Abstract
Aim
To evaluate the efficacy and safety of a dual‐hormone artificial pancreas (DH) in type 1 diabetes.
Material and Methods
PubMed, Embase, the Cochrane Library and ClinicalTrials.gov were searched for studies published up to February 16, 2022. We included randomized controlled trials that compared DH with singlehormone artificial pancreas (SH), continuous subcutaneous insulin infusion (CSII) or sensor‐augmented pumps (SAP), and predictive low glucose suspend systems (PLGS) in type 1 diabetes. The primary outcome was percent time in target (3.9‐10 mmol/L [70‐180 mg/dL]). Data were summarized as mean differences (MDs) or risk differences (RDs).
Results
A total of 17 randomized crossover trials (438 participants) were included. There were nine trials of DH versus SH, 13 trials of DH versus SAP/CSII, and two trials of DH versus PLGS. For time in target, DH showed no significant difference in time in target compared with SH (MD 2.69%, 95% confidence interval [CI] −0.38 to 5.76) but resulted in 16.05% (95% CI 12.06 to 20.05) and 6.89% (95% CI 2.63 to 11.14) more time in target range compared with SAP/CSII and PLGS, respectively. DH slightly reduced time in hypoglycaemia (MD −1.20%, 95% CI −1.85 to −0.56) but increased the risk of gastrointestinal symptoms (RD 0.18, 95% CI 0.08 to 0.27) compared with SH.
Conclusions
The results of this study suggest that DH has a comparable effect on time in target compared with SH, but is associated with a longer time in target range compared with SAP/CSII and PLGS. The DH slightly reduced time in hypoglycaemia but may increase the risk of gastrointestinal symptoms compared with the SH.
PROSPERO registration number: CRD42022314015.
Keywords: artificial pancreas, hypoglycaemia, insulin infusion systems, meta‐analysis, type 1 diabetes
1. INTRODUCTION
Type 1 diabetes is a chronic autoimmune disease characterized by insulin deficiency and resultant hyperglycaemia. 1 Intensive glycaemic control for type 1 diabetes leads to a reduction in microvascular complications and cardiovascular morbidity but achieving near normoglycaemia is challenging. 2 , 3 Many patients with type 1 diabetes do not achieve glycaemic targets despite improved insulin pumps and blood glucose meters, continuous glucose monitoring devices, and integrated sensor‐augmented pump systems (SAP) with automatic threshold suspend capabilities. 4 The artificial pancreas, a novel technology, is a closed‐loop system automatically administering an appropriate insulin dose based on glucose sensor readings and a dosing algorithm. 5 , 6 There are two types of artificial pancreas, singlehormone systems (SH) that infuse insulin and dualhormone systems (DH) that infuse both insulin and glucagon (or pramlintide). Two meta‐analyses concluded that the artificial pancreas systems could improve glucose control compared with conventional insulin pump therapy in outpatients with type 1 diabetes, but only seven trials assessing DH were included. 7 , 8 To the best of our knowledge, no previous meta‐analysis focusing on DH has been published. Quantification of the benefits of adding glucagon to the artificial pancreas is essential because the cost, system complexity, and difficulty of use are lower for the SH. 9 , 10 It is necessary to synthesize evidence of DH for glycaemic control in patients with type 1 diabetes. Therefore, we performed a meta‐analysis of DH for glycaemic control in type 1 diabetes compared with SH and other treatments, both in outpatient and inpatient settings.
2. METHODS
2.1. Data sources and searches
We conducted this meta‐analysis according to the Preferred Reporting Items for Systematic reviews and Meta‐Analyses (PRISMA) guidelines, 11 the protocol was registered on PROSPERO (CRD42022314015). We searched for literature published on Embase, PubMed and Cochrane Library, and the grey literature from the ClinicalTrials.gov website until February 16, 2022. Keywords including “type 1 diabetes”, “dual‐hormone”, and “bihormonal” were used to search; the detailed search strategy is shown in the Supplementary material. Our search was restricted to papers published in English. Additionally, we identified references by searching the reference lists of included studies and relevant reviews.
2.2. Study selection
We included randomized controlled trials (RCTs) comparing DH with SH, SAP or continuous subcutaneous insulin infusion (CSII), and predictive low glucose suspend systems (PLGS) in adults and children with type 1 diabetes, irrespective of trial design (parallel or crossover), setting (outpatient or inpatient), or intervention duration. Outpatient setting was defined as the participant's home, hotel, or a diabetes camp. Observational studies, reviews, conference papers, comments and editorials were excluded.
The primary outcome was the percentage of time of the total duration of the intervention that blood glucose was within target range (3.9‐10 mmol/L [70‐180 mg/dL]). 12 Secondary outcomes included time in hypoglycaemia (below 3.9 mmol/L [70 mg/dL]), time in extreme hypoglycaemia (below 3.0 or 3.3 mmol/L [54 or 60 mg/dL]), time in hyperglycaemia (above10 mmol/L [180 mg/dL]), time in extreme hyperglycaemia (13.9 mmol/L [above 250 mg/dL]), hypoglycaemic events (as defined in each individual study), and any gastrointestinal symptom.
2.3. Data extraction and quality assessment
Two authors reviewed titles and abstracts independently to identify eligible studies that met prespecified inclusion criteria and extracted the data. When consensus was lacking, a third reviewer was consulted. Study characteristics (eg, year of publication, study design, and sample size), intervention and comparator characteristics, patient characteristics (eg, age, diabetes duration, and baseline glycated haemoglobin [HbA1c]), and outcomes were extracted. The risk of bias of RCTs was assessed using the Cochrane Collaboration's tool. 13 We extracted 24‐hour outcomes for studies conducted over 24 hours and overnight outcomes for studies conducted overnight. The quality of evidence for each outcome was evaluated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework. 14
2.4. Data synthesis and analysis
We conducted DerSimonian and Laird random‐effects meta‐analysis when data were available for at least two studies. 15 Three comparators (SH, PLGS and SAP/CSII) were analysed separately. Time in target range, hypoglycaemia, extreme hypoglycaemia, hyperglycaemia, and extreme hyperglycaemia were analysed as mean differences (MDs) with their SEs. Incidence of hypoglycaemic events and any gastrointestinal symptoms were pooled as risk differences (RDs) with 95% confidence intervals (CIs). Medians were assumed to equal means and the SD was calculated as interquartile range/1.35, as recommended by the Cochrane Collaboration. 16 We combined data from both parallel trials and crossover trials. If crossover trials did not report the mean and SE of the paired differences, we planned a priori to analyse all studies using group means and SDs, assuming a correlation coefficient of 0.5. Because of poor reporting of crossover trials, 17 binary data were pooled in the same way as parallel trials. Statistical heterogeneity among the studies was assessed with the chi‐squared test and I 2 statistic. I 2 values of 25%, 50% and 75% have been suggested to be indicators of low, moderate and high heterogeneity, respectively. 18 Publication bias was assessed using a funnel plot for the primary outcome and Egger's test, 19 , 20 where a P value less than 0.05 indicates the presence of publication bias.
For the primary outcome, we conducted prespecified subgroup analyses based on study setting (outpatient or inpatient), population (adult or adolescent), and duration of intervention (24 hours or overnight). P for the difference was calculated using random‐effects meta‐regression, and a difference between the estimates of these subgroups was considered significant if P interaction < 0.10. 21 All the analyses were performed with Stata 14.
3. RESULTS
3.1. Characteristics of included studies
This systematic literature search initially identified 460 records and, after excluding duplicates and irrelevant papers, 53 papers were evaluated in full text for eligibility (Figure S1). Finally, 17 randomized crossover trials (438 participants) in 16 papers were included in the present meta‐analysis. 9 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 Five studies were three‐way crossover trials, 9 , 29 , 30 , 31 , 36 and one study was a four‐way crossover trial. 26 We included nine trials in the analysis of DH versus SH, 13 trials of DH versus SAP/CSII, and two trials of DH versus PLGS. Three trials only enrolled adolescents, 29 , 34 , 35 two trials 9 , 31 enrolled patients aged 12 and above but only one trial 9 reported the results of adolescents. Insulin and glucagon artificial pancreas systems were used in all trials, except one 32 which used an insulin and pramlintide artificial pancreas system. Eight trials were conducted in the United States, 25 , 26 , 27 , 33 , 34 , 35 , 36 seven were conducted in Canada, 9 , 22 , 28 , 29 , 30 , 31 , 32 and two were conducted in the Netherlands. 23 , 24 Four trials had inpatient settings, 22 , 28 , 32 , 33 and the remaining 13 trials had outpatient settings. The characteristics of individual studies are summarized in Table 1. Most examined items were assessed as being of low or unclear risk of bias except blinding. Because of the nature of the intervention, blinding for participants and personnel was impracticable. The detailed risk of bias assessment results are shown in Table S1. The quality of evidence for each outcome was rated according to the GRADE framework (Table S2).
TABLE 1.
Study characteristics and patient demographics
| Study | Location | Trial registration | Comparison | N | Age range | Intervention duration | Follow‐up | Setting | HbA1c levels, % b | Diabetes duration, years b |
|---|---|---|---|---|---|---|---|---|---|---|
| Castellanos (2021) 25 | United States | NCT03840278 | SH | 10 | 21‐74 | 24 h | 7 days | Outpatient | Range: 5.7‐10.6 | NR |
| Wilson (2020) 36 | United States | NCT03424044 | SH, PLGS | 23 | 21‐50 | 24 h | 76 hours | Outpatient (exercise) | 7.1 (0.9) | 16.7 (8.1) |
| Castle (2018) 26 | United States | NCT02862730 | SH, PLGS, SAP | 20 | 21‐45 | 24 h | 4 days | Outpatient (exercise) | 7.5 (0.9) | 20.2 (8.9) |
| Haidar (2017) 30 | Canada | NCT01966393 | SH, SAP | 23 | 19‐71 | 24 h | 60 hours | Outpatient | 7.5 (0.8) | 24.0 (15.0) |
| Haidar (2016) 31 | Canada | NCT01905020 | SH, SAP | 28 | ≥12 | Overnight | 6 nights | Outpatient | 7.5 (1.0) | 18.0 (12.0) |
| Haidar_a (2015) 29 | Canada | NCT02189694 | SH, CSII | 33 | 9‐17 | Overnight | 3 nights | Outpatient | 8.3 (0.8) | 7.5 (4.0) |
| Haidar_b (2015) 9 | Canada | NCT01754337 | SH, CSII | 30 | 12‐69 | 24 h | 24 hours | Outpatient (exercise) | 7.7 (1.0) | 16.0 (11.0) |
| Abitbol (2018) 22 | Canada | NCT02282254 | SH | 35 | ≥18 | Overnight | 12 hours | Inpatient | 7.7 (0.7) | 26.9 (16.1) |
| Haidar (2020) 32 | Canada | NCT02814123 | SH | 27 | ≥18 | 24 h | 24 hours | Inpatient | 7.8 (0.9) | 23.0 (14.0) |
| Haidar (2013) 28 | Canada | NCT01297946 | CSII | 15 | ≥18 | 15 h | 15 hours | Inpatient (exercise) | 7.9 (0.7) | 26.5 (14.8) |
| Russell_a (2014) 34 | United States | NCT01762059 | CSII/SAP | 20 | 21‐75 | 24 h | 5 days | Outpatient | 7.1 (0.8) | 24.0 (11.0) |
| Russell_b (2014) 34 | United States | NCT01833988 | CSII/SAP | 32 | 12‐20 | 24 h | 5 days | Outpatient | 8.2 (1.0) | 9.0 (5.0) |
| Russell (2016) 35 | United States | NCT02105324 | CSII/SAP | 19 | 6‐11 | 24 h | 5 days | Outpatient | 7.8 (0.8) | 5.0 (2.2) |
| Jacobs (2016) 33 | United States | NCT02241889 | SAP | 21 | 18‐45 | 22 h | 22 hours | Inpatient (exercise) | 7.5 (1.0) | 15.4 (9.5) |
| Blauw (2016) 24 | The Netherlands | NCT02160275 | CSII | 10 | 18‐75 | 24 h | 4 days | Outpatient | 7.7 (7.4‐8.0) a | 18.0 (14.8‐29.5) a |
| El‐Khatib (2017) 27 | United States | NCT02092220 | CSII/SAP | 39 | ≥18 | 24 h | 11 days | Outpatient | 7.7 (1.2) | 16.9 (9.6) |
| Blauw (2021) 23 | The Netherlands | NCT03858062 | CSII/SAP | 23 | ≥18 | 24 h | 14 days | Outpatient | 7.3 (7.1‐8.1) a | 23.0 (14.0‐34.5) a |
Abbreviations: CSII, continuous subcutaneous insulin infusion; N, number of participants; NR, not reported; PLGS, predictive low glucose suspend systems; SAP, sensor‐augmented pumps; SH, singlehormone artificial pancreas systems.
Data are median (interquartile range).
Data are mean (SD) unless otherwise indicated.
3.2. Primary outcome
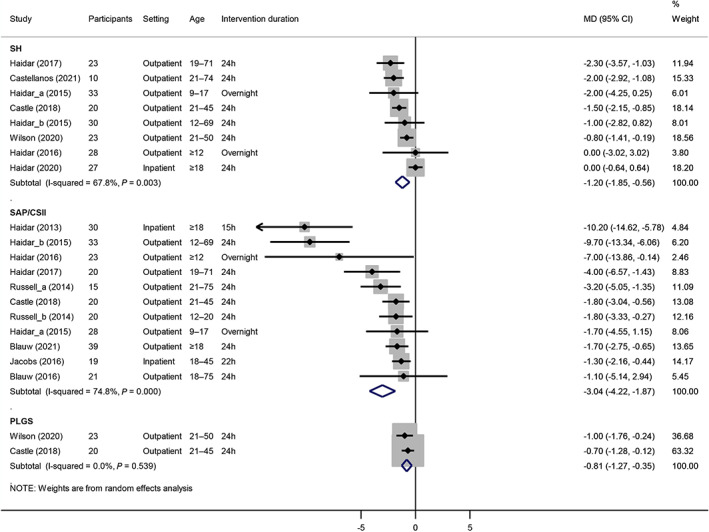
All meta‐analysis results are presented as pooled effect estimates for DH versus control treatments. There was no significant difference in time in target range between DH and SH in nine trials (MD 2.69%, 95% CI −0.38 to 5.76, P = 0.09, I 2 = 63%; GRADE: low). Compared with SAP/CSII, DH resulted in 16.05% (95% CI 12.06 to 20.05, P < 0.001, I 2 = 83%; GRADE: moderate) more time in target range in 13 trials. Compared with PLGS, DH increased 6.89% (95% CI 2.63 to 11.14, P = 0.002, I 2 = 0%; GRADE: low) more time in target range in two trials (Figure 1).
FIGURE 1.

Forest plot for time in target range comparing dual‐hormone artificial pancreas systems (DH) with single‐hormone artificial pancreas systems (SH), sensor‐augmented pumps (SAP)/ continuous subcutaneous insulin infusion (CSII), and predictive low glucose suspend systems (PGLS). MD, mean difference
The primary outcomes stratified by study setting, population and duration of intervention are shown in Table S3. Compared with SH, the use of DH showed a significant improvement (P = 0.03) in time in target range in inpatient settings (without exercise) but not in outpatient settings, and a significant interaction (P = 0.09) was observed. No significant difference was observed in other subgroup analyses comparing DH with SH. When comparing DH with SAP/CSII, outpatient setting was associated with a greater difference for time in target compared with inpatient setting (with exercise), although the test for interaction was not significant (P = 0.11). The more favourable effect of DH use compared with SAP/CSII use was more evident for time in target range in overnight and adolescent subgroup analyses. No subgroup analysis was performed for DH versus PLGS because only two trials were included.
A post hoc sensitivity analysis was performed by excluding a rapid insulin and pramlintide artificial pancreas system. 32 The time in target range was also similar in the DH and SH groups (MD 1.38%, 95% CI −1.14 to 3.90, P = 0.28, I 2 = 40%). There was no significant publication bias, based on Egger's test, among the studies that compared DH with SH (P = 0.13) and SAP/CSII (P = 0.98), and the funnel plots did not show evidence of publication bias visually (Figures S2 and S3).
3.3. Second outcomes
In eight trials, DH showed more favourable effects on time in hypoglycaemia compared with SH (MD −1.20%, 95% CI −1.85 to −0.56, P < 0.001, I 2 = 68%), compared with SAP/CSII in 11 trials (MD −3.04%, 95% CI −4.22 to −1.87, P < 0.001, I 2 = 75%), and compared with PLGS in two trials (MD −0.81%, 95% CI −1.27 to −0.35, P = 0.001, I 2 = 0% [Figure 2]).
FIGURE 2.
Forest plot for time in hypoglycaemia comparing dual‐hormone artificial pancreas systems (DH) with single‐hormone artificial pancreas systems (SH), sensor‐augmented pumps (SAP)/ continuous subcutaneous insulin infusion (CSII), and predictive low glucose suspend systems (PGLS). MD, mean difference
Time in extreme hypoglycaemia was shortened by DH use compared with SH in eight trials (MD −0.15%, 95% CI −0.28 to −0.02, P = 0.02, I 2 = 26%) and compared with SAP/CSII in 12 trials (MD −1.31%, 95% CI −1.87 to −0.76, P < 0.001, I 2 = 86%), but there was no difference between DH and PLGS in two trials (MD −0.03%, 95% CI −0.16 to 0.10, P = 0.65, I 2 = 0% [Figure S4]).
There was no difference in time in hyperglycaemia between DH and SH in nine trials (MD −1.97%, 95% CI −5.18 to 1.24, P = 0.23, I 2 = 75%). DH was associated wth 10.17% (95% CI −14.87 to −5.46, P < 0.001, I 2 = 89%) less time in hyperglycaemia compared with SAP/CSII in 13 trials. Similarly, DH resulted in 6.16% (95% CI −10.41 to −1.90, P = 0.005, I2 = 0%) less time in hyperglycaemia compared with PLGS in two trials (Figure 3).
FIGURE 3.
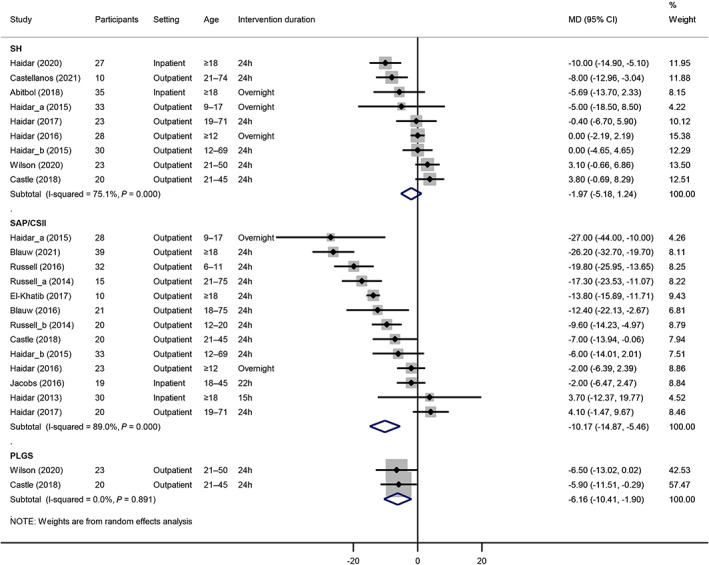
Forest plot for time in hyperglycaemia comparing dual‐hormone artificial pancreas systems (DH) with single‐hormone artificial pancreas systems (SH), sensor‐augmented pumps (SAP)/ continuous subcutaneous insulin infusion (CSII), and predictive low glucose suspend systems (PGLS). MD, mean difference
For time in extreme hyperglycaemia, there was no significance when comparing DH with SH in four trials (MD 1.03%, 95% CI −0.86 to 2.92, P = 0.29, I 2 = 76%) and DH with PLGS in two trials (MD −1.56%, 95% CI −3.65 to 0.53, P = 0.14, I 2 = 0%). DH resulted in 5.89% (95% CI −8.65 to −3.13, P < 0.001, I 2 = 63%) less time in hyperglycaemia compared with SAP/CSII in five trials (Figure S5).
There was no significant difference in the risk of hypoglycaemic events between DH and SH in six trials (RD −0.07, 95% CI −0.14 to 0.001, P = 0.05, I 2 = 0%) but DH was associated with a lower risk of hypoglycaemic events in five trials compared with SAP/CSII (RD −0.35, 95% CI −0.47 to −0.23, P < 0.001, I 2 = 0% [Figure S6]).
In four trials, DH was associated with a higher risk of any gastrointestinal symptoms compared with SH (RD 0.18, 95% CI 0.08 to 0.27, P < 0.001, I 2 = 0%), compared with SAP/CSII in six trials (RD 0.13, 95% CI 0.05 to 0.21, P = 0.002, I 2 = 30%), and compared with PLGS in two trials (RD 0.15, 95% CI 0.01 to 0.30, P = 0.04, I 2 = 0% [Figure S7]).
4. DISCUSSION
This meta‐analysis included 17 randomized crossover trials involving 438 patients, and provided an overview of glycaemic control of DH compared with SH, SAP/CSII and PLGS in patients with type 1 diabetes. This study demonstrated that DH had a comparable effect on the proportion of time in target compared with SH, but had favourable effects compared with SAP/CSII and PLGS in outpatients with type 1 diabetes. Similar results were observed after stratifying by population (adult or adolescent) and duration of intervention (24 hours or overnight) when comparing DH with SH and SAP/CSII. Use of DH slightly reduced time in hypoglycaemia compared with SH, SAP/CSII and PLGS, and significantly decreased time in hyperglycaemia compared with SAP/CSII and PLGS. It should also be noted that DH was associated with a higher risk of gastrointestinal symptoms than the other three comparators. This is the first comprehensive meta‐analysis to investigate the efficacy and safety of DH compared with other treatments in patients with type 1 diabetes.
Previous meta‐analyses focused on the comparison between SH and SAP/CSII, and SH showed favourable effects both overnight and over a 24‐hour period. 7 , 8 , 37 , 38 Our study showed that DH had a favourable effect compared with SAP/CSII. Two studies demonstrated that DH use was associated with a greater improvement in time in target range compared with SH in subgroup analysis, 7 , 8 which is inconsistent with our meta‐analysis; however, our study included more trials, performed a head‐to‐head comparison, and was more reliable. No previous meta‐analysis has been conducted to compare glycaemic control between DH and PLGS. Characteristics of different artificial pancreas systems and conventional insulin treatments have been reviewed comprehensively in two reviews. 6 , 39
At first, we used a correlation coefficient of 0.5 to calculate the mean and SE of the paired differences if there was no reporting in crossover trials. Post hoc validation for correlation coefficient was performed using a method recommended by the Cochrane Collaboration, 16 and was 0.53 for time in target in one trial. 36
In subgroup analyses of DH versus SH, time in target was nonsignificantly higher in the outpatient setting, but was significantly higher in the inpatient setting. The inpatients in two trials were asked to refrain from vigorous exercise. 22 , 32 An outpatient environment is more challenging than an inpatient one because large variations in meals and activity levels influence insulin requirements. 34 In subgroup analyses of DH versus SAP/CSII, time in target was significantly higher in the outpatient setting, but nonsignificant in the inpatient setting. Only two trials were conducted in inpatient settings, therefore the CI was wide due to lower power. The intervention period consisted of an exercise session in two trials. 28 , 33
There was clinical heterogeneity across studies because of differences in study settings, duration of intervention, patient age, insulin and glucagon preparations, continuous glucose monitoring systems, artificial pancreas algorithms, and insulin pumps. For the primary outcome, studies that compared DH with SAP/CSII had higher statistical heterogeneity than studies that compared DH with SH (I 2 83% vs. 63%). Only the subgroup analysis for study setting explained substantial heterogeneity. Heterogeneity was moderate or high for time in target, time in hypoglycaemia, and time in hyperglycaemia when comparing DH with SH and SAP/CSII. There was very low heterogeneity in two trials that compared DH with PLGS.
This study demonstrated that DH therapy increased the risk of gastrointestinal symptoms, both in insulin and glucagon systems and in an insulin and pramlintide system in type 1 diabetes. Although most gastrointestinal symptoms reported are mild or moderate and may be alleviated by some treatments, this adverse effect is a potential limitation when using DH in the real world. 36 Improving compliance is important for use of artificial pancreas therapy in a real‐world setting. 40
This study has several strengths. The meta‐analysis was performed according to the PRISMA guidelines and a protocol registered in PROSPERO. We conducted a comprehensive search of multiple databases and included all available RCTs that evaluated DH with three comparators. The risk of bias for included trials was assessed using a valid methodological tool, and the quality of evidence for each outcome was evaluated using GRADE. Subgroup analyses were performed to explain heterogeneity, and sensitivity analyses were conducted to examine the robustness of the findings. We also acknowledge some limitations. First, the sample size was small in each trial, reducing the precision of effect estimates. Second, most included trials were considered to have a high risk of performance bias owing to the infeasibility of blinding patients and physicians to the allocation assignments. Third, statistical assumptions were made in this study; we retrieved means and SDs from medians and interquartile ranges, respectively. This could be most problematic within the secondary analysis of time in extreme hypoglycaemia and time in extreme hyperglycaemia, and a correlation coefficient of 0.5 was assumed to calculate the mean and SE of the paired differences. Fourth, there was moderate or high heterogeneity for time in target, time in hypoglycaemia, and time in hyperglycaemia. Fifth, the evidence for DH versus SH was insufficient as only two studies that examined this were included. Sixth, the heterogeneity statistic I 2 could be biased in the subgroup analyses due to the small number of studies. 41 Finally, the results of this meta‐analysis might not apply to some clinically relevant subgroups, such as those with increased hypoglycaemia burden, hypoglycaemia unawareness, and high HbA1c levels.
In conclusion, the results of this meta‐analysis suggest that DH therapy has a comparable effect on time in target range compared with SH and increased percentage of time in target range compared with SAP/CSII and PLGS, respectively. Use of DH slightly reduced time in hypoglycaemia compared with SH, SAP/CSII and PLGS, and decreased time in hyperglycaemia compared with SAP/CSII and PLGS. It should be noted that DH may be associated with an increased risk of gastrointestinal symptoms. Cost‐effectiveness should be analysed and compared between DH and SH in further research.
AUTHOR CONTRIBUTIONS
K. Yu and F. Sun conceived the study. B. Zeng and K. Yu designed the study. B. Zeng, L. Gao and H. Jia undertook the literature review and extracted the data. B. Zeng and Q. Yang coded the statistical analysis, figures, and appendix. B. Zeng and H. Jia interpreted the data and wrote the first draft of the manuscript. All authors reviewed and revised subsequent drafts and approved the final version.
FUNDING INFORMATION
This work was supported by the National Natural Science Foundation of China (72074011). PROSPERO number: CRD42020170061.
CONFLICT OF INTEREST
No potential conflicts of interest relevant to this article were reported.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/dom.14781.
Supporting information
Appendix S1 Supporting Information
ACKNOWLEDGMENTS
This work was supported by the National Natural Science Foundation of China (72074011). PROSPERO number: CRD42020170061.
Zeng B, Jia H, Gao L, Yang Q, Yu K, Sun F. Dual‐hormone artificial pancreas for glucose control in type 1 diabetes: A meta‐analysis. Diabetes Obes Metab. 2022;24(10):1967‐1975. doi: 10.1111/dom.14781
Funding information National Natural Science Foundation of China; National Natural Science Foundation of China
Contributor Information
Kai Yu, Email: wzxkjk@126.com.
Feng Sun, Email: sunfeng@bjmu.edu.cn.
DATA AVAILABILITY STATEMENT
The datasets used and/or analysed during the present study are available from the corresponding author on reasonable request.
REFERENCES
- 1. DiMeglio LA, Evans‐Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391:2449‐2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nathan DM. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care. 2014;37:9‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fullerton B, Jeitler K, Seitz M, Horvath K, Berghold A, Siebenhofer A. Intensive glucose control versus conventional glucose control for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2014;2014:Cd009122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miller KM, Foster NC, Beck RW, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D exchange clinic registry. Diabetes Care. 2015;38:971‐978. [DOI] [PubMed] [Google Scholar]
- 5. Haidar A. The artificial pancreas: how closed‐loop control is revolutionizing diabetes. IEEE Control Syst Mag. 2016;36:28‐47. [Google Scholar]
- 6. Moon SJ, Jung I, Park CY. Current advances of artificial pancreas systems: a comprehensive review of the clinical evidence. Diabetes Metab J. 2021;45:813‐839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weisman A, Bai JW, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta‐analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. 2017;5:501‐512. [DOI] [PubMed] [Google Scholar]
- 8. Bekiari E, Kitsios K, Thabit H, et al. Artificial pancreas treatment for outpatients with type 1 diabetes: systematic review and meta‐analysis. BMJ. 2018;361:k1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Haidar A, Legault L, Messier V, Mitre TM, Leroux C, Rabasa‐Lhoret R. Comparison of dual‐hormone artificial pancreas, single‐hormone artificial pancreas, and conventional insulin pump therapy for glycaemic control in patients with type 1 diabetes: an open‐label randomised controlled crossover trial. Lancet Diabetes Endocrinol. 2015;3:17‐26. [DOI] [PubMed] [Google Scholar]
- 10. Haidar A, Smaoui MR, Legault L, Rabasa‐Lhoret R. The role of glucagon in the artificial pancreas. Lancet Diabetes Endocrinol. 2016;4:476‐479. [DOI] [PubMed] [Google Scholar]
- 11. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maahs DM, Buckingham BA, Castle JR, et al. Outcome measures for artificial pancreas clinical trials: a consensus report. Diabetes Care. 2016;39:1175‐1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924‐926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7:177‐188. [DOI] [PubMed] [Google Scholar]
- 16. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0; 2011. [updated March 2011]. https://handbook.cochrane.org [Google Scholar]
- 17. Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues. Int J Epidemiol. 2002;31:140‐149. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327:557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour‐enhanced meta‐analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61:991‐996. [DOI] [PubMed] [Google Scholar]
- 20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ. 1997;315:629‐634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: a tutorial. Clin Epidemiol Global. 2019;7:192‐198. [Google Scholar]
- 22. Abitbol A, Rabasa‐Lhoret R, Messier V, et al. Overnight glucose control with dual‐ and single‐hormone artificial pancreas in type 1 diabetes with hypoglycemia unawareness: a randomized controlled trial. Diabetes Technol Ther. 2018;20:189‐196. [DOI] [PubMed] [Google Scholar]
- 23. Blauw H, Onvlee AJ, Klaassen M, van Bon AC, DeVries JH. Fully closed loop glucose control with a bihormonal artificial pancreas in adults with type 1 diabetes: an outpatient, randomized, crossover trial. Diabetes Care. 2021;44:836‐838. [DOI] [PubMed] [Google Scholar]
- 24. Blauw H, van Bon AC, Koops R, DeVries JH. Performance and safety of an integrated bihormonal artificial pancreas for fully automated glucose control at home. Diabetes Technol Ther. 2016;18:671‐677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Castellanos LE, Balliro CA, Sherwood JS, et al. Performance of the insulin‐only ilet bionic pancreas and the bihormonal ilet using dasiglucagon in adults with type 1 diabetes in a home‐use setting. Diabetes Care. 2021;44:e118‐e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Castle JR, El Youssef J, Wilson LM, et al. Randomized outpatient trial of single‐ and dual‐hormone closed‐loop systems that adapt to exercise using wearable sensors. Diabetes Care. 2018;41:1471‐1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. El‐Khatib FH, Balliro C, Hillard MA, et al. Home use of a bihormonal bionic pancreas versus insulin pump therapy in adults with type 1 diabetes: a multicentre randomised crossover trial. Lancet. 2017;389:369‐380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Haidar A, Legault L, Dallaire M, et al. Glucose‐responsive insulin and glucagon delivery (dual‐hormone artificial pancreas) in adults with type 1 diabetes: a randomized crossover controlled trial. CMAJ. 2013;185:297‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haidar A, Legault L, Matteau‐Pelletier L, et al. Outpatient overnight glucose control with dual‐hormone artificial pancreas, single‐hormone artificial pancreas, or conventional insulin pump therapy in children and adolescents with type 1 diabetes: an open‐label, randomised controlled trial. Lancet Diabetes Endocrinol. 2015;3:595‐604. [DOI] [PubMed] [Google Scholar]
- 30. Haidar A, Messier V, Legault L, Ladouceur M, Rabasa‐Lhoret R. Outpatient 60‐hour day‐and‐night glucose control with dual‐hormone artificial pancreas, single‐hormone artificial pancreas, or sensor‐augmented pump therapy in adults with type 1 diabetes: an open‐label, randomised, crossover, controlled trial. Diabetes Obes Metab. 2017;19:713‐720. [DOI] [PubMed] [Google Scholar]
- 31. Haidar A, Rabasa‐Lhoret R, Legault L, et al. Single‐ and dual‐hormone artificial pancreas for overnight glucose control in type 1 diabetes. J Clin Endocrinol Metab. 2016;101:214‐223. [DOI] [PubMed] [Google Scholar]
- 32. Haidar A, Tsoukas MA, Bernier‐Twardy S, et al. A novel dual‐hormone insulin‐and‐pramlintide artificial pancreas for type 1 diabetes: a randomized controlled crossover trial. Diabetes Care. 2020;43:597‐606. [DOI] [PubMed] [Google Scholar]
- 33. Jacobs PG, El Youssef J, Reddy R, et al. Randomized trial of a dual‐hormone artificial pancreas with dosing adjustment during exercise compared with no adjustment and sensor‐augmented pump therapy. Diabetes Obes Metab. 2016;18:1110‐1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Russell SJ, El‐Khatib FH, Sinha M, et al. Outpatient glycemic control with a bionic pancreas in type 1 diabetes. N Engl J Med. 2014;371:313‐325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Russell SJ, Hillard MA, Balliro C, et al. Day and night glycaemic control with a bionic pancreas versus conventional insulin pump therapy in preadolescent children with type 1 diabetes: a randomised crossover trial. Lancet Diabetes Endocrinol. 2016;4:233‐243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wilson LM, Jacobs PG, Ramsey KL, et al. Dual‐hormone closed‐loop system using a liquid stable glucagon formulation versus insulin‐only closed‐loop system compared with a predictive low glucose suspend system: an open‐label, outpatient, single‐center, crossover, randomized controlled trial. Diabetes Care. 2020;43:2721‐2729. [DOI] [PubMed] [Google Scholar]
- 37. Eckstein ML, Weilguni B, Tauschmann M, et al. Time in range for closed‐loop systems versus standard of care during physical exercise in people with type 1 diabetes: a systematic review and meta‐analysis. J Clin Med. 2021;10:2445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fang Z, Liu M, Tao J, Li C, Zou F, Zhang W. Efficacy and safety of closed‐loop insulin delivery versus sensor‐augmented pump in the treatment of adults with type 1 diabetes: a systematic review and meta‐analysis of randomized‐controlled trials. J Endocrinol Invest. 2021;45:471‐481. [DOI] [PubMed] [Google Scholar]
- 39. Bakhtiani PA, Zhao LM, El Youssef J, Castle JR, Ward WK. A review of artificial pancreas technologies with an emphasis on bi‐hormonal therapy. Diabetes Obes Metab. 2013;15:1065‐1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Horowitz ME, Kaye WA, Pepper GM, et al. An analysis of Medtronic MiniMed 670G insulin pump use in clinical practice and the impact on glycemic control, quality of life, and compliance. Diabetes Res Clin Pract. 2021;177:108876. [DOI] [PubMed] [Google Scholar]
- 41. von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta‐analyses. BMC Med Res Methodol. 2015;15:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supporting Information
Data Availability Statement
The datasets used and/or analysed during the present study are available from the corresponding author on reasonable request.


