Abstract
Introduction
Supported self-management empowering people with asthma to detect early deterioration and take timely action reduces the risk of asthma attacks. Smartphones and smart monitoring devices coupled with machine learning could enhance self-management by predicting asthma attacks and providing tailored feedback.
We aim to develop and assess the feasibility of an asthma attack predictor system based on data collected from a range of smart devices.
Methods and analysis
A two-phase, 7-month observational study to collect data about asthma status using three smart monitoring devices, and daily symptom questionnaires. We will recruit up to 100 people via social media and from a severe asthma clinic, who are at risk of attacks and who use a pressurised metered dose relief inhaler (that fits the smart inhaler device).
Following a preliminary month of daily symptom questionnaires, 30 participants able to comply with regular monitoring will complete 6 months of using smart devices (smart peak flow meter, smart inhaler and smartwatch) and daily questionnaires to monitor asthma status. The feasibility of this monitoring will be measured by the percentage of task completion. The occurrence of asthma attacks (definition: American Thoracic Society/European Respiratory Society Task Force 2009) will be detected by self-reported use (or increased use) of oral corticosteroids. Monitoring data will be analysed to identify predictors of asthma attacks. At the end of the monitoring, we will assess users’ perspectives on acceptability and utility of the system with an exit questionnaire.
Ethics and dissemination
Ethics approval was provided by the East of England - Cambridge Central Research Ethics Committee. IRAS project ID: 285 505 with governance approval from ACCORD (Academic and Clinical Central Office for Research and Development), project number: AC20145. The study sponsor is ACCORD, the University of Edinburgh.
Results will be reported through peer-reviewed publications, abstracts and conference posters. Public dissemination will be centred around blogs and social media from the Asthma UK network and shared with study participants.
Keywords: Asthma, Health informatics, Information technology, World Wide Web technology
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study combines objective data collected from multiple smart monitoring devices available on the market.
Stratified analysis and individualised asthma attack prediction models are not expected, due to the limited number of participants and study period.
Participants are limited to patients with severe asthma at risk of acute attacks, and to those using a pressurised metered dose relief inhaler that fits our smart device.
Introduction
Asthma is a variable condition, affecting around 5.4 million people in the UK.1 Every 10 s in the UK alone, someone has an asthma attack. Some of these attacks are life-threatening with over 1400 annual deaths estimated in the UK.1 2 Since there is no known cure for asthma, self-management is a key part of patient care; this involves detecting deterioration and taking appropriate action to maintain control and prevent the threatened attack.3 The most common symptoms of asthma are wheezing, cough, chest tightness and shortness of breath.
Traditional self-management action plans use symptom scores, sometimes supplemented by peak flow measurements, to determine a patient’s asthma condition.4–6 Keeping track of relief inhaler usage can also help measure asthma control.7 However, patients may regard this level of monitoring as tedious as it involves high levels of active engagement on their part.
Increasingly, smart monitoring devices and ‘mobile-health’ (mHealth) technologies are being developed to support asthma self-management.8 Some notable examples include myAsthma9 and Asthma MD.10 myAsthma stores personalised action plans, includes instructional videos about inhaler techniques, tracks symptoms and peak flow, and provides local weather forecasts. AsthmaMD10 has similar features to support self-management and can provide customised notifications. However, these tools still require a high level to active engagement to monitor one’s asthma.
There has been an increasing number of mHealth studies to predict asthma attacks and develop passive monitoring to support asthma self-management,11 including the use of smart peak flow meters,12 night-time activity tracking,13 14 smart inhalers,15 smartphone-administrated questionnaires6 16 17 and weather data.18 19 However, the combined use of the monitoring devices available to asthma patients to develop asthma attack prediction models is largely unexplored. In addition, while there have been some studies that explored the use of machine learning algorithms for chronic disease management with home-monitoring data,20 there is still no mHealth system that is widely used by asthma patients. One of the key bottlenecks for the limited progress is the difficulty of collecting asthma monitoring data and the lack of availability of such datasets from existing studies. Apart from the Asthma Mobile Health Study,21 no other asthma mHealth dataset is publicly available to be able to investigate the development and validation of asthma attack prediction algorithm.
A related study is the myAirCoach study,22 which investigated asthma home-monitoring using connected devices. However, their participants conducted daily monitoring for the first month with an additional randomly allocated 2 weeks, compared with 7 months in total proposed in this study. To our knowledge, the dataset from myAirCoach is not publicly available and it has not yet been used to test any machine learning-based algorithms for asthma attack prediction.23 24
In this study, we will collect novel asthma monitoring data that will facilitate the development of an asthma attack prediction algorithm leveraging available, approved asthma monitoring devices in the market. This study will also enable us to test whether unobtrusive, passive monitoring and machine learning could help minimise the need for active patient data collection while maintaining accuracy for predicting attacks. We envisage that an mHealth system that leverages machine learning to predict asthma attacks with passive monitoring will enhance patient adherence and improve patient self-management.
The overarching aim of this study is to develop and assess the feasibility and acceptability of an asthma self-management system using existing smart devices, collect novel monitoring data and leverage machine learning to explore the feasibility of an asthma attack prediction algorithm based on passive monitoring.
Methods and analysis
Study population
To maximise the chances of collecting data related to attacks in a short time-span, we will focus on patients with moderate to severe risk of attacks. Two key predictors are a recent history of attacks and people with severe asthma.25 26 We will thus focus on adult asthma patients who have had at least one course of oral corticosteroid for an acute asthma attack in the past 12 months, and people attending a secondary care severe asthma clinic. See table 1 for inclusion and exclusion criteria.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria: |
|
| Exclusion criteria: |
|
Social media recruitment consists of sending tweets on Twitter and posting on Facebook via the Asthma+Lung UK and Asthma UK Centre for Applied Research (AUKCAR) accounts, which total around 175 000 followers. The Norfolk and Norwich University Hospital will help identify potentially eligible patients for the study and direct them to the online information and expression of interest.
Potential participants will complete an online questionnaire to identify whether they are eligible to participate. Informed consent will be collected via online surveys, a secure online platform for collecting questionnaire data. Potential participants will be given time to read the participant information sheet before deciding whether to participate.
Sample size calculation
To achieve the objectives of this study, we need to collect sufficient data need to train an asthma attack prediction model.
In the study population of UK Optimum Patient Care Research Database and Clinical Practice Research Datalink, 41% of the patients who had multiple (two or more) attacks in the baseline year also had multiple attacks in the following year.26
Based on 30 participants with daily monitoring, 3098 recordings (= 30 people×30 days × (85% retention at baseline,27–29 50% retention at 6 months27 28 30 31) × 85% adherence29 30) for each of the daily measurements can be expected in phase 2. Also, 12 recorded asthma attacks are expected, assuming an average of one attack observed per participant in 41% of phase 2 participants during the study period.26 To use the novelty detection algorithm iForest (which can be trained even if the data collected does not include any attacks), a sample of 256 recordings or data points would suffice.32 Other machine learning classification algorithms will also obtain high accuracy on this sample size.
Recruitment strategy
Using a similar recruitment method, Hui et al recruited 87 participants using social media alone, the majority within the first month after the initial invitational message, although the number of those who continued to use the app dropped to 15 (17% of the total initially recruited participants) after 30 days.27 Moreover, only 5% of identified participants through practices agreed to join their study, which totalled 28 participants from five practices.27 However, the attrition rate for participants recruited through practices was lower, 63% vs 83% reduction in social media participants; only 25% of users were still using the app after 30 days.27 The eligibility criteria (≥16 years, an asthma prescription in the previous year, registered with a UK general practitioner (GP)) is more relaxed than the proposed criteria. However, this study incentivises entry of data in the first 28 days by giving adherent participants access to phase 2 (where participants are sent smart devices) which is likely to result in much more than 25% passing 30 days of participation. The adherence to 4 weeks of monitoring with daily questionnaires and activity monitors has seen values upwards of 95%.29
Following the previous research, which recruited participants through Asthma UK’s social media (at the time of writing had 175 000 followers), around 87 participants are expected to be eligible and join this study. In addition, around six participants identified and invited via are expected to be eligible and join from Norfolk and Norwich University Hospital. Of which, 47 people (50% of 93 respondents) are expected to complete phase 1. Thus, including 30 participants is achievable using the outlined recruitment method.
Outcomes
Primary endpoints
The primary endpoints of this study are adherence to monitoring, which are defined by the collection of data using different devices. For each task, we will measure the percentage of total days completed.
Secondary endpoints
The secondary endpoints of this study are asthma attacks. Primarily, we use severe asthma attacks as defined in the American Thoracic Society (ATS)/European Respiratory Society (ERS) Task Force 2009 statement.33 The definition is as follows:
Severe asthma attacks are events that require urgent action on the part of the patient and physician to prevent a serious outcome. Such attacks are defined as a deterioration requiring use of systemic corticosteroids (or an increase from a stable maintenance dose).33
Severe asthma attacks will be identified using the use of systemic corticosteroids question on the weekly self-reported questionnaire. Courses of corticosteroids separated by 1 week or more will be treated as separate severe attacks.
We will also explore the use of moderate asthma attacks, as defined in the ATS/ERS Task Force 2009 statement.33 The definition is as follows:
A moderate asthma attack is an event that, when recognised, should result in a temporary change in treatment to prevent the attack from becoming severe. Such attacks are defined as a deterioration that does not require use of systemic corticosteroids.33 Moderate asthma attacks include a deterioration in symptoms, lung function and/or increased rescue bronchodilator use that lasts for 2 days or more but are not severe enough to warrant systemic corticosteroid use.
Moderate asthma attacks will be identified using the questions about relief inhaler usage, symptoms (day symptoms, nocturnal symptoms, interference with usual activities, shortness of breath, wheezing), and unscheduled care (GP, emergency room and hospitalisations) in the daily and weekly self-reported questionnaires.
Data collection
The data collection period is split into two phases:
Questionnaire monitoring, daily for 1 month.
Smart device and questionnaire monitoring, daily for 6 months. 30 participants who keep a regular diary in phase one will be given three smart devices (smart inhaler, smart peak flow meter, smartwatch) to collect data automatically as they use the devices, in addition to completing daily and weekly questionnaires. We will choose participants for this phase with a range of ages, gender, and smoking status, and with different types of asthma triggers.
At the end of phase 2, we will send a questionnaire asking for feedback about using the smart devices and whether participants think they could be useful to help them look after their asthma.
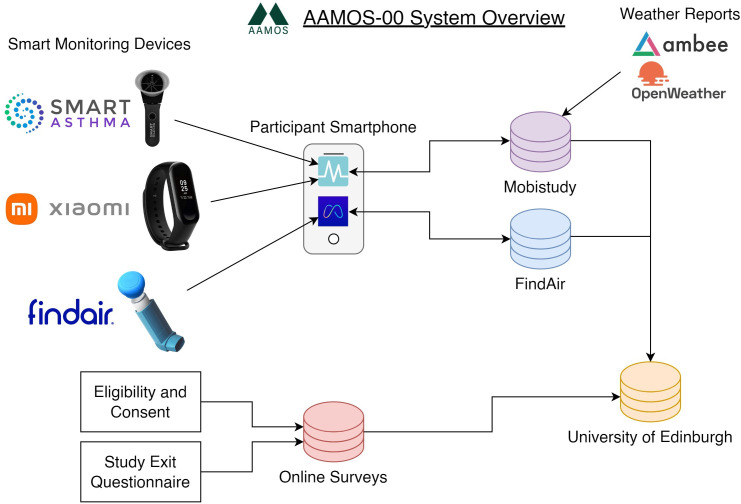
We will be using Mobistudy to centralise most of the data collection, only the smart inhaler usage and exit questionnaire will not be collected via Mobistudy (see figure 1).
Figure 1.
AAMOS-00 system overview. AAMOS, Asthma Attack Management Online System.
Data collection mobile app (Mobistudy)
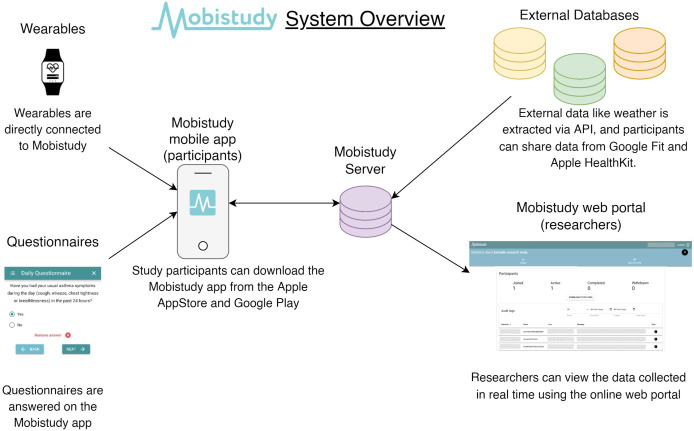
Mobistudy34 is an open-source platform facilitating mHealth studies available on Android and iOS managed by Malmö University, Sweden. The platform has three key components: a mobile app for participants, a REST Application Programming Interface (API) server, and a web portal for researchers (see figure 2). The platform supports multiple studies and participants of the Asthma Attack Management Online System (AAMOS-00) study will be given a study invite code to join the AAMOS-00 study within Mobistudy.
Figure 2.
Mobistudy system overview. API, Application Programming Interface.
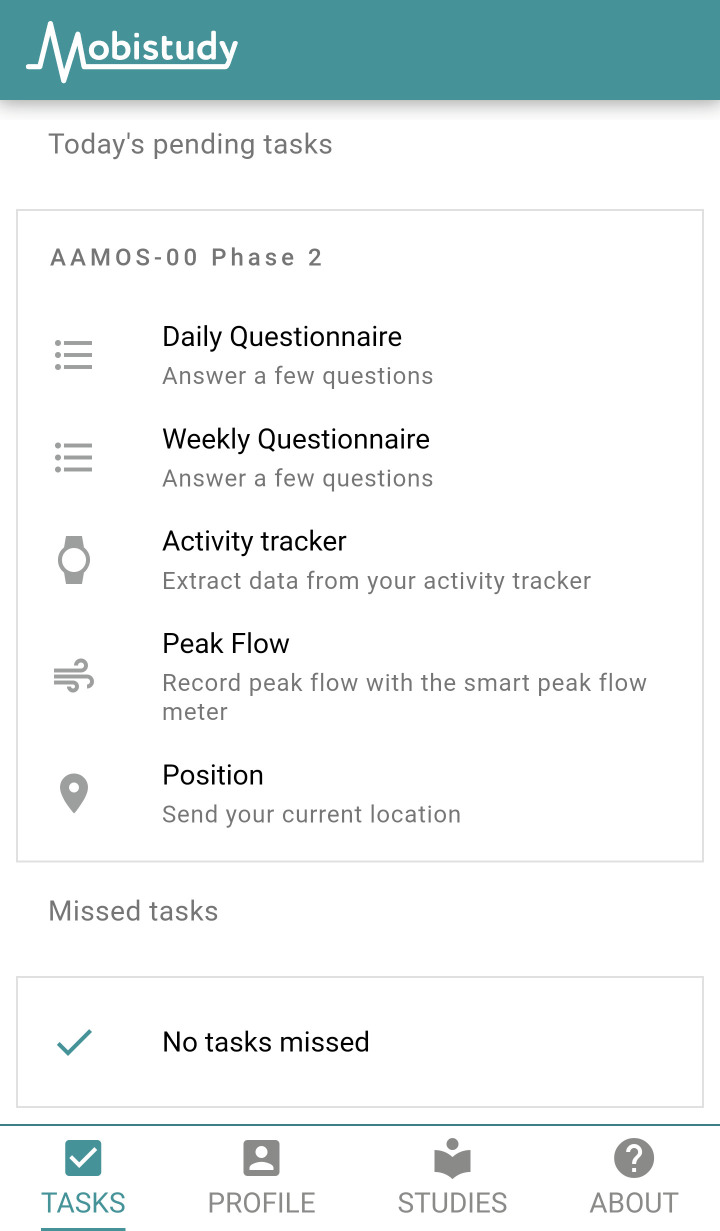
Each daily and weekly assessment, such as questionnaires and peak flow measurement, will appear as an individual task of the home page on the participant’s app (see figure 3). Once the task is completed, it will be removed from today’s to-do list and the data is sent directly to the server via the phone internet connection. In real time, the research team will be able to view the collected data via the online web portal for researchers.
Figure 3.
Participant’s app home page. AAMOS, Asthma Attack Management Online System.
Phase 1
There will be a total of four questionnaires:
A daily questionnaire that asks six questions about daily symptoms experienced, medication usage and the triggers encountered. This will take around 2 min to complete.
A weekly questionnaire that asks 10 questions about asthma symptoms in more detail, medication usage and healthcare engagement. This will take around 5 min to complete.
A questionnaire that asks 11 questions at the start of phase 1 about current asthma condition and history.
A questionnaire that asks five questions about race and smoking status. Additionally, some demographic information will be collected from the Mobistudy profile of participants, such as height, weight and age.
The completion rate (50%) of the daily and weekly questionnaire will be used to determine the eligibility of a participant to join phase 2.
Phase 2
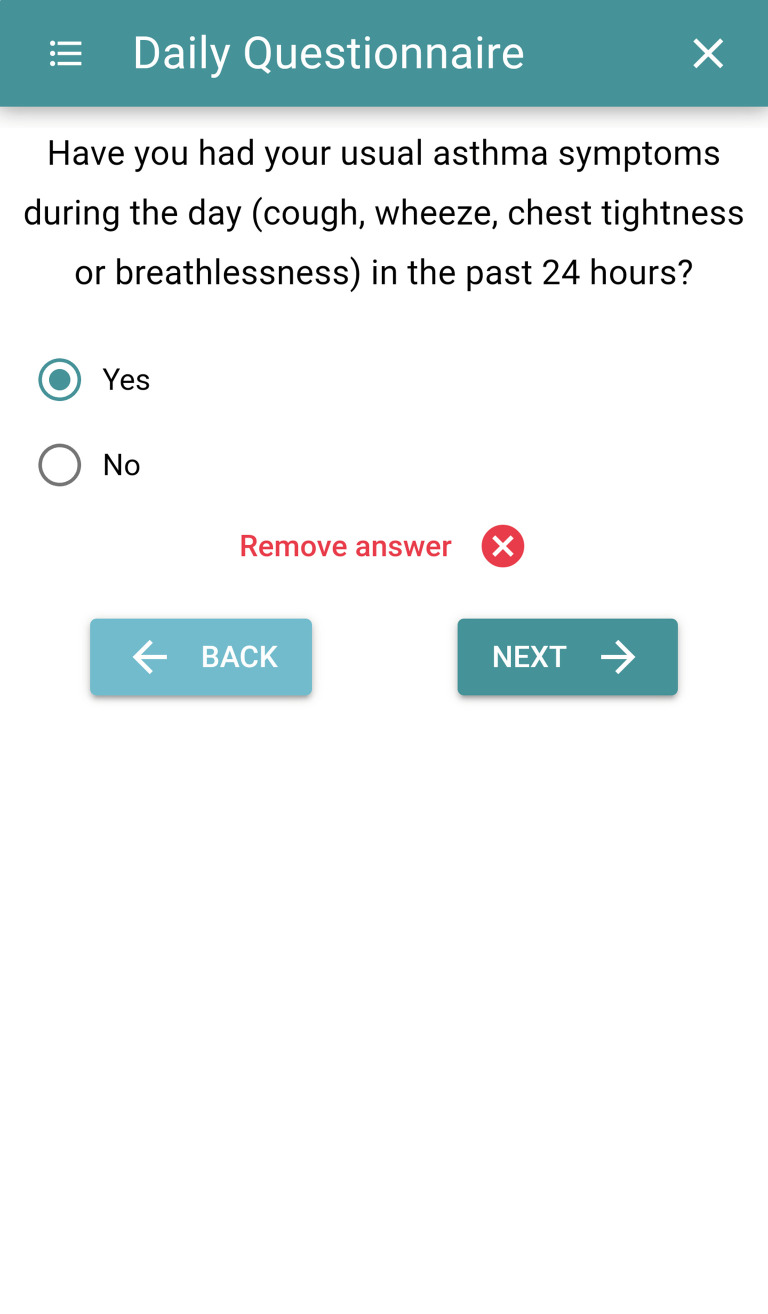
In addition to the daily and weekly questionnaires (see figure 4), in phase 2 participants will be asked to collect data using three smart monitoring devices: Smart Peak Flow Meter (by Smart Asthma35), FindAir ONE (by FindAir36) smart inhaler and MiBand3 (by Xiaomi37) smartwatch.
Figure 4.
Questionnaire delivered by Mobistudy.
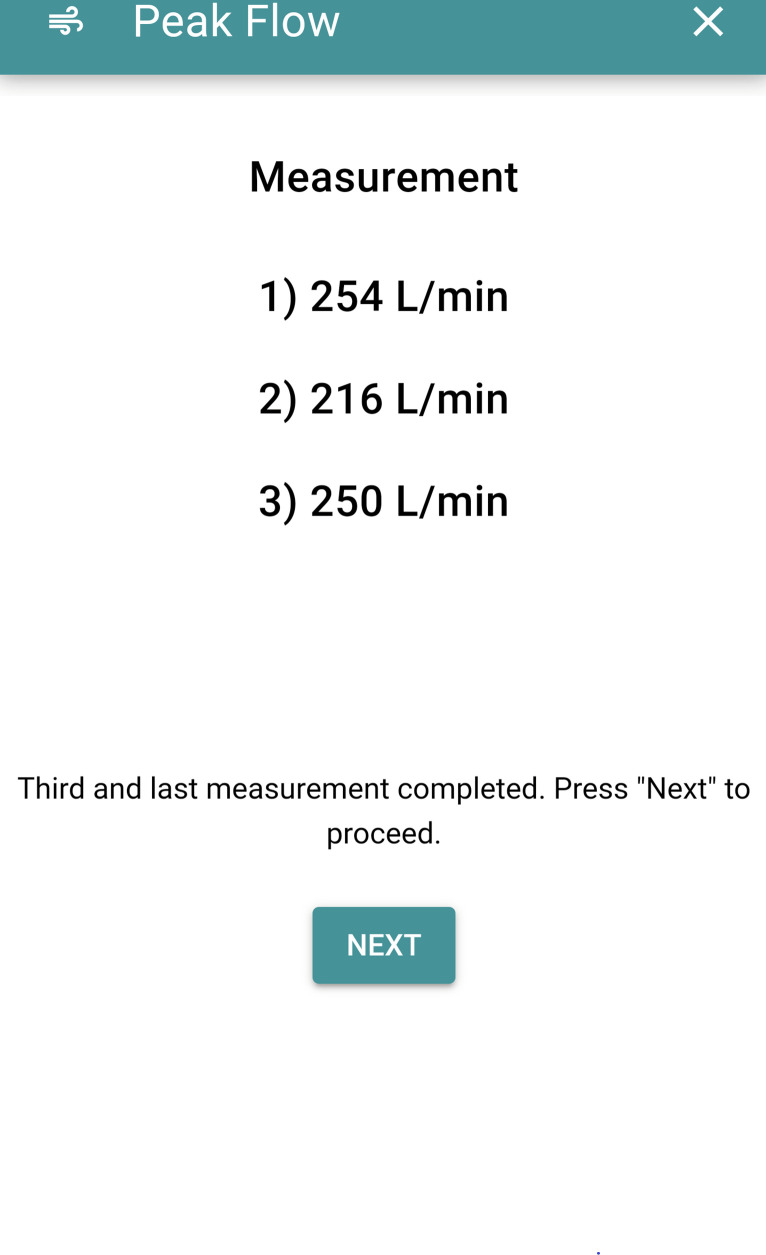
Participants will be given the smart peak flow meter to take a peak expiratory flow measurement twice a day, once in the morning and once at night; each measurement takes the best of three tries (see figure 5). They will also be provided in-app written instructions before each set of measurements on using the peak flow meter. Furthermore, participants recruited through the Norfolk and Norwich University Hospital have been trained to use a peak flow meter by the practice. To connect the smart peak flow meter to the smartphone, participants can either use the audio-jack connection or a bluetooth adapter.
Figure 5.
Smart peak flow meter task.
The FindAir ONE smart inhaler attaches to the top of pressurised metered dose relief inhalers, it records the time at which the inhaler is used. The device can be moved to a new inhaler if participants change medication. The device will be connected to participants’ smartphone by Bluetooth to the FindAir mobile app. The data will be transferred from the FindAir server and thence to the research team using FindAir’s API. The data collection will happen in the background once the participant has set up the connection between their mobile app and the AAMOS-00 study.
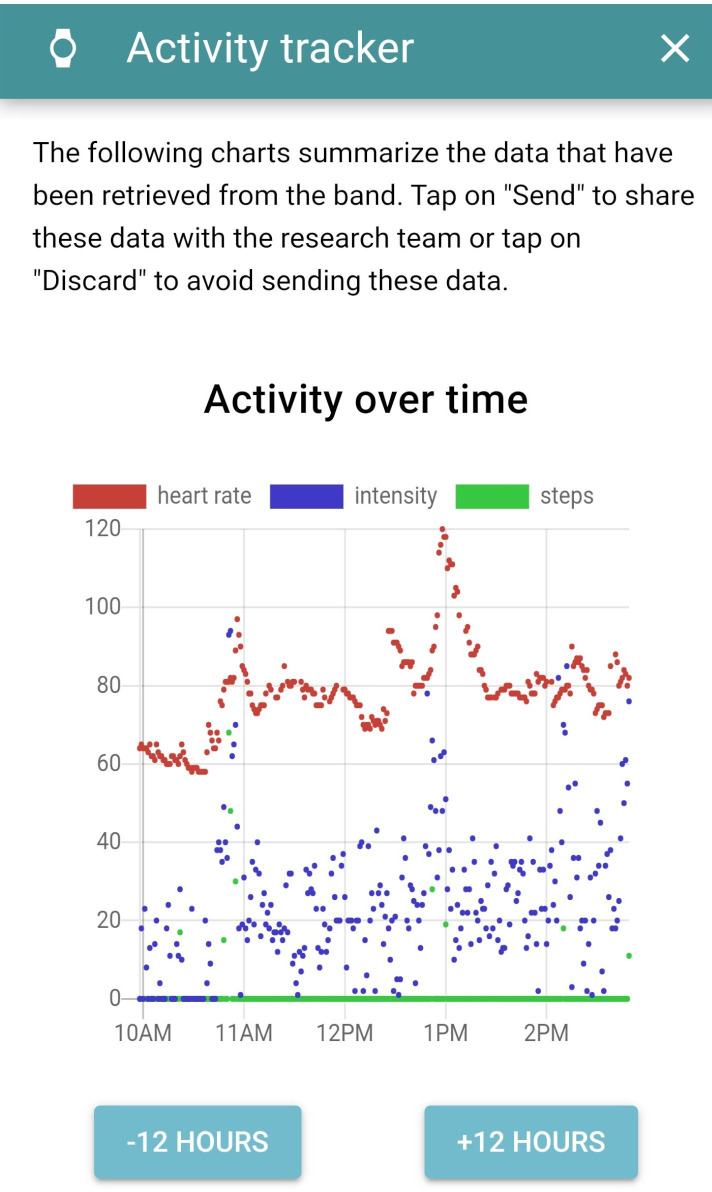
Using the MiBand3, we will collect minute-by-minute data on heart rate, step count, activity intensity and activity type. The watch will connect to the participant’s smartphone via Bluetooth and to the Mobistudy app. Participants will be asked to upload the data from the watch at least once every 3 days. This also gives a chance for users to review their activity (see figure 6).
Figure 6.
Smartwatch data.
Local daily weather reports will be obtained using the phone’s location combined with the data from Open Weather Maps’38 and Ambee’s39 API. The weather data will include the temperature, humidity, clouds, wind, air quality index and pollen levels of grass, tree and weeds measured at a 1 km resolution (see figure 7).
Figure 7.
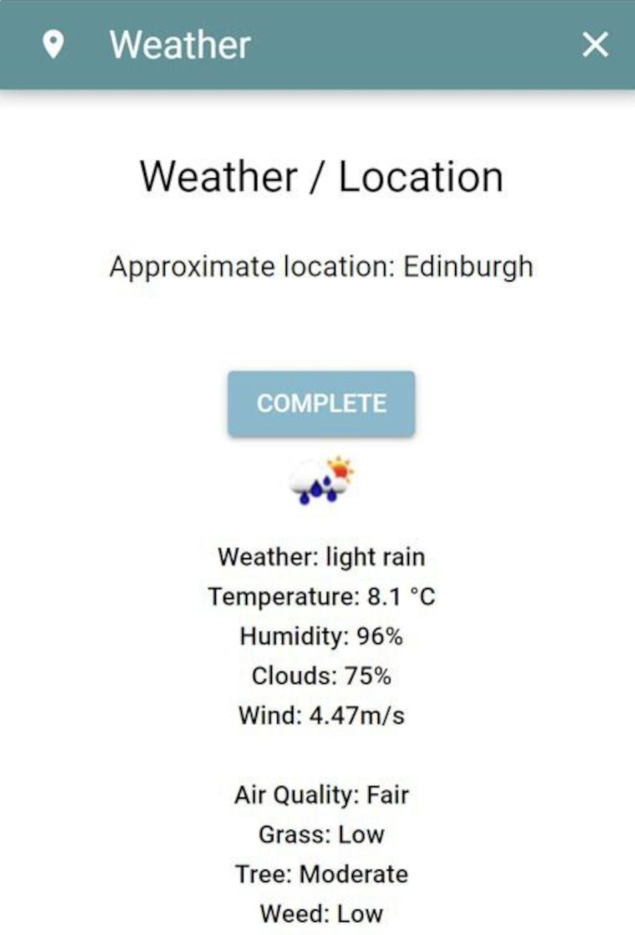
Local weather data.
Exit questionnaire at the end of phase 2
At the end of phase 2, a survey will gather data regarding users’ perspective of the acceptability and utility of the monitoring system. The survey combines validated questionnaires on usability and acceptance (SUS40 and uMARS41) with questions about motivations to use technology (mTEI42) and desired features in an asthma management system.
See table 2 for a summary of the study’s activities.
Table 2.
Summary of data collection
| Assessment | Screening | Day 1 baseline | Phase 1 | Day 31 baseline | Phase 2 | Study exit |
| Assessment of eligibility criteria | Once | Once | ||||
| Written informed consent | Once | |||||
| Demographic data, contact details | Once | |||||
| Weight/height | Once | |||||
| Known triggers | Once | |||||
| Peak flow | Twice daily | |||||
| Heart rate | Automated | |||||
| Activity | Automated | |||||
| Location, air quality and allergens | Daily | |||||
| Inhaler usage | Daily and weekly | Automated | ||||
| Symptoms | Daily and weekly | Daily | ||||
| Triggers encountered | Daily | Daily | ||||
| Healthcare usage | Weekly | Weekly | ||||
| Feedback | Once at the end |
At the end of the study, participants will be compensated for mobile data charges that may have incurred from participating in the study, £5 per month. Participants are also able to continue using the smart devices beyond the study.
Following ethics approval in December 2020, we aim to complete the study by June 2023.
Data analysis plan
Feasibility (from usage data)
Combining the usage data from phase 1 and 2 of questionnaire completion and device usage will compute compliance to the monitoring regime to assess if it is feasible for patients to use the monitoring devices in their daily lives.
We will also use activity logs on the server, and communication over email with patients, to identify major technical issues and shortcomings of the technology.
Acceptability (from survey data)
The data from the final questionnaire will be mostly ordinal data, with some free-text answers. Free text will be processed for thematic text analysis, identifying overall acceptability and recurring topics present in the feedback. The ordinal data from answers on a Likert scale will provide measures of acceptability.
Exploring asthma attack prediction (using monitoring data)
Severe asthma attacks will be identified by the reports of oral corticosteroid usage (or an increased dose from normal). Moderate and severe asthma attacks will be identified from the daily and weekly data, to observe a change in control from the norm lasting 2 days or more. Sensitivity analysis will be conducted using different features to define an asthma attack, such as hospitalisations and changes in peak flow. Data collected from participants who have withdrawn from the study will be used up to the last recording.
The methods of linear fit and bin-algorithms will be used to collate and produce summary variables over irregular time series and to handle missing data.6 After processing the data, machine learning classifiers will be trained to predict asthma attacks. Evaluation of these classifiers will allow comparison with the benchmarks set using daily questionnaires alone.6 However, due to the selection of participants with higher adherence to monitoring in phase 2 of this AAMOS-00 study, the longitudinal data collected in this study are likely to be more complete than the data collected by the wide range of participants in the Asthma Mobile Health Study.43
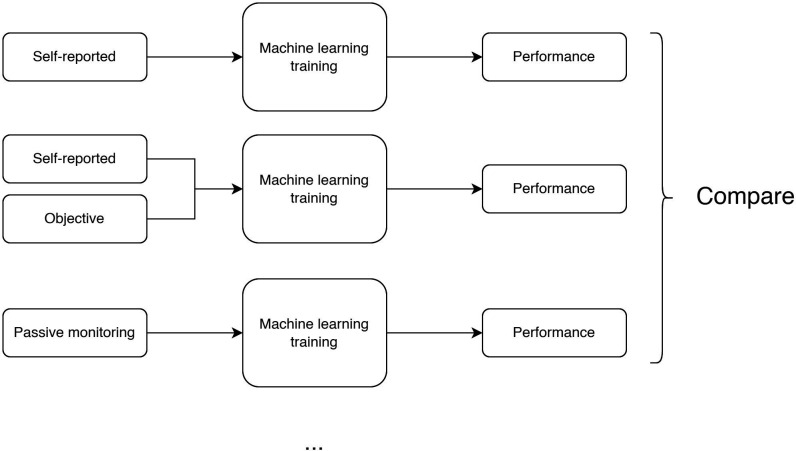
Using different subsets of the data and features, we will test the performance of predictions made using different modes of monitoring, such as self-reported data alone, self-reported and objective data (active and passive monitoring), and passive monitoring data only (see figure 8). Our previous analysis using only self-reported data achieved area under the curve (AUC) >0.87 and we expect the performance to increase with the addition of objective data.6
Figure 8.
Exploring asthma attack prediction.
There is no consensus on the optimal algorithm for classification as previous studies are not comparable.11 Therefore, we have taken a broad approach to use five state-of-the-art algorithm classes including Bayesian networks, decision trees, iForest, logistic regression and support vector machines.44 45 From the classifiers, a severe asthma attack predictor will be built on the device and questionnaire data, at a patient level and population level. Also, feature selection will be used to identify the most useful features in the prediction models.
Furthermore, if there are sufficient data, retrospective analysis will simulate the effects of limiting the use of active monitoring data, to simulate patients only taking active measurements (eg, peak flow and symptom diary) when prompted. Moreover, there will be simulation of the general population using samples of the data, where adherence to monitoring is lower than the select population. For assessing the performance of the models built in this study, we will use k-fold cross validation.44 The performance metrics will include the common machine learning metrics such as AUC the receiver operating characteristic curve, sensitivity and specificity.
Strengths and limitations
This study combines objective data collected from multiple smart monitoring devices available on the market. Not only will this independently test the monitoring devices in the real world, but also patients will be able to continue using the devices they have found useful beyond the study. It also allows other researchers to reproduce the study with the current or latest versions of the devices.
Due to the limited number of participants and study period, stratified analysis and individualised asthma attack prediction models are not expected. However, 7 months of daily monitoring per participant will provide insightful data.
This study is limited to patients with severe asthma at risk of acute attacks, and the findings may not generalise to the wider asthma population. Furthermore, only participants using a pressurised metered dose relief inhaler that fits our smart device are able to join the study, which is around 80% of the UK’s asthma population.46 If there are sufficient data, we will explore the generalisability of the results through simulating different adherence to monitoring.
The anonymised research data will be stored at Edinburgh DataShare (a digital repository of research data produced at the University of Edinburgh),47 which researchers can access for their own research.
Patient and public involvement
Patient and public involvement (PPI) is part of the project from the beginning. This study is nested within the Asthma AUKCAR and has been reviewed by their AUKCAR PPI members.
All the participant and public-facing documents and study objectives have been reviewed by AUKCAR PPI members before the start of the study and edited accordingly. Such a close PPI involvement ensures that the participant and public facing material is accessible. As an example, we attempted to explain several technical terms (such as ‘pMDI’) in more detail in the participant documents and added pictures of pressured metered dose inhalers after feedback from PPI members.
The findings about feasibility and acceptability will be interpreted with input from PPI members. Furthermore, we plan to continue working with PPI members to develop a system that supports asthma self-management.
Dissemination
We will be reporting the results in peer-reviewed journal publications and conference presentations. Dissemination of the results will also include the AUKCAR network with blogs and social media to reach an audience who is interested in the used of smart monitoring devices for asthma.
We will also be sharing links to publications and summaries with study participants.
Ethics
This study has received ethics approval by the East of England - Cambridge Central Research Ethics Committee. IRAS Project ID: 285 505.
Data availability
At the end of the study, the anonymised research data will be stored at Edinburgh DataShare (a digital repository of research data produced at the University of Edinburgh) in perpetuity. Researchers will be able to access and download the data from the website for their own research.
Conclusions
This study will collect an important and novel dataset, where asthma patients use a combination of multiple market-available mHealth monitoring devices in the real world. We plan to use the rich dataset to improve existing asthma attack prediction algorithms and use the feedback from participants to design a patient-centred asthma self-management system. This study is the first step in developing the Asthma Attack Management Online System (AAMOS), which will support asthma patients with real-time tailored feedback based on machine learning driven by mHealth data.
Supplementary Material
Acknowledgments
We thank the AUKCAR PPI for their comments on the study. We thank Malmö University for their support with data collection. We thank Smart Respiratory Products Ltd for providing the Smart Peak Flow Meter and associated software. We thank FindAir for providing the FindAir ONE devices and FindAir's API. We thank Ambee for providing the pollen data. We thank Dr Sarah Brown (Edinburgh Innovations, University of Edinburgh, UK) for organising the contracts required for the study.
Footnotes
Contributors: KCHT, HP, AMW and SAS designed the study. SAS is the study guarantor. KCHT and DS set up the data collection system. KCHT drafted the manuscript which was critically revised by HP, AMW, DS and SAS. All authors approved the final version of the manuscript.
Funding: This work was supported by Asthma + Lung UK as part of the Asthma UK Centre for Applied Research grant number AUK-AC-2018-01. Support from Malmö University is co-funded by the Knowledge Foundation KK-stiftelsen.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Asthma UK. Asthma facts and statistics. Available: https://www.asthma.org.uk/about/media/facts-and-statistics/ [Accessed 01 Mar 2021].
- 2.Iacobucci G. Asthma deaths rise 33% in past decade in England and Wales. BMJ 2019;366:l5108. 10.1136/bmj.l5108 [DOI] [PubMed] [Google Scholar]
- 3.Pinnock H, Parke HL, Panagioti M, et al. Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Med 2017;15:64. 10.1186/s12916-017-0823-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scottish Intercollegiate Guidelines Network/ British Thoracic Society . SIGN 158 British guideline on the management of asthma. London/Edinburgh: BTS/SIGN, 2019
- 5.Juniper EF, O'Byrne PM, Guyatt GH, et al. Development and validation of a questionnaire to measure asthma control. Eur Respir J 1999;14:902–7. 10.1034/j.1399-3003.1999.14d29.x [DOI] [PubMed] [Google Scholar]
- 6.Tsang KCH, Pinnock H, Wilson AM, et al. Application of machine learning to support self-management of asthma with mHealth. Annu Int Conf IEEE Eng Med Biol Soc 2020;2020:5673–7. 10.1109/EMBC44109.2020.9175679 [DOI] [PubMed] [Google Scholar]
- 7.Su JG, Barrett MA, Henderson K, et al. Feasibility of deploying inhaler sensors to identify the impacts of environmental triggers and built environment factors on asthma short-acting bronchodilator use. Environ Health Perspect 2017;125:254–61. 10.1289/EHP266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tinschert P, Jakob R, Barata F, et al. The potential of mobile Apps for improving asthma self-management: a review of publicly available and Well-Adopted asthma Apps. JMIR Mhealth Uhealth 2017;5:e113. 10.2196/mhealth.7177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MyAsthma . The asthma APP for managing your symptoms. Available: https://mymhealth.com/myasthma [Accessed 10 Mar 2021].
- 10.AsthmaMD . Asthma control iPhone APP | AsthmaMD. Available: https://www.asthmamd.org/ [Accessed 10 Mar 2021].
- 11.Tsang KCH, Pinnock H, Wilson AM, et al. Application of machine learning algorithms for asthma management with mHealth: a clinical review. J Asthma Allergy 2022;15:855–73. 10.2147/JAA.S285742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finkelstein J, Jeong IC, cheol JI. Machine learning approaches to personalize early prediction of asthma exacerbations. Ann N Y Acad Sci 2017;1387:153–65. 10.1111/nyas.13218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Castner J, Jungquist CR, Mammen MJ, et al. Prediction model development of women's daily asthma control using fitness tracker sleep disruption. Heart Lung 2020;49:548–55. 10.1016/j.hrtlng.2020.01.013 [DOI] [PubMed] [Google Scholar]
- 14.Huffaker MF, Carchia M, Harris BU, et al. Passive nocturnal physiologic monitoring enables early detection of exacerbations in children with asthma. A proof-of-concept study. Am J Respir Crit Care Med 2018;198:320–8. 10.1164/rccm.201712-2606OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tibble H, Chan A, Mitchell EA, et al. A data-driven typology of asthma medication adherence using cluster analysis. Sci Rep 2020;10:14999. 10.1038/s41598-020-72060-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tinschert P, Rassouli F, Barata F, et al. Nocturnal cough and sleep quality to assess asthma control and predict attacks. J Asthma Allergy 2020;13:669–78. 10.2147/JAA.S278155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang O, Minku LL, Gonem S. Detecting asthma exacerbations using daily home monitoring and machine learning. J Asthma 2021;58:1518–27. 10.1080/02770903.2020.1802746 [DOI] [PubMed] [Google Scholar]
- 18.Khasha R, Sepehri MM, Mahdaviani SA. An ensemble learning method for asthma control level detection with Leveraging medical knowledge-based classifier and supervised learning. J Med Syst 2019;43:158. 10.1007/s10916-019-1259-8 [DOI] [PubMed] [Google Scholar]
- 19.Alharbi E, Abdullah M. Asthma attack prediction based on weather factors. PEN 2019;7:408–19. 10.21533/pen.v7i1.422 [DOI] [Google Scholar]
- 20.Exarchos KP, Beltsiou M, Votti C-A, et al. Artificial intelligence techniques in asthma: a systematic review and critical appraisal of the existing literature. Eur Respir J 2020;56. doi: 10.1183/13993003.00521-2020. [Epub ahead of print: 03 09 2020]. [DOI] [PubMed] [Google Scholar]
- 21.Chan Y-FY, Wang P, Rogers L, et al. The asthma mobile health study, a large-scale clinical observational study using ResearchKit. Nat Biotechnol 2017;35:354–62. 10.1038/nbt.3826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Honkoop PJ, Simpson A, Bonini M, et al. MyAirCoach: the use of home-monitoring and mHealth systems to predict deterioration in asthma control and the occurrence of asthma exacerbations; study protocol of an observational study. BMJ Open 2017;7:e013935. 10.1136/bmjopen-2016-013935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khusial RJ, Honkoop PJ, Usmani O, et al. Effectiveness of myAirCoach: a mHealth self-management system in asthma. J Allergy Clin Immunol Pract 2020;8:1972–9. 10.1016/j.jaip.2020.02.018 [DOI] [PubMed] [Google Scholar]
- 24.myAirCoach . D7.6 data management plan (second year update), 2016. Available: https://www.myaircoach.eu/content/d76-data-management-plan-second-year-update [Accessed 20 Aug 2022].
- 25.Blakey JD, Price DB, Pizzichini E, et al. Identifying risk of future asthma attacks using UK medical record data: a respiratory effectiveness group initiative. J Allergy Clin Immunol Pract 2017;5:1015–24. 10.1016/j.jaip.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 26.Price D, Wilson AM, Chisholm A, et al. Predicting frequent asthma exacerbations using blood eosinophil count and other patient data routinely available in clinical practice. J Asthma Allergy 2016;9:1–12. 10.2147/JAA.S97973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hui CY, McKinstry B, Walton R, et al. A mixed method observational study of strategies to promote adoption and usage of an application to support asthma self-management. J Innov Health Inform 2019;25:243–53. 10.14236/jhi.v25i4.1056 [DOI] [PubMed] [Google Scholar]
- 28.Pathiravasan CH, Zhang Y, Trinquart L, et al. Adherence of mobile App-Based surveys and comparison with traditional surveys: eCohort study. J Med Internet Res 2021;23:e24773. 10.2196/24773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu X, Tupy S, Robertson S, et al. Successful adherence and retention to daily monitoring of physical activity: lessons learned. PLoS One 2018;13:e0199838. 10.1371/journal.pone.0199838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Senturia YD, McNiff Mortimer K, Baker D, et al. Successful techniques for retention of study participants in an inner-city population. Control Clin Trials 1998;19:544–54. 10.1016/S0197-2456(98)00032-4 [DOI] [PubMed] [Google Scholar]
- 31.Compernolle S, Vandelanotte C, Cardon G, et al. Effectiveness of a web-based, computer-tailored, pedometer-based physical activity intervention for adults: a cluster randomized controlled trial. J Med Internet Res 2015;17:e38. 10.2196/jmir.3402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu FT, Ting KM, Zhou Z-H. Isolation Forest. In: 2008 Eighth IEEE International Conference on Data Mining. IEEE 2008.:413–22. 10.1109/ICDM.2008.17 [DOI] [Google Scholar]
- 33.Reddel HK, Taylor DR, Bateman ED, et al. An official American thoracic Society/European respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009;180:59–99. 10.1164/rccm.200801-060ST [DOI] [PubMed] [Google Scholar]
- 34.Salvi D, Magnus Olsson C, Ymeri G. Mobistudy: mobile-based, platform-independent, multi-dimensional data collection for clinical studies.. In: 11th International Conference on the Internet of Things. St.Gallen, Switzerland ACM, 2021:219–22. [Google Scholar]
- 35.Smart Asthma . Available: https://smartasthma.com/ [Accessed 09 Mar 2022].
- 36.FindAir . Available: https://findair.eu/ [Accessed 09 Mar 2022].
- 37. Xiaomi UK. Available: https://www.mi.com/uk/ [Accessed 09 Mar 2022].
- 38.OpenWeatherMap . Available: https://openweathermap.org/ [Accessed 14 Jun 2021].
- 39.Ambee . Available: https://www.getambee.com/ [Accessed 14 Jun 2021].
- 40.Brooke J. SUS: A ‘Quick and Dirty’ Usability Scale. In: Usability Evaluation In Industry. CRC Press, 1996: 207–12. [Google Scholar]
- 41.Stoyanov SR, Hides L, Kavanagh DJ, et al. Development and validation of the user version of the mobile application rating scale (uMARS). JMIR Mhealth Uhealth 2016;4:e72. 10.2196/mhealth.5849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dewar AR, Bull TP, Malvey DM, et al. Developing a measure of engagement with telehealth systems: the mHealth technology engagement index. J Telemed Telecare 2017;23:248–55. 10.1177/1357633X16640958 [DOI] [PubMed] [Google Scholar]
- 43.Chan Y-FY, Bot BM, Zweig M, et al. The asthma mobile health study, smartphone data collected using ResearchKit. Sci Data 2018;5:180096. 10.1038/sdata.2018.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning. In: York N, Springer NY, eds. 2nd, 2009.
- 45.Bishop CM. Pattern recognition and machine learning. Berlin, Heidelberg: Springer, 2006. [Google Scholar]
- 46.Lavorini F, Corrigan CJ, Barnes PJ, et al. Retail sales of inhalation devices in European countries: so much for a global policy. Respir Med 2011;105:1099–103. 10.1016/j.rmed.2011.03.012 [DOI] [PubMed] [Google Scholar]
- 47.The University of Edinburgh. Edinburgh DataShare. Available: https://datashare.ed.ac.uk/ [Accessed 15 Aug 2022].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
At the end of the study, the anonymised research data will be stored at Edinburgh DataShare (a digital repository of research data produced at the University of Edinburgh) in perpetuity. Researchers will be able to access and download the data from the website for their own research.