Abstract
Introduction
Although a trustworthy connection between doctor and patient is crucial in clinical practice, it could be hindered by different cultural and linguistic backgrounds. Moreover, an effective doctor–patient interaction could be even more challenging in andrological fields, in which psychological and social components are predominant.
Aim
To analyse the doctor–patient relationship in the andrological field, applying both qualitative and quantitative analyses.
Methods
monocentric, cross‐sectional, observational study was performed between May and December 2018. During the study, all patients aged >18 years attending the Modena Andrology Unit for couple infertility or erectile dysfunction were enrolled and the doctor–patients interaction recorded. Patients were divided into two groups depending on their medical seeking and were further divided between native and non‐native speakers of Italian. All patients underwent a routine andrological examination. Every first medical consultation was audio‐recorded and transcribed using “ELAN” software for socio‐linguistic analysis. Transcriptions underwent qualitative analysis through conversation analysis. Then, quantitative analyses were performed, and interaction parameters underwent correlation analyses.
Results
Twenty‐five patients were enrolled. The analysis of the andrological interview allowed to recognise five consecutive phases, following a semi‐standardized pattern. Patients without linguistic barriers and with infertility problems showed more autonomous contribution during the consultation. No difference arose in the sexual dysfunctions group. Doctor's explanations were frequent, but when linguistic barrier was present or Italian patients seemed less talkative, explanations were shorter, and doctors tried to use other conversational mechanisms to promote understanding. Patient's variables were significantly lower compared to the doctor, considering the number of turns (p = 0.025) and their minimum (p = 0.032), maximum (p < 0.001), and average durations (p < 0.001). Only patient's latency was significantly higher than the doctor's (p = 0.001).
Conclusion
This is the first attempt to analyse the doctor–patient relationship in andrology using authentic audio‐recorded consultations. The results confirmed that a patient‐centred communication must be applied also in andrological consultations. However, the topics discussed may require more “medical formulation” to be acceptable to the participants in this context.
Keywords: andrology visit, communication, doctor–patient interactions, turns
1. INTRODUCTION
The creation of a trustworthy relationship between doctor and patient is crucial in clinical practice, orienting decision‐making and affecting therapeutic success. 1 , 2 , 3 This relationship has received philosophical, literary and social attention since the times of Hippocrates, who conceived the doctor's medical authoritativeness as a key in maintaining a trustworthy relationship and taught the so‐called “doctor‐centred” approach. 4 Only in the second half of the 19th century, the point of view on the doctor–patient relationship began to change through a more patient‐inclusive approach, 5 , 6 which radically changed the relationship with the patient in the direction of increasing communication effectiveness. Not surprisingly, the doctor–patient interaction aroused interest in socio‐linguistic research. Studies on interaction, which were made possible by the growing possibility of collecting recorded and transcribed medical consultations, highlighted that the primacy of the clinician's knowledge as an expert could barely be exercised without a relevant contribution of the patients providing information on their problems and worries. 7 Thus, an approach “focussed on the patient” developed, in which the doctors encourage the patients to manifest their feelings, sensations and worries, and to actively participate in the co‐construction of the interaction. 3 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 Hitherto, patient‐centred approaches in the doctor–patient relationship are considered the most effective forms of communication in all medical fields. 8 , 10 , 11 , 13 , 17 , 18 , 19 , 20 , 21 , 22 In particular, patient‐focussed communication displays four relevant features: (i) patient's active participation and conveyance of personal feelings, experiences and opinions; (ii) active listening and support from the doctor eliciting the patients’ personal contribution; (iii) mutual understanding and affinity based on the doctors’ possibility to interpret the patients’ contributions; (iv) information exchange and decisions sharing between doctor and patient. 23 , 24
Promoting an effective doctor–patient relationship is a daunting task, 25 especially in the case of different cultural and linguistic backgrounds. Indeed, language obstacles and their unfamiliarity with the medical context may prevent migrant patients to be talkative and proactive, adding another critical issue to the doctor–patient relationship. 26 , 27 , 28 , 29 , 30 , 31 In particular, social difficulties could emerge in specific medical scenarios, such as the andrological context we are focussing on here. Andrology is a medicine branch deputed to diagnose, treat and manage male reproductive organs’ diseases, which could compromise physical development, sexual activity and fertility. 32 , 33 The andrologist deals transversally with the male patient as a whole, from the problems of the reproductive to those of the sexual sphere. Andrological disturbances are very frequent in the male population, with different incidences depending on age. 33 Among andrological problems, erectile dysfunction (ED) is the most frequent reason for andrological consultation, followed by male fertility pathologies. 34
By evaluating the sexual habit of both the man and the couple, the andrologist works in a delicate context in which building a trustworthy relationship is fundamental to forge a diagnostic–therapeutic alliance. 35 , 36 Indeed, the doctor must juggle among intimate and private information, in which the psychological aspect cannot be disregarded. 37 In addition, a variable psychological component should be considered behind several sexual disorders and an effective doctor–patient interaction could unravel this psychological component. While there is a wide literature on the doctor–patient relationship in several medical fields, 2 , 3 , 4 , 7 , 38 , 39 , 40 , 41 , 42 no studies are currently available in andrology, where the psychological and social components are predominant. Moreover, there are no guidelines concerning the way in which andrological assessment should be performed, and specifically on how to gather information of interest. In this setting, several questionnaires and structured interviews have been developed, 43 , 44 , 45 , 46 , 47 in order to objectivise subjective data, to reduce the patient's discomfort and to reach a diagnosis. However, there is a lack of consistency in these structured interviews and the doctor–patient relationship is not qualitatively investigated.
With this in mind, we designed the current study aimed to analyse the doctor–patient interaction in the andrological field using both qualitative and quantitative methods.
2. MATERIALS AND METHODS
2.1. Study design and participants
A monocentric, cross‐sectional, observational study was carried out at the Andrology Unit, Department of Biomedical Metabolic and Neural Sciences of the University of Modena and Reggio Emilia (Italy) between May and December 2018. All patients aged over 18 attending either for couple infertility or ED were considered eligible, irrespective of their ethnic origin and the potential presence of a language barrier.
Among the andrological issues investigated, couple infertility was defined as the absence of conception after at least 12 months of unprotected sexual intercourses, 48 while ED was defined as the persistent or recurrent inability to reach and/or maintain a penile erection firm enough to have satisfactory sexual intercourses. 49 Enrolled patients were divided into two groups according to the reason for their access to medical consultation, that is, couple infertility or ED. Then, both groups were further subdivided based on their familiarity with the Italian language, thus basically forming one group of native Italian speakers and the other group of non‐native speakers.
2.2. Data collection
The study consisted in the audio recording of the first consultation performed at the Andrology Unit. During the consultation, enrolled patients underwent a routine andrological examination, according to clinical practice. In particular, personal and family histories were investigated, with a specific focus on sexual life and risk factors for pituitary–gonadal axis impairment. During the consultation, physical genital examination was performed. Lastly, the doctors reported the diagnostic orientation based on the data collected during the consultation and their diagnostic–therapeutic proposals.
Every audio‐recorded consultation was cleared of the identification data of the patients and sent to the colleagues operating at the Department of Studies on Language and Culture (University of Modena and Reggio Emilia, Modena, Italy), for socio‐linguistic analysis. All recordings were manually transcribed using “ELAN” software (2020, Nijmegen: Max Planck Institute for Psycholinguistics, The Language Archive. Retrieved from https://archive.mpi.nl/tla/elan), which allows to time‐align accurate transcriptions of speakers’ utterances to the audio and enables to extract some quantitative data relating to the speakers’ turns, their duration, and their latency.
2.3. Data analysis
Transcriptions were investigated applying different methods. First, qualitative analysis was performed considering the two different types of consultations. The following aspects were investigated using conversation analysis (henceforth CA) 50 : (i) inversion and mixing of the anamnesis and of the presentation of the medical problem, (ii) questions to the patient and doctor's feedback to the patient's answers, (iii) doctor's reactions to the patient's expanded responses and initiatives, (iv) doctor's explanations, (v) repair strategies to solve problems of understanding, (vi) comments by the andrologist on the patient's contributions to the conversation, (vii) use of a shared language (Italian or English), and (viii) failure by the doctor to “take charge” of the patient. The main objectives of qualitative analyses were: (i) the description of the interaction structure of this under‐investigated consultation type and (ii) the evaluation of the synchronisation between the patient and the doctor's actions. In this setting, according to CA, several variables were extracted, such as turn‐at‐talk, which represents every turn of speech in the conversation between doctor and patient, and turn length, expressed as minimum and maximum time. In particular, the following parameters were considered: sequence, topic processing and alignment. 51 , 52 , 53 , 54 Sequences indicate that every single turn‐at‐talk is produced in reaction to the former and creates the conditions to choose between the several possibilities of the next turn. 54 Topic processing represents the conditions in which turns’ contents are linked to each other according to a recognisable theme‐based rationale, so that an interaction narrative is built. 52 , 53 Alignment means that every turn‐at‐talk is included and meaningful in relation to a specific kind of “institutional” interaction. 55 Coordination of these parameters is essential in the interaction to achieve synchronisation of the actions of all participants. An inadequate synchronisation blocks, or otherwise hinders, coordination, and the consequent success of the interaction. The presence of synchronisation in the doctor–patient interaction leads the patient to understand his problem from the medical point of view, allowing the doctor to provide the relevant informative items.
Second, quantitative analyses were performed. In particular, the following interaction‐related parameters were extracted from ELAN transcriptions of audio recordings: number of turns uttered by each speaker, their duration per speaker and their latency per speaker, that is, the time delay between two turns‐at‐talk. Two variables were considered for each parameter. The number of turns was expressed in continuous variable, while their duration and latency were expressed in seconds. All variables extracted were compared among groups and subgroups, using the “Statistical Package for the Social Sciences” software for Windows (version 26.0; SPSS Inc., Chicago, IL, USA). Correlation analyses were performed considering interaction parameters. Since seven parameters were considered, Bonferroni's adjustments were performed and p < 0.007 were considered statistically significant.
2.4. Ethical statement
The present study was approved by the Ethical Committee of Modena (Prot. Azienda Ospedaliero‐Universitaria (AOU) 0008554/18 ‐ 05/04/2018) and each patient provided written informed consent for the enrolment. This study complied with the ethical standards of the Helsinki Declaration (1975, revised in 2013).
3. RESULTS
Twenty‐five consecutive patients (mean age 44.4 ± 12.0 years) with sexual dysfunction or couple infertility were enrolled. Among these, 11 showed difficulties in communicating in Italian, whereas 14 did not.
Patients were divided into two groups according to the reason why the andrological consult was requested: (i) group A: ED (12 patients, 48%); (ii) group B: couple infertility (13 patients, 52%) (Figure 1). The mean age was significantly higher in group A compared to group B (38.2 ± 3.7 years vs. 51.9 ± 14.2 years, p = 0.001). Patients were further divided into two subgroups, according to the existence of language barriers: (i) group 1: no linguistic difficulties (14 patients, 56%); (ii) group 2: linguistic difficulties (11 patients, 44%) (Figure 1). Thus, the overall study group was divided into four subgroups: (i) group 1A: 7 patients (28%); (ii) group 1B: 7 patients (28%); (iii) group 2A: 5 patients (20%); (iv) group 2B: 6 patients (24%) (Figure 1).
FIGURE 1.
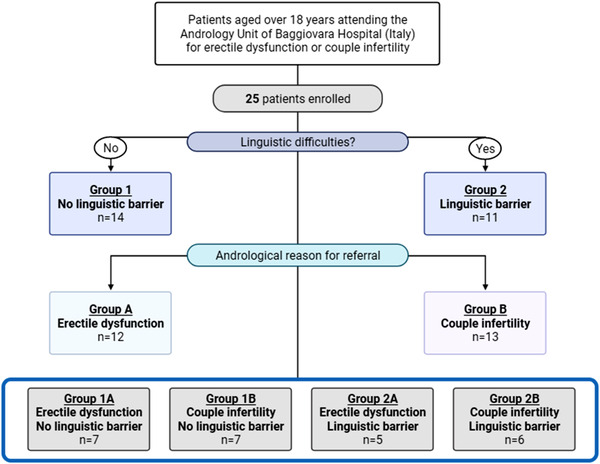
Flow‐chart of the study. Enrolled patients were divided into four subgroups according to the andrological reason for consultation (i.e., erectile dysfunction or couple infertility) and to the presence or not of a linguistic barrier
3.1. Quantitative analysis
Patient's variables were significantly lower compared to the doctor, considering the number of turns (p = 0.025) and their minimum (p = 0.032), maximum (p < 0.001), and average durations (p < 0.001). Only patient's latency was significantly higher than the doctor's (p = 0.001) (Table 1). Considering patient's communication parameters, a significant direct correlation was found between average turn duration and maximum turn duration (rho = 0.758, p < 0.001), while no other correlations were detected. Considering doctor's communication parameters, an inverse correlation was depicted between the turn number and the average turn duration (rho = –0.540, p = 0.002) and between minimum and maximum turn duration (rho = –0.486, p = 0.006). Finally, a direct correlation was found between maximum and average turn duration (rho = 0.864, p < 0.001). Comparing the communication parameters between the patient and the physician, no significant correlations were highlighted.
TABLE 1.
Quantitative analyses. Turn number, duration and latency of patients and doctor, considering the entire study group. Data are expressed as mean ± standard deviation
| Patient | Physician | |
|---|---|---|
| Number of turns | 117.7 ± 52.5 | 145.6 ± 44.1 |
| Duration of turns (min) (s) | 0.2 ± 0.1 | 0.3 ± 0.1 |
| Duration of turns (max) (s) | 16.2 ± 12.0 | 66.8 ± 68.7 |
| Average duration of turns (s) | 2.14 ± 1.1 | 5.2 ± 2.0 |
| Latency (s) | 24.4 ± 23.3 | 2.4 ± 2.8 |
Considering the subdivision according to the reason for the consultation, the average turn duration and the latency remained significantly different between patients and doctors (p < 0.001 and p = 0.050, respectively), whereas the number of turns resulted similar (p = 0.541) (Table 2). On the contrary, in group B all parameters assessed remained significantly different between patients and doctors (p = 0.011, p < 0.001 and p = 0.006, respectively) (Table 2). These results confirm that the communication characteristics detected in the entire study group are independent of the clinical reason for referral.
TABLE 2.
Quantitative analyses. Turns number, average duration and latency of patients and physician, comparing patients complaining of erectile dysfunction (group A) and couple infertility (group B). Data are expressed as mean ± standard deviation
| Group A | Group B | |||||
|---|---|---|---|---|---|---|
| Patient | Physician | p value | Patient | Physician | p value | |
| Number of turns (n) | 137.9 ± 51.1 | 154.8 ± 49.7 | 0.541 | 101.12 ± 49.0 | 138.1 ± 38.8 | 0.011 |
| Average duration of turns (s) | 2.4 ± 1.4 | 5.6 ± 2. | <0.001 | 1.8 ± 0.7 | 4.9 ± 1.6 | <0.001 |
| Latency (s) | 21.5 ± 21.0 | 2.0 ± 2.9 | 0.033 | 26.8 ± 25.4 | 2.6 ± 2.8 | 0.031 |
Considering the subdivision according to the presence of a linguistic barrier, the patient's average turn duration was significantly lower than the doctor's one (Table 3). Similarly, the patient's latency was significantly higher, while the turn number did not differ (Table 3). The patient's communication parameters did not differ between the two groups, while only the physician's average turn duration was significantly different (Table 3). At post hoc test, the doctor's average duration was significantly higher in group 1 compared to group 2 (p < 0.001). Comparing the patient to the physician, only in group 2 a direct significant correlation was found between the doctor's average turn duration and the patient's latency (rho = 0.755, p = 0.007).
TABLE 3.
Quantitative analyses. Turns number, average duration and latency of patients and physician, dividing patients according to the presence of language barriers (groups 2). Data are expressed as mean ± standard deviation
| Group 1 | Group 2 | Overall p‐value | ||||||
|---|---|---|---|---|---|---|---|---|
| Patient | Physician | p value | Patient | Physician | p value | Patient | Physician | |
| Age (years) | 47.21± 14.3 | ‐ | ‐ | 42.4 ± 8.9 | ‐ | ‐ | 0.506 | ‐ |
| Number of turns (n) | 105.6 ± 34.5 | 128.6 ± 33.3 | 0.085 | 127.1 ± 60.3 | 167.5 ± 45.5 | 0.091 | 0.523 | 0.086 |
| Average duration of turns (s) | 2.6 ± 1.5 | 6.8 ± 2.0 | <0.001 | 1.6 ± 0.3 | 4.0 ± 0.6 | <0.001 | 0.107 | <0.001 |
| Latency (s) | 19.4 ± 18.9 | 2.7 ± 3.0 | 0.003 | 28.4 ± 28.2 | 1.4 ± 2.1 | 0.005 | 0.572 | 0.363 |
The mean patient's turn duration remained significantly lower compared to the doctor in all groups (Table 4). The patient's latency was significantly higher only in groups 1A, 1B and 2B, while the number of turns comparing patient and doctor was similar in all groups (Table 4). The considered variables did not differ between the subgroups for both patient and doctor (Table 4). Moreover, no differences were seen among groups considering the patient (Table 4). Similarly, the number of turns and the latency did not differ among groups (Table 4). However, the average duration was significantly different, with higher average at group 1A compared to 2A and 2B (p = 0.018 and p = 0.013 respectively) at post hoc analyses (Table 4).
TABLE 4.
Quantitative analyses. Turns number, average duration and latency of patients and physician, dividing patients according to the clinical reason for medical consultation (groups A or B), the presence of language barriers (groups 2). Data are expressed as mean ± standard deviation
|
Group 1A |
Group 1B |
|||||||
|---|---|---|---|---|---|---|---|---|
| Patient | Physician | p value | Patient | Physician | p value |
p value patient |
p value doctor |
|
| Age (years) | 56.2 ± 15.5 | ‐ | ‐ | 38.3 ± 3.8 | ‐ | ‐ | 0.026 | ‐ |
| Number of turns (n) | 122.4 ± 38.0 | 130.0 ± 28.6 | 0.805 | 88.9 ± 22.1 | 127.1 ± 39.8 | 0.073 | 0.073 | 0.902 |
| Average duration of turns (s) | 3.01 ± 1.8 | 7.1 ± 2.6 | 0.007 | 2.1 ± 1.0 | 6.4 ± 1.2 | 0.001 | 0.383 | 0.902 |
| Latency (s) | 15.5 ± 13.5 | 3.0 ± 3.9 | 0.007 | 23.3 ± 23.5 | 2.4 ± 2.0 | 0.011 | 0.620 | 0.999 |
|
Group 2A |
Group 2B |
P value patient |
p value doctor |
|||||
|---|---|---|---|---|---|---|---|---|
| Age (years) | 47.3 ± 10.9 | ‐ | ‐ | 38.3 ± 4.4 | ‐ | ‐ | 0.247 | ‐ |
| Number of turns (n) | 161.2 ± 40.7 | 192.4 ± 53.3 | 0.310 | 98.7 ± 61.7 | 146.8 ± 27.2 | 0.180 | 0.126 | 0.177 |
| Average duration of turns (s) | 1.6 ± 0.4 | 3.9 ± 0.1 | 0.008 | 1.7 ± 0.3 | 4.0 ± 0.8 | 0.002 | 0.792 | 0.792 |
| Latency (s) | 24.7 ± 29.2 | 0.7 ± 0.9 | 0.151 | 31.5 ± 29.7 | 2.0 ± 2.7 | 0.015 | 0.537 | 0.792 |
| p value ‐ number of turns | 0.247 | 0.162 | ‐ | 0.247 | 0.162 | ‐ | ||
| p value ‐ average turns duration | 0.175 | <0.001 | ‐ | 0.175 | <0.001 | ‐ | ||
| p value ‐ latency | 0.83 | 0.680 | ‐ | 0.83 | 0.680 | ‐ | ||
3.2. Qualitative analysis
The andrological consultation started with an “opening phase”, in which the doctor introduced the reason for the consultation, trying to reduce the psychological burden typical of the context. The second step consisted in the “data collection phase”, during which the doctor proceeded with history taking. In other medical fields, the first phase of the consultation was either history taking, or the patient's explanation of the problem. Here, this anomalous trend was particularly evident in group A, when sexual dysfunctions were reported. In this setting, the doctor introduced the problem to the patient, who showed his acceptance of the problem's description as given by the doctor. Only in one case out of 12, this introduction was not accepted by the patient, who showed his willingness and interest in presenting his problem first. In group B, interaction beginnings were less uniform and some exceptions were observed, that is, when the “opening phase” was not performed and the “data collection phase” was anticipated, in 4 out of 17 patients. Moreover, in case of linguistic barriers (group 2), turns‐at‐talk were longer and more complex, because the foreign patients appeared “less competent on the subject” than the Italian patients, or less able to talk about it, and their narratives took more turns.
The “data collection phase” was performed following a specific sequence of actions: (i) question from the doctor, (ii) patient response, (iii) feedback from the doctor who formulated the patient's answer by summarising, explaining, developing it or by commenting on it, 24 , 56 (iv) patient confirmation feedback, and (v) feedback from the doctor (i.e., “Okay”). This sequence was repeated to complete the medical history collection, following a semi‐standardized pattern, in order to analyse all possible signs and symptoms indicative of an endocrine dysfunction underlying the disorder complained by the patient. After each sequence, having ensured that the information was shared, the doctor moved on to another topic. This sequence of actions however took different forms. Reductions made the transition to the next topic less effective. Instead, expansions by patients who autonomously asked questions to the doctor or added information optimised information exchange. This occurred largely with patients without linguistic barriers (group 1) and with problems of infertility. Indeed, in this group, the patient's autonomous contributions occurred 18 times in group 1A and 29 times in group 1B. In group 2, patients intervened with independent contributions 18 times in group 2A and only 14 times in group 2B. The difference with respect to group 1, which was found only in the case of couple infertility (29 in 1B vs. 14 in 2B), could be explained by both the greater competence of Italian patients, and by a sort of “inhibition” or difficulty that the foreign patient could experience in talking about reproduction in a language that is not his own. To these spontaneous patient's contributions, the doctor answered mainly by supporting their production and showing interest through answers or questions for in‐depth analysis, although there were cases in which s/he treated the expansion as inadequate or premature in this consultation phase and therefore postponed its treatment to a later phase. It is interesting to note that no difference shows up in the group of patients with sexual dysfunctions, suggesting that when the problem is (or is perceived as) the single patient's, rather than the couple's, inhibition may be higher.
The third step was the “problem‐description phase”. During this phase, the patient exposed the problem to the doctor and the sequential structure mirrored that of the previous phase. The fourth step was the “physical examination phase”, followed by the “closing phase”, during which the doctor explained the diagnostic orientation and the next steps in the diagnostic/therapeutic path. Doctor's explanations were generally standardized, being preliminary to further investigations, and required minimal feedback from the patient. Sometimes patients showed their understanding through the repetition of words uttered by the doctor, but they rarely intervened with requests for clarification or comments. Doctor's explanations were generally introduced by a “then” connector, which signalled the passage from a phase in which the patient was not directly involved to a phase in which the doctor gets back to the patient offering him an explanation of the results of the examination and the further steps to be taken. In this final phase, repair sequences to solve problems of understanding occurred mainly in group 2, where linguistic barriers were present. Although rare, such sequences included either the reformulation of the doctor's question, where the doctor repeated the same content in simpler terms, which was interactively effective, or the replacement of the patient's response, where it is the doctor who provides the answers in the place of the patient. Though such communicative technique may be used as a proposal of an answer, rather than a patient's proper answer, it appeared less effective. Repairs occurred only 21 times, concentrated in three particularly complicated consultations.
Synchronisation was evaluated by analysing the number of inversions and mixing between the “data collection phase” and the “problem‐description phase”. These occurred in 6 out of 12 consultations (50.0%) in group A and in 2 out of 13 (15.4%) in group B. Moreover, the synchronisation was evaluated counting the number of patient's confirmation feedbacks, followed by simple minimal responses by the doctor (i.e., “Okay”) enabling the patient to verify that his confirmation had been recorded. Generally, the doctor's minimal response was followed by a new question, acting as a transition between the different topics. This interaction sequence was mainly detected in group A. Synchronisation was also evaluated by analysing the doctor's reaction to the patient's expanded responses and initiatives. Two different actions were found in this setting: (i) either the doctor collaborated in the production of expanded responses and initiatives, expressing interest in the patient's contribution through articulated feedback and thereby supporting the patient's narrative and showing closeness; (ii) or the doctor postponed the topic to a later stage, treating the patient's initiative or expansion as inadequate or premature for the ongoing consultation phase. This happened generally in group 2B, that is, when infertility problems were evaluated and linguistic barriers were present.
Finally, doctor's explanations were analysed as signs of doctor–patient interaction effectiveness. They were very frequent in all consultations of all groups, but the reduction in the time devoted to them can be seen as an indicator of communication problems. When linguistic barriers were present or Italian patients seemed less talkative, explanations were shorter and doctors put in place conversational mechanisms aiming at promoting understanding, such as the reformulation of their question and the replacement of the patient's answers we commented above.
4. DISCUSSION
This study provides for the first time a qualitative and quantitative description of the doctor–patient interaction in the andrological field. Here, we describe an unstructured andrological interview composed of five consecutive phases. In the “opening phase”, the doctor introduces the consultation, helping the patient to enter an intimate setting and limiting the potential psychological burden of andrological concerns. The following phase, that is, the “data collection phase”, allows the doctor to collect all relevant information required to reach a diagnosis. During the “problem‐description phase”, the patient is finally “free” to report/describe his andrological problem. The sequential structure followed in both the second and third consultation phase helps the patient to retrace the same pattern, allowing a better and orderly description of his problem. The fourth phase, that is, the “physical examination phase”, completes the information detected during the preceding phases. Finally, during the “closing phase”, the doctor refers the diagnostic orientation and proposes the following diagnostic/therapeutic steps needed. This doctor–patient interaction does not follow the conventional sequence generally observed in other medical fields. 54 , 57 In our practice, history taking actually precedes the presentation of the sexual problem by the patient, which allows us to put him at ease, even when the topics discussed can make him uncomfortable or create embarrassing situations. Indeed, it is well known that andrological issues could create discomfort to the patient, when sexual problems are debated 58 , 59 , 60 or distress, when infertility/sterility issues have been touched. 61 , 62 , 63 Moreover, the fact that the andrological consultation proceeds with a semi‐standardized interview allows us to obtain all relevant information to frame the patient's disorder or problem, without “getting lost” in the emotional aspects that could confuse or delay the diagnostic framework. Our approach could be considered semi‐standardized, since it follows a specific structure but allows the patient to intervene by expanding and completing the different phases of the interview. However, the first substantial difference between patients with and without linguistic barrier emerges precisely from the evaluation of the number and quality of the expansions proposed by the patient. Indeed, patients without linguistic barrier seem to be more prone and above all more prepared to actively intervene in the consultation, both with expansions to their answers to the doctor and with questions they autonomously produce. However, once the anamnestic collection and the physical examination are over, and the doctor explains the diagnosis orientation and what will be the next diagnostic or therapeutic steps, patients rarely provide comments or ask for clarifications but only produce minimal responses, thereby acknowledging receipt and showing that the explanations provided are exhaustive. During this “closing phase”, the doctor effectively puts in place communication repair mechanisms which, as expected, are mainly necessary in case of linguistic barrier.
Overall, the qualitative analysis of the doctor–patient interaction in the andrological field, although only exploratory, confirms that the synchronisation among participants is structured as for other medical fields. 64 , 65 , 66 Indeed, the evaluation of the type and frequency of sequences that promote patient participation confirmed the effectiveness of our semi‐standardized approach, detecting only few communication challenges when no language barriers are present. In this context, a low number of inversions or synchronisation issues were recorded, associated with good collaboration between doctor and patient. This collaboration emerges from the qualitative analysis of doctors’ responses to patients’ contributions. When linguistic barriers are present, such responses are more frequent, especially if the topic is infertility. In this context, emotional aspects, influenced by the different cultural background of the patient, can significantly limit the doctor–patient interaction. As shown in Niemants, 67 doctors can however actively promote patients’ participation and expression by showing their understanding of (i) the answers foreign patients produce—sometimes hardly—in response to doctors’ questions, and (ii) the questions foreign patients autonomously ask, especially after the examination phase, when they traditionally play a major role in doctor–patient interactions. 68 Moreover, the synchronisation effectiveness is also suggested by the presence of numerous interventions by the doctor to explain and detail the results obtained during the consultation. 54 When these explanations seem to be insufficient, the doctor puts in place further repair mechanisms that allow a complete understanding. 69 These expanded responses and patient initiatives are important phenomena in medical fields. 53 , 70
In our practice, we routinely apply semi‐standardized consultations, characterized by a direct start of the medical history collection and a specific step‐by‐step interview. This structure allows the doctor to control the interaction, improving the communication effectiveness. In particular, this approach allows the patient to verify that his confirmation has been registered and helps the doctor to move on to another topic after making sure that information has been shared. Although this kind of consultations seems to follow a rigid pattern, it is more flexible than other structured interviews suggested so far. 43 , 44 , 45 Indeed, our approach allows for some interactional space that patients take to intervene and express their opinion, as shown in the qualitative data. This semi‐standardized approach shows the advantage of a freer interview since, unlike questionnaires, it leaves room for the patient to talk about a variety of more or less related topics and therefore enables the doctor to collect additional information that perhaps would otherwise be unreported. Moreover, this approach could be customized according to the medical reason and/or the presence of a linguistic barrier, an issue which deserves further exploration. Time devoted to explanations is reduced both in case of patients with linguistic barrier and in some cases of Italian patients who are not very participatory. The latter is the case of men with infertility complaints who participate in the consultation with their partner. It is largely demonstrated that fertility issues create psychological distress in the couple and mainly in the female partner. 71 , 72 , 73 This determines a “prevarication” of the female partner on the patient himself, 74 which sometimes inhibits the patient's participation in the interaction and shall therefore be further investigated combining qualitative and quantitative methods.
In this first study, we tried to “quantify” the doctor–patient interaction through the evaluation of the number and duration of turns‐at‐talk. The doctor–patient interaction should consider human characteristics, but also education and skills. 75 , 76 These latter are not addressed in our works but should carefully considered. In this setting, the European Society for Sexual Medicine (ESSM) and the Multidisciplinary Joint Committee for Sexual Medicine (MJCSM) tried to guarantee the highest standards of care in the field of sexual medicine. 77 Here, with a conventional statistical approach, we can obtain a first representation of the doctor–patient interaction, but this study clearly suggests that the transcription of their actual turns‐at‐talk could be useful to better understand how doctor‐patient communication occurs in andrology. Our study shows that in a common andrological consultation the doctor generally talks more than the patient. The difference does not regard the number of turns, which seems to be slightly higher for doctors, but no statistical differences are depicted. The duration of the turns, instead, is higher for the doctor. Therefore, the doctor generally speaks longer than the patient, probably because of the lengthy explanations s/he engages in, in both presenting the disease and the therapeutic approach. As a confirmation, the length of the doctor's turns‐at‐talk is independent of the clinical motivation that led the patient to ask for the andrological consultation. Finally, our data suggest that the latency was higher for patients rather than doctors, although this difference seems to be evident only in the infertility set of data. Thus, the latency probably reflects the obviously lower scientific information of the patient on the subject treated. This hypothesis though contrasts with observations that, given the actual wide dissemination of scientific information, 78 patients are generally knowledgeable about the topic, precisely when the issue addressed is couple infertility. Interestingly, the latency seems to be an important parameter that doctor unintentionally considers during the consultation. Indeed, when the patients’ latency increases, the time needed for the doctor to explain necessarily increases and the doctor talks longer.
In conclusion, this is the first attempt to analyse the doctor–patient relationship in andrology by making use of authentic audio‐recorded consultations. Not differently from other settings, it appears clear that a patient‐centred communication should be applied in andrological consultations to promote patients’ participation and to obtain an effective interaction. The topics discussed, however, getting deep into the intimacy of the patients, may require more “medical formulation” to be acceptable for the participants. This suggests that “patient‐centredness” may take a different meaning in the context of andrological diseases. In this respect, more studies are still needed to better explain how to optimize the patients’ contribution in this type of setting.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
AUTHOR CONTRIBUTIONS
Daniele Santi conceived the study, collected and analysed the data, interpreted results and drafted the article. Giorgia Spaggiari collected and analysed the data, interpreted results and drafted the article. Marilina Romeo and Riccardo Ebert drafted the article. Federico Corradini, Claudio Baraldi, Antonio RM Granata, Vincenzo Rochira, Manuela Simoni and Laura Gavioli revised the article critically for important intellectual content. Natacha S. A. Niemants analysed the data and revised the article critically for important intellectual content. All authors approved the final version of the manuscript.
ACKNOWLEDGEMENTS
The study was funded by FAR grant of the University of Modena and Reggio Emilia (Protocol number 17189 of January 30, 2018).
Santi D, Spaggiari G, Romeo M, et al. Qualitative and quantitative analysis of doctor–patient interactions during andrological consultations. Andrology. 2022;10:1240–1249. 10.1111/andr.13225
REFERENCES
- 1. Dorr Goold S, Lipkin M, Jr . The doctor–patient relationship: challenges, opportunities, and strategies. J Gen Intern Med. 1999;14(Suppl 1):S26‐S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ha JF, Longnecker N. Doctor–patient communication: a review. Ochsner J. 2010;10(1):38‐43. [PMC free article] [PubMed] [Google Scholar]
- 3. Hoff T, Collinson GE. How do we talk about the physician–patient relationship? What the nonempirical literature tells us. Med Care Res Rev. 2017;74(3):251‐285. [DOI] [PubMed] [Google Scholar]
- 4. Dorr Goold S, Lipkin M, Jr . The doctor–patient relationship: challenges, opportunities, and strategies. J Gen Intern Med. 1999;14(Suppl 1):S26‐S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Coletti F. Galateo de' Medici e de' Malati. Padova: Coi tipi di A. Bianchi; 1853. [Google Scholar]
- 6. Chiappa GA. Raccolta di opuscoli medici. Pietro Bizzoni; 1828. [Google Scholar]
- 7. Communication in Medical Care: Interaction between Primary Care Physicians and Patients. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- 8. Mead N, Bower P. Patient‐centredness: a conceptual framework and review of the empirical literature. Soc Sci Med (1982). 2000;51(7):1087‐1110. [DOI] [PubMed] [Google Scholar]
- 9. Barry CA, Stevenson FA, Britten N, Barber N, Bradley CP. Giving voice to the lifeworld. More humane, more effective medical care? A qualitative study of doctor–patient communication in general practice. Soc Sci Med (1982). 2001;53(4):487‐505. [DOI] [PubMed] [Google Scholar]
- 10. Epstein RM, Franks P, Shields CG, et al. Patient‐centered communication and diagnostic testing. Ann Fam Med. 2005;3(5):415‐421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zandbelt LC, Smets EM, Oort FJ, Godfried MH, de Haes HC. Patient participation in the medical specialist encounter: does physicians’ patient‐centred communication matter? Patient Educ Couns. 2007;65(3):396‐406. [DOI] [PubMed] [Google Scholar]
- 12. Schouten BC, Meeuwesen L, Tromp F, Harmsen HA. Cultural diversity in patient participation: the influence of patients’ characteristics and doctors’ communicative behaviour. Patient Educ Couns. 2007;67(1‐2):214‐223. [DOI] [PubMed] [Google Scholar]
- 13. Dale J, Sandhu H, Lall R, Glucksman E. The patient, the doctor and the emergency department: a cross‐sectional study of patient‐centredness in 1990 and 2005. Patient Educ Couns. 2008;72(2):320‐329. [DOI] [PubMed] [Google Scholar]
- 14. Arnold RM, Elliot GM. The discourse of medicine: the dialectics of medical interviews. Lang Soc. 1989;18(1):116‐121. [Google Scholar]
- 15. Costello BA, Roberts F. Medical recommendations as joint social practice. Health Commun. 2001;13(3):241‐260. [DOI] [PubMed] [Google Scholar]
- 16. Peräkylä A, Ruusuvuori J. Components of participation in healthcare consultations. A conceptual model for research. Open University: Milton Keynes; 2007. [Google Scholar]
- 17. Castro EM, Van Regenmortel T, Vanhaecht K, Sermeus W, Van Hecke A. Patient empowerment, patient participation and patient‐centeredness in hospital care: a concept analysis based on a literature review. Patient Educ Couns. 2016;99(12):1923‐1939. [DOI] [PubMed] [Google Scholar]
- 18. Chatwin J, Watt I, Collins S, R F. A feeling of equality: some interactional features that build rapport and mutuality in a clinical encounter. 2007.
- 19. Heritage J, Lindström A. Knowledge, empathy, and emotion in a medical encounter. Emot Interact. 2012;98(2):256‐273. [Google Scholar]
- 20. Kale E, Finset A, Eikeland HL, Gulbrandsen P. Emotional cues and concerns in hospital encounters with non‐Western immigrants as compared with Norwegians: an exploratory study. Patient Educ Couns. 2011;84(3):325‐331. [DOI] [PubMed] [Google Scholar]
- 21. Ruusuvuori J. Managing affect: integration of empathy and problem‐solving in health care encounters. Discourse Stud. 2007;9(5):597‐622. [Google Scholar]
- 22. Stone AM. Patient and provider interaction: a global health communication perspective, by Lisa Sparks and Melinda Villagran. Health Commun. 2011;26(8):777‐778. [Google Scholar]
- 23. Epstein RM, Franks P, Fiscella K, et al. Measuring patient‐centered communication in patient–physician consultations: theoretical and practical issues. Soc Sci Med (1982). 2005;61(7):1516‐1528. [DOI] [PubMed] [Google Scholar]
- 24. Formulation in general practice consultations. Text Talk. 2004;24(2):147‐170. [Google Scholar]
- 25. Peräkylä A, Ruusuvuori J, Thompson A. Components of participation in healthcare consultations. In Collins S, Britten N, Ruusuvuori J, Thompson A, eds. A Conceptual Model for Research. Milton Keynes: Open University Press; 2007. [Google Scholar]
- 26. Belpiede A. Mediazione culturale: esperienze e percorsi formativi /a cura di Anna Belpiede. Torino: UTET; 2002. [Google Scholar]
- 27. Luatti L. Atlante della mediazione linguistico culturale : nuove mappe per la professione di mediatore. Milano: Franco Angeli; 2006. [Google Scholar]
- 28. Esposito M, Vezzadini S. La mediazione interculturale come intervento sociale. Milan: Franco Angeli; 2011. [Google Scholar]
- 29. Gurrieri GC. Mediare culture: nuove professioni tra comunicazione e intervento. Carocci; 2003. [Google Scholar]
- 30. Luatti L. Mediatori atleti dell'incontro: luoghi, modi e nodi della mediazione interculturale. Vannini; 2011. [Google Scholar]
- 31. Baraldi C. Interpreting as dialogic mediation: the relevance of expansions. In Baraldi C, Gavioli L, eds. Coordinating Participation in Dialogue Interpreting. John Benjamins Publishing Company; 2012:297‐326. [Google Scholar]
- 32. Jannini EA, Lenzi A, Isidori A, Fabbri A. Subclinical erectile dysfunction: proposal for a novel taxonomic category in sexual medicine. J Sex Med. 2006;3(5):787‐794. [DOI] [PubMed] [Google Scholar]
- 33. De Rose AF, Gallo F, Bini PM, Gattuccio I, Chiriacò V, Terrone C. Epidemiology of sexual disorders in general medical practice: an Italian survey. Urologia. 2019;86(2):79‐85. [DOI] [PubMed] [Google Scholar]
- 34. Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381(9861):153‐165. [DOI] [PubMed] [Google Scholar]
- 35. Mengesha ZB, Perz J, Dune T, Ussher J. Preparedness of health care professionals for delivering sexual and reproductive health care to refugee and migrant women: a mixed methods study. Int J Environ Res Public Health. 2018;15(1):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Botfield JR, Newman CE, Lenette C, Albury K, Zwi AB. Using digital storytelling to promote the sexual health and well‐being of migrant and refugee young people: a scoping review. Health Educ J. 2017;77(7):735‐748. [Google Scholar]
- 37. Silverman D, Peräkylä A. AIDS counselling: the interactional organisation of talk about ‘delicate’ issues. Sociol Health Illness. 1990;12(3):293‐318. [Google Scholar]
- 38. McLawhorn AS, De Martino I, Fehring KA, Sculco PK. Social media and your practice: navigating the surgeon–patient relationship. Curr Rev Musculoskel Med. 2016;9(4):487‐495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Taube KM. Patient–doctor relationship in dermatology: from compliance to concordance. Acta Dermato‐venereol. 2016;96(217):25‐29. [DOI] [PubMed] [Google Scholar]
- 40. Wendling CA. Evolution of the perception of the relationship between doctor and breast cancer patient. Adv Mind Body Med. 2016;30(1):28‐31. [PubMed] [Google Scholar]
- 41. Krishna R. The impact of health information technology on the doctor–patient relationship in child and adolescent psychiatry. Child Adolesc Psychiatr Clin North America. 2017;26(1):67‐75. [DOI] [PubMed] [Google Scholar]
- 42. Mariampillai JE, Eskas PA, Heimark S, et al. Apparent treatment‐resistant hypertension: patient–physician relationship and ethical issues. Blood Pressure. 2017;26(3):133‐138. [DOI] [PubMed] [Google Scholar]
- 43. Corona G, Ricca V, Bandini E, et al. SIEDY scale 3, a new instrument to detect psychological component in subjects with erectile dysfunction. J Sex Med. 2012;9(8):2017‐2026. [DOI] [PubMed] [Google Scholar]
- 44. Corona G, Ricca V, Boddi V, et al. Autoeroticism, mental health, and organic disturbances in patients with erectile dysfunction. J Sex Med. 2010;7(1 Pt 1):182‐191. [DOI] [PubMed] [Google Scholar]
- 45. Petrone L, Mannucci E, Corona G, et al. Structured interview on erectile dysfunction (SIEDY): a new, multidimensional instrument for quantification of pathogenetic issues on erectile dysfunction. Int J Impot Res. 2003;15(3):210‐220. [DOI] [PubMed] [Google Scholar]
- 46. Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822‐830. [DOI] [PubMed] [Google Scholar]
- 47. Qiao Z, Li X, Liu H, et al. Using statistics and data mining approaches to analyze male sexual behaviors and use of erectile dysfunction drugs based on large questionnaire data. Stud Health Technol Inform. 2017;235:206‐210. [PubMed] [Google Scholar]
- 48. WHO . WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed, 2010. [Google Scholar]
- 49. Hazir B, Haberal HB, Asci A, Muneer A, Gudeloglu A. Erectile dysfunction management: a critical appraisal of clinical practice guidelines with the AGREE II instrument. Int J Impot Res. 2021. [DOI] [PubMed] [Google Scholar]
- 50. Sacks H, Schegloff EA, Jefferson G. A simplest systematics for the organization of turn‐taking for conversation. Language. 1974;50(4):696‐735. [Google Scholar]
- 51. Goodwin C, Heritage J. Conversation analysis. Annu Rev Anthropol. 1990;19(1):283‐307. [Google Scholar]
- 52. Norrick NR. Conversational Narrative: Storytelling in Everyday Talk. John Benjamins; 2000. [Google Scholar]
- 53. Stivers T, Heritage J. Breaking the sequential mold: Answering ‘more than the question’ during comprehensive history taking. Text Talk. 2001;21(1‐2):151‐185. [Google Scholar]
- 54. Walker HK, Hall WD, Hurst JW. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. Boston: Butterworths; 1990. [PubMed] [Google Scholar]
- 55. Copyright © 1990, Butterworth Publishers, a division of Reed Publishing; 1990.
- 56. Heritage J, Clayman S. Patients’ presentations of medical issues: the doctor's problem; 2010:101‐118.
- 57. Beach WA, Dixson CN. Revealing moments: formulating understandings of adverse experiences in a health appraisal interview. Soc Sci Med. 2001;52(1):25‐44. [DOI] [PubMed] [Google Scholar]
- 58. Lamb G, Heritage J, Clayman S. Talk‐in‐action: identities, interaction and institutions. J Lang Polit. 2012;11:306‐310. [Google Scholar]
- 59. Fuzzell L, Fedesco HN, Alexander SC, Fortenberry JD, Shields CG. “I just think that doctors need to ask more questions”: Sexual minority and majority adolescents' experiences talking about sexuality with healthcare providers. Patient Educ Couns. 2016;99(9):1467‐1472. [DOI] [PubMed] [Google Scholar]
- 60. East L, Jackson D, Manias E, Dunning T, Hutchinson M. Patient perspectives and experiences of sexual health conversations and cardiovascular disease: a qualitative study. J Clin Nurs. 2021;30(21‐22):3194‐3204. [DOI] [PubMed] [Google Scholar]
- 61. Chung E, Gilbert B, Perera M, Roberts MJ. Premature ejaculation: a clinical review for the general physician. Aust Fam Physician. 2015;44(10):737‐743. [PubMed] [Google Scholar]
- 62. Elyasi F, Parkoohi PI, Naseri M, et al. Relationship between coping/attachment styles and infertility‐specific distress in Iranian infertile individuals: a cross‐sectional study. Int J Reprod Biomed. 2021;19(4):347‐360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Jacob JA, Aleyamma TK, Kuruvilla A, Gopalakrishnan R. Common mental disorders, quality of life and explanatory models in men undergoing infertility treatment in a tertiary care hospital: a cross‐sectional study. J Psychosom Res. 2021;147:110536. [DOI] [PubMed] [Google Scholar]
- 64. Pozza A, Dèttore D, Coccia ME. Depression and anxiety in pathways of medically assisted reproduction: the role of infertility stress dimensions. Clin Pract Epidemiol Ment Health. 2019;15:101‐109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Beach WA. Transitional regularities for ‘casual’ “Okay” usages. J Pragmatics. 1993;19(4):325‐352. [Google Scholar]
- 66. Baraldi C. Language mediation as communication system. Commun Theory. 2017;27(4):367‐387. [Google Scholar]
- 67. Baraldi C, Gavioli L. Effective communication and knowledge distribution in healthcare interaction with migrants. Health Commun. 2020;36: 1‐9. [DOI] [PubMed] [Google Scholar]
- 68. Niemants N. La participation des migrants en santé reproductive : le cas des consultations d'andrologie. Éla Études de linguistique appliquée. 2021;202(2):207‐218. [Google Scholar]
- 69.Byrne P, Long B.Doctors talking to patients. Psychol Med. 1977;7(4):735‐735. [Google Scholar]
- 70. Baraldi C, Luppi L. Ways of overcoming linguistic barriers in healthcare intercultural communication. Lang Intercult Commun. 2015;15(4):581‐599. [Google Scholar]
- 71. Robinson JD, Heritage J. The structure of patients’ presenting concerns: the completion relevance of current symptoms. Soc Sci Med. 2005;61(2):481‐493. [DOI] [PubMed] [Google Scholar]
- 72. Chan CHY, Lau BHP, Tam MYJ, Ng EHY. Preferred problem solving and decision‐making role in fertility treatment among women following an unsuccessful in vitro fertilization cycle. BMC Womens Health. 2019;19(1):153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Frederiksen Y, Farver‐Vestergaard I, Skovgård NG, Ingerslev HJ, Zachariae R. Efficacy of psychosocial interventions for psychological and pregnancy outcomes in infertile women and men: a systematic review and meta‐analysis. BMJ Open. 2015;5(1):e006592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Nicoloro‐SantaBarbara J, Busso C, Moyer A, Lobel M. Just relax and you'll get pregnant? Meta‐analysis examining women's emotional distress and the outcome of assisted reproductive technology. Soc Sci Med. 2018;213:54‐62. [DOI] [PubMed] [Google Scholar]
- 75. Kim M, Yi SJ, Hong JE. Experiences of women with male factor infertility under in vitro fertilization. Int J Environ Res Public Health. 2020;17(21). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Jannini EA, Reisman Y. Medicine without sexual medicine is not medicine: an MJCSM and ESSM petition on sexual health to the political and university authorities. J Sex Med. 2019;16(6):943‐945. [DOI] [PubMed] [Google Scholar]
- 77. Carrell DT, Rajpert‐De Meyts E, Krausz C, et al. The need of continuous focus on improved mentoring of trainees and young investigators in the field of andrology: highlights of current programs and opportunities for the future. Andrology. 2014;2(5):649‐651. [DOI] [PubMed] [Google Scholar]
- 78. Serefoglu EC, Reisman Y, Bitzer J, Vignozzi L, Jannini EA. The only available certification for sexual medicine: the Fellow of the European Committee Sexual Medicine (FECSM). Int J Impot Res. 2021. [DOI] [PubMed] [Google Scholar]
- 79. Peng Y, Yin P, Deng Z, Wang R. Patient–physician interaction and trust in online health community: the role of perceived usefulness of health information and services. Int J Environ Res Public Health. 2019;17(1):139. [DOI] [PMC free article] [PubMed] [Google Scholar]


