Abstract
A patient with pneumonia had a fever for 2 weeks. After the initial anti-infection treatment failed, he was diagnosed with C. psittaci pneumonia complicated with organizing pneumonia, through next-generation sequencing (mNGS) of bronchoalveolar lavage fluid (BALF) and lung biopsy. He was treated with antibiotics and corticosteroids for 2 months.
Keywords: Chlamydia psittaci, Organizing pneumonia, Metagenomic next-generation sequencing, Lung biopsy, Treatment
Highlights
-
•
Chlamydia psittaci pneumonia complicated with organizing pneumonia is rare.
-
•
It can be diagnosed by next-generation sequencing (mNGS) of bronchoalveolar lavage fluid (BALF) and lung biopsy.
-
•
Treatment of moxifloxacin sequential to clarithromycin combined with corticosteroids is effective, and the prognosis is satisfactory.
-
•
We introduce a rare case of C. psittaci pneumonia complicated with organizing pneumonia, and the treatment is successful.
Introduction
C. psittaci pneumonia accounts for about 1 % of community-acquired pneumonia [1]. Exposure to birds or poultry is a major risk factor for C. psittaci pneumonia [2]. The clinical manifestations of C. psittaci pneumonia are atypical and can involve different organs or tissues [3], among which, the lung is the most frequently involved organ. Organizing pneumonia secondary to C. psittaci pneumonia is rare, and there are some difficulties in diagnosis and treatment. At present, pathologically confirmed cases of secondary organic pneumonia caused by C. psittaci have not yet been reported. Several cases of severe C. psittaci pneumonia suspected to be organic pneumonia have been reported previously, but they had not been confirmed histologically, and treatment was difficult.
We introduce a rare case of C. psittaci pneumonia complicated with organizing pneumonia. The patient received effective treatment and had good prognosis.
Case report
A 56-year-old man was admitted to our hospital on August 28, 2021 with a 2-week history of fever. Two weeks prior, the patient had developed a fever, with a temperature reaching 39 °C, accompanied by cold and chills. He received anti-infection treatment at a local hospital, but the fever persisted. He was then transferred to our hospital. The patient had no recent history of contact with poultry or birds. Physical examination upon admission revealed a body temperature of 37.7 °C, pulse rate of 84 bpm, blood pressure of 165/81 mmHg, respiratory rate of 45 bpm, and no rales in either lung. Laboratory examination indicated white blood cell (WBC) 7.39 × 10^9/L, neutrophil percentage 80.0 %, hemoglobin 130 g/L, platelet 243 × 10^9/L, C-reactive protein (CRP) 127.74 mg/L, erythrocyte sedimentation rate (ESR) 101 mm/h, neuron-specific enolase 24.15 ng/mL, and ferritin 812.28 ng/mL. There were no obvious abnormalities in blood culture, sputum culture, procalcitonin (PCT), liver and kidney function, coagulation function, IgM detection of respiratory pathogens, autoantibodies, electrocardiogram, and ultrasonic cardiogram. Abdominal ultrasonography showed a hypoechoic area in the liver, indicating a heterogeneous fatty liver. Chest computed tomography (CT) showed a patchy high-density shadow spread in the lower lobe of the left lung, as well as the presence of an air bronchogram sign (Fig. 1 A).
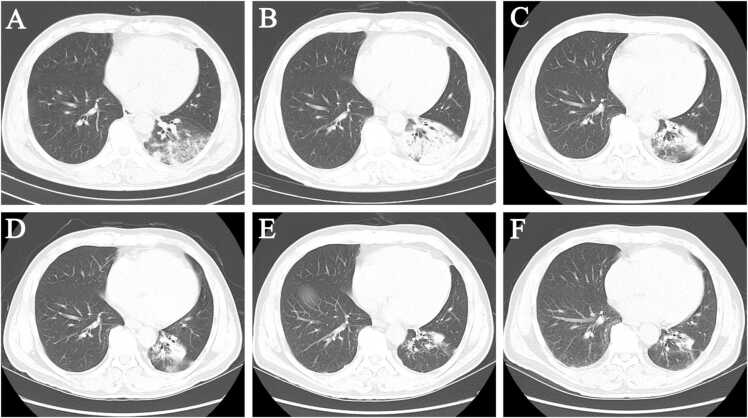
Fig. 1.
Chest computed tomography scan at admission (A), 12d later (B), 21d later (C), 33d later (D), 40d later (E), and 54d later (F).
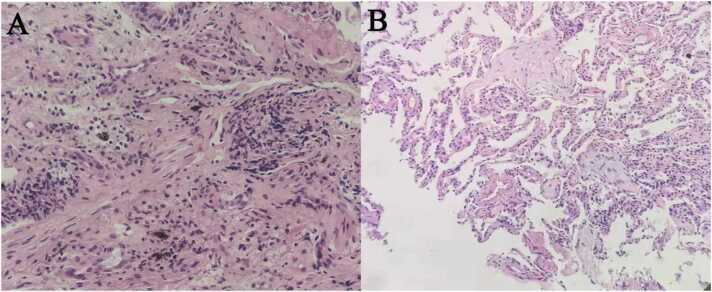
After admission, the patient was treated with intravenous piperacillin/tazobactam (4.5 g 8-hourly). However, his temperature remained constant. On day 3 of admission, he was switched to biapenem (0.3 g 6-hourly). At the same time, the patient was advised to undergo bronchoscopy, which showed no foreign bodies, neoplasms, caseous lesions, or bleeding. Radial ultrasound bronchoscopy (RP-EBUS) demonstrated a hypoechoic shadow in the left posterior basal segment, and a biopsy was performed. mNGS of BALF showed evidence of C. psittaci infection. On day 6 of admission, intravenous moxifloxacin (0.4 g daily) was administered. Re-examination showed the following: WBC, 4.87 × 10^9/L; CRP, 12.73 mg/L; and ESR, 66 mm/h. The patient had no fever, and was discharged after 4 days. After discharge, moxifloxacin (0.4 g daily) was administered orally. On day 4 after discharge, bronchoscopic lung biopsy revealed chronic inflammation of the respiratory tract mucosa with submucosal fibrovascular hyperplasia, and the surrounding lung tissue showed changes of organizing pneumonic (Fig. 2). Re-examination of chest CT indicated that the pneumonia had progressed to more severe disease (Fig. 1 B). The patient was diagnosed with C. psittaci pneumonia secondary to organizing pneumonia and was re-hospitalized. The patient was treated with intravenous moxifloxacin (0.4 g daily) and methylprednisolone (40 mg daily for 7 days, 20 mg daily for 7 days) for 2 weeks. Re-examination showed that CRP had returned to normal level, and he was discharged. After discharge, moxifloxacin (0.4 g daily) was administered orally for 1 week. Then, he was switched to clarithromycin (0.5 g daily) orally for another 1 month. Simultaneously, the patient continued oral methylprednisolone (16 mg for 2 weeks, then gradually reduced). The total course of moxifloxacin sequential clarithromycin and glucocorticoid therapy was 2 months, and the patient stopped taking the medication by himself. The white blood cell count and CRP levels were normal upon outpatient re-examination, and chest CT suggested gradual absorption of the lung lesions (Fig. 1 C–F). The patient was followed up for 6 months and reported no discomfort.
Fig. 2.
Pathologic examination showed (hematoxylin-eosin staining, A: x 400, B: x 100): chronic inflammation of the respiratory tract mucosa with submucosal fibrovascular hyperplasia, and the surrounding lung tissue showed changes of organizing pneumonic.
Discussion
C. psittaci pneumonia is a zoonosis caused by the spread of C. psittaci from birds to humans. Its symptoms include fever, headache, myalgia, dry cough, changes in consciousness, photophobia, hepatosplenomegaly, and pharyngitis [4]. Severe cases may include rhabdomyolysis [5], severe pneumonia [6]. In this case, the patient did not have other organ dysfunction, but did present with organizing pneumonia, which has been rarely reported.
The imaging manifestations of C. psittaci pneumonia are nonspecific and can be characterized by massive or bilateral pneumonia [7], consolidation with bronchial inflation signs, or a small amount of pleural effusion [8]. The patient presented with a patchy high-density shadow on one side with an inflatable bronchial sign, which was consistent with the above characteristics. C. psittaci is an intracellular Gram-negative bacterium that is difficult to culture. mNGS can be used as an early and effective method for diagnosing C. psittaci pneumonia [9]. The treatment of C. psittaci should include antibiotics with strong Gram-negative activity in cells, such as tetracycline, macrolides, and quinolones. In Chinese patients, the resistance rate to macrolides and tetracyclines has increased, and some reports have suggested that quinolones are effective [10]. In this report, the patient was diagnosed with C. psittaci pneumonia complicated with organizing pneumonia, and moxifloxacin and clarithromycin were used successively, with remarkable effects.
Organizing pneumonia secondary to C. psittaci pneumonia is a rare condition, and the time boundary between infection and organizing pneumonia is unclear. The diagnosis of organizing pneumonia mainly depends on pathological examination. Currently, the treatment mostly refers to glucocorticoid treatment of interstitial lung disease, which has a significant effect [11], but the reduction process is prone to relapse. It has been reported that macrolides can achieve good results in patients with mild organizing pneumonia [12]. In our case, the patient was ultimately switched to clarithromycin for 1 month. The total course of moxifloxacin sequential to clarithromycin and corticosteroids was 2 months, and the prognosis was good during follow-up.
Although there have been some reports of C. psittaci pneumonia and organizing pneumonia worldwide, to the best of our knowledge, few histologically confirmed cases of secondary organizing pneumonia caused by C. psittaci have been reported. Several cases of severe C. psittaci pneumonia suspected to organizing pneumonia have been reported previously [13], [14]. However, they had not been confirmed histologically.
In conclusion, we present a case of C. psittaci pneumonia complicated with organizing pneumonia. He was successfully treated with moxifloxacin sequential to clarithromycin combined with corticosteroids for 2 moths, and the prognosis was good.
CRediT authorship contribution statement
Yidan Gao designed the report and was responsible for writing articles; Ling Gong and Jing liu collected case materials and accessed to literature; Gongying Chen, and Xiangbo Zhang were responsible for analyzing and supplementing medical records; Xiang Zhou evaluated and reviewed articles. All authors read and approved the final version of the manuscript.
Ethical approval
We hereby confirm that we have read and complied with the policy on ethical consent.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of Competing Interest
We declare that we have no competing interest associated with this manuscript.
Acknowledgment
We would like to thank the patient who contribute to the progress of science. Furthermore, we would like to thank all our colleagues, who have also participated in the clinical management of this patient.
Contributor Information
Yidan Gao, Email: 1363352490@qq.com.
Xiangbo Zhang, Email: Xiangbo0426@163.com.
Jing Liu, Email: liujing07251@163.com.
Ling Gong, Email: linggong0426@163.com.
Gongying Chen, Email: gongyingc@163.com.
Xiang Zhou, Email: zhouxiang011923@163.com.
References
- 1.Gu L., Liu W., Ru M., et al. The application of metagenomic next-generation sequencing in diagnosing Chlamydia psittaci pneumonia: a report of five cases. BMC Pulm Med. 2020;20(1):1–7. doi: 10.1186/s12890-020-1098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hogerwerf L., Gier B D.E., et al. Chlamydia psittaci (psittacosis) as a cause of community-acquired pneumonia: a systematic review and meta-analysis. Epidemiol Infect. 2017;145(15):3096–3105. doi: 10.1017/S0950268817002060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hogerwerf L., Roof I., Jong M., et al. Animal sources for zoonotic transmission of psittacosis: a systematic review. BMC Infect Dis. 2020;20:192. doi: 10.1186/s12879-020-4918-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewardson A.J., Grayson M.L. Psittacosis. Infect Dis Clin N Am. 2010;24(1):7–25. doi: 10.1016/j.idc.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Zhang A.B., Xia X.Q., Yuan X.L., et al. Chlamydia psittaci severe pneumonia complicated by rhabdomyolysis: a case series. Infect Drug Resist. 2022;15:873–881. doi: 10.2147/IDR.S355024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu X.D., Li Y.Y., Zhang M., et al. Etiology of severe community-acquired pneumonia in adults based on metagenomic next-generation sequencing: a prospective multicenter study. Infect Dis Ther. 2020;9(4):1003–1015. doi: 10.1007/s40121-020-00353-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi Y.F., Chen J.X., Shi X.H., et al. A case of Chlamydia psittaci caused severe pneumonia and meningitis diagnosed by metagenome next-generation sequencing and clinical analysis: a case report and literature review. BMC Infect Dis. 2021;21(1):621. doi: 10.1186/s12879-021-06205-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Branley J.M., Weston K.M., England J., et al. Clinical features of endemic community-acquired psittacosis. New Microbes New Infect. 2014;2(1):7–12. doi: 10.1002/2052-2975.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang H., Zhan D., Chen D., et al. Next-generation sequencing diagnosis of severe pneumonia from fulminant psittacosis with multiple organ failure: a case report and literature review. Ann Transl Med. 2020;8(6):401. doi: 10.21037/atm.2020.03.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boeck C.D., Dehollogne C., Dumont A., et al. Managing a cluster outbreak of psittacosis in Belgium linked to a pet shop visit in The Netherlands. Epidemiol Infect. 2016;144(08):1710–1716. doi: 10.1017/S0950268815003106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cordier J.-F. Cryptogenic organising pneumonia. Eur Respir J. 2006;28(2):422–446. doi: 10.1183/09031936.06.00013505. [DOI] [PubMed] [Google Scholar]
- 12.Pathak V., Kuhn J.M., Durham C., et al. Macrolide use leads to clinical and radiological improvement in patients with cryptogenic organizing pneumonia. Ann Am Thorac Soc. 2014;11(1):87–91. doi: 10.1513/AnnalsATS.201308-261CR. [DOI] [PubMed] [Google Scholar]
- 13.Okubo T., Miyazaki E., Ueo M., et al. A case of psittacosis with wandering infiltrates developing to acute respiratory distress syndrome. Nihon Kokyuki Gakkai Zasshi. 2007;45(5):419–423. [PubMed] [Google Scholar]
- 14.Zuzek R., Green M., May S. Severe psittacosis progressing to suspected organizing pneumonia and the role of corticosteroids. Respir Med Case Rep. 2021;34 doi: 10.1016/j.rmcr.2021.101486. [DOI] [PMC free article] [PubMed] [Google Scholar]