Abstract
Objective
To investigate longitudinal, predictive associations between community participation, positive affect, social support, and functional independence for individuals post-stroke at 3 and 12 months post-discharge.
Design
Longitudinal design.
Subjects
Data from 544 participants were obtained from the Stroke Recovery in Underserved Populations (2005–06) database.
Methods
A cross-lagged panel network analysis to identify the complex set of predictive relationships between community participation, positive affect, social support, and functional independence 3 months post-discharge to 12 months post-discharge.
Results
Community participation, particularly religious/spiritual activities, was an early predictor of later motor (functional) independence and social support. In addition, positive affect was an early predictor of social support.
Conclusion
While participation in social situations is a desired outcome post-stroke, the results of this study indicate the importance of identifying early factors that influence community participation throughout the recovery process.
LAY ABSTRACT
The ability to participate in desired activities is a common outcome goal of rehabilitation for stroke survivors. However, there are many factors that influence success in achieving this goal, including support from family and friends, mental health, and functional independence. This study sought to understand how these factors influence each other and participation over time. The results indicate that early participation post-stroke is an important predictor of later motor independence and social support needs. The results indicate that, while participation is often viewed as a rehabilitation outcome, understanding participation as a predictor of other rehabilitation outcomes is also important.
Key words: stroke, participation, aphasia, positive emotion, network, support
Stroke survivors are immediately faced with new challenges, impacting their engagement in fulfilling activities (i.e. participation). One way to assess progress post-stroke is to consider the individual’s ability to participate in life situations (1, 2), which may include activities with others. In addition to the social aspect of participation, other aspects of participation include learning and applying knowledge, mobility, self-care, domestic life, interpersonal interactions and relationships (3, 4). Unfortunately, many stroke survivors report difficulties in participation (5) and do not feel confident in participating upon discharge (6).
Many researchers are interested in determining predictors of participation post-stroke, including social, mental health, and functional (motor and cognitive-linguistic) factors. Social support has a strong, positive relationship with participation (7, 8), with feelings of connectedness as an integral component (9). However, a catastrophic event, like a stroke, can increase the risk of mental health disorders, including major depression (10). Many studies focus on negative affect (or feelings of negative emotions) and risk factors of depression, including social isolation, living alone, and functional limitations (11, 12). However, positive affect and resiliency is less often the focus of research, despite its role in positive rehabilitation outcomes post-stroke (13–15).
In addition, functional independence is critical to engaging in activities. Physical impairments due to stroke may reduce opportunities for participation (16, 17), as individuals may not be able to engage easily with others, particularly outside of the home. Even when accounting for social support, physical limitations still impede full participation by stroke survivors (18). Participation also requires cognitive and linguistic skills. Stroke survivors with impaired cognitive-linguistic abilities tend to have lower participation post-stroke (19–21), particularly in stroke survivors with a left hemisphere stroke resulting in aphasia (22). Thus, intact cognitive and linguistic abilities are a necessary aspect of successful communication, without which individuals may be unable to fully participate in activities.
While prior research often focuses on these factors, often one at a time, as predictors of participation post-stroke, these factors are quite entangled and influential on each other, as well as directly on participation (23–27). In a systematic review, Ezekiel et al. (23) found that depressive symptoms, cognitive functioning, and mobility were strongly associated with participation in stroke; however, the authors noted that the full extent of the association of these factors with participation was unclear, in part due to which factors and how many measures of each factor are considered across studies. Complex relationships among diverse measures can be difficult to fully capture and visualize with traditional statistical approaches. Instead, the aim of the current study is to use network analysis to model the interaction of social support, positive affect, functional independence, and community participation from 3 to 12 months post-discharge from rehabilitation hospitals.
Network analysis has been used to investigate a variety of phenomena (28–31), including post-stroke depression (32) and aphasia (33). With the network analysis approach, no single factor is the dependent variable. Instead, this approach allows for examination of all complex relationships between factors simultaneously, while considering the temporality of effects. In addition, our approach looks at individual facets of community participation (e.g. socializing outside the home), positive emotions (e.g. feeling hopeful about the future), and functioning (e.g. social cognition), rather than collapsing them in broad categories. This approach provides more granularity when understanding the complexity of participation post-stroke. The aim and approach of this study aligns with the International Classification of Functioning, Disability and Health (ICF) framework (2), which recognizes that functioning and disability are dynamic, multi-dimensional, and non-linear.
An additional exploratory aim seeks to assess whether the complexity of participation factors differ between people with and without aphasia. Approximately one-third of stroke survivors have aphasia (34) and their language impairments may differentially impact participation post-stroke (22).
METHODS
Study design
This study is a retrospective analysis of de-identified data obtained from the publicly available database, Stroke Recovery in Underserved Populations (2005–2006) (SRUP). SRUP is an observational follow-up study of persons who had a stroke and received inpatient medical rehabilitation services during 2005–06 (35). Participants receive a number of assessments upon entry, upon discharge, 3 months post-discharge, and 12 months post-discharge from the rehabilitation hospital. For additional details about the SRUP, readers are referred to (25) and to https://www.icpsr.umich.edu/web/ADDEP/studies/36422.
Participants
The SRUP database contains data from more than 1,200 stroke survivors from 11 rehabilitation hospitals in the USA. The present retrospective analysis only includes data from participants with no missingness on the measures of interest (below), resulting in a total of 544 participants. Of these participants, 229 persons in the sample had aphasia as a symptom of stroke. Table I presents demographic characteristics of the sample when they entered the rehabilitation hospital.
Table I.
Demographic characteristics
| Total N | 544 |
| Mean age (SD) | 67.78 (13.00) |
| Mean years of education (SD) | 12.51 (3.11) |
| Mean number of comorbidities (SD) | 2.79 (1.27) |
| Mean number of days in hospital (SD) | 19.91 (10.98) |
| Female (%) | 283 (52.02) |
| Ethnicity/race (%) | |
| White | 415 (76.29) |
| Black | 93 (17.10) |
| Hispanic | 24 (4.41) |
| Other | 12 (2.21) |
| Diagnosis of aphasia (%) | |
| Aphasia | 229 (42.10) |
| No aphasia | 315 (57.90) |
SD: standard deviation.
Measures
This study focused on 4 categories of measures in the study of participation post-stroke: community participation, positive affect, social support, and functional independence. Across the 4 categories of measures, we had 12 variables of interest: community participation (n = 4), positive affect (n = 4), social support (n = 1), and functional independence (n = 3). For the current analysis, data were obtained on these specific measures at 3 months post-rehabilitation discharge (T1) and 12 months post-rehabilitation discharge (T2). The means and standard deviations (SD) of all the measures are provided in the Supplementary material Table S1.
Community participation was measured with the PAR-PRO: Home and Community Participation Questionnaire (36). Scores on the PAR-PRO reflect a broad construct of participation, as it covers 4 domains of participation: socializing inside the home, socializing outside the home, recreation and leisure, and religious or spiritual activities. Participants rate, for each domain, how much they participated in these domains during the past 2 weeks on a 5-point Likert scale (with higher scores indicating more frequent participation).
Positive affect, or the feeling of positive emotions, was measured using the 4 positively scaled items from the Center for Epidemiologic Studies – Depression Scale (CES-D) (37). These 4 items were “I felt that I was just as good as others” (CES-D item 4), “I felt hopeful about the future” (CES-D item 8), “I was happy” (CES-D item 12), and “I enjoyed life” (CES-D item 12). Participants rate for each statement how often they felt that way over the past week on a 5-point Likert scale (with higher scores indicating more frequent feelings).
Social support was measured using the total score on the 11-item Duke – University of North Carolina Functional Social Support Questionnaire (38). Items include “I get help around the house” and “I get invitations to go out and do things with other people.” Participants rate for each question how much support they receive from other people on a 5-point Likert scale (with higher scores indicating higher perceived social support).
Functional independence was measured using 3 subscales of the Functional Independence Measure (FIM) (39). The subscales assessed the domains of motor abilities, social cognition, and communication. Participants rate for each functional activity how much assistance they require on a 7-point Likert scale (with higher scores indicating more functional support).
Statistical analysis
A cross-lagged panel network (CLPN) (40–42) was used to analyse a temporal, post-stroke participation network. In a CLPN, the effects of nodes (i.e. variables) at T1 on all other nodes at T2 are estimated, controlling for auto-regressive effects (i.e. regressing each node at T2 on itself at T1). In the participation network, nodes included were variables representing community participation and previously studied predictive factors of positive affect, social support, and functional independence collected at 3 months (i.e. T1) and 12 months (i.e. T2) post-discharge. A 10-fold cross-validation with Least Absolute Shrinkage and Selection Operator regularization to shrink very small associations to zero was applied. Since CLPN is a directed network, centrality indices of out expected influence (out-EI; sum of the values of outgoing edges from a variable) and in expected influence (in-EI; sum of the values of incoming edges to a variable) were calculated to determine the centrality of the variables in our network. R package glmnet (43) was used to calculate regularized regression and qgraph (44) was used to visualize the network. Nodes in the network were placed according to the Fruchterman & Reingold algorithm (45), which places more strongly connected nodes close together.
Stability and the accuracy of edges were estimated using the R package bootnet (46), with 95% confidence intervals (95% CI) around the edge weights using non-parametric bootstrapping. Case-dropping subset bootstrapping approach was used to calculate correlational stability (CS) coefficient. CS coefficient, ranging from 0 to 1, can be used to determine the stability of the centrality indices. A CS coefficient greater than 0.50 infers stability. The edge weight difference tests and centrality difference tests were calculated to determine whether differences between node centralities and edges were statistically significant.
Lastly, to address the exploratory aim, 2 CLPNs were constructed using data from persons with aphasia and persons without aphasia. To assess the similarity in the group-based participation networks, the edges of the CLPNs were compared by calculating the correlation between edge lists and the cumulative percentage of overlapping associations between both networks.
RESULTS
The results presented below are from 544 individuals with stroke who were assessed 3 and 12 months post-discharge from rehabilitation hospitals. Fig. 1 shows the overall CLPN with auto-regressive edges removed for ease of interpretation (see Supplementary material Table S2 and Fig. S1 for all edges and edge weights). A total of 67 cross-lagged edges and all auto-regressive edges were present in the model. In the participation network, the strongest cross-lagged edges were FIM-Social Cognition (F2) → FIM-Motor (F3) [β = 0.56], Religious/Spiritual activities (C4) → FIM-Motor (F3) [β = 0.45], Happy (P3) → Social Support (S) [β = 0.30] and Socializing Outside the Home (C1) → Social Support (S) [β = 0.25].
Fig. 1.
Cross-Lagged Panel Network of Persons with Stroke. Each node represents a variable, with colour of nodes corresponding to a priori categories of measures. Directed edges between nodes represent a cross-lagged association, where Variable A at Time 1 predicts Variable B at Time 2, while controlling for all other associations. Blue edges denote positive associations and red edges denote negative associations. Thicker edges depict stronger associations than thinner edges.
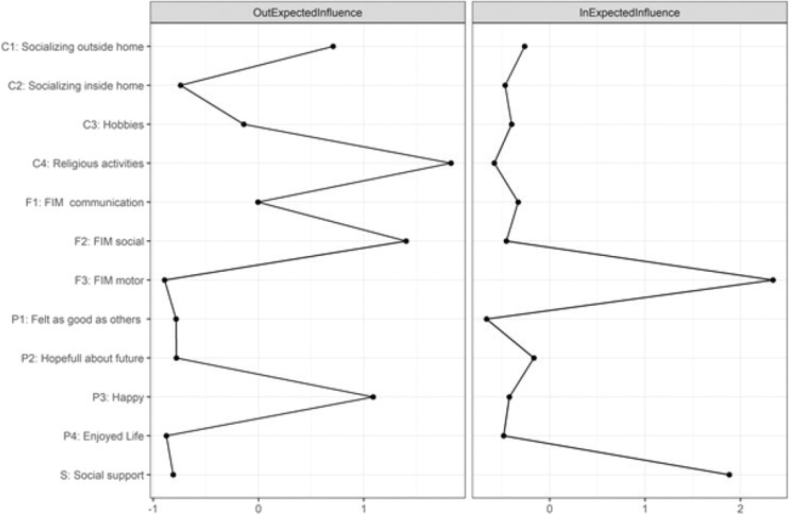
Centrality estimates are plotted in Fig. 2. Variables with the highest out-EI included Religious/Spiritual activities, FIM-Social Cognition, and Happy. Enjoyed Life and FIM-Motor had the lowest out-EI, followed closely by several others. Variables with the highest in-EI were FIM-Motor and Social Support. Felt as Good as Others had the lowest in-EI, followed closely by several others.
Fig. 2.
Centrality Indices of Persons with Stroke Cross-Lagged Panel Network. Expected influence centrality indices estimates with larger values suggesting higher expected influence. Z-scores shown on x-axis rather than raw centrality indices.
The accuracy and stability of the results were tested. Bootstrapped confidence intervals around edge weights were small to large (see Supplementary material Fig. S2). The in/out- EI centrality indices were not stable (CS coefficient = 0.21 and 0.13, respectively) and thus should be interpreted with caution. Edge weight difference tests and centrality difference tests are presented in the Supplementary material Fig. S3 and Fig. S4.
Exploratory aim
In comparing a CLPN based on data from persons with aphasia with a CLPN based on data from persons without aphasia, the coefficient of similarity was very low, 0.07. Only 44% of edges present in the aphasia network were also found in the no aphasia network. In the aphasia network, the strongest cross-lagged edge was Happy (P3) → FIM-Motor (F3) [β = –1.67], while the strongest cross-lagged edge in the no aphasia network was FIM-Social Cognition (F2) → FIM-Motor (F3) [β = 0.89]. See Supplementary material for CLPNs with auto-regressive edges (Fig. S5 and S6) and adjacency matrices with edge weights (Table S3 and S4).
DISCUSSION
This study aimed to assess the complex relationships between social support, positive affect, functional independence, and community participation in stroke survivors from 3 to 12 months post-discharge. Using network analysis, the results indicate that expected factors of social support, positive affect, and functional independence had early predictive influence on later participation. However, the results also showed that early participation predicted later abilities of the aforementioned factors. In addition, this exploratory analysis showed differences in the structure of the participation network between stroke survivors with and without aphasia.
One novel finding from the participation network is the role of early community participation on later functional independence and social support. Community participation at 3 months post-discharge was associated with higher social support and motor (functional) support at 12 months post-discharge from rehabilitation hospitals. These results suggest that individuals who participate early in recovery may have better support systems maintained over time. One community participation variable particularly stood out in this analysis: religious/spiritual activities. Such an activity is often engaged in with others in a social setting outside of the home. Participating in religious/spiritual activities, and other highly socialized activities, may provide increased benefit compared with less socialized activities (e.g. participating in a hobby at home by oneself ). For example, highly socialized activities provide a larger, welcoming community of social support that shares understanding of and provides aid to the stroke survivor beyond a caregiver or family unit (47).
Positive affect also had an important role in predicting later social support and participation. In the overall participation network, social support at 12 months post-discharge was predicted by feelings of happiness at 3 months post-discharge. This finding aligns with work on psychiatric illness: individuals who are happier tend to seek out others for help, while individuals who are depressed tend to withdraw from others (48). Relatedly, in the exploratory analysis, positive affect played a larger role in the aphasia participation network than the no aphasia participation network. While this result should be interpreted with caution, due to small sample sizes for each stroke patient group, it may reflect the critical role of positive emotion when faced with impairments in communication, which particularly increases difficulty in participation for those with aphasia.
Study limitations
This study has some limitations, including the availability of data in the SRUP (e.g. missing data on time post-stroke). The current analyses only considers 2 time points post-stroke: 3 months and 12 months. It is possible that the factors investigated in this study may interact and change in different ways over longer periods of time. Finally, the network analysis approach provides one method to analyse a large number of variables simultaneously, with multiple tools to investigate the resulting network structures. Centrality indices used in the current study is one approach to capture important nodes in the network, but see (49) for a discussion in interpreting centrality indices. Other measures of network structure, such as community structure, clustering coefficients, and degree, might also be considered to identify how the multiple factors studied in the current paper interact and influence each other.
CONCLUSION
The network analysis approach used in the current study provides an opportunity for future studies to comprehensively model the ICF framework and better identify how action on 1 aspect of the model can influence other aspects (50). Fig. 3 provides an example of a multi-layered network that critically allows one to examine the relationship of variables within a given domain (e.g. body structure and function), as well as the interaction of variables across domains (e.g. participation and environmental factors). While much more data is needed, and careful linking of clinical assessments to nodes in the network would be required (51, 52), such a complex systems approach with network analysis will allow researchers to identify key nodes/variables in an individuals’ ICF model that are well-connected (i.e. likely to have a widespread or strong influence on others). Thus, if the complex system is known, rehabilitation goals can be better targeted early on to improve outcomes for a patient in an efficient and effective manner that has cross-domain impact on the patient’s quality of life.
Fig. 3.

ICF Model as a Multi-layered Network. Multiple layers represent different ICF domains with nodes connected across layers (dashed lines) and within each layer (solid lines).
To conclude, these results highlight the need to address participation ability early in recovery, rather than just as a goal to be attained through rehabilitation. To do so, practitioners should be cognizant of and work toward increasing social and functional support systems and mental health of stroke survivors. This includes providing resources for mobility services, support groups for the stroke survivor and their caregiver/family, and mental health counselling. Practitioners need to take time to identify activities that are of importance to the stroke survivor, including those outside of the home, that can serve not only as points of participation, but also additional resources and supports to be used throughout the recovery process.
Supplementary Material
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Woodman P, Riazi A, Pereira C, Jones F. Social participation post stroke: a meta-ethnographic review of the experiences and views of community-dwelling stroke survivors. Disabil Rehabil 2014; 36: 2031–2043. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (SHO). International Classification for Functioning, Disability, and Health (ICF). Geneva: WHO; 2001. [Google Scholar]
- 3.Cieza A, Ewert T, Berdirhan Ustun T, Chatterji S, Kostanjsek N, Stucki G. Development of ICF Core Sets for patients with chronic conditions. J Rehabil Med 2004; 44 (Suppl): 9–11. [DOI] [PubMed] [Google Scholar]
- 4.Bickenbach J, Cieza A, Selb M, Stucki G. ICF core sets: manual for clinical practice for the ICF research branch, in cooperation with the WHO collaborating centre for the family of international. Göttingen: Hogrefe Publishing; 2012. [Google Scholar]
- 5.Eriksson G, Baum M, Wolf T, Connor L. Perceived participation after stroke: the influence of activity retention, reintegration, and perceived recovery. Am J Occup Ther 2013; 67: e131–138. [DOI] [PubMed] [Google Scholar]
- 6.Cott C, Wiles R, Devitt R. Continuity, transition and participation: preparing clients for life in the community post-stroke. Disabil Rehabil 2007; 29: 1566–1574. [DOI] [PubMed] [Google Scholar]
- 7.Erler KS, Sullivan V, Mckinnon S, Inzana R. Social support as a predictor of community participation after stroke. Front Neurol 2019; 10: 1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elloker T, Rhoda A. The relationship between social support and participation in stroke: a systematic review. Afr J Disabil 2018; 7: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haun J, Rittman M, Sberna M. The continuum of connectedness and social isolation during post stroke recovery. J Aging Stud 2008; 22: 54–64. [DOI] [PubMed] [Google Scholar]
- 10.Åström M, Adolfsson R, Asplund K. Major depression in stroke patients: a 3-year longitudinal study. Stroke 1993; 24: 976–982. [DOI] [PubMed] [Google Scholar]
- 11.Ouimet MA, Primeau F, Cole MG. Psychosocial risk factors in poststroke depression: a systematic review. Can J Psychiatr 2001; 46: 819–828. [DOI] [PubMed] [Google Scholar]
- 12.Hinojosa R, Haun J, Sberna Hinojosa M, Rittman M. Social isolation poststroke: relationship between race/ethnicity, depression, and functional independence. Top Stroke Rehabil 2015; 18: 79–86. [DOI] [PubMed] [Google Scholar]
- 13.Ostir G, Berges I, Ottenbacher M, Graham J, Ottenbacher K. Positive emotion following a stroke. J Rehabil Med 2008; 40: 477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berges I, Seale G, Ostir G. The role of positive affect on social participation following stroke. Disabil Rehabil 2012; 34: 2119–2123. [DOI] [PubMed] [Google Scholar]
- 15.Seale G, Berges I, Ottenbacher K, Ostir G. Change in positive emotion and recovery of functional status following stroke. Rehabil Psychol 2010; 55: 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cruice M, Worrall L, Hickson L, Murison R. Finding a focus for quality of life with aphasia: Social and emotional health, and psychological well-being. Aphasiology 2003; 17: 333–353. [Google Scholar]
- 17.Törnbom K, Persson H, Lundälv J, Sunnerhagen K. Self-assessed physical, cognitive, and emotional impact of stroke at 1 month: the importance of stroke severity and participation. J Stroke Cerebrovasc Dis 2017; 26: 57–63. [DOI] [PubMed] [Google Scholar]
- 18.Beckley M. Community participation following cerebrovascular accident: impact of the buffering model of social support. Am J Occup Ther 2006; 60: 129–135. [DOI] [PubMed] [Google Scholar]
- 19.Dalemans R, Witte L De, Wade D, van den Heuval W. Social participation through the eyes of people with aphasia. Int J Lang Commun Disord 2010; 45: 537–550. [DOI] [PubMed] [Google Scholar]
- 20.Andersson S, Fridlund B. The aphasic person’s views of the encounter with other people: a grounded theory analysis. J Psychiatr Ment Health Nurs 2002; 9: 285–292. [DOI] [PubMed] [Google Scholar]
- 21.Parr S. Living with severe aphasia: tracking social exclusion. Aphasiology 2007; 21: 98–123. [Google Scholar]
- 22.Hilari K. The impact of stroke: are people with aphasia different to those without? Disabil Rehabil, 2011; 33: 211–218. [DOI] [PubMed] [Google Scholar]
- 23.Desrosiers J, Noreau L, Rochette A, Bourbonnais D, Bravo G, Bourget A. Predictors of long-term participation after stroke. Disabil Rehabil 2006; 28: 221–230. [DOI] [PubMed] [Google Scholar]
- 24.Ezekiel L, Collett J, Mayo N, Pang L, Field L, Dawes H. Factors associated with participation in life situations for adults with stroke: a systematic review. Arch Phys Med Rehabil 2019; 100: 945–955. [DOI] [PubMed] [Google Scholar]
- 25.Hewetson R, Cornwell P, Shum D. Social participation following right hemisphere stroke: influence of a cognitive-communication disorder. Aphasiology 2018; 32: 164–182. [Google Scholar]
- 26.Silva SM, Corrêa JCF, Pereira GS, Corrêa FI. Social participation following a stroke: an assessment in accordance with the International Classification of Functioning, Disability and Health. Disabil Rehabil 2019; 41: 879–886. [DOI] [PubMed] [Google Scholar]
- 27.Zhang B, Shen C, Zhu Q, Ma G, Wang W. Processing of facial expressions of emotions in Antisocial, Narcissistic, and Schizotypal personality disorders: an event-related potential study. Personal Individ Differ 2016; 99: 1–6. [Google Scholar]
- 28.Borsboom D. A network theory of mental disorders. World Psychiatr 2017; 16: 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burger J, Stroebe MS, Perrig-Chiello P, Schut HA, Spahni S, Eisma MC, et al. Bereavement or breakup: Differences in networks of depression. J Affect Disord 2020; 267: 1–8. [DOI] [PubMed] [Google Scholar]
- 30.Newman ME, Barabási ALE, Watts DJ. The structure and dynamics of networks. Princeton, NJ: Princeton University Press; 2006. [Google Scholar]
- 31.Strogatz SH. Exploring complex networks. Nature 2001; 410: 268–276. [DOI] [PubMed] [Google Scholar]
- 32.Ashaie S, Hung J, Funkhouser C, Shankman S, Cherney L. Depression over time in persons with stroke: a network analysis approach. J Affect Disord Rep 2021; 4: 100131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ashaie S, Castro N. Exploring the complexity of aphasia with network analysis. J Speech Lang Hear Res 2021; 64: 3928–3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Aphasia Association . Aphasia fact sheet. [Accessed 17 January 2022]. Available from: https://www.aphasia.org/aphasia-resources/aphasia-factsheet/
- 35.Ostir G, Ottenbacher K, Kuo Y. Stroke Recovery in Underserved Populations 2005–2006 [United States]. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; [Accessed 3 May 2016]. [Google Scholar]
- 36.Ostir G, Granger C, Black T, Roberts P, Burgos L, Martinkewiz P, et al. Preliminary results for the PAR-PRO: a measure of home and community participation. Arch Phys Med Rehabil 2006; 87: 1043–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Radloff L. The CES-D Scale: A Self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. [Google Scholar]
- 38.Broadhead W, Gehlbach S, De Gruy F, Kaplan B. The Duke-UNC Functional Social Support Questionnaire: measurement of social support in family medicine patients. Med Care 1988; 26: 709–723. [DOI] [PubMed] [Google Scholar]
- 39.Keith R, Granger C, Hamilton B, Sherwin F. The Functional Independence Measure: a new tool for rehabilitation. Adv Clin Rehabil 1987; 1: 16–18. [PubMed] [Google Scholar]
- 40.Funkhouser CJ, Chacko AA, Correa KA, Kaiser AJ, Shankman SA. Unique longitudinal relationships between symptoms of psychopathology in youth: a cross- lagged panel network analysis in the ABCD study. J Child Psychol Psychiatr 2021; 62: 184–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karalunas SL, Antovich D, Goh PK, Martel MM, Tipsord J, Nousen EK, et al. Longitudinal network model of the co-development of temperament, executive functioning, and psychopathology symptoms in youth with and without ADHD. Dev Psychopathol 2021; 33: 1803–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rhemtulla M, van Bork R, Cramer A. Cross-lagged network models. Multivar Behav Res, in press; 2022. [Google Scholar]
- 43.Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw 2010; 33: 1–22. [PMC free article] [PubMed] [Google Scholar]
- 44.Epskamp S, Cramer A, Waldorp L, Schmittmann V, Borsboom D. qgraph: Network visualizations of relationships in psychometric data. J Stat Softw 2012; 45: 1–18. [Google Scholar]
- 45.Fruchterman TMJ, Reingold EM. Graph drawing by force-directed placement. Softw Pract Exp 1991; 21: 1129–1164. [Google Scholar]
- 46.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods 2018; 50: 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith F, Jones C, Gracey F, Mullis R, Coulson N, De Simoni A. Emotional adjustment post-stroke: a qualitative study of an online stroke community. Neuropsychol Rehabil 2021; 31: 414–431. [DOI] [PubMed] [Google Scholar]
- 48.Maulik PK, Eaton W, Bradshaw C. The role of social network and support in mental health service use: findings from the Baltimore ECA study. Psychiatr Serv 2009; 60: 1222–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hallquist MN, Wright AG, Molenaar PC. Problems with centrality measures in psychopathology symptom networks: why network psychometrics cannot escape psychometric theory. Multivar Behav Res 2021; 5: 199–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.You M, Fang W, Wang X, Yang T. Modelling of the ICF core sets for chronic ischemic heart disease using the LASSO model in Chinese patients. Health Qual Life Outcomes 2018; 16: 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med 2005; 37: 212–218. [DOI] [PubMed] [Google Scholar]
- 52.Cieza A, Fayed N, Bickenbach J, Prodinger B. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil 2019; 41: 574–583. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.