Abstract
Introduction
The COVID-19 outbreak forced Italian citizens into a generalized quarantine from March to May 2020. The quarantine is a successful measure to reduce the virus's spread through physical and social distancing, but it can also have negative psychological consequences on the population. People experience high levels of worry and anxiety and have to cope with the consequences of the health emergency. The aim of this study was to preliminarily assess the causal relations among coping, worry and state anxiety at the time of COVID-19 first wave, and the mediation role of worry between coping and state anxiety.
Methods
During March 2020, 1273 Italian citizens completed an ad hoc online survey composed of sociodemographic and preoccupation-related questions, and standardized self-report questionnaire (Brief COPE, Penn State Worry Questionnaire and State-Trait Anxiety Inventory-State form). Three separate mediation models were performed.
Results
The relationship between coping strategies (i.e.: problem-focused coping, emotion-focused coping and dysfunctional coping) and state anxiety resulted to be mediated by worry. Dysfunctional and problem-focused coping had a negative effect on anxiety scores and this effect was amplified by high levels of worry. Emotion-focused coping reduced state anxiety scores through its effect on reducing the levels of worry, which in turn was related to a reduction in anxiety.
Conclusion
The present study offers first evidence for the mediation role of worry in the relation between coping and anxiety during quarantine caused by COVID-19 pandemic. It supports the clinical importance of investigating people's coping strategies along with the levels of (cognitive) worry and their long-term effects on the psychological well-being during the outbreak, in order to deliver adequate personalized interventions. Psychological support should enhance emotion-focused coping strategies that have a protective effect on both worry and anxiety.
Keywords: COVID-19, Quarantine, Coping, Worry, Anxiety
Résumé
Introduction
L’épidémie de COVID-19 a contraint les citoyens italiens à une quarantaine généralisée de mars à mai 2020. La quarantaine est une mesure efficace pour réduire la propagation du virus grâce à l’éloignement physique et social, mais elle peut également avoir des conséquences psychologiques négatives sur la population. Les gens éprouvent des niveaux élevés d’inquiétude et d’anxiété et doivent faire face aux conséquences de l’urgence sanitaire. Le but de cette étude a été d’évaluer de manière préliminaire les relations causales entre l’adaptation, l’inquiétude et l’anxiété d’état au moment de la première vague de COVID-19, et le rôle médiateur de l’inquiétude entre l’adaptation et l’anxiété d’état.
Méthodes
Au cours du mois de mars 2020, 1273 citoyens italiens ont rempli une enquête ad hoc en ligne composée de questions concernant des données socio-démographiques et liées aux préoccupations, et d’un questionnaire d’auto-évaluation standardisé (Brief COPE, Penn State Worry Questionnaire et State-Trait Anxiety Inventory, l’échelle d’anxiété – État). Trois modèles de médiation distincts ont été réalisés.
Résultats
La relation entre les stratégies d’adaptation (c’est-à-dire l’adaptation centrée sur le problème, l’adaptation centrée sur les émotions et l’adaptation dysfonctionnelle) et l’anxiété liée à l’état a été influencée par l’inquiétude. L’adaptation dysfonctionnelle et axée sur les problèmes a eu un effet négatif sur les scores d’anxiété et cet effet a été amplifié par des niveaux élevés d’inquiétude. L’adaptation axée sur les émotions a réduit les scores d’anxiété d’état par son effet sur la réduction des niveaux d’inquiétude, qui à son tour était liée à une réduction de l’anxiété.
Conclusion
La présente étude offre une première preuve du rôle médiateur de l’inquiétude dans la relation entre l’adaptation et l’anxiété pendant la quarantaine causée par la pandémie de COVID-19. Elle soutient l’importance clinique d’étudier les stratégies d’adaptation des personnes ainsi que les niveaux d’inquiétude (cognitive) et leurs effets à long terme sur le bien-être psychologique pendant l’épidémie, afin de fournir des interventions personnalisées adéquates. Le soutien psychologique devrait améliorer les stratégies d’adaptation axées sur les émotions qui ont un effet protecteur sur l’inquiétude et l’anxiété.
Mots clés: COVID-19, Quarantaine, Coping, Inquiétude, Anxiété
1. Introduction
COVID-19 is the most recent infectious disease, which is affecting people worldwide, spreading from a region of China, Wuhan, since December 2019 (Wang, Horby, Hayden, & Gao, 2020). It causes fever, cough and breathing difficulties and in more cases a severe acute respiratory syndrome, which could lead to death. Due to its severity and rapid spread around the world, the World Health Organization stated on March 11 that COVID-19 can be characterized as a pandemic (WHO, 2020). After this declaration of emergency, the Italian government issued a prime ministerial decree (DCPM) in which quarantine had been extended to all Italian citizens, launching the lockdown phase until May 2020, except for workers involved in fundamental activities such as food sales, pharmacies, pet shops, laundries, gas stations (DPCM. 11 March 2020, n. 64). Quarantine, a successful measure to reduce viruses’ spread (Patel et al., 2020), is characterized by physical as well as social distances becoming a painful experience due to the separation from loved ones, the loss of freedom, the fear of contagiousness for themselves and others, economic difficulties, and the interruption of developmental tasks in emerging adults and of life plans, that has negative psychological consequences, such as psychological distress (anxiety, depression, general distress) on general population (Alkhamees et al., 2020, Brooks et al., 2020, Fernández et al., 2020, Fiorillo et al., 2020, Mucci et al., 2020, Smorti et al., 2020).
This pandemic represents a new and unexpected traumatic event, both for the socio-economic crisis and psychological impact (Chen et al., 2020, Pons et al., 2020), and have similarities and differences with other natural disasters, such as hurricanes, and previous epidemics, e.g., SARS, MERS and Ebola (Brooks et al., 2020, Ćosić et al., 2020, Fiorillo et al., 2020, Jungmann and Witthöft, 2020, Mathew et al., 2020, Serafini et al., 2020, Shah et al., 2021, Wang et al., 2020c). This is the first time that a global pandemic has such disruptive effects on people's lives (i.e., national closures, travel bans, social distancing), which consequently cause long lasting psychological burdening (Fiorillo et al., 2020).
The World Health Organization officially stated that a considerable degree of fear, worry and concern overwhelmed people, and anxiety was one of the main psychological outcomes experienced by the worldwide population during the quarantine caused by COVID-19 pandemic (WHO, 2021). People could experience a predictable state of non-clinical anxiety in the face of uncertainty, as it is a natural reaction to stressful, challenging, and unknown situations (Oliveri et al., 2016). Nevertheless, during the first wave of COVID-19 outbreak, some studies already reported that severe levels of anxiety were associated to the social distancing and isolation imposed by the lockdown measures, and consequently to the pervasive sense of loneliness and low perceived social support (Brooks et al., 2020, Fiorillo et al., 2020, Khan et al., 2020, Mucci et al., 2020, Serafini et al., 2020, Shah et al., 2021, Xiong et al., 2020, Lee and You, 2020). In particular, emerging adults, female and people living alone experienced higher anxiety levels (Mazza et al., 2020, Sebri et al., 2021, Shah et al., 2021, Wang et al., 2020d). Recent studies reported that people's psychological distress reached the threshold of clinical relevance (Cai et al., 2020, Li, 2020, McCracken et al., 2020, Xiong et al., 2020).
The unexpected intensity and severity of COVID-19 left many people physically and psychologically unprepared to cope with this situation (Fiorillo et al., 2020, Serafini et al., 2020), and individuals showed variability in interpreting, accepting and coping to the emergency context (Park et al., 2020, Vijayaraghavan and Singhal, 2020, Wang et al., 2020c). Coping is defined as the cognitive and behavioral strategies that people use to manage external and/or internal needs perceived as burdensome, or exceeding their resources (Folkman and Lazarus, 1988, Martínez et al., 2020). In general, different coping strategies to face with stressful situations have a different impact on the quality of life (Wang, Xia et al., 2020). Coping strategies are infinite and have traditionally been classified into categories such as problem-focused versus emotion-focused, functional versus dysfunctional, approach versus avoidance, engagement versus disengagement, and primary versus secondary control coping (Fink, 2016, García et al., 2018). However, up to now there is not a unique classification of these strategies. Following the coping classification in emotion- and problem-focused coping and dysfunctional coping (Coolidge et al., 2000, Cooper et al., 2006, Cooper et al., 2008, García et al., 2018), during COVID-19 pandemic recent studies showed that problem-focused coping and emotion-focused coping were the most common strategies used by people to deal with quarantine (Li, 2020, Park et al., 2020, Sebri et al., 2021). Instead, during previous epidemics, such as SARS outbreak, emotion-focused coping (e.g., acceptance, religion, seeking emotional support) was the predominant coping strategy, because they could not solve the problem directly, but they needed to overcome the crisis emotionally (Cava et al., 2005, Yeung and Fung, 2007). Preliminary studies reported that emotion-focused coping was associated with lower levels of worry and psychological distress both in previous crisis and during COVID-19 (Adams et al., 2011, Jin et al., 2016, Sebri et al., 2021, Yeung and Fung, 2007). In particular, people tended to “seek emotional support” by spending time with kids and partners or focusing on family members, making phone calls to friends and loved ones (Fu et al., 2020, Park et al., 2020, Rahman et al., 2020, Sebri et al., 2021). The use of this strategy was a protective factor during COVID-19 quarantine (Serafini et al., 2020) and female and caregivers tended to use this strategy more often than other people (Park et al., 2020, Sebri et al., 2021). The “seeking emotion support” was one of the common strategies even during past epidemics (Chew et al., 2020).
The problem-focused coping was often associated with a reduction in anxiety levels during COVID-19 pandemic (Fu et al., 2020, Rogowska et al., 2020). Nevertheless, strategies such as active coping or planning were mostly used in patients with anxiety disorders (Pozzi et al., 2015) and was also indicated as a risk factor for many PTSD symptoms during the experience of Hurricane Katrina (Glass et al., 2009). Other studies did not find any relation between problem-focused coping and distress levels (Littleton et al., 2007, Main et al., 2011).
Dysfunctional coping strategies, such as substance use/abuse or self-distraction, were constantly associated with negative outcomes, anxiety and higher levels of worry, after traumatic events such as sexual abuse or assault, domestic violence, burn injury, etc. (Littleton et al., 2007), or during SARS outbreak (Main et al., 2011, Maunder et al., 2006), and after the exposure to Hurricanes (Scott et al., 2010). Even during the COVID-19 pandemic, people tended to use self-distraction and substance use/abuse as coping strategies to deal with the health emergency context. Such dysfunctional coping strategies were again related to high psychological distress and worry, especially in younger people, gender minorities and in people who were financially unstable (Chen et al., 2020, Park et al., 2020, Rahman et al., 2020, Wang et al., 2020c).
Worry resulted to be a common reaction to COVID-19 pandemic: it reduces the cognitive resources needed for emotional processing and drives the attention on the perceived threat (Zysberg & Zisberg, 2020). Borkovec et al. (1983) defined worry as a sequence of negative and relatively uncontrollable thoughts and images about future events with uncertain outcomes, that evoke negative emotions and strictly high levels of anxiety and distress (Kelly & Miller, 1999). On the basis of Borkovec’ Cognitive Avoidance Theory of Worry (Sibrava & Borkovec, 2006), Gana et al. (2001) found a causal and unidirectional relationship between worry and anxiety that is worry causes anxiety, and a difference between the two constructs, that were shown to be separated, especially for the somatic aspects belonging to anxiety. There were some controversies about similarities and differences between worry and anxiety (Gana et al., 2001, Zebb and Beck, 1998). Worry has been conceptualized as a cognitive construct while anxiety was referred to an emotional arousal including unpleasant feeling of fear, dread or danger of something unknown, a visceral somatic activation (sympathetic and parasympathetic nervous system) and to behavioral responses such as avoidance and escape (Borkovec, 2002, Capobianco et al., 2018, Davey, 1994, Gana et al., 2001, Zebb and Beck, 1998). Worry and anxiety were highly correlated, being the two main constructs of Generalized Anxiety Disorder (GAD; American Psychiatric Association, 2013), but worry may work through different paths and processes than anxiety (Zysberg & Zisberg, 2020). When faced with a negative/uncertain event, people experience worry, which is characterized by repetitive thoughts focused on various aspects of a threat, which can help people to deal with and analyze the threats. This form of repetitive thinking was also considered part of a cognitive coping mechanism, in order to control intrusive thoughts about potentially aversive situations (Yook et al., 2010). The risk is that this aspect of worry might turn into rumination, a clinical symptom (Anniko et al., 2019, Donovan et al., 2017, Lewis et al., 2018). As mentioned before, COVID-19 has disrupted people's daily routine and caused high level of worry linked to the fear of contracting the virus, the risk of death of a loved one, the financial consequences, causing high levels of distress and anxiety, and a lower life satisfaction (Kivi et al., 2021, McKnight-Eily et al., 2021). Age and gender resulted to influence the levels of worry: older adults seemed to be less worried than younger people, and males were less worried than females (Barber and Kim, 2021, Zysberg and Zisberg, 2020). This finding was in line with previous research carried out in the field of natural disaster (Barber and Kim, 2021, Hunt et al., 2003). This doubtful situation and the overloaded information from social media enhanced the level of worry in the general population (Baiano et al., 2020, Lu et al., 2020), as also occurred during past epidemic and pandemic (Cowling et al., 2010, Ro et al., 2017). In particular, Ho et al. (2020) found that receiving information about COVID-19 from traditional media, internet media and friends enhanced the level of worry (Ho et al., 2020). Previous studies showed that worry positively correlates with Posttraumatic Stress Disorder (PTSD) (Arnaboldi et al., 2017, Bardeen et al., 2013, Oliveri et al., 2019, Tull et al., 2011) and anxiety disorders (Muris et al., 2005, Raes, 2010, Yook et al., 2010), and prior researchers investigated the mediation role of worry in causing neuroticism, intolerance of uncertainty (IU) and self-compassion, and anxiety disorders (Muris et al., 2005, Raes, 2010, Yook et al., 2010).
Despite the huge literature about the psychological impact of COVID-19, there are no studies that investigated in detail the causal relation among worry, coping strategies, and anxiety. The aim of this study was to explore the mediation role of worry between coping strategies and level of state anxiety during the first wave of COVID-19 pandemic in a sample of the Italian population. In particular, we formulated four hypotheses: (H1) the use of emotion- and problem-focused coping should reduce worry and anxiety; (H2) the use of dysfunctional coping should increase worry and anxiety; (H3) worry should have a positive correlation with anxiety; (H4) worry should mediate the relation between coping strategies (problem-, emotion-focused and dysfunctional coping) and anxiety.
2. Materials and methods
2.1. Participants
From 20 March to 27 March 2020, a total of 1273 Italian citizens from different regions voluntarily accepted to participate in this cross-sectional observational study, during their quarantine due to Coronavirus pandemic, and completed a series of had hoc questions and standardized questionnaires. All the participants signed an online informed consent and exclusion criteria were age < 18 years, incomplete answers, and the lack of signed informed consent. All the documents of the survey have been managed online because of the impossibility to meet people during quarantine. Nevertheless, contacts of authors have been provided to the participants in order to assist them for any query and issue.
2.2. Measures
A structured and self-administered ad hoc questionnaire (Appendix A) was created to assess the following domains.
2.2.1. Sociodemographic aspects and current status
The questionnaire included a set of specific questions to depict some personal information, such as gender, age, educational level, current employment, and current state of working (“What is your current working status?” Multiple choice: smart working, obligatory holidays, paid leave, unemployment insurance, closing my business as owner, currently at work, being unemployed), current region of residence (“In which region do you currently live?”), living arrangement (“With whom do you currently live?” Multiple choice: alone, with my family of origin, with my partner and/or children or with roommates), participants’ health status (“Did you test positive for COVID-19? Answer yes only in case of a proven positive test”) and close family and friend's health status (“Has anyone very close to you (relatives/friends) tested positive for COVID-19? Answer yes only in case of proven positive test. If yes, please specify who”).
In additions to this ad hoc questions, three self-report and standardized questionnaires had been administered, asking participants to refer to the imminent situation.
2.2.2. State-Trait Anxiety Inventory (STAI-Y1)
Is a self-report tool widely applied for assessing the state anxiety (Spielberger et al., 1983). Compared to the STAI-X original form, this version better discriminates anxiety from depression symptoms (Crawford et al., 2011). The state anxiety subscale is composed of 20 items, rated on a 4-points Likert scale ranging from 1 = “for nothing” to 4 = “very much” with the specific aim of assessing transitory emotional responses that include unpleasant feelings (worry, nervousness, and apprehension). Some examples of items are: “I feel secure”, “I feel frightened”, “I feel nervous”. High total score indicates higher anxiety. The STAI-Y1 is a reliable and valid tool for assessing anxiety states, even in a sample of healthy subjects (Potvin et al., 2011). The reliability of the original STAI-Y1 scale was assessed on male and female samples categorized according to age group or job. Specifically, internal consistency coefficients for the scale have ranged from .86 to .93 in the male sample divided in working adults, college students, high school students and military recruits and from .93 to .95 in the female sample. Following the age group, Cronbach's alpha ranged from .92 to .93 in the male sample and from .90 to .94 in the female sample (Spielberger et al., 1983). Our study confirms the excellent internal consistency of the instrument (α = .94). The Italian version was translated and validated by Pedrabissi and Santinello (1989), that also reported average scores of the validation sample were 36 ± 9.7 for men; 39.93 ± 11 for women (Pedrabissi & Santinello, 1989).
2.2.3. Brief–COPE
The shortened version of the COPE Inventory (Carver, 1997, Carver et al., 1989) consists in 28-items assessing 14 coping strategies that could be classified in to three domains: use of instrumental support, active coping, and planning as problem-focused coping; use of emotional support, acceptance, positive reframing, humor, and religion as emotion-focused coping; self-distraction, venting, behavioral disengagement, self-blame, denial, and substance use as dysfunctional coping (Coolidge et al., 2000, Cooper et al., 2006, Cooper et al., 2008, García et al., 2018). This version has the advantage of measuring coping strategies both in normal situations, called trait coping, and in specific stressful situations, called state or situational coping (Sartori & Rappagliosi, 2011). Cooper et al. (2008) evaluated the internal consistencies of the Brief COPE and found a good internal consistency for emotion-focused (α = 0.72), problem-focused (α = 0.84), and dysfunctional subscales (α = 0.75). Items of the situational version of the questionnaire are rated on a 4-point Likert Scale from 0 = “I did not do this absolutely” to 3 = “I am used to do this” in reference to how frequent is the application of such strategies to face this particular stressful event (Monzani et al., 2015). In the present study, people were asked to refer to the quarantine due to COVID-19 pandemic and some examples of the items were: “I’ve been taking action to try to make the situation better”, “I’ve been learning to live with it”, “I’ve been refusing to believe that it has happened”. Higher scores on each subscale indicates a greater use of those particular strategies. This short form decreases the amount of response time requested without losing psychometric properties and its reliability and validity (Carver, 1997, Crisp et al., 2013), moreover, it was widely validated around the world, even in Italy (Kimemia et al., 2011, Monzani et al., 2015, Scardaccione, 2008). The reliability analysis was carried out by Carver (1997), who found a good internal reliability as the values were higher than .50, despite the scales being composed of only two items (Carver, 1997). Moreover, Monzani et al. (2015) reported the omega value for all the subscales of the Italian situational version of Brief COPE (Monzani et al., 2015). In our study, the internal consistency (Cronbach's alpha) for emotion-focused coping is α = .61; for problem-focused coping is α = .70; for dysfunctional coping is α = .61.
2.2.4. Penn State Worry Questionnaire (PSWQ)
This scale assesses the intensity or inadequacy of worry and the tendency of worry to generalize to various situations. In particular, this instrument is used to identify pathological symptoms of concern that characterize generalized anxiety disorder (GAD), but without a diagnostic value (Dear et al., 2011). PSWQ is a short self-report questionnaire (16-items) rated on a 5-points Likert scale ranging from 1 = “not at all typical of me” to 5 = “very typical of me” (Meyer et al., 1990). The total score is calculated by summing the results of each item, with a reverse score of 5-items (item 1, 3, 8, 10 and 11). The total score can range from low (16–39), to moderate (40–59) or high (60–80) levels of worry. Meyer et al. (1990) tested PSWQ reliability and validity through different studies on samples of psychology college students and reported an internal consistency ranged from .91 to .95 (Meyer et al., 1990). This questionnaire was validated in an Italian version and showed high internal consistency (α = .85) and good test-retest reliability (Morani et al., 1999). Some examples of the items are: “I know I should not worry about things, but I just cannot help it”, “I have been a worrier all my life” and “I do not tend to worry about things”. In our study, PSWQ has an excellent internal consistency (α = .91).
2.3. Procedure
Since 20-Mar, 2020 a Qualtrics survey link (Qualtrics is an online management platform, designed to allow researchers to create surveys, gather and analyze data collected) has been shared through social media (Facebook, Linkedin, Researchgate, Twitter, Whatsapp). We choose to combine a self-selection online survey method of non-probability sampling with a snowball sampling technique, because it was the best method to invite a large number of people from all Italian regions during quarantine (Oliver et al., 2020). In the first sheet of the survey, the explanation of the study was presented, so that people could decide if they were interested to give their contribution. All the participants, that accepted to participate, were invited to sign an informed consent, and were informed that all the responses would remain strictly confidential and anonymous. The study was conducted according to the Declaration of Helsinki and the Ethical Committee of the European Institute of Oncology approved the study under the protocol nr R1423/21-IEO 1495.
2.4. Data analysis
All the analyses have been performed with SPSS version 26. The snowball sampling strategy is associated to the risk of collecting incomplete data, falsified answers, low-quality answers (Contandriopoulos et al., 2019). To ensure data quality, we tried to maximize the engagement of participants by stressing the relevance of this study as also a way to raise their voice reporting their psychological well-being status; we did not consider the incomplete questionnaires in the analysis; finally we checked the trend in participants’ responses in both PSWQ and STAI-Y1 to verify the overall coherence of participant's reported anxiety and worry levels. Descriptive statistics were employed to describe the characteristics of the sample and of the overall questionnaires total scores, while correlations (Pearson r and Spearman ρ) were performed to preliminary test the relationship between our variables of interest. Moreover, we performed U Mann–Whitney analysis as the variables do not follow a normal distribution to explore differences in the questionnaires between male and female. Cronbach alpha was computed to assess the reliability of questionnaires. Finally, to assess if the relationship between state anxiety and coping strategies were mediated by worry, we performed mediation analysis with PROCESS macro, using model 4 (Hayes & Rockwood, 2017). The mediation was tested using path analysis technique. Unstandardized indirect effects were computed for 5000 bootstrapped samples, and the 95% confidence interval was computed by determining the indirect effects at the 2.5th and 97.5th percentiles. As reported by Fairchild and McDaniel (2017), the mediation analysis with cross-sectional data brings with it some fair prejudices, and the percentage of the variance that is shared among constructs is not considered. Longitudinal mediation models may provide a better representation of the mechanisms behind psychological processes. Nevertheless the current study has an explanatory aim and it is part of a longitudinal study, with a follow-up at the end of the lockdown (T1 = mid-May 2020) and three months after the end of the first lockdown (T2 = mid-September 2020), and this preliminary mediation analysis helps to identify a causal model among coping strategies, anxiety and worry that will be further investigated/confirmed at a long-term.
3. Results
3.1. Descriptive statistics and levels of worry, anxiety and coping
Participants were from all Italian regions, though most were from Northern Italy (n = 903; 70.9%). The age of participants ranged from 18 to 80 (M = 35.12 years; SD = 11.52), 24.5% were males (n = 312) and 75.5% were females (n = 961). Most participants had a high educational level, degree or over (n = 824; 64.7%). The sample included mostly workers, particularly 44.3% of participants (n = 560) were blue-collar workers and 411 (32.5%) were white-collar workers. Only 61 participants were health care professionals (4.8%). The rest of the sample was composed of students and 71 were unemployed. Regarding the working status, half of workers continued working during this period, 412 of them were forced to work at home in smart working (32.5%). Almost all lived with family, 423 of them lived with the family of origin (33.2%) and 627 were living with a partner and/or child (49.2%).
Total scores of the questionnaires are reported in Table 1 . Considering PSWQ scores, the mean of our sample was in a range of moderate level of worry (44.17 ± 12.107), while the mean of State Anxiety scores was higher than the cut off for both in men and women (males: 46.31 ± 11.31; females: 52.78 ± 11.04), indicating a significant level of anxiety in our population. Moreover, our sample mainly used problem- and emotion-focused coping to deal with COVID-19 quarantine than dysfunctional coping. We performed Mann–Whitney U test to explore gender differences in psychological variables. Results showed that the levels of worry (U = 109757, p = .000), state anxiety (U = 101148, p = .000), problem-focused coping (U = 119903, p = .000), emotion-focused coping (U = 127618, p = .000) and dysfunctional coping (U = 127024, p = .000) in the female group were significantly higher than in the male group.
Table 1.
Mean scores of psychological variables.
| Psychological variables | Mean (SD) | Range | Mean male (SD) | Mean female (SD) |
|---|---|---|---|---|
| Worry | 44.17 (12.11) | 16–80 | 42.5 (11.1) | 47.4 (12.9) |
| Problem-focused coping | 16.88 (3.29) | 6–24 | 15.9 (3.2) | 17.2 (3.2) |
| Emotion-focused coping | 24.45 (4.20) | 10–40 | 23.6 (4) | 24.7 (4.2) |
| Dysfunctional coping | 22.75 (4.03) | 12–48 | 22 (4.4) | 22.9 (3.9) |
| Anxiety | 51.19 (11.45) | 20–80 | 46.3 (11.3) | 52.8 (11) |
Table 2 shows the correlations between sociodemographic variables and psychological aspects. However, we only reported in the text correlations with a score greater than .20, deeming it the recommended minimum to represent a significant effect for social science data (Ferguson, 2009). In particular, the use of dysfunctional coping strategies was related to higher levels of both anxiety (r = .33, p < .01, 95% CI) and worry (r = .37, p < .01, 95% CI). As expected, higher levels of worry were correlated with higher levels of anxiety (r = .66, p < .01, 95% CI).
Table 2.
Correlation coefficients for the main variables in the study.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1 | Age | – | ||||||
| 2 | Educational levela | .03 | – | |||||
| 3 | Worry | −.10** | −.06* | – | ||||
| 4 | Dysfunctional coping | −.09** | .00 | .37** | – | |||
| 5 | Problem-focused coping | −.00 | .18** | .07* | .30** | – | ||
| 6 | Emotion-focused coping | .03 | .16** | −.11** | .23** | .56** | – | |
| 7 | Anxiety | .02 | −.04 | .66** | .33** | .11** | −.17** | – |
aSpearman's correlation coefficients.
*p ≤ .05.; **p ≤ .01; ***p ≤ .001.
3.2. Mediational analysis
3.2.1. State anxiety and coping strategies
Three separate mediation models were performed.
In all the models, we tested the significance of the indirect effect of the mediator (PSWQ) on the dependent variable (STAI Y1) using a bootstrapping procedure.
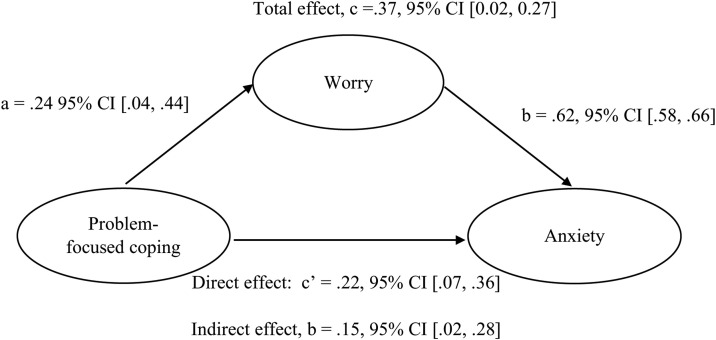
As Fig. 1 illustrates, in a mediation model including problem-focused coping as a predictor of state anxiety, there was a significant indirect effect of this coping strategies on state anxiety through worry. Testing the significance of the indirect effect with bootstrapping methods, we obtained an unstandardized indirect effect = .15, 95% CI [0.02, 0.28], with a standardized indirect effect of .04, 95% CI [0.005, 0.08]. Specifically, the effect of problem-focused coping strategies on state anxiety when worry is held constant (called the direct effect of problem-focused coping) was smaller than the total effect of this coping strategies on state anxiety without controlling for worry (direct effect of X: b = .22, p < .003; total effect of X on Y: b = .37, p < .001).
Fig. 1.
Model of problem-focused coping as a predictor of State Anxiety, mediated by worry. The confidence interval for the indirect effect is a BCa bootstrapped CI based on 5000 samples. Total effect, c = .37, 95% CI [0.02, 0.27]. Note. The regression coefficient between coping and state anxiety, after controlling for worry, is reported in parenthesis.
Summarizing, higher use of problem-focused coping strategies predicted higher levels of both anxiety and worry. The relationship between this coping style and anxiety was also mediated by worry levels: increasing levels of worry were associated with enhanced anxiety symptoms.
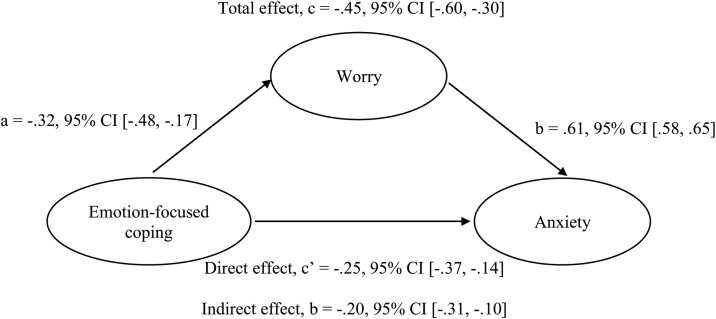
As reported in Fig. 2 the relationship between emotion-focused coping on state anxiety, mediated by worry, yielded to a significant indirect effect of worry on state anxiety. The bootstrapped unstandardized indirect effect was −2, and the 95% CI [−0.3, −0.1]. Thus, the indirect effect was statistically significant. The standardized indirect effect was −07, 95% CI [−0.11, −0.04]. In particular, the total effect of emotion-focused coping on state anxiety, without controlling the mediator, was significant (b = −.45, p < .001) and greater than the direct effect of this coping strategies on anxiety symptoms, when the mediator is held constant (b = −.25, p < .001), so a greater use of this coping strategy decreased the level of both anxiety and worry. As Fig. 2 shows, the use of emotion-focused coping strategies lead to a decrease of anxiety symptoms, as well as a reduction of levels of worry. On the contrary, higher levels of worry predicted higher anxiety scores. Even in this model, worry could be considered a mediator of the effect of emotion-focused coping and anxiety.
Fig. 2.
Model of emotion-focused coping as a predictor of State Anxiety, mediated by worry. The confidence interval for the indirect effect is a BCa bootstrapped CI based on 5000 samples. Total effect, c = −.45, 95% CI [−.60, −30]. Note. The regression coefficient between coping and state anxiety, after controlling for worry, is reported in parenthesis.
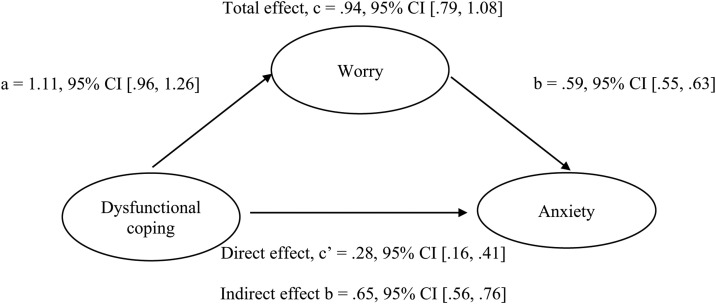
Finally, as Fig. 3 shows, there was a significant indirect effect of worry as a mediator of the impact of dysfunctional coping on perceived state anxiety. Through bootstrapping methods, we obtained an unstandardized indirect effect = .65, 95% CI [0.56, 0.76], and a standardized indirect effect of .23, 95% CI [0.19, 0.26]. Precisely, the effect of dysfunctional coping on state anxiety, without controlling worry, was significant (b = .94, p < .001), so a greater use of this coping strategy enhanced anxiety symptoms. Moreover, the direct effect of dysfunctional coping on anxiety scores, when worry is held constant, was smaller than the total effect (b = .28, p < .001).
Fig. 3.
Model of dysfunctional coping as a predictor of State Anxiety, mediated by worry. The confidence interval for the indirect effect is a BCa bootstrapped CI based on 5000 samples. Total effect, c = .94, 95% CI [.79, 1.08]. Note. The regression coefficient between coping and state anxiety, after controlling for worry, is reported in parenthesis.
Specifically, for what concern the relationship between dysfunctional coping and state anxiety, results showed that higher levels of dysfunctional coping were associated with both enhanced worry levels and anxiety symptoms. The relationship was also mediated by worry. Similar to the other mediation models, worry and state anxiety had a positive relationship, with more anxiety symptoms predicted by enhanced worry.
4. Discussion
The aim of this study was to investigate the effect of coping strategies on anxiety levels in the Italian population, approximately three weeks after the beginning of the quarantine due to COVID-19, and to explore worry as a potential mediator in such a relationship. COVID-19 pandemic represented a new and unexpected traumatic event that unfortunately is still ongoing (Chen et al., 2020, Pons et al., 2020). Data used in our secondary analysis on existing data was collected during the initial phase of COVID-19 pandemic, when all Italian citizens were in quarantine for the first time. Globally, our results showed a negative impact of COVID-19 quarantine on this sample, reporting moderate level of worry and high level of state anxiety and these findings were consistent with previous studies on COVID-19 pandemic (Brooks et al., 2020, Fiorillo et al., 2020, Khan et al., 2020, Mucci et al., 2020, Serafini et al., 2020, Shah et al., 2021, WHO, 2021, Xiong et al., 2020). Moreover, even in our sample, females experienced higher levels of anxiety than males (Mazza et al., 2020, Shah et al., 2021, Wang et al., 2020d).
Coping strategies are necessary for the individual resilience and adaptation process, indeed, when people experience a critical event, they start an appraisal process that ends with the identification of a coping method. In a situation without precedent, Brooks et al. (2020) suggested spreading out practical advice on coping strategies and stress management techniques to help people mitigate quarantine negative consequences. In line with previous studies, our sample tended to use both problem-focused coping and emotion-focused coping (Li, 2020, Park et al., 2020, Sebri et al., 2021).
Mediation analysis results showed that the use of different coping strategies, on a case-by-case basis, reduced or enhanced state anxiety scores, and such effects were exacerbated by the reduction or increase of worry levels, the mediator variable, which in turns provoked a further reduction or enhance in anxiety. Specifically, problem-focused and dysfunctional coping predicted higher level of state anxiety, and such relationships were mediated by worry, on which these coping strategies had an increasing effect, and which in turn caused an increase in anxiety. Thus, the effect on anxiety scores of dysfunctional and problem-focused coping were amplified by the presence of high levels of worry. Previous studies both on past epidemics and on COVID-19 pandemic (Chen et al., 2020, Littleton et al., 2007, Main et al., 2011, Maunder et al., 2006, Park et al., 2020, Rahman et al., 2020, Scott et al., 2010, Wang et al., 2020c) confirmed that the use of dysfunctional coping is maladaptive, enhancing the levels of both anxiety and worry during quarantine. On the contrary, we found that also the problem-focused coping have a negative effect on anxiety and this result is in contrast with what has been observed in previous studies (Fu et al., 2020, Rogowska et al., 2020). This could be also due to the different tools administered to evaluate the coping strategies.
The emotion-focused coping proved to be an excellent coping strategy even during this health emergency, by reducing the state anxiety scores through its effect on the levels of worry, which mediates the effects on anxiety as observed in our results. Our findings showed that emotion-focused coping strategies might be the most efficient modality to react toward a scaring/threatening event such as this pandemic, and to deal with a quarantine, by reducing the “disturbing” mediation effect of worry. This finding was also in line with evidence coming from past epidemics (Adams et al., 2011, Jin et al., 2016, Yeung and Fung, 2007). Emotion-focused coping is referred to the ability to regulate negative emotions caused by the stressful event, making an attempt to control the suffering, the inner arousal, the intrusive thoughts, by adopting active strategies such as talking or writing about emotions through therapy or journaling, accepting the situation and the related emotions, practicing mindful meditation or seeking for emotional social support. This could be important especially when people realize that they cannot do anything directly to figure out the problem or avoid it, but they can just follow the government rules, stay at home and adapt to the situation. All the information from mass media and social media reinforced these guidelines, and therefore people could only try to manage and regulate the negative emotional responses caused by the situation (Brivio et al., 2020).
These results further highlight the importance to act immediately on negative and relatively uncontrollable thoughts generated by a situation that risks to become a psychological emergency as well as an health emergency: worst-case images about future events with uncertain outcomes can foster the cognitive component of emotional arousal (worry), along with maladaptive coping strategies (dysfunctional coping). Being aware of coping strategies that people put in place most frequently and the relevance that worry could have at clinical level might be the first step to plan personalized intervention based on people's characteristics and personal tendencies (Cutica et al., 2014, Oliveri et al., 2020). People feelings of anxiety and worry during quarantine are normal until they become unmanageable; in this case they could lead to PTSD symptoms with the prolongation of the quarantine or after it is over, and people can gradually return to their lives (Liu et al., 2020a, Wang et al., 2020b, Brivio et al., 2021). Our findings provide some guidance, such as that clinical and psychological support should be based on the emotion-focused coping strategies, more than problem-focused strategies: people could try to accept and not to avoid negative feelings, and learn new ways to express them. Some strategies that people could use are talking with friends several times in a day (emotional support), shifting the way they see the problem (positive reframing), following yoga, meditation or training lessons on the computer. Psychologist could consider providing a sort of psychoeducation tools or interventions for the general population in order to explain the emotion-focused coping strategies that people could use to deal with worry and anxiety, underlying that in this emergency situation it is normal to experience repetitive negative thoughts caused by the fear of contracting the virus, the distress for the economic consequences, the grief for a loved one and the loss of freedom. Based on our findings that showed differences in the effect of coping strategies on emotions, the content of psychoeducational interventions must be focused on the needs of people. Clinically relevant levels of worry and anxiety could be tackled with evidence-based treatments (e.g., cognitive-behavioral therapy) aiming at improving adaptive coping strategies and personal resources, acquire some awareness and sense of self-efficacy. The recent literature emphasized the utility of eHealth or the use of new technologies in cancer management, to empower people, to promote the personal health and quality of life (Monzani and Pizzoli, 2020, Renzi et al., 2017): we believe the same idea could be used in this emergency context to help people in modulating worry and anxiety and prevent the risk of virus transmission due to in-person intervention. In China online mental health services or tele mental health were used to facilitate the development of Chinese public emergency interventions (Liu et al., 2020b, Zhou et al., 2020). In Italy, the Ministry of Health and Civil Protection, with the technological support offered free of charge by TIM, activated an emergency number active every day, from 8 to 24, in which specialized professionals, psychologists, psychotherapists and psychoanalysts respond to help people coping with COVID-19. Overall, the current literature confirms the efficacy of videoconferencing psychotherapy during the pandemic (Fernández-Álvarez & Fernández-Álvarez, 2021).
This study has some limitations. A first limitation is the cross-sectional nature of the study that limits the degree to which causal relationships can be inferred. Indeed, also the use of the STAI questionnaire that included two items related to worry could be a bias. However, the presence of previous studies that use worry as a mediator on anxiety, using PSWQ and STAI-Y, provides a sufficiently compelling case for the mediational modeling that was conducted. Moreover, to overcome this limitation, this study was implemented in a longitudinal design to verify that the direction of causation, as preliminarily hypothesized and tested in this study could be confirmed. Future research could change the tool for evaluating anxiety with a tool that includes item on the somatic characteristics of anxiety.
Second, the massive sampling strategy through social media, even if it was the only way to collect responses due to the social distancing, was associated with some biases and certain risks in data quality. In particular, some participants might have falsified the answers or might have responded superficially. Anyway, we opted for some expedients described in the methods to minimize these risks.
Finally, participants were laypeople not positive to COVID-19, mainly females and young. Further research should examine to what extent the relationship among variables reported here could also be generalized to older people, to people who are positive to COVID-19 and to healthcare workers.
5. Conclusion
In conclusion, and notwithstanding the above limitations, the present study expands the previous knowledge about the psychological impact of COVID-19 pandemic by providing the first evidence for the mediation role of repetitive thinking (worry) in the relation between coping strategies and anxiety during quarantine caused by COVID-19 pandemic. This study potentially contributes to understand the aspects where a psychological support should be focused in order to improve resilience during the COVID-19 epidemic.
Disclosure of interest
The authors declare that they have no competing interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author, C.C., upon reasonable request.
Author contribution statement
CC conceived the design of the present study and was in charge of overall direction and planning under the supervision of GP. SFMP analyzed data. CC, SFP and SO discussed the results and commented on the manuscript. All the authors wrote the final version of the manuscript.
Acknowledgment
We would like to thank Valeria Sebri, Giulia Ongaro and Lucrezia Savioni, Ph.D. students within the European School of Molecular Medicine (SEMM), for their contribution in creating this survey and in collecting data.
Clizia Cincidda and Silvia F.M. Pizzoli are PhD student in the European School of Molecular Medicine (SEMM).
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5x1000 funds.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.erap.2021.100671.
Appendix A. Supplementary data
References
- Adams T., Anderson L., Turner M., Armstrong J. Coping through a disaster: Lessons from hurricane Katrina. Journal of Homeland Security and Emergency Management. 2011;8(1) doi: 10.2202/1547-7355.1836. [DOI] [Google Scholar]
- Alkhamees A.A., Aljohani M.S., Alghesen M.A., Alhabib A.T. Psychological distress in quarantine designated facility during COVID-19 pandemic in Saudi Arabia. Risk management and healthcare policy. 2020;13:3103–3120. doi: 10.2147/RMHP.S284102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. 2013. Diagnostic and statistical manual of mental disorders. [DOI] [Google Scholar]
- Anniko M.K., Boersma K., Tillfors M. Sources of stress and worry in the development of stress-related mental health problems: A longitudinal investigation from early- to mid-adolescence. Anxiety, stress, and coping. 2019;32(2):155–167. doi: 10.1080/10615806.2018.1549657. [DOI] [PubMed] [Google Scholar]
- Arnaboldi P., Riva S., Crico C., Pravettoni G. A systematic literature review exploring the prevalence of posttraumatic stress disorder and the role played by stress and traumatic stress in breast cancer diagnosis and trajectory. Breast Cancer: Targets and Therapy. 2017;9:473–485. doi: 10.2147/BCTT.S111101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baiano C., Zappullo I., the LabNPEE Group, Conson M. Tendency to worry and fear of mental health during Italy's COVID-19 lockdown. International Journal of Environmental Research and Public Health. 2020;17(16):5928. doi: 10.3390/ijerph17165928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber S.J., Kim H. COVID-19 worries and behavior changes in older and younger men and women. The journals of gerontology. Series B, Psychological sciences and social sciences. 2021;76(2):e17–e23. doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardeen J.R., Fergus T.A., Wu K.D. The interactive effect of worry and intolerance of uncertainty on posttraumatic stress symptoms. Cognitive therapy and research. 2013;37(4):742–751. doi: 10.1007/s10608-012-9512-1. [DOI] [Google Scholar]
- Borkovec T.D., Robinson E., Pruzinsky T., DePree J.A. Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy. 1983;21(1):9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- Borkovec T.D. Life in the future versus life in the present. Clinical Psychology: Science and Practice. 2002;9(1):76–80. doi: 10.1093/clipsy.9.1.76. [DOI] [Google Scholar]
- Brivio E., Oliveri S., Pravettoni G. Empowering communication in emergency contexts: Reflections from the Italian coronavirus outbreak. Mayo Clinic Proceedings. 2020;95(5):849–851. doi: 10.1016/j.mayocp.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brivio E., Oliveri S., Guiddi P., Pravettoni G. Incidence of PTSD and generalized anxiety symptoms during the first wave of COVID-19 outbreak: An exploratory study of a large sample of the Italian population. BMC Public Health. 2021;21(1):1158. doi: 10.1186/s12889-021-11168-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Z., Zheng S., Huang Y., Zhang X., Qiu Z., Huang A., et al. Emotional and cognitive responses and behavioral coping of Chinese medical workers and general population during the pandemic of COVID-19. International journal of environmental research and public health. 2020;17(17):6198. doi: 10.3390/ijerph17176198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capobianco L., Morris J.A., Wells A. Worry and rumination: Do they prolong physiological and affective recovery from stress? Anxiety, stress, and coping. 2018;31(3):291–303. doi: 10.1080/10615806.2018.1438723. [DOI] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol's too long: Consider the brief COPE. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver C.S., Scheier M.F., Weintraub J.K. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Cava M.A., Fay K.E., Beanlands H.J., McCay E.A., Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nursing. 2005;22(5):398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [DOI] [PubMed] [Google Scholar]
- Chen B., Sun J., Feng Y. How have COVID-19 isolation policies affected young people's mental health? - Evidence from Chinese college students. Frontiers in psychology. 2020;11:1529. doi: 10.3389/fpsyg.2020.01529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew Q.H., Wei K.C., Vasoo S., Chua H.C., Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID-19 pandemic. Singapore medical journal. 2020;61(7):350–356. doi: 10.11622/smedj.2020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contandriopoulos D., Sapeha H., Larouche C. Some insights related to social network analysis data collection challenges – a research note. International Journal of Social Research Methodology. 2019;22(5):463–468. doi: 10.1080/13645579.2019.1574957. [DOI] [Google Scholar]
- Coolidge F.L., Segal D.L., Hook J.N., Stewart S. Personality disorders and coping among anxious older adults. Journal of anxiety disorders. 2000;14(2):157–172. doi: 10.1016/s0887-6185(99)00046-8. [DOI] [PubMed] [Google Scholar]
- Cooper C., Katona C., Livingston G. Validity and reliability of the brief COPE in carers of people with dementia: The LASER-AD Study. The Journal of nervous and mental disease. 2008;196(11):838–843. doi: 10.1097/NMD.0b013e31818b504c. [DOI] [PubMed] [Google Scholar]
- Cooper C., Katona C., Orrell M., Livingston G. Coping strategies and anxiety in caregivers of people with Alzheimer's disease: The LASER-AD study. Journal of affective disorders. 2006;90(1):15–20. doi: 10.1016/j.jad.2005.08.017. [DOI] [PubMed] [Google Scholar]
- Ćosić K., Popović S., Šarlija M., Kesedžić I. Impact of human disasters and COVID-19 pandemic on mental health: Potential of digital psychiatry. Psychiatria Danubina. 2020;32(1):25–31. doi: 10.24869/psyd.2020.25. [DOI] [PubMed] [Google Scholar]
- Cowling B.J., Ng D.M., Ip D.K., Liao Q., Lam W.W., Wu J.T., et al. Community psychological and behavioral responses through the first wave of the 2009 influenza A(H1N1) pandemic in Hong Kong. The Journal of infectious diseases. 2010;202(6):867–876. doi: 10.1086/655811. [DOI] [PubMed] [Google Scholar]
- Crawford J., Cayley C., Lovibond P.F., Wilson P.H., Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for Self-Report Mood Scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS) Australian Psychologist. 2011;46(1):3–14. doi: 10.1111/j.1742-9544.2010.00003.x. [DOI] [Google Scholar]
- Crisp C.C., Vaccaro C.M., Pancholy A., Kleeman S., Fellner A.N., Pauls R. Is female sexual dysfunction related to personality and coping? An exploratory study. Sexual Medicine. 2013;1(2):69–75. doi: 10.1002/sm2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutica I., Vie G.M., Pravettoni G. Personalised medicine: The cognitive side of patients. European Journal of Internal Medicine. 2014;25(8):685–688. doi: 10.1016/j.ejim.2014.07.002. [DOI] [PubMed] [Google Scholar]
- Davey G.C.L. In: Wiley series in clinical psychology. Worrying: Perspectives on theory, assessment and treatment. Davey G.C.L., Tallis F., editors. John Wiley & Sons; USA: 1994. Pathological worrying as exacerbated problem-solving; pp. 35–59. [Google Scholar]
- Dear B.F., Titov N., Sunderland M., McMillan D., Anderson T., Lorian C., et al. Psychometric comparison of the generalized anxiety disorder scale-7 and the Penn State Worry Questionnaire for Measuring Response during treatment of generalised anxiety disorder. Cognitive behaviour therapy. 2011;40(3):216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- Donovan C.L., Holmes M.C., Farrell L.J., Hearn C.S. Thinking about worry: Investigation of the cognitive components of worry in children. Journal of affective disorders. 2017;208:230–237. doi: 10.1016/j.jad.2016.09.061. [DOI] [PubMed] [Google Scholar]
- DPCM. 11 marzo 2020, n. 64, in materia di “Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n.6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19, applicabili sull’intero territorio nazionale”. http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=73643.
- Fairchild A.J., McDaniel H.L. Best (but oft-forgotten) practices: mediation analysis. The American journal of clinical nutrition. 2017;105(6):1259–1271. doi: 10.3945/ajcn.117.152546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson C.J. An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice. 2009;40(5):532–538. doi: 10.1037/a0015808. [DOI] [Google Scholar]
- Fernández R.S., Crivelli L., Guimet N.M., Allegri R.F., Pedreira M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. Journal of affective disorders. 2020;277:75–84. doi: 10.1016/j.jad.2020.07.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Álvarez J., Fernández-Álvarez H. Videoconferencing psychotherapy during the pandemic: Exceptional times with enduring effects? Frontiers in psychology. 2021;12:589536. doi: 10.3389/fpsyg.2021.589536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink G. Vol. 1. Academic Press; USA: 2016. (Stress: Concepts, cognition, emotion, and behavior: Handbook of stress series). [Google Scholar]
- Fiorillo A., Sampogna G., Giallonardo V., Del Vecchio V., Luciano M., Albert U., et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. European psychiatry: The journal of the Association of European Psychiatrists. 2020;63(1):e87. doi: 10.1192/j.eurpsy.2020.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S., Lazarus R.S. Coping as a mediator of emotion. Journal of Personality and Social Psychology. 1988;54(3):466–475. doi: 10.1037/0022-3514.54.3.466. [DOI] [PubMed] [Google Scholar]
- Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S., et al. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Translational psychiatry. 2020;10(1):1–9. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gana K., Martin B., Canouet M. Worry and anxiety: Is there a casual relationship? Psychopathology. 2001;34(5):221–229. doi: 10.1159/000049314. [DOI] [PubMed] [Google Scholar]
- García F.E., Barraza-Peña C.G., Wlodarczyk A., Alvear-Carrasco M., Reyes-Reyes A. Psychometric properties of the Brief COPE for the evaluation of coping strategies in the Chilean population. Psicologia: Reflexão e Crítica. 2018;31:22. doi: 10.1186/s41155-018-0102-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass K., Flory K., Hankin B.L., Kloos B., Turecki G. Are coping strategies, social support, and hope associated with psychological distress among hurricane Katrina survivors? Journal of Social and Clinical Psychology. 2009;28(6):779–795. doi: 10.1521/jscp.2009.28.6.779. [DOI] [Google Scholar]
- Hayes A.F., Rockwood N.J. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy. 2017;98:39–57. doi: 10.1016/j.brat.2016.11.001. [DOI] [PubMed] [Google Scholar]
- Ho H.Y., Chen Y.L., Yen C.F. Different impacts of COVID-19-related information sources on public worry: An online survey through social media. Internet interventions. 2020;22:100350. doi: 10.1016/j.invent.2020.100350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt S., Wisocki P., Yanko J. Worry and use of coping strategies among older and younger adults. Journal of anxiety disorders. 2003;17(5):547–560. doi: 10.1016/s0887-6185(02)00229-3. [DOI] [PubMed] [Google Scholar]
- Jin X., Wu L., Becken S., Ding P. How do worry, self-efficacy, and coping interact? Examining Chinese tourists to Australia. Journal of China Tourism Research. 2016;12(3–4):374–393. doi: 10.1080/19388160.2016.1251868. [DOI] [Google Scholar]
- Jungmann S.M., Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? Journal of anxiety disorders. 2020;73:102239. doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimemia M., Asner-Self K., Daire A. An exploratory factor analysis of the brief COPE with a sample of Kenyan Caregivers. International Journal for the Advancement of Counselling. 2011;33(3):149–160. doi: 10.1007/s10447-011-9122-8. [DOI] [Google Scholar]
- Kelly W.E., Miller M.J. A discussion of worry with suggestions for counselors. Counseling and Values. 1999;44(1):55–66. doi: 10.1002/j.2161-007X.1999.tb00152.x. [DOI] [Google Scholar]
- Khan S., Siddique R., Li H., Ali A., Shereen M.A., Bashir N., et al. Impact of coronavirus outbreak on psychological health. Journal of global health. 2020;10(1):010331. doi: 10.7189/jogh.10.010331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivi M., Hansson I., Bjälkebring P. Up and about: Older adults’ well-being during the COVID-19 pandemic in a Swedish Longitudinal Study. The journals of gerontology. Series B, Psychological sciences and social sciences. 2021;76(2):e4–e9. doi: 10.1093/geronb/gbaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M., You M. Psychological and behavioral responses in South Korea during the early stages of coronavirus disease 2019 (COVID-19) International journal of environmental research and public health. 2020;17(9):2977. doi: 10.3390/ijerph17092977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis E.J., Yoon K.L., Joormann J. Emotion regulation and biological stress responding: Associations with worry, rumination, and reappraisal. Cognition & emotion. 2018;32(7):1487–1498. doi: 10.1080/02699931.2017.1310088. [DOI] [PubMed] [Google Scholar]
- Li Q. Psychosocial and coping responses toward 2019 coronavirus diseases (COVID-19): A cross-sectional study within the Chinese general population. QJM: Monthly journal of the Association of Physicians. 2020;113(10):731–738. doi: 10.1093/qjmed/hcaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littleton H., Horsley S., John S., Nelson D.V. Trauma coping strategies and psychological distress: A meta-analysis. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies. 2007;20(6):977–988. doi: 10.1002/jts.20276. [DOI] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.-T., Liu Z., Hu S., et al. Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.-W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. Journal of Medical Virology. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main A., Zhou Q., Ma Y., Luecken L.J., Liu X. Relations of SARS-related stressors and coping to Chinese college students’ psychological adjustment during the 2003 Beijing SARS epidemic. Journal of Counseling Psychology. 2011;58(3):410–423. doi: 10.1037/a0023632. [DOI] [PubMed] [Google Scholar]
- Martínez J.P., Méndez I., Ruiz-Esteban C., Fernández-Sogorb A., García-Fernández J.M. Profiles of burnout, coping strategies and depressive symptomatology. Frontiers in psychology. 2020;11:591. doi: 10.3389/fpsyg.2020.00591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew R., Sahu A., Mohindra R. Catastrophe and the cure: Looking beyond the COVID-19 pandemic. The International Journal of Health Planning and Management. 2020;36(1):212–214. doi: 10.1002/hpm.3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. International journal of environmental research and public health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. Psychological impact of COVID-19 in the Swedish population: Depression, anxiety, and insomnia and their associations to risk and vulnerability factors. European Psychiatry. 2020;63(1):e81. doi: 10.1192/j.eurpsy.2020.81. (1–9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight-Eily L.R., Okoro C.A., Strine T.W., Verlenden J., Hollis N.D., Njai R., et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic – United States, April and May 2020. MMWR. Morbidity and mortality weekly report. 2021;70(5):162–166. doi: 10.15585/mmwr.mm7005a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer T.J., Miller M.L., Metzger R.L., Borkovec T.D. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Monzani D., Pizzoli S.F.M. P5 eHealth: An agenda for the health technologies of the future. Springer International Publishing; 2020. The prevention of chronic diseases through eHealth: A practical overview; pp. 33–51. [DOI] [Google Scholar]
- Monzani D., Steca P., Greco A., D’Addario M., Cappelletti E., Pancani L. The situational version of the brief COPE: Dimensionality and relationships with goal-related variables. Europe's Journal of Psychology. 2015;11(2):295–310. doi: 10.5964/ejop.v11i2.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morani S., Pricci D., Sanavio E. Penn State Worry Questionnaire e Worry Domains Questionnaire. Presentazione delle versioni italiane ed analisi della fedeltà. Psicoterapia Cognitiva e Comportamentale. 1999;5(3):195–209. [Google Scholar]
- Mucci F., Mucci N., Diolaiuti F. Lockdown and isolation: Psychological aspects of COVID-19 pandemic in the general population. Clinical Neuropsychiatry: Journal of Treatment Evaluation. 2020;17(2):63–64. doi: 10.36131/CN20200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P., Roelofs J., Rassin E., Franken I., Mayer B. Mediating effects of rumination and worry on the links between neuroticism, anxiety and depression. Personality and Individual Differences. 2005;39(6):1105–1111. doi: 10.1016/j.paid.2005.04.005. [DOI] [Google Scholar]
- Oliver N., Barber X., Roomp K., Roomp K. Assessing the impact of the COVID-19 pandemic in Spain: Large-scale, online, self-reported population survey. Journal of medical Internet research. 2020;22(9):e21319. doi: 10.2196/21319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveri S., Arnaboldi P., Pizzoli S., Faccio F., Giudice A.V., Sangalli C., et al. PTSD symptom clusters associated with short- and long-term adjustment in early diagnosed breast cancer patients. Ecancer medical science. 2019;13:917. doi: 10.3332/ecancer.2019.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveri S., Durosini I., Cutica I., Cincidda C., Spinella F., Baldi M., et al. Health orientation and individual tendencies of a sample of Italian genetic testing consumers. Molecular Genetics & Genomic Medicine. 2020;8(8):e1291. doi: 10.1002/mgg3.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveri S., Howard H.C., Renzi C., Hansson M.G., Pravettoni G. Anxiety delivered direct-to-consumer: Are we asking the right questions about the impacts of DTC genetic testing? Journal of medical genetics. 2016;53(12):798–799. doi: 10.1136/jmedgenet-2016-104184. [DOI] [PubMed] [Google Scholar]
- Park C.L., Russell B.S., Fendrich M., Finkelstein-Fox L., Hutchison M., Becker J. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. Journal of general internal medicine. 2020;35(8):2296–2303. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel A., Patel S., Fulzele P., Mohod S., Chhabra K.G. Quarantine an effective mode for control of the spread of COVID-19? A review. Journal of family medicine and primary care. 2020;9(8):3867–3871. doi: 10.4103/jfmpc.jfmpc_785_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrabissi L., Santinello M. Verifica della validità dello STAI forma Y di Spielberger. Verification of the validity of the STAI, Form Y, by SpielbergerGiunti Organizzazioni Speciali. 1989;191–192:11–14. [Google Scholar]
- Pons J., Ramis Y., Alcaraz S., Jordana A., Borrueco M., Torregrossa M. Where did all the sport go? Negative impact of COVID-19 lockdown on life-spheres and mental health of Spanish young athletes. Frontiers in psychology. 2020;11:611872. doi: 10.3389/fpsyg.2020.611872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potvin O., Bergua V., Meillon C., Le Goff M., Bouisson J., Dartigues J.F., et al. Norms and associated factors of the STAI-Y State anxiety inventory in older adults: Results from the PAQUID study. International psychogeriatrics. 2011;23(6):869–879. doi: 10.1017/S1041610210002358. [DOI] [PubMed] [Google Scholar]
- Pozzi G., Frustaci A., Tedeschi D., Solaroli S., Grandinetti P., Di Nicola M., et al. Coping strategies in a sample of anxiety patients: Factorial analysis and associations with psychopathology. Brain and behavior. 2015;5(8):e00351. doi: 10.1002/brb3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raes F. Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and Individual Differences. 2010;48(6):757–761. doi: 10.1016/j.paid.2010.01.023. [DOI] [Google Scholar]
- Rahman M.A., Hoque N., Alif S.M., Salehin M., Islam S., Banik B., et al. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Globalization and health. 2020;16(1):95. doi: 10.1186/s12992-020-00624-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renzi C., Fioretti C., Oliveri S., Mazzocco K., Zerini D., Alessandro O., et al. A qualitative investigation on patient empowerment in prostate cancer. Frontiers in psychology. 2017;8:1215. doi: 10.3389/fpsyg.2017.01215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ro J.S., Lee J.S., Kang S.C., Jung H.M. Worry experienced during the 2015 Middle East Respiratory Syndrome (MERS) pandemic in Korea. PloS one. 2017;12(3):e0173234. doi: 10.1371/journal.pone.0173234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogowska A.M., Kuśnierz C., Bokszczanin A. Examining anxiety, life satisfaction, general health, stress and coping styles during COVID-19 pandemic in polish sample of university students. Psychology Research and Behavior Management. 2020;13:797–811. doi: 10.2147/PRBM.S266511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartori R., Rappagliosi C.M. Stress e insegnamento: Contributro all’indagine sulle strategie di coping degli insegnanti in Italia. Stress and teaching: A contribution to the enquiry on the coping strategies of teachers in ItalyJournal of Educational, Cultural and Psychological Studies. 2011;4:147–165. [Google Scholar]
- Scardaccione G. In: Responsabilità e disimpegno. Di Francesco G., Feriozzi F., Scardaccione G., editors. SIGRAF Edizioni Scientifiche; Pescara: 2008. Personalità e capacità di coping: quanto si influenzano reciprocamente in un campione di studenti della Facoltà di Scienze Sociali [Personality and coping skills: how much they influence each other in a sample of students of the Faculty of Social Sciences] pp. 69–125. [Google Scholar]
- Scott S.L., Carper T.M., Middleton M., White R., Renk K., Grills-Taquechel A. Relationships among locus of control, coping behaviors, and levels of worry following exposure to hurricanes. Journal of Loss and Trauma. 2010;15(2):123–137. doi: 10.1080/15325020902925985. [DOI] [Google Scholar]
- Sebri V., Cincidda C., Savioni L., Ongaro G., Pravettoni G. Worry during the initial height of the COVID-19 crisis in an Italian sample. The Journal of general psychology. 2021;148(3):327–359. doi: 10.1080/00221309.2021.1878485. (Advance online publication) [DOI] [PubMed] [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM: Monthly journal of the Association of Physicians. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201. (Advance online publication) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S., Mohammad D., Qureshi M., Abbas M.Z., Aleem S. Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID-19) pandemic. Community mental health journal. 2021;57(1):101–110. doi: 10.1007/s10597-020-00728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibrava N.J., Borkovec T.D. In: Worry and its psychological disorders: Theory, assessment and treatment. Davey G.C.L., Wells A., editors. Wiley Publishing; 2006. The cognitive avoidance theory of worry; pp. 239–256. [DOI] [Google Scholar]
- Smorti M., Ponti L., Cincidda C. Life satisfaction linked to different independence-from-parents conditions in Italian emerging adults. Journal of Youth Studies. 2020;23(4):530–544. doi: 10.1080/13676261.2019.1634250. [DOI] [Google Scholar]
- Spielberger C.D., Gorsuch R.L., Lushene R. Consulting Psychologists Press, Inc. Mind Garden, Inc; California: 1983. State-Trait Anxiety Inventory for adults sampler set manual, instrument and scoring guide. [DOI] [Google Scholar]
- Tull M.T., Hahn K.S., Evans S.D., Salters-Pedneault K., Gratz K.L. Examining the role of emotional avoidance in the relationship between posttraumatic stress disorder symptom severity and worry. Cognitive Behaviour Therapy. 2011;40(1):5–14. doi: 10.1080/16506073.2010.515187. [DOI] [PubMed] [Google Scholar]
- Vijayaraghavan P., Singhal D. A descriptive study of Indian General Public's Psychological responses during COVID-19 pandemic lockdown period in India. PsyArXiv [Preprint] 2020 doi: 10.31234/osf.io/jeksn. [DOI] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. The Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Xia Q., Xiong Z., Li Z., Xiang W., Yuan Y., et al. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey. PloS one. 2020;15(5):e0233410. doi: 10.1371/journal.pone.0233410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International journal of environmental research and public health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Director-general's opening remarks at the media briefing on COVID-19, March 11th, 2020.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- World Health Organization . Regional Office for Europe; 2021. Mental health and COVID-19. ( https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technical-guidance/noncommunicable-diseases/mental-health-and-covid-19) [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L., Gill H., Phan L., et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of affective disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung D.Y., Fung H.H. Age differences in coping and emotional responses toward SARS: A longitudinal study of Hong Kong Chinese. Aging & Mental Health. 2007;11(5):579–587. doi: 10.1080/13607860601086355. [DOI] [PubMed] [Google Scholar]
- Yook K., Kim K.H., Suh S.Y., Lee K.S. Intolerance of uncertainty, worry, and rumination in major depressive disorder and generalized anxiety disorder. Journal of Anxiety Disorders. 2010;24(6):623–628. doi: 10.1016/j.janxdis.2010.04.003. [DOI] [PubMed] [Google Scholar]
- Zebb B.J., Beck J.G. Worry versus anxiety. Is there really a difference? Behavior modification. 1998;22(1):45–61. doi: 10.1177/01454455980221003. [DOI] [PubMed] [Google Scholar]
- Zhou X., Snoswell C.L., Harding L.E., Bambling M., Edirippulige S., Bai X., et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemedicine Journal and E-Health: The Official Journal of the American Telemedicine Association. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- Zysberg L., Zisberg A. Days of worry: Emotional intelligence and social support mediate worry in the COVID-19 pandemic. Journal of health psychology. 2020 doi: 10.1177/1359105320949935. (1359105320949935. Advance online publication) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, C.C., upon reasonable request.