Abstract
Purpose:
Children who are deaf or hard of hearing (DHH) and who use hearing aids or cochlear implants are more likely than their peers with typical hearing to exhibit behavior problems. Although multiple evidence-based interventions for child behavior problems exist, they are rarely delivered to children who are DHH, and no rigorous randomized controlled trials have been conducted to determine their effects with this population. This protocol describes a study aiming to test the effectiveness of an evidence-based behavioral parent training intervention adapted for parents of young children who are DHH and simultaneously to assess key implementation outcomes and multilevel contextual factors influencing implementation.
Method:
The protocol for a Type 1 hybrid effectiveness–implementation trial of a behavioral parent training intervention for parents of young children who are DHH is presented, including details of the study design, participants, assessments, and analyses. Using a stakeholder-engaged, mixed-methods approach, we will test the effects of the intervention versus treatment as usual on parenting behaviors, child behaviors, and a range of secondary effectiveness outcomes, including adherence to using hearing aids and cochlear implants as well as measures of child speech and language. We will assess the acceptability, feasibility, fidelity, and costs of the intervention from the perspectives of peer coaches who deliver the intervention, hearing health care clinicians (including audiologists and speech-language pathologists), and administrators of programs serving young children who are DHH.
Conclusions:
Results of this trial will inform future efforts to close the gap between prevalence of behavioral problems in young children who are DHH and access to and use of evidence-based interventions to prevent and treat them. If effective, this intervention could be widely implemented using strategies informed by the findings of this study to benefit young children who are DHH and followed in hearing health care and their families.
Children who are deaf or hard of hearing (DHH) are at increased risk for disruptive behavior problems (Hindley et al., 1994) but are less likely than their peers with typical hearing to receive behavioral interventions (Fellinger et al., 2012; Sessa & Sutherland, 2013; Vernon & Leigh, 2007). The public health burden posed by behavioral problems in children who are DHH is significant: As the most common neonatal sensory disorder in the United States, infant hearing loss occurred in 1.7 per 1,000 births in 2019 (Centers for Disease Control and Prevention, 2021), though the prevalence of hearing loss in children is near 15% (Mehra et al., 2009). Timely initiation of hearing rehabilitation using hearing aids (HAs) or cochlear implants (CIs) improves language development and social adjustment (Yoshinaga-Itano, 2004; Yoshinaga-Itano et al., 1998). Unfortunately, the benefits from treatment of hearing loss and speech-language therapy do not necessarily extend to child behaviors; in nearly half of children who are DHH, behavioral problems persist after standard early intervention (e.g., hearing health care, and speech and language therapy; Stevenson et al., 2011; Theunissen et al., 2014), sometimes into adolescence (Stevenson et al., 2017).
In the general population, very young children with disruptive behavior problems are at increased risk for escalating behaviors, including bullying, physical aggression, vandalism, and criminal acts (Moffitt, 1993). Without intervention, behavioral problems often persist into adolescence and beyond (Keenan & Wakschlag, 2002; Lavigne et al., 2009). Children with disruptive behavior problems frequently experience comorbid internalizing symptoms (i.e., depression and anxiety; Granic & Lougheed, 2016), which are difficult to detect in young children (Tandon et al., 2009). Parents of children with disruptive behavior problems experience high levels of stress and impaired family functioning. Additionally, untreated early-onset disruptive behavior problems lead to a nearly 10-fold increase in costs associated with education, health, and criminal justice through early adulthood (Pelham et al., 2007; Reinke et al., 2012; Schaeffer et al., 2006).
Behavioral Problems Among Children Who Are Deaf or Hard of Hearing
Approximately 20% of young children with typical hearing exhibit early disruptive behavior problems (Perou et al., 2013). Young children who are DHH, however, are more than twice as likely to exhibit these problems (Hindley et al., 1994). Even after ongoing use of HA/CI, nearly 50% of preschool-age children who are DHH experience significant behavior problems (Hindley et al., 1994; Hindley & Kitson, 2000). A common behavioral issue reported among young children who are DHH is resistance or refusal to use HA/CI (Muñoz et al., 2015; Walker et al., 2013). A few studies have investigated hearing device adherence among young children, suggesting that the vast majority (> 80%) of parents overestimate the amount of time their preschool-age child who is DHH adheres to HA/CI use (Moeller et al., 2009; Walker et al., 2013), and nearly one third report that their child's mood, fatigue, or temperament pose obstacles to adherence (Moeller et al., 2009). Lack of adherence to HA/CI use is associated with poor language outcomes (Tomblin et al., 2015), and poor language outcomes are associated with child behavior problems (Levickis et al., 2018)—highlighting a potential vicious circle in many families of young children who are DHH. Professional guidelines for hearing health care providers encountering this common behavioral challenge in their patients are limited to parent education recommendations (American Academy of Audiology, 2013; American Speech-Language-Hearing Association, 2020), and evidence is very limited for interventions targeting parents' responses to their children's lack of adherence with HA/CI (Muñoz et al., 2016, 2021).
The persistence of behavioral problems despite effective hearing and language interventions suggests that improved hearing and language alone may not resolve this issue. Lack of adherence with HA/CI is only one example of behavioral challenges parents encounter with their young children who are DHH; others include “acting out,” peer problems, and defiance (i.e., externalizing behaviors), as well as moodiness, irritability, and anxiety (i.e., internalizing behaviors). Multiple studies have attempted to elucidate the etiology of behavioral problems in DHH children (Barker et al., 2009). Multiple contributing factors have been hypothesized, including poor integration of cognitive function (Dharitri & Murthy, 1990), difficulty controlling visual attention resources (Dye & Hauser, 2014), “sensory overload” in environmental surroundings (Hogan et al., 2011), sensory deprivation (Horn et al., 2005), and low lingual competency (Stevenson et al., 2010). Compelling evidence for the role of language in the development of child behavior problems was reported from a study of children between the ages of 18 months and 5 years who were severely to profoundly deaf (Barker et al., 2009), and in typical hearing children with behavioral problems, language deficits have also been observed (e.g., Levickis et al., 2018); but again, improvements in DHH children's language outcomes have not been universally followed by reductions in behavioral problems.
Parenting Behaviors as a Target of Intervention: Behavioral Parent Training
Parenting behaviors are a known contributing factor to disruptive behavior problems but have rarely been addressed in the literature on behavioral problems in DHH children. This omission is noteworthy for three reasons: (a) the extensive evidence that inconsistent and/or coercive discipline causes and maintains child behavior problems (Stormshak et al., 2000); (b) commonalities and overlap among multiple theories emphasizing the role of parenting behaviors in the development and maintenance of child behavior problems (Bandura, 1977; Patterson et al., 1989; Patterson & Yorger, 2002); and (c) the modifiable nature of parenting behaviors (Webster-Stratton et al., 2004), making them a key target for prevention and intervention—especially in early childhood, when emergence of behavioral problems predicts future psychosocial challenges for a substantial proportion of children (Lavigne et al., 2001).
The contribution of parenting behaviors to the development and maintenance of child disruptive behavior problems is explained by social cognitive theory (Bandura, 1977), Patterson's coercion theory (Patterson et al., 1989), and the developmental model for early-onset antisocial behavior (Patterson & Yorger, 2002). Each of these theories posits that parents and children influence each other's behaviors: Parents react to children's behaviors, children respond to the parent, and so on. In families in which young children exhibit behavioral problems, negative behaviors (e.g., oppositional behavior and aggression) are often inadvertently reinforced and thus maintained. Young children with disruptive behavior problems tend to elicit repeated demands from parents, frequently resulting in parents either escalating efforts to obtain compliance or “giving up”—either way, children's negative behaviors are reinforced. Moreover, these children's positive behaviors are rarely reinforced. Over time, both children and parents develop entrenched patterns of behavior that are difficult to break. Persistent negative parent–child behavioral patterns are also associated with child internalizing behaviors (i.e., depression and anxiety; Granic & Lougheed, 2016) and with parent depression (Gross et al., 2008).
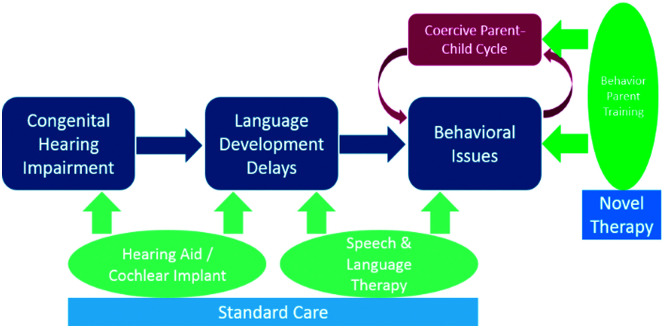
Coercive cycles of parent–child interaction may begin with parent factors (e.g., high stress and low coping skills) or with child factors (e.g., hyperactivity and challenges in executive functioning) that may or may not be developmentally typical. Regardless of the catalyst, coercive parent–child cycles strengthen and maintain negative behaviors in both the parent and the child. In the population of parents of children who are DHH and use HAs and CIs, we posit that coercive cycles may begin with problem behaviors related to delays in language development (Barker et al., 2009) and communication challenges, but that for some parents and children, they become entrenched over time and persist even after hearing and language interventions yield improvements in those domains, suggesting the need for novel intervention beyond the standard of care for young children who are DHH (see Figure 1). The potential value of interventions interrupting these coercive cycles—particularly as a complement to the standard of care in hearing health care and early intervention services with children who are DHH—is highlighted in the numerous studies describing the high prevalence of behavioral problems in this population but low availability and access to preventive and clinical behavioral interventions.
Figure 1.
Behavioral parent training to address negative child behaviors with parents of children who are deaf or hard of hearing.
Serving as both a preventive and clinical intervention for disruptive behavior problems, behavioral parent training (BPT) has consistently demonstrated efficacy and effectiveness over 40 years of studies with children with typical hearing (Menting et al., 2013; Michelson et al., 2013; Webster-Stratton & Hammond, 1997; Webster-Stratton et al., 2004). Meta-analysis of BPT has revealed a set of intervention components consistently associated with significant effects on measures of child and parent behaviors: increasing positive parent–child interactions and communication skills; teaching parents to be consistent with limit setting, consequences, and routines; and coaching parents in practicing new skills during sessions (Kaminski et al., 2008). Positive long-term outcomes in parenting practices and child behaviors have been reported (Webster-Stratton et al., 2011), including reduced antisocial behaviors and drug use by adolescents whose parents received BPT in the elementary school years (Stormshak & Dishion, 2009).
Analyses of BPT's costs and benefits demonstrate its cost-effectiveness in averting later antisocial behaviors, compared with the few effective alternatives to early identification and intervention (e.g., day treatment and intensive supervision of adolescents; Dretzke et al., 2005). Recent evidence reveals additional positive effects of BPT on internalizing symptoms (i.e., depression and anxiety) in children, on stress and depressive symptoms in parents (Gonzalez & Jones, 2016), and on language outcomes among children with developmental delay (Garcia et al., 2015). The extensive literature demonstrating positive effects of BPT on child, parent, and family functioning—even in the context of adverse childhood experiences such as chronic health conditions—led the Centers for Disease Control and Prevention to include delivery of evidence-based parenting interventions as one of four goals in its resource guide for enhancing safety and stability for children (Centers for Disease Control and Prevention, 2014).
There is a significant gap, however, in the delivery of behavioral interventions to parents of children who are DHH, though the need for these interventions has been articulated (Fellinger, 2011; Stevenson et al., 2011). In our previous research with parents of preschool-age children who were DHH and used HA and/or CI (Fiorillo et al., 2017), we confirmed others' findings that parents of young children who were DHH (n = 50) were significantly more likely to report concerns about child emotional or behavioral problems, compared with parents of children with typical hearing (n = 39). Based on a structured clinical diagnostic interview, nearly half of the children who were DHH met the criteria for oppositional defiant disorder, one of the most common behavioral disorders in children; in comparison, only one in five children with typical hearing met criteria. Similarly, parent report of impairment in child or family functioning related to behavioral problems was significantly higher in parents of children who were DHH (43% among parents of children using HA and 48% among parents of children using CI) than in parents of children with typical hearing (15%). Differences in levels of child behavior problems and perceived impairment remained significant after controlling for child language development. Given the higher prevalence of parental concern among parents of children who were DHH, results regarding receipt of behavioral treatment targeting child behaviors were stark: Although 8% of children with typical hearing had received behavioral interventions (in line with national estimates among preschool-age children), no parents of children who were DHH had received such services.
BPT may be a useful addition to the existing array of services provided to young children who are DHH and followed in hearing health care. This intervention targets essential parenting behaviors (e.g., positive behavioral supports, parent–child communication, consistent limit setting, and positive parent–child routines) that are highly relevant to the behavioral challenges described by parents of young children who are DHH and that complement services offered by other providers (e.g., speech-language pathology and audiology). To our knowledge, there are no rigorous randomized trials of BPT for parents of young children who are DHH and followed in hearing health care (Muñoz et al., 2021). Given the known challenges in accessing mental health preventive and intervention services experienced by individuals who are DHH, in conjunction with high levels of behavioral problems reported by parents of young children who are DHH, this gap is concerning.
Rationale for a Hybrid Effectiveness–Implementation Trial of BPT
Development and testing of behavioral interventions is a time-consuming process. The field of implementation science highlights the importance of integrating research on effectiveness and implementation to decrease the time required to translate research findings into practice (Curran et al., 2012). With an estimated 17-year lag before even half of evidence-based interventions are integrated into usual care (Balas & Boren, 2000; Grant et al., 2003; Morris et al., 2011), early consideration of implementation outcomes and barriers and facilitators to future implementation can speed up this time to translation.
With evidence that a disproportionate number of young children who are DHH experience behavioral problems, a lack of evidence-based preventive and clinical interventions for this public health problem, and inadequate access to and availability of mental health services for this population, use of a hybrid effectiveness–implementation design (Curran et al., 2012) is a promising approach to (a) test the effectiveness of a BPT intervention while (b) simultaneously assessing its potential for widespread implementation, if warranted. Implementation outcomes of particular interest at this stage of investigation include multilevel perspectives on the acceptability, feasibility, fidelity, and costs of intervention delivery (Proctor et al., 2011)—all important considerations for the eventual adoption, implementation, reach, and maintenance of an intervention and its ultimate public health impact (Glasgow et al., 2019).
The potential for implementation of any evidence-based intervention is determined by multilevel contextual factors influencing whether, how, why, where, and by whom an intervention is adopted and delivered (Nilsen & Bernhardsson, 2019). Exploring these factors with guidance from a contextual framework offers a systematic approach to identifying potential barriers and facilitators to future implementation. The Consolidated Framework for Implementation Research (CFIR), for example, posits 39 contextual factors that may influence implementation, organized under five domains: interventionist characteristics, characteristics of the intervention, inner setting, outer setting, and process (Damschroder et al., 2009). Exploring the potential barriers and facilitators to implementation within specific CFIR contextual domains in a hybrid effectiveness–implementation trial can facilitate planning for future implementation strategies harnessing facilitators and addressing barriers.
Study Goals and Hypotheses
Funded by the National Institute on Deafness and Other Communication Disorders, this R01 Type 1 hybrid effectiveness–implementation trial (a) tests the effectiveness of a stakeholder-informed BPT intervention delivered by peer coaches to parents of young children who are DHH; (b) assesses secondary effects on adherence to wearing devices and on language outcomes; and (c) collects implementation data—including acceptability, adoption, feasibility, fidelity, and costs—to inform subsequent implementation trials. By using a hybrid design (Curran et al., 2012) rather than focusing on effectiveness alone, this trial prepares for potential scale-up of the intervention, assessing preliminary implementation outcomes (Proctor et al., 2011) and contextual factors that may serve as barriers or facilitators to future widespread implementation (Damschroder et al., 2009). The extensive stakeholder engagement informing the selection, adaptation, and testing of a BPT intervention in this project highlights the importance of partnering with hearing health care professionals and programs in reaching the population of young children who are DHH and their families, rather than relying on the limited availability of mental health systems and professionals who are typically unfamiliar with the needs and experiences of this population (Fellinger et al., 2012; Sessa & Sutherland, 2013; Vernon & Leigh, 2007).
We will test four hypotheses about the effectiveness of a BPT intervention adapted for parents of young children who are DHH and address two research questions about its preliminary implementation outcomes and contextual factors potentially influencing implementation. Our effectiveness hypotheses are as follows: Compared with those assigned to treatment as usual (TAU), parent–child dyads assigned to the adapted BPT intervention will demonstrate:
H1: increased use of positive parenting strategies (primary outcome),
H2: lower levels of child disruptive behavior problems (secondary outcome),
H3: increased adherence to wearing hearing devices as prescribed (exploratory outcome), and
H4: better language development outcomes over time (exploratory outcome).
Our implementation research questions are as follows:
RQ1: What are the initial implementation outcomes (i.e., acceptability, feasibility, fidelity, and costs) of adapted BPT delivery in this trial, observed from multilevel perspectives?
RQ2: What are the multilevel contextual factors potentially influencing adapted BPT implementation in this trial?
Method
Overview and Design
This two-arm randomized controlled trial (RCT) uses mixed methods to test the effectiveness of a BPT intervention for parents of young children who are DHH compared to TAU and to simultaneously assess implementation outcomes and contextual factors theorized to influence implementation from the perspective of multilevel stakeholders. Parents of children ages 3–6 years who are DHH and use HA, CI, or bone-conduction devices will be individually randomized to receive FCU-DHH (Family Check-Up for Children Who Are DHH), a BPT intervention adapted for this population from the evidence-based Family Check-Up (FCU) or TAU. Nine peer coaches will be trained and supervised in the delivery of FCU-DHH to parents randomized to the intervention arm. Parent–child dyads and peer coaches will participate in the study for approximately 3 years.
The Type 1 hybrid effectiveness–implementation design was selected based on criteria put forth by Curran et al. (2012): The intervention (BPT) has strong face validity, suggesting that it may benefit recipients in the new setting or population, that it has a strong base of evidence in different but related populations, and that it poses minimal risk. When these criteria are met, a Type 1 hybrid is warranted, combining a traditional effectiveness trial of an intervention delivered in “real-world” settings (rather than in the tightly controlled efficacy trial context) with assessment of preliminary implementation outcomes and exploration of potentially influential contextual factors.
The primary effectiveness outcome is parenting behavior at 6-month follow-up. Secondary effectiveness outcomes include child behaviors, adherence to using HA/CI as prescribed, and language outcomes over time; measures include parent report, observation, medical records, and administration of standardized instruments to children. Implementation outcomes are selected from Proctor's taxonomy (Proctor et al., 2011) and include acceptability, feasibility, fidelity, and costs. Finally, contextual factors theorized to influence implementation are operationalized through CFIR (Damschroder et al., 2009) and include factors from three of the five CFIR domains: interventionist characteristics, characteristics of the intervention, and outer setting characteristics. Assessment of implementation outcomes and contextual factors involves a range of data collection from multilevel stakeholders, including parents, peer coaches, and administrators, who will complete quantitative measures and qualitative key informant interviews. Video-recorded intervention sessions, ratings of fidelity, and process records tracking costs will also yield implementation data. Together, these data will comprise a mixed-method, multilevel evaluation of the effects and implementation of FCU-DHH; if effective, subsequent trials will test strategies for implementation and dissemination to inform broad implementation of this intervention for parents of young children who are DHH.
The research will be conducted and reported in accordance with the requirements of the Consolidated Standards of Reporting Trials (CONSORT) statement (Schulz et al., 2010), and qualitative analyses will adhere to the COREQ guidelines (Tong et al., 2007). The trial is approved by the University of Kentucky Institutional Review Board (IRB), which serves as the single-site IRB on behalf of our partnering institutions and agencies, and it is registered at clinicaltrials.gov (NCT03916146).
Application of the CFIR
We selected CFIR to guide our questions about factors influencing intervention implementation because of its comprehensive coverage of multilevel contextual constructs and domains (Damschroder et al., 2009). As in many studies guided by CFIR (e.g., Damschroder & Lowery, 2013; Keith et al., 2017; Safaeinili et al., 2020), we focus on domains and constructs anticipated to be most applicable to our trial but may learn about additional constructs and domains through our qualitative inquiry. We selected three CFIR domains as most salient: interventionist characteristics, characteristics of the intervention, and outer setting. We anticipate that contextual factors including attitudes and self-efficacy of peer coaches; stakeholders' perceptions of the complexity, adaptability, and “fit” of the intervention for the target population and interventionists; and outer setting characteristics such as rurality, access to behavioral services, and socioeconomic conditions may all be identified as barriers or facilitators to implementation in this trial.
Implementation of the FCU-DHH will be by peer coaches through a state chapter of a national parent support organization for families with children who are DHH. If effective, there is potential for widespread dissemination and implementation of FCU-DHH through this partnership; future investigations would need to assess the influence of both process and inner setting domains in implementation trials and select implementation strategies to maximize facilitators and overcome barriers identified in all five CFIR domains.
Setting
This study is set in Kentucky, where hospitals currently screen 98% of newborns for congenital hearing loss (Kentucky Cabinet for Health and Family Services, n.d.). The state Office for Children with Special Health Care Needs (OCSHCN) manages Kentucky's Early Hearing Detection and Intervention Program, including the Newborn Hearing Screening Program, tracking and providing follow-up for newborns referred for diagnostic testing, as well as providing assistance to families seeking diagnostic, medical management, HA assessment and funding, early intervention, and other resources. Direct audiology services for children who are DHH are provided by OCSHCN at sites across the state, in addition to services available through academic, private, and nonprofit hearing health care programs. Early intervention services for birth-to-3 children with developmental delays or established risk concerns are provided through Kentucky First Steps. Additionally, the Kentucky Department of Education provides resources and supports to the Kentucky School for the Deaf and to districts, parents, and service providers across the state for students who are DHH. Limited Deaf Mental Health Services are provided through regional community mental health centers through the state Division of Behavioral Health. Families of children who are DHH in Kentucky may also access the state chapter of Hands & Voices, a nonprofit, nonbiased parent support program. Finally, the Kentucky Commission on the Deaf and Hard of Hearing advocates for DHH individuals on legislative issues, provides information and referrals for services, and pursues a strategic plan to address the needs of DHH individuals in Kentucky.
Study Arms
The overarching goals of this trial are to determine whether FCU-DHH results in improved parent and child outcomes compared to TAU and to understand the quality of implementation and reasons for any variation. Thus, the study arms include the intervention (FCU-DHH) and a control TAU condition. As this study is a hybrid effectiveness–implementation trial, we will not restrict participants from accessing outside or additional services regardless of study arm. Participation in services or supports outside the study will be tracked as part of standard data collection.
Intervention Arm: FCU-DHH
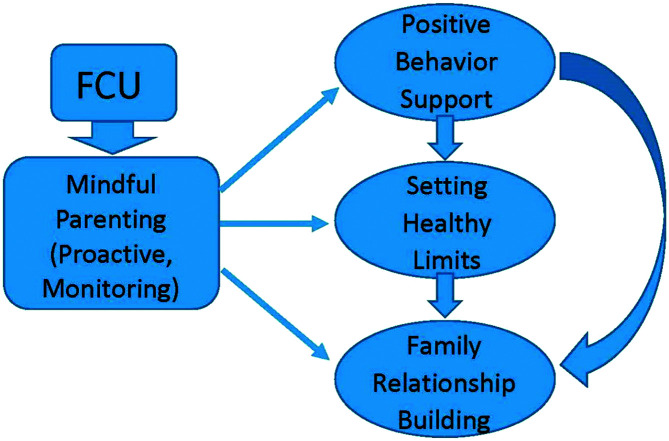
Based on the FCU, FCU-DHH is a BPT adapted for parents of young children who are DHH. The original FCU (Dishion et al., 2008; Stormshak & Dishion, 2009) is an evidence-based BPT focused on harnessing parents' motivation to change and providing them with skills training used preventively or as a clinical intervention. The FCU posits that reinforcement (both positive and negative) develops and maintains continuous patterns of children's negative behaviors followed by parents' coercive behaviors. The intervention relies on focused assessment, motivational interviewing (Miller & Rollnick, 2002), and structured feedback, emphasizing strengths and providing tailored direction toward possible areas of change (see Figure 2). This brief intervention is typically delivered in annual home visits by mental health professionals (Fosco et al., 2013). The first two to three sessions of the FCU involve rapport building and identification of parent concerns and areas of strength; structured assessment of parenting skills via questionnaires and videotaped parent–child tasks; and structured discussion of assessment results, with a focus on parent motivation and a menu of skills training options. If families choose to pursue skills training, then visual aids, videotaped interactions, role play, coaching, in vivo practice, and homework are provided, tailored to the specific skills jointly selected by the parent(s) and interventionist (increasing positive reinforcement, setting consistent and enforceable rules, etc.).
Figure 2.
The family check-up (FCU) model (Dishion et al., 2008; Stormshak & Dishion, 2009).
Based on formative work with parents and service providers who work with the DHH child population and guided by a Community Advisory Board (CAB) that include multilevel stakeholders, the FCU was adapted for parents of young children who are DHH in five ways: (a) The intervention is delivered by a peer coach who is another parent of a child who is DHH; (b) role play scenarios, examples, and homework are targeted to parents of children who are DHH; and existing resources on (c) improving parent–child communication, (d) child development specific to children who are DHH, and (e) advocacy for parents and children are provided by peer coaches to parents as appropriate (Cornell et al., 2018; Studts, 2019). These five adaptations to the original intervention's context and content (Stirman et al., 2013) resulted in the FCU-DHH. Parents randomized to the intervention arm will receive up to six FCU-DHH sessions annually, depending on their needs and preferences. Each session lasts approximately 1 hr, follows the FCU-DHH manual, and is delivered by the same peer coach using online video technology (e.g., Zoom). Sessions are typically delivered weekly for up to 6 weeks but may be spread out over up to a 12-week period.
Control Arm: TAU
The control condition is TAU, in which parent–child dyads will participate in all assessments and receive only usual care. Usual care may vary for dyads in this study arm and includes audiology services, speech-language therapy, and other early intervention and school-based services. Parents in the control arm are not limited from seeking other forms of intervention and support, which will be tracked through research assessments.
Power and Sample Size
The sample size for the RCT is based on power calculations for our primary effectiveness outcome: parenting behaviors, measured by self-report 6 months after baseline. (Note that parenting behaviors measured with the observational Dyadic Parent–Child Interaction Coding System [DPICS; Eyberg et al., 2013] will be assessed annually and analyzed over time, allowing us to triangulate results and include both self-report and observational assessments of parenting behaviors.) Though the design is an individually randomized trial, the FCU-DHH will be delivered by nine peer coaches. To account for the possibility of clustering of outcomes from parent–child dyads who receive the intervention from the same person, we assumed an intracluster correlation coefficient value of .05 to appropriately inflate the required number of dyads in the intervention arm. Furthermore, as previous trials of BPT report medium-sized standardized effects on parenting behaviors (measured with the Parenting Young Children [PARYC] and other self-report and observational measures; Eyberg et al., 2013; Lachman et al., 2016; Lundahl et al., 2006; McEachern et al., 2012; Tonge et al., 2006), we assume an effect size of 0.60. Based on a two-sided test (5% significance level), with 45 parent–child dyads in the control arm and 61 in the intervention arm, we would have 80% power to detect the intervention effect on our primary outcome (parenting behaviors measured at the first 6-month follow-up). Our planned sample size of 53 and 72 parent–child dyads in the control and intervention arms, respectively, is based on increasing the required sample size by 15% to account for possible attrition, though every effort will be made to retain close to 100% of participants. Additional analyses (e.g., the observational DPICS measure of parenting behaviors, child behavior, and language outcomes) will take advantage of the large number of assessment time points planned over 3 years of data collection, so the sample size proposed may be conservative. Regarding child behavior outcomes specifically, standardized effects of BPT are reportedly even higher, suggesting that we will have more than adequate power to test this indicator of effectiveness.
In addition to the 125 parent–child dyads enrolled in the RCT, study participants will include nine peer coaches and 10 hearing health care providers and administrators. These participants will provide data on implementation outcomes and contextual factors, as will a subset of parents (N = 10) from the intervention arm of the RCT with varying effectiveness outcomes and acceptability ratings of the FCU-DHH.
Participants
Parent–Child Dyads
Eligible participants for the RCT will meet the following criteria: (a) Parent is at least 18 years old and is the custodial guardian; (b) child is aged 3–6 years at baseline and lives the majority of time in the parent's home; (c) child is DHH and has used an HA, CI, or bone-conduction device for at least 6 months; (d) parent can read English and can either speak/understand English or use American Sign Language; and (e) parent currently lives in Kentucky with no plans to move out of state for the next 3 years. Parents who have an active child protective services case, have accessed mental health services for the child prior to the trial, or participated in our formative research informing intervention adaptations will not be eligible. Inclusion criteria are intentionally broad due to the effectiveness emphasis of this trial and the evidence for the FCU's effects on parenting behaviors as both a preventive and a clinical intervention. Eligible and interested participants will complete the informed consent process with research staff, reviewing all study procedures, risks, benefits, protections, and alternatives. Parents will provide consent for themselves and their child to participate, and children ages 6 years and above will provide assent.
Peer Coaches
An important qualification for the interventionists in this study was based on strong parent preferences that delivery of the FCU-DHH be by another parent of a child who is DHH (Cornell et al., 2018; Studts, 2019). In response to this preference, we partnered with the Kentucky chapter of Hands & Voices, the largest parent organization in the United States for families raising children who are DHH (http://www.handsandvoices.org). The Kentucky chapter provides a Hands & Voices family support program called “Guide by Your Side” (GBYS), in which parents of children who are DHH are trained to provide unbiased support to other families; our nine FCU-DHH peer coaches will be Guides. Peer coaches will be both interventionists and participants, because implementation data on interventionist characteristics, perceptions of intervention characteristics, acceptability, feasibility, fidelity, and costs will be collected from them throughout the study. A key implementation question addressed by this study is whether peer coaches who are not mental health professionals can deliver the FCU-DHH with high enough fidelity to achieve expected parenting and child outcomes.
Following the informed consent process, peer coaches will be trained in the original FCU by certified trainers from the REACH Institute at Arizona State University, where the FCU intervention is housed. The standard FCU training is an eight-module online learning course, followed by a 2-day highly interactive workshop covering the evidence for the intervention; motivational interviewing techniques; ecological assessments of family strengths and needs; provision of assessment-based motivational feedback; social cognitive and behavioral principles underlying skills training; and how to teach three core practices (positive behavior support, limit setting, and relationship building). A combination of didactic, discussion, modeling, and role play activities are used, and trainees are provided with resources for service delivery. We will expand the training to include human subjects protection training and additional training on the FCU-DHH adaptations (e.g., use of common scenarios described by parents of children who are DHH in role plays; incorporating language facilitation skills and resources to promote parent–child communication), reporting laws and safety protocols, and secure data management practices. During the 3-year intervention period, peer coaches will receive weekly individual supervision from a certified FCU trainer/supervisor, including feedback and coaching based on fidelity (COACH) assessments (Smith et al., 2013). They will also receive group and individual consultation to select relevant resources (communication strategies, and advocacy skills and strategies) for each participating family from the executive director of the Kentucky chapter of Hands & Voices, who assisted with designing these adaptations for FCU-DHH.
Time spent by peer coaches in training, preparation, and intervention delivery will be paid by Hands & Voices at the same rate that the coaches are compensated for their work in the GBYS program; these costs will be reimbursed to Hands & Voices through a subcontract from the principal investigator's institution.
Hearing Health Care Key Stakeholders
Clinicians who provide services to young children who are DHH and their families—primarily comprising audiologists and speech-language pathologists—will participate in key informant interviews addressing their perceptions of the acceptability and feasibility of FCU-DHH, as well as contextual factors serving as barriers or facilitators to its implementation. Administrators of state and regional programs and agencies serving the target population will also participate in key informant interviews to ensure that multilevel perspectives are obtained.
Recruitment and Randomization
Parent–child dyads will be recruited from hearing health care practices across the commonwealth of Kentucky. To maximize our success in recruiting parents, we have partnered with the Kentucky OCSHCN, which annually serves approximately 200 preschool-age DHH children across the state. Additionally, we will recruit parents from private and academic hearing health care practices. Because BPT is used both preventively and as a clinical intervention, there are no requirements that parents report high levels of behavior problems in their children at baseline. Parent–child dyads will be randomized after baseline assessment in a 5:7 ratio to control or intervention to approximately achieve our planned sample size of 53 dyads in the control arm and 72 dyads in the intervention arm. To increase balance between conditions, block randomization will be stratified by hearing device (CI vs. HA or bone-conduction device) and family poverty level (above or below 200% of the federal poverty line), given the associations among these variables, child behavior, and parenting behavior.
The nine peer coaches will be recruited from the Kentucky chapter of Hands & Voices. The 10 hearing health care clinicians and administrators will be recruited with the assistance of our CAB from hearing health care practices and related organizations and agencies across the state. The subset of 10 parents invited to complete key informant interviews will be purposively selected to represent diverse outcomes (e.g., high and low scores for satisfaction with the FCU-DHH) and sociodemographic characteristics (e.g., high and low levels of household income, variable race, and ethnicity).
Assessments
Parent–child dyads in both study arms will complete identical research assessments at baseline and every 6 months for 36 months, for a total of seven time points. The baseline assessments will be administered online using survey software and a video conferencing platform, with assistance from research staff trained in all data collection instruments. Subsequent annual assessments will be conducted in person and will include child language measures. All 6-month follow-up assessments will be completed by parents online (or by mail, if preferred), with research staff assistance available if needed. Research staff administering assessments receive extensive training and ongoing supervision to maintain fidelity to assessment protocols. These research staff will be masked to participants' randomized assignments. Parents will receive $75 for the baseline assessments; $50 for each of the 6-, 18-, and 30-month assessments; and $100 for each of the 12-, 24-, and 36-month assessments. At the end of the trial, parent participants will receive an additional payment of $100 if all seven sets of research assessments are completed, an additional $75 if six sets of assessments are completed, and an additional $50 if five sets of assessments are completed. With parent permission, children will choose a small age-appropriate toy following each of their three speech and language assessments (12, 24, and 36 months). Note that to reflect real-world service delivery, parents in the FCU-DHH arm will not be compensated for attending intervention sessions. The parents (N = 10) purposively selected for key informant interviews will receive an additional $25.
Assessments of peer coaches will occur pre-implementation (pre- and posttraining), throughout implementation, and postimplementation of FCU-DHH. Data collection from peer coaches will involve completion of self-report measures, process logs, and key informant interviews. Assessments of hearing health care clinicians and administrators will take place immediately following the completion of the intervention period, involving self-report measures and key informant interviews. Peer coaches will receive $25 for completion of pre-implementation measures, and peer coaches, clinicians, and administrators will receive $50 for completing postimplementation measures and key informant interviews.
Effectiveness Outcomes
The primary outcome (parenting behaviors at 6-month follow-up) is assessed with the PARYC (McEachern et al., 2012), a reliable and valid self-report instrument developed to assess the use of parenting strategies targeted in the FCU. Parenting behaviors will also be assessed annually with the DPICS (Eyberg et al., 2013), a rigorous, validated observational measure in which parent and child behaviors in video-recorded standardized tasks are rated by trained research staff. Measures of secondary outcomes include child behaviors (subscale and total scores on the Child Behavioral Checklist; Achenbach & Rescorla, 2000), parent report, and objective adherence to HA/CI (measured in minutes using data logging [Walker et al., 2013]; based on formative data, 90% of children are expected to use HA or bone-conduction devices vs. CI), and established expressive and receptive language measures (see Table 1; Dunn & Dunn, 2007; Fenson et al., 2007; Goldman & Fristoe, 2015; Gritz et al., 1993; Osberger et al., 1993; Zimmerman et al., 2011). Given the lack of previous research on effects of BPT on behaviors and language outcomes of children who are DHH, these secondary outcomes are exploratory. Audiology assessment data (aided and unaided pure-tone thresholds) will also be collected from children's hearing health care practices with parental consent and child assent as appropriate. Important covariates will be obtained through the demographic/clinical history questionnaire and medical records (history of prematurity, age of child, type and severity of hearing loss, etiology of hearing loss, family history of hearing loss, other medical or developmental conditions, medical management and surgical history for hearing loss, stability of hearing loss [stable or progressive], age of diagnosis, age of amplification and/or implantation, history of speech assessment, and speech therapy history). Parent and family characteristics will be obtained via the demographic/clinical history questionnaire and the established measures (Beck et al., 1996; Gilmore & Cuskelly, 2009; Nock & Photos, 2006) listed in Table 1.
Table 1.
Assessment schedule for parent–child dyads (intervention and control arms).
| Measure | Time points (months) |
||||||
|---|---|---|---|---|---|---|---|
| 0 | 6 | 12 | 18 | 24 | 30 | 36 | |
| Parent-completed measures | |||||||
| Demographic/history questionnaire | X | ||||||
| Parenting Young Children | X | X | X | X | X | X | X |
| Child Behavior Checklist | X | X | X | X | X | X | X |
| HA/CI adherence questionnaire | X | X | X | X | |||
| Parenting Sense of Competence Scale | X | X | X | X | X | X | X |
| Beck Depression Inventory–II | X | X | X | X | X | X | X |
| Parent Motivation Inventory | X | X | X | X | |||
| MacArthur–Bates Communicative Development Inventories | X | X | X | X | |||
| Meaningful Auditory Integration Scale | X | X | X | X | |||
| Therapy Attitude Inventory (FCU-DHH arm only) | X | X | X | ||||
| Child-completed measures | |||||||
| Peabody Picture Vocabulary Test | X | X | X | ||||
| Preschool Language Scales/Clinical Evaluation of Language Fundamentals | X | X | X | ||||
| Goldman-Fristoe Test of Articulation | X | X | X | ||||
| Beginner's Intelligibility Test | X | X | X | ||||
| Researcher-completed measures | |||||||
| Medical record extraction (including data logging) | X | X | X | X | |||
| DPICS (parent–child interaction ratings) | X | X | X | X | |||
Note. HA = hearing aid; CI = cochlear implant; FCU-DHH = Family Check-Up for Children Who Are Deaf or Hard of Hearing; DPICS = Dyadic Parent–Child Interaction Coding System.
Implementation Outcomes: Acceptability, Feasibility, Fidelity, and Costs
Acceptability will be measured using the peer coach–completed Therapist Satisfaction Index (Addis & Krasnow, 2000); the parent-completed Therapy Attitude Inventory (Brestan et al., 1999; for all parents receiving the FCU-DHH); and key informant interviews with a subset of parents and with peer coaches, providers, and administrators. Peer coaches, providers, and administrators will also complete the Acceptability of Intervention Measure (Weiner et al., 2017) following implementation of FCU-DHH. Feasibility will be assessed using process measures including the number of parent–infant dyads contacted, screened for eligibility, and enrolled, as well as numbers of dyads lost to follow-up, with reasons recorded when known. The number of peer coach contacts with each dyad will also be recorded. Peer coaches, providers, and administrators will also complete the Feasibility of Intervention Measure (Weiner et al., 2017) following implementation of FCU-DHH. Fidelity of FCU-DHH delivery will be measured using peer coach–completed session fidelity checklists and observational fidelity ratings conducted by the clinical supervisor on two randomly selected videotaped FCU-DHH sessions per peer coach per year (Dishion et al., 2010; Smith et al., 2013). Studies of the level of fidelity required to attain significant improvements in parent behaviors for the original FCU provide benchmarks against which peer coaches' fidelity will be assessed (Smith et al., 2013). Assessment of costs will focus on documenting costs of FCU-DHH implementation and training; per-family costs associated with peer coach time in session preparation and delivery, supervision contacts, and additional contacts with families; and family-related expenses. Direct costs will include peer coach training, program implementation (peer coach time, materials, and staff turnover; estimated using process logs and trial documentation), parent time (time spent in sessions; estimated using Bureau of Labor Statistics [BLS] data on average wages in Kentucky), and nonadherence costs (no-show FCU-DHH appointments; estimated using costs of peer coach and supervisor time not used but paid). Indirect costs include opportunity costs of time (e.g., loss of productivity/wages) for the parents, estimated using BLS wage data and calculated time away from work (using process data on session duration). Research activity costs (e.g., data collection and human subjects protection training) will not be included.
Contextual Factors Influencing Implementation From CFIR
Survey measures of CFIR implementation factors (Damschroder et al., 2009) include peer coach (interventionist) characteristics: demographics (age, sex, education, and previous related training and experience), attitude toward evidence-based interventions (Evidence-Based Practice Attitude Scale, 15-item version; Aarons et al., 2010), and self-efficacy to deliver the intervention (Counselor Activity Self-Efficacy Scales; Lent et al., 2003). Characteristics of the intervention (e.g., usability, complexity, and quality of evidence base) will be assessed using the Perceived Characteristics of Intervention Scale (Cook et al., 2015), completed by peer coaches, providers, and administrators. Finally, measures of outer setting characteristics include county population size and presence/number of competing service providers, to be collected from existing sources (e.g., state and census data, median household income, and behavioral provider referral lists). Qualitative key informant interviews will also be conducted using semistructured interview guides designed to assess each CFIR domain, targeted to each stakeholder group (i.e., parents, peer coaches, clinicians, and administrators). See Table 2 for a summary of implementation measures administered to peer coaches, clinicians, and administrators (not including process measures and key informant interviews).
Table 2.
Assessment schedule for peer coaches, providers, and administrators.
| Measure | Time point |
|
|---|---|---|
| Pre-implementation | Postimplementation | |
| Peer coach–completed measures | ||
| Demographic questionnaire | X | |
| Training/practice acceptability | X | |
| EBPAS-15 | X | X |
| Counselor Activity Self-Efficacy Scales | X | X |
| Perceived Characteristics of Intervention Tool | X | X |
| Therapist Satisfaction Index | X | |
| Provider- and administrator-completed measures | ||
| Demographic questionnaire | X | |
| Acceptability of Intervention Measure | X | |
| Feasibility of Intervention Measure | X | |
| Researcher-completed measures | ||
| COACH fidelity observation ratings | Throughout implementation period | |
Note. EBPAS-15 = Evidence-Based Practice Attitude Scale (15-item version).
Data Analysis
The convergent mixed-methods design (Creswell et al., 2011) of this study will involve quantitative analyses of both effectiveness and implementation data, qualitative analyses of effectiveness and implementation data, and intentional integration of results through sampling and interpretation to provide comprehensive understanding of the effects of FCU-DHH and its implementation.
Effectiveness Outcomes
All tests will be two-sided with a 5% significance level and will be conducted in SAS. Analysis methods will account for clustering within peer coaches (i.e., statistical correlation among the outcomes from participants who share the same interventionist). Therefore, analysis of our primary outcome (parenting behaviors as measured by PARYC score at the first 6-month follow-up) will be achieved with linear mixed-effects modeling, with random effects to account for this clustering (Fitzmaurice et al., 2011). A fixed effect for trial arm (FCU-DHH vs. TAU) will be the primary covariate of interest. Additional analyses will address each outcome over time (i.e., PARYC scores, DPICS scores, measures of child behavior, parent report and objective adherence with HA/CI, and language development). In longitudinal analyses, linear mixed-effects modeling will be adjusted to account for the additional level of correlation among outcomes from the same subject (e.g., a random time effect or an unstructured covariance). Fixed effects will include trial arm, time (categorical or continuous variable), and their interaction, with the interaction being of primary interest. Because rolling study enrollment is necessary, some parent–child dyads may have fewer observations than others. Recommended statistical approaches will be used for missing data within interventionists (e.g., multiple imputation at the subject and cluster level; Gomes et al., 2013). Sensitivity analyses will be considered and dictated by the type of missing data. We will measure potentially important predictors (e.g., sex, race, parental age, socioeconomic status, degree of hearing loss, type of hearing rehabilitation device, and baseline language development) and statistically compare the balance of the two trial arms. Secondary analyses will include these variables as covariates. Stratified randomization will be accounted for in analyses.
Implementation Outcomes and Contextual Factors
The convergent mixed-methods design (Creswell et al., 2011) will allow simultaneous consideration of quantitative and qualitative data from multiple perspectives to contextualize and gain a more complete understanding of key implementation factors linked with the effectiveness and implementation outcomes of the FCU-DHH. Because most implementation data in this Type 1 hybrid trial come from a small sample (N = 30) of parents, peer coaches, providers, and administrators, analyses are primarily descriptive and intended to inform a future implementation trial and potential scale-up of the FCU-DHH, if effective. For quantitative measures of implementation outcomes and factors, descriptive statistics will summarize data within and across the peer coaches. If analyses detect between-coaches differences in effectiveness outcomes, differences in coach-specific implementation outcomes and factors will be examined to identify possible patterns contributing to differential effectiveness. Exploratory analyses targeting implementation outcomes and factors will be conducted between intervention coaches regardless of effectiveness outcomes, using models appropriate for the small sample size and levels of data.
Recordings of key informant interviews will be transcribed verbatim and analyzed using directed content analysis (Hsieh & Shannon, 2005), in which contextual factors serving as barriers and facilitators to implementation will be coded using CFIR domains and constructs. Rigorous procedures will be used to ensure the validity and reliability of qualitative analyses, including iterative development of codebooks, use of multiple coders, and resolution of discordant coding through review, discussion, and revision until consensus is reached. Member checking will be conducted with two participants from each group of key informant interviews (parents, peer coaches, providers, and administrators) to ensure that valid inferences are made through coding procedures (Fielding & Fielding, 1988). Finally, we will develop a summative grid of identified themes and joint displays integrating qualitative and quantitative results. Results will comprehensively describe the implementation experience according to key stakeholders and identify potential multilevel barriers and facilitators important to understand and address in future research and implementation efforts of FCU-DHH.
Discussion
Young children who are DHH and use HA/CI may benefit from evidence-based behavioral interventions, but there is a significant gap between this need and the actual provision of these interventions to this population (Fellinger et al., 2012; Hindley et al., 1994; Sessa & Sutherland, 2013; Vernon & Leigh, 2007). Additionally, there is a lack of research in this area, with few published studies addressing the behavioral issues of children who are DHH and even fewer testing potential solutions (Muñoz et al., 2021). In this Type 1 hybrid effectiveness–implementation trial, we will rigorously test the effectiveness of an evidence-based BPT intervention adapted for parents of young children who are DHH. By simultaneously assessing implementation outcomes and contextual factors serving as barriers or facilitators to implementation, we will obtain important information regarding the potential of scaling up this approach, if it is found to be effective.
The FCU-DHH intervention is based on a BPT intervention shown to be highly effective in families with children with typical hearing experiencing a wide range of behavioral challenges (Dishion et al., 2008; Stormshak & Dishion, 2009). With adaptations based on extensive stakeholder engagement to increase the salience of the intervention for a new target population (Cornell et al., 2018; Studts, 2019), ongoing partnerships with our state chapter of Hands & Voices and the OCSHCN, and guidance from our active CAB, we will conduct the first RCT of a BPT intervention for parents of young children who are DHH. Our examination of implementation outcomes (Proctor et al., 2011) and contextual factors influencing implementation (Damschroder et al., 2009) will inform subsequent studies testing implementation strategies to increase access to effective BPT in this understudied population.
Strengths of this project include buy-in from key stakeholder groups and organizations; delivery of FCU-DHH by “real-world” Hands & Voices parent guides; and a rigorous RCT design testing intervention effects on outcomes that are meaningful to parents of children who are DHH and to other stakeholders, including audiologists, speech-language pathologists, and hearing health care administrators (e.g., parenting behavior, child behavior, and HA/CI adherence). Additionally, our continuous stakeholder engagement throughout the project; assessment of implementation outcomes including acceptability, feasibility, fidelity, and costs; and exploration of multilevel contextual factors affecting implementation will inform future studies, practice, and policy regarding the behavioral intervention needs of families with children who are DHH.
Acknowledgments
The protocol described was supported by National Institute on Deafness and Other Communication Disorders Award R01DC016957 (Studts, PI). All project costs ($2,851,335) are financed with this Federal support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank the parents and service providers who shared valuable information about their perspectives, experiences, and preferences in our formative work. Additionally, the authors would like to thank the research assistants and interventionists who contributed to preliminary studies for this trial, including Meagan Pilar, Allie Merritt, Cady Cornell, Mallory Antel, Vashisht Madabhushi, Meghan Phelan, Laura Bellnier, Emily Goble, Heather Davis, and Tess Smith. The authors also thank Cathy Lester, Sarah Roof, and Lori Travis for their ongoing work to connect us with state partnering agencies and Lisa Kovacs, Hands & Voices Director of Programs, for contributions to training and adaptation resources. Special thanks to Yasaman Parsi, the REACH Institute, and Jessica Jaramillo for exceptional training and support in the FCU. We acknowledge the University of Kentucky Center for Clinical and Translational Science (UL1TR001998) and the University of Kentucky College of Medicine for supporting our preliminary studies. Finally, we are grateful to the members of our Hearing and Behavior Community Advisory Board, who informed this work each step of the way.
Funding Statement
The protocol described was supported by National Institute on Deafness and Other Communication Disorders Award R01DC016957 (Studts, PI). All project costs ($2,851,335) are financed with this Federal support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank the parents and service providers who shared valuable information about their perspectives, experiences, and preferences in our formative work. Additionally, the authors would like to thank the research assistants and interventionists who contributed to preliminary studies for this trial, including Meagan Pilar, Allie Merritt, Cady Cornell, Mallory Antel, Vashisht Madabhushi, Meghan Phelan, Laura Bellnier, Emily Goble, Heather Davis, and Tess Smith. The authors also thank Cathy Lester, Sarah Roof, and Lori Travis for their ongoing work to connect us with state partnering agencies and Lisa Kovacs, Hands & Voices Director of Programs, for contributions to training and adaptation resources. Special thanks to Yasaman Parsi, the REACH Institute, and Jessica Jaramillo for exceptional training and support in the FCU. We acknowledge the University of Kentucky Center for Clinical and Translational Science (UL1TR001998) and the University of Kentucky College of Medicine for supporting our preliminary studies.
References
- Aarons, G. A. , Glisson, C. , Hoagwood, K. , Kelleher, K. , Landsverk, J. , & Cafri, G. (2010). Psychometric properties and U.S. national norms of the Evidence-Based Practice Attitude Scale (EBPAS). Psychological Assessment, 22(2), 356–365. https://doi.org/10.1037/a0019188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach, T. M. , & Rescorla, L. A. (2000). Manual for ASEBA preschool forms and profiles. University of Vermont Department of Psychiatry. [Google Scholar]
- Addis, M. E. , & Krasnow, A. D. (2000). A national survey of practicing psychologists' attitudes toward psychotherapy treatment manuals. Journal of Consulting and Clinical Psychology, 68(2), 331–339. https://doi.org/10.1037//0022-006x.68.2.331 [DOI] [PubMed] [Google Scholar]
- American Academy of Audiology. (2013). American Academy of Audiology clinical practice guidelines: Pediatric amplification. https://audiology-web.s3.amazonaws.com/migrated/PediatricAmplificationGuidelines.pdf_539975b3e7e9f1.74471798.pdf
- American Speech-Language-Hearing Association. (2020). Practice portal: Permanent childhood hearing loss. https://www.asha.org/practice-portal/clinical-topics/permanent-childhood-hearing-loss/#collapse_6
- Balas, E. A. , & Boren, S. A. (2000). Managing clinical knowledge for health care improvement. In McCray I. J. B. A. T. (Ed.), Yearbook of medical informatics (pp. 65–70). Thieme. https://doi.org/10.1055/s-0038-1637943 [PubMed] [Google Scholar]
- Bandura, A. (1977). Social learning theory. Prentice Hall. [Google Scholar]
- Barker, D. H. , Quittner, A. L. , Fink, N. E. , Eisenberg, L. S. , Tobey, E. A. , Niparko, J. K. , & Team, C. I. (2009). Predicting behavior problems in deaf and hearing children: The influences of language, attention, and parent–child communication. Development and Psychopathology, 21(2), 373–392. https://doi.org/10.1017/S0954579409000212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. T. , Steer, R. A. , & Brown, G. K. (1996). Manual for the Beck Depression Inventory–II. The Psychological Corporation. https://doi.org/10.1037/t00742-000 [Google Scholar]
- Brestan, E. V. , Jacobs, J. R. , Rayfield, A. D. , & Eyberg, S. M. (1999). A consumer satisfaction measure for parent–child treatments and its relation to measures of child behavior change. Behavior Therapy, 30(1), 17–30. https://doi.org/10.1016/S0005-7894(99)80043-4 [Google Scholar]
- Centers for Disease Control and Prevention. (2014). Essentials for childhood: Steps to create safe, stable, nurturing relationships and environments. https://www.cdc.gov/violenceprevention/pdf/essentials_for_childhood_framework.pdf
- Centers for Disease Control and Prevention. (2021). CDC Early Hearing Detection and Intervention (EHDI) Hearing Screening & Follow-up Survey (HSFS). https://www.cdc.gov/ncbddd/hearingloss/2019-data/documents/01-2019-HSFS-Data-Summary-h.pdf
- Cook, J. M. , Thompson, R. , & Schnurr, P. P. (2015). Perceived Characteristics of Intervention Scale. Assessment, 22(6), 704–714. https://doi.org/10.1177/1073191114561254 [DOI] [PubMed] [Google Scholar]
- Cornell, C. B. , Antel, M. N. , Merritt, A. S. , Jacobs, J. A. , Bush, M. L. , & Studts, C. R. (2018). Adaptations to the family check-up for deaf and hard of hearing children: A qualitative analysis. 146th Annual Meeting of the American Public Health Association, San Diego, CA, United States. [Google Scholar]
- Creswell, J. , Klassen, A. , Plano Clark, V. , & Smith, K. C. (2011). Best practices for mixed methods research in the health sciences. National Institutes of Health. https://doi.org/10.1037/e566732013-001 [Google Scholar]
- Curran, G. M. , Bauer, M. , Mittman, B. , Pyne, J. M. , & Stetler, C. (2012). Effectiveness–implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50(3), 217–226. https://doi.org/10.1097/MLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder, L. J. , Aron, D. C. , Keith, R. E. , Kirsh, S. R. , Alexander, J. A. , & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4(1), 50. https://doi.org/10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder, L. J. , & Lowery, J. C. (2013). Evaluation of a large-scale weight management program using the Consolidated Framework for Implementation Research (CFIR). Implementation Science, 8(1), 51. https://doi.org/10.1186/1748-5908-8-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharitri, R. , & Murthy, V. N. (1990). Hearing impaired children: Their behaviour problems and parental attitudes. Journal of Clinical Psychology, 17, 12–16. [Google Scholar]
- Dishion, T. J. , Knutson, M. , Brauer, L. , Gill, A. , & Risso, J. (2010). Family check-up: COACH ratings manual. Child and Family Center, University of Oregon. [Google Scholar]
- Dishion, T. J. , Shaw, D. , Connell, A. , Gardner, F. , Weaver, C. , & Wilson, M. (2008). The family check-up with high-risk indigent families: Preventing problem behavior by increasing parents' positive behavior support in early childhood. Child Development, 79(5), 1395–1414. https://doi.org/10.1111/j.1467-8624.2008.01195.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dretzke, J. , Frew, E. , Davenport, C. , Barlow, J. , Stewart-Brown, S. , Sandercock, J. , Bayliss, S. , Raftery, J. , Hyde, C. , & Taylor, R. (2005). The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children. Health Technology Assessment, 9(50), 1–233. https://doi.org/10.3310/hta9500 [DOI] [PubMed] [Google Scholar]
- Dunn, L. M. , & Dunn, D. M. (2007). PPVT-4: Peabody Picture Vocabulary Test–Fourth Edition. APA PsycTests. https://doi.org/10.1037/t15144-000 [Google Scholar]
- Dye, M. W. , & Hauser, P. C. (2014). Sustained attention, selective attention and cognitive control in deaf and hearing children. Hearing Research, 309, 94–102. https://doi.org/10.1016/j.heares.2013.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg, S. M. , Nelson, M. M. , Ginn, N. C. , Bhuiyan, N. , & Boggs, S. R. (2013). Dyadic Parent–Child Interaction Coding System, Fourth Edition (DPICS-IV) comprehensive manual for research and training. PCIT International. [Google Scholar]
- Fellinger, J. (2011). The effect of early confirmation of hearing loss on the behaviour in middle childhood of children with bilateral hearing impairment. Developmental Medicine and Child Neurology, 53(3), 198. https://doi.org/10.1111/j.1469-8749.2010.03875.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellinger, J. , Holzinger, D. , & Pollard, R. (2012). Mental health of deaf people. The Lancet, 379(9820), 1037–1044. https://doi.org/10.1016/S0140-6736(11)61143-4 [DOI] [PubMed] [Google Scholar]
- Fenson, L. , Marchman, V. A. , Thal, D. J. , Dale, P. S. , Reznick, J. S. , & Bates, E. (2007). MacArthur–Bates Communicative Development Inventories. Brookes. https://doi.org/10.1037/t11538-000 [Google Scholar]
- Fielding, N. G. , & Fielding, J. L. (1988). Linking data. Sage. [Google Scholar]
- Fiorillo, C. E. , Rashidi, V. , Westgate, P. M. , Jacobs, J. A. , Bush, M. L. , & Studts, C. R. (2017). Assessment of behavioral problems in children with hearing loss. Otology & Neurotology, 38(10), 1456–1462. https://doi.org/10.1097/MAO.0000000000001583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzmaurice, G. M. , Laird, N. M. , & Ware, J. H. (2011). Applied longitudinal analysis (2nd ed.). Wiley. https://doi.org/10.1002/9781119513469 [Google Scholar]
- Fosco, G. M. , Frank, J. L. , Stormshak, E. A. , & Dishion, T. J. (2013). Opening the “black box”: Family check-up intervention effects on self-regulation that prevents growth in problem behavior and substance use. Journal of School Psychology, 51(4), 455–468. https://doi.org/10.1016/j.jsp.2013.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, D. , Bagner, D. M. , Pruden, S. M. , & Nichols-Lopez, K. (2015). Language production in children with and at risk for delay: Mediating role of parenting skills. Journal of Clinical Child and Adolescent Psychology, 44(5), 814–825. https://doi.org/10.1080/15374416.2014.900718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore, L. , & Cuskelly, M. (2009). Factor structure of the Parenting Sense of Competence Scale using a normative sample. Child: Care Health and Development, 35(1), 48–55. https://doi.org/10.1111/j.1365-2214.2008.00867.x [DOI] [PubMed] [Google Scholar]
- Glasgow, R. E. , Harden, S. M. , Gaglio, B. , Rabin, B. , Smith, M. L. , Porter, G. C. , Ory, M. G. , & Estabrooks, P. A. (2019). RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Frontiers in Public Health, 7, 64. https://doi.org/10.3389/fpubh.2019.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, R. , & Fristoe, M. (2015). Goldman-Fristoe Test of Articulation–Third Edition. Pearson. [Google Scholar]
- Gomes, M. , Díaz-Ordaz, K. , Grieve, R. , & Kenward, M. G. (2013). Multiple imputation methods for handling missing data in cost-effectiveness analyses that use data from hierarchical studies: An application to cluster randomized trials. Medical Decision Making, 33(8), 1051–1063. https://doi.org/10.1177/0272989X13492203 [DOI] [PubMed] [Google Scholar]
- Gonzalez, M. A. , & Jones, D. J. (2016). Cascading effects of BPT for child internalizing problems and caregiver depression. Clinical Psychology Review, 50, 11–21. https://doi.org/10.1016/j.cpr.2016.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granic, I. , & Lougheed, J. P. (2016). The role of anxiety in coercive family processes with aggressive children. In Dishion T. J. & Snyder J. J. (Eds.), The Oxford handbook of coercive relationship dynamics (pp. 231–248). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199324552.013.18 [Google Scholar]
- Grant, J. , Green, L. , & Mason, B. (2003). Basic research and health: A reassessment of the scientific basis for the support of biomedical science. Research Evaluation, 12(3), 217–224. https://doi.org/10.3152/147154403781776618 [Google Scholar]
- Gritz, E. R. , Carr, C. R. , Rapkin, D. , Abemayor, E. , Chang, L. J. , Wong, W. K. , Belin, T. R. , Calcaterra, T. , Robbins, K. T. , & Chonkich, G. (1993). Predictors of long-term smoking cessation in head and neck cancer patients. Cancer Epidemiology, Biomarkers & Prevention, 2(3), 261–270. [PubMed] [Google Scholar]
- Gross, H. E. , Shaw, D. S. , Moilanen, K. L. , Dishion, T. J. , & Wilson, M. N. (2008). Reciprocal models of child behavior and depressive symptoms in mothers and fathers in a sample of children at risk for early conduct problems. Journal of Family Psychology, 22(5), 742–751. https://doi.org/10.1037/a0013514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindley, P. & Kitson, N. (Eds.). (2000). Mental health and deafness. Whurr. [Google Scholar]
- Hindley, P. A. , Hill, P. D. , McGuigan, S. , & Kitson, N. (1994). Psychiatric disorder in deaf and hearing impaired children and young people: A prevalence study. The Journal of Child Psychology and Psychiatry, 35(5), 917–934. https://doi.org/10.1111/j.1469-7610.1994.tb02302.x [DOI] [PubMed] [Google Scholar]
- Hogan, A. , Shipley, M. , Strazdins, L. , Purcell, A. , & Baker, E. (2011). Communication and behavioural disorders among children with hearing loss increases risk of mental health disorders. Australian and New Zealand Journal of Public Health, 35(4), 377–383. https://doi.org/10.1111/j.1753-6405.2011.00744.x [DOI] [PubMed] [Google Scholar]
- Horn, D. L. , Pisoni, D. B. , Sanders, M. , & Miyamoto, R. T. (2005). Behavioral assessment of prelingually deaf children before cochlear implantation. Laryngoscope, 115(9), 1603–1611. https://doi.org/10.1097/01.mlg.0000171018.97692.c0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh, H. F. , & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Kaminski, J. W. , Valle, L. A. , Filene, J. H. , & Boyle, C. L. (2008). A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology, 36(4), 567–589. https://doi.org/10.1007/s10802-007-9201-9 [DOI] [PubMed] [Google Scholar]
- Keenan, K. , & Wakschlag, L. S. (2002). Can a valid diagnosis of disruptive behavior disorder be made in preschool children? American Journal of Psychiatry, 159(3), 351–358. https://doi.org/10.1176/appi.ajp.159.3.351 [DOI] [PubMed] [Google Scholar]
- Keith, R. E. , Crosson, J. C. , O'Malley, A. S. , Cromp, D. , & Taylor, E. F. (2017). Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: A rapid-cycle evaluation approach to improving implementation. Implementation Science, 12(1), 15. https://doi.org/10.1186/s13012-017-0550-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kentucky Cabinet for Health and Family Services. (n.d.). Newborn hearing screening program. https://chfs.ky.gov/agencies/ccshcn/Pages/newbornscreening.aspx
- Lachman, J. M. , Sherr, L. , Cluver, L. , Ward, C. L. , Hutchings, J. , & Gardner, F. (2016). Integrating evidence and context to develop a parenting program for low-income families in South Africa. Journal of Child and Family Studies, 25(7), 2337–2352. https://doi.org/https://doi.org/10.1007/s10826-016-0389-6 [Google Scholar]
- Lavigne, J. V. , Cicchetti, C. , Gibbons, R. D. , Binns, H. J. , Larsen, L. , & DeVito, C. (2001). Oppositional defiant disorder with onset in preschool years: Longitudinal stability and pathways to other disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 40(12), 1393–1400. https://doi.org/10.1097/00004583-200112000-00009 [DOI] [PubMed] [Google Scholar]
- Lavigne, J. V. , Lebailly, S. A. , Hopkins, J. , Gouze, K. R. , & Binns, H. J. (2009). The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child and Adolescent Psychology, 38(3), 315–328. https://doi.org/10.1080/15374410902851382 [DOI] [PubMed] [Google Scholar]
- Lent, R. W. , Hill, C. E. , & Hoffman, M. A. (2003). Development and validation of the Counselor Activity Self-Efficacy Scales. Journal of Counseling Psychology, 50(1), 97–108. https://doi.org/https://doi.org/10.1037/0022-0167.50.1.97 [Google Scholar]
- Levickis, P. , Sciberras, E. , McKean, C. , Conway, L. , Pezic, A. , Mensah, F. K. , Bavin, E. L. , Bretherton, L. , Eadie, P. , Prior, M. , & Reilly, S. (2018). Language and social-emotional and behavioural wellbeing from 4 to 7 years: A community-based study. European Child & Adolescent Psychiatry, 27(7), 849–859. https://doi.org/10.1007/s00787-017-1079-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl, B. , Risser, H. J. , & Lovejoy, M. C. (2006). A meta-analysis of parent training: Moderators and follow-up effects. Clinical Psychology Review, 26(1), 86–104. https://doi.org/10.1016/j.cpr.2005.07.004 [DOI] [PubMed] [Google Scholar]
- McEachern, A. D. , Dishion, T. J. , Weaver, C. M. , Shaw, D. S. , Wilson, M. N. , & Gardner, F. (2012). Parenting Young Children (PARYC): Validation of a self-report parenting measure. Journal of Child and Family Studies, 21(3), 498–511. https://doi.org/10.1007/s10826-011-9503-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehra, S. , Eavey, R. D. , & Keamy, D. G. (2009). The epidemiology of hearing impairment in the United States: Newborns, children, and adolescents. Otolaryngology—Head & Neck Surgery, 140(4), 461–472. https://doi.org/10.1016/j.otohns.2008.12.022 [DOI] [PubMed] [Google Scholar]
- Menting, A. T. , Orobio de Castro, B. , & Matthys, W. (2013). Effectiveness of the incredible years parent training to modify disruptive and prosocial child behavior: A meta-analytic review. Clinical Psychology Review, 33(8), 901–913. https://doi.org/10.1016/j.cpr.2013.07.006 [DOI] [PubMed] [Google Scholar]
- Michelson, D. , Davenport, C. , Dretzke, J. , Barlow, J. , & Day, C. (2013). Do evidence-based interventions work when tested in the “real world?” A systematic review and meta-analysis of parent management training for the treatment of child disruptive behavior. Clinical Child and Family Psychology Review, 16(1), 18–34. https://doi.org/10.1007/s10567-013-0128-0 [DOI] [PubMed] [Google Scholar]
- Miller, W. R. , & Rollnick, S. (2002). Motivational interviewing: Preparing people for change (2nd ed.). Guildford. https://doi.org/10.1097/01445442-200305000-00013 [Google Scholar]
- Moeller, M. P. , Hoover, B. , Peterson, B. , & Stelmachowicz, P. (2009). Consistency of hearing aid use in infants with early-identified hearing loss. American Journal of Audiology, 18(1), 14–23. https://doi.org/10.1044/1059-0889(2008/08-0010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt, T. E. (1993). Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychological Review, 100(4), 674–701. https://doi.org/10.1037/0033-295X.100.4.674 [PubMed] [Google Scholar]
- Morris, Z. S. , Wooding, S. , & Grant, J. (2011). The answer is 17 years, what is the question: Understanding time lags in translational research. Journal of the Royal Society of Medicine, 104(12), 510–520. https://doi.org/10.1258/jrsm.2011.110180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz, K. , Nichols, N. , & Hills, S. (2021). Psychosocial experiences of parents of young children who use hearing devices: A scoping review. Journal of Early Hearing Detection and Intervention, 6(1), 90–95. https://doi.org/https://doi.org/10.26077/2656-d109 [Google Scholar]
- Muñoz, K. , Olson, W. A. , Twohig, M. P. , Preston, E. , Blaiser, K. , & White, K. R. (2015). Pediatric hearing aid use. Ear and Hearing, 36(2), 279–287. https://doi.org/10.1097/AUD.0000000000000111 [DOI] [PubMed] [Google Scholar]
- Muñoz, K. , Rusk, S. E. , Nelson, L. , Preston, E. , White, K. R. , Barrett, T. S. , & Twohig, M. P. (2016). Pediatric hearing aid management: Parent-reported needs for learning support. Ear and Hearing, 37(6), 703–709. https://doi.org/10.1097/AUD.0000000000000338 [DOI] [PubMed] [Google Scholar]
- Nilsen, P. , & Bernhardsson, S. (2019). Context matters in implementation science: A scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Services Research, 19(1), 189. https://doi.org/10.1186/s12913-019-4015-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock, M. K. , & Photos, V. I. (2006). Parent motivation to participate in treatment: Assessment and prediction of subsequent participation. Journal of Child and Family Studies, 15(3), 333–346. https://doi.org/https://doi.org/10.1007/s10826-006-9022-4 [Google Scholar]
- Osberger, M. J. , Maso, M. , & Sam, L. K. (1993). Speech intelligibility of children with cochlear implants, tactile aids, or hearing aids. Journal of Speech and Hearing Research, 36(1), 186–203. https://doi.org/10.1044/jshr.3601.186 [DOI] [PubMed] [Google Scholar]
- Patterson, G. R. , DeBaryshe, B. D. , & Ramsey, E. (1989). A developmental perspective on antisocial behavior. American Psychologist, 44(2), 329–335. https://doi.org/10.1037/0003-066X.44.2.329 [DOI] [PubMed] [Google Scholar]
- Patterson, G. R. , & Yorger, K. A. (2002). A developmental model for early- and late-onset antisocial behavior. In Reid J. B., Snyder J., & Patterson G. R. (Eds.), Antisocial behavior in children and adolescents: A developmental analysis and model for intervention (pp. 147–172). American Psychological Association. https://doi.org/10.1037/10468-007 [Google Scholar]
- Pelham, W. E. , Foster, E. M. , & Robb, J. A. (2007). The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Journal of Pediatric Psychology, 32(6), 711–727. https://doi.org/10.1093/jpepsy/jsm022 [DOI] [PubMed] [Google Scholar]
- Perou, R. , Bitsko, R. H. , Blumberg, S. J. , Pastor, P. , Ghandour, R. M. , Gfroerer, J. C. , Hedden, S. L. , Crosby, A. E. , Visser, S. N. , Schieve, L. A. , Parks, S. E. , Hall, J. E. , Brody, D. , Simile, C. M. , Thompson, W. W. , Baio, J. , Avenevoli, S. , Kogan, M. D. , Huang, L. N. , & Centers for Disease Control and Prevention. (2013). Mental health surveillance among children—United States, 2005-2011. Morbidity and Mortality Weekly Reports Supplements, 62(2), 1–35. [PubMed] [Google Scholar]
- Proctor, E. , Silmere, H. , Raghavan, R. , Hovmand, P. , Aarons, G. , Bunger, A. , Griffey, R. , & Hensley, M. (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health, 38(2), 65–76. https://doi.org/10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinke, W. M. , Eddy, J. M. , Dishion, T. J. , & Reid, J. B. (2012). Joint trajectories of symptoms of disruptive behavior problems and depressive symptoms during early adolescence and adjustment problems during emerging adulthood. Journal of Abnormal Child Psychology, 40(7), 1123–1136. https://doi.org/10.1007/s10802-012-9630-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safaeinili, N. , Brown-Johnson, C. , Shaw, J. G. , Mahoney, M. , & Winget, M. (2020). CFIR simplified: Pragmatic application of and adaptations to the Consolidated Framework for Implementation Research (CFIR) for evaluation of a patient-centered care transformation within a learning health system. Learning Health Systems, 4(1), e10201. https://doi.org/10.1002/lrh2.10201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaeffer, C. M. , Petras, H. , Ialongo, N. , Masyn, K. E. , Hubbard, S. , Poduska, J. , & Kellam, S. (2006). A comparison of girls' and boys' aggressive-disruptive behavior trajectories across elementary school: Prediction to young adult antisocial outcomes. Journal of Consulting and Clinical Child Psychology, 74(3), 500–510. https://doi.org/10.1037/0022-006X.74.3.500 [DOI] [PubMed] [Google Scholar]
- Schulz, K. F. , Altman, D. G. , Moher, D. , & CONSORT Group. (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Trials, 11(1), 32. https://doi.org/10.1186/1745-6215-11-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sessa, B. , & Sutherland, H. (2013). Addressing mental health needs of deaf children and their families: The National Deaf Child and Adolescent Mental Health Service. The Psychiatrist, 37(5), 175–178. https://doi.org/10.1192/pb.bp.112.038604 [Google Scholar]
- Smith, J. D. , Dishion, T. J. , Shaw, D. S. , & Wilson, M. N. (2013). Indirect effects of fidelity to the family check-up on changes in parenting and early childhood problem behaviors. Journal of Consulting and Clinical Child Psychology, 81(6), 962–974. https://doi.org/10.1037/a0033950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson, J. , McCann, D. C. , Law, C. M. , Mullee, M. , Petrou, S. , Worsfold, S. , & Kennedy, C. R. (2011). The effect of early confirmation of hearing loss on the behaviour in middle childhood of children with bilateral hearing impairment. Developmental Medicine and Child Neurology, 53(3), 269–274. https://doi.org/10.1111/j.1469-8749.2010.03839.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson, J. , McCann, D. C. , Watkin, P. , Worsfold, S. , Kennedy, C. , & Hearing Outcomes Study Team. (2010). The relationship between language development and behaviour problems in children with hearing loss. The Journal of Child Psychology and Psychiatry, 51(1), 77–83. https://doi.org/10.1111/j.1469-7610.2009.02124.x [DOI] [PubMed] [Google Scholar]
- Stevenson, J. , Pimperton, H. , Kreppner, J. , Worsfold, S. , Terlektsi, E. , & Kennedy, C. (2017). Emotional and behaviour difficulties in teenagers with permanent childhood hearing loss. International Journal of Pediatric Otorhinolaryngology, 101, 186–195. https://doi.org/10.1016/j.ijporl.2017.07.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirman, S. W. , Miller, C. J. , Toder, K. , & Calloway, A. (2013). Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implementation Science, 8(1), 65. https://doi.org/10.1186/1748-5908-8-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stormshak, E. A. , Bierman, K. L. , McMahon, R. J. , & Lengua, L. J. (2000). Parenting practices and child disruptive behavior problems in early elementary school. Journal of Clinical Child Psychology, 29(1), 17–29. https://doi.org/10.1207/S15374424jccp2901_3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stormshak, E. A. , & Dishion, T. J. (2009). A school-based, family-centered intervention to prevent substance use: The family check-up. American Journal of Drug and Alcohol Abuse, 35(4), 227–232. https://doi.org/10.1080/00952990903005908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studts, C. R. (2019). Adaptation and implementation of an evidence-based parenting intervention for families of children who are DHH. 2019 American Speech-Language-Hearing Association Convention, Orlando, FL, United States. [Google Scholar]
- Tandon, M. , Cardeli, E. , & Luby, J. (2009). Internalizing disorders in early childhood: A review of depressive and anxiety disorders. Child and Adolescent Psychiatric Clinics of North America, 18(3), 593–610. https://doi.org/10.1016/j.chc.2009.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theunissen, S. C. , Rieffe, C. , Kouwenberg, M. , De Raeve, L. J. , Soede, W. , Briaire, J. J. , & Frijns, J. H. (2014). Behavioral problems in school-aged hearing-impaired children: The influence of sociodemographic, linguistic, and medical factors. European Child and Adolescent Psychiatry, 23(4), 187–196. https://doi.org/10.1007/s00787-013-0444-4 [DOI] [PubMed] [Google Scholar]
- Tomblin, J. B. , Harrison, M. , Ambrose, S. E. , Walker, E. A. , Oleson, J. J. , & Moeller, M. P. (2015). Language outcomes in young children with mild to severe hearing loss. Ear and Hearing, 36(Suppl. 1), 76S–91S. https://doi.org/10.1097/AUD.0000000000000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Tonge, B. , Brereton, A. , Kiomall, M. , Mackinnon, A. , King, N. , & Rinehart, N. (2006). Effects on parental mental health of an education and skills training program for parents of young children with autism: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 45(5), 561–569. https://doi.org/10.1097/01.chi.0000205701.48324.26 [DOI] [PubMed] [Google Scholar]
- Vernon, M. , & Leigh, I. W. (2007). Mental health services for people who are deaf. American Annals of the Deaf, 152(4), 374–381. https://doi.org/10.1353/aad.2008.0005 [DOI] [PubMed] [Google Scholar]
- Walker, E. A. , Spratford, M. , Moeller, M. P. , Oleson, J. , Ou, H. , Roush, P. , & Jacobs, S. (2013). Predictors of hearing aid use time in children with mild-to-severe hearing loss. Language, Speech, and Hearing Services in Schools, 44(1), 73–88. https://doi.org/10.1044/0161-1461(2012/12-0005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton, C. , & Hammond, M. (1997). Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology, 65(1), 93–109. https://doi.org/10.1037//0022-006x.65.1.93 [DOI] [PubMed] [Google Scholar]
- Webster-Stratton, C. , Reid, M. J. , & Hammond, M. (2004). Treating children with early-onset conduct problems: Intervention outcomes for parent, child, and teacher training. Journal of Clinical Child and Adolescent Psychology, 33(1), 105–124. https://doi.org/10.1207/S15374424JCCP3301_11 [DOI] [PubMed] [Google Scholar]
- Webster-Stratton, C. , Rinaldi, J. , & Jamila, M. R. (2011). Long-term outcomes of incredible years parenting program: Predictors of adolescent adjustment. Child and Adolescent Mental Health, 16(1), 38–46. https://doi.org/10.1111/j.1475-3588.2010.00576.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner, B. J. , Lewis, C. C. , Stanick, C. , Powell, B. J. , Dorsey, C. N. , Clary, A. S. , Boynton, M. H. , & Halko, H. (2017). Psychometric assessment of three newly developed implementation outcome measures. Implementation Science, 12(1), 108. https://doi.org/10.1186/s13012-017-0635-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshinaga-Itano, C. (2004). Levels of evidence: Universal newborn hearing screening (UNHS) and early hearing detection and intervention systems (EHDI). Journal of Communication Disorders, 37(5), 451–465. https://doi.org/10.1016/j.jcomdis.2004.04.008 [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano, C. , Sedey, A. L. , Coulter, D. K. , & Mehl, A. L. (1998). Language of early- and later-identified children with hearing loss. Pediatrics, 102(5), 1161–1171. https://doi.org/10.1542/peds.102.5.1161 [DOI] [PubMed] [Google Scholar]
- Zimmerman, I. L. , Steiner, V. G. , & Pond, R. E. (2011). Preschool Language Scales. Pearson Education. https://doi.org/10.1037/t15141-000 [Google Scholar]



 This work is licensed under a
This work is licensed under a