Abstract
Objective:
To characterize quantitative studies on coaching interventions for professional surgeons to understand how surgical coaching is defined; examine how different coaching programs are designed, implemented, and evaluated; and identify any relevant research gaps.
Background:
Surgical coaching is gaining attention as an approach that could help surgeons optimize performance and improve overall wellbeing. However, surgical coaching programs and definitions of coaching vary widely between studies.
Methods:
A systematic literature search of PubMed, Scopus, Web of Science, CENTRAL, clinicaltrials.gov, and WHO ICTRP was conducted according to the PRISMA-ScR framework to identify studies and registered clinical trials written in English. Original quantitative studies on coaching interventions for professional surgeons were included. Characteristics of the coachees, coaching programs, study designs, outcomes, and findings were charted and analyzed.
Results:
From 2589 references, 8 studies (6 published; 2 registered trials) met inclusion criteria. Published studies targeted technical or nontechnical skills, included 2–26 surgeons as coachees, and used coaches who were surgeons. Two studies demonstrated that surgeons react positively to coaching. Studies showed inconsistent effects on technical/nontechnical skills. Only two studies measured patient adverse events and reported no significant positive impacts. The registered randomized trials targeted surgeons’ physiological parameters or wellbeing and used professional coaches. These trials measure surgeon and patient outcomes.
Conclusions:
There is an emerging interest in coaching programs to improve surgeons’ performance by targeting their professional skills and personal factors. However, more randomized trials are needed to evaluate the impact of coaching interventions on patient outcomes and surgeon wellness.
Keywords: coaching, nontechnical skills, technical skills, wellbeing, performance
Mini Abstract: This scoping review revealed that very few studies have quantitatively assessed coaching programs for surgeons focus on technical and nontechnical skills. Studies demonstrate that coaching is well accepted by surgeons. However, effects on technical/nontechnical skills are inconsistent and no evidence confirms that coaching improves patient outcomes. Additional randomized control trials are needed to evaluate the effects of surgical coaching on surgeons’ performance, patient safety, and surgeons’ wellness.
INTRODUCTION
Professional surgeons are expected to maintain peak performance throughout their careers. However, opportunities for continuous professional development (CPD) are often limited to short courses, lectures, and self-study. These methods have been criticized because they do not adhere to the principles of adult learning theories, which promote the use reflection, personalized feedback, and individualized goal setting for skill acquisition and behavior change.1,2 Furthermore, opportunities for CPD generally do not address the full range of factors that can affect a surgeon’s performance, including burnout, stress management, and wellbeing.3,4
Surgical coaching has been proposed as a solution that could be used to improve surgeons’ performance and overall wellbeing.5 Unlike mentoring and teaching, which involve advising and unidirectional knowledge transfer, coaching involves an exchange that guides the coachee to identify their own solutions.6 The potential benefits of coaching for surgeons have attracted increasing attention.5 However, this field of research is still developing, and the content and objectives of coaching programs are highly variable. Past reviews have included studies assessing coaching for surgeons in training, and have limited their scope to only include coaching interventions aiming to improve technical or nontechnical skills.7–12 No previous review has evaluated coaching interventions for professional surgeons targeting any aspect of their professional skills or personal development. This scoping review aims to identify quantitative studies on coaching interventions for practicing surgeons to clarify how surgical coaching is defined, to analyze how these interventions are designed, implemented, and evaluated, and to illuminate relevant research gaps in the field.
METHODS
Literature Search
The study protocol was registered a priori with the Open Science Framework (https://osf.io/3kzp4/). A systematic database search using PubMed, Scopus, and Web of Science was conducted in accordance with the PRISMA-ScR guidelines.13 Unpublished studies were identified using Cochrane CENTRAL, clinicaltrials.gov, and WHO ICTRP. Studies in English published or registered from the inception of each database up until the final search in March 2021 were included. Search algorithms for each database are detailed in Supplementary Table 1, http://links.lww.com/AOSO/A133. The reference lists of all included articles and relevant review articles were manually searched to identify additional studies.
Eligibility Criteria and Study Selection
Studies involving original quantitative research on coaching for professional surgeons were eligible. Interventions that included only unidirectional or intraoperative feedback, that involved only surgeons in training, were based around learning a new procedure, or reported only qualitative results were excluded. Two authors (S.C.S. and A.D) independently screened the titles and abstracts of identified citations according to the eligibility criteria. The full texts of all selected studies were screened by S.C.S and A.D. using the eligibility criteria to determine admissibility for data extraction. Disagreements between reviewers were resolved through discussion and mutual agreement.
Data Extraction and Analysis
One investigator (S.C.S.) extracted data using a predetermined form (Supplemental Table 2, http://links.lww.com/AOSO/A133). The data extraction was verified by another investigator (A.D.). Study outcomes were categorized using Kirkpatrick’s 4-level evaluation model adapted for coaching.14 Study designs were classified using a simplified version of Grading of Recommendations Assessment, Development, and Evaluation (GRADE) (randomized trials were considered “high” evidence level, quasi-experimental studies with contemporaneous controls were “moderate” and without controls were “low,” cross-sectional studies were “very low”).15
RESULTS
Four thousand two hundred twenty-six records were identified (Supplemental Figure 1, http://links.lww.com/AOSO/A133). Once duplicates were removed, 2589 references remained. After title and abstract screening, 27 articles were identified for full-text review. Ultimately, 6 published studies and 2 ongoing registered trials were selected for analysis.
Coaching Definitions and Goals
Each study was assigned an identifier based on the first or last author’s last name and the publication year (Table 1). Five of the six published articles defined coaching, peer coaching, surgical coaching, or surgical peer coaching. Common themes that emerged were the importance of a one-on-one, nonhierarchical coach-coachee relationship, the use of objective feedback, and setting individualized goals to refine existing skills.
TABLE 1.
List of Articles Selected for Inclusion and Their Definitions of Coaching
| No. | Title | Study ID | Coaching Definitions(s) | Study Objectives |
|---|---|---|---|---|
| 1 | A statewide surgical coaching program provides opportunity for continuous professional development | Greenberg et al16 | Coaching—“an experiential process for improving any aspect of surgical performance, including technical, cognitive, and interpersonal skills… based upon a partnership between 2 surgeons in which one facilitates the other’s pursuit of self-identified goals through collaborative analysis, peer support, and constructive feedback. Coaching emphasizes the development and refinement of the learner’s existing skills and his/her empowerment to make changes to practice” Peer coaching—“a distinctive type of coaching in which peers at a similar level of knowledge engage in an equal noncompetitive relationship” |
To develop and implement an evidence-based peer coaching program for board-eligible/certified surgeons across practice settings in the state of Wisconsin. The four main objectives were to identify the goals of surgeons participating in the peer coaching, evaluate the extent that the coaching session adhered to the stated goal, evaluate the effectiveness of surgeon coaches to employ activities of coaching; evaluate the perceived value of participation in a surgical coaching program |
| 2 | Targeted surgical coaching can improve operative self-assessment ability: A single-blinded nonrandomized trial | Bull et al17 | Surgical coaching—“a constructive relationship that provides objective feedback to individuals about a broad range of factors influencing operative performance. There is a focus on improvement and refinement of existing skills, rather than teaching new techniques or philosophies. Individualized approaches are required to effectively implement these objectives. Excellent coaching interactions encourage discussion, affirm positive beliefs, and challenge assumptions” | To investigate the effect of targeted surgical coaching on self-assessment of laparoscopic skill |
| 3 | Team Leader Coaching Intervention: An Investigation of the Impact on Team Processes and Performance Within a Surgical Context | Maynard et al18 | Coaching—“a process of equipping people with the tools, knowledge, and opportunities they need to develop themselves and become more effective.” Leadership coaching—“targeted interventions that involve a formal one-on-one relationship between a leader and a coach (who has no formal supervisor authority over the person being coached), with the purpose of improving the leader’s effectiveness” |
To determine whether a team leader coaching intervention can improve episodic team processes and enhance operating team outcomes |
| 4 | Surgical Coaching for Operative Performance Enhancement (SCOPE): skill ratings and impact on surgeons’ practice | Pradarelli et al19 | Surgical peer coaching—a “series of structured one-on-one discussions over time… provides space for surgeons to reflect on their performance with another surgeon (i.e., a peer coach) and make changes to their own practice” | To better understand the impact of coaching on surgeons’ performance, to measure surgeons’ technical and nontechnical skills throughout a longitudinal surgical coaching program |
| 5 | Feasibility of Surgeon-Delivered Audit and Feedback Incorporating Peer Surgical Coaching to Reduce Fistula Incidence following Cleft Palate Repair: A Pilot Trial | Sitzman et al20 | Surgical coaching—“a social interaction that aims to develop expertise by setting specific goals and providing feedback to achieve those goals” | To determine the feasibility of a surgeon-delivered audit and feedback intervention incorporating peer surgical coaching. |
| 6 | Association of a Statewide Surgical Coaching Program with Clinical Outcomes and Surgeon Perceptions | Greenberg et al21 | N/A | To assess the association between participation in a surgical coaching program and risk-adjusted outcomes |
| 7 | Evaluation of Coaching Impact on Surgical Outcomes | Duclos22 | N/A | To evaluate the impact of a customized surgical coaching program, targeting surgeons’ physiological factors (sleep, stress, physical activity), on the occurrence of patient major adverse events. |
| 8 | Effect of Coaching on Surgeon Wellbeing, Job Satisfaction, & Fulfillment | Dyrbye23 | N/A | To determine if individualized professional coaching improves physicians’ sense of wellbeing and jobsatisfaction. |
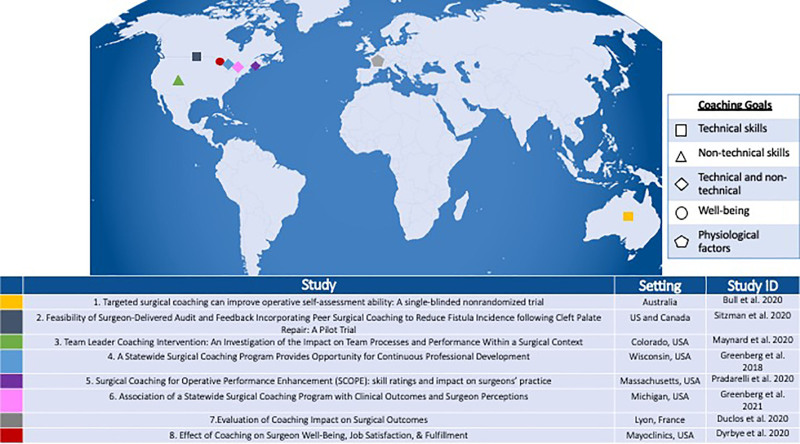
Details about the coaching programs are provided in Table 2. The coaching goals of all published studies targeted technical or nontechnical skills. Two studies focused on improving specific technical skills defined by the investigators.17,20 One study focused on leadership, a nontechnical skill, to improve episodic team processes.18 Three studies allowed coachees to identify their own goals related to their intraoperative performance.16,19,21 The registered trials target surgeons’ wellbeing and physiological factors.22,23 Figure 1 provides a visualization of the different interventions’ coaching goals and their settings.
TABLE 2.
Description of Coaching Programs
| Coaching Intervention Goals | Description of Coaches | Interaction | Coaching “Material” Used to Evaluate | Study ID | |||||
|---|---|---|---|---|---|---|---|---|---|
| Type of Intervention Goala | Overall Goalsa Defined by Coachees or Investigators? | Details About Coaching Goalsa | How Many? | Who Were the Coaches? | Were the Coaches Trained? | In Person? | Surgery Observed? | Metrics/Assessment Tools Used to Evaluate Coachees | |
| Technical skills | Investigators | Improve technical performance of cleft palate repair (decreasing fistula incidence) | 2 | Surgeons (peer) | No | In person | Video recording of operation in OR | Audit and feedback—collects standardized outcome measurements and reports individual and peer group results. | Sitzman et al20 |
| Investigators | Improve accuracy of self-assessment of laparoscopic operative skill using the OSATS scale | 2 | Surgeons (study investigators) | Specialists in rater training and coaching techniques | In person | Video recording of operation in OR | Coachees assessed the same peer surgery video at baseline, midway, and completion of the interventionto provide a point of reference for improving their use of the OSATS scale. |
Bull et al17 | |
| Nontechnical skills | Investigators | Leadership training to improve episodic team processes (transition, action, interpersonal) and team performance outcomes (surgical delays and distractions) | 1 | Surgeon (retired) | Certified in Crew Resource Management training | In person | Observation in OR | Coded assessment of surgical delays and distractions, and interpersonal, transition, and action processes | Maynard et al18 |
| Technical and/or nontechnical skills | Coachee | 6 coachees identified nontechnical goals (teaching, leadership, communication), 3 identified technical goals (new procedure, improving efficiency), and 2 did not identify a specific focus | 8 | Surgeons (peer) | 4-hour training session, training manual, and instructional videos | In person | Video recording of operation in OR | None | Greenberg et al16 |
| Coachee | Coachees could focus on any aspect of intraoperative performance, including technical skills, nontechnical skills (situational awareness, decision making, teamwork, leadership), or intraoperative teaching skills | 23 | Surgeons (peer) | 3-hour training session and weekly emails with coaching tips | In person | Observation in OR | OSATS and NOTTS | Pradarelli et al19 | |
| Coachee | No details about individual coachee’s goals were provided. | 15 | Surgeons (peer) | 4-hour training and “refresher” on coaching principles before each session | In person | Video recording of operation in OR | Operative time and 30-day patient complications | Greenberg et al21 | |
| Physiological factors | Coachee | Improve physiological factors to enhance surgeons’ performance and improve patient outcomes | N/A | Nonsurgeon | Certified professional coach | By videoconference | None | Charting system providing patient outcomes and profiling of individual surgeons as feedback | Duclos22 |
| Wellbeing | Coachee | Improve wellbeing (Burnout, job satisfaction, professional fulfillment) | N/A | Nonsurgeon | Certified professional coach | By phone | N/A | N/A | Dyrbye23 |
aThe goal the coachee was aiming to achieve over the course of the intervention. This goal was either defined by the study investigators or the coachees themselves.
OR, operating room; OSATS, objective structured assessment of technical skills; NOTTS, nontechnical skills for surgeons.
FIGURE 1.
Visualization of the coaching goals and settings of the interventions.
Participating Surgeon Coachees and Coaches
A median of 20 surgeons were included as coachees (Supplemental Table 3, http://links.lww.com/AOSO/A133). Two studies included coachees from only one surgical specialty.16,20 The six other studies included surgeons from multiple specialties (Table 3). Only one study recruited surgeons from a single center and included both attending surgeons and surgeons in training in the coachee group.17
TABLE 3.
Description of Study Designs, Coachees, and Study Setting
| Study Design | Coachee Population | ||||
|---|---|---|---|---|---|
| (GRADE Study Design)a | Mixed Methods? | Multi- or Monospecialty | No. | Study Setting | |
| Cross-sectional | No control (Very low) | Yes | Multispecialty | 11 | WI, USA |
| Quasi-Experimental | Before-After without contemporaneous control (Low) |
No | Multispecialty | 4b | Australia |
| Yes | Multispecialty | 23 | Boston, MA, USA | ||
| Before-After with contemporaneous control (Moderate) | No | Multispecialty | 20 | Rocky Mountain Region of CO, USA | |
| Yes | Monospecialty | 26 | MI, USA | ||
| Yes | Monospecialty | 2 | Across the U.S. and Canada | ||
| Experimental | Cluster-randomized trial (High) |
Yes | Multispecialty | 20 | Lyon, France |
| Crossover-randomized trial (High) |
No | Multispecialty | 80 | Mayoclinic, USA Multicenter |
|
aGRADE - simplified version of the Grading of Recommendations Assessment, Development, and Evaluation system - cross-sectional studies with no control group were classified as “very low”, quasi-experimental designs with no controls were classified as “low”, quasi-experimental designs with contemporaneous controls were classified as “moderate”, and experimental studies were classified as “high”. These ratings categorize studies based on their design, and unlike the comprehensive GRADE scale, do not fully reflect the validity or reliability of the research.
bStudy included 12 total coachees, but only 4 were attending surgeons, while 3 were fellows and 5 were residents.
In all of the published studies the coaches were professional surgeons; however, the studies differed in the level of training the coaches received. In one of the two studies that focused on technical skills, the coaches were surgeons who had lower fistula incidences than the coachees, but had no specific training in coaching techniques.20 In the other study, the coaches were study investigators, who were surgeons with considerable experience or training in coaching.17 Maynard et al18 implemented a team leader coaching intervention, which used a retired surgeon who was certified in Crew Resource Management training as a coach.
In the three studies that let coachees identify their own technical or nontechnical goals, the coachees were assigned peer coaches. The formats of these interventions were based on the Wisconsin Surgical Coaching Program (WSCP).24 Coaches attended a 3- to 4-hour training session in the beginning of the study, and received other training materials to help them maintain and deepen their understanding of coaching throughout the intervention. The coaches were selected based on a variety of factors. In Greenberg et al,16 coaches were chosen based on peer nominations from members of the Wisconsin Surgical Society. In Smink et al19 coaches were chosen by a local faculty surgeon at each academic medical center, based on their familiarity with the participants or the surgeons’ preferences. In Dimick et al21 members of the Michigan Bariatric Surgery Collaborative with the lowest rates of surgical complications were asked to participate as coaches. The ongoing trials differ from the published studies in that the coaches have specific training in coaching but are not surgeons.22,23
Coaching Interactions and Observation of Surgery
In the studies that provided the relevant information, the frequency and length of coaching sessions varied across the studies and among coachees, with surgeons attending between 1 and 8 sessions that ranged from 21 to 96 minutes in length. Details about the different coaching interventions can be found in Supplemental Table 4, http://links.lww.com/AOSO/A133. Coaching sessions took place in person in all of the published studies, whereas the registered trials by Dyrbye23 and Duclos et al22 will use coaching by phone or videoconference.
The coaching interactions were centered around the analysis of the coachees’ operations in all published studies. In four of these studies, video recordings of the coachee’s operations were discussed.16,17,20,21 In the other two published studies coaches observed the coachees operate in real time, and the coaching session took place at a later time.18,19 Conversely, the two registered trials do not include observations of coachees’ operations either in real time or by video recording (Table 2).22,23
Assessment Tools and Improvement Solutions
Only one published study provided assessment data in addition to coaching.20 This study combined coaching with an “audit and feedback” system, which provided each coachee with feedback about their own and the whole groups’ surgical outcomes before the coachee met with the coach. Four other published studies used metrics or scoring systems to evaluate surgeons’ technical or nontechnical skills or intraoperative performance but did not provide the information to the coachees as feedback.17–19,21 Duclos et al22 will use a charting system and individualized profiles to provide feedback, as well as modules of improvement to help guide surgeons during the intervention.
Study Designs and Outcomes
Study designs with corresponding GRADE levels are presented in Table 4. One study was cross-sectional,16 five were quasi-experimental studies with or without contemporaneous control groups,17–21 and the two ongoing registered trials were cluster or crossover-randomized designs.22,23 Four of the studies used mixed methods.
TABLE 4.
Study Outcomes and Findings
| Quantitative Outcomes | Findings | Study ID | ||||
|---|---|---|---|---|---|---|
| Kirkpatrick 1 (Reaction) | Kirkpatrick 3 (Behavior) | Kirkpatrick 4 (Results) | ||||
| Surgeons’ Reactions About Being Coached | Surgeons’ Technical Skills | Surgeons’ Nontechnical Skills | Surgeons’ Wellness | Patient Outcomes | Positive Outcome(s) ? | |
| Coachees used 5-point likert scales to evaluate the effectiveness of the coaches and to evaluate the program following the intervention | Yes | Greenberg et al16 | ||||
| A likert type participant questionnaire was used to evaluate the surgeons’ opinions about the coaching intervention and coaching in general, after the program | Improvement of self-assessment accuracy (using OSATS scale) compared to expert rating and correlation of self-assessment with expert ratings. | Yes | Bull et al17 | |||
| Summary assessment of the coachee’s overall technical skill and ratings for each of five domains of technical skills using the OSATS framework. | The Nontechnical Skills for Surgeons assessment tool was used to rate coachees performance on each of four domains of nontechnical skill: situation awareness, decision making, communication and teamwork. | No | Pradarelli et al19 | |||
| Evaluated episodic team processes (interpersonal, transition, and action processes measured by SME) and subsequent team performance outcomes (delays and distractions) | Yes | Maynard et al18 | ||||
| Operative time | 30-day overall complications and 30-day surgical complications | Operative time: yes; Patient outcomes: No |
Greenberg et al21 | |||
| Ornonasal fistula incidence | No | Sitzman et al20 | ||||
| Operative time | Burnout (MBI), Psycho-social risk (self-reported 26 item Karasek questionnaire) | Occurrence of major adverse event, death, unplanned stay in intensive care unit, unplanned reoperation, and intraoperative and post-operative complications | Duclos22 | |||
| MBI, Job satisfaction (self-reported Physician Job Satisfaction Scale score) and professional fulfillment (change in Empowerment at Work Scale) | Dyrbye23 | |||||
We used an adapted Kirkpatrick model to categorize the studies’ outcomes. Outcomes related to surgeons’ reactions to the coaching intervention or coaching in general were classified as level 1. Outcomes measuring technical or nontechnical skills, knowledge, or attitudes in a simulated environment were considered level 2. Outcomes measuring technical or nontechnical skill or changes in behavior measured in the operating room or in real life were classified as level 3. Patient outcomes or surgeon-centered outcomes were classified as level 4.
OSATS, Objective Structured Assessment of Technical Skills; MBI, Maslach Burnout Inventory Scale; SME, subject matter expert.
The following types of outcomes were identified: surgeons’ reactions about being coached, surgeons’ technical skills, surgeons’ nontechnical skills, surgeons’ wellness, and patient outcomes. Two studies addressed surgeon’s reactions about being coached, and were classified as Kirkpatrick level 1.16,17 No studies measured knowledge or skill acquisition in relation to coaching sessions using questionnaires, surveys, a simulated environment, or any other learning evaluation strategy. Therefore, no results were considered Kirkpatrick level 2 (learning). Four studies reported results related to surgeons’ technical skills during real operations, including OSATS skill ratings and operative time, and were classified as Kirkpatrick level 3 (behavior).17,19,21,22 Two studies reported outcomes related to nontechnical skills in the operating room and were also classified as Kirkpatrick level 3. One used the NOTTS scale, and the other coded team processes during surgery.18,19 The two registered trials plan to report surgeon wellness results, including measures of burnout, job satisfaction, and professional fulfillment, which were categorized as Kirkpatrick level 4 (results).22,23 Two published studies and one registered trial report patient outcomes, and were also classified as Kirkpatrick level 4.20–22
Main Findings
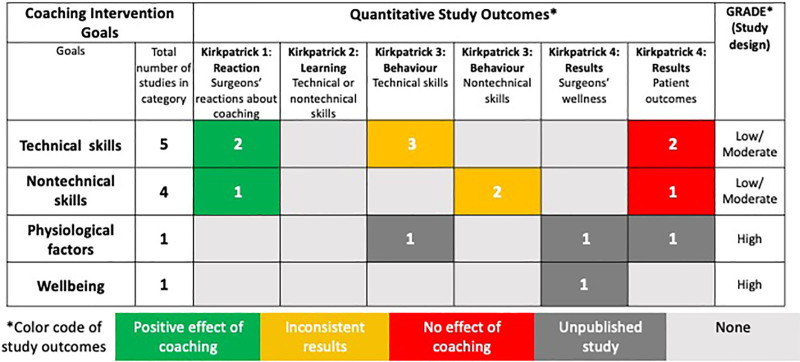
Results from published studies are summarized in Supplementary Table 5, http://links.lww.com/AOSO/A133 and Table 4. The two studies with Kirkpatrick level 1 analyses demonstrated that surgeons considered coaching to be effective, and reacted positively to the intervention.16,17 Of the four studies with Kirkpatrick level 3 evaluations, two showed that coaching improved technical skills, one showed that coaching improved nontechnical skills,17,18,21 but one found that coaching had no effect on technical/nontechnical skills.19 The two studies with Kirkpatrick level 4 evaluations failed to show that coaching significantly improved patient outcomes.20,21
To highlight research gaps, main findings were charted in Figure 2 according to studies’ coaching goals and measured outcomes.
FIGURE 2.
Research gaps diagram classifying studies by coaching goal, outcome, design GRADE, and findings. Study findings are represented by colors. Green represents positive findings, yellow mixed findings, and red negative findings. Dark gray represents outcomes of trials that have not been published yet. Light gray represents outcomes that were not evaluated by any of the studies included in the review. We used an adapted Kirkpatrick model to categorize the studies’ outcomes. Outcomes related to surgeons’ reactions to the coaching intervention or coaching in general were classified as Kirkpatrick level 1. Outcomes measuring technical or nontechnical skills, knowledge, or attitudes in a simulated environment were considered Kirkpatrick level 2. Outcomes measuring technical or nontechnical skill or changes in behavior measured in the operating room or in real life were classified as Kirkpatrick level 3. Patient outcomes or surgeon-centered outcomes were classified as Kirkpatrick level 4. We used an approach inspired by the GRADE system to to classify evidence levels based on intervention study designs. Randomized trials were considered “high,” quasi-experimental studies with contemporaneous controls were categorized as “moderate” and without controls as “low.”
DISCUSSION
Coaching is an emerging field that has been gaining traction as a possible approach to improve the performance and overall wellbeing of professional surgeons. However, the results of this scoping review show that very few quantitative studies have actually addressed this subject. Furthermore, all of the published studies have focused on coaching to improve surgeons’ technical or nontechnical skills in the operating room. Overall, the level of evidence from these nonrandomized studies is suboptimal with limited samples of coachees. Although the studies reported that surgeons generally considered coaching to be beneficial, their findings also showed that coaching had contrasting effects on surgeons’ skills and demonstrated no significant impact on patient outcomes. In contrast, the coaching strategies of the two registered randomized trials that were identified diverge from the previously published studies by employing professional coaches to help surgeons achieve goals related to the surgeons’ wellbeing and physiological factors.
The inconsistency in how coaching is defined in the literature represents a barrier that could prevent surgical coaching from being effectively studied or adopted on a large scale.16,25 Indeed, our results demonstrated that the definitions used to describe surgical coaching varied between the studies. However, a comparison and synthesis of the different definitions revealed common themes, which we incorporated in the following working definition: surgical coaching is a nonhierarchical relationship between an individual coachee (surgeon) and a coach (trained or untrained surgeon, or nonsurgeon professional coach) that aims to refine the coachee’s skills (technical or nontechnical) and/or capacities (physical or mental) through individualized goal setting, objective feedback, and self-assessment, and ultimately empowers the surgeon to find strategies to achieve their personal objectives. This definition differentiates surgical coaching from mentoring, which is instructional and involves counseling and advising, generally by an expert.25 The definition also aligns surgical coaching with goal-oriented coaching, which is nondirective, solution-focused, and performance-driven.25
Coaching can be used to help an individual achieve personal and professional goals that can be related to both performance and overall wellbeing.26 Nevertheless, one of the primary findings of this scoping review was that all of the published studies’ coaching goals centered around improving technical and/or nontechnical skills. Three of the studies’ overall goals were specified by the study investigators, and included decreasing fistula incidence after cleft palate surgery, improving self-assessment skills, and improving surgeons’ team leadership skills.17,18,20 The three other studies followed the basic structure established by the WSCP framework, and allowed coachees to identify any coaching goal related to intraoperative performance. Interestingly, rather than focusing on technical and nontechnical skills, the goals of the ongoing registered trials are related to wellbeing, stress management, sleep, and physical activity.22,23 This may reflect an expanding recognition of the important role physician wellness plays in health-care system performance.27
Another common theme that emerged was that all of the coaches in the published studies were surgeons. However, there were differences in the coaches’ levels of expertise and training. Two of the studies used expert coaches, who were not only surgeons, but also had training and expertise in the skills they were coaching.17,18 Both of these studies showed positive outcomes. The four other studies paired coachees with other surgeons who provided feedback as peer coaches, either following a training course to teach them core coaching principles16,19,21 or not.20 The three studies in which surgeons attended training sessions showed mixed results,16,19,21 whereas the study that used untrained peer coaches did not show positive results.20 Although the evidence remains much too limited to draw any definitive conclusions, these results underscore that formal training could potentiate the benefits of peer coaching.
Peer coaching between two surgeons with similar skill levels adds the benefit of fostering trust, which can lead to mutually beneficial discussions.21 Nevertheless, several disadvantages of peer coaching have also been recognized. For example, social and cultural influences may prevent peers from critically evaluating a colleague’s performance.28 On the other hand, surgeon coaches may shift into a mentoring or teaching mindset, and offer advice or direction, which does not promote the coachees’ sense of autonomy.29 Furthermore, both surgeons must find the time in their demanding schedules to attend peer coaching sessions, making time constraints a potentially limiting factor.16
In contrast to the published studies, the two ongoing trials reported that they will use coaches who are not surgeons.21,23 This choice appears to be in accordance with the studies’ goals, which are not related to surgical skills. This approach could potentially help surgeons fit coaching into their busy schedules. A previous study showed that professional coaching could decrease burnout and improve quality of life among physicians.30 This study also highlighted that physicians may feel less concerned about confidentiality and more comfortable opening up to credentialed coaches than peer coaches, as they adhere to a professional code of ethics.30 Therefore, this type of coaching may be particularly suited for addressing burnout in surgeons as well as other personal goals.
Assessment and feedback data have been shown to be crucial to performance enhancement and CPD.31 However, physicians’ judgments about their performance are unreliable.31,32 Bull et al17 addressed this issue through coaching surgeons’ self-assessment skills. Another possible solution is to provide surgeons with external assessment data to guide their self-assessments. Coaching can help surgeons engage with objective assessment data and plan and implement their responses. These activities have been shown to optimize physicians’ reactions to assessment data.31 Although four studies used scales or performance metrics to assess coachees’ performance, none shared this assessment data with the coachees in addition to the coaching exchanges.17–19,21
Furthermore, evaluating change strategies and measuring outcomes are core components of CPD for physicians.31,33 Coaches observed coachees operations in five studies.16–19,21 The coachee’s performance was subsequently discussed during the coaching session. This provided the opportunity for the coaches and coachees to evaluate change strategies employed by the surgeons during their operations. However, none of the published studies, and only one registered trial, provided coachees with external assessment data that tracked their performance or patient outcomes, providing objective feedback during the coaching program.22
One common limitation of the published studies was a potential lack of generalizability either because the study had a small sample size, the study included coachees from only one surgical specialty, or the study was not multi-centric.17,18,20,21 An additional possible limitation is that the success of a coaching intervention can depend on the efficacy of the coach, the motivation of the coachee, and the quality of the coaching relationship.34,35 Future studies could address this by including metrics to assess coaching program implementation, and to confirm the coaches’ and coachees’ adhesion to the program, their motivation, and their feelings about the coaching relationship. Furthermore, none of the studies tested the effects of combining coaching with solutions to help coachees achieve their goals. Bundling coaching with replicable strategies, tools, or exercises, such as procedure-specific checklists, team training, simulation sessions, or wellness techniques, with proven benefits could improve the reproducibility, and possibly the efficacy, of coaching interventions.36–41
Due to the very limited number of studies identified, the variability of the study designs and outcomes, and the lack of control groups in half of the published studies, it is difficult to come to any definitive conclusions about the efficacy of coaching for professional surgeons at this time. However, the evidence from studies included in this review does corroborate the findings of qualitative studies showing that professional surgeons consider peer coaching for intraoperative skills to be beneficial. Future studies are needed to determine whether surgeons consider other styles of coaching or coaching interventions with goals unrelated to technical or nontechnical proficiency to be valuable. Mixed-methods study designs, as used in four of the studies included in this review, could be particularly useful for exploring these research questions.
The studies examining the impacts of coaching on surgeons’ technical and nontechnical skills reported conflicting results, and used suboptimal study designs.17–19,21 In addition, the two studies that measured the effects of surgical coaching on patient outcomes did not report positive results.20,21 Overall, additional adequately powered, multi-site, randomized trials are needed to determine whether coaching impacts professional surgeons’ performance and patient outcomes. Moreover, future studies could explore the impacts of combining different styles of coaching with assessment data for objective feedback and/or replicable solutions to help surgeons achieve their goals.
CONCLUSIONS
The small number of studies that quantitatively evaluated the effects of coaching for professional surgeons indicate that coaching is well accepted, but the effects of coaching on their technical and nontechnical skills have been inconsistent, and no studies conclusively demonstrate impacts on patient safety. The findings of this scoping review ultimately suggest a potential framework for subsequent studies on surgical coaching. Future coaching programs may consider the integration of objective metrics to provide feedback to individual surgeons as well as accurate program implementation assessment. Furthermore, evaluations of coaching programs should not only evaluate surgeons’ performance, but should also consider assessing patient outcomes and surgeons’ overall wellness, using appropriate randomized trial designs.
Supplementary Material
Footnotes
Published online 8 July 2022
This work was supported by European Research Council Starting Grant TopSurgeons (ERC-2018-STG 801660).
Disclosure: The authors declare that they have nothing to disclose.
S.C.S. and A.D. participated in the research design, performance of the research, data analysis, and writing of the article. S.M. participated in performance of the research and writing of the article. J.-C.L. and M.J.C. participated in writing the article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Rashid P. Surgical education and adult learning: integrating theory into practice. F1000Res. 2017;6:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pradarelli JC, Hu YY, Dimick JB, et al. The value of surgical coaching beyond training. Adv Surg. 2020;54:31–47. [DOI] [PubMed] [Google Scholar]
- 3.Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93:1571–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. [DOI] [PubMed] [Google Scholar]
- 5.Pradarelli JC, Yule S, Smink DS. Performance coaching for practicing surgeons enhancing clinical performance, well-being, and trainee experience. J Surg Educ. 2020;77:495–498. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg CC, Klingensmith ME. The continuum of coaching: opportunities for surgical improvement at all levels. Ann Surg. 2015;262:217–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Gabri D, McDow AD, Quamme SP, et al. Surgical coaching for advancement of global surgical skills and capacity: a systematic review. J Surg Res. 2020;246:499–505. [DOI] [PubMed] [Google Scholar]
- 8.Gagnon LH, Abbasi N. Systematic review of randomized controlled trials on the role of coaching in surgery to improve learner outcomes. Am J Surg. 2018;216:140–146. [DOI] [PubMed] [Google Scholar]
- 9.Min H, Morales DR, Orgill D, et al. Systematic review of coaching to enhance surgeons’ operative performance. Surgery. 2015;158:1168–1191. [DOI] [PubMed] [Google Scholar]
- 10.Valanci-Aroesty S, Alhassan N, Feldman LS, et al. Implementation and effectiveness of coaching for surgeons in practice - a mixed studies systematic review. J Surg Educ. 2020;77:837–853. [DOI] [PubMed] [Google Scholar]
- 11.Augestad KM, Butt K, Ignjatovic D, et al. Video-based coaching in surgical education: a systematic review and meta-analysis. Surg Endosc. 2020;34:521–535. [DOI] [PubMed] [Google Scholar]
- 12.Louridas M, Sachdeva AK, Yuen A, et al. Coaching in surgical education: a systematic review. Ann Surg. 2021;275:80–84. [DOI] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. [DOI] [PubMed] [Google Scholar]
- 14.Kirkpatrick DL. Techniques for evaluating training programs.Evaluating training programs. 1975:1-7. [Google Scholar]
- 15.Guyatt GH, Oxman AD, Vist GE, et al. ; GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenberg CC, Ghousseini HN, Pavuluri Quamme SR, et al. ; Wisconsin Surgical Coaching Program. A statewide surgical coaching program provides opportunity for continuous professional development. Ann Surg. 2018;267:868–873. [DOI] [PubMed] [Google Scholar]
- 17.Bull NB, Silverman CD, Bonrath EM. Targeted surgical coaching can improve operative self-assessment ability: a single-blinded nonrandomized trial. Surgery. 2020;167:308–313. [DOI] [PubMed] [Google Scholar]
- 18.Maynard MT, Mathieu JE, Rapp TL, et al. Team leader coaching intervention: an investigation of the impact on team processes and performance within a surgical context. J Appl Psychol. 2021;106:1080–1092. [DOI] [PubMed] [Google Scholar]
- 19.Pradarelli JC, Yule S, Lipsitz SR, et al. Surgical Coaching for Operative Performance Enhancement (SCOPE): skill ratings and impact on surgeons’ practice. Surg Endosc. 2021;35:3829–3839. [DOI] [PubMed] [Google Scholar]
- 20.Sitzman TJ, Tse RW, Allori AC, et al. Feasibility of surgeon-delivered audit and feedback incorporating peer surgical coaching to reduce fistula incidence following cleft palate repair: a pilot trial. Plast Reconstr Surg. 2020;146:144–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenberg CC, Byrnes ME, Engler TA, et al. Association of a statewide surgical coaching program with clinical outcomes and surgeon perceptions. Ann Surg. 2021;273:1034–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duclos A. Evaluation of coaching impact on surgical outcomes (TopSurgeons) NCT04532658. September 9, 2020. Available at: https://clinicaltrials.gov/ct2/show/NCT04532658.
- 23.Dyrbye LN. Effect of coaching on surgeon well-being, job satisfaction, & fulfillment NCT04235751. June 16, 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04235751?cond=%28Surgeon+OR+surgery%29+AND+coaching&draw=2&rank=3.
- 24.Greenberg CC, Ghousseini HN, Pavuluri Quamme SR, et al. Surgical coaching for individual performance improvement. Ann Surg. 2015;261:32–34. [DOI] [PubMed] [Google Scholar]
- 25.Ives Y. What is ‘Coaching’? An exploration of conflicting paradigms. Int J Evid Based Coach Mentor. 2008;6:100–113. [Google Scholar]
- 26.Grant AM. Solution-focused cognitive–behavioral coaching for sustainable high performance and circumventing stress, fatigue, and burnout. Consult Psychol J Pract Res. 2017;69:98–111. [Google Scholar]
- 27.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714–1721. [DOI] [PubMed] [Google Scholar]
- 28.Zahid A, Hong J, Young CJ. Coaching experts: applications to surgeons and continuing professional development. Surg Innov. 2018;25:77–80. [DOI] [PubMed] [Google Scholar]
- 29.Beasley HL, Ghousseini HN, Wiegmann DA, et al. Strategies for building peer surgical coaching relationships. JAMA Surg. 2017;152:e165540. [DOI] [PubMed] [Google Scholar]
- 30.Dyrbye LN, Shanafelt TD, Gill PR, et al. Effect of a professional coaching intervention on the well-being and distress of physicians: a pilot randomized clinical trial. JAMA Intern Med. 2019;179:1406–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sargeant J, Bruce D, Campbell CM. Practicing physicians’ needs for assessment and feedback as part of professional development. J Contin Educ Health Prof. 2013;33 Suppl 1:S54–S62. [DOI] [PubMed] [Google Scholar]
- 32.Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296:1094–1102. [DOI] [PubMed] [Google Scholar]
- 33.Reed VA, Schifferdecker KE, Turco MG. Motivating learning and assessing outcomes in continuing medical education using a personal learning plan. J Contin Educ Health Prof. 2012;32:287–294. [DOI] [PubMed] [Google Scholar]
- 34.Baron L, Morin L. The coach-coachee relationship in executive coaching: a field study. Hum Resour Dev Q. 2009;20:85–106. [Google Scholar]
- 35.Bozer G, Sarros JC, Santora JC. The role of coachee characteristics in executive coaching for effective sustainability. J Manag Dev. 2013;32:277–294. [Google Scholar]
- 36.Aggarwal R, Mytton OT, Derbrew M, et al. Training and simulation for patient safety. Qual Saf Health Care. 2010;19(Suppl 2):i34–i43. [DOI] [PubMed] [Google Scholar]
- 37.Catchpole KR, de Leval MR, McEwan A, et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth. 2007;17:470–478. [DOI] [PubMed] [Google Scholar]
- 38.Crossley J, Marriott J, Purdie H, et al. Prospective observational study to evaluate NOTSS (Non-Technical Skills for Surgeons) for assessing trainees’ non-technical performance in the operating theatre. Br J Surg. 2011;98:1010–1020. [DOI] [PubMed] [Google Scholar]
- 39.Rui M, Lee JE, Vauthey JN, et al. Enhancing surgical performance by adopting expert musicians’ practice and performance strategies. Surgery. 2018;163:894–900. [DOI] [PubMed] [Google Scholar]
- 40.Wetzel CM, George A, Hanna GB, et al. Stress management training for surgeons-a randomized, controlled, intervention study. Ann Surg. 2011;253:488–494. [DOI] [PubMed] [Google Scholar]
- 41.Walker IA, Reshamwalla S, Wilson IH. Surgical safety checklists: do they improve outcomes? Br J Anaesth. 2012;109:47–54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.