Abstract
Objectives
To investigate whether having a purpose in life (Ikigai) is associated with risk of cardiovascular disease (CVD) mortality and whether the association varies by employment status.
Design
Prospective cohort study.
Setting
Residents in 45 municipalities, Japan.
Participants
29 517 men and 41 984 women aged 40–79 years, free of CVD and cancer at baseline from 1988 to 1990.
Primary outcome measures
CVD mortality.
Results
During the median follow-up of 19.1 years, 4680 deaths (2393 men and 2287 women) from total CVD were observed. Greater Ikigai was associated with a lower risk of CVD mortality, and the result was stronger for men than for women. Stratified by employment status, the inverse association was confined to unemployed persons. Among unemployed persons, the multivariable HRs of total CVD were higher for moderate and high versus low levels of Ikigai. Multivariable HRs (95% CIs) were 0.74 (0.57 to 0.97) and 0.69 (0.52 to 0.93), P for trend <0.044, respectively in men, and 0.78 (0.64 to 0.95) and 0.77 (0.61 to 0.97), P for trend=0.039 in women. No association was observed among the employed, including part-time workers, self-employed and homemakers for both men and women. Such an inverse association remained even after excluding early deaths within 5 years from the baseline survey.
Conclusion
Higher levels of Ikigai were associated with a lower risk of CVD mortality, especially for unemployed men and women.
Keywords: epidemiology, occupational & industrial medicine, social medicine, stroke medicine, coronary heart disease
Strengths and limitations of this study.
Strengths included a population-based cohort study, a large sample size and a long follow-up period.
Another strength was the adjustment for many confounding factors including lifestyle habits, social and psychological factors and medical histories such as hypertension and diabetes mellitus.
Limitation was a self-administered single-item questionnaire on the purpose in life (Ikigai) to assess exposure at the baseline survey.
Introduction
Recently, there has been growing evidence that positive psychological factors, such as life satisfaction, happiness, life enjoyment, optimism and purpose in life, have been associated with favourable health outcomes, including reduced risk of cardiovascular disease (CVD), in activities of daily living, cognitive impairment and all-cause mortality.1–6 A meta-analysis of 17 studies (mainly from the USA, Canada and Europe) reported that psychological factors, such as meaning in life, purpose of life, life satisfaction, positive effect and self-esteem, were considered essential components of well-being.7 In another meta-analysis, high life purpose was associated with a 17% lower risk of all-cause mortality and cardiovascular events such as myocardial infarction, cardiac death and stroke.8
‘Ikigai’ is a Japanese concept similar to ‘purpose in life’, ‘meaning of life’, ‘life worth living’ and ‘reason to live’, which can be translated as ‘that which most makes one’s life seem worth living’.9 In Japanese, Ikigai is defined as a comprehensive concept related to life satisfaction, self-esteem, self-efficacy, morale and cognitive evaluation of the meaning of one’s life.10Ikigai involves more than enjoyment, pleasure or happiness and provides significance for one’s value in life, including subjective motivation for a living.11 In a previous prospective cohort study of 43 391 Japanese adults over 7 years’ follow-up, the presence of a sense of Ikigai was associated with decreased risk of all-cause and cardiovascular mortality among middle-aged and elderly Japanese men and women.12 A panel study of 6739 US adults aged 53–105 years over a 4-year follow-up showed that a higher level of purpose in life was associated with a 22% reduced incidence of stroke after adjustment for age, gender, race/ethnicity and socioeconomic status.13
A meta-analysis of 42 cross-sectional and prospective cohort studies providing data on more than 20 million people showed that unemployment was associated with an increased risk of all-cause mortality, with a 63% higher risk for those who experienced unemployment than those who did not.14 Unemployment status was associated with an increased incidence of cardiovascular events such as coronary heart disease and stroke associated with.15–17 A study based on a population-wide dataset of 3 084 137 Belgian individuals aged 25–59 at the 2001 census showed that unemployment status was associated with health problems such as cardiovascular, endocrine and psychiatric disorders.18 According to a study of 297 construction workers followed for 2 years, the longer the unemployment, the greater rise in blood pressure levels.19 Poor health is a direct or indirect consequence of unemployment, and this causal relationship was mediated by health behaviours such as tobacco or alcohol consumption.20–23
No study, however, has focused on the impact of Ikigai on mortality risk by employment status. We hypothesise that Ikigai positively impacts cardiovascular health even in an unemployed situation. We aimed to test this hypothesis using a long-term follow-up of a large-scale prospective cohort study of Japanese adults.
Methods
Study population
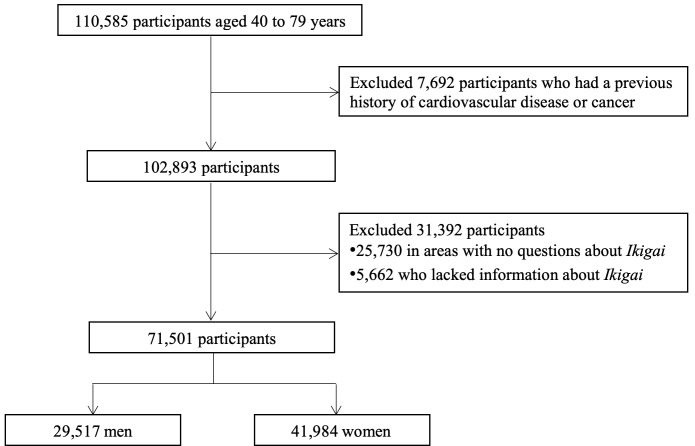
The Japan Collaborative Cohort Study for the Evaluation of Cancer Risks (JACC study) enrolled residents in 45 area around Japan between 1988 and 1990. Participants were required to conduct self-administered questionnaires about their lifestyle and medical history concerning CVD and cancer at baseline. The details of the study procedure are described elsewhere.24 Briefly, a total of 110 585 subjects (46 395 men and 64 190 women) aged 40–79 years old participated in the JACC study at the baseline survey. Among the participants, 7692 were excluded due to a history of CVD or cancer at baseline. Additionally, 31 392 (25 730 participants in areas with no questions about Ikigai and 5662 participants who lacked information about Ikigai) were excluded. Finally, 71 501 participants (29 517 men and 41 984 women) were eligible for inclusion in the analyses (figure 1). Prior to the completion of the questionnaire, the participants were provided informed consent to be involved in this epidemiological study. Individual informed consent was obtained from each participant in 36 out of the 45 study areas (written consent in 35 areas and oral consent in 1 area). In the remaining 9 areas, group consent was obtained from each community representative.
Figure 1.
Flowchart for the selection of the study participants.
Mortality surveillance
The date and cause of death for participants were determined by reviewing all death certificates from each area. According to the International Classification of Diseases, 10th revision, cause-specific mortality was defined within total CVD mortality (I01–I99). Type-specific CVD mortality was defined as I60.0–I69.8 for total stroke, I20.0–I25.5 for coronary heart disease, I50.0–I50.9 for heart failure and other CVDs. Total stroke was divided into three subtypes: cerebral infarction (I63.0–I63.9), haemorrhagic stroke (I60.0–I61.9) and stroke of undetermined type (I62.0–I62.9 and I64–I69.8). From baseline until 31 December 2009, a total of 15 801 participants were censored because of death, and 3986 were censored because they moved out of their original residential area; follow-up was terminated at the end of 1999 (four areas), 2003 (four areas) and 2008 (two areas). The median follow-up period was 19.1 years (IQR, 10.4 to 20.7).
Baseline measurement
At baseline, we used a self-administered questionnaire to obtain information on age, body mass index (BMI) (calculated by dividing body weight in kg by height m2), smoking status, alcohol consumption, sleep duration, walking time per day, sports activity time per week, education level, marital status, employment status and psychological conditions such as Ikigai, perceived mental stress, sense of life enjoyment and medical history of hypertension and diabetes mellitus. Ikigai was assessed using the question ‘How much Ikigai do you feel in your daily life?’ and responses were assessed using a four-point Likert scale: ‘low’, ‘moderate’, ‘high’ and ‘very high’. We collapsed ‘very high’ into ‘high’ for the analyses, as did previous studies.25 26 Other psychological conditions were evaluated by single-item questions using four points Likert scale.
Statistical analysis
For each participant, we calculated the person-years of follow-up from the baseline surveys between 1988 and 1990 to the first endpoint of death, moving from the community or the end of 2009. Mortality rates for CVD were estimated according to the perceived levels of Ikigai at baseline. We compared sex-specific and age-adjusted mean or prevalence of baseline risk characteristics according to perceived levels of Ikigai among participants using the linear regression or Mantel-Haenszel test.
The analysis used a Cox proportional hazards model to calculate sex-specific HRs and 95% CIs of CVD according to perceived levels of Ikigai at baseline and the risk of mortality from CVD at follow-up. The adjustment was done for age and then for other potential confounders: BMI (< 18.5, 18.5 to <25.0, 25.0–30.0, 30.0–35.0 and ≥35.0 kg/m2), smoking status (never, ex-smoker and current smoker), alcohol consumption (never, ex-drinker, 1–20 and ≥20.0 g ethanol per day), sports activity time per week (almost never, 1–2, 3–4 and ≥5 hours/week), walking time per day (almost never, 0.5, 0.6–0.9 and ≥1 hours/day), education levels (<13, 13–15, 16–18 and ≥19 years), marital status (living with a spouse, divorced, bereaved and single), sleep duration per day (<5, 5, 6, 7, 8, 9 and ≥10 hours/day), perceived mental stress (low, moderate, high, very high), sense of life enjoyment (always, sometimes, moderate, never) and medical history of hypertension and diabetes (yes or no). Missing values for these covariates were treated as additional missing categories, and the model contained these dummy variables. Furthermore, the stratified analysis was performed for six categories of employment status; employed, self-employed, part-time workers, homemakers, unemployed and others. Homemakers were regarded as the category of employed because they were primarily women, and many of them were assumed to have motivation for children and housework in Japan. In addition, we conducted a sensitivity analysis to exclude those who died early and those who moved and were censored in the first 5 years of follow-up and the type-specific CVD analysis for total stroke, ischaemic stroke, haemorrhagic stroke, stroke of undetermined type, coronary heart disease, heart failure and other CVDs. To test for linear trends across the Ikigai categories for baseline risk characteristics and HRs, ordering variable of Ikigai (1: low, 2: moderate, 3: high) was used. Probability values for statistical significance were two-tailed, and a p value <0.05 was regarded as statistically significant. The statistical analyses were carried out using SAS V.9.4 (SAS Institute, Cary, North Carolina, USA).
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Results
During a follow-up of 1 160 648 person-years, the deaths of 4680 (men and women: 2393 and 2287) due to total CVD were documented. Other deaths from major CVD types were 2053 (1047 and 1006) total strokes, 716 (398 and 318) ischaemic strokes, 739 (344 and 395) haemorrhagic strokes, 598 (305 and 293) strokes of undetermined type, 975 (550 and 425) coronary heart diseases, 792 (361 and 431) heart failures and 860 (435 and 425) other CVDs.
Table 1 shows the mean values or prevalence of cardiovascular risk factors and health behaviours at baseline according to Ikigai level. In both men and women, those with high Ikigai tended to have higher levels of the following factors: BMI, self-employed, higher education (≥16 years), current alcohol consumption, never smoking, living with a spouse, sports activity (≥1–2 hours/week), walking time (≥1 hours/day), low perceived mental stress and high life enjoyment. Unlike men, women with high Ikigai tended to be employed or part-time workers.
Table 1.
Sex-specific mean values and proportions of baseline characteristics according to the perceived levels of Ikigai
| Men | Women | |||||||
| Low | Moderate | High | PTrend | Low | Moderate | High | PTrend | |
| No. at risk, n (%) | 2197 (7.4) | 12 240 (41.5) | 15 080 (51.1) | 3819 (9.1) | 20 308 (48.4) | 17 857 (42.5) | ||
| Age, years, mean (SD) | 57.4 (10.5) | 57.2 (10.1) | 56.8 (10.2) | <0.001 | 58.1 (10.8) | 57.7 (10.0) | 56.8 (9.9) | <0.001 |
| Body mass index, kg/m2, mean (SD) | 22.5 (2.9) | 22.5 (2.8) | 22.8 (2.8) | <0.001 | 23.1 (3.5) | 22.8 (3.1) | 23.1 (3.1) | <0.001 |
| Employment status, n (%) | <0.001 | <0.001 | ||||||
| Employed | 560 (25.5) | 4658 (38.1) | 5362 (35.6) | 385 (10.1) | 2714 (13.4) | 2550 (14.3) | ||
| Self-employed | 423 (19.3) | 3860 (31.5) | 5669 (37.6) | 367 (9.6) | 3137 (15.4) | 3321 (18.6) | ||
| Part-time worker | 24 (1.1) | 267 (2.2) | 282 (1.9) | 290 (7.6) | 1987 (9.8) | 1779 (10.0) | ||
| Unemployed | 436 (19.8) | 2262 (18.5) | 1802 (11.9) | 894 (23.4) | 4364 (21.5) | 2637 (14.8) | ||
| Homemaker | 2 (0.1) | 13 (0.1) | 9 (0.1) | 685 (17.9) | 6201 (30.5) | 4908 (27.5) | ||
| Other | 752 (34.2) | 1180 (9.6) | 1956 (13) | 1198 (31.4) | 1905 (9.4) | 2662 (14.9) | ||
| Education level, n (%) | <0.001 | <0.001 | ||||||
| <16 years | 714 (48.0) | 4465 (39.1) | 4079 (30.2) | 1329 (49.8) | 7686 (40.7) | 4826 (30.6) | ||
| 16–18 years | 556 (37.4) | 5252 (46.0) | 6515 (48.3) | 1128 (42.3) | 9580 (50.7) | 8874 (56.3) | ||
| ≥19 years | 217 (14.6) | 1712 (15.0) | 2891 (21.4) | 210 (7.9) | 1639 (8.7) | 2052 (13.0) | ||
| Alcohol consumption, n (%) | <0.001 | <0.001 | ||||||
| Never | 412 (19.6) | 2225 (19.0) | 2514 (17.3) | 2691 (77.2) | 14 305 (76.2) | 12 042 (72.0) | ||
| Past | 221 (10.5) | 694 (5.9) | 738 (5.1) | 97 (2.8) | 294 (1.6) | 283 (1.7) | ||
| Current | 1468 (69.9) | 8814 (75.1) | 11 264 (77.6) | 697 (20.0) | 4173 (22.2) | 4408 (26.3) | ||
| Smoking status, n (%) | 0.007 | |||||||
| Never | 413 (19.6) | 2322 (19.9) | 3153 (21.8) | 3053 (91.6) | 16 664 (93.5) | 14 943 (93.6) | ||
| Past | 507 (24.1) | 2945 (25.2) | 3627 (25.0) | 68 (2.0) | 253 (1.4) | 214 (1.3) | ||
| Current | 1186 (56.3) | 6416 (54.9) | 7708 (53.2) | 212 (6.4) | 911 (5.1) | 814 (5.1) | ||
| Marital status, n (%) | <0.001 | <0.001 | ||||||
| Living with a spouse | 1708 (86.0) | 10 358 (93.0) | 13 424 (95.4) | 2530 (75.4) | 15 317 (83.9) | 14 081 (84.8) | ||
| Widowed | 127 (6.4) | 391 (3.5) | 368 (2.6) | 620 (18.5) | 2257 (12.4) | 2009 (12.1) | ||
| Divorced | 56 (2.8) | 182 (1.6) | 149 (1.1) | 90 (2.7) | 417 (2.3) | 344 (2.1) | ||
| Single | 95 (4.8) | 210 (1.9) | 134 (1.0) | 114 (3.4) | 276 (1.5) | 176 (1.1) | ||
| Sports activity time, n (%) | <0.001 | <0.001 | ||||||
| Never | 1705 (81.2) | 8431 (72.5) | 9060 (62.6) | 3105 (86.6) | 14 951 (79.3) | 11 876 (70.6) | ||
| 1–2 hours/week | 213 (10.1) | 1787 (15.4) | 2807 (19.4) | 272 (7.6) | 2343 (12.4) | 2803 (16.7) | ||
| 3–4 hours/week | 108 (5.1) | 721 (6.2) | 1302 (9.0) | 129 (3.6) | 851 (4.5) | 1188 (7.1) | ||
| ≥5 hours/week | 73 (3.5) | 687 (5.9) | 1307 (9.0) | 79 (2.2) | 720 (3.8) | 956 (5.7) | ||
| Walking time, n (%) | <0.001 | <0.0001 | ||||||
| Never | 294 (18.8) | 1354 (11.6) | 1307 (9.5) | 390 (14.3) | 1852 (9.7) | 1221 (7.7) | ||
| 0.5 hours/day | 302 (19.3) | 2268 (19.4) | 2453 (17.8) | 525 (19.3) | 3444 (18.0) | 2596 (16.4) | ||
| 0.5–1 hours/day | 271 (17.3) | 2339 (20.0) | 2788 (20.3) | 558 (20.5) | 4198 (21.9) | 3249 (20.5) | ||
| ≥1 hours/day | 695 (44.5) | 5757 (49.1) | 7195 (52.4) | 1246 (45.8) | 9690 (50.5) | 8777 (55.4) | ||
| Sleep duration, hours/day, mean (SD) | 7.6 (1.3) | 7.5 (1.1) | 7.4 (1.1) | 0.009 | 7.2 (1.3) | 7.1 (1.1) | 7.1 (1.0) | 0.008 |
| Perceived mental stress, n (%) | <0.001 | <0.001 | ||||||
| Low | 378 (17.7) | 1382 (11.4) | 3107 (20.9) | 541 (14.6) | 2319 (11.6) | 4300 (24.4) | ||
| Moderate | 1029 (48.1) | 8237 (68.2) | 8332 (55.9) | 1838 (49.8) | 13 907 (69.8) | 10 169 (57.6) | ||
| High | 733 (34.3) | 2451 (20.3) | 3458 (23.2) | 1315 (35.6) | 3699 (18.6) | 3184 (18.0) | ||
| Sense of life enjoyment, n (%) | <0.001 | <0.001 | ||||||
| Low | 417 (19.2) | 399 (3.3) | 193 (1.3) | 775 (20.7) | 686 (3.4) | 184 (1.0) | ||
| Moderate | 965 (44.4) | 9101 (75.0) | 5612 (37.5) | 1753 (46.7) | 15 044 (75.2) | 5937 (33.5) | ||
| High | 230 (10.6) | 2640 (21.7) | 8265 (55.2) | 315 (8.4) | 4288 (21.4) | 10 234 (57.8) | ||
| History of hypertension, n (%) | 485 (24.7) | 2305 (20.5) | 2698 (19.2) | 0.050 | 975 (28.0) | 4107 (22.3) | 3433 (20.8) | 0.188 |
| History of diabetes mellitus, n (%) | 153 (8.1) | 729 (6.6) | 895 (6.5) | 0.888 | 197 (5.9) | 735 (4.1) | 566 (3.5) | 0.062 |
Table 2 shows the sex-specific risk of mortality from total CVD according to the level of Ikigai, stratified by employment status. Men who had moderate and high Ikigai had a lower risk of mortality from total CVD than those with low Ikigai. Multivariable HRs (95% CIs) were 0.80 (0.68 to 0.93) and 0.74 (0.64 to 0.87); P for trend <0.001, respectively. A similar inverse association was observed among unemployed men, multivariable HRs (95% CIs) were 0.74 (0.57 to 0.97) and 0.69 (0.52 to 0.93); P for trend=0.044, respectively. Women who had moderate and high Ikigai levels tended to have a lower risk of mortality from total CVD than those with low Ikigai. But, tests for trend were not statistically significant: multivariable HRs (95% CI) were 0.87 (0.75 to 1.00) and 0.88 (0.76 to 1.03); P for trend=0.136, respectively. Among unemployed women, those who had moderate and high Ikigai had a lower risk of mortality from total CVD than those who had low Ikigai; tests for trend were statistically significant: multivariable HRs (95% CI) were 0.78 (0.64 to 0.95) and 0.77 (0.61 to 0.97); P for trend=0.039, respectively. No associations were observed among the unemployed, including part-time workers, self-employed and homemakers for both men and women.
Table 2.
Sex-specific, age-adjusted and multivariable HRs and 95% CIs of total cardiovascular mortality according to the perceived levels of Ikigai, stratified by employment status
| Men | Women | |||||||
| Low | Moderate | High | PTrend | Low | Moderate | High | PTrend | |
| All | ||||||||
| No. at risk | 2197 | 12 240 | 15 080 | 3819 | 20 308 | 17 857 | ||
| No. of person-years | 32 824 | 191 424 | 244 694 | 61 744 | 330 980 | 298 982 | ||
| No. of deaths | 251 | 1007 | 1135 | 307 | 1129 | 851 | ||
| Age-adjusted HR (95% CI) | 1.00 | 0.66 (0.58 to 0.76) | 0.57 (0.50 to 0.65) | <0.001 | 1.00 | 0.75 (0.66 to 0.86) | 0.68 (0.60 to 0.78) | <0.001 |
| Multivariable* HR (95% CI) | 1.00 | 0.80 (0.68 to 0.93) | 0.74 (0.64 to 0.87) | <0.001 | 1.00 | 0.87 (0.75 to 1.00) | 0.88 (0.76 to 1.03) | 0.136 |
| Employed | ||||||||
| No. at risk | 560 | 4658 | 5362 | 385 | 2714 | 2550 | ||
| No. of person-years | 9479 | 80 287 | 92 997 | 6695 | 48 860 | 46 328 | ||
| No. of deaths | 22 | 193 | 192 | 7 | 43 | 44 | ||
| Age-adjusted HR (95% CI) | 1.00 | 0.92 (0.59 to 1.44) | 0.73 (0.47 to 1.14) | 0.051 | 1.00 | 0.85 (0.38 to 1.89) | 0.89 (0.40 to 1.97) | 0.916 |
| Multivariable* HR (95% CI) | 1.00 | 1.02 (0.63 to 1.63) | 0.80 (0.49 to 1.31) | 0.116 | 1.00 | 0.82 (0.35 to 1.95) | 1.01 (0.41 to 2.48) | 0.679 |
| Self-employed | ||||||||
| No. at risk | 423 | 3860 | 5669 | 367 | 3137 | 3321 | ||
| No. of person-years | 6347 | 61 848 | 93 546 | 6025 | 53 663 | 56 797 | ||
| No. of deaths | 35 | 290 | 425 | 9 | 113 | 102 | ||
| Age-adjusted HR (95% CI) | 1.00 | 0.76 (0.54 to 1.08) | 0.71 (0.50 to 1.00) | 0.120 | 1.00 | 1.14 (0.58 to 2.25) | 0.98 (0.50 to 1.94) | 0.523 |
| Multivariable* HR (95% CI) | 1.00 | 0.86 (0.60 to 1.24) | 0.85 (0.59 to 1.22) | 0.682 | 1.00 | 1.30 (0.62 to 2.73) | 1.29 (0.60 to 2.76) | 0.782 |
| Part-time workers | ||||||||
| No. at risk | 24 | 267 | 282 | 290 | 1987 | 1779 | ||
| No. of person-years | 336 | 4037 | 4344 | 4941 | 34 182 | 30 244 | ||
| No. of deaths | 2 | 27 | 24 | 7 | 28 | 33 | ||
| Age-adjusted HR (95% CI) | 1.00 | 0.78 (0.18 to 3.28) | 0.51 (0.12 to 2.20) | 0.287 | 1.00 | 0.55 (0.24 to 1.25) | 0.73 (0.32 to 1.65) | 0.279 |
| Multivariable* HR (95% CI) | 1.00 | 0.91 (0.17 to 4.76) | 0.70 (0.12 to 4.06) | 0.762 | 1.00 | 0.88 (0.34 to 2.25) | 0.79 (0.30 to 2.04) | 0.866 |
| Homemakers | ||||||||
| No. at risk | 2 | 13 | 9 | 685 | 6201 | 4908 | ||
| No. of person-years | 33 | 164 | 137 | 10 963 | 100 252 | 80 823 | ||
| No. of deaths | 0 | 0 | 0 | 46 | 266 | 184 | ||
| Age-adjusted HR (95% CI) | – | – | – | – | 1.00 | 0.67 (0.49 to 0.91) | 0.57 (0.41 to 0.78) | 0.003 |
| Multivariable* HR (95% CI) | – | – | – | – | 1.00 | 0.83 (0.59 to 1.17) | 0.84 (0.58 to 1.22) | 0.576 |
| Unemployed | ||||||||
| No. at risk | 436 | 2262 | 1802 | 894 | 4364 | 2637 | ||
| No. of person-years | 4821 | 27 595 | 23 334 | 11 864 | 62 898 | 38 599 | ||
| No. of deaths | 84 | 368 | 250 | 145 | 555 | 306 | ||
| Age-adjusted HR (95% CI) | 1.00 | 0.63 (0.50 to 0.80) | 0.48 (0.37 to 0.61) | <0.001 | 1.00 | 0.70 (0.58 to 0.84) | 0.62 (0.51 to 0.76) | <0.001 |
| Multivariable* HR (95% CI) | 1.00 | 0.74 (0.57 to 0.97) | 0.69 (0.52 to 0.93) | 0.044 | 1.00 | 0.78 (0.64 to 0.95) | 0.77 (0.61 to 0.97) | 0.039 |
| Others | ||||||||
| No. at risk | 752 | 1180 | 1956 | 1198 | 1905 | 2662 | ||
| No. of person-years | 11 808 | 17 493 | 30 335 | 21 257 | 31 124 | 46 191 | ||
| No. of deaths | 108 | 129 | 244 | 93 | 124 | 182 | ||
| Age-adjusted HR (95% CI) | 1.00 | 0.62 (0.48 to 0.80) | 0.67 (0.53 to 0.84) | <0.001 | 1.00 | 0.81 (0.62 to 1.06) | 0.83 (0.65 to 1.06) | 0.253 |
| Multivariable* HR (95% CI) | 1.00 | 0.64 (0.47 to 0.87) | 0.76 (0.59 to 0.97) | 0.016 | 1.00 | 0.91 (0.64 to 1.29) | 1.00 (0.76 to 1.31) | 0.813 |
*Adjusted for age, body mass index, smoking status, alcohol consumption, sports activity, walking time, sleep duration, education level, employment status, marital status, sense of life enjoyment, perceived mental stress, medical history of hypertension and diabetes mellitus.
Table 3 shows the sensitivity analysis in which we censored individuals who died and those who moved during the first 5 years of follow-up, having excluded individuals who had an early death. The inverse associations did not differ materially for both men and women.
Table 3.
Sex-specific, multivariable HRs and 95% CIs of total cardiovascular mortality according to the perceived levels of Ikigai after exclusion of deaths occurred 1–5 years from the baseline among unemployed persons
| Ikigai | ||||
| Low | Moderate | High | PTrend | |
| Men | ||||
| At risk | 436 | 2262 | 1802 | |
| Person-years | 4821 | 27 595 | 23 334 | |
| No. of deaths | 84 | 368 | 250 | |
| Multivariable* HR | 1.00 | 0.74 (0.57 to 0.97) | 0.69 (0.52 to 0.93) | 0.044 |
| 79 | 358 | 243 | ||
| Deaths within 1 year exclude* | 1.00 | 0.74 (0.56 to 0.97) | 0.68 (0.51 to 0.92) | 0.044 |
| 73 | 343 | 232 | ||
| Deaths within 2 years exclude* | 1.00 | 0.77 (0.58 to 1.02) | 0.71 (0.52 to 0.96) | 0.087 |
| 67 | 318 | 223 | ||
| Deaths within 3 years exclude* | 1.00 | 0.75 (0.56 to 1.01) | 0.71 (0.52 to 0.98) | 0.104 |
| 60 | 299 | 210 | ||
| Deaths within 4 years exclude* | 1.00 | 0.78 (0.57 to 1.06) | 0.72 (0.52 to 1.01) | 0.157 |
| 56 | 282 | 201 | ||
| Deaths within 5 years exclude* | 1.00 | 0.75 (0.55 to 1.04) | 0.69 (0.49 to 0.98) | 0.115 |
| Women | ||||
| No. at risk | 894 | 4364 | 2637 | |
| No. of person-years | 11 864 | 62 898 | 38 599 | |
| No. of deaths | 145 | 555 | 306 | |
| Multivariable* HR | 1.00 | 0.78 (0.64 to 0.95) | 0.77 (0.61 to 0.97) | 0.039 |
| 138 | 540 | 299 | ||
| Deaths within 1 year excluded* | 1.00 | 0.78 (0.64 to 0.96) | 0.78 (0.62 to 0.98) | 0.056 |
| 134 | 526 | 290 | ||
| Deaths within 2 years excluded* | 1.00 | 0.79 (0.64 to 0.97) | 0.78 (0.61 to 0.98) | 0.061 |
| 125 | 498 | 281 | ||
| Deaths within 3 years excluded* | 1.00 | 0.77 (0.62 to 0.96) | 0.78 (0.61 to 1.00) | 0.057 |
| 113 | 480 | 273 | ||
| Deaths within 4 years excluded* | 1.00 | 0.81 (0.65 to 1.02) | 0.83 (0.65 to 1.08) | 0.193 |
| 112 | 462 | 267 | ||
| Deaths within 5 years excluded* | 1.00 | 0.78 (0.62 to 0.97) | 0.80 (0.62 to 1.04) | 0.092 |
*Adjusted for age, body mass index, smoking status, alcohol consumption, sports activity, walking time, sleep duration, education level, employment status, marital status, sense of life enjoyment, perceived mental stress, medical history of hypertension and diabetes mellitus.
†
Table 4 shows the risk of mortality from CVD types according to the perceived levels of Ikigai among the unemployed. Unemployed men and women with high Ikigai had lower risks of mortality from total stroke, stroke subtypes (ischaemic stroke, haemorrhagic stroke and stroke of determined type), coronary heart disease, heart failure and other CVDs than those with low Ikigai. After adjusting for CVD risk factors, the inverse association remained statistically significant for total stroke, stroke of determined type and coronary heart disease.
Table 4.
Age-adjusted and sex-adjusted and multivariable HRs and 95% CIs of mortality from type-specific cardiovascular diseases according to the perceived levels of Ikigai among unemployed persons
| Ikigai | PTrend | ||||
| Low | Moderate | High | |||
| Total stroke | No. at risk | 1330 | 6626 | 4439 | |
| No. of person-years | 16 684 | 90 493 | 61 933 | ||
| No. of deaths | 107 | 375 | 242 | ||
| Age-adjusted, sex-adjusted HR (95% CI) | 1.00 | 0.58 (0.47 to 0.72) | 0.51 (0.41 to 0.65) | <0.001 | |
| Multivariable* HR (95% CI) | 1.00 | 0.72 (0.57 to 0.91) | 0.74 (0.56 to 0.96) | 0.022 | |
| Ischaemic stroke | No. of deaths | 37 | 157 | 91 | |
| Age-adjusted, sex-adjusted HR (95% CI) | 1.00 | 0.70 (0.49 to 1.00) | 0.54 (0.37 to 0.80) | 0.007 | |
| Multivariable* HR (95% CI) | 1.00 | 0.82 (0.56 to 1.20) | 0.80 (0.51 to 1.24) | 0.555 | |
| Haemorrhagic stroke | No. of deaths | 30 | 95 | 67 | |
| Age-adjusted, sex-adjusted HR (95% CI) | 1.00 | 0.54 (0.36 to 0.82) | 0.54 (0.35 to 0.83) | 0.008 | |
| Multivariable* HR (95% CI) | 1.00 | 0.74 (0.47 to 1.19) | 0.84 (0.49 to 1.42) | 0.425 | |
| Stroke of undetermined type | No. of deaths | 40 | 123 | 84 | |
| Age-adjusted, sex-adjusted HR (95% CI) | 1.00 | 0.51 (0.36 to 0.73) | 0.47 (0.32 to 0.69) | <0.001 | |
| Multivariable* HR (95% CI) | 1.00 | 0.61 (0.41 to 0.90) | 0.61 (0.39 to 0.96) | 0.041 | |
| Coronary heart disease | No. of deaths | 43 | 196 | 99 | |
| Age-adjusted, sex-adjusted HR (95% CI) | 1.00 | 0.75 (0.54 to 1.05) | 0.51 (0.36 to 0.74) | <0.001 | |
| Multivariable* HR (95% CI) | 1.00 | 0.77 (0.54 to 1.10) | 0.64 (0.43 to 0.97) | 0.103 | |
| Heart failure | No. of deaths | 43 | 187 | 120 | |
| Age-adjusted, sex-adjusted HR (95% CI) | 1.00 | 0.73 (0.52 to 1.01) | 0.65 (0.46 to 0.92) | 0.055 | |
| Multivariable* HR (95% CI) | 1.00 | 0.90 (0.63 to 1.30) | 1.01 (0.67 to 1.52) | 0.663 | |
| Other CVDs | No. of deaths | 36 | 165 | 95 | |
| Age-adjusted, sex-adjusted HR (95% CI) | 1.00 | 0.75 (0.52 to 1.08) | 0.60 (0.40 to 0.87) | 0.023 | |
| Multivariable* HR (95% CI) | 1.00 | 0.75 (0.51 to 1.11) | 0.64 (0.42 to 1.00) | 0.144 | |
*Adjusted for age, sex, body mass index, smoking status, alcohol consumption, sports activity, walking time, sleep duration, education level, employment status, marital status, sense of life enjoyment, perceived mental stress, medical history of hypertension and diabetes mellitus.
CVD, cardiovascular disease.
Discussion
In a large prospective cohort study, higher levels of Ikigai were associated with a lower risk of mortality from total CVD among unemployed men and women after adjustment for known cardiovascular risk factors, but such as inverse association was not observed for the employed. The lower risk of CVD mortality among the unemployed was observed even after excluding early deaths within 5 years from the baseline survey. Furthermore, the risk reduction was evident for total stroke and coronary heart disease among the unemployed people.
The underlying biological mechanisms for the potential preventive effect of Ikigai on mortality from CVD remained unclear, but some reasons have been addressed. Elevated levels of inflammatory markers such as C reactive protein and interleukin-6 were associated with an increased CVD risk.27–29 A previous study using data from a 10-year panel survey of 985 adults aged 25–74 years residing in the USA showed that people with a higher purpose in life had lower physiological function scores, calculated by summarising biomarkers such as resting blood pressure, heart rate variability, low-density lipoprotein cholesterol, glycosylated haemoglobin, plasma C reactive protein, interleukin-6, urinary measures of epinephrine/norepinephrine and cortisol levels.30 Another study of 135 older women aged 61–91 years found that those with higher scores of purpose in life had lower levels of the soluble IL-6 receptor, an inflammatory marker for stroke, coronary heart disease as well as rheumatoid arthritis and Alzheimer’s disease.31
Two other prospective cohort studies using 9.1-year follow-up data for 941 persons and 6-year follow-up data for 2478 persons showed that the risk reductions associated with positive psychological factors in all-cause mortality and stroke incidence were stronger in men than in women.32 33 A previous report of the JACC study with a 12.5-year follow-up showed that men with higher Ikigai had a reduced risk of CVD mortality but not women.34 We observed a similar inverse association of CVD mortality risk in the present study and extended the evidence that the inverse association between Ikigai and CVD mortality risk was confined to unemployed men and women.
The present study has several strengths compared with previous studies. First, a population-based cohort study with a large sample size and a more extended follow-up period allowed us to assess the risk of cardiovascular mortality according to the perceived levels of Ikigai, stratified by employment status. Second, we adjusted for many confounding factors including lifestyle habits, social and psychological factors and medical histories such as hypertension and diabetes mellitus. There were some limitations to our study. First, psychological factors such as Ikigai were evaluated by a self-administered single-item questionnaire. It has been noted that Ikigai encompasses not only eudaimonic well-being, that is, well-being that pertains to internal virtue and pursuing human capacity,35 but also aspects of hedonic well-being characterised by pleasure and satisfaction not necessarily resulting from a virtuous activity.36 Unemployed persons with Ikigai were possibly likely to have available eudaimonic or hedonic well-being in their daily lives. However, the present study did not provide information on the details of Ikigai. Second, the presence of illness and preclinical conditions may have influenced Ikigai at baseline, which could lead to reverse causality. Therefore, we excluded histories of CVD and cancer and also conducted a sensitivity analysis in which individuals who died or moved during the first 5 years of follow-up were censored and found that the inverse association between Ikigai and the risk of CVD mortality remained unchanged. Lastly, although we adjusted for numerous potential confounders, some unmeasured confounders, such as the usage of medical services, may still be present. A previous study using a national panel study of 7168 US adults showed that having a purpose in life was associated with a higher likelihood of using healthcare services such as cholesterol tests, colonoscopies, mammogram/X-ray, pap smear and prostate examinations.37
Conclusion
We found that higher levels of Ikigai were associated with a lower risk of CVD mortality, specifically for unemployed men and women. Having Ikigai might be useful for the risk reduction of CVD mortality among the unemployed.
Supplementary Material
Acknowledgments
We express our sincere thanks to Dr Kunio Aoki and Dr Yoshiyuki Ohno, Professors Emeritus of the Nagoya University School of Medicine and former chairpersons of the JACC Study. We are also greatly indebted to Dr Haruo Sugano, former Director of the Cancer Institute, Tokyo, who contributed greatly to the initiation of the JACC Study; to Dr Tomoyuki Kitagawa, Director Emeritus of the Cancer Institute of the Japanese Foundation for Cancer Research and former project leader of the Grant-in-Aid for Scientific Research on Priority Area 'Cancer' and to Dr Kazao Tajima, Aichi Cancer Center, who was the previous project leader of the Grant-in-Aid for Scientific Research on Priority Area of Cancer Epidemiology. Writing Committee Members for the JACC Study Group Dr Akiko Tamakoshi (present chairperson of the study group), Hokkaido University Graduate School of Medicine; Dr Mitsuru Mori and Dr Fumio Sakauchi, Sapporo Medical University School of Medicine; Dr Yutaka Motohashi, Akita University School of Medicine; Dr Ichiro Tsuji, Tohoku University Graduate School of Medicine; Dr Yoshikazu Nakamura, Jichi Medical School; Dr Hiroyasu Iso, Osaka University School of Medicine; Dr Haruo Mikami, Chiba Cancer Center; Dr Michiko Kurosawa, Juntendo University School of Medicine; Dr Yoshiharu Hoshiyama, Yokohama Soei University; Dr Naohito Tanabe, University of Niigata Prefecture; Dr Koji Tamakoshi, Nagoya University Graduate School of Health Science; Dr Kenji Wakai, Nagoya University Graduate School of Medicine; Dr Shinkan Tokudome, National Institute of Health and Nutrition; Dr Koji Suzuki, Fujita Health University School of Health Sciences; Dr Shuji Hashimoto, Fujita Health University School of Medicine; Dr Shogo Kikuchi, Aichi Medical University School of Medicine; Dr Yasuhiko Wada, Faculty of Nutrition, University of Kochi; Dr Takashi Kawamura, Kyoto University Center for Student Health; Dr Yoshiyuki Watanabe, Kyoto Prefectural University of Medicine Graduate School of Medical Science; Dr Kotaro Ozasa, Radiation Effects Research Foundation; Dr Tsuneharu Miki, Kyoto Prefectural University of Medicine Graduate School of Medical Science; Dr Chigusa Date, School of Human Science and Environment, University of Hyogo; Dr Kiyomi Sakata, Iwate Medical University; Dr Yoichi Kurozawa, Tottori University Faculty of Medicine; Dr Takesumi Yoshimura and Dr Yoshihisa Fujino, University of Occupational and Environmental Health; Dr Akira Shibata, Kurume University; Dr Naoyuki Okamoto, Kanagawa Cancer Center and Dr Hideo Shio, Moriyama Municipal Hospital.
Footnotes
Contributors: HI and AT conceived and designed the study. JM and KS drafted the plan for the data analyses. JM and TK conducted data analysis. SI and TK provided statistical expertise and interpreted the data. JM drafted the manuscript. HI and KS analysed and interpreted the data, and critically revised the manuscript. JM, KS and HI had primary responsibility for final content. All authors were involved in the interpretation of the results and revision of the manuscript and approved the final version of the manuscripts. JM, KS and HI are guarantors.
Funding: This study has been supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (MEXT) (MonbuKagaku-sho); Grants-in-Aid for Scientific Research on Priority Areas of Cancer and Grants-in-Aid for Scientific Research on Priority Areas of Cancer Epidemiology from MEXT (Nos. 61010076, 62010074, 63010074, 1010068, 2151065, 3151064, 4151063, 5151069, 6279102, 11181101, 17015022, 18014011, 20014026, 20390156, 26293138) and JSPS KAKENHI No.16H06277. This research was also supported by Grant-in-Aid from the Ministry of Health, Labour and Welfare, Health and Labor Sciences research grants, Japan (Comprehensive Research on Cardiovascular Disease and Lifestyle Related Diseases: H20-Junkankitou [Seishuu]-Ippan-013; H23-Junkankitou [Seishuu]-Ippan-005); an Intramural Research Fund (22-4-5) for Cardiovascular Diseases of National Cerebral and Cardiovascular Center; Comprehensive Research on Cardiovascular Diseases and Lifestyle Related Diseases (H26-Junkankitou [Seisaku]-Ippan-001) and H29-Junkankitou [Seishuu]-Ippan-003 and 20FA1002.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available. The raw/processed data required to reproduce these findings cannot be shared at this time as the data also form part of an ongoing study.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the ethics committees of Hokkaido University, Hokkaido, Japan, and Osaka University, Osaka, Japan. number/ID 14285-6. Participants gave informed consent to participate in the study before taking part.
References
- 1.Collins AL, Glei DA, Goldman N. The role of life satisfaction and depressive symptoms in all-cause mortality. Psychol Aging 2009;24:696–702. 10.1037/a0016777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koivumaa-Honkanen H, Honkanen R, Viinamäki H, et al. Self-Reported life satisfaction and 20-year mortality in healthy Finnish adults. Am J Epidemiol 2000;152:983–91. 10.1093/aje/152.10.983 [DOI] [PubMed] [Google Scholar]
- 3.Steptoe A. Happiness and health. Annu Rev Public Health 2019;40:339–59. 10.1146/annurev-publhealth-040218-044150 [DOI] [PubMed] [Google Scholar]
- 4.Shirai K, Iso H, Ohira T, et al. Perceived level of life enjoyment and risks of cardiovascular disease incidence and mortality: the Japan public health Center-Based study. Circulation 2009;120:956–63. 10.1161/CIRCULATIONAHA.108.834176 [DOI] [PubMed] [Google Scholar]
- 5.Rozanski A, Bavishi C, Kubzansky LD, et al. Association of optimism with cardiovascular events and all-cause mortality: a systematic review and meta-analysis. JAMA Netw Open 2019;2:e1912200. 10.1001/jamanetworkopen.2019.12200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tomioka K, Kurumatani N, Hosoi H. Relationship of having hobbies and a purpose in life with mortality, activities of daily living, and instrumental activities of daily living among community-dwelling elderly adults. J Epidemiol 2016;26:361–70. 10.2188/jea.JE20150153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang M, Wang D, Guerrien A. A systematic review and meta-analysis on basic psychological need satisfaction, motivation, and well-being in later life: contributions of self-determination theory. Psych J 2020;9:5–33. 10.1002/pchj.293 [DOI] [PubMed] [Google Scholar]
- 8.Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: a meta-analysis. Psychosom Med 2016;78:122–33. 10.1097/PSY.0000000000000274 [DOI] [PubMed] [Google Scholar]
- 9.Mathews G. What makes life worth living? how Japanese and Americans make sense of their worlds. Berkeley: University of California Press, 1996. [Google Scholar]
- 10.Shirai K, Iso H, Fukuda H, et al. Factors associated with "Ikigai" among members of a public temporary employment agency for seniors (Silver Human Resources Centre) in Japan; gender differences. Health Qual Life Outcomes 2006;4:12. 10.1186/1477-7525-4-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss RS, Bass SA, Heimovitz HK, et al. Japan's silver human resource centers and participant well-being. J Cross Cult Gerontol 2005;20:47–66. 10.1007/s10823-005-3797-4 [DOI] [PubMed] [Google Scholar]
- 12.Sone T, Nakaya N, Ohmori K, et al. Sense of life worth living (ikigai) and mortality in Japan: Ohsaki study. Psychosom Med 2008;70:709–15. 10.1097/PSY.0b013e31817e7e64 [DOI] [PubMed] [Google Scholar]
- 13.Kim ES, Sun JK, Park N, et al. Purpose in life and reduced incidence of stroke in older adults: 'The Health and Retirement Study'. J Psychosom Res 2013;74:427–32. 10.1016/j.jpsychores.2013.01.013 [DOI] [PubMed] [Google Scholar]
- 14.Roelfs DJ, Shor E, Davidson KW, et al. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med 2011;72:840–54. 10.1016/j.socscimed.2011.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meneton P, Kesse-Guyot E, Méjean C, et al. Unemployment is associated with high cardiovascular event rate and increased all-cause mortality in middle-aged socially privileged individuals. Int Arch Occup Environ Health 2015;88:707–16. 10.1007/s00420-014-0997-7 [DOI] [PubMed] [Google Scholar]
- 16.Gallo WT. Evolution of research on the effect of unemployment on acute myocardial infarction risk. Arch Intern Med 2012;172:1737–8. 10.1001/jamainternmed.2013.1835 [DOI] [PubMed] [Google Scholar]
- 17.Brenner MH. The impact of unemployment on heart disease and stroke mortality in European Union countries. EU publications, 2016. [Google Scholar]
- 18.Vanthomme K, Gadeyne S. Unemployment and cause-specific mortality among the Belgian working-age population: the role of social context and gender. PLoS One 2019;14:e0216145. 10.1371/journal.pone.0216145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janlert U. Unemployment and blood pressure in Swedish building labourers. J Intern Med 1992;231:241–6. 10.1111/j.1365-2796.1992.tb00530.x [DOI] [PubMed] [Google Scholar]
- 20.Weden MM, Astone NM, Bishai D. Racial, ethnic, and gender differences in smoking cessation associated with employment and joblessness through young adulthood in the US. Soc Sci Med 2006;62:303–16. 10.1016/j.socscimed.2005.06.009 [DOI] [PubMed] [Google Scholar]
- 21.Janlert U. Unemployment as a disease and diseases of the unemployed. Scand J Work Environ Health 1997;23 Suppl 3:79–83. [PubMed] [Google Scholar]
- 22.Backhans MC, Balliu N, Lundin A, et al. Unemployment is a risk factor for hospitalization due to alcohol problems: a longitudinal study based on the Stockholm public health cohort (SPHC). J Stud Alcohol Drugs 2016;77:936–42. 10.15288/jsad.2016.77.936 [DOI] [PubMed] [Google Scholar]
- 23.Hammarström A. Health consequences of youth unemployment--review from a gender perspective. Soc Sci Med 1994;38:699–709. 10.1016/0277-9536(94)90460-X [DOI] [PubMed] [Google Scholar]
- 24.Tamakoshi A, Ozasa K, Fujino Y, et al. Cohort profile of the Japan collaborative cohort study at final follow-up. J Epidemiol 2013;23:227–32. 10.2188/jea.JE20120161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yasukawa S, Eguchi E, Ogino K, et al. "Ikigai", Subjective Wellbeing, as a Modifier of the Parity-Cardiovascular Mortality Association - The Japan Collaborative Cohort Study. Circ J 2018;82:1302–8. 10.1253/circj.CJ-17-1201 [DOI] [PubMed] [Google Scholar]
- 26.Tanno K, Sakata K, Japan Collaborative Cohort Study for Evaluation of Cancer . Psychological factors and mortality in the Japan collaborative cohort study for evaluation of cancer (JACC). Asian Pac J Cancer Prev 2007;8 Suppl:113–22. [PubMed] [Google Scholar]
- 27.De Martinis M, Franceschi C, Monti D, et al. Inflammation markers predicting frailty and mortality in the elderly. Exp Mol Pathol 2006;80:219–27. 10.1016/j.yexmp.2005.11.004 [DOI] [PubMed] [Google Scholar]
- 28.Harris TB, Ferrucci L, Tracy RP, et al. Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am J Med 1999;106:506–12. 10.1016/s0002-9343(99)00066-2 [DOI] [PubMed] [Google Scholar]
- 29.Reuben DB, Cheh AI, Harris TB, et al. Peripheral blood markers of inflammation predict mortality and functional decline in high-functioning community-dwelling older persons. J Am Geriatr Soc 2002;50:638–44. 10.1046/j.1532-5415.2002.50157.x [DOI] [PubMed] [Google Scholar]
- 30.Zilioli S, Slatcher RB, Ong AD, et al. Purpose in life predicts allostatic load ten years later. J Psychosom Res 2015;79:451–7. 10.1016/j.jpsychores.2015.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedman EM, Hayney M, Love GD, et al. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychol 2007;26:305–13. 10.1037/0278-6133.26.3.305 [DOI] [PubMed] [Google Scholar]
- 32.Giltay EJ, Geleijnse JM, Zitman FG, et al. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. Arch Gen Psychiatry 2004;61:1126–35. 10.1001/archpsyc.61.11.1126 [DOI] [PubMed] [Google Scholar]
- 33.Ostir GV, Markides KS, Peek MK, et al. The association between emotional well-being and the incidence of stroke in older adults. Psychosom Med 2001;63:210–5. 10.1097/00006842-200103000-00003 [DOI] [PubMed] [Google Scholar]
- 34.Tanno K, Sakata K, Ohsawa M, et al. Associations of ikigai as a positive psychological factor with all-cause mortality and cause-specific mortality among middle-aged and elderly Japanese people: findings from the Japan collaborative cohort study. J Psychosom Res 2009;67:67–75. 10.1016/j.jpsychores.2008.10.018 [DOI] [PubMed] [Google Scholar]
- 35.Ryff CD. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom 2014;83:10–28. 10.1159/000353263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trudel-Fitzgerald C, Millstein RA, von Hippel C, et al. Psychological well-being as part of the public health debate? Insight into dimensions, interventions, and policy. BMC Public Health 2019;19:1712. 10.1186/s12889-019-8029-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proc Natl Acad Sci U S A 2014;111:16331–6. 10.1073/pnas.1414826111 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available. The raw/processed data required to reproduce these findings cannot be shared at this time as the data also form part of an ongoing study.