20 min, 5% B.
The autosampler unit was maintained at 7 ºC. A volume of 8 µL of each sample was injected in triplicate and analyzed in positive and negative mode. The untargeted metabolomics samples were analyzed in an HRMS with electrospray ionization and scanning in full MS mode (m/z 70–800) with data-dependent acquisition (dd-MS2, top-10 DDA). The source ionization parameters were: spray voltage of 3.90 kV (positive mode) and 2.90 kV (negative mode); capillary temperature, 380 °C; auxiliary gas temperature, 380 °C; 60 sheath gas and 20 auxiliary gas. The mass spectrometer for MS1 and MS2 were set as follows: (a) MS1 = resolution of 70 000, AGC target 1e6, maximum IT 100 ms; (b) MS2 = resolution of 17 500, AGC target 1e5, maximum IT 50 ms, loop count 10, isolation window 2.0 m/z, HCD normalized collision energy of 30.
Before analyzing the samples, the UHPLC–HRMS system was conditioned with 10 injections of 8 µL of pool plasma, using the same parameters described above. Blank samples and quality controls (QC) were analyzed in the same way as the experimental samples. QC samples were injected and analyzed at six different times during the experiment to assess the equipment's stability and reproducibility. A washing protocol was applied between each biological sample. Retention time, peak shape, and intensity of the internal standard were monitored to evaluate the system suitability.
Data processing and metabolomics statistical analysis
Raw files from UHPLC–HRMS were analyzed by Compound Discoverer 3.1 (Thermo Fisher, USA) using an untargeted metabolomic workflow that aligns the MS chromatographic peaks, matches, and compares parents and fragments ions to identify the metabolites present in the samples. The putative metabolite identifications was supported by comparison with data from the Human Metabolome Database (HMDB), Kyoto Encyclopedia of Genes and Genomes (KEGG), NIST-Wiley Mass Spectral Library (NIST), Lipid Maps, BioCyc Database Collection (BioCyc), MassBank, and MZcloud. Thus, the identification of metabolites or putative metabolites was based on a spectrum-structure match of accurate mass and tandem mass data of external libraries, providing a level 2 identification54. Five ppm of mass accuracy, 106 of minimum peak intensity, and 0.2 min of retention time variance were accepted for compound detections.
The average of the triplicate injection was used as a unique value, and the data were normalized by log10 transformation and sample median subtraction. Statistical analyses performed to detect differentially expressed metabolites were carried out in RStudio software. A multilevel sparse partial least squares discriminant analysis (sPLS-DA) was performed using ‘mixOmics’ R package55. This multivariate analysis classifies the samples by performing a multivariate regression while considering the complex structure of repeated measurements. The metabolite abundance matrix (706 plasma compounds) was used as predictors and time point (Basal, Low, and Restored testosterone) as the response variable. The most informative compounds to discriminate samples were selected through a LASSO penalization implemented in the ‘mixOmics’ R package. With the selected compounds, an unsupervised hierarchical clustering plus heatmap was performed using the ‘pheatmap’ R library. In addition to the multivariable analysis, a paired ANOVA (afex::aov_ez R function) followed by FDR correction was performed to determine significant overall differences among the time points. To detect differences between individual time points, i.e., Basal versus Low, Low versus Restored, and Basal versus Restored, we used the ‘emmeans’ R package for pairwise post hoc multiple comparisons with a p-value adjustment equivalent to the Tukey test (obtained through the ‘pair’ R function). Metabolites with an adjusted p value < 0.05 were considered significant. The Log2 fold-change of each comparison was correlated to increment or decrease in metabolites abundance. In this way, negative values were linked to relatively high abundant metabolites and positive values to relatively low abundant metabolites.
All known compounds present in HMDB and KEGG responsible for the cluster separation were employed in the pathways analysis, among them, only six were non-significant (ANOVA paired analysis, q value > 0.05). More information about all compounds pointed by sPLS-DA, such as normalized average area value and Log2 fold-change, is present in the supplementary data (Table S1).
MetaboAnalyst 5.0 was employed to analyze the pathways associated with the statistically significant and deregulated metabolites56. In this sense, metabolic Set Enrichment Analysis based on search in The Small Molecule Pathway Database (SMPDB) library were performed57.
Ethical approval
This study was registered and approved by the Regional Ethical Review Board Lund (Approval number: DNR 2014/ 311). All experiments were performed in accordance with relevant guidelines and regulations.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Supplementary Information
Acknowledgements
We are grateful to the Laboratório de Apoio ao Desenvolvimento Tecnológico (LADETEC) of the Institute of Chemistry from the Federal University of Rio de Janeiro for providing high-quality infrastructure for the UHPLC–HRMS analysis.
Author contributions
J.S.G., G.M., F.C.S.N., G.B.D. designed metabolomics experiments. J.S.G., G.M. performed metabolomics experiments. J.S.G., I.P., G.M., A.S., F.C.S.N., G.B.D., J.M. analyzed the data. JSG draft the manuscript. K.B.S., I.P., G.M., A.S., F.C.S.N., G.B.D., A.G., R.A., J.M., G.M-V. revised the paper. G.B.D., F.C.S.N., A.G., G.M-V., J.M. funding acquisition. IP and AS performed statistical analyses. J.S.G., I.P., K.B.S., G.M., R.A., G.M-V., A.G., G.B.D., A.S., F.C.S.N., J.M. provided the scientific oversight of the study.
Funding
Open access funding provided by Lund University. The Brazilian National Research Council (CNPq, 308341-2019-8 (G.B.D.); 315167/2020-3 (F.C.S.N)), the Carlos Chagas Filho Rio de Janeiro State Research Foundation (FAPERJ, E-26/210.173/2018 (G.B.D.); 26/202.650/2018 (F.C.S.N.)), and the Interreg V EU program, ReproUnion 2.0 20201846 generously providing funding to support the execution of this study.
Data availability
The data acquired in this study are available from the corresponding authors on request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors jointly supervised this work: Aniel Sanchez, Fábio César Sousa Nogueira and Johan Malm.
Contributor Information
Aniel Sanchez, Email: aniel.sanchez@med.lu.se.
Fábio César Sousa Nogueira, Email: fabiocsn@iq.ufrj.br.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-19494-w.
References
- 1.Bain J. The many faces of testosterone. Clin. Interv. Aging. 2008;2:567–576. doi: 10.2147/CIA.S1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sato K, Iemitsu M, Aizawa K, Ajisaka R. Testosterone and DHEA activate the glucose metabolism-related signaling pathway in skeletal muscle. Am. J. Physiol.-Endocrinol. Metab. 2008;294:E961–E968. doi: 10.1152/ajpendo.00678.2007. [DOI] [PubMed] [Google Scholar]
- 3.Mitsuhashi K, et al. Testosterone stimulates glucose uptake and GLUT4 translocation through LKB1/AMPK signaling in 3T3-L1 adipocytes. Endocrine. 2016;51:174–184. doi: 10.1007/s12020-015-0666-y. [DOI] [PubMed] [Google Scholar]
- 4.Wilson C, et al. Testosterone increases GLUT4-dependent glucose uptake in cardiomyocytes. J Cell Physiol. 2013;228:2399–2407. doi: 10.1002/jcp.24413. [DOI] [PubMed] [Google Scholar]
- 5.Kelly DM, Jones TH. Testosterone: a metabolic hormone in health and disease. J. Endocrinol. 2013;217:R25–R45. doi: 10.1530/JOE-12-0455. [DOI] [PubMed] [Google Scholar]
- 6.Ferrando AA, et al. Testosterone administration to older men improves muscle function: molecular and physiological mechanisms. Am. J. Physiol.-Endocrinol. Metab. 2002;282:E601–E607. doi: 10.1152/ajpendo.00362.2001. [DOI] [PubMed] [Google Scholar]
- 7.Mahmoud A, Comhaire FH. Mechanisms of disease: late-onset hypogonadism. Nat. Clin. Pract. Urol. 2006;3:430–438. doi: 10.1038/ncpuro0560. [DOI] [PubMed] [Google Scholar]
- 8.Gagliano-Jucá T, Basaria S. Testosterone replacement therapy and cardiovascular risk. Nat. Rev. Cardiol. 2019;16:555–574. doi: 10.1038/s41569-019-0211-4. [DOI] [PubMed] [Google Scholar]
- 9.Elagizi A, Köhler TS, Lavie CJ. Testosterone and cardiovascular health. Mayo Clin. Proc. 2018;93:83–100. doi: 10.1016/j.mayocp.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Zheng R, et al. Risk factors for hypogonadism in male patients with type 2 diabetes. J. Diabetes Res. 2016;2016:1–8. doi: 10.1155/2016/8610501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McBride JA, Carson CC, Coward RM. Testosterone deficiency in the aging male. Ther. Adv. Urol. 2016;8:47–60. doi: 10.1177/1756287215612961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shigehara K, Izumi K, Kadono Y, Mizokami A. Testosterone and bone health in men: A narrative review. J. Clin. Med. 2021;10:530. doi: 10.3390/jcm10030530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodrigues dos Santos M, Bhasin S. Benefits and Risks of testosterone treatment in men with age-related decline in testosterone. Annu. Rev. Med. 2021;72:75–91. doi: 10.1146/annurev-med-050219-034711. [DOI] [PubMed] [Google Scholar]
- 14.Gooren L. Androgen deficiency in the aging male: benefits and risks of androgen supplementation. J. Steroid Biochem. Mol. Biol. 2003;85:349–355. doi: 10.1016/S0960-0760(03)00206-1. [DOI] [PubMed] [Google Scholar]
- 15.SaboorAftab SA, Kumar S, Barber TM. The role of obesity and type 2 diabetes mellitus in the development of male obesity-associated secondary hypogonadism. Clin. Endocrinol. (Oxf.) 2013;78:330–337. doi: 10.1111/cen.12092. [DOI] [PubMed] [Google Scholar]
- 16.Dimitriadis GK, et al. Metabolic phenotype of male obesity-related secondary hypogonadism pre-replacement and post-replacement therapy with intra-muscular testosterone undecanoate therapy. Endocrine. 2018;60:175–184. doi: 10.1007/s12020-017-1516-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haring R. Perspectives for metabolomics in testosterone replacement therapy. J. Endocrinol. 2012;215:3–16. doi: 10.1530/JOE-12-0119. [DOI] [PubMed] [Google Scholar]
- 18.Carneiro G, Radcenco AL, Evaristo J, Monnerat G. Novel strategies for clinical investigation and biomarker discovery: a guide to applied metabolomics. Horm. Mol. Biol. Clin. Investig. 2019;38:20180045. doi: 10.1515/hmbci-2018-0045. [DOI] [PubMed] [Google Scholar]
- 19.Jacob M, Lopata AL, Dasouki M, Abdel Rahman AM. Metabolomics toward personalized medicine. Mass Spectrom. Rev. 2019;38:221–238. doi: 10.1002/mas.21548. [DOI] [PubMed] [Google Scholar]
- 20.Sahlin KB, et al. Short-term effect of pharmacologically induced alterations in testosterone levels on common blood biomarkers in a controlled healthy human model. Scand. J. Clin. Lab. Invest. 2020;80:25–31. doi: 10.1080/00365513.2019.1689429. [DOI] [PubMed] [Google Scholar]
- 21.Pla I, et al. A pilot proteomic study reveals different protein profiles related to testosterone and gonadotropin changes in a short-term controlled healthy human cohort. J. Proteomics. 2020;220:103768. doi: 10.1016/j.jprot.2020.103768. [DOI] [PubMed] [Google Scholar]
- 22.Sahlin KB, et al. Short-term effect of induced alterations in testosterone levels on fasting plasma amino acid levels in healthy young men. Life. 2021;11:1276. doi: 10.3390/life11111276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giwercman A, et al. Novel protein markers of androgen activity in humans: proteomic study of plasma from young chemically castrated men. Elife. 2022;11:e74638. doi: 10.7554/eLife.74638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zitzmann M. Testosterone deficiency, insulin resistance and the metabolic syndrome. Nat. Rev. Endocrinol. 2009;5:673–681. doi: 10.1038/nrendo.2009.212. [DOI] [PubMed] [Google Scholar]
- 25.Fanelli G, Gevi F, Belardo A, Zolla L. Metabolic patterns in insulin-sensitive male hypogonadism. Cell Death Dis. 2018;9:653. doi: 10.1038/s41419-018-0588-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gevi F, Fanelli G, Zolla L. Metabolic patterns in insulin-resistant male hypogonadism. Cell Death Dis. 2018;9:671. doi: 10.1038/s41419-018-0587-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Monnerat G, et al. Aging-related compensated hypogonadism: Role of metabolomic analysis in physiopathological and therapeutic evaluation. J. Steroid Biochem. Mol. Biol. 2018;183:39–50. doi: 10.1016/j.jsbmb.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Frederiksen L, Højlund K, Hougaard DM, Brixen K, Andersen M. Testosterone therapy increased muscle mass and lipid oxidation in aging men. Age. 2012;34:145–156. doi: 10.1007/s11357-011-9213-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Birzniece V, Meinhardt UJ, Handelsman DJ, Ho KKY. Testosterone stimulates extra-hepatic but not hepatic fat oxidation (Fox): comparison of oral and transdermal testosterone administration in hypopituitary men. Clin. Endocrinol. (Oxf.) 2009;71:715–721. doi: 10.1111/j.1365-2265.2009.03524.x. [DOI] [PubMed] [Google Scholar]
- 30.Salehzadeh F, Rune A, Osler M, Al-Khalili L. Testosterone or 17β-estradiol exposure reveals sex-specific effects on glucose and lipid metabolism in human myotubes. J. Endocrinol. 2011;210:219–229. doi: 10.1530/JOE-10-0497. [DOI] [PubMed] [Google Scholar]
- 31.McCann MR, George De la Rosa MV, Rosania GR, Stringer KAL. Carnitine and acylcarnitines: mitochondrial biomarkers for precision medicine. Metabolites. 2021;11:51. doi: 10.3390/metabo11010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peng Y, et al. Testosterone induces renal tubular epithelial cell death through the HIF-1α/BNIP3 pathway. J. Transl. Med. 2019;17:62. doi: 10.1186/s12967-019-1821-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pedersen L, Christensen LL, Pedersen SM, Andersen M. Reduction of calprotectin and phosphate during testosterone therapy in aging men: a randomized controlled trial. J. Endocrinol. Invest. 2017;40:529–538. doi: 10.1007/s40618-016-0597-3. [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Charchar FJ. Establishment of sex difference in circulating uric acid is associated with higher testosterone and lower sex hormone-binding globulin in adolescent boys. Sci. Rep. 2021;11:17323. doi: 10.1038/s41598-021-96959-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alvim RO, et al. Influence of muscle mass on the serum uric acid levels in children and adolescents. Nutr. Metab. Cardiovasc. Dis. 2020;30:300–305. doi: 10.1016/j.numecd.2019.08.019. [DOI] [PubMed] [Google Scholar]
- 36.Filler G, et al. Is testosterone detrimental to renal function? Kidney Int. Rep. 2016;1:306–310. doi: 10.1016/j.ekir.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baxmann AC, et al. Influence of muscle mass and physical activity on serum and urinary creatinine and serum cystatin C. Clin. J. Am. Soc. Nephrol. CJASN. 2008;3:348–354. doi: 10.2215/CJN.02870707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nickolas TL, Barasch J, Devarajan P. Biomarkers in acute and chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 2008;17:127–132. doi: 10.1097/MNH.0b013e3282f4e525. [DOI] [PubMed] [Google Scholar]
- 39.Kurahashi H, et al. Testosterone replacement elevates the serum uric acid levels in patients with female to male gender identity disorder. Endocr. J. 2013;60:1321–1327. doi: 10.1507/endocrj.EJ13-0203. [DOI] [PubMed] [Google Scholar]
- 40.Ferrando AA, Sheffield-Moore M, Paddon-Jones D, Wolfe RR, Urban RJ. Differential anabolic effects of testosterone and amino acid feeding in older men. J. Clin. Endocrinol. Metab. 2003;88:358–362. doi: 10.1210/jc.2002-021041. [DOI] [PubMed] [Google Scholar]
- 41.Jourdan M, et al. Citrulline stimulates muscle protein synthesis in the post-absorptive state in healthy people fed a low-protein diet—a pilot study. Clin. Nutr. 2015;34:449–456. doi: 10.1016/j.clnu.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goron A, et al. Citrulline stimulates muscle protein synthesis, by reallocating ATP consumption to muscle protein synthesis. J. Cachexia Sarcopenia Muscle. 2019;10:919–928. doi: 10.1002/jcsm.12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang X, Chinkes DL, Wolfe RR. The anabolic effect of arginine on proteins in skin wound and muscle is independent of nitric oxide production. Clin. Nutr. 2008;27:649–656. doi: 10.1016/j.clnu.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 44.Kelly DM, et al. Testosterone suppresses the expression of regulatory enzymes of fatty acid synthesis and protects against hepatic steatosis in cholesterol-fed androgen deficient mice. Life Sci. 2014;109:95–103. doi: 10.1016/j.lfs.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 45.Liu X, et al. FSH regulates fat accumulation and redistribution in aging through the Gαi/Ca 2+ /CREB pathway. Aging Cell. 2015;14:409–420. doi: 10.1111/acel.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu Z, et al. FSH and FOXO1 Regulate genes in the sterol/steroid and lipid biosynthetic pathways in granulosa cells. Mol. Endocrinol. 2009;23:649–661. doi: 10.1210/me.2008-0412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lucki NC, Sewer MB. Multiple roles for sphingolipids in steroid hormone biosynthesis. Subcell Biochem. 2008;49:387–412. doi: 10.1007/978-1-4020-8831-5_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lucki NC, Sewer MB. The interplay between bioactive sphingolipids and steroid hormones. Steroids. 2010;75:390–399. doi: 10.1016/j.steroids.2010.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee DM, et al. Association of hypogonadism with vitamin D status: the European Male Ageing Study. Eur. J. Endocrinol. 2012;166:77–85. doi: 10.1530/EJE-11-0743. [DOI] [PubMed] [Google Scholar]
- 50.Pasquali R, et al. European society of endocrinology clinical practice guideline: Endocrine work-up in obesity. Eur. J. Endocrinol. 2020;182:G1–G32. doi: 10.1530/EJE-19-0893. [DOI] [PubMed] [Google Scholar]
- 51.Agus A, Planchais J, Sokol H. Gut Microbiota regulation of tryptophan metabolism in health and disease. Cell Host Microbe. 2018;23:716–724. doi: 10.1016/j.chom.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 52.Tetel MJ, de Vries GJ, Melcangi RC, Panzica G, O’Mahony SM. Steroids, stress and the gut microbiome-brain axis. J. Neuroendocrinol. 2018;30:e12548. doi: 10.1111/jne.12548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hussain T, et al. Relationship between gut microbiota and host-metabolism: Emphasis on hormones related to reproductive function. Anim. Nutr. 2021;7:1–10. doi: 10.1016/j.aninu.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schymanski EL, et al. Identifying small molecules via high resolution mass spectrometry: communicating confidence. Environ. Sci. Technol. 2014;48:2097–2098. doi: 10.1021/es5002105. [DOI] [PubMed] [Google Scholar]
- 55.Rohart F, Gautier B, Singh A, Lê Cao K-A. mixOmics: An R package for ‘omics feature selection and multiple data integration. PLOS Comput. Biol. 2017;13:e1005752. doi: 10.1371/journal.pcbi.1005752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pang Z, et al. MetaboAnalyst 5.0: narrowing the gap between raw spectra and functional insights. Nucleic Acids Res. 2021;49:W388–W396. doi: 10.1093/nar/gkab382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chong, J., Wishart, D. S. & Xia, J. Using MetaboAnalyst 4.0 for Comprehensive and Integrative Metabolomics Data Analysis. Curr. Protoc. Bioinforma.68, (2019). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data acquired in this study are available from the corresponding authors on request.