Summary
Background
Few studies have demonstrated the impact of irritable bowel syndrome (IBS) on work and activities of daily living.
Methods
We collected demographic, gastrointestinal symptom, psychological health and quality of life data from 752 adults with Rome IV‐defined IBS. We used the work productivity and activity impairment questionnaire for irritable bowel syndrome and the work and social adjustment scale to examine the degree of both impairment at work and in activities of daily living, as well as factors associated with these.
Results
Of 467 individuals who were employed, 133 (28.5%) reported absenteeism, 373 (85.6%) presenteeism and 382 (81.8%) overall work impairment. A mean of 1.97 hours of work per week was lost due to IBS. Extrapolating this across the entire UK, we estimate that between 72 and 188 million hours of work are lost per year due to IBS in individuals of working age. Among all 752 participants, 684 (91.0%) reported any activity impairment with 220 (29.3%) reporting impairment in home management, 423 (56.3%) in social leisure activities, 207 (27.5%) in private leisure activities, and 203 (27.0%) in maintaining close relationships. Severe IBS, higher levels of anxiety, depression, somatization and gastrointestinal symptom‐specific anxiety, and lower levels of IBS‐related quality of life were associated with impairment in both work and activities of daily living.
Conclusion
Patients with IBS experience a substantial impact on their work and activities of daily living because of their IBS. Future studies should assess the impact of medical interventions on the ability to work and participate in social activities.
Keywords: absenteeism, activities of daily living, irritable bowel syndrome, presenteeism, work

1. INTRODUCTION
Irritable bowel syndrome (IBS) is a disorder of gut‐brain interaction (DGBI), characterised by recurrent abdominal pain associated with a change in stool form or frequency. It affects between 5% and 10% of people worldwide. 1 Because the pathophysiology of IBS is complex and incompletely understood, there is no identifiable biomarker to help make a diagnosis of IBS. 2 Instead, in the absence of red flags, the diagnosis is reached via symptom‐based criteria proposed by the Rome Foundation, with the latest iteration being the Rome IV criteria, 3 and limited investigations. 4 , 5 Patients with IBS, therefore, form a heterogeneous group of individuals with a similar phenotype of abdominal pain and change in bowel habit but are likely to have different underlying causes for their symptoms. Without an identifiable target for therapy, treatment strategies focus on alleviating predominant symptom(s), and drug efficacy in randomised controlled trials is, therefore, modest. 6 , 7 , 8 , 9 , 10
For most patients, IBS is chronic, with a relapsing and remitting course. 11 Quality of life of people with IBS is affected to the same degree as those with organic gastrointestinal diseases, such as Crohn's disease. 12 Direct healthcare costs of IBS are substantial, estimated at between £1.3 and £2 billion per year in a recent UK study, 13 but the full economic consequences are likely to be even higher due to the effect of IBS on the ability to work. In qualitative studies examining the impact of IBS on work and activities of daily living patients with IBS state that their symptoms leave them fearful, embarrassed or ashamed. 14 , 15 , 16 , 17 The unpredictability of symptoms leads to loss of freedom or spontaneity. 14 Individuals also report feeling embarrassed using toilets at work or in public, or having to pass flatus, due to their IBS symptoms. 15 Other themes include fear of symptoms of urgency or faecal incontinence and the fact that bowel symptoms make it difficult to have physical relationships. 15 Finally, patients report stigma associated with a “functional” disease and the lack of a structural cause for their symptoms makes it difficult for colleagues, friends or family to understand. 14 To gain control of various work and personal situations, patients often make adjustments some of which, such as activity avoidance, are maladaptive in nature. 15 , 16 , 17 Although qualitative studies facilitate understanding of themes underlying impairment at work or in activities of daily living, they lack the ability to determine the proportion of individuals affected by their IBS symptoms and to identify predictors of work and activity impairment.
A previous cross‐sectional study in secondary care demonstrated that one‐quarter of participants with Rome III IBS reported absenteeism, more than 80% presenteeism and that work impairment was associated with severity of IBS, quality of life and gastrointestinal symptom‐specific anxiety. 18 Two previous studies have attempted to quantify the impact of IBS on activities of daily living but they were either small, containing only 42 patients, 19 or recruited individuals with Rome III IBS. 20 The impact of IBS, defined according to the Rome IV criteria, on work and activity impairment among a wider population of individuals with IBS is, therefore, unknown. We examined these issues in a cross‐sectional study recruiting a large cohort of people with IBS.
2. METHODS
2.1. Participants and setting
We recruited individuals registered with ContactME‐IBS, a national UK registry of 4280 members with IBS who are interested in volunteering for research. 21 We have reported data from this cohort previously. 22 Briefly, individuals find out about the registry via numerous sources including their general practitioner (GP), specialist hospital clinics, posters in pharmacies or social media. Individuals enrol by completing a short questionnaire about their bowel symptoms and providing contact details. The registry is run by County Durham and Darlington NHS Foundation Trust. Among all registrants, 2268 (53%) have seen their GP with IBS, and another 1455 (34%) a gastroenterologist. There were no exclusion criteria apart from the inability to understand written English. We contacted all registered individuals, via electronic mailshot, in July 2021, directing them to a website where they could access study information. Those willing to participate completed an online questionnaire, with responses stored in an online database. Non‐responders received a reminder email in August 2021. Participants were given a chance to win one of three gift cards (worth £200, £100 or £50). The University of Leeds research ethics committee approved the study in March 2021 (MREC 20–051).
2.2. Data collection and synthesis
2.2.1. Demographic and symptom data
We collected basic demographic data, including age, gender, lifestyle (tobacco and alcohol consumption), ethnicity, marital status, educational level and annual income. We also asked respondents to state whether their IBS symptoms commenced after an acute enteric infection. We defined the presence of IBS according to the Rome IV questionnaire, 23 assigning this to all individuals according to the scoring algorithm proposed for its use. 3 We categorised the IBS subtype according to the criteria recommended in the questionnaire, using the proportion of time stools were abnormal according to the Bristol stool form scale. We asked all participants to select their most troublesome symptom from a list of five possibilities, including abdominal pain, constipation, diarrhoea, bloating/distension or urgency.
2.2.2. IBS symptom severity and impact
We assessed the severity of symptoms using the IBS severity scoring system (IBS‐SSS), 24 which measures presence, severity and frequency of abdominal pain, presence and severity of abdominal distension, satisfaction with bowel habit and degree to which IBS symptoms are affecting, or interfering with, the individual's life. The IBS‐SSS is scored from 0 to 500 points, with <75 indicating remission of symptoms; 75–174 mild symptoms; 175–299 moderate symptoms; and 300–500 severe symptoms.
2.2.3. Mood and somatic symptoms
We used the hospital anxiety and depression scale (HADS) to collect anxiety and depression data. The total HADS score ranges from 0 to 21 for either anxiety or depression. We categorised severity for each into normal (total HADS depression or anxiety score 0–7), borderline normal (8–10), or abnormal (≥11). 25 We collected somatic symptom data using the patient health questionnaire‐12 (PHQ‐12), 26 derived from the validated PHQ‐15. 27 The total PHQ‐12 score ranges from 0 to 24. We categorised severity into high (total PHQ‐12 ≥ 13), medium (8–12), low (4–7), or minimal (≤3).
2.2.4. Gastrointestinal symptom‐specific anxiety
We used the visceral sensitivity index (VSI), 28 which measures gastrointestinal symptom‐specific anxiety. Replies to each of the 15 items are provided on a 6‐point scale from “strongly disagree” (score 0) to “strongly agree” (score 5). We divided these data into equally sized tertiles, as there are no validated cut offs to define low, medium or high levels of gastrointestinal symptom‐specific anxiety.
2.2.5. IBS‐related quality of life
We used the irritable bowel syndrome quality of life (IBS‐QOL), a validated IBS‐specific questionnaire, to measure health‐related quality of life in individuals with IBS. 29 , 30 The IBS‐QOL consists of 34 items, each ranked on a 5‐point Likert scale ranging from 0 to 4, with a total possible score of 0–136 and lower scores indicating better quality of life. The 34 items are based on the following eight variables: dysphoria, interference with activity, body image, health worry, food avoidance, social reactions, sexual activity and relationships. Score were transformed to a 0‐ to 100‐point scale with zero indicating the worst quality of life and 100 indicating the best quality of life. We divided these data into equally sized tertiles, as there are no validated cut offs to define low, medium or high levels of quality of life.
2.2.6. Impact of IBS on work and activities of daily living
We used the work productivity and activity impairment questionnaire for irritable bowel syndrome (WPAI:IBS), 31 which is validated to assess the level of work productivity loss in people with IBS who are employed, as well as impairment in activities of daily living. There are four domains: absenteeism (percentage of work hours missed because of IBS); presenteeism (percentage of impairment experienced whilst working because of IBS); overall work impairment (percentage of work productivity loss); and activity impairment (percentage impairment in activities of daily living). We also used the work and social adjustment scale (WSAS), 32 which has been used to measure the impact of IBS on individuals' ability to work, manage at home, engage in social and private leisure activities, and maintain close relationships. 33 , 34 , 35 , 36 The five domains are scored on a 9‐point scale from “not at all” (score 0), through “definitely” (score 4), to “very severely” (score 8).
2.3. Statistical analysis
We included only participants who met Rome IV criteria for IBS in the analysis. We dichotomised the presence (≥1%) or absence (0%) of absenteeism, presenteeism, overall work impairment or activity impairment and presence (score ≥4 [“definitely” impacting]) or absence (score <4) of an impact of IBS on home management activities, social leisure activities, private leisure activities or maintaining close relationships. We examined the characteristics of participants in each of these groups. We compared categorical variables using a χ2 test and continuous data using an independent samples t‐test, with statistical significance defined as a p value <0.01. We performed logistic regression, controlling for all baseline demographic data (including annual income), IBS subtype, duration, severity and impact of IBS symptoms, most troublesome symptom, presence of meal‐related symptoms, presence of continuous abdominal pain, opiate use, number of IBS‐related drugs in the last 12 months, mood and somatic symptom reporting, gastrointestinal symptom‐specific anxiety and IBS‐related quality of life to examine factors associated with absenteeism, presenteeism, overall work impairment or activity impairment, as well as impairment of home management activities, social leisure activities, private leisure activities or maintaining close relationships. We reported results with odds ratios (ORs) with 95% confidence intervals (CIs).
We used a contemporaneous prevalence of Rome IV IBS in the UK of 4.6%, derived from the Rome Foundation three‐nation prevalence study, 37 to extrapolate the total number of hours of work lost because of IBS per person from this study across the entire UK adult working population (aged 18–64), using published census data, 38 , 39 , 40 and the assumption that individuals worked an average of 46 weeks per year. In the current study, most participants had consulted with a doctor, which may skew the results. We, therefore, contacted the authors of the three‐nation Rome Foundation study to obtain the prevalence of individuals with Rome IV IBS consulting a doctor for IBS in the UK, which was 2.8% (data on file, personal communication: Dr Olafur Palsson, University of North Carolina, Chapel Hill, NC, USA). We used these data to perform a more conservative sensitivity analysis of the number of hours of work lost because of IBS. We used SPSS for Windows (version 27.0 SPSS, Chicago, IL) to perform all analyses.
3. RESULTS
In total, 1278 (29.9%) of 4280 registrants completed the questionnaire. Of these, 752 (58.8%) met Rome IV criteria for IBS (mean age 45.3 years (range 18–81 years), 655 (87.1%) female). In total, 136 (18.1%) had IBS with constipation (IBS‐C), 306 (40.7%) IBS‐D, 301 (40.0%) IBS with mixed bowel habits (IBS‐M), and 9 (1.2%) IBS unclassified (IBS‐U). Of the 752 individuals who met Rome IV criteria for IBS, 484 (64.4%) were employed, 467 (96.5%) of whom provided complete data. Of the 268 individuals who were not currently in employment, 189 (70.5%) stated that they were either retired or not employed for reasons other than their IBS, implying that 79 (10.5%) of the 752 people with Rome IV IBS were unemployed partly as a result of their condition. The median level of absenteeism in all 467 employed individuals with Rome IV IBS was 0.0% ((interquartile range [IQR] 0.0%–2.9%), presenteeism 35.0% (IQR 20.0%–60.0%) and overall work impairment 30.0% (IQR 10.0%–60.0%). Among all 752 individuals, median activity impairment was 40.0% (IQR 20.0%–70.0%)).
Among working age (18–64 inclusive) employed individuals with Rome IV IBS, the mean number of hours of work lost because of IBS was 1.97 hours per week and, therefore, 90.5 hours per year. According to UK census data, there are 39,361,324 adults aged 18–64 in the UK. With a prevalence of 4.6% of Rome IV‐defined IBS in the UK, 37 and an employment rate of 72.2% (479 of 663 individuals of working age with Rome IV IBS) in the current study, there are likely to be 1,307,268 employed individuals of working age with Rome IV IBS. This implies the total amount of work lost to IBS is 118,213,657 hours. In our sensitivity analysis, assuming 2.8% of the UK adult population have Rome IV IBS and will consult a physician (data on file, personal communication: Dr Olafur Palsson, University of North Carolina, Chapel Hill, NC, USA), 37 there are likely to be 795,729 employed individuals of working age with Rome IV IBS who have consulted a physician in the UK. Applying our data to these figures yielded an estimated total of 71,956,139 hours of work lost due to IBS.
3.1. Characteristics of patients with impairment at work and in activities of daily living because of IBS
We examined the characteristics of 133 (28.5%) individuals who reported any absenteeism, 373 (85.6%) any presenteeism, 382 (81.8%) any overall work impairment, and 684 (91.0%) any activity impairment compared with those who did not (Figure 1). Participants with any absenteeism were significantly less likely to be married (56.4% vs 70.7%, p = 0.003), and significantly more likely to have severe IBS (61.7%, vs. 39.5%, p < 0.001), higher levels of anxiety (60.9%, vs. 44.9%, p = 0.006), depression (25.6%, vs. 16.8%, p < 0.001), somatization (37.6%, vs. 25.1%, p = 0.009), and gastrointestinal symptom‐specific anxiety (47.4%, vs. 28.4%, p < 0.001), and lower quality of life (44.4%, vs. 21.3%, p < 0.001) (Table 1). Those with any presenteeism were significantly more likely to be younger (mean age, 40.1 vs. 45.6, p < 0.001), have more severe IBS (47.2%, vs 31.7%, p < 0.001), higher levels of somatization (28.4%, vs. 19.0%, p = 0.008) and gastrointestinal symptom‐specific anxiety (35.9%, vs 19.0%, p < 0.001), and have lower quality of life (30.8%, vs. 9.5%, p < 0.001). Participants with overall work impairment were significantly more likely to be younger (mean age, 40.1 vs. 44.7, p < 0.001), to have higher levels of gastrointestinal symptom‐specific anxiety (36.4%, vs 22.4%, p < 0.001), and lower quality of life (31.2%, vs. 12.9%, p < 0.001). Finally, those with any activity impairment were significantly more likely to have severe IBS (49.9%, vs. 26.5%, p < 0.001), higher levels of anxiety (51.9%, vs. 33.8%, p = 0.004), depression (26.2%, vs. 5.9%, p < 0.001), somatization (32.5%, vs. 16.2%, p < 0.001), and gastrointestinal symptom‐specific anxiety (36.7%, vs. 10.3%, p < 0.001), and lower quality of life (34.4%, vs. 5.9%, p < 0.001).
FIGURE 1.
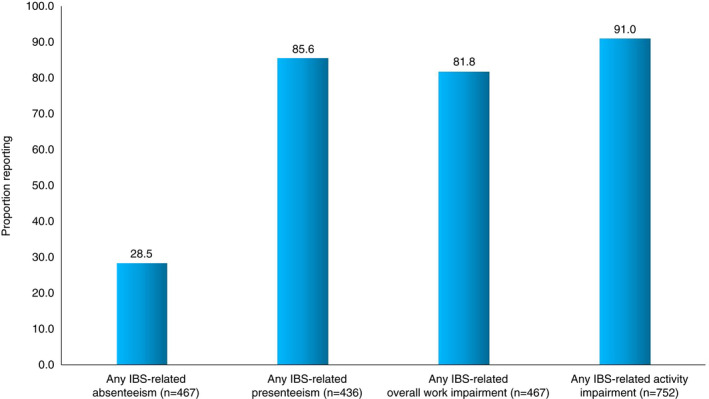
Impairment at work and in activities of daily living because of IBS.
TABLE 1.
Characteristics of individuals with Rome IV IBS who reported absenteeism, Presenteeism, overall work impairment and activity impairment compared with those who did not
| Absenteeism (n = 467) | Presenteeism (n = 436) | Overall work impairment (n = 467) | Activity impairment (n = 752) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 133) | No (n = 334) | p value | Yes (n = 373) | No (n = 63) | p value | Yes (n = 382) | No (n = 85) | p value | Yes (n = 684) | No (n = 68) | p value | |
| Female (%) | 116 (87.2) | 297 (88.9) | 0.6 | 327 (87.7) | 55 (87.3) | 0.94 | 336 (88.0) | 77 (90.6) | 0.49 | 597 (87.3) | 58 (85.3) | 0.64 |
| Mean age (SD) | 39.5 (11.6) | 41.5 (11.5) | 0.096 | 40.1 (11.4) | 45.6 (11.5) | <0.001 | 40.1 (11.4) | 44.7 (11.5) | <0.001 | 45.0 (14.9) | 48.6 (13.3) | 0.057 |
| White ethnicity (%) | 127 (95.5) | 322 (96.4) | 0.64 | 357 (95.7) | 61 (96.8) | 0.68 | 366 (95.8) | 83 (97.6) | 0.43 | 662 (96.8) | 67 (98.5) | 0.43 |
| Married (%) | 75 (56.4) | 236 (70.7) | 0.003 | 248 (66.5) | 45 (71.4) | 0.44 | 251 (65.7) | 60 (70.6) | 0.39 | 441 (64.5) | 46 (67.6) | 0.6 |
| Smoker (%) | 19 (14.3) | 32 (9.6) | 0.14 | 42 (11.3) | 5 (7.9) | 0.43 | 44 (11.5) | 7 (8.2) | 0.38 | 71 (10.4) | 11 (16.2) | 0.14 |
| Alcohol user (%) | 77 (57.9) | 210 (62.9) | 0.32 | 232 (62.2) | 39 (61.9) | 0.97 | 237 (62.0) | 50 (58.8) | 0.58 | 390 (57.0) | 49 (72.1) | 0.016 |
| University or postgraduate level of education (%) | 60 (45.1) | 166 (49.7) | 0.37 | 178 (47.7) | 30 (47.6) | 0.99 | 184 (48.2) | 42 (49.4) | 0.84 | 288 (42.1) | 26 (38.2) | 0.54 |
| Annual income of £30,000 or more (%) | 47 (37.0) | 123 (38.4) | 0.78 | 131 (36.6) | 29 (50.0) | 0.05 | 134 (36.5) | 36 (45.0) | 0.16 | 173 (27.9) | 24 (40.0) | 0.049 |
| IBS after acute enteric infection (%) | 22 (16.5) | 37 (11.1) | 0.11 | 51 (13.7) | 6 (9.5) | 0.37 | 52 (13.6) | 7 (8.2) | 0.18 | 85 (12.4) | 6 (8.8) | 0.39 |
| Meal‐related symptoms ≥ 50% of the time (%) | 101 (75.9) | 258 (77.2) | 0.76 | 292 (78.3) | 44 (69.8) | 0.14 | 299 (78.3) | 60 (70.6) | 0.13 | 512 (74.9) | 49 (72.1) | 0.61 |
| IBS subtype (%) | 0.074 | 0.45 | 0.78 | 0.63 | ||||||||
| IBS‐C | 18 (13.5) | 74 (22.2) | 72 (19.3) | 15 (23.8) | 73 (19.1) | 19 (22.4) | 126 (18.4) | 10 (14.7) | ||||
| IBS‐D | 64 (48.1) | 126 (37.7) | 155 (41.6) | 20 (31.7) | 158 (41.4) | 32 (37.6) | 281 (41.1) | 25 (36.8) | ||||
| IBS‐M | 51 (38.3) | 132 (39.5) | 144 (38.6) | 28 (44.4) | 149 (39.0) | 34 (40.0) | 269 (39.3) | 32 (47.1) | ||||
| IBS‐U | 0 (0.0) | 2 (0.6) | 2 (0.5) | 0 (0.0) | 2 (0.5) | 0 (0.0) | 8 (1.2) | 1 (1.5) | ||||
| Most troublesome symptom (%) | 0.09 | 0.11 | 0.09 | 0.22 | ||||||||
| Abdominal pain | 31 (23.3) | 68 (20.4) | 86 (23.1) | 7 (11.1) | 88 (23.0) | 11 (12.9) | 156 (22.8) | 13 (19.1) | ||||
| Constipation | 8 (6.0) | 21 (6.3) | 24 (6.4) | 5 (7.9) | 24 (6.3) | 5 (5.9) | 50 (7.3) | 3 (4.4) | ||||
| Diarrhoea | 27 (20.3) | 44 (13.2) | 60 (16.1) | 7 (11.1) | 62 (16.2) | 9 (10.6) | 109 (15.9) | 8 (11.8) | ||||
| Bloating/distension | 32 (24.1) | 121 (36.2) | 117 (31.4) | 28 (44.4) | 119 (31.2) | 34 (40.0) | 190 (27.8) | 28 (41.2) | ||||
| Urgency | 35 (26.3) | 80 (24.0) | 86 (23.1) | 16 (25.4) | 89 (23.3) | 26 (30.6) | 179 (26.2) | 16 (23.5) | ||||
| Opiate use (%) | 27 (20.3) | 43 (12.9) | 0.042 | 51 (13.7) | 6 (9.5) | 0.37 | 54 (14.1) | 16 (18.8) | 0.27 | 135 (19.7) | 13 (19.1) | 0.9 |
| Duration of IBS diagnosis, year(s) (%) | 0.82 | 0.32 | 0.45 | 0.17 | ||||||||
| 1 | 5 (3.8) | 11 (3.3) | 11 (2.9) | 3 (4.8) | 11 (2.9) | 5 (5.9) | 24 (3.5) | 1 (1.5) | ||||
| 2 | 9 (6.8) | 17 (5.1) | 22 (5.9) | 3 (4.8) | 22 (5.8) | 4 (4.7) | 39 (5.7) | 2 (2.9) | ||||
| 3 | 10 (7.5) | 27(8.1) | 31 (8.3) | 5 (7.9) | 32 (8.4) | 5 (5.9) | 50 (7.3) | 4 (5.9) | ||||
| 4 | 4 (3.0) | 17 (5.1) | 16 (4.3) | 5 (7.9) | 16 (4.2) | 5 (5.9) | 28 (4.1) | 5 (7.4) | ||||
| 5 | 9 (6.8) | 16 (4.8) | 22 (5.9) | 0 (0.0) | 23 (6.0) | 2 (2.4) | 38 (5.6) | 0 (0.0) | ||||
| >5 | 96 (72.2) | 246 (73.7) | 271 (72.7) | 47 (74.6) | 278 (72.8) | 64 (75.3) | 505 (73.8) | 56 (82.4) | ||||
| Number of IBS drugs in the last 12 months (%) | 0.028 | 0.027 | 0.27 | 0.019 | ||||||||
| 0 | 8 (6.0) | 59 (17.7) | 48 (12.9) | 16 (25.4) | 48 (12.6) | 19 (22.4) | 78 (11.4) | 18 (26.5) | ||||
| 1 | 35 (26.3) | 85 (25.4) | 93 (24.9) | 21 (33.3) | 97 (25.4) | 23 (27.1) | 174 (25.4) | 15 (22.1) | ||||
| 2 | 42 (31.6) | 84 (25.1) | 105 (28.2) | 11 (17.5) | 106 (27.7) | 20 (23.5) | 184 (26.9) | 12 (17.6) | ||||
| 3 | 20 (15.0) | 52 (15.6) | 60 (16.1) | 7 (11.1) | 61 (16.0) | 11 (12.9) | 118 (17.3) | 11 (16.2) | ||||
| 4 | 16 (12.0) | 36 (10.8) | 43 (11.5) | 7 (11.1) | 44 (11.5) | 8 (9.4) | 69 (10.1) | 7 (10.3) | ||||
| ≥5 | 12 (9.0) | 18 (5.4) | 24 (6.4) | 1 (1.6) | 26 (6.8) | 4 (4.7) | 61 (8.9) | 5 (7.4) | ||||
| IBS‐SSS severity (%) | <0.001 | <0.001 | 0.087 | <0.001 | ||||||||
| Remission | 1 (0.8) | 5 (1.5) | 2 (0.5) | 4 (6.3) | 3 (0.8) | 3 (3.5) | 4 (0.6) | 3 (4.4) | ||||
| Mild | 7 (5.3) | 51 (15.3) | 43 (11.5) | 13 (20.6) | 44 (11.5) | 14 (16.5) | 65 (9.5) | 21 (30.9) | ||||
| Moderate | 43 (32.3) | 146 (43.7) | 152 (40.8) | 26 (41.3) | 154 (40.3) | 35 (41.2) | 274 (40.1) | 26 (38.2) | ||||
| Severe | 82 (61.7) | 132 (39.5) | 176 (47.2) | 20 (31.7) | 181 (47.4) | 33 (38.8) | 341 (49.9) | 18 (26.5) | ||||
| HADS anxiety categories (%) | 0.006 | 0.24 | 0.44 | 0.004 | ||||||||
| Normal | 25 (18.8) | 98 (29.3) | 96 (25.7) | 22 (34.9) | 96 (25.1) | 27 (31.8) | 171 (25.0) | 29 (42.6) | ||||
| Borderline abnormal | 27 (20.3) | 86 (25.7) | 91 (24.4) | 16 (25.4) | 93 (24.3) | 20 (23.5) | 158 (23.1) | 16 (23.5) | ||||
| Abnormal | 81 (60.9) | 150 (44.9) | 186 (49.9) | 25 (39.7) | 193 (50.5) | 38 (44.7) | 355 (51.9) | 23 (33.8) | ||||
| HADS depression categories (%) | ||||||||||||
| Normal | 56 (42.1) | 213 (63.8) | <0.001 | 210 (56.3) | 44 (69.8) | 0.11 | 213 (55.8) | 56 (65.9) | 0.12 | 349 (51.0) | 55 (80.9) | <0.001 |
| Borderline abnormal | 43 (32.3) | 65 (19.5) | 88 (23.6) | 12 (19.0) | 89 (23.3) | 19 (22.4) | 156 (22.8) | 9 (13.2) | ||||
| Abnormal | 34 (25.6) | 56 (16.8) | 75 (20.1) | 7 (11.1) | 80 (20.9) | 10 (11.8) | 179 (26.2) | 4 (5.9) | ||||
| PHQ‐12 severity (%) | 0.009 | 0.008 | 0.13 | <0.001 | ||||||||
| Low | 2 (1.5) | 21 (6.3) | 17 (4.6) | 5 (7.9) | 17 (4.5) | 6 (7.1) | 25 (3.7) | 11 (16.2) | ||||
| Mild | 25 (18.8) | 86 (25.7) | 81 (21.7) | 25 (39.7) | 84 (22.0) | 27 (31.8) | 153 (22.4) | 23 (33.8) | ||||
| Moderate | 56 (42.1) | 143 (42.8) | 169 (45.3) | 21 (33.3) | 170 (44.5) | 29 (34.1) | 284 (41.5) | 23 (33.8) | ||||
| Severe | 50 (37.6) | 84 (25.1) | 106 (28.4) | 12 (19.0) | 111 (29.1) | 23 (27.1) | 222 (32.5) | 11 (16.2) | ||||
| VSI scores (%) | <0.001 | <0.001 | 0.001 | <0.001 | ||||||||
| Low | 24 (18.0) | 129 (38.6) | 109 (29.2) | 34 (54.0) | 111 (29.1) | 42 (49.4) | 203 (29.7) | 44 (64.7) | ||||
| Medium | 46 (34.6) | 110 (32.9) | 130 (34.9) | 17 (27.0) | 132 (34.6) | 24 (28.2) | 230 (33.6) | 17 (25.0) | ||||
| High | 63 (47.4) | 95 (28.4) | 134 (35.9) | 12 (19.0) | 139 (36.4) | 19 (22.4) | 251 (36.7) | 7 (10.3) | ||||
| IBS‐QOL score (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Low | 59 (44.4) | 71 (21.3) | 115 (30.8) | 6 (9.5) | 119 (31.2) | 11 (12.9) | 235 (34.4) | 4 (5.9) | ||||
| Medium | 50 (37.6) | 116 (34.7) | 136 (36.5) | 17 (27.0) | 139 (36.4) | 27 (31.8) | 239 (34.9) | 13 (19.1) | ||||
| High | 24 (18.0) | 147 (44.0) | 122 (32.7) | 40 (63.5) | 124 (32.5) | 47 (55.3) | 210 (30.7) | 51 (75.0) | ||||
There were no predictors of absenteeism on logistic regression. Younger participants (OR per year = 0.95; 95% CI 0.92–0.98), those with abdominal bloating or distension as their most troublesome symptom (OR = 0.19; 95% CI 0.06–0.64), compared with abdominal pain or with higher IBS‐related quality of life (OR = 0.13; 95% CI 0.03–0.54) were less likely to report presenteeism. Younger participants (OR per year = 0.96; 95% CI 0.94–0.99), those with bloating or distension (OR = 0.25; 95% CI 0.10–0.62) or urgency as their most troublesome symptom (OR = 0.22; 95% CI 0.08–0.59), compared with abdominal pain or with higher IBS‐related quality of life (OR = 0.16; 95% CI 0.05–0.49) were less likely to report overall work impairment. Finally, smokers (OR = 0.24; 95% CI 0.09–0.65) were less likely to report any activity impairment, and those with moderate IBS (OR = 3.10; 95% CI 1.37–7.02), compared with those with mild IBS, or moderate levels of somatisation (OR = 5.84; 95% CI 1.714–19.87), compared with those with low levels of somatisation, more likely.
3.2. Characteristics of patients with impairment in home management, social leisure activities, private leisure activities and maintaining close relationships because of IBS
Of all 752 individuals with Rome IV IBS, we examined the characteristics of those who reported that IBS affected their home management (220 (29.3%)), social leisure activities (423 (56.3%)), private leisure activities (207 (27.5%)), and close relationships (203 (27.0%)) above a threshold score of ≥4 (Figure 2). There was a significantly lower proportion of individuals with alcohol use (p < 0.001 for trend for all analyses) among those who reported that IBS affected any of the four areas of activities of daily living (Table 2). We observed a smaller proportion of individuals with an annual income of £30,000 or more among those with impairment in activities of daily living but this was only statistically significant in those with impairment in social leisure activities (24.3% vs 34.8%, p = 0.002). There were significantly higher proportions of individuals with more severe IBS, higher levels of anxiety, depression, somatization and gastrointestinal‐specific anxiety scores, and lower IBS‐related quality of life in those who reported an impact of IBS on any of the four areas of activity of daily living (p < 0.001 for trend for all analyses).
FIGURE 2.
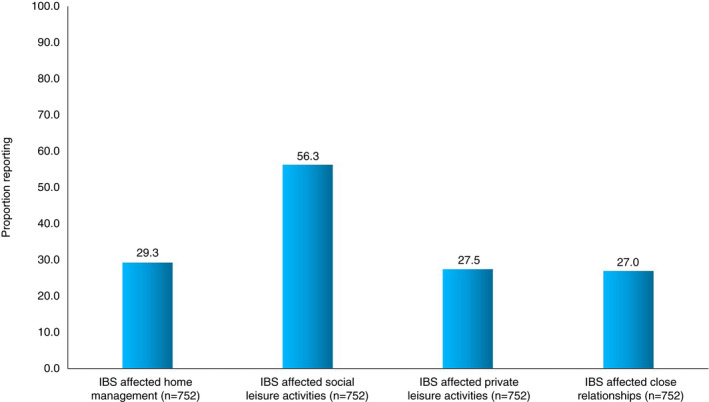
Impairment in home management, social leisure activities, private leisure activities and maintaining close relationships because of IBS.
TABLE 2.
Characteristics of individuals with Rome IV IBS who reported that IBS affected their home management, social leisure activities, private leisure activities and close relationships compared with those who did not
| IBS affects home management (n = 752) | IBS affects social leisure activities (n = 752) | IBS affects private leisure activities (n = 752) | IBS affects close relationships (n = 752) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 220) | No (n = 532) | p value | Yes (n = 423) | No (n = 329) | p value | Yes (n = 207) | No (n = 545) | p value | Yes (n = 203) | No (n = 549) | p value | |
| Female (%) | 192 (87.3) | 463 (87.0) | 0.93 | 370 (87.5) | 285 (86.6) | 0.73 | 179 (86.5) | 476 (87.3) | 0.75 | 172 (84.7) | 483 (88.0) | 0.24 |
| Mean age (SD) | 45.4 (13.7) | 45.3 (15.2) | 0.98 | 45.1 (14.6) | 45.6 (15.1) | 0.61 | 45.3 (14.0) | 45.3 (15.1) | 0.98 | 44.8 (13.9) | 45.5 (15.1) | 0.54 |
| White ethnicity (%) | 208 (94.5) | 521 (97.9) | 0.014 | 410 (96.9) | 319 (97.0) | 0.98 | 197 (95.2) | 532 (97.6) | 0.082 | 195 (96.1) | 534 (97.3) | 0.39 |
| Married (%) | 128 (58.2) | 359 (67.5) | 0.015 | 253 (59.8) | 234 (71.1) | 0.001 | 122 (58.9) | 365 (67.0) | 0.039 | 99 (48.8) | 388 (70.7) | <0.001 |
| Smoker (%) | 33 (15.0) | 49 (9.2) | 0.02 | 50 (11.8) | 32 (9.7) | 0.36 | 31 (15.0) | 51 (9.4) | 0.027 | 30 (14.8) | 52 (9.5) | 0.038 |
| Alcohol user (%) | 94 (42.7) | 345 (64.8) | <0.001 | 201 (47.5) | 238 (72.3) | <0.001 | 94 (45.4) | 345 (63.3) | <0.001 | 95 (46.8) | 344 (62.7) | <0.001 |
| University or postgraduate level of education (%) | 82 (37.3) | 232 (43.6) | 0.11 | 167 (39.5) | 147 (44.7) | 0.15 | 71 (34.3) | 243 (44.6) | 0.011 | 70 (34.5) | 244 (44.4) | 0.014 |
| Annual income of £30,000 or more (%) | 42 (21.9) | 155 (31.8) | 0.011 | 91 (24.3) | 106 (34.8) | 0.002 | 41 (22.4) | 156 (31.4) | 0.022 | 41 (23.2) | 156 (31.0) | 0.048 |
| IBS after acute enteric infection (%) | 30 (13.6) | 61 (11.5) | 0.41 | 62 (14.7) | 29 (8.8) | 0.015 | 31 (15.0) | 60 (11.0) | 0.14 | 22 (10.8) | 69 (12.6) | 0.52 |
| Meal‐related symptoms ≥ 50% of the time (%) | 0 | 391 (73.5) | 0.28 | 327 (77.3) | 234 (71.1) | 0.053 | 162 (78.3) | 399 (73.2) | 0.16 | 160 (78.8) | 401 (73.0) | 0.11 |
| IBS subtype (%) | 0.5 | 0.02 | 0.047 | 0.36 | ||||||||
| IBS‐C | 33 (15.0) | 103 (19.4) | 70 (16.5) | 66 (20.1) | 27 (13.0) | 109 (20.0) | 32 (15.8) | 104 (18.9) | ||||
| IBS‐D | 96 (43.6) | 210 (39.5) | 193 (45.6) | 113 (34.3) | 99 (47.8) | 207 (38.0) | 93 (45.8) | 213 (38.8) | ||||
| IBS‐M | 88 (40.0) | 213 (40.0) | 155 (36.6) | 146 (44.4) | 79 (38.2) | 222 (40.7) | 76 (37.4) | 225 (41.0) | ||||
| IBS‐U | 3 (1.4) | 6 (1.1) | 5 (1.2) | 4 (1.2) | 2 (1.0) | 7 (1.3) | 2 (1.0) | 7 (1.3) | ||||
| Most troublesome symptom (%) | 0.003 | 0.001 | 0.017 | 0.17 | ||||||||
| Abdominal pain | 66 (30.0) | 103 (19.4) | 89 (21.0) | 80 (24.3) | 52 (25.1) | 117 (21.5) | 52 (25.6) | 117 (21.3) | ||||
| Constipation | 7 (3.2) | 46 (8.6) | 23 (5.4) | 30 (9.1) | 6 (2.9) | 42 (8.6) | 11 (5.4) | 42 (7.7) | ||||
| Diarrhoea | 34 (15.5) | 83 (15.6) | 67 (15.8) | 50 (15.2) | 33 (15.9) | 84 (15.4) | 30 (14.8) | 87 (15.8) | ||||
| Bloating/distension | 56 (25.5) | 162 (30.5) | 111 (26.2) | 107 (32.5) | 52 (25.1) | 166 (30.5) | 49 (24.1) | 169 (30.8) | ||||
| Urgency | 57 (25.9) | 138 (25.9) | 133 (31.4) | 62 (18.8) | 64 (30.9) | 131 (24.0) | 61 (30.0) | 134 (24.4) | ||||
| Opiate use (%) | 72 (32.7) | 76 (14.3) | <0.001 | 107 (25.3) | 41 (12.5) | <0.001 | 70 (33.8) | 78 (14.3) | <0.001 | 59 (29.1) | 89 (16.2) | <0.001 |
| Duration of IBS diagnosis, year(s) (%) | 0.26 | 0.83 | 0.58 | 0.36 | ||||||||
| 1 | 5 (2.3) | 20 (3.8) | 14 (3.3) | 11 (3.3) | 7 (3.4) | 18 (3.3) | 5 (2.5) | 20 (3.6) | ||||
| 2 | 10 (4.5) | 31 (5.8) | 21 (5.0) | 20 (6.1) | 14 (6.8) | 27 (5.0) | 12 (5.9) | 29 (5.3) | ||||
| 3 | 13 (5.9) | 41 (7.7) | 32 (7.6) | 22 (6.7) | 15 (7.2) | 39 (7.2) | 17 (8.4) | 37 (6.7) | ||||
| 4 | 7 (3.2) | 26 (4.9) | 16 (3.8) | 17 (5.2) | 5 (2.4) | 28 (5.1) | 5 (2.5) | 28 (5.1) | ||||
| 5 | 16 (7.3) | 22 (4.1) | 24 (5.7) | 14 (4.3) | 9 (4.3) | 29 (5.3) | 14 (6.9) | 24 (4.4) | ||||
| >5 | 169 (76.8) | 392 (73.7) | 316 (74.7) | 245 (74.5) | 157 (75.8) | 404 (74.1) | 150 (73.9) | 411 (74.9) | ||||
| Number of IBS drugs in the last 12 months (%) | 0.004 | 0.009 | 0.003 | <0.001 | ||||||||
| 0 | 19 (8.6) | 77 (14.5) | 42 (9.9) | 54 (16.4) | 17 (8.2) | 79 (14.5) | 14 (6.9) | 82 (14.9) | ||||
| 1 | 54 (24.5) | 135 (25.4) | 101 (23.9) | 88 (26.7) | 52 (25.1) | 137 (25.1) | 52 (25.6) | 137 (25.0) | ||||
| 2 | 51 (23.2) | 145 (27.3) | 110 (26.0) | 86 (26.1) | 47 (22.7) | 149 (27.3) | 41 (20.2) | 155 (28.2) | ||||
| 3 | 41 (18.6) | 88 (16.5) | 79 (18.7) | 50 (15.2) | 35 (16.9) | 94 (17.2) | 37 (18.2) | 92 (16.8) | ||||
| 4 | 23 (10.5) | 53 (10.0) | 43 (10.2) | 33 (10.0) | 26 (12.6) | 50 (9.2) | 25 (12.3) | 51 (9.3) | ||||
| ≥5 | 32 (14.5) | 34 (6.4) | 48 (11.3) | 18 (5.5) | 30 (14.5) | 36 (6.6) | 34 (16.7) | 32 (5.8) | ||||
| IBS‐SSS severity (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Remission | 0 (0.0) | 7 (1.3) | 0 (0.0) | 7 (2.1) | 0 (0.0) | 7 (1.3) | 0 (0.0) | 7 (1.3) | ||||
| Mild | 12 (5.5) | 74 (13.9) | 22 (5.2) | 64 (19.5) | 7 (3.4) | 79 (14.5) | 6 (3.0) | 80 (14.6) | ||||
| Moderate | 43 (19.5) | 257 (48.3) | 131 (31.0) | 169 (51.4) | 45 (21.7) | 255 (46.8) | 48 (23.6) | 252 (45.9) | ||||
| Severe | 165 (75.0) | 194 (36.5) | 270 (63.8) | 89 (27.1) | 155 (74.9) | 204 (37.4) | 149 (73.4) | 210 (39.3) | ||||
| HADS anxiety categories (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Normal | 39 (17.7) | 161 (30.3) | 85 (20.1) | 115 (35.0) | 30 (14.5) | 170 (31.2) | 23 (11.3) | 177 (32.2) | ||||
| Borderline abnormal | 33 (15.0) | 141 (26.5) | 81 (19.1) | 93 (28.3) | 34 (16.4) | 140 (25.7) | 41 (20.2) | 133 (24.2) | ||||
| Abnormal | 148 (67.3) | 230 (43.2) | 257 (60.8) | 121 (36.8) | 143 (69.1) | 235 (43.1) | 139 (68.5) | 239 (43.5) | ||||
| HADS depression categories (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Normal | 61 (27.7) | 343 (64.5) | 161 (38.1) | 243 (73.9) | 55 (26.6) | 349 (64.0) | 56 (27.6) | 348 (63.4) | ||||
| Borderline abnormal | 56 (25.5) | 109 (20.5) | 114 (27.0) | 51 (15.5) | 47 (22.7) | 118 (21.7) | 47 (23.2) | 118 (21.5) | ||||
| Abnormal | 103 (46.8) | 80 (15.0) | 148 (35.0) | 35 (10.6) | 105 (50.7) | 78 (14.3) | 100 (49.3) | 83 (15.1) | ||||
| PHQ‐12 severity (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Low | 4 (1.8) | 32 (6.0) | 13 (3.1) | 23 (7.0) | 4 (1.9) | 32 (5.9) | 5 (2.5) | 31 (5.6) | ||||
| Mild | 24 (10.9) | 152 (28.6) | 71 (16.8) | 105 (31.9) | 30 (14.5) | 146 (26.8) | 27 (13.3) | 149 (27.1) | ||||
| Moderate | 74 (33.6) | 233 (43.8) | 170 (40.2) | 137 (41.6) | 68 (32.9) | 239 (43.9) | 72 (35.5) | 235 (42.8) | ||||
| Severe | 118 (53.6) | 115 (21.6) | 169 (40.0) | 64 (19.5) | 105 (50.7) | 128 (23.5) | 99 (48.8) | 134 (24.4) | ||||
| VSI scores (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Low | 42 (19.1) | 205 (38.5) | 74 (17.5) | 173 (52.6) | 28 (13.5) | 219 (40.2) | 31 (15.3) | 216 (39.3) | ||||
| Medium | 59 (26.8) | 188 (35.3) | 138 (32.6) | 109 (33.1) | 61 (29.5) | 186 (34.1) | 56 (27.6) | 191 (34.8) | ||||
| High | 119 (54.1) | 139 (26.1) | 211 (49.9) | 47 (14.3) | 118 (57.0) | 140 (25.7) | 116 (57.1) | 142 (25.9) | ||||
| IBS‐QOL score (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Low | 139 (63.2) | 100 (18.8) | 215 (50.8) | 24 (7.3) | 134 (64.7) | 105 (19.3) | 142 (70.0) | 97 (17.7) | ||||
| Medium | 60 (27.3) | 192 (36.1) | 149 (35.2) | 103 (31.3) | 57 (27.5) | 195 (35.8) | 47 (23.2) | 205 (37.3) | ||||
| High | 21 (9.5) | 240 (45.1) | 59 (13.9) | 202 (61.4) | 16 (7.7) | 245 (45.0) | 14 (6.9) | 247 (45.0) | ||||
Following logistic regression, those who reported constipation (OR = 0.15; 95% CI 0.05–0.46) or urgency (OR = 0.40; 95% CI 0.20–0.78) as their most troublesome symptom, compared with those reporting abdominal pain, those with borderline abnormal anxiety scores (OR = 0.22; 95% CI 0.10–0.49), compared with those with normal scores, and those with higher IBS‐related quality of life (OR = 0.05; 95% CI 0.02–0.13) were less likely to report impairment in home management, and those with higher levels of depression (OR = 3.30; 95% CI 1.73–6.31) more likely. Those who drank alcohol (OR = 0.42; 95% CI 0.27–0.65), those with borderline abnormal anxiety scores (OR = 0.41; 95% CI 0.22–0.76), compared with those with normal scores, or with higher IBS‐related quality of life (OR = 0.08; 95% CI 0.04–0.16) were less likely to report impairment of social leisure activities, and those who had attended university or gained a postgraduate level of education (OR = 2.46; 95% CI 1.54–3.93) or those who had severe IBS (OR = 3.61; 95% CI 1.77–7.36) more likely. Individuals with higher levels of depression (OR = 4.35; 95% CI 2.33–8.14) were more likely to report impairment in private leisure activities, and those with higher IBS‐related quality of life (OR = 0.12; 95% CI 0.05–0.28) less likely. Finally, those with higher levels of depression (OR = 2.82; 95% CI 1.47–5.41) were more likely to report impairment in close relationships, and those who were married (OR = 0.35; 95% CI 0.21–0.57) or with higher IBS‐related quality of life (OR = 0.04; 95% CI 0.01–0.10) less likely.
4. DISCUSSION
We recruited 752 individuals with Rome IV‐defined IBS to examine the impact of IBS on work and activities of daily living. Our data suggest that approximately 10% of individuals were unemployed partly as a result of their condition. Of those who were employed, nearly 30% reported absenteeism and over 80% presenteeism or overall work impairment because of their IBS. 90% of participants reported their IBS symptoms interfered with activities of daily living, with over 50% reporting interference with social leisure activities and over 25% reporting interference with home management, private leisure activities or close relationships. Those with any absenteeism were significantly more likely to report more severe IBS, higher anxiety, depression, somatization and gastrointestinal‐specific anxiety scores, and lower IBS‐related quality of life whereas those with any presenteeism were significantly more likely to report more severe IBS, higher somatization and gastrointestinal‐specific anxiety scores, and lower IBS‐related quality of life. In terms of activities of daily living, individuals with impairment in home management, social leisure activities, personal leisure activities or close relationships were significantly more likely to have more severe IBS, higher anxiety, depression, somatization and gastrointestinal‐specific anxiety scores, and lower IBS‐related quality of life. Our results also showed that there were several independent predictors of work or activity impairment, including younger age, presence of abdominal pain, severity of IBS symptoms, anxiety, depression and reduced IBS‐related quality of life.
We recruited individuals who self‐identified as having IBS and also met the Rome IV criteria. They are, therefore, likely to represent individuals with IBS in the UK because some had never seen a doctor for their IBS, some had seen a primary care physician, and some had seen a gastroenterologist. Our sample also included participants from different age groups, levels of education and income brackets, suggesting that individuals at different career stages have been included in our study. We used validated questionnaires, including the WPAI:IBS, which has been validated for its use in patients with IBS, 31 and has been used widely. 18 , 41 , 42 , 43 We obtained near‐complete data for variables of interest because we used mandatory fields in our online questionnaire.
Although we used a national UK registry to obtain a sample of individuals with IBS, we were unable to check participants' medical records to rule out other organic gastrointestinal diseases that present with similar symptoms such as celiac disease or inflammatory bowel disease, 44 , 45 nor did we ask them if they had these conditions. Instead, we assumed that, as they were registered with an IBS research registry, they genuinely had IBS. Given that IBS is more prevalent than these conditions, UK national guidance recommends these conditions are ruled out prior to a diagnosis of IBS, 46 , 47 and almost 90% of the ContactME‐IBS registrants have seen a GP or a gastroenterologist for IBS, we believe this is a reasonable assumption. All involved individuals were UK residents, 97% were White, 87% were female and most had IBS‐D or IBS‐M. The results, therefore, are not applicable to individuals outside the UK or from other ethnic groups and may be less relevant to men and those with IBS‐C. Using an online questionnaire meant we were unable to assess the number and characteristics of individuals who accessed the questionnaire but chose not to complete it. Although the WSAS is a validated questionnaire, has been widely used in studies in IBS, and is sensitive to change in IBS treatment trials, 33 , 34 , 35 , 36 it has not been validated formally in IBS, and may not be an accurate tool to compare activity impairment across different diseases. 48 However, it is often utilised to measure the impact of diseases on different aspects of activities of daily living, without conducting a qualitative study with focused interviews, which are not only laborious and expensive but also lack the ability to identify predictors of activity impairment. Previous studies attempting to quantify the impact of IBS on activities of daily living have also resorted to generic, rather than disease‐specific, questionnaires. 19 , 20 Although the WPAI:IBS and WSAS examine the extent to which IBS impacts on work and activities of daily living, they are unable to capture the complex feelings and emotions, such as fear of uncertainty, loss of freedom and shame, as well as the reasons for behavioural adaptations, such as activity avoidance, which can be examined in qualitative studies. 14 , 15 , 16 , 17 As this was a cross‐sectional study, some of the associations or the lack of associations observed that may be expected, could be due to individuals having already altered their working patterns, employment status, home or social activities as a result of their symptoms prior to this study. Similarly, findings such as a reduced likelihood of smokers reporting activity impairment may also relate to reverse causation, with smokers being more likely to have a pre‐existing sedentary lifestyle unrelated to IBS. Finally, given the study was conducted during the COVID‐19 pandemic, with the resultant shift towards home working and reduced social interactions, we cannot exclude the possibility that the true effect of IBS on work and activities of daily living has been underestimated.
Prior studies have demonstrated that a substantial proportion of individuals with IBS report absenteeism, presenteeism, overall work impairment and activity impairment. 18 , 41 , 42 , 43 Frandemark et al. reported absenteeism among almost 25% of participants and presenteeism in over 80%, 18 whereas other studies have only reported mean levels of absenteeism or presenteeism. In contrast to our study recruiting individuals with all IBS subtypes, these studies were more selective, recruiting only people who had consulted a doctor for their IBS in primary or secondary care, 18 , 42 only those with IBS‐D, 43 or only employees of a bank. 41 Although Frandemark et al. examined the associations between work impairment and psychological comorbidities, 18 data on anxiety, depression and somatic symptoms were only available in a subset of 155 participants. To our knowledge, there are limited studies attempting to quantify the impact of IBS on activities of daily living. 19 , 20 Two small studies recruited only 42 patients from secondary care, 19 and 179 participants with Rome III‐defined IBS from the community. 20 In the larger of these two studies, impairment of activities of daily living was associated with severe IBS, anxiety, depression and gastrointestinal symptom‐specific anxiety. A large cross‐sectional survey, conducted in almost 2000 people with IBS, reported that symptoms affected productivity on average 8 days per month and led to approximately 1.5 days of absence from work per month. 49
We have demonstrated that a large proportion of individuals with IBS experience impairment in their personal and professional lives because of their disorder. Although this was a cross‐sectional study, our use of the WPAI:IBS, which has been validated for use in IBS, allowed us to establish that the impairment to work and activities of daily living seen are likely to be a direct consequence of IBS. It is, perhaps, not surprising that those with more severe symptoms and lower IBS‐related quality of life report the greatest impact on work and activities of daily living. Our findings related to the association of psychological comorbidities with work and activity impairment are interesting. Although these psychological comorbidities may themselves impact on work and activities of daily living, our participants attributed their impairment to IBS symptoms, not to these psychological comorbidities. However, psychological comorbidity is also associated with a worse prognosis in IBS, 50 which may be a confounding factor. Individuals with IBS may also lack the resilience to deal with the impact of symptoms of IBS and develop maladaptive behaviours, such as activity avoidance, further compounding the impact of IBS on their quality of life. 51 , 52 Our observation that the time since diagnosis was not associated with a reduction in impairment at work or in activities of daily living is also noteworthy, suggesting that those with a longer duration of disease may not have found constructive adaptations to their personal or professional lives to reduce the impact of IBS.
The results from our study have important implications. Firstly, people of working age with IBS should be aware that impairment at work because of their disorder is, perhaps, more common than readily acknowledged, likely due to the embarrassing nature of symptoms or the feeling that a “functional” disease without an identifiable structural cause is not a legitimate one. Instead, they should feel empowered to discuss their illness with their employer and occupational health physician so that reasonable adjustments can be made to balance work requirements with living with IBS. 17 Secondly, employers should appreciate that IBS is prevalent and is likely to impact on absenteeism and productivity and, ultimately, have cost implications. Creating a more supportive environment with increased awareness of IBS and improved policies about health disclosures and discrimination, as well as flexible working patterns and better access to clean toilet facilities, may help reduce the impact of IBS on work. 53 Thirdly, clinicians should be mindful that IBS impacts on a range of activities including work, ability to perform household tasks, attend social events or have close intimate relationships. Asking patients about the impact of IBS on their own lives, together with active listening and an empathetic approach, may help establish a trusting patient‐doctor relationship, which is essential for the acceptance of the diagnosis and may aid adherence to a shared management plan. 54 , 55 Fourthly, IBS‐specific cognitive behavioural therapy, which uses repeated exposure to activities like physical exertion, food or stressful situations that elicit symptoms, with management of elicited emotions and responses, has been shown to be an effective treatment. 9 Future studies should investigate whether this can reduce the impact of IBS on work and activities of daily living. Fifthly, compared with other symptoms of IBS, predominant abdominal pain appeared to be an independent predictor of presenteeism and overall work impairment. This is, perhaps, not surprising given that abdominal pain severity appears to drive healthcare‐seeking behaviour. 56 , 57 Finally, the results of studies such as ours can be used to inform cost‐effectiveness analyses, 58 , 59 to facilitate value‐based care in IBS.
In summary, our results show that approximately 10% of individuals are unemployed partly as a result of their condition. Among those who are employed, almost one‐in‐three individuals with IBS report absenteeism, and over 80% presenteeism and overall work impairment because of their IBS. We estimate that, in the UK, between 72 and 188 million hours of work are lost per year due to the condition. More than 90% of participants reported that IBS symptoms interfered with their activities of daily living, with over 50% reporting interference with social leisure activities and over 25% reporting interference with home management, private leisure activities and close relationships. Future studies should focus on examining whether the level of impairment at work and in activities of daily living fluctuates over time and, although a cure for IBS is unrealistic and most treatments are of modest efficacy, whether healthcare interventions to help patients find solutions to their daily struggles are effective in reducing the impact of IBS in this regard.
AUTHOR CONTRIBUTIONS
Vivek Goodoory: Conceptualization (equal); data curation (equal); formal analysis (equal); investigation (equal); methodology (equal); project administration (equal); writing – original draft (equal); writing – review and editing (equal). Cho Ee Ng: Conceptualization (equal); data curation (equal); methodology (equal); project administration (equal); resources (equal); software (equal); writing – review and editing (equal). Christopher Black: Conceptualization (equal); investigation (equal); methodology (equal); supervision (equal); writing – review and editing (equal). Alexander Ford: Conceptualization (equal); formal analysis (equal); funding acquisition (equal); methodology (equal); supervision (equal); writing – original draft (equal); writing – review and editing (equal).
AUTHORSHIP
Guarantor of the article: Alexander C. Ford.
ACKNOWLEDGEMENTS
We are grateful to the patients who gave their time freely to answer our questionnaire. We thank Dr Olafur Palsson for answering our queries about his study.
Declaration of personal interests: Vivek C. Goodoory: none. Cho Ee Ng: none. Christopher J. Black: none. Alexander C. Ford: none.
Declaration of funding interests: Unrestricted research monies were provided by Tillotts Pharma UK Ltd (Grant number: RG.GASS.124592). The funder had no input into the concept, design, analysis, or reporting of the study.
Goodoory VC, Ng CE, Black CJ, Ford AC. Impact of Rome IV irritable bowel syndrome on work and activities of daily living. Aliment Pharmacol Ther. 2022;56:844–856. 10.1111/apt.17132
The Handling Editor for this article was Dr Colin Howden, and it was accepted for publication after full peer‐review.
Funding informationUnrestricted research monies were provided by Tillotts Pharma UK Ltd (Grant number: RG.GASS.124592). The funder had no input into the concept, design, analysis, or reporting of the study.
REFERENCES
- 1. Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta‐analysis. Lancet Gastroenterol Hepatol. 2020;5(10):908–17. [DOI] [PubMed] [Google Scholar]
- 2. Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol Hepatol. 2016;1(2):133–46. [DOI] [PubMed] [Google Scholar]
- 3. Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, et al. Bowel disorders. Gastroenterology. 2016;150(6):1393–407. [DOI] [PubMed] [Google Scholar]
- 4. Black CJ, Drossman DA, Talley NJ, Ruddy J, Ford AC. Functional gastrointestinal disorders: advances in understanding and management. Lancet. 2020;396(10263):1664–74. [DOI] [PubMed] [Google Scholar]
- 5. Black CJ, Craig O, Gracie DJ, Ford AC. Comparison of the Rome IV criteria with the Rome III criteria for the diagnosis of irritable bowel syndrome in secondary care. Gut. 2021;70(6):1110–6. [DOI] [PubMed] [Google Scholar]
- 6. Black CJ, Burr NE, Camilleri M, Earnest DL, Quigley EM, Moayyedi P, et al. Efficacy of pharmacological therapies in patients with IBS with diarrhoea or mixed stool pattern: systematic review and network meta‐analysis. Gut. 2020;69(1):74–82. [DOI] [PubMed] [Google Scholar]
- 7. Black CJ, Burr NE, Quigley EMM, Moayyedi P, Houghton LA, Ford AC. Efficacy of Secretagogues in patients with irritable bowel syndrome with constipation: systematic review and network meta‐analysis. Gastroenterology. 2018;155(6):1753–63. [DOI] [PubMed] [Google Scholar]
- 8. Black CJ, Staudacher HM, Ford AC. Efficacy of a low FODMAP diet in irritable bowel syndrome: systematic review and network meta‐analysis. Gut. 2021;71:1117–26. 10.1136/gutjnl-2021-325214 [DOI] [PubMed] [Google Scholar]
- 9. Black CJ, Thakur ER, Houghton LA, Quigley EMM, Moayyedi P, Ford AC. Efficacy of psychological therapies for irritable bowel syndrome: systematic review and network meta‐analysis. Gut. 2020;69(8):1441–51. [DOI] [PubMed] [Google Scholar]
- 10. Black CJ, Yuan Y, Selinger CP, Camilleri M, Quigley EMM, Moayyedi P, et al. Efficacy of soluble fibre, antispasmodic drugs, and gut‐brain neuromodulators in irritable bowel syndrome: a systematic review and network meta‐analysis. Lancet Gastroenterol Hepatol. 2020;5(2):117–31. [DOI] [PubMed] [Google Scholar]
- 11. Ford AC, Forman D, Bailey AG, Axon AT, Moayyedi P. Irritable bowel syndrome: a 10‐yr natural history of symptoms and factors that influence consultation behavior. Am J Gastroenterol. 2008;103(5):1229–39. quiz 40. [DOI] [PubMed] [Google Scholar]
- 12. Pace F, Molteni P, Bollani S, Sarzi‐Puttini P, Stockbrugger R, Bianchi Porro G, et al. Inflammatory bowel disease versus irritable bowel syndrome: a hospital‐based, case‐control study of disease impact on quality of life. Scand J Gastroenterol. 2003;38(10):1031–8. [DOI] [PubMed] [Google Scholar]
- 13. Goodoory VC, Ng CE, Black CJ, Ford AC. Direct healthcare costs of Rome IV or Rome III‐defined irritable bowel syndrome in the United Kingdom. Aliment Pharmacol Ther. 2022;56:110–20. 10.1111/apt.16939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Drossman DA, Chang L, Schneck S, Blackman C, Norton WF, Norton NJ. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Dig Dis Sci. 2009;54(7):1532–41. [DOI] [PubMed] [Google Scholar]
- 15. Farndale R, Roberts L. Long‐term impact of irritable bowel syndrome: a qualitative study. Prim Health Care Res Dev. 2011;12(1):52–67. [DOI] [PubMed] [Google Scholar]
- 16. Jakobsson Ung E, Ringstrom G, Sjövall H, Simrén M. How patients with long‐term experience of living with irritable bowel syndrome manage illness in daily life: a qualitative study. Eur J Gastroenterol Hepatol. 2013;25(12):1478–83. [DOI] [PubMed] [Google Scholar]
- 17. Frandemark A, Tornblom H, Simren M, Jakobsson S. Maintaining work life under threat of symptoms: a grounded theory study of work life experiences in persons with irritable bowel syndrome. BMC Gastroenterol. 2022;22(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Frandemark A, Tornblom H, Jakobsson S, Simren M. Work productivity and activity impairment in irritable bowel syndrome (IBS): a multifaceted problem. Am J Gastroenterol. 2018;113(10):1540–9. [DOI] [PubMed] [Google Scholar]
- 19. Corney RH, Stanton R. Physical symptom severity, psychological and social dysfunction in a series of outpatients with irritable bowel syndrome. J Psychosom Res. 1990;34(5):483–91. [DOI] [PubMed] [Google Scholar]
- 20. Ballou S, Keefer L. The impact of irritable bowel syndrome on daily functioning: characterizing and understanding daily consequences of IBS. Neurogastroenterol Motil. 2017;29(4):e12982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. County Durham and Darlington NHS Foundation Trust . ContactME‐IBS [Internet]: County Durham and Darlington NHS Foundation Trust; 2021 [cited 2022 May 5]. 2021. Available from: https://www.contactme‐ibs.co.uk.
- 22. Goodoory VC, Ng CE, Black CJ, Ford AC. Willingness to accept risk with medication in return for cure of symptoms among patients with Rome IV irritable bowel syndrome. Aliment Pharmacol Ther. 2022;55:1311–9. 10.1111/apt.16816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Palsson OS, Whitehead WE, van Tilburg MA, Chang L, Chey W, Crowell MD, et al. Rome IV diagnostic questionnaires and tables for investigators and clinicians. Gastroenterology. 2016;150(6):1481–91. [DOI] [PubMed] [Google Scholar]
- 24. Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11(2):395–402. [DOI] [PubMed] [Google Scholar]
- 25. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. [DOI] [PubMed] [Google Scholar]
- 26. Spiller RC, Humes DJ, Campbell E, Hastings M, Neal KR, Dukes GE, et al. The patient health questionnaire 12 somatic symptom scale as a predictor of symptom severity and consulting behaviour in patients with irritable bowel syndrome and symptomatic diverticular disease. Aliment Pharmacol Ther. 2010;32(6):811–20. [DOI] [PubMed] [Google Scholar]
- 27. Kroenke K, Spitzer RL, Williams JB. The PHQ‐15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66. [DOI] [PubMed] [Google Scholar]
- 28. Labus JS, Bolus R, Chang L, Wiklund I, Naesdal J, Mayer EA, et al. The visceral sensitivity index: development and validation of a gastrointestinal symptom‐specific anxiety scale. Aliment Pharmacol Ther. 2004;20(1):89–97. [DOI] [PubMed] [Google Scholar]
- 29. Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43(2):400–11. [DOI] [PubMed] [Google Scholar]
- 30. Drossman DA, Patrick DL, Whitehead WE, Toner BB, Diamant NE, Hu Y, et al. Further validation of the IBS‐QOL: a disease‐specific quality‐of‐life questionnaire. Am J Gastroenterol. 2000;95(4):999–1007. [DOI] [PubMed] [Google Scholar]
- 31. Reilly MC, Bracco A, Ricci JF, Santoro J, Stevens T. The validity and accuracy of the work productivity and activity impairment questionnaire‐‐irritable bowel syndrome version (WPAI:IBS). Aliment Pharmacol Ther. 2004;20(4):459–67. [DOI] [PubMed] [Google Scholar]
- 32. Mundt JC, Marks IM, Shear MK, Greist JH. The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180:461–4. [DOI] [PubMed] [Google Scholar]
- 33. Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al. Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial. Health Technol Assess. 2006;10(19i):iii‐iv, ix‐x, 1–67. [DOI] [PubMed] [Google Scholar]
- 34. Moss‐Morris R, McAlpine L, Didsbury LP, Spence MJ. A randomized controlled trial of a cognitive behavioural therapy‐based self‐management intervention for irritable bowel syndrome in primary care. Psychol Med. 2010;40(1):85–94. [DOI] [PubMed] [Google Scholar]
- 35. Everitt HA, Landau S, O'Reilly G, Sibelli A, Hughes S, Windgassen S, et al. Assessing telephone‐delivered cognitive‐behavioural therapy (CBT) and web‐delivered CBT versus treatment as usual in irritable bowel syndrome (ACTIB): a multicentre randomised trial. Gut. 2019;68(9):1613–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Everitt HA, Landau S, O'Reilly G, Sibelli A, Hughes S, Windgassen S, et al. Cognitive behavioural therapy for irritable bowel syndrome: 24‐month follow‐up of participants in the ACTIB randomised trial. Lancet Gastroenterol Hepatol. 2019;4(11):863–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Palsson OS, Whitehead W, Tornblom H, Sperber AD, Simren M. Prevalence of Rome IV functional bowel disorders among adults in the United States, Canada, and the United Kingdom. Gastroenterology. 2020;158(5):1262–73 e3. [DOI] [PubMed] [Google Scholar]
- 38. United Kingdom Government . Age groups [Internet]. [London]: United Kingdom Government; 2020 [cited 2022 January 18]. 2020. Available from: https://www.ethnicity‐facts‐figures.service.gov.uk/uk‐population‐by‐ethnicity/demographics/age‐groups/latest.
- 39. Scotland's census . Census table data [internet]. [Edinburgh]: Scotland's Census; 2011 [cited 2022 January 21]. 2014. Available from: https://www.scotlandscensus.gov.uk/census‐results/download‐data/census‐table‐data/#section2.
- 40. Northern Ireland Statistics and Research Agency (NISRA) . 2011 Census ‐ Population Tables [Internet]. [Belfast]: NISRA; 2011 [cited 2022 January 21]. 2014. Available from: https://www.nisra.gov.uk/publications/2011‐census‐population‐tables.
- 41. Dean BB, Aguilar D, Barghout V, Kahler KH, Frech F, Groves D, et al. Impairment in work productivity and health‐related quality of life in patients with IBS. Am J Manag Care. 2005;11(1 Suppl):S17–26. [PubMed] [Google Scholar]
- 42. Pare P, Gray J, Lam S, Balshaw R, Khorasheh S, Barbeau M, et al. Health‐related quality of life, work productivity, and health care resource utilization of subjects with irritable bowel syndrome: baseline results from LOGIC (longitudinal outcomes study of gastrointestinal symptoms in Canada), a naturalistic study. Clin Ther. 2006;28(10):1726–35. discussion 10‐1. [DOI] [PubMed] [Google Scholar]
- 43. Buono JL, Carson RT, Flores NM. Health‐related quality of life, work productivity, and indirect costs among patients with irritable bowel syndrome with diarrhea. Health Qual Life Outcomes. 2017;15(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sainsbury A, Sanders DS, Ford AC. Prevalence of irritable bowel syndrome‐type symptoms in patients with celiac disease: a meta‐analysis. Clin Gastroenterol Hepatol. 2013;11(4):359–65.e1. [DOI] [PubMed] [Google Scholar]
- 45. Fairbrass KM, Costantino SJ, Gracie DJ, Ford AC. Prevalence of irritable bowel syndrome‐type symptoms in patients with inflammatory bowel disease in remission: a systematic review and meta‐analysis. Lancet Gastroenterol Hepatol. 2020;5(12):1053–62. [DOI] [PubMed] [Google Scholar]
- 46. Hookway C, Buckner S, Crosland P, Longson D. Irritable bowel syndrome in adults in primary care: summary of updated NICE guidance. BMJ. 2015;350:h701. [DOI] [PubMed] [Google Scholar]
- 47. Vasant DH, Paine PA, Black CJ, Houghton LA, Everitt HA, Corsetti M, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021;70(7):1214–40. [DOI] [PubMed] [Google Scholar]
- 48. Thandi G, Fear NT, Chalder T. A comparison of the work and social adjustment scale (WSAS) across different patient populations using Rasch analysis and exploratory factor analysis. J Psychosom Res. 2017;92:45–8. [DOI] [PubMed] [Google Scholar]
- 49. Ballou S, McMahon C, Lee HN, Katon J, Shin A, Rangan V, et al. Effects of irritable bowel syndrome on daily activities vary among subtypes based on results from the IBS in America survey. Clin Gastroenterol Hepatol. 2019;17(12):2471–8 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Goodoory VC, Mikocka‐Walus A, Yiannakou Y, Houghton LA, Black CJ, Ford AC. Impact of psychological comorbidity on the prognosis of irritable bowel syndrome. Am J Gastroenterol. 2021;116(7):1485–94. [DOI] [PubMed] [Google Scholar]
- 51. Parker CH, Naliboff BD, Shih W, Presson AP, Kilpatrick L, Gupta A, et al. The role of resilience in irritable bowel syndrome, other chronic gastrointestinal conditions, and the general population. Clin Gastroenterol Hepatol. 2021;19(12):2541–50 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Park SH, Naliboff BD, Shih W, Presson AP, Videlock EJ, Ju T, et al. Resilience is decreased in irritable bowel syndrome and associated with symptoms and cortisol response. Neurogastroenterol Motil. 2018;30(1):e13155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. de Jong M, de Boer AG, Tamminga SJ, Frings‐Dresen MH. Quality of working life issues of employees with a chronic physical disease: a systematic review. J Occup Rehabil. 2015;25(1):182–96. [DOI] [PubMed] [Google Scholar]
- 54. Drossman DA, Ruddy J. Improving patient‐provider relationships to improve health care. Clin Gastroenterol Hepatol. 2020;18(7):1417–26. [DOI] [PubMed] [Google Scholar]
- 55. Drossman DA, Chang L, Deutsch JK, Ford AC, Halpert A, Kroenke K, et al. A review of the evidence and recommendations on communication skills and the patient‐provider relationship: a Rome foundation working team report. Gastroenterology. 2021;161(5):1670–88 e7. [DOI] [PubMed] [Google Scholar]
- 56. Black CJ, Yiannakou Y, Guthrie E, West R, Houghton LA, Ford AC. Longitudinal follow‐up of a novel classification system for irritable bowel syndrome: natural history and prognostic value. Aliment Pharmacol Ther. 2021;53(10):1126–37. [DOI] [PubMed] [Google Scholar]
- 57. Talley NJ, Boyce PM, Jones M. Predictors of health care seeking for irritable bowel syndrome: a population based study. Gut. 1997;41(3):394–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Shah ED, Salwen‐Deremer JK, Gibson PR, Muir JG, Eswaran S, Chey WD. Comparing costs and outcomes of treatments for irritable bowel syndrome with diarrhea: cost‐benefit analysis. Clin Gastroenterol Hepatol. 2022;20(1):136–44 e31. [DOI] [PubMed] [Google Scholar]
- 59. Shah ED, Salwen‐Deremer JK, Gibson PR, Muir JG, Eswaran S, Chey WD. Pharmacologic, dietary, and psychological treatments for irritable bowel syndrome with constipation: cost utility analysis. MDM Policy Pract. 2021;6(1):2381468320978417. [DOI] [PMC free article] [PubMed] [Google Scholar]


