Abstract
As of November 2021, several SARS‐CoV‐2 variants appeared and became dominant epidemic strains in many countries, including five variants of concern (VOCs) Alpha, Beta, Gamma, Delta, and Omicron defined by the World Health Organization during the COVID‐19 pandemic. As of August 2022, Omicron is classified into five main lineages, BA.1, BA.2, BA.3, BA.4, BA.5 and some sublineages (BA.1.1, BA.2.12.1, BA.2.11, BA.2.75, BA.4.6) (https://www.gisaid.org/). Compared to the previous VOCs (Alpha, Beta, Gamma, and Delta), all the Omicron lineages have the most highly mutations in the spike protein, and with 50 mutations accumulated throughout the genome. Early data indicated that Omicron BA.2 sublineage had higher infectivity and more immune escape than the early wild‐type (WT) strain, the previous VOCs, and BA.1. Recently, global surveillance data suggest a higher transmissibility of BA.4/BA.5 than BA.1, BA.1.1 and BA.2, and BA.4/BA.5 is becoming dominant strain in many countries globally.
Keywords: BA.2, BA.5, immune escape, SARS‐CoV‐2 Omicron variant, vaccine effectivity
1. INTRODUCTION
During the COVID‐19 epidemic, several SARS‐CoV‐2 variants 1 , 2 , 3 have emerged and SARS‐CoV‐2 variants continue to alter the trajectory of the COVID‐19 pandemic, 4 causing severe damage to human health and the medical system globally. 5 , 6 , 7 As of August 2, 2022, there have been 575 887 049 confirmed cases of COVID‐19 worldwide, including 6 398 412 deaths, reported to the World Health Organization (WHO) (https://covid19.who.int/).
At present, the WHO has designated five variants of concern (VOC), including Alpha (B.1.1.7), 1 Beta (B.1.351), 2 Gamma (P.1), 3 Delta (B.1.617.2), 8 and Omicron (B.1.1.529). 9 B.1.1.529 was first detected in specimens on November 11, 2021, in Botswana and on November 14, 2021, in South Africa. 9 On November 26, the WHO defined it as the fifth VOC and named it Omicron. Then, a variant of Omicron, the BA.1 lineage, rapidly spread worldwide and outcompeted other VOCs. Subsequently, another variant of Omicron, the BA.2 lineage, was identified in late 2021 in patients in countries including Denmark, South Africa, and India. 10 Notably, studies have shown that BA.2 may be ∼30% more transmissible than BA.1, but does not appear to cause more severe disease. 11 , 12 Since then, BA.2 has increased in many countries, and is more transmissible and possesses a selective advantage over BA.1. 13 , 14 The fourth COVID‐19 wave of South Africa was associated with BA.1 and BA.2. 15 , 16 , 17 In South Africa from April 2022, BA.4 and BA.5 have rapidly replaced BA.2 and initiated the fifth COVID‐19 wave, accounted for more than 50% of sequenced cases. 18 , 19 , 20 The current review article aims to analyse the characteristics of key spike mutations, epidemic characteristics, humoral and cellular immunity, and vaccine effectiveness of five Omicron lineages, especially Omicron BA.2, BA.4, and BA.5. We hope to provide a scientific reference for monitoring, control measures, and vaccine development strategies for the five main Omicron lineages.
1.1. Spike mutations of SARS‐CoV‐2 Omicron lineages
The earliest BA.2 sequence was uploaded from South Africa on November 27, 2021. 21 On December 7, the Omicron sublineage was detected in South Africa, and the Nextstrain defined it as 21 L, Omicron (21 L, BA.2). The Omicron (21 L, BA.2) spike protein contains 29 amino acid substitutions and one insertion (T19I, L24S, ins25PPA, D142D, V213G, G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, G446S, S477N, T478K, E484A, Q493R, Q498R, N501Y, Y505H, D614G, H655Y, N679K, P681H, N764K, D796Y, Q954H, N969K) (https://www.nicd.ac.za/diseases-a-z-index/disease-index-covid-19/sars-cov-2-genomic-surveillance-update/). There are 20 identical spike mutations (G142D, G339D, S373P, S375F, K417N, N440K, S477N, T478K, E484A, Q498R, N501Y, Y505H, D614G, H655Y, N679K, P681H, N764K, D796Y, Q954H, N969K) in all five Omicron lineages (BA.1, BA.2, BA.3, BA.4, and BA.5) and BA.1.1, BA.2.12.1 sublineage, 22 as shown in Figure 1 and Table 1.
Figure 1.
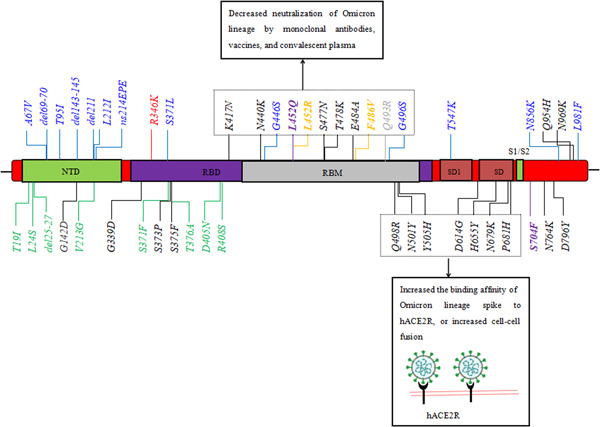
Spike mutations affect the biological behavior of five SARS‐CoV‐2 Omicron lineages. Blue, BA.1 has an additional six amino acid deletions, three insertions, and nine substitutions compared to BA.2; Red, BA.1.1 contains unique mutation R346K compared to BA.1; Green, BA.2 has eight specific mutations compared to BA.1, BA.1.1, BA.3, BA.4, and BA.5; Purple, BA.2.12.1 contains unique mutation L452Q + S704F compared to BA.2; Yellow, BA.4 and BA.5 have specific del69‐70, L452R, F486V, R493Q compared with BA.2; Black, all Omicron lineage have 20 identical spike mutations.
Table 1.
The characteristic of spike mutations of five SARS‐CoV‐2 Omicron lineages
| Pango lineage | Nextstrain | GISAID clade | Amino acid mutations in spike | Earliest document samples | Spread faster in some countries |
|---|---|---|---|---|---|
| BA.1 | 21K | GR/484A | A67V, del69‐70, T95I, G142D, del143‐145, del211, L212I, ins214EPE, G339D, S371L, S373P, S375F, K417N, N440K, G446S, S477N, T478K, E484A, Q493R, G496S, Q498R, N501Y, Y505H, T547K, D614G, H655Y, N679K, P681H, N764K, D796Y, N856K, Q954H, N969K, L981F (BA.1 + R346K, known as BA.1.1) |
BA.1: South Africa, November 2021; BA.1.1: South Africa, December 2021 |
BA.1 variant is the dominant strain in November (73%), December (94%), and January (55%) in South Africaa BA.1 dominated in January at 46.3% in the USA b BA.1 is become the dominant variant in the EU/EEA on the first 2 months of 2022. BA.1.1 dominated in February (73.9%) in the USA b |
| BA.2 | 21L | GRA | T19I, L24S, del25‐27, D142D, V213G, G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, S477N, T478K, E484A, Q493R, Q498R, N501Y, Y505H, D614G, H655Y, N679K, P681H, N764K, D796Y, Q954H, N969K (BA.2 + L452Q, S704F, known as BA.2.12.1) |
BA.2: South Africa, December 2021; BA.2.12.1: USA, December 2021 |
BA.2 dominated in February (86%) and March (78%) in South Africaa The sequence of BA.2 increased from 42.4% to 75.9% between March 13 and April 16, 2022 in the USA b The sequence of BA.2.12.1 increased from 24.1% to 59.1% between April 17 and May 28, 2022 in the USAb |
| BA.3 | 21M | GRA | A67V, del69‐70, T95I, G142D, del143‐145, del211, L212I, G339D, S371F, S373P, S375F, D405N, K417N, N440K, G446S, S477N, T478K, E484A, Q493R, Q498R, N501Y, Y505H, D614G, H655Y, N679K, P681H, N764K, D796Y, Q954H, N969K |
South Africa, November 2021; |
BA.3 continues to be detected at low levels and did not become the dominant epidemic lineages |
| BA.4 | 22A | GRA22A | T19I, L24S, del25‐27, del69‐70, D142D, V213G, G339D, S371F, S373P, S375F, T376A, D405N, R408S, K417N, N440K, G446S, L452R, S477N, T478K, E484A, F486V, Q498R, N501Y, Y505H,T547K D614G, H655Y, N679K, P681H, N764K, D796Y, Q954H, N969K |
South Africa, January 2022 |
BA.4 and BA.5 are together dominant in April (72%), May (92%), June (91%), July (93%) in South Africaa |
| BA.5 | 22B | GRA | BA.4 and BA.5 have identical spike proteins |
Both structural modeling and pseudovirus experiments indicated that receptor‐binding domian (RBD) with N440K, S477N, T478K, 23 E484A, Q493R, N501Y, 24 Q498R, 25 and Y505H mutations could increase the binding affinity and tightness of RBD to human angiotensin‐converting enzyme 2 (hACE2), thus increasing the infectivity of SARS‐CoV‐2 Omicron variants. It is worth noting that there are triple mutations “H655Y + N679K + P681H,” near the furin cleavage site of the Omicron lineages spike protein. 26 Previous studies indicated that “H655Y + N679K + P681H” might accelerate S1/S2 cleavage through furin protease and facilitate efficient viral entry into the host, leading to enhanced replication ability and viral infectivity. 27 Compared to the previous VOCs (Alpha, Beta, Gamma, Delta), Omicron and its lineages were the most highly mutated strains and contained at least 32 mutations in the spike protein, which was twice as many as the Delta variant (https://www.gisaid.org/). Omicron and its lineages had a higher positive electrostatic surface than previous VOCs, which could increase the binding affinity and tightness of RBD to negative electrostatic hACE2. However, some in silico analyses 28 , 29 predict that the Omicron spike has a higher binding affinity to ACE2 than Delta (Delta is 60% more transmissible than the highly infectious Alpha variant). The K417N, N440K, 30 S477N, 31 T478K, E484A, 32 and N501Y 33 , 34 mutations were shown to evade neutralization by convalescent sera, some monoclonal antibodies (mAbs), and postvaccine serum. 35 , 36 , 37
Compared to Omicron BA.1, BA.1.1, BA.3, BA.4, and BA.5, the BA.2 lineage is missing the 69–70 deletion, 38 , 39 which is associated with S gene target failure (SGTF) and has been the nicknamed as “stealth” variant. This makes tracking its transmission by SGTF detection challenging. 39 The protein–protein docking model indicated that the docking energies of wild‐type (WT), BA.1, BA.1.1, BA.2, and BA.3 were −799.6, −943.4, −946.8, −974.0, and −999.3, respectively, with hACE2. The docking results showed that BA.2 and BA.3 had a higher affinity for hACE2 than WT, BA.1, and BA.1.1, indicating that BA.2 had a higher potential for transmission than BA.1 based on both protein–protein docking servers. 40 Structural predictions pointed out that a key difference in the spike protein between BA.2 and BA.1 is the N‐terminal domain surface in the BA.2 is more enlarged and flattened than BA.1. 41 This structural change is due to the lack of 143–145 deletion in BA.2, leading to BA.2 having a higher positive electrostatic surface potential, which can facilitate the interaction between BA.2‐RBD and hACE2. 42 , 43 Compare to BA.2, BA.4, and BA.5 have the additional spike mutations del69‐70, L452R, F486V, and R493Q, a reversion mutation. Notably, F486V mutation carried by BA.4/5 reduced receptor affinity due to reduced hydrophobic interactions, while R493Q reversion mutation restored a hydrogen bond with H34 and avoided charge repulsion by K31, and increased the affinity between BA.4/5 RBD and hACE2. 44
The Omicron variant not only accumulated a large number of mutations in the spike protein but also in open reading frame 1ab (ORF1ab), nucleocapsid (N) protein, envelope (E) protein and membrane (M) protein (including NSP1–S135R; PLpro–T24I, G489S; NSP4–L264F, T327I, L438F, T492I; 3CL–P132H; NSP6–del105‐108, F108L; NSP12–P323L; 189 V; NSP13–R392C; NSP14–I42 V; NSP15–T112I; ORF3a–T223I; E–T9I; M–Q19E; N–P13 L, del31‐33, R203K, G204R, S413R. (Data available from https://www.nicd.ac.za/latest-confirmed-cases-of-covid-19-in-south-africa/). Domenico Benvenuto et al. 45 used the amino acid change stability analysis and showed that mutations in NSP6 decrease the stability of the protein structures. P323L mutation in NSP12 can reduce the fidelity of viral gene replication. 46 Johnson and colleagues reported that the R203K + G204R mutation increases N protein phosphorylation and impacts the local charge of the N protein, and the R203K/G204R mutations may promote the binding of RNA by increasing the positive charge to increase the RNP assembly efficiency, which can accelerate virus replication. 47 , 48
Altogether, the Omicron lineages has the largest number of mutations throughout the genome. All these mutations can affect the biological characteristics of the Omicron lineages, including increasing the transmissibility ans causing immune escape compared to the WT and the previous VOCs (Alpha, Beta, Gamma, Delta).
1.2. Virological characteristics of SARS‐CoV‐2 Omicron lineages
In vitro, cell culture experiments show that BA.2 is more replicative in human nasal epithelial cells and more fusogenic than BA.1, and the morphology of syncytia infected with BA.2 was significantly (1.52‐fold) larger than BA.1. 13 In vivo, in the lung periphery, the viral RNA load of BA.2 was 9.3‐fold and 11‐fold higher than those of BA.1 and B.1.1 at the same timepoint, respectively. 13
Statistical analysis from a Bayesian model, which represents the epidemic dynamics of SARS‐CoV‐2 lineages, shows that the effective reproduction number (Rt) of BA.2 is 2.51‐fold (Rt, 95% CI: 2.48–2.55) 49 and 1.26 −1.4‐fold (Rt, 95% CI: 1.25–1.52) higher than Delta and BA.1, respectively (Rt, which measures how many secondary cases are generated by a single primary case at time t). 13 Similarly, epidemiological studies indicated that Ct mean values for positive swabs infected with BA.2 (E gene: 23.7, N gene: 25.9) were lower (p < 0.005) than BA.1 (E gene: 26.3, N gene: 27.7) and BA.1.1 (E gene: 24.5, N gene 26.6). 50 , 51
Pseudovirus studies indicated that the Rt of BA.4, BA.5, and BA.2.12.1 were 1.19‐, 1.21‐, and 1.13‐fold higher than BA.2, respectively. In particular, pseudovirus infectivity showed that the infectivity of BA.4/5 pseudovirus was 18.3‐fold higher than BA.2. Cell culture experiments showed that BA.2.12.1 and BA.4/5 more efficiently replicate in human alveolar epithelial cells than BA.2, with the levels of viral RNA in the supernatant of rBA.4/5‐infected cultures being 34‐fold higher than rBA.2. 52 In addition, a multinomial logistic regression model showed that the growth advantages for BA.4 and BA.5 per day over BA.2 in South Africa. 53
Altogether, the Rt of BA.2 is higher than BA.1 and BA.1.1, while the effective Rt of BA.4 and BA.5 are higher than BA.2. Particularly, the risk of BA.4 and BA.5 for global health is potentially higher than BA.2.
1.3. The outbreak of BA.2, BA.4, and BA.5
According to the data from NICD, BA.1 is the dominant strain in November (73%), December (94%), and January (55%) in South Africa. Sequence analysis showed that the proportion of confirmed cases of BA.2 increased from 43% (1175/2721) to 94% (764/811), while the proportion of confirmed cases of the BA.1 variant decreased from 55% (1479/2721) to 2% (36/811) from January to March in South Africa. Subsequently, BA.4 and BA.5 have rapidly replaced BA.2, reaching more than 50% of sequenced cases in South Africa by the first week of April 2022. While BA.1 was the predominant sublineage in January (55%), BA.2 dominated in February (86%) and March (78%). BA.4 and BA.5 are together dominant in April (73%), May (93%), June (91%), July (93%) in South Africa (Data available from: https://www.nicd.ac.za/latest-confirmed-cases-of-covid-19-in-south-africa/).
A first study conducted in Denmark reported a higher contagiousness with the 21 L/BA.2 Omicron variant (n = 2122) than with the Omicron 21 K/BA.1 variant (n = 5,702). 49 Since then, the prevalence of BA.1 increased from 2.8% in Week 48% to 71.9% in Week 51 in 2021, thereafter declining to 7% by Week 5 in 2022, accompanied by BA.2 increased from less than 0.1% to 89.2% of sequenced samples during this period. 19 Recently, there is an increasing trend in the proportions for BA.5 observed in Portugal, BA.5 already accounted for ∼37% of the positive cases as of May 8, 2022. From July 4 to 17, 2022, BA.4/BA.5 accounted for 93.2% of the total sequence from 14 European countries (Data available from: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-sars-cov-2-omicron-sub-lineages-ba4-and-ba5).
In the United Kingdom in mid‐November 2021, an increase in a second Omicron sublineage BA.2 was observed in early January 2022. 54 , 55 Among 1195 positive samples, only one (0.1%: 0.0–0.5) corresponded to the Delta variant and the remainder were Omicron lineages: 32.7%, 39.6%, 27.7% were BA.1, BA.1.1, BA.2, respectively. 51 Specifically, of the 212 positive swabs with determined sublineages from participants living in London to February 21, 2022, all sublineages were Omicron and 94 (44.3%; 95% CI: 37.8–51.1) were BA.2. In the United Kingdom, of the sequenced episodes from July 10 to 17, 2022, 78.7%, 17.2%, 3.4% were BA.5, BA.4, BA.2, respectively, and 0.7% were classified as other (Data available from: https://www.gov.uk/government/news/covid-19-variants-identified-in-the-uk).
BA.2 was first identified in the United States from a sample collected on December 14, 2021, in New Jersey. As of April 16, 2022, the sequence of BA.2 accounts for 75.9%, BA.2.12.1 accounts for 18.2%, BA.1.1 accounts for 4.8%, BA.1 accounts for 0.7% of the total sequence in the United States. BA.2.12.1 was the dominant strain in May, as of the late of May 2022, the sequence of BA.2.12.1 accounted for 61.3%. Notably, BA.5 increased from 9.4% in June 4 to 56% in July 2. As of July 30, 2022, the sequence of BA.5 accounts for 85.5% of the total sequence (Data available from: https://covid.cdc.gov/covid-data-trackerhttps://covid.cdc.gov/covid-data-tracker/#variant-proportions).
In conclusion, BA.4 and BA.5 variants may be more transmissible than the other Omicron lineages and spread widely in many countries worldwide.
1.4. Low risk of severe clinical outcomes of patients infected with Omicron lineages
Epidemiologic surveillance has revealed that the proportion of hospitalizations and deaths did not increase with the number of COVID‐19 cases following emergence of the Omicron variant globally, with a 20%–80% reduction in risk of hospital admission. 56 , 57 , 58 , 59 , 60 , 61 Recently, multivariable analysis in Africa showed that, after controlling factors associated with hospitalization and severity (age, sex, presence of comorbidity, health care sector, province, previous SARS‐CoV‐2 infection, and SARS‐CoV‐2 vaccination status), the odds of hospital admission and severe disease did not differ between individuals with BA.2 infection and those with BA.1 infection, with adjusted odds ratios (aORs) 0.96 (95% CI: 0.85–1.09) and (aORs) 0.91 (95% CI: 0.68–1.22), respectively. 62 , 63 Similarly, one clinical study from southern California revealed that 30‐day risks of hospital admission, symptomatic hospital admission, ICU admission, mechanical ventilation, and mortality were not different among cases with BA.1/BA.1.1, and BA.2 infections diagnosed over this period; 30‐day risks of these outcomes were 13.3 versus 14.7, 11.5 versus 12.6, 0.4 versus 0.5, 0.0 versus 0.5, and 1.0 versus 0.5 per 1000 persons, respectively. 64 Moreover, the adjusted hazard of severe hospitalization or death in the BA.4/BA.5 wave was similar to the BA.1 wave (adjusted hazard ratio [aHR] 1.12; 95% CI: 0.93; 1.34). 65
These data demonstrated that although BA.2, BA.4, and BA.5 might have a competitive advantage over BA.1, infections with BA.2, BA.4, and BA.5 were not associated with differential risk of severe outcomes compared to BA.1/BA.1.1.
1.5. Decreased neutralization of Omicron lineages by mAbs, vaccines, and convalescent plasma
Molecular evidence pointed out that mutations (such as K417N, N440K, G446S, S477N, T478K, E484A, Q493K, G496S, and N501Y) could cause a reduction in neutralizing activity of mAbs, convalescent plasma, and serum‐induced by vaccines. 35 , 36 , 37 , 66 BA.2 has an additional three deletions and seven substitutions compared to BA.1, three of which lie in the RBD. 14 Structure and molecular analysis demonstrated that mutations in BA.1 (S371L, G446S, and G496S) and BA.2 (S371F, T376A, D405N, and R408S) have the potential to affect antibody binding. In especial, BA.1 G446S, G496S and BA.2 D405N, R408S lie at the edge of the ACE2 interaction sites, 67 these distant mutations undermine the neutralization of BA.2 by some therapeutic antibody. 14 In silico structural analysis showed that both L452R and L452Q conferred resistance largely to Classes 2 and 3 RBD mAbs, specially L452R. F486V broadly caused steric hindrance to binding by Class 2 RBD mAbs such as REGN10933, and LY‐CoV555. 44
Cell culture infection assays revealed that BA.2 variant was almost completely resistant to two therapeutic mAbs, casirivimab and idevimab, in contrast to their significant neutralizing activities against WT, Alpha, Gamma, and Delta. Similarly, BA.2 was 35‐fold more resistant to sotrovimab than the ancestral D614G‐bearing BA.1.1. 13 , 68 The FRNT50 values of sotrovimab and imdevimab+casirivimab combination therapy for BA.2 were 12.2 to 49.7‐fold, 43.0 to 143.6‐fold higher than WT and other VOCs (Alpha, Beta, Gamma, and Delta). (FRNT50: the titer of monoclonal antibodies required for a 50% reduction in the number of infectious foci). 69 Moreover, pseudovirus neutralization showed that compared to BA.2 and BA.2.12.1, BA.4/5 showed substantially greater neutralization resistance to two Class 2 RBD mAbs as well as modest resistance to two Class 3 RBD mAbs. 44 BA.4/BA.5 has been found to be 4–20 times more resistant to mAbs such as cilgavimab and evusheld than BA.2.
Pseudovirus neutralization revealed that the geometric mean neutralizing antibody titers (GMTs) of the initial two doses of the BNT162b2 vaccine against WT, BA.1, and BA.2 were 658, 29, and 24, respectively. Six months after the initial two BNT162b2 immunizations, the GMTs was 129 against WT but less than 20 against all the Omicron lineages. 70 The GMTs of 1‐month postdose 3 of BNT162b2 vaccine against BA.1‐, BA.2‐, BA.2.12.1‐, BA.3‐, BA.4/5‐ were 3.4‐, 4.5‐, 4.2‐, 6.2‐, and 13.0‐fold lower than that WT GMT, respectively. 71 , 72 . In particular, the GMTs of booster dose of BNT162b2 against BA.2.12.1 and BA.4/BA.5 was decreased by 2.2‐ and 3.3‐fold lower than BA.1. 73 Similarly, one report from UK Health Security Agency demonstrated that vaccine effectiveness against symptomatic disease was 63.6% (95% CI: 58.8–67.8%) and 67.1% (95% CI: 54.2–76.3%) for BA.1 and BA.2, respectively, within the first 2 weeks of receiving two doses of BNT162b2, ChAdOx1‐S or mRNA‐1273. This dropped to 17.4% (95% CI: 15.2–19.4%) and 24.3% (95% CI: 20.3–28.0%) after 25 or more weeks for BA.1 and BA.2, respectively. 74 Additionally, individuals who received inactivated vaccine (CoronaVac) or ZF2001 booster 6 months after two doses of CoronaVac, BA.4/BA.5 showed even stronger antibody escape than BA.1, BA.1.1, and BA.2. 75
Animal experiments have shown that both BA.1 and BA.2 were highly resistant to convalescent sera who had infected with WT, Alpha, and Delta. BA.2 was significantly (2.9‐fold) more resistant to BA.1‐infected convalescent hamster sera than BA.1. 13 Moreover, one preprint from University of Texas Medical Branch showed that the neutralization activity of BA.1‐infected convalescent plasma against BA.2 and BA.3 was 4.2‐, 4.4‐fold lower than against homologous BA.1, respectively. 76 Compared with the median neutralization titers of plasma from individuals infected with BA.1 or BA.2 against BA.1, the median titer was lower by 1.5‐ and 2.9‐fold against the BA.2.12.1 and BA.4/BA.5. 73 The median neutralization titers of BA.1 convalescents plasma against BA.2.13, BA.2.12.1, and BA.4/5 were reduced by 2.0‐, 3.7‐, and 8.0‐ fold, compared to that against BA.1, respectively. 75
These results suggest that the neutralizing activity against BA.4 or BA.5 by mAbs, vaccination and previous SARS‐CoV‐2 infection were lower than against BA.1 and BA.2, which indicate that the SARS‐CoV‐2 Omicron variant has continued to evolve with increasing immune escape.
1.6. Vaccine effectiveness against Omicron BA.2, BA.4, and BA.5
UKHSA reported that effectiveness of only prior infection, only three‐dose BNT162b2 vaccination, hybrid immunity of prior infection and two‐dose BNT162b2 vaccination, and hybrid immunity of prior infection and three‐dose BNT162b2 vaccination against symptomatic BA.2 infection was 46.1% (95% CI: 39.5–51.9%), 52.2% (95% CI: 48.1–55.9%), 55.1% (95% CI: 50.9–58.9%), 77.3% (95% CI: 72.4–81.4%), respectively. 74 Meanwhile, BNT162b2 vaccination and hybrid immunity showed strong effectiveness >70% against severe, critical, or fatal COVID‐19 due to BA.2 infection. However, the highest protection was that of hybrid immunity of prior infection and recent booster vaccination, at ∼80%. Similar levels and patterns of effectiveness were observed for BA.2 by mRNA‐1273 vaccine. 72 Among those who received any booster dose of vaccine (BNT162b2, mRNA‐1273, ChAdOx1‐S), vaccine effectiveness increased to 71.3% (95% CI: 69.6–72.9%) and 72.2% (95% CI: 67.0–76.5%) for BA.1 and BA.2, respectively, after a week. 74
In an analysis restricted to the BA.4/BA.5 period, prior diagnosed infection remained strongly protective against severe hospitalization or death (aHR 0.23; 95% CI: 0.10; 0.52) as did vaccination (the only vaccines available in South Africa to date are BNT162b and Ad26. COV2.S) aHR 95% CI: 0.20 (0.08–0.49); 0.39 (0.25–0.59), and 0.51 (0.27–0.99) for “boosted,”“two doses” and “single dose,” respectively. 65
Although BA.2, BA.4, and BA.5 can evade polyclonal neutralizing antibody responses, boosting vaccination with the current vaccine (ChAdOx1, BNT162b2, mRNA‐1273) may provide sufficient protection against symptomatic disease caused by BA.2, BA.4, and BA.5.
1.7. T‐cell mediated immune response against Omicron lineage infection
Previous studies have shown that early induction of antigen‐specific CD4 + T‐cells following vaccination is associated with generation of antibody and CD8 + T‐cell responses against SARS‐CoV‐2 infection. 77 Patients with mild COVID‐19 is associated with increased the number of CD8 + T‐cells in bronchoalveloar lavage fluid, 78 CD8 + T‐cell mediated effectively eliminate the virus, 79 and strengthen CD8 + T‐cell reactivity to SARS‐CoV‐2 antigen. 80
Recently, one study reported that the median effector T‐cell reactivity against WT, Delta and Omicron spike was 152, 155, and 114 for individuals with prior infection, 43, 34, and 42 for individuals after primary series vaccination (without prior infection), 311, 277, and 315 for individuals with prior infection after primary series vaccination, respectively. Moreover, T‐cell response increases by 20.1‐ and 20.4‐fold against WT and Omicron following the booster vaccination, respectively. 81 Similarly, several studies predicted that the memory mediated by T cells in individuals with prior infection (WT or previous VOCs) and vaccination (with EMA‐approved vaccines) has preserved reactivity to the Omicron variant, especially their reactivity is enhanced by booster vaccination. 82 , 83 , 84 , 85 , 86 , 87 Surprisingly, the percentage of participants with prior infection and/or vaccination had a >50% reduction in T‐cell response to Omicron spike was higher than Delta (21.2% vs. 9.7%), potentially due to escape of HLA‐I restricted epitopes. 83 ” Therefore, it is important to understand protection against these VOCs may be hidden in cross‐reactive SARS‐CoV‐2‐specific T‐cell mediated immunity.
In the future, more attention should be given to the effects of mutations on specific T‐cell immune responses to explore the dynamics and diversity of cellular immune responses. It is meaningful to better understand SARS‐CoV‐2‐specific T‐cell immunity and its vaccine for immunocompromised patients infected with Omicron lineages, or even other future SARS‐CoV‐2 variants.
2. CONCLUSION
To date, the Omicron lineage is the most frequently mutated variant among VOCs. It has 50 mutations in the whole genome and 26–32 mutations in the spike protein. As of August 2022, Omicron is classified into five main lineages, BA.1, BA.2, BA.3, BA.4, BA.5 and some sub‐lineages (BA.1.1, BA.2.12.1, BA.2.11, BA.2.75, BA.4.6). Many mutations of Omicron lineage spike are linked to heightened infectivity and easily evasion the neutralizing activity of convalescent plasma and mAbs and vaccine sera compared with other VOCs (Alpha, Beta, Gamma, Delta). In particular, BA.5 is becoming the main epidemic variant in many countries worldwide instead of BA.2.
AUTHOR CONTRIBUTIONS
Yongbing Zhou conceived and wrote the manuscript and prepared figure. Huilin Zhi contributed to the data collection and prepared figure. Yong Teng contributed to the modification and revision of the manuscript. All authors contributed to this article and approved the submitted versions.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Zhou Y, Zhi H, Teng Y. The outbreak of SARS‐CoV‐2 Omicron lineages, immune escape, and vaccine effectivity. J Med Virol. 2022;1‐9. 10.1002/jmv.28138
DATA AVAILABILITY STATEMENT
The data supporting this study's findings are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Leung K, Shum MH, Leung GM, Lam TT, Wu JT. Early transmissibility assessment of the N501Y mutant strains of SARS‐CoV‐2 in the United Kingdom, October to November 2020. Euro Surveill. 2021;26(1):2002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Makoni M. South Africa responds to new SARS‐CoV‐2 variant. Lancet. 2021;397:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Faria NR, Mellan TA, Whittaker C, et al. Genomics and epidemiology of the P.1 SARS‐CoV‐2 lineage in Manaus, Brazil. Science. 2021;372:815‐821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tian D, Sun Y, Xu H, Ye Q. The emergence and epidemic characteristics of the highly mutated SARS‐CoV‐2 Omicron variant. J Med Virol. 2022;2022(4):2376‐2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tian D, Ye Q. Hepatic complications of COVID‐19 and its treatment. J Med Virol. 2020;92:1818‐1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ye Q, Wang B, Zhang T, Xu J, Shang S. The mechanism and treatment of gastrointestinal symptoms in patients with COVID‐19. Am J Physiol Gastrointest Liver Physiol. 2020;319:G245‐G252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Han X, Ye Q. Kidney involvement in COVID‐19 and its treatments. J Med Virol. 2021;93(3):1387‐1395. [DOI] [PubMed] [Google Scholar]
- 8. Singh J, Rahman SA, Ehtesham NZ, Hira S, Hasnain SE. SARS‐CoV‐2 variants of concern are emerging in India. Nat Med. 2021;27:1131‐1133. [DOI] [PubMed] [Google Scholar]
- 9. Organization WH, Statement on Omicron sublineage BA.2. Geneva: World Health Organization February 2022. 2022. https://www.who.int/news/item/22-02-2022-statement-on-omicron-sublineage-ba.2
- 10. Walter N, Jassat W, DATCOV‐Gen . Clinical severity of Omicron sub‐lineage BA.2 compared to BA.1 in South Africa. medRxiv. 2022. 10.1101/2022.02.17.22271030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pastorio C, Zech F, Noettger S. Determinants of spike infectivity, processing and neutralization in SARS‐CoV‐2 Omicron subvariants BA.1 and BA.2. Cell Host Microbe. 2022;30(9):1255‐1268. 10.1101/2022.04.13.488221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kurhade C, Zou J, Xia H, et al. Neutralization of Omicron BA.1, BA.2, and BA.3 SARS‐CoV‐2 by 3 doses of BNT162b2 vaccine. Emerg Microbes Infect. 2022;11:1‐18. 10.1080/22221751.2022.2099305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yamasoba D, Kimura I, Nasser H. Virological characteristics of SARS‐CoV‐2 BA.2 variant. medRxiv. 2022. 10.1101/2022.02.14.480335 [DOI] [Google Scholar]
- 14. Zhou H, Tada T, Dcosta BM, Landau NR. Neutralization of SARS‐CoV‐2 Omicron BA.2 by therapeutic monoclonal antibodies. bioRxiv. 2022. 10.1101/2022.02.15.480166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fang Z, Peng L, Lucas C, et al. Heterotypic vaccination responses against SARS‐CoV‐2 Omicron BA.2. Cell Discov. 2022;8(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khandia R, Singhal S, Alqahtani T, et al. Emergence of SARS‐CoV‐2 Omicron (B.1.1.529) variant, salient features, high global health concerns and strategies to counter it amid ongoing COVID‐19 pandemic. Environ Res. 2022;209:112816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mohapatra RK, Kandi V, Verma S, Dhama K. Challenges of the Omicron (B.1.1.529) variant and its lineages: a global perspective. ChemBioChem. 2022;23(9):e202200059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tegally H, Moir M, Everatt J, et al. Continued emergence and evolution of omicron in South Africa: new BA.4 and BA.5 lineages. Nat Med. 2022. medRxiv; 10.1038/s41591-022-01911-2 [DOI] [Google Scholar]
- 19. Lyngse FP, Kirkeby C, Halasa T, et al. Transmission of SARS‐CoV‐2 Omicron VOC subvariants BA.1 and BA.2: evidence from Danish households. bioRixv preprint. 2022. 10.2807/1560-7917 [DOI] [Google Scholar]
- 20. Chen J, Qiu Y, Wang R, Wei GW. Persistent Laplacian Projected Omicron BA.4 and BA.5 to become new dominating variants. May 2022 arXiv:2205.00532v1. [DOI] [PMC free article] [PubMed]
- 21. GISAID . hCoV‐19 tracking of variants (see menu option BA.2). 2021. Accessed December 29, 2021. https://www.epicov.org/epi3/frontend#34a5cd
- 22. Rajpal VR, Sharma S, Kumar A, et al. Title: ‘is omicron mild’? Testing this narrative with the mutational landscape of its three lineages and response to existing vaccines and therapeutic antibodies. J Med Virol. 2022;94(8):3521‐3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Starr TN, Greaney AJ, Hilton SK, et al. Deep mutational scanning of SARS‐CoV‐2 receptor binding domain reveals constraints on folding and ACE2 binding. Cell. 2020;182(5):1295‐1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu H, Zhang Q, Wei PC, et al. The basis of a more contagious 501Y.V1 variant of SARS‐COV‐2. bioRxiv. 2021. 10.1101/2021.02.02.428884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shah M, Woo HG. Omicron: a heavily mutated SARS‐CoV‐2 variant exhibits stronger binding to ACE2 and potently escapes approved COVID‐19 therapeutic antibodies. Front Immunol. 2022;12:830527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sabir DK. Analysis of SARS‐COV2 spike protein variants among Iraqi isolates. Gene Rep. 2022;26:101420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mertens J, Coppens J, Loens K, et al. Monitoring the SARS‐CoV‐2 pandemic: screening algorithm with single nucleotide polymorphism detection for the rapid identification of established and emerging variants. Clin Microbiol Infect. 2022;28(1):124‐129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Genovese L, Zaccaria M, Farzan M, et al. Investigating the mutational landscape of the SARS‐CoV‐2 Omicron variant via ab initio quantum mechanical modeling. bioRxiv, 2021. 10.1101/2021.12.01.470748v1 [DOI] [Google Scholar]
- 29. Rath SL, Padhi AK, Mandal N. Scanning the RBD‐ACE2 molecular interactions in Omicron variant. Biochem Biophys Res Commun. 2022;592:18‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Planas D, Bruel T, Grzelak L, et al. Sensitivity of infectious SARS‐CoV‐2 B.1.1.7 and B.1.351 variants to neutralizing antibodies. Nat Med. 2021;27:917‐924. [DOI] [PubMed] [Google Scholar]
- 31. Kemp SA, Collier DA, Datir RP, et al. SARS‐CoV‐2 evolution during treatment of chronic infection. Nature. 2021;592:277‐282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang Z, Schmidt F, Weisblum Y, et al. mRNA vaccine‐elicited antibodies to SARS‐CoV‐2 and circulating variants. Nature. 2021;592:616‐622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li Q, Nie J, Wu J, et al. SARS‐CoV‐2 501Y.V2 variants lack higher infectivity but do have immune escape. Cell. 2021;184:2362‐2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wang R, Zhang Q, Ge J, et al. Analysis of SARS‐CoV‐2 variant mutations reveals neutralization escape mechanisms and the ability to use ACE2 receptors from additional species. Immunity. 2021;54:1611‐1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chi X, Yan R, Zhang J, et al. A neutralizing human antibody binds to the N‐terminal domain of the Spike protein of SARS‐CoV‐2. Science. 2020;369:650‐655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Callaway E. Delta coronavirus variant: scientists brace for impact. Nature. 2021;595:17‐18. [DOI] [PubMed] [Google Scholar]
- 37. Chung H, Noh JY, Koo BS, Hong JJ, Kim HK. SARS‐CoV‐2 mutations acquired during serial passage in human cell lines are consistent with several of those found in recent natural SARS‐CoV‐2 variants. Comput Struct Biothchnol J. 2022;20:1925‐1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Guo Q, A R, Liang L, et al. An imported case of BA.2 lineage of Omicron variant COVID‐19 ‐ Guangdong Province, China, December 28, 2021. China CDC Wkly. 2021;4:98‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. The Guardian . 2022. Scientists find ‘stealth’ version of Omicron that may be harder to track. Accessed December 29, 2021. https://www.theguardian.com/world/2021/dec/07/scientists-find-stealth-version-of-omicron-not-identifiable-with-pcr-testcovid-variant
- 40. Kumar S, Karuppanan K, Subramaniam G. Omicron (BA.1) and sub‐variants (BA.1, BA.2 and BA.3) of SARS‐CoV‐2 spike infectivity and pathogenicity: a comparative sequence and structural‐based computational assessment. J Med Virol. 2022;94:4780‐4791. 10.1002/jmv.27927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fantini J, Yahi N, Colson P, Chahinian H, La Scola B, Raoult D. The puzzling mutational landscape of the SARS‐2‐variant Omicron. J Med Virol. 2022;94(5):2019‐2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fantini JYN, Azzaz F, Chahinian H. Structural dynamics of SARS‐CoV‐2 variants: a health monitoring strategy for anticipating Covid‐19 outbreaks. J Infect. 2021;83:197‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Colson P, Delerce J, Beye M, et al. First cases of infection with the 21L/BA.2 Omicron variant in Marseille, France. J Med Virol. 2022;94(7):3421‐3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wang Q, Guo Y, Iketani S, et al. SARS‐CoV‐2 Omicron BA.2.12.1, BA.4, and BA.5 subvariants evolved to extend antibody evasion. Nature. 2022;608:603‐608. 10.1038/s41586-022-05053-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Benvenuto D, Angeletti S, Giovanetti M, et al. Evolutionary analysis of SARS‐CoV‐2: how mutation of Non‐Structural Protein 6 (NSP6) could affect viral autophagy. J Infect. 2020;81:e24‐e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sahin E, Bozdayi G, Yigit S, et al. Genomic characterization of SARS‐CoV‐2 isolates from patients in Turkey reveals the presence of novel mutations in spike and nsp12 proteins. J Med Virol. 2021;93:6016‐6026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Johnson BA, Zhou Y, Lokugamage KG, et al. Nucleocapsid mutations in SARS‐CoV‐2 augment replication and pathogenesis. PLoS Pathog. 2022;18(6):e1010627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wu H, Xing N, Meng K, et al. Nucleocapsid mutations R203K/G204R increase the infectivity, fifitness, and virulence of SARS‐CoV‐2. Cell Host Microbe. 2021;29(12):1788‐1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ito K, Piantham C, Nishiura H. Estimating relative generation times and relative reproduction numbers of Omicron BA.1 and BA.2 with respect to Delta in Denmark. Math Biosci Eng. 2022;19(9):9005‐9017. 10.1101/2022.03.02.22271767 [DOI] [PubMed] [Google Scholar]
- 50. Qassim SH, Chemaitelly H, Ayoub HH, et al. Effects of BA.1/BA.2 subvariant, vaccination, and prior infection on infectiousness of SARS‐CoV‐2 Omicron infections. J Travel Med. 2022:taac068. 10.1093/jtm/taac068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hyam MC, Tang D, Eales O, et al. The Omicron SARS‐CoV‐2 epidemic in England during February 2022. Lancet Reg Health Eur. 2022;21:100462 10.1101/2022.03.10.22272177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kimura I, Yamasoba D, Tamura T, et al. Virological characteristics of the novel SARS‐CoV‐2 Omicron variants including BA.2.12.1, BA.4 and BA.5. bioRxiv. 10.1101/2022.05.26.493539 [DOI] [Google Scholar]
- 53. Tegally H, Moir M, Everatt J, et al. Emergence of SARS‐CoV‐2 Omicron lineages BA.4 and BA.5 in South Africa. Nature Med. 2022. 10.1038/s41591-022-01911-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Andrews N, Stowe J, Kirsebom F, et al. Covid‐19 vaccine effectiveness against the Omicron (B.1.1.529) variant. N Engl J Med. 2022;386(16):1532‐1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. UKHSA . 2022. SARS‐CoV‐2 variants of concern and variants under investigation in England: technical briefing. Accessed January 28, 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1050999/Technical-Briefing-35-28
- 56. Nyberg T, Ferguson NM, Nash SG, et al. Comparative analysis of the risks of hospitalisation and death associated with SARS‐CoV‐2 Omicron (B.1.1.529) and Delta (B.1.617.2) variants in England: a cohort study. Lancet. 2022;399(10332):1303‐1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bager P, Wohlfahrt J, Bhatt S, et al. Reduced risk of hospitalisation associated with infection with SARS‐CoV‐2 Omicron variant versus Delta variant in Denmark: an observational cohort study. Lancert Infect Dis. 2022;22(7):967‐976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wolter N, Jassat W, Walaza S, et al. Early assessment of the clinical severity of the SARS‐CoV‐2 omicron variant in South Africa: a data linkage study. Lancet. 2022;399(10323):437‐446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sheikh A, Kerr S, Woolhouse M, McMenamin J, Robertson C, EAVE C. Severity of Omicron variant of concern and effectiveness of vaccine boosters against symptomatic disease in Scotland (EAVE II): a national cohort study with nested test‐negative design. Lancet Infect Dis. 2022;22(7):959‐966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lauring AS, Tenforde MW, Chappell JD, et al. Clinical severity of, and effectiveness of mRNA vaccines against, Covid‐19 from Omicron, Delta, and Alpha SARS‐CoV‐2 variants in the United States: prospective observational study. BMJ. 2022;376:e069761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ulloa AC, Buchan SA, Daneman N, Brown KA. Estimates of SARS‐CoV‐2 Omicron Variant Severity in Ontario, Canada. JAMA. 2022;327(13):1286‐1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wolter N, Jassat W, DATCOV‐Gen . Clinical severity of Omicron sub‐lineage BA.2 compared to BA.1 in South Africa. medRxiv. 2022. 10.1101/2022.02.17.22271030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Davies M‐A, Kassanjee R, Rousseau P, et al. Outcomes of laboratory‐confirmed SARSCoV‐2 infection in the Omicron‐driven fourth wave compared with previous waves in the Western Cape Province, South Africa. Trop Med Int Health. 2022;27:564‐573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lewnard JA, Hong VX, Patel MM, Kahn R, Lipsitch M, Tartof MF. Clinical outcomes associated with SARS‐CoV‐2 Omicron (B.1.1.529) variant and BA.1/BA.1.1 or BA.2 subvariant infection in Southern California. Nat Med. 2022. 10.1038/s41591-022-01887-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Davies MA, Morden E, Rosseau P, et al. Outcomes of laboratory‐confirmed SARS‐CoV‐2 infection during resurgence driven by Omicron lineages BA.4 and BA.5 compared with previous waves in the Western Cape Province, South Africa. medRxiv. 2022. 10.1101/2022.06.28.22276983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Tian D, Sun Y, Zhou J, Ye Q. The global epidemic of SARS‐CoV‐2 variants and their mutational immune escape. J Med Virol. 2021;94:847‐857. 10.1002/jmv.27376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Nutalai R, Zhou D, Tuekprakhon A, et al. Potent cross‐reactive antibodies following Omicron breakthrough in vaccinees. Cell. 2022;185(12):2116‐2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ohashi H, Akazawa D, Kim SK, et al. Different efficacies of neutralizing antibodies and antiviral drugs on SARS‐CoV‐2 Omicron subvariants, BA.1 and BA.2. Antiviral Res. 2022;205:105372. 10.1101/2022.02.27.482147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Takashita E, Kinoshita N, Yamayoshi S, et al. Efficacy of antiviral agents against the SARS‐CoV‐2 Omicron subvariant BA.2. N Engl J Med. 2022;386(15):1475‐1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Yu J, Collier AY, Rowe M, et al. Neutralization of the SARS‐CoV‐2 Omicron BA.1 and BA.2 variants. N Engl J Med. 2022;386(16):1579‐1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kurhade C, Zou J, Xia H, et al. Neutralization of Omicron BA.1, BA.2, and BA.3 SARS‐CoV‐2 by 3 doses of BNT162b2 vaccine. Emerg Microbes Infect. 2022;6:1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Chemaitelly H, Abu‐Raddad LJ. Duration of mRNA vaccine protection against SARS‐CoV‐2 Omicron BA.1 and BA.2 subvariants in Qatar. Lancet. 2022;399:771‐773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Hachmann NP, Miller J, Collier AY, et al. Neutralization escape by SARS‐CoV‐2 Omicron subvariants BA.2.12.1, BA.4, and BA.5. N Engl J Med. 2022;387(1):86‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kirsebom FCM, Andrews N, Stowe J, et al. COVID‐19 vaccine effectiveness against the omicron BA.2 variant in England. Lancet Infect Dis. 2022;22(7):931‐933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Cao Y, Yisimayi A, Jian F, et al. BA.2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection. Nature. 2022;608:593‐602. 10.1038/s41586-022-04980-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zou J, Chaitanya K, Xia HJ, et al. Cross‐neutralization of Omicron BA.1 against BA.2 and BA.3 SARS‐CoV‐2. Nat commun. 2022;13(1):2956. 10.1101/2022.03.30.486409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Painter MM, Mathew D, Goel RR, et al. Rapid induction of antigen‐specifific CD4+ T cells is associated with coordinated humoral and cellular immunity to SARS‐CoV‐2 mRNA vaccination. Immunity. 2021;54:2133‐2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Liao M, Liu Y, Yuan J, et al. Single‐cell landscape of bronchoalveolar immune cells in patients with COVID‐19. Nat Med. 2020;26:842‐844. [DOI] [PubMed] [Google Scholar]
- 79. Tan AT, Linster M, Tan CW, et al. Early induction of functional SARS‐CoV‐2‐specifific T cells associates with rapid viral clearance and mild disease in COVID‐19 patients. Cell Rep. 2021;34:108728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Peng Y, Mentzer AJ, Liu G, et al. Broad and strong memory CD4+ and CD8+ T cells induced by SARS‐CoV‐2 in UK convalescent individuals following COVID‐19. Nat Immunol. 2020;21:1336‐1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Naranbhai V, Nathan A, Kaseke C, et al. T cell reactivity to the SARS‐CoV‐2 Omicron variant is preserved in most but not all individuals. Cell. 2022;185:1041‐1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Li Y, Wang X, Jin J, et al. T‐cell responses to SARS‐CoV‐2 Omicron spike epitopes with mutations after the third booster dose of an inactivated vaccine. J Med Virol. 2022;94:3998‐4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. May DH, Rubin BER, Dalai SC, et al. Immunosequencing and epitope mapping reveal substantial preservation of the T cell immune response to Omicron generated by SARS‐CoV‐2 vaccines. medRxiv. 2021. 10.1101/2021.12.20.21267877 [DOI] [Google Scholar]
- 84. Gao Y, Cai C, Grifoni A, et al. Ancestral SARS‐CoV‐2‐specific T cells cross‐recognize the Omicron variant. Nature Med. 2022;28:472‐476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Keeton R, Tincho MB, Ngomti A, et al. T cell responses to SARS‐CoV‐2 spike cross‐recognize Omicron. Nature. 2022;603:488‐492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Liu J, Chandrashekar A, Sellers D, et al. Vaccines elicit highly conserved cellular immunity to SARS‐CoV‐2 Omicron. Nature. 2022;603:493‐496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Tarke A, Coelho CH, Zhang Z, et al. SARS‐CoV‐2 vaccination induces immunological T cell memory able to cross‐recognize variants from Alpha to Omicron. Cell. 2022;185:847‐859. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting this study's findings are available from the corresponding author upon reasonable request.


