Abstract
Osteoporosis is the most common metabolic bone disease in the USA and the world. It is a subclinical condition until complicated by fracture(s). These fractures place an enormous medical and personal burden on individuals who suffer from them and take a significant economic toll. Any new fracture in an adult aged 50 years or older signifies imminent elevated risk for subsequent fractures, particularly in the year following the initial fracture. What a patient perceives as an unfortunate accident may be seen as a sentinel event indicative of bone fragility and increased future fracture risk even when the result of considerable trauma. Clinical or subclinical vertebral fractures, the most common type of osteoporotic fractures, are associated with a 5-fold increased risk for additional vertebral fractures and a 2- to 3-fold increased risk for fractures at other sites. Untreated osteoporosis can lead to a vicious cycle of recurrent fracture(s), often resulting in disability and premature death. In appropriate patients, treatment with effective antifracture medication prevents fractures and improves outcomes. Primary care providers and medical specialists are critical gatekeepers who can identify fractures and initiate proven osteoporosis interventions. Osteoporosis detection, diagnosis, and treatment should be routine practice in all adult healthcare settings. The Bone Health and Osteoporosis Foundation (BHOF) – formerly the National Osteoporosis Foundation – first published the Clinician’s Guide in 1999 to provide accurate information on osteoporosis prevention and treatment. Since that time, significant improvements have been made in diagnostic technologies and treatments for osteoporosis. Despite these advances, a disturbing gap persists in patient care. At-risk patients are often not screened to establish fracture probability and not educated about fracture prevention. Most concerning, the majority of highest risk women and men who have a fracture(s) are not diagnosed and do not receive effective, FDA-approved therapies. Even those prescribed appropriate therapy are unlikely to take the medication as prescribed. The Clinician’s Guide offers concise recommendations regarding prevention, risk assessment, diagnosis, and treatment of osteoporosis in postmenopausal women and men aged 50 years and older. It includes indications for bone densitometry as well as fracture risk thresholds for pharmacologic intervention. Current medications build bone and/or decrease bone breakdown and dramatically reduce incident fractures. All antifracture therapeutics treat but do not cure the disease. Skeletal deterioration resumes sooner or later when a medication is discontinued—sooner for nonbisphosphonates and later for bisphosphonates. Even if normal BMD is achieved, osteoporosis and elevated risk for fracture are still present. The diagnosis of osteoporosis persists even if subsequent DXA T-scores are above − 2.5. Ongoing monitoring and strategic interventions will be necessary if fractures are to be avoided. In addition to pharmacotherapy, adequate intake of calcium and vitamin D, avoidance of smoking and excessive alcohol intake, weight-bearing and resistance-training exercise, and fall prevention are included in the fracture prevention armamentarium. Where possible, recommendations in this guide are based on evidence from RCTs; however, relevant published data and guidance from expert clinical experience provides the basis for recommendations in those areas where RCT evidence is currently deficient or not applicable to the many osteoporosis patients not considered for RCT participation due to age and morbidity.
Keywords: Fractures; FRAX®; Osteoporosis; Primary care management of osteoporosis; Vertebral imaging; Fracture risk stratification; Bisphosphonate holiday; Novel antifracture therapies (romosozumab, denosumab, abaloparatide)
Synopsis of major recommendations to the clinician
These recommendations apply to postmenopausal women and men aged 50 years and older.
Universal recommendations
Counsel individual patients on their risk for osteoporosis, fractures, and potential consequences of fractures (functional deterioration, loss of independence, increased mortality).
Recommend a diet with adequate total calcium intake (1000 mg/day for men aged 50–70 years; 1200 mg/day for women ≥ 51 years and men ≥ 71 years), incorporating calcium supplements if intake is insufficient.
Monitor serum 25-hydroxyvitamin D levels.
Maintain serum vitamin D sufficiency (≥ 30 ng/mL but below ≤ 50 ng/mL) [1–3]. Prescribe supplemental vitamin D (800–1000 units/day) as needed for individuals aged 50 years and older to achieve a sufficient vitamin D level. Higher doses may be necessary in some adults, especially those with malabsorption. (Note: in healthy individuals a serum 25(OH) vitamin D level ≥ 20 ng/mL may be sufficient, but in the setting of known or suspected metabolic bone disease ≥ 30 ng/mL is appropriate.)
Identify and address modifiable risk factors associated with falls, such as sedating medications, polypharmacy, hypotension, gait or vision disorders, and out-of-date prescription glasses.
Provide guidance for smoking cessation, and avoidance of excessive alcohol intake; refer for care as appropriate.
Counsel or refer patients for instruction on balance training, muscle-strengthening exercise, and safe movement strategies to prevent fracture(s) in activities of daily life.
In community-dwelling patients, refer for at-home fall hazard evaluation and remediation.
In post-fracture patients who are experiencing pain, prescribe over-the-counter analgesia, heat/ice home care, limited bed rest, physical therapy, and alternative non-pharmacologic therapies when appropriate. In cases of intractable or chronic pain, refer to a pain specialist or physiatrist.
Coordinate post-fracture patient care via fracture liaison service (FLS) and multidisciplinary programs in which patients with recent fractures are referred for osteoporosis evaluation and treatment, rehabilitation, and transition management.
Diagnostic assessment recommendations
Investigate any broken bone in adulthood as suspicious for osteoporosis, regardless of cause [4, 5].
Measure height annually, preferably with a wall-mounted stadiometer (without shoes).
Record history of falls.
Perform BMD testing in the following:
–Women aged ≥ 65 years and men aged ≥ 70 years.
–Postmenopausal women and men aged 50–69 years, based on risk profile.
–Postmenopausal women and men aged ≥ 50 years with history of adult-age fracture.
–DXA facilities that employ accepted quality assurance measures.
–The same facility and on the same densitometry device for each test whenever possible.
Maintain diagnosis of osteoporosis in patient diagnosed by fracture in adulthood or T-score (− 2.5 or below), even if subsequent DXA T-score is above − 2.5.
To detect subclinical vertebral fractures, perform vertebral fracture imaging (X-ray or DXA vertebral fracture assessment) in the following:
–Women aged 65 years and older if T-score is less than or equal to − 1.0 at the femoral neck [6].
–Women aged 70 years or older and men aged 80 years or older if T-score is less than or equal to − 1.0 at the lumbar spine, total hip, or femoral neck.
–Men aged 70–79 years if T-score is less than or equal to − 1.5 at the lumbar spine, total hip, or femoral neck.
–Postmenopausal women and men aged ≥ 50 years with the following specific risk factors:
○Fracture(s) during adulthood (any cause).
○Historical height loss of ≥ 1.5 in. (defined as the difference between the current height and peak height) [7].
○Prospective height loss of ≥ 0.8 in. (defined as the difference between the current height and last documented height measurement) [7].
○Recent or ongoing long-term glucocorticoid treatment.
○Diagnosis of hyperparathyroidism [8].
Rule out secondary causes of bone loss, osteoporosis, and/or fractures.
In appropriate untreated postmenopausal women, selectively measure bone turnover markers to help gauge rapidity of bone loss.
Prior to elective orthopedic procedures, evaluate skeletal health and measure BMD as indicated by risk profile (e.g., inflammatory arthritis, osteoarthritis, chronic kidney disease, or adverse events from surgery or other risk factors) [9–11].
Pharmacologic treatment recommendations
No uniform recommendation applies to all patients. Management plans must be individualized.
Current FDA-approved pharmacologic options for osteoporosis are as follows:
–Bisphosphonates (alendronate, ibandronate, risedronate, zoledronic acid)
–Estrogen-related therapy (ET/HT, raloxifene conjugated estrogens/ bazedoxifene)
–Parathyroid hormone analogs (teriparatide, abaloparatide)
–RANK-ligand inhibitor (denosumab)
–Sclerostin inhibitor (romosozumab)
–Calcitonin salmon
Consider initiating pharmacologic treatment in postmenopausal women and men ≥ 50 years of age who have the following:
–Primary fracture prevention:
○T-score ≤ − 2.5 at the femoral neck, total hip, lumbar spine, 33% radius (some uncertainty with existing data) by DXA.
○Low bone mass (osteopenia: T-score between − 1.0 and − 2.5) at the femoral neck or total hip by DXA with a 10-year hip fracture risk ≥ 3% or a 10-year major osteoporosis-related fracture risk ≥ 20% (i.e., clinical vertebral, hip, forearm, or proximal humerus) based on the US-adapted FRAX® model.
–Secondary fracture prevention:
○Fracture of proximal humerus, pelvis, or distal forearm in persons with low bone mass (osteopenia: T-score between − 1.0 and − 2.5). The decision to treat should be individualized in persons with a fracture of the proximal humerus, pelvis, or distal forearm who do not have osteopenia or low BMD [12, 13].
Initiate antiresorptive therapy following discontinuation of denosumab, teriparatide, abaloparatide, or romosozumab.
Monitoring patients and treatment response
Perform BMD testing 1 to 2 years after initiating or changing medical therapy for osteoporosis and at appropriate intervals thereafter according to clinical circumstances.
–More frequent BMD testing may be warranted in higher-risk individuals (multiple fractures, older age, very low BMD).
–Less frequent BMD testing may be warranted as follow-up for patients with initial T-scores in the normal or slightly below normal range (osteopenia) and for patients who have remained fracture free on treatment.
In patients receiving osteoporosis pharmacologic treatment:
–Routinely reassess risk for fracture, patient satisfaction and adherence with therapy, and need for continued or modified treatment. The appropriate interval between initiation and reassessment differs with agent prescribed.
–Serially measure changes in BMD at lumbar spine, total hip, or femoral neck; if lumbar spine, hip, or both are not evaluable or according to clinical judgment, consider monitoring at 33% distal radius.
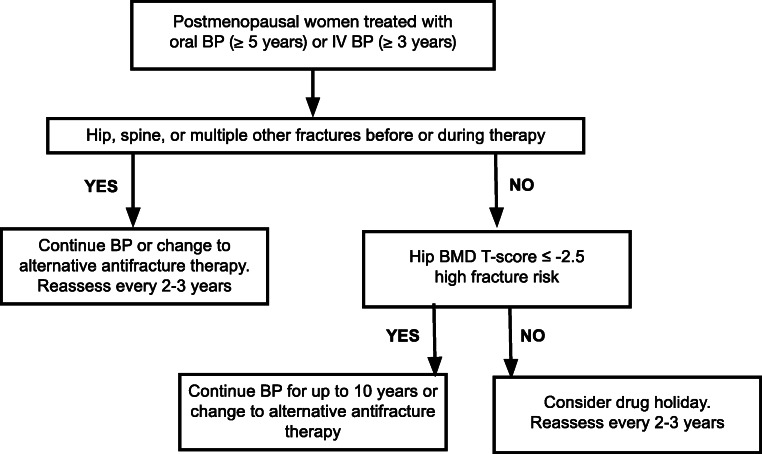
–Reassess patient and BMD status for consideration of a drug holiday after 5 years of oral and 3 years of intravenous bisphosphonate in patients who are no longer at high risk of fracture (T-score ≥ − 2.5, no new fractures) [14].
–At each healthcare encounter, ask open-ended questions about treatment to elicit patient feedback on possible side effects and concerns. Communicate risk-benefit trade-offs and confirm understanding: both the risk of adverse events with treatment (usually very low) and risk of fractures and their negative consequences without treatment (usually much higher).
Osteoporosis: impact and overview
Osteoporosis is a disease characterized by low bone density, deterioration of bone tissue, disrupted bone microarchitecture, compromised bone strength, and fracture. According to the World Health Organization (WHO) diagnostic classification, osteoporosis is defined by BMD at the hip or lumbar spine that is less than or equal to 2.5 standard deviations below the mean BMD of a young adult reference population (T-score).
Osteoporosis is a risk factor for fracture, just as hypertension is for stroke and hypercholesterolemia is for heart disease. While risk is highest in individuals with extremely low BMD, the majority of fractures occur in patients with T-scores better than − 2.5. Non-BMD factors contribute to fracture risk, such as falls, frailty, and poor bone quality.
Scope of the problem
Osteoporosis affects an enormous number of people, both men and women, of all races. Among Caucasian adults in the USA aged 50 years and older, about 50% of women and 20% of men will experience an osteoporotic fracture in their remaining lifetime [15]. Rates of fracture differ by ethnic/racial population and skeletal site.
For fracture at any site in women, after adjusting for BMD, weight, and other covariates, non-Hispanic white and Hispanic-American women have the highest risk for fracture, followed by Native Americans, African Americans, and Asian Americans [16, 17]. For hip fracture in men, the age-adjusted incidence was highest for non-Hispanic white men, similar among Hispanic-American and black men, and lowest in Asian men.
In a 2014 cross-sectional analysis of data from five large independent cohorts (in the USA and Asia), prevalence of self-reported non-traumatic fracture in men was non-Hispanic white American 17.1%; Afro-Caribbean, 5.5%; African American, 15.1%; Hispanic-American, 13.7%; Asian American, 10.5%; Hong Kong Chinese, 5.6%, and Korean, 5.1% [18] .
Many factors are thought to contribute to these divergent fracture rates including BMD, cortical thickness, access to healthcare, comorbidities (such as diabetes), and skeletal geometry (e.g., hip axis length) [20]. Fracture rates do not track uniformly with the risk of osteoporosis among different racial/ethnic groups. For example, while fewer African Americans have osteoporosis, those diagnosed with osteoporosis experience fracture rates comparable to Non-Hispanic Whites and experience worse overall post-fracture outcomes [19]. Native Americans have BMD similar to Non-Hispanic Whites but higher rates of hip fracture, possibly reflecting challenges with screening, nutrition, lifestyle, and follow-up (Fig. 1).
Fig. 1.
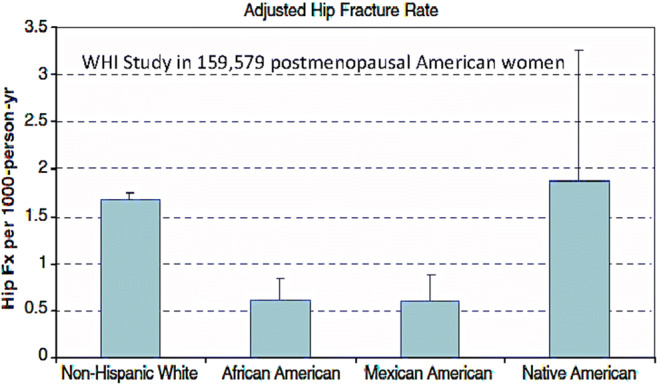
Hip fracture incidence in postmenopausal women across ethic/racial populations in WHI data (from Nelson DA et al. Osteoporos Int. 2011) [19]
Based on data from the National Health and Nutrition Examination Survey III (NHANES III), BHOF previously estimated that more than 10.2 million Americans have osteoporosis and an additional 43.4 million have low bone density [21]. Prevalence of fractures continues to increase as the population ages. It is currently projected that 12.3 million Americans have osteoporosis [22]. At present the 2 million new cases of osteoporotic fracture per year exceeds the annual number of new cases of myocardial infarction, breast cancer, and prostate cancer combined [23–25]. Annual fracture incidence is expected to increase 68%, to 3.2 million by 2040 [26].
Osteoporosis remains a disease that is underdiagnosed and undertreated despite effective antifracture interventions and the potentially lethal consequences of fractures [27]. Hip fractures significantly increase risk of death in the year following fracture and are highly predictive of additional fractures. Nonetheless, as many as 80–95% of patients in some practice settings are discharged following hip fracture repair with no antifracture treatment or management plan [28–30].
Crisis in osteoporosis patient care
The benefits of timely diagnosis and treatment have been well documented. Treatment reduces fracture incidence, forestalling injury, disability, and excess mortality. This effect is seen in Medicare claims analyses demonstrating a significant drop in age-adjusted risk for hip fracture in the ten years between 2002 and 2012. This decade-long decline coincided with the advent of bone density testing and application of effective osteoporosis therapies.
However, after declining for decades, incidence rates plateaued between 2013 and 2015 (Fig. 2) [31]. Although more data are needed to draw causal conclusions, it is likely that multiple factors have contributed. In the USA, patient access to osteoporosis care has declined. There are fewer office-based DXA facilities performing smaller numbers of DXA studies. Fewer women and men are diagnosed with osteoporosis and/or treated to prevent fractures. Not surprisingly, we have seen an uptick in fractures.
Fig. 2.
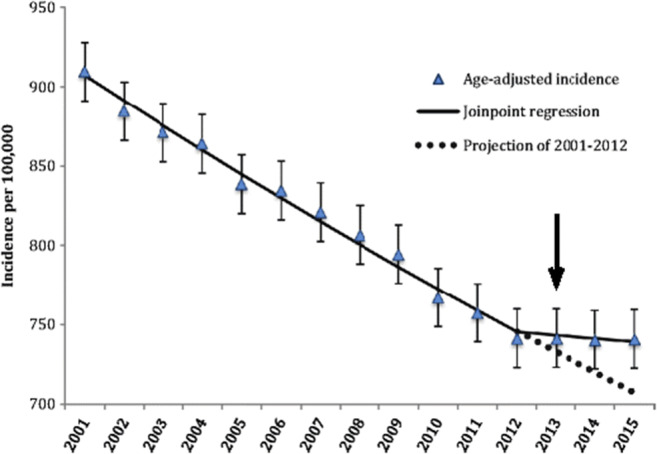
Incidence of hip fractures (age-adjusted) between 2002 and 2015 according to Medicare claims. Note the decade-long decline in hip fractures and plateau between the years 2013 to 2015. (Lewiecki EM, et al. [2018] Osteoporos Int. Reprinted with added arrow by permission of author.) [31]
The osteoporosis treatment gap (difference between number meeting treatment indications and number receiving treatment) is recognized globally as a crisis in patient care [21, 32, 33]. Since many factors contribute to this crisis, multifactorial approaches should be considered to reverse the trend, including cultivating trust in at-risk patients; generating more data on comparative effectiveness and safety of current osteoporosis drugs; engaging physicians, governmental, and public health organizations; improving insurance coverage for key fracture prevention services, including FLS programs; and adopting quality measures to incentivize clinicians, hospitals, and health systems to routinely screen and treat high-risk patients.
Medical impact
Fractures and their complications are the clinical sequelae of osteoporosis. The most common fractures are those of the vertebrae (lumbar spine), proximal femur (hip), and distal forearm (wrist). Most fractures in older adults are due at least in part to low bone mass, even when they result from considerable trauma. All fractures are associated with some degree of low BMD and increased risk of subsequent fracture in older adults [5]. In fact, a large cohort study found high-trauma and low-trauma fractures to be comparably predictive of low BMD and elevated future fracture risk [4].
A recent fracture at any major skeletal site in an adult ≥ 50 years of age should be considered a sentinel event that indicates urgent need for further assessment and treatment. Fractures of fingers, toes, face, and skull are not considered osteoporotic fractures since they are typically traumatic and unrelated to bone fragility.
Fractures may be followed by full recovery or by chronic pain, disability, and premature death. Hip, vertebral, and distal radius fractures lead to a substantial reduction in quality of life, with the greatest hardship among hip fracture patients [34]. Low-energy fractures of the pelvis and/or humerus are common in people with osteoporosis and contribute to increased morbidity and mortality. Psychosocial symptoms, most notably depression and loss of self-esteem, are common consequences of fracture, as patients grapple with pain, physical limitations, and loss of independence.
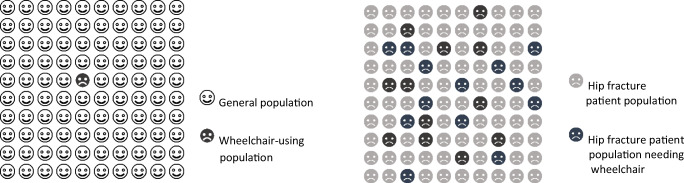
Hip fractures
Hip fractures are associated with 8.4–36% excess mortality at 1 year, with higher mortality in men than in women [26, 35]. Hip fracture can have devastating impacts on a patient’s life. Approximately 20% of hip fracture patients require long-term nursing home care, and 60% do NOT fully regain pre-fracture independence [27]. In addition, hip fractures are associated with a 2.5-fold increased incidence of secondary fractures [36].
Vertebral fractures
Although the majority of vertebral fractures are subclinical, they can cause pain, disability, deformity, and premature death [37]. Pain and postural changes associated with multiple vertebral compression fractures (kyphosis) can limit mobility and independent function, resulting in significantly diminished quality of life [38]. Multiple thoracic fractures can cause restrictive lung disease. Lumbar fractures can alter abdominal anatomy, leading to constipation, abdominal pain, early satiety, and weight loss. Vertebral fractures, whether clinically apparent or silent, are associated with a 5-fold increased risk for additional vertebral fractures and a 2- to 3-fold increased risk for fractures at other sites.
Wrist fractures
Wrist fractures are five times more common in women than men. They tend to occur earlier in life than other fractures (i.e., between 50 and 60 years of age). When wrist fractures are recognized as evidence of bone fragility and appropriate osteoporosis treatment is prescribed, future fractures could be avoided. While less disabling than hip or vertebral fractures, wrist fractures can be equally detrimental to quality of life, causing pain and limiting activities necessary for independent living.
Wrist fractures are strongly predictive of future fractures, as demonstrated in longitudinal studies of women in the Women’s Health Initiative (WHI) and men in the Osteoporotic Fractures in Men Study (MrOs) [39–41]. Among recipients of Medicare, increased risk of other fractures following a wrist fracture (regardless of BMD) is comparable to risk following hip or spine fracture in the year after the index event [12]. Low BMD at spine, hip, or forearm is a risk factor for wrist fractures in women and men; however, BMD alone is an imperfect predictor of fracture. In women with forearm fractures, advanced imaging with high-resolution peripheral quantitative computed tomography (HR-pQCT) has identified poor bone quality in fracturing women and girls compared with their nonfracturing peers at similar BMDs: lower total and trabecular bone density, decreased trabecular number and thickness, and lower cortical density and thickness. These differences in bone quality remained after adjusting for age and BMD at the hip and 33% radius [42].
Unfortunately, rates of evaluation and treatment for osteoporosis after wrist fractures are low in women and even lower in men [43]. Seventy-nine percent of adult male wrist fracture patients in one prospective, randomized study did not receive a bone density test following fracture repair [44]. This is significant because patients who received BMD measurement were more likely to be prescribed effective antifracture therapy.
As the population ages, it is critical for clinicians to intervene after a sentinel fracture. Appropriate, timely intervention offers the best opportunity to prevent the cycle of recurrent fractures, disability, and premature death in these patients [45].
Economic toll
The personal and economic costs of fractures are enormous. Fractures result in more than 432,000 hospital admissions, almost 2.5 million medical office visits, and about 180,000 nursing home admissions in the US [26]. Annual fracture-related costs are expected to increase from $57 billion to over $95 billion by 2040 [26]. This heavy toll could be significantly reduced with routine use of effective treatments and screenings, including VFA in women aged 65 and older with osteopenia (T-score ≤ − 1.0) [23, 27].
Basic pathophysiology
The human skeleton is comprised of living tissue. Critical to locomotion, skeletal bone houses much of the hematopoietic system and is the major repository for calcium and phosphorus—minerals essential to multiple physiologic systems. Constant serum calcium and adequate cellular calcium and phosphorus are maintained by a complex system of regulatory hormones that act directly on bone and indirectly on other tissues, such as the intestine and kidney. These demands can challenge skeletal equilibrium. When inadequate mineral is present in serum, it is withdrawn from skeletal stores. Over time, continued removal of bone tissue degrades skeletal microarchitecture thereby elevating risk for fractures that occur spontaneously or from minimal trauma.
Skeletal lifecycle
During childhood and adolescence, bones undergo a process called modeling, during which new bone is formed at one site and old bone is removed from another site within the same bone. This process enables individual bones to develop in size, shape, and position. Childhood and adolescence are critical periods of skeletal accrual. This is particularly important for girls, who acquire 40–50% of their total bone mass during early teen years.
During rapid skeletal growth in childhood and adolescence, it takes several months to mineralize the protein scaffolding for new bone, called osteoid. This lag between formation and mineralization produces periods of relatively low bone density and increased propensity to fracture, particularly between ages 10 and 14 years [46]. In the early 20s, fracture rates level off with attainment of peak bone mass. Mineral density stabilizes in most adults by their early 40s, when it begins a gradual decline, which accelerates at menopause in women (~ 2%/year for the 10 years following menopause) [47]. Age-related bone loss thins trabecular bone and increases cortical porosity, creating the preconditions for future fragility and fractures.
Genetic factors appear to account for 60-80% of total adult bone mass [48]. Substantial contributions are made by multiple modifiable factors that include nutrition, physical activity, smoking, chronic illness, and bone-damaging medications. Suboptimal bone acquisition is associated with fracture earlier in adulthood. Conversely, high peak adult bone mass, all other things being equal, protects against osteoporosis later in life.
Bone remodeling
The skeleton responds dynamically to hormonal, mechanical, and pharmacologic stimuli through the resorption and formation processes of bone remodeling, or turnover. After epiphyseal closure, the skeleton repairs damage through bone remodeling, which occurs on bone surfaces throughout the skeleton. The majority of bone surface area resides in trabecular bone, the resilient bony latticework predominantly found inside vertebrae. Remodeling is initiated by bone-resorbing cells, osteoclasts, that breakdown and remove damaged bone in a process called resorption. Excavated bone is replaced with new bone produced by osteoblasts.
The mechanisms that regulate bone formation involve complex interactions but are mediated, in part, by cells called osteocytes. Osteocytes play a role in both bone modeling and remodeling. For example, at sites of specific mechanical strain, osteocytes produce less sclerostin, a cytokine and powerful inhibitor of bone formation. The result is stimulation of new bone formation. In several RCTs, a fully human neutralizing sclerostin antibody drug called romosozumab has blocked sclerostin, thereby markedly increasing bone formation and decreasing bone resorption [49].
Osteocytes make RANK-ligand (RANKL) a cytokine required for osteoclast formation. The fully human monoclonal antibody to RANKL, denosumab, is a potent antiresorptive drug that directly inhibits osteoclast formation, causes apoptosis of mature osteoclasts, and leads to decreased bone resorption and higher BMD. In addition to these agents, the anabolic PTH analogs (teriparatide and abaloparatide) affect remodeling- and modeling-based bone formation, leading to a net increase in BMD (see US FDA-Approved Drugs for Osteoporosis).
Pathogenesis of osteoporosis
In healthy young adults, the bone turnover cycle is balanced such that resorption is matched by formation. Bone remodeling accelerates in settings of chronic disease, aging, and a variety of mechanical, hormonal, and biochemical exposures such as glucocorticoids. Over time, this process leads to greater and greater deficits in mineralized bone.
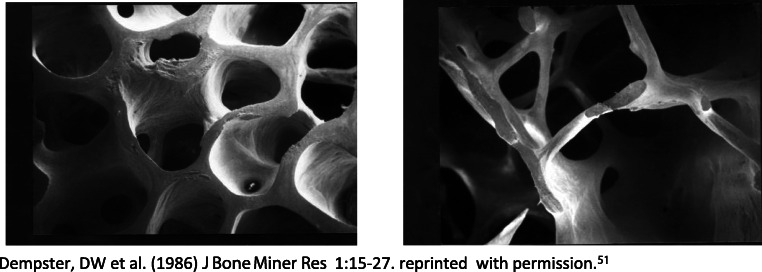
Accelerated bone turnover affects cortical and trabecular bone somewhat differently. Bone resorption takes place on the surface of the bone. Because of its higher ratio of surface area to mass, trabecular bone is depleted more rapidly than cortical bone. With each remodeling cycle, there is a net loss of bone tissue. When bone remodeling rates increase—for example, in the setting of estrogen deficiency at menopause—bone loss is seen first at skeletal sites rich in trabecular bone, such as the spine, while sites that have a mix of cortical and trabecular bone, such as the hip, develop clinically apparent loss of bone later (Fig. 3).
Fig. 3.
Micrographs of normal (left) and osteoporotic (right) bone. As trabecular mineral is depleted, individual bony plates and connecting branches are lost, leaving less resilient, weaker bone that is more likely to fail under normally tolerated mechanical loads. Dempster, DW et al. (1986) J Bone Miner Res 1:15-27. Reprinted with permission [50]
Diagnostic considerations
BHOF recommends a multimodal, comprehensive approach to diagnosis of osteoporosis: detailed assessment of individual fracture risk, personal and family history, physical examination, and in patients with suggestive presentations (such as height loss, back pain, and/or fractures), focused studies to rule out secondary causes of bone fragility and vertebral imaging to detect prevalent fractures.
This is a process of screening and evaluation. Fracture risk increases exponentially with age and BMD declines with age. Screening of all older persons on this basis is appropriate. In persons with fractures or conditions associated with elevated fracture risk, more detailed evaluation is needed to monitor and manage their skeletal health. Referral to a metabolic bone specialist may be appropriate [51].
Fracture risk assessment
All postmenopausal women and men aged 50 years and older should be evaluated for osteoporosis risk in order to determine need for BMD testing and/or vertebral imaging. In general, the more risk factors, the more likely a patient will break a bone.
Osteoporotic fractures are preventable. Even after a fracture, osteoporosis is treatable. However, because there are no warning signs, many people with osteoporosis are not diagnosed until a fracture occurs. Factors that have been associated with an increased risk of osteoporosis-related fracture are listed in Table 1. Primary among these is history of broken bones in adulthood, with highest risk in first 1–2 years after the initial fracture [52, 53]. Patients must be evaluated soon after a fracture and receive appropriate treatments to optimize risk reduction.
Table 1.
Conditions, diseases, and medications that cause or contribute to osteoporosis and/or fractures.
| Lifestyle factors | ||
| Alcohol abuse | Excessive thinness | Excess vitamin A |
| Frequent falling | High salt intake | Immobilization |
| Inadequate physical activity | Low calcium intake | Smoking (active or passive) |
| Vitamin D insufficiency/deficiency | ||
| Genetic diseases | ||
| Cystic fibrosis | Ehlers-Danlos | Gaucher’s disease |
| Hemochromatosis | Hypophosphatasia | Hypophosphatemia |
| Marfan syndrome | Menkes steely hair syndrome | Osteogenesis imperfecta |
| Parental history of hip fracture | Porphyria | Homocystinuria |
| Hypogonadal states | ||
| Anorexia nervosa | Androgen insensitivity | Female athlete triad |
| Hyperprolactinemia | Hypogonadism | Panhypopituitarism |
| Premature menopause (< 40 years) | Turner’s and Klinefelter’s syndromes | |
| Endocrine disorders | ||
| Obesity | Cushing’s syndrome | Diabetes mellitus (types 1 and 2) |
| Hyperparathyroidism | Thyrotoxicosis | |
| Gastrointestinal disorders | ||
| Celiac disease | Bariatric surgery | Gastric bypass |
| Gastrointestinal surgery | Inflammatory bowel disease including Crohn’s disease and ulcerative colitis | Malabsorption syndromes |
| Pancreatic disease | Primary biliary cirrhosis | |
| Hematologic disorders | ||
| Hemophilia | Leukemia and lymphomas | Monoclonal gammopathies |
| Multiple myeloma | Sickle cell disease | Systemic mastocytosis |
| Thalassemia | ||
| Rheumatologic and autoimmune diseases | ||
| Ankylosing spondylitis | Other rheumatic and autoimmune diseases | |
| Rheumatoid arthritis | Systemic lupus | |
| Neurological and musculoskeletal risk factors | ||
| Epilepsy | Muscular dystrophy | Multiple sclerosis |
| Parkinson’s disease | Spinal cord injury | Stroke |
| Miscellaneous conditions and diseases | ||
| HIV/AIDS | Amyloidosis | Chronic metabolic acidosis |
| Chronic obstructive lung disease | Congestive heart failure | Depression |
| Renal disease (CKD III, CKD IV, CKD V/ESRD) | Hypercalciuria | Idiopathic scoliosis |
| Post-transplant bone disease | Sarcoidosis | Weight loss |
| Hyponatremia | ||
| Medications | ||
| Aluminum-containing antacids | Androgen deprivation therapy | Anticoagulants (unfractionated heparin) |
| Anticonvulsants (e.g., phenobarbital, phenytoin, valproate) | Aromatase inhibitors | Barbiturates |
| Cancer chemotherapeutic drugs | Cyclosporine A and tacrolimus | Glucocorticoids (≥ 5.0 mg/day prednisone or equivalent for ≥ 3 months) |
| GnRH (gonadotropin-releasing hormone) agonists and antagonists | Medroxyprogesterone acetate | Methotrexate |
| Parenteral nutrition | Proton pump inhibitors | Selective serotonin reuptake inhibitors |
| Tamoxifen (premenopausal use for breast cancer treatment) | Thiazolidinediones (such as pioglitazone and rosiglitazone) | Thyroid replacement hormone (in excess) |
Most fractures in older adults are associated with a fall. Falls occur in approximately one third of adults aged 65 years and older and this risk increases with age. Fall risk assessment is, therefore, a key component of primary and secondary fracture prevention. Factors associated with falls are shown in Table 2. The most important of these are history of falling, muscle weakness, gait and balance disturbances, sedating or hypnotic medications, visual impairment, and any condition associated with dizziness, such as dehydration and orthostatic hypotension [55, 56]. Importantly, multiple studies have demonstrated the safety and efficacy of physical therapy and exercise regimens targeted to fall risk reduction.
Table 2.
Major risk factors for falls
| Medical risk factors | |
| •Advanced age | |
| •Arthritis | |
| •Female gender | |
| •Poor vision | |
| •Urinary urgency or incontinence | |
| •Previous fall | |
| •Orthostatic hypotension | |
| •Impaired transfer and mobility | |
| •Medications that cause dizziness or sedation (narcotic analgesics, anticonvulsants, psychotropics) | |
| •Malnutrition/parenteral nutrition (vitamin D deficiency, insufficient protein) | |
| Neurological and musculoskeletal risk factors | |
| •Poor balance | |
| •Weak muscles/sarcopenia | |
| •Gait disturbances | |
| •Kyphosis (abnormal spinal curvature) | |
| •Reduced proprioception | |
| •Diseases and/or therapies that cause sedation, dizziness, weakness, or lack of coordination | |
| •Alzheimer’s/other dementia, delirium, Parkinson disease, and stroke | |
| Environmental risk factors | |
| •Low-level lighting | |
| •Obstacles in the walking path | |
| •Loose throw rugs | |
| •Stairs | |
| •Lack of assistive devices in bathrooms | |
| •Slippery outdoor conditions | |
| Psychological risk factors | |
| •Anxiety and agitation | |
| •Depression | |
| •Diminished cognitive acuity | |
| •Fear of falling |
From: Health professional’s guide to the rehabilitation of the patient with osteoporosis [54]
Evaluation of patients with fractures
In patients aged 50 years or older, consider hip, vertebral, and/or forearm fractures to be highly suggestive of osteoporosis or other metabolic bone disease, unless excluded by clinical evaluation and imaging. Risk for fracture at all sites rises substantially in the period immediately following an initial fracture. Therefore, any fracture in adulthood should be viewed as a red flag signaling urgent need for focused attention [57].
Secondary skeletal etiologies should be investigated in all patients who present with fractures, low bone mass, or osteoporosis (Table 3). Chronic kidney disease, hyperparathyroidism, osteomalacia, and other diseases can cause skeletal fragility, multiple vertebral fractures, and very low bone density. For some metabolic bone diseases, osteoporosis therapies are not appropriate and may be harmful (e.g., osteomalacia or aplastic bone disease). Relevant blood and urine studies (Table 3) to rule out secondary etiologies should be obtained prior to initiating antifracture therapy. Patients found to have secondary, treatable causes of bone fragility may require no additional therapy once the underlying condition is addressed (Table 1).
Table 3.
Exclusion of secondary causes of osteoporosis
| Diagnostic studies for secondary causes of osteoporosis | |
| Blood or serum | |
| 1 Complete blood count (CBC) | |
| 2 Albumin | |
| 3 Chemistry levels (albumin-adjusted calcium, renal function, phosphorus, and magnesium) | |
| 4 Liver function tests | |
| 5 25(OH) vitamin D | |
| 6 Parathyroid hormone (PTH) | |
| 7 Total testosterone and gonadotropin (men aged 50–69 years) | |
| Consider in select patients | |
| •Serum protein electrophoresis (SPEP), serum immunofixation, serum free kappa and lambda light chains | |
| •Thyroid-stimulating hormone (TSH) +/− free T4 | |
| •Tissue transglutaminase antibodies (and IgA levels) | |
| •Iron and ferritin levels | |
| •Homocysteine (to evaluate for homocystinuria) | |
| •Prolactin level | |
| •Tryptase | |
| •Biochemical markers of bone turnover | |
| Urine | |
| 1 24-h urinary calcium and creatinine | |
| Consider in select patients | |
| •Protein electrophoresis (UPEP) and kappa and lambda light chains | |
| •Salivary cortisol and/or Urinary free cortisol level | |
| •Urinary histamine |
Osteoporosis affects a significant number of men, yet largely goes undetected and untreated. Some of the laboratory testing to assess secondary etiologies in men differs from that in women. Screening BMD and vertebral imaging recommendations are outlined in Tables 6 and 7. For additional guidance, readers should refer to Osteoporosis in Men: an Endocrine Society Clinical Practice Guideline, which provides a detailed approach to evaluation and treatment of osteoporosis in men [58].
Table 6.
Indications for BMD testing
| Consider BMD testing in the following individuals | |
| Women ≥ 65 years of age and men ≥ 70 years of age, regardless of clinical risk factors | |
| Younger postmenopausal women, women in the menopausal transition, and men aged 50 to 69 years with clinical risk factors for fracture | |
| Adults who have a fracture at age 50 years and older | |
| Adults with a condition (e.g., rheumatoid arthritis, organ transplant) or taking a medication (e.g., glucocorticoids, aromatase inhibitors, androgen deprivation therapy) associated with low bone mass or bone loss |
Table 7.
Indications for vertebral imaging
| Consider vertebral imaging tests for the following individuals*** | |
| •All women aged ≥ 65 years and all men aged ≥ 80 years if T-score at the lumbar spine, total hip, or femoral neck is ≤ − 1.0 [6]. | |
| •Men aged 70 to 79 years if T-score at the lumbar spine, total hip, or femoral neck is ≤ − 1.5 | |
| •Postmenopausal women and men age ≥ 50 years with specific risk factors: | |
| °Fracture during adulthood (age ≥ 50 years) | |
| °Historical height loss of 1.5 in. or more* | |
| °Prospective height loss of 0.8 in. or more** | |
| °Recent or ongoing long-term glucocorticoid treatment | |
| °Medical conditions associated with bone loss such as hyperparathyroidism |
*Current height compared to peak height during young adulthood
**Cumulative height loss measured during interval medical assessment
***If bone density testing is not available, vertebral imaging may be considered based on age alone
Bone mineral density (BMD) measurement and classification
DXA measurement of hip and lumbar spine is the preferred method for establishing and/or confirming a diagnosis of osteoporosis, predicting future fracture risk, and monitoring patients. Areal BMD by DXA is expressed in absolute terms of grams of mineral per square centimeter scanned (g/cm2) and as a relationship to two BMD norms: an age-, sex-, and ethnicity-matched reference population (Z-score), or a young-adult reference population (T-score). The International Society for Clinical Densitometry (ISCD) recommends using a Caucasian (non-race adjusted) young female normative database for women AND men of ALL ethnic groups. Recommendations may vary with use of sex- and race-adjusted young normal controls for T-scores and these are used by some co-authors of this guide [59].
The difference between a patient’s BMD and the mean BMD of the reference population, divided by the standard deviation of the reference population, is used to calculate Z-scores and T-scores. An individual’s BMD is reported as the standard deviations above or below the mean BMD, as outlined in Table 4. The BMD diagnosis of normal bone mass, low bone mass (osteopenia), and osteoporosis are based on this World Health Organization (WHO) diagnostic classification [60].
Table 4.
Defining osteoporosis by BMD: WHO classification by T-score
| WHO definition of osteoporosis based on BMD | ||
|---|---|---|
| Classification | BMD | T-score |
| Normal | Within 1.0 SD of the mean level for a young-adult reference population | T-score at − 1.0 and above |
| Low bone mass (osteopenia) | Between 1.0 and 2.5 SD below that of the mean level for a young-adult reference population | T-score between − 1.0 and − 2.5 |
| Osteoporosis | 2.5 SD or more below that of the mean level for a young-adult reference population | T-score at or below − 2.5 |
BMD has been shown to correlate well with bone strength. The recent FNIH Bone Quality Study found that improvements in DXA-based BMD predicted reductions in fracture risk. In a meta-regression analysis of 38 placebo-controlled trials of 19 osteoporosis medications, with ~ 111,000 study participants, the FNIH study group found that increased BMD at the total hip and lumbar spine predicted fracture risk reduction at both of these sites [61]. Larger increases in BMD were associated with greater reductions in risk. For example, a 2% increase in total hip BMD could be expected to reduce vertebral fracture risk by 28% and hip fracture risk by 16%, while a 6% increase in hip BMD would result in a 66% reduction in vertebral fracture risk and a 40% reduction in risk factors for hip fractures (Table 5).
Table 5.
Increases in BMD and associated estimated fracture risk reduction (FNIH Study) (Larger improvements in DXA-based BMD are associated with greater reductions in fracture risk, particularly for vertebral and hip fractures [62]
| % increase in BMD | % reduction in vertebral fracture | % reduction in hip fracture | |
|---|---|---|---|
| At total hip | |||
| 2% | 28% | 16% | |
| 4% | 51% | 29% | |
| 6% | 66% | 40% | |
| At femoral neck | |||
| 2% | 28% | 15% | |
| 4% | 55% | 32% | |
| 6% | 72% | 46% | |
| At lumbar spine | |||
| 2% | 28% | 22% | |
| 4% | 62% | 38% | |
| 6% | 79% | 51% | |
DXA scans are associated with exposure to trivial amounts of radiation. These highly sensitive measurements of lumbar spine, hip, and/or forearm must be performed by trained technologists on well-calibrated instruments. For meaningful interpretation, serial scans should be performed on the same densitometry device at the same facility.
In postmenopausal women and men aged 50 years and older, WHO diagnostic T-score criteria (normal, low bone mass, and osteoporosis) are applied to BMD measurement by central DXA at the lumbar spine and femoral neck [62]. BMD measured by DXA at the 33% radius is used for diagnosing osteoporosis when hip or lumbar spine cannot be measured; scans are unusable or cannot be interpreted, in clinical conditions associated with low forearm BMD, or as dictated by clinical judgment [59, 62].
It is important to note that DXA of the lumbar spine can be difficult to accurately interpret. This is in large part due to degenerative changes in the lumbar spine, very common in older adults, that are typically characterized by localized bone proliferation. In this setting, DXA findings can overestimate spinal BMD and underestimate fracture risk. Patients with degenerative spinal changes may benefit from trabecular volumetric BMD (vBMD) measured with quantitative computed tomography (QCT), which is less affected by these changes, although this technology is not widely available [63, 64].
These diagnostic classifications should not be applied to everyone. Premenopausal women, men less than 50 years of age, and children cannot be diagnosed on the basis of densitometric criteria alone. In populations between 20 and 50 years of age, the ISCD recommends that ethnicity- or race-adjusted Z-scores be used instead. Z-scores of − 2.0 or lower are classified as low BMD for chronological age and those above − 2.0 classified as within the expected range for age [59]. In children, height-for-age Z-score (HAZ) (BMC/BMDhaz) has been demonstrated to most effectively offset the effect of short or tall stature on BMC/BMD Z-scores. A calculator for pediatric Z-score adjustment is available at https://zscore.research.chop.edu.
Who should be tested?
The decision to perform initial bone density measurement should be based on an individual’s fracture risk profile and skeletal health assessment. Measuring bone density is not indicated unless test results will influence treatment and management decisions. The BHOF recommends screening densitometry in women aged ≥ 65 years and men aged ≥ 70 years, younger postmenopausal women aged 50–64 years, and men aged 50-69 years with risk factors for osteoporosis. The BHOF also recommends BMD testing for women and men with fracture(s). These recommendations are in concert with those of the ISCD and Endocrine Society clinical practice guidelines for osteoporosis in men [58, 59]. BHOF recommendations for BMD testing are listed in Table 6. Routine bone density measurement is not recommended for children or adolescents and is not routinely indicated in healthy young men or premenopausal women unless there is a significant fracture history or specific risk factors for bone loss (such as glucocorticoid use).
Recommended screening densitometry in men
BHOF (formerly NOF) and other societies recommend BMD testing in men to inform clinical decisions regarding treatment (Table 6). This includes men aged 70 years and older regardless of risk factors, men aged 50–69 years with clinical risk factors for fracture, and men who have broken a bone at age 50 years or older. In addition, men with conditions or on treatments associated with bone loss or low bone mass should be considered appropriate candidates for BMD screening (in its 2018 report, the US Preventive Services Task Force [USPSTF] confirmed the utility of BMD by DXA in predicting fracture in both women and men, but they found insufficient evidence at that time to recommend routine testing in men) [22, 65].
Vertebral fracture assessment
Vertebral fracture in an adult aged 50 years or older is diagnostic of osteoporosis, even in the absence of a bone density diagnosis. The presence of a single vertebral fracture signifies a 5-fold increased risk for additional vertebral fractures and a 2- to 3- fold increased risk for hip or other fractures [66].
Unfortunately, most vertebral fractures are subclinical and/or completely asymptomatic. As a result, they may go undiagnosed for many years. At the same time, a high proportion of women with asymptomatic vertebral fractures have BMD levels that would not warrant treatment based on BMD alone [67]. The finding of a previously unrecognized vertebral fracture may change a patient’s diagnostic classification, alter fracture risk calculations, and determine treatment decisions [68]. Proactive investigation is required to detect these fractures so that further bone damage can be prevented.
Traditionally, conventional lateral thoracic/lumbar spine X-ray has been considered the gold standard for identification of vertebral fractures and minor vertebral deformities. However, DXA-assisted vertebral fracture assessment (DXA-VFA) is emerging as an alternative to radiography for its convenience, low cost, and minimal radiation exposure. Recently performed MRI or CT imaging studies done for other purposes can and should also be evaluated for presence of vertebral fractures or evidence of vertebral deformity.
Because subclinical vertebral fractures are so prevalent in older individuals, vertebral fracture assessment is recommended for the high-risk individuals listed in Table 7 [7, 8, 69]. As demonstrated in a recent study, incorporation of DXA-VFA into routine DXA screening for postmenopausal women with osteopenia or osteoporosis (T-score ≤ − 1, aged ≥ 65 years) has demonstrated cost-effectiveness for predicting increased risk of osteoporotic fractures [6].
Baseline DXA-VFA imaging provides a benchmark for future comparison when DXA-BMD is reassessed or when suggestive symptoms present: such as prospective height loss, new back pain, or postural changes [7]. Follow-up vertebral imaging may also be appropriate for patients being considered for a bisphosphonate holiday (temporary suspension of pharmacotherapy), since discontinuing antifracture therapy would not be advisable in patients who have recent vertebral fractures [70].
Using US-adapted Fracture Risk Assessment Tool (FRAX®)
The Fracture Risk Assessment Tool (FRAX®) was developed to calculate 10-year probabilities of hip fracture and major osteoporotic fracture (defined as clinical vertebral, hip, forearm or proximal humerus fracture). The FRAX® algorithm takes into account the validated clinical risk factors for fractures shown in Table 8. FRAX® is validated for women and men aged 40–90 years. FRAX® was tested in treatment-naïve patients not on osteoporosis medications. It may, however, be useful for assessing risk in previously treated individuals who have discontinued bisphosphonate therapy for 2 years or non-bisphosphonate therapy for 1 year [65, 71].
Table 8.
Risk factors included in the Fracture Risk Assessment Model (FRAX®)
| Clinical risk factors included in FRAX® Tool | |
|---|---|
| Age | Alcohol intake (3 or more drinks/day) |
| BMD at femoral neck (g/cm2) | BMI (low body mass index, kg/m2) |
| Female sex | Oral glucocorticoid intake ≥ 5 mg/day of prednisone for > 3 months (ever) |
| Parental history of hip fracture | Prior osteoporotic fracture (including clinical and subclinical vertebral fractures) |
| Rheumatoid arthritis | Smoking (current) |
| Secondary causes of osteoporosis: type 1 diabetes, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, hypogonadism or premature menopause (< 40 years), chronic malnutrition or malabsorption, and chronic liver disease | |
A country-specific FRAX® score can be calculated with BMD, without BMD, with BMD and body mass index (BMI), or with BMI alone. Studies have demonstrated modest agreement between assessments of FRAX®-with-BMD and FRAX®-with-BMI (correlation coefficient ~ 0.5) [72]. While FRAX®-with-BMI may overestimate probability in older frail adults, it may underestimate fracture risk in younger patients compared to FRAX-with-BMD [73, 74].
FRAX® can be calculated with either femoral neck BMD or total hip BMD (in g/cm2), but, when available, femoral neck BMD is preferred. The use of BMD from non-hip sites is not recommended. Caution should be taken when using FRAX® without BMD to estimate fracture risk. (Although FRAX® allows input of T-score, we do not recommend this since the reference database for T-score calculation with clinical DXA systems may not be the same as that used in the FRAX® algorithm.)
Therapeutic intervention recommendations in FRAX® incorporate data on risk-benefit analyses, cost-effectiveness of treatments, and competition for resources in the USA [75, 76].These recommendations exist for guidance purposes only and are not absolute rules. Developers of FRAX® determined that for many secondary causes of osteoporosis, fracture risk is mediated primarily through impact on BMD [77]. For this reason, when low femoral neck BMD is entered into FRAX®, the secondary causes of osteoporosis button is automatically inactivated.
FRAX® scores should not deter clinicians or patients from considering intervention strategies when clinically assessed risk indicates utility. Conversely, these recommendations do not mandate treatment, particularly in patients with bone mass that is low but above the osteoporosis range. For patients with scores above FRAX® treatment thresholds, who do not have prevalent fracture of the hip or spine or secondary risk factors for accelerated bone loss, it is currently unclear if pharmacologic treatment significantly improves fracture risk with a reasonable number needed to treat. Management decisions must be made on a case-by-case basis [78, 79].
FRAX and US ethnicity data
The US adaptation of FRAX requires selecting 1 of 4 ethnicities for each patient (Caucasian, Black, Hispanic, Asian). Among these populations, data indicates differences in fracture risk even at the same BMD. Although many limitations to this methodology have been described, it provides fracture risk stratification that can direct treatment to high-risk individuals most likely to benefit and avoid treatment of those at low risk [80]. Other countries, including some with considerable ethnic diversity, have used an alternative approach, with a single version of FRAX regardless of ethnicity.
FRAX® with trabecular bone score
Trabecular bone score (TBS) is an assessment of how evenly or unevenly mineral is structurally distributed in trabecular bone. A TBS is generated from lumbar spine BMD images using software installed on a DXA machine. No additional scan time or radiation exposure is required. The TBS gray-scale texture model captures local differences in mineral concentrations, providing an index of bone microarchitecture that predicts fracture risk independent of BMD and FRAX® scores. TBS is correlated with BMD at spine and hip as well as with FRAX® risk projections for hip and major osteoporotic fracture [81, 82]. Adding TBS to FRAX®, which is possible on late-model densitometry devices, increases the ability of FRAX® to predict fractures (TBS-adjusted FRAX®) [83].
TBS is most applicable to patients who have low bone mass, rather than those with osteoporosis according to BMD criteria, for whom treatment is already indicated [84, 85]. TBS is FDA approved and provides additional utility in fracture risk assessment among people with secondary causes of bone loss and fractures, such as type 2 diabetes [83, 86, 87].
Potential limitations of FRAX®
The FRAX® tool is not a perfect predictor of fracture and its use requires clinical judgment. Because data validating the relative weight of all known risk factors are not yet available, they are not included in the FRAX® algorithm. These variables include risks associated with falls, non-DXA bone density measurements, rapidity of bone loss, specific secondary causes of osteoporosis (e.g., type 2 diabetes), and multiple fractures experienced in a short period of time. Other risks that are important in older adults not included in FRAX include frailty, multiple comorbid conditions, multiple medications associated with falls/fractures, and life expectancy.
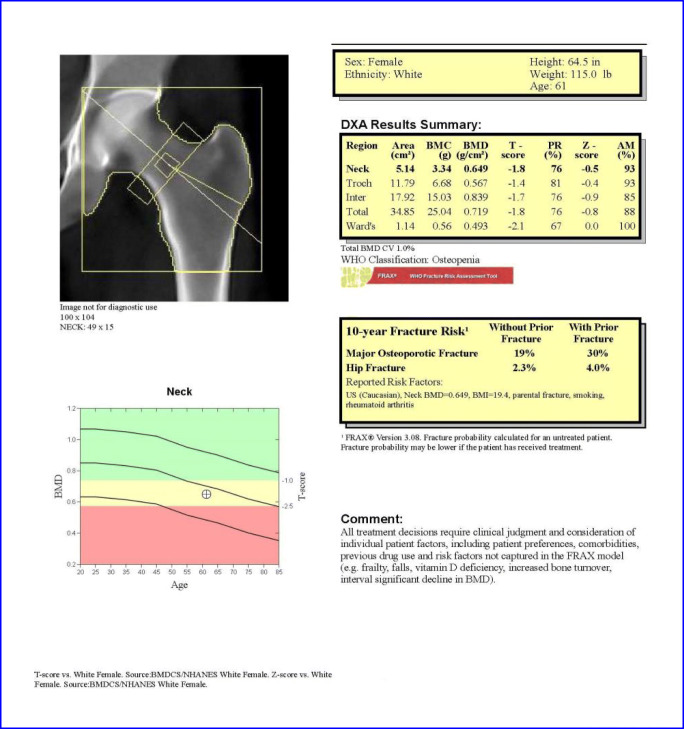
The FRAX® tool is most useful in patients with low femoral neck BMD. The FRAX® algorithm has not been validated for use with lumbar spine BMD. Utilizing FRAX® in patients with low BMD at the lumbar spine, but relatively normal BMD at the femoral neck, underestimates fracture risk (Fig. 4).
Fig. 4.
Hip BMD showing low bone mass and a history of a fracture. The FRAX® score indicates an elevated absolute risk of major osteoporotic and hip fracture
The yes/no scoring employed by FRAX® computes average risk associated with individual clinical variables. As a result, dose–response effects of risk factors included in FRAX® are lost. For such variables, presumably higher doses increase risk more than lower doses. (Adjustments to FRAX to better account for dose effect of glucocorticoid dose have been proposed [88].)
The FRAX® algorithm is available at http://www.bonehealthandosteoporosis.org as well as at http://www.sheffield.ac.uk/FRAX. It is available on newer DXA systems or with software upgrades that provide the FRAX® scores as well as the TBS-adjusted FRAX® on the bone density report.
Alternative bone densitometry technologies
Technologies other than DXA can be used to assess BMD, bone structure, bone strength, and fracture risk.These include quantitative computed tomography (QCT) to measure volumetric (v) BMD of the spine and proximal femur and derive areal BMD values that can be used for diagnostic classification with the WHO criteria and for input for FRAX. Opportunistic QCT uses QCT images performed for non-skeletal indications to detect fractures and measure BMD with synchronous or asynchronous calibration [89]. Quantitative ultrasound (QUS) measures non-BMD parameters of bone strength that are correlated with fracture risk. Imaging technologies used in research settings and sometimes in clinical practice include: pulse echo ultrasound (PEUS), and finite element analysis (FEA) with biomechanical computed tomography (BCT) [90, 91]. Other bone imaging tools largely used in research include peripheral QCT (pQCT), high-resolution pQCT (HR-pQCT), and magnetic resonance imaging (MRI).
Biochemical markers of bone turnover
While not currently FDA approved for diagnosis of osteoporosis, measurements of biochemical bone turnover markers (BTMs) can play a role in assessing fracture risk in appropriate individuals: for example, to gauge rate of bone loss in women following treatment for breast cancer.
Products of the remodeling process can be measured as indicators of turnover activity. Biochemical markers of bone remodeling include resorption markers serum C-telopeptide (CTX) and urinary N-telopeptide (NTX) and formation markers serum amino-terminal propeptide of type 1 procollagen (P1NP), bone-specific alkaline phosphatase (BALP), and osteocalcin (OC).
BTMs may [92]:
Predict rapidity of bone loss in untreated postmenopausal women.
Predict extent of fracture risk reduction when repeated after 3–6 months of treatment with FDA-approved therapies.
Predict magnitude of BMD increases with FDA-approved therapies.
Characterize patient compliance and persistence with osteoporosis therapy using a serum CTX for an antiresorptive medication and P1NP for an anabolic therapy (least significant change [LSC] is approximately a 40% reduction in CTX).
Potentially be used during a bisphosphonate holiday to suggest when medication should be restarted, although more data are needed to support this recommendation.
The FNIH Bone Quality Project conducted a large analysis of antiresorptive therapies to evaluate the utility of BTM changes as a surrogate for fracture risk reduction in drug development. In a recent pooled meta-regression analysis of antiresorptive therapies, changes in CTX or NTX did not predict antifracture efficacy. Changes in the bone formation markers BALP and P1NP, however, were strongly predictive of risk reduction for vertebral fractures, but these changes did not reach significance for non-vertebral or hip fractures [93].
Universal bone health recommendations
Several interventions to preserve bone strength can be recommended to the general population. These include adequate intake of calcium and vitamin D, cessation of tobacco use, identification and treatment of excessive alcohol intake, regular weight-bearing and muscle-strengthening exercise, and remediation of conditions associated with falls, such as visual impairment and use of sedating medications.
Adequate intake of calcium
Sufficient calcium intakes are necessary for acquisition of peak bone mass and maintenance of bone health across the lifespan. The skeleton contains 99% of the body’s calcium stores; when the exogenous supply is inadequate, bone tissue is resorbed from the skeleton to maintain constant serum calcium levels.
BHOF supports the Institute of Medicine’s (IOM) calcium intake recommendations: 1000 mg/day for men aged 19–70 years and women aged 19–50 years; 1200 mg/day for women 51 years and older and men 71 years and older (Tables 9 and 10) [95]. There is no evidence that calcium intakes in excess of recommended amounts confer additional bone benefit. However, there is evidence that intake of supplemental calcium above 1200 to 1500 mg/day can increase risk for developing kidney stones in at-risk individuals [96].
Table 9.
Estimating daily dietary calcium intake
| Step 1: Estimate calcium intake from calcium-rich foods* | |||
|---|---|---|---|
| Product | # of servings/day | Estimated calcium/serving, in mg | Calcium in mg |
|
Milk (8 oz) Almond/soy milk (8 oz) |
__________ |
× 300 × 450 |
= __________ |
| Yogurt (6 oz) | __________ | × 300 | = __________ |
| Cheese (1 oz or 1 cubic in.) | __________ | × 200 | = __________ |
| Fortified foods or juices | __________ | × 80 to 1000** | = __________ |
| Tofu, firm (8 oz) | __________ | × 250 | = __________ |
| Subtotal | = __________ | ||
| Step 2: Add 250 mg for non-dairy sources to subtotal | + 250 | ||
| Total calcium, in mg | = __________ | ||
*About 75 to 80% of the calcium consumed in American diets is from dairy products
**Calcium content of fortified foods varies, and it is important to review individual labels
Table 10.
| Life stage group | Calcium IOM/NOF (mg/day) |
Calcium Safe upper limit (mg/day) |
Vitamin D IOM/NOF (units/day) |
Vitamin D Safe upper limit (units/day) |
|---|---|---|---|---|
| 51–70-year-old women | 1200 | 2500 | 600/800–1000 | 4000 |
| 51–70-year-old men | 1000 | 2000 | 600/800–1000 | 4000 |
| 71+-year-old men and women | 1200 | 2000 | 800/800–1000 | 4000 |
A balanced diet rich in low-fat dairy products, select dark greens, fish with bone, fruits, vegetables, and fortified foods (like the nondairy supplemented beverages including orange juice, or soy and almond milk) provides calcium as well as numerous nutrients needed for good health. Table 9 illustrates a simple method for estimating the calcium in a patient’s diet. Most people do not get enough. Average daily dietary calcium intake for adults age ≥ 50 years is 600 to 700 mg/day. Increasing dietary calcium is the first-line approach, but calcium supplements should be used when an adequate dietary intake cannot be achieved [97, 98].
Calcium intake recommendations refer to milligrams of elemental calcium in the supplement. Content varies: calcium carbonate contains 40% elemental calcium by weight, whereas calcium citrate contains 21%. Patients should be advised to read the Supplement Facts panel for elemental calcium content when choosing a supplement.
Supplemental calcium is most widely available as calcium carbonate and calcium citrate. Calcium carbonate requires stomach acid for absorption and so is best taken with food, while calcium citrate is absorbed equally well on an empty stomach. Calcium of all types is best absorbed in doses of ~ 500 mg or less. Splitting doses may be needed to ensure optimal absorption [99].
Calcium citrate is useful for people with achlorhydria, inflammatory bowel disease, absorption disorders, and those on proton pump inhibitors that reduce gastric acid. Individuals who experience gastrointestinal side effects taking calcium carbonate may benefit from taking multiple small doses, taking calcium carbonate with meals and/or switching to calcium citrate. Other varieties of calcium commonly in supplements or fortified foods include gluconate, lactate, and phosphate. Calcium citrate malate is a well-absorbed form of calcium found in some fortified juices. Elemental calcium in fortified foods varies.
Some studies have reported increased risk of cardiovascular disease linked to calcium supplements with or without vitamin D, but conflicting data are reported [100–103]. A large systematic review and meta-analysis including RCTs and cohort studies found no evidence that calcium with or without vitamin D increased cardiovascular disease [104]. The large VITamin D and OmegA-3 Trial (VITAL), sponsored by the NIH, tested supplemental vitamin D (2000 units/day) on cardiovascular outcomes and found no adverse effects [105].
Adequate intake of vitamin D
Vitamin D facilitates calcium absorption that is necessary for mineralization of bone. The BHOF recommends a daily intake of 800 to 1000 units of vitamin D for adults aged 50 years and older. The Institute of Medicine Dietary Reference Intakes for vitamin D are 600 units daily until age 70 years and 800 units/day for adults age 71 years and older. The IOM recommendations for vitamin D are based on intakes sufficient to maintain a serum 25(OH)D of 20 ng/mL in ≥ 97.5% of population [94]. A slightly higher serum 25(OH)D level (approximately 30 ng/mL) is associated with optimal calcium absorption and so is preferred by the BHOF [106–110]. The upper limits for vitamin D intake according to the IOM is 4000 units/day for adults, above which there is a potential for adverse effects. The current normal range for 25(OH)D levels is 20 to 50 ng/mL. Some studies suggest that excessive intake of vitamin D may have adverse impacts on bone through increased risk for falls and fractures [110, 111].
Chief dietary sources of vitamin D include fortified milk (400 units per quart) and breakfast cereals (generally 40–300 units per serving), saltwater fish (e.g., salmon, mackerel, tuna), and cod liver oil. Some, but not all non-dairy milk substitutes, such as rice or soy milk, are supplemented with vitamin D and calcium and so it is important to read the labels. Some calcium supplements and most multivitamin tablets contain vitamin D. Supplementation with either vitamin D2 (ergocalciferol) or vitamin D3 (cholecalciferol) is effective, but cholecalciferol, which is the form produced in humans, is preferable. Vitamin D2 is derived from plant sources and may be preferred by individuals on a strict vegan/vegetarian diet.
Many conditions prevalent in older patients contribute to vitamin D deficiency, such as chronic renal insufficiency and limited sun exposure due to disability. Of note, a high prevalence of vitamin D deficiency is seen in patients with advanced osteoarthritis presenting for total hip replacement as well as in hip fracture patients with osteoporosis (including those on antifracture medications) [9, 112]. Vitamin D deficiency should be corrected to optimize surgical and/or pharmacologic outcomes.
Supplemental vitamin D should be administered in amounts capable of raising serum 25(OH)D levels to approximately 30 ng/mL (75 nmol/L) and maintaining it at this level. Adults who are vitamin D deficient are typically treated with 50,000 units of vitamin D2 or vitamin D3 once a week (or the equivalent daily dose of 7000 units vitamin D2 or vitamin D3) for 5–8 weeks to achieve a 25(OH)D blood level of approximately 30 ng/mL. This regimen should be followed by maintenance therapy of 1000 to 2000 units/day or whatever dose is needed to maintain the target serum level [113, 114]. Adults with ongoing malabsorption may require higher replacement doses of vitamin D to reach and sustain sufficiency.
Supplemental vitamin D and BMD
Systematic reviews and meta-analyses have found insufficient or conflicting evidence to support the use of supplemental vitamin D alone (without calcium) to promote musculoskeletal health in adults living in the community [115–119]. The large VITAL study in generally healthy women and men (≥ 55/≥ 50 years respectively) not selected for low bone mass or vitamin D insufficiency, reported no effect of high-dose, supplemental vitamin D (cholecalciferol 2000 units/day) versus placebo on BMD or bone structural measures over 2 years [120, 121]. Effects did not vary by sex, race/ethnicity, body mass index, or baseline 25(OH)D levels. The baseline 25(OH)D level (mean) was 27 ng/mL, suggesting that VITAL participants may already be at serum vitamin D levels sufficient to support normal bone health. These findings do not apply to persons with extremely low vitamin D levels or osteoporosis or younger adults. Ongoing studies in VITAL are examining effects of supplemental vitamin D on incident fractures among 25,871 women and men nationwide [121, 122].
Supplemental vitamin D and fall risk
A possible role for supplemental vitamin D in fall prevention has been a subject of study and inconclusive data. Results from the VITAL study, the largest placebo-controlled RCT of supplemental vitamin D on health outcomes, did not support the use of supplemental vitamin D (2000 units/day vs placebo groups) to prevent falls in generally healthy population not selected for high falls risk or vitamin D insufficiency [123]. These findings are consistent with recent meta-analyses and other randomized controlled studies in populations around the world that have not found supplemental vitamin D to be effective in reducing fall risk [118, 124–126].
Vitamin D absorption and synthesis
Gastrointestinal absorption of vitamin D differs between individuals and can be significantly decreased in patients with celiac disease, inflammatory bowel disease, bariatric surgery, and other disorders. Variability in skin activation and synthesis of vitamin D results from differences in pigmentation, season (weak UV light in the winter and fall), time spent outdoors, and use of sunscreens. For example, African Americans have lower 25(OH)D levels than non-Hispanic white Americans due to decreased skin activation (and possibly differences in vitamin D binding proteins). People who live in northern latitudes typically experience a decrease in serum vitamin D in winter that rebounds in spring and summer.
Cessation of tobacco use and avoidance of excessive alcohol intake
The use of tobacco products is detrimental to the skeleton as well as to overall health [127–130]. BHOF strongly recommends smoking cessation to support primary and secondary prevention of osteoporosis.
Moderate alcohol intake has no known negative effect on bone and may even be associated with slightly higher bone density and lower risk of fracture in postmenopausal women. However, alcohol intake of more than two drinks a day for women or three drinks a day for men may be detrimental to bone health. It has been associated with reduced calcium absorption and increased risk for falls. Clinicians should identify patients at risk for chronic heavy drinking and/or binge drinking who require further evaluation and treatment [131].
Regular weight-bearing and muscle-strengthening physical activity
The BHOF strongly endorses physical activity at all ages, both for fracture prevention and overall fitness. In childhood and adolescence, consistent weight-bearing and high-impact activities contribute to acquisition of optimal peak bone mass [132]. Weight-bearing exercises (in which bones and muscles work against gravity with feet and legs bearing body weight) include walking, jogging, tai chi, stair climbing, dancing, and tennis. Muscle-strengthening exercises include weight training and resistive exercises, such as yoga, Pilates, and boot camp calisthenics. To avoid injury, patients should be evaluated before initiating a new exercise program, particularly one involving compressive or contractile stressors (such as running or weightlifting).
A multicomponent program is recommended for people with osteoporosis: one that includes progressive resistance training, balance training, back extensor strengthening, core stabilizers, cardiovascular conditioning, and impact or ground-reaction forces to stimulate bone. In people with osteoporosis, improved fall outcomes have been documented following high-intensity exercise programs that combine resistance, balance, and weight-bearing activities [133–136]. In research settings, structured exercise programs have resulted in modest increases in bone density [137–139]. Muscle growth has been reported even in frail elderly individuals with established sarcopenia (age-related muscle loss) who participate in short-burst high-intensity exercise. For safety, any such program of physical activity must be developed and supervised by certified fitness personnel experienced with skeletal fragility in geriatric patients. (See “Protecting fragile bones in daily life and recreation” section.)
Motivating patients to stick with a program of physical activity
Sticking with any lifestyle change can be difficult. However, persistence is easier when that change is linked to something of value to an individual. In this case, what probably matters most is preserving independence by avoiding an injury that results in nursing home admission. Visual aids that show graphical comparisons of risk, can help patients see the connection between bone health recommendations and quality of life.
Consultation with a trained physical therapist and/or participation in group exercise led by certified fitness personnel help ensure patient safety, motivate daily participation, and promote social engagement. As long as principles of safe movement are followed, walking and daily activities such as housework and gardening are practical ways to contribute to maintenance of fitness and bone mass.
Fall prevention strategies
Among adults aged 65 or older, falls are the leading cause of both fatal and nonfatal injuries including the majority of all fractures and over 90% of hip fractures [142–144]. According to CDC statistics, in 2018, more than 32,000 adults aged ≥ 65 years were killed by unintentional fall injuries [145].
Major risk factors for falls are shown above in Table 2. Many of these are modifiable: muscle strength and balance can be improved through targeted exercise; visual impairment can be addressed; severe vitamin D deficiency can be corrected; fall hazards in the home and work environment can be remediated; and medications that induce dizziness and disorientation can be replaced or reduced.
Multiple studies have demonstrated the efficacy of therapeutic physical activity in reducing falls. A recent meta-analysis of RCTs investigating moderate-intensity multicomponent physical activity (aerobic, balance, and strength training) 3 times a week for 1 year or more reported significant fall reductions: 22% lower risk for falls and 26% lower risk for injurious falls. Risk of fractures was reduced by 16%, although the significance of this finding is weakened by the small number of fractures in the study (p = .05) [146]. For individuals who have already experienced a fall, regular weight-bearing and muscle-strengthening physical activity may reduce the risk of future falls and fractures [124, 147–149].
A 12-month, single-blinded RCT among 345 high-risk older adults aged ≥ 70 years who had fallen in the year prior compared usual care (geriatrician provided fall prevention instruction) or a home-based exercise program focused on strength and balance training. At 1 year, fall incidence was 74% lower in the home-based exercise group than in the group that received usual care. No adverse events related to the intervention were reported [150].
Regarding fracture outcomes among persons with osteoporosis, there are few exercise/physical activity studies with fractures as a primary endpoint. However, a recent meta-analysis examining physical activity and fall outcomes in older adults in the general population provides evidence that physical activity may prevent fractures in older adults [135]. Another meta-analysis of 10 studies (n = 4047) reported that physical activity may reduce the number of older community-dwelling adults experiencing ≥ 1 fall-related fracture (RR 0.73, 95% CI 0.56 to 0.95), but the evidence is judged to be of low certainty [151].
In the WHI, among 77,206 postmenopausal women across the USA followed for a mean of 14 years, there was an association between higher levels of physical activity and lower total fracture risk and lower risk for hip fracture. It is important to note that even low-intensity activities such as walking or gardening reduced risk for hip fracture when compared to sedentary activities [152].
There are a limited number of studies with men and few RCT exercise studies with fracture outcomes comparing those who exercise to those who did not exercise.
US FDA-approved drugs for osteoporosis
Current FDA-approved pharmacologic therapeutics for prevention and/or treatment of postmenopausal osteoporosis include bisphosphonates (alendronate, alendronate plus D, ibandronate, risedronate, and zoledronic acid), estrogens (estrogen and/or hormone therapy), estrogen agonist/antagonist (raloxifene), tissue-selective estrogen complex (conjugated estrogens/bazedoxifene), parathyroid hormone (PTH [1–34], teriparatide), analog of parathyroid hormone-related peptide (PTHrP [1–34], abaloparatide), RANKL inhibitor (denosumab), fully human monoclonal antibody to sclerostin (romosozumab), and calcitonin. Please see product-specific prescribing information for details of their use (Table 11).
Table 11.
FDA-approved drugs for osteoporosis [153]
| Drug name | Brand name | Form/dosing | Approval for |
|---|---|---|---|
| Bisphosphonates | |||
| Alendronate | Generic alendronate and Fosamax®, Fosamax Plus D™ |
Oral (tablet) Daily/weekly |
Women and men |
| Alendronate | Binosto® |
Effervescent tablet Weekly |
Women and Men |
| Ibandronate | Boniva® |
Oral (tablet) Monthly |
Women |
| Ibandronate | Boniva® |
Injection Quarterly |
Women |
| Risedronate | Actonel®/Actonel® w/ calcium |
Oral (tablet) Daily/weekly/twice monthly/monthly; monthly with calcium |
Women and men |
| Risedronate | Atelvia™ |
Oral delayed-release (tablet) Weekly |
Women |
| Zoledronic acid | Reclast® |
IV infusion Once a year/once every 2 years |
Women and men |
| Estrogen-related therapies | |||
| Estrogen | Multiple brands |
Oral (tablet) Daily |
Women |
| Estrogen | Multiple brands |
Transdermal (skin patch) Twice weekly/weekly |
Women |
| Raloxifene | Evista® |
Oral (tablet) Daily |
Women |
| Conjugated estrogens/bazedoxifene | Duavee® |
Oral (tablet) Daily |
Women |
| Parathyroid hormone analogs | |||
| Abaloparatide | Tymlos® |
Injection Daily (for 2 years) |
Women |
| Teriparatide | Forteo® |
Injection Daily (for 2 years) |
Women and men |
| Denosumab | Prolia™ |
Injection Every 6 months |
Women and men |
| Sclerostin inhibitor | |||
| Romosozumab | Evenity™ |
Injection (2) Monthly for 12 months |
Women |
| Calcitonin Salmon | |||
| Calcitonin | Fortical®/Miacalcin® |
Nasal spray Daily |
Women |
| Calcitonin | Miacalcin® |
Injection Schedule varies |
Women |
Antifracture benefits of FDA-approved drugs for osteoporosis have been studied primarily in postmenopausal women. We have more limited fracture data on efficacy in patients with secondary causes of osteoporosis (e.g., diabetes, glucocorticoids) and men diagnosed with osteoporosis by fracture or T-score.
Potential benefits and risks of therapy should be assessed in the context of a drug’s fracture efficacy, onset of effect, duration parameters, magnitude of effect, and site of optimal fracture prevention (spine vs hip). In general, a therapy that has been shown to reduce risk of both vertebral and non-vertebral fractures (alendronate, risedronate, zoledronic acid, denosumab, teriparatide, abaloparatide, or romosozumab) should be considered over one that has not (raloxifene, calcitonin, ibandronate). In most of these pivotal studies, participants were on appropriate amounts of calcium and vitamin D.
The BHOF does not advocate the use of drugs that are not approved by the FDA for prevention and/or treatment of osteoporosis.
Bisphosphonates (alendronate, ibandronate, risedronate, zoledronic acid)
Bisphosphonates are a class of potent antiresorptive agents. Composed of two phosphate groups, bisphosphonates have also been called diphosphonates. All bisphosphonates can affect renal function and are contraindicated in patients with estimated glomerular filtration rate (GFR) below 30–35 mL/min. Bisphosphonates may cause or exacerbate hypocalcemia, and therefore, hypocalcemia must be corrected before treatment.
Alendronate, brand name: Fosamax®, Fosamax Plus D, Binosto™ (liquid preparation) and generic alendronate
Alendronate sodium is approved by the FDA for prevention (5 mg daily and 35 mg weekly tablets) and treatment of postmenopausal osteoporosis (10 mg daily tablet, 70 mg weekly tablet [most commonly used dose], 70 mg weekly tablet with 2800 units or 5600 units of vitamin D3, and 70 mg effervescent tablet). Alendronate is approved as treatment to increase bone mass in men with osteoporosis and for treatment of osteoporosis in men and women taking glucocorticoids [154].
Drug efficacy
Alendronate reduces incidence of spine and hip fractures by about 50% over 3 years in patients with prior vertebral fracture and in patients who have hip T-scores diagnostic of osteoporosis (≤ − 2.5) [155, 156]. It reduces incidence of vertebral fractures by 48% over 3 years in patients without prior vertebral fracture.
Administration
Oral alendronate (generic and Fosamax®) tablets must be taken at least 30 min before the first food, beverage, or medication of the day with plain water only. Tablets must be swallowed whole with a full glass of plain water (6 to 8 oz). Effervescent alendronate (Binosto) must be dissolved in 4 oz of room temperature water and taken on an empty stomach first thing in the morning. Patients should remain upright and eat/drink nothing for 30 min following ingestion.
Side effects and drug safety
Side effects are similar for all oral bisphosphonate medications and include gastrointestinal problems such as difficulty swallowing, esophageal inflammation, stomach pain, and rare cases of atypical femur fractures (AFF) and osteonecrosis of the jaw (ONJ). (See boxed discussion below.) Ocular inflammation (anterior uveitis and episcleritis) has been documented. All bisphosphonates can affect renal function and are contraindicated in patients with estimated GFR below 30–35 mL/min.
Ibandronate, brand name: Boniva® and generic ibandronate
Oral and intravenous ibandronate sodium are approved by the FDA for treatment of postmenopausal osteoporosis (150 mg monthly tablet and 3 mg every 3 months by intravenous injection). Oral ibandronate is also approved for prevention of postmenopausal osteoporosis and is available as a generic in the USA.
Drug efficacy
Ibandronate reduces incidence of vertebral fractures by about 33–50% over 3 years but does not reduce risk of non-vertebral fracture (hip/nonhip) [157].
Administration
Oral ibandronate must be taken on an empty stomach, first thing in the morning, with 8 oz of plain water (no other liquid). Tablets must be swallowed whole with a full glass of plain water (6 to 8 oz). After taking ibandronate, patients must remain upright and wait at least 60 min before eating, drinking, or taking any other medication. Intravenous ibandronate, 3 mg/3 mL prefilled syringe, is administered over 15 to 30 s once every 3 months. Serum creatinine should be checked before each injection.
Side effects and drug safety
Side effects are similar for all oral bisphosphonate medications and include gastrointestinal problems such as difficulty swallowing, esophageal inflammation, and stomach pain and rare cases of AFF and ONJ. (See boxed discussion below.) Ocular inflammation has been documented. Like other bisphosphonates, ibandronate may cause or exacerbate hypocalcemia, and therefore, hypocalcemia must be corrected before treatment. All bisphosphonates can affect renal function and are contraindicated in patients with estimated glomerular filtration rate (GFR) below 30–35 mL/min.
Risedronate, brand name: Actonel®, Atelvia™, and generic risedronate
Risedronate sodium is approved by the FDA for prevention and treatment of postmenopausal osteoporosis (5 mg daily tablet; 35 mg weekly tablet; 35 mg weekly delayed-release tablet; 75 mg tablets taken on two consecutive days every month; and 150 mg tablet taken monthly). Actonel® is approved to increase bone mass in men with osteoporosis and to prevent and treat osteoporosis in men and women who are either initiating or taking glucocorticoids [158, 159].
Drug efficacy
Compared with placebo, risedronate reduced incidence of vertebral fractures by 39%, hip fractures by 27%, and non-vertebral fractures by 22% in a meta-analysis conducted by Barrionuevo et al. in 2019 [160]. Significant risk reduction occurred within 1 year of treatment in patients with a prior vertebral fracture.
Administration
Oral risedronate (generic and Actonel®) must be taken on an empty stomach, first thing in the morning, with 8 oz of plain water (no other liquid). Tablets must be swallowed whole with a full glass of plain water (6 to 8 oz). After taking risedronate, patients must remain upright and wait at least 30 min before eating, drinking, or taking any other medication.
Oral delayed-release risedronate (Atelvia®) is taken not on an empty stomach, but directly after breakfast with ≥ 4 oz of plain water (no other liquid). Patients should remain upright (sitting or standing) for at least 30 min.
Side effects and drug safety
Side effects are similar for all oral bisphosphonate medications and include gastrointestinal problems such as difficulty swallowing, esophageal inflammation, and stomach pain and rare cases of AFF and ONJ. (See boxed discussion below.) Ocular inflammation (anterior uveitis and episcleritis) has been documented. All bisphosphonates can affect renal function and are contraindicated in patients with estimated GFR below 30–35 mL/min. Because risedronate can cause or exacerbate hypocalcemia, hypocalcemia must be corrected before treatment. All bisphosphonates can affect renal function and are contraindicated in patients with estimated glomerular filtration rate (GFR) below 30–35 mL/min.
Zoledronic acid, brand name: Reclast®
Zoledronic acid is approved by the FDA for prevention and treatment of osteoporosis in postmenopausal women (5 mg once yearly for treatment and once every 2 years for prevention). It is approved to improve bone mass in men with osteoporosis and for prevention and treatment of osteoporosis in men and women expected to be on glucocorticoid therapy for at least 12 months. (Efficacy of less-frequent dosing is currently being investigated.) Zoledronic acid is indicated for prevention of new clinical fractures in patients (both women and men) who have recently had a low-trauma hip fracture. A recent placebo-controlled study in women aged ≥ 65 years with low hip BMD found that zoledronic acid administered every 18 months for 6 years reduced vertebral and non-vertebral fractures. In this study, the number needed to treat to prevent 1 incident fracture was 15 [161].
Drug efficacy
Zoledronic acid reduces incidence of vertebral fractures by 62–70% (with significant reduction at 1 year), hip fractures by 41%, and non-vertebral fractures by 21–25% over 3 years in patients with osteoporosis defined by prevalent vertebral fractures and/or osteoporosis by BMD of the hip [160].
Administration of zoledronic acid compared with placebo in postmenopausal women with low bone mass every 18 months reduces vertebral fractures by 55%, non-vertebral fractures by 34% and forearm and wrist fractures by 44% at 6 years [161].
Administration
Zoledronic acid (generic and Reclast®), 5 mg in 100 mL, is given once yearly by intravenous infusion administered over at least 15 min. Some physicians infuse this over 30 min. Flu-like symptoms (arthralgia, headache, myalgia, fever) have occurred in 32% of patients after the first dose, 7% after the second dose, and 3% after the third dose. To reduce likelihood of acute-phase reactions, patients should be well hydrated, drink 2 glasses of water before the infusion and pre-treat with acetaminophen (unless contraindicated).
Side effects and drug safety
We recommend a 25(OH) vitamin D level should be obtained and any vitamin D deficiency or insufficiency corrected before treatment. Zoledronic acid may cause or exacerbate hypocalcemia, and therefore, hypocalcemia must be corrected before treatment. Zoledronic acid is contraindicated in patients with creatinine clearance less than 35 mL/min or in patients with evidence of acute renal impairment. Creatinine clearance should be measured prior to each dose [162]. Ocular inflammation (anterior uveitis and episcleritis) has been documented [163]. (See boxed discussion below.)
Estrogen-related therapies (ET/HT, raloxifene, conjugated estrogens/bazedoxifene)
A variety of medications that act on estrogen receptors in bone are prescribed to prevent the bone loss associated with postmenopausal osteoporosis.
ET/HT
ET brand names: e.g., Climara®, Estrace®, Estraderm®, Estratab®, Ogen®, Premarin®, Vivelle®; HT brand names: e.g., Activella®, Femhrt®, Premphase®, Prempro®. Estrogen/hormone therapy is approved by the FDA for prevention of osteoporosis and relief of vasomotor symptoms and vulvovaginal atrophy associated with menopause. Women with an intact uterus require HT (combined estrogen and progestin) to protect uterine lining. Women who have had a hysterectomy are treated with ET (estrogen alone).
Drug efficacy
The Women’s Health Initiative (WHI) found that 5 years of oral HT (Prempro®) reduced incidence of clinical vertebral fractures and hip fractures by 34% and other osteoporotic fractures by 23% [164]. Meta-analysis sponsored by the Endocrine Society found that HT reduced fractures of the spine by 35%, hip by 28%, and non-vertebral skeleton by 22% [160].
Drug administration
ET/HT is available in a wide variety of oral and transdermal preparations that contain estrogen only, progestin only, and combination estrogen-progestin. ET/HT dosages include cyclic, sequential, and continuous regimens. When treatment is discontinued, bone loss can be rapid. Follow-on antifracture agents should be considered to maintain BMD.
Side effects and drug safety
Potential risks for women include biliary issues, breast cancer (with combined estrogen–progestin), endometrial hyperplasia/cancer (with inadequately opposed estrogen). Initial WHI data found elevated risk of myocardial infarction, stroke, pulmonary emboli, and deep vein thrombosis during 5 years of treatment with conjugated equine estrogen and medroxyprogesterone acetate (Prempro®) [165, 166]. Subsequent analyses of WHI substudy data showed no increase in cardiovascular disease in women starting treatment within 10 years of menopause [167].
The North American Menopause Society (NAMS) and American Association of Clinical Endocrinologists (AACE)/American College of Endocrinology (ACE) recommend tailoring ET/HT formulation, dose, and route of administration to individual postmenopausal women. Risk-benefit profiles differ by patient age, time since menopause, and other factors [168, 169].
The Endocrine Society guidelines recommend ET/HT to prevent fractures in some high-fracture-risk postmenopausal women < 60 years of age or < 10 years past menopause who are experiencing vasomotor and/or climacteric symptoms and cannot take bisphosphonates or denosumab [170].
When ET/HT use is considered solely for fracture prevention, the FDA recommends that approved non-estrogen treatments first be carefully considered.
Raloxifene, brand name: Evista® and generic raloxifene
Raloxifene is an estrogen agonist/antagonist (selective estrogen receptor modulator/SERM) approved by the FDA for both prevention and treatment of osteoporosis in postmenopausal women. Raloxifene is indicated for the reduction in risk of invasive breast cancer in postmenopausal women with osteoporosis [171–174]. Raloxifene does not reduce the risk of coronary heart disease.
The Endocrine Society guidelines recommend raloxifene or combination conjugated equine estrogen/bazedoxifene to prevent vertebral fractures in postmenopausal women who have low risk of deep vein thrombosis for whom bisphosphonates or denosumab are not appropriate or for women with a history of or high risk for breast cancer [166].
Drug efficacy
Raloxifene reduces incidence of vertebral fractures by about 30–40% in patients with a prior vertebral fracture and by about 55% in patients without a prior vertebral fracture. Raloxifene does not reduce risk of non-vertebral fractures.
Drug administration
Raloxifene is available as a 60-mg tablet, which may be taken with or without food (60 mg).
Side effects and drug safety
Raloxifene increases risk for deep vein thrombosis to a degree similar to that observed with estrogen. It can increase hot flashes and cause leg cramps.
Conjugated estrogens/bazedoxifene, brand name: Duavee®
Conjugated estrogens/bazedoxifene is FDA approved as an oral tablet for women who suffer from moderate-to-severe hot flashes associated with menopause and to prevent osteoporosis after menopause.
Conjugated estrogens/bazedoxifene combines conjugated estrogen with bazedoxifene, an estrogen agonist/antagonist. Bazedoxifene reduces risk for endometrial hyperplasia eliminating need for progestins in women who have not undergone hysterectomy.
Drug efficacy
In pivotal trials, this combination drug significantly increased mean lumbar spine BMD (treatment difference 1.51%) at 12 months compared to placebo in women who had been postmenopausal between 1 and 5 years. Treatment with conjugated estrogens/bazedoxifene also increased total hip BMD. The treatment difference in total hip BMD at 12 months was 1.21% [175–178].
Drug administration
Available as a tablet containing conjugated estrogens and bazedoxifene 0.45 mg/20 mg, to be taken once daily without regard to meals.
Conjugated estrogens/bazedoxifene is intended only for postmenopausal women who have not had hysterectomy. Like other products containing estrogen, its use should be consistent with treatment goals and risks for the individual woman. When being considered solely for the prevention of osteoporosis, such use should be limited to women who are at significant risk of fracture and only after carefully considering alternatives that do not contain estrogen. When treatment is discontinued, bone loss can be rapid. An antifracture agent should be considered to maintain BMD.
Side effects and drug safety
Side effects of conjugated estrogens/bazedoxifene include muscle spasms, nausea, diarrhea, dyspepsia, upper abdominal pain, oropharyngeal pain, dizziness, and neck pain. Because this product contains estrogen, it is approved with the same Boxed Warning and other Warnings and Precautions that have been approved with estrogen products.
Parathyroid hormone analogs (teriparatide, abaloparatide)
Parathyroid hormone (PTH) regulates calcium homeostasis. Constant high exposure to PTH causes bone resorption, while intermittent administration of exogenous recombinant PTH stimulates bone formation. Two anabolic agents derived from synthetic analogs of PTH are currently FDA approved: teriparatide and abaloparatide.
Teriparatide, brand name: Forteo® and the bioequivalent Bonsity™
Teriparatide is a synthetic fragment of human PTH that is approved by the FDA for treatment of osteoporosis in men and women at high risk for fracture (which is defined as a history of osteoporotic fracture, multiple risk factors for fracture, or failure/intolerance to other available osteoporosis therapy). It is approved to treat glucocorticoid-induced osteoporosis in men and women at high risk for fracture [179]. The FDA has approved an expanded indication for teriparatide for treatment of osteoporosis associated with sustained systemic glucocorticoid therapy (≥ 5 mg/day of prednisone). Forteo® is currently available as 20 μg daily subcutaneous injection. Biosimilar preparations are now available as the patented expired in 2019.
Drug efficacy
Teriparatide reduces risk of vertebral fractures by 65–77%, and non-vertebral fractures by 35–53% in patients with osteoporosis, after an average of 18 months of therapy [180]. The VERO trial that compared teriparatide and risedronate in postmenopausal women with severe osteoporosis reported ~ 56% fewer new vertebral fractures in the teriparatide group after 24 months [181]. It is important to follow teriparatide treatment with an antiresorptive agent, usually a bisphosphonate or denosumab, to maintain or further increase BMD.
Drug administration
Teriparatide is administered by 20 μg daily subcutaneous injection. When treatment is discontinued, bone loss can be rapid and alternative agents should be considered to maintain BMD. Treatment duration was previously restricted to 24 months, but this was recently changed to open the possibility of longer treatment in high-risk patients.
Side effects and drug safety
Side effects of teriparatide include transient orthostatic hypotension, leg cramps, and nausea. Teriparatide transiently increases serum calcium which may predispose patients to digitalis toxicity. It should be used with caution in patients with active or recent kidney stones, hypercalcemia and hypercalcemic disorders, and/or cutaneous calcification.
Until recently, teriparatide treatment was restricted to 2 years in response to elevated osteosarcoma seen in rodent studies. Increased osteosarcoma was not observed in humans during 15 years of post-marketing studies. As a result, the revised teriparatide label now states that use for more than 2 years during a patient's lifetime can be considered if a patient remains at or has returned to having a high risk for fracture.
Its use should be avoided in settings of increased risk for osteosarcoma: Paget’s disease of the bone, prior radiation therapy involving the skeleton, open epiphyses (children and young adults), history of bone metastases or malignancies, unexplained elevated alkaline phosphatase, and hereditary disorders predisposing to osteosarcoma [182].
Abaloparatide, brand name: Tymlos®
Abaloparatide is a synthetic peptide analog of human PTH-related protein approved by the FDA for treatment of osteoporosis in postmenopausal women at high risk for fracture defined as a history of osteoporotic fracture, multiple risk factors for fracture, or failure/intolerance to other available osteoporosis therapy.
Drug efficacy
Abaloparatide reduces risk of new vertebral fractures by about 86% and non-vertebral fractures by about 43% in postmenopausal women with osteoporosis, after an average of 18 months of therapy [183]. In an extension study (ACTIVE-Extend) after 18 months of abaloparatide or placebo, the addition of 6 months of oral alendronate for a total of up to 24 months of therapy resulted in a relative risk reduction of radiographic spine fractures by 87%, non-vertebral fractures by 52%, and major osteoporotic fractures by 58% [184].
Drug administration
Abaloparatide is administered by 80 μg daily subcutaneous injection in the periumbilical area of the abdomen. When treatment is discontinued, bone loss can be rapid. An antiresorptive agent should be considered to maintain BMD. Abaloparatide treatment duration is recommended not to exceed 24 months.
Side effects drug safety
Side effects of abaloparatide include leg cramps, nausea, and dizziness. Avoid use in patients with increased risk of osteosarcoma (e.g., Paget’s disease of bone, bone metastases, prior skeletal radiation). Patients with hypercalcemia, or a history of an unexplained elevated alkaline phosphatase or skeletal malignancy should not receive abaloparatide therapy. Abaloparatide may increase urinary calcium. It should be used with caution in patients with active or recent kidney stones because of the potential to exacerbate this condition. It is common practice to follow abaloparatide treatment with an antiresorptive agent, usually a bisphosphonate or denosumab, to maintain or further increase BMD.
RANKL inhibitor (denosumab)
The cytokine RANK-ligand (RANKL) produced by osteocytes is required for osteoclast formation. Suppressing RANKL blocks osteoclast formation, leading to less bone resorption and higher bone density.
Denosumab, brand name Prolia®
Denosumab is a fully human monoclonal antibody against RANKL approved by the FDA for treatment of men and women at high risk for fracture (which is defined as a history of osteoporotic fracture and/or multiple risk factors for fracture). It is approved for treatment of patients who have failed or are intolerant to other available osteoporosis therapy, to treat postmenopausal women with osteoporosis at high risk for fracture, to increase bone mass in men with osteoporosis at high risk for fracture, to treat glucocorticoid-induced osteoporosis in men and women at high risk for fracture, to increase bone mass in men at high risk for fracture receiving androgen deprivation therapy for nonmetastatic prostate cancer, and to increase bone mass in women at high risk for fracture receiving adjuvant aromatase inhibitor therapy for breast cancer.
Drug efficacy
Denosumab is one of the most potent antiresorptive drugs available to treat osteoporosis because it directly inhibits osteoclast formation and causes apoptosis of mature osteoclasts. Denosumab reduces incidence of vertebral fractures by about 68% at 1 year, hip fractures by about 40% and non-vertebral fractures by about 20% at 3 years, with continued fracture reduction in studies extended to 5 years [160, 185, 186]. Longer-term use is associated with a significant 48% reduction in the risk of all upper limb fractures and a 43%, 43%, and 58% reduction in risk of forearm, wrist, and humerus fractures at 7 years [187, 188].
Drug administration
Denosumab is administered as 60 mg subcutaneous injection by a health professional every 6 months.
Side effects and drug safety
Denosumab may cause or exacerbate hypocalcemia, and therefore, hypocalcemia must be corrected before treatment. Denosumab has been associated with hypersensitivity reactions, including angioedema, erythema multiforme, dermatitis, rash, and urticaria. Studies have reported higher incidence of serious infection in women taking denosumab; however, no clear clinical pattern has emerged to suggest a relationship to duration of exposure to denosumab [189]. Safety profiles overall are similar to bisphosphonates and placebo, with no new safety concerns emerging in extension trials up to 10 years, although a theoretical infection risk exists with RANKL inhibition and prescribing information states that patients on concomitant immunosuppressant agents or with impaired immune systems may be at increased risk for serious infections [190, 191]. Denosumab has been associated with very rare cases of AFF and ONJ. (See boxed discussion below.)
Discontinuation of denosumab treatment is associated with rapid bone loss that may result in multiple vertebral fractures, especially in patients with a prior vertebral fracture [192]. For this reason, a drug holiday is not appropriate with denosumab. During periods of suspended treatment, and as recommended by the FDA, alternate antiresorptive therapy should be considered to maintain gains in bone density. Following denosumab with alendronate has been shown to preserve bone mass, while following it with teriparatide has been associated with bone loss at some skeletal sites [193].
Sclerostin inhibitor (romosozumab)
Romosozumab-aqqg, brand name EVENITY™
Romosozumab is a fully human monoclonal antibody to sclerostin. It is currently FDA-approved for treatment of osteoporosis in postmenopausal women at high risk for fracture—defined as a history of osteoporotic fracture, or multiple risk factors for fracture, or poor response or intolerance to other available osteoporosis therapies. (Romosozumab is approved for men with osteoporosis at high risk of fracture in some countries but not in the USA.)
Drug efficacy
Romosozumab reduces fractures and increases BMD at the lumbar spine and total hip more than placebo, alendronate, and teriparatide in postmenopausal women with low bone mass [194–196]. In the pivotal FRAME trial, romosozumab compared to placebo for 12 months reduced risk of new vertebral fracture by 73% and clinical fractures by 36% [196]. In the ARCH study, high-risk postmenopausal women had significantly fewer fractures when treated with romosozumab than with alendronate (48% fewer new vertebral fractures, 19% fewer non-vertebral fractures, and 38% fewer hip fractures) for 12 months [197].
Extension studies have reported BMD trending back towards pretreatment levels after discontinuing therapy. Follow-on therapy with denosumab and, to a lesser degree, alendronate preserve or continue to accrue BMD benefits following romosozumab therapy [196, 198, 199].
Drug administration
Romosozumab (210 mg) is administered in monthly doses by subcutaneous injection for 12 months. Each dose consists of two injections (105 mg each) that are given one immediately following the other by a healthcare professional. Use is limited to 1 year due to the waning of bone-forming effect after 12 months/doses.
Side effects and drug safety
Romosozumab received FDA approval with a boxed warning stating that it may increase risks for myocardial infarction, stroke, and cardiovascular (CV) death. It should not be taken by women who experienced a stroke or CV event in the previous year. Romosozumab may cause hypocalcemia, and therefore, hypocalcemia must be corrected before treatment. In studies, romosozumab has been associated with hypersensitivity reactions, including angioedema, erythema multiforme, dermatitis, rash, and urticaria. Romosozumab has been associated with rare cases of AFF and ONJ (fewer cases than denosumab). (See boxed discussion below.)
Calcitonin salmon
Calcitonin is a hormone endogenous in humans that is found in salmon and other fish, reptiles, birds, and mammals. It works by preventing bone breakdown, thereby increasing bone density. Because more effective drugs are available for prevention of bone loss and reduction of fracture risk, calcitonin salmon is considered second-line therapy reserved for women in whom alternative treatments are not suitable.
Calcitonin, brand name, Miacalcin® or Fortical® and generic calcitonin
Calcitonin is FDA approved for the treatment of osteoporosis in postmenopausal women who are at least 5 years following menopause.
Drug efficacy
In two RCTs, calcitonin salmon nasal spray increased lumbar vertebral BMD relative to placebo in women with low bone mass who were greater than 5 years post menopause. No increase in BMD has been demonstrated in cortical bone of the forearm or hip.
Calcitonin reduces vertebral fracture occurrence by about 30% in those with prior vertebral fractures but does not reduce the risk of non-vertebral fractures [200]. Calcitonin significantly reduces pain associated with vertebral, crush fractures in many patients, making early mobilization possible [201, 202].
Drug administration
Calcitonin is administered in 200-unit doses delivered as a single daily intranasal spray. Subcutaneous administration by injection also is available.
Side effects and drug safety
Intranasal calcitonin can cause rhinitis, epistaxis, and allergic reactions. Long-term post-marketing data meta-analysis of 21 RCTs found cancer risk was higher among calcitonin salmon-treated patients (4.1%) compared with placebo-treated patients (2.9%); therefore, the need for continued therapy should be reevaluated on a periodic basis. Because of its risk–benefit profile, calcitonin is banned in Canada and Europe; it is infrequently used in the USA [203, 204].
Possible adverse events associated with antiresorptive therapies: ONJ and AFF
People using bisphosphonates and denosumab are at low but increased risk for ONJ, a condition in which bone is persistently exposed (usually following an extraction), and AFF, in which a femur breaks spontaneously, often with no warning. Romosozumab use has rarely been associated with ONJ and AFF according to the current studies.
Osteonecrosis of the jaw (ONJ).
ONJ is more frequently associated with high-dose intravenous bisphosphonate treatment for cancer (96% of cases reported). For patients taking oral bisphosphonates to manage osteoporosis, the incidence of ONJ is estimated to be between 1/10,000 and 1/100,000 and is only slightly higher than the ONJ incidence in the general population[205–207]. The risk of ONJ appears to increase with bisphosphonate treatment beyond 5 years. ONJ has been reported in > 2% of studied cancer patients taking high doses of denosumab (XGEVA®) [208].
The American Dental Association (ADA) reports that sound oral hygiene practices and regular dental care may be the optimal method for lowering risk of drug-related ONJ. No validated diagnostic technique is currently available to determine which patients are at increased risk. The magnitude of risk reduction associated with discontinuing antiresorptive therapy even in those with ONJ is not known but must be weighed against known negative outcomes of low bone density and fractures [207, 209, 210].
Atypical femur fracture (AFF)
While reports show that ONJ is more common in cancer patients treated with bisphosphonates, rates of AFF appear lower in these patients, possibly related to shorter duration of use or other mechanisms [205, 211, 212]. AFFs can occur with little or no trauma and may be bilateral. AFF incidence is very low in the general untreated population. Higher risk is associated with Asian ethnicity (North American), lateral bowing of the femur, autoimmune disease, and glucocorticoid use [213]. AFF has been reported in people taking bisphosphonates, denosumab, and romosozumab (association with duration of use is not established).
AFFs are often preceded by pain in the thigh and/or groin area. Clinicians should closely monitor symptoms related to these unusual fractures, proactively questioning patients about occurrence of any thigh and/or groin pain. Patients who present with this prodrome may have experienced stress fracture in the subtrochanteric region or femoral shaft. Bilateral femoral X-rays should be ordered, followed by an MRI or a radionuclide bone scan when clinical suspicion is high enough [214].
Another option, available on newer DXA systems, is single-energy X-ray absorptiometry, an imaging method that detects early signs of AFF [215]. The femur is imaged using a single X-ray beam to detect localized cortical abnormalities characteristic of an incomplete atypical femur fracture. The test is generally rapid (under 1 min) and can be used to identify AFF in patients on bisphosphonates, denosumab, or romosozumab, who are experiencing groin or thigh pain suggestive of stress fracture in the subtrochanteric region or femoral shaft.
Surgical fixation of one or both femurs is required in some cases of AFF; whereas, medical conservative treatment is appropriate in other cases. If AFF is confirmed, bisphosphonates should be discontinued [14]. Although off-label treatment with an anabolic agent following AFF in association with bisphosphonate use is promising, there are limited data to support this regimen [216].
For patients taking bisphosphonates for osteoporosis, the absolute risk of AFF is low: ranging between 3.2 and 50 cases/100,000 person-years, an estimate that appears to double with prolonged duration of bisphosphonate use (> 3 years, median duration 7 years), and decline rapidly with discontinuation [206, 217].
AFF has been seen in patients taking denosumab for osteoporosis (1/2343 patients in the FREEDOM Trial extension followed for 10 years) [218, 219]. Denosumab treatment should be discontinued in the event of the rare occurrence of AFF in patients on denosumab. Another antiresorptive therapy should be started for a few years after stopping denosumab (post AFF) [220].
Romosozumab has rarely been associated with ONJ or AFF. However, because it is a weak antiresorptive, these adverse side effects are biologically plausible.
When discussing risk of ONJ and AFF with high-risk adults, it is important to make clear that the risk for fracture associated with not treating far exceeds the risk for these unusual adverse effects of treatment [212, 221, 222]. Although more data are needed, clinical approaches are being implemented to minimize risk.
Treatment considerations: pharmacologic therapy
(Note: Risk reduction data for vertebral and non-vertebral fractures being discussed in this Guide come from the FDA Prescribing Information, which includes RCTs. In the absence of head-to-head trials, direct comparisons of risk reduction among drugs cannot be made.)
All patients being considered for osteoporosis treatment should be counseled on risk factor reduction, including the importance of calcium, vitamin D, elimination of tobacco use, moderation of alcohol intake, physical activity, and fall prevention (Table 12). Prior to initiating treatment, patients should be evaluated for secondary causes of bone fragility and have BMD measurements by central DXA, when available, and vertebral imaging studies when appropriate. (See vertebral imaging above.)
Table 12.
Treatment of osteoporosis in postmenopausal women and men aged 50 years and older
| General principles | |
|---|---|
| •Obtain a detailed patient history pertaining to clinical risk factors for osteoporosis-related fractures and falls. | |
| •Perform physical examination, measure height, and obtain diagnostic studies to evaluate for signs of osteoporosis and its secondary causes. | |
| •Modify diet/supplements, lifestyle, and other modifiable clinical risk factors for fracture. | |
| •Perform vertebral imaging when appropriate to complete risk assessment. | |
| •Decisions on whom to treat and how to treat should be based on clinical judgment using this Guide and all available clinical information. | |
| Consider FDA-approved medical therapies based on the following in adults ≥ 50 years | |
| •Fracture of vertebrae (clinical or subclinical), hip, wrist, pelvis, or humerus. | |
| •DXA T-score − 2.5 or lower in the lumbar spine, femoral neck, or total hip. Predictive value of isolated measurement of 1/3 radius is currently being investigated (use clinical judgment). | |
| •Low bone mass (osteopenia) and a US-adapted WHO 10-year probability of a hip fracture ≥ 3% or 10-year probability of any major osteoporosis-related fracture ≥ 20%. | |
| •Patient preferences may indicate treatment for people with 10-year fracture probabilities above or below these levels. | |
| Consider non-medical therapeutic interventions | |
| •Evaluate and address modifiable risk factors related to bone loss and/or falling. | |
| •Referral for physical and/or occupational therapy evaluation (e.g., walking aids and other assistive devices). | |
| •Encourage weight-bearing, muscle-strengthening, and balance-training activities and refer as needed. | |
| Follow-up | |
| •Patients not requiring medical therapies at the time of initial evaluation should be clinically reevaluated as medically appropriate. | |
| •Patients taking FDA-approved medications should have laboratory and bone density reevaluation after 2 years or more frequently when medically appropriate. | |
| •To identify any new vertebral fractures that have occurred in the interval, vertebral imaging should be repeated if there is documented height loss, new back pain, postural change, or suspicious finding on chest X-ray, following the last (or first) vertebral imaging test and in patients being considered for a temporary cessation of bisphosphonate therapy. | |
| •Regularly assess compliance and persistence with the therapeutic regimen (at least annually). |
Postmenopausal women and men aged 50 years and older presenting with the following should be considered for treatment:
A hip or vertebral fracture (clinically apparent or found on vertebral imaging) regardless of T-score. There are abundant data in patients with spine or hip fractures treated with approved pharmacologic agents that fracture incidence goes down. This is true for patients with previous fractures whether the T-score classification is normal, low bone mass (i.e., osteopenia), or osteoporosis [155, 157, 185, 200, 223–227]. In patients with a hip or spine fracture, T-score is not as important as fracture history in predicting future risk of fracture and antifracture efficacy from treatment.
A fracture of the pelvis, proximal humerus, or distal forearm in a person with low bone mass or osteopenia, whether a postmenopausal woman or a man aged ≥ 50 years [40, 41, 228]. In persons with fractures of the pelvis, proximal humerus, or distal forearm who do not have osteopenia or low BMD, the decision to treat should be individualized [12, 13].
T-score ≤ − 2.5 at the femoral neck, total hip, lumbar spine, or 33% radius (significant correlation between T-scores at the wrist, hip, and lumbar spine T-score has been reported in research). Decades of high-quality evidence demonstrate that pharmacotherapy prevents fracture in patients with osteoporosis by BMD-DXA at any clinically relevant site [65, 164, 180, 183–185, 196, 198, 224, 228–237].
Low bone mass and FRAX® score above recommended treatment threshold. High fracture risk and need for pharmacologic intervention are indicated by T-score between − 1.0 and − 2.5 at the femoral neck or total hip and a 10-year probability of a hip fracture ≥ 3% or a 10-year probability of a major osteoporosis-related fracture ≥ 20% based on the US-adapted FRAX® algorithm [17, 18, 76, 238]. A major osteoporotic fracture is defined as a fracture at the hip, wrist, humerus, or spine. Although FRAX®-calculated fracture risk prediction has been confirmed in multiple studies, there are relatively few data confirming fracture risk reductions in patients selected for treatment on the basis of FRAX® score alone.
Setting and reaching goals of therapy
With the availability of measurable benchmarks such as BMD, fracture incidence, and biochemical markers of bone turnover, the “treat-to-target” strategy of outcomes-focused therapy, monitoring, and reassessment can be applied to management of osteoporosis.
For appropriate patients initiating therapy, a reasonable 3-year target outcome could be to increase T-score from − 2.8 to > − 2.5 and have no fractures. Stable BMD and a year with no new fractures could be a measurable goal for someone with low BMD and prior fragility fractures. In both cases, if the patient is not on track to reach the target or fails to reach the target, consideration should be given to clinical reassessment and possibly a change in therapy.
However, fundamental to the concept of “treat-to-target” is the principle that response to therapy is not necessarily sufficient to achieve an acceptable level of risk. A patient may reach their “target” BMD and still be at unacceptably high risk for fracture. This principle has implications for the selection of initial therapy to reduce fracture risk [239]. For example, while an oral bisphosphonate alone can reduce risk to an acceptable level in a moderate-risk patient (T-score > − 2.5, no fractures, low FRAX®), it may not be sufficient in a high-risk patient (T-score < − 2.5, multiple fractures, high FRAX® score). In the high-risk patient, an anabolic agent followed by antiresorptive therapy might have a better chance of achieving meaningful increases in bone density than antiresorptive therapy alone.
Treat-to-target management recommendations
The ideal medication for initiating therapy is one best able to sufficiently reduce risk, while accommodating a patient’s needs and preferences. Consistent with the treat-to-target concept, individual patients with osteoporosis should be risk stratified before initiating treatment. Site-specific vulnerabilities can be factored in, such as recent wrist or vertebral fracture, and presented to the patient along with fracture reduction data for each of the treatments.
Speed of effect onset should be considered in relation to a patient’s imminent fracture risk. In some settings, such as recent fracture or very low BMD, an agent with rapid effect onset may be preferable to one that takes longer to act. Many RCTs of osteoporosis therapies have shown benefit for fracture reduction at the spine within the first year of treatment (e.g., zoledronic acid, denosumab, and romosozumab) [33, 240]. It is important to treat patients promptly after a fracture to reduce future risk. A patient with a recent fracture and/or very low BMD (e.g., T-score < − 3.0) is at especially elevated risk and more rapid-acting aggressive antifracture therapy should be considered.
A systematic review and meta-analysis of 107 RCTs of osteoporosis interventions in postmenopausal women (mean age 66 years) with primary osteoporosis was performed and included in the 2019 Endocrine Society Clinical Practice Guideline [166]. The Endocrine Society’s treatment algorithm provides guidance on the management of postmenopausal osteoporosis according to fracture risk:
Low risk: (No previous spine or hip fracture; a T-score at hip and spine above − 1.0 and a FRAX® score below treatment thresholds.) Reassess fracture risk in 2 to 4 years.
Moderate risk: (No previous spine or hip fracture; a T-score between − 1.0 and − 2.5 and a FRAX® score below treatment thresholds.) Reassess fracture risk in 2 to 4 years.
High risk: (Prior spine or hip fracture; or a lumbar spine or hip T-score of − 2.5 or below; and/or a FRAX® 10-year absolute fracture risk above treatment threshold.) Initial treatment with bisphosphonates (alendronate, risedronate, or zoledronic acid). Initial treatment with denosumab as alternative therapy to reduce fracture risk. (Ibandronate not recommended to reduce hip and non-vertebral fractures.)
Raloxifene or bazedoxifene to prevent vertebral fractures in women with a high risk of breast cancer. In postmenopausal women, estrogen treatment to reduce the risk of vertebral fractures in women with a low risk for deep vein thrombosis and for whom bisphosphonates or denosumab are not appropriate. Nasal spray calcitonin should be prescribed only in women who cannot tolerate raloxifene, bisphosphonates, estrogen, denosumab, abaloparatide, or teriparatide or for whom these therapies are not considered appropriate.
Very high risk: (Multiple spine fractures/hip fracture and T-score of − 2.5 or lower at lumbar spine or hip.) Teriparatide or abaloparatide treatment for up to 2 years or romosozumab for 1 year. Following a course of anabolic, treatment with antiresorptive osteoporosis therapies should be used to maintain bone density gains.
More information on the Endocrine Society treatment algorithm is presented in the Endocrine Society published Clinical Practice Guideline [166].
Sequential and combination therapy
Patients with recent fractures and/or very low BMD (e.g., T-score < − 3.0) are at especially high risk for future fracture(s). Monotherapy with antiresorptives may not be sufficient to lower risk to acceptable levels in such patients. Consideration of more aggressive therapy with combination or sequential use of antifracture medications may be warranted [197, 241–245].
Combination and/or sequential use of anabolic (e.g., teriparatide) and potent antiresorptive (e.g., denosumab) have been shown to increase BMD and improve bone microarchitecture and strength more effectively than monotherapy with any one agent [239, 241, 242, 246]. Combination therapy in which an anabolic agent and antiresorptive therapy are co-administered may be appropriate in a setting of very high risk, such as multiple vertebral fractures. Further studies are needed to test effects of combination therapy on incident fractures. There are no indications for combining two antiresorptive treatments.
There is accumulating evidence that BMD and fracture outcomes are significantly influenced by the order in which antifracture agents are administered. An anabolic agent administered following antiresorptive therapy has demonstrably less impact on BMD than if the anabolic is administered first [247–249]. Anabolic therapy after a potent antiresorptive agent may be followed by an attenuation of effect or even bone loss [193, 250]. When sequential treatment is considered, starting with anabolic therapy and following with an antiresorptive agent is preferred.
Multiple variables affect outcomes: agent prescribed, patient characteristics, and duration of treatment, for example. More research is needed to determine the best order and most appropriate drugs for combination and sequential therapy in individual patients.
Improving patient adherence with prescribed treatment
An estimated 25–30% of osteoporosis patients do not start taking their prescribed medication and 50% or more do not continue treatment after 1 year [251, 252]. The consequences are significant: 30% higher incidence of fracture in non-adherent patients compared to adherent patients with attendant higher morbidity, mortality, and healthcare costs [253, 254].
Patients may unintentionally fail to initiate treatment due to forgetfulness, complexity of treatment regimen, and/or drug affordability [255]. In patients who intentionally do not adhere to recommended treatment, the main reasons cited in studies include limited knowledge of osteoporosis, fear of side effects, distrust of physicians or medication in general, and a lack of belief in the need for medication and/or its effectiveness [256–259].
Acceptance of risk is sometimes influenced by competing priorities. This is reflected in findings from a systematic review of research on women’s preferences and values in relation to osteoporosis management published by Barrionuevo et al. in 2019 [260]. The top-ranked consideration was a tie between drug effectiveness and side effects. Not as important were convenience and frequency of doses. (Oral doses were preferred except in the case of biannual or annual dosing, in which case, injection ranked higher.) Even less important were cost and duration of treatment.
Patients often do not understand their personal risk for fractures and the profoundly negative impact that fractures could have on their quality of life, particularly their ability to live independently [261]. This is a challenge inherent to treating “silent diseases” like osteoporosis in which symptoms do not get observably better or worse in response to therapy.
Patient awareness of risk for fractures and their devastating consequences does not guarantee acceptance of antifracture treatment. The 2019 Patient Oriented Value Report commissioned by BHOF appears to indicate that even when awareness of risks and available treatments were high, most individuals at risk for a fragility fracture choose not to take medications needed to reduce their risk. Various factors were associated with willingness to start or continue treatment: dual anabolic–antiresorptive action increased acceptance of a novel treatment agent; history of fragility fracture increased willingness to continue treatment. In a subset of patients, side effects and/or cost burden severely limited willingness to start and stay on treatment [262].
Getting off to a good start matters. Population studies of patients taking oral bisphosphonates demonstrate a strong association between optimal adherence the first year of treatment and higher rates of adherence in subsequent years. This suggests that focused support and monitoring early in treatment may help improve a patient’s long-term adherence and fracture outcomes.
When discussing medication options with patients, solicit their questions and concerns regarding the drug, dosing regimen (daily, weekly, monthly, every 6 months, or yearly), its benefits, and side effects. Asking questions about patient preferences and addressing fears and misconceptions as part of the medication selection process can promote better adherence to prescribed treatment and better outcomes in the form of fractures and disability prevented.
Duration of treatment
Like any lifelong chronic disease, osteoporosis is most successfully managed with continued therapy and monitoring. Therapeutic benefits can be maintained only with treatment. Once pharmacologic therapy is stopped, BMD and fracture risk can be expected to return to baseline or worse—slowly, in the case of bisphosphonates, or quickly, in the case of non-bisphosphonates, when discontinuation is associated with accelerated bone turnover, rapid bone loss, and increased risk for spontaneous fractures.
Successful treatment can increase BMD, reduce fracture risk, and improve T-score to the low bone mass or even the normal range. However, in a person with a history of osteoporosis, a T-score in the osteopenic or normal range does not change their diagnosis. The patient still has osteoporosis. BMD may be improved, and fracture risk reduced; however, microarchitectural deterioration remains, as do disease processes responsible for that deterioration.
With this in mind, serial DXA scans must be interpreted in the context of past DXA T-scores, fracture history, and the other factors that established the original osteoporosis diagnosis [263]. Changing a patient’s diagnosis to osteopenia from osteoporosis could limit that patient’s treatment options and may be detrimental to their bone health.
Available evidence indicates the incidence of rare adverse events such as AFF increases with longer-term antiresorptive therapy (over 3 or 5 years depending on agent) [217, 264]. Consideration of potential risks associated with continued therapy must be weighed against potential risks of discontinuing therapy.
Bisphosphonate holiday
For patients on bisphosphonates who appear to be at modest risk of fracture (e.g., T-score > − 2.5 and no recent fracture) temporary discontinuation (“holiday”) can be considered after 3 years on an intravenous therapy or 5 years on an oral therapy. A bisphosphonate holiday is defined as a temporary suspension of bisphosphonate therapy (up to 5 years) [166, 265]. For patients who continue to demonstrate high fracture risk (e.g., T-score ≤ − 2.5 and/or recent fracture), continued treatment with a bisphosphonate or alternate therapy should be considered up to 10 years with an oral bisphosphonate and up to 6 years with annual IV zoledronic acid. This suggestion is consistent with ASBMR task force recommendations on managing patients on long-term bisphosphonate therapy [14].
The rationale for a bisphosphonate holiday is the expectation that prolonged skeletal retention will confer antifracture benefits for some period of time, perhaps several years, in appropriately selected patients. A period off the drug may reduce risk for ONJ and AFF [221, 229]. Decisions about how long to treat with a particular drug must be tailored to individual patients, applying the best available clinical guidelines and expert recommendations [266].
For patients treated with a non-bisphosphonate, therapeutic effect rapidly dissipates with discontinuation. Studies indicate that discontinuing denosumab results in increased bone turnover markers, reduced BMD, and increased risk of multiple vertebral fractures, especially in patients with a prior vertebral fracture [192, 267]. The Endocrine Society guideline for treatment of postmenopausal osteoporosis recommends that denosumab be continued for 5 to 10 years depending on fracture risk [166]. After discontinuing treatment with denosumab, it is recommended by the FDA that patients be switched to another antiresorptive agent, such as a bisphosphonate, to preserve bone density gains [268]. Studies are ongoing to assess the time course for starting antiresorptive therapies after stopping denosumab.
The management algorithm for bisphosphonate treatment in postmenopausal osteoporosis shown in Fig. 6 is based on ASBMR task force evaluation of data from the Fracture Intervention Trial Long-term Extension (FLEX) and the Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly (HORIZON) extension studies [14]. It suggests that women who experience a fracture before or after being treated with bisphosphonates (oral 5 years, IV 3 years) should continue bisphosphonate therapy (oral up to 10 years, IV up to 6 years). Patients who fracture on therapy should be assessed for adherence and secondary causes of osteoporosis. (Note: We lack sufficient data to make specific recommendations regarding alternative antifracture therapy after prolonged bisphosphonate treatment.)
Fig. 5.
This contrast between percentage of people in general population who use wheelchairs (0.859 in 100) and the percentage who use wheelchairs following hip fracture (25 in 100). Sources: 2010 US Census Data [140, 141]
Fig. 6.
Management of long-term bisphosphonate (BP) treatment in postmenopausal women. Note: This flowchart illustrates ASBMR task force recommendations for management of patients taking bisphosphonates. All other osteoporosis drugs lose effect rapidly when discontinued and must be promptly followed by alternative antifracture therapies. Adler RA, et al. (2016), J Bone Miner Res [15]
High fracture risk in this algorithm is defined by older age (70–75 years), 1 or more clinical risk factors for fracture, and/or FRAX score above country-specific intervention thresholds. Recommended reassessment includes clinical evaluation, risk assessment, and bone density measurement by DXA. The interval between DXA scans should be based upon changes that are detectable and clinically significant. Reassessment may be necessary at less than 2 years in patients with a new fracture or in patients who can be expected to experience rapid bone loss due to new clinical risk factors (such as initiation of aromatase inhibitor or androgen deprivation therapy) (See Fig. 6).
Pharmacotherapy should be periodically reviewed to determine whether treatment should be continued, changed, stopped, or resumed. It is reasonable to evaluate patients every 1 to 2 years during any hiatus from active bisphosphonate treatment.
Further research is needed to clarify best practices in this area, although, as noted by the ASBMR in their report, due to advanced age, life expectancy, and comorbidities, it is unlikely that future RCTs will provide data for formulating definitive recommendations in this patient population.
Antifracture treatment in men with osteoporosis
Medications currently FDA approved for osteoporosis treatment in men include: bisphosphonates alendronate, risedronate, and zoledronic acid; bone anabolic teriparatide; and the RANKL inhibitor denosumab. Unless contraindicated, osteoporosis treatment in hypogonadal men with testosterone levels < 200 mg/dL and symptoms of androgen deficiency should include consideration of testosterone therapy. In hypogonadal men at high risk for fracture who are receiving testosterone, addition of a proven antifracture therapy is indicated [58].
All FDA-approved medications to treat osteoporosis in men have been demonstrated in RCTs to increase BMD. Comparable RCT data for fracture risk reduction exist but are more limited. Fixed-effects meta-analyses of 22 studies demonstrated significantly fewer vertebral fractures in men taking alendronate (67% reduction) and risedronate (57% reduction), but not in men taking calcitonin or denosumab [269]. Another meta-analysis, conducted for the USPSTF found that available data suggest zoledronic acid reduces risk of morphometric vertebral fractures in men by 67%, with no comparable reduction in risk of clinical vertebral fractures or hip fractures [22].
None of the RCTs evaluating efficacy of bisphosphonates in treating men with cancer treatment-induced bone loss (CTIBL) have been powered to evaluate fracture rates as a primary outcome. However, the denosumab Hormone Ablation Bone Loss Trial (HALT) was adequately powered to demonstrate a statistically significant decrease in new vertebral fractures in men treated for 3 years with denosumab (1.5% versus 3.9% with placebo, relative risk = 0.38; 95% CI = 0.19–0.78; P = 0.006) [270, 271].
Antifracture treatment in patients treated with glucocorticoids
An estimated 3% of adults aged 50 years and older are treated with glucocorticoids [272]. Glucocorticoid therapy is associated with an early increased risk of fractures through multiple mechanisms, including accelerated bone resorption; alterations in PTH pulsatility; and reduction in bone formation, sex steroids, and renal calcium reabsorption [273]. Glucocorticoids cause a dose-dependent loss of BMD in the spine and hip, with the greatest loss in vertebral trabecular bone [274]. Among glucocorticoid users, fracture incidence rises with longer-term use of prednisone (over 5 years), higher doses (> 7.5 mg/day), older age (> 55 years), female sex, and Caucasian ethnicity [275].
The American College of Rheumatology (ACR) 2017 guidelines recommend risk stratifying patients when making decisions about antifracture treatment. Adults ≥ 40 years of age receiving long-term glucocorticoids should be designated as either moderate-to-high risk or low risk of fracture based on BMD, fracture history, and 10-year FRAX® fracture score (with glucocorticoid use selected on FRAX calculator). FRAX® calculations assume a prednisolone dose of 2.5–7.5 mg/day (prednisolone and prednisone doses are nearly equivalent). For people taking higher doses (> 7.5 mg/day), proportional increases in fracture risk can be approximated by raising the FRAX® score: a relative 15% for major osteoporotic fracture and 20% for hip fracture risk [88]. For example, a hip fracture risk estimated at 2.0% with glucocorticoid use checked in FRAX® should be increased to 2.4% if the patient’s prednisone dose is higher than 7.5 mg/day.
Regardless of glucocorticoid dose, patients who exceed the adjusted FRAX® intervention threshold should receive antifracture pharmacotherapy. Likewise, treatment should be initiated in postmenopausal women and men ≥ 50 years of age on glucocorticoid therapy who experience a fragility fracture and/or have a T-score of − 2.5 or lower.
Antifracture treatment in glucocorticoid users has been shown in a Cochrane analysis of RCTs to reduce new vertebral fractures by 43%, similar to effects seen in postmenopausal osteoporosis [276]. In a 3-year study reported by Saag et al., teriparatide produced greater increases in BMD and fewer new vertebral fractures than alendronate in comparable glucocorticoid-treated patients [277]. No significant difference was observed in hip or non-spine fracture outcomes.
Meta-analysis of 3 large RCTs suggests that denosumab is effective in treating patients on glucocorticoids, outperforming bisphosphonates in its effects on lumbar spine and total hip BMD in patients with GIOP. The studies were not sufficiently powered for fracture outcomes [278].
There has been concern that, theoretically, denosumab could increase infection risk in patients on glucocorticoids or concomitant biologic therapies. Data currently available suggest any such increased risk is low and/or comparable to that seen with risedronate and zoledronic acid [279–282].
Antifracture treatment for older-old adults
Current data show that antifracture treatment confers benefits throughout old age. In healthy community-dwelling adults over age 75 years, reported fracture reduction with zoledronic acid, denosumab, teriparatide, and abaloparatide is similar to that seen in younger community-dwelling adults [237, 283–285]. In frail elderly long-term care patients, safety and BMD improvement have been demonstrated in RCTs of alendronate and zoledronic acid treatment [286, 287].
Monitoring treatment response
Appropriate response to treatment and the need for continued medication to treat osteoporosis should be reviewed annually. Clinical assessment should be performed to identify new fractures, falls, and/or new or worsening comorbidities. Repeat bone densitometry and vertebral imaging should be done in patients exhibiting signs of vertebral fracture, such as height loss or back pain. It may be appropriate to measure biochemical markers of bone turnover in specific patients.
Ongoing clinical assessment
It is important to have accurate baseline values against which to compare serial test results. For example, significant height loss detected through yearly measurement may be an indicator of disease progression. Wall-mounted stadiometers are more reliable than freestanding devices. Patients who lose 0.8 in. or more in height either acutely or 1.5 in. cumulatively should have repeat vertebral imaging to determine if fractures have occurred since prior tests. Vertebral fracture while on treatment is associated with very high fracture risk. Consideration of untreated secondary causes of bone loss and/or changes to therapy are appropriate in such patients.
Typically, subclinical morphometric vertebral fractures are diagnostic of osteoporosis. In a patient with significant height loss, diagnosis can be confirmed with VFA performed at the same time as BMD on most modern DXA systems or with conventional lateral thoracic and lumbar spine X-ray.
Serial BMD measurement
Central DXA assessment of the total hip, femoral neck, or lumbar spine is the “gold standard” for serial assessment of BMD. Biological changes in BMD are small compared to inherent error in the test itself, and accurate interpretation of serial BMD studies requires knowing the smallest change in BMD that exceeds testing error. This least significant change (LSC) differs with the densitometry device used, patient assessed, measurement site, and technologist’s skill with patient positioning and test analysis [288]. BMD changes of less than 3–6% at the hip and 2–4% at the spine may be due to precision error of the testing itself. The BHOF recommends considering monitoring BMD at the 33% radius in patients for whom BMD cannot be measured at the spine or hip and in those with hyperparathyroidism or hyperthyroidism or on androgen deprivation therapy for prostate cancer, in those undergoing orthopedic surgery of an upper extremity, or according to clinical judgment [8, 11]. Information on how to assess precision and calculate the LSC for a particular device and/or facility is available at http://www.ISCD.org.
Serial central DXA testing is an important component of osteoporosis management. Measurements for monitoring patients should be performed in accordance with medical necessity, expected response, and in consideration of local regulatory requirements. According to the ISCD, intervals between testing should be guided by the clinical status of each patient. A follow-up BMD should be done after 1 year of initial therapy or a change in therapy, with longer intervals once an effective treatment is established. The American College of Physicians recommends against monitoring BMD in postmenopausal women within a 5-year treatment interval. However, this recommendation was based on low-quality evidence and was rated as a weak recommendation [289]. The BHOF recommends repeating BMD assessments every 2 years in adults ages 65 and older, with the understanding that testing less or more frequently may be warranted in individual patients.
DXA is currently the preferred approach for monitoring treatment response. According the ISCD, if DXA is not available, QCT of the spine or hip or pQCT of the radius can be used in high-risk individuals for decisions regarding treatment. Information about the use of these measures and QCT-based finite element analysis for clinical decisions regarding monitoring and treatment can be found on the ISCD website at https://iscd.org/learn/official-positions/adult-positions/ [59, 290, 291]. Of note: central QCT requires high exposure to ionizing radiation [292].
Biochemical markers of bone turnover
Monitoring bone turnover markers is an alternative way of identifying poor response or nonadherence to therapy. In large RCTs, decreased biochemical markers of bone resorption after 3–6 months of treatment with specific antiresorptive therapies and increased biochemical markers of formation after 1–3 months of specific anabolic therapies have been predictive of greater BMD responses and (in some cases) fracture risk reduction [93, 293]. In order to be meaningful, changes in biochemical markers must exceed the LSC for the specific biomarker being measured. The LSC is calculated by multiplying the “precision error” of a biochemical formation marker (laboratory provided) by 2.77 (95% confidence level). Tests should be obtained early morning after overnight fast to offset effects of diurnal variation and diet. Serial measurements should be made at the same time of day at the same laboratory. (See “Biochemical markers of bone turnover” section.)
Vertebral imaging/vertebral fracture assessment (VFA)
When current imaging by MRI and/or CT performed for other purposes is available, it should be evaluated for identification of vertebral fractures. Vertebral fractures can be directly imaged using standard lateral spine X-ray or DXA-based VFA. Once the first vertebral imaging test has been performed to determine prevalent vertebral fractures (indications above), repeat testing should be performed to identify incident vertebral fractures if there is a change in the patient’s status suggestive of new fracture, including documented height loss, undiagnosed back pain, postural change, or a finding of new vertebral deformity on chest X-ray [67]. If patients are being considered for a bisphosphonate holiday, vertebral imaging can be done to identify any fractures that have occurred during treatment, which would indicate the need for continued treatment with bisphosphonates or another antifracture agent. (See “Vertebral fracture assessment” section.)
Rehabilitation following fragility fracture
Patient care following fragility fracture is a complex process involving three components: minimizing pain, reducing fracture risk, and improving function. Such multifaceted care is most effectively accomplished by a coordinated team of health professionals, often overseen by a primary care provider or, in ideal circumstances, by dedicated fracture liaison (FLS) personnel.
Ongoing physical activity that supports healing and maintenance of bone mass is a key part of rehabilitation following fracture. For patients with fractures or at high risk for fractures instruction in safe body mechanics can reduce disability, improve physical function and quality of life, and lower risk for injurious falls.
The most common fragility fractures are those of the proximal femur (hip), vertebrae (spine), and distal forearm (wrist) [294]. All contribute to disability, pain, and reduced quality of life. An estimated 21% of hip fracture patients 60 years and older die in the year following fracture [295, 296]. Vertebral fractures, which can cause pain and disability, confer smaller but significant increases in hospitalization and mortality risk [297, 298].
Hip fracture rehabilitation
Hip fracture typically requires surgical repair or replacement (proximal femur and/or acetabulum). While RCT data are sparse on the impact of specific rehabilitation protocols, settings, and durations, large observational studies conducted in Italy and Taiwan suggest a mortality benefit for patients who receive intensive, inpatient rehabilitation following hip fracture [299, 300]. Patients who received continuous inpatient rehabilitation had lower death rates at 6 and 12 months than those receiving no therapy or, in the case of the Italian study, those receiving outpatient physical therapy. Furthermore, in a small, randomized trial of functionally limited older adults who had received standard rehabilitation after hip fracture, an additional program of home-based function-oriented activities resulted in modest improvement at 6 and 9 months after randomization. Additional RCTs are needed to assess the clinical relevence of these findings [301].
Fewer than half of hospitalized hip fracture patients recover their pre-fracture competence in activities of daily living [302]. Only one fourth regains previous levels of social functioning [303]. Six months after a fracture, just 15% of hip fracture patients can walk across a room unaided [304]. Consequently, 10–20% of those living independently before a hip fracture require institutional long-term care afterwards [305].
Vertebral fracture rehabilitation
Two thirds of vertebral fractures are subclinical “silent” fractures. The typical symptomatic vertebral compression fracture is characterized by intense back pain lasting more than a couple of days that gets better when the patient lies down. If a spine fracture is suspected, further evaluation by X-ray, MRI, CT, or VFA can confirm the diagnosis.
Vertebral fractures do not usually require hospitalization [306]. However, multiple thoracic and lumbar fractures can cause spinal deformity, leading to restrictive lung disease, constipation, pain, distention, and reduced appetite [307, 308]. Chronic pain, postural weakness, and altered gait can result in impairment equal to that following a hip fracture.
Treatment for acute vertebral fracture includes use of analgesics, bracing (for 2 to 6 weeks), and partial bed rest (4 days or less). If bed rest is recommended, a few 30- to 60-min periods each day of sitting upright and walking around are valuable to avoid stiffness and prevent loss of bone and muscle tissue. Prolonged inactivity should be avoided. Removal of mechanical loads and/or resistive stresses stimulates bone resorption, further weakening bone and muscle [309, 310].
A variety of light-weight back braces and postural supports are available that restrict spinal motion near a fracture site to ease pain and promote healing. Bracing may facilitate stimulation of proprioception to improve spinal extensor muscle control. These orthoses are custom molded and can be fitted by a physiatrist, physical therapist, or other trained clinician. A systematic review, including 4 RCTs (n = 281), investigated effects of spinal orthoses after a vertebral fracture during the acute and chronic phases post-fracture. Evidence for the benefit of bracing on pain in the acute phase (3–12 weeks after fracture) is lacking. However, there is low-quality evidence (high risk of bias due to no blinding) that bracing may have beneficial effects on pain, spinal strength, kyphosis, pulmonary volume, and quality of life at 6 months following fracture. Bracing worn 2 hours a day over 6 months appears beneficial. Type of brace does not appear to make a difference. There is no evidence that bracing improves physical function or disability [311].
Wrist fracture rehabilitation
Osteoporosis-related forearm or wrist fractures (fractures of the 1/3 radius, ulna, or both) are the most common fractures of the upper extremities. Depending on the type of fracture, treatment may consist of splint, cast, or brace immobilization. If a radius fracture is not displaced, a cast or functional brace is used until there is radiographic evidence of union. Surgical treatment has been used more recently because of faster functional recovery. Open reduction with internal fixation (ORIF) and closed reduction with percutaneous pinning (CRPP) are procedures often used for unstable distal radius fractures [39, 312, 313]. During the cast or bracing stage, arm elevation, early mobilization, and edema-control measures are implemented.
There is literature to suggest that early rehabilitation focused on digital mobility yields superior functional outcomes and patient satisfaction [314]. Targeted therapy can improve finger dexterity, even while the hand is immobilized in a cast. Unfortunately, 90% of wrist fracture patients are not referred to physical/occupational therapy during this critical period.
Management of acute fracture pain
Because pain is a barrier to movement and activity, effective pain management is a cornerstone of fracture rehabilitation, preservation of bone tissue, and ongoing fracture prevention. Conservative therapeutic options for acute pain from recent vertebral fractures include analgesics such as acetaminophen, nonsteroidal anti-inflammatory drugs, narcotics, and calcitonin, as well as limited bed rest, bracing, physical therapy, nerve root blocks, and epidural injections.
Multifactorial pain management strategies are currently underutilized. The recent US National Pain Strategy Report emphasizes the need for development and implementation of effective interdisciplinary pain treatment programs focused on patient-directed self-care that employ a range of approaches, both pharmacologic and non-pharmacologic [315]. Multimodal pain management is now a mandated performance measure for hospitals and medical facilities accredited by The Joint Commission (USA). These modalities include acupuncture therapy, chiropractic therapy, ice/heat, massage therapy, physical therapy (PT), electrical stimulation (E-Stim), relaxation therapy, and cognitive behavioral therapy (CBT) [316].
In the 3–5 days immediately following fracture, acetaminophen and/or low-dose narcotics administered around the clock (rather than as needed for pain) can work very well in appropriate patients [317]. When given on a regular schedule over several weeks, this regimen allows patients to remain active and avoid disuse-related muscle and bone loss. Specialist referral is advisable if neurologic involvement is suspected.
Calcitonin salmon has been shown to dramatically reduce acute pain due to recent, nontraumatic osteoporotic vertebral crush fractures. One small RCT that randomized patients to calcitonin nasal spray or placebo spray plus high-dose acetaminophen reported that calcitonin-treated patients had significantly better pain control. This was associated with weeks-earlier mobilization and functional improvement (sitting, standing, walking).
To prevent falls, it is essential to consider disorientation, sedation, and other potential side effects of pain medications, either alone or in combination with other drugs. Because many fracture patients are medicated simultaneously for multiple comorbid conditions, a medical history should include careful attention to potential polypharmacy and drug interactions that could contribute to fall-inducing side effects.
Surgical procedures for acute painful vertebral fracture
A primary source of the intense pain caused by vertebral fracture is movement of fracture margins and/or bone fragments against one another. This is a particular problem in the lumbar spine, which is highly articulated to allow free flexion and rotation. Immobilizing fractured vertebral bone dramatically reduces pain. Prolonged bed rest is not an ideal remedy given resultant deconditioning and bone loss. Extended bracing and physical therapy have been used for this purpose.
Patients with severe acute fracture pain may benefit from referral to a pain specialist and/or interventional radiologist. Unremitting pain that persists despite conservative therapy may respond to short-term specialist treatment and/or minimally invasive vertebral augmentation surgery [318, 319].
Although RCTs comparing vetebroplasty/kyphoplasty to medical management (but not to placebo) have reported conflicting results, some studies found short-term pain control with vertebral augmentation [320–323]. However, when in 2019, the second ASBMR task force compared vertebral augmentation procedures to sham procedures (with/without injected analgesia), it reported little benefit of vertebroplasty for pain control in either acute or sub-acute fracture and insufficient evidence to recommend kyphoplasty over nonsurgical management [324].
Serious complications reported with these procedures include cement pulmonary embolism, osteomyelitis, and epidural cement leak. While fractures of adjacent vertebrae have been reported, analyses of study data are inconclusive [325–328]. Additional long-term data from large well-designed, placebo or sham-operated controlled RCTs are needed to clarify issues related to safety and efficacy of these procedures. Treatment for severe pain should be individualized. Whether recommending specialist surgical or nonsurgical management for pain associated with spine fractures, clinicians should prescribe antifracture pharmacotherapy for the underlying osteoporosis.
Managing chronic post-fracture pain
Acute pain typically resolves 6–8 weeks following vertebral fracture. However, some people have pain for months or years after a fracture heals. Persistent pain like this can make it difficult to sleep, walk, and eat; it can make a person irritable or depressed by depriving him or her of independence and meaningful participation in self-care and community life.
The need for continued activity to prevent loss of bone and muscle mass underlines the importance of pain control. Untreated pain is a strong incentive to avoid potentially painful activities and develop sedentary behavior. This can quickly lead to musculoskeletal deterioration and frailty. Early and sustained physical engagement is essential to restoration of function and quality of life.
Complications of analgesic drugs, such as addiction, kidney failure, and gastrointestinal bleeding, limit their long-term use for many patients. Increasingly, clinicians are employing a variety of non-pharmacologic approaches to managing persistent pain, including cognitive behavioral therapy, hypnosis, mindfulness training, biofeedback, and stress management. As there are few studies of psychological therapies for chronic pain, available evidence is of low-to-moderate quality, and data in support of one modality over another are not currently available [329–331]. Additional research is needed that focuses on risks and benefits for people with osteoporosis and related fractures [332] (Table 13).
Table 13.
| Pain management measure | Applications and considerations for osteoporosis patient care |
|---|---|
| Acetaminophen | 650 mg orally every 4–6 h; maximum dose 4000 mg/day for treatment of mild to moderate pain. No evidence of benefit for neuropathic pain. Liver damage risk (overdose) [336]. |
| Acupuncture | Acupuncture has been demonstrated to control pain in patients with chronic low back pain. Many health insurance providers now offer coverage for these therapies; however, the quality of evidence for their efficacy is low (issues of study design, placebo effect, etc.) [337]. |
|
Antidepressants Amitriptyline Duloxetine |
First-line therapies for neuropathic pain. Amitriptyline (tricyclic antidepressant) 25–100 mg orally once daily or in 2 divided doses. Max single dose 75 mg, doses > 75/day should be used with caution in adults > 65 years [336]. Duloxetine serotonin–norepinephrine reuptake inhibitor (SNRI) 60–120 mg orally once daily or in 2 divided doses. Side effects common to both: somnolence, increased suicidal thoughts, headache, dizziness, dry mouth. Additional side effects amitriptyline: tremor, tachycardia, orthostatic hypotension, constipation, weight gain, urinary incontinence (multiple contraindications). Additional side effects duloxetine: increased blood pressure [338]. |
| (Nonsteroidal) anti-inflammatories (NSAIDs) | Dose depends on drug. Beneficial for suppressing mild-to-moderate inflammation-related pain. May delay bone healing following fracture, except anti-COX-2 NSAIDs. Over-the-counter NSAIDS taken every 6 h following fracture or alternating with acetaminophen can help with pain relief. Adverse reactions of concern include gastrointestinal bleeding, renal insufficiency, myocardial infarction, stroke, and dizziness. No evidence of benefit for neuropathic pain. |
|
Antiepileptics Gabapentin Pregabalin |
First-line therapies for neuropathic pain. Gabapentin 900–3600 mg orally in 3 divided doses. Pregabalin 300–600 mg/day orally in 2 divided doses [336]. Side effects in common: dizziness, somnolence, headache, peripheral edema, nausea, blurred vision, and increased suicidal thoughts. Use with caution in patients with impaired renal function. Abuse and dependence have been reported. Additional side effects/risks of gabapentin: fever, infection, lack of coordination. Additional side effects of pregabalin: weight gain and disorientation. |
| Antispasmodics | Efficacy in relieving pain is not well established and risk for adverse (anticholinergic) effects is high [339]. May increase risk for falls, constipation, and indigestion. |
| Aspirin | 350–650 mg orally every 4 h; maximum dose 3600 mg/day [336]. Beneficial for mild pain (temporary uses). Adverse reactions of concern include gastrointestinal bleeding, tinnitus, insomnia, and dizziness. No evidence of benefit for neuropathic pain. |
| Bed rest (limited/intermittent) | While prolonged bed rest causes bone and muscle loss, immediately following vertebral compression fracture, patients are generally prescribed an initial period of strict bed rest (no sitting or standing) [340]. Even when a patient is back on his/her feet, lying flat for 10 min every couple of hours, for example, is recommended to support activity by keeping pain under control. Further RCT evidence is needed to support specific protocols for rest during recuperation from vertebral fracture [341]. |
| Bracing and spinal orthoses | A variety of soft, semirigid, rigid, and dynamic braces are available for use following vertebral fracture to control pain, promote fracture consolidation, support posture, and improve balance, physical function, and quality of life [342]. Patients typically are instructed to wear orthoses for 12 to 24 weeks until resolution of pain and vertebral instability. RCT data are currently lacking to make evidence-based recommendations []. |
| Calcitonin salmon | Calcitonin salmon has been found to mitigate acute pain from recent vertebral fractures. Limiting use duration is recommended due to potential increased risk for cancer. Not shown to be effective at ameliorating chronic pain from vertebral fractures [343]. |
| Cognitive behavioral therapy (CBT) | Although RCT data are not available, studies have demonstrated CBT and other psychosocial complementary therapies can improve function and quality of life in patients suffering from chronic pain [344, 345]. |
| Complementary therapies | Deep breathing, progressive muscle relaxation, guided imagery, and other relaxation techniques can help release muscle tension and direct a patient’s attention away from pain and related anxiety. Biofeedback therapy can be helpful for managing acute and/or chronic pain due to fractures. Referral should be made to biofeedback specialist [336]. |
| Electric stimulation (E-Stim) | E-Stim, also called transdermal electrical nerve stimulation (TENS), considered an effective non-pharmacologic therapy for chronic pain, uses transmission of a mild electrical current applied to a patient’s skin at the site of injury or pain [346]. Referral to physiatry or physical therapy is required. |
| Ice and heat | Application of ice and/or heat, alternating or individually, can promote healing and be effective in reducing swelling, improving blood flow, and relieving pain of muscle spasms. Specific injury dictates appropriate method, purpose, and application (e.g., heat may not be appropriate for acute fracture with inflammation). |
| Massage | Although no large-scale RCT data exist, evidence from small studies suggest that massage may improve post-fracture pain and disability compared to sham therapies and other non-manipulative interventions (such as relaxation techniques). The ACP guideline on management of chronic low back pain includes a strong recommendation for massage therapy, chiropractic therapy, or spinal manipulation (acknowledged low-quality evidence) [347]. Intense or deep-tissue massage therapy should be avoided in people who have experienced fragility fractures. Cases of massage-induced fractures have been reported [348]. |
| Nerve root block injection | Percutaneous dorsal root ganglion block (nerve block) has been demonstrated to provide immediate and prolonged improvement of chronic pain from vertebral osteoporotic compression fracture in patients who failed conservative treatment or had residual pain after vertebroplasty [349, 350]. Lidocaine injection provides significant short-term (up to 2 weeks) pain relief in new fractures [351] and may promote early mobilization. The AAOS includes nerve root block in its recommended treatments of acute pain following vertebral fracture [352]. |
| Opioids | Opioids are very effective analgesia for acute pain. However, if used chronically, they lose potency, induce dependence, raise risk for addiction, and lead to constipation, falls, and central sensitization. Recommended only for very short-term use with acute fractures. Hence, non-narcotic treatments are preferred. |
|
Topical pain relievers Capsaicin Lidocaine |
Lidocaine 1.8% or 5% patch applied to intact skin at site of pain for up 12 h daily is recommended for chronic peripheral neuropathic pain. Capsaicin 8% patch is a second-line therapy that can be applied in a clinical setting every 3 months [336]. Side effects common to both: application site pain/skin irritation, pruritus, and erythema. Capsaicin can increase blood pressure transiently and can lead to desensitization. Over-the-counter preparations of menthol, methyl salicylate, or OTC capsaicin have shown little to no effect on chronic pain. |
| Vertebroplasty/kyphoplasty | (Not generally recommended) Little benefit of vertebroplasty for pain control and there is insufficient evidence to recommend kyphoplasty over nonsurgical management [311]. |
Patients with pain following fragility fractures may benefit from one or more of the therapeutic interventions described in Table 13. Recommendations are based on available evidence with limited RCT data to support the clinical effectiveness of many of these practices. It is highly recommended that patients work alongside trained professionals and/or an interprofessional team for a given modality.
Protecting fragile bones in daily life and recreation
Following a fragility fracture, modifications to standard activities of daily life and recreation should be considered to prevent subsequent injury. A trained physical therapist and/or occupational therapist can be instrumental in educating patients about safe body dynamics (Fig. 7).
Fig. 7.
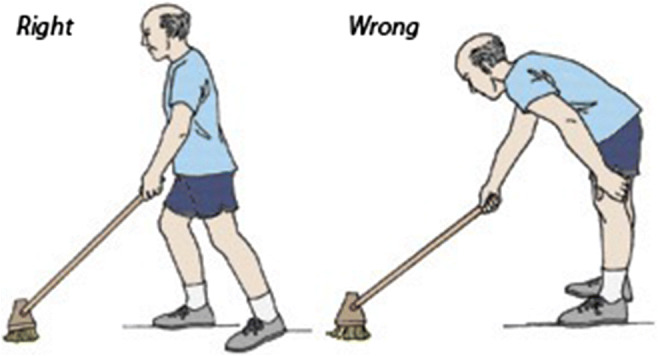
Daily activities and household chores can be modified to minimize risk for vertebral fractures. (NOF [2019] Boning Up on Osteoporosis) [354]
Avoidance of prolonged or excessive loading of individual skeletal sites is a fundamental principle of safety for people with osteoporosis. Distribution of skeletal load is achieved by alignment of the head, shoulders, spine, hips, knees, and ankles, which centers the body’s mass over the lower extremities. The following should be avoided in patients with bone fragility. (Spine-sparing modifications provided.)
Slouching, with head forward, trunk collapsed, and hips positioned forward of center of gravity.
– Modification: Support back while seated to maintain aligned posture with head in neutral alignment.
– Modification: Alternate periods of prolonged standing or sitting with 5–10 min of walking or lying supine.
Lifting an object by bending forward from the waist with legs straight.
– Modification: Bend with knee and hips not spine, stand close to load when bending, hold load close to body.
– Modification: Use grabber to lift lightweight objects, step forward with back straight and knee bent to lower body.
Vacuuming with rotated trunk and feet planted, pushing and pulling with arm fully extended, bending and twisting at waist.
– Modification: Step to turn so that leading foot, torso, and extended arm face the same direction.
– Modification: Shift weight from front to back foot with a straight spine to move the vacuum back and forth.
Recreational pursuits and athletic activities that exert intense forces on weakened bone and/or involve abrupt or high-impact loading can break bones in people with osteoporosis http://www.bonehealthandosteoporosis.org/wp-content/uploads/BoningUpBrochure_8.5x11.pdf [355–357]. Fortunately, many can be modified for safety with input from a trained physical therapist. Ensuring that patients understand potential risks, while focusing on safe approaches to preferred pastimes and sports enables patients to stay active. Potentially injurious activities for individuals with osteoporosis include the following:
Jumping rope or jumping on a trampoline
Horseback riding, downhill skiing, parasailing, sky diving
Running/jogging (beneficial for hip BMD, can be dangerous for low spinal BMD)
Golf, tennis/racquet ball, and bowling (done conventionally with twisting at waist)
The fear of fracture can be a powerful incentive to avoid physical activity, causing predictable harm to bone, muscle, and general health. Spine-sparing strategies for approaching tasks and pastimes help prevent injury while promoting continued mobility and self-confidence. Rather than blanket restrictions (e.g., no bending, no lifting > 10 lb). BHOF recommends guidance on spine-sparing techniques (e.g., hip hinge) by trained occupational and/or physical therapy professionals who have experience working with older individuals.
Safety considerations for physical activity
Older adults with low bone density, osteoporosis, and fractures can safely benefit from activities that promote muscle strength and balance. In the LIFTMOR study, supervised high-intensity physical activity increased bone density, improved function, and reduced kyphosis in postmenopausal women aged 65 ± 5 years with osteoporosis and osteopenia—without elevating risk for vertebral fractures [358, 354].
On the other hand, when done incorrectly, high-intensity and/or impact activities can cause musculoskeletal injuries, especially in people with vertebral fractures, sarcopenia, or cognitive impairment. However, with appropriate technique, intensity, and therapeutic progression, even these vulnerable populations can realize improvements in physical performance [359, 360].
Supervision is recommended to ensure physical activities are safe and sustainable given an individual’s health status, bone fragility, and overall fitness. Individuals with low bone density, osteoporosis, or spinal kyphosis should engage in physical activities with a straight or supported back. Activities that are typically performed with flexion (forward bending under stress) should be avoided unless they are modified to protect the spine. Extreme, end-of-range flexion or rotation should be avoided, especially when loaded (as in lifting objects from the floor). Slow, controlled twisting with the spine supported is acceptable as is midrange (but not end-range) spine flexion/extension in which some of the body’s weight is supported by extremities (bent knee, arm behind back, etc.) (Fig. 8).
Fig. 8.
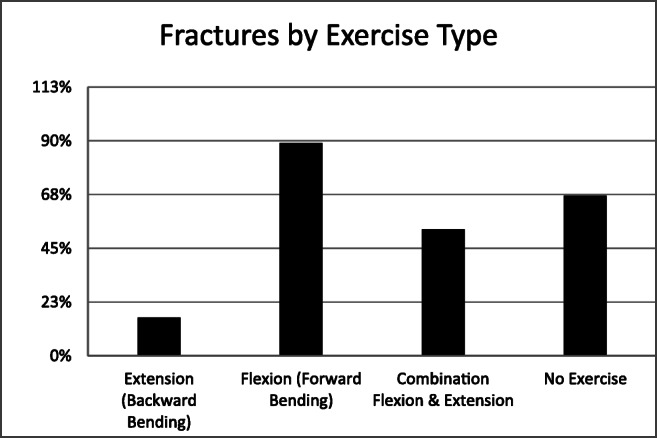
For people with osteoporosis, the harm or benefit conferred by exercise depends on the specific movement involved. Activities that require spinal flexion (forward bending) increase risk of vertebral fracture, while activities that involve spinal extension decrease risk [355]. (Source: Sinaki M, Mikkelsen BA [1984] Arch Phys Med Rehabi)
Recommended progressive resistance training, balance training, and increased loading exercises include the following (Table 14):
Table 14.
How much physical activity? NOF recommendations for people with osteopenia and osteoporosis [54, 357].
| Weight-bearing activities | 30 min on most days of the week in a single 30-min session or in multiple sessions spread throughout the day. (The stimulus has to be greater than what body is used to.) |
|---|---|
| Muscle-strengthening activities | Two to three days per week. Can be done all at once or in multiple short sessions, full body or one body part per day. (For example, arms one day, legs the next and trunk the next.) |
| Balance, posture, and functional activities | Every day or as often as needed. Focus on area of most need: If patient has fallen, balance activities should be emphasized. If patient is hyperkyphotic, focus should be on posture activities. If patient has trouble climbing stairs or getting up from the couch, he/she should do more functional exercises. These activities can be performed at one time or spread throughout the day. |
Lifting weights using back-safe position and technique
Pulling elastic exercise bands
Correct use of weight machines (back lying, side lying, etc.)
Lifting one’s own body weight, such as one-foot stands, and toe rises
Balance exercises that strengthen legs and challenge balance, such as tai chi or slow/controlled dancing
Balance exercises with cognitive element progressing in complexity, e.g., walking a pattern, walking a pattern while holding a cup (mimics real life high-fall-risk situations)
Posture exercises that strengthen back extensor muscles and improve core stability
Functional exercises (simulating common movements/ADLs)
The American Board of Physical Therapy Specialties offers certification to qualified physical therapists who specialize in geriatrics. Patients can find a board-certified geriatric physical therapist in their area through the public portal on the American Physical Therapy Association’s website (http://apta.org).
Secondary fracture prevention
Ideally, all at-risk individuals could be identified and managed to prevent their first fracture (primary prevention). Improvements have been made in detection and management of osteoporosis in women aged 65 years and older. Medicare utilization data show many women in this age group are currently screened by DXA in compliance with HEDIS measures, an increase from 64.4% in 2006 to 72.5% in 2017. Improvements have been seen in treatment following fracture (secondary prevention). Medicare utilization data show testing and treatment rates following any fracture increased from 20.4% in 2007 to 41.1% in 2020 [361]. However, analysis of Medicare data from 2008 to 2014 found that following hip fracture repair, fewer than 1 in 5 women received recommended interventions, despite being at very high risk for future fractures [362].
Other studies have shown even worse rates, with up to 95% of patients discharged following hip fracture repair with no antifracture treatment and a 2.5-fold increased risk of future fracture [29, 30, 363]. Failure to treat high-risk patients can lead to disability and premature death that might have been avoided with appropriate care.
Patient perceptions and beliefs contribute to underutilization of effective osteoporosis therapies. As detailed in the ASBMR report on secondary fracture prevention, most patients do not recognize fracture as a symptom of disease [363, 364]. Clinicians may find it challenging to convince a patient that tripping and breaking a bone is not bad luck, or a particularly hard fall, it is osteoporosis and it will lead to additional fractures if untreated, particularly in the short term.
Understanding the link between treatment and fracture is critical to motivating patients to undertake the many individual steps required to reduce their risk. Simple interventions to preserve bone strength can be recommended at each office visit. In addition to antifracture medication, these interventions include adequate intake of calcium, vitamin D, and protein; regular participation in weight-bearing and muscle-strengthening physical activity; cessation of tobacco use; and recognition and treatment of alcohol abuse.
There are structural factors that contribute to the problem of osteoporosis underdiagnosis and undertreatment as well. Skeletal health overlaps multiple specialties of practice, in both inpatient and outpatient settings. In today’s fragmented healthcare environment, it can be unclear who is responsible for bone health. The orthopedic surgeon who repairs a hip fracture may assume the primary care doctor has it covered, while the primary care doctor assumes the orthopedist took care of any needed bone-related diagnosis and/or treatment when the patient was hospitalized. Continuity of care is complicated by multiple handoffs, particularly after hospitalization: skilled nursing stay, home health, etc. Not only that, there is the challenge of identifying patients at highest risk due to the fact that most fractures occur in people with bone density above the threshold diagnostic of osteoporosis. They have low bone density, but not low enough to meet bone density criteria for intervention [365].
Institutional approaches to secondary fracture prevention have been initiated in the USA and abroad to ensure that patients who fracture are evaluated, treated, and followed so that the potential cascade of fractures is stopped after the first. Evidence-based practice models have emerged that can be adapted for various clinical practice settings. One such model gaining acceptance is the fracture liaison service (FLS).
The fracture liaison service model of care
The FLS system of care in the USA was developed through the National Bone Health Alliance (NBHA), a public–private partnership of 50-plus member organizations along with representatives from the Centers for Disease Control and Prevention, Centers for Medicare & Medicaid Services, National Institutes of Health, and the US Food and Drug Administration [13].
In an FLS system, a multidisciplinary team of healthcare providers works in coordination to implement evidence-based diagnostic and treatment protocols to follow for post-fracture care. The process is overseen by an FLS coordinator (a nurse or other allied health professional) who is charged with overall organization, tracking, and documentation of post-fracture patient care. It is a simple concept, yet its implementation is complicated, requiring planning, division of responsibilities, coordination of staff, systematic and consistent patient monitoring, and knowledge of billing and coding technicalities. Because management of osteoporosis is a multidimensional and long-term undertaking, treatment plan coordination is critical to its effectiveness. Equally critical is patient collaboration. Every aspect of the plan must accommodate patient needs, goals, values, habits, abilities, and living conditions [366, 367].
Since early pilot programs began a decade ago, FLS programs have been successful in the USA and abroad. They have markedly reduced recurrent fractures, particularly in closed medical systems, by targeting interventions at post-fracture patients, recognizing that this group is at highest risk of future fractures.
FLS pilot programs outcomes to date include the following:
Kaiser Permanente’s Healthy Bones program, which has led to an overall 38% reduction in their program’s expected hip fracture rate since 1998.
Geisinger Health System osteoporosis disease management program, which achieved $7.8 million in cost savings over 5 years through reduction of secondary fractures.
American Orthopaedic Association’s Own the Bone program has significantly improved rates of treatment and counseling, BMD testing, initiation of pharmacotherapy, and coordination of care for patients following fragility fracture [368].
NBHA FLS Demonstration Project, a turnkey FLS solution created for sites to automate, benchmark, and improve performance related to selected osteoporosis/post-fracture quality measures demonstrated an increase in DXA and vitamin D level testing and treatment following implementation of the FLS program in three academic hospital settings [45].
The goal of the FLS model, like any practice management program is to ensure patients with a fracture are evaluated and treated for their underlying osteoporosis, while making the best use of clinician time and expertise. Creative approaches optimize use of electronic medical records and practice management software, delegate tasks, automate as much as possible, take advantage of the patient’s waiting room time, and team up colleagues, specialists, allied health professionals, and support staff. There are many tools available for every type of practice, from sole practitioner to hospital-based multispecialty clinic.
Recommendations for secondary fracture prevention
In 2019, a coalition convened by the ASBMR published Clinical Recommendations for Secondary Fracture Prevention to treat the osteoporosis in women and men aged 65 years or older who suffer a spine or hip fracture. Here is a concise summary of the coalition’s recommendations [363].
1. Women and men aged 65 years and older who sustain a spine or hip fracture should be managed by an FLS or a multidisciplinary team to evaluate and treat their underlying osteoporosis and reduce risk of another bone fracture in the next 1–2 years.
2. Primary care and other healthcare providers should be informed about their patient’s fracture, diagnosis of osteoporosis, and future fracture risk, as well as the availability of effective treatment to reduce fracture risk.
3. These women and men should be evaluated for fall risk and provided with referrals as needed (PT, OT, ophthalmology, etc.) to initiate fall prevention measures.
4. Women and men who sustain a spine or hip fracture should be offered effective therapy to reduce their risk for future fractures. Intravenous or oral pharmacological treatments can be started in the hospital or at discharge, although some clinicians prefer to wait to start intravenous zoledronic acid for few weeks (note zoledronic acid is FDA-approved in patients with hip fractures to be prescribed with vitamin D). Treatment should not be delayed.
5. Because osteoporosis is a lifelong condition, long-term follow-up and care should be provided for all affected patients [369].
|
Free or low-cost fracture prevention resources • Fall prevention: Centers for Disease Control and Prevention: STEADI (Stopping Elderly Accidents, Deaths & Injuries) tool kit for health care providers. https://www.cdc.gov/steadi/index.html • General guidance for living with osteoporosis: Boning Up on Osteoporosis. Available at BHOF website: www.bonehealthandosteoporosis.org. • Patient education videos on exercise for people with osteoporosis: https://www.nof.org/patients/fracturesfall-prevention/safe-move-ment-exercise-videos/ • BoneFIT™ an exercise training workshop developed by Osteoporosis Canada to train physical therapists and fitness instructors working with people who have osteoporosis (and are fragile). To learn about the program, including online and in-person training opportunities, please visit: https://osteoporosis.ca/health-care-professionals/bonefit. • American Dental Association (ADA): NOF-ADA joint letter on what is known regarding risk for ONJ and risk for fracture in patients with osteoporosis. Available at http://www.bonehealthandosteoporosis.org/wp-content/uploads/ONJ-letter-FINAL-BHOF.pdf. • ASBMR’s Secondary Fracture Prevention Initiative Coalition comprised of organizations and government agencies is directed at engaging healthcare professionals across multiple disciplines to evaluate and treat women and men age 65 years and older with a hip or vertebral fracture to reduce future risk. https://www.secondaryfractures.org/about-coalition. • American Orthopedic Association Own the Bone® Post-Fragility Fracture Quality Improvement Program. http://www.aoassn.org. (847) 318-7336. • American Orthopedic Association Own the Bone® Orthopaedic Bone Health ECHO®. Each month, a panel of experts will host participants on a videoconferencing platform (Zoom) to discuss current topics related to bone health and to initiate a dialogue around patient cases presented by participants. https://www.ownthebone.org/OTB/Education/ • Bone Health & Osteoporosis Foundation (BHOF) Fracture Prevention Resources. https://www.bonehealthandosteoporosis.org/preventing-fractures/. • FLS Bone Health ECHO (Extension for Community Healthcare Outcomes) program offers case-based clinical discussions on a wide range of topics of interest. By participating, attendees will be able to receive free CME, connect with experts in the field, share case studies, and so much more. http://www.nbha.org/projects/echo. • Bone Source®. Through the BoneSource® website, BHOF offers a variety of programs, tools, and resources to meet the unique needs of healthcare professionals who provide bone health care. https://www.bonehealthandosteoporosis.org/?s=bone+source. (800) 231-4222. |
Remaining questions
This guide has focused on prevention, diagnosis, and treatment of osteoporosis in postmenopausal women and men aged 50 years and older. Much is known about osteoporosis in this population. However, many additional issues urgently need epidemiologic, clinical, and economic research. For example:
What can be done to improve patient adherence and persistence with prescribed antifracture medications.
What is optimal timing and duration of bisphosphonate drug holiday?
What can be done to determine effectiveness of FLS in different care models and to promote the FLS model to improve identification, diagnosis, and treatment following an acute fracture?
How can FLS programs be implemented and funded nationwide to ensure treatment of patients with fragility fractures and reduce the imminent risk of fractures and other complications?
How can the FRAX® algorithm be expanded to incorporate information on lumbar spine BMD and on multiple fractures into its quantitative risk assessment?
Can a fracture risk calculator be developed for patients who have already initiated pharmacologic therapy? Would a calculator be helpful in determining when to initiate a bisphosphonate holiday and/or reinstitute therapy in high-risk patients?
What is the optimal type, intensity, duration, and frequency of exercise programs for osteoporosis prevention and treatment?
For individuals with vertebral fractures, what exercise is safe and effective in lowering incidence of fractures and falls and improving patient-centered outcomes (pain, function).
How effective and safe are different FDA-approved treatments in preventing fractures in patients with low bone mass (osteopenia)? Do benefits exceed risks?
What approaches are most effective in treating osteoporosis in patients with spinal cord injuries and other disabilities?
How can we standardize radiological technologies for diagnosis of vertebral fractures (e.g., X-rays, CT, and MRI) to make them more quantitative, accurate, and consistent, particularly in the case of mild fractures?
What is the role of DXA forearm bone density measurement in predicting wrist and other fragility fractures? Is an isolated forearm BMD diagnostically sufficient to support treatment?
Will use of DXA to assess atypical femur fractures improve early diagnosis or will false positives result in unneeded imaging and heightened costs and/or concerns?
How can we better assess bone strength using non-invasive technologies and thus better identify patients at high-risk for fracture?
What is the optimal approach to treating atypical femur fracture?
How should bone turnover biomarkers and/or BMD be used to monitor the duration of bisphosphonate holidays?
What are the effects of combined anabolic and antiresorptive therapies on fracture outcomes?
Can we identify agents that will significantly increase bone mass and restore normal bone structure?
Can future osteoporosis therapies cure this prevalent disease?
The Bone Health and Osteoporosis Foundation (BHOF) is committed to continuing the effort to answer these and other questions related to this debilitating disease with the goal of eliminating osteoporosis as a threat to the health of present and future generations. For additional resources on osteoporosis and bone health, visit http://www.bonehealthandosteoporosis.org.
Summary
The osteoporosis treatment gap is truly a public health crisis, putting patients at risk for fragility fractures that cause avoidable suffering, disability, dependence, and premature death and cost millions in healthcare expenditures. To close this gap in care, we need to engage physicians, governmental entities, and public health organizations in efforts to improve access and insurance coverage for key fracture prevention services. Osteoporosis detection, diagnosis, and treatment must become routine components of clinical practice. Healthcare providers of all types can lend their support by raising awareness of fracture prevention and bone preservation interventions and lifestyle modifications among patients, caregivers, and fellow health professionals.
We have the tools at our disposal. Proven diagnostic technologies and bone-sparing therapies are widely available at low cost. Pharmacologic agents that build bone and/or decrease bone breakdown dramatically reduce fracture incidence. Non-pharmacologic interventions preserve bone tissue, build muscle, and help prevent falls and fall-related fractures. However, these and other effective strategies are underutilized at every stage of healthcare delivery from inpatient to at-home and continuing care.
However effective, no single intervention or modality is adequate to preserve bone and prevent fractures in vulnerable patients. Collaborative approaches piloted in FLS programs are multifactorial and wholistic. They start with the recognition that a fracture in an adult is a clinical sign of osteoporosis that warrants further investigation to identify and mitigate underlying conditions that contribute to bone loss and fractures. Multifaceted patient care must be coordinated to ensure implementation of the full range of pharmacologic, dietary, fall prevention, physical therapy, and exercise recommendations.
As our population ages, preservation of skeletal health becomes more important every year. By applying recommended fracture risk assessment, pharmacologic treatment, risk reduction counseling, and long-term monitoring, clinicians across the healthcare spectrum who care for adults can contribute to extending the healthy independent lives of their patients.
Glossary
Abaloparatide (Tymlos®): An anabolic therapy approved for the treatment of osteoporosis. The pivotal study indicates that abaloparatide, compared with placebo, reduced the risk of new vertebral fractures by 86% and non-vertebral fractures by 43% after 18 months of therapy in patients with osteoporosis.
Alendronate (Fosamax®, Binosto™): A bisphosphonate approved by the US Food and Drug Administration for prevention and treatment of osteoporosis; accumulates and persists in the bone. Studies indicate about a 50% reduction in vertebral and hip fractures in patients with osteoporosis.
Atypical femur fractures (AFF): These are atraumatic or spontaneous fractures characterized by distinct radiographic and clinical features that resemble stress fractures (transverse fracture line, periosteal callus formation at the fracture site, little or no comminution, prodromal pain, and bilaterally, in some instances). These fractures are thought to be associated with long-term use of potent antiresorptive medications and are distinguished from ordinary osteoporotic femoral diaphyseal fractures.
Biochemical markers of bone turnover: Biochemical markers of bone remodeling can be measured in serum and urine. These include the resorption markers serum C-telopeptide (CTX) and urinary N-telopeptide (NTX) and the formation markers serum bone specific alkaline phosphatase (BALP), osteocalcin (OC), and amino-terminal propeptide of type 1 procollagen (P1NP). Elevated markers of bone turnover may predict bone loss, while declines in these markers after 3–6 months of treatment may suggest fracture risk reduction.
Bone Health and Osteoporosis Foundation (BHOF): In October 2021, the National Osteoporosis Foundation (NOF) changed its name to the Bone Health and Osteoporosis Foundation (BHOF) to reflect the Foundation’s dual focus on preventing osteoporosis and fracture in addition to osteoporosis diagnosis and treatment across the lifespan.
Bone mineral density (BMD): A risk factor for fractures. By DXA, BMD is expressed as the amount of mineralized tissue in the area scanned (g/cm2); with QCT, BMD is expressed as the amount per volume of bone (mg/cm3). Hip BMD by DXA is considered the best predictor of hip fracture; it appears to predict other types of fractures as well as measurements made at other skeletal sites. Lumbar spine BMD may be preferable to assess changes early in menopause and after bilateral ovariectomy and may be better than hip BMD in predicting risk of spine fractures especially in women in their 50s and 60s.
Calcitonin (Miacalcin® or Fortical®): A polypeptide hormone that inhibits the resorptive activity of osteoclasts. Second-line antifracture treatment (less effective than alternatives). Nasal spray and injection available. Documented to significantly reduce acute pain of recent vertebral crush fractures. Short-term use advised due to cancer risk.
Calcium: A mineral that plays an essential role in development and maintenance of a healthy skeleton. The vast majority of the body’s calcium is stored in bone. If intake is inadequate, calcium is mobilized from the skeleton to maintain a normal blood calcium level. In addition to being a substrate for bone mineralization, calcium is an inhibitor of bone remodeling through suppression of circulating parathyroid hormone.
Cancellous bone: The spongy, or trabecular, tissue in the middle of bone (e.g., vertebrae) and at the end of the long bones. Also called trabecular bone.
Cortical bone: The dense outer layer of bone.
Denosumab: A fully human monoclonal antibody to RANK-ligand (RANKL) approved by the FDA for the treatment of osteoporosis in postmenopausal women at high-risk of fracture and other indications. In the pivotal study, denosumab reduces the incidence of vertebral fractures by about 68%, hip fractures by about 40%, and non-vertebral fractures by about 20% over 3 years.
Dual-energy X-ray absorptiometry (DXA): A diagnostic test used to assess bone density at various skeletal sites using radiation exposure about one-tenth that of a standard chest X-ray. Central DXA (lumbar spine, hip) is the preferred measurement for definitive diagnosis of osteoporosis and for monitoring the effects of therapy.
Estrogen: One of a group of steroid hormones that control female sexual development; directly affects bone mass through estrogen receptors in bone, reducing bone turnover and bone loss. Indirectly increases intestinal calcium absorption and renal calcium conservation and, therefore, improves calcium balance. See hormone therapy.
Estrogen agonists/antagonists: A group of compounds that act on a subset of estrogen receptors in the body, also known as selective estrogen receptor modulators (SERMs). Examples are the pharmaceutical agents raloxifene and bazedoxifene.
Exercise: An intervention long associated with healthy bones, despite limited evidence for significant beneficial effect on BMD or fracture risk reductions. Studies evaluating exercise are ongoing; however, enough is known about the positive effect of exercise on fall prevention to support its inclusion in a comprehensive fracture prevention program.
Food and Drug Administration (FDA): The US FDA is responsible for protecting the public health by assuring the safety, effectiveness, quality, and security of human and veterinary drugs, vaccines and other biological products, and medical devices. The FDA is responsible for the safety and security of most of our nation’s food supply, all cosmetics, dietary supplements, and products that give off radiation.
Fracture: Breakage of a bone, either complete or incomplete whether from trauma, repetitive stress, or bone insufficiency. Osteoporosis can contribute to any fracture at any skeletal site, but overwhelmingly affects sites that predominate in trabecular bone: femoral neck, total hip, spine, and forearm. Fractures in cortical bone dense sites are less likely to be attributed to osteoporosis, such as fingers, toes, skull, and face. Vertebral compression fractures are the most common type of osteoporotic fracture.
Fracture liaison service (FLS): A coordinated care system headed by an FLS coordinator (a nurse practitioner, physician’s assistant, nurse or other health professional) who ensures that individuals who suffer a fracture receive appropriate diagnosis, treatment and support.
FRAX®: The World Health Organization Fracture Risk Assessment Tool. https://www.bonehealthandosteoporosis.org and https://www.sheffield.ac.uk/FRAX.
Hormone/estrogen therapy (HT/ET) (HT—Activella®, Femhrt®, Premphase®, Prempro®; ET—Climara®, Estrace®, Estraderm®, Estratab®, Ogen®, Ortho-Est®, Premarin®, Vivelle®): HT is a general term for all types of estrogen replacement therapy when given along with progestin, cyclically or continuously. HT is generally prescribed for women after natural menopause or bilateral ovariectomy with progestin required to protect the uterus from unopposed estrogen. ET is prescribed for postmenopausal women who have had a hysterectomy. Studies indicate that 5 years of HT may decrease vertebral fractures by 35 to 50% and non-vertebral fractures by about 25%. Ten or more years of use might be expected to decrease the rate of all fractures by about 50%.
Ibandronate (Boniva®): A bisphosphonate approved by the FDA for the prevention and treatment of postmenopausal osteoporosis. Ibandronate reduces incidence of vertebral fractures by about 50% over 3 years. Ibandronate in the large RCTs did not reduce hip or non-spine fractures.
Least significant change (LSC): A measure utilized as part of DXA precision assessment that helps to determine if a BMD change can be ascribed to treatment effects or is due to measurement error.
Low bone mass (osteopenia): The designation for bone density between 1.0 and 2.5 standard deviations below the mean BMD of a young adult reference population (T-score between − 1.0 and − 2.5).
Modeling: The term for skeletal processes that involves shaping the bone during growth and replace damaged bone with new bone throughout the lifecycle. Modeling occurs on bone surfaces without prior bone resorption.
Non-vertebral fractures: Fractures of the hip, wrist, forearm, leg, ankle, foot, and other sites.
Normal bone mass: The designation for bone density within 1 standard deviation of the mean BMD of a young adult reference population (T-score at − 1.0 and above).
Osteopenia: See low bone mass.
Osteoporosis: A chronic, progressive disease characterized by low bone mass, microarchitectural deterioration of bone tissue, decreased bone strength, bone fragility, and a consequent increase in fracture risk; BMD 2.5 or more standard deviations below the mean BMD of a young adult reference population (T-score at or below − 2.5).
Peak bone mass: The maximum bone mass accumulated during young adult life (late teens to early 20s).
Peripheral DXA: A DXA test used to assess bone density in the forearm, finger, and heel.
Physiatrist: A physician who specializes in medicine and rehabilitation, or physiatry.
Previous fracture: A risk factor for future fractures, defined here as a history of a previous fracture after age 40 years.
PTH (1-34), teriparatide, (Forteo®): An anabolic therapy approved for the treatment of osteoporosis. The pivotal study indicates a 65% reduction in vertebral fractures and a 40 to 50% reduction in non-vertebral fractures after 18 months of therapy in patients with osteoporosis.
Quantitative computed tomography (QCT): A diagnostic test used to assess volumetric bone density; reflects three-dimensional BMD. Usually used to assess the lumbar spine but has been adapted for other skeletal sites (e.g., hip). It is also possible to measure trabecular and cortical bone density in the periphery by peripheral QCT (pQCT) or high-resolution pQCT (HRpQCT).
Quantitative ultrasound densitometry (QUS): A diagnostic test used to assess bone density at the calcaneus or tibia. Ultrasound measurements correlate only modestly with other assessments of bone density in the same patient, yet some prospective studies indicate that ultrasound may predict fractures as effectively as other measures of bone density.
Raloxifene (Evista®): An estrogen agonist/antagonist (or selective estrogen receptor modulator) approved by the FDA for prevention and treatment of osteoporosis. It lowers the risk of vertebral fracture by about 30% in patients with and about 55% in patients without prior vertebral fracture. Raloxifene is approved for the prevention of breast cancer.
RANKL: Receptor activator of nuclear factor kappa-B (RANK) ligand (RANKL)
Remodeling: Also called bone turnover, remodeling is the process by which the skeleton repairs damage and maintains serum calcium levels through the ongoing lifelong dual processes of bone resorption (breakdown) and formation.
Resorption: The breakdown and removal of bone tissue during bone remodeling.
Risedronate (Actonel®, Atelvia®): A bisphosphonate approved by the FDA for prevention and treatment of osteoporosis. It lowers the risk of vertebral fracture by about 41–49% and non-vertebral fractures by about 36%.
Risk factors: For osteoporotic fractures, risk factors include low BMD, parental history of hip fracture, low body weight, previous fracture, smoking, excess alcohol intake, glucocorticoid use, secondary causes of osteoporosis (e.g., rheumatoid arthritis), and history of falls. These readily accessible and commonplace factors are associated with the risk of hip fracture and, in most cases, with that of vertebral and other types of fracture as well.
Romosozumab (Evenity™): The FDA-approved bone anabolic agent, romosozumab is a fully human monoclonal antibody to sclerostin that both increases BMD and decreases fracture incidence in women with postmenopausal osteoporosis. Reported 73% (95% CI 53–84%) relative risk reduction in morphometric vertebral fracture after 12 months.
Secondary causes of osteoporosis: Osteoporosis that is drug-induced or caused by many disorders such as malabsorption, hyperthyroidism, renal disease, and chronic obstructive pulmonary disease.
Secondary fracture prevention: While primary fracture prevention comprises measures to promote and maintain BMD above − 2.50 so as to prevent an initial osteoporosis-related fracture, secondary fracture prevention is antifracture treatment after a patient has had an osteoporosis-related fracture, to prevent second and subsequent fractures.
Standard deviation (SD): A statistical measure of variance in a population.
T-score: In describing BMD, the number of standard deviations above or below the mean BMD of a young adult reference population.
Teriparatide: See PTH (1-34), teriparatide, (Forteo®).
Vitamin D: A group of fat-soluble sterol compounds that includes ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). These compounds are ingested from plant and animal sources; cholecalciferol is also formed in skin on exposure to ultraviolet light. When activated in the liver and then the kidney, vitamin D promotes calcium absorption. Vitamin D replacement increases muscle strength in patients with severe vitamin D deficiency. A 25(OH) D level of approximately 30 ng/mL (75 nmol/L) is considered by many bone health experts to be optimal.
Zoledronic acid (Reclast®): A bisphosphonate approved by the FDA for treatment of postmenopausal osteoporosis and to reduce risk of subsequent fracture in those with prior hip fracture. It lowers risk of vertebral fractures by about 70%, hip fractures by about 41% and non-vertebral fractures by about 25%.
Z-score: In describing BMD, the number of standard deviations above or below the mean BMD for persons of the same age, sex, and ethnicity.
Subject Specialist Contributors
Kathryn E. Ackerman, MD, MPH, FACSM; Douglas Bauer, MD; Theresa Chiaia, PT, DPT; Polly deMille, RN, MA, RCEP, CSCS, USAT; Thomas F. Koinis, MD; Wendy Katzman, PT, DPTSc (Dsc), OCS; Rick Pope, MPAS, PA-C, DFAAPA, CPAAPA; Heidi Skolnik, MS, CDN, FACSM
Abbreviations
- AACE
American Association of Clinical Endocrinologists
- AFF
Atypical femur fractures
- ASBMR
American Society for Bone and Mineral Research
- BASP
Bone-specific alkaline phosphatase
- BCT
Biomechanical computed tomography analysis
- BHOF
Bone Health and Osteoporosis Foundation
- BMD
Bone mineral density
- BTMs
Bone turnover markers
- CTX
Carboxy-terminal cross-linked telopeptides of type 1 collagen
- CV
Cardiovascular
- DXA
Dual X-ray absorptiometry
- ET/HT
Estrogen/hormone therapy
- FDA
US Food and Drug Administration
- FLS
Fracture liaison service
- FNIH
Foundation for the National Institutes of Health
- FRAX®
Fracture Risk Assessment Tool
- HR-pQCT
High-resolution peripheral quantitative computed tomography
- IOM
Institute of Medicine
- ISCD
International Society for Clinical Densitometry
- LSC
Least significant change
- MRI
Magnetic resonance imaging
- NBHA
National Bone Health Alliance
- NOF
National Osteoporosis Foundation
- NTX
Amino-terminal cross-linked telopeptides of type 1 collagen
- OC
Osteocalcin
- ONJ
Osteonecrosis of the jaw
- P1NP
Amino-terminal propeptide of type 1 procollagen
- pQCT
Peripheral quantitative computed tomography
- PTH
Parathyroid hormone
- PTHrP
Analog of parathyroid hormone-related peptide
- QCT
Quantitative computed tomography
- QUS
Quantitative ultrasound
- RANKL
Receptor activator of nuclear factor κB ligand
- RCT
Randomized controlled trials
- TBS
Trabecular bone score
- USPSTF
US Preventive Services Task Force
- VFA
Vertebral fracture assessment
- WHI
Women’s Health Initiative
Funding
Funding for the development of this document was provided by the Bone Health and Osteoporosis Foundation.
Declarations
Conflict of interest
2020 Clinician’s Guide Update Committee: Meryl S. LeBoff, MD; NIA R01 AG071611; NIAMS R01 AR070854; NIAMS R01 AR059775; Amgen; Susan L. Greenspan, MD, no disclosures; Karl Insogna, MD, no disclosures; E. Michael Lewiecki, MD, Radius, Amgen, Mereo, Bindex, Alexion; Kenneth G. Saag, MD, no disclosures; Andrea Singer, MD, Amgen, Radius Health, UCB; Ethel S. Siris, MD, no disclosures. Subject Specialist Contributors: Kathryn E. Ackerman, MD, MPH, FACSM; Douglas C Bauer, MD, no disclosures; Theresa Chiaia PT, DPT no disclosures; Polly de Mille RN, MA, RCEP, CSCS, USAT, no disclosures; Thomas F. Koinis, MD, no disclosures; Wendy Katzman, PT, DPTSc (DSc), OCS, no disclosures; Rick Pope MPAS, PA-C, DFAAPA, CPAAPA, no disclosures; Heidi Skolnik, MS, CDN, FACSM, American Dairy Association, Sport Advisory Panel. Bone Health and Osteoporosis Foundation Staff: Claire Gill no disclosures, Ami R. Patel no disclosures, Kelly A. Trippe no disclosures.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
7/28/2022
A Correction to this paper has been published: 10.1007/s00198-022-06479-8
Contributor Information
M. S. LeBoff, Email: mleboff@bwh.harvard.edu
S. L. Greenspan, Email: greenspn@pitt.edu
K. L. Insogna, Email: karl.insogna@yale.edu
E. M. Lewiecki, Email: mlewiecki@gmail.com
K. G. Saag, Email: ksaag@uab.edu
A. J. Singer, Email: singeraf@gunet.georgetown.edu
E. S. Siris, Email: es27@cumc.columbia.edu
References
- 1.Holick MF, Binkley NC, Bischoff-Ferrari HA, Endocrine Society et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 2.Ross AC, Manson JE, Abrams SA, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–58. doi: 10.1210/jc.2010-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dudenkov DV, Yawn BP, Oberhelman SS, et al. Changing incidence of serum 25-hydroxyvitamin d values above 50 ng/mL: a 10-year population-based study. Mayo Clin Proc. 2015;90(5):577–586. doi: 10.1016/j.mayocp.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leslie WD, Schousboe JT, Morin SN, et al. Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int Jun. 2020;31(6):1059–1067. doi: 10.1007/s00198-019-05274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mackey DC, Lui LY, Cawthon PM, Study of Osteoporotic Fractures (SOF) and Osteoporotic Fractures in Men Study (MrOS) Research Groups et al. High-trauma fractures and low bone mineral density in older women and men. JAMA. 2007;298(20):2381–2388. doi: 10.1001/jama.298.20.2381. [DOI] [PubMed] [Google Scholar]
- 6.Yang J, Cosman F, Stone PW, Li M, Nieves JW. Vertebral fracture assessment (VFA) for osteoporosis screening in US postmenopausal women: is it cost-effective? Osteoporos Int. Dec. 2020;31(12):2321–2335. doi: 10.1007/s00198-020-05588-6. [DOI] [PubMed] [Google Scholar]
- 7.Hillier TA, Lui LY, Kado DM, et al. Height loss in older women: risk of hip fracture and mortality independent of vertebral fractures. J Bone Miner Res. 2012;27(1):153–159. doi: 10.1002/jbmr.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bilezikian JP, Brandi ML, Eastell R. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3561–3569. doi: 10.1210/jc.2014-1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glowacki J, Hurwitz S, Thornhill TS, Kelly M, LeBoff MS. Osteoporosis and vitamin-D deficiency among postmenopausal women with osteoarthritis undergoing total hip arthroplasty. J Bone Joint Surg Am. 2003;85(12):2371–2377. doi: 10.2106/00004623-200312000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Bernatz JT, Brooks AE, Squire MW, Illgen RI, 2nd, Binkley NC, Anderson PA. Osteoporosis is common and undertreated prior to total joint arthroplasty. J Arthroplasty. 2019;34(7):1347–1353. doi: 10.1016/j.arth.2019.03.044. [DOI] [PubMed] [Google Scholar]
- 11.Anderson PA, Morgan SL, Krueger D, et al. Use of bone health evaluation in orthopedic surgery: 2019 ISCD Official Position. J Clin Densitom. 2019;22(4):517–543. doi: 10.1016/j.jocd.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Bynum JPW, Bell JE, Cantu RV, et al. Second fractures among older adults in the year following hip, shoulder, or wrist fracture. Osteoporosis Int. 2016;27(7):2207–2215. doi: 10.1007/s00198-016-3542-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25(5):1439–1443. doi: 10.1007/s00198-014-2655-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adler RA, El-Hajj Fuleihan G, Bauer DC, Camacho PM, et al. Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016;31(1):16–35. doi: 10.1002/jbmr.2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Osteoporosis Foundation (2014) Clinician’s Guide to Prevention and Treatment of Osteoporosis. National Osteoporosis Foundation, Washington, DC [DOI] [PMC free article] [PubMed]
- 16.Cauley JA, Lui LY, Ensrud KE, et al. Bone mineral density and the risk of incident nonspinal fractures in black and white women. JAMA. 2005;293(17):2102–2108. doi: 10.1001/jama.293.17.2102. [DOI] [PubMed] [Google Scholar]
- 17.Liu XS, Walker MD, McMahon DJ, Udesky J, Liu G, Bilezikian JP, Guo XE. Better skeletal microstructure confers greater mechanical advantages in Chinese-American women versus white women. J Bone Miner Res. 2011;26(8):1783–1792. doi: 10.1002/jbmr.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shin MH, Zmuda JM, Barrett-Connor E, Osteoporotic Fractures in Men (MrOS) Research Group et al. Race/ethnic differences in associations between bone mineral density and fracture history in older men. Osteoporos Int. 2014;25(3):837–845. doi: 10.1007/s00198-013-2503-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cauley JA, Chalhoub D, Kassem AM, Fuleihan G-H. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10(6):338–351. doi: 10.1038/nrendo.2014.51. [DOI] [PubMed] [Google Scholar]
- 20.Nelson DA, Beck TJ, Wu G, et al. Ethnic differences in femur geometry in the women’s health initiative observational study. Osteoporos Int. 2011;22(5):1377–1388. doi: 10.1007/s00198-010-1349-4. [DOI] [PubMed] [Google Scholar]
- 21.Wright NC, Looker A, Saag K, et al. The recent prevalence of osteoporosis and low bone mass based on bone mineral density at the femoral neck or lumbar spine in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–2526. doi: 10.1002/jbmr.2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Viswanathan M, Reddy S, Berkman N, et al. Screening to prevent osteoporotic fractures: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;319(24):2532–2551. doi: 10.1001/jama.2018.6537. [DOI] [PubMed] [Google Scholar]
- 23.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 24.Benjamin EJ, Virani SS, Callaway CW, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 25.American Cancer Society. Surveillance research (2019) Available at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/estimated-new-cases-for-the-four-major-cancers-by-sex-and-age-group-2019.pdf Accessed January 2019.
- 26.Lewiecki EM, Ortendahl JD, Vanderpuye-Orgle J, et al. Healthcare policy changes in osteoporosis can improve outcomes and reduce costs in the United States. JBMR Plus. 2019;3(9):e10192. doi: 10.1002/jbm4.10192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Office of the Surgeon General (US) (2004) Bone health and osteoporosis: a report of the Surgeon General. Office of the Surgeon General (US), Rockville [PubMed]
- 28.Roerholt C, Eiken P, Abrahamsen B. Initiation of anti-osteoporotic therapy in patients with recent fractures: a nationwide analysis of prescription rates and persistence. Osteoporos Int. 2009;20(2):299–307. doi: 10.1007/s00198-008-0651-x. [DOI] [PubMed] [Google Scholar]
- 29.Liu SK, Munson JC, Bell JE, et al. Quality of osteoporosis care of older Medicare recipients with fragility fractures: 2006 to 2010. J Am Geriatr Soc. 2013;61(11):1855–1862. doi: 10.1111/jgs.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim SC, Kim MS, Sanfélix-Gimeno G, et al. Use of osteoporosis medications after hospitalization for hip fracture: a cross-national study. Am J Med. 2015;128(5):519–26.e1. doi: 10.1016/j.amjmed.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lewiecki EM, Wright NC, Siris E, et al. Hip fracture trends in the United States, 2002 to 2015. Osteoporos Int. 2018;29(3):717–722. doi: 10.1007/s00198-017-4345-0. [DOI] [PubMed] [Google Scholar]
- 32.Khosla S, Shane E. A crisis in the treatment of osteoporosis. J Bone Miner Res. 2016;31(8):1485–1487. doi: 10.1002/jbmr.2888. [DOI] [PubMed] [Google Scholar]
- 33.Roux C, Briot K. Osteoporosis in 2017: addressing the crisis in the treatment of osteoporosis. Nat Rev Rheumatol. 2018;14(2):67–68. doi: 10.1038/nrrheum.2017.218. [DOI] [PubMed] [Google Scholar]
- 34.Svedbom A, Borgstöm F, Hernlund E, et al. Quality of life for up to 18 months after low-energy hip, vertebral, and distal forearm fractures-results from the ICUROS. Osteoporos Int. 2018;29(3):557–566. doi: 10.1007/s00198-017-4317-4. [DOI] [PubMed] [Google Scholar]
- 35.Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20(10):1633–1650. doi: 10.1007/s00198-009-0920-3. [DOI] [PubMed] [Google Scholar]
- 36.Colón-Emeric C, Kuchibhatla M, Pieper C, et al. The contribution of hip fracture to risk of subsequent fractures: data from eight longitudinal studies. Osteoporos Int. 2003;11:879–883. doi: 10.1007/s00198-003-1460-x. [DOI] [PubMed] [Google Scholar]
- 37.Lewiecki EM, Laster AJ. Clinical review: clinical applications of vertebral fracture assessment by dual-energy x-ray absorptiometry. J Clin Endo Metab. 2006;91(11):4215–4222. doi: 10.1210/jc.2006-1178. [DOI] [PubMed] [Google Scholar]
- 38.Johansson L, Svensson HK, Karlsson J, et al. Decreased physical health-related quality of life-a persisting state for older women with clinical vertebral fracture. Osteoporos Int. 2019;30(10):1961–1971. doi: 10.1007/s00198-019-05044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Crandall CJ, Hovey KM, Cauley JA, Andrews CA, Curtis JR, Wactawski-Wende J, Wright NC, Li W, LeBoff MS. Wrist fracture and risk of subsequent fracture: findings from the Women’s Health Initiative Study. J Bone Miner Res. 2015;30(11):2086–2095. doi: 10.1002/jbmr.2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wright NC, Hooker ER, Nielson CM, et al. The epidemiology of wrist fractures in older men: the Osteoporotic Fractures in Men (MrOS) study. Osteoporos Int. 2018;29(4):859–870. doi: 10.1007/s00198-017-4349-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crandall CJ, Hovey KM, Andrews CA, Cauley JA, Manson JE, Wactawski-Wende J, Wright NC, Li W, Beavers K, Curtis JR, LeBoff MS. Bone mineral density predictor of subsequent wrist fractures: findings from the Women’s Health Initiative Study. J Clin Endo Metab. 2015;100(11):4315–4324. doi: 10.1210/jc.2015-2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rozental TD, Deschamps LN, Taylor A, et al. Premenopausal women with a distal radial fracture have deteriorated trabecular bone density and morphology compared with controls without a fracture. J Bone Joint Surg Am. 2013;95(7):633–642. doi: 10.2106/JBJS.L.00588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harper CM, Fitzpatrick SK, Zurakowski D, Rozental TD. Distal radial fractures in older men. A missed opportunity? J Bone Joint Surg Am. 2014;96(21):1820–1827. doi: 10.2106/JBJS.M.01497. [DOI] [PubMed] [Google Scholar]
- 44.Rozental TD, Makhni EC, Day CS, Bouxsein ML. Improving evaluation and treatment for osteoporosis following distal radial fractures. A prospective randomized intervention. J Bone Joint Surg Am. 2008;90(5):953–961. doi: 10.2106/JBJS.G.01121. [DOI] [PubMed] [Google Scholar]
- 45.Greenspan SL, Singer A, Vujevich K, et al. Implementing a fracture liaison service open model of care utilizing a cloud-based tool. Osteoporos Int. 2018;29(4):953–960. doi: 10.1007/s00198-017-4371-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Naranje SM, Erali RA, Warner WC, Jr, Sawyer JR, Kelly DM. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36(4):e45–e48. doi: 10.1097/BPO.0000000000000595. [DOI] [PubMed] [Google Scholar]
- 47.Finkelstein JS, Brockwell SE, Mehta V, et al. Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J Clin Endocrinol Metab. 2008;93(3):861–868. doi: 10.1210/jc.2007-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rizzoli R, Bianchi ML, Garabédian M, McKay HA, Moreno LA. Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone. 2010;46(2):294–305. doi: 10.1016/j.bone.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 49.McClung MR. Sclerostin antibodies in osteoporosis: latest evidence and therapeutic potential. Ther Adv Musculoskelet Dis. 2017;9(10):263–270. doi: 10.1177/1759720X17726744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dempster DW, Shane E, Horbert W, Lindsay R. A simple method for correlative light and scanning electron microscopy of human iliac crest bone biopsies: qualitative observations in normal and osteoporotic subjects. J Bone Miner Res. 1986;1(1):15–21. doi: 10.1002/jbmr.5650010105. [DOI] [PubMed] [Google Scholar]
- 51.Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2020 update. Endocr Pract. 2020;26(1):1–46. doi: 10.4158/GL-2020-0524SUPPL. [DOI] [PubMed] [Google Scholar]
- 52.Balasubramanian A, Zhang J, Chen L, et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos Int. 2019;30(1):79–92. doi: 10.1007/s00198-018-4732-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sheer RL, Barron RL, Sudharshan L, Pasquale MK. Validated prediction of imminent risk of fracture for older adults. Am J Manag Care. 2020;26(3):e91–e97. doi: 10.37765/ajmc.2020.42641. [DOI] [PubMed] [Google Scholar]
- 54.National Osteoporosis Foundation (2003) Health professional’s guide to rehabilitation of the patient with osteoporosis. National Osteoporosis Foundation, Washington, DC [DOI] [PubMed]
- 55.American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49:664–672. doi: 10.1046/j.1532-5415.2001.49115.x. [DOI] [PubMed] [Google Scholar]
- 56.U.S. Centers for Disease Control and Prevention (CDC) (2019) STEADI (Stopping Elderly Accidents, Deaths & Injuries) tool kit for health care providers. Available at: https://www.cdc.gov/steadi/index.html/. Accessed November 2019
- 57.van den Bergh JP, van Geel TA, Geusens PP. Osteoporosis, frailty and fracture: implications for case finding and therapy. Nat Rev Rheumatol. 2012;8(3):163–172. doi: 10.1038/nrrheum.2011.217. [DOI] [PubMed] [Google Scholar]
- 58.Watts NB, Adler RA, Bilezikian JP, Endocrine Society et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(6):1802–1822. doi: 10.1210/jc.2011-3045. [DOI] [PubMed] [Google Scholar]
- 59.International Society for Clinical Densitometry (2019) ISCD OFFICIAL POSITIONS – ADULT. Available at: https://iscd.org/learn/official-positions/adult-positions/ Accessed October 2019
- 60.Kanis JA, Melton LJ, 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9(8):1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 61.Bouxsein ML, Eastell R, Lui LY, FNIH bone quality project et al. Change in bone density and reduction in fracture risk: a meta-regression of published trials. J Bone Miner Res. 2019;34(4):632–642. doi: 10.1002/jbmr.3641. [DOI] [PubMed] [Google Scholar]
- 62.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312(7041):1254–1259. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tenne M, McGuigan F, Besjakov J, Gerdhem P, Åkesson K. Degenerative changes at the lumbar spine--implications for bone mineral density measurement in elderly women. Osteoporos Int. 2013;24(4):1419–1428. doi: 10.1007/s00198-012-2048-0. [DOI] [PubMed] [Google Scholar]
- 64.Okano I, Salzmann SN, Jones C, et al. The impact of degenerative disc disease on regional volumetric bone mineral density (vBMD) measured by quantitative computed tomography. Spine J. 2020;20(2):181–190. doi: 10.1016/j.spinee.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 65.Curry SJ, Krist AH, Owens DK, US Preventive Services Task Force et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(24):2521–2531. doi: 10.1001/jama.2018.7498. [DOI] [PubMed] [Google Scholar]
- 66.Ross PD, Davis JW, Epstein RS, Wasnich RD. Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med. 1991;114(11):919–923. doi: 10.7326/0003-4819-114-11-919. [DOI] [PubMed] [Google Scholar]
- 67.El Maghraoui A, Rezqi A, Mounach A, Achemlal L, Bezza A, Ghozlani I. Systematic vertebral fracture assessment in asymptomatic postmenopausal women. Bone. 2013;52(1):176–180. doi: 10.1016/j.bone.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 68.Lenchik L, Rogers LF, Delmas PD, Genant HK. Diagnosis of osteoporotic vertebral fractures: importance of recognition and description by radiologists. Am J Roentgenology. 2004;183(4):949–958. doi: 10.2214/ajr.183.4.1830949. [DOI] [PubMed] [Google Scholar]
- 69.Buckley L, Guyatt G, Fink HA, et al. 2017 American College of Rheumatology Guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheumatol. 2017;69(8):1521–1537. doi: 10.1002/art.40137. [DOI] [PubMed] [Google Scholar]
- 70.Schousboe JT, Ensrud KE, Nyman JA, Kane RL, Melton LJ., 3rd Potential cost-effective use of spine radiographs to detect vertebral deformity and select osteopenic post-menopausal women for amino-bisphosphonate therapy. Osteoporos Int. 2005;16(12):1883–1893. doi: 10.1007/s00198-005-1956-7. [DOI] [PubMed] [Google Scholar]
- 71.Kanis, J.A., McCloskey, E.V., Johansson, H. et al. (2010) Development and use of FRAX® in osteoporosis. Osteoporos Int 21, 407–413 [DOI] [PubMed]
- 72.Imerci A, Yalın Kılınç C, Aydogan NH, Karalezli MN, Savran A (2017) Fracture Risk Assessment Tool (FRAX®) results calculated with and without bone mineral density values for the evaluation of fracture risk in postmenopausal women with osteopenia. J Clin Densitom 3. pii:S1094-6950(16)30259-1 [DOI] [PubMed]
- 73.Greenspan SL, Perera S, Nace D, et al. FRAX or fiction: determining optimal screening strategies for treatment of osteoporosis in residents in long term care facilities. J Am Geriatr Soc. 2012;60(4):684–690. doi: 10.1111/j.1532-5415.2011.03884.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Roux S, Cabana F, Carrier N, et al. The World Health Organization Fracture Risk Assessment Tool (FRAX) underestimates incident and recurrent fractures in consecutive patients with fragility fractures. J Clin Endocrinol Metab. 2014;99(7):2400–2408. doi: 10.1210/jc.2013-4507. [DOI] [PubMed] [Google Scholar]
- 75.Tosteson ANA, Melton LJ, 3rd, Dawson-Hughes B, et al. National Osteoporosis Foundation Guide Committee. Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int. 2008;19(4):437–447. doi: 10.1007/s00198-007-0550-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dawson-Hughes B, Tosteson ANA, Melton LJ, 3rd, et al. National Osteoporosis Foundation Guide Committee. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the U.S.A. Osteoporos Int. 2008;19(4):449–458. doi: 10.1007/s00198-008-0559-5. [DOI] [PubMed] [Google Scholar]
- 77.Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX® and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19(4):385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Albert SG, Reddy S. Efficacy of drugs for treatment of osteoporosis: a meta-analysis. Endocr Pract. 2017;23(7):841–856. doi: 10.4158/EP161678.RA. [DOI] [PubMed] [Google Scholar]
- 79.Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, McCloskey EV, Advisory Board of the National Osteoporosis Guideline Group A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Archives of Osteoporosis. 2016;11(1):25. doi: 10.1007/s11657-016-0278-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lewiecki EM, Wright NC, Singer AJ. Racial disparities, FRAX, and the care of patients with osteoporosis. Osteoporos Int. 2020;31:2069–2071. doi: 10.1007/s00198-020-05655-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Martineau P, Leslie WD, Johansson H, et al. Clinical utility of using lumbar spine trabecular bone score to adjust fracture probability: the Manitoba BMD Cohort. J Bone Miner Res. 2017;32(7):1568–1574. doi: 10.1002/jbmr.3124. [DOI] [PubMed] [Google Scholar]
- 82.Goldman AL, Donlon CM, Cook NR, Manson JE, Buring JE, Copeland T, Yu CY, LeBoff MS. VITamin D and OmegA-3 TriaL (VITAL) bone health ancillary study: clinical factors associated with trabecular bone score in women and men. Osteoporos Int. 2018;29(11):2505–2515. doi: 10.1007/s00198-018-4633-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Couraud G, Souffir C, Gaigneux E, Kolta S, Roux C, Briot K. Adjusting FRAX® on TBS for identification of subjects at high risk of fractures. Bone. 2017;101:214–218. doi: 10.1016/j.bone.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 84.Shevroja E, Lamy O, Kohlmeier L, Koromani F, Rivadeneira F, Hans D. Use of trabecular bone score (TBS) as a complementary approach to dual-energy x-ray absorptiometry (DXA) for fracture risk assessment in clinical practice. J Clin Densitom. 2017;20(3):334–345. doi: 10.1016/j.jocd.2017.06.019. [DOI] [PubMed] [Google Scholar]
- 85.Leslie WD, Shevroja E, Johansson H, et al. Risk-equivalent T-score adjustment for using lumbar spine trabecular bone score (TBS): the Manitoba BMD registry. Osteoporos Int. 2018;29(3):751–758. doi: 10.1007/s00198-018-4405-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.McCloskey EV, Odén A, Harvey NC, et al. A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res. 2016;31(5):940–948. doi: 10.1002/jbmr.2734. [DOI] [PubMed] [Google Scholar]
- 87.Su Y, Leung L, Hans D, Lamy O, Kwok T. The added value of trabecular bone score to FRAX® to predict major osteoporotic fractures for clinical use in Chinese older people: the Mr. OS and Ms. OS cohort study in Hong Kong. Osteoporos Int. 2017;28(1):111–117. doi: 10.1007/s00198-016-3741-1. [DOI] [PubMed] [Google Scholar]
- 88.Kanis JA, Johansson H, Oden A, McCloskey EV. Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int. 2011;22(3):809–816. doi: 10.1007/s00198-010-1524-7. [DOI] [PubMed] [Google Scholar]
- 89.Lenchik L, Weaver AA, Ward RJ, Boone JM, Boutin RD. Opportunistic screening for osteoporosis using computed tomography: state of the art and argument for paradigm shift. Curr Rheumatol Rep. 2018;20(12):74. doi: 10.1007/s11926-018-0784-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Karjalainen JP, Riekkinen O, Töyräs J, Jurvelin JS, Kröger H. New method for point-of-care osteoporosis screening and diagnostics. Osteoporos Int. 2016;27(3):971–977. doi: 10.1007/s00198-015-3387-4. [DOI] [PubMed] [Google Scholar]
- 91.Keaveny T, Clarke B, Cosman F, et al. Biomechanical computed tomography analysis (BCT) for clinical assessment of osteoporosis. Osteoporos Int. 2020;31:1025–1048. doi: 10.1007/s00198-020-05384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Burch J, Rice S, Yang H, et al. Systematic review of the use of bone turnover markers for monitoring the response to osteoporosis treatment: the secondary prevention of fractures, and primary prevention of fractures in high-risk groups. Health technology assessment (Winchester, England) 2014;18(11):1–206. doi: 10.3310/hta18110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bauer DC, Black DM, Bouxsein ML, Foundation for the National Institutes of Health (FNIH) Bone Quality Project et al. Treatment-related charges in bone turnover and fracture risk reduction in clinical trials of anti-resorptive drugs: a meta-regression. J Bone Miner Res. 2018;33(4):634–642. doi: 10.1002/jbmr.3355. [DOI] [PubMed] [Google Scholar]
- 94.Ross AC, Manson JE, Abrams SA, et al. The 2011 dietary reference intakes for calcium and vitamin d: what dietetics practitioners need to know. J Am Diet Assoc. 2011;111(4):524–527. doi: 10.1016/j.jada.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 95.Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, editors (2011) Dietary reference intakes for calcium and vitamin D. Washington (DC): National Academies Press (US); 2011. Available from: http://www.ncbi.nlm.nih.gov/books/NBK56070/ Accessed August 2018 [PubMed]
- 96.Jackson RD, LaCroix AZ, Gass M, Women’s Health Initiative Investigators et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354(7):669–683. doi: 10.1056/NEJMoa055218. [DOI] [PubMed] [Google Scholar]
- 97.Larsen ER, Mosekilde L, Foldspang A. Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. J Bone Miner Res. 2004;19(3):370–378. doi: 10.1359/JBMR.0301240. [DOI] [PubMed] [Google Scholar]
- 98.Weaver CM, Alexander DD, Boushey CJ, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016;27(1):367–376. doi: 10.1007/s00198-015-3386-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.National Institutes of Health Office of Dietary Supplements. Calcium: fact sheet for health professionals. Available at: https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional Accessed October 2019
- 100.Prentice RL, Pettinger MB, Jackson RD, et al. Health risks and benefits from calcium and vitamin D supplementation: Women’s Health Initiative clinical trial and cohort study. Osteoporos Int. 2013;24(2):567–580. doi: 10.1007/s00198-012-2224-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Reid IR, Bolland MJ. Calcium supplements: bad for the heart? Heart. 2012;98(12):895–896. doi: 10.1136/heartjnl-2012-301904. [DOI] [PubMed] [Google Scholar]
- 102.Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;19:342. doi: 10.1136/bmj.d2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Moyer VA, Preventive Services Task Force US (2013) Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 158(9):691–696. 10.7326/0003-4819-158-9-201305070-00603 [DOI] [PubMed]
- 104.Chung M, Tang AM, Fu Z, Wang DD, Newberry SJ. Calcium intake and cardiovascular disease risk: an updated systematic review and meta-analysis. Ann Intern Med. 2016;165(12):856–866. doi: 10.7326/M16-1165. [DOI] [PubMed] [Google Scholar]
- 105.Manson JE, Cook NR, Lee IM, VITAL research group et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J. 2019;380(1):33–44. doi: 10.1056/NEJMoa1809944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Heaney RP. The vitamin D requirement in health and disease. J Steroid Biochem Mol Biol. 2005;97(1-2):13–19. doi: 10.1016/j.jsbmb.2005.06.020. [DOI] [PubMed] [Google Scholar]
- 107.Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr. 2003;22(2):142–146. doi: 10.1080/07315724.2003.10719287. [DOI] [PubMed] [Google Scholar]
- 108.Vieth R, Holick MF (2018) Chapter 57B - the IOM—Endocrine Society controversy on recommended vitamin d targets: in support of the Endocrine Society position. In: Feldman D, Pike JW, Bouillon R, Vitamin D (eds) In, vol 1, 4th edn. Biochemistry, physiology and diagnostics, Academic Press. Elsevier Inc, London
- 109.Holick MF, Siris ES, Binkley N, et al. Prevalence of vitamin D inadequacy among postmenopausal north American women receiving osteoporosis therapy. J Clin Endocrinol Metab. 2005;90(6):3215–3224. doi: 10.1210/jc.2004-2364. [DOI] [PubMed] [Google Scholar]
- 110.Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, et al. Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med. 2016;176(2):175–183. doi: 10.1001/jamainternmed.2015.7148. [DOI] [PubMed] [Google Scholar]
- 111.Sanders KM, Stuart AL, Williamson EJ, et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303(18):1815–1822. doi: 10.1001/jama.2010.594. [DOI] [PubMed] [Google Scholar]
- 112.LeBoff MS, Hawkes WG, Glowacki J, Yu-Yahiro J, Hurwitz S, Magaziner J. Vitamin D-deficiency and post-fracture changes in lower extremity function and falls in women with hip fractures. Osteoporos Int. 2008;19(9):1283–1290. doi: 10.1007/s00198-008-0582-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988-1994 compared with 2000-2004. Am J Clin Nutr. 2008;88(6):1519–1527. doi: 10.3945/ajcn.2008.26182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–693. doi: 10.1093/ajcn/72.3.690. [DOI] [PubMed] [Google Scholar]
- 115.Chung M, Lee J, Terasawa T, Lau J, Trikalinos TA. Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155(12):827–838. doi: 10.7326/0003-4819-155-12-201112200-00005. [DOI] [PubMed] [Google Scholar]
- 116.Newberry SJ, Chung M, Shekelle PG, et al. Vitamin D and calcium: a systematic review of health outcomes (update) Evid Rep Technol Assess (Full Rep). 2014;217:1–929. doi: 10.23970/AHRQEPCERTA217. [DOI] [PubMed] [Google Scholar]
- 117.Avenell A, Mak JC, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev. 2014;14(4):CD000227. doi: 10.1002/14651858.CD000227.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Reid IR, Bolland MJ, Grey A. Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet. 2014;383(9912):146–155. doi: 10.1016/S0140-6736(13)61647-5. [DOI] [PubMed] [Google Scholar]
- 119.Bolland MJ, Grey A, Avenell A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. 2018;6(11):847–858. doi: 10.1016/S2213-8587(18)30265-1. [DOI] [PubMed] [Google Scholar]
- 120.LeBoff MS, Yue AY, Copeland T, Cook NR, Buring JE, Manson JE. VITAL-Bone Health: rationale and design of two ancillary studies evaluating the effects of vitamin D and/or omega-3 fatty acid supplements on incident fractures and bone health outcomes in the VITamin D and OmegA-3 TriaL (VITAL) Contemp Clin Trials. 2015;41:259–268. doi: 10.1016/j.cct.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.LeBoff MS, Chou SH, Murata EM, Donlon CM, Cook NR, Mora S, Lee IM, Kotler G, Bubes V, Buring JE, Manson JE. Effects of supplemental vitamin D on bone health outcomes in women and men in the VITamin D and OmegA-3 TriaL (VITAL) J Bone Miner Res. 2020;35(5):888–893. doi: 10.1002/jbmr.3958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Donlon CM, LeBoff MS, Chou SH, Cook NR, Copeland T, Buring JE, Bubes V, Kotler G, Manson JE. Baseline characteristics of participants in the VITamin D and OmegA-3 TriaL (VITAL): Effects on bone structure and architecture. Contemp Clin Trials. 2018;67:56–67. doi: 10.1016/j.cct.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.LeBoff MS, Murata EM, Cook NR, Cawthon P, Chou SH, Kotler G, Bubes V, Buring JE, Manson JE. VITamin D and OmegA-3 TriaL (VITAL): effects of vitamin D supplements on risk of falls in the US population. J Clin Endocrinol Metab. 2020;105(9):2929–2938. doi: 10.1210/clinem/dgaa311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gillespie LD, Robertson MC, Gillespie WJ et al (2012) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev (9):CD007146 [DOI] [PMC free article] [PubMed]
- 125.Khaw KT, Stewart AW, Waayer D, et al. Effect of monthly high-dose vitamin D supplementation on falls and non-vertebral fractures: secondary and post-hoc outcomes from the randomised, double-blind, placebo-controlled ViDA trial. Lancet Diabetes Endocrinol. 2017;5(6):438–447. doi: 10.1016/S2213-8587(17)30103-1. [DOI] [PubMed] [Google Scholar]
- 126.Uusi-Rasi K, Patil R, Karinkanta S, et al. Exercise and vitamin D in fall prevention among older women: a randomized clinical trial. JAMA Internl Med. 2015;175(5):703–711. doi: 10.1001/jamainternmed.2015.0225. [DOI] [PubMed] [Google Scholar]
- 127.Ayo-Yusuf OA, Olutola BG. Epidemiological association between osteoporosis and combined smoking and use of snuff among South African women. Niger J Clin Pract. 2014;17:174–177. doi: 10.4103/1119-3077.127542. [DOI] [PubMed] [Google Scholar]
- 128.Waugh EJ, Lam MA, Hawker GA, McGowan J, Papaioannou A, Cheung AM. Risk factors for low bone mass in healthy 40-60 year old women: a systematic review of the literature. Osteoporos Int. 2009;20:1–21. doi: 10.1007/s00198-008-0643-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Benson BW, Shulman JD. Inclusion of tobacco exposure as a predictive factor for decreased bone mineral content. Nicotine Tob Res. 2005;7:719–724. doi: 10.1080/14622200500259119. [DOI] [PubMed] [Google Scholar]
- 130.Krall EA, Dawson-Hughes B. Smoking increases bone loss and decreases intestinal calcium absorption. J Bone Miner Res. 1999;14:215–220. doi: 10.1359/jbmr.1999.14.2.215. [DOI] [PubMed] [Google Scholar]
- 131.Mikosch P. Alcohol and bone. Wiener medizinische Wochenschrift. 2014;164(1-2):15–24. doi: 10.1007/s10354-013-0258-5. [DOI] [PubMed] [Google Scholar]
- 132.Burrows M. Exercise and bone mineral accrual in children and adolescents. J Sports Sci Med. 2007;6(3):305–312. [PMC free article] [PubMed] [Google Scholar]
- 133.Giangregorio LM, Papainoannou A, MacIntyre NJ, et al. Too fit to fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int. 2014;25:821–835. doi: 10.1007/s00198-013-2523-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Senderovich H, Tang H, Belmont S. The role of exercises in osteoporotic fracture prevention and current care gaps. Where are we now? Recent updates. Rambam Maimonides Medical Journal. 2017;8(3):e0032. doi: 10.5041/RMMJ.10308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA. 2017;318(17):1687–1699. doi: 10.1001/jama.2017.15006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Sherrington C, Fairhall N, Wallbank G et al (2019) Exercise for preventing falls in older people living in the community: an abridged Cochrane Systematic Review. Br J Sports Med [DOI] [PubMed]
- 137.Watson SL, Weeks BK, Weis LJ, Horan SA, Beck BR. Heavy resistance training is safe and improves bone, function, and stature in postmenopausal women with low to very low bone mass: novel early findings from the LIFTMOR trial. Osteoporos Int. 2015;26(12):2889–2894. doi: 10.1007/s00198-015-3263-2. [DOI] [PubMed] [Google Scholar]
- 138.Greenway KG, Walkley JW, Rich PA. Impact exercise and bone density in premenopausal women with below average bone density for age. Eur J Appl Physiol. 2015;115(11):2457–2469. doi: 10.1007/s00421-015-3225-6. [DOI] [PubMed] [Google Scholar]
- 139.Katzman WB, Vittinghoff E, Lin F, et al. Targeted spine strengthening exercise and posture training program to reduce hyperkyphosis in older adults: results from the study of hyperkyphosis, exercise, and function (SHEAF) randomized controlled trial. Osteoporos Int. 2017;28(10):2831–2841. doi: 10.1007/s00198-017-4109-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Brault MW (2012) Americans With Disabilities: 2010. Report number P70-131. Available at https://www.census.gov/library/publications/2012/demo/p70-131.html. Accessed 12/20
- 141.Salpakoski A, Törmäkangas T, Edgren J, et al. Walking recovery after a hip fracture: a prospective follow-up study among community-dwelling over 60-year old men and women. Biomed Res Int. 2014;2014:289549. doi: 10.1155/2014/289549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jager TE, Weiss HB, Coben JH, Pepe PE. Traumatic brain injuries evaluated in U.S. emergency departments, 1992–1994. Academic Emergency Medicine. 2000;7(2):134–140. doi: 10.1111/j.1553-2712.2000.tb00515.x. [DOI] [PubMed] [Google Scholar]
- 143.Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA. Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int. 1993;52:192–198. doi: 10.1007/BF00298717. [DOI] [PubMed] [Google Scholar]
- 144.Wainwright SA, Marshall LM, Ensrud KE, Study of Osteoporotic Fractures Research Group et al. Hip fracture in women without osteoporosis. J Clin Endocrinol Metab. 2005;90:2787–2793. doi: 10.1210/jc.2004-1568. [DOI] [PubMed] [Google Scholar]
- 145.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2020) Web–based Injury Statistics Query and Reporting System (WISQARS). Available at: https://www.cdc.gov/injury/wisqars/fatal.html/ Accessed March 15, 2020
- 146.de Souto Barreto P, Rolland Y, Vellas B, Maltais M (2018) Association of long-term exercise training with risk of falls, fractures, hospitalizations, and mortality in older adults: a systematic review and meta-analysis. JAMA Intern Med Published online December 28 2018 [DOI] [PMC free article] [PubMed]
- 147.Granacher U, Gollhofer A, Hortobágyi T, Kressig RW, Muehlbauer T. The importance of trunk muscle strength for balance, functional performance and fall prevention in seniors: a systematic review. Sports Med. 2013;43(7):627–641. doi: 10.1007/s40279-013-0041-1. [DOI] [PubMed] [Google Scholar]
- 148.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(12):2234–2243. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 149.Choi M, Hector M (2012) Effectiveness of intervention programs in preventing falls: a systematic review of recent 10 years and meta-analysis. J Am Med Dir Assoc 13(2):188.e13-21 [DOI] [PubMed]
- 150.Liu-Ambrose T, Davis JC, Best JR, et al. Effect of a home-based exercise program on subsequent falls among community-dwelling high-risk older adults after a fall: a randomized clinical trial. JAMA. 2019;321(21):2092–2100. doi: 10.1001/jama.2019.5795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Sherrington C, Fairhall NJ, Wallbank GK et al (2019) Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 1(1):CD012424 [DOI] [PMC free article] [PubMed]
- 152.LaMonte MJ, Wactawski-Wende J, Larson JC, Mai X, Robbins JA, LeBoff MS, Chen Z, Jackson RD, LaCroix AZ, Ockene JK, Hovey KM. Cauley JA (2019) Association of physical activity and fracture risk among postmenopausal women. JAMA Netw Open. 2019;2(10):e1914084. doi: 10.1001/jamanetworkopen.2019.14084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.NOF (2021) Medication and Treatment Adherence: The Hows and Whys of Osteoporosis Medications. Available at http://www.nof.org/patients/treatment/medicationadherence/
- 154.Saag KG, Emkey R, Schnitzer TJ, et al. Glucocorticoid-Induced Osteoporosis Intervention Study Group. Alendronate for the prevention and treatment of glucocorticoid-induced osteoporosis. NEJM. 1998;339(5):292–299. doi: 10.1056/NEJM199807303390502. [DOI] [PubMed] [Google Scholar]
- 155.Black DM, Cummings SR, Karpf DB et al. Fracture Intervention Trial Research Study Group (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet 348(9041):1535-1541 [DOI] [PubMed]
- 156.Cummings SR, Black DM, Thompson DE, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA. 1998;280(24):2077–2082. doi: 10.1001/jama.280.24.2077. [DOI] [PubMed] [Google Scholar]
- 157.Chesnut CH, 3rd, Skag A, Christiansen C, et al. Oral Ibandronate Osteoporosis Vertebral Fracture Trial in North America and Europe (BONE). Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res. 2004;19(8):1241–1249. doi: 10.1359/JBMR.040325. [DOI] [PubMed] [Google Scholar]
- 158.Eastell R, Devogelaer JP, Peel NF, et al. Prevention of bone loss with risedronate in glucocorticoid-treated rheumatoid arthritis patients. Osteoporos Int. 2000;11(4):331–337. doi: 10.1007/s001980070122. [DOI] [PubMed] [Google Scholar]
- 159.McClung MR, Benhamou CL, Man Z, et al. A novel monthly dosing regimen of risedronate for the treatment of postmenopausal osteoporosis: 2-year data. Calcif Tissue Int. 2013;92(1):59–67. doi: 10.1007/s00223-012-9668-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Barrionuevo PM, Kapoor E, Asi N, et al. Efficacy of pharmacological therapies for the prevention of fractures in postmenopausal women: a network meta-analysis. J Clin Endocrinol Metab. 2019;104(5):1623–1630. doi: 10.1210/jc.2019-00192. [DOI] [PubMed] [Google Scholar]
- 161.Reid IR, Horne AM, Mihov B, et al. Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med. 2018;379(25):2407–2416. doi: 10.1056/NEJMoa1808082. [DOI] [PubMed] [Google Scholar]
- 162.U.S. Food and Drug Administration. (2017) Reclast (zoledronic acid): drug safety communication - new contraindication and updated warning on kidney impairment. [Correction in: Endocr Pract. 2017 23(12):1488. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-new-contraindication-and-updated-warning-kidney-impairment-reclast Accessed August 2018.
- 163.Patel DV, Bolland M, Nisa Z, et al. Incidence of ocular side effects with intravenous zoledronate: secondary analysis of a randomized controlled trial. Osteoporos Int. 2015;26(2):499–503. doi: 10.1007/s00198-014-2872-5. [DOI] [PubMed] [Google Scholar]
- 164.Rossouw JE, Anderson GL, Prentice RL et al. Writing Group for the Women's Health Initiative Investigators (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principle results from the Women’s Health Initiative randomized controlled trial. JAMA 288(3):321-333 [DOI] [PubMed]
- 165.Crandall CJ, Hovey KM, Andrews C, et al. Comparison of clinical outcomes among users of oral and transdermal estrogen therapy in the Women’s Health Initiative Observational Study. Menopause. 2017;24(10):1145–1153. doi: 10.1097/GME.0000000000000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1595–1622. doi: 10.1210/jc.2019-00221. [DOI] [PubMed] [Google Scholar]
- 167.Manson JE, Allison MA, Rossouw JE, Carr JJ et al WHI and WHI-CACS Investigators (2007) Estrogen therapy and coronary-artery calcification. N Engl J Med 356:2591–2602 [DOI] [PubMed]
- 168.The NAMS Hormone Therapy Position Statement Advisory Panel (2017) The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753. doi: 10.1097/GME.0000000000000921. [DOI] [PubMed] [Google Scholar]
- 169.Cobin RH, Goodman NF; AACE Reproductive Endocrinology Scientific Committee (2017) American Association of Clinical Endocrinologists and American College of Endocrinology position statement on menopause-2017 Update. Endocr Pract 23(7):869-80. (Erratum in: Endocr Pract 2017 23[12]:1488) [DOI] [PubMed]
- 170.Cobin RH, Goodman NF: AACE Reproductive Endocrinology Scientific Committee (2017) American Association of Clinical Endocrinologists and American College of Endocrinology position statement on menopause-2017 UPDATE. Endocr Pract 23(7):869-880 [DOI] [PubMed]
- 171.Cauley JA, Norton L, Lippman ME, et al. Continued breast cancer risk reduction in postmenopausal women treated with raloxifene: 4-year results from the MORE trial. Multiple outcomes of raloxifene evaluation. Breast Cancer Res Treat. 2001;65(2):125–134. doi: 10.1023/A:1006478317173. [DOI] [PubMed] [Google Scholar]
- 172.Martino S, Cauley, JA, Barrett-Connor E et al. CORE Investigators (2004) Continuing outcomes relevant to Evista: breast cancer incidence in postmenopausal osteoporotic women in a randomized trial of raloxifene. J Natl Cancer Inst 96(23):1751-1761 [DOI] [PubMed]
- 173.Vogel VG, Costantino JP, Wickerham DL et al. National Surgical Adjuvent Breast and Bowel Project (NSABP) (2006) Effects of tamoxifen vs. raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 295(23):2727-2741 [DOI] [PubMed]
- 174.Barrett-Connor E, Mosca L, Collins P et al. Raloxifene Use for The Heart (RUTH) Trial Investigators (2006) Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med 355(2):125-137 [DOI] [PubMed]
- 175.Gennari L, Merlotti D, De Paola V, Martini G, Nuti R. Bazedoxifene for the prevention of postmenopausal osteoporosis. Ther Clin Risk Manag. 2008;4(6):1229–1242. doi: 10.2147/TCRM.S3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lindsay R, Gallagher JC, Kagan R, Pickar JH, Constantine G. Efficacy of tissue-selective estrogen complex of bazedoxifene/conjugated estrogens for osteoporosis prevention in at-risk postmenopausal women. Fertil Steril. 2009;92(3):1045–1052. doi: 10.1016/j.fertnstert.2009.02.093. [DOI] [PubMed] [Google Scholar]
- 177.Mirkin S, Komm BS, Pan K, Chines AA. Effects of bazedoxifene/conjugated estrogens on endometrial safety and bone in postmenopausal women. Climacteric. 2013;16(3):338–346. doi: 10.3109/13697137.2012.717994. [DOI] [PubMed] [Google Scholar]
- 178.Pinkerton JV, Pickar JH, Racketa J, Mirkin S. Bazedoxifene/conjugated estrogens for menopausal symptom treatment and osteoporosis prevention. Climacteric. 2012;15(5):411–418. doi: 10.3109/13697137.2012.696289. [DOI] [PubMed] [Google Scholar]
- 179.Saag K, Shane E, Boonen S. Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med. 2007;357(20):2028–2039. doi: 10.1056/NEJMoa071408. [DOI] [PubMed] [Google Scholar]
- 180.Neer RM, Arnaud CD, Zanchetta JR, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344(19):1434–1441. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 181.Kendler DL, Marin F, Zerbini CAF, et al. Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet. 2018;391(10117):230–240. doi: 10.1016/S0140-6736(17)32137-2. [DOI] [PubMed] [Google Scholar]
- 182.Eli Lilly and Company. FORTEO — teriparatide injection, solution. Highlights of prescribing information. Revised: 4/2021. Available at: https://uspl.lilly.com/forteo/forteo.html#pi/ Accessed December 2021.
- 183.Miller PD, Hattersley G, Riis BJ et al. ACTIVE Study Investigators (2016) Effect of abaloparatide vs placebo on new vertebral fractures in postmenopausal women with osteoporosis: a randomized clinical trial. JAMA 316(7):722-733 [DOI] [PubMed]
- 184.Cosman F, Miller PD, Williams GC, et al. Eighteen months of treatment with subcutaneous abaloparatide followed by 6 months of treatment with alendronate in postmenopausal women with osteoporosis: results of the ACTIVExtend Trial. Mayo Clin Proc 2017 Feb. 2017;92(2):200–210. doi: 10.1016/j.mayocp.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 185.Cummings SR, San Martin J, McClung MR, FREEDOM Trial et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–765. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]
- 186.Zaheer S, LeBoff M, Lewiecki EM. Denosumab for the treatment of osteoporosis. Expert Opin Drug Metab Toxicol. 2015;11(3):461–470. doi: 10.1517/17425255.2015.1000860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bilezikian JP, Lin CJF, Brown JP, et al. Long-term denosumab treatment restores cortical bone loss and reduces fracture risk at the forearm and humerus: analyses from the FREEDOM Extension cross-over group. Osteoporos Int. 2019;30(9):1855–1864. doi: 10.1007/s00198-019-05020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Papapoulos S, Lippuner K, Roux C, et al. The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM Extension study. Osteoporos Int. 2015;26(12):2773–2783. doi: 10.1007/s00198-015-3234-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Watts NB, Roux C, Modlin JF, et al. Infections in postmenopausal women with osteoporosis treated with denosumab or placebo: coincidence or causal association? Osteoporos Int. 2012;23(1):327–337. doi: 10.1007/s00198-011-1755-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Choi NK, Solomon DH, Tsacogianis TN, Landon JE, Song HJ, Kim SC. Comparative safety and effectiveness of denosumab versus zoledronic acid in patients with osteoporosis: a cohort study. J Bone Miner Res. 2017;32(3):611–617. doi: 10.1002/jbmr.3019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.U.S. Food and Drug Administration. Prolia® (denosumab) highlights of prescribing information. Available online at: https://www.proliahcp.com/?gclid=Cj0KCQjwjOrtBRCcARIsAEq4rW7usz0F7Zns1WRKvbttfSeUe10bri0Y4E6-ziiTVad5SflYzPCAYF0aAqTTEALw_wcB&gclsrc=aw.ds/ Accessed 10/2019.
- 192.Cummings SR, Ferrari S, Eastell R, et al. Vertebral fractures after discontinuation of denosumab: a post hoc analysis of the randomized placebo-controlled FREEDOM Trial and its extension. J Bone Miner Res. 2018;33:190–198. doi: 10.1002/jbmr.3337. [DOI] [PubMed] [Google Scholar]
- 193.Leder BZ, Tsai JN, Uihlein AV, et al. Denosumab and teriparatide transitions in postmenopausal osteoporosis (the DATA-Switch study): extension of a randomised controlled trial. Lancet. 2015;386:1147–1155. doi: 10.1016/S0140-6736(15)61120-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Keaveny TM, Crittenden DB, Bolognese MA, et al. Greater gains in spine and hip strength for romosozumab compared with teriparatide in postmenopausal women with low bone mass. J Bone Miner Res. 2017;32(9):1956–1962. doi: 10.1002/jbmr.3176. [DOI] [PubMed] [Google Scholar]
- 195.Keaveny TM, Crittenden DB, Bolognese MA, et al. Effects of romosozumab compared with teriparatide on bone density and mass at the spine and hip in postmenopausal women with low bone mass. J Bone Miner Res. 2017;32(1):181–187. doi: 10.1002/jbmr.2932. [DOI] [PubMed] [Google Scholar]
- 196.Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375(16):1532–1543. doi: 10.1056/NEJMoa1607948. [DOI] [PubMed] [Google Scholar]
- 197.Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377(15):1417–1427. doi: 10.1056/NEJMoa1708322. [DOI] [PubMed] [Google Scholar]
- 198.Cosman F, Crittenden DB, Ferrari S, et al. Romosozumab FRAME Study: a post hoc analysis of the role of regional background fracture risk on nonvertebral fracture outcome. J Bone Miner Res. 2018;33(8):1407–1416. doi: 10.1002/jbmr.3439. [DOI] [PubMed] [Google Scholar]
- 199.McClung MR, Brown JP, Diez-Perez A, et al. Effects of 24 months of treatment with romosozumab followed by 12 months of denosumab or placebo in postmenopausal women with low bone mineral density: a randomized, double-blind, phase 2, parallel group study. J Bone Miner Res. 2018;33(8):1397–1406. doi: 10.1002/jbmr.3452. [DOI] [PubMed] [Google Scholar]
- 200.Chesnut CH, 3rd, Silverman S, Andriano K, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: the prevent recurrence of osteoporotic fractures study. PROOF Study Group. Am J Med. 2000;109(4):267–276. doi: 10.1016/s0002-9343(00)00490-3. [DOI] [PubMed] [Google Scholar]
- 201.Lyritis GP, Paspati I, Karachalios T, Ioakimidis D, Skarantavos G, Lyritis PG. Pain relief from nasal salmon calcitonin in osteoporotic vertebral crush fractures. A double blind, placebo-controlled clinical study. Acta Orthop Scand Suppl. 1997;275:112–114. doi: 10.1080/17453674.1997.11744761. [DOI] [PubMed] [Google Scholar]
- 202.Lyritis GP, Ioannidis GV, Karachalios T, et al. Analgesic effect of salmon calcitonin suppositories in patients with acute pain due to recent osteoporotic vertebral crush fractures: a prospective double-blind, randomized, placebo-controlled. Clin J Pain. 1999;15(4):284–289. doi: 10.1097/00002508-199912000-00004. [DOI] [PubMed] [Google Scholar]
- 203.Overman RA, Borse M, Gourlay ML. Salmon calcitonin use and associated cancer risk. Ann Pharmacother. 2013;47(12):1675–1684. doi: 10.1177/1060028013509233. [DOI] [PubMed] [Google Scholar]
- 204.Food and Drug Administration. Questions and answers: changes to the indicated population for miacalcin (calcitonin-salmon). Available online at: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/questions-and-answers-changes-indicated-population-miacalcin-calcitonin-salmon Accessed August 2018.
- 205.Khosla S, Burr D, Cauley J et al. American Society for Bone and Mineral Research (2007) Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 22(10):1470-1491 [DOI] [PubMed]
- 206.Woo S, Hellstein J, Kalmar J (2006) Systematic review: Bisphosphonates and osteonecrosis of the jaws. Ann Intern Med 144(10):753–761 [published correction appears in Ann Intern Med. 2006 Aug 1;145(3):235]. [DOI] [PubMed]
- 207.Khan AA, Morrison A, Hanley DA et al. International Task Force on Osteonecrosis of the Jaw (2015) Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res 30(1):3-23 [DOI] [PubMed]
- 208.Boquete-Castro A, Gómez-Moreno G, Calvo-Guirado JL, Aguilar-Salvatierra A, Delgado-Ruiz RA. Denosumab and osteonecrosis of the jaw. A systematic analysis of events reported in clinical trials. Clin Oral Implants Res. 2016;27(3):367–375. doi: 10.1111/clr.12556. [DOI] [PubMed] [Google Scholar]
- 209.Yarom N, Shapiro CL, Peterson DE, et al. Medication-related osteonecrosis of the jaw: MASCC/ISOO/ASCO Clinical Practice Guideline. J Clin Oncol. 2019;37(25):2270–2290. doi: 10.1200/JCO.19.01186. [DOI] [PubMed] [Google Scholar]
- 210.American Dental Association. Osteoporosis medications and medication-related osteonecrosis of the jaw. Oral Health Topics. Available at: https://www.ada.org/en/member-center/oral-health-topics/osteoporosis-medications/ Accessed January 2019.
- 211.Fusco V, Santini D, Campisi G, et al. Medication-related osteonecrosis of the jaw: MASCC/ISOO/ASCO Clinical Practice Guideline. J Clin Oncol. 2019;37(25):2270–2290. doi: 10.1200/JCO.19.01186. [DOI] [PubMed] [Google Scholar]
- 212.Black DM, Abrahamsen B, Bouxsein ML, Einhorn T, Napoli N. Atypical femur fractures - review of epidemiology, relationship to bisphosphonates, prevention. and clinical management. Endocr Rev. 2019;40(2):333–368. doi: 10.1210/er.2018-00001. [DOI] [PubMed] [Google Scholar]
- 213.Starr J, Tay YKD, Shane E. Current understanding of epidemiology, pathophysiology, and management of atypical femur fractures. Curr Osteoporos Rep. 2018;16:519–529. doi: 10.1007/s11914-018-0464-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Shane E, Burr D, Abrahmsen B, et al. American Society for Bone and Mineral Research. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29(1):1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 215.McKenna MJ, McKiernan FE, McGowan B, et al. Identifying incomplete atypical femoral fractures with single-energy absorptiometry: declining prevalence. J Endocr Soc. 2017;1(3):211–220. doi: 10.1210/js.2016-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Greenspan SL, Vujevich K, Britton C, et al. Teriparatide for treatment of patients with bisphosphonate-associated atypical fracture of the femur. Osteoporos Int. 2018;29(2):501–506. doi: 10.1007/s00198-017-4286-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Black DM, Geiger EJ, Eastell R, et al. (2020) Atypical femur fracture risk versus fragility fracture prevention with bisphosphonates N Engl J Med. Aug 20;383(8):743-753 [DOI] [PMC free article] [PubMed]
- 218.Amgen (2020) Extension study to evaluate the long term safety and efficacy of denosumab in the treatment of osteoporosis. (ClinicalTrials.gov Identifier: NCT00523341) Retrieved from https://clinicaltrials.gov/ct2/show/study/NCT00523341
- 219.Bone HG, Wagman RB, Brandi ML, et al. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol. 2017;5(7):513–523. doi: 10.1016/S2213-8587(17)30138-9. [DOI] [PubMed] [Google Scholar]
- 220.van de Laarschot DM, McKenna MJ, Abrahamsen B, et al. Medical management of patients after atypical femur fractures: a systematic review and recommendations from the European Calcified Tissue Society. J Clin Endocrinol Metab. 2020;105(5):1682–1699. doi: 10.1210/clinem/dgz295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Schilcher J, Michaelsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364:1728–1737. doi: 10.1056/NEJMoa1010650. [DOI] [PubMed] [Google Scholar]
- 222.Dell RM, Al A, Greene DF, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res. 2012;27:2544–2550. doi: 10.1002/jbmr.1719. [DOI] [PubMed] [Google Scholar]
- 223.Harris ST, Watts NB, Genant HK, et al. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. JAMA. 1999;282(14):1344–1352. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 224.Reginster J, Minne HW, Sorensen OH, et al. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int. 2000;11(1):83–91. doi: 10.1007/s001980050010. [DOI] [PubMed] [Google Scholar]
- 225.Kanis JA, Barton IP, Johnell O. Risedronate decreases fracture risk in patients selected solely on the basis of prior vertebral fracture. Osteoporos Int. 2005;16(5):475–482. doi: 10.1007/s00198-004-1698-y. [DOI] [PubMed] [Google Scholar]
- 226.Ettinger B, Black DM, Mitlak BH, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 18. 1999;282(7):637–645. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 227.Lyles KW, Colón-Emeric CS, Magaziner JS et al. HORIZON Recurrent Fracture Trial (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Eng J Med 357(18):1799-1809 [DOI] [PMC free article] [PubMed]
- 228.Eftekhar-Sadat B, Ghavami M, Toopchizadeh V, Ghahvechi Akbari M. Wrist bone mineral density utility in diagnosing hip osteoporosis in postmenopausal women. Ther Adv Endocrinol Metab. 2016;7(5-6):207–211. doi: 10.1177/2042018816658164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Black DM, Schwartz AV, Ensrud KE et al. FLEX Research Group (2006) Effects of continuing or stopping alendronate after 5 years of treatment: The Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296(24):2927–2938 [DOI] [PubMed]
- 230.Miller PD, McClung MR, Macovei L, et al. Monthly oral ibandronate therapy in postmenopausal osteoporosis: 1-year results from the MOBILE study. J Bone Miner Res. 2005;20(8):1315–1322. doi: 10.1359/JBMR.050313. [DOI] [PubMed] [Google Scholar]
- 231.Reginster JY, Adami S, Lakatos P, et al. Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2-year results from the MOBILE study. Ann Rheu Dis. 2006;65(5):654–661. doi: 10.1136/ard.2005.044958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Eisman JA, Civitelli R, Adami S, et al. Efficacy and tolerability of intravenous ibandronate injections in postmenopausal osteoporosis: 2-year results from the DIVA study. J Rheumatol. 2008;35(3):488–497. [PubMed] [Google Scholar]
- 233.McClung MR, Geusens P, Miller PD et al. Hip Intervention Program Study Group (2001) Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med 344(5):333-340 [DOI] [PubMed]
- 234.Black DM, Delmas PD, Eastell R, et al. HORIZON Pivotal Fracture Trial Group (2003) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Eng J Med 0. 2007;356(18):1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 235.Sorensen OH, Crawford GM, Mulder H, et al. Long-term efficacy of risedronate: a 5-year placebo-controlled clinical experience. Bone 32:(2):120-126 [DOI] [PubMed]
- 236.Anderson GL, Limacher M, Assaf AR, Women’s Health Initiative Steering Committee et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 237.Cosman F, Hattersley G, Hu MY, Williams GC, Fitzpatrick LA, Black DM. Effects of abaloparatide-SC on fractures and bone mineral density in subgroups of postmenopausal women with osteoporosis and varying baseline risk factors. J Bone Miner Res. 2017;32(1):17–23. doi: 10.1002/jbmr.2991. [DOI] [PubMed] [Google Scholar]
- 238.Kanis JA, Johansson H, Oden A, et al. The effects of a revision for the USA. Osteoporos Int. 2010;21(1):35–40. doi: 10.1007/s00198-009-1033-8. [DOI] [PubMed] [Google Scholar]
- 239.Cummings SR, Cosman F, Lewiecki EM, et al. Goal-directed treatment for osteoporosis: a progress report from the ASBMR-NOF working group on goal-directed treatment for osteoporosis. J Bone Miner Res. 2017;32:3–10. doi: 10.1002/jbmr.3039. [DOI] [PubMed] [Google Scholar]
- 240.Roux C, Briot K. Imminent fracture risk. Osteoporos Int. 2017;28(6):1765–1769. doi: 10.1007/s00198-017-3976-5. [DOI] [PubMed] [Google Scholar]
- 241.Tsai JN, Uihlein AV, Burnett-Bowie SA, et al. Comparative effects of teriparatide, denosumab, and combination therapy on peripheral compartmental bone density, microarchitecture, and estimated strength: the DATA-HRpQCT Study. J Bone Miner Res. 2015;30(1):39–45. doi: 10.1002/jbmr.2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Leder BZ, Tsai JN, Neer RM, Uihlein AV, Wallace PM, Burnett-Bowie SA. Response to therapy with teriparatide, denosumab, or both in postmenopausal women in the DATA (Denosumab And Teriparatide Administration) Study randomized controlled trial. J Clin Densitom. 2016;19(3):346–351. doi: 10.1016/j.jocd.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 243.Lou S, Lv H, Li Z, Tang P. Combination therapy of anabolic agents and bisphosphonates on bone mineral density in patients with osteoporosis: a meta-analysis of randomised controlled trials. BMJ Open. 2018;8:e015187. doi: 10.1136/bmjopen-2016-015187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Cosman F, Nieves JW, Dempster DW. Treatment sequence matters: anabolic and antiresorptive therapy for osteoporosis. J Bone Miner Res. 2017;32:198–202. doi: 10.1002/jbmr.3051. [DOI] [PubMed] [Google Scholar]
- 245.Tsai JN, Lee H, David NL, Eastell R, Leder BZ (2019) Combination denosumab and high dose teriparatide for postmenopausal osteoporosis (DATA-HD): a randomised, controlled phase 4 trial. Lancet Diabetes Endocrinol 7(10):767–775 [DOI] [PMC free article] [PubMed]
- 246.Tsai JN, Uihlein AV, Burnett-Bowie SM, et al. Effects of two years of teriparatide, denosumab, or both on bone microarchitecture and strength (DATA-HRpQCT study) J Clin Endocrinol Metab. 2016;101(5):2023–2030. doi: 10.1210/jc.2016-1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Haas AV, LeBoff MS. Osteoanabolic agents for osteoporosis. J Endocr Soc. 2018;2(8):922–932. doi: 10.1210/js.2018-00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Obermayer-Pietsch BM, Marin F, McCloskey EV et al. EUROFORS Investigators (2008) Effects of two years of daily teriparatide treatment on BMD in postmenopausal women with severe osteoporosis with and without prior antiresorptive treatment. J Bone Miner Res 23(10):1591–1600 [DOI] [PubMed]
- 249.Boonen S, Marin F, Obermayer-Pietsch B et al. EUROFORS Investigators (2008). Effects of previous antiresorptive therapy on the bone mineral density response to two years of teriparatide treatment in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 93(3):852–860 [DOI] [PubMed]
- 250.Miller PD, Delmas PD, Lindsay R et al. Open-label Study to Determine How Prior Therapy with Alendronate or Risedronate in Postmenopausal Women with Osteoporosis Influences the Clinical Effectiveness of Teriparatide Investigators (2008) Early responsiveness of women with osteoporosis to teriparatide after therapy with alendronate or risedronate. J Clin Endocrinol Metab 93(10):3785-3793 [DOI] [PMC free article] [PubMed]
- 251.Modi A, Siris ES, Tang J, Sen S (2015) Cost and consequences of noncompliance with osteoporosis treatment among women initiating therapy. Curr Med Res Opin 31(4):757-765 [DOI] [PubMed]
- 252.Hui RL, Adams AL, Niu F et al (2017) Predicting adherence and persistence with oral bisphosphonate therapy in an integrated health care delivery system. J Manag Care Spec Pharm 23(4):503–512 [DOI] [PMC free article] [PubMed]
- 253.Raybould G, Babatunde O, Evans AL, Jordan JL, Paskins Z (2018) Expressed information needs of patients with osteoporosis and/or fragility fractures: a systematic review. Arch Osteoporos 13(1):55 [DOI] [PMC free article] [PubMed]
- 254.Ross S, Samuels E, Gairy K, Iqbal S, Badamgarav E, Siris E. A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health. 2011;14:571–581. doi: 10.1016/j.jval.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 255.Lewiecki EM. The role of risk communication in the care of osteoporosis. Curr Osteoporos Rep. 2010;9:141–148. doi: 10.1007/s11914-011-0056-1. [DOI] [PubMed] [Google Scholar]
- 256.Lindsay BR, Olufade T, Bauer J, Babrowicz J, Hahn R. Patient-reported barriers to osteoporosis therapy. Arch Osteoporos. 2016;11(1):19. doi: 10.1007/s11657-016-0272-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Scoville EA, Ponce de Leon Lovaton P, Shah ND, Pencille LJ, Montori VM. Why do women reject bisphosphonates for osteoporosis? A videographic study. PLoS One. 2011;6:e18468. doi: 10.1371/journal.pone.0018468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Yood RA, Mazor KM, Andrade SE, Emani S, Chan W, Kahler KH. Patient decision to initiate therapy for osteoporosis: the influence of knowledge and beliefs. J Gen Intern Med. 2008;23:1815–1821. doi: 10.1007/s11606-008-0772-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Yu J, Brenneman SK, Sazonov V, Modi A. Reasons for not initiating osteoporosis therapy among a managed care population. Patient Prefer Adherence. 2015;9:821–830. doi: 10.2147/PPA.S81963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Barrionuevo PM, Gionfriddo MR, Castaneda-Guarderas A, et al. Women’s values and preferences regarding osteoporosis osteoporosis treatments: a systematic review. J Clin Endocrinol Metab. 2019;104(5):1631–1636. doi: 10.1210/jc.2019-00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Hall SF, Edmonds SW, Lou Y, et al. Patient-reported reasons for nonadherence to recommended osteoporosis pharmacotherapy. J Am Pharm Assoc. 2017;57(4):503–509. doi: 10.1016/j.japh.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.National Osteoporosis Foundation (2019) Patient Perception of Value in Healthcare: Osteoporosis and Bone Fragility A Patient-Oriented Value (POV™) Report. Prepared by Connect 4 Strategies, LLC, on behalf of National Osteoporosis Foundation. July 29, 2019
- 263.Lewiecki EM, Binkley N, Bilezikian JP. Treated osteoporosis is still osteoporosis. J Bone Miner Res. 2019;34(4):605–606. doi: 10.1002/jbmr.3671. [DOI] [PubMed] [Google Scholar]
- 264.Black DM, Reid IR, Boonen S, et al. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT) J Bone Miner Res. 2012;27:243–254. doi: 10.1002/jbmr.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Black DM, Bauer DC, Schwartz AV, Cummings SR, Rosen CJ. Continuing bisphosphonate treatment for osteoporosis--for whom and for how long? N Engl J Med. 2012;366(22):2051–2053. doi: 10.1056/NEJMp1202623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Boonen S, Ferrari S, Miller PD. Postmenopausal osteoporosis treatment with antiresorptives: effects of discontinuation or long-term continuation on bone turnover and fracture risk—a perspective. J Bone Miner Res. 2012;27(5):963–974. doi: 10.1002/jbmr.1570. [DOI] [PubMed] [Google Scholar]
- 267.Miller PD, Bolognese MA, Lewiecki EM et al AMG Bone Loss Study Group (2008) Effect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trial. Bone 43:222–229 [DOI] [PubMed]
- 268.Tsourdi E, Langdahl B, Cohen-Solal M, et al. Discontinuation of denosumab therapy for osteoporosis: a systematic review and position statement by ECTS. Bone. 2017;105:11–17. doi: 10.1016/j.bone.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 269.Nayak S, Greenspan SL. Osteoporosis treatment efficacy for men: a systematic review and meta-analysis. J Am Geriatr Soc. 2017;65(3):490–495. doi: 10.1111/jgs.14668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Smith MR, Egerdie B, Hernández Toriz N et al. Denosumab HALT Prostate Cancer Study Group (2009) Denosumab in men receiving androgen-deprivation therapy for prostate cancer. N Engl J Med 361(8):745–755 [DOI] [PMC free article] [PubMed]
- 271.Brown-Glaberman U, Stopeck AT. Impact of denosumab on bone mass in cancer patients. Clin Pharmacol. 2013;5:117–129. doi: 10.2147/CPAA.S30330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Overman RA, Toliver JC, Yeh JY, Gourlay ML, Deal CL. United States adults meeting 2010 American College of Rheumatology criteria for treatment and prevention of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken). 2014;66:1644–1652. doi: 10.1002/acr.22346. [DOI] [PubMed] [Google Scholar]
- 273.Compston J. Glucocorticoid-induced osteoporosis: an update. Endocrine. 2018;61(1):7–16. doi: 10.1007/s12020-018-1588-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.van Staa TP, Leufkens HG, Abenhaim L et al (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology (Oxford) 39(12):1383–1389 [DOI] [PubMed]
- 275.Donnan PT, Libby G, Boyter AC, Thompson P. The population risk of fractures attributable to oral corticosteroids. Pharmacoepidemiol Drug Saf. 2005;14(3):177–186. doi: 10.1002/pds.1075. [DOI] [PubMed] [Google Scholar]
- 276.Allen CS, Yeung JH. Bisphosphonates for steroid-induced osteoporosis. Cochrane Database Syst Rev. 2016;10:CD001347. doi: 10.1002/14651858.CD001347.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Saag KG, Zanchetta JR, Devogelaer JP, et al. Effects of teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: thirty-six-month results of a randomized, double-blind, controlled trial. Arthritis Rheu. 2009;60(11):3346–3355. doi: 10.1002/art.24879. [DOI] [PubMed] [Google Scholar]
- 278.Yanbeiy ZA, Hansen KE. Denosumab in the treatment of glucocorticoid-induced osteoporosis: a systematic review and meta-analysis. Drug Des Devel Ther. 2019;13:2843–2852. doi: 10.2147/DDDT.S148654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Saag KG, Wagman RB, Geusens P, et al. Denosumab versus risedronate in glucocorticoid-induced osteoporosis: a multicentre, randomised, double-blind, active-controlled, double-dummy, non-inferiority study. Lancet Diabetes Endocrinol. 2018;6(6):445–454. doi: 10.1016/S2213-8587(18)30075-5. [DOI] [PubMed] [Google Scholar]
- 280.Toulis KA, Anastasilakis AD (2010) Increased risk of serious infections in women with osteopenia or osteoporosis treated with denosumab. Osteoporos Int 21(11):1963-1964. Epub 2009 Dec 15. No abstract available. (Erratum in: Osteoporos Int 2010 Nov;21[11]:1965) [DOI] [PubMed]
- 281.Curtis JR, Xie F, Yun H, Saag KG, Chen L, Delzell E. Risk of hospitalized infection among rheumatoid arthritis patients concurrently treated with a biologic agent and denosumab. Arthritis Rheumatol. 2015;67(6):1456–1464. doi: 10.1002/art.39075. [DOI] [PubMed] [Google Scholar]
- 282.Lau AN, Wong-Pack M, Rodjanapiches R, et al. Occurrence of serious infection in patients with rheumatoid arthritis treated with biologics and denosumab observed in a clinical setting. J Rheumatol. 2018;45(2):170–176. doi: 10.3899/jrheum.161270. [DOI] [PubMed] [Google Scholar]
- 283.Boonen S, Black DM, Colón-Emeric CS, et al. Efficacy and safety of a once-yearly intravenous zoledronic acid 5 mg for fracture prevention in elderly postmenopausal women with osteoporosis aged 75 and older. J Am Geriatr Soc. 2010;58(2):292–299. doi: 10.1111/j.1532-5415.2009.02673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.McClung MR, Boonen S, Törring O, et al. Effect of denosumab treatment on the risk of fractures in subgroups of women with postmenopausal osteoporosis. J Bone Min Res. 2012;27:211–218. doi: 10.1002/jbmr.536. [DOI] [PubMed] [Google Scholar]
- 285.Boonen S, Marin F, Mellstrom D. Safety and efficacy of teriparatide in elderly women with established osteoporosis: bone anabolic therapy from a geriatric perspective. J Am Geriatr Soc. 2006;54(5):782–789. doi: 10.1111/j.1532-5415.2006.00695.x. [DOI] [PubMed] [Google Scholar]
- 286.Greenspan SL, Schneider DL, McClung MR, et al. Alendronate improves bone mineral density in elderly women with osteoporosis residing in long-term care facilities. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2002;136(10):742–746. doi: 10.7326/0003-4819-136-10-200205210-00009. [DOI] [PubMed] [Google Scholar]
- 287.Greenspan SL, Perera S, Ferchak MA, Nace DA, Resnick NM. Efficacy and safety of single-dose zoledronic acid for osteoporosis in frail elderly women: a randomized clinical trial. JAMA Intern Med. 2015;175(6):913–921. doi: 10.1001/jamainternmed.2015.0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Bonnick SL. Dual-energy x-ray absorptiometry: interpreting reports and serial measurements. Clin Obstet Gynecol. 2013;56(4):677–685. doi: 10.1097/GRF.0b013e3182a8240c. [DOI] [PubMed] [Google Scholar]
- 289.Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818–839. doi: 10.7326/M15-1361. [DOI] [PubMed] [Google Scholar]
- 290.Nishiyama KK, Macdonald HM, Hanley DA, Boyd SK. Women with previous fragility fractures can be classified based on bone microarchitecture and finite element analysis measured with HR-pQCT. Osteoporos Int. 2013;24(5):1733–1740. doi: 10.1007/s00198-012-2160-1. [DOI] [PubMed] [Google Scholar]
- 291.Viceconti M, Qasim M, Bhattacharya P, Li X. Are CT-based finite element model predictions of femoral bone strengthening clinically useful? Curr Osteoporos Rep. 2018;16(3):216–223. doi: 10.1007/s11914-018-0438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Oei L, Koromani F, Rivadeneira F, Zillikens MC, Oei EH. Quantitative imaging methods in osteoporosis. Quant Imaging Med Surg. 2016;6(6):680–698. doi: 10.21037/qims.2016.12.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Vasikaran S, Eastell R, Bruyère O et al. IOF-IFCC Bone Marker Standards Working Group (2011) Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int 22(2):391–420 [DOI] [PubMed]
- 294.Melton LJIII. How many women have osteoporosis now? J Bone Miner Res. 1995;10:175–177. doi: 10.1002/jbmr.5650100202. [DOI] [PubMed] [Google Scholar]
- 295.Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL (2010) The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil 1(1):6–14 [DOI] [PMC free article] [PubMed]
- 296.Forsén L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short and long term excess mortality according to age and gender. Osteoporos Int. 1999;10(1):73–78. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 297.Kado DM, Duong T, Stone KL, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14(7):589–594. doi: 10.1007/s00198-003-1412-5. [DOI] [PubMed] [Google Scholar]
- 298.Ensrud KE, Thompson DE, Cauley JA, et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc. 2000;48(3):241–249. doi: 10.1111/j.1532-5415.2000.tb02641.x. [DOI] [PubMed] [Google Scholar]
- 299.Pan PJ, Lin PH, Tang GJ, Lan TY. Comparisons of mortality and rehospitalization between hip-fractured elderly with outpatient rehabilitation and those without: A STROBE-compliant article. Medicine (Baltimore) 2018;97(19):e0644. doi: 10.1097/MD.0000000000010644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Tedesco D, Gibertoni D, Rucci P, et al. Impact of rehabilitation on mortality and readmissions after surgery for hip fracture. BMC Health Serv Res. 2018;18(1):701. doi: 10.1186/s12913-018-3523-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Latham NK, Harris BA, Bean JF, et al. Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial. JAMA. 2014;311(7):700–708. doi: 10.1001/jama.2014.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Vochteloo AJ, Moerman S, Tuinebreijer WE, et al. More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int. 2013;13(2):334–341. doi: 10.1111/j.1447-0594.2012.00904.x. [DOI] [PubMed] [Google Scholar]
- 303.Greendale GA, Barrett-Connor E (1996) Outcomes of osteoporotic fractures. In: Marcus R, Freedman D, Kelsey J (eds) Osteoporosis. Academy Press, Orlando, FL
- 304.Marottoli RA, Berkman LF, Cooney LM., Jr Decline in physical function following hip fracture. J Am Geriatr Soc. 1992;4(9):861–866. doi: 10.1111/j.1532-5415.1992.tb01980.x. [DOI] [PubMed] [Google Scholar]
- 305.Dyer SM, Crotty M, Fairhall N et al. Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16(1):158 [DOI] [PMC free article] [PubMed]
- 306.Alexandru D, So W. Evaluation and management of vertebral compression fractures. Perm J. 2012;16(4):46–51. doi: 10.7812/TPP/12-037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 1990;141:68–71. doi: 10.1164/ajrccm/141.1.68. [DOI] [PubMed] [Google Scholar]
- 308.Leidig G, Minne HW, Sauer P, et al. A study of complaints and their relation to vertebral destruction in patients with osteoporosis. J Bone Miner Res. 1990;8(3):217–229. doi: 10.1016/0169-6009(90)90107-Q. [DOI] [PubMed] [Google Scholar]
- 309.Kortebein P, Symons TB, Ferrando A, et al. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63(10):1076–1081. doi: 10.1093/gerona/63.10.1076. [DOI] [PubMed] [Google Scholar]
- 310.Krolner B, Toft B. Vertebral bone loss: an unheeded side effect of therapeutic bed rest. Clin Sci Br. 1983;64(5):537–540. doi: 10.1042/cs0640537. [DOI] [PubMed] [Google Scholar]
- 311.Kato T, Inose H, Ichimura S et al (2019) Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: a prospective, randomized, multicenter study. J Clin Med 8(2):198 [DOI] [PMC free article] [PubMed]
- 312.Ware LC (1993) Internal/external fixation of wrist and distal forearm fractures In: Clark GL, Wilgis EFS, Aiello B, Ckhous D, Eddington LV, eds. Hand rehabilitation, a practical guide. New York. NY: Churchill Livingstone 1993:299–305
- 313.Rozental TD, Shah J, Chacko AT, Zurakowski D. Prevalence and predictors of osteoporosis risk in orthopaedic patients. Clin Orthop Relat Res. 2009;468(7):1765–1772. doi: 10.1007/s11999-009-1162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Kuo LC, Yang TH, Hsu YY, et al. Is progressive early digit mobilization intervention beneficial for patients with external fixation of distal radius fracture? A pilot randomized controlled trial. Clin Rehabil. 2013;27(11):983–993. doi: 10.1177/0269215513487391. [DOI] [PubMed] [Google Scholar]
- 315.The Interagency Pain Research Coordinating Committee (2018) National Pain Strategy: a comprehensive population health-level strategy for pain. Available at: https://www.iprcc.nih.gov/national-pain-strategy-overview Accessed (December 2019)
- 316.The Joint Commission (2017) Pain assessment and management standards for hospitals. R3 Report|Requirement, Rationale, Reference. Issue 11, August 29, 2017. Available online at: https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/r3_report_issue_11_pain_assessment_8_25_17_final.pdf?db=web&hash=938C24A464A5B8B5646C8E297C8936C1&hash=938C24A464A5B8B5646C8E297C8936C1 Accessed July 2019.
- 317.Nafziger AN, Barkin RL. Opioid therapy in acute and chronic pain. J Clin Pharmacol. 2018;58(9):1111–1122. doi: 10.1002/jcph.1276. [DOI] [PubMed] [Google Scholar]
- 318.Buchbinder R, Johnston RV, Rischin KJ, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2018;4:CD006349. doi: 10.1002/14651858.CD006349.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Wang B, Zhao CP, Song LX, Zhu L. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: a meta-analysis and systematic review. J Orthop Surg Res. 2018;13(1):264. doi: 10.1186/s13018-018-0952-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Mattie R, Laimi K, Yu S, Saltychev M. Comparing percutaneous vertebroplasty and conservative therapy for treating osteoporotic compression fractures in the thoracic and lumbar spine: a systematic review and meta-analysis. J Bone Joint Surg Am. 2016;98(12):1041–1051. doi: 10.2106/JBJS.15.00425. [DOI] [PubMed] [Google Scholar]
- 321.Rodriguez AJ, Fink HA, Mirigian L, et al. Pain, quality of life, and safety outcomes of kyphoplasty for vertebral compression fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2017;32(9):1935–1344. doi: 10.1002/jbmr.3170. [DOI] [PubMed] [Google Scholar]
- 322.Boonen S, Van Meirhaeghe J, Bastian L, et al. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res. 2011;26(7):1627–1637. doi: 10.1002/jbmr.364. [DOI] [PubMed] [Google Scholar]
- 323.Blasco J, Martinez-Ferrer A, Macho J, et al. Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up. controlled trial. J Bone Miner Res. 2012;27(5):1159–1166. doi: 10.1002/jbmr.1564. [DOI] [PubMed] [Google Scholar]
- 324.Ebeling PR, Akesson K, Bauer DC et al (2019) The efficacy and safety of vertibral augmentation: a second ASBMR Task Force report. J Bone Miner Res 34(1): 3–21 [DOI] [PubMed]
- 325.Chen Z, Wu Y, Ning S, Ma T, Wu Z. Risk factors of secondary vertebral compression fracture after percutaneous vertebroplasty or kyphoplasty: a retrospective study of 650 patients. Med Sci Monit. 2019;25:9255–9261. doi: 10.12659/MSM.915312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Zhang H, Xu C, Zhang T, Gao Z, Zhang T. Does percutaneous vertebroplasty or balloon kyphoplasty for osteoporotic vertebral compression fractures increase the incidence of new vertebral fractures? A meta-analysis. Pain Physician. 2017;20(1):E13–E28. doi: 10.36076/ppj.2017.1.E13. [DOI] [PubMed] [Google Scholar]
- 327.Li HM, Zhang RJ, Gao H, et al. New vertebral fractures after osteoporotic vertebral compression fracture between balloon kyphoplasty and nonsurgical treatment PRISMA. Medicine (Baltimore) 2018;97(40):e12666. doi: 10.1097/MD.0000000000012666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Voormolen MH, Lohle PN, Lampmann LE, et al. Prospective clinical follow-up after percutaneous vertebroplasty in patients with painful osteoporotic vertebral compression fractures. J Vasc Interv Radiol. 2006;17(8):1313–1320. doi: 10.1097/01.RVI.0000231952.75209.4A. [DOI] [PubMed] [Google Scholar]
- 329.Markozannes G, Aretouli E, Rintou E, et al. An umbrella review of the literature on the effectiveness of psychological interventions for pain reduction. BMC Psychol. 2017;5(1):31. doi: 10.1186/s40359-017-0200-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Eccleston C, Crombez G (2017) Advancing psychological therapies for chronic pain. F1000Res 6:461. Published 2017 Apr 11. [DOI] [PMC free article] [PubMed]
- 331.Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015;h444:350. doi: 10.1136/bmj.h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Cai G, Laslett LL, Aitken D, et al. Effect of zoledronic acid and denosumab in patients with low back pain and modic change: a proof-of-principle trial. J Bone Miner Res. 2018;33(5):773–782. doi: 10.1002/jbmr.3376. [DOI] [PubMed] [Google Scholar]
- 333.Paolucci T, Saraceni VM. Piccinini G (2016) Management of chronic pain in osteoporosis: challenges and solutions. J Pain Res. 2016;9:177–186. doi: 10.2147/JPR.S83574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Catalano A, Martino G, Morabito N, et al. Pain in osteoporosis: from pathophysiology to therapeutic approach. Drugs Aging. 2017;34(10):755–765. doi: 10.1007/s40266-017-0492-4. [DOI] [PubMed] [Google Scholar]
- 335.Lange U, Teichmann J, Uhlemann C. Current knowledge about physiotherapeutic strategies in osteoporosis prevention and treatment. Rheumatol Int. 2005;26(2):99–106. doi: 10.1007/s00296-004-0528-z. [DOI] [PubMed] [Google Scholar]
- 336.Finnerup NB. Nonnarcotic methods of pain management. N Engl J Med. 2019;380:2440–2448. doi: 10.1056/NEJMra1807061. [DOI] [PubMed] [Google Scholar]
- 337.Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol. 2006;164(5):487–496. doi: 10.1093/aje/kwj224. [DOI] [PubMed] [Google Scholar]
- 338.Kremer M, Yalcin I, Goumon Y, et al. A dual noradrenergic mechanism for the relief of neuropathic allodynia by the antidepressant drugs duloxetine and amitriptyline. J Neurosci. 2018;38(46):9934–9954. doi: 10.1523/JNEUROSCI.1004-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Tick H, Nielsen A, Pelletier KR et al. Pain Task Force of the Academic Consortium for Integrative Medicine and Health (2018) Evidence-based nonpharmacologic strategies for comprehensive pain care: the Consortium Pain Task Force white paper. Explore (NY) 14(3):177-211 [DOI] [PubMed]
- 340.Abe T, Shibao Y, Takeuchi Y, et al. Initial hospitalization with rigorous bed rest followed by bracing and rehabilitation as an option of conservative treatment for osteoporotic vertebral fractures in elderly patients: a pilot one arm safety and feasibility study. Arch Osteoporos. 2018;13(1):134. doi: 10.1007/s11657-018-0547-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Parreira PCS, Maher CG, Megale RZ, March L, Ferreira ML. An overview of clinical guidelines for the management of vertebral compression fracture: a systematic review. Spine J. 2017;17(12):1932–1938. doi: 10.1016/j.spinee.2017.07.174. [DOI] [PubMed] [Google Scholar]
- 342.Newman M, Minns Lowe C, Barker K. Spinal orthoses for vertebral osteoporosis and osteoporotic vertebral fracture: a systematic review. Arch Phys Med Rehabil. 2016;97(6):1013–1025. doi: 10.1016/j.apmr.2015.10.108. [DOI] [PubMed] [Google Scholar]
- 343.Knopp-Sihota JA, Newburn-Cook CV, Homik J, Cummings GG, Voaklander D. Calcitonin for treating acute and chronic pain of recent and remote osteoporotic vertebral compression fractures: a systematic review and meta-analysis. Osteoporos Int. 2012;23(1):17. doi: 10.1007/s00198-011-1676-0. [DOI] [PubMed] [Google Scholar]
- 344.Jalali ZM, Farghadani A, Ejlali-Vardoogh M. Effect of cognitive-behavioral training on pain self-efficacy, self-discovery, and perception in patients with chronic low-back pain: a quasi-experimental study. Anesth Pain Med. 2019;9(2):e78905. doi: 10.5812/aapm.78905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Knoerl R, Lavoie Smith EM, Weisberg J. Chronic pain and cognitive behavioral therapy: an integrative review. West J Nurs Res. 2016;38(5):596–628. doi: 10.1177/0193945915615869. [DOI] [PubMed] [Google Scholar]
- 346.Andronis L, Kinghorn P, Qiao S, Whitehurst DG, Durrell S, McLeod H. Cost-effectiveness of non-invasive and non-pharmacological interventions for low back pain: a systematic literature review . Appl Health Econ Health Policy. 2017;15(2):173–201. doi: 10.1007/s40258-016-0268-8. [DOI] [PubMed] [Google Scholar]
- 347.Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 348.Guo Z, Chen W, Su Y, Yuan J, Zhang Y. Isolated unilateral vertebral pedicle fracture caused by a back massage in an elderly patient: a case report and literature review. Eur J Orthop Surg Traumatol. 2013;23(Suppl 2):S149–S153. doi: 10.1007/s00590-012-1031-y. [DOI] [PubMed] [Google Scholar]
- 349.Huang WC, Lin MH, Lee MH, et al. Percutaneous dorsal root ganglion block for treating lumbar compression fracture-related pain. Acta Neurochir (Wien). 2018;160(6):1283–1289. doi: 10.1007/s00701-018-3535-7. [DOI] [PubMed] [Google Scholar]
- 350.Zuo XH, Zhu XP, Bao HG, et al. Network meta-analysis of percutaneous vertebroplasty, percutaneous kyphoplasty, nerve block, and conservative treatment for nonsurgery options of acute/subacute and chronic osteoporotic vertebral compression fractures (OVCFs) in short-term and long-term effects. Medicine (Baltimore) 2018;97(29):e11544. doi: 10.1097/MD.0000000000011544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Ohtori S, Yamashita M, Inoue G, et al. L2 spinal nerve-block effects on acute low back pain from osteoporotic vertebral fracture. J Pain. 2009;10(8):870–875. doi: 10.1016/j.jpain.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 352.Esses SI, McGuire R, Jenkins J, et al. The treatment of symptomatic osteoporotic spinal compression fractures. J Am Acad Orthop Surg. 2011;19(3):176–182. doi: 10.5435/00124635-201103000-00007. [DOI] [PubMed] [Google Scholar]
- 353.Hansen KA, McKernan LC, Carter SD, Allen C, Wolever RQ. A replicable and sustainable whole person care model for chronic pain. J Altern Complement Med. 2019;25(S1):S86–S94. doi: 10.1089/acm.2018.0420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR. High-intensity exercise did not cause vertebral fractures and improves thoracic kyphosis in postmenopausal women with low to very low bone mass: the LIFTMOR trial. Osteoporos Int. 2019;30(5):957–964. doi: 10.1007/s00198-018-04829-z. [DOI] [PubMed] [Google Scholar]
- 355.Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984;65:593–596. [PubMed] [Google Scholar]
- 356.Ekin JA, Sinaki M. Vertebral compression fractures sustained during golfing: report of three cases. Mayo Clin Proc. 1993;68:566–570. doi: 10.1016/S0025-6196(12)60371-1. [DOI] [PubMed] [Google Scholar]
- 357.National Osteoporosis Foundation (2019) Boning up on osteoporosis. National Osteoporosis Foundation, Arlington, VA
- 358.Watson SL, Weeks BK, Weis LJ, Harding AT, Horam SA, Beck BR. High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with women with osteopenia and osteoporosis: the LIFTMOR randomized controlled trial. J Bone Miner Res. 2018;33(2):211–220. doi: 10.1002/jbmr.3284. [DOI] [PubMed] [Google Scholar]
- 359.Skelton DA, Mavroeidi A. Which strength and balance activities are safe and efficacious for individuals with specific challenges (osteoporosis, vertebral fractures, frailty, dementia)? 2018. J Frailty Sarcopenia Falls. 2018;3(2):85–104. doi: 10.22540/JFSF-03-085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Liu CK, Leng X, Hsu FC, Kritchevsky SB, et al. The impact of sarcopenia on a physical activity intervention: the Lifestyle Interventions and Independence for Elders Pilot Study (LIFE-P) J Nutr Health Aging. 2014;18(1):59–64. doi: 10.1007/s12603-013-0369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.National Committee for Quality Assurance (NCQA) (2014) Report cards health plans state of health care quality 2014: osteoporosis testing in older women. Available at https://www.ncqa.org/hedis/measures/osteoporosis-management-in-women-who-had-a-fracture-omw/ Accessed January 2019
- 362.Gillespie CW, Morin PE. Osteoporosis-related health services utilization following first hip fracture among a cohort of privately insured women in the United States: an observational study. J Bone Miner Res. 2017;32(5):1052–1061. doi: 10.1002/jbmr.3079. [DOI] [PubMed] [Google Scholar]
- 363.Conley RB, Adib G, Adler RA, et al. Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition. J Bone Miner Res. 2020;35(1):36–52. doi: 10.1002/jbmr.3877. [DOI] [PubMed] [Google Scholar]
- 364.Boudreau DM, Yu O, Balasubramanian A, et al. A survey of women’s awareness of and reasons for lack of postfracture osteoporotic care. J Am Geriatr Soc. 2017;65(8):1829–1835. doi: 10.1111/jgs.14921. [DOI] [PubMed] [Google Scholar]
- 365.Schuit SC, van der Klift M, Weel AE, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004;34:195–202. doi: 10.1016/j.bone.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 366.Åkesson K, Marsh D, Mitchell PJ et al. IOF Fracture Working Group (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135-2152 [DOI] [PMC free article] [PubMed]
- 367.Eisman JA, Bogoch ER, Dell R et al. ASBMR Task Force on Secondary Fracture Prevention (2012) Making the first fracture the last fracture: ASBMR task-force report on secondary fracture prevention. J Bone Miner Res 27(10):2039–2046 [DOI] [PubMed]
- 368.Bunta AD, Edwards BJ, Macaulay WB, Jr, et al. Own the Bone, a system-based intervention, improves osteoporosis care after fragility fractures. J Bone Joint Surg Am. 2016;98(24):e109. doi: 10.2106/JBJS.15.01494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Lewiecki EM, Binkley NC, Bilezikian JP. Treated osteoporosis is still osteoporosis. J Bone Miner Res. 2018;34(4):3671. doi: 10.1002/jbmr.3671. [DOI] [PubMed] [Google Scholar]