Abstract
Background
All chronic liver diseases could lead to liver fibrosis. Accurate diagnosis and stage of fibrosis were important for the medical determination, management, and therapy. Liver biopsy was considered to be the gold criteria of fibrosis diagnosis. However, liver biopsy was an invasive method with some drawbacks. Non‐invasive tests for liver fibrosis included radiologic method and serum‐based test. Radiologic examination was influenced by obesity, cost, and availability. Serum‐based test was widely used in the screening and diagnostic of liver fibrosis. However, the accuracy was still needed to be improved.
Methods
Recent studies showed serum non‐coding RNAs: microRNA, long non‐coding RNA(lncRNA), and circular RNA(circRNA), which have the potentiality to be non‐invasive markers for liver fibrosis. The recent progress was summarized in this review.
Results
These studies showed serum non‐coding RNAs exerted a good diagnostic performance for liver fibrosis. A panel that included several non‐coding RNAs could increase the accuracy of single marker.
Conclusions
Serum microRNAs, lncRNAs, and circRNAs could be potential non‐invasive markers for diagnosis and stage of liver fibrosis. More high‐quality clinical study is needed for further research.
Keywords: circRNA, diagnosis, liver fibrosis, lncRNA, microRNA, stage
MicroRNAs, lncRNAs, circRNAs and exosomes which were released from liver enter into circulating vessels. The blood which contain these molecules are drawed from patients. Then the blood specimen are tested for diagnose of early fibrosis or stage fibrosis in patients with liver diseases.
![]()
1. INTRODUCTION
Although the liver has regeneration capacity, chronic liver injury would lead to liver fibrosis. 1 Advanced fibrosis would result in liver‐related mortality: liver failure, and hepatocellular carcinoma. 2 The diagnosis of early liver fibrosis and accurate fibrosis stage was important for the screening, diagnosis, and treatment of liver fibrosis. Liver biopsy was the gold method to examine fibrosis. However, it has several implications: inconvenience for doctors and patients, invasive method which could cause pain and bleeding, and indeterminacy due to that specimen was only a very small part of the liver. 3 Non‐invasive tests for fibrosis were developed, which include radiologic and serum‐based test. Radiologic examinations include ultrasonography, magnetic resonance imaging, and elastography; however, they also have some implications: obesity impact, inconvenience, and high cost. 4 Serum‐based methods include serum algorithm model based on indirect markers such as liver function markers and serum direct markers which were correlated with fibrosis. 4 Recent studies have shown that serum non‐coding RNAs such as microRNA, long non‐coding RNA(lncRNA), and circular RNA(circRNA) played important roles in the diagnosis and stage of liver fibrosis. 5 , 6 , 7 The recent progress were summarized in this review. It may be that the microRNAs, lncRNAs, and circRNAs which were released from the liver could enter into circulating vessels and subsequently be detected for the diagnosis and stage of liver fibrosis (Figure 1).
FIGURE 1.
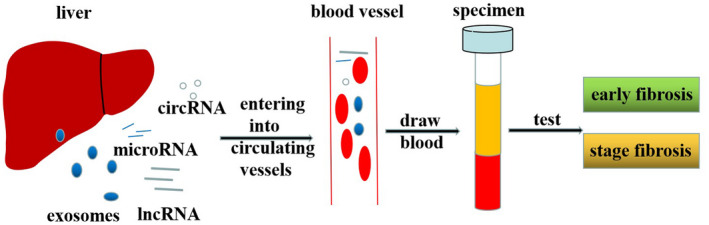
MicroRNAs, lncRNAs, circRNAs and exosomes which were released from liver enter into circulating vessels. The blood which contain these molecules are drawed from patients. Then the blood specimen are tested for diagnose of early fibrosis or stage fibrosis in patients with liver diseases.
2. MICRORNA
MicroRNAs were a class of about 22 nt regulatory non‐coding RNAs which were produced in virtually all cells in the body. 8 , 9 MicroRNAs could repress the expression of its target genes through binding to the 3’ UTR of complementary mRNAs. 10 , 11 Research also showed microRNAs played important roles in HBV and HCV‐related liver injury and fibrosis. 12 , 13 The role of serum microRNAs for the diagnosis and stage of liver fibrosis was summarized in this part (Table 1).
TABLE 1.
Serum microRNAs for diagnosis and stage of liver fibrosis
| Number | MicroRNA | Diseases | Country | Fibrosis diagnostic method | Expression/source | Cohort | AUC for fibrosis | AUC for early fibrosis | AUC for late fibrosis | AUC for stage fibrosis or late fibrosis | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | microRNA21 | CHB | China | Liver biopsy | Up/serum | 28 | NT | NT | NT | 0.64 | 16 |
| AIH | America | Liver biopsy | Up/serum | 46 | NT | NT | NT | NT | 17 | ||
| CHB | China | Liver biopsy | Up/serum | 123 | NT | NT | NT | 0.7589 | 18 | ||
| 2 | MicroRNA122 | CHC | Egypt | Liver biopsy | Up/serum | 40 | NT | 1.0 | NT | Can not | 25 |
| CHC | German | Liver biopsy | Up/serum | 68 | NT | NT | NT | Can not | 26 | ||
| CHB | Japan | Liver biopsy | Up/serum | 91 | NT | NT | NT | 0.668 | 27 | ||
| MAFLD | Egypt | Fibro‐scan | Up/serum | 120 | NT | NT | NT | NT | 28 | ||
| 3 | let‐7a‐5p | CHC | Japan | Liver biopsy | Up/serum | 84 | NT | NT | NT | 0.892 | 30 |
| schistosomiasis infected patients | Australia | Ultrasound | NT/serum | 163 | NT | NT | NT | 0.6598 | 31 | ||
| 4 | let‐7d‐5p | schistosomiasis infected patients | Australia | Ultrasound | NT/serum | 163 | NT | NT | NT | 0.6270 | 31 |
| 5 | microRNA214 | Biliary atresia | Japan | Liver biopsy | NT/serum | 28 | NT | NT | NT | 0.805 | 33 |
| 6 | microRNA155 | NT(liver cirrhosis) | China | Liver biopsy | NT//plasma exsosomes | 94 | NT | NT | 0.971 | NT | 40 |
| CHC | Egypt | Liver biopsy | NT/serum | 145 | NT | NT | NT | Can not | 41 | ||
| 7 | MicroRNA29a | NT | Germany | NT | Down/serum | 67 | NT | NT | 0.838 | NT | 46 |
| CHC,CHB | France | NT | Down in severe fibrosis /serum | 72,83 | NT | NT | NT | NT | 47 | ||
| 8 | MicroRNA‐1373g‐3p | CHC | China | Liver biopsy | Up in moderate to severe fibrosis compared to mild fibrosis/serum | 61 | NT | NT | NT | 0.790 | 49 |
| CHC | China | Liver biopsy | Up in moderate to severe fibrosis compared to mild fibrosis/serum | 112 | NT | NT | NT | 0.841‐0.933 | 50 | ||
| 9 | MicroRNA34a | CHC | China | Liver biopsy | Up/serum | 41 | NT | 0.8274 | 0.8904 | NT | 54 |
| 10 | MicroRNA17 | CHB | China | Liver biopsy | Up/serum | 200 | NT | 0.685 | 0.9169 | NT | 58 |
| 11 | MicroRNA20a | CHC | America | Liver biopsy | Up/serum | 44 | 0.704 | NT | NT | NT | 60 |
| 12 | MicroRNA138 | CHC | Egypt | Liver biopsy | Up/serum | 71 | NT | 0.866 | 0.924 | NT | 63 |
| 13 | microRNA150‐5p | schistosomiasis infected patients | Australia | Ultrasonography | Down in severe fibrosis compared to mild fibrosis/serum | 163 | NT | NT | NT | 0.6838 | 31 |
| 14 | microRNA146a‐5p | schistosomiasis infected patients | Australia | Ultrasonography | Down in severe fibrosis compared to mild fibrosis/serum | 163 | NT | NT | NT | 0.6575 | 31 |
| schistosomiasis infected patients | Australia | Ultrasound | Down/serum exosomes | 104 | 0.6315 | NT | NT | NT | 64 | ||
| 15 | microRNA532‐5p | schistosomiasis infected patients | Australia | Ultrasound | Down/serum exosomes | 104 | 0.6884 | NT | NT | NT | 64 |
| 16 | MicroRNA29b | CHB | China | Liver biopsy | Down in severe fibrosis compared to mild fibrosis/serum | 123 | NT | NT | NT | 0.7237 | 18 |
| 17 | MicroRNA29c | CHB | China | Liver biopsy | Down in severe fibrosis compared to mild fibrosis/serum | 123 | NT | NT | NT | 0.8121 | 18 |
| 18 | MicroRNA143 | CHB | China | Liver biopsy | Down in severe fibrosis compared to mild fibrosis/serum | 123 | NT | NT | NT | 0.8123 | 18 |
| 19 | MicroRNA223 | CHB | China | Liver biopsy | Down in severe fibrosis compared to mild fibrosis/serum | 123 | NT | NT | NT | 0.7806 | 18 |
| 20 | MicroRNA374 | CHB | China | Liver biopsy | Down in severe fibrosis compared to mild fibrosis/serum | 123 | NT | NT | NT | 0.7282 | 18 |
Abbreviations: CHB, chronic HBV hepatitis; CHC, chronic HCV hepatitis; MAFLD, metabolic‐associated fatty liver disease; NT, Not mentioned.
2.1. MicroRNA21
It has been shown that microRNA21 played an important role in liver fibrosis. 14 , 15 Research by Wu et al showed the expression of circulating microRNA21 in serum was significantly correlated with liver fibrosis stages of CHB patients in China, which was according to METAVIR score system through liver biopsy. 16 Twenty‐eight patients with CHB were enrolled and further analysis showed microRNA21 exhibited an inferior predictive performance to stage liver fibrosis as compared to the FIB4 and APRI. 16 The AUC for microRNA21 to differentiate patients with mild fibrosis (F1 and F2) from those with severe fibrosis (F3 and F4) was 0.64. 16 That is to say serum microRNA21 was correlated with fibrosis stages, but the diagnostic performance is not good enough to distinguish fibrosis stages of CHB patients. 16 It was still unknown that whether serum microRNA21 could discriminate early liver fibrosis from healthy controls or not. 17 Another research by Migita et al enrolled 46 type 1 autoimmune hepatitis (AIH) patients who underwent liver biopsy, 40 patients with chronic hepatitis C virus (CHC), and 13 healthy controls in America. 17 Results showed the expression of serum microRNA21 was significantly elevated in AIH patients than CHC patients and healthy controls. 17 The serum microRNA21 was reversely correlated with liver fibrosis stages of AIH. 17 However, the diagnostic performance of microRNA21 for liver fibrosis in AIH patients was not exerted. Research by Bao et al enrolled 123 CHB patients who underwent liver biopsy and 20 healthy controls. Results showed that the expression of microRNA21 in serum was much higher in CHB patients than healthy controls. 18 The expression of serum microRNA21 was also reversely correlated with fibrosis stages of CHB patients, which was consistent with that in AIH patients. 18 The AUC for serum microRNA21 to distinguish the patients with mild fibrosis (F0–F2) from those with severe fibrosis (F3–F4) was 0.7589. 18 Taken all these researches, it is concluded that serum microRNA21 could be a potential marker for the diagnosis of early fibrosis and staging fibrosis in AIH and CHB patients.
2.2. MicroRNA122
MicroRNA122 which was an abundant microRNA in the liver accounted for about 70% of all hepatic microRNAs. 19 , 20 MicroRNA122 had a strong association with HBV and HCV replication and regulated several metabolic processes including oxidation, synthesis fatty acid, and cholesterol biosynthesis. 21 , 22 , 23 , 24 Research by Omran et al enrolled 40 Egyptian CHC patients who underwent liver biopsy and 20 healthy controls. 25 The results showed the expression of serum microRNA122 was much higher in CHC patients than that of healthy controls. 25 Further analysis showed the AUC of microRNA122 to differentiate CHC patients with early fibrosis from healthy controls was 1. 25 The sensitivity and specificity was 100% and 100%, respectively. 25 These results indicated serum microRNA122 could be a potential non‐invasive marker for early fibrosis diagnosis in CHC patients. However, the research showed serum microRNA122 could not distinguish mild fibrosis (F1, F2) from severe fibrosis (F3, F4) in CHC patients. 25 Research by Bihrer et al enrolled 68 therapy‐naive German CHC patients who underwent liver biopsy and 19 healthy controls and the results were accordant with the research by Omran et al. 26 The expression of serum microRNA122 was elevated in CHC patients than healthy controls and serum microRNA122 has no correlation with liver fibrosis stages in CHC patients. 26 Similar results were gained in another research by Nakamura et al. 27 The research by Nakamura et al also enrolled 91 Japanese CHB patients who received liver biopsy and 23 healthy controls. 27 Results showed the expression of serum microRNA122 was much higher in CHB patients than that of healthy controls. 27 Further results showed the serum microRNA122 was down‐regulated in CHB patients with severe fibrosis (F3, F4) compared with CHB patients with mild or moderate fibrosis (F1 or F2). 27 ROC analysis showed the AUC of serum microRNA122 to predict severe fibrosis in CHB patients was 0.668. 27 That is to say serum microRNA122 could differentiate mild or moderate fibrosis from healthy controls and also distinguish differentiate mild or moderate fibrosis from severe fibrosis in CHB patients. However, it is hard for serum microRNA122 to distinguish healthy people from CHB patients with severe fibrosis. 27 Research by Hegazy et al enrolled 120 Egyptian patients with metabolic‐associated fatty liver disease (MAFLD), who underwent Fibro‐scan examination to stage liver fibrosis. 28 Results showed serum microRNA122 was up‐regulated in MAFLD patients with fibrosis than controls. 28 However, the expression of serum microRNA122 decreased gradually from patients with mild fibrosis (F1) to patients with severe fibrosis (F4). 28 The expression pattern of serum microRNA122 was similar to that in CHB patients. 28 In conclusion, serum microRNA122 could be a potential non‐invasive marker for early fibrosis diagnosis and could be used to distinguish fibrosis stages among patients with liver fibrosis.
2.3. Let‐7
It has been reported that several let‐7 family numbers were correlated with the progression of liver fibrosis in HCV‐infected patients. 29 Research by Matsuura et al enrolled 84 Japanese CHC patients who underwent liver biopsy. 30 Results showed serum let‐7a‐5p expression was significantly lower in patients with severe fibrosis(F4) than in those with mild and moderate fibrosis (F1–F3). 30 ROC analysis showed the AUC of serum let‐7a‐5p to differentiate CHC patients with liver cirrhosis from those with fibrosis was 0.892. 30 The sensitivity and specificity were 92% and 80%, respectively. 30 These results indicated serum let‐7a‐5p could be a potential marker to distinguish CHC patients with severe fibrosis from those with mild and moderate fibrosis. 30 Another research by Cai et al enrolled 163 schistosomiasis japonica patients with liver fibrosis. 31 The liver fibrosis was staged by ultrasound methods. Results showed the expression of serum let‐7a‐5p and let‐7d‐5p were negatively correlated with fibrosis stages. 31 The expressions of let‐7a‐5p and let‐7d‐5p were significantly higher in patients with mild fibrosis (Grade0 and 1) than in those with moderate or severe fibrosis (Grade2 and 3). 31 ROC analysis showed the AUC of let‐7a‐5p and let‐7d‐5p to distinguish schistosomiasis japonica patients with mild fibrosis (Grade0 and 1) from those with severe fibrosis (Grade2 and 3) were 0.6598 and 0.6270, respectively. 31 In conclusion, these results indicated that let‐7 (let‐7a‐5p and let‐7d‐5p) could serve as a potential marker to differentiate severe fibrosis from mild fibrosis in CHC and schistosomiasis japonica‐infected patients.
2.4. MicroRNA214
MicroRNA array analysis showed microRNA214 was up‐regulated during hepatic stellate cell (HSC) activation. 32 MicroRNA214 could promote HSC activation and liver fibrosis through inhibiting suppressors‐of‐fused homolog (Sufu) expression. 32 The expression of microRNA214 was higher in patients with liver cirrhosis than in those without cirrhosis. 32 Research by Yoneyama et al enrolled 54 Japanese Biliary atresia (BA) patients with different fibrosis by liver biopsy, among whom the serum of 28 BA patients was also collected. 33 Results showed the expression of microRNA214 was significantly higher in BA patients with severe fibrosis (F3–F4) than in those with mild fibrosis (F0–F2). 33 ROC analysis showed the AUC of serum microRNA214 to distinguish BA patients with severe fibrosis from those with mild fibrosis was 0.805 (95%CI:0.591–0.921). 33 The sensitivity and specificity were 58.8% and 90.9%,respectively. 33 These results showed serum microRNA214 could be a potential marker to distinguish BA patients with severe liver fibrosis from those with mild liver fibrosis.
2.5. MicroRNA155
It has been shown that microRNA155 was closely related to hepatic cancer and hepatitis. 34 , 35 , 36 Several studies also show that microRNA155 plays a promoting role in renal, cardiac, and liver fibrosis. 37 , 38 , 39 Research by Niu et al enrolled 94 patients with cirrhosis and 50 healthy volunteers. 40 The expression of microRNA155 in exosomes from the plasma of patients and healthy controls were detected by quantitative real‐time polymerase chain reaction (qPCR) method. 40 Results showed the expression of microRNA155 in exosomes was higher in patients with liver cirrhosis than that of healthy controls. 40 ROC analysis showed the AUC of microRNA155 to distinguish liver cirrhosis from healthy controls was 0.971. 40 The sensitivity and specificity were 93.62% and 94%, respectively. 40 Another research by Shaker et al enrolled 145 Egyptian CHC patients who underwent liver biopsy. 41 Results showed the expression of microRNA155 was not significantly different among CHC patients with different fibrosis stages. 41 These results showed microRNA155 may be a potential marker for the diagnosis of liver cirrhosis. However, it is hard for serum microRNA155 to stage liver fibrosis in CHC patients. It also needs further research to verify its potential use for the diagnosis of early liver fibrosis.
2.6. MicroRNA29
Several studies have shown that microRNA29 plays an important role in liver fibrosis and cardiac fibrosis, lung fibrosis, systemic sclerosis, and keloid. 42 , 43 MicroRNA29 played a protective role in liver injury and fibrosis. 44 , 45 Research by Roderburg et al showed microRNA29 was down‐regulated in fibrotic liver tissues in mice and humans. 46 Sixty‐seven German patients with chronic liver diseases at different stages and 17 healthy volunteers were enrolled in this study. 46 Results showed the expression of microRNA29a in serum was much lower in patients with liver fibrosis than that of healthy controls. 46 Further analysis showed the serum microRNA29a expression was higher in patients with Child A stage than that of patients with Child B and C stages. 46 There is a significantly positive correlation between the expression of serum microRNA29a and MELD‐score. 46 ROC analysis showed the AUC of serum microRNA29a to distinguish patients with liver fibrosis and healthy people was 0.838. 46 Another research by Appourchaux et al enrolled 83 CHB and 72 CHC patients in France. 47 Results showed that the expression of serum microRNA29a was much lower in patients with severe fibrosis (F3, F4) than those with early or mild fibrosis (F0, F1, F2). 47 These results showed serum microRNA29 could be a potential non‐invasive marker for the diagnostic and stage of liver fibrosis and cirrhosis.
2.7. MicroRNA‐1373g‐3p
MicroRNA‐1273 g‐3p was a member of microRNA‐1273 family which was newly discovered in 2011. 48 Research by Niu et al showed up‐regulation of microRNA‐1273 could increase the expression of smooth muscle actin alpha (a‐SMA), alpha1 chains of type I collagen (Col1A1), and reduce the apoptosis of HSC. 49 Sixty‐one Chinese CHC patients who underwent biopsy and 20 healthy volunteers were enrolled in this study. 49 The expression of microRNA‐1273 g‐3p in serum of patients and healthy controls was detected by the qPCR method. 49 Results showed the expression of serum microRNA‐1273 g‐3p was much higher in CHC patients with moderate to severe fibrosis (F2–F4) than that in those with mild fibrosis (F < 2). 49 ROC analysis showed the AUC of serum microRNA‐1273 g‐3p to predict moderate to severe fibrosis among CHC patients with fibrosis was 0.790 (95% CI:0.675–0.904). 49 Another research by Nan et al enrolled 112 Chinese CHC patients who underwent biopsy. 50 The expression of serum microRNA‐1273g‐3p was positively correlated with fibrosis stages of CHC patients. ROC analysis showed the AUC of serum microRNA‐1273g‐3p to predict the early or mild fibrosis (F = 1) among CHC patients with fibrosis was 0.841 (95% CI:0.761–0.921). 50 The sensitivity and specificity were 85% and 69%, respectively. 50 Further analysis showed the AUC for serum microRNA‐1273g‐3p to distinguish CHC patients with severe fibrosis (F4) from patients with mild to moderate fibrosis was 0.933 (95% CI:0.874–0.993). 50 The sensitivity and specificity were 80% and 95%, respectively. 50 These results indicated serum microRNA‐1273g‐3p could be a potential marker to stage liver fibrosis in CHC patients. It still needs further research to confirm the capacity of serum microRNA‐1273g‐3p to diagnose early liver fibrosis.
2.8. MicroRNA34a
Several studies have shown that microRNA34a plays a promoting role in liver fibrosis through activation of HSC cells and inducing hepatocytes apoptosis. 51 , 52 , 53 Research by Li et al enrolled 41 Chinese CHC patients and 18 healthy volunteers. 54 The expression of microRNA34a was detected by the qPCR method. 54 Results showed the expression of serum microRNA34a was higher in CHC patients than that of healthy controls. 54 There is no significant difference between CHC patients with no fibrosis (F0) and healthy controls. 54 The expression of serum microRNA34a in CHC patients with mild fibrosis (F1, F2) was significantly higher than that of healthy participants. 54 The expression of serum microRNA34a in CHC patients with severe fibrosis (F3, F4) was significantly different from that in healthy controls, CHC patients with no fibrosis(F0), and CHC patients with mild fibrosis (F1, F2). 54 ROC analysis showed the AUC of serum microRNA34a to differentiate CHC patients with mild fibrosis from healthy controls was 0.8274 (95% CI:0.681–0.973). 54 The sensitivity and specificity were 71.4% and 83.3%, respectively. 54 The AUC of serum microRNA34a to distinguish CHC patients with severe fibrosis (F3, F4) from healthy controls was 0.8904 (95% CI:0.789–0.992). 54 The sensitivity and specificity were 77.8% and 88.3%, respectively. 54 These results showed serum microRNA34a could be a potential marker to diagnose early or mild fibrosis and severe fibrosis in CHC patients. However, it is needed to confirm the proficiency of serum microRNA34a in a big cohort. It is still unknown whether serum micro34a could stage liver fibrosis or not.
2.9. MicroRNA17
Several studies have shown that microRNA17 played a promoting role in renal fibrosis, cystic fibrosis, and liver fibrosis. 55 , 56 , 57 Research by Li et al enrolled 200 Chinese CHB patients with liver fibrosis who underwent liver biopsy and 50 healthy participants. 58 The CHB patients were staged into four different stages::S0‐1 (mild fibrosis), S2 (pronounced fibrosis), S3 (advanced fibrosis), and S4 (cirrhosis). 58 The expression of serum microRNA17 was detected in the serum of patients and controls by qPCR. 58 Results showed the expression of serum microRNA17 was much higher in patients with liver fibrosis than that of healthy controls. 58 However, the expression of serum microRNA17 decreased gradually from mild fibrosis (S0–S1) to cirrhosis (S4). 58 ROC analysis showed the AUC of serum microRNA17 to distinguish CHB patients with mild fibrosis (S0‐S1) from healthy controls was 0.685 (95% CI: 0.5813–0.7894). 58 The AUC of serum microRNA17 to differentiate CHB patients with S2 fibrosis from healthy controls was 0.6716 (95% CI: 0.5622–0.781). 58 The AUC of microRNA17 to differentiate CHB patients with S3 fibrosis and S4 fibrosis from healthy controls was 0.7932 and 0.9169, respectively. 58 These results indicated serum microRNA17 could be a potential non‐invasive marker for the diagnosis of early and severe fibrosis in CHB patients. However, the potential of microRNA17 to stage liver fibrosis should be further researched.
2.10. MicroRNA20a
It has been reported that microRNA20a played an important role in liver fibrosis through PTEN/PI3K/Akt pathway. 59 To further research the role of microRNA20a in liver diseases, 44 HCV‐infected patients, 20 non‐HCV patients with liver fibrosis diagnosed by liver biopsy, and 22 healthy volunteers in America were enrolled in the study by Shrivastava et al. 60 MicroRNA20a was highly expressed in the serum of HCV‐infected patients with fibrosis as compared with non‐HCV‐related patients with fibrosis and healthy volunteers. 60 The expression of serum microRNA20a gradually increased from early fibrosis (F0–F2) to late fibrosis stage (F3–F4) in HCV‐infected patients. 60 ROC analysis showed microRNA20a had an AUC of 0.704 (95%CI: 0.571–0.836) with a sensitivity of 61.4% and specificity of 81.8% in discriminating HCV‐infected patients with fibrosis from healthy controls. 60 The AUC of serum microRNA20a to differentiate non‐HCV‐related patients with fibrosis from HCV‐infected patients with fibrosis was 0.679 (95%CI: 0.542–0.817). 60 These results showed serum microRNA20a could be a potential marker for the diagnosis of early fibrosis and staging liver fibrosis in HCV‐infected patients. However, it is still needed to confirm the result in a big cohort.
2.11. MicroRNA138
Studies have shown that microRNA138 played an inhibitory role in lung fibrosis through YAP‐Twist axis and regulating ZEB2. 61 , 62 To further research the potential of serum microRNA138 as a non‐invasive marker for fibrosis, 36 Egyptian CHC patients with early fibrosis (F1, F2), 35 Egyptian CHC patients with late fibrosis (F3, F4), and 40 healthy participants were enrolled in the study by Ahwany et al. 63 The fibrosis stage was divided by liver biopsy according to the Metavir scoring system. 63 The expression of serum microRNA138 in CHC patients and healthy controls was detected by the qPCR method. 63 Results showed serum microRNA138 was highly expressed in CHC patients with fibrosis as compared with that of healthy controls. 63 The expression of microRNA138 was higher in CHC patients with late fibrosis than that of CHC patients with early fibrosis. 63 ROC analysis showed the AUC of serum microRNA138 to differentiate CHC patients with early fibrosis from healthy controls was 0.866 (95%CI: 0.756–0.941), with 89.3% sensitivity and 71.4% specificity. 63 Serum microRNA138 could gain an AUC of 0.924 for discriminating CHC patients with late fibrosis from healthy controls. 63 These results indicated serum microRNA138 could be a potential non‐invasive marker for the diagnosis of early and late fibrosis in CHC patients. 63 However, it still needs further research to study whether serum microRNA138 could stage liver fibrosis in CHC patients and other liver diseases or not.
2.12. Other microRNAs
The expression of many serum microRNAs was dis‐regulated during the liver fibrosis process in many liver diseases. Research by Cai et al enrolled 163 Australian patients with schistosomiasis and the fibrosis grade in patients was divided through ultrasonography. 31 Results showed the expression of serum microRNA150‐5p and microRNA146a‐5p was significantly correlated with fibrosis grade. 31 The expression of serum microRNA150‐5p and microRNA146a‐5p was lower in patients with severe fibrosis (grade 2 and 3) than that of patients with mild fibrosis (grade 0 and 1). 31 ROC analysis showed the AUC of serum microRNA150‐5p and microRNA146a‐5p to distinguish patients with mild fibrosis from those with severe fibrosis was 0.6838 and 0.6575, respectively. 31 The AUC of serum microRNA150‐5p and microRNA146a‐5p together to differentiate patients with mild fibrosis from those with severe fibrosis could be 0.6950. 31 These results indicated that serum microRNA150‐5p and microRNA146a‐5p could be potential non‐invasive markers to separate schistosomiasis‐infected patients with mild fibrosis from those with severe fibrosis. Another research by Cai et al enrolled 104 Australian patients with schistosomiasis and the expression of microRNAs in serum exosomes of patients was detected by the qPCR method. 64 Results showed microRNA146a‐5p and microRNA532‐5p in exosomes were significantly correlated with fibrosis grades. 64 The expression of microRNA146a‐5p and microRNA532‐5p was lower in patients with no fibrosis (grade: 0) than that of patients with fibrosis (grade: 1–3). 64 ROC analysis showed the AUC of exosomal microRNA146a‐5p and microRNA532‐5p to distinguish patients with no fibrosis and patients with fibrosis was 0.6315 and 0.6884, respectively. 64 The AUC of combing exosomal microRNA146a‐5p and microRNA532‐5p to predict patients with fibrosis could be 0.6962. 64 These results showed that exosomal microRNA146a‐5p and microRNA532‐5p could be a potential non‐invasive marker to predict liver fibrosis in patients with schistosomiasis. Research by Bao et al enrolled 123 Chinese treatment‐naive CHB patients who underwent biopsy. 18 Results showed the expression of serum microRNA29a, 29b, 29c, 143, 223, 21, and 374 was lower in CHB patients with late liver fibrosis (S3–S4) than that of those with early liver fibrosis (S1‐S2). 18 ROC analysis showed the AUC of microRNA29a, 29b, 29c, 143, 223, 21 and 374 to differentiate CHB patients with early fibrosis from those with late fibrosis was 0.8030, 0.7237, 0.8121, 0.8123, 0.7806, 0.7589, and 0.7282, respectively. 18 The AUC of the panel of microRNA29a, microRNA143, microRNA223, and platelet count(PLT) to distinguish CHB patients with early fibrosis from those with late fibrosis could be 0.936 which was superior to aspartate aminotransferase to platelet patio index (APRI) and fibrosis 4 score (FIB‐4). 18 These results showed serum microRNAs could be potential markers for fibrosis stage in CHB patients. Research by Appourchaux et al enrolled 102 French CHB patients and 178 CHC patients who underwent biopsy. 47 Results showed the expression of microRNA29a, 92a, and 122 were significantly down‐regulated and microRNA146a and 222 were significantly up‐regulated in CHB patients with late fibrosis (F3–F4) than those with mild fibrosis (F1–F2). 47 However, the expression of these microRNAs was not significantly different between CHC patients with mild and late fibrosis. 47 ROC analysis showed the AUC of the panel of serum microRNA122, micrRNA222, platelet count, and alkaline phosphatase(ALP) to distinguish the CHB patients with late fibrosis from those with early fibrosis was 0.86 which was superior to APRI and FIB‐4. 47 These results showed a combination of serum microRNAs and baseline predictors could be non‐invasive markers for fibrosis stage in CHB patients. Research by Shaker et al enrolled 145 Egyptian HCV‐infected patients who underwent biopsy. 41 Results showed serum microRNA122 was significantly down‐regulated and serum microRNA203a and microRNA223 were significantly up‐regulated in patients with moderate to severe fibrosis (Fγ2) as compared with patients with no to mild fibrosis (F0–F1). 41 The expression of serum microRNA126, 129, 203a, 223 was higher in patients with fibrosis(Fγ3) and cirrhosis (F = 4) than in those with fibrosis F0–F2 and F0–F3, respectively. 41 ROC analysis showed the AUC of the panel of microRNA129, microRNA223, aminotransferase aspartate(AST), and platelet count to predict patients with fibrosis Fγ2, Fγ3, and F = 4 among CHC patients could be 0.785, 0.91, and 0.96, respectively, which were superior to APRI and FIB‐4. 41 These results showed the model of serum microRNAs and other related liver markers could be a potential non‐invasive marker for fibrosis stage in CHC patients.
3. LNCRNAs
Long non‐coding RNAs (lncRNAs) are a class of more than 200 nt non‐coding RNA. 65 LncRNAs could serve as ceRNA to regulate the roles of microRNA to participate the physiological and pathological progress. 65 LncRNA plays an important role in the development and progression of many diseases such as cancer, diabetes, cardiovascular diseases, and so on. 65 , 66 The role of lncRNAs on liver diseases has been researched. 65 , 66 The role of serum lncRNAs on the diagnosis of liver fibrosis was summarized (Table 2).
TABLE 2.
Serum lncRNAs and circRNAs for diagnosis and stage of liver fibrosis
| Number | LncRNA or CircRNAs | Diseases | Country | Fibrosis diagnostic method | Expression/source | Cohort | AUC for fibrosis | AUC for early fibrosis | AUC for late fibrosis | AUC for stage fibrosis | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | lincRNA‐p21 | CHB | China | Liver biopsy | Down/serum | 417 | 0.854 | 0.760 | 0.935 | 0.875‐0.954 | 71 |
| 2 | Scarna10 | Liver fibrosis | China | Liver biopsy | Up/serum | 38 | NT | NT | NT | NT | 74 |
| 3 | MEG3 | CHB | China | Liver biopsy | Down/serum | 100 | 0.8844 | 0.5237 | 0.9395 | 0.7861‐0.8281 | 85 |
| 4 | GAS5 | CHB | China | Liver biopsy | Down/serum | 518 | 0.993 | NT | NT | NT | 96 |
| NAFLD | Korea | Liver biopsy | Up/plasma | 51 | NT | NT | NT | NT | 97 | ||
| 5 | RABGAP1L‐DT‐206 | NAFLD | Egypt | Transient elastography | Up/serum | 100 | 0.844 | NT | NT | 0.944 | 98 |
| 6 | H19 | Biliary atresia | China | surgery | Up/exosomes | 16 | NT | NT | NT | NT | 108 |
| 7 | MALAT1 | CHB | China | Liver biopsy | Up/serum | 151 | 0.901 | NT | NT | NT | 112 |
| 8 | TGFB2‐OT1 | NAFLD | Italy | Liver biopsy | Up/serum | 63 and 50 | NT | NT | NT | 0.786‐0.797 | 113 |
| 9 | CircMTO1 | CHB | China | Liver biopsy | Down/serum | 360 | 0.914 | 0.847 | 0.962 | 0.762‐0,880 | 115 |
Abbreviations: CHB, chronic HBV hepatitis; CHC, chronic HCV hepatitis; NAFLD, Nonalcoholic fatty liver disease; NT, not mentioned.
3.1. LincRNA‐p21
Long intergenic non‐coding RNA‐p21 (lincRNA‐p21) was about 3 kb long and located approximately 15 kb upstream of cycle regulator gene p21/Cdkn1a. 67 Research demonstrated that lincRNA‐p21 could regulate cell proliferation, cycle, apoptosis, DNA damage response, metabolism, and reprogramming. 67 , 68 , 69 , 70 Research by Yu et al showed that the level of lincRNA‐p21 was lower in the serum of CHB patients than in healthy controls. 71 The study enrolled 417 therapy‐naive patients with CHB and 363 healthy controls, most of them were Chinese people. 71 All CHB patients underwent liver biopsy to divide into different fibrosis stages (F0 = no fibrosis, F6 = cirrhosis) according to the Ishak scoring system. 71 The serum level of lincRNA‐p21 was negatively correlated with fibrosis stages. 71 Further receiver operating characteristic curve (ROC) analysis showed serum lincRNA‐p21 could distinguish CHB patients with fibrosis from healthy people, the area under the ROC curve (AUC) was 0.854 (95% confidence interval [CI]: 0.805–0.894) with 100% sensitivity and 70% specificity, when the cutoff value was 3.65. 71 ROC analysis showed lincRNA‐p21 could differentiate CHB patients with low fibrosis scores (F0–F1 stage) from healthy controls and the AUC was 0.760 (95% CI: 0.682–0.826). 71 The AUC of serum lincRNA‐p21 to differentiate CHB patients with medium fibrosis (F2–F4 stages) from healthy controls was 0.856 (95% CI: 0.801–0.901) with 100% sensitivity and 73.3% specificity. 71 The AUC of serum lincRNA‐p21 to differentiate CHB patients with high fibrosis (F5–F6 stages) from healthy controls was 0.935 (95% CI: 0.882–0.969) with 100% sensitivity and 77.5% specificity. 71 LincRNA‐p21 could also discriminate CHB patients with different fibrosis scores. 71 The AUC of lincRNA‐p21 to differentiate CHB patients with medium fibrosis scores from patients with low fibrosis scores was 0.875 (95% CI: 0.800–0.930) with 70.9% sensitivity and 92.3% specificity. 71 The AUC of serum lincRNA‐p21 was 0.954 (95% CI: 0.859–0.993) with 81.4% sensitivity and 96.1% specificity in distinguishing CHB patients with high fibrosis scores from those with medium scores. 71 These results were very meaningful and they indicated serum lincRNA‐p21 could be a potential non‐invasive marker for the early diagnosis of liver fibrosis. They also indicated that lincRNA‐p21 could be used as a potential marker to stage fibrosis in CHB patients. LincRNA‐p21 showed better sensitivity in differentiating CHB patients with different fibrosis scores from healthy people than that in staging liver fibrosis in CHB patients. The specificity of lincRNA‐p21 was better in staging liver fibrosis in CHB patients than that in differentiating CHB patients with liver fibrosis from healthy people. Serum lincRNA‐p21 had no significant correlation with HBV replication and liver function. 71 But serum lincRNA‐p21 was negatively correlated with fibrosis markers:α‐smooth muscle actin(α‐SMA) and Collagen Type I Alpha 1 Chain (Col1A1). 71 These results further showed lincRNA‐p21 could be a potential marker for liver fibrosis. A previous study demonstrated lincRNA‐p21 could inhibit hepatic stellate cell (HSC) activation. 72 All these researches demonstrated that lincRNA‐p21 played an important role in fibrosis. However, another research showed the expression of serum lincRNA‐p21 was higher in patients with CHB, HBV cirrhosis, CHC, or alcoholic liver disease than that of healthy controls. 73 The result was inconsistent with the former research by Yu et al. The reason may be due to the difference of cohort size, sample storage condition and time, case selection, and so on. Further research is needed to confirm that lincRNA‐p21 could be a marker for liver fibrosis by enrolling more cases and standardizing sample storage condition and time.
3.2. Scarna10
Scarna10 was a 300 nt long lncRNA and up‐regulated in mouse fibrosis livers according to microarray analysis. 74 Further experiments showed the expression of scarna10 was up‐regulated in fibrosis mouse models treated with CCl4 or bile duct ligation (BDL). 74 The expression of scarna10 was higher in human livers with fibrosis than in healthy controls, gradually rose from patients with no fibrosis (F0) to those with severe fibrosis (F4) and was positively correlated with Col1A1, not ALT, AST, or α‐SMA. 74 The serum scarna10 in 38 patients with fibrosis was higher than that of 35 healthy people. 74 The expression of scarna10 in the serum of 45 humans with cirrhosis was higher than that of humans with fibrosis. 74 These results indicated scarna10 could be a potential non‐invasive marker for liver fibrosis. However, the diagnostic performance of scarna10 for liver fibrosis has not been researched. It is also needed to explore the potential application value of scarna10 in different types of liver diseases.
3.3. MEG3
Maternally expressed gene 3 (MEG3) was a 1.6 kb long lncRNA. 75 MEG3 was expressed in many tissues and could act as a tumor suppressor. 75 Its loss of expression has been observed in different types of cancer such as liver cancer, lung cancer, gastric cancer, and so on. 76 , 77 , 78 Research showed MEG3 played an important role in fibrosis diseases, such as liver fibrosis, pulmonary fibrosis, renal fibrosis, and cardiac fibrosis. 79 , 80 , 81 , 82 MEG3 played an inhibitory role in the activation of HSC and the expression of MEG3 decreased both in vivo and in vitro during fibrosis progression. 83 , 84 These results indicated that MEG3 might be a potential marker for liver fibrosis. Research by Chen et al showed serum MEG3 expression was lower in CHB patients than that in healthy controls. 85 100 Chinese CHB patients and 80 healthy controls were enrolled in the study. 85 CHB patients were divided into mild fibrosis (F0–F1), middle‐level fibrosis (F2–F4), and high‐level fibrosis (F5–F6) through liver biopsy examination based on ISHAK method (F0 = no fibrosis, F6 = cirrhosis). 85 Results showed serum MEG3 expression was negatively correlated with the fibrosis degree. 85 The AUC of serum MEG3 to distinguish CHB patients with fibrosis from healthy people was 0.8844 and cutoff was 5.112. 85 The AUC of serum MEG3 to differentiate CHB patients with low‐level fibrosis from healthy people was 0.5237 and cutoff value was 2.988. 85 The AUC of serum MEG3 to differentiate CHB patients with middle and high‐level fibrosis from healthy control were 0.7085 and 0.9395, respectively. 85 These results indicated that serum MEG3 exerted better diagnostic performance in differentiating CHB patients with middle and high‐level fibrosis from healthy controls than that in distinguishing CHB patients with low‐level fibrosis from healthy participants. The diagnostic performance of serum MEG3 was not good enough to differentiate CHB patients with low‐level fibrosis from healthy controls. The reason may be that patients with no fibrosis (F0) accounted for almost 50% of the patients with mild fibrosis (F0, F1). The AUC of serum MEG3 to distinguish CHB patients with medium fibrosis from those with mild fibrosis was 0.8281. 85 The AUC of serum MEG3 to differentiate CHB patients with high fibrosis from those with medium fibrosis was 0.7861. 85 These results indicated serum MEG3 could be used to distinguish fibrosis stages. Further experiments showed serum MEG3 was negatively correlated with α‐SMA and Col1A1. 85 However, serum MEG3 has no significant correlation with HBV DNA, ALT, bilirubin, or albumin level. 85 Another study enrolled 12 CHB patients with mild fibrosis (F < 2), 13 patients with moderate to severe fibrosis (2 < F < 4), and 25 healthy people and the fibrosis stages of patients were based on the 4 factors (FIB‐4). 86 The expression of serum MEG3 was lower in patients with liver fibrosis than in healthy controls. 86 The serum MEG3 expression was lower in patients with moderate to severe fibrosis than that in patients with mild fibrosis. 86 These results were consistent with the research by Chen et al. All the above research indicated serum MEG3 could be a potential marker for diagnosis and stage of liver fibrosis in CHB patients.
3.4. GAS5
Growth arrest‐specific transcript 5 (GAS5) could act as a tumor suppressor and is often lowly expressed in different types of cancer. 87 , 88 Research has shown that GAS5 played an inhibitory role in organ fibrosis such as liver fibrosis, renal fibrosis, cardiac fibrosis, oral submucous fibrosis, and so on and the expression of GAS5 was down‐regulated in fibrosis tissues. 89 , 90 , 91 , 92 Previous studies have demonstrated that the expression of GAS5 was reduced in mouse and human fibrosis livers and activated HSC, and could inhibit liver fibrosis. 89 , 93 , 94 The study by Guo et al enrolled 518 CHB patients who underwent liver biopsy and 420 healthy controls in China and the results showed the expression of serum GAS5 was lower in CHB patients than in healthy controls. 95 ROC analysis showed the serum GAS5 could differentiate CHB patients with fibrosis from healthy people with an AUC of 0.993 (95% confidence interval [CI]: 0.972 to 0.992). 95 The cutoff value was 2.88, which was ∆Ct(Ct target‐Ct reference). 95 The sensitivity and specificity were 93.1% and 100%, respectively. 95 Serum GAS5 exerted good diagnostic performance to distinguish CHB patients with fibrosis from healthy people. The expression of serum GAS5 gradually decreased from CHB patients with mild fibrosis (F0–F1) to medium fibrosis (F2–F4) and severe fibrosis (F5–F6). 95 These results indicated GAS5 could be used to stage liver fibrosis. Further analysis showed the expression of serum GAS5 decreased in a HAI score‐dependent manner. 95 The expression of serum GAS5 was lower in CHB patients with elevated ALT than that of normal ALT. 95 The expression of serum GAS5 was not significantly different between hepatitis B virus e antigen (HBeAg) positive and negative CHB patients. 95 These results indicated the expression of serum GAS5 might be correlated with neco‐inflammation and liver damage of liver fibrosis. Another study enrolled 51 patients with nonalcoholic fatty liver disease (NAFLD) who underwent liver biopsy in Korea. 96 The results showed that plasma GAS5 expression was higher in patients with advanced fibrosis than in those without. 96 However, the expression of plasma GAS5 was lower in patients with cirrhosis than in those with fibrosis. 96 The result disagreed with the research by Guo et al. This may be due to the different amount of enrolled cases, patients from different countries, and different etiology. In conclusion, serum GAS5 was a potential marker for liver fibrosis in CHB patients.
3.5. RABGAP1L‐DT‐206
It is less known about the role of lncRNA‐RABGAP1L‐DT‐206 in liver fibrosis. Research by Albadawy et al showed the expression of serum RABGAP1L‐DT‐206 was dysregulated in NASH/NAFLD patients. 97 A total of 200 participants in Egypt were enrolled in this study. 97 There were 100 healthy controls, 60 NASH/NAFLD patients without advanced fibrosis, and 40 patients with advanced fibrosis. 97 The fibrosis staging was based on transient elastography (Fibroscan). 97 Research showed the serum lncRNA‐RABGAP1L‐DT‐206 expression was higher in NASH/NAFLD patients than that of healthy controls. 97 ROC analysis showed the AUC of serum RABGAP1L‐DT‐206 to differentiate NASH patients with fibrosis from healthy controls was 0.844 (95% confidence interval [CI]: 0.82–0.905). 97 The cutoff value which was ∆Ct(Ct target‐Ct reference) was 4.8. 97 The sensitivity and specificity were 81% and 83%, respectively. 97 Further analysis showed the AUC of serum RABGAP1L‐DT‐206 to distinguish NASH/NAFLD patients with advanced fibrosis (F3–F4) from those with mild fibrosis (F0–F2) was 0.944 (95% confidence interval [CI]: 0.869–1), when the cutoff value was 3.4. 97 The sensitivity and specificity were 100% and 79%, respectively. 97 The RABGAP1L‐DT‐206 may influence liver inflammation through a stimulator of interferon genes (STING) signaling pathway. 97 These results indicated serum RABGAP1L‐DT‐206 could be a potential non‐invasive marker for the diagnosis and stage of liver fibrosis in NASH/NAFLD patients.
3.6. H19
LncRNA H19 was a long non‐coding RNA with 2.3 kb length. 98 Research has demonstrated that H19 played an important role in liver fibrosis, lung fibrosis, renal fibrosis, cardiac fibrosis, and oral submucous fibrosis. 99 , 100 , 101 , 102 , 103 Several researches further demonstrated H19 played a promoting role in liver fibrosis and the expression of H19 increased in fibrotic liver tissues. 99 , 104 , 105 Research by Xiao et al showed the expression of H19 was higher in liver tissues and serum exosomes of biliary atresia (BA) patients who underwent liver surgery than in healthy controls in China. 106 The exosomes were extracted from serum of 8 BA patients with mild fibrosis (F1, F2), 8 BA patients with severe fibrosis (F3, F4), and age‐matched controls. 106 Results showed that the expression of H19 in serum exosomes was higher in BA patients than in healthy controls. 106 The expression of H19 was higher in BA patients with severe fibrosis than those with mild fibrosis. 106 These results showed that H19 could be a potential marker for the diagnosis of liver fibrosis in BA patients. However, the diagnostic performance of H19 in liver fibrosis among patients with BA and other liver diseases needed to be further researched.
3.7. MALAT1
It has been shown that metastasis‐associated lung adenocarcinoma transcript 1 (MALAT1) played an important and promoting role in liver fibrosis. 107 , 108 , 109 151 CHB patients with liver fibrosis who underwent liver biopsy in China were enrolled in the research by Wang et al. 110 Results showed the expression of serum MALAT1 was significantly higher in CHB patients with liver fibrosis than that of healthy controls. 110 ROC analysis showed the AUC of serum MALAT1 to differentiate CHB patients with fibrosis from healthy controls was 0.901 (95% confidence interval [CI]: 0.869–1). 110 The cutoff value which was ∆Ct(Ct target‐Ct reference) was 2.81. 110 The sensitivity and specificity were 0.781 and 0.968, respectively. 110 These results showed serum MALAT1 could be a potential marker for the diagnosis of liver fibrosis in CHB patients. Further results showed the serum MALAT1 expression gradually increased with the fibrosis stage. 110 This indicated serum MALAT1 could help to stage liver fibrosis. However, the diagnostic performance of serum MALAT1 to stage liver fibrosis was not exerted. Further analysis showed the expression of serum MALAT1 was negatively correlated with inflammation factors: tumor necrosis factorα (TNFα), interleukin‐6 (IL‐6), and C‐reactive protein (CRP). Serum MALAT1 expression was positively correlated with markers of fibrosis: hyaluronic acid (HA), precollagen III (PCIII), collagen IV (C‐IV), and laminin (LN). These results indicated MALAT1 might exert its role by influencing inflammation and fibrosis of liver. In a word, MALAT1 could be a potential non‐invasive marker to diagnose liver fibrosis in CHB patients.
3.8. TGFB2‐OT1
Seventy‐one NAFLD patients diagnosed by liver biopsy and 28 controls in Italy were enrolled in a study by Mauro et al. 111 Microarray analysis showed the expression of lncRNA TGFB2‐OT1 was up‐regulated in patients with severe liver fibrosis (F3–F4) versus those with mild fibrosis. 111 The up‐regulated expression of TGFB2‐OT1 was further validated in an independent internal cohort which included 63 NAFLD patients and 25 controls, and an external cohort including 50 NAFLD patients. 111 Further analysis showed serum TGFB2‐OT1 expression was positively correlated with FIB‐4, liver stiffness measurements, Kleiner lobular inflammation, and fibrosis scores. 111 ROC analysis showed the AUC of serum TGFB2‐OT1 in internal and external cohort for distinguishing NAFLD patients with severe fibrosis (F3–F4) from those with mild fibrosis were 0.797 (95%CI: 0.697–0.981) and 0.786 (95%CI: 0.623–0.950), respectively. 111 The sensitivity was 65% and 62.5%, respectively. 111 The specificity was 81.3% and 94.4%, respectively. 111 Serum TGFB2‐OT1 gained a similar diagnostic performance in different cohorts. The AUC for serum TGFB2‐OT1 plus FIB‐4, and TGFB2‐OT1 plus Fibroscan to differentiate CHB patients with severe fibrosis (F3–F4) from those with mild fibrosis could be 0.891 and 0.892, respectively. These results indicated serum lncRNA TGFB2‐OT1 could be a potential non‐invasive marker for liver fibrosis staging in NAFLD patients.
4. CIRCRNAs
4.1. CircMTO1
CircMTO1 (hsa_circ_0007874) was a circular RNA (circRNA) which was derived from the mitochondrial tRNA translation optimization 1 (MTO1) gene. 112 CircMTO1 was down‐regulated in hepatocellular carcinoma (HCC) tissues and played an inhibitory role in HCC progression. 112 To research serum circRNAs as markers for liver fibrosis, research by Zheng et al enrolled 360 Chinese treatment‐naive CHB patients who underwent liver biopsy and 360 healthy controls. 113 The expression of serum circMTO1 was detected by the qPCR method. 113 Results showed serum circMTO1 was significantly down‐regulated in CHB patients as compared with healthy controls. 109 The expression of serum circMTO1 was significantly negatively correlated with fibrosis markers of Col1A1 and α‐SMA. 113 The CHB patients were divided into three groups: mild fibrosis (F0–F1), moderate fibrosis (F2–F4), and severe fibrosis (F5–F6). 113 The expression of serum circMTO1 was gradually down‐regulated from CHB patients with mild fibrosis to those with severe fibrosis. 113 The expression of serum circMTO1 was also gradually down‐regulated in CHB patients with histological activity index (HAI) score increasing. 113 The ROC analysis showed the AUC of serum circMTO1 to discriminate CHB patients from healthy people, CHB patients with mild fibrosis from healthy people, CHB patients with moderate fibrosis from healthy people, CHB patients with severe fibrosis from healthy people, CHB patients with moderate fibrosis from CHB patients with mild fibrosis, CHB patients with high fibrosis from CHB patients with mild fibrosis and CHB patients with high fibrosis from CHB patients with moderate fibrosis was 0.914, 0.847, 0.934, 0.962, 0.774, 0.880, and 0.762. 113 Further analysis showed serum circMTO1 was not correlated with viral replication and liver function. 113 These results showed serum circMTO1 could be a non‐invasive marker for diagnosis of early or mild fibrosis and fibrosis stage in CHB patients.
5. CONCLUSION
These researches have shown that serum microRNAs, lncRNAs, and circRNAs could be potential non‐invasive markers for early fibrosis diagnosis or staging fibrosis. However, there were still no multiple‐center clinical trial in most research. It still needs further research to study the clinical practice of serum non‐coding RNAs in big cohorts. Single serum microRNA, lncRNA, or circRNA may not be good enough for clinical practice. A panel which included several non‐coding RNAs or combination with other serum markers such as APBI, FIB‐4 could increase the accuracy of serum markers to predict liver fibrosis or stage fibrosis. More high‐quality researches are needed to promote the clinical application of the serum non‐coding RNAs in patients with liver fibrosis.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
ACKNOWLEDGMENTS
This word was supported by the funding of the Scientific and technological innovation project of the China Academy of Chinese Medical Sciences (CI2021A008010).
Liu C, Hou X, Mo K, et al. Serum non‐coding RNAs for diagnosis and stage of liver fibrosis. J Clin Lab Anal. 2022;36:e24658. doi: 10.1002/jcla.24658
Contributor Information
Guijian Liu, Email: liuguijian@163.com.
Zongdai Pan, Email: zongdai2002@foxmail.com.
DATA AVAILABILITY STATEMENT
All the data in this review were cited from the references. No new data were generated.
REFERENCES
- 1. Zoubek ME, Trautwein C, Strnad P. Reversal of liver fibrosis: from fiction to reality. Best Pract Res Clin Gastroenterol. 2017;31:129‐141. [DOI] [PubMed] [Google Scholar]
- 2. Huang Y, de Boer WB, Adams LA, MacQuillan G, Bulsara MK, Jeffrey GP. Image analysis of liver biopsy samples measures fibrosis and predicts clinical outcome. J Hepatol. 2014;61:22‐27. [DOI] [PubMed] [Google Scholar]
- 3. Loomba R, Adams LA. Advances in non‐invasive assessment of hepatic fibrosis. Gut. 2020;69:1343‐1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lai M, Afdhal NH. Liver Fibrosis Determination. Gastroenterol Clin North Am. 2019;48:281‐289. [DOI] [PubMed] [Google Scholar]
- 5. do Amaral AE, Cisilotto J, Creczynski‐Pasa TB, de Lucca Schiavon L. Circulating miRNAs in nontumoral liver diseases. Pharmacol Res. 2017;128:274‐287. [DOI] [PubMed] [Google Scholar]
- 6. De Vincentis A, Rahmani Z, Muley M, et al. Long noncoding RNAs in nonalcoholic fatty liver disease and liver fibrosis: state‐of‐the‐art and perspectives in diagnosis and treatment. Drug Discov Today. 2020;25:1277‐1286. [DOI] [PubMed] [Google Scholar]
- 7. Yang YR, Hu S, Bu FT, et al. Circular RNA CREBBP Suppresses Hepatic Fibrosis Via Targeting the hsa‐miR‐1291/LEFTY2 Axis. Front Pharmacol. 2021;12:741151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bartel DP. Metazoan microRNAs. Cell. 2018;173:20‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ludwig N, Leidinger P, Becker K, et al. Distributionof miRNA expression across human tissues. Nucleic Acids Res. 2016;44:3865‐3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136:215‐233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Huntzinger E, Izaurralde E. Gene silencing by microRNAs: contributions of translational repression and mRNA decay. Nat Rev Genet. 2011;12:99‐110. [DOI] [PubMed] [Google Scholar]
- 12. Li G, Cai G, Li D, Yin W. MicroRNAs and liver disease: viral hepatitis, liver fibrosis and hepatocellular carcinoma. Postgrad Med J. 2013;90:106‐112. [DOI] [PubMed] [Google Scholar]
- 13. Li H, Jiang JD, Peng ZG. MicroRNA‐mediated interactions between host and hepatitis C virus. World J Gastroenterol. 2016;22:1487‐1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Xue J, Xiao T, Wei S, et al. miR‐21‐regulated M2 polarization of macrophage is involved in arsenicosis‐induced hepatic fibrosis through the activation of hepatic stellate cells. J Cell Physiol. 2021;236:6025‐6041. [DOI] [PubMed] [Google Scholar]
- 15. Lai S, Iwakiri Y. Is miR‐21 a potent target for liver fibrosis? Hepatology. 2018;67:2082‐2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu HC, Huang CL, Wang HW, et al. Serum miR‐21 correlates with the histological stage of chronic hepatitis B‐associated liver fibrosis. Int J Clin Exp Pathol. 2019;12:3819‐3829. [PMC free article] [PubMed] [Google Scholar]
- 17. Migita K, Komori A, Kozuru H, et al. Circulating microRNA Profiles in Patients with Type‐1 Autoimmune Hepatitis. PLoS One. 2015;10:e0136908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bao SX, Zheng JM, Li N, et al. Serum MicroRNA levels as a noninvasive diagnostic biomarker for the early diagnosis of hepatitis B virus‐related liver fibrosis. Gut Liver. 2017;11:860‐869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lagos‐Quintana M, Rauhut R, Yalcin A et al: Identification of tissue‐specific microRNAs from mouse. CurrBiol 12: 735–739, 2002. [DOI] [PubMed] [Google Scholar]
- 20. Chang J, Nicolas E, Marks D, et al. miR‐122, a mammalian liver‐specific microRNA, is processed from hcr mRNA and may downregulate the high affinity cationic amino acid transporter CAT‐1. RNA Biol. 2004;1:106‐113. [DOI] [PubMed] [Google Scholar]
- 21. Lanford RE, Hildebrandt‐Eriksen ES, Petri A, et al. Therapeutic silencing of microRNA‐122 in primates with chronic hepatitis C virus infection. Science. 2010;327:198‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang S, Qiu L, Yan X, et al. Loss of microRNA 122 expression in patients with hepatitis B enhances hepatitis B virus replication through cyclin G(1)‐modulated P53 activity. Hepatology. 2012;55:730‐741. [DOI] [PubMed] [Google Scholar]
- 23. Ali B, Henning G, Jacob G, et al. The epigenetic drug discovery landscape for metabolic associated fatty liver disease. Trends Genet. 2020;36:429‐441. [DOI] [PubMed] [Google Scholar]
- 24. Eslam M, Valenti L, Romeo S. Genetics and epigenetics of NAFLD and NASH: clinical impact. J Hepatol. 2018;68:268‐279. [DOI] [PubMed] [Google Scholar]
- 25. Omran AAS, Osman KS, Kamel HM, Abdel‐Naem EA, El‐Deen Hasan DE. MicroRNA‐122 as a Novel Non‐Invasive Marker of Liver Fibrosis in Hepatitis C Virus Patients. Clin Lab. 2016;62:1329‐1337. [DOI] [PubMed] [Google Scholar]
- 26. Bihrer V, Friedrich‐Rust M, Kronenberger B, et al. Serum miR‐122 as a biomarker of necroinflammation in patients with chronic hepatitis C virus infection. Am J Gastroenterol. 2011;106:1663‐1669. [DOI] [PubMed] [Google Scholar]
- 27. Nakamura M, Kanda T, Jiang X, et al. Serum microRNA‐122 and Wisteria floribunda agglutinin‐positive Mac‐2 binding protein are useful tools for liquid biopsy of the patients with hepatitis B virus and advanced liver fibrosis. PLoS One. 2017;12:e0177302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hegazy MA, Abd ALgwad I, Fadl SA, et al. Serum Micro‐RNA‐122 Level as a Simple Noninvasive Marker of MAFLD Severity. Diabetes Metab Syndr Obes. 2021;14:2247‐2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Matsuura K, De Giorgi V, Schechterly C, et al. Circulating let‐7 levels in plasma and extracellular vesicles correlate with hepatic fibrosis progression in chronic hepatitis C. Hepatology. 2016;64:732‐745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matsuura K et al. Circulating let‐7 Levels in Serum Correlate With the Severity of Hepatic Fibrosis in Chronic Hepatitis C. Open Forum Infect Dis. 2018;5:ofy268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cai PF, Mu Y, Olveda RM, Ross AG, Olveda DU, McManus DP. Circulating miRNAs as footprints for liver fibrosis grading in schistosomiasis. EBioMedicine. 2018;37:334‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ma L, Yang X, Wei R, et al. MicroRNA‐214 promotes hepatic stellate cell activation and liver fbrosis by suppressing Sufu expression. Cell Death Dis. 2018;9:718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yoneyama T, Ueno T, Masahata K, et al. Elevation of microRNA‐214 is associated with progression of liver fibrosis in patients with biliary atresia. Pediatr Surg Int. 2022;38:115‐122. [DOI] [PubMed] [Google Scholar]
- 34. Bala S, Csak T, Saha B, et al. The pro‐inflammatory effects of miR‐155 promote liver fibrosis and alcohol‐induced steatohepatitis. J Hepatol. 2016;64:1378‐1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hyun J, Park J, Wang S, et al. MicroRNA Expression Profiling in CCl(4)‐Induced Liver Fibrosis of Mus musculus. Int J Mol Sci. 2016;17:961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fu X, Wen H, Jing L, et al. MicroRNA‐155‐5p promotes hepatocellular carcinoma progression by suppressing PTEN through the PI3K/Akt pathway. Cancer Sci. 2017;108:620‐631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Xi W, Zhao X, Wu M, Jia W, Li H. Lack of microRNA‐155 ameliorates renal fibrosis by targeting PDE3A/TGF‐beta1/Smad signaling in mice with obstructive nephropathy. Cell Biol Int. 2018;42:1523‐1532. [DOI] [PubMed] [Google Scholar]
- 38. Wei Y, Yan X, Yan L, et al. Inhibition of microRNA‐155 ameliorates cardiac fibrosis in the process of angiotensin II‐induced cardiac remodeling. Mol Med Rep. 2017;16:7287‐7296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ali AM, El‐Tawil OS, Al‐Mokaddem AK, Abd El‐Rahman SS. Promoted inhibition of TLR4/miR‐155/NF(k)B p65 signaling by cannabinoid receptor 2 agonist (AM1241), aborts inflammation and progress of hepatic fibrosis induced by thioacetamide. Chem Biol Interact. 2021;336:109398. [DOI] [PubMed] [Google Scholar]
- 40. Niu LJ, Zhang YM, Huang T, Sun XF, Luo SX. Exosomal microRNA‐155 as a biomarker for hepatic fibrosis diagnosis and progression. Ann Transl Med. 2021;9:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shaker OG, Senousy MA. Serum microRNAs as predictors for liver fibrosis staging in hepatitis C virus‐associated chronic liver disease patients. J Viral Hepat. 2017;24:636‐644. [DOI] [PubMed] [Google Scholar]
- 42. Deng Z, He Y, Yang X, et al. MicroRNA‐29: a crucial player in fibrotic disease. Mol Diagn Ther. 2017;21:285‐294. [DOI] [PubMed] [Google Scholar]
- 43. Ge Y, Chen G, Sun L, Liu F. MicroRNA‐29 and fibrosis diseases. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2011;36:908‐912. [DOI] [PubMed] [Google Scholar]
- 44. Lin HY, Wang FS, Yang YL, Huang YH. MicroRNA‐29a Suppresses CD36 to Ameliorate High Fat Diet‐Induced Steatohepatitis and Liver Fibrosis in Mice. Cell. 2019;8:1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tiao MM, Wang FS, Huang LT, et al. MicroRNA‐29a protects against acute liver injury in a mouse model of obstructive jaundice via inhibition of the extrinsic apoptosis pathway. Apoptosis. 2014;19:30‐41. [DOI] [PubMed] [Google Scholar]
- 46. Roderburg C, Urban GW, Bettermann K, et al. Micro‐RNA profiling reveals a role for miR‐29 in human and murine liver fibrosis. Hepatology. 2011;53:209‐218. [DOI] [PubMed] [Google Scholar]
- 47. Appourchaux K, Dokmak S, Resche‐Rigon M, et al. MicroRNA‐based diagnostic tools for advanced fibrosis and cirrhosis in patients with chronic hepatitis B and C. Sci Rep Actions. 2016;6:34935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ivashchenko A, Berillo O, Pyrkova A, Niyazova R. Binding sites of miR‐1273 family on the mRNA of target genes. Biomed Res Int. 2014;620530:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Niu X, Fu N, Du J, et al. miR‐1273g‐3p modulates activation and apoptosis of hepatic stellate cells by directly targeting PTEN in HCV‐related liver fibrosis. FEBS Lett. 2016;590:2709‐2724. [DOI] [PubMed] [Google Scholar]
- 50. Nan Y, Niu X, Wang R, et al. microRNA‐1273g‐3p is a useful non‐invasive test for the prediction of liver fibrosis in patients with chronic hepatitis C. Exp Ther Med. 2019;17:1817‐1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pan Y, Wang J, He L, Zhang F. MicroRNA‐34a promotes EMT and liver fibrosis in primary biliary cholangitis by regulating TGF‐beta1/smad pathway. J Immunol Res. 2021;2021:6890423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Tian XF, Ji FJ, Zang HL, Cao H. Activation of the miR‐34a/SIRT1/p53 Signaling Pathway Contributes to the Progress of Liver Fibrosis via Inducing Apoptosis in Hepatocytes but Not in HSCs. PLoS One. 2016;11:e0158657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Li X, Chen Y, Wu S, et al. microRNA‐34a and microRNA‐34c promote the activation of human hepatic stellate cells by targeting peroxisome proliferator‐activated receptor γ. Mol Med Rep. 2015;11:1017‐1024. [DOI] [PubMed] [Google Scholar]
- 54. Li X, Zhang W, Xu K, Lu J. miR‐34a promotes liver fibrosis in patients with chronic hepatitis via mediating Sirt1/p53 signaling pathway. Pathol Res Pract. 2020;216:152876. [DOI] [PubMed] [Google Scholar]
- 55. Fu H, Chu D, Geng X. Downregulation of miR‐17 suppresses TGF‐beta1‐mediated renal fibrosis through targeting Smad7. Mol Cell Biochem. 2021;476:3051‐3064. [DOI] [PubMed] [Google Scholar]
- 56. Oglesby IK, Vencken SF, Agrawal R, et al. miR‐17 overexpression in cystic fibrosis airway epithelial cells decreases interleukin‐8 production. Eur Respir J. 2015;46:1350‐1360. [DOI] [PubMed] [Google Scholar]
- 57. Zaafan MA, Abdelhamid AM. Dasatinib ameliorates thioacetamide‐induced liver fibrosis: modulation of miR‐378 and miR‐17 and their linked Wnt/beta‐catenin and TGF‐beta/smads pathways. J Enzyme Inhib Med Chem. 2022;37:118‐124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gao F, Li K, Li Y, et al. Serum miR‐17 levels in patients with hepatitis B virus induced liver fibrosis. Eur Rev Med Pharmacol Sci. 2020;24:6245‐6251. [DOI] [PubMed] [Google Scholar]
- 59. Zhu L, Mou Q, Wang Y, Zhu Z, Cheng M. Resveratrol contributes to the inhibition of liver fibrosis by inducing autophagy via the microRNA‐20a‐mediated activation of the PTEN/PI3K/AKT signaling pathway. Int J Mol Med. 2020;46:2035‐2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shrivastava S, Petrone J, Steele R, Lauer GM, Di Bisceglie AM, Ray RB. Up‐regulation of circulating miR‐20a is correlated with hepatitis C virus‐mediated liver disease progression. Hepatology. 2013;58:863‐871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zhao X, Sun J, Chen Y, et al. lncRNA PFAR Promotes Lung Fibroblast Activation and Fibrosis by Targeting miR‐138 to Regulate the YAP1‐Twist Axis. Mol Ther. 2018;26:2206‐2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wu Q, Gui W, Jiao B, Han L, Wang F. miR‐138 inhibits epithelial‐mesenchymal transition in silica‐induced pulmonary fibrosis by regulating ZEB2. Toxicology. 2021;461:152925. [DOI] [PubMed] [Google Scholar]
- 63. El‐Ahwany E, Nagy F, Zoheiry M, et al. Circulating miRNAs as predictor markers for activation of hepatic stellate cells and progression of HCV‐induced liver fibrosis. Electron Physician. 2016;8:1804‐1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Cai P, Mu Y, Olveda RM, Ross AG, Olveda DU, McManus DP. Serum Exosomal miRNAs for Grading Hepatic Fibrosis Due to Schistosomiasis. Int J Mol Sci. 2020;21:3560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Beermann J, Piccoli MT, Viereck J, Thum T. Non‐coding RNAs in development and disease: background, mechanisms, and therapeutic approaches. Physiol Rev. 2016;96:1297‐1325. [DOI] [PubMed] [Google Scholar]
- 66. Harries LW. Long non‐coding RNAs and human disease. Biochem Soc Trans. 2012;40:902‐906. [DOI] [PubMed] [Google Scholar]
- 67. Huarte M, Guttman M, Feldser D, et al. A large intergenic noncoding RNA induced by p53 mediates global gene repression in the p53 response. Cell. 2010;142:409‐419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Yoon JH, Abdelmohsen K, Srikantan S, et al. LincRNA‐p21 suppresses target mRNA translation. Mol Cell. 2012;47:648‐655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Tang SS, Zheng BY, Xiong XD. LincRNA‐p21: Implications in Human Diseases. Int J Mol Sci. 2015;16:18732‐18740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Chen S, Liang H, Yang H, et al. LincRNa‐p21: function and mechanism in cancer. Med Oncol. 2017;34:98. [DOI] [PubMed] [Google Scholar]
- 71. Yu F, Zhou G, Huang K, et al. Serum lincRNA‐p21 as a potential biomarker of liver fibrosis in chronic hepatitis B patients. J Viral Hepat. 2017;24:580‐588. [DOI] [PubMed] [Google Scholar]
- 72. Zheng J, Dong P, Mao Y, et al. lincRNA‐p21 inhibits hepatic stellate cell activation and liver fibrogenesis via p21. FEBS J. 2015;282:4810‐4821. [DOI] [PubMed] [Google Scholar]
- 73. Wang S, Jiang J, Zhang C, Zhang X, Wang C. Serum lincRNA‐p21 expression in primary liver diseases and liver metastatic diseases. Pathol Res Pract. 2019;215:779‐783. [DOI] [PubMed] [Google Scholar]
- 74. Zhang K, Han Y, Hu Z, et al. SCARNA10, a nuclear‐retained long non‐coding RNA, promotes liver fibrosis and serves as a potential biomarker. Theranostics. 2019;9:3622‐3638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Zhou Y, Zhang X, Klibanski A. MEG3 noncoding RNA: a tumor suppressor. J Mol Endocrinol. 2012;48:R45‐R53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Anwar SL, Krech T, Hasemeier B, et al. Loss of imprinting and allelic switching at the DLK1‐MEG3Locus in human hepatocellular carcinoma. PLoS ONE. 2012;7:e49462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lu KH, Li W, Liu XH, et al. Long non‐coding RNA MEG3 inhibits NSCLC cells proliferation and induces apoptosis by afecting p53 expression. BMC Cancer. 2013;13:461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Yan J, Guo X, Xia J, et al. MiR‐148a regulates MEG3 in gastric cancer by targeting DNA methyltransferase 1. Med Oncol. 2014;31:879. [DOI] [PubMed] [Google Scholar]
- 79. Wu YY, Wu S, Li XF, et al. LncRNA MEG3 reverses CCl 4‐induced liver fibrosis by targeting NLRC5. Eur J Pharmacol. 2021;911:174462. [DOI] [PubMed] [Google Scholar]
- 80. Gao Q, Chang X, Yang M, et al. LncRNA MEG3 restrained pulmonary fibrosis induced by NiO NPs via regulating hedgehog signaling pathway‐mediated autophagy. Environ Toxicol. 2022;37:79‐91. [DOI] [PubMed] [Google Scholar]
- 81. Xue R, Li Y, Li X, Ma J, An C, Ma Z. miR‐185 affected the EMT, cell viability, and proliferation via DNMT1/MEG3 pathway in TGF‐β1‐induced renal fibrosis. Cell Biol Int. 2019;43:1152‐1162. [DOI] [PubMed] [Google Scholar]
- 82. Piccoli MT, Gupta SK, Viereck J, et al. Inhibition of the cardiac fibroblast‐enriched lncRNA Meg3 prevents cardiac fibrosis and diastolic dysfunction. Circ Res. 2017;121:575‐583. [DOI] [PubMed] [Google Scholar]
- 83. He Y, Wu YT, Huang C, et al. Inhibitory effects of long noncoding RNA MEG3 on hepatic stellate cells activation and liver fibrogenesis. Biochim Biophys Acta. 1842;2204‐2215:2014‐2215. [DOI] [PubMed] [Google Scholar]
- 84. Yu F, Geng W, Dong P, Huang Z, Zheng J. LncRNA‐MEG3 inhibits activation of hepatic stellate cells through SMO protein and miR‐212. Cell Death Dis. 2018;9:1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Chen MJ, Wang XG, Sun ZX, Liu XC. Diagnostic value of LncRNA‐MEG3 as a serum biomarker in patients with hepatitis B complicated with liver fibrosis. Eur Rev Med Pharmacol Sci. 2019;23:4360‐4367. [DOI] [PubMed] [Google Scholar]
- 86. Qin R, Huang W, Huang Y, et al. lncRNA MEG3 modulates hepatic stellate cell activation by sponging miR‐145 to regulate PPARγ. Mol Med Rep. 2022;25:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Wang K, Li J, Xiong G, et al. Negative regulation of lncRNA GAS5 by miR‐196a inhibits esophageal squamous cell carcinoma growth. Biochem Biophys Res Commun. 2018;495:1151‐1157. [DOI] [PubMed] [Google Scholar]
- 88. Cao S, Liu W, Li F, Zhao W, Qin C. Decreased expression of lncRNA GAS5 predicts a poor prognosis in cervical cancer. Int J Clin Exp Pathol. 2014;7:6776‐6783. [PMC free article] [PubMed] [Google Scholar]
- 89. Dong Z, Li S, Wang X, et al. lncRNA GAS5 restrains CCl(4)‐induced hepatic fibrosis by targeting miR‐23a through the PTEN/PI3K/Akt signaling pathway. Am J Physiol Gastrointest Liver Physiol. 2019;316:G539‐G550. [DOI] [PubMed] [Google Scholar]
- 90. Liu HL, Chen CH, Sun YJ. Overexpression of lncRNA GAS5 attenuates cardiac fibrosis through regulating PTEN/MMP‐2 signal pathway in mice. Eur Rev Med Pharmacol Sci. 2019;23:4414‐4418. [DOI] [PubMed] [Google Scholar]
- 91. Tao H, Shi P, Zhao XD, Xuan HY, Ding XS. MeCP2 inactivation of LncRNA GAS5 triggers cardiac fibroblasts activation in cardiac fibrosis. Cell Signal. 2020;74:109705. [DOI] [PubMed] [Google Scholar]
- 92. Lin CY, Liao YW, Hsieh PL, et al. LncRNA GAS5‐AS1 inhibits myofibroblasts activities in oral submucous fibrosis. J Formos Med Assoc. 2018;117:727‐733. [DOI] [PubMed] [Google Scholar]
- 93. Yu F, Zheng J, Mao Y, et al. Long non‐coding RNA growth arrest‐specific transcript 5 (GAS5) inhibits liver fibrogenesis through a mechanism of competing endogenous RNA. J Biol Chem. 2015;290:28286‐28298. doi: 10.1074/jbc.M115.683813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Su SB, Tao L, Liang XL, Chen W: Long noncoding RNA GAS5 inhibits LX‐2 cells activation by suppressing NF‐kappaB signalling through regulation of the miR‐433‐3p/TLR10 axis. Dig Liver Dis. 2021;54:1066‐1075. [DOI] [PubMed] [Google Scholar]
- 95. Guo Y, Li C, Zhang R, et al. Epigenetically‐regulated serum GAS5 as a potential biomarker for patients with chronic hepatitis B virus infection. Cancer Biomark. 2021;32:137‐146. [DOI] [PubMed] [Google Scholar]
- 96. Han MH, Lee JH, Kim G, et al. Expression of the Long Noncoding RNA GAS5 Correlates with Liver Fibrosis in Patients with Nonalcoholic Fatty Liver Disease. Genes (Basel). 2020;11:545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Albadawy R, Agwa SHA, Khairy E, et al. Circulatory endothelin 1‐regulating RNAs panel: promising biomarkers for non‐invasive NAFLD/NASH diagnosis and stratification: clinical and molecular pilot study. Genes (Basel). 2021;12:1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Xiao Z, Qiu Y, Lin Y, et al. Blocking lncRNA H19‐miR‐19aId2 axis attenuates hypoxia/ischemia induced neuronal injury. Aging (Albany NY). 2019;11:3585‐3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Song Y, Liu C, Liu X, et al. H19 promotes cholestatic liver fibrosis by preventing ZEB1‐mediated inhibition of epithelial cell adhesion molecule. Hepatology. 2017;66:1183‐1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Lu Q, Guo Z, Xie W, et al. The lncRNA H19 mediates pulmonary fibrosis by regulating the miR‐196a/COL1A1 axis. Inflammation. 2018;41:896‐903. [DOI] [PubMed] [Google Scholar]
- 101. Shi S, Song L, Yu H, et al. Knockdown of LncRNA‐H19 ameliorates kidney fibrosis in diabetic mice by suppressing miR‐29a‐mediated EndMT. Front Pharmacol. 2020;11:586895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Huang ZW, Tian LH, Yang B, Guo RM. Long noncoding RNA H19 acts as a competing endogenous RNA to mediate CTGF expression by sponging miR‐455 in cardiac fibrosis. DNA Cell Biol. 2017;36:759‐766. [DOI] [PubMed] [Google Scholar]
- 103. Yu CC, Liao YW, Hsieh PL, Chang YC. Targeting lncRNA H19/miR‐29b/COL1A1 axis impedes myofibroblast activities of precancerous oral submucous fibrosis. Int J Mol Sci. 2021;22:2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Zhu J, Luo Z, Pan Y, et al. H19/miR‐148a/USP4 axis facilitates liver fibrosis by enhancing TGF‐beta signaling in both hepatic stellate cells and hepatocytes. J Cell Physiol. 2019;234:9698‐9710. [DOI] [PubMed] [Google Scholar]
- 105. Wang C, Deng J, Deng H, et al. A novel Sox9/lncRNA H19 axis contributes to hepatocyte death and liver fibrosis. Toxicol Sci. 2020;177:214‐225. [DOI] [PubMed] [Google Scholar]
- 106. Xiao Y, Liu R, Li X, et al. Long noncoding RNA H19 contributes to cholangiocyte proliferation and cholestatic liver fibrosis in biliary atresia. Hepatology. 2019;70:1658‐1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Shu B, Zhou YX, Li H, Zhang RZ, He C, Yang X. The METTL3/MALAT1/PTBP1/USP8/TAK1 axis promotes pyroptosis and M1 polarization of macrophages and contributes to liver fibrosis. Cell Death Discov. 2021;7:368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Yu F, Lu Z, Cai J, et al. MALAT1 functions as a competing endogenous RNA to mediate Rac1 expression by sequestering miR‐101b in liver fibrosis. Cell Cycle. 2015;14:3885‐3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Leti F, Legendre C, Still CD, et al. Altered expression of MALAT1 lncRNA in nonalcoholic steatohepatitis fibrosis regulates CXCL5 in hepatic stellate cells. Transl Res. 2017;190:25‐39.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Wang Y, Mou Q, Zhu Z, Zhao L, Zhu L. MALAT1 promotes liver fibrosis by sponging miR‐181a and activating TLR4‐NF‐kappaB signaling. Int J Mol Med. 2021;48:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Di Mauro S, Scamporrino A, Petta S, et al. Serum coding and non‐coding RNAs as biomarkers of NAFLD and fibrosis severity. Liver Int. 2019;39:1742‐1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Han D, Li JX, Wang HM, et al. Circular RNA circMTO1 acts as the sponge of microRNA‐9 to suppress hepatocellular carcinoma progression. Hepatology. 2017;66(4):1151‐1164. [DOI] [PubMed] [Google Scholar]
- 113. Wang W, Dong RL, Guo Y, et al. CircMTO1 inhibits liver fibrosis via regulation of miR‐17‐5p and Smad7. J Cell Mol Med. 2019;23:5486‐5496. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data in this review were cited from the references. No new data were generated.


