Abstract
A male predominance was observed in esophageal and gastric cancers, though present limited data has revealed variations by age. We aim to investigate the global age‐specific sex differences in esophageal squamous cell carcinoma (ESCC), esophageal adenocarcinoma (EAC), gastric cardia cancer (GCC) and gastric noncardia cancer (GNCC). Data on esophageal and gastric cancers incidence by diagnosis year, sex, histology, subsite and age group were extracted from 171 registries in 54 countries included in the last two volumes (X and XI, 2003‐2012) of Cancer Incidence in Five Continents, which contributing to over 80% of the global burdens of these cancers. Age‐standardized incidence rates (ASIRs) and male‐to‐female ASIRs ratios were estimated for esophageal and gastric cancers, by histological subtype and subsite, globally and by country. We consistently observed a male predominance in esophageal and gastric cancers across the world from 2003 to 2012, with male‐to‐female ASIRs ratios of 6.7:1 for EAC, 3.3:1 for ESCC, 4.0:1 for GCC and 2.1:1 for GNCC. The sex differences were consistent across time periods but varied significantly by age across the life span. Across the four cancer types, the male‐to‐female incidence rate ratios increased from young ages, approaching a peak at ages 60‐64, but sharply declined thereafter. Similar “low‐high‐low” trends of age‐specific sex ratio were observed in other digestive cancers including liver, pancreas, colon and rectum with peak ages ranging from 50 to 65. Age‐dependent risk factors warrant further investigation to aid our understanding of the underlying etiologies of esophageal and gastric cancers by histological subtype and subsite.
Keywords: esophageal adenocarcinoma, esophageal squamous cell carcinoma, gastric cardia cancer, gastric noncardia cancer, male‐to‐female age‐standardized incidence rates ratio
What's new?
Marked differences exist between men and women in the incidence of esophageal and gastric cancers. These disparities, however, are not explained solely by variances between the sexes in the distribution of major risk factors, suggesting that other factors are involved. Here, investigation of esophageal and gastric cancer incidence in 54 countries worldwide reveals consistent male predominance in the incidence of these malignancies. The ratio of male‐to‐female incidence increased through life, peaking at ages 60‐64 and declining thereafter. The findings warrant further investigation to identify mechanisms underlying age‐related changes in risk and possible shared etiologies of esophageal and gastric cancers.
Abbreviations
- ASIRs
age‐standardized incidence rates
- CI5
Cancer Incidence in Five Continents
- CIs
confidence intervals
- EAC
esophageal adenocarcinoma
- EC
esophageal cancer
- ESCC
esophageal squamous cell carcinoma
- GC
gastric cancer
- GCC
gastric cardia cancer
- GNCC
gastric noncardia cancer
- H. pylori
Helicobacter pylori
- SEER
Surveillance, Epidemiology, and End Results
1. INTRODUCTION
Gastric cancer (GC) and esophageal cancer (EC) rank as the fifth and seventh most common cancer sites worldwide in 2020. 1 Striking sex differences in esophageal cancer and gastric cancer are well‐described and have been attributed to differences in the distributions of major risk factors between the sexes. 2 , 3 , 4 , 5 These include smoking, alcohol drinking and family history, as well as subtype‐specific factors, including gastroesophageal reflux diseases and Helicobacter pylori (H. pylori). 2 , 3 , 4 More recent research has however shown that these determinants cannot fully explain the sex‐specific differences. 5 , 6 , 7
Moreover, accruing evidence has shown that the gender differences in gastrointestinal cancers varied by age and major histological subtypes and subsites, 6 , 8 , 9 including esophageal adenocarcinoma (EAC), esophageal squamous cell carcinoma (ESCC), gastric cardia cancer (GCC) and gastric noncardia cancer (GNCC). 1 , 8 , 10 , 11 Previous results reported the highest male‐to‐female incidence ratio of up to 10:1 in EAC, 8 and the lowest ratio of 1.6:1 in GNCC, 11 though these studies were limited to specific regions or countries. 8 , 11 , 12 In addition, studies showed different changing patterns of sex differences with age by subtype, with a declining trend of the male‐to‐female incidence ratio of EAC with age, but a “low‐high‐low” pattern of sex ratio curve for GCC with age. 8 , 13
Over the past decades, the global cancer burden and profiles of various risk factors have evolved with rapid economic development. 1 For gastrointestinal cancers, it is important to better understand the sex‐specific variations in esophageal and gastric cancers and how they change over time. It is also informative to illustrate the changing patterns of the sex differences by age to generate hypotheses for future etiological studies, given age is a vital indicator highly relevant to economy, life span and various known or putative risk factors (eg, reproductive and hormonal factors).
This global study aims to assess the long‐term changing patterns of age‐ and sex‐specific differences in esophageal cancer and gastric cancer, by pathological subtype and anatomic subsite. Using the detailed information available in the Cancer Incidence in Five Continents (CI5) from 2003 to 2012, we investigate the population‐based male‐to‐female incidence rates ratios of esophageal and gastric cancers by subtype, sex and 5‐year age group, in selected countries. The identified patterns in our study seek to aid our understanding of the underlying etiological mechanisms of sex differences in these two common cancers, and inform future cancer prevention and control studies.
2. MATERIALS AND METHODS
2.1. Data source
We extracted EC and GC incidence and population data from the CI5 website, which contains incidence data from cancer registries worldwide of high quality. 14 , 15 The last two volumes from X to XI were used, containing detailed data for new cases diagnosed from 2003 to 2012 by morphology, subsite, sex and 5‐year age group. EC and GC were evaluated overall and by subtype and subsite, including EAC, ESCC, GCC and GNCC. We also extracted data from CI5 X to XI for other digestive cancers including liver, colon, rectum and pancreas, to compare the age‐specific sex differences among different gastrointestinal cancer sites. 14 , 15
There were 171 population‐based cancer registries from 54 countries reporting 10 consecutive years of data from 2003 to 2012. We used data from the National Program of Cancer Registries to estimate the burdens in the United States to reach a higher coverage of the population‐based cancer registry. Multiple subnational cancer registries in the same countries were aggregated to obtain a national proxy of cancer risk. For the EC analysis, we further excluded nine registries which recorded less than five EAC or ESCC cases in each volume, and four registries with more than 75% of EC cases assigned unspecified histology. Finally, a total of 158 out of 171 registries were included covering 53 countries (Table S1), which contributed to 83.49% of the global EC burden. 16 We further imputed EC cases which were reported as unspecified type into EAC, ESCC or other histological types according to the proportion of each type by sex and 5‐year age group in the available reported morphological category. The subsites of GC were defined according to the International Classification of Diseases, 10th Revision as follows: GCC (C16.0) and GNCC (C16.1‐9), whereby cancers with overlapping (C16.8) or undefined (C16.9) topography were considered GNCC according to evidence from the clinical observations along with previous results. 17 We additionally excluded one registry which reported less than five GCC or GNCC cases in each volume and 27 registries with more than 85% of GC cases assigned unspecified histology (C16.5‐9), hence, a total of 143 out of 171 registries were included in the GC analysis, corresponding to 43 countries covering 81.56% of the global GC burden 16 (Table S1). We further extracted 10 consecutive years of GC data from 2003 to 2012 from 18 registries from Surveillance, Epidemiology, and End Results (SEER) in the United States and 22 registries from Chinese National Central Cancer Registry which covered 3.34% (44.4 million) of the Chinese population. 18 , 19 GCC and GNCC was classified into one of four types: intestinal, diffuse, mixed carcinomas, or indeterminate, according to the Laurén classification, which has proven useful in evaluating the natural history of GC, especially with regard to its association with environmental factors. The age‐specific trends in incidence rates of intestinal type and diffuse type of GCC and GNCC in the United States and China were analyzed by sex.
2.2. Statistical analyses
According to the CI5 volumes, we assessed cancer incidence data overall and by two time periods: 2003‐2007, 2008‐2012. Cancer cases were grouped into 5‐year age groups to calculate age‐specific rates, beginning from 20 to 24 and ending with 85 years onward. Due to the small number of young cases, the age groups below 20 years were not included. For the different age groups, incidence rates by time period were calculated by dividing the number of incident cancer cases in each period by the male or female population in each period, as appropriate. The global and national age‐standardized incidence rates (ASIRs) and the 95% confidence intervals (CIs) of EC and GC were calculated using the direct method with the Segi's World Standard Population as the reference, by sex, cancer subtype or subsite and time period. Moreover, the global and national male‐to‐female incidence rates ratios of EC and GC were calculated, overall and by histological subtype and subsite, and subsequently derived for the corresponding age groups. The 95% CIs were estimated assuming the count data had a Poisson distribution. Analyses were performed with SAS, version 9.4, software (SAS Institute, Cary, NC).
3. RESULTS
Table 1 presents the global and national estimations of the male‐to‐female ASIRs ratios for esophageal cancer and gastric cancer, overall and by cancer subtype and subsite. We observed a significant international male predominance of EC and GC with a male‐to‐female ASIRs ratio of 6.7:1 for EAC and 3.3:1 for ESCC from 2003 to 2012. The male‐to‐female ASIRs ratio was lower in GC compared to that of EC, with a stable ratio of 4.0:1 for GCC and 2.1:1 for GNCC. Similar patterns of sex differences were found for different subtypes and subsites of EC and GC across the world, yet some variations existed by country. In Republic of Korea and a belt of Baltic/European countries, including Belarus, Ukraine, Slovakia, Lithuania, Latvia, Estonia, we observed extremely high sex ratio exceeding 10:1 for ESCC, but not for EAC or GC. In contrast, comparable rates of ESCC and EAC were found in the United Kingdom, Ireland, New Zealand and some Western Asian countries, including Saudi Arabia, Turkey and Israel. The estimations of the international ASIRs for EAC, ESCC, GCC and GNCC from 2003 to 2012 by sex, age group and country are shown in Tables S2 and S3.
TABLE 1.
Global and national estimations of male‐to‐female age‐standardized incidence rate ratios and 95% CIs for esophageal cancer and gastric cancer, overall and by subtype and subsite (2003‐2012) a
| World region | Population | Time period | Male‐to‐female age‐standardized incidence rate ratios (95% CIs) | |||||
|---|---|---|---|---|---|---|---|---|
| Esophageal cancer | ESCC | EAC | Gastric cancer | GCC | GNCC | |||
| Global | Total | 2003‐2012 | 4.28 (4.25, 4.31) | 3.27 (3.24, 3.30) | 6.68 (6.61, 6.76) | 2.23 (2.22, 2.24) | 3.99 (3.94, 4.03) | 2.05 (2.04, 2.05) |
| 2003‐2007 | 4.24 (4.20, 4.28) | 3.30 (3.26, 3.34) | 6.62 (6.51, 6.73) | 2.22 (2.21, 2.23) | 3.94 (3.88, 4.00) | 2.04 (2.03, 2.05) | ||
| 2008‐2012 | 4.31 (4.27, 4.35) | 3.25 (3.21, 3.29) | 6.74 (6.63, 6.84) | 2.24 (2.23, 2.25) | 4.03 (3.97, 4.09) | 2.05 (2.04, 2.06) | ||
| Northern America | Canada | 2003‐2012 | 3.84 (3.69, 4.00) | 1.90 (1.79, 2.02) | 6.82 (6.41, 7.26) | 2.17 (2.11, 2.24) | 4.23 (3.99, 4.48) | 1.67 (1.62, 1.73) |
| 2003‐2007 | 3.67 (3.46, 3.89) | 1.89 (1.74, 2.06) | 6.73 (6.13, 7.39) | 2.29 (2.20, 2.38) | 4.68 (4.28, 5.11) | 1.77 (1.69, 1.85) | ||
| 2008‐2012 | 3.99 (3.77, 4.21) | 1.91 (1.75, 2.07) | 6.87 (6.33, 7.46) | 2.07 (1.99, 2.16) | 3.89 (3.60, 4.21) | 1.59 (1.52, 1.66) | ||
| United States | 2003‐2012 | 4.70 (4.64, 4.76) | 2.34 (2.30, 2.39) | 7.87 (7.73, 8.02) | 2.01 (2.00, 2.03) | 4.48 (4.39, 4.57) | 1.50 (1.48, 1.51) | |
| 2003‐2007 | 4.61 (4.52, 4.69) | 2.35 (2.29, 2.42) | 7.82 (7.61, 8.03) | 2.04 (2.01, 2.06) | 4.48 (4.36, 4.62) | 1.54 (1.51, 1.56) | ||
| 2008‐2012 | 4.79 (4.71, 4.87) | 2.33 (2.27, 2.39) | 7.92 (7.72, 8.12) | 2.00 (1.97, 2.02) | 4.47 (4.36, 4.59) | 1.46 (1.44, 1.48) | ||
| South America | Argentina | 2003‐2012 | 2.68 (2.40, 3.01) | 2.10 (1.83, 2.40) | 5.14 (4.11, 6.43) | 2.57 (2.33, 2.84) | 4.96 (3.27, 7.52) | 2.45 (2.22, 2.71) |
| 2003‐2007 | 2.79 (2.38, 3.27) | 2.44 (2.03, 2.94) | 4.11 (2.98, 5.68) | 2.59 (2.25, 2.98) | 6.33 (2.95, 13.56) | 2.47 (2.14, 2.86) | ||
| 2008‐2012 | 2.58 (2.19, 3.03) | 1.76 (1.45, 2.15) | 6.31 (4.62, 8.61) | 2.56 (2.23, 2.94) | 4.44 (2.70, 7.31) | 2.43 (2.10, 2.80) | ||
| Brazil | 2003‐2012 | 4.28 (3.54, 5.18) | 4.16 (3.42, 5.05) | 9.90 (3.23, 30.33) | 2.19 (1.99, 2.41) | 3.21 (2.27, 4.52) | 2.11 (1.91, 2.33) | |
| 2003‐2007 | 4.00 (3.09, 5.18) | 3.84 (2.97, 4.98) | – | 2.10 (1.84, 2.40) | 3.09 (1.92, 4.97) | 2.03 (1.76, 2.33) | ||
| 2008‐2012 | 4.85 (3.67, 6.43) | 4.66 (3.47, 6.25) | 10.38 (3.25, 33.19) | 2.26 (1.96, 2.59) | 2.95 (1.79, 4.86) | 2.20 (1.90, 2.55) | ||
| Chile | 2003‐2012 | 2.17 (1.86, 2.54) | 2.26 (1.91, 2.68) | 4.58 (2.81, 7.47) | 2.41 (2.21, 2.63) | 3.56 (2.61, 4.85) | 2.32 (2.12, 2.54) | |
| 2003‐2007 | 2.06 (1.67, 2.56) | 2.32 (1.83, 2.94) | 2.75 (1.52, 4.96) | 2.46 (2.17, 2.80) | 4.01 (2.54, 6.35) | 2.35 (2.06, 2.69) | ||
| 2008‐2012 | 2.18 (1.73, 2.74) | 2.04 (1.59, 2.60) | 4.87 (1.97, 12.06) | 2.68 (2.38, 3.02) | 3.68 (2.42, 5.60) | 2.59 (2.29, 2.93) | ||
| Colombia | 2003‐2012 | 2.05 (1.76, 2.38) | 1.55 (1.30, 1.87) | 4.09 (3.04, 5.50) | 1.88 (1.78, 1.99) | 3.79 (3.07, 4.69) | 1.78 (1.68, 1.88) | |
| 2003‐2007 | 2.15 (1.76, 2.63) | 1.67 (1.31, 2.12) | 4.53 (2.95, 6.95) | 1.92 (1.78, 2.08) | 3.42 (2.55, 4.60) | 1.84 (1.69, 1.99) | ||
| 2008‐2012 | 1.91 (1.53, 2.39) | 1.39 (1.05, 1.84) | 3.74 (2.47, 5.65) | 1.84 (1.70, 1.99) | 4.18 (3.09, 5.66) | 1.71 (1.58, 1.86) | ||
| Ecuador | 2003‐2012 | 2.87 (2.11, 3.91) | 3.20 (2.19, 4.67) | 3.38 (1.75, 6.53) | 1.44 (1.35, 1.54) | 2.42 (1.74, 3.38) | 1.41 (1.32, 1.51) | |
| 2003‐2007 | 3.54 (2.26, 5.53) | 4.64 (2.59, 8.32) | 1.71 (0.77, 3.84) | 1.49 (1.36, 1.63) | 3.49 (2.03, 5.98) | 1.44 (1.32, 1.58) | ||
| 2008‐2012 | 2.16 (1.43, 3.26) | 2.03 (1.22, 3.37) | 6.21 (2.20, 17.51) | 1.43 (1.31, 1.57) | 2.08 (1.37, 3.15) | 1.40 (1.28, 1.54) | ||
| Eastern Asia | Republic of Korea | 2003‐2012 | 14.72 (14.03, 15.45) | 16.12 (15.31, 16.97) | 5.87 (4.97, 6.94) | 2.53 (2.51, 2.55) | 3.62 (3.47, 3.78) | 2.50 (2.48, 2.52) |
| 2003‐2007 | 15.00 (14.00, 16.08) | 16.57 (15.38, 17.86) | 5.42 (4.33, 6.77) | 2.54 (2.51, 2.57) | 3.43 (3.22, 3.66) | 2.51 (2.48, 2.54) | ||
| 2008‐2012 | 14.49 (13.56, 15.48) | 15.73 (14.66, 16.88) | 6.59 (5.13, 8.47) | 2.52 (2.50, 2.55) | 3.77 (3.56, 4.00) | 2.48 (2.46, 2.51) | ||
| China | 2003‐2012 | 2.57 (2.51, 2.63) | 2.54 (2.48, 2.61) | 3.10 (2.80, 3.42) | 2.03 (2.00, 2.06) | 3.11 (2.99, 3.24) | 1.89 (1.86, 1.92) | |
| 2003‐2007 | 2.53 (2.44, 2.61) | 2.49 (2.41, 2.58) | 3.53 (3.01, 4.15) | 2.03 (1.99, 2.07) | 3.06 (2.89, 3.24) | 1.89 (1.85, 1.94) | ||
| 2008‐2012 | 2.60 (2.52, 2.69) | 2.59 (2.50, 2.69) | 2.79 (2.46, 3.17) | 2.02 (1.98, 2.06) | 3.15 (2.97, 3.33) | 1.88 (1.84, 1.92) | ||
| Japan | 2003‐2012 | 6.37 (6.18, 6.57) | 6.38 (6.18, 6.58) | 7.72 (6.74, 8.84) | 2.71 (2.69, 2.74) | 3.85 (3.69, 4.02) | 2.66 (2.63, 2.68) | |
| 2003‐2007 | 6.74 (6.42, 7.07) | 6.89 (6.55, 7.25) | 6.56 (5.32, 8.09) | 2.65 (2.61, 2.69) | 3.59 (3.35, 3.85) | 2.60 (2.56, 2.64) | ||
| 2008‐2012 | 6.11 (5.87, 6.36) | 6.03 (5.79, 6.29) | 8.67 (7.26, 10.35) | 2.76 (2.73, 2.80) | 4.06 (3.84, 4.29) | 2.69 (2.66, 2.73) | ||
| South‐Eastern Asia | Thailand | 2003‐2012 | 6.72 (6.05, 7.46) | 7.32 (6.53, 8.19) | 4.50 (3.08, 6.57) | 1.59 (1.42, 1.78) | 1.89 (1.31, 2.73) | 1.56 (1.39, 1.76) |
| 2003‐2007 | 6.13 (5.32, 7.07) | 6.74 (5.77, 7.88) | 4.55 (2.73, 7.59) | 1.58 (1.35, 1.86) | 1.49 (0.85, 2.62) | 1.59 (1.34, 1.89) | ||
| 2008‐2012 | 7.45 (6.38, 8.69) | 7.98 (6.76, 9.41) | 4.48 (2.54, 7.89) | 1.57 (1.35, 1.83) | 2.24 (1.38, 3.63) | 1.50 (1.28, 1.77) | ||
| South‐Central Asia | India | 2003‐2012 | 1.55 (1.49, 1.61) | 1.50 (1.44, 1.56) | 2.87 (2.40, 3.43) | 1.96 (1.86, 2.06) | 2.52 (2.14, 2.97) | 1.90 (1.81, 2.01) |
| 2003‐2007 | 1.52 (1.43, 1.61) | 1.49 (1.41, 1.58) | 2.04 (1.53, 2.71) | 1.96 (1.82, 2.11) | 2.30 (1.76, 3.00) | 1.94 (1.79, 2.09) | ||
| 2008‐2012 | 1.58 (1.50, 1.66) | 1.50 (1.43, 1.58) | 3.50 (2.77, 4.42) | 1.95 (1.82, 2.08) | 2.67 (2.17, 3.29) | 1.87 (1.74, 2.01) | ||
| Western Asia | Saudi Arabia | 2003‐2012 | 1.26 (1.00, 1.59) | 0.99 (0.76, 1.30) | 2.44 (1.52, 3.94) | 1.83 (1.58, 2.13) | 3.24 (2.23, 4.71) | 1.60 (1.35, 1.88) |
| 2003‐2007 | 1.34 (0.95, 1.90) | 1.10 (0.75, 1.62) | 3.15 (1.30, 7.62) | 1.98 (1.57, 2.49) | 2.74 (1.59, 4.72) | 1.84 (1.42, 2.37) | ||
| 2008‐2012 | 1.23 (0.90, 1.68) | 0.93 (0.63, 1.36) | 2.23 (1.26, 3.95) | 1.73 (1.42, 2.11) | 3.94 (2.35, 6.60) | 1.42 (1.14, 1.76) | ||
| Turkey | 2003‐2012 | 1.67 (1.49, 1.89) | 1.36 (1.19, 1.56) | 4.21 (3.07, 5.77) | 2.06 (1.97, 2.16) | 2.56 (2.26, 2.90) | 1.98 (1.89, 2.09) | |
| 2003‐2007 | 1.64 (1.38, 1.94) | 1.29 (1.07, 1.56) | 5.89 (3.33, 10.41) | 1.94 (1.81, 2.08) | 2.21 (1.81, 2.69) | 1.91 (1.77, 2.05) | ||
| 2008‐2012 | 1.65 (1.40, 1.94) | 1.36 (1.13, 1.64) | 3.57 (2.43, 5.25) | 2.12 (1.99, 2.26) | 2.74 (2.34, 3.21) | 2.02 (1.88, 2.16) | ||
| Israel | 2003‐2012 | 2.01 (1.79, 2.25) | 1.17 (1.00, 1.35) | 4.67 (3.81, 5.71) | 1.82 (1.74, 1.91) | 3.10 (2.75, 3.51) | 1.65 (1.56, 1.73) | |
| 2003‐2007 | 1.97 (1.69, 2.29) | 1.20 (0.98, 1.46) | 4.10 (3.17, 5.30) | 1.82 (1.70, 1.94) | 2.89 (2.44, 3.42) | 1.66 (1.55, 1.79) | ||
| 2008‐2012 | 2.10 (1.80, 2.45) | 1.15 (0.93, 1.41) | 5.51 (4.13, 7.35) | 1.81 (1.69, 1.93) | 3.38 (2.86, 4.00) | 1.60 (1.49, 1.72) | ||
| Cyprus | 2003‐2012 | 3.12 (1.98, 4.90) | 1.86 (1.06, 3.27) | 6.23 (2.63, 14.74) | 1.82 (1.57, 2.11) | 5.83 (3.34, 10.16) | 1.60 (1.37, 1.86) | |
| 2003‐2007 | 3.87 (1.91, 7.83) | 2.41 (0.92, 6.32) | 4.93 (1.63, 14.93) | 2.15 (1.70, 2.72) | 10.08 (3.09, 32.89) | 1.85 (1.45, 2.37) | ||
| 2008‐2012 | 2.64 (1.46, 4.78) | 1.56 (0.77, 3.17) | 8.67 (2.14, 35.12) | 1.60 (1.32, 1.94) | 4.26 (2.23, 8.13) | 1.42 (1.16, 1.74) | ||
| Eastern Europe | Belarus | 2003‐2012 | 18.00 (16.27, 19.92) | 20.77 (18.46, 23.36) | 9.38 (7.61, 11.56) | 2.41 (2.36, 2.47) | 3.60 (3.28, 3.96) | 2.35 (2.30, 2.41) |
| 2003‐2007 | 17.11 (14.84, 19.74) | 20.85 (17.58, 24.73) | 7.67 (5.80, 10.14) | 2.42 (2.34, 2.49) | 3.67 (3.23, 4.18) | 2.35 (2.28, 2.43) | ||
| 2008‐2012 | 19.24 (16.67, 22.20) | 21.00 (17.85, 24.71) | 12.31 (8.96, 16.92) | 2.42 (2.34, 2.49) | 3.60 (3.13, 4.13) | 2.36 (2.28, 2.44) | ||
| Czech Republic | 2003‐2012 | 6.42 (5.98, 6.89) | 5.50 (5.03, 6.01) | 8.69 (7.70, 9.80) | 1.98 (1.92, 2.04) | 3.86 (3.51, 4.24) | 1.80 (1.74, 1.86) | |
| 2003‐2007 | 6.89 (6.20, 7.66) | 6.09 (5.33, 6.96) | 8.67 (7.23, 10.39) | 2.05 (1.96, 2.14) | 4.26 (3.73, 4.87) | 1.85 (1.76, 1.94) | ||
| 2008‐2012 | 6.05 (5.51, 6.65) | 5.06 (4.49, 5.70) | 8.60 (7.32, 10.10) | 1.90 (1.82, 1.99) | 3.48 (3.05, 3.98) | 1.75 (1.66, 1.83) | ||
| Poland | 2003‐2012 | 6.38 (5.72, 7.12) | 6.38 (5.66, 7.19) | 6.29 (4.71, 8.40) | 2.54 (2.43, 2.66) | 4.96 (4.25, 5.80) | 2.36 (2.25, 2.48) | |
| 2003‐2007 | 6.57 (5.61, 7.69) | 6.98 (5.87, 8.29) | 5.11 (3.42, 7.62) | 2.49 (2.34, 2.66) | 4.27 (3.41, 5.34) | 2.36 (2.21, 2.53) | ||
| 2008‐2012 | 6.13 (5.26, 7.15) | 5.84 (4.95, 6.89) | 7.59 (4.99, 11.55) | 2.56 (2.40, 2.73) | 5.66 (4.56, 7.03) | 2.33 (2.17, 2.49) | ||
| Slovakia | 2003‐2012 | 11.39 (9.98, 12.99) | 12.06 (10.41, 13.96) | 8.25 (6.04, 11.26) | 2.23 (2.13, 2.33) | 3.92 (3.38, 4.53) | 2.07 (1.98, 2.18) | |
| 2003‐2007 | 11.62 (9.81, 13.77) | 12.16 (10.07, 14.68) | 8.36 (5.59, 12.51) | 2.28 (2.15, 2.42) | 4.18 (3.48, 5.02) | 2.11 (1.98, 2.24) | ||
| 2008‐2012 | 11.04 (8.96, 13.60) | 11.83 (9.36, 14.96) | 8.28 (5.08, 13.50) | 2.15 (2.00, 2.32) | 3.50 (2.74, 4.48) | 2.03 (1.88, 2.20) | ||
| Bulgaria | 2003‐2012 | 5.75 (5.16, 6.41) | 5.50 (4.84, 6.25) | 6.81 (5.52, 8.40) | 2.19 (2.12, 2.26) | 3.14 (2.84, 3.48) | 2.10 (2.03, 2.17) | |
| 2003‐2007 | 5.82 (4.98, 6.79) | 5.81 (4.81, 7.02) | 5.58 (4.24, 7.34) | 2.20 (2.11, 2.30) | 3.41 (2.93, 3.97) | 2.11 (2.02, 2.20) | ||
| 2008‐2012 | 5.70 (4.89, 6.63) | 5.28 (4.43, 6.29) | 8.46 (6.09, 11.76) | 2.17 (2.07, 2.27) | 2.94 (2.57, 3.36) | 2.08 (1.98, 2.18) | ||
| Ukraine | 2003‐2012 | 12.80 (12.26, 13.37) | 15.70 (14.90, 16.54) | 6.51 (6.01, 7.06) | 2.40 (2.37, 2.43) | 3.50 (3.38, 3.63) | 2.30 (2.27, 2.32) | |
| 2003‐2007 | 12.53 (11.80, 13.30) | 16.11 (14.95, 17.35) | 6.15 (5.52, 6.84) | 2.38 (2.34, 2.42) | 3.39 (3.22, 3.56) | 2.29 (2.25, 2.32) | ||
| 2008‐2012 | 13.13 (12.34, 13.97) | 15.42 (14.33, 16.60) | 6.95 (6.16, 7.85) | 2.42 (2.38, 2.46) | 3.66 (3.47, 3.87) | 2.31 (2.27, 2.35) | ||
| Northern Europe | Iceland | 2003‐2012 | 4.29 (3.07, 5.99) | 1.95 (1.17, 3.23) | 7.64 (4.60, 12.70) | 1.59 (1.27, 1.99) | 3.79 (1.96, 7.33) | 1.39 (1.09, 1.77) |
| 2003‐2007 | 3.00 (1.86, 4.85) | 2.54 (1.32, 4.89) | 3.88 (1.81, 8.31) | 1.83 (1.35, 2.50) | 3.31 (1.38, 7.95) | 1.66 (1.20, 2.32) | ||
| 2008‐2012 | 5.92 (3.70, 9.47) | 1.37 (0.60, 3.08) | 12.54 (6.26, 25.10) | 1.38 (0.99, 1.92) | 4.55 (1.66, 12.45) | 1.16 (0.81, 1.66) | ||
| Ireland | 2003‐2012 | 2.33 (2.18, 2.49) | 1.19 (1.08, 1.31) | 4.83 (4.33, 5.38) | 2.11 (1.99, 2.24) | 3.00 (2.70, 3.34) | 1.81 (1.69, 1.94) | |
| 2003‐2007 | 2.34 (2.12, 2.58) | 1.22 (1.06, 1.40) | 4.78 (4.08, 5.59) | 2.10 (1.93, 2.29) | 2.82 (2.39, 3.33) | 1.89 (1.72, 2.09) | ||
| 2008‐2012 | 2.33 (2.12, 2.56) | 1.17 (1.02, 1.35) | 4.86 (4.18, 5.64) | 2.12 (1.95, 2.29) | 3.13 (2.72, 3.61) | 1.73 (1.57, 1.90) | ||
| Lithuania | 2003‐2012 | 9.80 (8.62, 11.15) | 10.77 (9.27, 12.52) | 6.20 (4.71, 8.16) | 2.37 (2.27, 2.47) | 4.70 (3.80, 5.83) | 2.30 (2.21, 2.40) | |
| 2003‐2007 | 10.73 (8.90, 12.95) | 11.32 (9.11, 14.07) | 8.60 (5.70, 12.96) | 2.48 (2.34, 2.62) | 4.48 (3.30, 6.10) | 2.42 (2.28, 2.56) | ||
| 2008‐2012 | 9.04 (7.57, 10.79) | 10.30 (8.36, 12.68) | 4.52 (3.10, 6.60) | 2.25 (2.12, 2.39) | 5.01 (3.72, 6.75) | 2.17 (2.04, 2.31) | ||
| Norway | 2003‐2012 | 3.50 (3.18, 3.85) | 2.25 (1.95, 2.59) | 5.42 (4.71, 6.23) | 1.89 (1.78, 2.00) | 3.75 (3.28, 4.27) | 1.54 (1.45, 1.64) | |
| 2003‐2007 | 3.58 (3.11, 4.12) | 2.29 (1.87, 2.81) | 5.99 (4.84, 7.40) | 1.85 (1.71, 2.00) | 3.63 (3.02, 4.36) | 1.52 (1.40, 1.66) | ||
| 2008‐2012 | 3.45 (3.02, 3.93) | 2.24 (1.84, 2.73) | 5.05 (4.19, 6.08) | 1.93 (1.78, 2.10) | 3.84 (3.18, 4.64) | 1.57 (1.44, 1.73) | ||
| Denmark | 2003‐2012 | 3.12 (2.92, 3.34) | 2.14 (1.95, 2.34) | 5.15 (4.63, 5.72) | 2.23 (2.11, 2.36) | 4.44 (4.03, 4.90) | 1.39 (1.30, 1.50) | |
| 2003‐2007 | 2.89 (2.62, 3.18) | 1.94 (1.70, 2.21) | 4.99 (4.28, 5.82) | 2.16 (2.00, 2.34) | 4.32 (3.75, 4.98) | 1.39 (1.26, 1.54) | ||
| 2008‐2012 | 3.33 (3.04, 3.64) | 2.32 (2.05, 2.63) | 5.26 (4.55, 6.07) | 2.30 (2.13, 2.49) | 4.56 (3.98, 5.21) | 1.39 (1.25, 1.54) | ||
| Estonia | 2003‐2012 | 8.29 (6.78, 10.14) | 8.52 (6.84, 10.61) | 7.78 (4.42, 13.71) | 2.07 (1.94, 2.21) | 3.74 (2.95, 4.72) | 1.97 (1.84, 2.10) | |
| 2003‐2007 | 7.97 (5.90, 10.75) | 8.06 (5.85, 11.12) | 6.71 (2.87, 15.72) | 1.96 (1.80, 2.15) | 3.19 (2.29, 4.44) | 1.88 (1.72, 2.07) | ||
| 2008‐2012 | 8.68 (6.62, 11.39) | 9.01 (6.67, 12.18) | 9.03 (4.23, 19.26) | 2.20 (2.01, 2.41) | 4.36 (3.12, 6.09) | 2.07 (1.88, 2.28) | ||
| Latvia | 2003‐2012 | 10.60 (8.81, 12.75) | 11.04 (9.00, 13.55) | 9.49 (5.92, 15.23) | 2.25 (2.12, 2.39) | 4.25 (3.08, 5.87) | 2.19 (2.06, 2.33) | |
| 2003‐2007 | 8.55 (6.76, 10.81) | 8.94 (6.92, 11.56) | 6.86 (3.75, 12.53) | 2.31 (2.13, 2.49) | 5.35 (3.45, 8.30) | 2.24 (2.07, 2.42) | ||
| 2008‐2012 | 14.37 (10.60, 19.47) | 14.96 (10.63, 21.06) | 15.68 (7.24, 33.94) | 2.15 (1.95, 2.37) | 3.20 (1.97, 5.19) | 2.11 (1.91, 2.34) | ||
| United Kingdom | 2003‐2012 | 2.71 (2.67, 2.75) | 1.14 (1.12, 1.17) | 5.06 (4.95, 5.17) | 2.39 (2.35, 2.42) | 4.00 (3.88, 4.13) | 1.96 (1.92, 1.99) | |
| 2003‐2007 | 2.62 (2.56, 2.68) | 1.15 (1.11, 1.19) | 5.00 (4.84, 5.15) | 2.42 (2.37, 2.47) | 3.88 (3.72, 4.05) | 2.03 (1.98, 2.07) | ||
| 2008‐2012 | 2.79 (2.73, 2.85) | 1.14 (1.10, 1.18) | 5.11 (4.96, 5.26) | 2.36 (2.31, 2.41) | 4.14 (3.96, 4.33) | 1.89 (1.85, 1.94) | ||
| Southern Europe | Malta | 2003‐2012 | 4.14 (2.90, 5.93) | 2.83 (1.74, 4.60) | 6.66 (3.69, 12.03) | 2.21 (1.84, 2.65) | 6.22 (3.57, 10.83) | 1.82 (1.50, 2.22) |
| 2003‐2007 | 3.80 (2.24, 6.46) | 1.72 (0.87, 3.39) | 10.99 (3.54, 34.08) | 2.06 (1.58, 2.69) | 6.99 (3.27, 14.92) | 1.58 (1.18, 2.12) | ||
| 2008‐2012 | 4.50 (2.77, 7.31) | 5.47 (2.63, 11.34) | 4.70 (2.33, 9.48) | 2.33 (1.81, 3.00) | 5.73 (2.54, 12.93) | 2.03 (1.55, 2.65) | ||
| Portugal | 2003‐2012 | – | – | – | 2.44 (2.02, 2.95) | 6.72 (3.13, 14.46) | 2.24 (1.84, 2.74) | |
| 2003‐2007 | – | – | – | 2.31 (1.79, 2.98) | 4.24 (1.70, 10.56) | 2.17 (1.66, 2.84) | ||
| 2008‐2012 | – | – | – | 2.62 (1.97, 3.48) | 21.61 (4.97, 93.96) | 2.34 (1.75, 3.14) | ||
| Italy | 2003‐2012 | 4.09 (3.87, 4.32) | 3.59 (3.37, 3.83) | 6.80 (6.08, 7.61) | 1.95 (1.91, 1.98) | 4.28 (4.00, 4.60) | 1.79 (1.76, 1.83) | |
| 2003‐2007 | 4.32 (3.99, 4.67) | 4.01 (3.65, 4.39) | 7.29 (6.15, 8.64) | 1.98 (1.92, 2.03) | 4.24 (3.83, 4.70) | 1.84 (1.78, 1.89) | ||
| 2008‐2012 | 3.88 (3.60, 4.18) | 3.22 (2.94, 3.52) | 6.47 (5.57, 7.52) | 1.92 (1.87, 1.97) | 4.32 (3.92, 4.76) | 1.75 (1.70, 1.81) | ||
| Slovenia | 2003‐2012 | 6.42 (5.41, 7.62) | 6.06 (5.01, 7.34) | 10.23 (6.61, 15.82) | 2.32 (2.19, 2.46) | 4.13 (3.45, 4.94) | 2.12 (1.99, 2.26) | |
| 2003‐2007 | 6.96 (5.45, 8.87) | 6.68 (5.11, 8.73) | 8.47 (4.63, 15.48) | 2.40 (2.20, 2.61) | 4.91 (3.77, 6.39) | 2.16 (1.97, 2.36) | ||
| 2008‐2012 | 5.91 (4.64, 7.53) | 5.49 (4.18, 7.20) | 12.91 (6.86, 24.31) | 2.25 (2.07, 2.45) | 3.52 (2.76, 4.50) | 2.09 (1.92, 2.29) | ||
| Spain | 2003‐2012 | 7.35 (6.80, 7.94) | 7.04 (6.41, 7.72) | 8.89 (7.68, 10.29) | 2.26 (2.19, 2.33) | 5.25 (4.74, 5.82) | 2.03 (1.96, 2.09) | |
| 2003‐2007 | 8.44 (7.56, 9.42) | 8.41 (7.36, 9.61) | 9.26 (7.53, 11.40) | 2.31 (2.22, 2.41) | 5.05 (4.37, 5.83) | 2.10 (2.01, 2.20) | ||
| 2008‐2012 | 6.37 (5.72, 7.10) | 5.85 (5.14, 6.66) | 8.49 (6.91, 10.44) | 2.20 (2.10, 2.30) | 5.47 (4.73, 6.33) | 1.94 (1.85, 2.04) | ||
| Western Europe | Belgium | 2003‐2012 | 3.76 (3.58, 3.95) | 2.70 (2.53, 2.87) | 7.04 (6.47, 7.66) | 2.22 (2.14, 2.30) | 5.04 (4.62, 5.50) | 1.74 (1.67, 1.81) |
| 2003‐2007 | 3.82 (3.55, 4.12) | 2.89 (2.62, 3.18) | 6.60 (5.82, 7.48) | 2.33 (2.20, 2.46) | 4.97 (4.33, 5.71) | 1.91 (1.80, 2.03) | ||
| 2008‐2012 | 3.71 (3.48, 3.96) | 2.56 (2.35, 2.78) | 7.39 (6.60, 8.27) | 2.15 (2.05, 2.26) | 5.08 (4.54, 5.68) | 1.61 (1.52, 1.70) | ||
| Switzerland | 2003‐2012 | 3.78 (3.47, 4.11) | 2.74 (2.47, 3.05) | 7.29 (6.27, 8.47) | 2.00 (1.88, 2.12) | 3.96 (3.45, 4.54) | 1.61 (1.51, 1.73) | |
| 2003‐2007 | 3.82 (3.38, 4.33) | 2.90 (2.49, 3.38) | 6.63 (5.30, 8.30) | 2.00 (1.84, 2.18) | 3.80 (3.13, 4.61) | 1.65 (1.50, 1.82) | ||
| 2008‐2012 | 3.73 (3.33, 4.18) | 2.60 (2.25, 3.00) | 7.85 (6.41, 9.62) | 1.99 (1.83, 2.17) | 4.08 (3.37, 4.95) | 1.58 (1.44, 1.75) | ||
| Austria | 2003‐2012 | 5.29 (4.89, 5.72) | 4.54 (4.11, 5.01) | 6.99 (6.13, 7.98) | 1.84 (1.78, 1.91) | 4.08 (3.67, 4.52) | 1.64 (1.58, 1.70) | |
| 2003‐2007 | 5.74 (5.12, 6.44) | 4.85 (4.21, 5.59) | 8.03 (6.58, 9.81) | 1.81 (1.73, 1.90) | 4.08 (3.51, 4.76) | 1.63 (1.55, 1.72) | ||
| 2008‐2012 | 4.92 (4.42, 5.49) | 4.24 (3.70, 4.88) | 6.30 (5.27, 7.52) | 1.90 (1.81, 1.99) | 4.07 (3.53, 4.69) | 1.67 (1.58, 1.76) | ||
| France | 2003‐2012 | 5.98 (5.63, 6.35) | 5.32 (4.95, 5.71) | 9.01 (7.97, 10.18) | 2.48 (2.39, 2.59) | 6.17 (5.57, 6.85) | 1.94 (1.85, 2.03) | |
| 2003‐2007 | 6.37 (5.83, 6.97) | 5.77 (5.20, 6.40) | 9.39 (7.80, 11.30) | 2.63 (2.48, 2.78) | 7.69 (6.52, 9.06) | 2.07 (1.94, 2.21) | ||
| 2008‐2012 | 5.62 (5.17, 6.11) | 4.88 (4.43, 5.39) | 8.72 (7.40, 10.26) | 2.36 (2.23, 2.49) | 5.27 (4.62, 6.02) | 1.82 (1.70, 1.94) | ||
| Germany | 2003‐2012 | 4.17 (3.96, 4.39) | 3.27 (3.06, 3.48) | 6.94 (6.34, 7.60) | 1.83 (1.78, 1.88) | 3.97 (3.72, 4.25) | 1.49 (1.45, 1.54) | |
| 2003‐2007 | 4.18 (3.87, 4.50) | 3.27 (2.99, 3.58) | 7.91 (6.85, 9.15) | 1.79 (1.72, 1.86) | 3.93 (3.56, 4.34) | 1.49 (1.42, 1.56) | ||
| 2008‐2012 | 4.15 (3.87, 4.45) | 3.24 (2.96, 3.55) | 6.41 (5.71, 7.20) | 1.88 (1.81, 1.96) | 3.99 (3.65, 4.37) | 1.50 (1.43, 1.57) | ||
| The Netherlands | 2003‐2012 | 3.34 (3.23, 3.45) | 1.66 (1.57, 1.75) | 5.59 (5.34, 5.86) | 2.15 (2.08, 2.21) | 4.00 (3.76, 4.26) | 1.74 (1.68, 1.80) | |
| 2003‐2007 | 3.33 (3.17, 3.50) | 1.67 (1.55, 1.80) | 5.88 (5.47, 6.31) | 2.25 (2.16, 2.35) | 4.22 (3.86, 4.62) | 1.82 (1.74, 1.91) | ||
| 2008‐2012 | 3.34 (3.19, 3.49) | 1.64 (1.53, 1.77) | 5.39 (5.07, 5.73) | 2.05 (1.97, 2.14) | 3.80 (3.48, 4.15) | 1.67 (1.59, 1.75) | ||
| Australia/New Zealand | Australia | 20032012 | 3.08 (2.97, 3.20) | 1.51 (1.43, 1.59) | 6.70 (6.29, 7.14) | 2.22 (2.16, 2.29) | 4.10 (3.86, 4.36) | 1.74 (1.69, 1.81) |
| 20032007 | 2.95 (2.79, 3.11) | 1.54 (1.42, 1.66) | 6.34 (5.78, 6.95) | 2.23 (2.14, 2.33) | 4.41 (4.02, 4.83) | 1.75 (1.66, 1.83) | ||
| 2008‐2012 | 3.21 (3.04, 3.38) | 1.49 (1.38, 1.60) | 7.03 (6.45, 7.67) | 2.21 (2.12, 2.30) | 3.85 (3.55, 4.18) | 1.74 (1.66, 1.83) | ||
| New Zealand | 2003‐2012 | 2.72 (2.50, 2.94) | 1.09 (0.96, 1.23) | 6.44 (5.63, 7.36) | 1.94 (1.82, 2.08) | 4.24 (3.67, 4.89) | 1.48 (1.37, 1.59) | |
| 20032007 | 2.72 (2.42, 3.05) | 1.17 (0.98, 1.40) | 6.44 (5.31, 7.80) | 1.90 (1.73, 2.09) | 4.72 (3.80, 5.87) | 1.43 (1.29, 1.59) | ||
| 2008‐2012 | 2.72 (2.43, 3.04) | 1.02 (0.85, 1.21) | 6.44 (5.34, 7.75) | 2.00 (1.82, 2.20) | 3.91 (3.23, 4.73) | 1.53 (1.37, 1.71) | ||
Abbreviations: EAC, esophageal adenocarcinoma; ESCC, esophageal squamous cell carcinoma; GCC, gastric cardia cancer; GNCC, gastric noncardia cancer.
Using Segi's World Standard Population as reference.
The identified sex differences significantly varied by age and cancer subtype and subsite (Figure 1). The most notable male predominance was found in EAC across all age groups with double peaks. The male‐to‐female incidence rate ratios of EAC began to increase from young ages at 3:1 in age group of 20‐24 years, and reached the first peak at age of 25‐29 years with a sex ratio of 6:1 (male vs female rate: 0.06 vs 0.01) (Table 2). After a slightly decline, the ratio approached the second peak in age group of 50‐64 years for a ratio of 8:1, thereafter declined to 4:1 at age of 85 onward. For ESCC, males presented higher incidence rates than females from a young age, with a peak ratio of 3.8:1 (male vs female: 16.17 vs 4.24) at age of 60‐64 years with declines thereafter. A similarly changing pattern was found for GCC with a peak ratio of 4.5:1 (male vs female: 10.96 vs 2.43) at age of 60‐64 years. In contrast, we observed lower incidence rates of GNCC in males than in females in age groups younger than 40, nevertheless the incidence rates of males surpassed those of females approaching a peak male‐to‐female ratio of just 2.5:1 (male vs female: 49.14 vs 19.93) at age of 60‐64 years.
FIGURE 1.
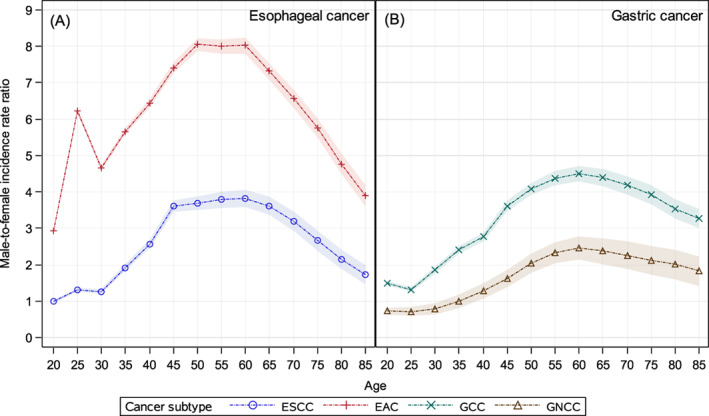
Global patterns of age‐specific male‐to‐female incidence rate ratios of esophageal squamous cell carcinoma, esophageal adenocarcinoma, gastric cardia cancer and gastric noncardia cancer (2003‐2012). EAC, esophageal adenocarcinoma; ESCC, esophageal squamous cell carcinoma; GCC, gastric cardia cancer; GNCC, gastric noncardia cancer [Color figure can be viewed at wileyonlinelibrary.com]
TABLE 2.
Global patterns of age‐specific incidence rate, male‐to‐female incidence rate ratios and 95% CIs for esophageal squamous cell carcinoma, esophageal adenocarcinoma, gastric cardia cancer and gastric noncardia cancer (2003‐2012)
| Cancer type | Age group | Incidence rate per 100 000 in males (95% CIs) | Incidence rate per 100 000 in females (95% CIs) | Male‐to‐female incidence rate ratios (95% CIs) |
|---|---|---|---|---|
| Esophageal squamous cell carcinoma (ESCC) | 20‐24 | 0.01 (0.01, 0.01) | 0.01 (0.01, 0.01) | 0.98 (0.57, 1.69) |
| 25‐29 | 0.03 (0.02, 0.03) | 0.02 (0.02, 0.03) | 1.31 (0.93, 1.83) | |
| 30‐34 | 0.08 (0.07, 0.09) | 0.06 (0.06, 0.07) | 1.26 (1.04, 1.54) | |
| 35‐39 | 0.28 (0.26, 0.30) | 0.14 (0.13, 0.16) | 1.92 (1.70, 2.16) | |
| 40‐44 | 0.96 (0.92, 0.99) | 0.37 (0.35, 0.39) | 2.57 (2.40, 2.76) | |
| 45‐49 | 2.89 (2.82, 2.95) | 0.80 (0.77, 0.83) | 3.61 (3.44, 3.78) | |
| 50‐54 | 6.42 (6.32, 6.52) | 1.74 (1.69, 1.79) | 3.69 (3.57, 3.81) | |
| 55‐59 | 11.14 (11.00, 11.28) | 2.94 (2.87, 3.01) | 3.78 (3.68, 3.89) | |
| 60‐64 | 16.17 (15.99, 16.36) | 4.24 (4.15, 4.34) | 3.81 (3.72, 3.90) | |
| 65‐69 | 21.22 (20.98, 21.46) | 5.86 (5.75, 5.98) | 3.62 (3.54, 3.70) | |
| 70‐74 | 24.21 (23.93, 24.50) | 7.60 (7.46, 7.75) | 3.19 (3.12, 3.26) | |
| 75‐79 | 24.09 (23.77, 24.43) | 9.06 (8.90, 9.24) | 2.66 (2.60, 2.72) | |
| 80‐84 | 23.34 (22.93, 23.76) | 10.90 (10.68, 11.12) | 2.14 (2.09, 2.20) | |
| 85+ | 21.53 (21.04, 22.03) | 12.48 (12.24, 12.73) | 1.72 (1.67, 1.78) | |
| Esophageal adenocarcinoma (EAC) | 20‐24 | 0.02 (0.01, 0.02) | 0.01 (0.00, 0.01) | 2.92 (1.61, 5.31) |
| 25‐29 | 0.06 (0.05, 0.07) | 0.01 (0.01, 0.01) | 6.23 (4.08, 9.51) | |
| 30‐34 | 0.14 (0.12, 0.15) | 0.03 (0.02, 0.04) | 4.66 (3.67, 5.92) | |
| 35‐39 | 0.38 (0.36, 0.40) | 0.07 (0.06, 0.08) | 5.66 (4.84, 6.60) | |
| 40‐44 | 1.04 (1.00, 1.07) | 0.16 (0.15, 0.18) | 6.44 (5.84, 7.10) | |
| 45‐49 | 2.40 (2.34, 2.45) | 0.32 (0.30, 0.34) | 7.41 (6.92, 7.94) | |
| 50‐54 | 5.00 (4.91, 5.09) | 0.62 (0.59, 0.65) | 8.05 (7.64, 8.47) | |
| 55‐59 | 8.89 (8.76, 9.01) | 1.11 (1.07, 1.15) | 8.00 (7.68, 8.34) | |
| 60‐64 | 13.77 (13.60, 13.95) | 1.72 (1.66, 1.78) | 8.03 (7.74, 8.32) | |
| 65‐69 | 17.68 (17.46, 17.90) | 2.42 (2.34, 2.49) | 7.31 (7.07, 7.56) | |
| 70‐74 | 21.79 (21.52, 22.06) | 3.32 (3.23, 3.42) | 6.56 (6.35, 6.76) | |
| 75‐79 | 26.73 (26.39, 27.08) | 4.63 (4.51, 4.76) | 5.77 (5.60, 5.94) | |
| 80‐84 | 32.86 (32.37, 33.35) | 6.89 (6.71, 7.06) | 4.77 (4.63, 4.91) | |
| 85+ | 34.47 (33.85, 35.10) | 8.84 (8.63, 9.05) | 3.90 (3.79, 4.02) | |
| Gastric cardia cancer (GCC) | 20‐24 | 0.04 (0.03, 0.05) | 0.03 (0.02, 0.03) | 1.49 (1.09, 2.02) |
| 25‐29 | 0.08 (0.07, 0.09) | 0.06 (0.05, 0.07) | 1.32 (1.07, 1.62) | |
| 30‐34 | 0.23 (0.22, 0.25) | 0.13 (0.11, 0.14) | 1.85 (1.62, 2.12) | |
| 35‐39 | 0.52 (0.50, 0.55) | 0.22 (0.20, 0.24) | 2.41 (2.18, 2.66) | |
| 40‐44 | 1.11 (1.07, 1.15) | 0.40 (0.38, 0.43) | 2.76 (2.58, 2.96) | |
| 45‐49 | 2.28 (2.23, 2.34) | 0.63 (0.60, 0.66) | 3.62 (3.43, 3.82) | |
| 50‐54 | 4.16 (4.08, 4.24) | 1.02 (0.98, 1.06) | 4.08 (3.91, 4.26) | |
| 55‐59 | 7.25 (7.14, 7.37) | 1.66 (1.60, 1.71) | 4.38 (4.22, 4.53) | |
| 60‐64 | 10.96 (10.81, 11.12) | 2.43 (2.36, 2.50) | 4.51 (4.37, 4.65) | |
| 65‐69 | 15.70 (15.49, 15.91) | 3.57 (3.48, 3.66) | 4.40 (4.27, 4.53) | |
| 70‐74 | 20.28 (20.02, 20.55) | 4.85 (4.74, 4.97) | 4.18 (4.07, 4.30) | |
| 75‐79 | 23.79 (23.46, 24.12) | 6.05 (5.91, 6.19) | 3.93 (3.83, 4.04) | |
| 80‐84 | 25.21 (24.78, 25.65) | 7.16 (6.98, 7.34) | 3.52 (3.42, 3.63) | |
| 85+ | 22.88 (22.38, 23.40) | 6.98 (6.79, 7.17) | 3.28 (3.17, 3.40) | |
| Gastric noncardia cancer (GNCC) | 20‐24 | 0.22 (0.20, 0.23) | 0.30 (0.28, 0.32) | 0.73 (0.65, 0.81) |
| 25‐29 | 0.61 (0.58, 0.64) | 0.86 (0.82, 0.90) | 0.71 (0.67, 0.76) | |
| 30‐34 | 1.59 (1.54, 1.64) | 2.03 (1.98, 2.09) | 0.78 (0.75, 0.81) | |
| 35‐39 | 3.34 (3.27, 3.41) | 3.38 (3.32, 3.46) | 0.99 (0.96, 1.02) | |
| 40‐44 | 6.73 (6.63, 6.82) | 5.28 (5.19, 5.37) | 1.27 (1.25, 1.30) | |
| 45‐49 | 12.16 (12.03, 12.29) | 7.49 (7.39, 7.60) | 1.62 (1.59, 1.65) | |
| 50‐54 | 20.99 (20.81, 21.17) | 10.28 (10.15, 10.40) | 2.04 (2.01, 2.07) | |
| 55‐59 | 32.17 (31.93, 32.41) | 13.80 (13.65, 13.96) | 2.33 (2.30, 2.36) | |
| 60‐64 | 49.14 (48.81, 49.47) | 19.93 (19.73, 20.13) | 2.47 (2.44, 2.50) | |
| 65‐69 | 73.73 (73.28, 74.18) | 31.04 (30.77, 31.32) | 2.38 (2.35, 2.40) | |
| 70‐74 | 98.87 (98.28, 99.46) | 43.87 (43.52, 44.22) | 2.25 (2.23, 2.28) | |
| 75‐79 | 113.4 (112.7, 114.1) | 53.56 (53.15, 53.99) | 2.12 (2.10, 2.14) | |
| 80‐84 | 122.1 (121.1, 123.1) | 60.86 (60.34, 61.38) | 2.01 (1.98, 2.03) | |
| 85+ | 119.7 (118.5, 120.9) | 65.46 (64.89, 66.03) | 1.83 (1.80, 1.85) |
We additionally analyzed the age‐specific sex difference of other digestive cancer types, and found that the male‐to‐female incidence rates ratios of cancers of the liver, colon, rectum and pancreas consistently presented a “low‐high‐low” pattern, with a declining age from 50 to 65 years (Figure 2). Males presented a higher incidence rate than that of females across different ages in gastrointestinal cancers, except for cancers of stomach before age of 40 and colon and pancreas before age of 30.
FIGURE 2.
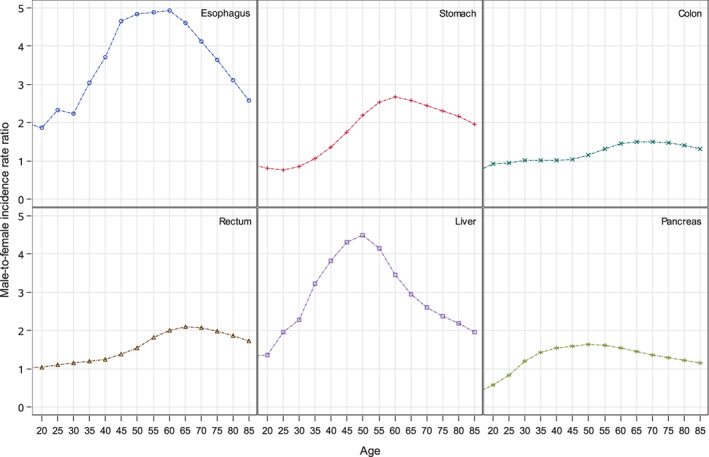
Global patterns of age‐specific male‐to‐female incidence rate ratios of gastrointestinal cancers (2003‐2012) [Color figure can be viewed at wileyonlinelibrary.com]
Further analysis on the trends of age‐specific incidence rate of the intestinal type and diffuse type of GCC and GNCC with available data from China and the United States is shown in Figure S1. In general, the intestinal and diffuse types were more equally distributed between sexes before age of 40 in GCC, but became to be more prevalent in males than females after 40 years. In GNCC, however, females presented a higher incidence rate than males for the diffuse type before age of 40.
Globally, we found significant higher sex ratios of EAC than those of ESCC across all age groups, and identified similar patterns of age‐specific sex differences in many European countries (Austria, Belgium, Denmark, France, Germany, Ireland, Italy, Norway, Switzerland, the Netherlands and the United Kingdom), some North American countries (Canada and the United States), Oceanian countries (Australia and New Zealand) and a few Asian countries (Israel and Japan). However, higher sex ratios of ESCC than EAC were observed in Belarus, Republic of Korea and Ukraine, while comparable sex ratios between EAC and ESCC were observed in China, Philippines and Uruguay (Figure 3). For gastric cancer, the sex ratios were significantly higher in GCC than that in GNCC across the world, and similar “low‐high‐low” trends of GCC were observed in many countries, including Australia, Austria, Belgium, Canada, Czech Republic, France, Germany, Italy, Japan, Latvia, Lithuania, Slovakia, the United Kingdom and the United States (Figure 4).
FIGURE 3.
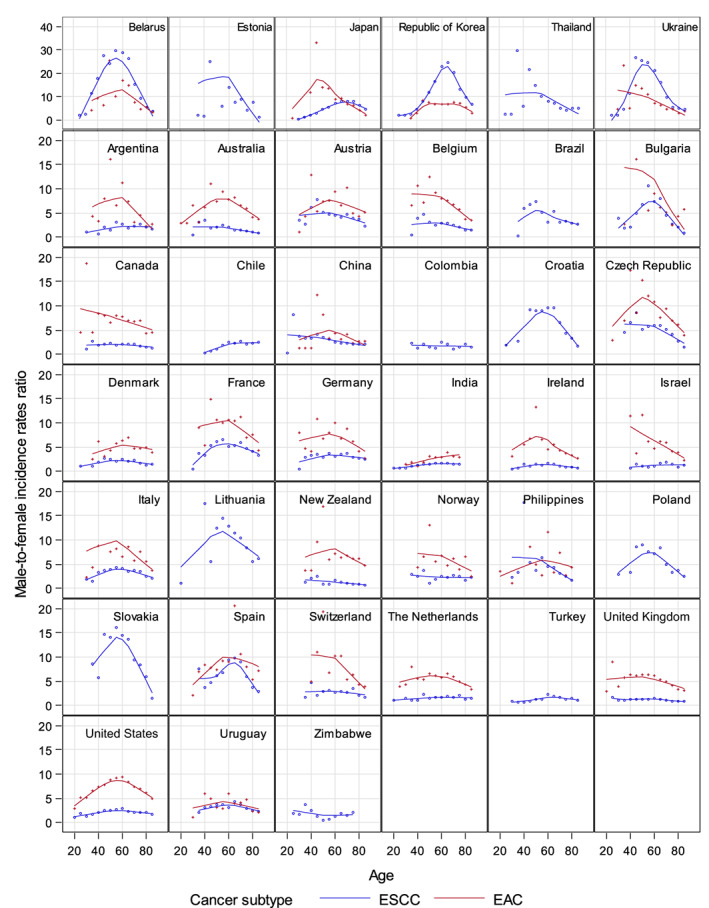
Trends of age‐specific male‐to‐female incidence rates ratios of esophageal squamous cell carcinoma and esophageal adenocarcinoma in 39 selected countries (2003‐2012). Countries that reported sex‐specific incidence data of ESCC or EAC with more than ten 5‐year age groups and with data of age groups younger than 45 were included in this analysis. EAC, esophageal adenocarcinoma; ESCC, esophageal squamous cell carcinoma [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 4.
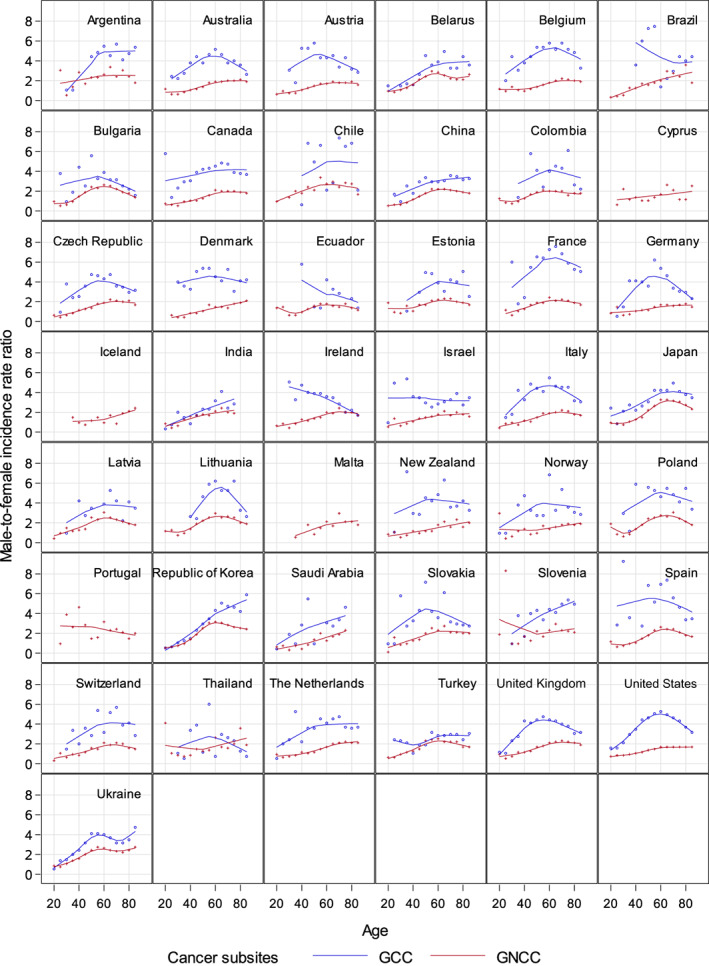
Trends of age‐specific male‐to‐female incidence rates ratios of gastric cardia cancer and gastric noncardia cancer in 43 selected countries (2003‐2012). Countries that reported sex‐specific incidence data of GCC or GNCC with more than ten 5‐year age groups and with data of age groups younger than 45 were included in this analysis. GCC, gastric cardia cancer; GNCC, gastric noncardia cancer [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
A male predominance was observed worldwide in esophageal cancer and gastric cancer, with male‐to‐female ASIRs ratios of 6.7:1 for EAC, 3.3:1 for ESCC, 4:1 for GCC and 2.1:1 for GNCC. Notably, the sex differences varied by age. The male‐to‐female incidence rate ratios of four target cancer types consistently increased from young ages approaching peak ages around 60‐64 years, though the EAC presented an additional peak age at 25‐29 years. The consistent sharp decline of sex differences from the age of 65 across four cancer types suggest important underlying etiological mechanisms linked to age that warrant future investigation.
The observed male predominance appears age‐dependent, and varies by country. Globally, we identified a “double‐peak” pattern of age‐specific male‐to‐female incidence rates ratios for EAC, with two peaks at age of 25‐29 and 50‐64 years. Other studies conducted in older people showed a single peak at 50‐59 years in the United States, 10 but double peaks at age of 50‐54 and 60‐64 years in Sweden. 8 For ESCC, GCC and GNCC, we found a consistent “low‐high‐low” pattern of sex ratios with peak age at 60‐64 years, which was consistent with previous findings from Sweden and the United States. 8 Notably, the male predominance was inversed in GNCC before age of 40 years. Available data from China and the United States indicated an attribution from a higher incidence of the diffuse type of GNCC in females than males at younger ages, which was in line with the results from the United Kingdom and Finland. 13 , 20
Over past decades, we observed marked declines in the incidence of GNCC and ESCC, 21 , 22 slight decline trend of GCC, 23 , 24 , 25 but an upward trend of EAC 26 in both sexes. Similar patterns between the sexes indicated substantial transitions in major environmental risk factor profiles, including significant declines in smoking and heavy alcohol consumption for ESCC, 1 , 21 , 26 a decreased prevalence of H. pylori infection and improvements in the preservation and storage of foods for GNCC, 1 , 27 and an increased prevalence of obesity and gastroesophageal reflux disease paralleled with reduction of H. pylori infection for EAC and GCC. 1 , 17 , 21 , 26 , 28
The changing prevalence of these aforementioned risk factors contributed to different changing patterns of EC and GC burden with a mix of birth cohort and period effects, 21 however, they cannot fully explain the observed male predominance which consistent across four cancer types and over time. 5 , 9 , 29 Some risk factors, including smoking and alcohol consumption, may partly contribute to the extremely high sex ratios of ESCC in some Baltic/European countries. 5 , 9 , 29 Other factors highly relevant to age, that is, endogenous hormones, 5 , 6 , 9 , 30 have been suspected considering the consistent “low‐high‐low” trends of age‐specific sex ratio in different digestive cancers with peak ages at 50‐64 years. A hypothesis was postulated that sex hormones, for example, estrogen, may act as a protective factor and delay the cancer onset in females at younger age but lead to a catch‐up of cancer onset after menopause. This hypothesis is supported by the accruing evidences that later menopause, reproductive factors and estrogen hormone replacement therapies were associated with lower risks of EC and GC. 31 , 32 , 33 , 34 Furthermore, recent results from prospective studies showed an inverse association between circulating estradiol levels and risks of EAC and GCC. 35 An alternative explanation could be that the carcinogenesis of EC and GC are partly driven by androgen, with sex differences diminishing at older ages because of the gradually decreasing levels of androgen. This is supported by studies reporting prostate cancer patients receiving antiandrogen therapies had lower rates of EC and GC, 36 and higher levels of circulating testosterone decreased the risk of EAC. 37 Given complex interactions between environmental exposures and endogenous hormones, sex differences in immune function and response may also play a role. 38 , 39 Future basic and experimental studies are required to help elucidate the underlying etiological mechanisms of the marked age‐dependent sex differences.
There are a number of strengths associated with our study. We used 10 consecutive years of high‐quality data from population‐based cancer registries to ensure comparability and validity of cancer incidence of EC and GC from an international perspective. Secondly, we evaluated the age‐specific sex differences with the male‐to‐female incidence rates ratios in concert with the absolute risk differences in incidence between sexes. The sex ratios are less likely to be affected by changes in diagnostic techniques, tumor definitions, misclassifications and coding practices. There were also several limitations. First, we used the best available data from CI5 which included cancer incidence data from high‐quality population‐based cancer registries, but nevertheless the data was limited by the extent to which histological and subsite information were available from each cancer registry and the results need to be interpreted with caution. Secondly, CI5 does not include information on histological subtypes of GC, thus we cannot discriminate the major subtypes such as diffuse and intestinal cancer across the world. Yet, we explored the country‐specific histological analysis using available data from China and the United States. Thirdly, we assigned C16.8‐16.9 as GNCC which may led to a slight underestimation of ASIRs of GCC. 17 However, the impact of possible misclassifications of overlapping or unspecified GC on the sex ratios are likely to be minor using the most recent 10‐year data, equally affecting males and females, and this would not materially affect the overall patterns reported here.
In conclusion, we observed an age‐dependent male predominance of esophageal cancer and gastric cancer internationally. The consistent changing patterns with age and a sharp decline after the age of 65 across all four cancer types implies important underlying pathological or etiological mechanisms, or common changes of environmental or endogenous risk factors with age. Hence, age‐dependent risk factors warrant further investigations to aid our understanding of the mechanism behind the sex‐specific differences of EC and GC observed today.
AUTHOR CONTRIBUTIONS
Shaoming Wang: Conceptualization, Methodology, Formal analysis, Writing‐Original draft preparation, Writing‐Reviewing and Editing, Funding acquisition; Rongshou Zheng: Methodology, Software, Formal analysis, Writing‐Reviewing and Editing; Melina Arnold, Christian Abnet and Freddie Bray: Methodology, Writing‐Reviewing and Editing; Hongmei Zeng, Siwei Zhang, Ru Chen, Kexin Sun and Li Li: Writing‐Reviewing and Editing; Lan An: Software, Writing‐Reviewing and Editing; Wenqiang Wei: Conceptualization, Writing‐Reviewing and Editing; Funding acquisition; Jie He: Conceptualization, Writing‐Reviewing and Editing; All authors have seen and approved the final version of the manuscript for publication. All the work reported in the paper has been performed by the authors, unless clearly specified in the text.
FUNDING INFORMATION
This work was supported by grants from the Beijing Nova Program (No. Z201100006820069), CAMS Innovation Fund for Medical Sciences (CIFMS, grant number: 2021‐I2M‐1‐023) and National Key R&D Program of China (grant numbers: 2016YFC0901400, 2016YFC0901404). The study funders had no role in the design of the study; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
CONFLICT OF INTEREST
All authors declare no potential conflicts of interests.
ETHICS STATEMENT
Ethical approval is not applicable to our study.
Supporting information
Appendix S1 Supporting Information
ACKNOWLEDGEMENTS
The authors gratefully acknowledge all cancer registries and their staff who have contributed in sharing their data needed for our study.
Wang S, Zheng R, Arnold M, et al. Global and national trends in the age‐specific sex ratio of esophageal cancer and gastric cancer by subtype. Int J Cancer. 2022;151(9):1447‐1461. doi: 10.1002/ijc.34158
Shaoming Wang and Rongshou Zheng contributed equally to our study.
Funding information Beijing Nova Program, Grant/Award Number: Z201100006820069; CAMS Innovation Fund for Medical Sciences, Grant/Award Number: 2021‐I2M‐1‐023; National Key R&D Program of China, Grant/Award Numbers: 2016YFC0901400, 2016YFC0901404
Contributor Information
Wenqiang Wei, Email: weiwq@cicams.ac.cn.
Jie He, Email: hejie@cicams.ac.cn.
DATA AVAILABILITY STATEMENT
The data underlying this article are available in Cancer Incidence in Five Continents from International Agency for Research on Cancer at http://ci5.iarc.fr and the Surveillance, Epidemiology, and End Results (SEER) Program from National Cancer Institute at https://seer.cancer.gov/. Data of 22 registries from Chinese National Central Cancer Registry are available on request to the corresponding author Wenqiang Wei (weiwq@cicams.ac.cn).
REFERENCES
- 1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209‐249. [DOI] [PubMed] [Google Scholar]
- 2. Abnet CC, Arnold M, Wei WQ. Epidemiology of esophageal squamous cell carcinoma. Gastroenterology. 2018;154:360‐373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Coleman HG, Xie SH, Lagergren J. The epidemiology of esophageal adenocarcinoma. Gastroenterology. 2018;154:390‐405. [DOI] [PubMed] [Google Scholar]
- 4. Thrift AP. The epidemic of oesophageal carcinoma: where are we now? Cancer Epidemiol. 2016;41:88‐95. [DOI] [PubMed] [Google Scholar]
- 5. Petrick JL, Cook MB. Do sex hormones underlie sex differences in cancer incidence? Testing the intuitive in esophageal adenocarcinoma. Am J Gastroenterol. 2020;115:211‐213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lagergren J, Lagergren P. Recent developments in esophageal adenocarcinoma. CA Cancer J Clin. 2013;63:232‐248. [DOI] [PubMed] [Google Scholar]
- 7. Thrift AP. Global burden and epidemiology of Barrett oesophagus and oesophageal cancer. Nat Rev Gastroenterol Hepatol. 2021;18:432‐443. [DOI] [PubMed] [Google Scholar]
- 8. Rutegard M, Shore R, Lu Y, et al. Sex differences in the incidence of gastrointestinal adenocarcinoma in Sweden 1970‐2006. Eur J Cancer. 2010;46:1093‐1100. [DOI] [PubMed] [Google Scholar]
- 9. Xie SH, Lagergren J. The male predominance in esophageal adenocarcinoma. Clin Gastroenterol Hepatol. 2016;14:338‐347.e1. [DOI] [PubMed] [Google Scholar]
- 10. Cook MB, Dawsey SM, Freedman ND, et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomarkers Prev. 2009;18:1174‐1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yao Q, Qi X, Xie SH. Sex difference in the incidence of cardia and non‐cardia gastric cancer in the United States, 1992‐2014. BMC Gastroenterol. 2020;20:418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xie SH, Lagergren J. A global assessment of the male predominance in esophageal adenocarcinoma. Oncotarget. 2016;7:38876‐38883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sipponen P, Correa P. Delayed rise in incidence of gastric cancer in females results in unique sex ratio (M/F) pattern: etiologic hypothesis. Gastric Cancer. 2002;5:213‐219. [DOI] [PubMed] [Google Scholar]
- 14. Bray F, Colombet M, Mery L, et al. Cancer Incidence in Five Continents. Vol XI (electronic version). Lyon: International Agency for Research on Cancer; 2017; http://ci5.iarc.fr. Accessed March 18, 2021. [Google Scholar]
- 15. Forman D, Bray F, Brewster D, et al. Cancer Incidence in Five Continents. Vol X. IARC Scientific Publication No. 164. Lyon: International Agency for Research on Cancer; 2014. [Google Scholar]
- 16. Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer; 2020. https://gco.iarc.fr/today. Accessed September 17, 2021. [Google Scholar]
- 17. Arnold M, Ferlay J, van Berge Henegouwen MI, Soerjomataram I. Global burden of oesophageal and gastric cancer by histology and subsite in 2018. Gut. 2020;69:1564‐1571. [DOI] [PubMed] [Google Scholar]
- 18. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115‐132. [DOI] [PubMed] [Google Scholar]
- 19. Zhang S, Sun K, Zheng R, et al. Cancer incidence and mortality in China, 2015. J Natl Cancer Center. 2021;1:2‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Derakhshan MH, Liptrot S, Paul J, Brown IL, Morrison D, McColl KEL. Oesophageal and gastric intestinal‐type adenocarcinomas show the same male predominance due to a 17 year delayed development in females. Gut. 2009;58:16‐23. [DOI] [PubMed] [Google Scholar]
- 21. Rumgay H, Arnold M, Laversanne M, et al. International trends in esophageal squamous cell carcinoma and adenocarcinoma incidence. Am J Gastroenterol. 2021;116(5):1072‐1076. doi: 10.14309/ajg.0000000000001121 [DOI] [PubMed] [Google Scholar]
- 22. Arnold M, Park JY, Camargo MC, Lunet N, Forman D, Soerjomataram I. Is gastric cancer becoming a rare disease? A global assessment of predicted incidence trends to 2035. Gut. 2020;69:823‐829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Camargo MC, Anderson WF, King JB, et al. Divergent trends for gastric cancer incidence by anatomical subsite in US adults. Gut. 2011;60:1644‐1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dikken JL, Lemmens VE, Wouters MW, et al. Increased incidence and survival for oesophageal cancer but not for gastric cardia cancer in the Netherlands. Eur J Cancer. 2012;48:1624‐1632. [DOI] [PubMed] [Google Scholar]
- 25. Schmassmann A, Oldendorf MG, Gebbers JO. Changing incidence of gastric and oesophageal cancer subtypes in central Switzerland between 1982 and 2007. Eur J Epidemiol. 2009;24:603‐609. [DOI] [PubMed] [Google Scholar]
- 26. Arnold M, Laversanne M, Brown LM, Devesa SS, Bray F. Predicting the future burden of esophageal cancer by histological subtype: international trends in incidence up to 2030. Am J Gastroenterol. 2017;112:1247‐1255. [DOI] [PubMed] [Google Scholar]
- 27. Howson CP, Hiyama T, Wynder EL. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol Rev. 1986;8:1‐27. [DOI] [PubMed] [Google Scholar]
- 28. Kamangar F, Dawsey SM, Blaser MJ, et al. Opposing risks of gastric cardia and noncardia gastric adenocarcinomas associated with Helicobacter pylori seropositivity. J Natl Cancer Inst. 2006;98:1445‐1452. [DOI] [PubMed] [Google Scholar]
- 29. Freedman ND, Derakhshan MH, Abnet CC, Schatzkin A, Hollenbeck AR, McColl KEL. Male predominance of upper gastrointestinal adenocarcinoma cannot be explained by differences in tobacco smoking in men versus women. Eur J Cancer. 2010;46:2473‐2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chandanos E, Lagergren J. The mystery of male dominance in oesophageal cancer and the potential protective role of oestrogen. Eur J Cancer. 2009;45:3149‐3155. [DOI] [PubMed] [Google Scholar]
- 31. Green J, Roddam A, Pirie K, et al. Reproductive factors and risk of oesophageal and gastric cancer in the Million Women Study cohort. Br J Cancer. 2012;106:210‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lagergren K, Lagergren J, Brusselaers N. Hormone replacement therapy and oral contraceptives and risk of oesophageal adenocarcinoma: a systematic review and meta‐analysis. Int J Cancer. 2014;135:2183‐2190. [DOI] [PubMed] [Google Scholar]
- 33. Green J, Czanner G, Reeves G, et al. Menopausal hormone therapy and risk of gastrointestinal cancer: nested case‐control study within a prospective cohort, and meta‐analysis. Int J Cancer. 2012;130:2387‐2396. [DOI] [PubMed] [Google Scholar]
- 34. Cronin‐Fenton DP, Murray LJ, Whiteman DC, et al. Reproductive and sex hormonal factors and oesophageal and gastric junction adenocarcinoma: a pooled analysis. Eur J Cancer. 2010;46:2067‐2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Petrick JL, Hyland PL, Caron P, et al. Associations between prediagnostic concentrations of circulating sex steroid hormones and esophageal/gastric cardia adenocarcinoma among men. J Natl Cancer Inst. 2019;111:34‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Davis EJ, Beebe‐Dimmer JL, Yee CL, Cooney KA. Risk of second primary tumors in men diagnosed with prostate cancer: a population‐based cohort study. Cancer. 2014;120:2735‐2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Xie SH, Ness‐Jensen E, Rabbani S, et al. Circulating sex hormone levels and risk of esophageal adenocarcinoma in a prospective study in men. Am J Gastroenterol. 2020;115:216‐223. [DOI] [PubMed] [Google Scholar]
- 38. Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16:626‐638. [DOI] [PubMed] [Google Scholar]
- 39. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7‐33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supporting Information
Data Availability Statement
The data underlying this article are available in Cancer Incidence in Five Continents from International Agency for Research on Cancer at http://ci5.iarc.fr and the Surveillance, Epidemiology, and End Results (SEER) Program from National Cancer Institute at https://seer.cancer.gov/. Data of 22 registries from Chinese National Central Cancer Registry are available on request to the corresponding author Wenqiang Wei (weiwq@cicams.ac.cn).


