Abstract
Genome-wide association studies unveiled the associations between the single nucleotide polymorphism rs16969968 of CHRNA5, encoding the nicotinic acetylcholine receptor alpha5 subunit (α5SNP), and nicotine addiction, cancer, and COPD independently. Here, we investigated α5SNP-induced epithelial remodeling and inflammatory response in human COPD airways. We included 26 α5SNP COPD patients and 18 wild-type α5 COPD patients in a multi-modal study. A comparative histologic analysis was performed on formalin-fixed paraffin-embedded lung tissues. Isolated airway epithelial cells from bronchial brushings were cultivated in the air-liquid interface. Broncho-alveolar fluids were collected to detect inflammatory mediators. Ciliogenesis was altered in α5SNP COPD bronchial and bronchiolar epithelia. Goblet cell hyperplasia was exacerbated in α5SNP small airways. The broncho-alveolar fluids of α5SNP COPD patients exhibited an increase in inflammatory mediators. The involvement of the rs16969968 polymorphism in airway epithelial remodeling and related inflammatory response in COPD prompts the development of innovative personalized diagnostic and therapeutic strategies.
Keywords: COPD, airways, epithelial remodeling, nicotinic receptors, rs16969968, inflammation
1. Introduction
Chronic obstructive pulmonary disease (COPD) is among the leading causes of mortality and morbidity in the world [1]. Smoking and, more generally, harmful particle inhalation are the main identified risk factors [2,3]. The remodeling of the airways and an abnormal inflammatory response are the hallmarks of COPD [4,5,6,7]. Despite numerous large genetic studies on COPD whole lungs or biological fluids [8,9,10], only alpha-1-antitrypsin deficiency has been translated into health treatment and care [11,12].
Genome-wide association studies (GWAS) linked single nucleotide polymorphisms of nicotinic acetylcholine receptors (nAchRs) to pulmonary diseases [9]. The rs16969968 polymorphism is localized at position Chr15q25.1, and codes for the CHRNA5 subunit with the modification D398N (α5SNP) [13,14,15]. Recent studies have unveiled associations between α5SNP and lung cancer [16,17,18], nicotine addiction [19], and COPD independently [20]. This is particularly important since the rs16969968 polymorphism is estimated to be present in about 60% of the worldwide population [20,21].
We previously demonstrated using in vivo, ex vivo, and in vitro approaches the contribution of α5SNP in airway epithelial remodeling and the development of emphysema in murine models, by inducing molecular and cellular changes and promoting the inflammatory response [22,23]. In addition, α5SNP nasal polyps were more inflamed and presented secretory cell hyperplasia compared to α5WT. Here, we aimed to study the role of the rs16969968 polymorphism in bronchial and bronchiolar remodeling and immune response in COPD tissues, isolated airway epithelial cells, and broncho-alveolar lavage fluids (BALF) from COPD patients.
2. Materials and Methods
2.1. Human Subjects
Patients scheduled for fiberoptic bronchoscopy and/or lung resection for cancer (University Hospital of Reims, France) were recruited prospectively (n = 44, Supplementary Materials: Table S1) following standards established and approved by the institutional review board of the University Hospital of Reims, France (IRB Reims-CHU 20110612), and included in the cohort for research and innovation in chronic inflammatory respiratory diseases (RINNOPARI, NCT02924818). The study included patients with COPD who gave their consent. At inclusion, age, sex, smoking history, and pulmonary function test results were recorded. All mild, moderate, severe, and very severe stage COPD patients were recruited for all the analyses, except for the immunohistochemistry and the immunofluorescent stainings, where only mild and moderate COPD patients were used. At inclusion, all patients were stable with no acute exacerbation of COPD for at least 4 weeks. Subjects who had ceased smoking for more than 6 months were considered former smokers.
2.2. Bronchoalveolar Lavage Fluids (BALF)
The bronchoalveolar lavage fluids were sampled as previously described [24]. We performed the inflammatory mediators’ analysis on the proximal fraction corresponding to the bronchial compartment (n = 7).
2.3. Human Primary Airway Epithelial Cell Culture
Human primary airway epithelial cells (hAEC) were obtained from bronchial brushings of COPD patients (n = 10) to establish air-liquid interface (ALI) cultures as previously described [22,24]. The cells were recovered by scraping the brushes and dissociation using trypsin-versene. They were counted with ADAM (NanoEnTek) according to NanoEnTek instructions. One hundred and fifty thousand cells were seeded on 12-well plates containing 0.4 µm Transwells (Corning, Fisher Scientific, New York, NY, USA) coated with 0.3 mg/mL collagen type IV from the human placenta (Sigma-Aldrich, Saint-Louis, MO, USA). PneumaCult-EX (PnC-Ex, Stem Cell, Vancouver, BC, Canada) medium was used for initial proliferation in the apical and basal chambers. Upon reaching cell confluency, the apical medium was removed, and the basal medium was replaced by PneumaCult-ALI (PnC-ALI, StemCell, Vancouver, BC, Canada) medium. The culture medium was changed every 2 days and the cells were kept for 15 days in incubators at 37 °C, 5% CO2.
2.4. Genotyping
Epithelial cell pellets from bronchial brushings and tissue sections (4 sections of 20 µm of thickness each) trimmed from formalin-fixed paraffin-embedded (FFPE) lung tissue blocks were processed for DNA purification using the GenElute™ FFPE RNA/DNA Purification Plus Kit, according to the manufacturer’s instructions [22]. The CHRNA5 gene was amplified with DNA polymerase TaKaRa LA Taq (TAKARA Bio Inc., Shiga, Japan) using the following primers: forward 5′-AGTCATGTAGACAGGTACTTCACTCAG-3′, reverse 5′-TGGAAGAAGATCTGCATTTG-3′. The amplification products were digested with the Taq I enzyme, recognizing the following sequence: 5′-TCGA-3′, only present in the α5WT sequence. The digestion products were then separated by agarose gel electrophoresis and the gels were imaged using a LAS-1000 Imager for analysis (Aïda software, Raytest, Courbevoie, France). Eighteen patients were α5WT (41%); 24 were heterozygous α5SNP (54.5%); and 2 were homozygous α5SNP (4.5%).
2.5. Immunohistochemistry and Immunofluorescent Stainings
Immunohistochemistry and immunofluorescent stainings were performed on FFPE lung tissues distant from the tumor (n = 24). Three μm sections were processed for hematoxylin and eosin staining and analyzed on a white light Eclipse Ci-L microscope (Nikon, Tokyo, Japan) equipped with a DS-Fi2 camera (20× Ph) to assess epithelium height in bronchi and bronchioles. The FFPE lung tissue section slides were deparaffinized and blocked with 10% BSA in PBS for 30 min at room temperature. The tissue sections were then incubated with the primary antibodies as listed in Supplementary Materials: Table S2 overnight at 4 °C in 3% BSA in PBS. After washing with PBS, a second primary antibody was used for 2 h at room temperature (antibodies are listed in Supplementary Materials: Table S2). The sections were washed with PBS and incubated with the appropriate secondary antibodies in PBS for 30 min at room temperature. The DNA was stained with DAPI for 20 min at room temperature. Images were acquired on a Zeiss AxioImageur (20× Ph) with ZEN software (v2.0.0.0 2012, Zeiss, Marly le Roi, France) and processed with ImageJ (v1.53q, National Institutes of Health, Bethesda, MD, USA) for analysis. Five random fields per section were taken for the bronchial analyses. All the structures were imaged to quantify basal cell expression, ciliated cells (primary and motile cilia), and proliferative and secretory cells (Muc5ac, Muc5b, and uteroglobin) for bronchiolar analyses. For each field, a threshold was established by subtracting the background with a rolling ball radius of 50.0 pixels, setting the minimum at 0. Basal, proliferative, and PCC were expressed as a number relative to the total area. Motile cilia are expressed as a percentage of recovery of the epithelium surface, while secretory cells as a normalized mean grey value between the two groups.
2.6. Whole-Mount Immunofluorescent Stainings
Methanol-fixed hAEC from ALI cultures were rehydrated by decreasing methanol concentrations (75%, 50%, and 25% methanol/PBT) before a post-fixation with acetone. The cells were then blocked with 10% BSA in PBT (PBS + 1% DMSO + 0.1% Triton) for 2 h at room temperature and incubated for one night at 4 °C in 3% BSA/PBT with the primary antibody anti-Arl13b (17711-1-ap, ProteinTech, Manchester, UK). The DNA was stained with DAPI for 20 min at room temperature. The clarification of the cells was achieved by a glycerol gradient (25%, 50%, and 75%) before mounting the slides. The images were acquired on a Zeiss AxioImager (20× Ph) with ZEN software (V2.0.0.0, 2012, Zeiss, Marly le Roi, France) and processed with ImageJ (v1.53q, National Institutes of Health, Bethesda, MD, USA). Primary and motile cilia recovery were quantified and related to the total area. The lengths were measured as described previously [24].
2.7. May-Grünwald-Giemsa Stainings
May-Grünwald-Giemsa (MGG) staining was performed on FFPE lung tissues (n = 11). Slides were deparaffinized and rehydrated by decreasing ethanol concentrations (100%, 95%, and 70%). Then, the slides were placed in Jenner Stain Stock solution at 50% (eosin, methylene blue, 26114-01, CliniSciences, Nanterre, France), followed by Giemsa Stain Stock solution at 6% (eosin, methylene blue, azure B, GGS500, CliniSciences, Nanterre, France). The slides were dehydrated using ethanol gradients (95% and 100%) and xylene solution before mounting. The images were acquired on a slide scanner (VS120, Olympus, Tokyo, Japan) with Olyvia software (Olympus OlyVIA 2.9, Tokyo, Japan). Bronchi were imaged and inflammatory cells, namely the eosinophils, basophils, neutrophils, and lymphocytes, were manually counted using QuPath software, Belfast, UK [25]. The epithelial length was set as a reference.
2.8. Microbiological Analysis
Endobronchial samples (bronchial aspiration or BALF, n = 15) were collected, and extended microbiological culture was performed, as previously described [26,27]. The samples and their dilutions (1/1.000 for bronchial aspiration) were cultured in Columbia blood agar, chocolate agar, Schaedler agar, and Pseudomonas selective cetrimide agar (Thermo Fisher Scientific, Waltham, MA, USA), at 37 ℃ for 48 h for aerobic and 5% CO2 cultures and 5 days for anaerobic cultures. All colonies that appeared to be morphologically distinct were quantified as colony-forming unit (CFU) per mL and identified using MALDI-TOF mass spectrometry (MALDI Biotyper®, Bruker Daltonics, Billerica, MA, USA). The α-diversity of the airway microbiota was evaluated with the Shannon index (a marker of intra-individual diversity).
2.9. Immunoblot Analysis
Cytokines and chemokines expression in BALF (1 mL, n = 3 α5WT, and n = 4 α5SNP) were assayed by a proteome profiler array according to the R&D system’s instructions (ARY022B). The final detection was obtained by streptavidin-HRP and chemiluminescence. The membranes were then imaged using a LAS-4000 gel imager (Fujifilm, Tokyo, Japan) for analyses (Supplemental Figure S5). The detected signals were digitally quantified using ImageJ. The values were normalized to the positive and negative controls for each membrane. A cut-off was applied considering an interval of 5% between the mean grey values of the range of positive minus negative controls. All inflammatory mediators whose expression was lower than this value were considered undetected. The α5SNP expression was normalized to α5WT and reported to 1. The abundance represented the quantities of inflammatory mediators’ expression in the BALF of COPD patients, including α5WT and α5SNP. It was defined by standardizing the difference between the positive and negative controls of both α5WT and α5SNP COPD patients. All the inflammatory mediators’ expression values were calibrated on this difference in expression in the two groups and then normalized to their negative control. The results were expressed as mean values of each group and reported in the heatmap according to their abundance in BALF. Very high: comparative detection higher than 50% of positive control; high: between 50 and 25%; medium: between 25 and 10%; low: between 10 and 5%; and very low: less than 5%.
2.10. Statistics
The data are expressed as mean values ± SEM, and percentages. Differences between groups were determined using the Student’s t-test one-tailed or to the hypothetical value of 1.00, representing the reference for the α5WT subjects. For microbiological analysis, Mann–Whitney and Fisher’s tests were used. A p-value < 0.05 was considered significant.
3. Results
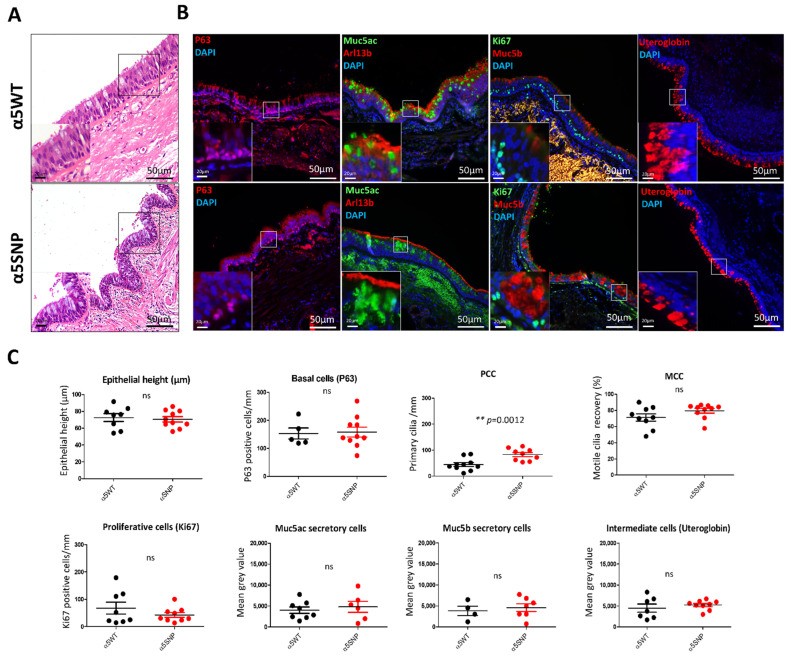
We first analyzed the impact of α5SNP on bronchial remodeling, using genotyped lung tissues obtained from COPD patients. The epithelial height and proliferation index did not differ between α5SNP and α5WT respiratory epithelia (Figure 1).
Figure 1.
Bronchial epithelial remodeling in rs16969968 (α5SNP) COPD patients. (A): Hematoxylin and eosin staining showing the epithelial height of α5SNP and α5WT COPD patients. (B): Examples of the microscopic acquisition of immunofluorescent stainings for basal cells (P63, red), ciliated cells (Arl13b, red), proliferative cells (Ki67, green), mucins secretory cells (Muc5ac, green; Muc5b, red), and intermediate cells (Uteroglobin, red). Nuclei are stained in blue (DAPI). Magnification corresponding to the selected area is represented. (C): Dot plots (means with SEM) representing measurements of the epithelial height, the number of basal, proliferative, and primary ciliated cells per mm, motile cilia recovery (%), and the mean grey values of mucins (Muc5ac, Muc5b) and uteroglobin-associated fluorescence of α5SNP and α5WT COPD patients. **, p <0.01 α5WT vs. α5SNP; ns, non-significant.
Interestingly, there was a 54% increase in primary ciliated cells (PCC) (83.30 ± 7.69 PCC/mm of epithelium vs. 44.94 ± 7.66, p < 0.01) in α5SNP COPD epithelia (Figure 1b,c and Supplementary Materials: Figure S1). Mucins secretory cells were also increased in α5SNP but did not reach statistical significance (Figure 1b,c). Basal, multiciliated (MCC), and intermediate cells were equally distributed (Figure 1b,c). We further assessed cilia alterations in α5SNP COPD bronchial airway epithelial cells (AEC) isolated from bronchial brushes. There was no difference in the numbers of basal, MCC, and Muc5ac secretory cells between α5SNP and α5WT AEC (Supplementary Materials: Figure S2). Since PCCs are rapidly disassembled in the fresh AEC isolation, we cultured AEC in air-liquid interface (ALI) conditions. We confirmed the alteration of primary ciliogenesis during differentiation with a 67% increase of PCC (75.25 ± 3.23% vs. 50.56 ± 2.61%, p < 0.05) in α5SNP COPD patients compared to α5WT (Supplementary Materials: Figure S3).
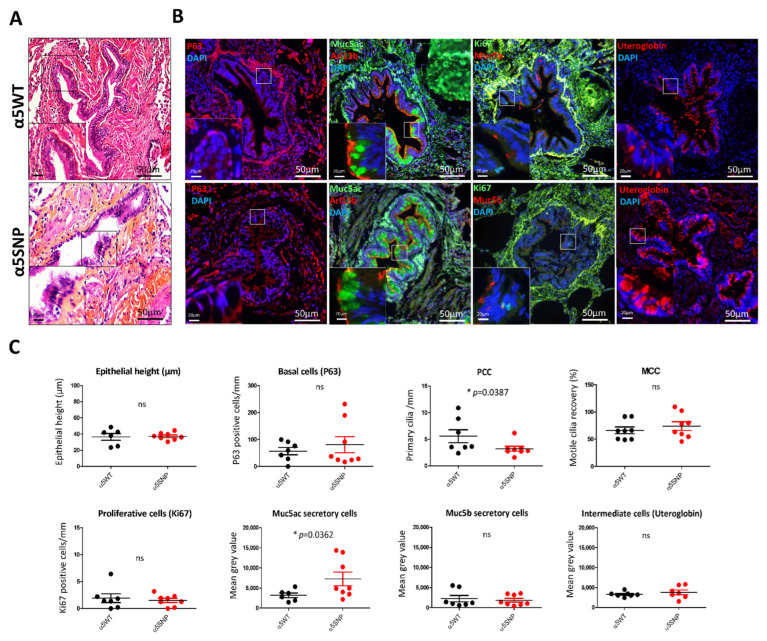
Given that COPD is also considered a small airway disease, we assessed bronchiolar remodeling [28]. The epithelial height and proliferation index did not differ between the two groups (Figure 2a,c).
Figure 2.
Bronchiolar epithelial remodeling in rs16969968 (α5SNP) COPD patients. (A): Hematoxylin and eosin staining showing the epithelial height of α5SNP and α5WT COPD patients. (B): Examples of the microscopic acquisition of immunofluorescent stainings for basal cells (P63, red), ciliated cells (Arl13b, red), proliferative cells (Ki67, green), mucins secretory cells (Muc5ac, green; Muc5b, red), and intermediate cells (Uteroglobin, red). Nuclei are stained in blue (DAPI). Magnification corresponding to the selected area is represented. (C): Dot plots (means with SEM) representing measurements of the epithelial height, the number of basal, proliferative, and primary ciliated cells per mm, motile cilia recovery (%), and the mean grey values of mucins (Muc5ac, Muc5b) and uteroglobin-associated fluorescence of α5SNP and α5WT COPD patients. *, p < 0.05 α5WT vs. α5SNP; ns, non-significant.
In contrast, when compared with α5WT, α5SNP bronchiolar epithelium was characterized by a 57% decrease in the number of PCC (3.21 ± 0.46 PCC/mm of epithelium vs. 5.59 ± 1.21, p < 0.05) and a 44% increase in Muc5ac secretory cells (7236 mean grey value ± 1717 vs. 3171 ± 583.3, p < 0.05) (Figure 2b,c). The basal, MCC, and intermediate cells were not affected (Figure 2b,c).
We next analyzed the airway microbiota using an extended culture approach and mass spectrometry identification [29]. There was no difference between the α5SNP and α5WT COPD patients’ airway microbiota regarding bacterial distribution and microbiota diversity (Supplementary Materials: Figure S4).
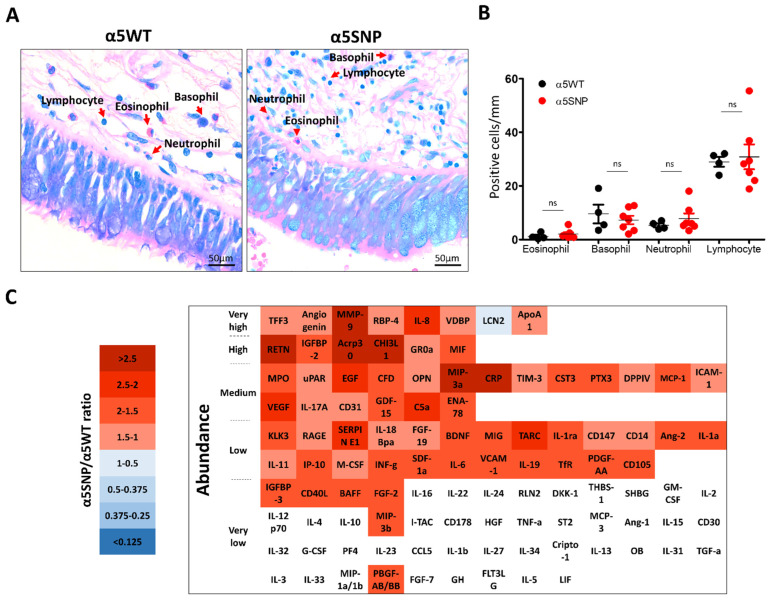
Finally, we analyzed peribronchial recruitment of inflammatory populations (basophils, eosinophils, neutrophils, and lymphocytes), and inflammatory mediators’ (pro- and anti-inflammatory) secretions in BALF obtained from α5SNP and α5WT COPD patients in the proximal compartment (Supplementary Materials: Figure S5). There was no difference in the immune cell distribution (Figure 3a,b).
Figure 3.
Lung inflammatory response in rs16969968 (α5SNP) COPD patients. (A): Microscopic acquisitions showing peribronchial recruitment of immune populations in α5SNP and α5WT COPD patients. (B): Dot plot showing the number of eosinophils, basophils, neutrophils, and lymphocytes per mm of epithelium in α5SNP vs. α5WT COPD patients. (C): Heatmap presenting the ratios of inflammatory mediators’ expression in broncho-alveolar lavage fluids of α5SNP vs. α5WT COPD patients. Downregulated inflammatory mediators are presented in blue, and upregulated ones are in red. The inflammatory mediators whose expression is lower than the detection cut-off value (5% of positive control) are identified in white. The inflammatory mediators are categorized according to their detected abundance in the broncho-alveolar lavage fluids of COPD patients (from very high, >50% of the detection of the positive control; to very low, <5% of the detection of the positive control). ns, non-significant.
TFF3, angiogenin, MMP-9, IL-8, RBP-4, VDBP, Apo-A1, and LCN2 were the most abundant inflammatory mediators detected in COPD patients (Figure 3c). Sixty-two were upregulated in α5SNP COPD BALF (Figure 3c), while total cell counts were similar and below 300,000 cells/mL (data not shown). Six inflammatory mediators (MMP-9, RETN, Acrp30, CHI3L1, MIP-3a, and CRP) were more than 2.5 times upregulated in α5SNP COPD BALF (Figure 3c, and Supplementary Materials: Figure S6).
4. Discussion
Taken together, our findings highlight an impairment of PCC and Muc5ac secretory cells in α5SNP COPD patients’ epithelia and dysregulation of inflammatory mediators’ production. We could not evaluate PCC in our previous studies because of the sparsity of basal cells in mice airways. Nonetheless, the epithelial remodeling and the alteration of the inflammatory response were consistent [23]. Further clinical investigations will focus on the quantification of human lung inflammatory populations in α5SNP COPD patients.
Primary cilia are sensor organelles playing a crucial role in cellular development (proliferation and differentiation) and the reparation process. Anomalies in the structure and/or functions of cilia are responsible for ciliopathies [30]. The number of primary cilia is increased in the bronchial epithelium and decreased in the bronchiolar epithelium of α5SNP COPD patients, suggesting an alteration of the progenitor cell fate toward an arrest of the cell cycle or a loss of stemness. The apparent discrepancy in PCC pointed towards the dual functions of non-differentiated cells in various airway compartments: the alteration of primary cilia may inhibit epithelial repair in bronchi, while it may induce bronchiolar remodeling. These findings are consistent with our previous work regarding the role of primary cilia in COPD pathogenesis and support the implication of α5SNP in airway plasticity in COPD [31,32].
Mucins play an important role as innate immune mediators. They are involved in the clearance of microorganisms and pollutants. The increase of Muc5ac secretion in bronchiolar epithelium without changes in motile cilia recovery suggests an accumulation of mucus in the airway, leading to the airway obstruction described in COPD [33,34,35].
Despite no difference in peribronchial recruitment of inflammatory populations between α5SNP and α5WT COPD BALF, six inflammatory mediators were highly upregulated in α5SNP COPD BALF, including MMP-9 and CHI3L1, which are associated with lung remodeling; Acrp30 and CRP, both markers of systemic inflammation; and MIP-3a, which is indirectly related to the activation of NF-kB and STAT3 signaling pathways [36]. Moreover, the large upregulation of detected inflammatory mediators highlights a global dysregulation of the immune response [22,37].
Our analyses were limited by the small sample size for each parameter, although we included a total of 44 patients. There were only two homozygous α5SNP patients (one fiberoptic bronchoscopy and one lung resection), therefore we could not evaluate the additive effect of the polymorphism. We focused on bronchial and bronchiolar remodeling, but it would also be important to investigate alveolar remodeling to complete the analysis. Despite these limitations, we report the first cellular and molecular clues deciphering the genetic impact of α5SNP in COPD patients.
These findings support the involvement of the rs16969968 polymorphism in airway epithelial remodeling and related inflammatory response in COPD patients. The characterization of rs16969968 may contribute to the development of innovative personalized diagnostic and therapeutic strategies in COPD.
Acknowledgments
We thank the members of the Inserm UMR-S 1250 unit and our collaborators for their helpful comments and insights. We thank the Platform of Cell and Tissue Imaging (PICT) for technical assistance. This research was carried out in the framework of the Federative Research Structure CAP-Santé and benefited from the Project Research and Innovation in Inflammatory Respiratory Diseases (RINNOPARI).
Abbreviations
| BALF | Broncho-alveolar lavage fluids |
| COPD | Chronic obstructive pulmonary disease |
| FFPE | Formalin-fixed paraffin-embedded |
| GWAS | Genome-wide association studies |
| hAEC | human Airway epithelial cell |
| MGG | May-Grünwald-Giemsa |
| nAChR | Nicotinic acetylcholine receptor |
| SNP | Single-nucleotide polymorphism |
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cells11192937/s1, Figure S1: Identification of primary ciliated cells in bronchial epithelia of α5SNP and α5WT COPD patients; Figure S2: Impact of polymorphism rs16969968 (α5SNP) on cellular distribution in the bronchial epithelium in freshly isolated airway epithelial cells as collected previously [24]; Figure S3: Impact of polymorphism rs16969968 (α5SNP) on cellular differentiation in the bronchial epithelium in human AEC air-liquid interface cultures after 15 days as collected previously [24]; Figure S4: Impact of polymorphism rs16969968 (α5SNP) on bacterial airway microbiota in COPD patients; Figure S5: Inflammatory mediators’ detection in BALF of α5SNP and α5WT COPD patients; Figure S6: Impact of polymorphism rs16969968 (α5SNP) on inflammatory mediators’ detection in BALF of COPD patients; Table S1: characteristics of patients; Table S2: list of antibodies.
Author Contributions
Conceptualization, V.D.; methodology, L.S.C., J.-M.P., A.M., T.G., G.D. (Gaëtan Deslée) and V.D.; validation, L.S.C., G.D. (Gaëtan Deslée) and V.D.; formal analysis, L.S.C., J.-M.P., A.M., T.G., G.D. (Gaëtan Deslée) and V.D.; investigation, L.S.C., Z.D., J.-M.P., J.A., L.M.G.P., M.A.D., A.B., N.L., A.M., T.G. and V.D.; resources, J.-M.P., J.A., G.D. (Gonzague Delepineand), M.P., A.M., T.G. and G.D. (Gaëtan Deslée); data curation, J.-M.P., M.P., A.M., T.G. and G.D. (Gaëtan Deslée); writing—original draft preparation, L.S.C. and V.D.; writing—review and editing, L.S.C., Z.D., J.-M.P., J.A., L.M.G.P., M.A.D., A.B., U.M., P.G., M.P., A.M., T.G., G.D. (Gaëtan Deslée) and V.D.; visualization, L.S.C. and V.D.; supervision, G.D. (Gaëtan Deslée) and V.D.; project administration, V.D.; funding acquisition, U.M., P.G., M.P., G.D. (Gaëtan Deslée) and V.D. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Subjects were recruited from the Department of Pulmonary Medicine at the University Hospital of Reims (France) and included in the cohort for Research and Innovation in Chronic Inflammatory Respiratory Diseases (RINNOPARI, NCT02924818). The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee for the protection of human beings involved in biomedical research (CCP Dijon EST I, N°2016-A00242-49, June 2016).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data generated or analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
Deslée reports personal fees from Nuvaira, personal fees from BTG/PneumRx, personal fees from Chiesi, personal fees from Boehringer, and personal fees from Astra Zeneca, outside the submitted work. Dormoy reports personal fees from Chiesi and Astra Zeneca outside the submitted work. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research was funded by the University of Reims Champagne-Ardenne (URCA), the French National Institute of Health and Medical Research (Inserm) and a grant from the Research Institute in Public Health (IReSP) in association with the National Institute of Cancer (INCa) (IRESP-19-PINACRAECOPD).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.López-Campos J.L., Tan W., Soriano J.B. Global burden of COPD. Respirology. 2016;21:14–23. doi: 10.1111/resp.12660. [DOI] [PubMed] [Google Scholar]
- 2.Christenson S.A., Smith B.M., Bafadhel M., Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022;399:2227–2242. doi: 10.1016/S0140-6736(22)00470-6. [DOI] [PubMed] [Google Scholar]
- 3.Gaffney A., Christiani D.C. Gene–Environment Interaction from International Cohorts: Impact on Development and Evolution of Occupational and Environmental Lung and Airway Disease. Semin. Respir. Crit. Care Med. 2015;36:347–357. doi: 10.1055/s-0035-1549450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brightling C., Greening N. Airway inflammation in COPD: Progress to precision medicine. Eur. Respir. J. 2019;54:1900651. doi: 10.1183/13993003.00651-2019. [DOI] [PubMed] [Google Scholar]
- 5.Lu Z., Van Eeckhoutte H.P., Liu G., Nair P.M., Jones B., Gillis C.M., Nalkurthi B.C., Verhamme F., Buyle-Huybrecht T., Vandenabeele P., et al. Necroptosis Signaling Promotes Inflammation, Airway Remodeling, and Emphysema in Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2021;204:667–681. doi: 10.1164/rccm.202009-3442OC. [DOI] [PubMed] [Google Scholar]
- 6.Vitenberga Z., Pilmane M., Babjoniševa A. An Insight into COPD Morphopathogenesis: Chronic Inflammation, Remodeling, and Antimicrobial Defense. Medicina. 2019;55:496. doi: 10.3390/medicina55080496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y., Xu J., Meng Y., Adcock I.M., Yao X. Role of inflammatory cells in airway remodeling in COPD. Int. J. Chronic Obstr. Pulm. Dis. 2018;13:3341–3348. doi: 10.2147/COPD.S176122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lam D.C.-L., Luo S.Y., Fu K.-H., Lui M.M.-S., Chan K.-H., Wistuba I.I., Gao B., Tsao S.-W., Ip M.S.-M., Minna J.D. Nicotinic acetylcholine receptor expression in human airway correlates with lung function. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2016;310:L232–L239. doi: 10.1152/ajplung.00101.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shrine N., Guyatt A.L., Erzurumluoglu A.M., Jackson V.E., Hobbs B.D., Melbourne C.A., Batini C., Fawcett K.A., Song K., Sakornsakolpat P., et al. New genetic signals for lung function highlight pathways and chronic obstructive pulmonary disease associations across multiple ancestries. Nat. Genet. 2019;51:481–493. doi: 10.1038/s41588-018-0321-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilk J.B., Shrine N.R.G., Loehr L.R., Zhao J.H., Manichaikul A., Lopez L.M., Smith A.V., Heckbert S.R., Smolonska J., Tang W., et al. Genome-Wide Association Studies Identify CHRNA5/3 and HTR4 in the Development of Airflow Obstruction. Am. J. Respir. Crit. Care Med. 2012;186:622–632. doi: 10.1164/rccm.201202-0366OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strange C. Alpha-1 Antitrypsin Deficiency Associated COPD. Clin. Chest Med. 2020;41:339–345. doi: 10.1016/j.ccm.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Strnad P., McElvaney N.G., Lomas D.A. Alpha1-Antitrypsin Deficiency. N. Engl. J. Med. 2020;382:1443–1455. doi: 10.1056/NEJMra1910234. [DOI] [PubMed] [Google Scholar]
- 13.Bierut L.J., Stitzel J., Wang J.C., Hinrichs A.L., Grucza R., Xuei X., Saccone N.L., Saccone S.F., Bertelsen S., Fox L., et al. Variants in Nicotinic Receptors and Risk for Nicotine Dependence. Am. J. Psychiatry. 2008;165:1163–1171. doi: 10.1176/appi.ajp.2008.07111711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maskos U. The nicotinic receptor alpha5 coding polymorphism rs16969968 as a major target in disease: Functional dissection and remaining challenges. J. Neurochem. 2020;154:241–250. doi: 10.1111/jnc.14989. [DOI] [PubMed] [Google Scholar]
- 15.Weiss R.B., Baker T.B., Cannon D.S., von Niederhausern A., Dunn D.M., Matsunami N., Singh N.A., Baird L., Coon H., McMahon W.M., et al. A Candidate Gene Approach Identifies the CHRNA5-A3-B4 Region as a Risk Factor for Age-Dependent Nicotine Addiction. PLoS Genet. 2008;4:e1000125. doi: 10.1371/journal.pgen.1000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amos C.I., Wu X., Broderick P., Gorlov I.P., Gu J., Eisen T., Dong Q., Zhang Q., Gu X., Vijayakrishnan J., et al. Genome-wide association scan of tag SNPs identifies a susceptibility locus for lung cancer at 15q25.1. Nat. Genet. 2008;40:616–622. doi: 10.1038/ng.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hung R.J., McKay J.D., Gaborieau V., Boffetta P., Hashibe M., Zaridze D., Mukeria A., Szeszenia-Dabrowska N., Lissowska J., Rudnai P., et al. A susceptibility locus for lung cancer maps to nicotinic acetylcholine receptor subunit genes on 15q25. Nature. 2008;452:633–637. doi: 10.1038/nature06885. [DOI] [PubMed] [Google Scholar]
- 18.Thorgeirsson T.E., Geller F., Sulem P., Rafnar T., Wiste A., Magnússon K.P., Manolescu A., Thorleifsson G., Stefansson H., Ingason A., et al. A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature. 2008;452:638–642. doi: 10.1038/nature06846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Tobacco and Genetics Consortium Genome-wide meta-analyses identify multiple loci associated with smoking behavior. Nat. Genet. 2010;42:441–447. doi: 10.1038/ng.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hopkins R.J., Duan F., Gamble G.D., Chiles C., Cavadino A., Billings P., Aberle D., Young R.P. Chr15q25 genetic variant (rs16969968) independently confers risk of lung cancer, COPD and smoking intensity in a prospective study of high-risk smokers. Thorax. 2021;76:272–280. doi: 10.1136/thoraxjnl-2020-214839. [DOI] [PubMed] [Google Scholar]
- 21.Pillai S.G., Ge D., Zhu G., Kong X., Shianna K.V., Need A., Feng S., Hersh C.P., Bakke P., Gulsvick A., et al. A Genome-Wide Association Study in Chronic Obstructive Pulmonary Disease (COPD): Identification of Two Major Susceptibility Loci. PLoS Genet. 2009;5:e1000421. doi: 10.1371/journal.pgen.1000421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diabasana Z., Perotin J.-M., Belgacemi R., Ancel J., Mulette P., Launois C., Delepine G., Dubernard X., Mérol J.-C., Ruaux C., et al. Chr15q25 Genetic Variant rs16969968 Alters Cell Differentiation in Respiratory Epithelia. Int. J. Mol. Sci. 2021;22:6657. doi: 10.3390/ijms22136657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Routhier J., Pons S., Freidja M.L., Dalstein V., Cutrona J., Jonquet A., Lalun N., Mérol J.-C., Lathrop M., Stitzel J.A., et al. An innate contribution of human nicotinic receptor polymorphisms to COPD-like lesions. Nat. Commun. 2021;12:6384. doi: 10.1038/s41467-021-26637-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ancel J., Belgacemi R., Perotin J.-M., Diabasana Z., Dury S., Dewolf M., Bonnomet A., Lalun N., Birembaut P., Polette M., et al. Sonic hedgehog signalling as a potential endobronchial biomarker in COPD. Respir. Res. 2020;21:207. doi: 10.1186/s12931-020-01478-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bankhead P., Loughrey M.B., Fernández J.A., Dombrowski Y., McArt D.G., Dunne P.D., McQuaid S., Gray R.T., Murray L.J., Coleman H.G., et al. QuPath: Open source software for digital pathology image analysis. Sci. Rep. 2017;7:16878. doi: 10.1038/s41598-017-17204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Einarsson G.G., Ronan N.J., Mooney D., McGettigan C., Mullane D., NiChroinin M., Shanahan F., Murphy D.M., McCarthy M., McCarthy Y., et al. Extended-culture and culture-independent molecular analysis of the airway microbiota in cystic fibrosis following CFTR modulation with ivacaftor. J. Cyst. Fibros. 2021;20:747–753. doi: 10.1016/j.jcf.2020.12.023. [DOI] [PubMed] [Google Scholar]
- 27.Sherrard L.J., Einarsson G., Johnston E., O’Neill K., McIlreavey L., McGrath S.J., Gilpin D.F., Downey D., Reid A., McElvaney N.G., et al. Assessment of stability and fluctuations of cultured lower airway bacterial communities in people with cystic fibrosis. J. Cyst. Fibros. 2019;18:808–816. doi: 10.1016/j.jcf.2019.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McDonough J.E., Yuan R., Suzuki M., Seyednejad N., Elliott W.M., Sanchez P.G., Wright A.C., Gefter W.B., Litzky L., Coxson H.O., et al. Small-Airway Obstruction and Emphysema in Chronic Obstructive Pulmonary Disease. N. Engl. J. Med. 2011;365:1567–1575. doi: 10.1056/NEJMoa1106955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muggeo A., Perotin J.-M., Brisebarre A., Dury S., Dormoy V., Launois C., Ancel J., Mulette P., de Champs C., Deslée G., et al. Extended Bacteria Culture-Based Clustering Identifies a Phenotype Associating Increased Cough and Enterobacterales in Stable Chronic Obstructive Pulmonary Disease. Front. Microbiol. 2021;12:781797. doi: 10.3389/fmicb.2021.781797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Braun D.A., Hildebrandt F. Ciliopathies. Cold Spring Harb. Perspect. Biol. 2017;9:a028191. doi: 10.1101/cshperspect.a028191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perotin J.-M., Coraux C., Lagonotte E., Birembaut P., Delépine G., Polette M., Deslee G., Dormoy V. Alteration of primary cilia in COPD. Eur. Respir. J. 2018;52:1800122. doi: 10.1183/13993003.00122-2018. [DOI] [PubMed] [Google Scholar]
- 32.Perotin J.-M., Polette M., Deslée G., Dormoy V. CiliOPD: A ciliopathy-associated COPD endotype. Respir. Res. 2021;22:74. doi: 10.1186/s12931-021-01665-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma J., Rubin B.K., Voynow J.A. Mucins, Mucus, and Goblet Cells. Chest. 2018;154:169–176. doi: 10.1016/j.chest.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 34.Radicioni G., Ceppe A., Ford A.A., E Alexis N., Barr R.G., Bleecker E.R., Christenson S.A., Cooper C.B., Han M.K., Hansel N.N., et al. Airway mucin MUC5AC and MUC5B concentrations and the initiation and progression of chronic obstructive pulmonary disease: An analysis of the SPIROMICS cohort. Lancet Respir. Med. 2021;9:1241–1254. doi: 10.1016/S2213-2600(21)00079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dunican E.M., Elicker B.M., Henry T., Gierada D.S., Schiebler M.L., Anderson W., Barjaktarevic I., Barr R.G., Bleecker E.R., Boucher R.C., et al. Mucus Plugs and Emphysema in the Pathophysiology of Airflow Obstruction and Hypoxemia in Smokers. Am. J. Respir. Crit. Care Med. 2021;203:957–968. doi: 10.1164/rccm.202006-2248OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Imaizumi Y., Sugita S., Yamamoto K., Imanishi D., Kohno T., Tomonaga M., Matsuyama T. Human T cell leukemia virus type-I Tax activates human macrophage inflammatory protein-3α/CCL20 gene transcription via the NF-κB pathway. Int. Immunol. 2002;14:147–155. doi: 10.1093/intimm/14.2.147. [DOI] [PubMed] [Google Scholar]
- 37.Burgoyne R.A., Fisher A.J., Borthwick L.A. The Role of Epithelial Damage in the Pulmonary Immune Response. Cells. 2021;10:2763. doi: 10.3390/cells10102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during the current study are available from the corresponding author upon reasonable request.