Abstract
Background:
Dietary quality indices are practical as an instrument to investigate the extent of adhering to a special diet to prevent cardiovascular disease (CVD) in type 2 diabetes mellitus (T2DM). Considering the lack of any systematic review with regards to this issue, our aim was to examine observational studies to test the relationship between dietary quality indices and CVD risk factors in T2DM.
Methods:
Systematic search was performed in Web of knowledge, PubMed, Cochrane, Science direct, Google Scholar and Scopus databases from January 1990 to July 2020. The studies exploring the relationship between dietary quality indices (diet quality score (DQS), dietary diversity score (DDS), healthy diet indicator (HDI), healthy eating index (HEI), diet quality index (DQI), Mediterranean diet score (MDS)) and lipid profile, anthropometric indices, glucose profile as well as blood pressure were eligible to be included in this review. Overall, mean changes, odd ratio (RR), correlation coefficients, and beta coefficient of outcomes were extracted, with the quality assessment of studies performed applying The Newcastle-Ottawa scale.
Results:
From among 1627 papers, 10 articles were included: Eight cross-sectional and two prospective (cohort) studies. The association between HEI as well as MDS and CVD risk factors was more evident in the included studies. Fasting blood sugar, hemoglobin A1c, body mass index, and waist circumference revealed the greatest inverse significant relationship with dietary quality indices in adults with T2DM.
Conclusion:
Overall, the findings of this study suggest that the level of CVD risk factors in T2DM decreases significantly with increase in the score of dietary quality indices. Further studies in future are required to confirm these findings.
Keywords: Cardiovascular diseases, diabetes mellitus, diet, food quality.
Introduction
Diabetes is known as a prevalent metabolic disease. This disorder is a developing hazard and serious world health organization (WHO) alarm as a risk factor for cardiovascular disease (CVD).[1,2] Poor blood glucose control can lead to multiple critical complications, such as cardiovascular disturbances, retinopathy, and renal failure.[3] CVD such as hypertension and myocardial ischemia is considered as the most common cause of death worldwide.[4,5] Family history, genetics, and lifestyle factors, identified as the major modifiable agents, can have significant effects on the progress of type 2 diabetes (T2DM) and CVD.[6]
Nutritional status is an adjustable environmental factor of diabetes, and nutrition therapy plays a substantial role in preventing the associated complications.[7] Based on the reaction between nutritious elements and synergistic effects of micro- and macronutrients in a complete diet, previous studies have aimed to reveal the relationship between dietary quality indices and chronic diseases.[8,9] The Diet Quality Index-International (DQI-I; based on the worldwide national dietary guidelines), The Healthy Diet Indicator (HDI; according to the World Health Organization dietary guidelines), the Healthy Eating Index-2010 (HEI-2010; based on the Food Guide Pyramid), and Mediterranean Diet Score (MDS; based on the Mediterranean eating pattern) are four quality indices.[10,11] Overall, diet quality indices recommend use of healthy nutrients groups, such as fruits, essential fatty acids, legumes, cereals, fish and vegetables, as well as sustaining variety, moderation, and balance in nutrients intake.[12]
Epidemiological evidence has indicated that a higher adherence to the diet quality indices was inversely correlated with the risk of obesity, CVD, diabetes, metabolic syndrome, and cancer.[9,13,14] However, some previous reports suggest that the results obtained from different studies on measuring the relationship between dietary quality and some cardiovascular disease risk factors differ across various populations.[11,15,16] Although investigation of the current databases indicates that so far no systematic review has been done for assessing the relationship between diet quality indices and cardiovascular disease risk factors in T2DM patients, a systematic review in 2017 by investigating 34 papers indicated that some indicators of dietary quality such as HEI have an inverse relationship with obesity in healthy individuals.[17]
Concerning the synergistic effect of each of the cardiovascular risk factors in T2DM patients and the increase in the prevalence of these factors, it seems that a systematic review is required to examine the relationship between diet quality indices and the most important CVD risk factors in T2DM patients. The results of the present study can be practical in modifying the dietary quality of T2DM patients and in preventing from this disease.
Materials and Methods
Study protocol
The current study was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)[18] and was registered in the PROSPERO with the code of CRD42020191933. According to the current study design, ethical approval was not required due to the local regulations.
Inclusion and exclusion criteria
Studies were required to meet the inclusion criteria as follows: 1) Studies that were published as an original research paper, with full-text availability. 2) The study participants were individuals aged 18 years or older with T2DM at study baseline. 3) Studies employing a valid method for assessing dietary intake (e.g. Food Frequency Questionnaire (FFQ) or 24-h recall). 4) Studies analyzing the correlation between dietary patterns scores (including the Healthy Eating Index (HEI), Alternative Healthy Eating Index (AHEI), the Healthy Diet Indicator (HDI), the Dietary Diversity Score (DDS), the Dietary Quality Score (DQS), the Diet Quality Index (DQI), relative Mediterranean diet score (rMED) and Mediterranean diet score (MDS)) and a suitable outcome measure. 5) Studies measuring at least one intended outcome from one of following measures: Lipid profile (low-density lipoprotein- cholesterol (LDL-C), high-density lipoprotein-cholesterol (HDL-C), total cholesterol (TC), triglyceride (TG)) (mg/dl), blood pressure (mmHg), blood glucose (mg/dL), HbA1c (%), body mass index (kg/m2) and waist circumference (cm). 6) Studies conducted through cross-sectional and prospective (cohort) design. The exclusion criteria included: 1) Studies with special participants (e.g. lactating or pregnant women, infants, children, and adolescents. 2) Studies with unclear described data about the study methods, issue, analysis method of the results, and participants features. 3) Studies assessing specific foods or nutrients only. 4) Studies conducted on nonhuman subjects.
Data sources and search strategy
An online search was performed for studies assessing the correlation between dietary quality indices and CVD risk factors in adults with T2DM, using Web of knowledge, PubMed, Cochrane, Science direct, Google Scholar and Scopus databases. It was completed by publisher databases such as Elsevier, Wiley online, and springer link from January 1990 to July 2020. Existing reviews and reference lists of suitable studies were manually searched for the supplementary data. No language limitation was applied in the literature search. The search terms considered for searching in PubMed were as follows: “diet quality indices”, “dietary quality index”, “dietary quality score”, “healthy diet indicator”, “healthy eating index”, “alternative healthy eating index”, “Mediterranean diet score”, “relative Mediterranean diet score”, “dietary diversity score” AND “cardiovascular diseases”, “risk factors”, “obesity”, “abdominal obesity”, “metabolic syndrome”, “diabetes”, “lipid markers”, “low density lipoproteins”, “high density lipoproteins”, “cholesterol”, “triglyceride”, “HbA1c”, “fasting blood glucose”, “2hPP”, “body mass index”, “blood pressure”, “waist circumference”. The data terms were searched as medical subject headings (MESH) terms or free text. End Note software was used to manage the search results.
Study selection
Authors individually assessed the list of identified references to consider eligibility for inclusion. Any disagreements were resolved by consensus. In the first step, the studies extracted from searching the electronic databases were classified based on the title and abstract, with duplicate publications removed. Thus, the included papers which did not meet the study purposes were excluded. In the next step, selection of the included studies was performed by reading and screening both abstract and full text according to eligibility criteria from the remaining papers. In cases where the results of a study had been published in several articles, the paper with the most complete result was registered in this review. Finally, authors checked the reference lists of the included studies to find other relevant papers.
Method of quality assessment
Quality assessment was done using The Newcastle-Ottawa scale, for evaluating the quality of non-randomized studies in review papers. This tool utilizes a “star” approach to quality assessment of non-randomized studies in three sections: Comparability of study groups, ascertainment of outcomes, and the selection of participants.[19] The maximum score of the scale was nine stars. Studies meeting a score of nine stars were considered as the highest quality.
Data extraction and analysis
Data extraction was conducted using Microsoft Excel software as well as an adapted form by the authors, and further confirmed by a research assistant. Data extracted contained the tittle of the study, purpose and study design, location, the demographic data of participants including age, gender, BMI and sample size, study populations, inclusion and exclusion criteria, measurement instruments, the time of study, outcome information and the results of analysis, dietary assessment method (e.g. 24-h recall or FFQ) and type of dietary quality indices used in included studies. All disagreements were resolved via discussion among authors. Note that Cohen's kappa statistics was used to determine the reviewer agreement statistics.
Results
Search results
Based on the search strategy in the databases mentioned above, 1627 papers were found. Then, 161 papers were removed because of being duplicate. Next, the papers which were irrelevant to our search subject in terms of title and abstract, where also excluded, whereby 69 papers remained for investigating eligibility criteria. In the final step, 10 papers entered the qualitative synthesis phase, and 59 papers were further eliminated because of investigating irrelevant outcomes and not conducting the study on the target population of interest in the present study. Figure 1 displays the search stages.
Figure 1.
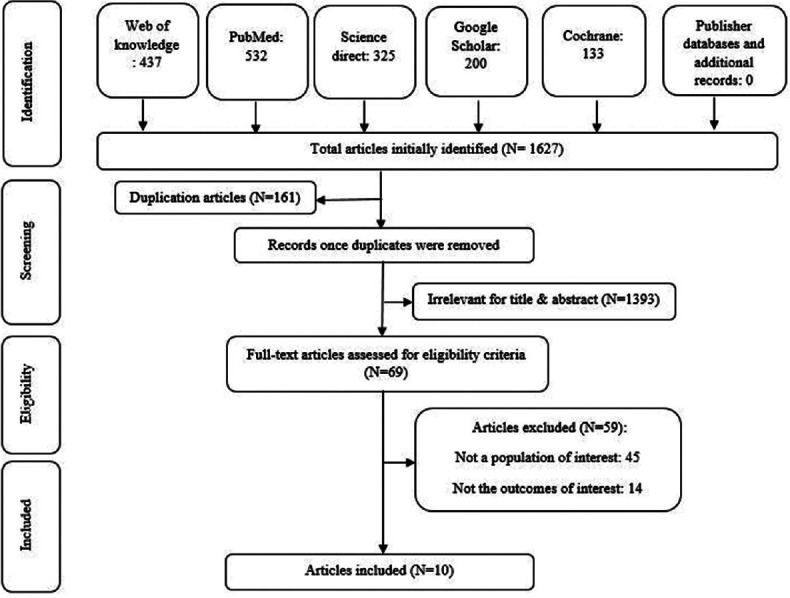
Flow chart of study selection
Quality assessment
Based on Newcastle-Ottawa scale, the minimum score belonged to the study by Tiew et al.,[20] while the maximum was found for studies by Daneshzad et al.,[9] and Wu et al.[21] The mean total score of this scale for the included studies was 7.7. Generally, the studies included in the final stage obtained a suitable score.
Study characteristics
The number of patients included in the qualitative synthesis studies in the analysis phase was 6237 with the age range of 35-84 years. Considering the gender of participants, 50.9% were male and 49.1% were female. Overall, the criterion for diabetes diagnosis in preliminary studies was HbA1c ≥6.5% and FBS ≥126 mg/dl. Out of 10 papers investigated in this study, 8 articles had a cross-sectional design, while 2 articles had been performed as prospective cohort study.[11,21] The follow-up duration in the cohort studies was around four years. The country of publication of papers was as follows: USA (n = 3), England (n = 3), South Korea (n = 1), Bangladesh (n = 1), Switzerland (n = 1), and Spain (n = 1). These papers had been published between 2010 and 2019 [Table 1].
Table 1.
Characteristics of the Qualitative Synthesis Studies for Diet Quality Indices and CVD Risk Factors in T2DM
| Author/Year | Location | Study Design | Sample Size | Sex | Age Range (Years) | Index | Outcome | Food Measurements | Adjusment | Quality assessment Score | Findings |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Giugliano et al. (2010)[24] | USA | cross-sectional | 555 men with T2DM | M: 100% | 35-70 Years | MDS | BMI, WC, Hb A1c, TG, TC, HDL-C, 2hpp glucose | FFQ | - | 8 | Total: High scores of MDS were associated with higher values of HDL-C and lower values of BMI, WC, 2hpp glucose, HbA1c, TG and TC |
| Kim et al. (2013)[11] | South Korea | cross-sectional | 110 patients with T2DM | F: 0% M: 43.6% F: 56.4% |
54.6±8.9 Years | DQI-I | Hb A1c, FBS, 2hpp glucose | 24-h recall | Age, BMI, and energy intake. | 8 | Total: High scores of indices were associated with lower values of 2hpp glucose, FBS and Hb A1c (except for AHEI) |
| Tiew et al. (2014)[21] | Bangladesh | Cross-sectional | 108 patients with T2DM | M: 49.6% | 54.05±10.30 Years | AHEI HDI DDS |
BMI and WC | FFQ | - | 6 | Total: High scores of DDS were associated with lower values of BMI and WC |
| Bonaccio et al. (2016)[10] | England | prospective | 1995 Patients with T2DM | F: 50.4% M: 66.1% |
62.6±10.2 Year | MDS | BMI, blood glucose | FFQ | - | 7 | Total: MDS was unrelated to blood glucose and BMI |
| Wu et al. (2016)[20] | England | prospective studies | 124 Patients with T2DM | F: 33.9% M: 52.4% |
61.2±11 Year | AHEI-2010 | BMI, WC, SBP, DBP, FBS, HbA1c, TG, LDL-C | 24-h recall | gender, age, physical activity, CVD history, the presence and treatment of CVD risk factors. BMI was controlled for all of the outcomes except for BMI | 9 | Total: Higher AHEI scores were significantly correlated with lower BMI, WC and serum LDL-C |
| Cheung et al. (2018)[23] | England | Cross-sectional | 211 patients with T2DM | F: 47.6% M: 54.5% |
54.0±8.6 Years | DQI | BMI | FFQ | - | 7 | Total: High scores of indexes had an inverse association with BMI |
| Vitale et al. (2018)[26] | Switzerland | Cross-sectional | 2568 patients with T2DM | F: 45.5% M: 59.7% |
50-70 Years | MDS (rMED) | AHEI-2010 BMI, HbA1c, LDL-C, HDL-C, SBP, DBP | FFQ | - | 8 | Total: High scores of rMED were associated with higher value of the HDL-C and lower values of BMI, HbA1c, SBP, DBP and LDL-C |
| Daneshzad et al. (2019)[9] | USA | Cross-sectional | 230 patients with T2DM | F: 40.3% M: 0% |
59.90±9.20 Years | HEI-2010 | BMI, WC, FBS, 2hpp, HbA1c, TC, TG, LDL-C, SBP, DBP | FFQ | age, socio-economic status, physical activity and energy intake | 9 | Total: HEI and DQI-I scores were unrelated to BMI, WC, HbA1c, 2hpp glucose, TC, TG, LDL-C, SBP and DBP. High scores of HEI were associated with lower value of FBS |
| Celada Roldan (2019)[25] | Spain | Cross-sectional | 107 patients with T2DM | F: 100% M: 45.55% |
61.16±23 Years | DQI-I MDS |
BMI, FBS, TC, TG, LDL-C, HDL-C, HbA1c | NR | - | 7 | Total: High scores of MDS were associated with higher value of the HDL-C and lower values of BMI, HbA1c, FBS, TC, TG and LDL-C |
| Antonio et al. (2019)[22] | USA | Cross-sectional | 229 patients with T2DM | F: 54.45% M: 37.9% |
63.25±5.25 Years | HEI-2010 | WC, SBP | FFQ | - | 8 | Total: High scores of HEI were associated with lower values of HbA1c and FBS |
| F: 62.1% | DBP, FBS, HbA1c, TC, TG |
CVD; cardiovascular disease, T2DM; type 2 diabetes mellitus, M; male, F; female, MDS; Mediterranean diet score, DQI-I; diet quality index-international, AHEI; alternative healthy eating index, HDI; healthy diet indicator, DDS; dietary diversity score, HEI; healthy eating index, rMED; relative Mediterranean diet score, FFQ; food frequency questionnaire, BMI; body mass index, WC; waist circumference, HbA1c; hemoglobin A1c, LDL-C; Low-density lipoprotein cholesterol, HDL-C; high-density lipoprotein cholesterol, TG; total cholesterol, TG; triglycerides, SBP; systolic blood pressure, DBP; diastolic blood pressure, FBS; fasting blood sugar, 2hpp; 2 hour post prandial
For investigating the type of the dietary quality indices used in the studies, HEI and its modified version (AHEI) had the maximum frequency among the included studies. On the other hand, HDI and DDS had the minimum frequency. The total mean score of each of the indices mentioned in the qualitative synthesis studies was as follows: DQI and HEI greater than 50, MDS larger than 4, and AHEI greater than 39. Also, the mean HDI score among all participants in one study was 5.[10,20] DDS index included two subgroups called food group score (FGS) and serving score (SS). Their total mean score was 4.12 and 12.75 respectively in one study.[20] Assessment of food intake in the included studies had been performed using FFQ and 24-h recall [Table 1].
Outcomes
The relationship between HEI as well as AHEI and CVD risk factors in T2DM
The relationship between many CVD risk factors and HEI had been examined in two cross-sectional studies. Also, one prospective study and two cross-sectional studies had tested the relationship between AHEI and some CVD risk factors among T2DM patients [Table 1]. Fasting blood sugar (FBS) decreased in two studies following elevation of the mean HEI score (mean ± SE: 149.08 ± 6.04 (mg/dl) compared to 171.72 ± 5.77 (mg/dl); P = 0.017, median (interquartile range): 130 (mg/dl) (103-177) compared to 168 (mg/dl) (131-207); P <0.001).[9,22] HbA1c diminished in only one study with elevation of HEI score (median (interquartile range): 7.8% (6.7-9.4) compared to 8.5% (7.4-10.0); P = 0.002).[22] However, the rise of the HEI score had no significant effect on BMI, WC, 2-hour postprandial (2hpp) blood glucose, systolic blood pressure (SBP), diastolic blood pressure (DBP), TC, TG, and LDL-C in any of the studies (p >0.05). Meanwhile, elevation of the AHEI score resulted in diminished BMI, WC, LDL-C, 2HPP blood glucose, and FBS in some studies (p <0.05), but it had no effect on TG and HbA1c (β: -0.02, 0.094; P >0.05).[10,21,23] Note that in the study by Antonio et al.,[22] again elevation of HEI score had no significant effect on WC and HDL regarding the gender of participants (p >0.05).
The relationship between MDS as well as rMED indices and CVD risk factors of T2DM
Three studies had explored the relationship between MDS (two cross-sectional studies and one prospective study) and one study had examined the relationship between rMED and CVD risk factors in T2DM patients [Table 1]. Investigation of lipid profile in these studies showed that elevation of MDS score had led to a significant reduction in TG, TC, and LDL-C, as well as significant rise of HDL-C (p <0.05).[11,24,25] However, its increase had no effect on blood pressure status of the patients (percentage of hypertensive individuals in 1st tertile compared to 3rd tertile: 58% compared to 58%; P = 0.16).[24] Most of the papers investigating MDS index in the present study suggested that the increase in the score of this index would lead to significant reduction of HbA1C, FBS, and 2hpp blood glucose (p <0.05).[24,25] However, the study by Bonaccio et al.,[11] rejected the reducing effect of MDS index on blood glucose (mean ± SD: 155.0 ± 45.9 mg/dl compared to 153.1 ± 42.2 mg/dl; P = 0.67). With regards to investigating anthropometric indices, BMI and WC value decreased considerably with the increase in MDS in some studies; however, the study by Bonaccio et al.,[11] emphasized lack of effectiveness of changes in the score of MDS index on BMI (p = 0.25).[11] The results obtained from investigating rMED index suggests that elevation of the score of this index results in significant decline of BMI, HbA1c, SBP, DBP, LDL-C, and significant rise of HDL-C (mean ± SD: 30.0 ± 4.2 kg/m2, 7.63 ± 0.48%, 133.3 ± 23.7 mg/dl, 78.6 ± 8.5 mg/dl, 101.5 ± 31.2 mg/dl, 46.8 ± 12.4 mg/dl compared to 30.6 ± 4.5 kg/m2, 7.69 ± 0.52%, 135.3 ± 14.9 mg/dl, 80.7 ± 8.7 mg/dl, 105.1 ± 31.9 mg/dl, 45.3 ± 11.6 mg/dl; P <0.05).[26]
The relationship between DQI and CVD risk factors in T2DM
The relationship between DQI and CVD risk factors of T2DM had been investigated in three studies.[9,10,23] The results suggested that revision of DQI score had no effect on LDL, TG, TC, SBP, and DBP (p >0.05) [Table 1]. With regards to T2DM measurement indices, Kim et al.,[10] findings also confirmed the significantly reducing effect of DQI score elevation on FBS, HbA1c, and 2hpp blood glucose (correlation coefficients: -0.220, -0.206, -0.296; P = 0.025, 0.036, 0.002).[10] However, the study by Daneshzad et al.,[9] indicated that the increase in the DQI score had no effect on HbA1c (mean ± SE: 7.50 ± 0.13% compared to 7.47 ± 0.13%; P = 0.565). Also, the study by Cheung et al.,[23] suggested a significant reduction of BMI with increase in DQI score (Beta coefficients (SE): − 0.94 (0.46); P = 0.044). On the other hand, the results of another study suggested no effect of DQI score variations on BMI and WC (mean ± SE: 29.73 ± 0.52 kg/cm2 compared to 29.41 ± 0.53 kg/cm2; P = 0.452, Odds ratios (OR) CI (95%): 0.52 (0.23, 1.18) compared to 0.59 (0.0.26, 1.34); P = 0.0494).[9]
The relationship between HDI as well as DDS and CVD risk factors of T2DM
Overall, two studies had dealt with investigating the relationship between HDI as well as DDS and some CVD risk factors in T2DM [Table 1]. Kim et al.,[10] found that elevation of HDI score would result in reduced FBS, 2hpp blood glucose, and HbA1c (Correlation coefficients: -0.226, -0.263, -0.280; P = 0.021, 007, 0.004).[10] In addition, overall elevation of DDS score in the study by Tiew et al.,[21] including FGS and SS, was also associated with a significant fall in BMI and WC (FGS; β (95% CI): -0.68 (-1.30, -0.07), -0.67 (-1.25, -0.08); P = 0.028, 0.026), (SS; β (95% CI): -3.85 (-6.50, -1.20), -3.87 (-6.41, -1.33); P = 0.005, 0.003).[20]
Discussion
The present systematic review dealt with investigating the relationship between the dietary quality indices and the agents of measuring CVD risk factors including glucose and lipid profile, blood pressure, as well as anthropometric indicators in type II diabetes patients. Generally, from among the five studies examining HEI and AHEI, three studies suggested an inverse relationship between HEI and FBS as well as HbA1c, along with inverse relationship between AHEI and BMI, WC, LDL-C, 2hpp blood glucose, and FBS.
MDS showed an inverse relationship with BMI, WC, TG, TC, LDL-C, FBS, HbA1c, and 2hPP, and a direct relationship with HDL-C. Following the increase in rMED score, the level of BMI, HbA1c, SBP, DBP, and LDL-C diminished while HDL rose. From among three studies investigating DQI, one study revealed an inverse relationship between this index and BMI, FBS, HbA1c, and 2hpp blood glucose. The values of FBS, 2hpp blood glucose, and HbA1c revealed an inverse relationship with HDI. Also, BMI and WC indicated an inverse relationship with DDS. Note that the dietary quality indices investigated in this study had no desired effect over the other CVD risk factors mentioned in the Table 1.
Diabetes as well as the issues related to preventing and treating this disease have various aspects. Nevertheless, the main focus on managing diabetes is controlling CVD risk factors.[25] Based on the results of papers examined in the present study, usage of HEI in comparison to other dietary quality indices may have greater similarity to the dietary pattern of diabetic patients.[27] Accordingly, the observations related to the effect of HEI on CVD risk factors in diabetic patients also find greater expression power. HEI-2000 contains a low lipid content as well as high fiber, antioxidant, tryptophan, and lipoic acid content. These compounds have a useful effect on the cardiovascular function.[28,21] In line with the results of our study, Saraf-Bank et al.[29] found that there is an inverse relationship between HEI-2010 and WC, BP, and TG as well as low HDL-C level among healthy individuals. Also, Chiuve et al.,[30] found that diabetics with a higher AHEI score had a lower 10-year coronary heart disease risk. This risk reduction may be due to lowering fat intake and controlling the lipid profile in these patients.[30,21] The anti-inflammatory and antithrombotic mechanism of the Mediterranean diet have been proven in several epidemiological studies for reducing blood pressure and increasing insulin sensitivity. These effects are associated with some compounds of this diet including vegetables and fish.[31,32] In parallel with the results obtained in the present study, PREDIMED study suggested that the Mediterranean diet resulted in diminished diabetes complications in 7000 patients with CVD risk factors.[25] It seems that another preventive effect of the Mediterranean diet against cardiovascular disease as well as its relationship with T2DM may be associated with carbohydrate metabolism.[33] Confirming this hypothesis, Ajala et al.,[34] reported that Mediterranean diet can potentially contribute to reducing HbA1c level.
Although few of the papers assessed in the present study had explored the effects of DDS, HDI, and DQI on CVD risk factors, the results of previous studies are also notable. Alkerwi et al.,[35] indicated that the score of DQI had an inverse relationship with WC, BP, LDL-C, and TC in 1352 healthy individuals. However, Alvarez et al.,[36] reported that DQI may not be a sensitive index to investigate the relationship between dietary quality and CVD risk factors. Previous studies testing DDS index have reported contradictory effects of this index on some CVD risk factors. The results of the present study suggested that DDS index has an inverse relationship with the value of anthropometric indices. On the other hand, Jayawardena et al.,[37] found that the increase in DDS score had a direct relationship with the rise in the level of abdominal fat and weight gain in healthy individuals. As a possible hypothesis, the extent of adhering to diabetic diet may influence the results of measuring dietary quality in diabetes patients. Tiew et al.,[20] observed that diabetics refrain from eating foods and dairies. This is due to fear of overconsumption of sweets in fruits as well as the fat in dairies, while dairies have anti-obesity, blood pressure reducing, and blood glucose reducing effects.[20] Thus, if the dietary quality in diabetics compared to healthy individuals is measured using different instruments, more desired results can be achieved.
Generally, the sociodemographic situation, differences in the measurement method of CVD risk factors, the data collection instrument associated with the dietary intake, the method of calculating the dietary quality indices, health status, level of education, occupation and income of individuals, their place of residence, and gender may explain the discrepant results across studies.[9,23,38] Harrington et al.,[39] reported that a low level of personal education about nutritional recommendations is directly associated with a low dietary quality. On the other hand, the prevalence of T2DM is also higher in those with a low level of education.[40] The costs associated with diet and food price can also influence the diversity in food selection. Reduction in dietary diversity may lead to diminished dietary quality.[41] Blaylock et al.,[42] suggested that those with a low level of income have also a lower dietary quality. Thus, the role of place of residence can also be important in the association with level of income. Those who live in developed countries, compared to the individuals living in developing countries, have a higher level of education and income, which can in turn affect the dietary quality of people.
One of the important points observed in the included studies is the energy intake. Although some studies had adjusted the energy intake, some others had neglected it. The level of energy intake acts like a double-edged sword. Some studies suggest that increase in the energy intake leads to obesity, while if the rise in the consumption of healthy and diverse food causes balanced increase in the energy intake, the quality of the diet consumed grows and CVD risk factors diminishes in diabetics.[43,44] Daneshzad et al.,[9] observed that the energy intake did not differ significantly in the HEI-2010 and DQI scored subgroups. On the other hand, with increase in the score of these indices, DBP and SBP, LDL-C, TG, TC, 2hPP, HbA1c, WC, and BMI also decreased. Meanwhile, reducing energy intake through special dietary patterns and increasing consumption of plant-based diets in diabetics can modify the complications and symptoms of the disease.[23] Thus, this hypothesis can be noted that energy intake in the form of dietary patterns, in addition to balancing the food intake, can also lead to enhanced dietary quality and reduced CVD complications as well as symptoms.
The results of previous studies suggest that the extent of adhering to consuming some nutrients such as cholesterol and sodium is greater in men than in women.[17,45] This may be associated with increased energy intake by men. Based on the above point, the incidence of CVD risk factors may increase in T2DM men compared to women.[46] In line with these results, Giugliano et al.,[24] who worked on men, also found that the extent of adhering to MDS index was inversely associated with TC and TG, HbA1c, 2hPP, WC, and BMI. However, Daneshzad et al.,[9] who studied women, rejected this result. On the other hand, Antonio et al.,[22] observed that the extent of adhering to HEI index has no significant relationship with WC and HDO concerning gender. Regardless of the type of the dietary quality indices, this hypothesis can be mentioned that although some studies reported increased incidence of CVD risk factors in men compared to women in T2DM, controlling consumption of harmful nutrients such as cholesterol and sodium as healthy dietary patterns can also have more desired effects on men compared to women suffering T2DM.
The limitations of the present study were as follows: 1) considering the relationship between dietary quality and level of well-being, most of the studies had also been performed in developed countries with a relatively good level of welfare, which may affect the results. On the other hand, in other populations, the obtained results may be different; 2) most of the included studies had been done cross-sectionally, and only two had been performed as prospective. This can create bias and affect our conclusion to some extent; 3) in spite of the importance of adjusting confounding variables (especially energy intake), some studies had not done that, and the results of these studies may have lower validity; 4) Considering the heterogeneity of qualitative synthesis studies, it was not possible to perform a meta-analysis.
In conclusion, the findings of this review suggest that the dietary quality plays a significant role in the scenario of the relationship between diet and CVD risk factors in T2DM. It also creates a new perspective for designing effective strategies in future to develop this scenario. Most of the included studies showed an inverse relationship between dietary quality indices and CVD risk factors in T2DM. Generally, from among all of the examined risk factors, the main inverse effect of the dietary quality indices in the studies was observed on glucose profile and anthropometric indices. Further studies seem to be warranted to confirm these findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tripathi BK, Srivastava AK. Diabetes mellitus: Complications and therapeutics. Med Sci Monit. 2006;12:RA130–RA47. [PubMed] [Google Scholar]
- 2.Krug EG. Trends in diabetes: Sounding the alarm. Lancet. 2016;387:1485–6. doi: 10.1016/S0140-6736(16)30163-5. [DOI] [PubMed] [Google Scholar]
- 3.Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: A review of current evidence. Diabetologia. 2019;62:3–16. doi: 10.1007/s00125-018-4711-2. [DOI] [PubMed] [Google Scholar]
- 4.Vedanthan R, Ray M, Fuster V, Magenheim E. Hypertension treatment rates and health care worker density: An analysis of worldwide data. Hypertension. 2019;73:594–601. doi: 10.1161/HYPERTENSIONAHA.118.11995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fakhri M, Sarokhani D, Ghiasi B, Dehkordi AH. Prevalence of hypertension in cardiovascular disease in Iran: Systematic review and meta-analysis. Int J Prev Med. 2020;11:56. doi: 10.4103/ijpvm.IJPVM_351_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liccardo D, Cannavo A, Spagnuolo G, Ferrara N, Cittadini A, Rengo C, et al. Periodontal disease: A risk factor for diabetes and cardiovascular disease. Int J Mol Sci. 2019;20:1414. doi: 10.3390/ijms20061414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsirou E, Grammatikopoulou MG, Theodoridis X, Gkiouras K, Petalidou A, Taousani E, et al. Guidelines for medical nutrition therapy in gestational diabetes mellitus: Systematic review and critical appraisal. J Acad Nutr Diet. 2019;119:1320–39. doi: 10.1016/j.jand.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Ocké MC. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc Nutr Soc. 2013;72:191–9. doi: 10.1017/S0029665113000013. [DOI] [PubMed] [Google Scholar]
- 9.Daneshzad E, Larijani B, Azadbakht L. Diet quality indices and cardiovascular diseases risk factors among diabetic women. J Sci Food Agric. 2019;99:5926–33. doi: 10.1002/jsfa.9867. [DOI] [PubMed] [Google Scholar]
- 10.Kim J, Cho Y, Park Y, Sohn C, Rha M, Lee M-K, et al. Association of dietary quality indices with glycemic status in Korean patients with type 2 diabetes. Clin Nutr Res. 2013;2:100–6. doi: 10.7762/cnr.2013.2.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Donati MB, et al. Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. Eur J Prev Cardiol. 2016;23:400–7. doi: 10.1177/2047487315569409. [DOI] [PubMed] [Google Scholar]
- 12.Gil Á, de Victoria EM, Olza J. Indicators for the evaluation of diet quality. Nutr Hosp. 2015;31((Suppl 3)):128–44. doi: 10.3305/nh.2015.31.sup3.8761. [DOI] [PubMed] [Google Scholar]
- 13.Gopinath B, Rochtchina E, Flood V, Mitchell P. Diet quality is prospectively associated with incident impaired fasting glucose in older adults. Diabet Med. 2013;30:557–62. doi: 10.1111/dme.12109. [DOI] [PubMed] [Google Scholar]
- 14.Xu Z, Steffen LM, Selvin E, Rebholz CM. Diet quality, change in diet quality and risk of incident CVD and diabetes. Public Health Nutr. 2020;23:329–38. doi: 10.1017/S136898001900212X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nicklas TA, O’Neil CE, Fulgoni VL., III Diet quality is inversely related to cardiovascular risk factors in adults. J Nutr. 2012;142:2112–8. doi: 10.3945/jn.112.164889. [DOI] [PubMed] [Google Scholar]
- 16.Guillermo C, Boushey CJ, Franke AA, Monroe KR, Lim U, Wilkens LR, et al. Diet quality and biomarker profiles related to chronic disease prevention: The multiethnic cohort study. J Am Coll Nutr. 2020;39:216–23. doi: 10.1080/07315724.2019.1635921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asghari G, Mirmiran P, Yuzbashian E, Azizi F. A systematic review of diet quality indices in relation to obesity. Br J Nutr. 2017;117:1055–65. doi: 10.1017/S0007114517000915. [DOI] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Peterson J, Welch V, Losos M, Tugwell P, editors. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 20.Tiew KF, Chan YM, Lye MS, Loke SC. Factors associated with dietary diversity score among individuals with type 2 diabetes mellitus. J Health Popul Nutr. 2014;32:665–76. [PMC free article] [PubMed] [Google Scholar]
- 21.Wu PY, Huang CL, Lei WS, Yang SH. Alternative health eating index and the dietary guidelines from American diabetes association both may reduce the risk of cardiovascular disease in type 2 diabetes patients. J Hum Nutr Diet. 2016;29:363–73. doi: 10.1111/jhn.12317. [DOI] [PubMed] [Google Scholar]
- 22.Antonio JP, Sarmento RA, de Almeida JC. Diet quality and glycemic control in patients with type 2 diabetes. J Acad Nutr Diet. 2019;119:652–8. doi: 10.1016/j.jand.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Cheung LTF, Chan RSM, Ko GTC, Lau ESH, Chow FC, Kong APS. Diet quality is inversely associated with obesity in Chinese adults with type 2 diabetes. Nutr J. 2018;17:63. doi: 10.1186/s12937-018-0374-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giugliano F, Maiorino MI, Bellastella G, Autorino R, De Sio M, Giugliano D, et al. Adherence to mediterranean diet and erectile dysfunction in men with type 2 diabetes. J Sex Med. 2010;7:1911–7. doi: 10.1111/j.1743-6109.2010.01713.x. [DOI] [PubMed] [Google Scholar]
- 25.Celada Roldan C, Tarraga Marcos ML, Madrona Marcos F, Solera Albero J, Salmeron Rios R, Celada Rodriguez A, et al. Adhesion to the mediterranean diet in diabetic patients with poor control. Clin Investig Arterioscler. 2019;31:210–7. doi: 10.1016/j.arteri.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Vitale M, Masulli M, Calabrese I, Rivellese AA, Bonora E, Signorini S, et al. Impact of a mediterranean dietary pattern and its components on cardiovascular risk factors, glucose control, and body weight in people with type 2 diabetes: A real-life study. Nutrients. 2018;10:1067. doi: 10.3390/nu10081067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schap T, Kuczynski K, Hiza H. Healthy eating index—Beyond the score. J Acad Nutr Diet. 2017;117:519–21. doi: 10.1016/j.jand.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Pan Y, Pratt CA. Metabolic syndrome and its association with diet and physical activity in US adolescents. J Am Diet Assoc. 2008;108:276–86. doi: 10.1016/j.jada.2007.10.049. discussion 286. [DOI] [PubMed] [Google Scholar]
- 29.Saraf-Bank S, Haghighatdoost F, Esmaillzadeh A, Larijani B, Azadbakht L. Adherence to healthy eating index-2010 is inversely associated with metabolic syndrome and its features among Iranian adult women. Eur J Clin Nutr. 2017;71:425–30. doi: 10.1038/ejcn.2016.173. [DOI] [PubMed] [Google Scholar]
- 30.Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–18. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li H, Kong XB, Zhang HL, Wu J. Adherence to mediterranean diet and erectile dysfunction in men with type 2 diabetes. J Sex Med. 2011;8:631. doi: 10.1111/j.1743-6109.2010.01877.x. [DOI] [PubMed] [Google Scholar]
- 32.Iimuro S, Yoshimura Y, Umegaki H, Sakurai T, Araki A, Ohashi Y, et al. Dietary pattern and mortality in Japanese elderly patients with type 2 diabetes mellitus: Does a vegetable-and fish-rich diet improve mortality?An explanatory study. Geriatr Gerontol Int. 2012;12:59–67. doi: 10.1111/j.1447-0594.2011.00813.x. [DOI] [PubMed] [Google Scholar]
- 33.Elhayany A, Lustman A, Abel R, Attal-Singer J, Vinker S. A low carbohydrate mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: A 1-year prospective randomized intervention study. Diabetes Obes Metab. 2010;12:204–9. doi: 10.1111/j.1463-1326.2009.01151.x. [DOI] [PubMed] [Google Scholar]
- 34.Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013;97:505–16. doi: 10.3945/ajcn.112.042457. [DOI] [PubMed] [Google Scholar]
- 35.Alkerwi AA, Vernier C, Crichton GE, Sauvageot N, Shivappa N, Hébert JR. Cross-comparison of diet quality indices for predicting chronic disease risk: Findings from the Observation of cardiovascular risk factors in luxembourg (ORISCAV-LUX) study. Br J Nutr. 2015;113:259–69. doi: 10.1017/S0007114514003456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alvarez-Alvarez I, Toledo E, Lecea O, Salas-Salvadó J, Corella D, Buil-Cosiales P, et al. Adherence to a priori dietary indexes and baseline prevalence of cardiovascular risk factors in the PREDIMED-Plus randomised trial. Eur J Nutr. 2020;59:1219–32. doi: 10.1007/s00394-019-01982-x. [DOI] [PubMed] [Google Scholar]
- 37.Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Yadav B, Hills AP. High dietary diversity is associated with obesity in Sri Lankan adults: An evaluation of three dietary scores. BMC Public Health. 2013;13:314. doi: 10.1186/1471-2458-13-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hosseini-Esfahani F, Jessri M, Mirmiran P, Bastan S, Azizi F. Adherence to dietary recommendations and risk of metabolic syndrome: Tehran lipid and glucose study. Metabolism. 2010;59:1833–42. doi: 10.1016/j.metabol.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 39.Harrington J, Fitzgerald AP, Layte R, Lutomski J, Molcho M, Perry IJ. Sociodemographic, health and lifestyle predictors of poor diets. Public Health Nutr. 2011;14:2166–75. doi: 10.1017/S136898001100098X. [DOI] [PubMed] [Google Scholar]
- 40.Quinlan J, Lee L, Mangroo A, Vierow K. Evaluation of MyPlate as a dietary learning tool among young adults. J Acad Nutr Diet. 2012;112:A85. [Google Scholar]
- 41.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87:1107–17. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- 42.Blaylock J, Smallwood D, Kassel K, Variyam J, Aldrich L. Economics, food choices, and nutrition. Food Policy. 1999;24:269–86. [Google Scholar]
- 43.Savy M, Martin-Prevel Y, Danel P, Traissac P, Dabiré H, Delpeuch F. Are dietary diversity scores related to the socio-economic and anthropometric status of women living in an urban area in Burkina Faso? Public Health Nutr. 2008;11:132–41. doi: 10.1017/S1368980007000043. [DOI] [PubMed] [Google Scholar]
- 44.Azadbakht L, Esmaillzadeh A. Dietary diversity score is related to obesity and abdominal adiposity among Iranian female youth. Public Health Nutr. 2011;14:62–9. doi: 10.1017/S1368980010000522. [DOI] [PubMed] [Google Scholar]
- 45.Meisinger C, Döring A, Thorand B, Heier M, Löwel H. Body fat distribution and risk of type 2 diabetes in the general population: Are there differences between men and women?The MONICA/KORA Augsburg cohort study. Am J Clin Nutr. 2006;84:483–9. doi: 10.1093/ajcn/84.3.483. [DOI] [PubMed] [Google Scholar]
- 46.Van Dam RM, Willett WC, Rimm EB, Stampfer MJ, Hu FB. Dietary fat and meat intake in relation to risk of type 2 diabetes in men. Diabetes Care. 2002;25:417–24. doi: 10.2337/diacare.25.3.417. [DOI] [PubMed] [Google Scholar]


