Abstract
Objective
The objective of this study is to compare the effectiveness of complex physical therapy combined with intermittent pneumatic compression (CPT + IPC) versus Kinesio taping (KT) for breast cancer‐related lymphedema.
Methods
A cross‐over clinical trial was conducted in 43 women with lymphedema. All participants received two interventions: CPT + IPC and KT, both lasting 3 weeks and a washout period. The main outcome variable was the relative volume change (RVC). The secondary variables were Satisfaction Questionnaire about Textile Therapeutic Devices used for Breast Cancer‐Related Lymphedema, Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire, motion range of upper limb and lymphedema‐related symptoms.
Results
The RVC reduction was greater with CPT + IPC (−2.2%, SD = 4.7) versus KT (−0.9%, SD = 1.7) (P = 0.002). KT was more satisfactory than multilayer bandaging (8.9 points difference, P < 0.001) and improved DASH score more than CPT + IPC (14.3 points difference, P = 0.002). Regarding motion ranges, only shoulder movements showed significant improvement with CPT + IPC compared with KT (differences between 5.6° and 11.4°). Of the symptoms assessed, only pain reduction showed a significant improvement with KT versus CPT + IPC (0.5 points, P = 0.035).
Conclusions
CPT + IPC achieved higher RVC and greater improvement in th shoulder motion range than KT. Conversely, KT was more satisfactory than multilayer bandaging, obtained better DASH scores and relieved pain more than CPT + IPC.
Clinical Registration
ClinicalTrial registration number: NCT03051750 (date of registration 14 February 2017).
Keywords: complex physical therapy, intermittent pneumatic compression, Kinesio taping, lymphedema, relative volume change, satisfaction
1. INTRODUCTION
Upper‐limb lymphedema is one of the most important sequels of breast cancer (Burkhardt et al., 2014). At present, complex physical therapy (CPT) is considered the reference treatment for lymphedema (Ezzo et al., 2015). The intensive phase of this therapy includes manual lymph drainage, multilayer bandaging, skin care and daily exercising of the upper limb (Ezzo et al., 2015; Poage et al., 2008). The combined use of intensive CPT with intermittent pneumatic compression (CPT + IPC) has shown effectiveness for reducing the volume of breast cancer‐related lymphedema (Schaverien et al., 2018).
On the other hand, Kinesio taping is also employed in certain lymphedema cases given its potential effect on lymph drainage (Tsai et al., 2009). However, evidence regarding its effectiveness is scarce and on occasions contradictory, and additional randomised trials are needed to elucidate the proper use of Kinesio taping for treating lymphedema (Gatt et al., 2017; Kasawara et al., 2018).
Although CPT is safe and effective for the majority of women, some studies have warned about the challenge it poses for patients to comply with it and also the difficulties of clinical application related to the multiple components of the treatment, cost, time and low adherence in the long term (Cemal et al., 2011; Fu, 2014). Specifically, multilayer bandages that are applied in CPT are uncomfortable and make lymphedema more visible, resulting in low tolerance and adherence to the treatment (Poage et al., 2008). On the other hand, despite the wounds it can cause to the skin (Gatt et al., 2017), Kinesio taping can be a more comfortable and economic therapy than multilayer bandaging (Pajero Otero et al., 2021; Torres‐Lacomba et al., 2020; Tsai et al., 2009), with an estimated saving of €626.90 over a 4‐week treatment (Melgaard, 2016).
To our knowledge, there are no former trials assessing the effectiveness of Kinesio taping versus CPT + IPC for treating breast cancer‐related lymphedema. Therefore, the main aim of this trial was to compare the effect on the relative volume change (RVC) of lymphedema using Kinesio taping versus CPT + IPC. The secondary objectives were to contrast patient satisfaction with the textile devices employed in both therapies (Kinesio taping vs. multilayer bandaging) and the effect of both interventions on lymphedema‐related symptoms, functionality and motion ranges of the upper‐limb joints.
2. METHODS
The trial was conducted between February and December of 2016 at Hospital 12 de Octubre, in collaboration with the University of Castilla‐La Mancha and the Complutense University of Madrid. The study was approved by the Ethics Committee of Hospital 12 de Octubre (CEIC 16/014), complying with all criteria established by the CONSORT group (Table S1).
For the recruitment of participants, a randomised list was generated by a computer from all patients who had received assistance at the rehabilitation service for breast pathology of Hospital 12 de Octubre over the two previous years. The subjects were contacted by phone in a consecutive order to inform them about the trial, and those who accepted to participate were included until completing the estimated sample size. All subjects provided written informed consent. To ensure allocation blinding, an outside researcher supervised the balanced randomisation of the order of interventions by asking the participants to extract ballots from an opaque box. Seven women revoked their consent before beginning the study. All participants were asked to continue their lymphedema‐related self‐care (skin care and exercising protocol) throughout the trial (Ezzo et al., 2015).
The inclusion criteria to be selected were women >18 years of age, with breast cancer‐related lymphedema (volume increase >5% relative to the non‐affected arm [Fu, 2014] measured at the first day of treatment), who were treated at the rehabilitation service of the hospital where the trial was conducted and who could attend the hospital at each study phase. The exclusion criteria were having received physiotherapeutic treatment for lymphedema during the 3 months previous to the beginning of the trial, presence of breast cancer metastasis or any active tumour, undergoing systemic chemotherapy and/or radiotherapy, heart or kidney failure, pharmacological treatment with diuretics, bilateral axillary lymphadenectomy, malformation of the upper limb, cognitive impairment or mental retardation, any skin alteration in the upper limbs or back and allergy to Kinesio taping based on a previous test where 1 cm2 of Kinesio tape was applied to the healthy arm for 3 days.
A cross‐over clinical trial was designed with a balanced randomisation of the intervention order. The efficiency was compared between two different interventions for treating breast cancer‐related lymphedema: CPT + IPC versus Kinesio taping. The chronic nature of lymphedema (Finnane et al., 2015) and the ethical consideration of delivering the standard therapy to all participants justify the cross‐over design.
A trained external researcher evaluated every participant before and after each intervention. Blinding of patients or the researcher that delivered the intervention was not possible. The evaluators also could not be blinded due to the skin marks that remained several hours after removing either of the employed textile devices (Kinesio tape or multilayer bandage).
Clinical and sociodemographic variables were recorded at baseline. The collected data were age, body mass index (BMI), type of surgery, years since axillary surgery, amount of removed lymph nodes, radiotherapy, stage of lymphedema, years with lymphedema, side of the affected limb and whether it was the dominant arm and type of compression garment.
The RVC (Ancukiewicz et al., 2012) and the relative volume difference (RVD) (Deltombe et al., 2007) in the affected arm were the two variables used for determining the effect of the therapy. The RVC was the main variable and was calculated as RVC = [((A2U1)/(U2A1)) − 1], where A1 and A2 stand for the arm volumes on the same side of the affected breast at two time points, namely, before and after treatment, and U1 and U2 are the volumes of the unaffected arm. This equation accounts for the upper‐limb size, which prevents biases resulting from changes in the BMI throughout the intervention (Ancukiewicz et al., 2012). However, since RVC data in the current literature was insufficient for determining the sample size, the RVD was also calculated as follows RVD = [(A2 − A1)/(A2 + A1/2) × 100] (Deltombe et al., 2007), despite this formula not takes into consideration the volume of the unaffected limb. Following the same protocol as a former study by our group (Pajero Otero et al., 2019), circometry was the method chosen to estimate the volume in both arms, using a 1‐cm‐wide standard retractable measuring tape (Medi, Germany). The measurement points were the following anatomic references of the upper limb (Taylor et al., 2006): metacarpophalangeal heads, ulnar styloid, mid forearm, olecranon, mid arm and 65% distance from the olecranon to the acromion (López Martín et al., 2011). Participants were sitting, with the shoulder flexed (≈45°), elbow extended and hand palm resting on a table. The volume was estimated using a computerised calculation by López Martín et al. for converting limb measurements into volume via the following formula:
where V is the volume of the arm segment, C1 and C2 are the arm circumference at the endpoints of the segment and h is the distance between C1 and C2 (i.e. segment length) (Taylor et al., 2006).
In terms of secondary variables, the Satisfaction Questionnaire about Textile Therapeutic Devices used for Breast Cancer‐Related Lymphedema (SQ‐TTD‐BCRL) was selected for measuring the patient satisfaction with the textile device employed (multilayer bandage or Kinesio taping). This questionnaire comprises 20 questions scoring from 1 to 5, where 20 is the lowest total score, indicating the greatest satisfaction, and 100 points represent the lowest possible satisfaction (Pajero Otero et al., 2021). The functionality of the affected limb was measured via the Spanish version of the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire (Rosales et al., 2002), which was validated for women with breast cancer‐related lymphedema both in English (Dawes et al., 2008; Harrington et al., 2014) and Spanish (Puentes‐Gutierrez, 2015). The DASH questionnaire evaluates 30 items, each ranging from 1 to 5, and the overall score is transformed into a scale ranging from 0 to 100, where 0 is the best possible score and 100 the worst possible score, indicating maximum impairment (Puentes‐Gutierrez, 2015). The motion range of the affected arm joints was evaluated using a universal goniometer (Comed) to measure the following data: flexion, extension and abduction of the shoulder; flexion and extension of the elbow; and flexion and extension of the wrist. Patients were in a standing position during the goniometry of the shoulder and elbow and sitting for the goniometry of the wrist. Three measurements were recorded for every movement and their average was then obtained after discarding those differing >10°. Lymphedema‐related symptoms (pain, pressure, heaviness and hardness) were verbally reported on a numeric scale that ranged from 0 to 5 (0 = no symptom, 1 = very light, 2 = light, 3 = moderate, 4 = severe, 5 = unbearable) (Pajero Otero et al., 2019).
Patients were treated with two interventions, each lasting 3 weeks, whose order was randomised by blocks. Group A received CPT + IPC during the first phase of the intervention and Kinesio taping during the second one, whereas Group B received the same therapies in the reverse order. A washout period of 3 months before the beginning of the trial was established for both groups. The washout period between treatments was 6 months. According to Czerniec et al. (2016), breast cancer‐related lymphedema does not fluctuate significantly over periods of 6 months. Therefore, delivering both treatments in Springtime and Autumn avoids the extreme temperatures of Summer and Winter in Spain, minimising potential weather effects (Gordon et al., 2009).
The CPT + IPC intervention was delivered from Monday to Friday over three consecutive weeks. This therapy comprised a 30‐min manual lymph drainage following the Vodder method combined with 30 min of intermittent sequential IPC at 40 mm Hg (Feldman et al., 2012), which was delivered via a Lympha‐Tron DL 1200 Doctor Life device, and finished with the application of a multilayer bandage. The manual lymph drainage consisted of stimulating the neck first (lateral and posterior cervical nodes and supraclavicular fossae) followed by an approach to the affected side of the thorax by stimulating the anterior and posterior axillo‐axillary bypass. Finally, manual lymph drainage was applied to the affected upper limb, starting from the most proximal towards distal segments, applying drainage in a centripetal direction in each area and stimulating the Mascagni pathway in the arm region. The duration of each massage phase was based on the study by Szolnoky et al. (2013), who obtained better results applying 30 min of manual lymph drainage + 30 min of IPC compared to 60 min of manual lymph drainage alone. The multilayer bandage included a tubular cotton bandage (Tubigrip®), a 10‐cm‐wide and 2‐mm‐thick foam bandage (Texafoam®) and a short 8‐cm‐wide stretch bandage (Rosidal®K). These were applied in a spiral shape, overlapping every two thirds, and with decreasing compression from the knuckles to the axilla (Ergin et al., 2018). Fingers showing lymphedema were dressed in a 4‐cm‐wide non‐cohesive elastic bandage (Elastomull®). Participants were asked to wear the multilayer bandage until the following day (except when it caused pain or prevented any daily‐life activity) and to remove it at home before attending the next session for personal hygiene and arm skin hydration purposes. They were also requested to report daily on how long they wore the multilayer bandage in order to monitor adherence.
The Kinesio taping treatment followed the method by Sijmonsma, consisting of three 1.25‐cm‐wide individual strips, which were placed in parallel, starting at the contralateral axilla, then over the back making waves and through the upper limb in a spiroid shape up to the wrist. They were applied without tension and with the skin previously stretched to its maximum in order to achieve convolutions (Bosman, 2014; Sijmonsma, 2010) (Figure 1). The Kinesio taping was maintained 24 h a day for three consecutive weeks and a physiotherapist renovated it every three to 5 days.
FIGURE 1.

Spiroid technique for applying Kinesio taping from the contralateral axilla up to the homolateral wrist to the breast cancer‐related lymphedema. Source: Hospital 12 de Octubre. Participating patient who signed consent for the use of this image for scientific purposes
The calculation of the sample size was based on a former study that estimated an intra‐ and inter‐rater reliability of 3.2% (SD = 4.6) for the RVD (Deltombe et al., 2007). Considering that the expected difference between therapies should be higher than this measurement error, a sample size of 50 participants was obtained (25 in each group) for an average RVD ≥ 3.2% (SD = 4.6) between interventions, a confidence level of 95%, a power of 80% and a dropout rate of 30%.
An intention‐to‐treat analysis with the last recorded observation was conducted in the cases of patients who quit the trial prior to the end of the intervention. Statistical significance was set at 5% for all tests. Descriptive statistical models were employed for demographic and clinical variables at baseline. Quantitative variables were tested for normality, and a paired Student's t test or Wilcoxon test were employed when the data were found to be normally distributed or not, respectively. Qualitative ordinal variables were analysed with the Wilcoxon test. The Mann–Whitney U test was used for comparing the two study arms to assess the potential effect of the intervention order and the Wilcoxon test was employed for evaluating the carry‐over and period effects. The statistical analyst was blinded to the intervention, and all analyses were performed using the SPSS 24.0 software.
3. RESULTS
Fifty women were randomised before the beginning of the trial, of which 43 participated. Two subjects quit throughout the study for not being able to comply with the treatment and evaluation dates due to health problems, and one patient from Group B did not receive the second intervention because of not showing lymphedema after the first treatment with CPT + IPC. Hence, 40 women completed all phases of the trial. The intention‐to‐treat analysis included the 43 participants who began the study by entering the last recorded observation (Figure 2). No intergroup differences were found in the collected sociodemographic and clinical variables at baseline (Table 1). None of the included subjects presented stage I or stage III lymphedema.
FIGURE 2.
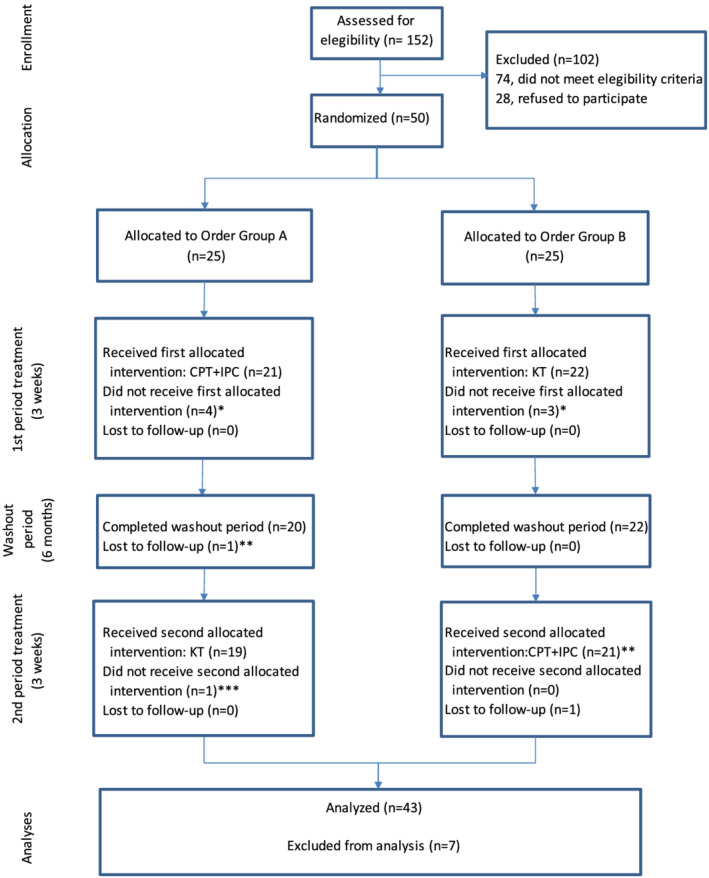
Flowchart for the participants. CPT, complex physical therapy; IPC, intermittent pneumatic compression; KT, Kinesio taping. *Seven participants declined beginning the trial. **Two participants abandoned the trial before finalisation. ***One participant did not receive the second phase of treatment since she did not suffer from lymphedema any longer
TABLE 1.
Baseline sociodemographic and clinical characteristics of participants and comparison between groups
|
Group A N = 21 |
Group B N = 22 |
P value | |
|---|---|---|---|
| Age (years), mean (SD) | 59.4 (12.2) | 63.0 (11.3) | 0.301 b |
| Body mass index, mean (SD) | 29.2 (3.7) | 29.6 (5.3) | 0.970 a |
| Surgery (lumpectomy/mastectomy) | 9/12 (42.9%) | 7/15 (31.9%) | 0.536 c |
| Radiotherapy (yes/no) | 18/3 (85.7%) | 18/4 (81.8%) | 1.000 c |
| Years since lymph node dissection, mean (SD) | 8.2 (7.2) | 8.7 (10.2) | 0.677 b |
| Lymph nodes removed, mean (SD) | 17.3 (6.4) | 21.0 (8.1) | 0.110 b |
| Phase of lymphedema (IIA/IIB) | 4/17 (19.0%) | 6/16 (27.3%) | 0.720 c |
| Volume difference between upper limbs (%), mean (SD) | 18.2% (10.5) | 19.0% (12.2) | 0.779 a |
| Years with lymphedema, mean (SD) | 5.8 (5.75) | 8.4 (8.3) | 0.386 b |
| Lymphedema in right/left upper limb | 14/7 (66.7%) | 12/10 (54.5%) | 0.536 c |
| Dominant upper‐limb lymphedema (yes/no) | 15/6 (71.4%) | 12/10 (54.5%) | 0.347 c |
| Compression garment (yes/no) | 16/5 (76.2%) | 16/6 (72.7%) | 1.000 c |
| Gauntlet (yes/no) | 9/12 (42.9%) | 6/16 (27.3%) | 0.347 c |
| Pain (0–5), mean (SD) | 1.0 (1.0) | 1.5 (1.4) | 0.331 b |
| Tightness (0–5), mean (SD) | 1.9 (1.1) | 1.9 (1.5) | 0.898 b |
| Heaviness (0–5), mean (SD) | 2.4 (1.4) | 1.9 (1.3) | 0.271 b |
| Hardness (0–5), mean (SD) | 1.9 (1.2) | 1.8 (1.5) | 0.589 b |
| DASH (0–100), mean (SD) | 42.0 (15.9) | 39.5 (20.7) | 0.609 b |
| Flexion of shoulder (degrees), mean (SD) | 138.0 (28.5) | 131.0 (30.3) | 0.324 a |
| Extension of shoulder (degrees), mean (SD) | 45.0 (13.2) | 43.1 (8.0) | 0.394 a |
| Abduction of shoulder (degrees), mean (SD) | 125.7 (36.6) | 123.3 (42.8) | 0.715 a |
| Flexion of elbow (degrees), mean (SD) | 143.9 (3.5) | 142.2 (5.4) | 0.380 a |
| Extension of elbow (degrees), mean (SD) | 10.6 (7.3) | 11.8 (7.0) | 0.670 a |
| Flexion of wrist (degrees), mean (SD) | 71.0 (10.2) | 70.2 (9.3) | 0.932 a |
| Extension or wrist (degrees), mean (SD) | 55.2 (15.9) | 56.4 (13.0) | 0.817 |
Abbreviation: DASH, Disabilities of the Arm, Shoulder and Hand.
Student's t test for independent samples.
Mann–Whitney U test.
Pearson's chi‐squared test.
The reduction observed in the lymphedema by comparing the RVC was greater in the intervention with CPT + IPC (−2.2%, SD = 4.7) versus Kinesio taping (−0.9%, SD = 1.7; P = 0.002). However, statistically significant differences were not found when comparing the RVD from CPT + IPC (−2.4%, SD = 2.5) versus Kinesio taping (−1.6%, SD 2.0; P = 0.09) (Table 2). No period (Z = −1.6; P = 0.11) or carry‐over (Z = −0.4; P = 0.70) effects were observed, or any effect of the intervention order (t = −0.7; P = 0.51) for the upper‐limb volume. In the intervention with CPT + IPC, the average duration of wearing the multilayer bandage was 15.2 h per day (SD = 5.0), and no correlation was found between this variable and the RVC (Spearman's rank correlation coefficient = −0.2; P = 0.23). In terms of patient satisfaction with the therapeutic textile devices, Kinesio taping obtained a higher score than multilayer bandaging in all evaluated dimensions, except for perceived benefits, where no differences were noted between both systems (Table 2).
TABLE 2.
Relative volume change, relative volume difference and score in the questionnaire about satisfaction with textile therapeutic devices for breast Cancer‐related lymphedema
| Outcome (units) | CPT + IPC | KT | CPT + IPC minus KT | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | P value | |
| Relative volume change (%) | −2.2 (4.7) | −0.9 (1.7) | −1.3 (5.0) | 0.002 a |
| Relative volume difference (%) | −2.4 (2.5) | −1.6 (2.0) | −0.8 (3.1) | 0.090 b |
| SQ‐TTD‐BCRL | ||||
| Total score (20–100) | 49.2 (12.8) | 40.3 (12.2) | 8.9 (12.2) | <0.001 b |
| Mood (6–30) | 14.1 (5.9) | 12.1 (5.5) | 2.0 (4.7) | 0.008 a |
| Patient comfort (9–45) | 24.7 (6.1) | 18.2 (6.4) | 6.5 (7.0) | <0.001 a |
| Patient compliance (2–10) | 4.3 (2.0) | 3.2 (1.6) | 1.2 (2.2) | 0.001 a |
| Perceived benefits (3–15) | 6.1 (2.1) | 6.9 (2.9) | 0.8 (2.7) | 0.076 a |
Note: Values in bold represent statistically significant differences (P < 0.05).
Abbreviations: CPT, complex physical therapy; IPC, intermittent pneumatic compression; KT, Kinesio taping; SQ‐TTD‐BCRL, Satisfaction Questionnaire about Textile Therapeutic Devices used for Breast Cancer‐Related Lymphedema.
Wilcoxon signed‐rank test.
Student's t test.
Table 3 shows the outcomes for all the remaining secondary variables. Functionality assessed via the DASH questionnaire experienced a greater improvement with Kinesio taping versus CPT + IPC, with an intergroup difference of 14.3 points (SD = 27.8; P = 0.002). In terms of motion ranges of the arm joints, the CPT + IPC group showed a greater improvement versus Kinesio taping for the flexion (5.6°, SD = 20.0; P = 0.049), extension (5.0°, SD = 9.5; P = 0.001) and abduction (11.4°, SD = 30.7; P = 0.024) of the shoulder. On the contrary, no differences were found between therapies in the motion ranges of the elbow and wrist. Pain was the only lymphedema‐related symptom where a statistically significant improvement was observed, with Kinesio taping showing greater improvement versus CPT + IPC (0.5 points, SD = 1.5; P = 0.035) (Table 3).
TABLE 3.
DASH score; motion ranges of arm joints; and pain, tightness, heaviness and hardness verbally reported on a numeric scale
| Outcome (units) | CPT + IPC | KT | CPT + IPC minus KT |
|---|---|---|---|
| Post‐intervention minus baseline | Post‐intervention minus baseline | ||
| Mean (SD) | Mean (SD) | Mean (SD) | |
| P value | P value | P value | |
| DASH (0–100) | 8.4 (24.7) | −5.9 (16.6) | 14.3 (27.8) |
| P = 0.031 a | P = 0.026 a | P = 0.002 a | |
| Flexion of shoulder (degrees) | 1.7 (10.7) | −3.9 (13.4) | 5.6 (20.0) |
| P = 0.276 b | P = 0.054 b | P = 0.049 c | |
| Extension of shoulder (degrees) | 2.2 (8.5) | −2.8 (6.0) | 5.0 (9.5) |
| P = 0.088 b | P = 0.004 b | P = 0.001 c | |
| Abduction of shoulder (degrees) | 8.8 (23.8) | −2.5 (18.4) | 11.4 (30.7) |
| P = 0.015 b | P = 0.562 b | P = 0.024 c | |
| Flexion of elbow (degrees) | −0.7 (12.5) | 1.5 (5.4) | −2.1 (13.2) |
| P = 0.444 b | P = 0.035 b | P = 0.408 c | |
| Extension of elbow (degrees) | 2.9 (9.3) | 2.2 (11.2) | 0.7 (12.5) |
| P = 0.221 b | P = 0.264 b | P = 0.623 c | |
| Flexion of wrist (degrees) | −1.7 (8.2) | 0.4 (5.6) | −2.1 (11.3) |
| P = 0.228 b | P = 0.609 b | P = 0.378 c | |
| Extension of wrist (degrees) | 0.6 (8.1) | 0.0 (6.0) | 0.7 (10.1) |
| P = 0.910 b | P = 0.865 b | P = 0.910 c | |
| Pain (0–5) | 0.1 (1.3) | −0.3 (1.1) | 0.5 (1.5) |
| P = 0.723 b | P = 0.065 b | P = 0.035 c | |
| Tightness (0–5) | −0.1 (1.1) | −0.5 (1.0) | 0.4 (1.6) |
| P = 0.264 b | P = 0.001 b | P = 0.103 c | |
| Hardness (0–5) | −0.3 (1.1) | −0.3 (1.1) | 0.0 (1.3) |
| P = 0.027 b | P = 0.047 b | P = 0.978 c | |
| Heaviness (0–5) | −0.3 (1.4) | −0.6 (1.1) | 0.3 (1.8) |
| P = 0.227 b | P = 0.002 b | P = 0.237 c |
Note: Values in bold represent statistically significant differences (P < 0.05).
Abbreviations: CPT, complex physical therapy; DASH, Disabilities of the Arm, Shoulder and Hand; IPC, intermittent pneumatic compression; KT, Kinesio taping.
Student's t test for DASH scores.
Wilcoxon signed‐rank test for within‐group comparison.
Wilcoxon signed‐rank test for between‐group comparison.
The observed adverse effects were light and included itching, reddening, paresthesia, and skin peeling, with no significant differences between groups for any of them (Table 4). No participant suffered serious adverse effects during any of the treatments, although three women in the group receiving CPT + IPC as the first treatment reported erysipelas during the washout period.
TABLE 4.
Adverse effects during each therapy
| Adverse event | CPT + IPC | KT | P value |
|---|---|---|---|
| Itching | 6 | 6 | 1 a |
| Reddening | 6 | 11 | 0.176 a |
| Paresthesia | 1 | 1 | 1 b |
| Skin peeling | 0 | 4 | 0.116 b |
Abbreviations: CPT, complex physical therapy; IPC, intermittent pneumatic compression; KT, Kinesio taping.
Chi‐squared test.
Fisher's exact test.
4. DISCUSSION
This trial observed a greater reduction in the RVC of the upper limb with lymphedema during the intensive phase of CPT + IPC compared to Kinesio taping. No differences were noted in the RVD between both interventions. In terms of both RVC and RVD, the intergroup difference did not reach 3.2%, the value that Deltombe et al. (2007) determined to be the minimum intra‐ and inter‐rater reliability for measuring upper‐limb lymphedema. Hence, this study considered that none of the delivered therapies attained a clinically significant effect for reducing breast cancer‐related lymphedema.
To our knowledge, this is the first randomised clinical trial that compared CPT + IPC against Kinesio taping alone for treating breast cancer‐related lymphedema. Despite the different designs found in the literature, several studies reported similar outcomes to those observed in this work. Some trials that delivered CPT + IPC substituting multilayer bandages by Kinesio taping also found greater volume reductions using multilayer bandages versus Kinesio taping (Smykla et al., 2013; Taradaj et al., 2016; Torres‐Lacomba et al., 2020; Tsai et al., 2009), whereas other authors observed that both therapies produced very similar results (Conejo Tirado & Súarez Arcos, 2012; Pekyavaş et al., 2014). In light of these outcomes, the use of Kinesio taping within CPT did not appear to be more effective than multilayer bandaging for reducing the lymphedema volume (Gatt et al., 2017; Kasawara et al., 2018). The protocols for applying CPT and/or IPC were very diverse and showed significant variability in terms of the reported reductions in the lymphedema volume, although all previous studies obtained a greater reduction in the lymphedema volume than that observed in the CPT + IPC group of this trial. These differences could be due to the lack of adherence to multilayer bandaging, among other reasons. According to Forner‐Cordero et al. (2010), an adherence to the treatment with multilayer bandaging of ≥90% of time improves the therapy outcomes, which is in agreement with the postulates establishing that multilayer bandaging appears to be the most important component of CPT (Ezzo et al., 2015). Therefore, the low adherence to multilayer bandages (average use of 15.1 h/day) this trial obtained, which is considerably lower than the recommended 23 h/day, could be responsible for the reduced effectiveness. Other randomised trials that employed Kinesio taping alone and compared it against multilayer bandaging or no intervention (Malicka et al., 2014; Pajero Otero et al., 2019; Tantawy et al., 2019) reported greater improvement in the lymphedema volume using Kinesio taping. Therefore, the independent use of Kinesio tape could be better than not receiving any treatment or be recommended for patients who cannot wear multilayer bandages or report low adherence to it (Tsai et al., 2009).
This trial observed a higher degree of patient satisfaction with the textile devices with Kinesio taping compared to multilayer bandaging, similarly to the outcomes of a former study for validating the SQ‐TTD‐BCRL (Pajero Otero et al., 2021). Other works about Kinesio taping that employed different measurement tools also perceived Kinesio taping as more comfortable and satisfactory for the patients than multilayer bandaging (Conejo Tirado & Súarez Arcos, 2012; Melgaard, 2016; Torres‐Lacomba et al., 2020; Tsai et al., 2009). Therefore, Kinesio taping appears to be a more valued therapy for lymphedema patients in terms of satisfaction and comfort for performing daily‐life activities and allowing them to wear their usual clothing (Melgaard, 2016; Tsai et al., 2009). Intergroup differences were observed in functionality, as measured via the DASH questionnaire, where Kinesio taping was significantly superior to the CPT + IPC intervention. This outcome can be considered clinically relevant since the difference was >10.83 points, as Franchignoni et al. (2014) established. No studies were found that employed the DASH questionnaire for assessing Kinesio taping for treating lymphedema; however, Tantawy et al. (2019) employed the Shoulder Pain and Disability Index (SPADI) questionnaire and also reported an improvement in functionality with the Kinesio taping therapy. Such improvement can be mainly related to better ease of movement with Kinesio taping versus multilayer bandages.
The motion ranges of arm joints increased significantly more with CPT + IPC than Kinesio taping for the flexion, extension and abduction of the shoulder. However, the improvement did not reach the minimally detectable change set by Rasmussen et al. (2020) at 20.8° and 10.2° for abduction and flexion, respectively. Few trials can be found that assessed this variable. Szuba et al. (2002) did not observe any changes in the motion range after delivering CPT + IPC. A former study by this research group (Pajero Otero et al., 2019) observed light improvements in the motion range of arm joints after applying Kinesio tape that did not reach the minimally detectable change. The better outcomes this trial obtained in the shoulder motion range following the CPT + IPC treatment versus Kinesio taping can be due to the more frequent physiotherapist–patient relationship during the CPT + IPC phase, which can act as a reminder for the exercising protocol that all participants received for their daily routine.
In terms of lymphedema‐related symptoms, no differences were found between the two interventions except for pain, a variable that experienced a greater improvement with the Kinesio taping therapy. The benefits of Kinesio taping on pain could result from the effect of lifting the skin, which creates convolutions that enlarge the dermis area and inhibits the free nerve endings (Pekyavaş et al., 2014; Tsai et al., 2009). However, despite not finding intergroup differences for the remainder of the assessed symptoms, all of them improved in the Kinesio taping group compared to baseline. These results are in agreement with previous studies (Pajero Otero et al., 2019; Pekyavaş et al., 2014; Torres‐Lacomba et al., 2020). Adverse effects were mainly related to skin problems and comparable to those reported in other trials (Gatt et al., 2017; Pajero Otero et al., 2019). They can be considered as light adverse effects, even when skin peeling, which affected the arm with lymphedema of 9.5% of participants, can imply a risk for infection (Asdourian et al., 2016).
Among the limitations of this study is the lack of participants with sub‐clinical lymphedema or at stage I, as well as the low adherence to multilayer bandaging. These factors can result in an underestimation of the intervention outcomes since other trials with higher adherence and patients at stage I obtained better results. Additionally, there was no follow‐up after the therapies ended. The isolated application of Kinesio taping may have reduced the effectiveness of the intervention by not being complemented by the other components of CPT. Additionally, the use of a non‐validated verbal scale for the assessment of symptoms related to BCRL may have introduced a measurement bias. Finally, a cost‐analysis was not conducted, which can aid in determining the choice between treatments. Further multicentric clinical trials with specific protocols for the employed therapies and the inclusion of a cost‐effectiveness calculation are required to help decide between multilayer bandaging and Kinesio taping depending on the degree and treatment phase of the breast cancer‐related lymphedema.
5. CONCLUSIONS
Neither Kinesio taping nor CPT combined with IPC achieved statistically significant changes in the lymphedema volume, symptoms and motion ranges of arm joints. Participants stated a higher satisfaction with Kinesio taping versus multilayer bandaging as measured via SQ‐TTD‐BCRL. The functionality of the upper limb further improved using Kinesio taping versus CPT combined with IPC as reported in the DASH questionnaire.
CONFLICT OF INTEREST
All the authors declare no competing interests.
Supporting information
Table S1. CONSORT Checklist of Items for Reporting Trials of Nonpharmacologic Treatments
ACKNOWLEDGEMENTS
We would like to thank the Rehabilitation Service of Hospital 12 de Octubre for their valuable contribution to this project. We would also like to acknowledge the retired physiotherapists who dedicated their time altruistically as external evaluators (Sobrado Lozano MP, Ananín Fernández MO and Moreno Poveda D), the students of Clinical Internship from the Complutense University of Madrid for helping in the executive organisation of the trial and the Instituto de Investigación i+12 of Hospital 12 de Octubre.
Pajero Otero, V. , García Delgado, E. , Martín Cortijo, C. , Rodríguez Ramos, M. L. , De Carlos Iriarte, E. , Gil García, A. , Romay‐Barrero, H. , & Avendaño‐Coy, J. (2022). Intensive complex physical therapy combined with intermittent pneumatic compression versus Kinesio taping for treating breast cancer‐related lymphedema of the upper limb: A randomised cross‐over clinical trial. European Journal of Cancer Care, 31(5), e13625. 10.1111/ecc.13625
Funding information This trial has been financed by the Instituto de Investigación i+12 via a call for the intensification of research activity granted to the main author Pajero Otero V. The materials employed were supplied by Hospital Universitario 12 de Octubre.
Funding information Instituto de Investigación i+12
DATA AVAILABILITY STATEMENT
The anonymised data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Ancukiewicz, M. , Miller, C. L. , Skolny, M. N. , O'Toole, J. , Warren, L. E. , Jammallo, L. S. , Specht, M. C. , & Taghian, A. G. (2012). Comparison of relative versus absolute arm size change as criteria for quantifying breast cancer‐related lymphedema: The flaws in current studies and need for universal methodology. Breast Cancer Research and Treatment, 135(1), 145–152. 10.1007/s10549-012-2111-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asdourian, M. S. , Skolny, M. N. , Brunelle, C. , Seward, C. E. , Salama, L. , & Taghian, A. G. (2016). Precautions for breast cancer‐related lymphoedema: Risk from air travel, ipsilateral arm blood pressure measurements, skin puncture, extreme temperatures, and cellulitis. The Lancet Oncology, 17(9), e392–e405. 10.1016/S1470-2045(16)30204-2 [DOI] [PubMed] [Google Scholar]
- Bosman, J. (2014). Lymphtaping for lymphoedema: An overview of the treatment and its uses. British Journal of Community Nursing, 19, S12–S18. 10.12968/bjcn.2014.19.Sup4.S12 [DOI] [PubMed] [Google Scholar]
- Burkhardt, M. , Belzner, M. , Berg, A. , & Fleischer, S. (2014). Living with breast cancer‐related lymphedema: A synthesis of qualitative research. Oncology Nursing Forum, 41(4), E220–E237. 10.1188/14.ONF.E220-E237 [DOI] [PubMed] [Google Scholar]
- Cemal, Y. , Pusic, A. , & Mehrara, B. J. (2011). Preventative measures for lymphedema: Separating fact from fiction. Journal of the American College of Surgeons, 213(4), 543–551. 10.1016/j.jamcollsurg.2011.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conejo Tirado, I. , & Súarez Arcos, M. (2012). Comparación entre la Terapia Compresiva y el Vendaje Neuromuscular en el tratamiento del Linfedema Postmastectomía. Noticias de Vendaje Neuromuscular, 8, 12–13. [Google Scholar]
- Czerniec, S. A. , Ward, L. C. , & Kilbreath, S. L. (2016). Breast cancer‐related arm lymphedema: Fluctuation over six months and the effect of the weather. Lymphatic Research and Biology, 14(3), 148–155. 10.1089/lrb.2015.0030 [DOI] [PubMed] [Google Scholar]
- Dawes, D. J. , Meterissian, S. , Goldberg, M. , & Mayo, N. E. (2008). Impact of lymphoedema on arm function and health‐related quality of life in women following breast cancer surgery. Journal of Rehabilitation Medicine, 40(8), 651–658. 10.2340/16501977-0232 [DOI] [PubMed] [Google Scholar]
- Deltombe, T. , Jamart, J. , Recloux, S. , Legrand, C. , Vandenbroeck, N. , Theys, S. , & Hanson, P. (2007). Reliability and limits of agreement of circumferential, water displacement, and optoelectronic volumetry in the measurement of upper limb lymphedema. Lymphology, 40, 26–34. [PubMed] [Google Scholar]
- Ergin, G. , Şahinoğlu, E. , Karadibak, D. , & Yavuzşen, T. (2018). Effect of bandage compliance on upper extremity volume in patients with breast cancer‐related lymphedema. Lymphatic Research and Biology, 16(6), 553–558. 10.1089/lrb.2017.0060 [DOI] [PubMed] [Google Scholar]
- Ezzo, J. , Manheimer, E. , McNeely, M. L. , Howell, D. M. , Weiss, R. , Johansson, K. I. , Bao, T. , Bily, L. , Tuppo, C. M. , Williams, A. F. , & Karadibak, D. (2015). Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database of Systematic Reviews, 5(5), 1–73. 10.1002/14651858.CD003475.pub2.Manual [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman, J. L. , Stout, N. L. , Wanchai, A. , Stewart, B. R. , Cormier, J. N. , & Armer, J. M. (2012). Intermittent pneumatic compression therapy: A systematic review. Lymphology, 45(1), 13–25. [PubMed] [Google Scholar]
- Finnane, A. , Janda, M. , & Hayes, S. C. (2015). Review of the evidence of lymphedema treatment effect. American Journal of Physical Medicine & Rehabilitation/Association of Academic Physiatrists, 94(6), 483–498. 10.1097/PHM.0000000000000246 [DOI] [PubMed] [Google Scholar]
- Forner‐Cordero, I. , Muñoz‐Langa, J. , Forner‐Cordero, A. , & Demiguel‐Jimeno, J. M. (2010). Predictive factors of response to decongestive therapy in patients with breast‐cancer‐related lymphedema. Annals of Surgical Oncology, 17(3), 744–751. 10.1245/s10434-009-0778-9 [DOI] [PubMed] [Google Scholar]
- Franchignoni, F. , Vercelli, S. , Giordano, A. , Sartorio, F. , Bravini, E. , & Ferriero, G. (2014). Minimal clinically important difference of the Disabilities of the Arm, Shoulder and Hand outcome measure (DASH) and its shortened version (QuickDASH). Journal of Orthopaedic and Sports Physical Therapy, 44(1), 30–39. 10.2519/jospt.2014.4893 [DOI] [PubMed] [Google Scholar]
- Fu, M. R. (2014). Breast cancer‐related lymphedema: Symptoms, diagnosis, risk reduction, and management. World Journal of Clinical Oncology, 5(3), 241–247. 10.5306/wjco.v5.i3.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatt, M. , Willis, S. , & Leuschner, S. (2017). A meta‐analysis of the effectiveness and safety of kinesiology taping in the management of cancer‐related lymphoedema. European Journal of Cancer Care, 26(5), 1–15. 10.1111/ecc.12510 [DOI] [PubMed] [Google Scholar]
- Gordon, S. , Sheppard, L. , & Selby, A. (2009). BCRL questionnaires: Climate and indigenous groups. Journal of Lymphoedema, 4(2), 44–51. Retrieved from http://ezp.slu.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2010510800&site=ehost-live [Google Scholar]
- Harrington, S. , Michener, L. A. , Kendig, T. , Miale, S. , & George, S. Z. (2014). Patient‐reported upper extremity outcome measures used in breast cancer survivors: A systematic review. Archives of Physical Medicine and Rehabilitation, 95(1), 153–162. 10.1016/j.apmr.2013.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasawara, K. , Mapa, J. M. R. , Ferreira, V. , Added, M. A. N. , Shiwa, S. Jr. , Carvas, N. Jr. , & Batista, P. A. (2018). Effects of Kinesio Taping on breast cancer‐related lymphedema: A meta‐analysis in clinical trials. Physiotherapy Theory and Practice, 34(5), 337–345. 10.1080/09593985.2017.1419522 [DOI] [PubMed] [Google Scholar]
- López Martín, M. , Valencia Álvarez, F. J. , González González, R. , Rodríguez Salvanés, F. J. , Crespo Cobo, P. , & Hernández García, M. A. (2011). Validación de herramienta informática para el cálculo de linfedema en pacientes con afectación unilateral de extremidad superior. Rehabilitación, 45(2), 127–133. 10.1016/j.rh.2011.03.008 [DOI] [Google Scholar]
- Malicka, I. , Rosseger, A. , Hanuszkiewicz, J. , & Woźniewski, M. (2014). Kinesiology Taping reduces lymphedema of the upper extremity in women after breast cancer treatment: A pilot study. Przeglad Menopauzalny = Menopause Review, 13(4), 221–226. 10.5114/pm.2014.44997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melgaard, D. (2016). What is the effect of treating secondary lymphedema after breast cancer with complete decongestive physiotherapy when the bandage is replaced with Kinesio Textape?—A pilot study. Physiotherapy Theory and Practice, 32(6), 446–451. 10.3109/09593985.2016.1143541 [DOI] [PubMed] [Google Scholar]
- Pajero Otero, V. , García Delgado, E. , Martín Cortijo, C. , Romay Barrero, H. M. , de Carlos Iriarte, E. , Avendaño‐Coy, J. , & Avendaño‐Coy, J. (2019). Kinesio taping versus compression garments for treating breast cancer‐related lymphedema: A randomized, cross‐over, controlled trial. Clinical Rehabilitation, 33(12), 1887–1897. 10.1177/0269215519874107 [DOI] [PubMed] [Google Scholar]
- Pajero Otero, V. , García Delgado, E. , Martín Cortijo, C. , Toribio Rubio, V. , Guijarro Cano, M. J. , Calvo Bóveda, C. , Martín‐Arriscado Arroba, C. , & Avendaño Coy, J. (2021). Development and evaluation of a satisfaction questionnaire about therapeutic textile devices used for breast cancer‐related lymphedema. Lymphatic Research and Biology, 20(2), 203–212. 10.1089/lrb.2020.0013 [DOI] [PubMed] [Google Scholar]
- Pekyavaş, N. Ö. , Tunay, V. B. , Akbayrak, T. , Kaya, S. , & Karataş, M. (2014). Complex decongestive therapy and taping for patients with postmastectomy lymphedema: A randomized controlled study. European Journal of Oncology Nursing, 18(6), 585–590. 10.1016/j.ejon.2014.06.010 [DOI] [PubMed] [Google Scholar]
- Poage, E. , Singer, M. , Armer, J. , Poundall, M. , & Shellabarger, M. J. (2008). Demystifying lymphedema: Development of the lymphedema Putting Evidence Into Practice Card. Clinical Journal of Oncology Nursing, 12(6), 951–964. 10.1188/08.CJON.951-964 [DOI] [PubMed] [Google Scholar]
- Puentes‐Gutierrez, A. B. (2015). Aplicabilidad del cuestionario DASH en mujeres con linfedema secundario a tratamiento de cáncer de mama. Universidad de Castilla‐La Mancha. Retrieved from https://ruidera.uclm.es/xmlui/bitstream/handle/10578/8931/TESISPuentesGuti%E9rrez.pdf?sequence=1&isAllowed=y [DOI] [PubMed] [Google Scholar]
- Rasmussen, G. H. F. , Kristiansen, M. , Arroyo‐Morales, M. , Voigt, M. , & Madeleine, P. (2020). Absolute and relative reliability of pain sensitivity and functional outcomes of the affected shoulder among women with pain after breast cancer treatment. PLoS ONE, 15(6), 1–16. 10.1371/journal.pone.0234118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosales, R. S. , Delgado, E. B. , & De La Lastra‐Bosch, I. D. (2002). Evaluation of the Spanish version of the DASH and Carpal Tunnel Syndrome health‐related quality‐of‐life instruments: Cross‐cultural adaptation process and reliability. The Journal of Hand Surgery, 27(2), 334–343. 10.1053/jhsu.2002.30059 [DOI] [PubMed] [Google Scholar]
- Schaverien, M. , Moeller, J. , & Cleveland, S. (2018). Non‐operative treatment of lymphedema. Seminars in Plastic Surgery, 32, 17–21. 10.1055/s-0038-1635119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sijmonsma, J. (2010). Lymph Taping. Fysionair. [Google Scholar]
- Smykla, A. , Walewicz, K. , Trybulski, R. , Halski, T. , Kucharzewski, M. , Kucio, C. , & Taradaj, J. (2013). Effect of Kinesiology Taping on breast cancer‐related lymphedema: A randomized single‐blind controlled pilot study. BioMed Research International, 2013, 767106. 10.1155/2013/767106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szolnoky, G. , Lakatos, B. , Keskeny, T. , Varga, E. , Varga, M. , Dobozy, A. , & Kemeny, L. (2013). Intermittent pneumatic compression acts synergistically with manual lymphatic drainage in complex decongestive physiotherapy for breast cancer treatment‐related lymphedema. Lymphology, 42(4), 188–194. Retrieved from https://journals.uair.arizona.edu/index.php/lymph/article/view/17076 [PubMed] [Google Scholar]
- Szuba, A. , Achalu, R. , & Rockson, S. G. (2002). Decongestive lymphatic therapy for patients with breast carcinoma‐associated lymphedema: A randomized, prospective study of a role for adjunctive intermittent pneumatic compression. Cancer, 95(11), 2260–2267. 10.1002/cncr.10976 [DOI] [PubMed] [Google Scholar]
- Tantawy, S. A. , Abdelbasset, W. K. , Nambi, G. , & Kamel, D. M. (2019). Comparative study between the effects of Kinesio taping and pressure garment on secondary upper extremity lymphedema and quality of life following mastectomy: A randomized controlled trial. Integrative Cancer Therapies, 18, 153473541984727. 10.1177/1534735419847276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taradaj, J. , Halski, T. , Rosinczuk, J. , Dymarek, R. , Laurowski, A. , & Smykla, A. (2016). The influence of Kinesiology Taping on the volume of lymphoedema and manual dexterity of the upper limb in women after breast cancer treatment. European Journal of Cancer Care, 25(4), 647–660. 10.1111/ecc.12331 [DOI] [PubMed] [Google Scholar]
- Taylor, R. , Jayasinghe, U. W. , Koelmeyer, L. , Ung, O. , & Boyages, J. (2006). Reliability and validity of arm volume measurements for assessment of lymphedema. Physical Therapy, 86(2), 205–214. 10.1093/ptj/86.2.205 [DOI] [PubMed] [Google Scholar]
- Torres‐Lacomba, M. , Navarro‐Brazález, B. , Prieto‐Gómez, V. , Ferrandez, J. C. , Bouchet, J. Y. , & Romay‐Barrero, H. (2020). Effectiveness of four types of bandages and kinesio‐tape for treating breast‐cancer‐related lymphoedema: A randomized, single‐blind, clinical trial. Clinical Rehabilitation, 34(9), 1230–1241. 10.1177/0269215520935943 [DOI] [PubMed] [Google Scholar]
- Tsai, H. J. , Hung, H. C. , Yang, J. L. , Huang, C. S. , & Tsauo, J. Y. (2009). Could Kinesio tape replace the bandage in decongestive lymphatic therapy for breast‐cancer‐related lymphedema? A pilot study. Supportive Care in Cancer, 17(11), 1353–1360. 10.1007/s00520-009-0592-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. CONSORT Checklist of Items for Reporting Trials of Nonpharmacologic Treatments
Data Availability Statement
The anonymised data that support the findings of this study are available from the corresponding author upon reasonable request.


