Abstract
Background
Baseline disparities in non-discretionary risk factors, i.e., those not readily altered, like family size and work environment, appear to underlie the disproportionate COVID-19 infection rates seen among Hispanic persons and, at surge onsets, Black persons. No study has systematically compared such risk factors by race/ethnicity among infected individuals.
Methods
Using a cross-sectional survey, we compared household, job, and socioeconomic characteristics among 260 Hispanic, non-Hispanic Black, and non-Hispanic White adults with confirmed or probable COVID-19 in New York from March to May 2020. We used logistic regression to identify independent relationships.
Results
In bivariate analysis, we found significant differences by race/ethnicity in the following: (1) rates of household crowding (p < 0.001), which were highest for Hispanic patients (45.1%) and lowest for White patients (0.9%); (2) rates of non-healthcare frontline work (p < 0.001), which were highest for Hispanic patients (71.0% of those employed) and lowest for White patients (31.4%); (3) rates of working close to people (p < 0.001), which were highest for Black patients (69.4%) and lowest for Hispanic patients (32.3%); and (4) rates of frontline healthcare work (p = 0.004), which were higher for Black (44.9%) and White (44.3%) patients than Hispanic patients (19.4%). Adjusting for covariates eliminated most differences but not that for household crowding.
Conclusions
Non-discretionary COVID-19 risk factors among patients in the initial surge differed substantially by race/ethnicity. Socioeconomic factors explained most differences, but household crowding was independently associated with Hispanic ethnicity. Our findings highlight the ongoing need for universal safeguards for US frontline workers, including mandated paid sick leave and expanded affordable housing options.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40615-022-01416-1.
Keywords: COVID-19, Disparities, Social determinants, Race, Ethnicity
There is extensive evidence that structural socioeconomic disparities underlie the disproportionate impact of COVID-19 on persons of color just as with H1N1 a decade earlier [1]. High case rates among Hispanic and, at surge onsets, Black persons [2] implicate household and job factors, specifically. Household size is correlated with COVID-19 infection rates [3] and is significantly larger, on average, for Hispanic than for White persons [4]. Black and Hispanic persons are overrepresented in the frontline (in-person) workforce [5], including some of the highest-risk areas, such as healthcare and food service [6]. Hispanic households are substantially more likely than White households to combine risk factors, e.g., crowding and the presence of an essential worker [7].
To date, no study has systematically compared such risk factors by race and ethnicity among individuals with COVID-19. It is therefore not known to what extent baseline differences diminish when each member of a sample under study represents a failure of social distancing and other safeguards, or whether sources of COVID-19 differ qualitatively by race/ethnicity. Podewils et al. [8], in Denver, compared a limited set of characteristics for Hispanic and non-Hispanic persons with and without COVID-19 and found larger households, more household sick contacts, and more essential work among infected Hispanic persons. In the present study, we gathered information about additional household and job-related exposure risks, demographics, and socioeconomic status from Hispanic, non-Hispanic Black, and non-Hispanic White patients with a history of known or probable COVID-19 (by laboratory or clinical criteria, respectively). Our objective was to identify sources of non-discretionary risk, i.e., those not readily altered, like family size and work environment, by race/ethnicity to aid targeted risk reduction efforts for future pandemics. Where possible, we compare rates of risk factors in our sample with those at the population level.
The study took place in the early spring of 2020 in Suffolk County, NY, USA, which, at the time, was among the top US counties for total COVID-19 caseload. By using data from the initial surge in an early epicenter of the pandemic, we minimize the effect of differential responses (e.g., vaccination rates) over time and draw attention instead to baseline vulnerabilities.
Methods
We surveyed adults with a history of confirmed or suspected COVID-19 about their risk factors for COVID-19 exposure at the time of illness. We conducted the survey by phone over 6 months, from June 1 to December 2, 2020. Subjects were patients treated during the initial surge of the pandemic at a large suburban teaching hospital located 60 miles from New York City in Suffolk County, NY, USA.
Sample
We performed an electronic data query of Hispanic, non-Hispanic Black (henceforth “Black”), and non-Hispanic White (henceforth “White”) patients age 18 and over seen in the medical (non-psychiatric) emergency department between March 15 and May 9, 2020, who were assigned any of the four COVID-19-related ICD-10 diagnosis codes (U07.1, U07.2, B97.29, Z20.828) or two viral pneumonia codes (J12.89 or J12.9) then in common use for confirmed, suspected, or possible COVID-19 infection. Demographic data in the electronic record were obtained by Patient Registration at the time of hospital intake. We performed electronic chart reviews on a random subset, balanced across race/ethnicity and study week where possible, to determine eligibility and obtain contact information. Patients were eligible for inclusion if they had a positive COVID-19 polymerase chain reaction (PCR) test or antibody test or met specific clinical criteria (Online Resource 1) derived from the available evidence at the time. Clinical criteria were deemed necessary as testing was inconsistently available to emergency department patients during that time and because negative results were unreliable. Characteristics were similar for the 54 (20.8%) patients without test confirmation. There were only two differences: (1) fewer patients with test-confirmed COVID-19 reported household sick contacts, and (2) controlling for test confirmation increased the Hispanic-White disparity in household crowding. Patients were excluded if they lacked capacity to consent, lived in a group home or skilled nursing facility, or had an acute psychiatric illness. Additional exclusion criteria applied during telephone screening included physical or mental distress; patients without a positive COVID-19 test were also asked whether a different cause for their symptoms had been found after discharge and were excluded if they responded in the affirmative.
We derived our target sample size from Quinn et al.’s [1] H1N1 study. Based on the 23% and 50% lower social distancing ability they found for English-fluent and Spanish-preferring Hispanic survey respondents, respectively, compared with White respondents, we aimed to enroll 120 patients in each group (assuming English-fluency in half of Hispanic respondents) for a power of 0.8 to detect Hispanic-White differences with a 95% confidence level. Electronic data query identified 3653 potential patients; 847 (40 per group per week where possible) were randomly selected for chart review. Of 603 meeting eligibility requirements, we enrolled 244 (40%) (see Online Resource 2 for inclusions and exclusions). In response to the lower-than-anticipated enrollment, which overwhelmingly reflected failure to contact, we randomly screened an additional 146. The enrollment rate for these was even lower, so we halted enrollment at 260 (overall response rate: 37%).
Survey Instrument and Measures
We adapted questions where possible from the 2019 American Community Survey [9] and from Quinn et al. [1] (with permission). Our questionnaire assessed demographics, spoken and written English understanding, socioeconomic status, household characteristics, and job characteristics. Where race/ethnicity differed between electronic registration data and survey response, we used the latter; this occurred twice. Household factors included dwelling type, number of rooms (including kitchen but excluding bathrooms), number of people, presence of children, and presence of household sick contacts. Crowding was defined as more people than rooms in a household.
Job factors were collected from patients who reported an employment status at the time of illness of “Employed full-time,” “Employed part-time,” or “Self-employed.” These characteristics included occupation, whether frontline (“Could your type of work be done from home if your employer allowed it?”), availability of sick leave (“At the time you got sick, did you have sick leave at your job?”), whether the temporary inability to work risked job loss (“Could you lose your job or business if you were temporarily unable to go to work?”), access to personal protective equipment (PPE) (“At the time you got sick, was your job providing personal protective equipment (PPE) like face masks against Coronavirus?”), and form of commute (“Prior to getting sick, how did you usually get to work each day?”); occupation was categorized by whether it was essential (per New York State Executive Order No. 202.6, March 2020), required close proximity to people (high “contact-intensity” [10]), or was in healthcare. Three subcategories of frontline workers were analyzed separately: frontline healthcare worker, frontline non-healthcare worker, and frontline essential worker (this subcategory consisted of both healthcare workers and non-healthcare workers).
The questionnaire comprised 39 closed-ended and 12 open-ended questions in 5 sections, was available in English and Spanish, and took 10–15 min to complete. After pilot testing with ten patients, we adjusted question order and wording, based on feedback. Hispanic patients were asked about spoken English comprehension after 35 had already been enrolled.
After an introductory letter to eligible patients, members of the research team, using a script, conducted recruitment, screening, consenting procedures, and questionnaire administration by phone, generally in one or two contacts. No incentives were offered. Study data were collected and managed using REDCap, an electronic data capture tool. The study was approved by Stony Brook University’s Institutional Review Board.
Statistical Analyses
We analyzed the data with Stata version 11 (StataCorp LP, College Station, TX, USA). We used descriptive statistics to summarize the data overall and by race/ethnicity, chi-square and Fisher’s exact test to analyze differences by race/ethnicity for categorical variables, and ANOVA for continuous variables. We then used logistic regression to further analyze the relationship between race/ethnicity and household and job-related COVID-19 risk factors: we report an unadjusted model and, using purposeful selection, a model adjusting for age, sex, eligibility of a child in the household for free school lunch (as a proxy for poverty), highest education level attained, whether the patient was an immigrant, written English ability, health insurance type, and dwelling type. Additional patient characteristics which were considered but ultimately omitted from the model include employment status (which could not be included when the dependent variable was work-related and had no significant effect on the relationship of race/ethnicity to household factors), annual household income (an income range and therefore not meaningfully interpretable given variable household size), and presence or absence of children (collinear with our choice of poverty measure); sex, health insurance type, English ability, and dwelling type did not appreciably alter the relationship between race/ethnicity and the dependent variable of interest (COVID-19 risk factor) when included in the multivariable analysis. Missing data were rare (0–2%) except for household income (17%) and spoken English ability (14%), which we omitted from the main analysis.
Results
Demographic and Socioeconomic Characteristics
A total of 260 patients (92 Hispanic, 65 Black, and 103 White) completed the survey. There were marked demographic and socioeconomic differences by race/ethnicity (p < 0.05) in all characteristics examined except sex (Table 1). Compared with other patients, Hispanic patients were younger and were more likely to have an annual household income below $50,000, to be unemployed, to lack a high school degree, to be uninsured, and, among those with children, to have a child eligible for free school lunch. Compared with White patients, Hispanic patients lived in fewer rooms, had larger households, and were more likely to live with children. Black patients fell between Hispanic and White patients on most measures. Most Hispanic patients and over a third of Black patients were foreign-born, the former most often from El Salvador or Ecuador and the latter from the Caribbean. Nearly half of Hispanic patients had a limited understanding of written English.
Table 1.
Demographic and socioeconomic characteristics by race/ethnicity of Patients in Suffolk County, NY, USA, with probable COVID-19 infection: March–May 2020
| Characteristic | All (n = 260) | Hispanic (n = 92) | Non-Hispanic Black (n = 65) | Non-Hispanic White (n = 103) | p-value |
|---|---|---|---|---|---|
| Agea | 49.6 (15.2) | 45.7 (14.2) | 51 (15.2) | 52.2 (15.4) | 0.007 |
| Sex (male) | 140 (53.9) | 52 (56.5) | 30 (46.2) | 58 (56.3) | 0.36 |
| Non-US-bornb | 102 (39.4) | 75 (82.4) | 23 (35.4) | 4 (3.9) | < 0.001 |
| ≤ 15 years in the USAb | 24 (9.3) | 23 (25.3) | 1 (1.5) | 0 (0.0) | < 0.001 |
| Limited English (written) | 47 (18.1) | 45 (48.9) | 1 (1.5) | 1 (1.0) | < 0.001 |
| Education (highest degree)c | |||||
| Associate’s, bachelor’s, or higher | 94 (36.4) | 19 (20.9) | 24 (37.0) | 51 (50.0) | < 0.001 |
| High school or GED | 116 (45.0) | 30 (33.0) | 38 (58.5) | 48 (47.1) | |
| No high school degree | 48 (18.6) | 42 (46.2) | 3 (4.6) | 3 (2.9) | |
| Annual household incomed | |||||
| < $50,000 | 78 (35.9) | 48 (65.8) | 14 (23.7) | 16 (18.8) | < 0.001 |
| $50–100 | 66 (30.4) | 15 (16.3) | 23 (35.4) | 28 (27.2) | |
| > $100,000 | 73 (33.6) | 10 (10.9) | 22 (33.9) | 41 (39.8) | |
| Child eligible for free school lunche | 54 (44.3) | 31 (57.4) | 17 (46.0) | 6 (19.4) | 0.003 |
| Health insurance | |||||
| Private | 154 (59.2) | 42 (45.7) | 36 (55.4) | 76 (73.8) | < 0.001 |
| Medicare | 49 (18.8) | 11 (12.0) | 15 (23.1) | 23 (22.3) | |
| Medicaid | 43 (16.5) | 20 (21.7) | 16 (24.6) | 7 (6.8) | |
| None | 24 (9.2) | 19 (20.7) | 3 (4.6) | 2 (1.9) | |
| Employment status | |||||
| Employed | 184 (70.8) | 65 (70.7) | 49 (75.4) | 70 (68.0) | 0.007 |
| Unemployed | 31 (11.9) | 18 (19.6) | 4 (6.2) | 9 (8.8) | |
| Retired | 36 (13.8) | 5 (5.4) | 11 (16.9) | 20 (19.4) | |
| Dwelling type | |||||
| House | 204 (78.5) | 64 (69.6) | 54 (83.1) | 86 (83.5) | 0.04 |
| Apartment | 38 (14.6) | 16 (17.4) | 9 (13.9) | 13 (12.6) | |
| Room | 17 (6.5) | 12 (13.0) | 2 (3.1) | 3 (2.9) | |
| Household | |||||
| Number of roomsa,b | 5.7 (2.5) | 4.6 (2.1) | 5.9 (2.6) | 6.4 (2.5) | < 0.001 |
| Number of peoplea,b | 3.8 (2.2) | 4.6 (2.5) | 3.8 (1.8) | 3.1 (1.6) | < 0.001 |
| Any children in household | 124 (47.7) | 54 (58.7) | 38 (58.4) | 32 (31.1) | < 0.001 |
Data are given as frequency (percentage) and percentages are based on sample sizes listed, unless otherwise specified
aData are given as mean (standard deviation)
bN = 259 (91 Hispanic, 65 Black, and 103 White patients)
cN = 258 (91 Hispanic, 65 Black, and 102 White patients)
dN = 217 (73 Hispanic, 59 Black, and 85 White patients); 43 (16.5%) patients declined to answer question
eN = 122 (54 Hispanic, 37 Black, and 31 White patients) out of 124 patients with children
Risk Factors for COVID-19 Exposure
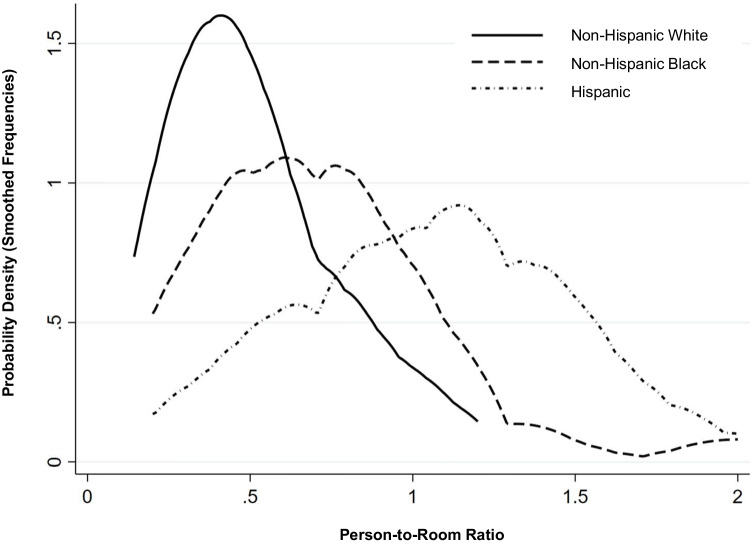
As seen in Table 2, there were high levels of non-discretionary risk factors for COVID-19 in all groups and significant differences by race/ethnicity. Nearly half of Hispanic patients, and far fewer Black and White patients, lived in crowded households (p < 0.001); the 2019 county rate for crowding among Hispanic persons, by comparison, was 7.3% [11]. Among childless households, crowding rates remained higher for Hispanic patients (p < 0.001). Figure 1, using smoothed frequency data as an alternative to overlapping histograms, shows the marked differences in the distribution of person-to-room ratios by race/ethnicity, particularly that between Hispanic patients and non-Hispanic White patients. Differences are seen with respect to both central tendency and total range: crowding or near-crowding held for a wide range of values in the Hispanic sample, as compared with relative concentrated person-to-room ratios centered just under 0.5 for White patients.
Table 2.
Prevalence of Non-Discretionary Risk Factors for COVID-19 Exposure, by Race/Ethnicity, Among Patients in Suffolk County, NY, With Probable COVID-19 Infection: March–May 2020
| Risk factor | Total | Hispanic | Non-Hispanic Black | Non-Hispanic White | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| na | No. (%) | n | No. (%) | n | No. (%) | n | No. (%) | ||
| Household crowding | 258 | 49 (19.0) | 91 | 41(45.1) | 65 | 7 (10.8) | 102 | 1 (0.9) | < 0.001 |
| Household crowding, no children | 134 | 11 (8.2) | 37 | 9 (24.3) | 27 | 2 (7.4) | 70 | 0 | < 0.001 |
| Household sick contact | 258 | 73 (28.3) | 90 | 34 (37.8) | 65 | 12 (18.5) | 103 | 27 (26.2) | 0.03 |
| Frontline worker | 181 | 150 (82.9) | 62 | 56 (90.3) | 49 | 41 (83.7) | 70 | 53 (75.7) | 0.08 |
| Frontline healthcare worker | 181 | 65 (35.9) | 62 | 12 (19.4) | 49 | 22 (44.9) | 70 | 31 (44.3) | 0.004 |
| Frontline non-healthcare worker | 181 | 85 (47.0) | 62 | 44 (71.0) | 49 | 19 (38.8) | 70 | 22 (31.4) | < 0.001 |
| Frontline essential worker | 181 | 132 (72.9) | 62 | 50 (80.7) | 49 | 35 (71.4) | 70 | 47 (67.1) | 0.21 |
| Works in close proximity to people | 180 | 91 (50.6) | 62 | 20 (32.3) | 49 | 34 (69.4) | 69 | 37 (53.6) | < 0.001 |
| No sick leave | 164b | 44 (26.8) | 52 | 19 (36.5) | 47 | 12 (25.5) | 65 | 13 (20.0) | 0.13 |
| Fears job loss if misses work | 175 | 43 (24.6) | 61 | 21 (34.4) | 47 | 11 (23.4) | 67 | 11 (16.4) | 0.06 |
| Little/no protective equipment (PPE) | 172 | 73 (42.4) | 60 | 26 (43.3) | 46 | 23 (50.0) | 66 | 24 (36.4) | 0.35 |
| Public/shared transportation | 181 | 18 (10.0) | 64 | 8 (12.6) | 48 | 6 (12.5) | 69 | 4 (5.7) | 0.36 |
aSample size varies by subpopulation under study: all patients (260), patients with childless households (136), working patients (184), or non-self-employed working patients (173). Additionally, three Hispanic patients provided incomplete job information, and one Hispanic and one White person did not provide household size. bEight patients responded “N/A” (not applicable) to this question
Fig. 1.
Kernel density estimates of person-to-room ratio—in effect, smoothed frequency data—scaled to an area under the curve equal to one. Title: Distribution of Household Person-to-room Ratios, by Race/Ethnicity, Among Patients in Suffolk County, NY, with Probable COVID-19 Infection: March-May 2020
In data not shown, household crowding was strongly associated with being an immigrant and, among immigrants, with being from Latin America (OR 6.40, 95% CI 3.19–12.86 and 19.89, 95% CI 2.54–155.66, respectively). Among Hispanic patients, the crowding rate was 48.7% for immigrants, and 31.3% for US-born patients, a non-significant difference, and no significant difference in crowding by birth country was found among the former (note: a majority of birth countries in Latin America were represented by fewer than 5 patients). However, the crowding rate of 85.7% for the seven patients born in Mexico was significantly higher than the rate of 44.8% for patients from other Latin American countries combined (p = 0.04).
As seen in Table 2, the likelihood of patients reporting having noted a sick contact at home when they became ill also varied significantly by race/ethnicity (p = 0.03): the highest rate was that among Hispanic patients (37.8%), and the lowest that among Black patients (18.5%).
A large majority of employed patients in each group had frontline jobs, with over two-thirds in each performing frontline essential work. Rates for both far exceeded recently published Figs. [12, 13]. A majority of Black and White patients and fewer Hispanic patients had jobs involving close physical proximity to others (p < 0.001); all rates exceeded a recent national rate of 21.6% [3]. Frontline healthcare work comprised over 40% of jobs for both Black and White patients and 19.4% for Hispanic patients; recent national [14] and local [15] population rates ranged from 10 to 16%. The next most common occupations for Hispanic patients were home, building, and landscaping services (19.4%) and food service (9.7%); for Black patients, law enforcement and corrections (14.3%); and for White patients, office work (11.4%). Rates of non-healthcare frontline work were high for Hispanic patients only (p < 0.001).
Job policy-related risk factors—inadequate PPE and lack of sick leave—were common in all groups. One in three healthcare workers lacked PPE. At least one in five patients in each group lacked access to sick leave, similar to the 2020 US Bureau of Labor Statistics rate [16]. Compared with White patients, Hispanic patients were more likely to lack sick leave and twice as likely to fear job loss for missing work (p < 0.05, not shown).
Table 3 shows the unadjusted and adjusted regression analyses for Hispanic and Black patients relative to White patients. The odds of household crowding were much greater for Hispanic patients than for White patients and remained significantly elevated in the adjusted model. In the unadjusted model, Hispanic patients were more likely than Black patients to have a household sick contact (OR 2.72, 95% CI 1.26–5.87, not shown). The odds of frontline work, lacking sick leave, and fearing job loss were higher for Hispanic patients than for White patients, and the odds of healthcare work lower; in the adjusted model these difference were no longer present but rates of inadequate PPE were higher for Black patients than for White patients.
Table 3.
Association of race/ethnicitya with non-discretionary risk factors for COVID-19 exposure among patients in Suffolk County, NY, USA, with probable COVID-19 infection March–May 2020
| Risk Factor | Unadjusted | Adjustedb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| nc | Hispanic | Non-Hispanic Black | nc | Hispanic | Non-Hispanic Black | |||||
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |||
| Household crowding | 258 | 82.82 (11.07–619.64) | < 0.001 | 12.19 (1.46–101.56) | 0.02 | 121 | 13.31 (1.12–158.42) | 0.04 | 1.77 (0.17–19.04) | 0.64 |
| Household sick contact | 258 | 1.71 (0.93–3.15) | 0.09 | 0.64 (0.30–1.37) | 0.25 | 120 | 0.31 (0.06–1.54) | 0.15 | 0.17 (0.04–0.63) | 0.008 |
| Frontline worker | 181 | 2.99 (1.10–8.17) | 0.03 | 1.64 (0.65–4.18) | 0.30 | 94 | 0.57 (0.07–4.65) | 0.60 | 0.69 (0.12–3.91) | 0.68 |
| Frontline healthcare worker | 181 | 0.30 (0.14–0.66) | 0.003 | 1.03 (0.49–2.14) | 0.95 | 94 | 0.36 (0.07–1.80) | 0.21 | 0.38 (0.10–1.49) | 0.16 |
| Frontline non-healthcare worker | 181 | 5.33 (2.53–11.23) | < 0.001 | 1.38 (0.64–2.97) | 0.41 | 94 | 1.92 (0.33–11.32) | 0.47 | 2.52 (0.51–12.43) | 0.28 |
| Frontline essential worker | 181 | 2.04 (0.91–4.55) | 0.08 | 1.22 (0.55–2.71) | 0.62 | 94 | 1.07 (0.20–5.83) | 0.94 | 0.65 (0.17–2.48) | 0.53 |
| Works in close proximity to people | 180 | 0.41 (0.20–0.84) | 0.02 | 1.96 (0.91–4.23) | 0.09 | 94 | 0.15 (0.02–0.98 | 0.05 | 2.20 (0.53–9.04) | 0.28 |
| No sick leave | 164 | 2.30 (1.00–5.28) | 0.05 | 1.37 (0.56–3.35) | 0.49 | 86 | 0.38 (0.04–3.16) | 0.37 | 0.77 (0.16–3.68) | 0.74 |
| Fears job loss if misses work | 175 | 2.67 (1.16–6.16) | 0.02 | 1.56 (0.61–3.96) | 0.35 | 91 | 0.76 (0.06–10.07) | 0.83 | 1.44 (0.19–10.79) | 0.72 |
| Little/no protective equipment (PPE) | 172 | 1.34 (0.65–2.74) | 0.43 | 1.75 (0.81–3.76) | 0.15 | 89 | 1.42 (0.25–8.03) | 0.69 | 5.38 (1.21–24.02) | 0.03 |
CI = confidence interval
aReference group is non-Hispanic White
bModels are adjusted for age, sex, income (eligibility of child for free lunch), education, whether US-born, written English ability, health insurance type, and dwelling type. Health insurance type and dwelling type were omitted from adjusted model for frontline worker, and shared transportation was omitted altogether as a risk factor, as adjusted models could not be fit in these cases.
cSee Table 2 footnotes for explanation of sample size variability
Discussion
We found high levels of non-discretionary risk for COVID-19 across race/ethnicity among patients with suspected COVID-19 in the initial surge in New York, but risk sources differed substantially. Hispanic patients had high rates of household crowding and sick contacts, non-healthcare frontline work, and socioeconomic disadvantage, while non-Hispanic Black and White patients faced risk largely through high rates of healthcare work. Sizeable minorities in all groups lacked access to sick leave and adequate PPE, the latter problem disproportionately affecting Black patients, after adjustment. Our patient sample, limited to the three largest US racial and ethnic groups, allowed for a focused comparative analysis, in particular that of Hispanic and non-Hispanic White persons, with their strikingly different infection rates and socioeconomic status, on average; Black persons comprise another key comparison group, with a socioeconomic status tending closer to that of Hispanic persons yet lower COVID-19 infection rate. To our knowledge, this is the first study to identify and compare non-discretionary risk factors for COVID-19 at home and at work among infected patients in these three groups.
Household Factors
The concentration of multiple high-risk characteristics in our data compared with population levels is noteworthy. In particular, the striking excess of household crowding among Hispanic patients—at 45.1%, 50 times the rate for White patients and four times that for Black patients—and their high rate of known household sick contacts suggest a substantial role for household COVID-19 transmission in this group. This is consistent with Cerami et al.’s [17] finding of a 51% transmission rate within non-White households compared with 19% in White households.
Ethnic and racial disparities in household crowding rates are incompletely understood. Like others [18], we found crowding rates to be strongly correlated with immigration. Yet, in our data, much of the effect was attributable to confounding by ethnicity: among Hispanic patients, who accounted for more than 80 percent of the household crowding in our sample, the crowding rate for immigrants was not significantly higher than the rate for US-born patients of nearly one in three. The association with Hispanic ethnicity, moreover, persisted after controlling for socioeconomic factors, as seen elsewhere [18, 19]. Cultural influences on tolerance for crowding and weighing of associated trade-offs may play a role [18, 19]. For example, norms appear to vary by race/ethnicity regarding the obligation to provide co-residence assistance to older family members when needed [20]. Notably, immigrants from Mexico, which itself has considerable crowding [21], had the highest crowding rates in our study. Evans et al. [22] found that with increasing persons per room, perceived crowding increased more slowly for Mexican-Americans than for Black and White persons, although psychological distress levels rose as fast as for White persons.
The role of culture in household crowding among Hispanic persons, if there is one, remains uncertain. Regardless of the precise nature of such an effect, however, dealing with the US housing crisis is of paramount importance to reducing crowding and its central role in disease spread, among the wider set of hardships a lack of housing creates. Inadequate access to suitable housing is a multifactorial problem compounded by poverty, immigration, and racism. It stems from insufficient housing stock, restrictive zoning laws, and, in some places, racist practices among banks and realtors. Long Island, NY, USA, where our study took place, has some of the country’s most exclusionary zoning policies, adopted to prevent racial integration and now contributing to a severe shortage of affordable housing [23]. Affordable starter homes are in short supply and accessory dwelling units—backyard cottages, garages, basements, etc.—and multi-family housing, which, importantly, have the potential to satisfy cultural preferences by allowing extended family to stay close by without crowding, are widely prohibited by zoning laws. Nor is recent evidence of racism in housing practices difficult to find. A 2019 Newsday investigation captured evidence of Long Island realtors systematically steering non-White customers toward separate and unequal neighborhoods and imposing more stringent financial conditions on them [24]. At the national level, a recent report from the Consumer Financial Protection Bureau found evidence that 16 major mortgage lenders had preferentially marketed to majority-White neighborhoods and discouraged non-White applicants, in violation of the Fair Housing Act of 1968 [25].
In January 2022, Governor of New York Kathy Hochul introduced two statewide proposals aimed at boosting housing options, neither of which proved politically viable: one would have allowed accessory dwelling units on single-family lots while the other would have relaxed legislation limiting new multifamily buildings near commuter rail stations [26]. For immigrants, this setback will likely mean the ongoing practice of shared and multi-generational living arrangements within single-family dwellings and a continued reliance on social networks for housing advice, the latter effectively narrowing the range of housing options they are likely to consider and further crowding ethnic enclaves short on high-quality housing [27]. Of note, Black and Hispanic households are twice as likely as White households to rent rather than to buy [28]—unsurprisingly, given the myriad obstacles to purchasing a home—and renting is associated with greater crowding [18].
Job Factors
The existence in all patient groups of excess levels of frontline work, frontline essential work, and work involving close proximity to people suggests that at least initially, non-discretionary job factors were central to COVID-19 transmission regardless of race or ethnicity. In addition, the uniform predominance of healthcare work across socioeconomic strata supports the idea that early in the pandemic, before mechanisms of spread were well understood and PPE was widely available, healthcare work played an outsized role in disease spread. This is consistent with Do and Frank’s [29] finding of disproportionately high COVID-19 positivity rates among healthcare workers in 2020.
Robust protective measures have since proven capable of mitigating substantial levels of job-associated infection risk, even the uniquely high levels of exposure in healthcare work [30]. By 2021, remarkably, rates of recent COVID-19 infection among healthcare workers had dropped below those of non-frontline workers [29]. States gaining access to paid sick leave after the Families First Coronavirus Response Act (FFCRA) went into effect in April 2020 also saw their caseloads drop [31]. Other key job measures include personal distancing and physical barriers where possible, testing protocols, formal quarantine procedures, and vaccine mandates.
Yet, the implementation of such policies and measures rests largely on the conscientiousness and resources of employers and is far from assured. In our study, a significant minority in each group, including a third employed in healthcare, lacked adequate PPE, and a similar number lacked sick leave. Though the Occupational Safety and Health Administration introduced federal workplace safety guidelines targeting COVID-19 prevention as early as March 2020, these went largely unenforced [32]. Those employed “off the books” are particularly vulnerable, and undocumented people may be unaware that they are still protected by OSHA or may fear reprisals for reporting violations. Jelliffe et al. [33] found that fewer than half of employees were aware of the FFCRA sick leave provisions as of fall in 2020 and that the share without access to needed sick leave had tripled during the pandemic. Since FFCRA expired at the end of 2020, paid sick leave is no longer federally mandated, and only a third of states now require it; New York is among these but was not at the time of our study.
Inadequate workplace protections contribute not only to COVID-19 infection rates but also to racial disparities. Non-White workers disproportionately hold low-wage jobs [12], with lower occupational standing and less leverage with which to demand protections [34]. They have reported lower access to PPE [30], for example, as we found for Black patients, after adjusting for socioeconomic factors. Low-income, non-White, and immigrant workers also face heightened pressure to work while sick, absent paid sick leave, and access to paid sick leave was disproportionately low among Hispanic workers in our study and others [36]. Sources of pressure include the threat of eviction or home foreclosure, limited job security, and, for undocumented immigrants, citizenship requirements and the threat of deportation. Many undocumented immigrants were either ineligible for federal assistance or were discouraged from pursuing it by immigration-related concerns, stemming in no small part from the Public Charge rule [35]. Non-White persons in general bear a disproportionate share of exemptions to FFCRA benefits [37]. It is unsurprising, therefore, that Hispanic workers were more likely than White workers in our study to fear job loss if they missed work and, elsewhere, to report working while sick [8].
Study Limitations
The principal limitation of our study is the response rate, particularly that among Hispanic patients. Contact and enrollment failure are recognized problems in research on immigrants, especially undocumented immigrants [38], and on people of lower socioeconomic status [39]. Our study may as a result be underpowered to identify all differences of interest; some apparent racial/ethnic differences—in the use of public or shared transportation, for example—did not reach statistical significance. Our confidence intervals were also quite large in some cases as a result, particularly for household crowding, limiting conclusions as to the true magnitude of observed differences. Despite these setbacks, however, we were able to identify several key between-group differences, in household crowding in particular, supporting the conclusion that risk factors for COVID-19 do vary by race/ethnicity among infected patients.
There is potential for recall bias in our study, as surveys were performed months after an illness in some cases. We anticipated that recall bias would be low for fixed structural factors at home or at work, as for demographic and socioeconomic factors, although certain characteristics may have changed over time within the study period, e.g., access to personal protective equipment and even household composition. We believe, however, that many or most patients are likely to have paid close attention to such details in the early months of the pandemic as they assessed their personal risk, particularly on becoming ill. Also, any recall bias present would be unlikely to have differed systematically among the groups being compared.
Among several additional limitations, our study looked only at patients we believed or knew had COVID-19, allowing direct comparison of risk factors but not correlation of these with infection rates, which has been done extensively elsewhere. Because the study took place early in the pandemic, a confirmatory COVID-19 test was inconsistently available, the accuracy of a negative test was uncertain, and a validated clinical algorithm was not available. However, the algorithm we designed was based on published data and was designed conservatively to minimize false positives. Also, the brief duration of the initial surge meant working quickly and including some survey questions not previously validated. Finally, there was a widespread lack of COVID-19 preparedness and access to consistent safety guidelines at the time, with the possible effect of reducing between-group differences.
Conclusions
We found high levels of non-discretionary risk for COVID-19 among patients with suspected COVID-19 in the initial surge, and several marked differences by race/ethnicity. Key differences included very high levels of crowding among Hispanic patients not entirely attributable to measured socioeconomic factors and overrepresentation of healthcare work among non-Hispanic White and Black patients. Our findings highlight multiple unmet needs. Protecting healthcare workers and other frontline workers from disease transmission on the job requires universal, comprehensive, and enforced workplace safeguards, along with mandated paid sick leave. These would indirectly protect households as well. However, we found at a local level that Hispanic persons and particularly immigrants face wide-ranging sources of risk for disease transmission, to a large extent reflecting socioeconomic disadvantage but likely also cultural to an extent, with respect to household crowding. Eliminating disparities in infection rates by race/ethnicity, socio-economic status, and for immigrants would additionally entail expanding housing stock; ending overly restrictive zoning laws, aggressively targeting discriminatory mortgage lending, and residential realtor practices; ensuring timely rent relief during a pandemic; and extending basic federal non-cash benefits to all in need, including non-citizens, with explicit assurances against deportation or ineligibility for citizenship as a consequence. Without substantial progress on disparities in structural risk factors, the next pandemic can be expected to deliver disparate outcomes once again.
Supplementary Information
Below is the link to the electronic supplementary material.
Author Contribution
Erika Newton, Rolando Valenzuela, Priscilla Cruz-Menoyo, Kimberly Feliberti, and Timothy Shub designed the study. All authors except Héctor Alcalá collected data. Erika Newton, Christina Melian, and Héctor Alcalá analyzed the data. The first draft of the manuscript was written by Erika Newton, and all of the authors critically reviewed the manuscript and approved the final version.
Declarations
Ethics Approval
The study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by Stony Brook University’s Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
Conflict Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Quinn SC, Kumar S, Freimuth VS, Musa D, Casteneda-Angarita N, Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health. 2011;101(2):285–293. doi: 10.2105/AJPH.2009.188029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hill L, Artiga S. COVID-19 cases and deaths by race/ethnicity: current data and changes over time. In: Coronavirus (COVID-19). Kaiser Family Foundation; 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/. Accessed 31 Aug 2022.
- 3.Federgruen A, Naha S. Crowding effects dominate demographic attributes in COVID-19 cases. Int J Infect Dis. 2021;102:509–516. doi: 10.1016/j.ijid.2020.10.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Census Bureau. America’s Families and Living Arrangements: 2020, Table AVG1. 2020. Washington, D.C. https://www.census.gov/data/tables/2020/demo/families/cps-2020.html. Accessed 31 Mar 2022.
- 5.Arasteh K. Prevalence of comorbidities and risks associated with COVID-19 among Black and Hispanic populations in New York City: an examination of the 2018 New York City Community Health Survey. J Racial Ethn Health Disparities. 2021;8(4):863–869. doi: 10.1007/s40615-020-00844-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Selden TM, Berdahl TA. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff (Millwood) 2020;39(9):1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- 7.Reitsma MB, Claypool AL, Vargo J, et al. Racial/ethnic disparities in COVID-19 exposure risk, testing, and cases at the subcounty level in California. Health Aff (Millwood) 2021;40(6):870–878. doi: 10.1377/hlthaff.2021.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Podewils LJ, Burket TL, Mettenbrink C, et al. Disproportionate incidence of COVID-19 infection, hospitalizations, and deaths among persons identifying as Hispanic or Latino — Denver, Colorado March–October 2020. Morb Mortal Wkly Rep. 2020;69(48):1812–1816. doi: 10.15585/mmwr.mm6948a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Census Bureau. 2019 American Community Survey questionnaire. Washington, DC; 2019 https://www2.census.gov/programs-surveys/acs/methodology/questionnaires/2019/quest19.pdf. Accessed 21 Mar 2022.
- 10.Leibovici F, Santacreu AM, Famiglietti M. Social distancing and contact-intensive occupations. In: On the Economy Blog. Federal Reserve Bank of St. Louis; 2020. https://www.stlouisfed.org/on-the-economy/2020/march/social-distancing-contact-intensive-occupations. Accessed 30 Mar 2022.
- 11.US Census Bureau. 2019 American Community Survey. 1-Year Estimates Detailed Tables, Table B250141. Washington, DC; 2019. https://data.census.gov/cedsci/table?q=United%20States&t=Hispanic%20or%20Latino%3AOccupants%20Per%20Room&g=0500000US36103&tid=ACSDT1Y2019.B25014I. Accessed 20 Mar 2022.
- 12.Goldman N, Pebley AR, Lee K, Andrasfay T, Pratt B. Racial and ethnic differentials in COVID-19-related job exposures by occupational standing in the US. PLoS ONE. 2021;16(9):e0256085. doi: 10.1371/journal.pone.0256085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubay L, Aarons J, Brown KS, Kenney GM. How risk of exposure to the coronavirus at work varies by race and ethnicity and how to protect the health and well-being of workers and their families. Urban Institute; 2020. https://www.urban.org/sites/default/files/publication/103278/how-risk-of-exposure-to-the-coronavirus-at-work-varies_1.pdf. Accessed 20 Mar 2022.
- 14.US Census Bureau. 2019 American Community Survey. 1-Year Estimates Detailed Tables, Table B24010I. Washington, DC; 2019. https://data.census.gov/cedsci/table?q=United%20States&t=Hispanic%20or%20Latino%3AOccupation&tid=ACSDT1Y2019.B24010I. Accessed 19 Mar 2022.
- 15.Long Island region economic snapshot. Office of the New York State Comptroller; 2019. https://www.osc.state.ny.us/files/local-government/publications/pdf/long-island-region.pdf. Accessed 19 Mar 2022.
- 16.U.S. Bureau of Labor Statistics. Paid sick leave benefits factsheet. 2020. https://www.bls.gov/ncs/ebs/factsheet/paid-sick-leave.htm. Accessed 20 Mar 2022.
- 17.Cerami C, Popkin-Hall ZR, Rapp T, et al. Household transmission of severe acute respiratory syndrome Coronavirus 2 in the United States: Living Density, Viral Load, and Disproportionate Impact on Communities of Color. Clin Infect Dis. 2022;74(10):1776–1785. doi: 10.1093/cid/ciab701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myers D, Baer WC, Choi SY. The changing problem of overcrowded housing. J Am Plann Assoc. 1996;62(1):66–84. doi: 10.1080/01944369608975671. [DOI] [Google Scholar]
- 19.Burr JA, Mutchler JE, Gerst K. Patterns of residential crowding among Hispanics in later life: immigration, assimilation, and housing market factors. J Gerontol Ser B. 2010;65B(6):772–782. doi: 10.1093/geronb/gbq069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burr JA, Mutchler JE. Race and ethnic variation in norms of filial responsibility among older persons. J Marriage Fam. 1999;61(3):674–687. doi: 10.2307/353569. [DOI] [Google Scholar]
- 21.OECD. Housing overcrowding. In: OECD Data. 2022. http://data.oecd.org/inequality/housing-overcrowding.htm. 10.1787/96953cb4-en. Accessed 19 Mar 2022.
- 22.Evans GW, Lepore SJ, Allen KM. Cross-cultural differences in tolerance for crowding: fact or fiction? J Pers Soc Psychol. 2000;79(2):204–210. doi: 10.1037/0022-3514.79.2.204. [DOI] [PubMed] [Google Scholar]
- 23.Kazis N. Ending exclusionary zoning in New York City’s suburbs. NYU Furman Center; 2020. https://furmancenter.org/research/publication/ending-exclusionary-zoning-in-new-york-city8217s-suburbs. Accessed 19 Mar 2022.
- 24.Choi A, Herbert K, Winslow O, Browne A. Undercover investigation reveals evidence of unequal treatment by real estate agents. Newsday. 2019. https://projects.newsday.com/long-island/real-estate-agents-investigation/. Accessed 7 June 2022.
- 25.Consumer Financial Protection Bureau. Supervisory Highlights, Issue 24, Summer 2021. https://www.consumerfinance.gov/data-research/research-reports/supervisory-highlights-issue-24-summer-2021/. Accessed 19 Mar 2022.
- 26.Chadha J, Garcia D. Hochul drops controversial proposals to boost housing. Politico; 2022. https://politi.co/36qDzQl. Accessed 6 Sep 2022.
- 27.Carrillo L, Pattillo M, Hardy E, Acevedo-Garcia D. Housing decisions among low-income Hispanic households in Chicago. Cityscape J Policy Dev Res. 2016;18(2):109–150. [Google Scholar]
- 28.Desilver D. As national eviction ban expires, a look at who rents and who owns in the U.S. Pew Research Center. 2021. https://www.pewresearch.org/fact-tank/2021/08/02/as-national-eviction-ban-expires-a-look-at-who-rents-and-who-owns-in-the-u-s/. Accessed 30 Mar 2022.
- 29.Do DP, Frank R. U.S. frontline workers and COVID-19 inequities. Prev Med. 2021;153:106833. 10.1016/j.ypmed.2021.106833 [DOI] [PMC free article] [PubMed]
- 30.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pichler S, Wen K, Ziebarth NR. COVID-19 emergency sick leave has helped flatten the curve in the United States. Health Aff (Millwood) 2020;39(12):2197–2204. doi: 10.1377/hlthaff.2020.00863. [DOI] [PubMed] [Google Scholar]
- 32.Do DP, Frank R. Using race- and age-specific COVID-19 case data to investigate the determinants of the excess COVID-19 mortality burden among Hispanic Americans. Demogr Res. 2021;44:699–718. doi: 10.4054/DemRes.2021.44.29. [DOI] [Google Scholar]
- 33.Jelliffe E, Pangburn P, Pichler S, Ziebarth NR. Awareness and use of (emergency) sick leave: US employees’ unaddressed sick leave needs in a global pandemic. Proc Natl Acad Sci. 2021;118(29):e2107670118. doi: 10.1073/pnas.2107670118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gaitens J, Condon M, Fernandes E, McDiarmid M. COVID-19 and essential workers: a narrative review of health outcomes and moral injury. Int J Environ Res Public Health. 2021;18(4):1446. doi: 10.3390/ijerph18041446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Touw S, McCormack G, Himmelstein DU, Woolhandler S, Zallman L. Immigrant Essential Workers Likely Avoided Medicaid And SNAP Because Of A Change To The Public Charge Rule. Health Aff (Millwood) 2021;40(7):1090–1098. doi: 10.1377/hlthaff.2021.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar S, Quinn SC, Kim KH, Daniel LH, Freimuth VS. The impact of workplace policies and other social factors on self-reported influenza-like illness incidence during the 2009 H1N1 pandemic. Am J Public Health. 2012;102(1):134–140. doi: 10.2105/AJPH.2011.300307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Long M. Gaps in the emergency paid sick leave law for health care workers. In: Coronavirus (COVID-19). Kaiser Family Foundation; 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/gaps-in-emergency-paid-sick-leave-law-for-health-care-workers/. Accessed 30 Mar 2022.
- 38.Olukotun O, Mkandawire-Valhmu L. Lessons learned from the recruitment of undocumented African immigrant women for a qualitative study. Int J Qual Methods. 2020;19:1–9. doi: 10.1177/1609406920904575. [DOI] [Google Scholar]
- 39.Martikainen P, Laaksonen M, Piha K, Lallukka T. Does survey non-response bias the association between occupational social class and health? Scand J Public Health. 2007;35(2):212–215. doi: 10.1080/14034940600996563. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.