Executive summary
As of May 31, 2022, there were 6·9 million reported deaths and 17·2 million estimated deaths from COVID-19, as reported by the Institute for Health Metrics and Evaluation (IHME; throughout the report, we rely on IHME estimates of infections and deaths; note that the IHME gives an estimated range, and we refer to the mean estimate). This staggering death toll is both a profound tragedy and a massive global failure at multiple levels. Too many governments have failed to adhere to basic norms of institutional rationality and transparency, too many people—often influenced by misinformation—have disrespected and protested against basic public health precautions, and the world's major powers have failed to collaborate to control the pandemic.
The multiple failures of international cooperation include (1) the lack of timely notification of the initial outbreak of COVID-19; (2) costly delays in acknowledging the crucial airborne exposure pathway of SARS-CoV-2, the virus that causes COVID-19, and in implementing appropriate measures at national and global levels to slow the spread of the virus; (3) the lack of coordination among countries regarding suppression strategies; (4) the failure of governments to examine evidence and adopt best practices for controlling the pandemic and managing economic and social spillovers from other countries; (5) the shortfall of global funding for low-income and middle-income countries (LMICs), as classified by the World Bank; (6) the failure to ensure adequate global supplies and equitable distribution of key commodities—including protective gear, diagnostics, medicines, medical devices, and vaccines—especially for LMICs; (7) the lack of timely, accurate, and systematic data on infections, deaths, viral variants, health system responses, and indirect health consequences; (8) the poor enforcement of appropriate levels of biosafety regulations in the lead-up to the pandemic, raising the possibility of a laboratory-related outbreak; (9) the failure to combat systematic disinformation; and (10) the lack of global and national safety nets to protect populations experiencing vulnerability.
This Commission report aims to contribute to a new era of multilateral cooperation based on strong UN institutions to reduce the dangers of COVID-19, forestall the next pandemic, and enable the world to achieve the agreed goals of sustainable development, human rights, and peace that governments are committed to pursue as members of the UN. We address this Commission report to the UN member states, the UN agencies and multilateral institutions, and multilateral processes such as the G20 and the G7. Our aim is to propose guideposts for strengthening the multilateral system to address global emergencies and to achieve sustainable development. In issuing this report, we commend the excellent work of many important international studies that have preceded our own, most notably those from the Independent Panel for Pandemic Preparedness and Response and the G20 High-Level Independent Panel on Financing the Global Commons on Pandemic Preparedness and Response.
Section 1 of this Commission report provides a conceptual framework for understanding pandemics. Section 2 provides an annotated chronology of the COVID-19 pandemic and thematic findings regarding several issues. Section 3 presents our policy recommendations, particularly around multilateral cooperation centred at WHO to address global health crises, and around investments in preparedness for future health crises through strong national health systems and international financing and technology cooperation with the world's lower-income regions.
Methodology
The Lancet COVID-19 Commission was established in July, 2020, with four main themes: developing recommendations on how to best suppress the epidemic; addressing the humanitarian crises arising from the pandemic; addressing the financial and economic crises resulting from the pandemic; and rebuilding an inclusive, fair, and sustainable world.1 The 28 Commissioners are global experts in public policy, international cooperation, epidemiology and vaccinology, economics and financial systems, sustainability sciences, and mental health. The Commissioners oversaw the work of 12 thematic Task Forces, which met on an ongoing basis (once every 2 weeks or once per month) to support the work of the Commission. These Task Forces included a total of 173 experts. The Commission Secretariat acted as liaison among the Task Forces. The Task Forces published short pieces on their respective areas of focus on the Commission website and in peer-reviewed journals, contributing to the efforts of the overall Commission.
Key findings.
-
•
The proximal origin of SARS-CoV-2 remains unknown. There are two leading hypotheses: that the virus emerged as a zoonotic spillover from wildlife or a farm animal, possibly through a wet market, in a location that is still undetermined; or that the virus emerged from a research-related incident, during the field collection of viruses or through a laboratory-associated escape. Commissioners held diverse views about the relative probabilities of the two explanations, and both possibilities require further scientific investigation. Identification of the origin of the virus will help to prevent future pandemics and strengthen public trust in science and public authorities.
-
•
WHO acted too cautiously and too slowly on several important matters: to warn about the human transmissibility of the virus, to declare a Public Health Emergency of International Concern, to support international travel protocols designed to slow the spread of the virus, to endorse the public use of face masks as protective gear, and to recognise the airborne transmission of the virus.
-
•
As the outbreak became known globally in early January, 2020, most governments around the world were too slow to acknowledge its importance and act with urgency in response. It was mainly the countries in WHO's Western Pacific region, primed by their experience with severe acute respiratory syndrome, that reacted with urgency to the outbreak, and that generally pursued a suppression strategy that led to low cumulative mortality, although the omicron variant (B.1.1.529) has been undoing some of these gains.
-
•
Coordination among governments was inadequate on policies to contain the pandemic, including travel protocols to slow the global transmission of the virus, testing strategies, public health and social measures, commodity supply chains, data standards and reporting systems, and advice to the public, despite the very high interdependence among countries.
-
•
Epidemic control was seriously hindered by substantial public opposition to routine public health and social measures, such as the wearing of properly fitting face masks and getting vaccinated. This opposition reflects a lack of social trust, low confidence in government advice, inconsistency of government advice, low health literacy, lack of sufficient behavioural-change interventions, and extensive misinformation and disinformation campaigns on social media. Public policies have also failed to draw upon the behavioural and social sciences; doing so would have led to more successful implementation of public health interventions and helped to increase social trust, prosociality, equity, and wellbeing. In many cases, policies and decision making have not been informed by robust and continuously updated evidence syntheses.
-
•
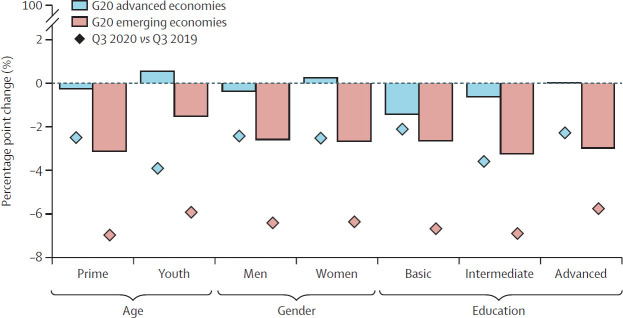
Public policies did not properly address the profoundly unequal effects of the pandemic. Heavily burdened groups include essential workers, who are already disproportionately concentrated in more vulnerable minority and low-income communities; children; women, who face employment, safety, and income losses, exacerbated by the adverse consequences of school closures; people living in congregate settings, such as prisons or care homes, especially for older populations; people living with chronic conditions and disability; Indigenous Peoples; migrants, refugees, and displaced populations; people without access to quality and affordable health care; and people who face the burdens of long COVID.
-
•
Among high-income countries, those with strong and resilient national health systems—including public health systems that complement clinical health care—have generally fared better at addressing COVID-19 and maintaining non-pandemic-related health services. In low-income and middle-income countries (LMICs), where health systems tend to be under-resourced and fragmented, better outcomes were seen when previous experiences with outbreaks and epidemics were built upon, and when community-based resources—notably community health workers—were used to support screening and contact-tracing capacity and trust-building within communities.
-
•
Rapid development of multiple vaccines has been a triumph of the research and development system and the result of long-standing public and private investment and cooperation. However, the lack of a multilateral and coordinated approach by governments to manage intellectual property rights, technology transfer, international financing, the allocation of vaccines from multinational pharmaceutical companies, and the support for vaccine production in LMICs for use in those countries, has come at a great cost in terms of inequitable access to vaccines.
-
•
Economic recovery depends on sustaining high rates of vaccination coverage and low rates of new, clinically significant COVID-19 infections, and on fiscal and monetary policies to mitigate the socioeconomic effects of the pandemic and prevent a financial crisis. Emergency global financing from the International Monetary Fund, the World Bank, and regional development banks had a salutary role, although much larger financial flows from high-income to low-income regions were warranted.
-
•
The sustainable development process has been set back by several years, with a deep underfinancing of investments needed to achieve the Sustainable Development Goals (SDGs) and the aims of the Paris Climate Agreement. In most countries, the pandemic diverted resources and policy attention away from longer-term goals, thereby reversing progress towards the SDGs in many countries.
Key recommendations.
-
•
The world requires globally coordinated efforts to bring an end to the COVID-19 pandemic on a rapid and equitable basis. Countries should maintain a vaccination-plus strategy that combines mass vaccination, availability and affordability of testing, treatment for new infections and long COVID (test and treat), complementary public health and social measures (including the wearing of face masks in some contexts), promotion of safe workplaces, and economic and social support for self-isolation. A vaccination-plus strategy with the goal of protecting populations should be implemented on a sustainable basis, rather than as a reactive policy that is abruptly turned on and off.
-
•
WHO, governments, and the scientific community should intensify the search for the origins of SARS-CoV-2, investigating both a possible zoonotic origin and a possible research-associated origin. The search for origins requires unbiased, independent, transparent, and rigorous work by international teams in virology, epidemiology, bioinformatics, and other related fields.
-
•
WHO should expand the WHO Science Council to apply urgent scientific evidence for global health priorities, including future emerging infectious diseases. This Council should include experts from diverse fields and from all six WHO regions, and should include younger people and have gender parity. Establishing an understanding of exposure routes and the highest-risk environments for transmission should always be among the first essential steps for scientists in response to future disease threats, because this knowledge should determine effective control strategies for reducing risk.
-
•
Governments, represented at the World Health Assembly (WHA) by their national health ministers, should establish stronger means of cooperation and coordination in the response to emerging infectious diseases. Strengthened cooperation should be incorporated in a new pandemic agreement and in updated International Health Regulations (IHR), as were adopted in 2005 after the outbreak of severe acute respiratory syndrome and which now need updating.
-
•
WHO should be strengthened. The WHA should create a WHO Global Health Board composed of the six WHO regions, represented by heads of state on a rotating basis, and selected by the governments of each region. Reforms of WHO should include a substantial increase of its core budget. The world community should not establish new centres of global health policy and finance that would compete with, or even undermine, the central role of WHO.
-
•
We call for a dual track to prevent future emerging infectious diseases. To prevent natural spillovers, governments should coordinate on the global surveillance and regulation of domestic animal and wild animal trade, and take stronger measures against dangerous practices. To prevent research-related spillovers, WHO should be given new oversight authority regarding the biosafety, biosecurity, and bio-risk management of national and international research programmes that are engaged in the collection, testing, and genetic manipulation of potentially dangerous pathogens.
-
•
The WHA, in conjunction with the G20 countries, should adopt a 10-year global strategy to bolster research and development capacity and commodity production capacity—including for vaccines—for every WHO region, including in the low-income regions of the world. WHO should help several low-income and middle-income countries (LMICs) to achieve WHO's stringent regulatory authority status.
-
•
Countries should strengthen national health systems on the foundations of public health and universal health coverage, grounded in human rights and gender equality. Strong public health systems should include strong relationships with local communities and community organisations; surveillance and reporting systems; robust medical supply chains; health-promoting building design and operation strategies; investments in research in behavioural and social sciences to develop and implement more effective interventions; promotion of prosocial behaviours; strong health education for health promotion, disease prevention, and emergency preparedness; effective health communication strategies; active efforts to address public health disinformation on social media; and continuously updated evidence syntheses. The health-care system should include universal health coverage that is centred around primary health care and ensures that patients have access to quality care for pandemic-related and non-pandemic-related health issues, including mental health. Community health workers and community-based organisations should be well trained and supported.
-
•
In addition to strengthening health systems, each country should determine and expand national pandemic preparedness plans to prevent and respond to newly emerging infectious diseases. Preparedness plans should include improved surveillance and monitoring; definition and protection of vulnerable groups; international notifications; cooperation within WHO regional groups; emergency financing; guidelines on behavioural, social, and environmental interventions, travel protocols, and safe schools and workplaces; robust health-commodity supply chains (eg, personal protective equipment, diagnostics, therapeutics, and vaccines); effective risk communication and active opposition to misinformation and disinformation; training of public health professionals; and provision of adequate staffing.
-
•
A new Global Health Fund should be created that is closely aligned with WHO. This Fund should combine and expand the operations of several existing health funds and add new funding for three windows of financing: commodities for disease control, pandemic preparedness and response, and primary health system strengthening in LMICs. We propose that the Global Health Fund should have its headquarters in (Continues on next page)(Key recommendations continued from previous page)Geneva, Switzerland, but have strong regional offices in each of the six WHO regions. The Fund would thereby have centralised overall funding but decentralised programme design and implementation, to foster strong ownership by the countries of each region and to reflect regional needs and priorities, rather than being under top-down control from Geneva or from a few donor countries.
-
•
The UN member states, with particular responsibility of the G20 countries, should adopt a new financial architecture to scale up financing for LMICs to meet the urgent challenges of pandemic preparedness, the Paris Climate Agreement, and the Sustainable Development Goals. The new financial architecture should include increased sustainable development funding from all sectors: official institutions, the private sector, foundations, and civil society.
The Commission issued its first statement in The Lancet 2 on the occasion of the UN General Assembly on Sept 14, 2020. The second statement of the Commission was published in The Lancet 3 on Feb 12, 2021, around the time of the launch of the global vaccination effort. In October, 2021, the Commission issued its third statement, directed towards the G20.4 For the final report of the Commission, each Task Force prepared a report drawing on original analysis and synthesis of evidence to generate recommendations relevant to their specific Task Force. Recommendations from these reports provide the basis for the Commission's final report. Additionally, the Secretariat oversaw a detailed analysis of the key policy recommendations of other COVID-19 commissions, panels, and working groups. The Secretariat and members of the Task Forces then examined the best available syntheses of evidence to inform and test the key claims made in the report.
The Commission focuses on the public policy of pandemic preparedness, response, and recovery, specifically in the areas of public health, virology, social policy, macroeconomics, international finance, and geopolitics. The Commission is not an investigative group, nor a body of biomedical specialists in key fields such as virology, vaccine development, and medicine. The Commission's focus is on science-based policy, global cooperation, and international finance.
The Commission uses UN nomenclature for all countries and locations mentioned in the report.
Section 1: conceptual framework for understanding pandemics
Five pillars of the successful fight against emerging infectious diseases
There are five basic pillars of a successful fight against emerging infectious diseases. The first is prevention: to stop an outbreak before it occurs by taking effective measures to prevent the emergence of a new and dangerous pathogen. The second is containment: to eliminate the transmission of disease from infected individuals to susceptible individuals after a disease has emerged. The third is health services: to save the lives of people with the disease and ensure the continuity of other health services, including those for mental health. The fourth is equity: to ensure that economic and social burdens are shared among the population and that the most vulnerable groups and individuals are protected. The fifth is global innovation and diffusion: to develop, produce, and distribute new therapeutics and vaccines in an equitable and efficient manner.
To accomplish these five pillars requires an ethical framework of prosociality—the orientation of individuals and government regulations to the needs of society as a whole, rather than to narrow individual interests.5, 6, 7, 8 In the 14th century, authorities in Venice, Italy, battled plague outbreaks by requiring ships to remain at anchor for 40 days before landing (the word quarantine derives from the Italian quaranta giorni, or forty days), as an early and incipient form of prosocial regulation.9 Prosociality nowadays includes voluntary behaviours by individuals, such as the proper use of face masks, in addition to government regulations, such as the enforcement of workplace safety standards, to prevent the transmission of disease.
Challenges of prosociality arise especially in circumstances of strategic dilemmas, in which the pursuit of narrow self-interest by each member of the society ends up weakening the society as a whole. By turning from the pursuit of narrow self-interest to the pursuit of shared interests, members of society can increase the wellbeing of all. Prosociality generally requires some form of the Golden Rule (doing to others what you would have done to you) or the Kantian Imperative (acting according to maxims that can be universal laws). Pandemics have many strategic dilemmas, and therefore require cooperative responses rather than selfish—and self-defeating—behaviours.
Prosociality was at a low ebb in many societies during the past 2 years. In many countries, social trust in government and other authorities among citizens has declined markedly in the past two decades (and over the past four decades in the United States)10—related, at least in part, to the persistent increase in socioeconomic inequalities. In places of low social trust, prosocial behaviours are rejected by many groups within society. Additionally, at the national level, many governments showed themselves to be untrustworthy and ineffective.11 At the global level, cooperation among governments was undermined by rancour among the major powers. This hostility gravely weakened the capacity of international institutions such as WHO to conduct their assigned roles in the pandemic response.
Success also requires preparedness. Building these five pillars after an outbreak has started is far too late, as the world has learned the hard way with COVID-19. This pandemic broke out at a moment of weak global preparedness. Despite ample previous warnings of increasing pandemic risks, at least since the outbreak of severe acute respiratory syndrome in 2003, most of the world was not prepared for COVID-19.
Rapid response to a new outbreak to control community transmission
When an outbreak occurs, time is of the essence. A core characteristic of emerging infectious diseases such as COVID-19 is the exponential growth of new infections in the initial stages of mass transmission. According to the basic model of the spread of an emerging infectious disease, the number of new infections per day is proportional to the number of infectious people in the population multiplied by the share of the population that is susceptible to infection (ie, the share of the population that lacks immunity). With the emergence of a new pathogen, most or all of the population is susceptible to infection, so the number of new cases is proportional to the number of current infectious cases, which implies an exponential growth of new infections.
A single new case of COVID-19 at the start of the pandemic became hundreds, or in some situations thousands, of cases within a month. The original SARS-CoV-2 variant that was first identified in Wuhan, China, had a doubling time of approximately 3 days, meaning that, over a 30-day month, a new (index) case would lead to roughly ten doublings, or 1024 (210) new infections on the tenth doubling.12
The basic lesson of this rapid growth of infections is the need to act on a new outbreak as soon as possible. If the public health system can quickly identify the index case, public health authorities can then trace the contacts of that person, so they can all be quarantined during the period of potential infectiousness to others.13, 14, 15 Case identification followed by contact tracing and isolation or quarantine can slow and reduce transmission.16, 17, 18 A major challenge to the test and quarantine approach for COVID-19 was the high proportion of asymptomatic infections, especially in young people.
The problem arises when community transmission (transmission among individuals beyond the index case) is already well underway, as public health workers might not be able to trace the contacts of hundreds of infected individuals. The ability of the public health system to identify cases, trace contacts, and isolate infected individuals can be overwhelmed in just a few weeks of uncontrolled community transmission.
Even with community transmission, all is not necessarily lost. Identifying and isolating a high proportion of infected individuals early in their infectious period, so that on average each infected person gives rise to less than one new infected person, is sufficient. With widespread access to quality and affordable community testing, infected individuals can learn quickly of their own SARS-CoV-2 infection and of their potential infectiousness to others, and can use face masks, adopt physical distancing, and isolate as soon as possible after infection. By doing so, these people are more likely to give rise to less than one new infection. This decline in infections can occur even without extensive contact tracing, but requires supportive personal behaviours and access to testing early in the epidemic, as was achieved in Republic of Korea.19 In short, pandemic control is based heavily on prosocial actions by individuals (eg, getting tested, keeping a physical distance, and isolating when infective), and these individual measures rely heavily on public policies (eg, trusted information for the community, access to testing sites, and an economic framework such as guaranteed paid leave) to support self-isolation.
Four COVID-19 control regimes
COVID-19 presents special challenges in terms of control, as transmission occurs from presymptomatic (before symptoms) and asymptomatic (without symptoms) individuals as well as from those with symptoms. Such transmission makes COVID-19 control especially difficult, because people who are infected are often not aware of their infectivity.
In technical terms, the reproduction number, R, denotes the number of infections caused by each infectious person. At the start of an outbreak, when no control measures have been put in place, R is denoted as R 0, called the basic reproduction rate. In the uncontrolled first wave of the COVID-19 pandemic in Wuhan, R 0 was around 2·4.20 With intensive contact tracing and the isolation of infected individuals, in addition to the implementation of a range of public health and social measures,21 the effective reproduction rate can be reduced to less than 1, and the epidemic will decline.
Epidemiologists therefore distinguish between four kinds of COVID-19 control regime. First is the uncontrolled scenario, R 0=2·4. In this case, the epidemic eventually ends when most of the population has been infected and therefore has eventually acquired immunity (at least temporarily). This kind of mass infection that eventually results in mass acquired immunity through natural infection is sometimes called the herd-immunity strategy.22 This strategy is highly problematic for COVID-19, because many infected people will die of the disease, and many who survive have what is known as long COVID.23
Second is the limited control case in which R is reduced to less than R 0=2·4 but remains greater than 1. In this case, the epidemic still grows exponentially, but less rapidly than with no control measures. The peak in the number of new infections per day is lower and occurs later than in the uncontrolled case. We have classified this control scenario as a mitigation strategy. During the COVID-19 pandemic, this strategy was often referred to as flattening the curve of the epidemic.24, 25 The eventual (cumulative) number of cases of infection during the epidemic is nearly the same as in the uncontrolled epidemic, but the infections are spread out over a longer time, and therefore put less pressure on the capacity of hospital and health-care systems at any given time.
Third, through the implementation of combinations of layered control measures—including widespread testing, contact tracing, and isolating; proper use of face masks; physical distancing; limitations on mass gatherings; and improved ventilation systems at workplaces—R decreases to less than 1, so the epidemic declines.16, 26 Early implementation of public health and social measures—including closing businesses and venues, banning public events, launching public information campaigns, and requiring the use of face masks—is more effective at keeping cumulative cases and deaths low than implementation at a later stage.27 We call this a suppression strategy. However, if circulation of the virus is not brought to zero, and infected people continue to arrive from other areas, this strategy needs to be implemented on an ongoing basis to contain each new outbreak in the community, and becomes progressively more difficult as highly transmissible variants emerge.
Fourth, by means of aggressive testing, contact tracing, and isolating, R is kept near 0. This strategy, which is sometimes called a containment strategy and was known in China as a zero-COVID strategy, can be viewed as an intensive application of the suppression strategy.28 In principle, deaths can be kept to near zero, and infections can be held to a very small portion of the population. A successful long-term exit from a containment strategy (ie, lifting of the containment measures) depends on the successful containment of transmission in the rest of the world, or on sufficient protection from vaccinations and highly effective therapeutics to tolerate a subsequent spread of the virus without incurring high death rates and serious disease. Some countries in the WHO Western Pacific region that adopted a containment strategy during the first 2 years of the pandemic later abandoned the strategy during the period in which the omicron variant (B.1.1.529) was dominant (known as the omicron wave), after a sufficiently high proportion of the population had been vaccinated.
What is the basis for choosing between these strategies? The herd-immunity strategy might be adopted if policy measures to reduce transmission are believed to be too onerous, too costly, or too ineffective to justify any steps to reduce R, or if the burden of infection in terms of deaths and illness is viewed as too small to justify any control measures. The herd-immunity strategy was originally advocated by some pundits on the grounds that acquired immunity would protect from COVID-19 reinfection for an extended period; however, it has since been found that immunity tends to wane over time, and new SARS-CoV-2 variants arise that evade acquired immunity. The herd-immunity strategy downplays not only the deaths but also the serious disease burden of long COVID.29
The flatten-the-curve strategy is likely to be adopted when the over-riding concern of policy makers is the surge of patients into the hospital system, and stronger control measures are viewed as too costly, unnecessary, or infeasible. The epidemic response of many governments has been led by political considerations and hospital-system administrators rather than by public health considerations and specialists.
The suppression strategy is likely to be adopted if suppression of the pandemic is deemed to be feasible and at sufficiently low cost to justify the stronger actions needed. Some opponents of the suppression strategy have argued that suppressing infection is futile, because in the future the virus will inevitably evade controls until herd immunity is reached. Yet this argument of futility misses an essential point, which is that a major purpose of suppression strategies is to buy time until the arrival of better tools—such as vaccines and therapeutics—at which time the response can be re-evaluated and perhaps eased. Even if a full-scale epidemic eventually arises, the temporary suppression of the epidemic by a year or two can buy time for mass vaccinations or the arrival of effective therapeutics, thereby saving lives and avoiding long-term health effects. The final tally of costs and benefits of a suppression strategy will necessarily be provisional until there is an exit policy, either through worldwide containment or through a high level of vaccination and access to effective medicines.
When the number of cases has already reached very high levels, even stronger measures—notably national lockdowns of the population, causing substantial dislocations of daily life and economic activity—might have to be invoked to regain some measure of control over the pandemic. Lockdowns with high rates of adherence can cause pronounced, albeit temporary, reductions of R, thereby causing a rapid decline in the number of new infections and the total number of infected people. If the lockdown is simply followed by a relaxation of controls to the pre-lockdown status quo, then R quickly returns to the pre-lockdown level, and within a short period of time the exponential growth of new infections restores the pre-lockdown rate of daily infections. The proper use of lockdowns is to serve as a temporary expedient to provide time for national health systems to build up and enable a more comprehensive set of public health and social measures, so that less disruptive measures—such as testing, contact tracing, and isolation—are in place after the lockdown is lifted.30
Prosociality for pandemic control
Suppression of the virus requires a range of public health and social measures, which are also known as prosocial behaviours. A person who tests positive for COVID-19 should not partake in activities that pose a risk of infection to others out of concern for others, not only for themselves, and they should reasonably be able to expect that others will behave in the same way. Additionally, encouraging prosocial behaviour during pandemics and beyond is valuable for mental and physical health, which could help to address the pervasive adverse effects of the pandemic on mental health, particularly during lockdown.31, 32, 33, 34
Prosocial behaviours include those that reduce transmission of the virus to others, support others to keep safe, promote health and social care within and outside health-care facilities, and promote social cohesiveness and mutual aid. Such prosocial actions include testing for infections, including frequent use of rapid diagnostic tests; isolating in the event of a positive test; precautionary quarantining after exposure, before receiving test results; wearing well fitting face masks in public indoor settings; maintaining physical distancing in public and other indoor spaces; meeting outdoors rather than indoors; working online from home where feasible; maximising outdoor air ventilation, upgrading filtration to minimum efficiency reporting value (MERV) 13 filters, and using portable air cleaners with high-efficiency particulate air filtration and other evidence-based air cleaning approaches—such as germicidal ultraviolet light—in high-risk settings, particularly when ventilation and filtration are not possible; and getting immunised as soon as vaccines are available.
National and local governments need to provide support so that people can make these necessary behaviour changes. Such support includes prompt deployment of high-quality testing, with widespread accessibility and affordability; government provision of public isolation and quarantine facilities for people living in conditions that prevent isolation at home; provision of financial and social support for people in isolation or quarantine; provision and deployment of high-quality and timely public information to support healthful and prosocial behaviours; increasing indoor air ventilation above minimum standards and enhancing air filtration efficiency (MERV 13 or higher) in mechanically ventilated buildings; and provision of free and easily accessible vaccination.
Crucially, prosociality applies between governments as well as between individuals. If two neighbouring countries have a shared open border, the maintenance of R near 0 is feasible only if both countries pursue a suppression (R<1) policy, supposing that it is not practical to either shut down travel between the two countries or to impose an effective quarantine on travellers between the two countries. A strategic dilemma results in which each government will follow a suppression strategy only if the other government also does so, but each government will adopt less effective control measures if the other government does so. In technical game theoretic terms, there are two Nash equilibria in pure strategies (suppression by both or limited control by both), with the suppression strategy Pareto-dominating the limited control equilibrium.
Two neighbouring governments could perhaps readily cooperate to agree to a joint suppression strategy. Yet when 27 EU countries or all 193 UN member states must cooperate on such measures, even if just a few governments do not pursue a suppression strategy, travellers from those countries will continue to spread the virus to the rest. Travel bans introduced by countries pursuing a suppression strategy could control the spread from a few recalcitrant countries with little international movement of people, but if even a few countries that host large numbers of international travellers fail to adopt suppression policies, most or all other countries will find continuing with such policies difficult. (China has done so, for example, but through very strict border controls and a substantial decline in cross-border travel.)
Such a strategic situation is known as a weakest-link game, because the outcome—in this case the chance of a suppression solution—depends on the weakest links among the national governments.35, 36, 37 One lesson from experimental research on weakest-link games is that when the game is played by just two players, or a small number greater than two, it is relatively straightforward for the players to align on the best strategy. However, when there are many players, the observed outcome often is highly inefficient.
In the context of COVID-19, a decentralised approach among many governments might end up with each choosing a very low degree of pandemic control because other countries are also doing so, even though every country would be better off if all pursued a suppression policy. The actions of each country have important effects, or externalities, on all other countries. When a single country chooses a suppression strategy, it renders a positive service to all other countries by greatly reducing the risk of its travellers bringing new infections to other parts of the world or of its population giving rise to new variants. If all countries choose suppression strategies, it would be possible to stop the epidemic without resorting to extended closure of international travels.
National governments should therefore coordinate their actions with the rest of the world to achieve a globally efficient and equitable outcome. Global cooperation should include standardisation of evidence-based public health and social measures to suppress viral transmission and to address other dimensions of the pandemic response, including disease surveillance with genomic monitoring for new variants, the sharing of epidemiological and genomic data, early warnings of outbreaks, and the pooling of resources to ensure universal and affordable access to drugs and vaccines. High-income countries have a very immediate and practical need to aid lower-income countries to take effective control measures that would otherwise be beyond their financial means. The slogan “no one is safe until everybody is safe” is not mere rhetoric, or a moral truth, but an epidemiological reality in a weakest-link context.
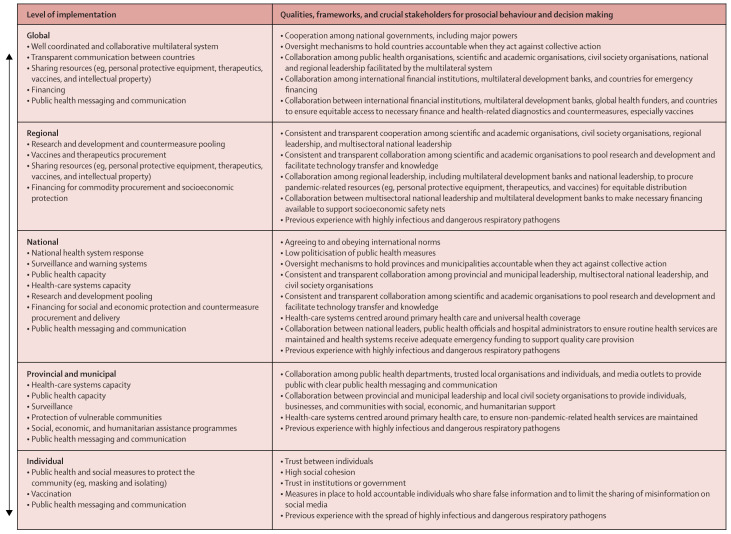
As detailed in figure 1 , at the individual level, trust in institutions and between individuals, and high social cohesion have been related to increased prosocial health behaviours, such as the wearing of face masks, physical distancing, and getting vaccinated. At the national level, low politicisation of public health measures, consistent and transparent collaboration among scientific and academic organisations and leadership, and oversight to encourage collective action can be linked to better national health systems responses, financing for social and economic protection, and accurate and consistent public health messaging. At the regional and international levels, a supported, well coordinated, and collaborative multilateral system that facilitates transparent cooperation among scientific and academic organisations, regional and national leadership, and international financial institutions is related to prosocial decision making. These levels of society and governance are mutually reinforcing, as they interact and influence one another. Therefore, as we continue to face this pandemic and prepare for the next, it is essential to appreciate and better understand the bottom-up and top-down processes in pandemic governance that encourage the needed prosocial behaviour.
Figure 1.
Synergies between prosociality and governance at each level of society
Section 2: a review of the global, regional, and national responses to COVID-19
The initial outbreak
On Dec 20, 2019, a cluster of atypical pneumonia cases was noted by clinicians in Wuhan. Around this time, as a result of these cases, concern was growing in the global scientific community about a new outbreak of severe acute respiratory syndrome or a related disease.38, 39, 40 However, some studies suggest that the virus, subsequently identified as SARS-CoV-2, was circulating several weeks before the identification of the cluster of cases in December,41, 42 and, according to some hypotheses, could have been circulating in one or more places outside of China before the outbreak in Wuhan.43 The exact timing and identity of the earliest cases remains uncertain, but this timing matters, as the world might have lost several precious weeks in containing the outbreak.
The origins of SARS-CoV-2
The proximal origins of SARS-CoV-2 are still not known. Identifying these origins would provide greater clarity into not only the causes of the current pandemic but also vulnerabilities to future outbreaks and strategies to prevent them. We concur with the position of 18 leading scientists who wrote in Science magazine44 in May, 2021: “We must take hypotheses about both natural and laboratory spillovers seriously until we have sufficient data.” As a group of 16 scientists communicated in The Lancet 45 in October, 2021: “Overwhelming evidence for either a zoonotic or research-related origin is lacking: the jury is still out.” More than 2 years into the pandemic, the search for the origin of SARS-CoV-2 remains incomplete and inconclusive.46, 47 Independent experts consulted by the Lancet COVID-19 Commission shared the view that hypotheses about both natural and laboratory spillovers are in play and need further investigation.
Although the proximal origins are unknown, SARS-CoV-2 is thought to derive from a bat SARS-CoV-related coronavirus with a furin cleavage site that enhances the capacity of the virus to infect human cells.48, 49 Furin cleavage sites are found naturally in almost every family of coronavirus,50, 51 although they have not been observed in other SARS-related coronaviruses (subgenus Sarbecoronavirus). Since 2006, following the emergence of severe acute respiratory syndrome, furin cleavage sites have also been the subject of laboratory manipulation, including their insertion into coronavirus spike proteins.52 The presence of the furin cleavage site in SARS-CoV-2 therefore does not by itself identify the proximal origin of the virus, whether natural or laboratory.
Two main possible pathways of emergence have been identified.53 The first is that SARS-CoV-2 emerged from a natural spillover event—that is, from a non-research-related zoonotic transmission of the virus from an animal to a human, and thereafter from human to human. The second is that the virus emerged from research-related activities, with three possible research-related pathways: the infection of a researcher in the field while collecting samples, the infection of a researcher in the laboratory while studying viruses collected in their natural habitat, and the infection of a researcher in the laboratory while studying viruses that have been genetically manipulated. Because both the pathways of natural transmission and of research-related transmission are feasible, preventing the emergence of future pandemic pathogens must include two distinct strategies: the prevention of natural (zoonotic) transmission and the prevention of research-related spillovers. Each of these strategies requires specific actions.
The first pathway of transmission risk is natural spillover. Most epidemics in history have involved the passage of a pathogen from an animal host to humans, followed by human-to-human transmission.54 For example, the proximal source of SARS-CoV, the virus that led to the outbreak of severe acute respiratory syndrome in 2003–04, was likely to have been exotic animals in a live animal market in Guangdong, China—most probably palm civets (Paguma larvata) and perhaps raccoon dogs (Nyctereutes procyonoides).55 The proximal reservoir of MERS-CoV, the virus that causes Middle East respiratory syndrome, is dromedary camels (Camelus dromedarius).56 In both cases, bats serve as the primary evolutionary source of the virus. Because both severe acute respiratory syndrome and Middle East respiratory syndrome result from natural spillovers of betacoronaviruses, the outbreaks of these diseases gave rise to concerns that future such spillovers would occur. SARS-CoV-2 might well be such an instance, especially given findings of SARS-CoV-2-like viruses in bats across east Asia.57 The dangers of zoonotic spillovers are increased by human encroachments into the habitats of animals that carry novel pathogens, such as through forest clearing, the handling of exotic animals in the illicit trade of wild species, in farms that raise domestic animals, and in food markets that sell and slaughter live animals.58, 59
The two subpathways for a natural spillover are direct bat-to-human transmission and transmission from bat to intermediate host to human. It is possible that the virus was passed directly from bats to humans because there are bat coronaviruses that can bind to human angiotensin-converting enzyme 2 and thereby infect humans without adaptation. Bats known to harbour these viruses are present across east Asia, including in central China.60 The other natural pathway is transmission from bats to an intermediate host mammal and then to a human.61 This pathway is plausible because many of the earliest known cases of COVID-19 in humans in Wuhan are associated with the Huanan Seafood Market, and this market sold animals such as raccoon dogs that are known to be susceptible to SARS-related coronaviruses.62 However, as no animals in the market tested positive for SARS-CoV-2, it is not known whether the COVID-19 cases associated with this market indicate the actual proximal origin of the virus or a secondary outbreak brought by humans to the marketplace. Because the first emergence of the virus could well have been in November, 2019, or even earlier, the cases associated with the Huanan Seafood Market in mid-December, 2019, could well indicate a human-to-human amplifier event rather than the original animal-to-human spillover. Despite the testing of more than 80 000 samples from a range of wild and farm animal species in China collected between 2015 and March, 2020, no cases of SARS-CoV-2 infection have been identified.47
Because betacoronaviruses related to SARS-CoV-2 are found across east Asia,63 the search for a natural source of SARS-CoV-2 should continue with high focus and intensity, as the eventual discovery of a natural reservoir of the virus might occur only after years of searching, and quite possibly outside of China.
The second possible pathway is a research-related or laboratory-associated release of the pathogen. Such a pathway could have involved a researcher becoming infected in the field or in the laboratory with a natural virus, or becoming infected in the laboratory with a genetically manipulated virus. Advances in biotechnology in the past two decades have made it possible to create new and highly dangerous pathogens through genetic manipulation—for example, creating chimeric viruses by combining the genetic material of more than one viral pathogen, or mutant viruses through the deliberate insertion of a furin cleavage site. The bioengineering of SARS-CoV-like viruses for the study and testing of potential drugs and vaccines advanced substantially after the outbreak of severe acute respiratory syndrome in the 2000s.52, 64 Laboratory experiments included the creation of novel viruses (eg, so-called consensus viruses that average the genetic code across a set of natural viruses), the mutation of viruses (such as through the insertion of a furin cleavage site), the creation of chimeric viruses, and the serial passaging of viruses through cell cultures to test their transmissibility, virulence, immunogenicity, and host tropism. Research that can increase the transmissibility and virulence of pathogens is called gain-of-function research of concern, although which specific experiments should fall into this category is contested by scientists. As laboratory technologies have rapidly advanced, many scientists have warned of the increasing risks of undersupervised and under-regulated genetic manipulation of SARS-CoV-like viruses and other potential pandemic pathogens.65 There is currently no system for the global monitoring and regulation of gain-of-function research of concern.
As of the time of publication of this report, all three research-associated hypotheses are still plausible: infection in the field, infection with a natural virus in the laboratory, and infection with a manipulated virus in the laboratory. No independent, transparent, and science-based investigation has been carried out regarding the bioengineering of SARS-like viruses that was underway before the outbreak of COVID-19. The laboratory notebooks, databases, email records, and samples of institutions involved in such research have not been made available to independent researchers. Independent researchers have not yet investigated the US laboratories engaged in the laboratory manipulation of SARS-CoV-like viruses, nor have they investigated the details of the laboratory research that had been underway in Wuhan.47 Moreover, the US National Institutes of Health (NIH) has resisted disclosing details of the research on SARS-CoV-related viruses that it had been supporting,66 providing extensively redacted information only as required by Freedom of Information Act lawsuits.67
In brief, there are many potential proximal origins of SARS-CoV-2, but there is still a shortfall of independent, scientific, and collaborative work on the issue. The search for the origins of the virus requires unbiased, independent, transparent, and rigorous work by international teams in the fields of virology, epidemiology, bioinformatics, and other related fields, and supported by all governments.
Early response to the COVID-19 outbreak in China and globally
Time is of the essence when a new infectious pathogen emerges. The early days of the COVID-19 outbreak are worth examining to understand how improved coordination and transparency, from the local to the international level, could have moderated the spread of the virus. There are still many gaps in our knowledge.
Whether identifiable cases appeared earlier than December, 2019, is unknown.68, 69, 70, 71, 72, 73 The precise timing of initial infections matters, because earlier warnings by local authorities and international observers to national and global health bodies would have made suppression of the outbreak more likely. Moreover, precise dating is helpful in discerning the most likely proximal origin of the virus.
There is currently no evidence that the Chinese central government in Beijing knew of the outbreak in Wuhan until late December, 2019.74 There seems to have been reticence in reporting the initial outbreak to the national authorities, as records of the initial outbreak remained among local Wuhan authorities. The early outbreak in Wuhan coincided with the Chinese Lunar New Year, involving extensive travel within China and large gatherings of people, which in turn could have facilitated the early spread of the virus to other parts of China and to other countries. By Jan 23, 2020, when China initiated its highly effective lockdown of Hubei Province, the virus was spreading around the world.
The outbreak first came to international attention on Dec 31, 2019, when the WHO Country Office in China noted an online report of a Wuhan-based outbreak of pneumonia of unknown cause.75 In response, WHO Headquarters contacted Chinese officials on Jan 1, 2020, for more information. On Jan 4, 2020, the head of the Chinese Centers for Disease Control and Prevention (CDC) telephoned his counterpart at the US CDC to inform the United States of the new outbreak. There are no published records of what was conveyed by the Chinese CDC on that occasion, although US officials probably had substantial cause for concern about human-to-human transmission. By early January, 2020, a preliminary genomic sequence of SARS-CoV-2 was available to the Wuhan Institute of Virology and to other scientists in China, who by then knew that Wuhan was facing a coronavirus epidemic.
On Jan 5, 2020, WHO made its first announcement of the Wuhan outbreak.75 On Jan 11, 2020, a scientist in China posted the genomic sequence of SARS-CoV-2 to a public database, and Chinese authorities posted the sequence the next day.76, 77 On Jan 17, 2020, the United States began screening passengers arriving from Wuhan at three airports: one in Los Angeles, CA; one in New York, NY; and one in Santa Fe, NM.78 On Jan 23, 2020, China announced a strict lockdown of Wuhan and five other provincial cities, covering a population of around 20 million people.79 On Jan 23, 2020, WHO declined to declare the novel coronavirus a global emergency,80 waiting until Jan 30, 2020 to declare a Public Health Emergency of International Concern.81
WHO at the centre of global cooperation and early shortcomings
The overwhelming case for global cooperation in response to an emerging infectious disease has long been recognised in international law, diplomacy, and practice. The late economist Richard Cooper argued that successful intergovernmental cooperation was in fact pioneered in an 1851 international conference on epidemic control, which led to the founding of the International Office of Public Hygiene in 1907, the precursor of WHO. WHO was established in 1948 and is now the central organising body for global cooperation on health.82, 83
Articles 21(a) and 22 of the WHO Constitution assign the World Health Assembly (WHA) the authority to adopt regulations “designed to prevent the international spread of disease”.84 These regulations, known as the International Health Regulations (IHR), were first adopted in 1969 and have been amended three times, most recently in 2005 after the outbreak of severe acute respiratory syndrome in 2003. These regulations remain in force for all WHO member states after adoption by the WHA, aside from member states that affirmatively opt out of the regulations within a prescribed period.
In principle, the IHR (2005), which are the governing regulations for the COVID-19 response, marked a decisive upgrade of international cooperation amid the massive expansion of international trade and travel in the early 2000s.85 The foreword of the IHR (2005) notes seven areas of revision and improvement of previous versions of the IHR, notably: (1) a wide scope of application, (2) obligations of member states to develop minimum core public health capacities, (3) responsibilities of member states to notify WHO of events that could constitute a public health emergency, (4) provisions authorising WHO to consider unofficial reports of public health events, (5) the power for WHO to designate a Public Health Emergency of International Concern (as was done on Jan 30, 2020 in the case of COVID-19), (6) protection of the human rights of persons and travellers, and (7) mechanisms for urgent communications between member states and WHO.85
Nonetheless, these measures failed to ensure a sufficiently robust global response to the emergence of SARS-CoV-2. In part, WHO fell victim to the increasing tensions between the United States and China, including the announcement in May, 2020, that the United States intended to withdraw from WHO, effective July, 202186—a decision that was later rescinded.87 More generally, WHO has lacked high-level political backing, financing, and convening power.88, 89
As a general matter, governance of WHO by the WHA, composed of the health ministers of each member state, proved to be inadequate for pandemic response for at least three reasons. First, the WHA meets only annually, whereas a pandemic requires daily hands-on action. Second, the WHA is too large a body to take executive decisions on behalf of the 193 WHO member states. Third, health ministers lack the political authority within their governments to guide whole-government decision making, and therefore do not have the political authority to guide strong and decisive WHO actions in emergency conditions. For these and related reasons, in 2021 the WHA launched a process of WHO reforms, starting a two-track process to determine whether to update the IHR (2005) and whether the WHA should develop a new global accord on pandemic prevention, preparedness, and response.90
In the swirl of uncertainty during the COVID-19 outbreak, WHO—acting under the IHR (2005)—repeatedly erred on the side of reserve rather than boldness. Initially, there were basic uncertainties about the infectiousness of the virus, its asymptomatic spread, and the methods of transmission, although over time the scientific community confirmed that considerable asymptomatic airborne transmission occurs and that the virus is highly transmissible. WHO was hesitant to act on these potentially grave risks until the uncertainties over viral transmission were better resolved, and was therefore slow to advocate policy responses commensurate with the actual dangers of the virus.
There is no doubt that false alarms about emerging infectious diseases can be politically costly, as was seen during the H1N1 influenza scare in 1976—an epidemic that never occurred91, 92—and the 2009 H1N1 influenza pandemic, which ultimately had a relatively low mortality rate of 0·1–0·7%.93 However, in the case of the 2009 H1N1 pandemic, politically cautious US national authorities deferred to local authorities with costly results worldwide, including the rapid global spread of the virus. Although over-reaction can be politically embarrassing, the COVID-19 pandemic has shown that centralised under-reaction can be devastating.
Acknowledging the uncertainties faced by WHO before the event, we list five areas in which WHO was too slow to act after the COVID-19 outbreak: (1) the recognition of asymptomatic human-to-human transmission, (2) the announcement of a Public Health Emergency of International Concern, (3) the advice on precautionary approaches to travel, (4) the advice on face masks, and (5) the acknowledgement of the crucial airborne exposure pathway of SARS-CoV-2, and the resulting implementation of appropriate risk reduction measures, such as increased ventilation and enhanced filtration, to slow the spread of the virus.
WHO first acknowledged the possibility of limited human-to-human transmission of COVID-19 on Jan 14, 2020, 2 weeks after the initial notification of the novel coronavirus from Chinese authorities. 8 days later, on Jan 22, 2020, WHO declared that human-to-human transmission was occurring, but clarity on the severity of COVID-19 infection was pending.94
On Jan 22, 2020, the WHO Director-General convened a closed-door meeting of virologists, public health researchers, and some government representatives, as the IHR (2005) process dictates.95 After this meeting, WHO declined to declare the rapid spread of the novel coronavirus a Public Health Emergency of International Concern, but changed its position around a week later with an announcement on Jan 30, 2020.95 This loss of a week enabled considerable global diffusion of the virus. Some observers, including the Independent Panel for Pandemic Preparedness and Response, argue that the term Public Health Emergency of International Concern does not properly convey the urgency of the situation, and that only after WHO used the term pandemic—which is not defined in IHR (2005)—was the outbreak taken seriously worldwide.96, 97, 98
A third consequential delay was the hesitation by WHO to recommend a more precautionary approach to travel from China.99 This delay contributed to the spread of the virus and limited the possibilities for risk mitigation. Before the onset of COVID-19, it was widely believed that travel restrictions were not highly effective for the control of emerging infectious diseases. With this perspective, the IHR (2005) does not recommend travel restrictions and requires countries that adopt them to provide the public health rationale and relevant scientific information.100 The IHR (2005) does allow for the early use of measures such as the collection of travel information and travel history from passengers and the use of screening.
By the time of the Jan 23, 2020 lockdown in Wuhan, infectious individuals had already dispersed to many other parts of the world.101 The first diagnosis of COVID-19 in the United States was on Jan 20, 2020,102 in a traveller who had returned to the United States from Wuhan on Jan 15, 2020. The first case in Europe was diagnosed on Jan 24, 2020, in Bordeaux, France.103 Of the first 47 people to be diagnosed in Europe,104 14 had recently visited China. Starting on Jan 10, 2020, and even as late as Feb 24, 2020, WHO continued to recommend that travellers practise usual precautions and advised against the application of travel or trade restrictions to countries with COVID-19 outbreaks.105, 106, 107, 108 Only in July, 2021, did WHO evolve towards a risk-based approach to international travel measures, which recommends the use of layers of containment that include contact tracing, screening for symptoms, diagnostic tests, use of face marks, and enhanced hygiene measures. A rapid review of international-travel-related control measures for COVID-19 found that travel restrictions can limit the spread of disease across national borders, and the combination of PCR testing and quarantines can together decrease transmission from travellers.109 However, a 2022 study found no evidence that border closures reduced the spread of COVID-19.110 Border measures can work only if they are timely, comprehensive, and complemented by policies to suppress local outbreaks that will continue to occur even with comprehensive travel measures.
Although the wearing of face masks has been widely accepted as a measure to decrease the spread of respiratory illnesses in the Western Pacific region, perhaps because of the experience of these countries with severe acute respiratory syndrome, WHO did not recommend use of face masks by the public until June 5, 2020—nearly 4 months after the declaration of the Public Health Emergency of International Concern.111, 112 Even then, WHO continued to caution of a lack of evidence that wearing face masks could prevent the spread of COVID-19. Until that point, WHO had advised that face masks should be used only in medical settings and by people who had symptoms of COVID-19.113, 114, 115
These delayed and vague recommendations from WHO continued until late April, 2021. One stark example is that even after receiving an open letter from 238 scientists in July, 2020, asking the organisation to address the airborne transmission of COVID-19, WHO did not change its stance on this issue until April 30, 2021.116 A rapid identification of dominant exposure routes for an emerging infectious disease is a crucial first step in the response to a new outbreak, because this knowledge helps to establish effective control strategies for reducing risk. Early in the outbreak, health authorities concentrated almost exclusively on spray transmission, leading to the emphasis on 1–2 m of physical distancing, extensive and frequent cleaning and disinfection of shared surfaces, and handwashing. Meanwhile, the threat of airborne transmission remained unrecognised and, as a result, the use of face coverings, ventilation, and air filtration as effective risk reduction measures were not adequately encouraged. Incorrect assumptions about airborne transmission persisted in the form of continued misallocation of time, energy, and resources, enabling the virus to continue to spread, almost unabated, for months.
A paradigm shift in how we view and address the transmission of respiratory infectious diseases
There are three methods of transmission of respiratory infectious diseases. The first and main method is airborne transmission, which occurs through the inhalation of viruses carried in microscopic respiratory particles (≤100 μm in diameter) suspended in the air, known as aerosols.117 This transmission can occur both in the near-field (within the vicinity of the infection source) and in the far-field (greater distances from the infection source). The second method is spray transmission, in which large droplets—large respiratory particles (>100 μm in diameter) that fall quickly to the ground (usually within 2 m of the source)—land directly on the mucous membranes of a susceptible person in the near-field. The third method of transmission occurs through touch, or indirect contact via a contaminated object known as a fomite, in which pathogens are transferred—usually by hand—to the mucous membranes of a susceptible person.
A paradigm shift in how we view and address the transmission of respiratory infectious diseases is underway.118 Airborne transmission in both the near-fields and the far-fields is a crucial, if not dominant, exposure pathway for SARS-CoV-2 and other respiratory viruses. Laboratory, field, modelling, and case studies have shown that airborne transmission through the inhalation of a virus-laden aerosol is important, if not dominant, for COVID-19.119, 120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132 Although transmission can occur through touch, it is rare for respiratory viruses, and touch and spray transmission are not likely to contribute to widespread transmission or superspreading events. As nearly all transmission occurs indoors, the way in which we design and operate building ventilation and filtration systems can reduce transmission.
Long-standing erroneous thinking about airborne transmission led WHO to discount the role of this transmission route at the start of the pandemic. The downplaying of airborne transmission can be traced to the misinterpretation of observations and experimental results from around 100 years ago. Because most transmission occurs when people are in close contact, it was wrongly assumed that transmission was through spray rather than through airborne aerosols. In fact, much of the close transmission is through aerosols, because people release considerable quantities of aerosol in addition to large droplets, especially when talking and coughing,133 and also because aerosol is most concentrated close to the source, like cigarette smoke particles near a smoker.134, 135 Therefore, although transmission via the airborne route by virus-laden aerosol can occur both in the near-field and in the far-field, the risk of near-field transmission for a single person in proximity to an infected person is generally greater than the risk of far-field transmission.134 Nonetheless, the greater frequency of transmission by close contact, combined with a desire of scientists to refute miasma theory—the prevailing theory of the transmission of respiratory infectious disease from the mid-to-late 19th century, in which vague explanations for the causes of disease, such as so-called bad air, were perpetuated with little to no causative basis136—led to the desire to promote infection-control recommendations centring on hygiene and sanitation. Such recommendations contributed to the perpetuation of the erroneous idea that spray transmission was the dominant mode of spread of respiratory infectious diseases, including COVID-19.136 Numerous publications have attempted to overturn mistaken ideas about transmission routes for respiratory infectious diseases,117, 137, 138, 139, 140, 141, 142, 143 and have initiated a paradigm shift towards more accurate definitions.117 Alas, WHO was slow to acknowledge the airborne transmission of SARS-CoV-2, and was therefore slow to emphasise the range of measures needed to limit indoor transmission.
Failures and successes of international cooperation
The world has paid a high price for the combination of poor preparedness and failures of cooperation to address COVID-19. The multiple failures of international cooperation include (1) the lack of timely notification of the initial outbreak of COVID-19; (2) costly delays in acknowledging the crucial airborne exposure pathway of SARS-CoV-2 and in implementing appropriate measures at the national and global levels to slow the spread of the virus; (3) the lack of coordination among countries regarding containment strategies; (4) the failure of governments to examine and adopt best evidence for controlling the pandemic and managing economic and social repercussions from other countries; (5) the shortfall of global funding for LMICs; (6) the failure to ensure adequate global supplies and equitable distribution of key commodities, including protective gear, diagnostics, medicines, medical devices, and vaccines, especially for LMICs; (7) the lack of timely, accurate, and systematic data on infections, deaths, variants, and health system responses; (8) the poor enforcement of appropriate levels of biosafety regulations in the lead-up to the pandemic, raising the possibility of a laboratory-related outbreak; (9) the inability or unwillingness to combat systematic disinformation; and (10) the lack of global and national safety nets to protect populations experiencing vulnerability.
Nonetheless, there have been some important bright spots in the national and global responses to COVID-19. The most important has been the public–private partnerships for the rapid development of vaccines. Also notable were the actions of higher-income countries to support households, businesses, and employers through fiscal and labour market measures to mitigate the adverse effects of the pandemic, and to inject funds into the health-care sector. We also highlight the positive role of the multilateral financial institutions. The World Bank provided nearly US$14 billion in fast-track support for COVID-19-related relief efforts and approved $12 billion in 2020 for countries to buy and deliver vaccines.144 The International Monetary Fund (IMF) also provided urgent support of approximately $170 billion for around 90 countries.
There were also important regional responses, such as the Caribbean Association of Doctors sharing epidemiological data on COVID-19 and the Caribbean Community ensuring coordinated action between countries, the EU's Inclusive Vaccine Alliance and ambitious recovery plan, and the African Vaccine Acquisition Task Team, a new initiative for surveillance enhancement and vaccine purchasing and sharing. Additionally, established health organisations such as the Global Fund to Fight AIDS, Tuberculosis, and Malaria (known as the Global Fund) partnered with countries to reprogramme up to 5% of their current grants towards supporting COVID-19 responses.145 There has also been rapid acceleration in the digital transformation of health systems and innovation in health-system delivery.
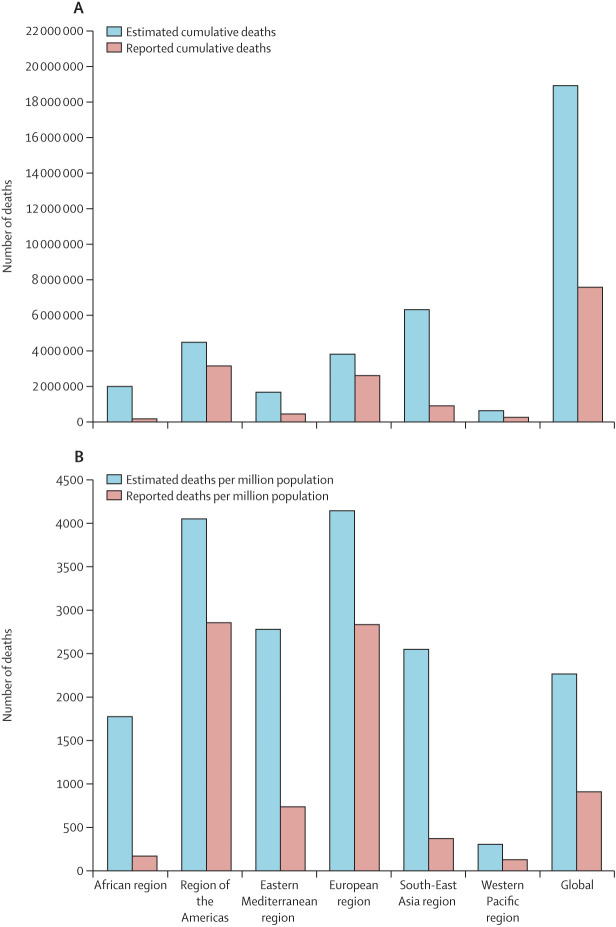
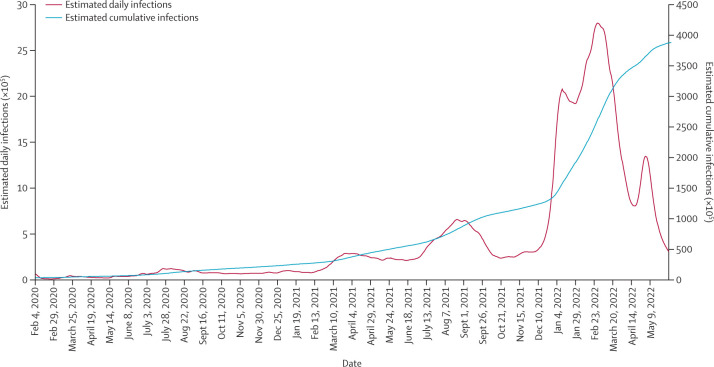
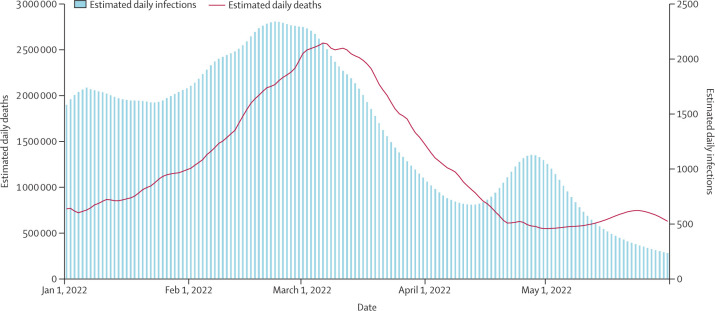
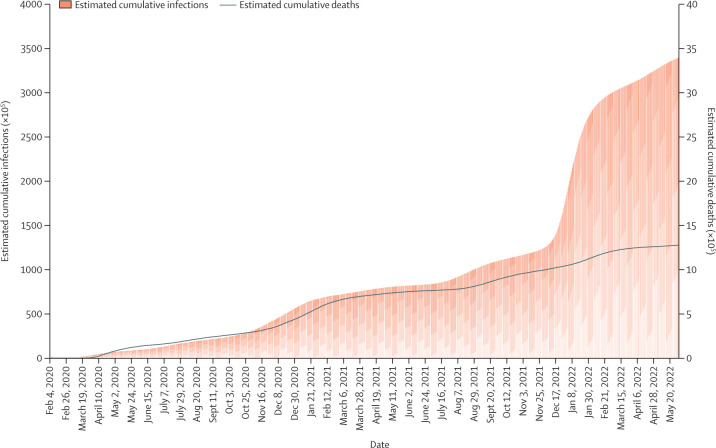
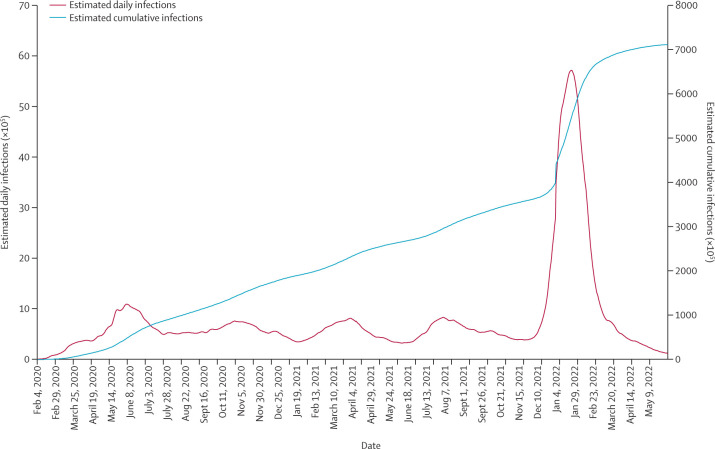
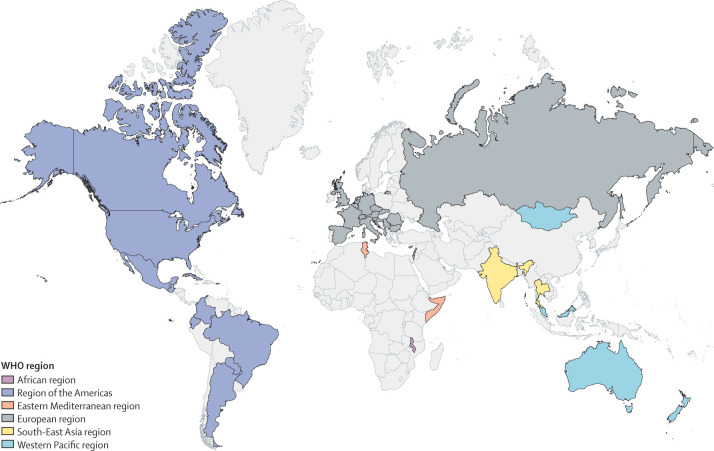
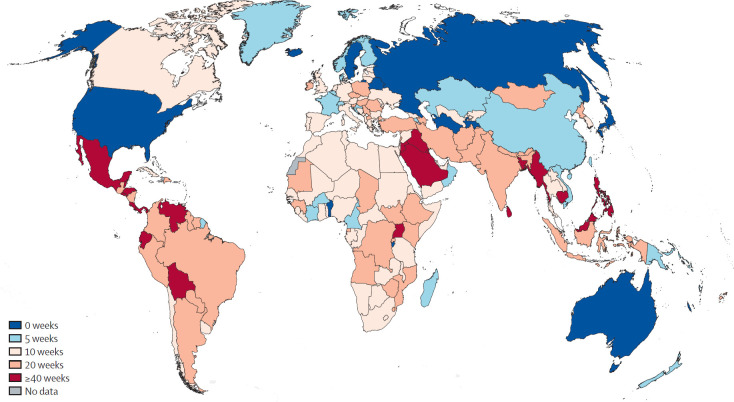
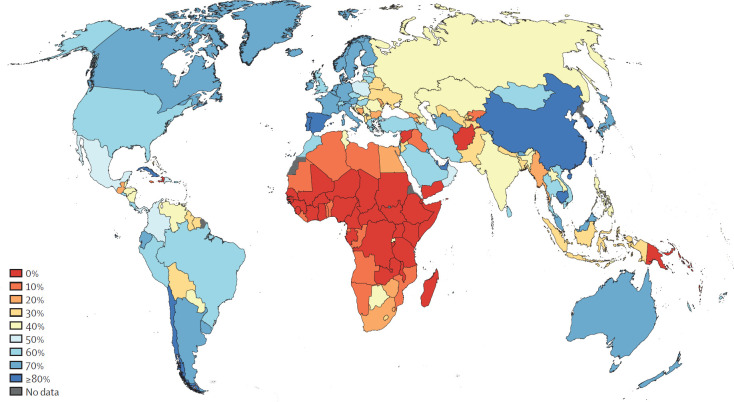
Regional differences in mortality rates
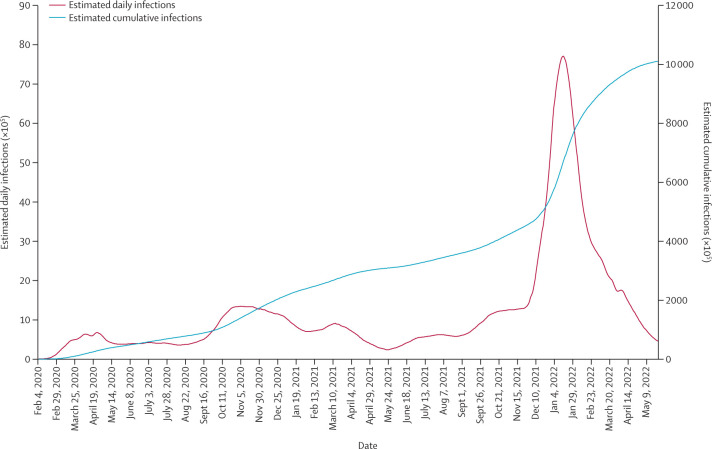
The official cumulative death toll from COVID-19, reported by the Institute for Health Metrics and Evaluation (IHME), was 6·9 million as of May 31, 2022. However, the IHME estimates the true death toll at more than twice this number, 17·2 million,146 and even higher values have been estimated by others (The Economist 147 estimates a death toll of 19·4 million as of February, 2022). Major differences in COVID-19 mortality are seen between WHO regions (for the countries in each WHO region, see appendix p 1). For each WHO region, we show the reported cumulative deaths and total cumulative deaths estimated by IHME until May 31, 2022, both in absolute numbers (figure 2A ) and per million population (figure 2B).
Figure 2.
Estimated and reported cumulative deaths from COVID-19, globally and by WHO region, as of May 31, 2022
Estimated and reported cumulative number of deaths (A) and cumulative number of deaths per million population (B), globally and by WHO region, as of May 31, 2022. All data are from the Institute for Health Metrics and Evaluation (IHME), accessed May 31, 2022.146 Note that the IHME reference scenario provides a range of cumulative and daily estimated infections and cumulative and daily estimated deaths, and we refer to the mean estimate in all figures. Reported cumulative and daily deaths from May 2 to May 31, 2022, were modelled on the basis of past data.
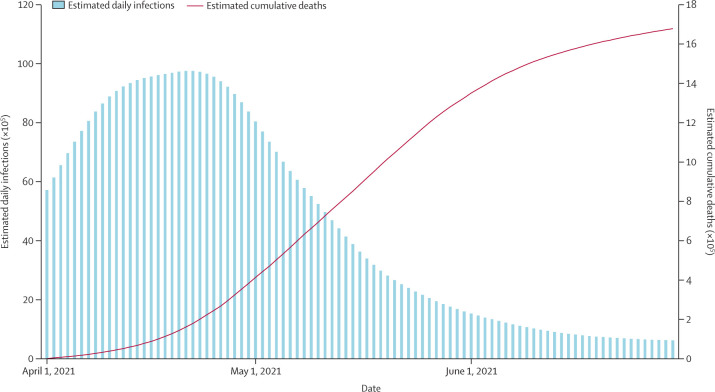
The WHO Western Pacific region, which includes east Asia and Oceania, stands out for its very low average mortality rate, both in terms of reported deaths (125 per million population) and estimated total deaths (300 per million population) attributed to COVID-19. The region with the next lowest number of reported deaths is the WHO African region, for which the reported death rate is 165 per million population; however, the total death rate estimated by IHME is more than ten times higher, at 1774 per million population. The undercounting of deaths is consistent with serosurveys (blood testing for previous infection) that suggest high infection rates in Africa and a massive undercounting of actual infections.148 The WHO South-East Asia region similarly has a relatively low reported mortality rate (366 per million population) and a far higher estimated total death rate (2549 per million population). It is well established that deaths from COVID-19 in India were vastly undercounted during the delta (B.1.617.2) wave of April–June, 2021.149 The WHO Eastern Mediterranean region has a mid-range reported death rate (734 per million population) and a high estimated total death rate (2779 per million population).
The remaining two WHO regions have the highest estimated total death rates: 4144 per million population for the European region and 4051 per million population for the region of the Americas. Particular attention should be paid to Latin America, which has the highest number of excess deaths relative to population. Although the region represents 8·4% of the global population, as of the middle of July, 2022, more than 111 614 cumulative cases of COVID-19 per million population and nearly 2603 deaths per million population from COVID-19 have been reported, according to Reuters.150
The international distribution of COVID-19 death rates is almost the opposite of what might have been expected before the pandemic. On the basis of the 2019 publication of the Global Health Security Index, which ranked the United States first and the UK second in the world in terms of preparedness for pandemics and epidemics, it was widely assumed that the United States and Europe had the strongest pandemic response capacities and would fare best in a pandemic.151 In general, the report gave high preparedness scores to countries in the European region and the region of the Americas, and generally much lower scores to the countries of the Western Pacific region. For example, China was ranked 30th and New Zealand was ranked 32nd. The 2019 assessment failed to predict the poor quality of the public policy response to the pandemic in the European region and the region of the Americas, and the much higher quality of response in the Western Pacific region. Other than in the Western Pacific region, national pandemic control systems were very disappointing compared with expectations in 2019.
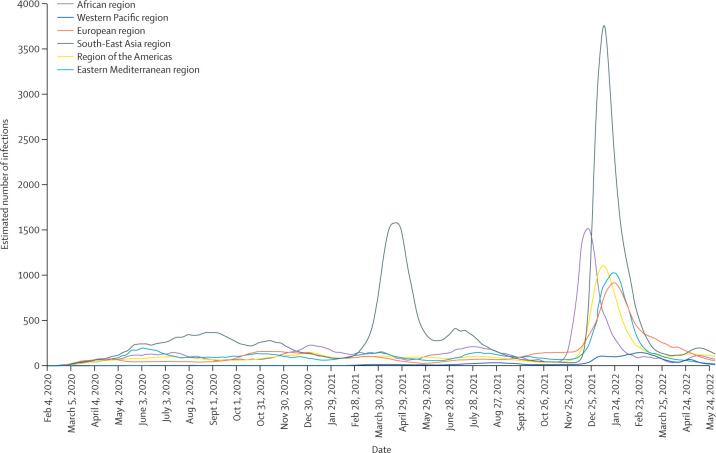
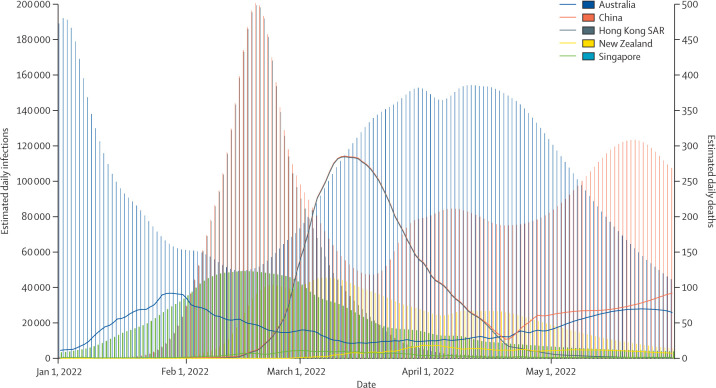
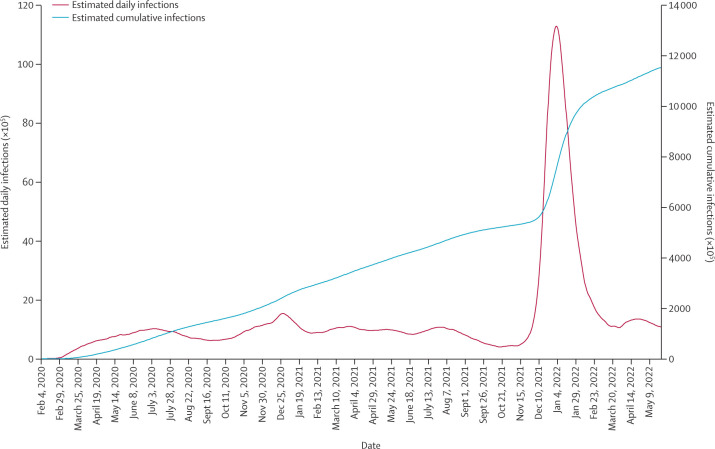
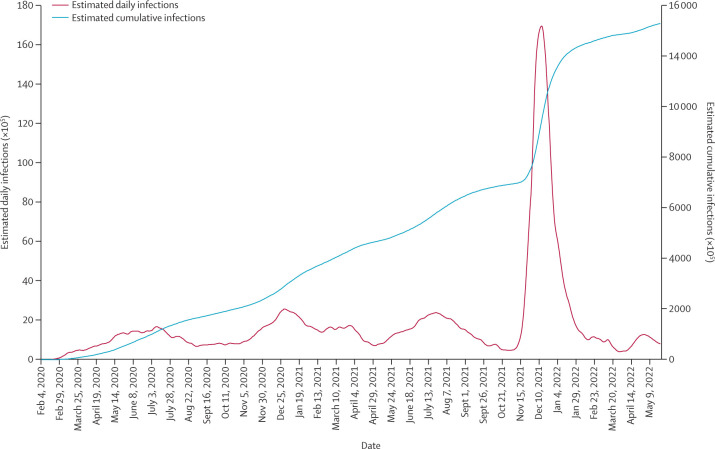
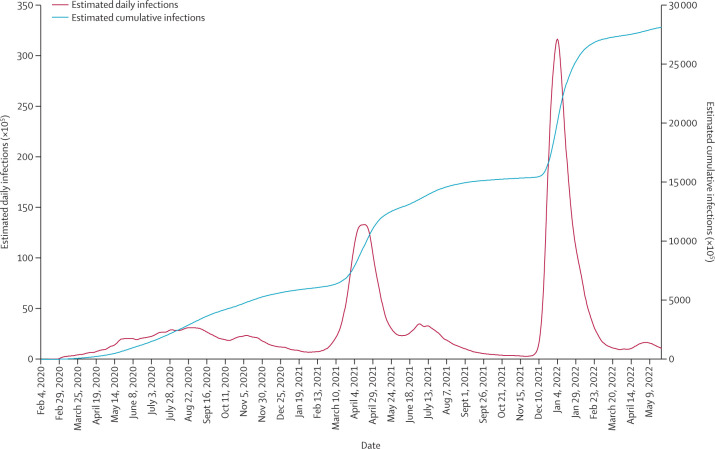
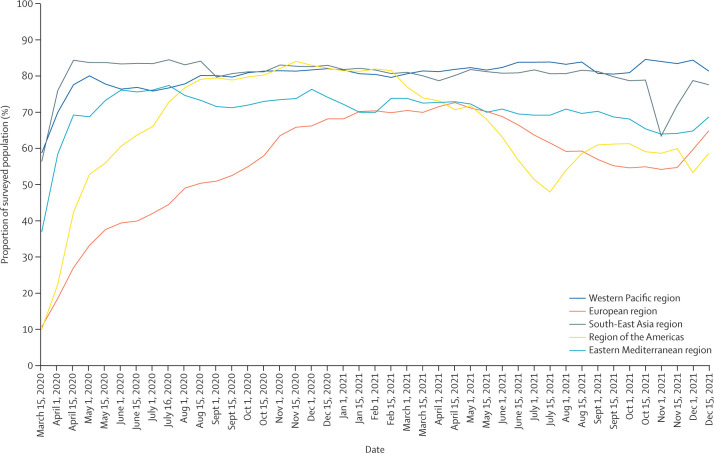
The broad pattern of SARS-CoV-2 transmission across regions can be seen in figure 3 . Only the Western Pacific region held the rate of new infections per day to very low levels. The other regions all experienced several waves, and none used the phases in which infection rates were low to move to a suppression strategy. The biggest wave in terms of deaths, claiming millions of lives in just a few weeks, was the delta wave from April to June, 2021. This wave resulted in astounding mortality, particularly in India, with an estimated 2 million deaths worldwide in these two months. The omicron variant brought another enormous global wave of infections, starting in December, 2021.
Figure 3.
Estimated number of infections per 100 000 population by WHO region, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
Other than regional cooperation among the countries of the Western Pacific region, there was little early effort across governments to coordinate approaches to limit transmission of the virus during the pandemic. National governments have failed to perceive, or to articulate, the core logic of a weakest-link game: to successfully control the transmission of the virus, each country is dependent upon the actions of other countries, so a cooperative approach is necessary to achieve the desired outcome. Instead, national governments generally took actions on their own with disregard for any effects on, or from, other countries.
Regional policy choices in confronting the pandemic
Suppression strategies in the Western Pacific region
The countries of the Western Pacific region generally adopted suppression strategies, and were broadly successful in their implementation. These strategies comprised two phases: from the outbreak in late 2019 until early 2022, when the omicron variant first emerged; and then from early 2022 onwards in the context of the omicron wave. During the first 2 years, the region generally suppressed transmission of the virus, during which they implemented a vaccination campaign in 2021. With the emergence of the omicron variant, most countries of this region then shifted from suppression to mitigation as they adopted a policy known as living with the virus, counting on high vaccination coverage to keep mortality rates relatively low. Only China maintained a suppression strategy during the omicron phase, resorting to new lockdowns of the population in major urban areas.
Following the initial outbreak in Wuhan at the end of December, 2019, around 3000 confirmed new cases of COVID-19 per day were reported in China during February, 2020. Thereafter, China succeeded in suppressing the pandemic to fewer than 100 new cases daily by early March, 2020, and to fewer than ten new cases per day by late April, 2020. The methods of suppressing transmission included a rigorous temporary lockdown of Hubei Province, combined with aggressive case-seeking, large-scale testing, tracing of contacts, use of QR codes to track the movement of individuals, and the isolation of all infectious people and their close contacts.152 China closed its international borders and required new arrivals to quarantine for an extended period. Notably, China was intent to contain the pandemic from Jan 23, 2020, adopting a policy that became known in China as the zero-COVID strategy.153, 154
From early 2020 onwards, Australia, Cambodia, China, Hong Kong SAR, Lao PDR, New Zealand, Singapore, Viet Nam, and several small Pacific island states attempted to pursue a suppression strategy based on the Asia-Pacific Strategy for Emerging Diseases and Public Health Emergencies, which was adopted by the WHO Western Pacific region in the aftermath of the epidemic of severe acute respiratory syndrome in 2003.155 Singapore was the only country of the Western Pacific region to have a substantial outbreak during the first half of 2020, which occurred when COVID-19 spread through the hostels of migrant workers.156 The other countries of the region maintained fewer than ten cases per million people per day for most of 2020.146
In 2020, transmission was suppressed without the benefit of vaccines. In 2021, countries of this region implemented successful vaccination campaigns alongside their suppression strategies. By the end of 2021, Australia, Cambodia, China, Hong Kong SAR, New Zealand, Singapore, and Viet Nam had all achieved full vaccination rates of adult populations of more than 60%.157 At the end of 2021, the omicron variant reached the region, and both the feasibility and desirability of continuing the suppression strategy were called into question. The R 0 of the omicron variant is several times higher than that of the previous variants, making the feasibility of a suppression policy exceedingly difficult (figure 4 ). The social costs of transmission of the virus were considerably reduced, but certainly not eliminated, by the widespread—though incomplete—vaccination coverage achieved during 2021.
Figure 4.
Estimated daily infections and estimated cumulative infections in the Western Pacific region, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
Owing to the difficulty in continuing the suppression strategy and the widespread vaccination coverage, most of the countries of the Western Pacific region relaxed their suppression strategies in early 2022, reverting to a more limited mitigation strategy. Cases of COVID-19 rapidly increased in Australia, Hong Kong SAR, New Zealand, Singapore, and Viet Nam in the first months of 2022, and deaths rose too, yet the death rates remained low because of the vaccination coverage (Figure 5, Figure 6 ). As a result, cumulative deaths per 100 000 population as of May, 2022, in the Western Pacific region were far lower than in any other region of the world. The suppression strategy during 2020 and 2021 therefore had a lasting benefit, as it gave time for high rates of vaccination coverage.
Figure 5.
Estimated daily infections and estimated daily deaths in the Western Pacific region during the omicron (B.1.1.529) wave, Jan 1–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
Figure 6.
Estimated daily infections and estimated daily deaths in Australia, China, Hong Kong SAR, New Zealand, and Singapore during the omicron (B.1.1.529) wave, Jan 1–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
China, in contrast to most of the other countries in the region, chose to maintain a strict suppression strategy even during the omicron wave. Given the remarkable infectivity of the omicron variant, suppression during this period has required new and stringent lockdowns of the populations in major urban centres that have omicron outbreaks, including Shanghai and Beijing. There has been debate within China about the balance of costs and benefits of the zero-COVID policy with such an infectious variant. China is using the period of lockdowns to increase vaccine coverage in the population that remains unvaccinated.
Flatten-the-curve policies in the Americas
The contrast between the policy response of the Western Pacific region with that of the region of the Americas has been stark from the outset. Few if any countries in the Americas were prepared for the pandemic. In the United States, the initial test kits provided by the US CDC were faulty,158 and during the first few months of 2020, the rate of testing was very low and tests were only available sporadically.159, 160, 161 Local public health departments capable of systematically testing, tracing, and isolating infected people were scarce, and US federal officials repeatedly downplayed the importance and risks of the outbreak. The United States, like many member countries of the Organisation for Economic Co-operation and Development, chronically underinvested in public health before the pandemic, devoting only 2·5–3% of the total health sector budget to public health.162, 163
The high mortality rate of the region of the Americas reflects the failures of this region to take concrete measures to suppress the epidemic, and high vulnerability to deaths from COVID-19 due to structural characteristics. Such characteristics include older populations;163, 164, 165 a high prevalence of comorbidities (eg, diabetes, chronic obstructive pulmonary disease, cardiovascular disease, and kidney disease) within the population;166, 167 the high proportion of the population living in congregate settings such as care homes,168, 169 prisons,170 worker hostels, and homeless centres;171 and social determinants of health including racial and ethnic disparities, income inequalities, and inequitable access to high-quality health care.172, 173 Another factor was the increase in anti-vaccine propaganda in the Americas that caused tens of millions of people to refuse vaccines, and hundreds of thousands to needlessly lose their lives.16, 174
Evidence suggests that the case ascertainment rate (defined as the number of confirmed new infections relative to the number of actual new infections) was much less than 20% in the first half of 2020175—meaning that viral transmission increased rapidly during February and March, 2020, with little awareness by authorities and the public until mid-to-late March. By early April, 2020, the United States was reporting around 30 000 cases per day (90 per million population), with the actual number of cases estimated to be more than five times higher. Between Feb 4, 2020, and May 31, 2022, there were an estimated 1·2 million deaths attributed to COVID-19 in the United States (figure 7 ).
Figure 7.
Estimated cumulative infections and estimated cumulative deaths in the United States, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
The situation in the rest of the Americas was similar (figure 8 ). The pandemic arrived several weeks later in much of Latin America, but it then raged with little respite or sustained control. In South America as a whole, confirmed new cases reached 60 per million population on May 22, 2020, and then never decreased below that rate until the end of 2021. Canada also sustained major waves of infection, although generally with fewer cases per day per million people than in the United States.
Figure 8.
Estimated cumulative infections and estimated daily infections in the region of the Americas, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
Many countries in the Americas imposed temporary lockdowns from roughly mid-March to the end of April, 2020. Yet, unlike in the Western Pacific region, these lockdowns were not meant to be a prelude to comprehensive suppression through testing, tracing, and isolating, and complementary policies on travel, public hygiene, and other regulations. The lockdowns in the Americas were generally designed to slow the transmission of the virus rather than to keep R below 1. These lockdowns were described by most countries as flattening the curve to avoid an overflow of patients with COVID-19 in hospitals. No countries in the Americas pursued a suppression strategy.
Flatten-the-curve policies in Europe
Governments in the European region did not aim to suppress the pandemic, only to slow the transmission of the virus. Several countries in western Europe saw large numbers of infections early in the pandemic—notably Belgium, France, Germany, Italy, Spain, and the UK. International travel to and from all these countries is extensive, and many infected people arrived from China during January and early February, 2020.176, 177 There was little testing in the first weeks of the outbreak, and a massive surge of cases occurred in March, 2020. To lessen the pressure on hospitals, European countries adopted tough lockdown measures,178 although—as in the region of the Americas—the focus was on flattening the curve rather than on ultimately suppressing the pandemic.
By June, 2020, case transmission in Europe declined to low levels (figure 9 ), yet European governments failed to implement continued rigorous measures of physical distancing (including the wearing of face masks and bans on large gatherings). On the contrary, the decline in the number of cases by June, 2020 led governments in Europe to rescind control measures and to encourage a return to life as usual, especially in the context of Europe's upcoming summer holidays; this relaxing of control measures led to another wave of infections in countries across Europe in September, 2020.179, 180
Figure 9.
Estimated cumulative infections and estimated daily infections in the European region, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
This second wave gave rise to renewed restrictions and partial lockdowns throughout Europe, which again led to a decline in cases by June, 2021. Once again, policies were eased in time for vacations in July, 2021, setting the basis for a third wave in October, 2021—this time due to the new delta variant, which was first identified in India. A moderate decline in cases of the delta variant by late October and November, 2021, was soon followed by a fourth wave of infections due to the omicron variant, beginning in December, 2021. Compared with other WHO regions, Europe was relatively more successful at vaccinating a substantial portion of its population rapidly in 2021, which contributed to limiting the number of severe cases and deaths in subsequent outbreaks later in 2021 and in 2022.181
Sub-Saharan Africa's hidden epidemic
At the outset of the pandemic, conditions of poverty, urban crowding, and fragmented health-care systems gave rise to fears that sub-Saharan Africa would suffer the most extreme outcomes in the world as the virus spread through the continent. On the surface, at least, that was not the case, as the numbers of reported cases and deaths remained low. Estimated infections are about 100 times higher than reported infections in the region, but still remain lower than in all other WHO regions (figure 10 ). Although some scientists speculated that pre-existing immunity from intensive exposure to other pathogens—including other coronaviruses—could have contributed to the African region's low reported case load,182 a simpler explanation now seems most likely. Several serosurveys suggest that Africa experienced large waves of infection but that most cases went unreported, in part because they did not lead to severe disease. A serosurvey in six districts of Zambia showed that the case ascertainment rate was only one reported case per 92 actual infections, or 1·1%.183 Similar findings apply to other countries—such as the Republic of the Congo,184 the Democratic Republic of the Congo,185 Malawi,186 and Kenya187—suggesting that up to 80% of the population had already been infected by COVID-19 before the arrival of the omicron variant.
Figure 10.
Estimated cumulative infections and estimated daily infections in the African region, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
Although partly attributable to low testing capacity, the under-reporting of cases is also driven to an important extent by Africa's demography: the population is young, giving rise to a relatively high proportion of asymptomatic and mild cases. The median age in Africa is around 18 years, compared with between 30 years and 35 years across Asia, the Americas, and Oceania, and around 42 years in Europe.188 Because the risk of severe disease and death from COVID-19 increases exponentially with age,189 it is not surprising that Africa—and sub-Saharan Africa in particular—has recorded relatively fewer deaths, despite very limited containment policies and generally inadequate health systems. Even estimates of the total number of deaths from COVID-19 in the African region, which are up to ten times higher than the official numbers, place it as the region with the second-lowest number of deaths per million people.
South-East Asia and the delta surge
The South-East Asia region saw a wide disparity in health-system capacities and consequent outcomes for COVID-19 management, spread, and mortality. Several countries (eg, Sri Lanka,190 Thailand,191 Lao PDR,192 and Cambodia193) were able to contain the spread of COVID-19 in the first year of the pandemic as a result of effective contact tracing, wearing of face masks, and physical distancing. Other countries (eg, Pakistan, Bangladesh, Malaysia, and India) saw sharp rises in infections, but death rates remained relatively low.146 The delta wave caused a spike in cases in most countries in the region, with much higher mortality, although actual deaths have been substantially under-reported in several countries (figure 11 ). This under-reporting was perhaps most notable in India during the delta wave from March to July, 2021. India was among the first countries to impose travel restrictions, suspend international flights, and impose a strict lockdown early in the pandemic.194 In March, 2020, India had 654 cumulative confirmed cases of COVID-19,146 and the adopted restrictions aimed to prevent community transmission and give the health system time to ramp up.
Figure 11.
Estimated cumulative infections and estimated daily infections in the South-East Asia region, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
After lockdown was relaxed at the end of May, 2020, India saw a surge of cases during June and July; however, because case counts had decreased by the end of the year, the Indian government relaxed most controls early in 2021.195 In March, 2021, two factors combined to markedly increase the number of infections. First, the highly infectious delta variant emerged, and other variants of concern arrived from other countries.196 Second, several events in the country—such as elections, public protests, and religious festivals—brought large aggregations of people together, and most participants in these events did not wear face masks.197, 198
The combination of new variants and crowds proved devastating in India. All levels of government—central, state, and local—were unprepared for the speed and the scale of the delta surge as it gathered momentum in March, 2021. Hospitals were overwhelmed within weeks, and breakdowns in the medical supply chain contributed to a severe shortage of oxygen, hospital beds, and pharmaceuticals.199 In smaller towns and rural areas, large numbers of patients went untreated.200
India reported roughly 20 million COVID-19 infections and 250 000 deaths attributed to the disease between Jan 1 and June 30, 2021, but the actual numbers are estimated to be vastly higher. Seroprevalence of COVID-19 IgG antibodies in non-vaccinated individuals older than 6 years increased from 24% in December, 2020 and January, 2021, to 62% in June and July, 2021, confirming that hundreds of millions of people were infected during the delta wave.201 The IHME estimates that there were around 417 million infections and 1·6 million deaths from COVID-19 in India between April 1 and July 1, 2021, compared with just 18 million reported cases and 252 997 reported deaths (figure 12 ). Another study estimates between 3·1 million and 3·4 million deaths from COVID-19 in India between the start of the pandemic and Sept 1, 2021, compared with 440 000 reported deaths; these figures suggest that the reported death count was roughly 14% of the actual value.149
Figure 12.
Estimated daily infections and estimated cumulative deaths in India during the delta (B.1.617.2) wave, April–June, 2021
Data from the Institute for Health Metrics and Evaluation, accessed Feb 19, 2022.146
After the delta surge, cases decreased markedly and vaccination efforts accelerated; as of Sept 1, 2022, more than 76% of the eligible population of India had been vaccinated with a single dose and more than 70% were fully vaccinated.202 Despite the omicron surge in January, 2022, hospitalisation rates and deaths remained low.
Across the South-East Asia region, the omicron wave saw infections spike, even in countries that had managed to contain the spread of COVID-19 in the first year of the pandemic (figure 11). However, hospitalisation rates and deaths remained low in most countries. By June, 2022, at least 60% of the population in all countries except Myanmar had received a full course of vaccination.181
The Eastern Mediterranean region
The Eastern Mediterranean region has reported relatively low death rates. However, as in the African and the South-East Asia regions, the number of deaths has been substantially under-reported (figure 13 ). With ongoing conflict in Palestine, Yemen, Syria, and Somalia, in addition to the takeover of Afghanistan by the Taliban in 2021, surveillance and health systems have limited capacity. Additionally, with the prevalence of refugees and displaced people congregating in emergency shelters and crowded settings, disease outbreaks are highly likely.
Figure 13.
Estimated cumulative infections and estimated daily infections in the Eastern Mediterranean region, Feb 4, 2020–May 31, 2022
Data from the Institute for Health Metrics and Evaluation, accessed May 31, 2022.146
This region has great extremes in terms of COVID-19 vaccination coverage. For example, in the United Arab Emirates, about 90% of the eligible population is fully vaccinated and 95% is vaccinated with at least a single dose as of June, 2022.203 However, in Yemen, only 2% of the population is fully vaccinated and 5% is vaccinated with at least one dose.204 In Afghanistan, about 13% of the eligible population is fully vaccinated, with about 10% projected to be vaccinated with at least a single dose.205 In addition to the destabilising effects of political instability and violence, the low vaccination rates are also related to low literacy rates and to vaccine hesitancy among the population.
Premature lifting of public health and social measures
In March, 2022, governments around the world removed many of the remaining public health and social measures regarding face masks, indoor gatherings, large events, physical distancing, and testing, especially in countries with high vaccination rates. This removal of measures coincided with the emergence and prevalence of the highly infectious omicron variant, with a reproduction rate estimated to be three to four times that of the delta variant.206 The omicron variant led to the greatest surge yet in the number of confirmed cases per day, estimated by the IHME to be roughly 45 million per day at the peak in January, 2022, compared with the previous worldwide peak of around 15 million per day in April, 2021. IHME estimates that 4·3 billion people, or 54% of the world's population, were infected with SARS-CoV-2 between Dec 1, 2021 and May 31, 2022.146
There are many costs associated with the premature lifting of public health and social measures. First, a considerable portion of the population is not immunised, and many vulnerable groups—such as people who are immunocompromised and who cannot mount an effective immune response to vaccination—will never be able to achieve effective immunity.207 Second, vaccination coverage provides only partial and waning protection against infection, although more protection against hospitalisation and death.208 Additionally, coverage of a population with a third booster dose is in general far lower than coverage with two vaccines. Third, further variants and returning waves of infection can be expected as current immunity wanes, so dismantling basic controls and even advertising the end of the pandemic is premature, and likely to be harmful when restrictions become necessary again. Fourth, high infection rates mean high rates of long COVID, which disrupts education and jobs, brings physical and mental suffering to individuals and their families, creates a considerable burden on health services, and undermines economic recovery.
One widespread view among epidemiologists is that the virus is likely to become endemic, recurring seasonally (notably during the cold weather in each hemisphere, because of the much greater risk of indoor transmission) yet with lower mortality, similar to the annual mortality burden of seasonal influenza,209 and with annual vaccines targeting the dominant variant, as for influenza.210, 211 However, there is little assurance that we have achieved such predictability, and influenza too can give rise to devastating new variants and pandemics, such as the outbreaks in 1957–58 and 1968 that are each estimated to have claimed between 1 million and 4 million lives.212, 213, 214 Although the omicron variant of SARS-CoV-2 has been less lethal than the preceding delta variant, future variants are as likely to be more virulent or less virulent, and existing vaccines are likely to become less protective against serious illness and death.
Three major risks should be kept in mind at this stage. First, future variants might be highly infectious and deadly. Second, people who are currently unvaccinated (ie, have not received any doses of a COVID-19 vaccine)—roughly 2·5 billion people or 33% of the global population as of Aug 19, 2022146—remain vulnerable to morbidity and mortality and provide opportunities for the virus to circulate freely, increasing the risk of dangerous mutations occurring. Third, the omicron wave has shown that serious economic disruptions can occur even in highly vaccinated populations,215 as it led to shortages of health and other essential workers, school closures, disruptions to business operations, and prevented the restoration of tourism and international travel.
Widespread political ineffectiveness
One of the most striking occurrences of the pandemic has been the irresponsibility of several influential political leaders. National and local politicians act on various motives, including political timelines and electoral cycles, fears of public backlash, narrow economic interests, and lack of knowledge and expertise. Because the pandemic was a novel experience for most leaders, humanity was vulnerable to their learning curves, ignorance, and mixed motives. National responses were often improvisational, occasionally bordering on the absurd.216 Several national leaders made highly irresponsible statements in the first few months of the outbreak, neglecting scientific evidence and needlessly risking lives with a view to keeping the economy open.217, 218, 219, 220, 221, 222, 223
Leadership styles and public messaging have been instrumental in building trust and leveraging effective responses, and we note that the gender of political leaders seems to have had a role in the rhetoric, with women leaders more often concerned than male leaders about individual-scale effects and social welfare.224, 225 A rather small group of governments, many led by women, kept death rates much lower than in other countries. The Western Pacific region—including Australia, China, New Zealand, Republic of Korea, and Taiwan, Province of China—was largely successful at maintaining relatively low death rates.226 In Europe, two Nordic countries stand out as having lower death rates than the rest of the continent—Iceland (about 210 deaths per million population227) and Norway (about 280 deaths per million population228). In contrast with its neighbour, Norway, Sweden's response was lax,229 resulting in a much higher death rate (about 1500 deaths per million population).230 National policy choices made a vast difference in health outcomes.
Disinformation in media
False news, propaganda, and demagoguery are nothing new. Yet the means of deploying these malicious forces change over time with each new medium of communication. In the past two centuries, newspapers, radio, and television have each served as purveyors of misinformation and disinformation. Now we are experiencing new forms of disinformation through digital media,231 which are especially powerful in disseminating ideas because of their reach (eg, Facebook has nearly 2·4 billion subscribers), immediacy, relative anonymity, and the ease of creating echo chambers of tightly clustered groups receiving utterly different impressions of the facts from other online communities.232, 233, 234, 235
The COVID-19 pandemic is not the first crisis in which misinformation has been shared,236 and it is not the only issue that is permeated by lies and distrust. The spread of misinformation and disinformation is common among climate change deniers, the tobacco industry's continued fight against warning labels, and parents who refuse or delay routine childhood vaccinations.237 The rapid speed at which news is shared, the deliberate spread of misinformation and disinformation by political leaders, and the lack of truth-telling and adequate oversight creates an overwhelming environment that fosters distrust in health officials and promotes the idea that individual opinions have equal weight to the best available scientific evidence.237, 238 This distrust has real-world consequences. One study in Italy found that poor public understanding of the risk of COVID-19 infection, even during the peak of COVID-19 incidence in 2020, was related to 11 411 people breaking lockdown regulations.238 Some media outlets erroneously promoted dangerous or experimental treatments, such as hydroxychloroquine and ivermectin, resulting in unnecessary visits to hospital emergency departments and shortages of such medications for people with legitimate needs.239, 240, 241
All countries proved to be highly vulnerable to disinformation and misinformation regarding the pandemic, with one study documenting that 46% of people in the UK and 48% of people in the United States were exposed to false information.242 A 2020 study of the most-viewed videos about COVID-19 on YouTube found that more than 43% of these videos contained misleading information.243 In the United States, the political far-right has promoted anti-science rhetoric, as shown by their opposition to COVID-19 vaccines and anti-COVID-19 prevention measures. Anti-science rhetoric and disinformation about COVID-19 are now promoted by several elected members of the US Congress,244 and are often disseminated by cable television news channels and podcasts. By some estimates, between 100 000 and 200 000 Americans lost their lives because they refused COVID-19 vaccinations and were open in their defiance.245 This anti-science movement has globalised with tragic consequences.246
Pope Francis raised his powerful voice against the dangerous infodemic regarding vaccines, declaring: “To be properly informed, to be helped to understand situations based on scientific data and not fake news, is a human right.”247 WHO is the leading international authority on health and should be supported by its member states and by other UN agencies to lead the global response to a health crisis. However, various political leaders publicly undermined WHO, disseminated campaigns against it and its advice, and even tried to halt its funding.234, 248, 249, 250, 251
Public attitudes towards pandemic control and investments in behavioural sciences
Public attitudes towards the pandemic differed markedly around the world. Public attitudes are shaped by various factors, including national culture, education level, peer groups, social media, and the actions and statements of national leaders. Other important aspects include emotions, past habits, capability, convenience, and social norms.252
Human behaviour is central to transmission of the disease and suppression of the pandemic. Behavioural science provides evidence about the effectiveness of interventions and policies across contexts and the processes required to bring about change; for example, evidence-based optimal behaviours for pandemic control include getting vaccinated and tested, isolating when infectious, wearing face masks, and physical distancing.253 At a minimum, behavioural change requires appropriate motivation, capability, and opportunity; the absence of any one of these will undermine public health efforts. The COM-B model252 is a synthesis of frameworks of behaviour change has identified nine types of intervention strategy and seven policy options to underpin them. These strategies are most effective when selected in combination and according to a scientific understanding of behaviour in the political and socioeconomic context.
Motivations for behaviour change include self-interest, belief in the effectiveness and feasibility of behaviours, and reducing aversive emotions. Capability includes knowing exactly what to do, when, and why, and is closely linked to health literacy. Desired behaviour will not occur with motivation and capability if people do not have the opportunity—both physical (eg, easy access to vaccines and financial resources to self-isolate) and social (eg, normative influences to wear face masks). Health and safety cultures relating to infectious diseases should be built into societies, embedding risk assessment and management into everyday life to maintain behaviours.254
There is evidence that trust in government helps to promote prosocial behaviours within the population. An empirical study published in 2021 concluded that greater trust in government regarding COVID-19 control was cultivated for governments that were perceived as well organised, fair, and to be disseminating clear messages and knowledge on COVID-19. This greater trust in government was also significantly associated with a greater adoption of health and prosocial behaviours and lower rates of decline in these behaviours over time.255
Differences in national cultures also shape national responses. Cultural psychologists, for example, have distinguished between so-called tight and loose cultures, with tight cultures characterised by strong public adherence to social norms and loose cultures by lax adherence.256 Societies also differ along a spectrum of individualism versus collectivism in terms of social norms, in which individualism champions the freedom of individual choice whereas collectivism champions conformity with the group. Tight and collective cultures were more attuned than loose and individualistic cultures to respect the social norms of physical distancing and to adhere to isolation when potentially infected, leading to greater success in controlling the pandemic.
Social media also had a crucial role in how public health and social measures were perceived by the public. Scientific understanding of the virus and its characteristics have continued to evolve throughout the pandemic, and as more information has been gathered about the genetic make-up, reproduction rate, and methods of transmission of the virus, and about new variants of concern, public health and social measures have had to be adjusted. However, the reliance of social media on so-called clickbait headlines and short commentaries has had a polarising effect on many communities. Social media left little room for the deep discussion of issues and enabled rapid orthodoxies to develop, which in turn often delegitimised necessary adjustments to advice and to public health and social measures in response to the evolving understanding of the virus. The preparedness of populations also differed as a result of their different exposures to and experiences with previous pandemics. Residents of countries in the Western Pacific region, remembering the 2003 epidemic of severe acute respiratory syndrome, strongly adopted public health and social measures such as wearing face masks, increasing hygiene, and avoiding large public gatherings. Figure 14 shows survey data from YouGov on the use of face masks in public places. Notably, survey participants in countries of the Western Pacific region and the South-East Asia region began wearing face masks early in the pandemic and maintained the highest reported use throughout 2020–21. Surveyed populations in the Eastern Mediterranean region, the European region, and the region of the Americas were later and slower to start wearing face masks, missing an early opportunity to suppress the pandemic. Additionally, after reaching a maximum in late 2020, the use of face masks declined in these regions at higher rates than in the Western Pacific region. YouGov did not conduct this survey in any countries in the African region.257
Figure 14.
Proportion of the surveyed population who wear face masks in public places by WHO region, March 15, 2020–Dec 15, 2021
Data from YouGov.257
Another indicator of public attitudes to prosocial public health measures is public protests over COVID-19 restrictions. The Carnegie Endowment for International Peace tracks global protest actions and identifies protests that are related to COVID-19.258 Such protests have overwhelmingly taken place in the region of the Americas and the European region, as shown in figure 15 . Emphasis on the value of liberty, in particular in high-income countries within these regions, has been widely invoked in these protests to reject mandates on face masks and vaccines, alleging that such mandates infringe on individual freedom.
Figure 15.
Countries in which coronavirus-related protests were held, March, 2020–November, 2021
Countries in which protests were held, coloured by WHO region. Protests were most heavily concentrated in the European region (dark grey; 22 protests) and the region of the Americas (dark blue; 16 protests), with only a few protests in the Western Pacific region (light blue; four protests), the South-East Asia region (yellow; two protests), the Eastern Mediterranean region (orange; five protests), and the African region (purple; one protest). For countries in light grey, no protests were recorded. Data from the Carnegie Endowment for International Peace.258
An additional and alarming aspect of the public response in many countries has been widespread vaccine hesitancy, encouraged by a hostile and coordinated anti-vaccine movement that has spread dangerous and false information about the health risks of vaccines and has campaigned against vaccine mandates. Anti-vaccine disinformation in the United States has been traced to well organised right-wing groups that use targeted social media.259 Global evidence suggests that vaccine hesitancy is highest among people with lower levels of formal education and with lower incomes, emphasising the need for more evidence-based health education and communication on preventive care and health maintenance in public schools and from government, trusted community leaders, and medical professionals, in addition to the regulation of anti-science messages on social media.174, 260, 261
Unequal health effects of the pandemic
The effects of the pandemic have been hugely unequal across the world, both within and between countries. Disease effects can be distinguished from economic and social effects, although they are deeply intertwined. Case fatality rates (defined as the number of confirmed deaths per confirmed case) have been high in older people, with mortality rates at least ten times higher in people older than 65 years than in those younger than 40 years. Other groups that have been disproportionately affected include people with comorbid medical conditions, particularly those with immunocompromised status; people living with physical disabilities or mental disorders; residents of congregant settings; and essential workers.262, 263, 264, 265, 266 First responders, service-sector workers, and other essential workers often receive low wages and, in some countries, low access to high-quality health care, and therefore disproportionately experience health, economic, and social effects. The majority of health-care workers, in particular, are women.
Ensuring mental health and wellbeing is a crucial part of preparedness and response to pandemics and other similar threats.267 There does not need to be a trade-off between saving lives and safeguarding mental health.268, 269 A study conducted across 15 countries found a small negative association between COVID-19 policy stringency and mental health, consistent with previous work, and a negative association between the intensity of the pandemic (measured by the average number of deaths per day per 100 000 people) and mental health. However, because early and targeted suppression policies not only minimise deaths but also lead to lower average levels of stringency through better transmission control, the mental health of people in countries that aimed to suppress the virus was found to be equivalent to or better than the mental health of people in countries with a flatten-the-curve strategy.270
It is clear that various aspects of mental health declined during the COVID-19 pandemic.271 Numerous sources documented a clear and consistent pattern of increased anxiety and depression in the early months of the pandemic, which declined during later months in some countries but not in others.272 A systematic review estimates more than 53 million additional cases of major depressive disorders and 76 million additional cases of anxiety disorders globally in 2020.273 Data on short-term emotions, life evaluations, loneliness, and self-harming behaviour were more mixed. Daily emotions were more negative (fewer positive emotions and more negative emotions), whereas reports of loneliness and self-harm initially increased but later returned to their pre-pandemic levels.
Population-level trends conceal the extreme strain felt by some individuals. Pre-existing inequalities in mental health have remained during the pandemic. For instance, people living in marginalised communities with lower socioeconomic status and mental health conditions reported poorer mental health than the general population.30, 274 The pandemic has also introduced new profiles of risk, with younger people (aged 18–34 years), women, and people with children under the age of 5 years showing the largest increase in psychological distress.275
Stark socioeconomic effects
Socioeconomic divides have widened since the start of the pandemic. First, essential workers are disproportionately concentrated among vulnerable minority and low-income communities. Since the start of the pandemic, many people whose work is computer-based or telephone-based have been encouraged to work from home.276, 277 People who could work online, such as office workers, fared better in terms of health and socioeconomic wellbeing than goods-producing workers (eg, those in agriculture, mining, manufacturing, or construction) and workers in industries categorised as essential (eg, health-care workers and grocery store workers) who have been required to work in-person. Onsite work often entailed substantial risk of infection (such as at meatpacking plants) or temporary closures of worksites. Workers of colour in the United States, who are over-represented in high-risk, essential industries, are also more likely than other populations to have lower incomes, live in multigenerational households, and use public transport to travel to work. These groups of workers have been at the greatest risk of serious illness and death from COVID-19.278 Inadequate efforts were made to prioritise the health and safety of these workers, first in requiring precautions in their workplaces, and later in reducing structural barriers to accessing vaccines when they became available.262, 263, 279
Workers in the retail trade, personal services, and leisure and accommodation (eg, restaurants, hotels, tourist locations, entertainment, and sports) were also especially affected by closures and lockdowns. Of the 22·1 million job losses in the United States between January and April, 2020, 8·3 million (38%) occurred in the leisure and hospitality sector,280 although this sector accounted for only 11% of pre-pandemic employment.281 In general, these differences strongly exacerbated income inequalities, as the online workforce is considerably higher paid on average. Additionally, informal employment accounts for 60% of global employment; the International Labour Organization projected in early 2020 that 1·6 billion informal workers would be the most severely affected and would lose 60% of their earnings in the first month of the pandemic.282
In India, nearly 1 million front-line community health workers went on strike in December, 2021, owing to a lack of protective equipment and wages of $40 a day, as they were asked to be the soldiers of the pandemic.283 Additionally, health workers worldwide are facing increased violence, initially because they were viewed as vectors of disease and then because of polarised politics surrounding vaccination.284
Second, women have borne a disproportionate socioeconomic burden,285 and existing widespread gender inequalities in terms of labour, income, personal safety, education, and food security intensified over the course of the pandemic, with important regional, national, and local variations and disparities.286, 287, 288 Although the overall death toll of COVID-19 is higher among men than women,289 survey results confirm a disproportionate effect of the pandemic on the livelihoods of female workers.290, 291, 292 Worldwide, women comprise 70% of front-line health and social workers.293 The poorest women subsidise health care globally; it is estimated that half of the contributions by women to health care, which totals approximately $1·5 trillion annually, are in underpaid and unpaid work.294 Women faced an enormous increase in the demands on their time during the pandemic.295, 296 When parents are charged with supervising a child's remote learning, or when they cannot rely on schools consistently being open (perhaps due to hybrid schooling situations or quarantines after COVID-19 exposures), they might not be able to do their own work. These situations had a disproportionate effect on women, who dropped out of the labour force at higher rates than men.297, 298 In Latin America, the share of women in the workforce declined from 51·4% in 2019 to 46·9% in 2020. In the United States, the number of women in the workforce who were mothers decreased by 21·1% between March and April, 2020, whereas the number of working fathers decreased by only 14·7%.299
Women are also disproportionately represented within the population of care centres for older people, many of which experienced outbreaks of COVID-19 and many deaths from the disease. In the United States, for example, women account for 70% of residents in nursing homes.285 Women faced an epidemic of domestic violence alongside the COVID-19 pandemic, as confirmed in several meta-analyses.300, 301 Additionally, a WHO survey showed that across 105 countries, 68% of women faced disruption in family planning services early in the pandemic.302
Third, children younger than 18 years are considerably affected by the indirect repercussions of the pandemic.303 Nearly 80 million children are at risk of vaccine-preventable diseases as a result of fragile health systems that have been disrupted by the pandemic.2 Children also face threats to their immediate and long-term wellbeing from interruption in other essential services, particularly in-person schooling.304
Resources permitting, schools provide food, safety, nurturance, sociality, cognitive development, and education.305 However, 195 countries closed schools during the pandemic, affecting more than 1·5 billion children and young people and posing enormous long-term and unrecoverable costs to them, their parents, and the economy.306 School closures have had devastating effects on student learning, mental health, socioemotional outcomes, and lifetime earning potential, such as education backslides, increasing drop-out rates, and increased abuse and neglect. In-person schooling was deprioritised even as other non-essential or less essential community and economic activities continued.307, 308, 309 School closures also affected the safety of children, increasing their exposure to abuse.310 Lack of economic support at home and the lack of protection offered by schools affected girls in particular, as it put them at increased risk of mental health problems, violence, child marriage, pregnancy, female genital mutilation, and HIV infection, with limited or no access to services.304, 310 11·2 million girls and young women globally are now at risk of not returning to care centres, schools, or universities.304
Across the United States and Mexico, at least 62 million elementary-age and secondary-school-age children (aged 5–18 years) were physically out of school for at least 13 months continuously.311 In Latin America, more than 165 million young people stopped attending classes in person.312 To deal with these school closures, the education sector pivoted to online learning and digital resources, immediately redefining access to learning by access to the internet.310 As of December, 2020, 64% of low-income students in the United States were attending school solely via computer, compared with 48% of high-income students. Black (66%) and Hispanic (64%) students were almost twice as likely as White (34%) students to be learning fully remotely, and were also twice as likely as White students who were also remote to have no live access to a teacher.311 UNICEF estimates that a third of the world's schoolchildren were unable to access digital learning.3
School closures have also affected children's physical health, food security, and nutritional status. Since the beginning of the pandemic, UNESCO estimates that nearly 370 million children across 50 countries have missed meals since school closures began, and that globally an estimated 39 billion in-school meals have been missed as a result of pandemic-induced school closures.313 An average of four in ten in-school meals have been missed by children around the world, and this number increases to as many as nine in ten in some countries.310
The absence of a structured, school-led routine and peer interactions has disrupted the lives of children; amplified the anxiety caused by isolation and their fears of the disease; and led to the loss of physical, intellectual, and social engagement. Motivation levels in children have declined because of the inability to play outdoors (which also affects their physical health), meet friends, and be in the classroom. Globally, a median of one in five young people aged 15–24 years said that they often felt depressed or had little interest in doing things.314
One estimate from the World Bank suggests that this generation of children could potentially lose an estimated $10 trillion globally in their life earnings.310 The loss of learning could also potentially increase learning poverty levels to 63% and drive countries even further off-track from achieving their learning poverty goals.315, 316 The estimated economic loss for south Asia due to school closure is projected to be between $622 billion (best-case scenario) and $880 billion (worst-case scenario).310 For 2020 alone, the IMF estimated learning losses from mandated school closures at 20–25% of the school year in advanced economies and twice that in emerging market and developing economies (figure 16 ).318
Figure 16.
Duration of school closures worldwide between March, 2020 and October, 2021
School closure is defined as the government-mandated closures of educational institutions affecting most or all (≥80%) of the student population enrolled from pre-primary to upper-secondary levels. Reproduced from Agarwal R,317 by permission of the International Monetary Fund.
As the pandemic entered its third year, schools continued to impose stringent restrictions. Although efforts should be made to reduce undue risk of infection to children, it should further be recognised that it is possible to keep schools open without putting students and adults at excessive risk.319, 320 Because of the lower risk of severe COVID-19 among children, and considering the harms of school closures, in-person learning should be prioritised.
Fourth, wealthy households experienced an increase in net worth even as hundreds of millions of workers worldwide lost their jobs. When the pandemic began, the major central banks (the Federal Reserve, the European Central Bank, the People's Bank of China, the Bank of Japan, and the Bank of England) engaged in massive monetary expansion, commencing around March 20, 2020, to forestall a credit squeeze or financial panic. This expansion resulted in an enormous increase in financial asset prices, especially of equities but also including real estate and wholly speculative assets such as cryptocurrencies and non-fungible tokens. The net worth of the richest ten people in the world increased to $1·5 trillion,321 and these ten people possess six times more wealth than the poorest 3·1 billion people.
Severe lockdowns also had important social, gender, and economic consequences. In Latin America, approximately 26 million people lost their jobs in 2020; this region had the largest losses in terms of hours worked worldwide and reduction of labour incomes.312 Lockdowns also resulted in increased gender-based violence. Although the United Nations Population Fund projected in April, 2020 that if the lockdown continued for 6 months or more, 31 million additional cases of gender-based violence could be expected to occur, lockdown policies remained gender-blind.322 Stringent lockdowns in India helped to slow the spread of COVID-19 but brought about severe economic and social hardships: gross domestic product (GDP) contracted by 24% for the second quarter of 2020 and 7·3% for the year 2020. An estimated 120 million jobs were lost for the duration of the lockdown, and millions of migrant workers returned to their home villages under severe distress, some trekking extremely long distances on foot, with little money, food, or water.323, 324, 325
Fifth, all regions have seen incidents of discrimination, xenophobia, racism, and attacks against people scapegoated for spreading the virus.326 For example, political leaders and media outlets referred to SARS-CoV-2 as the Chinese virus, and racially motivated crimes against members of the Asian American and Pacific Islander communities in the United States have surged.327, 328 Additionally, when scientists in South Africa detected a new COVID-19 variant (which was later named the omicron variant) and informed WHO, some countries immediately imposed travel bans on African countries that had not yet recorded the variant.329, 330, 331
Indigenous Peoples have a higher risk of infection with severe socioeconomic, cultural, and health consequences, due to poorer baseline health status and lower access to health care and sanitation services than the general population.332 Indigenous women and girls have often been disproportionately affected by the pandemic, as many live in extreme poverty with diminished incomes and limited access to mainstream and high-quality health care.333
Internally displaced people, including people in areas controlled by armed groups, are especially vulnerable to infectious diseases and have limited access to safe housing, sanitation, and health care.334 Similarly, refugees and asylum seekers who are forced to flee from their homes to escape war, persecution, or natural disaster often have no place to live other than refugee camps, which are often overcrowded and provide inadequate access to sanitary facilities. In such situations it is almost impossible to maintain physical distance, practise safe hand hygiene, and stay healthy.335 Without lasting and durable solutions for internally displaced people, refugees, asylum seekers, undocumented migrants, and people who are stateless, they will continue to face limited or even non-existent access to essential services, including social services and health care, even if the pandemic abates.
The burdens of long COVID
Long COVID, chronic COVID syndrome, long-haulers, post acute sequelae of COVID, or post-COVID condition are some of the terms used to denote the persistence of symptoms or emergence of new symptoms at least 3 months after SARS-CoV-2 infection, irrespective of viral status,336 with long COVID the most recognised term in scientific literature.337 WHO provides the clinical case definition of post-COVID condition as symptoms 3 months from the onset of COVID-19 that last for at least 2 months and cannot be explained by an alternative diagnosis.338 This syndrome and its underlying mechanisms are still poorly understood, as it affects people regardless of the severity of their COVID-19 infection, including younger adults, children, and those who were not hospitalised.23, 339, 340
Reported symptoms of long COVID include fatigue, cough, chest tightness, chest pain, shortness of breath, sore throat, abnormalities of taste and smell, palpitations, myalgia, joint pain, numbness or tingling, skin rashes, hair loss, diarrhoea, urological problems, headache, neurocognitive issues including altered memory and concentration, cognitive blunting (known as brain fog), insomnia, impaired balance and gait, and mental health problems such as anxiety, post-traumatic stress disorder, and depressive symptoms, and these symptoms can be continuous or relapsing and remitting in nature. People with long COVID often report impaired quality of life and issues with education and employment. The social and financial effects of COVID-19 also contribute to the issues surrounding long COVID, including mental ill health.336, 341, 342, 343, 344, 345
The accurate reporting of long COVID is complicated. Disparities in epidemiological data are probably the result of differences in the base population, the accuracy of diagnosis, the reporting systems, and the capability of health-care systems.337 There are several challenges in the diagnosis of long COVID, including the length of the follow-up period, the accuracy of self-reporting, the symptoms examined, the reliance on parent-reported symptoms for children, negative PCR tests (false-negative results) in some patients, an absence of antibodies in patients who do not seroconvert, and difficulties in establishing a direct link between symptoms and the infection.336, 337, 346, 347
Studies worldwide have reported various rates of long COVID and a wide range of symptoms; however, it is suggested that up to 35% of patients who were treated for COVID-19 on an outpatient basis and up to 87% of patients who were hospitalised with COVID-19 have continuing symptoms.348, 349 Underlying chronic conditions such as diabetes, hypertension, and cardiovascular diseases might also worsen after COVID-19 infection, requiring closer monitoring.336
Some risk factors for long COVID are older age, female sex, having more than five symptoms during the acute stage of the infection, comorbidities including the presence of autoantibodies, and previous psychiatric disorders.341, 350, 351, 352 Conversely, vaccination against COVID-19 reduces the odds of developing long COVID after infection, and some people who had been infected with COVID-19 before vaccination and had long COVID reported improved symptoms after vaccination.353, 354, 355 Women, who are over-represented among populations in understaffed, forward-facing patient care roles and often lack access to adequate personal protective equipment (PPE, which is often poorly fitting for female bodies), may have an increased risk of long COVID.356 UN Women reported in 2020 that around 70% of health-care workers infected in Spain, Italy, and the United States in the early months of the pandemic were women.357
Studies show that long COVID could be related to organ damage, persistence of the virus in the body, post-viral syndrome, persistence of chronic inflammation or immune response (autoantibody generation), post-critical-care syndrome, complications related to comorbidities, reactivation of the Epstein-Barr virus induced by COVID-19-related inflammation, and adverse effects of medications, among other factors.336, 358, 359, 360
Long COVID has substantial physical, mental, social, and economic effects, and long COVID might itself be an emerging pandemic.361 As COVID-19 is likely to become endemic, many people could have long-term health care and social care needs, which could overburden the systems of countries and of school and work environments. These people will require multidisciplinary and stigma-free care, which is not readily available in many settings.342, 362 Although the recording of exact epidemiological data for long COVID is difficult with existing knowledge and capacity of health-care systems, continuous research and regular surveillance—in addition to international scientific collaboration—are needed to inform health-care systems, social-care systems, and governments when developing treatment, rehabilitation, support algorithms, and policies and practices related to disability, education, occupation, and finance.337, 340, 363
The need for strong health systems
An effective response to COVID-19 and any future pandemic requires not only a checklist of policy actions but also health systems that can deliver needed outcomes and can provide support to individuals to perform prosocial behaviours. The United States provides an example: although the government was able to develop and distribute vaccines, only 64% of the population was fully vaccinated as of Jan 31, 2022. This relatively low level of vaccine coverage compared with that of other countries is a consequence of widespread public distrust in the government and public health departments in the United States. Public health officials have little community presence, except in emergencies, and therefore little opportunity to build or rebuild trust. As in many other countries, the United States has invested little in community-based public health services, with the preponderance of health outlays directed at health care rather than public health. Within the health-care sector, the focus has been on secondary and tertiary health care rather than on universal access to primary health care. In 2019, US public health outlays of $104·5 billion accounted for a mere 2·8% of the total health outlays of $3·759 trillion.364, 365
Many LMICs—particularly those that have faced other epidemics, such as HIV, Ebola, and Zika—were able to integrate their responses to COVID-19 with well established community screening and contact-tracing capacity, and to rapidly deploy community health workers.366 As members of the community they serve, community health workers are instrumental in improving population health,367, 368, 369 and are crucial in linking people to preventive and clinical services, dispelling misinformation, and fostering trust.370, 371 For example, in Bhutan, Brazil, and Kenya, community health workers had an essential role in pandemic responses, including encouraging the adoption of public health and social measures and vaccination uptake.372, 373, 374 However, despite their pivotal role, these workers continue to be undersupported and overworked.370, 375
Strong national health systems and universal health coverage have been priorities in the Sustainable Development Goal (SDG) era to prevent and treat communicable and non-communicable diseases and reduce catastrophic health expenditure. Countries with universal health coverage and health systems centred around primary health care, as called for by SDG Target 3.8, were able to scale up emergency services for patients with COVID-19 while continuing to ensure quality health care for health needs unrelated to the pandemic. There have been vast differences between the effects of COVID-19 on populations in countries with resilient national health systems and universal health coverage and in countries without such systems.376, 377, 378, 379, 380
In low-resource settings in particular, the COVID-19 pandemic has had a marked effect on immunisation programmes, maternal mortality, malaria control efforts, and prevention and treatment programmes for tuberculosis and HIV. Routine immunisation programmes for children have been disrupted and maternal deaths, stillbirths, ruptured ectopic pregnancies, and maternal depression have increased.381, 382 Estimates suggest that in 2020 there were 680 000 deaths from HIV,383 and an excess of 1·4 million tuberculosis deaths, 14 million malaria cases, and 69 000 malaria deaths globally.384, 385 Approximately two-thirds of these additional malaria deaths were linked to disruptions in the provision of malaria prevention, diagnosis, and treatment, such as anti-malaria drug coverage, the distribution of insecticide-treated nets, and diagnostics.385
High levels of income inequality breed a lack of social trust and solidarity,386, 387 which in turn erodes support for public services. In the absence of public services, inequalities persist or increase, creating a feedback loop of distrust and inequality that sociologist Bo Rothstein has called a “social trap”.388 The lack of social solidarity is especially acute regarding marginalised groups in society, such as people experiencing homelessness, people who are incarcerated, people who use drugs, people experiencing domestic abuse, people from racial and ethnic minorities, and people with low incomes. These highly vulnerable groups should be prioritised by the public health system.
Public health services also address another dimension of vulnerability that is largely overlooked by the curative health system: the high and increasing prevalence of chronic, non-communicable diseases. COVID-19 has imposed especially high morbidity and mortality burdens on people with comorbid conditions, such as obesity, diabetes, kidney disease, and heart disease.264, 389, 390, 391 These chronic, non-communicable diseases can be mitigated through public health and social measures, through preventive and rehabilitative efforts to promote healthy behaviours such as nutritious diets and more active lifestyles, and by addressing the environmental determinants of non-communicable diseases, including air pollution and the built environment.392 Increasing evidence suggests that exposure to air pollution increases the risks associated with COVID-19 infection, including the mortality risk.393, 394, 395 The curative health industry pays little attention to the long-term health benefits of lifestyle and environmental changes to reduce risks.
The COVID-19 pandemic has also shown that insufficient attention was previously paid to the design and management of ventilation and filtration systems for healthy indoor environments, including safe workplaces, safe schools, and safe public transport. SARS-CoV-2 transmission occurs primarily indoors because of the high concentration of aerosols in indoor spaces with poor ventilation or filtration.396, 397, 398, 399 Outdoors, there is much greater dilution and dispersion of airborne particles, which considerably reduces the concentration of aerosols in the near-field and far-field.
Building-related interventions can reduce the spread of COVID-19. Inadequate ventilation and unfiltered, recirculated air have been associated with SARS-CoV-2 transmission in several studies that examined large outbreaks across various indoor environments,400 showing that building-level strategies are key to reducing the spread of airborne infectious diseases.40, 127, 401, 402, 403 Examples of effective building-level control measures include increasing outdoor air ventilation in buildings through mechanical heating, ventilation, and air conditioning systems and opening windows, and upper-room ultraviolet germicidal irradiation in high-risk settings.402, 404, 405, 406
Existing ventilation standards are not effective against the transmission of respiratory diseases.407, 408 It is imperative, for example, that the American Society of Heating, Refrigerating and Air-Conditioning Engineers, the US CDC, and WHO develop ventilation targets for respiratory infectious diseases, including for non-health-care settings. Strategies to improve ventilation include upgrading MERV filters in heating, ventilation, and air conditioning systems to MERV 13 and using portable air cleaners with high-efficiency particulate air filters. Setting ventilation rates on the basis of reducing risks to health (as opposed to only minimising energy consumption) and requiring upgraded filtration could help to reduce the risk of disease transmission within buildings.409, 410
Despite the relevance of buildings to disease transmission, case cluster investigations routinely—and mistakenly—fail to evaluate building performance or collect data on ventilation and filtration strategies. Such information could enable an understanding of the combination of environmental factors that lead to the highest risks and the most effective control strategies.411
Safe public transport
Relatively little scientific evidence is available to indicate how public transport vehicles, such as buses and trains, might facilitate viral transmission. Additional research in this area is important to ensure that public transport can operate as safely as possible, particularly as an affordable option for essential workers in urban areas. Research suggests that the risk of SARS-CoV-2 transmission on public transport can be substantially reduced by asking people who are unwell to refrain from its use, requiring or encouraging vaccination among passengers, changing transport schedules to reduce crowding, and improving ventilation or filtration. Buses can substantially improve ventilation by opening as many windows, doors, or roof hatches as feasible;412 deploying recirculating-air cleaning systems that use mechanical filtration or ultraviolet germicidal irradiation; and requiring passengers to wear face masks.
Although air travel can exacerbate the spread of infectious disease, and spread within aeroplanes has been reported, the risk of transmission of respiratory viruses among passengers in flight is low.413, 414, 415, 416, 417, 418 This low risk is attributed to onboard systems that deliver a 50:50 mix of outdoor air and recirculated air that passes through high-efficiency particulate air filters in most aeroplanes.419 In addition, the air is delivered and returned within each row, which renders ventilation highly effective. However, the ventilation systems are not always operating when aeroplanes are parked at the gate, and this represents a time of higher risk. A report published by the National Academies in 2013 highlighted this issue and recommended that gate-based ventilation be operational, especially during pandemics and periods of high risk.419
Rapid vaccine development yet unequal vaccine distribution and uptake
The bright spot of the pandemic has been the rapid deployment of scientific knowledge and evidence, most importantly in the development and introduction of effective vaccines. Putting aside the flawed and unequal distribution of vaccines, and the refusal to assist vaccine producers in LMICs to scale up and distribute vaccines that they themselves had developed, the rapid development of vaccines and scale-up of manufacturing capacities is an impressive example of private–public partnership and transnational scientific collaboration.
The US Government has had a long-term and pivotal role in funding the scientific development of several vaccine platforms, most notably the mRNA vaccine technologies that underpin the Pfizer-BioNTech and Moderna COVID-19 vaccines. The US Government was also deeply involved in 2020 in funding the rapid development, clinical trials, and production of Moderna's COVID-19 mRNA vaccine, whereas BioNTech received €100 million in financing from the European Investment Bank420 and a €375 million grant from the German government.421 US Government funding has come through multiple channels, including the NIH, the Department of Defense, the US Agency for International Development, and the US Department of Health and Human Services. Moderna's first grant from the Department of Defense (through the Defense Advanced Research Projects Agency) was in 2013,422 US Department of Health and Human Services funding dates to 2016,423 and $2·5 billion of funding in 2020 came from the US Department of Health and Human Services and the NIH.
The scale-up of vaccine manufacturing capacities was equally impressive. Despite setbacks early on, by September, 2022, more than 12·6 billion doses of a COVID-19 vaccine had been administered worldwide, with roughly 8·8 million doses administered every day.424 Although demand for boosters is growing, the main constraints against universal vaccination in 2022 are likely to be related to logistics and vaccine hesitancy rather than supply.
At least since the epidemic of severe acute respiratory syndrome, the US Government has been actively involved in researching betacoronaviruses and potential vaccines against the diseases they cause. A 2021 study estimates that the NIH spent $17·171 billion between 2000 and 2019 on vaccine platforms, of which an estimated $943 million was spent on mRNA vaccines and another $757 million was spent on vaccines targeting diseases caused by betacoronaviruses.425 US Government funding for clinical trials of the Moderna vaccine totalled an additional $4·9 billion in 2020.426 The NIH has long funded crucial bench research at the University of Pennsylvania that led to the use of a modified amino acid (pseudouridine) in the mRNA formulation of both the Pfizer-BioNTech and the Moderna vaccines.
The great success of vaccine development led to massive profits for the producers of mRNA vaccines, despite their support from public funds. The market capitalisation of Moderna increased from around $8 billion at the end of 2019 to $65 billion on Jan 24, 2022.427 Similarly, the market capitalisation of BioNTech increased from around $7 billion at the end of 2019 to $36 billion in January, 2022.428 Despite having had a decisive role in funding the development of these vaccines, the US Government did not share in the market returns, and indeed purchased the vaccines from these companies on a commercial basis.429
The US Government's long-term support of vaccine development research illustrates the crucial role of government funding for high-priority public goods such as vaccine technologies. Although private capital markets funded some research, funding and scientific support from the US Government was indispensable. Yet the US Government has not designed appropriate ways to manage the intellectual property that it co-funds and co-generates. Typically, intellectual property that has been funded by the US Government ends up entirely in non-governmental hands, whether at universities or companies. This discrepancy leads to an inequitable outcome (the privatisation of publicly funded wealth generation) and to an inefficient outcome (the underuse of intellectual property because of monopoly pricing by patent holders).
The result is the near-complete privatisation of the intellectual property that results from government funding. Universities and companies then exercise monopoly rights to the technologies under patent, and charge prices for vaccine doses that are much greater than the actual costs of manufacturing. In theory, mark-ups compensate companies and universities for their investments in research and development; however, their outlays in this area were partly funded by the government in the first place. Ultimately, taxpayers pay monopoly prices for vaccines that tax dollars helped to fund. Some governments in poorer countries lacked the means altogether to pay monopoly prices, and had to wait in the back of the queue for donations or discounts. By contrast, the AstraZeneca vaccine was developed by a not-for-profit partnership between AstraZeneca and the University of Oxford, UK. 2 billion doses of the vaccine were supplied to more than 170 countries (250 million doses supplied at-cost through the COVAX initiative) between January and November, 2021. However, AstraZeneca announced in November, 2021 that it planned to begin stepping down the provision of doses on a not-for-profit basis.430 As another example, the non-profit Texas Children's Hospital Center for Vaccine Development at Baylor College of Medicine, Texas, United States, worked with Biological E with no patents to produce and distribute a novel paediatric COVID-19 vaccine for emergency use in India, which was administered to more than 10 million adolescents in its first 10 days.431, 432
Alternative technologies, including recombinant protein COVID-19 vaccines, are not protected by patents and could have been made available early in the pandemic at very low cost or no cost to LMICs, alongside the patent-protected vaccines that use newer technologies. Some of the off-patent vaccines were produced at scale in LMICs by the Developing Country Vaccine Manufacturing Network (DCVMN). However, without early support from governments of high-income countries, complementary efforts to deploy vaccines based on more traditional, off-patent technologies lagged behind efforts by the major multinational pharmaceutical companies to bring newer vaccines to market. This neglect of existing technologies as a complementary strategy hampered the ability to make COVID-19 vaccines on a sufficient scale for the world. In addition, the national regulatory authorities of countries that host a DCVMN member are not designated as stringent, and therefore do not have the freedom to provide vaccines to COVAX or other LMICs. The failures to globalise the vaccine ecosystem to include production in a greater number of LMICs amplified global inequities in vaccine access.
Even without government funding, the patent system for vaccines is problematic. Large multinational pharmaceutical companies that develop vaccines are permitted monopolies on the production of these life-saving technologies during the terms of the patent and for the duration of applicable regulatory exclusivity, thereby leaving low-income countries with no effective access to vaccines other than through mechanisms such as the Global Alliance for Vaccines and Immunizations and official development assistance. The public also faces very high prices, mainly as taxpayers through government-funded vaccine-purchasing programmes.
A range of policy options incentivise research and development while also ensuring greater fairness in both the pricing of and access to vaccines. For example, governments could share in the profits in proportion to their investment share in research and development outlays. Governments could negotiate prices to balance the research and development incentives and fair access. Governments could force companies to license their intellectual property in return for reasonable fees, a process termed compulsory licensing. The US Government in fact proposed new World Trade Organization rules to facilitate compulsory licensing of the intellectual property of COVID-19 vaccines,433 but was met with initial strong resistance from European governments.434
The travails of COVAX
The COVAX (COVID-19 Vaccines Global Access) initiative was formed to accelerate the development and manufacturing of COVID-19 vaccines and to provide fair and equitable access to these vaccines for all countries. The launch of this initiative in April, 2020 was a timely and meritorious achievement, well before COVID-19 vaccines were proven and available. However, in practice, COVAX failed to deliver on its targets and timelines because vaccine-producing companies made contracts directly with the governments that paid the highest prices, rather than with COVAX, which insisted on lower prices for low-income countries. Moreover, vaccine-producing countries, such as India, imposed export bans on vaccines rather than delivering them to COVAX as promised.
As a result, COVAX was chronically short of vaccine supplies for LMICs, and was further unable to set dates and plans for vaccine delivery and use.435 Low-income countries in Africa were persistently last in line. As of January, 2022, the percentage of the population that was fully vaccinated was 71% in the EU and 63% in the United States, but only 10% in Africa and even lower in many countries, such as 2% in Nigeria (figure 17 ).181 In October, 2021, WHO called for every country to fully vaccinate at least 40% of their population by the end of the year;437 however, this goal was missed,438 almost without a word of remorse from high-income countries. Bottlenecks eased towards the end of 2021. By the end of the year, COVAX had delivered nearly 1 billion doses to 144 countries, and monthly deliveries were increasing and becoming more predictable, reaching 347 million doses in December, 2021.439 The EU, China, the United States, the Russian Federation, and India were all stepping up production and exports of vaccines, but not in a manner that was adequately coordinated among the vaccine-producing countries.
Figure 17.
Percentage of the world's population that is fully vaccinated as of Jan 6, 2022
Reproduced, with permission, from the International Monetary Fund.436
The COVAX Facility—a mechanism through which to procure and equitably distribute COVID-19 vaccines—was a worthy innovation in principle, but upstream science policy failures and downstream implementation failures prevented the widespread availability of effective and safe COVID-19 vaccines in low-income countries. Such failures included reserving financial incentives largely for multinational pharmaceutical companies to develop vaccines based on new technology—such as mRNA, adenovirus, or nanoparticle vaccines—without commensurate support for vaccines that used more traditional technology and could be made locally by vaccine producers in LMICs. Compounding this issue was a failure to make adjuvant technologies available to vaccine producers in LMICs. US Operation Warp Speed, the Coalition for Epidemic Preparedness Innovations, and other vaccine-funding initiatives operated on the premise that only multinational pharmaceutical companies had the ability to scale up and make effective vaccines, because of the mistaken belief that only new vaccine technologies could address the virus. The ability to grant emergency-use listing of COVID-19 vaccines was restricted to either WHO or one of the six stringent regulatory authorities in the United States, Canada, UK, EU, Australia, and Japan—once again excluding any national regulatory authority based in an LMIC. In addition, despite the COVAX framework, there were few instances in which the vaccine-producing countries (the United States, UK, China, India, the Russian Federation, and countries of the EU) worked operationally together to accelerate the equitable global uptake of vaccines.
Research governance
Despite many examples of research excellence during the pandemic, there has also been poor-quality research, subject to biases and with misleading results.440, 441 One such example is the controversy around the effectiveness of hydroxychloroquine, of which an initial study suggested effectiveness but several subsequent, well designed randomised controlled trials (RCTs) showed no benefit. Independent assessments of trial data and the potential for biases to influence findings provide safeguards against the reporting of misleading results. Registration of trials in a publicly accessible database is an essential step in assuring quality and reducing the risks of publication bias, whereby the results of negative studies are under-reported. The WHO International Clinical Trials Registry Platform provides an invaluable source of information on current trials evaluating a range of interventions.442 COVID-NMA is an example of an international initiative, led by a team of researchers from Cochrane and other institutions, that works in conjunction with WHO to generate up-to-date mapping of evidence from trials regarding COVID-19 drug treatments.443 COVID-NMA is one of many groups producing living evidence syntheses and improving future research by assessing the methodology and transparency of trials. Clinicians, policy makers, and people wanting to understand the best available evidence should consult robust sources such as this, and should not be swayed by the results of individual trials that have not been subject to such appraisal.444
Analysis of COVID-19 trials shows substantial imbalances between the numbers of drug trials (2465), vaccine trials (109), and public health trials (16), with public health trials in particular being under-represented.445 Many of the individual drug treatment trials for which results are available recruited small numbers of patients, such that the trials were underpowered and were not able to detect useful beneficial effects. Notable exceptions include the DisCoVeRy trial in patients who were hospitalised,446 and the PRINCIPLE trial, which recruited participants recovering from COVID-19 at home.447
Only three of the 16 trials of preventive interventions involved public health and social approaches: two RCTs on the effectiveness of wearing face masks and one RCT on physical distancing.448, 449 The failure to undertake large-scale RCTs of potentially useful interventions, particularly of social and behavioural interventions and of ventilation and filtration regimes, is a missed opportunity to document the effectiveness of affordable preventive measures. However, the study of behavioural interventions using observational data has also been helpful to control the pandemic.450 Research funders should ensure an appropriate balance between the evaluation of treatments in hospital and in community settings and preventive (including behavioural and social) and therapeutic interventions. WHO has an important role in monitoring the funding, recruitment, and analysis of intervention trials and in reporting progress regularly.
The scarcity of support for the development of new drugs, vaccines, and diagnostics by and for biotechnology companies and large-scale producers based in LMICs shows a marked research imbalance. Existing funds prioritised incentive financing for large and multinational pharmaceutical companies, with the expectation that discoveries would somehow quickly reach Africa, southeast Asia, and Latin America. This did not happen, and glaring vaccine inequities emerged as a result. A new financing mechanism is therefore needed for research and development in LMICs.
Pandemic economics
The COVID-19 pandemic led to a deep global recession in February–April, 2020. In March, 2020, uncertainty was so high that it led to a dash-for-cash and general malfunctioning in financial markets. Central banks and many governments acted promptly to ensure orderly conditions in financial markets and to protect vulnerable households and companies. Governments imposed severe mobility restrictions on all continents, resulting in what was termed the Great Lockdown. Global output in 2020 contracted by 3·1%, with losses particularly severe among advanced economies, which implemented the strictest lockdowns.451 The United States experienced a most unusual recession: it was by far the deepest but also the shortest on record. The National Bureau of Economic Research Dating Committee asserts that the contraction was limited to March and April, 2020.452 By Q3 of 2020, global output was already beginning to recover as people, companies, and governments learned more about the virus, uncertainty declined, and mobility restrictions were eased in many places. Like the initial contraction, the recovery was led by advanced economies. The recovery in the United States followed the same pattern, but was even more pronounced.
In the table , we compare the actual annualised growth in GDP between 2019 and 2022 with the IMF's pre-pandemic projections from the October 2019 World Economic Outlook.453, 454 In most countries, and in all WHO regions, actual growth was lower than had been predicted in the months before the pandemic. In a few cases, such as Taiwan, Province of China, actual growth (4·3%) was higher than had been predicted (2·0%). Note that actual growth here refers to the growth for 2019–22 as of the World Economic Outlook April, 2022. GDP refers to GDP measured at constant international prices.
Table.
Comparison between the International Monetary Fund's pre-pandemic projection for annualised growth from 2019 to 2022 and actual growth in gross domestic product from 2019 to 2022
| World Economic Outlook October 2019 projected growth for 2019–22 | World Economic Outlook April 2022 actual growth for 2019–22 | Actual minus expected growth rate 2019–22 | Estimated cumulative deaths per million population (as of May 31, 2022) | ||
|---|---|---|---|---|---|
| WHO region | |||||
| African region | 3·5% | 1·9% | −1·5% | 1575·6 | |
| Region of the Americas | 2·0% | 1·5% | −0·5% | 3995·5 | |
| Region of the Americas (excluding United States) | 2·3% | 0·8% | −1·5% | 4078·9 | |
| Eastern Mediterranean region | 2·9% | 2·7% | −0·2% | 2803·4 | |
| European region | 1·8% | 0·3% | −1·5% | 4289·5 | |
| South-East Asia region | 6·3% | 2·6% | −3·7% | 2545·6 | |
| Western Pacific region | 4·6% | 3·5% | −1·1% | 300·6 | |
| Western Pacific region (excluding China) | 2·4% | 1·2% | −1·2% | 1064·7 | |
| World | 3·5% | 2·0% | −1·5% | 2228·6 | |
| Country | |||||
| Brazil | 2·3% | 0·5% | −1·8% | 3648·0 | |
| China | 5·8% | 4·9% | −0·9% | 15·4 | |
| France | 1·3% | 0·4% | −0·9% | 2659·4 | |
| Germany | 1·3% | 0·1% | −1·3% | 2749·6 | |
| Italy | 0·7% | −0·3% | −0·9% | 4891·5 | |
| Mexico | 1·8% | −0·6% | −2·4% | 5723·5 | |
| New Zealand | 2·6% | 2·0% | −0·6% | 203·9 | |
| Republic of Korea | 2·6% | 1·9% | −0·7% | 500·7 | |
| Russian Federation | 2·0% | −2·3% | −4·3% | 5360·0 | |
| Taiwan, Province of China | 2·0% | 4·3% | 2·2% | 165·0 | |
| United Kingdom | 1·5% | 0·4% | −1·1% | 2910·4 | |
| United States | 1·8% | 1·9% | 0·1% | 3823·5 | |
Data from the World Economic Outlook October 2019,453 the World Economic Outlook April 2022,454 and the Institute of Health Metrics and Evaluation.146 Actual growth signifies the International Monetary Fund's estimates as of April, 2022. Gross domestic product is measured in international dollars at constant prices.
Notably, although all WHO regions experienced slower growth than had been predicted in October, 2019, the growth shortfalls in the Western Pacific region, the Eastern Mediterranean region, and the region of the Americas were lower than in other regions. In general, economies that followed a suppression approach—China, New Zealand, Taiwan, Province of China, and Republic of Korea—had smaller growth shortfalls than the rest of the world. The United States experienced no growth slowdown (at least based on the World Economic Outlook as of April, 2022), but also had a high level of cumulative deaths per million population.
The recessions induced by COVID-19 in many countries in 2020 were accompanied by substantial employment losses (figure 18 ). These losses were particularly large in emerging markets and differed in terms of the age and education level of the workers affected. Workers who had received tertiary education were generally the least affected by employment losses. Although employment levels recovered in many advanced economies in 2021 (except among workers with lower levels of education), emerging markets had more persistent employment losses as of March, 2022.455
Figure 18.
Change in employment-to-population ratio in G20 countries
Mean percentage point change in employment-to-population ratio between latest data (Q3 2021; except Argentina, Q2 2021) and Q3 2019. Prime: age 25–54 years; youth: age 15–24 years. For all other categories, ages 15–64 years are considered. Basic: primary and lower-secondary education; intermediate: upper-secondary and post-secondary, non-tertiary education; advanced: above post-secondary, non-tertiary education. Data are aggregates for G20 advanced economies (Canada, France, Italy, Republic of Korea, Spain, and United States) and emerging market economies (Argentina, Brazil, Mexico, and South Africa). Reproduced, with permission, from the International Monetary Fund.455
The changes in GDP measure the direct and indirect effects of the pandemic on output. However, beyond the losses of output, GDP does not measure the massive losses in societal wellbeing that are associated with illness and deaths as a result of COVID-19. To account for societal losses from excess deaths and disease, economists often estimate the monetary value of mortality and morbidity by assigning an economic value to a death or a year of illness. In the United States, for example, US federal agencies assign a value of a statistical life (VSL) to identify the societal benefits of measures to save lives or the costs of failures to save lives. Although there is no single authoritative estimate of VSL, US agencies typically place it between $5 million and $10 million per life lost. One study from early in the pandemic put the VSL in the United States at $4·5 million per life lost in 2020, considering age-specific mortality rates.456 Because the US GDP per capita was $63 500 in 2020, the VSL was approximately 70 times the GDP per capita.
Using such an estimate, the economic value of the loss of life is far larger than the loss of market output. As of the end of May, 2022, there had been approximately 3900 deaths attributed to COVID-19 per million people in the United States, or 0·39% of the population. Using a VSL equal to 70 times the GDP per capita, we see that the economic loss due to morality is therefore 70 × 0·39% of GDP, or 27% of annual GDP—a staggering sum, and far larger than the loss in market output. The global mortality at the end of May, 2022 was approximately 0·2% of the world's population. Using a global VSL equal to 70 times the world GDP per capita, the economic loss is 14% of annual world output. These are very rough illustrations, yet they make the point that the societal losses of life, put in monetary terms, have been enormous, and the societal benefits of reduced mortality rates are similarly enormous. Note that these very simple calculations also do not include any estimates of the costs of morbidity, including those of long COVID, which are also substantial.
The long-term economic scarring and legacies of the pandemic are as yet unknown. As of mid-2022, the United States had returned to the pre-pandemic level of economic activity, but was also experiencing inflation caused by the combination of pandemic-related expansion in demand with adverse supply shocks, the war in Ukraine, and the sanctions regime against the Russian Federation. Monetary policy tightening is ongoing. The tightening cycle is shared by many other advanced and emerging market economies. China's economic recovery is facing difficulties, resulting from continued sporadic lockdowns, supply chain disruptions, and financial stresses, including in the real estate sector. COVID-19 will lead to sustained and sizeable output losses in low-income and emerging economies, whereas advanced economies are expected to return closer to their pre-pandemic paths over the next 3 years.451 Uncertainty remains elevated.
Countries that are heavily dependent on tourism and travel suffered extreme losses of national output, and their economies have not yet recovered. Island countries in the Caribbean are a case in point,457 with countries in this region experiencing some of the largest GDP declines in the world in 2020: Aruba, −22%; Saint Lucia, −20%; Antigua and Barbuda, −20%; and Barbados, −18%, compared with declines of less than 5% in most high-income countries. Caribbean island economies did not bounce back in 2021, as travel and tourism remained depressed. Several oil-exporting countries also experienced a steep decline in GDP in 2020, but that decline was followed by a V-shaped recovery in 2021 as the global demand for petroleum recovered.
High-income countries were able to draw from domestic and international capital markets to finance increased government outlays at historically low interest rates in response to the pandemic, whereas low-income countries generally lacked access to international capital markets on comparably favourable terms. According to IMF data, the advanced economies increased their budget deficits relative to GDP by an average of 6·8 percentage points during 2020–21 compared with 2019. LMICs were much more constrained in their borrowing. Countries of sub-Saharan Africa, with the least access to capital markets, increased their deficit-to-GDP ratio by a mere 1·7 percentage points, with most of the increase driven by lower revenue. In essence, high-income countries used deficit financing to stabilise incomes and protect businesses from bankruptcy, whereas low-income countries had to reduce their expenditure. In 2021, high-income countries bounced back to growth with far more vigour than did low-income countries, and long-term prospects suggest a divergent recovery, with advanced economies returning to their pre-pandemic output paths while emerging markets and low-income countries are likely to face a permanent negative output shock.458 For the lowest-income countries, financial support should come in the form of grants and highly concessional long-term loans.
It is clear that economic prospects are intimately tied to pandemic developments. Suppression of the virus has the best outcomes for economics, health, and civil liberties.459 As hospitalisations and mortality increase, economic activity declines in response to both greater restrictions on economic activity imposed by governments trying to regain control of the situation, and labour shortages as people leave the workforce because of illness, school closures, and voluntary physical distancing.
As we have noted throughout this Commission report, the key to escaping both the pandemic and the economic fallout is widespread vaccination and basic public health precautions (a so-called vaccination-plus strategy), combined with the development and distribution of increasingly effective treatments for COVID-19 to lessen its health effects once contracted. The faster the world can act to vaccinate its population, the better the prospects for exiting the pandemic and achieving long-lasting economic recovery. In the words of the IMF Managing Director Kristalina Georgieva: “Vaccine policy is economic policy.”460
Global finance and the pandemic
Central banks around the world reacted swiftly to unprecedented financial disturbances in March, 2020. Through the aggressive easing of monetary policy, extension of various credit facilities, and liquidity swap lines, a vicious circle of negative macrofinancial feedback loops was stopped. Initially, emerging markets experienced large capital outflow, but these patterns reversed quickly as orderly market conditions were restored.
The World Bank approved a $14 billion fast-track facility for health emergency response on March 2, 2020, and this facility supported more than 100 countries with credits and grants within the subsequent 3-month period through the global health multiphase programmatic approach. These resources helped countries to source public health and social measure commodities, mobilise health workers, and expand care capacity through procurement of equipment and goods such as oxygen, as part of a $150 billion package announced in April, 2020 for health, social, and economic response. The World Bank also approved $12 billion for financing vaccine procurement and delivery in early October, 2020, even though these resources were limited by their requirement to be allocated on an individual-country basis.
The IMF provided two kinds of liquidity assistance for LMICs. The first was emergency credit lines and other IMF financing facilities in 2020–21, provided to around 90 countries and totalling roughly $170 billion. The second was the issuance of special drawing rights in 2021, amounting to $650 billion. However, this important infusion of liquidity was made in proportion to the existing IMF quotas, meaning that most of the special drawing rights allocation went to high-income countries, and only $30 billion to countries in Africa. Nonetheless, this liquidity infusion was still substantial relative to the GDP of many low-income countries—up to 11% of recipient country GDP in some cases. In 2022, the IMF established a new Resilience and Sustainability Trust—partly financed by high-income countries lending some of their special drawing rights to the Trust—which in turn will provide long-term financing to small and low-income countries to help them to tackle structural challenges of global relevance, such as pandemic preparedness and climate change, and thereby strengthen their resilience to shocks.
G20 countries also offered some relief via the Debt Service Suspension Initiative, which provided almost $13 billion in relief to 48 eligible countries before it expired at the end of 2021.461 Some lower-income countries decided not to participate in the programme given its potential effects on their future access to credit.
Unfortunately, the G20 did not do as much as it could have done to facilitate a coordinated response to COVID-19. As a powerful complement to the UN, comprising 19 national governments and the EU, the G20 represents 63% of the world's population and 87% of its economic output. The G20 is well poised to adopt a plan to support lower-income countries through foreign direct investment, trade agreements, official development assistance, and loans. Such financing could support achievement of the SDGs and the Paris Climate Agreement, including addressing many of the health, education, environmental, and infrastructure challenges that we have described and that are exacerbated by the COVID-19 pandemic.
G20 countries account for 90% of research expenditure, researchers, publications, and patents. 80% of countries worldwide invest less than 1% of GDP in research and development.462 Special attention should be paid to scaling up investment in research and development, especially through partnerships between governments, universities, and companies in G20 countries, and their counterparts in LMICs. There is a great need for long-term commitments to building capacity in LMICs, ensuring equity and maintenance of a worldwide network of collaboration. Such a plan could facilitate cooperation among scientists, sectors, and institutions to develop and produce tests, vaccines, therapeutics, and other goods, and therefore build capacity in the long term, not only for producing drugs and medical equipment but also to build a 21st-century knowledge economy. However, going forward, this initiative could be leveraged to create innovative, implementable, and coordinated programmes to support global research and development and to scale up investment in the production capacities of LMICs.
Global health financing
Health financing nowadays is primarily covered by national (domestic) resources, which includes government and private health expenditure in addition to out-of-pocket spending, with only very modest levels of international support by donors for LMICs.463, 464 Total official development assistance for health, as measured by the OECD Development Assistance Committee, came to a mere $23 billion as of 2019, or less than 0·05% of the GDP of donor governments.465 This assistance amounted to roughly 1·5% of the health financing of LMICs, a very modest sum.463 The pandemic did not alter this picture in any decisive way.
Even these modest amounts of official development assistance have proven decisive in scaling up disease control in many areas. The Global Fund and the Global Alliance for Vaccines and Immunizations have each saved tens of millions of lives with modest outlays of a few billion dollars per year.466, 467, 468 These programmes prove that international financing for health can result in practical solutions, despite being highly underfunded considering their missions.
The creation of the Access to COVID-19 Tools (ACT) Accelerator and COVAX in April, 2020 aimed to accomplish the same results for COVID-19, but both fell far short.469 Raising even a few billion dollars of international support for ACT Accelerator and COVAX proved extremely difficult, despite the urgency of the pandemic. The modest funding was insufficient to obtain crucial PPE supplies, testing supplies, and especially vaccines. Bilateral deals between countries and manufacturers for the purchase of these commodities were prioritised at the expense of COVAX. Many producing countries also implemented temporary export bans on essential products (eg, PPE, pharmaceuticals, and hand sanitiser), with wider effects on access for countries in need. The multilateral development banks similarly provided too little health financing, and too slowly, to make up the pandemic financing gap.470
The current proliferation of special health funds needs to be rationalised within a single global fund that is closely linked with WHO. The spread of small vertical health funds has become unmanageable, with many key functions slipping through the cracks. In addition to the Global Fund and the Global Alliance for Vaccines and Immunizations, the World Bank Group hosts the Global Financing Facility in support of Every Woman Every Child and the Pandemic Emergency Financing Facility for pandemic response. WHO has a Contingency Fund for Emergencies. The Pandemic Emergency Financing Facility and the Contingency Fund for Emergencies were established during the 2014–15 Ebola outbreak in west Africa. The COVAX Facility is part of the ACT Accelerator, which is co-managed by WHO, the Global Alliance for Vaccines and Immunizations, UNICEF, and a few partners. These multiple funds weaken the international response capacity in health emergencies.
Long-term economic and sustainable development recovery from the pandemic
The extended period of economic disruption is creating long-term economic and social scarring, including long-lasting difficulties for children whose schooling has been repeatedly disrupted; new debt crises among low-income countries that are facing sustained output and revenue losses amid the tightening of global financial conditions, and in some cases facing years of reduced numbers of tourists;471 long-term disabilities arising from long COVID and from the mental distress of the pandemic;271, 472, 473 long-term gender inequalities, as women have been on the front line of the pandemic and are disproportionately affected by poverty, with many being forced to reduce their participation in the workforce;474 and long-term social and political instability arising from increased income inequality and business disruptions as a result of COVID-19 that will take years to overcome.
The highly expansionary macroeconomic policies of 2020–21, in particular the enormous increases in the money supply in both the United States and the eurozone, have resulted in high inflation in 2022, with the longer-term consequences still to be seen. That the first 2 years of the pandemic were followed by the war in Ukraine and a stringent sanctions regime against the Russian Federation has further exacerbated the supply shocks due to COVID-19, and has given rise to the fear of an extended period of stagflation, in which the combination of monetary expansions and powerful supply shocks could lead to a combination of economic downturns and high inflation, an event not seen in the world economy since the 1970s.
We must also address the ongoing climate and ecosystem crises that threaten major global destabilisation. Earth is now 1·2°C hotter than the pre-industrial temperature, and the 8 years since 2014 have been the eight warmest years since records began in 1870. The next El Niño event, perhaps occurring as early as 2023, is likely to cause a large upward shift in worldwide temperatures, and the world could very soon exceed the 1·5°C threshold that was adopted as a guardrail by the Paris Climate Agreement.475
The COVID-19 pandemic threatens to divert global attention, financing, and scarce political capital away from the urgent agenda of sustainable development, including the SDGs and the Paris Climate Agreement. We must ensure that the focus on pandemic preparedness and response enhances rather than detracts from the broader sustainable development agenda. Europe's success in launching the European Green Deal while simultaneously confronting the COVID-19 pandemic shows the political feasibility of fighting the pandemic while also intensifying the policy commitments for sustainable development. The Next Generation EU fund commits €750 billion towards recovery and resilience with a focus on a green and digital transformation. In using the funds, EU member states must devote a minimum of 37% of the funding to climate change and a minimum of 20% to the digital transition.
The challenges of sustainable development in LMICs are far more acute. Even if the COVID-19 pandemic recedes soon, economic scarring will be long-lasting. Many lower-income countries lack the financial means to promote long-term recovery and to finance sustainable development and commitments under the Paris Climate Agreement. The IMF has established that what are classified as low-income developing countries—a group of 57 low-income and lower-middle-income developing countries—face a financing gap of $300 billion–$500 billion per year to achieve the SDGs, and this gap has increased as a result of the pandemic.476, 477 These funds could be mobilised by a combination of means: increased official development assistance, increased lending by the public development banks (both multilateral development banks and national development banks), increased market borrowing through sustainability-themed bonds (eg, green, social, SDG, or sustainability-linked bonds) and other means, and global coordinated taxation, for example on ultrahigh net worth, greenhouse gas emissions, and financial transactions.
There is an opportunity to integrate health, environmental sustainability, and equitable economic recovery into post-COVID stimulus packages, but the potential for doing so has not been realised. Many such packages are likely to result in numerous adverse environmental impacts, particularly because of increases in fossil fuel combustion,478 which not only accelerates climate change but also results in higher levels of air pollution. Long-term exposure to air pollution is thought to increase the risk of adverse outcomes of COVID-19 infection.395, 479
Despite widespread empirical evidence of the opportunities offered by green recovery strategies, current practice shows that most industrialised countries have only partly implemented sufficiently ambitious green stimulus packages.480, 481, 482, 483, 484, 485 A 2022 analysis shows that the pandemic economic recovery packages of the G20 countries, totalling $14 trillion, allocated only 6% of total stimulus spending to areas that reduced emissions, and 3% was allocated to activities that will increase emissions.486 Moreover, governments have focused their efforts on measures that could bring immediate benefits to employment and economic growth, such as investments in green energy and transportation, and renovations to increase the energy efficiency of buildings. Although very important, such interventions address only a part of the sustainability challenges faced by high-income countries: an analysis of recovery packages of European countries found that issues such as the agrifood system, circular economy, and nature-based solutions have received little attention so far, although many of these countries have relatively poor performance on such challenges.487 As the SDGs provide a holistic and inclusive framework that can be universally applied, their integration into public policies is crucial for an effective green transition. For this purpose, the appropriateness of investments and reforms can be analysed with the support of artificial intelligence methods such as machine learning,488 enabling a rapid assessment of national plans and corrective actions when needed.
Section 3: recommendations for ending the COVID-19 pandemic, preparing for the next, and long-term sustainable development
All ongoing risks highlight the continued urgency of global cooperation to end the COVID-19 pandemic and to prepare for future pandemics. Although we have largely failed in terms of global cooperation during the first 2 years of this pandemic, putting such cooperation into place is still urgent. We remain far from preparedness for future pandemics, and logic tells us that achieving safety will require the reinforcement of basic tools of pandemic control on a truly global basis: universal vaccine coverage, physical distancing, the use of face masks as appropriate, prudential controls on potential superspreader events, safe workplaces, surveillance for new variants, global protocols for safe international travel, and the scale-up of test-trace-and-isolate regimens to be put in place when community transmission is low to ensure that it is kept low.
Global and national strategies to end the COVID-19 pandemic
Governments must be vigilant about new variants of SARS-CoV-2 (especially for unvaccinated populations) and waning protection from vaccinations and previous infections. Strong monitoring and coordinated surveillance systems around the world need to be established to assess the risks of new waves of COVID-19. WHO, working with the main vaccine-producing companies and countries, needs to intensify its efforts to ensure high levels of immunisation coverage in all countries, especially in the low-income countries where vaccine coverage remains dangerously low. Countries must then implement a vaccination-plus control strategy that includes mass immunisation; the availability and affordability of testing; treatment for new infections (test and treat); rehabilitation and social support for people with long COVID; and complementary public health and social measures such as the use of face masks, the promotion of safe workplaces, and economic and social support for self-isolation. These vaccination-plus policies should be implemented with the goal of protecting populations on a sustainable basis, rather than implementing reactionary policies that either require the use of face masks and proof of vaccination or relax these requirements on the basis of the volatile reproduction rate of the virus at a given time. In calling for this vaccination-plus strategy, we strengthen the calls of many other commissions for the implementation of evidence-based public health and social measures to control transmission and protect the most vulnerable populations.96, 489, 490, 491
China, the United States, the EU, India, the Russian Federation, and other major regional and global powers must put aside their geopolitical rivalries to work together to end this pandemic and to prepare for the next one and for other global crises. Military conflicts and social turmoil can increase cases of COVID-19 and outbreaks of other infectious diseases and can affect surveillance systems, therefore amplifying humanitarian crises. In this global coordination and cooperation, UN institutions should be pre-eminent. The G20 should have a special role as the point of coordination among the world's major economies and financial centres, given the central role of global finance in pandemic preparedness, response, and recovery.
Intensified investigation into origins
As a Commission, we strongly support the call for an objective, open, data-driven, transparent, and independent scientific debate about the origin of SARS-CoV-2.44, 45 WHO, governments, and the scientific community should intensify the search for the origin of SARS-CoV-2, including a possible natural spillover or a possible research-related spillover.
In the absence of an unbiased, independent, and rigorous search for a natural origin by a multidisciplinary team of experts alongside an unbiased, independent, and rigorous investigation of the research-related hypotheses, the public's trust in science will be imperilled, with potentially grave long-term repercussions. It is therefore crucial to investigate all hypotheses fully, not only to ascertain the source of the pandemic and to protect against future emerging infectious diseases, but also to ensure the integrity of science itself. The perceived lack of transparency to date by leading scientific agencies and laboratories is troubling and needs to be addressed.
Maintain WHO as the lead institution for response to emerging infectious diseases
WHO should remain at the centre of the multilateral response to emerging infectious diseases. Yet WHO needs strengthening. Such strengthening should include new regulatory authority, more backing by national political leaders, more contact with the global scientific community, and a larger core budget to carry out its many crucial responsibilities. The capacity of WHO should also be complemented by far greater international finance to support the health systems, research and development, and biomedical production capacity of LMICs.
Establish a global pandemic agreement and strengthen the IHR
The weaknesses and shortfalls of the IHR (2005) in protecting the world against the COVID-19 pandemic have led to the decision by WHO member states to start the process to draft and negotiate new agreements on pandemic preparedness and response, including a possible new Pandemic Treaty. We echo many other reports on COVID-19 in calling for a global pandemic agreement and for a reassessment of and update to the IHR (2005).96, 489, 490, 492
We recommend the following as some of the core constituents of the new pandemic arrangements. First, bolstered WHO authority, with high-level political support from heads of government in a new Global Health Board. Second, the right of WHO to investigate in situ any events that could constitute a new global public health emergency. Third, the creation of a global surveillance and monitoring system for infectious disease outbreaks and transmission, building on existing initiatives493—both for disease forecasting and for making informed, data-driven decisions about workplace restrictions, resource allocations, and effective interventions to avoid untargeted, one-size-fits-all restrictions. Fourth, the approval by WHO, the International Civil Aviation Organization, and the International Maritime Organization of standing regulations regarding the processing and control of international travellers and international freight and shipping under global pandemic conditions. Finally, the publication of an annual WHO Report on Global Pandemic Preparedness and Response, which should include findings from the Global Preparedness Monitoring Board for review and adoption by the WHA. The WHA should then establish global health policies to address the gaps and weaknesses identified in the report by drawing on the successes of national and regional health strategies and policies, and adapting them to fit various contexts and country needs.
Reform of WHO governance
The effectiveness of WHO depends on backing by its member states and, most importantly, the political support of the major powers. We echo some of the recommendations made by other groups to bolster the role and financing of WHO in preventing and responding to future pandemics and strengthening public health systems globally.492
We strongly urge the creation of a new WHO Global Health Board to support WHO in its decision making and actions, especially on urgent and controversial matters. We support similar calls by other panels for a Global Health Threats Council or Global Health Threats Board.96, 490, 492, 494 This WHO Global Health Board should be composed of heads of government representing each of the six WHO regions, and elected by the member states of those regions. Efforts should be made to ensure inclusive decision making, including gender parity.
Additionally, a substantial increase to the core budget of WHO is required to increase its effectiveness at its headquarters in Geneva, at regional offices, and in countries around the world. Moreover, WHO needs the capacity to draw upon large-scale emergency financing in the case of a global public health emergency. WHO should continue to use the infrastructure it has built up so that this infrastructure is in place when another pandemic emerges. An emergency credit line at an international financial institution, designed as a key tool of the new Global Health Fund, could provide the necessary emergency financing channel.
Regulations for the prevention of pandemics from natural spillovers and research-related activities and for investigating their origins
There is a need for the primary prevention of pandemics through the implementation of preventive measures against both natural spillovers and spillovers from research-related activities. The prevention of natural spillovers would require a One Health approach—an integrated, unifying approach that aims to sustainably balance and optimise the health of people, animals and ecosystems495—including the strengthening of veterinary services, the regulation of trade in domestic and wild animals and of wildlife and livestock rearing, the prevention of deforestation, and the enhancement of pathogen-surveillance systems in domestic animals and in humans.496 Such measures are likely to be highly cost effective and would complement investments in the strengthening of national health systems, the development of vaccines and therapeutics, and other outbreak response strategies described in this report. Strategies to prevent research-related releases should include stronger international and national oversight of biosafety, biosecurity, and biorisk management, including the strict regulation of gain of function research of concern.
It is certain that future pandemics will arise from interactions between humans and animals, and that research on viruses will continue with the potential for accidents. It is therefore imperative that society enacts measures to reduce the possibility of both natural spillovers and spillovers from research-related activities, and acts rapidly if these scenarios do occur. Countries must adopt rigorous surveillance over the trade of domestic and wild animals and over research. Calls for One Health approaches to address the risks of the emergence and transmission of zoonotic diseases are common among reports on pandemic prevention and preparedness,489, 490, 492, 494 and many reports have called for greater global surveillance and monitoring of disease risks, with WHO as the coordinating power.
The WHA should also adopt new global regulations on biosafety to regulate pathogen-related fieldwork and laboratory work. We must be aware that the collection of viruses and other pathogens from nature can give rise to research-related spillovers. Such activities have been largely unregulated in the past. Moreover, we urgently need global oversight regarding potentially hazardous laboratory experimentation, including gain of function research of concern. The new global regulations should include inspection by international teams of facilities that are involved in the manipulation of dangerous pathogens. Moreover, scientists need to develop much safer means of research on the pathogenicity and infectivity of viruses than the gain of function research of concern methods that have spread with little oversight during the past 20 years. Even today, there is little understanding and clarity about the research on SARS-like viruses that was underway just before the COVID-19 pandemic. Additionally, because disease-causing pathogens are stored and studied in laboratories across the world, countries should maintain peace and address conflict with diplomacy rather than warfare, as armed conflict and the destruction of research institutions risk the escape of pathogens and subsequent outbreaks of disease.
When investigating the origins of any novel pathogen, potential hypotheses should not be prematurely rejected to ensure that time-sensitive data—such as early case information and laboratory records—are collected. Countries should encourage the examination of the originally submitted papers on the origins of emerging infectious diseases, the availability of raw scientific data, and the systematic review of grants and documents on planned research.
G20 support for finance, research and development, and the production capacities of LMICs
The G20 should plan and implement a 10-year effort, with accompanying financing, to ensure that all WHO regions—including the world's lower-income regions—have the capacity to research, develop, produce, and distribute all of the essential tools for pandemic control, including tests, diagnostics, vaccines, therapeutics, PPE, and human resources for health, among others.494 Specifically, this initiative should include capacity building and innovations for vaccine producers in LMICs and should extend stringent regulatory authority capacity to these countries.
Strengthen national health systems and increase investments in primary and public health
Governments should allocate an increased share of national income to their health systems, and in the case of low-income and lower-middle-income countries, development aid should complement domestic financing to ensure that all countries—including those with the lowest income—have strong public health systems and health-care systems that are centred around primary health care and can achieve universal health coverage, as called for by SDG 3. Along with increased investments in health systems and medical supply chains, there is also a need to increase support for research and development in the behavioural, social, and implementation sciences to ensure that public and primary health interventions and systems effectively serve their populations within their respective sociocultural and economic environments. The strengthening of health systems should address inequalities for health-care workers and communities in terms of gender, ethnicity and race, income, and accessibility. All reports that have been written on COVID-19 make strong recommendations for national health system strengthening for emergency preparedness and for the maintenance of primary and mental health care during emergencies.96, 490, 491, 492, 493, 494
Alongside the strengthening of health systems and the provision of universal health coverage, more investment is needed to ensure a standing public health capability that can operate effective surveillance systems in each country, adequately trained and resourced outbreak investigation, and response capacity and communications expertise. Quality health education must also become widely accessible. There should also be increased financing for programmes that address other major global health concerns, including HIV/AIDS, tuberculosis, malaria, childhood immunisations, maternal mortality, and neglected tropical diseases. Existing programmes should be enhanced with resiliency and long-term sustainability, and new programmes should be designed with resiliency and sustainability in mind.
Health workers, including community health workers, are essential to the function of resilient health systems, and these workers must be well trained, well paid, well supported, and provided with appropriate PPE. Sustainable investments in education and training programmes for community health workers, nurses, mid-level practitioners, and physicians in LMICs are necessary for health professionals in all countries to participate in patient-centred and population-centred health systems that are locally responsive and globally connected. Communities, civil society organisations, and local faith-based groups must be engaged in health-system strengthening, and these investments will not only improve pandemic responses but also improve the health of the populations during non-pandemic times.
National pandemic preparedness plans
The overarching lesson of the COVID-19 pandemic is the need for national preparedness along with global cooperation and concerted action. Most countries lack meaningful pandemic preparedness plans. The countries that made such plans, such as countries of the Western Pacific region after the outbreak of severe acute respiratory syndrome, have fared best in the COVID-19 pandemic. The enormous vulnerabilities that COVID-19 has exposed in high-income and low-income countries alike shows that plans should be comprehensive, cross-sectoral, and supported by global coordination. We support other commissions, including the Independent Panel for Pandemic Preparedness and Response,96 in recommending that each WHO member state should adopt, by law, national pandemic preparedness plans that meet international standards laid out in the Pandemic Treaty, and in supporting the WHO IHR regulations and the review of these regulations. Essential components of national pandemic preparedness plans are listed in the panel .
Panel. Essential components of national pandemic preparedness plans.
-
•
Improved primary health care and universal access to health care for all as a precondition for effective health systems and public health
-
•
Scale-up of community-based public health systems, integrated with primary health care, for surveillance, testing, tracing, monitoring, public education, and social support, and investment in a skilled workforce
-
•
Investment in public health and scientific literacy, including through educational programmes in schools and universities, to protect the public against misinformation and disinformation
-
•
Inclusive, diverse leadership at all levels of pandemic response by ensuring gender parity and including health workers, civil society, human rights experts, gender experts, and the expertise of social, political, and behavioural scientists
-
•
Investment in supporting scientists to present evidence more effectively to decision makers, and in supporting decision makers in their understanding of how to interpret evidence and implement science-based recommendations and policies
-
•
Investment in behavioural and social sciences research to develop and implement more effective interventions and policies to change behaviours, and therefore reduce the likelihood of pandemics and viral transmission and increase resilience
-
•
Protection of vulnerable groups, including older people, women, children, disadvantaged communities, refugees, Indigenous Peoples, people with disabilities, and people with comorbid medical conditions
-
•
Establishment of safe schools, workplaces, and public spaces, including investments in ventilation and filtration systems as tools to fight disease and promote long-term resilience, health, and wellbeing
-
•
Permission for schools to implement stringent and evidence-supported control strategies early in an outbreak situation, to prioritise in-person learning
-
•
Universal access to digital services, so that digital applications (such as government alerts, transfer payments, emergency services, and contract tracing) reach the entire population
-
•
Social support services that address gender-based violence, mental health disorders, loneliness, indigency, and other social needs
-
•
National and global supply chains for personal protective equipment, testing, diagnostics, vaccines, medicines, and other essential commodities, and management of medical consumable waste
-
•
Global coordination and standardisation of data collection, data quality, monitoring, and reporting, to ensure the disaggregation of data by relevant factors (eg, gender, age, race, and ethnicity)
-
•
Application of a gender-responsive approach to pandemics—including in terms of testing, treatment, and prevention—and equal pay for women workers, with special attention given to unpaid and underpaid workers in the health sector, especially community health workers
-
•
Universal adoption of updated medical, scientific, and public health training and airborne infectious disease exposure standards that reflect the paradigm shift towards more accurate definitions of transmission routes for respiratory infectious disease, and the most effective mitigation strategies for each one, including enhanced building ventilation and air filtration
The Global Health Fund
We call for the creation of an integrated and flexible Global Health Fund with three core financing windows: commodities for disease control, pandemic preparedness and response, and primary health system scale-up in LMICs. This Fund should have representation and leadership from LMICs. Funding for the first window would merge the efforts of the existing Global Fund and the Global Alliance for Vaccines and Immunizations.
The Global Health Fund would require annual disbursements of the order of $60 billion per year (around 0·1% of the GDP of the high-income countries, which is estimated by the IMF to be about $60 trillion in 2022).497 This recommended annual funding of $60 billion would be allocated roughly as follows: commodities, $20 billion per year; pandemic preparedness, $15 billion per year; and support for primary health systems, $25 billion per year. Although many reports on COVID-19 call for collective financing mechanisms for sustainable, predictable, flexible, and scalable financing for pandemic preparedness with the support of WHO, the G20, and the international financing institutions, here we are calling for increased support not only for pandemic preparedness but also for health systems and disease control more generally. We also highlight the design and political advantages of consolidating the target funding into a single Global Health Fund, which will ensure consistency, coordination with WHO, and a holistic vision of health that places the health system at the core.
The Global Health Fund should be closely aligned with the work of WHO. We propose that the Fund has its headquarters in Geneva, but has strong regional offices in each of the six WHO regions. As such, the Fund's overall funding would be centralised but programme design and implementation would be decentralised, fostering strong ownership by the countries of each region and reflecting regional needs and priorities, rather than operating under top-down control from Geneva or from a few donor countries.
The Global Health Fund should be supplemented by an emergency financing mechanism to enable a surge of funding in the face of a global health emergency. Such an emergency mechanism could rely on the borrowing authority of an international financial institution, such as the World Bank, to provide the ability to mobilise at least $10 billion immediately, and possibly far more, in the event of another major global public health emergency.
Sustainable development and a green recovery
We call on the G20 to conduct an urgent review of SDG financing options and to adopt a package of financing policies to expand SDG financing for LMICs in line with needs. As emphasised by the UN Secretary-General in his remarks to the General Assembly in January, 2022: “We must rescue the 2030 Agenda.”498 The COVID-19 pandemic is a setback for sustainable development globally, but building forward is a necessity. Bolstering SDG financing—especially for key physical and digital infrastructure, services, and social protection in low-income countries and LMICs—and the adoption and implementation of ambitious sustainable development policies can help to prevent future global shocks, including pandemics, cybersecurity events, or climate events, and to promote resilience.
Many options are available to scale up SDG financing: donor countries could scale up official development assistance, expand the financing of the multilateral development banks, and promote large flows from capital markets to sovereign borrowers. SDG-based lending should be offered at lower interest rates and longer maturities. Global coordination on tax enforcement and on new taxes (eg, a globally coordinated tax on ultrahigh net worth) could supplement current tax revenues. Other financing channels could include the issuance of SDG bonds by national, provincial, or municipal governments; the launch of an SDG Fund based on large-scale private philanthropy; and global coordination and management of levies on CO2 emissions.
Conclusion: protecting and promoting multilateralism
The COVID-19 crisis has exposed major weaknesses in the UN-based multilateral system, resulting from excessive nationalism, tensions among the major powers, chronic underfinancing of global public goods including the UN system itself, lack of flexibility of intellectual property regimes to ensure that global public goods are available to all, lack of adequate sustainable development financing for LMICs, and the erosion of political support for multilateral solutions by the major powers. Despite major efforts to stimulate recovery and a just transition to sustainable development, the lack of ambition in the global response to COVID-19 is like that of other pressing global challenges, such as the climate emergency; the loss of global biodiversity; the pollution of air, land, and water; the persistence of extreme poverty in the midst of plenty; and the large-scale displacement of people as a result of conflicts, poverty, and environmental stress.
In this light, our most basic recommendation is the strengthening of multilateralism in all crucial dimensions: political, cultural, institutional, and financial. We call for all countries, especially the richest and most powerful, to support, sustain, and bolster the work of the UN system. We call for awareness of the benefits of multilateralism, solidarity, cooperation, and the shared commitment to sustainable development, whether facing pandemics, ending poverty, keeping the peace, or meeting global environmental challenges. We strongly support the call of the UN Secretary-General for a new Common Agenda,499 and urge member states to engage in its implementation constructively and swiftly. We encourage member states to enrich their deliberations and decisions with the voices of civil society, the private sector, local governments, parliaments, academia, and young people, among others. We note the timeliness of recommitting to the Universal Declaration of Human Rights, the UN's moral charter, as we celebrate its 75th anniversary in 2023.
Declaration of interests
SSAK declares grants paid to the Centre for the AIDS Programme of Research in South Africa from the National Institutes of Health (National Institute of Allergy and Infectious Diseases), the South African Medical Research Council, the National Research Foundation, and the European and Developing Countries Clinical Trials Partnership. He is a vice-president of the International Science Council; a commissioner of the African Commission on COVID-19; and a member of the WHO Science Council, the Advisory Council of the Physicians for Human Rights, the Global Medical Advisory Board on COVID-19 for Sanofi Pasteur, and the Scientific Advisory Committee of the Bill & Melinda Gates Foundation. CBa declares consulting fees from and is a member of the advisory board of the Sustainable Development Solutions Network. MEB and PJH are co-directors of a team of scientists at Texas Children's Hospital Center for Vaccine Development, who are co-inventors of a COVID-19 recombinant protein vaccine technology owned by Baylor College of Medicine (BCM) that was licensed by BCM, non-exclusively and with no patent restrictions, to several companies committed to advancing vaccines for low-income and middle-income countries. The co-inventors have no involvement in license negotiations conducted by BCM. Similar to other research universities, a long-standing BCM policy provides its faculty and staff, who make discoveries that result in a commercial license, a share of any royalty income. To date, BCM has not distributed any royalty income to the co-inventors of the COVID-19 recombinant protein vaccine technology. Any such distribution will be undertaken in accordance with BCM policy. CBu declares grants from the Health Research Council of New Zealand, the New Zealand Ministry of Health, and the New Zealand Ministry of Foreign Affairs and Trade; consulting fees from Johnson & Johnson Japan; payment from University of Malaya; and is the president of the Society for Research on Nicotine and Tobacco—Oceania. GCB is co-chair of the UHC2030 International Alliance. AH declares grants and consulting fees from the Wellcome Trust and the Oak Foundation. NJ declares support from the UN Sustainable Development Solutions Network and consulting fees from the University of California, San Francisco Department of Humanities and Social Sciences and the Foundation for Global Governance and Sustainability. ET declares consulting fees from the United Nations Development Programme. VV-F and IS are co-chairs of the Nizami Ganjavi International Centre. MAP declares grants from the Rockefeller Foundation to his institution and is a member of the Board of Directors for Management Sciences for Health, and non-executive Governing Board member of Sidra Medicine. JT declares funds from the Victorian Government to BehaviourWorks Australia for surveys and research on COVID-19 related behaviours, from Monash University and from Melbourne Water. AG was a member of the Open Society Global Drug Policy Program until February, 2022. MH declares funds from the Victorian Government, the New South Wales Government, the Australian Government, and the Macquarie Foundation to the Burnet Institute, Melbourne, VIC, Australia for research and modelling work related to COVID-19, and grants from AbbVie and Gilead Sciences that are unrelated to this work. JVL declares grants from AbbVie, Gilead Sciences, MSD, and Roche Diagnostics, and consulting fees from NovVax, all unrelated to this work. All other authors declare no conflicts of interest. This report does not represent the institutions nor the organisations for which the authors work.
Acknowledgments
Acknowledgments
We thank Jesse Bloom (Fred Hutchinson Cancer Research Center, Seattle, WA, USA), Alina Chan (Broad Institute, Cambridge, MA, USA), Richard Ebright (Rutgers University, Piscataway, NJ, USA), and David Relman (Stanford University, Stanford, CA, USA), for sharing their knowledge. The Commission endeavoured to hear from a widely diverse group of scientists and to follow information as brought to the attention of the Commission.
Contributors
All authors contributed equally to this Commission report.
Supplementary Material
References
- 1.Sachs JD, Horton R, Bagenal J, Ben Amor Y, Karadag Caman O, Lafortune G. The Lancet COVID-19 Commission. Lancet. 2020;396:454–455. doi: 10.1016/S0140-6736(20)31494-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Lancet COVID-19 Commissioners. Task Force Chairs. Commission Secretariat Lancet COVID-19 Commission Statement on the occasion of the 75th session of the UN General Assembly. Lancet. 2020;396:1102–1124. doi: 10.1016/S0140-6736(20)31927-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Commissioners of the Lancet COVID-19 Commission. Task Force Chairs and members of the Lancet COVID-19 Commission. Commission Secretariat and Staff of the Lancet COVID-19 Commission Priorities for the COVID-19 pandemic at the start of 2021: statement of the Lancet COVID-19 Commission. Lancet. 2021;397:947–950. doi: 10.1016/S0140-6736(21)00388-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Lancet COVID-19 Commissioners and Commission Secretariat Statement on the occasion of the G20 Leaders' Summit 2021 Meeting in Rome. Oct 5, 2021. https://covid19commission.org/commpub/statement-on-the-occasion-of-the-g20-leaders-summit-2021-meeting-in-rome
- 5.Jensen K. Prosociality. Curr Biol. 2016;26:R748–R752. doi: 10.1016/j.cub.2016.07.025. [DOI] [PubMed] [Google Scholar]
- 6.Dinić BM, Bodroža B. COVID-19 protective behaviors are forms of prosocial and unselfish behaviors. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.647710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santamaría-García H, Burgaleta M, Legaz A, et al. The price of prosociality in pandemic times. Humanit Soc Sci Commun. 2022;9:15. [Google Scholar]
- 8.Campos-Mercade P, Meier AN, Schneider FH, Wengström E. Prosociality predicts health behaviors during the COVID-19 pandemic. J Public Econ. 2021;195 doi: 10.1016/j.jpubeco.2021.104367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention History of quarantine. July 20, 2020. https://www.cdc.gov/quarantine/historyquarantine.html
- 10.Pew Research Centre Public trust in government: 1958–2022. June 6, 2022. https://www.pewresearch.org/politics/2022/06/06/public-trust-in-government-1958-2022/
- 11.Lazarus JV, Ratzan S, Palayew A, et al. COVID-SCORE: a global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10) PLoS One. 2020;15 doi: 10.1371/journal.pone.0240011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sachs JD. Comparing COVID-19 control in the Asia-Pacific and North Atlantic regions. Asian Econ Pap. 2021;20:30–54. [Google Scholar]
- 13.Jenniskens K, Bootsma MCJ, Damen JAAG, et al. Effectiveness of contact tracing apps for SARS-CoV-2: a rapid systematic review. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-050519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Megnin-Viggars O, Carter P, Melendez-Torres GJ, Weston D, Rubin GJ. Facilitators and barriers to engagement with contact tracing during infectious disease outbreaks: a rapid review of the evidence. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anglemyer A, Moore THM, Parker L, et al. Digital contact tracing technologies in epidemics: a rapid review. Cochrane Database Syst Rev. 2020;8 doi: 10.1002/14651858.CD013699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Regmi K, Lwin CM. Factors associated with the implementation of non-pharmaceutical interventions for reducing coronavirus disease 2019 (COVID-19): a systematic review. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18084274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;9 doi: 10.1002/14651858.CD013574.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burns J, Movsisyan A, Stratil JM, et al. International travel-related control measures to contain the COVID-19 pandemic: a rapid review. Cochrane Database Syst Rev. 2021;3 doi: 10.1002/14651858.CD013717.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shuren J, Stenzel T. South Korea's implementation of a COVID-19 national testing strategy. Health Affairs. May 25, 2021 doi: 10.1377/forefront.20210521.255232. [DOI] [Google Scholar]
- 20.The Royal Society Reproduction number (R) and growth rate (r) of the COVID-19 epidemic in the UK: methods of estimation, data sources, causes of heterogeneity, and use as a guide in policy formulation. Sept 9, 2020. https://royalsociety.org/-/media/policy/projects/set-c/set-covid-19-R-estimates.pdf (preprint).
- 21.Ayouni I, Maatoug J, Dhouib W, et al. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21 doi: 10.1186/s12889-021-11111-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kulldorf M, Gupta S, Bhattacharya J. The Great Barrington Declaration. Oct 4, 2020. https://gbdeclaration.org/#read
- 23.Decary S, Dugas M, Stefan T, et al. Care models for long COVID— a living systematic review. First update—December, 2021. SPOR Evidence Alliance and COVID-END Network. December, 2021. https://sporevidencealliance.ca/wp-content/uploads/2021/12/Care-Models-for-Long-COVID_Update_2021.12.04.pdf
- 24.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thunström L, Newbold S, Finnoff D, Ashworth M, Shogren J. The benefits and costs of using social distancing to flatten the curve for COVID-19. J Benefit Cost Anal. 2020;11:179–195. [Google Scholar]
- 26.Walsh KA, Tyner B, Broderick N, et al. Effectiveness of public health measures to prevent the transmission of SARS-CoV-2 at mass gatherings: a rapid review. Rev Med Virol. 2022;32 doi: 10.1002/rmv.2285. [DOI] [PubMed] [Google Scholar]
- 27.Mendez-Brito A, El Bcheraoui C, Pozo-Martin F. Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. J Infect. 2021;83:281–293. doi: 10.1016/j.jinf.2021.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Organisation for Economic Co-operation and Development Flattening the COVID-19 peak: containment and mitigation policies. March 24, 2020. https://www.oecd.org/coronavirus/policy-responses/flattening-the-covid-19-peak-containment-and-mitigation-policies-e96a4226/
- 29.Bacon SL, Ribero PAB, Stojanovic J, Joyal-Desmarais K, Vieira AM, Yip D. Change in the level of vaccine protection over time in COVID-19 vaccinated individuals: a rapid review. SPOR Evidence Alliance and COVID-END. November, 2021. https://sporevidencealliance.ca/wp-content/uploads/2021/11/Waning-Vaccine-Effectiveness_Update-1-Report_2021.11.26.pdf
- 30.Muehlschlegel PA, Parkinson EA, Chan RY, Arden MA, Armitage CJ. Learning from previous lockdown measures and minimising harmful biopsychosocial consequences as they end: a systematic review. J Glob Health. 2021;11 doi: 10.7189/jogh.11.05008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Office for Health Improvement and Disparities Important findings. In: COVID-19 mental health and wellbeing surveillance: report. April 12, 2021. https://www.gov.uk/government/publications/covid-19-mental-health-and-wellbeing-surveillance-report/2-important-findings-so-far
- 32.Aknin LB, Whillans AV, Norton MI, Dunn EW. Happiness and prosocial behavior: an evaluation of the evidence. In: World Happiness Report. 2019. https://worldhappiness.report/ed/2019/happiness-and-prosocial-behavior-an-evaluation-of-the-evidence/
- 33.Rhoads SA, Gunter D, Ryan RM, Marsh AA. Global variation in subjective well-being predicts seven forms of altruism. Psychol Sci. 2021;32:1247–1261. doi: 10.1177/0956797621994767. [DOI] [PubMed] [Google Scholar]
- 34.Brethel-Haurwitz KM, Marsh AA. Geographical differences in subjective well-being predict extraordinary altruism. Psychol Sci. 2014;25:762–771. doi: 10.1177/0956797613516148. [DOI] [PubMed] [Google Scholar]
- 35.Sandler T. COVID-19 and collective action. Peace Econ Peace Sci Public Policy. 2020;26:1–8. doi: 10.1515/peps-2020-0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Caparrós A, Finus M. The corona-pandemic: a game-theoretic perspective on regional and global governance. Environ Res Econ. 2020;76:913–927. doi: 10.1007/s10640-020-00475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown G, Susskind D. International cooperation during the COVID-19 pandemic. Oxf Rev Econ Policy. 2020;36(suppl 1):S64–S76. [Google Scholar]
- 38.Pekar J, Worobey M, Moshiri N, Scheffler K, Wertheim JO. Timing the SARS-CoV-2 index case in Hubei Province. Science. 2021;372:412–417. doi: 10.1126/science.abf8003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roberts DL, Rossman JS, Jarić I. Dating first cases of COVID-19. PLoS Pathog. 2021;17 doi: 10.1371/journal.ppat.1009620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Margolin J, Meek JG. Intelligence report warned of coronavirus crisis as early as November: sources. ABC News. April 9, 2020 https://abcnews.go.com/Politics/intelligence-report-warned-coronavirus-crisis-early-november-sources/story?id=70031273 [Google Scholar]
- 43.Wu Z, Jin Q, Wu G, et al. SARS-CoV-2's origin should be investigated worldwide for pandemic prevention. Lancet. 2021;398:1299–1303. doi: 10.1016/S0140-6736(21)02020-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bloom JD, Chan YA, Baric RS, et al. Investigate the origins of COVID-19. Science. 2021;372:694. doi: 10.1126/science.abj0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van Helden J, Butler CD, Achaz G, et al. An appeal for an objective, open, and transparent scientific debate about the origin of SARS-CoV-2. Lancet. 2021;398:1402–1404. doi: 10.1016/S0140-6736(21)02019-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Intelligence Council Updated assessment on COVID-19 origins. Oct 29, 2021. https://www.dni.gov/files/ODNI/documents/assessments/Declassified-Assessment-on-COVID-19-Origins.pdf
- 47.WHO WHO-convened global study of origins of SARS-CoV-2: China part. March 30, 2021. https://www.who.int/publications/i/item/who-convened-global-study-of-origins-of-sars-cov-2-china-part
- 48.Boni MF, Lemey P, Jiang X, et al. Evolutionary origins of the SARS-CoV-2 sarbecovirus lineage responsible for the COVID-19 pandemic. Nat Microbiol. 2020;5:1408–1417. doi: 10.1038/s41564-020-0771-4. [DOI] [PubMed] [Google Scholar]
- 49.Hasan A, Paray BA, Hussain A, et al. A review on the cleavage priming of the spike protein on coronavirus by angiotensin-converting enzyme-2 and furin. J Biomol Struct Dyn. 2021;39:3025–3033. doi: 10.1080/07391102.2020.1754293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu Y, Zhao S. Furin cleavage sites naturally occur in coronaviruses. Stem Cell Res. 2020;50 doi: 10.1016/j.scr.2020.102115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu X, Wu Q, Zhang Z. Global diversification and distribution of coronaviruses with furin cleavage sites. Front Microbiol. 2021;12 doi: 10.3389/fmicb.2021.649314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Follis KE, York J, Nunberg JH. Furin cleavage of the SARS coronavirus spike glycoprotein enhances cell–cell fusion but does not affect virion entry. Virology. 2006;350:358–369. doi: 10.1016/j.virol.2006.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holmes EC, Goldstein SA, Rasmussen AL, et al. The origins of SARS-CoV-2: a critical review. Cell. 2021;184:4848–4856. doi: 10.1016/j.cell.2021.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wolfe ND, Dunavan CP, Diamond J. Origins of major human infectious diseases. Nature. 2007;447:279–283. doi: 10.1038/nature05775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shi Z, Hu Z. A review of studies on animal reservoirs of the SARS coronavirus. Virus Res. 2008;133:74–87. doi: 10.1016/j.virusres.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohd HA, Al-Tawfiq JA, Memish ZA. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) origin and animal reservoir. Virol J. 2016;13:87. doi: 10.1186/s12985-016-0544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mallapaty S. Coronaviruses closely related to the pandemic virus discovered in Japan and Cambodia. Nature. 2020;588:15–16. doi: 10.1038/d41586-020-03217-0. [DOI] [PubMed] [Google Scholar]
- 58.Chomel BB, Belotto A, Meslin FX. Wildlife, exotic pets, and emerging zoonoses. Emerg Infect Dis. 2007;13:6–11. doi: 10.3201/eid1301.060480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gibb R, Redding DW, Chin KQ, et al. Zoonotic host diversity increases in human-dominated ecosystems. Nature. 2020;584:398–402. doi: 10.1038/s41586-020-2562-8. [DOI] [PubMed] [Google Scholar]
- 60.Guo H, Hu B, Si H-R, et al. Identification of a novel lineage bat SARS-related coronaviruses that use bat ACE2 receptor. Emerg Microbes Infect. 2021;10:1507–1514. doi: 10.1080/22221751.2021.1956373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wardeh M, Baylis M, Blagrove MSC. Predicting mammalian hosts in which novel coronaviruses can be generated. Nat Commun. 2021;12:780. doi: 10.1038/s41467-021-21034-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xiao X, Newman C, Buesching CD, Macdonald DW, Zhou Z-M. Animal sales from Wuhan wet markets immediately prior to the COVID-19 pandemic. Sci Rep. 2021;11 doi: 10.1038/s41598-021-91470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Frutos R, Serra-Cobo J, Pinault L, Lopez Roig M, Devaux CA. Emergence of bat-related betacoronaviruses: hazard and risks. Front Microbiol. 2021;12 doi: 10.3389/fmicb.2021.591535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ng OW, Tan YJ. Understanding bat SARS-like coronaviruses for the preparation of future coronavirus outbreaks—implications for coronavirus vaccine development. Hum Vaccin Immunother. 2017;13:186–189. doi: 10.1080/21645515.2016.1228500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Inglesby TV, Lipsitch M. Proposed changes to U.S. policy on potential pandemic pathogen oversight and implementation. MSphere. 2020;5:e00919–e00990. doi: 10.1128/mSphere.00990-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Collins FS. Statement on misinformation about NIH support of specific “gain-of-function” research. May 19, 2021. https://www.nih.gov/about-nih/who-we-are/nih-director/statements/statement-misinformation-about-nih-support-specific-gain-function-research
- 67.Lerner S. NIH sent The Intercept 292 fully redacted pages related to virus research in Wuhan. The Intercept. Feb 20, 2022 https://theintercept.com/2022/02/20/nih-coronavirus-research-wuhan-redacted/ [Google Scholar]
- 68.Amendola A, Bianchi S, Gori M, et al. Evidence of SARS-CoV-2 RNA in an oropharyngeal swab specimen, Milan, Italy, early December 2019. Emerg Infect Dis. 2021;27:648–650. doi: 10.3201/eid2702.204632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Apolone G, Montomoli E, Manenti A, et al. Unexpected detection of SARS-CoV-2 antibodies in the prepandemic period in Italy. Tumori. 2021;107:446–451. doi: 10.1177/0300891620974755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Basavaraju SV, Patton ME, Grimm K, et al. Serologic testing of US blood donations to identify severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-reactive antibodies: December 2019–January 2020. Clin Infect Dis. 2021;72:e1004–e1009. doi: 10.1093/cid/ciaa1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carrat F, Figoni J, Henny J, et al. Evidence of early circulation of SARS-CoV-2 in France: findings from the population-based “CONSTANCES” cohort. Eur J Epidemiol. 2021;36:219–222. doi: 10.1007/s10654-020-00716-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gianotti R, Barberis M, Fellegara G, Galván-Casas C, Gianotti E. COVID-19-related dermatosis in November 2019: could this case be Italy's patient zero? Br J Dermatol. 2021;184:970–971. doi: 10.1111/bjd.19804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gragnani L, Monti M, Santini SA, et al. SARS-CoV-2 was already circulating in Italy, in early December 2019. Eur Rev Med Pharmacol Sci. 2021;25:3342–3349. doi: 10.26355/eurrev_202104_25746. [DOI] [PubMed] [Google Scholar]
- 74.Buckley C, Kirkpatrick DD, Qin A, Hernández JC. 25 days that changed the world: how COVID-19 slipped China's grasp. The New York Times, Dec 30, 2020; updated Nov 31, 2021. https://www.nytimes.com/2020/12/30/world/asia/china-coronavirus.html
- 75.WHO COVID-19—China. Jan 5, 2020. https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON229
- 76.Allam Z. Surveying the COVID-19 pandemic and its implications. Elsevier; Oxford: 2020. The first 50 days of COVID-19: a detailed chronological timeline and extensive review of literature documenting the pandemic; pp. 1–7. [Google Scholar]
- 77.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Grady D. Three U.S. airports to check passengers for a deadly Chinese coronavirus. The New York Times. Jan 17, 2020 https://www.nytimes.com/2020/01/17/health/china-coronavirus-airport-screening.html [Google Scholar]
- 79.Nature Coronavirus: the first three months as it happened. Nature. 2020 doi: 10.1038/d41586-020-00154-w. [DOI] [PubMed] [Google Scholar]
- 80.UN Coronavirus: ‘An emergency in China, but not yet a global health emergency’. UN News. Jan 23, 2020 https://news.un.org/en/story/2020/01/1055891 [Google Scholar]
- 81.WHO Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) Jan 30, 2020. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-nCoV)
- 82.Cooper RN. International economic cooperation: is it desirable? Is it likely? Bull Am Acad Arts Sci. 1985;39:11–35. [Google Scholar]
- 83.Cooper RN. In: Can nations agree? Issues in International Economic Cooperation. Cooper RN, Eichengreen B, Holtham G, Putnam RD, Henning CR, editors. Brookings Institution Press; Washington, DC: 1989. International cooperation in public health as a prologue to macroeconomic cooperation. [Google Scholar]
- 84.WHO Constitution of the World Health Organization, 45th edn. Oct 9, 2006. https://www.who.int/publications/m/item/constitution-of-the-world-health-organization
- 85.WHO International Health Regulations. 2005. https://www.who.int/publications/i/item/9789241580496 3rd edn.
- 86.Rogers K, Mandavilli A. Trump administration signals formal withdrawal from W.H.O. The New York Times. July 7, 2020 https://www.nytimes.com/2020/07/07/us/politics/coronavirus-trump-who.html [Google Scholar]
- 87.Keaton J. Associated Press; Jan 21, 2021. Biden's US revives support for WHO, reversing Trump retreat.https://apnews.com/article/us-who-support-006ed181e016afa55d4cea30af236227 [Google Scholar]
- 88.Gostin LO, Klock KA, Clark H, et al. Financing the future of WHO. Lancet. 2022;399:1445–1447. doi: 10.1016/S0140-6736(22)00533-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Daugirdas K, Burci GL. Financing the World Health Organization: what lessons for multilateralism? Int Org Law Rev. 2019;16:299–338. [Google Scholar]
- 90.WHO World Health Assembly agrees to launch process to develop historic global accord on pandemic prevention, preparedness and response. Dec 1, 2021. https://www.who.int/news/item/01-12-2021-world-health-assembly-agrees-to-launch-process-to-develop-historic-global-accord-on-pandemic-prevention-preparedness-and-response
- 91.Sencer DJ, Millar JD. Reflections on the 1976 swine flu vaccination program. Emerg Infect Dis. 2006;12:29–33. doi: 10.3201/eid1201.051007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Krause R. The swine flu episode and the fog of epidemics. Emerg Infect Dis. 2006;12:40–43. doi: 10.3201/eid1201.051132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Centers for Disease Control and Prevention 2009 H1N1 pandemic (H1N1pdm09 virus) 2019. https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html
- 94.WHO Mission summary: WHO field visit to Wuhan, China 20–21 January 2020. Jan 22, 2020. https://www.who.int/china/news/detail/22-01-2020-field-visit-wuhan-china-jan-2020
- 95.Maxmen A. Why did the world's pandemic warning system fail when COVID hit? Nature. 2021;589:499–500. doi: 10.1038/d41586-021-00162-4. [DOI] [PubMed] [Google Scholar]
- 96.The Independent Panel for Pandemic Preparedness & Response COVID-19: make it the Last Pandemic. 2021. https://theindependentpanel.org/wp-content/uploads/2021/05/COVID-19-Make-it-the-Last-Pandemic_final.pdf [DOI] [PMC free article] [PubMed]
- 97.Singh S, McNab C, Olson RM, et al. How an outbreak became a pandemic: a chronological analysis of crucial junctures and obligations in the early months of the COVID-19 pandemic. Lancet. 2021;398:2109–2124. doi: 10.1016/S0140-6736(21)01897-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.WHO WHO Director-General's opening remarks at the media briefing on COVID-19—11 March 2020. March 11, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
- 99.Nebehay S. Reuters; Feb 3, 2020. WHO chief says widespread travel bans not needed to beat China virus.https://www.reuters.com/article/us-china-health-who-idUSKBN1ZX1H3 [Google Scholar]
- 100.von Tigerstrom B, Wilson K. COVID-19 travel restrictions and the International Health Regulations (2005) BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wells CR, Sah P, Moghadas SM, et al. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci USA. 2020;117:7504–7509. doi: 10.1073/pnas.2002616117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Reuters Staff . Reuters; Jan 24, 2020. UPDATE 2-France confirms first three cases of coronavirus in Europe.https://www.reuters.com/article/china-health-france-idUSL8N29T5F4 [Google Scholar]
- 104.Spiteri G, Fielding J, Diercke M, et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.9.2000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.WHO WHO advice for international travel and trade in relation to the outbreak of pneumonia caused by a new coronavirus in China. Jan 10, 2020. https://www.who.int/news-room/articles-detail/who-advice-for-international-travel-and-trade-in-relation-to-the-outbreak-of-pneumonia-caused-by-a-new-coronavirus-in-china
- 106.WHO Updated WHO advice for international traffic in relation to the outbreak of the novel coronavirus 2019-nCoV. Jan 24, 2020. https://www.who.int/news-room/articles-detail/updated-who-advice-for-international-traffic-in-relation-to-the-outbreak-of-the-novel-coronavirus-2019-ncov-24-jan
- 107.WHO Updated WHO advice for international traffic in relation to the outbreak of the novel coronavirus 2019-nCoV. Jan 27, 2020. https://www.who.int/news-room/articles-detail/updated-who-advice-for-international-traffic-in-relation-to-the-outbreak-of-the-novel-coronavirus-2019-ncov
- 108.WHO Updated WHO recommendations for international traffic in relation to COVID-19 outbreak. Feb 29, 2020. https://www.who.int/news-room/articles-detail/updated-who-recommendations-for-international-traffic-in-relation-to-covid-19-outbreak
- 109.Burns J, Movsisyan A, Stratil JM, et al. International travel-related control measures to contain the COVID-19 pandemic: a rapid review. Cochrane Database Syst Rev. 2021;25 doi: 10.1002/14651858.CD013717.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shiraef MA, Friesen P, Feddern L, et al. Did border closures slow SARS-CoV-2? Sci Rep. 2022;12 doi: 10.1038/s41598-022-05482-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.WHO Advice on the use of masks in the context of COVID-19: interim guidance. 5 June 2020. https://apps.who.int/iris/handle/10665/332293
- 112.Mandavilli A. The New York Times; June 5, 2020. WHO finally endorses masks to prevent coronavirus transmission.https://www.nytimes.com/2020/06/05/health/coronavirus-masks-who.html [Google Scholar]
- 113.WHO Advice on the use of masks in the context of COVID-19, interim report. 6 April 2020. https://apps.who.int/iris/handle/10665/331693
- 114.Czypionka T, Greenhalgh T, Bassler D, Bryant MB. Masks and face coverings for the lay public: a narrative update. Ann Intern Med. 2021;174:511–520. doi: 10.7326/M20-6625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chamary J. Forbes; May 4, 2021. WHO finally admits coronavirus is airborne. It's too late.https://www.forbes.com/sites/jvchamary/2021/05/04/who-coronavirus-airborne/?sh=2a33b43a4472 [Google Scholar]
- 117.Marr LC, Tang JW. A paradigm shift to align transmission routes with mechanisms. Clin Infect Dis. 2021;73:1747–1749. doi: 10.1093/cid/ciab722. [DOI] [PubMed] [Google Scholar]
- 118.Morawska L, Allen J, Bahnfleth W, et al. A paradigm shift to combat indoor respiratory infection. Science. 2021;372:689–691. doi: 10.1126/science.abg2025. [DOI] [PubMed] [Google Scholar]
- 119.Ma J, Qi X, Chen H, et al. COVID-19 patients in earlier stages exhaled millions of SARS-CoV-2 per hour. Clin Infect Dis. 2020;72:e652–e654. doi: 10.1093/cid/ciaa1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Adenaiye OO, Lai J, Bueno de Mesquita PJ, et al. Infectious severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in exhaled aerosols and efficacy of masks during early mild infection. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lednicky JA, Lauzardo M, Fan ZH, et al. Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. Int J Infect Dis. 2020;100:476–482. doi: 10.1016/j.ijid.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Santarpia JL, Herrera VL, Rivera DN, et al. The size and culturability of patient-generated SARS-CoV-2 aerosol. J Expo Sci Environ Epidemiol. 2021;2021:1–6. doi: 10.1038/s41370-021-00376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Port JR, Yinda CK, Avanzato VA, et al. Increased aerosol transmission for B.1.1.7 (alpha variant) over lineage A variant of SARS-CoV-2. BioRxiv. 2021 doi: 10.1101/2021.07.26.453518. published online July 26. (preprint). [DOI] [Google Scholar]
- 124.Kutter JS, de Meulder D, Bestebroer TM, et al. SARS-CoV and SARS-CoV-2 are transmitted through the air between ferrets over more than one meter distance. Nat Commun. 2021;12 doi: 10.1038/s41467-021-21918-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Miller SL, Nazaroff WW, Jimenez JL, et al. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air. 2021;31:314–323. doi: 10.1111/ina.12751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Buonanno G, Morawska L, Stabile L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: prospective and retrospective applications. Environ Int. 2020;145 doi: 10.1016/j.envint.2020.106112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Azimi P, Keshavarz Z, Cedeno Laurent JG, Stephens B, Allen JG. Mechanistic transmission modeling of COVID-19 on the Diamond Princess cruise ship demonstrates the importance of aerosol transmission. Proc Natl Acad Sci USA. 2021;118 doi: 10.1073/pnas.2015482118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lendacki FR, Teran RA, Gretsch S, Fricchione MJ, Kerins JL. COVID-19 outbreak among attendees of an exercise facility—Chicago, Illinois, August–September 2020. MMWR Morb Mortal Wkly Rep. 2021;70:321–325. doi: 10.15585/mmwr.mm7009e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Groves LM, Usagawa L, Elm J, et al. Community transmission of SARS-CoV-2 at three fitness facilities—Hawaii, June–July 2020. MMWR Morb Mortal Wkly Rep. 2021;70:316–320. doi: 10.15585/mmwr.mm7009e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Li Y, Cheng P, Jia W. Poor ventilation worsens short-range airborne transmission of respiratory infection. Indoor Air. 2022;32 doi: 10.1111/ina.12946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ou C, Hu S, Luo K, et al. Insufficient ventilation led to a probable long-range airborne transmission of SARS-CoV-2 on two buses. Build Environ. 2022;207 doi: 10.1016/j.buildenv.2021.108414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Parhizkar H, Van Den Wymelenberg KG, Haas CN, Corsi RL. A quantitative risk estimation platform for indoor aerosol transmission of COVID-19. Risk Anal. 2021 doi: 10.1111/risa.13844. published online Oct 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bourouiba L. The fluid dynamics of disease transmission. Annu Rev Fluid Mech. 2021;53:473–508. [Google Scholar]
- 134.Chen W, Zhang N, Wei J, Yen HL, Li Y. Short-range airborne route dominates exposure of respiratory infection during close contact. Build Environ. 2020;176 doi: 10.1016/j.buildenv.2022.109166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cortellessa G, Stabile L, Arpino F, et al. Close proximity risk assessment for SARS-CoV-2 infection. Sci Total Environ. 2021;794 doi: 10.1016/j.scitotenv.2021.148749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Randall K, Ewing ET, Marr LC, Jimenez JL, Bourouiba L. How did we get here: what are droplets and aerosols and how far do they go? A historical perspective on the transmission of respiratory infectious diseases. Interface Focus. 2021;11 doi: 10.1098/rsfs.2021.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Allen JG, Marr LC. Recognizing and controlling airborne transmission of SARS-CoV-2 in indoor environments. Indoor Air. 2020;30:557–558. doi: 10.1111/ina.12697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Greenhalgh T, Jimenez JL, Prather KA, Tufekci Z, Fisman D, Schooley R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet. 2021;397:1603–1605. doi: 10.1016/S0140-6736(21)00869-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Milton DK. A Rosetta Stone for understanding infectious drops and aerosols. J Pediatric Infect Dis Soc. 2020;9:413–415. doi: 10.1093/jpids/piaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tang JW, Marr LC, Milton DK. Aerosols should not be defined by distance travelled. J Hosp Infect. 2021;115:131–132. doi: 10.1016/j.jhin.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Morawska L, Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ Int. 2020;139 doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Morawska L, Milton DK. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2020;71:2311–2313. doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Tang JW, Marr LC, Li Y, Dancer SJ. COVID-19 has redefined airborne transmission. BMJ. 2021;373:n913. doi: 10.1136/bmj.n913. [DOI] [PubMed] [Google Scholar]
- 144.The World Bank World Bank Group's operational response to COVID-19 (coronavirus)—projects list. March 14, 2022. https://www.worldbank.org/en/about/what-we-do/brief/world-bank-group-operational-response-covid-19-coronavirus-projects-list
- 145.The Global Fund Our response to COVID-19. https://www.theglobalfund.org/en/covid-19/
- 146.Institute for Health Metrics and Evaluation COVID-19 projections. May 31, 2022. https://covid19.healthdata.org/projections
- 147.The Economist; Nov 2, 2021. The pandemic's true death toll.https://www.economist.com/graphic-detail/coronavirus-excess-deaths-estimates [Google Scholar]
- 148.Usuf E, Roca A. Seroprevalence surveys in sub-Saharan Africa: what do they tell us? Lancet Glob Health. 2021;9:e724–e725. doi: 10.1016/S2214-109X(21)00092-9. [DOI] [PubMed] [Google Scholar]
- 149.Jha P, Deshmukh Y, Tumbe C, et al. COVID mortality in India: national survey data and health facility deaths. Science. 2022;375:667–671. doi: 10.1126/science.abm5154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Reuters COVID-19 tracker. https://graphics.reuters.com/world-coronavirus-tracker-and-maps/regions/latin-america-and-the-caribbean/
- 151.Nuclear Threat Initiative. Johns Hopkins Center for Health Security Global health security index: building collective action and accountability. October, 2019. https://www.ghsindex.org/wp-content/uploads/2020/04/2019-Global-Health-Security-Index.pdf
- 152.Yu X-Y, Xu C, Wang H-W, et al. Effective mitigation strategy in early stage of COVID-19 pandemic in China. Infect Dis Poverty. 2020;9:141. doi: 10.1186/s40249-020-00759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Silver A. COVID-19: why China is sticking to “zero tolerance” public health measures. BMJ. 2021;375 [Google Scholar]
- 154.Wang MM, Fleßa S. Overcoming COVID-19 in China despite shortcomings of the public health system: what can we learn? Health Econ Rev. 2021;11:25. doi: 10.1186/s13561-021-00319-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.WHO Asia Pacific strategy for emerging diseases and public health emergencies: advancing implementation of the International Health Regulations (2005) 2017. https://apps.who.int/iris/handle/10665/259094
- 156.Sim D, Xinghui K. South China Morning Post; April 17, 2020. How did migrant worker dormitories become Singapore's biggest coronavirus cluster?https://www.scmp.com/week-asia/explained/article/3080466/how-did-migrant-worker-dormitories-become-singapores-biggest [Google Scholar]
- 157.Mathieu E, Ritchie H, Ortiz-Ospina E, et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5:947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 158.Lee JS, Goldstein JM, Moon JL, et al. Analysis of the initial lot of the CDC 2019-Novel Coronavirus (2019-nCoV) real-time RT-PCR diagnostic panel. PLoS One. 2021;16 doi: 10.1371/journal.pone.0260487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Shear MD, Goodnough A, Kaplan S, Fink S, Thomas K, Weiland N. The New York Times; March 28, 2020. The lost month: how a failure to test blinded the U.S. to COVID-19.https://www.nytimes.com/2020/03/28/us/testing-coronavirus-pandemic.html [Google Scholar]
- 160.Solinas-Saunders M. The U.S. federal response to COVID-19 during the first 3 months of the outbreak: was an evidence-based approach an option? Am Rev Public Adm. 2020;50:713–719. [Google Scholar]
- 161.Schuchat A. Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:551–556. doi: 10.15585/mmwr.mm6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sepúlveda J, Feachem NS, Sanders K, Barker F. The United States' response to COVID-19: a case study of the first year. 2021. https://globalhealthsciences.ucsf.edu/sites/globalhealthsciences.ucsf.edu/files/covid-us-case-study.pdf
- 163.Organisation for Economic Co-operation and Development Health at a glance. 2021. https://www.oecd.org/health/health-at-a-glance/
- 164.Hoffmann C, Wolf E. Older age groups and country-specific case fatality rates of COVID-19 in Europe, USA and Canada. Infection. 2021;49:111–116. doi: 10.1007/s15010-020-01538-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Saxena S, Hashmi AZ. COVID-19 in older adults. Cleve Clin J Med. 2021 doi: 10.3949/ccjm.88a.ccc080. published Sept 14. [DOI] [PubMed] [Google Scholar]
- 166.Thakur B, Dubey P, Benitez J, et al. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci Rep. 2021;11 doi: 10.1038/s41598-021-88130-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Dorjee K, Kim H, Bonomo E, Dolma R. Prevalence and predictors of death and severe disease in patients hospitalized due to COVID-19: a comprehensive systematic review and meta-analysis of 77 studies and 38,000 patients. PLoS One. 2020;15 doi: 10.1371/journal.pone.0243191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Anand JC, Donnelly S, Milne A, et al. The COVID-19 pandemic and care homes for older people in Europe—deaths, damage and violations of human rights. Eur J Soc Work. 2021 doi: 10.1080/13691457.2021.1954886. published online Aug 12. [DOI] [Google Scholar]
- 169.Organisation for Economic Co-operation and Development Rising from the COVID-19 crisis: policy responses in the long-term care sector. Dec 15, 2021. https://www.oecd.org/coronavirus/policy-responses/rising-from-the-covid-19-crisis-policy-responses-in-the-long-term-care-sector-34d9e049/
- 170.Sims KM, Foltz J, Skidmore ME. Prisons and COVID-19 spread in the United States. Am J Public Health. 2021;111:1534–1541. doi: 10.2105/AJPH.2021.306352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ralli M, Cedola C, Urbano S, Morrone A, Ercoli L. Homeless persons and migrants in precarious housing conditions and COVID-19 pandemic: peculiarities and prevention strategies. Eur Rev Med Pharmacol Sci. 2020;24:9765–9767. doi: 10.26355/eurrev_202009_23071. [DOI] [PubMed] [Google Scholar]
- 172.Dalsania AK, Fastiggi MJ, Kahlam A, et al. The relationship between social determinants of health and racial disparities in COVID-19 mortality. J Racial Ethn Health Disparities. 2022;9:288–295. doi: 10.1007/s40615-020-00952-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Paremoer L, Nandi S, Serag H, Baum F. COVID-19 pandemic and the social determinants of health. BMJ. 2021;372:n129. doi: 10.1136/bmj.n129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Crawshaw J, Konnyu K, Castillo G, van Allen Z, Grimshaw JM, Presseau J. Factors affecting healthcare worker COVID-19 vaccination acceptance and uptake: a living behavioural science evidence synthesis (v5, Aug 31st, 2021) https://www.mcmasterforum.org/docs/default-source/product-documents/living-evidence-syntheses/covid-19-living-evidence-synthesis-4.5---factors-affecting-covid-19-vaccination-acceptance-and-uptake-among-the-general-public.pdf?sfvrsn=33dc4261_5
- 175.Pei S, Yamana TK, Kandula S, Galanti M, Shaman J. Burden and characteristics of COVID-19 in the United States during 2020. Nature. 2021;598:338–341. doi: 10.1038/s41586-021-03914-4. [DOI] [PubMed] [Google Scholar]
- 176.Pullano G, Pinotti F, Valdano E, Boëlle P-Y, Poletto C, Colizza V. Novel coronavirus (2019-nCoV) early-stage importation risk to Europe, January 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.4.2000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Nadeau SA, Vaughan TG, Scire J, Huisman JS, Stadler T. The origin and early spread of SARS-CoV-2 in Europe. Proc Natl Acad Sci USA. 2021;118 doi: 10.1073/pnas.2012008118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Organisation for Economic Co-operation and Development. EU Health at a glance: Europe 2020. Nov 19, 2020. [DOI]
- 179.European Commission Tourism and Transport Package. May 13, 2020. https://ec.europa.eu/commission/presscorner/detail/en/QANDA_20_870
- 180.Hodcroft EB, Zuber M, Nadeau S, et al. Spread of a SARS-CoV-2 variant through Europe in the summer of 2020. Nature. 2021;595:707–712. doi: 10.1038/s41586-021-03677-y. [DOI] [PubMed] [Google Scholar]
- 181.Our World in Data Coronavirus (COVID-19) vaccinations. https://ourworldindata.org/covid-vaccinations
- 182.Tso FY, Lidenge SJ, Peña PB, et al. High prevalence of pre-existing serological cross-reactivity against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) in sub-Saharan Africa. Int J Infect Dis. 2021;102:577–583. doi: 10.1016/j.ijid.2020.10.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Mulenga LB, Hines JZ, Fwoloshi S, et al. Prevalence of SARS-CoV-2 in six districts in Zambia in July, 2020: a cross-sectional cluster sample survey. Lancet Glob Health. 2021;9:e773–e781. doi: 10.1016/S2214-109X(21)00053-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Lobaloba Ingoba L, Djontu JC, Mfoutou Mapanguy CC, et al. Seroprevalence of anti-SARS-CoV-2 antibodies in a population living in Bomassa village, Republic of Congo. IJID Reg. 2022;2:130–136. doi: 10.1016/j.ijregi.2022.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Nkuba AN, Makiala SM, Guichet E, et al. High prevalence of anti-severe acute respiratory syndrome coronavirus 2 (anti-SARS-CoV-2) antibodies after the first wave of COVID-19 in Kinshasa, Democratic Republic of the Congo: results of a cross-sectional household-based survey. Clin Infect Dis. 2022;74:882–890. doi: 10.1093/cid/ciab515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Mandolo J, Msefula J, Henrion MYR, et al. SARS-CoV-2 exposure in Malawian blood donors: an analysis of seroprevalence and variant dynamics between January 2020 and July 2021. BMC Med. 2021;19:303. doi: 10.1186/s12916-021-02187-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Adetifa IMO, Uyoga S, Gitonga JN, et al. Temporal trends of SARS-CoV-2 seroprevalence during the first wave of the COVID-19 epidemic in Kenya. Nat Commun. 2021;12 doi: 10.1038/s41467-021-24062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Desjardins J. Mapped: the median age of the population on every continent. Feb 15, 2019. https://www.visualcapitalist.com/mapped-the-median-age-of-every-continent/
- 189.Goldstein JR, Lee RD. Demographic perspectives on the mortality of COVID-19 and other epidemics. Proc Natl Acad Sci USA. 2020;117:22035–22041. doi: 10.1073/pnas.2006392117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Amaratunga D, Fernando N, Haigh R, Jayasinghe N. The COVID-19 outbreak in Sri Lanka: a synoptic analysis focusing on trends, impacts, risks and science-policy interaction processes. Prog Disaster Sci. 2020 doi: 10.1016/j.pdisas.2020.100133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Tangkitvanich P. The paradox of Thailand's success in controlling COVID-19. Asian Econ Pap. 2021;20:175–199. [Google Scholar]
- 192.Silver A. COVID-19: what went wrong after initial success in Laos? BMJ. 2022;377:o994. doi: 10.1136/bmj.o994. [DOI] [PubMed] [Google Scholar]
- 193.Nit B, Samy AL, Tan SL, et al. Understanding the slow COVID-19 trajectory of Cambodia. Public Health Pract. 2021;2 doi: 10.1016/j.puhip.2020.100073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Government of India. Ministry of Information and Broadcasting India's response to COVID outbreak. March 28, 2020. https://pib.gov.in/PressReleasePage.aspx?PRID=1608727
- 195.Thiagarajan K. Why is India having a COVID-19 surge? BMJ. 2021;373 doi: 10.1136/bmj.n1124. [DOI] [PubMed] [Google Scholar]
- 196.Bian L, Gao Q, Gao F, et al. Impact of the delta variant on vaccine efficacy and response strategies. Expert Rev Vaccines. 2021;20:1201–1209. doi: 10.1080/14760584.2021.1976153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Raut AP, Huy NT. Political races, religious congregations, and inefficacious measures amid the second wave of COVID-19 in India. Am J Public Health. 2021;111:2100–2102. doi: 10.2105/AJPH.2021.306544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Rocha ICN, Pelayo MGA, Rackimuthu S. Kumbh Mela religious gathering as a massive superspreading event: potential culprit for the exponential surge of COVID-19 cases in India. Am J Trop Med Hyg. 2021;105:868–871. doi: 10.4269/ajtmh.21-0601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Unnithan S. India Today; May 1, 2021. Gasping for breath: India struggles to cope with an acute oxygen crisis in the midst of a deadly second COVID wave.https://www.indiatoday.in/magazine/cover-story/story/20210510-gasping-for-breath-india-struggles-to-cope-with-an-acute-oxygen-crisis-in-the-midst-of-a-deadly-second-covid-wave-1796992-2021-05-01 [Google Scholar]
- 200.Nagaraj A, Srivastava R. Reuters; May 5, 2021. As COVID-19 sweeps rural India, sick struggle to access healthcare.https://www.reuters.com/article/us-health-coronavirus-india-villages-idUSKBN2CM0WR [Google Scholar]
- 201.Murhekar MV, Bhatnagar T, Thangaraj JWV, et al. Seroprevalence of IgG antibodies against SARS-CoV-2 among the general population and healthcare workers in India, June–July 2021: a population-based cross-sectional study. PLoS Med. 2021;18 doi: 10.1371/journal.pmed.1003877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.COVID19 Bharat. https://covid19bharat.org
- 203.Institute for Health Metrics and Evaluation COVID-19 Projections—United Arab Emirates. https://covid19.healthdata.org/united-arab-emirates?view=vaccinations&tab=trend
- 204.Institute for Health Metrics and Evaluation COVID-19 Projections—Yemen. https://covid19.healthdata.org/yemen?view=vaccinations&tab=trend
- 205.Institute for Health Metrics and Evaluation COVID-19 Projections—Afghanistan. https://covid19.healthdata.org/afghanistan?view=vaccinations&tab=trend
- 206.Nishiura H, Kimihito I, Anzai A, Kobayashi T, Piantham C, Rodríguez-Morales AJ. Relative reproduction number of SARS-CoV-2 omicron (B.1.1.529) compared with delta variant in South Africa. J Clin Med. 2022;11:30. doi: 10.3390/jcm11010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Moayyedi P. The effects of vaccination in immunocompromised pediatric people. Jan 3, 2022. https://www.mcmasterforum.org/docs/default-source/product-documents/rapid-responses/the-effects-of-vaccination-in-immunocompromised-pediatric-people.pdf?sfvrsn=f8c1fe0d_11
- 208.Universidad de Antioquia. McMaster University. COVID-END COVID-19 living evidence synthesis # 8 (version 8.7) March 14, 2022. https://www.mcmasterforum.org/docs/default-source/product-documents/living-evidence-syntheses/covid-19-living-evidence-synthesis-8.7---what-is-the-effectiveness-of-available-covid-19-vaccines-for-children-and-adolescents-including-variants-of-concern.pdf?sfvrsn=77c144ec_7
- 209.Paget J, Spreeuwenberg P, Charu V, et al. Global mortality associated with seasonal influenza epidemics: new burden estimates and predictors from the GLaMOR Project. J Glob Health. 2019;9 doi: 10.7189/jogh.09.020421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Murray CJL. COVID-19 will continue but the end of the pandemic is near. Lancet. 2022;399:417–419. doi: 10.1016/S0140-6736(22)00100-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.WHO Two years on, we could be entering a new phase in the pandemic with plausible hope for stabilization, yet too early to drop our guard. Jan 24, 2022. https://www.who.int/europe/news/item/24-01-2022-two-years-on-we-could-be-entering-a-new-phase-in-the-pandemic-with-plausible-hope-for-stabilization-yet-too-early-to-drop-our-guard
- 212.Kilbourne ED. Influenza pandemics of the 20th century. Emerg Infect Dis. 2006;12:9–14. doi: 10.3201/eid1201.051254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Centers for Disease Control and Prevention 1957–1958 pandemic (H2N2 virus) Jan 2, 2019. https://www.cdc.gov/flu/pandemic-resources/1957-1958-pandemic.html
- 214.Centers for Disease Control and Prevention 1968 pandemic (H3N2 virus) Jan 2, 2019. https://www.cdc.gov/flu/pandemic-resources/1968-pandemic.html
- 215.International Monetary Fund World Economic Outlook Update, January 2022: rising caseloads, a disrupted recovery, and higher inflation. https://www.imf.org/en/Publications/WEO/Issues/2022/01/25/world-economic-outlook-update-january-2022
- 216.Stevens L. Gallup Blog; Dec 17, 2021. Nearly 3 in 10 doubt leaders value scientific expertise.https://news.gallup.com/opinion/gallup/358181/nearly-doubt-leaders-value-scientific-expertise.aspx [Google Scholar]
- 217.Summers J. NPR; Oct 2, 2020. Timeline: how Trump has downplayed the coronavirus pandemic.https://www.npr.org/sections/latest-updates-trump-covid-19-results/2020/10/02/919432383/how-trump-has-downplayed-the-coronavirus-pandemic [Google Scholar]
- 218.France 24; June 19, 2021. Bolsonaro's most controversial coronavirus quotes.https://www.france24.com/en/live-news/20210619-bolsonaro-s-most-controversial-coronavirus-quotes [Google Scholar]
- 219.Agren D. The Guardian; March 25, 2020. Coronavirus advice from Mexico's president: ‘Live life as usual’.https://www.theguardian.com/world/2020/mar/25/coronavirus-advice-from-mexicos-president-live-life-as-usual [Google Scholar]
- 220.Wolfe D, Dale D. CNN; Oct 31, 2020. ‘It's going to disappear’: a timeline of Trump's claims that COVID-19 will vanish.https://edition.cnn.com/interactive/2020/10/politics/covid-disappearing-trump-comment-tracker/ [Google Scholar]
- 221.Breuninger K. CNBC; March 24, 2020. Trump wants ‘packed churches’ and economy open again on Easter despite the deadly threat of coronavirus.https://www.cnbc.com/2020/03/24/coronavirus-response-trump-wants-to-reopen-us-economy-by-easter.html [Google Scholar]
- 222.Linthicum K. Los Angeles Times; March 19, 2020. Amid growing coronavirus threat, Mexico's president says he's putting trust in good-luck charms.https://www.latimes.com/world-nation/story/2020-03-19/as-mexican-peso-collapses-over-coronavirus-threat-criticism-falls-on-president-lopez-obrador [Google Scholar]
- 223.Grillo I. The New York Times; March 23, 2020. Mexico, the Coronavirus and the hugging president.https://www.nytimes.com/2020/03/23/opinion/mexico-coronavirus-amlo.html [Google Scholar]
- 224.Dada S, Ashworth HC, Bewa MJ, Dhatt R. Words matter: political and gender analysis of speeches made by heads of government during the COVID-19 pandemic. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2020-003910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Johnson C, Williams B. Gender and political leadership in a time of COVID. Polit Gend. 2020;16:943–950. [Google Scholar]
- 226.The Lancet Infectious Diseases. The COVID-19 infodemic. Lancet Infect Dis. 2020;20:875. doi: 10.1016/S1473-3099(20)30565-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Institute of Health Metrics and Evaluation COVID-19 projections: cumulative deaths—Iceland. Jan 20, 2022. https://covid19.healthdata.org/iceland?view=cumulative-deaths&tab=trend
- 228.Institute of Health Metrics and Evaluation COVID-19 projections: cumulative deaths—Norway. Jan 20, 2022. https://covid19.healthdata.org/norway?view=cumulative-deaths&tab=trend
- 229.Claeson M, Hanson S. COVID-19 and the Swedish enigma. Lancet. 2021;397:259–261. doi: 10.1016/S0140-6736(20)32750-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Institute of Health Metrics and Evaluation COVID-19 projections: cumulative deaths—Sweden. Jan 20, 2022. https://covid19.healthdata.org/sweden?view=cumulative-deaths&tab=trend
- 231.Iosifidis P, Nicoli N. Routledge; Abingdon: 2021. Digital democracy, social media and disinformation. [Google Scholar]
- 232.Singh S, Bagchi KKJ. Facebook. In: How internet platforms are combating disinformation and misinformation in the age of COVID-19. June 1, 2020. https://www.newamerica.org/oti/reports/how-internet-platforms-are-combating-disinformation-and-misinformation-age-covid-19/
- 233.Gabarron E, Oyeyemi SO, Wynn R. COVID-19-related misinformation on social media: a systematic review. Bull World Health Organ. 2021;99:455–463A. doi: 10.2471/BLT.20.276782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Gisondi MA, Barber R, Faust JS, et al. A deadly infodemic: social media and the power of COVID-19 misinformation. J Med Internet Res. 2022;24 doi: 10.2196/35552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Belluz J, Lavis J. The New York Times; Feb 8, 2022. Joe Rogan is a drop in the ocean of medical misinformation.https://www.nytimes.com/2022/02/08/opinion/joe-rogan-health-misinformation-solutions.html [Google Scholar]
- 236.Wang X, Zhang M, Fan W, Zhao K. Understanding the spread of COVID-19 misinformation on social media: the effects of topics and a political leader's nudge. J Assoc Inf Sci Technol. 2022;73:726–737. doi: 10.1002/asi.24576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Parmet WE, Paul J. COVID-19: the first posttruth pandemic. Am J Public Health. 2020;110:945–946. [Google Scholar]
- 238.Tagliabue F, Galassi L, Mariani P. The “pandemic” of disinformation in COVID-19. SN Compr Clin Med. 2020;2:1287–1289. doi: 10.1007/s42399-020-00439-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Nelson JQ. Fox News; July 21, 2020. Hydroxychloroquine could save up to 100,000 lives if used for COVID-19: Yale epidemiology professor.https://www.foxnews.com/media/hydroxychloroquine-could-save-lives-ingraham-yale-professor [Google Scholar]
- 240.South Carolina Department of Health and Environmental Control The dangers of using hydroxychloroquine and ivermectin for preventing or treating COVID-19. https://scdhec.gov/covid19/dangers-using-hydroxychloroquine-ivermectin-preventing-or-treating-covid-19
- 241.Mendel A, Bernatsky S, Askanase A, et al. Hydroxychloroquine shortages among patients with systemic lupus erythematosus during the COVID-19 pandemic: experience of the Systemic Lupus International Collaborating Clinics. Ann Rheum Dis. 2021;80:1–2. doi: 10.1136/annrheumdis-2020-218164. [DOI] [PubMed] [Google Scholar]
- 242.van der Linden S, Roozenbeek J, Compton J. Inoculating against fake news about COVID-19. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.566790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Li HOY, Bailey A, Huynh D, Chan J. YouTube as a source of information on COVID-19: a pandemic of misinformation? BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Hotez PJ. Mounting antiscience aggression in the United States. PLoS Biol. 2021;19 doi: 10.1371/journal.pbio.3001369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Jia KM, Hanage WP, Lipsitch M, Swerdlow DL. Excess COVID-19 associated deaths among the unvaccinated population ≥18 years old in the US, May 30–December 4, 2021. medRxiv. 2022 doi: 10.1101/2022.02.10.22270823. published online Feb 13. (preprint). [DOI] [Google Scholar]
- 246.Hotez PJ. Anti-science extremism in America: escalating and globalizing. Microbes Infect. 2020;22:505–507. doi: 10.1016/j.micinf.2020.09.005. [DOI] [PubMed] [Google Scholar]
- 247.EuroNews, AP . EuroNews; Jan 28, 2022. COVID vaccine misinformation violates human rights, says Pope Francis.https://www.euronews.com/my-europe/2022/01/28/covid-vaccine-misinformation-violates-human-rights-says-pope-francis [Google Scholar]
- 248.Shear MD. The New York Times; April 7, 2020. Trump attacks W.H.O. over criticisms of U.S. approach to coronavirus.https://www.nytimes.com/2020/04/07/us/politics/coronavirus-trump-who.html [Google Scholar]
- 249.Reuters Staff . Reuters; June 9, 2020. Brazil to consider leaving World Health Organization: Bolsonaro.https://www.reuters.com/article/us-brazil-bolsonaro-who-idUSKBN23G27R [Google Scholar]
- 250.Horton R. Offline: why President Trump is wrong about WHO. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30969-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Ricard J, Medeiros J. Using misinformation as a political weapon: COVID-19 and Bolsonaro in Brazil. Harv Kennedy Sch Misinformation Rev. 2020 doi: 10.37016/mr-2020-013. published online April 20. [DOI] [Google Scholar]
- 252.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Girum T, Lentiro K, Geremew M, Migora B, Shewamare S, Shimbre MS. Optimal strategies for COVID-19 prevention from global evidence achieved through social distancing, stay at home, travel restriction and lockdown: a systematic review. Arch Public Health. 2021;79:150. doi: 10.1186/s13690-021-00663-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Scientific Advisory Group for Emergencies SPI-B: Sustaining behaviours to reduce SARS-CoV-2 transmission, 22 April 2021. July 5, 2021. https://www.gov.uk/government/publications/spi-b-sustaining-behaviours-to-reduce-sars-cov-2-transmission-30-april-2021/spi-b-sustaining-behaviours-to-reduce-sars-cov-2-transmission-22-april-2021
- 255.Han Q, Zheng B, Cristea M, et al. Trust in government regarding COVID-19 and its associations with preventive health behaviour and prosocial behaviour during the pandemic: a cross-sectional and longitudinal study. Psychol Med. 2021 doi: 10.1017/S0033291721001306. published March 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Gelfand MJ, Jackson JC, Pan X, et al. The relationship between cultural tightness–looseness and COVID-19 cases and deaths: a global analysis. Lancet Planet Health. 2021;5:e135–e144. doi: 10.1016/S2542-5196(20)30301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.YouGov YouGov COVID-19 behaviour changes tracker: wearing a face mask when in public places. https://today.yougov.com/topics/international/articles-reports/2020/03/17/personal-measures-taken-avoid-covid-19
- 258.Carnegie Endowment for International Peace Global protest tracker. https://carnegieendowment.org/publications/interactive/protest-tracker
- 259.Center for Countering Digital Hate The disinformation dozen: why platforms must act on twelve leading online anti-vaxxers. March 24, 2021. https://counterhate.com/research/the-disinformation-dozen
- 260.Parthasarathi A, Puvvada RK, Basappa S, Thirumala Krishna M. Global intention of the general public to undergo COVID-19 vaccination: time trends and risk factors for vaccine refusal, a systematic review and meta-analysis [version 1; peer review: 1 approved with reservations] Wellcome Open Res. 2022;7:17. [Google Scholar]
- 261.Germani F, Biller-Andorno N. The anti-vaccination infodemic on social media: a behavioral analysis. PLoS One. 2021;16 doi: 10.1371/journal.pone.0247642. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 262.Wynants L, Calster B, Collins G, Riley R, Heinze G, Schuit E, et al. Prediction models for diagnosis and prognosis of COVID-19 infection: systematic review and critical appraisal. BMJ. 2020;369 doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Gates M, Pillay J, Wingert A, et al. Risk factors associated with severe outcomes of COVID-19: an updated rapid review to inform national guidance on vaccine prioritization in Canada. medRxiv. 2021 doi: 10.1101/2021.04.23.21256014. published online Nov 28. (preprint). [DOI] [Google Scholar]
- 264.Li X, Zhong X, Wang Y, Zeng X, Luo T, Liu Q. Clinical determinants of the severity of COVID-19: a systematic review and meta-analysis. PLoS One. 2021;16 doi: 10.1371/journal.pone.0250602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Himmels JPW, Borge TC, Brurberg KG, Gravningen KM. COVID-19: COVID-19 and risk factors for hospital admission, severe disease and death—a rapid review, 4th update. May, 2021. https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2021/covid-19-and-risk-factors-for-hospital-admission-severe-disease-and-death–a-rapid-review-4th-update-report-2021.pdf
- 266.Izcovich A, Ragusa MA, Tortosa F, et al. Prognostic factors for severity and mortality in patients infected with COVID-19: a systematic review. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Kola L, Kumar M, Kohrt BA, Fatodu T, Olayemi BA, Adefolarin AO. Strengthening public mental health during and after the acute phase of the COVID-19 pandemic. Lancet. 2022;399:1851–1852. doi: 10.1016/S0140-6736(22)00523-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Organisation for Economic Co-operation and Development A new benchmark for mental health systems: tackling the social and economic costs of mental ill-health. June 8, 2021. [DOI]
- 269.Organisation for Economic Co-operation and Development Tackling the mental health impact of the COVID-19 crisis: an integrated, whole-of-society response. May 12, 2021. https://www.oecd.org/coronavirus/policy-responses/tackling-the-mental-health-impact-of-the-covid-19-crisis-an-integrated-whole-of-society-response-0ccafa0b/
- 270.Aknin LB, Andretti B, Goldszmidt R, et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health. 2022;7:e417–e426. doi: 10.1016/S2468-2667(22)00060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Aknin LB, De Neve J-E, Dunn EW, et al. Mental health during the first year of the COVID-19 pandemic: a review and recommendations for moving forward. Perspect Psychol Sci. 2022;17:915–936. doi: 10.1177/17456916211029964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Sun Y, Wu Y, Bonardi O, et al. Comparison of mental health symptoms prior to and during COVID-19: evidence from a living systematic review and meta-analysis. medRxiv. 2021 doi: 10.1101/2021.05.10.21256920. published online May 11. (preprint). [DOI] [Google Scholar]
- 275.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Gaffney AW, Himmelstein DU, Woolhandler S. Trends and disparities in teleworking during the COVID-19 pandemic in the USA: May 2020–February 2021. J Gen Intern Med. 2021;36:3647–3649. doi: 10.1007/s11606-021-07078-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Goldman N, Pebley AR, Lee K, Andrasfay T, Pratt B. Racial and ethnic differentials in COVID-19-related job exposures by occupational standing in the US. PLoS One. 2021;16 doi: 10.1371/journal.pone.0256085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Feldman JM, Bassett MT. Variation in COVID-19 mortality in the US by race and ethnicity and educational attainment. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.35967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Njoku A, Joseph M, Felix R. Changing the narrative: structural barriers and racial and ethnic inequities in COVID-19 vaccination. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18189904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Falk G, Romero PD, Nicchitta IA, Nyhof EC. Unemployment rates during the COVID-19 pandemic. Aug 20, 2021. https://crsreports.congress.gov/product/pdf/R/R46554
- 281.Oxford Economics Tourism-related employment report—September 2021. http://blog.oxfordeconomics.com/content/us-travel-and-tourism-employment-report-september-2021
- 282.Lee S, Schmidt-Klau D, Verick S. The labour market impacts of the COVID-19: a global perspective. Indian J Labour Econ. 2020;63:11–15. doi: 10.1007/s41027-020-00249-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Srivastava S. Bloomberg; Dec 1, 2021. A million frontline COVID workers demand India boost $40 pay.https://www.bloomberg.com/news/articles/2021-12-01/women-on-frontlines-of-india-s-vaccine-drive-threaten-to-strike [Google Scholar]
- 284.Cukier A, Vogel L. Escalating violence against health workers prompts calls for action. CMAJ. 2021;193 doi: 10.1503/cmaj.1095980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Su Z, Cheshmehzangi A, McDonnell D, Šegalo S, Ahmad J, Bennett B. Gender inequality and health disparity amid COVID-19. Nurs Outlook. 2022;70:89–95. doi: 10.1016/j.outlook.2021.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Chu IY, Alam P, Larson HJ, Lin L. Social consequences of mass quarantine during epidemics: a systematic review with implications for the COVID-19 response. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Flor LS, Friedman J, Spencer CN, et al. Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: a comprehensive review of data from March, 2020, to September, 2021. Lancet. 2022;399:2381–2397. doi: 10.1016/S0140-6736(22)00008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Morgan R, Pimenta DN, Rashid S. Gender equality and COVID-19: act now before it is too late. Lancet. 2022;399:2327–2329. doi: 10.1016/S0140-6736(22)00278-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11 doi: 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Global Health 50/50. International Center for Research on Women. African Population and Health Research Center The sex, gender and COVID-19 project. 2021. https://globalhealth5050.org/the-sex-gender-and-covid-19-project/
- 291.International Labour Organization ILO monitor: COVID-19 and the world of work. Third edition. April 29, 2020. https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/documents/briefingnote/wcms_743146.pdf
- 292.Women in Informal Employment: Globalizing and Organizing COVID-19 and the informal economy: round 1 global summary. July, 2021. https://www.wiego.org/publications/covid-19-and-informal-economy-round-1-global-summary
- 293.Boniol M, McIsaac M, Xu L, Wuliji T, Diallo K, Campbell J. Gender equity in the health workforce: analysis of 104 countries. March, 2019. https://apps.who.int/iris/handle/10665/311314
- 294.WHO Delivered by women, led by men: a gender and equity analysis of the global health and social workforce. March, 2019. https://apps.who.int/iris/handle/10665/311322
- 295.Garijo B. COVID-19 highlights how caregiving fuels gender inequality. April 24, 2020. https://www.weforum.org/agenda/2020/04/covid-19-highlights-how-caregiving-fuels-gender-inequality/
- 296.National Collaborating Centre for Methods and Tools What is known about the impact of the COVID-19 pandemic on families with children? July 22, 2020. https://res.nccmt.ca/family-life-EN
- 297.Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustain Sci Pract Policy. 2020;16:67–73. [Google Scholar]
- 298.International Labour Organization Building forward fairer: women's rights to work and at work at the core of the COVID-19 recovery. July 19, 2021. https://www.ilo.org/gender/Informationresources/Publications/WCMS_814499/lang--en/index.htm
- 299.US Census Bureau Tracking job losses for mothers of school-age children during a health crisis. March 3, 2021. https://www.census.gov/library/stories/2021/03/moms-work-and-the-pandemic.html
- 300.Kourti A, Stavridou A, Panagouli E, et al. Domestic violence during the COVID-19 pandemic: a systematic review. Trauma Violence Abuse. 2021 doi: 10.1177/15248380211038690. published online Aug 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Piquero AR, Jennings WG, Jemison E, Kaukinen C, Knaul FM. Domestic violence during the COVID-19 pandemic—evidence from a systematic review and meta-analysis. J Crim Justice. 2021;74 doi: 10.1016/j.jcrimjus.2021.101806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.WHO Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report. Aug 27, 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1
- 303.National Collaborating Centre for Methods and Tools Rapid review update 1: what are the risk factors associated with severe COVID-19 outcomes in children 12 years and under? Jan 18, 2022. https://www.nccmt.ca/pdfs/res/risk-factors-children
- 304.Barron GC, Laryea-Adjei G, Vike-Freiberga V, et al. Safeguarding people living in vulnerable conditions in the COVID-19 era through universal health coverage and social protection. Lancet Public Health. 2022;7:e86–e92. doi: 10.1016/S2468-2667(21)00235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.UN Sustainable Development Group Policy brief: education during COVID-19 and beyond. August, 2020. https://unsdg.un.org/resources/policy-brief-education-during-covid-19-and-beyond
- 306.UNESCO 1.3 billion learners are still affected by school or university closures, as educational institutions start reopening around the world, says UNESCO. April 29, 2020. https://www.unesco.org/en/articles/13-billion-learners-are-still-affected-school-or-university-closures-educational
- 307.National Collaborating Centre for Methods and Tools . McMaster University; Hamilton, ON: 2021. Living rapid review update 16: what is the specific role of daycares and schools in COVID-19 transmission? [Google Scholar]
- 308.National Collaborating Centre for Methods and Tools Living rapid review update 4: what is known about the risk of transmission of COVID-19 within post-secondary institutions and the strategies to mitigate on-campus outbreaks? Feb 4, 2022. https://www.nccmt.ca/covid-19/covid-19-rapid-evidence-service/34
- 309.Xu W, Li X, Dong Y, et al. SARS-CoV-2 transmission in schools: an updated living systematic review (version 2; November 2020) J Glob Health. 2021;11 doi: 10.7189/jogh.11.10004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.The Lancet COVID-19 Commission India Task Force Reopening schools after COVID-19 closures. April, 2021. https://covid19commission.org/regional-task-force-india
- 311.Levinson M, Geller AC, Allen JG. Health equity, schooling hesitancy, and the social determinants of learning. Lancet Reg Health Am. 2021;2 doi: 10.1016/j.lana.2021.100032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.The Lancet COVID-19 Commission Regional Task Force: Latin America and the Caribbean Regional coordination for strengthening pandemic preparedness, vaccine access, and effective implementation of vaccine deployment plans. November, 2021. https://covid19commission.org/regional-task-force-lac
- 313.UNICEF Nutrition crisis looms as more than 39 billion in-school meals missed since start of pandemic—UNICEF and WFP. Jan 27, 2021. https://www.unicef.org/press-releases/nutrition-crisis-looms-more-39-billion-school-meals-missed-start-pandemic-unicef-and
- 314.UNICEF The state of the world's children 2021—on my mind: promoting, protecting and caring for children's mental health. October, 2021. https://www.unicef.org/reports/state-worlds-children-2021
- 315.UNESCO Learning poverty. 2019. https://gaml.uis.unesco.org/learning-poverty/
- 316.The World Bank Urgent, effective action required to quell the impact of COVID-19 on education worldwide. Jan 22, 2021. https://www.worldbank.org/en/news/immersive-story/2021/01/22/urgent-effective-action-required-to-quell-the-impact-of-covid-19-on-education-worldwide
- 317.Agarwal R. IMFBlog; Feb 3, 2022. Pandemic scars may be twice as deep for students in developing countries.https://blogs.imf.org/2022/02/03/pandemic-scars-may-be-twice-as-deep-for-students-in-developing-countries/ [Google Scholar]
- 318.International Monetary Fund Fiscal Monitor. April 2021. https://www.imf.org/en/Publications/FM/Issues/2021/03/29/fiscal-monitor-april-2021
- 319.Lessler J, Grabowski MK, Grantz KH, et al. Household COVID-19 risk and in-person schooling. Science. 2021;372:1092–1097. doi: 10.1126/science.abh2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Zimmerman KO, Akinboyo IC, Brookhart MA, et al. Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics. 2021;147 doi: 10.1542/peds.2020-048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Oxfam Ten richest men double their fortunes in pandemic while incomes of 99 percent of humanity fall. Jan 17, 2022. https://www.oxfam.org.uk/mc/np588q/
- 322.UN Population Fund Impact of the COVID-19 pandemic on family planning and ending gender-based violence, female genital mutilation and child marriage. April, 2020. https://www.unfpa.org/resources/impact-COVID-19-pandemic-family-planning-and-ending-gender-based-violence-female-genital
- 323.The World Bank GDP growth (annual %)—India. https://data.worldbank.org/indicator/NY.GDP.MKTP.KD.ZG?locations=IN
- 324.Vyas M. Impact of lockdown on labour in India. Indian J Labour Econ. 2020;63:1–5. doi: 10.1007/s41027-020-00259-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Adhikari A, Goregaonkar N, Narayanan R, Panicker N, Ramamoorthy N. Manufactured maladies: lives and livelihoods of migrant workers during COVID-19 lockdown in India. Indian J Labour Econ. 2020;63:969–997. doi: 10.1007/s41027-020-00282-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Devakumar D, Shannon G, Bhopal SS, Abubakar I. Racism and discrimination in COVID-19 responses. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Gover AR, Harper SB, Langton L. Anti-Asian hate crime during the COVID-19 pandemic: exploring the reproduction of inequality. Am J Crim Justice. 2020;45:647–667. doi: 10.1007/s12103-020-09545-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Zhang Y, Zhang L, Benton F. Hate crimes against Asian Americans. Am J Crim Justice. 2021 doi: 10.1007/s12103-020-09602-9. published online Jan 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Kagumire R. Al Jazeera; Dec 6, 2021. The colonial undertones of omicron travel bans.https://www.aljazeera.com/opinions/2021/12/6/the-colonial-roots-of-western-responses-to-omicron [Google Scholar]
- 330.Mallapaty S. Omicron-variant border bans ignore the evidence, say scientists. Nature. 2021;600:199. doi: 10.1038/d41586-021-03608-x. [DOI] [PubMed] [Google Scholar]
- 331.Mendelson M, Venter F, Moshabela M, et al. The political theatre of the UK's travel ban on South Africa. Lancet. 2021;398:2211–2213. doi: 10.1016/S0140-6736(21)02752-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.WHO WHO Director-General's opening remarks at the media briefing on COVID-19—20 July 2020. July 20, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—20-july-2020
- 333.UN Women Addressing the economic fallout of COVID-19: pathways and policy options for a gender-responsive recovery. 2020. https://www.unwomen.org/en/digital-library/publications/2020/06/policy-brief-addressing-the-economic-fallout-of-covid-19
- 334.Gillard E-C. Chatham House; Dec 16, 2020. COVID-19 vaccine: reaching people in areas controlled by armed groups.https://www.chathamhouse.org/2020/12/covid-19-vaccine-reaching-people-areas-controlled-armed-groups [Google Scholar]
- 335.UN High Commissioner for Refugees 1 percent of humanity displaced: UNHCR global trends report. June 18, 2020. https://www.unhcr.org/uk/news/press/2020/6/5ee9db2e4/1-cent-humanity-displaced-unhcr-global-trends-report.html
- 336.Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15:869–875. doi: 10.1016/j.dsx.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Crook H, Raza S, Nowell J, Young M, Edison P. Long COVID—mechanisms, risk factors, and management. BMJ. 2021;374 doi: 10.1136/bmj.n1648. [DOI] [PubMed] [Google Scholar]
- 338.WHO A clinical case definition of post COVID-19 condition by a Delphi consensus. Oct 6, 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 [DOI] [PMC free article] [PubMed]
- 339.Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis. 2021;53:737–754. doi: 10.1080/23744235.2021.1924397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Brackel CLH, Lap CR, Buddingh EP, et al. Pediatric long-COVID: an overlooked phenomenon? Pediatr Pulmonol. 2021;56:2495–2502. doi: 10.1002/ppul.25521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Nabavi N. Long COVID: how to define it and how to manage it. BMJ. 2020;370 doi: 10.1136/bmj.m3489. [DOI] [PubMed] [Google Scholar]
- 342.Aiyegbusi OL, Hughes SE, Turner G, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021;114:428–442. doi: 10.1177/01410768211032850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Graham EL, Clark JR, Orban ZS, et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized COVID-19 “long haulers”. Ann Clin Transl Neurol. 2021;8:1073–1085. doi: 10.1002/acn3.51350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Stefano GB. Historical insight into infections and disorders associated with neurological and psychiatric sequelae similar to long COVID. Med Sci Monit. 2021;27 doi: 10.12659/MSM.931447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Lamb LE, Timar R, Wills M, et al. Long COVID and COVID-19-associated cystitis (CAC) Int Urol Nephrol. 2022;54:17–21. doi: 10.1007/s11255-021-03030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Assaf G, Davis H, McCorkell L. An analysis of the prolonged COVID-19 symptoms survey by patient-led research team. May 11, 2020. https://patientresearchcovid19.com/research/report-1/
- 347.Falahi S, Kenarkoohi A. COVID-19 reinfection: prolonged shedding or true reinfection? New Microbes New Infect. 2020;38 doi: 10.1016/j.nmni.2020.100812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:993–998. doi: 10.15585/mmwr.mm6930e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Khamsi R. Rogue antibodies could be driving severe COVID-19. Nature. 2021;590:29–31. doi: 10.1038/d41586-021-00149-1. [DOI] [PubMed] [Google Scholar]
- 351.Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2022;28:611.e9–611.e16. doi: 10.1016/j.cmi.2021.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.UK Health Security Agency COVID-19 Evidence Team The effectiveness of vaccination against long COVID: a rapid evidence briefing. February, 2022. https://ukhsa.koha-ptfs.co.uk/cgi-bin/koha/opac-detail.pl?biblionumber=64359
- 354.Sivan M, Greenhalgh T, Milne R, Delaney B. Are vaccines a potential treatment for long COVID? BMJ. 2022;377:o988. doi: 10.1136/bmj.o988. [DOI] [PubMed] [Google Scholar]
- 355.Ayoubkhani D, Bermingham C, Pouwels KB, et al. Trajectory of long COVID symptoms after COVID-19 vaccination: community based cohort study. BMJ. 2022;377 doi: 10.1136/bmj-2021-069676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Women in Global Health Fit for women? Safe and decent PPE for women health and care workers. November, 2021. https://womeningh.org/resources/fitforwomen/
- 357.UN Women COVID-19: emerging gender data and why it matters. June 26, 2020. https://data.unwomen.org/resources/COVID-19-emerging-gender-data-and-why-it-matters
- 358.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Lan L, Xu D, Ye G, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323:1502–1503. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Gold JE, Okyay RA, Licht WE, Hurley DJ. Investigation of long COVID prevalence and its relationship to Epstein-Barr virus reactivation. Pathogens. 2021;10:763. doi: 10.3390/pathogens10060763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Iyengar KP, Jain VK, Vaishya R, Ish P. Long COVID-19: an emerging pandemic in itself. Adv Respir Med. 2021;89:234–236. doi: 10.5603/ARM.a2021.0040. [DOI] [PubMed] [Google Scholar]
- 362.Byrne EA. Understanding long COVID: nosology, social attitudes and stigma. Brain Behav Immun. 2022;99:17–24. doi: 10.1016/j.bbi.2021.09.012. [DOI] [PubMed] [Google Scholar]
- 363.Godeau D, Petit A, Richard I, Roquelaure Y, Descatha A. Return-to-work, disabilities and occupational health in the age of COVID-19. Scand J Work Environ Health. 2021;47:408–409. doi: 10.5271/sjweh.3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Centers for Medicare and Medicaid Services National health expenditures by type of service and source of funds, CY 1960–2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical
- 365.Organisation for Economic Co-operation and Development Health Expenditure. 2021. https://www.oecd.org/els/health-systems/health-expenditure.htm
- 366.Nachega JB, Atteh R, Ihekweazu C, et al. Contact tracing and the COVID-19 response in Africa: best practices, key challenges, and lessons learned from Nigeria, Rwanda, South Africa, and Uganda. Am J Trop Med Hyg. 2021;104:1179–1187. doi: 10.4269/ajtmh.21-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Perry HB, Chowdhury M, Were M, et al. Community health workers at the dawn of a new era: 11. CHWs leading the way to “Health for All”. Health Res Policy Syst. 2021;19(suppl 3):111. doi: 10.1186/s12961-021-00755-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Risko N, Werner K, Offorjebe OA, Vecino-Ortiz AI, Wallis LA, Razzak J. Cost-effectiveness and return on investment of protecting health workers in low- and middle-income countries during the COVID-19 pandemic. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Ballard M, Bancroft E, Nesbit J, et al. Prioritising the role of community health workers in the COVID-19 response. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Lotta G, Wenham C, Nunes J, Pimenta DN. Community health workers reveal COVID-19 disaster in Brazil. Lancet. 2020;396:365–366. doi: 10.1016/S0140-6736(20)31521-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Peretz PJ, Islam N, Matiz LA. Community health workers and COVID-19—addressing social determinants of health in times of crisis and beyond. N Engl J Med. 2020;383:e108. doi: 10.1056/NEJMp2022641. [DOI] [PubMed] [Google Scholar]
- 372.UNICEF Engaging communities to ensure safety and wellbeing of families during COVID-19 pandemic. June 18, 2021. https://www.unicef.org/bhutan/stories/engaging-communities-ensure-safety-and-wellbeing-families-during-covid-19-pandemic
- 373.Lotta G, Nunes J, Fernandez M, Garcia Correa M. The impact of the COVID-19 pandemic in the frontline health workforce: perceptions of vulnerability of Brazil's community health workers. Health Policy OPEN. 2022;3 doi: 10.1016/j.hpopen.2021.100065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Bhaumik S, Moola S, Tyagi J, Nambiar D, Kakoti M. Community health workers for pandemic response: a rapid evidence synthesis. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 376.Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. 2021;397:61–67. doi: 10.1016/S0140-6736(20)32228-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Haldane V, De Foo C, Abdalla SM, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27:964–980. doi: 10.1038/s41591-021-01381-y. [DOI] [PubMed] [Google Scholar]
- 378.Assefa Y, Gilks CF, van de Pas R, Reid S, Gete DG, Van Damme W. Reimagining global health systems for the 21st century: lessons from the COVID-19 pandemic. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2020-004882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.UN Global health and foreign policy: strengthening health system resilience through affordable health care for all—draft resolution/Brazil, Equatorial Guinea, Fiji, France, Indonesia, Mali, Mongolia, Norway, Senegal, Singapore, South Africa, Thailand and Viet Nam. Dec 3, 2020. https://digitallibrary.un.org/record/3894144?ln=en
- 380.The Lancet COVID-19 Commission Global Health Diplomacy Task Force Global diplomacy and cooperation in pandemic times: lessons and recommendations from COVID-19. December, 2021. https://covid19commission.org/s/GHD-Final-Note-Dec-2021.pdf
- 381.WHO At least 80 million children under one at risk of diseases such as diphtheria, measles and polio as COVID-19 disrupts routine vaccination efforts, warn GAVI, WHO and UNICEF. May 22, 2020. https://www.who.int/news/item/22-05-2020-at-least-80-million-children-under-one-at-risk-of-diseases-such-as-diphtheria-measles-and-polio-as-covid-19-disrupts-routine-vaccination-efforts-warn-gavi-who-and-unicef
- 382.Chmielewska B, Barratt I, Townsend R, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9:e759–e772. doi: 10.1016/S2214-109X(21)00079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.UNAIDS Global HIV & AIDS statistics—fact sheet. https://www.unaids.org/en/resources/fact-sheet
- 384.WHO Tuberculosis. Oct 14, 2021. https://www.who.int/news-room/fact-sheets/detail/tuberculosis
- 385.WHO More malaria cases and deaths in 2020 linked to COVID-19 disruptions. Dec 6, 2021. https://www.who.int/news/item/06-12-2021-more-malaria-cases-and-deaths-in-2020-linked-to-covid-19-disruptions
- 386.Graafland J, Lous B. Income inequality, life satisfaction inequality and trust: a cross country panel analysis. J Happiness Stud. 2019;20:1717–1737. [Google Scholar]
- 387.Paskov M, Dewilde C. Income inequality and solidarity in Europe. Res Soc Stratif Mobil. 2012;30:415–432. [Google Scholar]
- 388.Rothstein B, Uslaner EM. All for all: equality, corruption, and social trust. World Polit. 2005;58:41–72. [Google Scholar]
- 389.Flaherty GT, Hession P, Liew CH, et al. COVID-19 in adult patients with pre-existing chronic cardiac, respiratory and metabolic disease: a critical literature review with clinical recommendations. Trop Dis Travel Med Vaccines. 2020;6:16. doi: 10.1186/s40794-020-00118-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Shah H, Khan MSH, Dhurandhar NV, Hegde V. The triumvirate: why hypertension, obesity, and diabetes are risk factors for adverse effects in patients with COVID-19. Acta Diabetol. 2021;58:831–843. doi: 10.1007/s00592-020-01636-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Popkin BM, Du S, Green WD, et al. Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21 doi: 10.1111/obr.13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Frumkin H, Haines A. Global environmental change and noncommunicable disease risks. Annu Rev Public Health. 2019;40:261–282. doi: 10.1146/annurev-publhealth-040218-043706. [DOI] [PubMed] [Google Scholar]
- 393.Bourdrel T, Annesi-Maesano I, Alahmad B, Maesano CN, Bind M-A. The impact of outdoor air pollution on COVID-19: a review of evidence from in vitro, animal, and human studies. Eur Respir Rev. 2021;30 doi: 10.1183/16000617.0242-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Yao Y, Pan J, Liu Z, et al. Temporal association between particulate matter pollution and case fatality rate of COVID-19 in Wuhan. Environ Res. 2020;189 doi: 10.1016/j.envres.2020.109941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Pozzer A, Dominici F, Haines A, Witt C, Münzel T, Lelieveld J. Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc Res. 2020;116:2247–2253. doi: 10.1093/cvr/cvaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Bulfone TC, Malekinejad M, Rutherford GW, Razani N. Outdoor transmission of SARS-CoV-2 and other respiratory viruses: a systematic review. J Infect Dis. 2021;223:550–561. doi: 10.1093/infdis/jiaa742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Nishiura H, Oshitani H, Kobayashi T, et al. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19) medRxiv. 2020 doi: 10.1101/2020.02.28.20029272. published online April 16. (preprint). [DOI] [Google Scholar]
- 398.Qian H, Miao T, Liu L, Zheng X, Luo D, Li Y. Indoor transmission of SARS-CoV-2. Indoor Air. 2021;31:639–645. doi: 10.1111/ina.12766. [DOI] [PubMed] [Google Scholar]
- 399.The Lancet COVID-19 Commission Task Force on Safe Work. Safe School, and Safe Travel Six priority areas. https://covid19commission.org/safe-work-travel
- 400.Corsi R, Miller SL, VanRy MG, et al. Designing infectious disease resilience into school buildings through improvements to ventilation and air cleaning. 2021. Retrieved from https://covid19commission.org/safe-work-travel
- 401.Drinka PJ, Krause P, Schilling M, Miller BA, Shult P, Gravenstein S. Report of an outbreak: nursing home architecture and influenza-A attack rates. J Am Geriatr Soc. 1996;44:910–913. doi: 10.1111/j.1532-5415.1996.tb01859.x. [DOI] [PubMed] [Google Scholar]
- 402.Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55 doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Qian H, Zheng X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J Thorac Dis. 2018;10(suppl 19):S2295–S2304. doi: 10.21037/jtd.2018.01.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Wells W, Wells M, Wilder T. The environmental control of epidemic contagion: I. An epidemiologic study of radiant disinfection of air in day schools. Am J Hyg. 1942;35:97–121. [Google Scholar]
- 405.Li T, Liu Y, Di B, et al. Epidemiological investigation of an outbreak of pandemic influenza A (H1N1) 2009 in a boarding school: serological analysis of 1570 cases. J Clin Virol. 2011;50:235–239. doi: 10.1016/j.jcv.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 406.Sangeetha K. The University of Texas at Austin; 2019. A simulation framework to characterize the effect of ventilation control on airborne infectious disease transmission in schools. MSc thesis. [Google Scholar]
- 407.ASHRAE Standard 62.1-2019—Ventilation for acceptable indoor air quality. https://www.techstreet.com/ashrae/standards/ashrae-62-1-2019?product_id=2088533
- 408.Allen JG, Ibrahim AM. Indoor air changes and potential implications for SARS-CoV-2 transmission. JAMA. 2021;325:2112–2113. doi: 10.1001/jama.2021.5053. [DOI] [PubMed] [Google Scholar]
- 409.ASHRAE Standard 52.2-2017—method of testing general ventilation air-cleaning devices for removal efficiency by particle size. https://www.techstreet.com/standards/ashrae-52-2-2017?product_id=1942059
- 410.Morawska L, Tang JW, Bahnfleth W, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020;142 doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.The Lancet COVID-19 Commission Task Force on Safe Work. Safe School, and Safe Travel Building-related risk factors are a critical, but missing, component of SARS-CoV-2 outbreak investigations. March 1, 2021. https://covid19commission.org/safe-work-travel
- 412.Edwards NJ, Widrick R, Wilmes J, et al. Reducing COVID-19 airborne transmission risks on public transportation buses: an empirical study on aerosol dispersion and control. Aerosol Sci Technol. 2021;55:1378–1397. [Google Scholar]
- 413.Chen J, He H, Cheng W, et al. Potential transmission of SARS-CoV-2 on a flight from Singapore to Hangzhou, China: an epidemiological investigation. Travel Med Infect Dis. 2020;36 doi: 10.1016/j.tmaid.2020.101816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Pavli A, Smeti P, Hadjianastasiou S, et al. In-flight transmission of COVID-19 on flights to Greece: an epidemiological analysis. Travel Med Infect Dis. 2020;38 doi: 10.1016/j.tmaid.2020.101882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Speake H, Phillips A, Chong T, et al. Flight-associated transmission of severe acute respiratory syndrome coronavirus 2 corroborated by whole-genome sequencing. Emerg Infect Dis. 2020;26:2872–2880. doi: 10.3201/eid2612.203910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Walker CM, Ko G. Effect of ultraviolet germicidal irradiation on viral aerosols. Environ Sci Technol. 2007;41:5460–5465. doi: 10.1021/es070056u. [DOI] [PubMed] [Google Scholar]
- 417.Khanh NC, Thai PQ, Quach H-L, et al. Transmission of SARS-CoV 2 during long-haul flight. Emerg Infect Dis. 2020;26:2617–2624. doi: 10.3201/eid2611.203299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Choi EM, Chu DKW, Cheng PKC, et al. In-flight transmission of SARS-CoV-2. Emerg Infect Dis. 2020;26:2713–2716. doi: 10.3201/eid2611.203254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Airport Cooperative Research Program Infectious disease mitigation in airports and on aircraft. 2013. [DOI]
- 420.European Commission Investment Plan for Europe: European Investment Bank to provide BioNTech with up to €100 million in debt financing for COVID-19 vaccine development and manufacturing. Jan 24, 2022. https://ec.europa.eu/commission/presscorner/detail/ro/ip_20_1034
- 421.BioNTech BioNTech to receive up to €375M in funding from German Federal Ministry of Education and Research to support COVID-19 vaccine program BNT162. Sept 15, 2020. https://investors.biontech.de/news-releases/news-release-details/biontech-receive-eu375m-funding-german-federal-ministry
- 422.PRNewswire DARPA awards Moderna Therapeutics a grant for up to $25 million to develop messenger RNA therapeutics™. Oct 2, 2013. https://www.prnewswire.com/news-releases/darpa-awards-moderna-therapeutics-a-grant-for-up-to-25-million-to-develop-messenger-rna-therapeutics-226115821.html
- 423.Moderna mRNA Strategic collaborators: government organizations. 2021. https://test.modernatx.com/ecosystem/strategic-collaborators/mrna-strategic-collaborators-government-organizations
- 424.Bloomberg UK. More than 12.6 billion shots given: COVID-19 tracker. https://www.bloomberg.com/graphics/covid-vaccine-tracker-global-distribution/
- 425.Kiszewski AE, Cleary EG, Jackson MJ, Ledley FD. NIH funding for vaccine readiness before the COVID-19 pandemic. Vaccine. 2021;39:2458–2466. doi: 10.1016/j.vaccine.2021.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Siddalingaiah SV. Operation Warp Speed contracts for COVID-19 vaccines and ancillary vaccination materials. Congressional Research Service. March 1, 2021. https://crsreports.congress.gov/product/pdf/IN/IN11560
- 427.Companies Market Cap Market capitalization of Moderna (MRNA) https://companiesmarketcap.com/moderna/marketcap/
- 428.Companies Market Cap Market capitalization of BioNTech (BNTX) https://companiesmarketcap.com/biontech/marketcap/
- 429.Stevis-Gridneff M, Sanger-Katz M, Weiland N. The New York Times; June 9, 2021. A European official reveals a secret: the U.S. is paying more for coronavirus vaccines.https://www.nytimes.com/2020/12/18/upshot/coronavirus-vaccines-prices-europe-united-states.html [Google Scholar]
- 430.Espiner T. BBC News; Nov 12, 2021. AstraZeneca to take profits from COVID vaccine.https://www.bbc.com/news/business-59256223 [Google Scholar]
- 431.Hotez PJ, Bottazzi ME. Scientific American; Dec 30, 2021. A COVID vaccine for all.https://www.scientificamerican.com/article/a-covid-vaccine-for-all/ [DOI] [PubMed] [Google Scholar]
- 432.Thuluva S, Paradkar V, Turaga K, et al. Immunogenic superiority and safety of Biological E's CORBEVAX™ vaccine compared to COVISHIELD™ (ChAdOx1 nCoV-19) vaccine studied in a phase III, single blind, multicenter, randomized clinical trial. medRxiv. 2022 doi: 10.1101/2022.03.20.22271891. published online March 22, 2022. (preprint). [DOI] [Google Scholar]
- 433.United States Trade Representative Statement from Ambassador Katherine Tai on the COVID-19 trips waiver. May 5, 2021. https://ustr.gov/about-us/policy-offices/press-office/press-releases/2021/may/statement-ambassador-katherine-tai-covid-19-trips-waiver
- 434.EuroNews, AP . EuroNews; May 17, 2021. COVID-19 vaccine patents: EU nations divided over lifting intellectual property rights.https://www.euronews.com/2021/05/06/us-backs-waiver-on-intellectual-property-rights-for-covid-19-vaccines [Google Scholar]
- 435.Usher AD. A beautiful idea: how COVAX has fallen short. Lancet. 2021;397:2322–2325. doi: 10.1016/S0140-6736(21)01367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.International Monetary Fund COVID-19 global targets and progress tracker. https://www.imf.org/en/Topics/imf-and-covid19/COVID-19-Global-Targets-and-Progress-Tracker
- 437.WHO Strategy to achieve global COVID-19 vaccination by mid-2022. Oct 6, 2021. https://www.who.int/publications/m/item/strategy-to-achieve-global-covid-19-vaccination-by-mid-2022
- 438.Aizenman N. NPR; Dec 30, 2021. The goal: at least 40% vaxxed in all nations by year-end. This map shows how we stand.https://www.npr.org/sections/goatsandsoda/2021/12/30/1068920127/the-goal-at-least-40-vaxxed-in-all-nations-by-year-end-this-map-shows-how-we-sta [Google Scholar]
- 439.UNICEF COVID-19 vaccine market dashboard. Jan 27, 2022. https://www.unicef.org/supply/covid-19-vaccine-market-dashboard
- 440.InterAcademy Partnership Strengthening research on COVID-19 during the pandemic. May, 2021. https://www.interacademies.org/publication/strengthening-research-covid-19-during-pandemic
- 441.Global Commission on Evidence to Address Societal Challenges The Evidence Commission report: a wake-up call and path forward for decisionmakers, evidence intermediaries, and impact-oriented evidence producers. 2022. https://www.mcmasterforum.org/networks/evidence-commission/report/english
- 442.WHO International Clinical Trials Registry Platform (ICTRP) https://www.who.int/clinical-trials-registry-platform
- 443.COVID-NMA The COVID-NMA initiative. https://covid-nma.com/
- 444.COVID-END COVID-END inventory of evidence synthesis. https://www.mcmasterforum.org/networks/covid-end/resources-to-support-decision-makers/Inventory-of-best-evidence-syntheses
- 445.Behavioural, Environmental, Social and Systems Interventions Behavioural, Environmental, Social and Systems Interventions (for pandemic preparedness) https://www.bessi-collab.net/ [DOI] [PubMed]
- 446.Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.PRINCIPLE Helping to find treatments for COVID-19 from home. https://www.principletrial.org/
- 448.Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers: a randomized controlled trial. Ann Intern Med. 2021;174:335–343. doi: 10.7326/M20-6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Abaluck J, Kwong LH, Styczynski A, et al. Impact of community masking on COVID-19: a cluster-randomized trial in Bangladesh. Science. 2022;375 doi: 10.1126/science.abi9069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Hansen N-JH, Mano R. Mask mandates save lives. Aug 6, 2021. https://www.imf.org/en/Publications/WP/Issues/2021/08/05/Mask-Mandates-Save-Lives-460123 [DOI] [PMC free article] [PubMed]
- 451.International Monetary Fund World Economic Outlook October 2021: recovery during a pandemic—health concerns, supply disruptions, and price pressures. October, 2021. https://www.imf.org/en/Publications/WEO/Issues/2021/10/12/world-economic-outlook-october-2021
- 452.National Bureau of Economic Research US business cycle expansions and contractions. July 19, 2021. https://www.nber.org/research/data/us-business-cycle-expansions-and-contractions
- 453.International Monetary Fund World Economic Outlook, October 2019: global manufacturing downturn, rising trade barriers. October, 2019. https://www.imf.org/en/Publications/WEO/Issues/2019/10/01/world-economic-outlook-october-2019
- 454.International Monetary Fund World Economic Outlook, April 2022: war sets back the global recovery. April, 2022. https://www.imf.org/en/Publications/WEO/Issues/2022/04/19/world-economic-outlook-april-2022
- 455.International Monetary Fund G-20 surveillance note. February, 2022. https://www.imf.org/external/np/g20/021622.htm
- 456.Greenstone M, Nigam V. Does social distancing matter? March 27, 2020. https://bfi.uchicago.edu/insight/finding/does-social-distancing-matter/
- 457.Mooney H, Rosenblatt D, Ortiz de Mendívil C, et al. Inter-American Development Bank; August, 2021. Caribbean Quarterly Bulletin: the fragile path to recovery.https://publications.iadb.org/en/caribbean-quarterly-bulletin-volume-10-issue-2-august-2021 [Google Scholar]
- 458.International Monetary Fund Strengthening the credibility of public finances. October, 2021. https://www.imf.org/en/Publications/FM/Issues/2021/10/13/fiscal-monitor-october-2021
- 459.Oliu-Barton M, Pradelski BSR, Aghion P, et al. SARS-CoV-2 elimination, not mitigation, creates best outcomes for health, the economy, and civil liberties. Lancet. 2021;397:2234–2236. doi: 10.1016/S0140-6736(21)00978-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.International Monetary Fund Transcript of International Monetary Fund managing director Kristalina Georgieva's opening press conference, 2021 spring meetings. April 7, 2021. https://www.imf.org/en/News/Articles/2021/04/07/tr040721-transcript-of-imf-md-kristalina-georgievas-opening-press-conference-2021-spring-meetings
- 461.The World Bank Debt service suspension initiative. March 10, 2022. https://www.worldbank.org/en/topic/debt/brief/covid-19-debt-service-suspension-initiative
- 462.UNESCO UNESCO science report: the race against time for smarter development. 2021. https://www.unesco.org/reports/science/2021/en
- 463.Development Initiatives Aid spent on health: ODA data on donors, sectors, recipients. July 24, 2020. https://devinit.org/resources/aid-spent-health-oda-data-donors-sectors-recipients/
- 464.Micah AE, Cogswell IE, Cunningham B, et al. Tracking development assistance for health and for COVID-19: a review of development assistance, government, out-of-pocket, and other private spending on health for 204 countries and territories, 1990–2050. Lancet. 2021;398:1317–1343. doi: 10.1016/S0140-6736(21)01258-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Organisation for Economic Co-operation and Development Aid by DAC members increases in 2019 with more aid to the poorest countries. April 16, 2020. https://www.oecd.org/dac/financing-sustainable-development/development-finance-data/ODA-2019-detailed-summary.pdf
- 466.The Global Fund Results report. 2021. https://www.theglobalfund.org/en/results/
- 467.Friebel R, Silverman R, Glassman A, Chalkidou K. On results reporting and evidentiary standards: spotlight on the Global Fund. Lancet. 2019;393:2006–2008. doi: 10.1016/S0140-6736(18)33055-1. [DOI] [PubMed] [Google Scholar]
- 468.Zerhouni E. GAVI, the Vaccine Alliance. Cell. 2019;179:13–17. doi: 10.1016/j.cell.2019.08.026. [DOI] [PubMed] [Google Scholar]
- 469.Dalberg ACT-Accelerator strategic review. Oct 8, 2021. https://www.who.int/publications/m/item/act-accelerator-strategic-review
- 470.Okonjo-Iweala N, Shanmugaratnam T, Summers LH. Rethinking multilateralism for a pandemic era. December 2021. https://www.imf.org/en/Publications/fandd/issues/2021/12/Multilateralism-Pandemic-Era-Okonjo-Iweala-Shanmugaratnam-Summers
- 471.Behsudi A. Wish you were here: tourism-dependent economies are among those harmed the most by the pandemic. December, 2020. https://www.imf.org/en/Publications/fandd/issues/2020/12/impact-of-the-pandemic-on-tourism-behsudi
- 472.Bucciarelli V, Nasi M, Bianco F, et al. Depression pandemic and cardiovascular risk in the COVID-19 era and long COVID syndrome: gender makes a difference. Trends Cardiovasc Med. 2022;32:12–17. doi: 10.1016/j.tcm.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Orrù G, Bertelloni D, Diolaiuti F, et al. Long-COVID syndrome? A study on the persistence of neurological, psychological and physiological symptoms. Healthcare. 2021;9:575. doi: 10.3390/healthcare9050575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Tang V, Santiago A, Khan Z. Gender equality and COVID-19: policies and institutions for mitigating the crisis. July 28, 2021. https://www.imf.org/-/media/Files/Publications/covid19-special-notes/en-special-series-on-covid-19-gender-equality-and-covid-19.ashx
- 475.Hansen J, Sato M, Ruedy R. Global temperature in 2021. January 13, 2022. http://www.columbia.edu/~jeh1/mailings/2022/Temperature2021.13January2022.pdf
- 476.Gaspar V, Amaglobeli D, Garcia-Escribano M, Prady D, Soto M. Fiscal policy and development: human, social, and physical investment for the SDGs. Jan 23, 2019. https://www.imf.org/en/Publications/Staff-Discussion-Notes/Issues/2019/01/18/Fiscal-Policy-and-Development-Human-Social-and-Physical-Investments-for-the-SDGs-46444
- 477.Benedek D, Gemayel ER, Senhadji AS, Tieman AF. A post-pandemic assessment of the Sustainable Development Goals. April 27, 2021. https://www.imf.org/en/Publications/Staff-Discussion-Notes/Issues/2021/04/27/A-Post-Pandemic-Assessment-of-the-Sustainable-Development-Goals-460076
- 478.Bragge P, Becker U, Breu T, et al. How policymakers and other leaders can build a more sustainable post-COVID-19 ‘normal’. Discov Sustain. 2022;3:7. doi: 10.1007/s43621-022-00074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.Walton H, Evangelopoulos D, Kasdagli M, Selley L, Dajnak D, Katsouyanni K. Investigating links between air pollution, COVID-19 and lower respiratory infectious diseases. 2021. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/environmental-research-group/ReportfinalAPCOVID19_v10.pdf
- 480.Organisation for Economic Co-operation and Development The OECD Green Recovery Database—examining the environmental implications of COVID-19 recovery policies. April 19, 2021. https://www.oecd.org/coronavirus/policy-responses/the-oecd-green-recovery-database-47ae0f0d/
- 481.International Energy Agency Sustainable recovery tracker: monitoring progress towards sustainable recoveries from the COVID-19 crisis. April, 2022. https://www.iea.org/reports/sustainable-recovery-tracker
- 482.Oxford University Economic Recovery Project Global Recovery Observatory. https://recovery.smithschool.ox.ac.uk/tracking/#:~:text=The%20Global%20Recovery%20Observatory%20brings,more%20impactful%20and%20sustainable%20investment
- 483.Wuppertal Institute. E3G The Green Recovery Tracker. https://www.greenrecoverytracker.org/
- 484.International Institute for Sustainable Development Energy Policy Tracker. https://www.energypolicytracker.org/
- 485.Finance for Biodiversity Initiative Greenness of Stimulus Index. https://www.vivideconomics.com/casestudy/greenness-for-stimulus-index/
- 486.Nahm JM, Miller SM, Urpelainen J. G20's US$14-trillion economic stimulus reneges on emissions pledges. Nature. 2022;603:28–31. doi: 10.1038/d41586-022-00540-6. [DOI] [PubMed] [Google Scholar]
- 487.Lafortune G, Cortés Puch M, Mosnier A, et al. Europe Sustainable Development Report 2021: transforming the European Union to achieve the Sustainable Development Goals. Dec 14, 2021. https://www.sdgindex.org/esdr2021
- 488.Sachs J, Koundouri P, Becchett L, et al. Financing the joint implementation of the SDGs and the European Green Deal. May, 2022. https://egd-report.unsdsn.org/
- 489.WHO WHO's work in health emergencies—strengthening preparedness for health emergencies: implementation of the International Health Regulations (2005) May 5, 2021. https://www.icao.int/EURNAT/EUR%20and%20NAT%20Documents/COVID%2019%20Updates-%20CAPSCA%20EUR/05%20May%202021%20COVID19%20Updates/COVID19%20-%202021-05-07%20Updates/A74_9Add1-en.pdf
- 490.Global Preparedness Monitoring Board A world in disorder. Sept 14, 2020. https://www.gpmb.org/annual-reports/overview/item/2020-a-world-in-disorder
- 491.Sagan A, Webb E, Azzopardi-Muscat N, de la Mata I, McKee M, Figueras J. Health systems resilience during COVID-19: lessons for building back better. Nov 11, 2021. https://eurohealthobservatory.who.int/publications/i/health-systems-resilience-during-covid-19-lessons-for-building-back-better [PubMed]
- 492.McKee M. World Health Organization; 2021. Drawing light from the pandemic: a new strategy for health and sustainable development: a review of the evidence.https://eurohealthobservatory.who.int/publications/m/drawing-light-from-the-pandemic-a-new-strategy-for-health-and-sustainable-development [Google Scholar]
- 493.International Society for Infectious Diseases Surveillance. https://isid.org/surveillance/
- 494.G20 High Level Independent Panel A global deal for our pandemic age. June, 2021. https://pandemic-financing.org/report/foreword/
- 495.WHO One Health. https://www.who.int/health-topics/one-health#tab=tab_1
- 496.WHO Joint statement on the prioritization of monitoring SARS-CoV-2 infection in wildlife and preventing the formation of animal reservoirs. March 7, 2022. https://www.who.int/news/item/07-03-2022-joint-statement-on-the-prioritization-of-monitoring-sars-cov-2-infection-in-wildlife-and-preventing-the-formation-of-animal-reservoirs
- 497.International Monetary Fund Advanced economies datasets. April, 2022. https://www.imf.org/external/datamapper/profile/ADVEC
- 498.UN Secretary-General's remarks to the General Assembly on his priorities for 2022. Jan 21, 2022. https://www.un.org/sg/en/node/261520#:~:text=Excellencies%2C-,I%20want%20to%20begin%20the%20year%20by%20raising%20five%20alarms,in%20the%20COVID%2D19%20battle
- 499.UN Our common agenda: report of the Secretary-General. September, 2021. https://www.un.org/en/content/common-agenda-report/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.