Abstract
Purpose:
The external validity of aphasia treatment research relies on diverse and representative participants. The purposes of this study were (a) to examine whether reporting of patient-reported age, sex, and race/ethnicity has improved since Ellis (2009) and (b) to evaluate whether these demographic variables were consistent with population-level estimates of stroke survivor demographics in the United States.
Method:
A scoping review examined U.S.-based aphasia treatment studies published between 2009 and 2019 and characterized the percentage of studies reporting age, sex, and race/ethnicity. Summary statistics for these variables were calculated and compared statistically with a population-based study of stroke survivors.
Results:
It was found out that 97.1% of studies reported age, 93.5% reported sex, and 28.1% reported race and/or ethnicity. Within reporting studies, participant mean age was 58.04 years, 61.6% of participants were men, and 38.4% were women; 86.5% of participants were White, 11.0% were Black, 2.0% were Hispanic/Latino, and 0.5% fell in other racial categories. All three variables were statistically different from the study of Kissela et al. (2012).
Discussion:
Despite being highlighted as an issue by Ellis (2009), less than 30% of recent aphasia treatment studies reported race or ethnicity, and participants do not appear to be demographically representative compared with estimates of stroke survivors living in the United States. These issues may negatively impact the ecological validity of aphasia treatment research. Aphasia researchers should more consistently report participant race and ethnicity and follow current guidelines for increasing the demographic representation of women and minorities.
Aphasia is a language disorder caused by acquired brain injury, which negatively affects communication skills, life participation, and overall quality of life (Simmons-Mackie, 2018). Aphasia rehabilitation research aims to develop effective treatments that improve language, communication, and/or life participation of people living with aphasia. For aphasia rehabilitation research to achieve this goal, research participants should represent people living with aphasia. However, recruitment can be difficult in aphasia rehabilitation research due to issues such as communication and concomitant mobility limitations, low public awareness of aphasia, and limited access to patient populations. As a result, most aphasia research relies on convenience sampling, in which participants are enrolled based on their availability to researchers (Etikan et al., 2016). While this approach eases the burden of more systematic recruitment strategies, studies that rely on convenience sampling may not accurately reflect the demographics of people living with aphasia in the United States. For example, if a study primarily recruits participants from active members of a local, well-established aphasia community in an affluent area, their participants are unlikely to be representative of the local, regional, and/or national population of stroke survivors with aphasia.
This potential discrepancy between a study cohort and the general population of people with aphasia creates the potential for sampling bias, where research participants are not representative of the research population of interest (Pannucci & Wilkins, 2010). Lack of representation can occur across many dimensions, such as age, race/ethnicity, biological sex or gender, and languages spoken. It is crucial to ensure that research participants are representative of the general population along these dimensions because such representation ensures that research is more sensitive to the cultural and linguistic diversity of all people with aphasia. For example, racial minorities are marginalized across many domains, including health care and their experiences of disability differ significantly from the experiences of White people who are disabled (e.g., Fuller-Thomson et al., 2009; Harrison, 2009; Kelley-Moore & Ferraro, 2004; Lin et al., 2014; Warner & Brown, 2011). Interventions tailored to these differences in the lived experiences of people with aphasia can improve outcomes and satisfaction with care (Joo & Liu, 2020; Torres-Ruiz et al., 2018). Alternatively, systematic sampling bias across the aphasia literature may not only alter the findings in aphasia research but also result in less effective treatments when implemented in real-world clinical settings (Smith & Noble, 2014) by negatively affecting external validity. In other words, aphasia rehabilitation research may be failing to address the diverse needs and characteristics of all individuals with aphasia.
Several previous studies have sought to characterize patient characteristics and demographic variables in aphasia and related research. Brookshire (1983) reviewed adult aphasia patient characteristics from selected area journals published between 1973 and 1983. Brookshire (1983) reported that out of the 18 patient characteristics reviewed, including a number of demographic variables, age was the only variable to be reported over 90% of the time, with the severity of aphasia reported in 64% of studies, aphasia type in 54%, gender in 48%, and education in 35%. Roberts et al. (2003) characterized patient reporting characteristics for 43 variables in 100 aphasia studies published between 2001 and 2002 and described that only seven of the 43 initial variables were reported over 65% of the time, with age reported 92% of the time, gender 91%, lesion location at 83%, time-post onset at 83%, severity at 82%, etiology of aphasia at 80%, and type of aphasia at 78%. As noted in Ellis (2009), neither Brookshire (1983) nor Roberts et al. (2003) reported race/ethnicity as variables of interest. In response, Ellis (2009) investigated the reporting of race and ethnicity in adult neurogenic communication disorders research between 1997 and 2007 in the American Journal of Speech-Language Pathology (AJSLP) and the Journal of Speech, Language, and Hearing Research (JSLHR). Ellis (2009) reported that 14.7% of articles in AJSLP reported race/ethnicity (n = 34) and 13.4% of articles in JSLHR reported race/ethnicity (n = 82).
This work is a brief, secondary analysis of a recently published scoping review (Cavanaugh et al., 2021). We sought to examine whether the reporting of age, sex, and race/ethnicity has improved over the past decade since Ellis (2009) using data from aphasia treatment studies completed in the United States and published between 2009 and 2019. We also sought to evaluate whether these three demographic variables were consistent with population-level estimates of stroke survivor demographics in the United States. This study will address the following questions.
What are the reporting rates for age, gender, and race in the aphasia treatment literature from 2009 to 2019?
What are the reported participants' demographics in the aphasia treatment literature from 2009 to 2019?
In this sample of the aphasia treatment literature, were participants demographically representative of the population of stroke survivors in the United States?
Method
This study was a secondary analysis of an existing scoping review (Cavanaugh et al., 2021), and methods from the original study have been summarized below. While Cavanaugh et al. (2021) focused on characterizing dosage in the aphasia treatment literature published between 2009 and 2019, this study focused on demographics in a subset of articles where data were collected in the United States. This required additional extraction of demographic variables from these studies.
The scoping review in Cavanaugh et al. (2021) relied on the framework of Arksey and O'Malley (2005). Ovid Medline, Embase via Embase.com, EBSCO CINAHL, EBSCO ERIC, Ovid PsycINFO, the Cochrane Database of Systematic Reviews via Wiley, and Linguistics and Language Behavior Abstracts were searched via ProQuest (see Cavanaugh et al., 2021, for full details of the literature search). Research articles were collected using the following criteria: (a) studies that included patients who received community-based aphasia treatment services and (b) studies that focused on enhancing some aspect of communication for patients with aphasia.
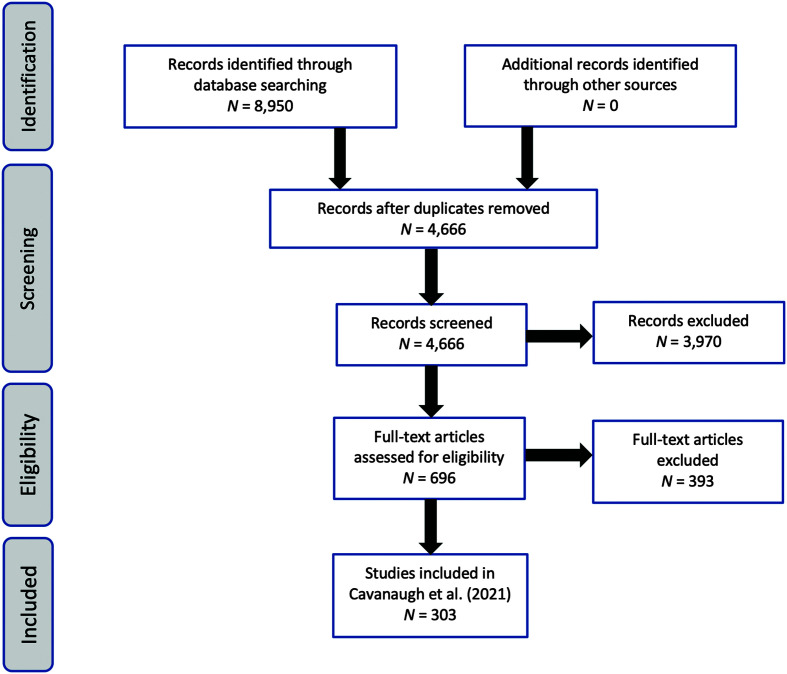
Briefly summarized, the review process for collected articles occurred across three levels. In Level 1, titles and abstracts were screened by a single author based on two criteria: (a) evaluated any behavioral intervention and (b) reported that the intervention was provided to individuals with acquired aphasia. In Level 2, each abstract was independently screened by two reviewers to determine if (a) the study examined the effects of a behavioral intervention(s) on a communication outcome; (b) the study intervention was not specifically targeted to people with aphasia admitted to a facility (i.e., rehabilitation hospitals or skilled-nursing facilities); and (c) treatment was not augmented by medication, brain stimulation, or non–speech-language interventions (e.g., acupuncture). In Level 3, the remaining articles were reviewed in full by two reviewers to ensure that they met all inclusion and exclusion criteria for the study. Disagreement was resolved through consensus with a third reviewer. See Figure 1 for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram describing identification, screening, eligibility, and inclusion. Adapted from Cavanaugh et al., 2021.
For data extraction, some studies reported individual data, whereas others reported aggregate demographic data across their participants or experimental groups (e.g., an immediate and a deferred treatment group). We extracted data at the level of detail in which it was reported.
Per Cavanaugh et al. (2021), we measured data extraction reliability by randomly selecting 10% of studies to be reviewed by a second independent coder. We measured reliability of data extraction as percent agreement between the two coders at the study, to account for the fact that some studies only reported data in aggregate. Therefore, the coders were considered in agreement if the values for a given extracted demographic variable were all the same for a given study.
To answer Question 1, the reporting rates were calculated as the percentage of studies reporting each demographic variable. For Question 2, the mean and median were calculated for age, and proportion for sex and race of the demographic values reported in each study. Descriptive statistics for age were weighted by the study sample size to account for studies that reported demographics in the aggregate. To answer Question 3 regarding demographic representation in recent aphasia treatment literature, we compared extracted demographic data with estimates of stroke prevalence in the Greater Cincinnati/Northern Kentucky Stroke Study, as reported by Kissela et al. (2012). This was a retrospective, population-based epidemiology study that examined stroke incidence trends, focused on racial disparities. The study population was “similar to the United States concerning median age, percent of Black participants, median household income, and education level; however, it did not contain a substantial proportion of persons of Hispanic ethnicity” (Kleindorfer et al., 2010 p. 1326).
Demographics from the scoping review sample were compared statistically with point estimates reported by Kissela et al. (2012). Age analyses employed a weighted least squares regression, equivalent to a standard t test with the additional capability of weighting observations by sample size from studies that only reported age in the aggregate. A one-sample proportion z test was used for sex and race comparisons. For race, the comparison was only conducted for Black and White racial categories, as these were the data available from Kissela et al. (2012). All three comparisons met standard modeling assumptions. Descriptive statistics and analyses were conducted using the statistical software R (R Core Team, 2020) Version 4.0.3.
Results
A total of 8,959 articles were identified through the literature search. Of these, 303 met the final criteria for inclusion in Cavanaugh et al. (2021). For this work, 139 of these articles collected participant data in the United States, which form the basis for the current report. In terms of reliability for Question 1 (reporting rates), percent agreement of data extraction was 100% for age and sex and 96.7% for race/ethnicity (i.e., 30/31 studies coded the same for this variable). For Question 2 (demographic variables), percent agreement of data extraction was 100% for race/ethnicity (i.e., 30/30 of the studies where coders both provided race/ethnicity date), 93.5% for sex, and 93.5% for age.
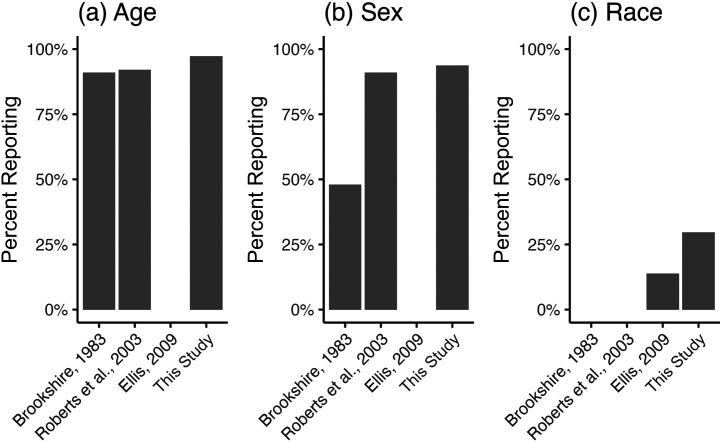
Regarding Question 1, it was found that 97.1% of the reviewed studies reported participant age, 93.5% reported participant sex, and 28.1% reported participant race/ethnicity. Figure 2 provides these reporting rates compared with previous reporting estimates discussed in the introduction (Brookshire, 1983; Ellis, 2009; Roberts et al., 2003).
Figure 2.
Percentage of studies included in Brookshire (1983), Roberts et al. (2003), and Ellis (2009) and this study, which reported participant age, sex, and race/ethnicity demographics. Brookshire (1983) and Roberts et al. (2003) did not seek to characterize race/ethnicity demographics.
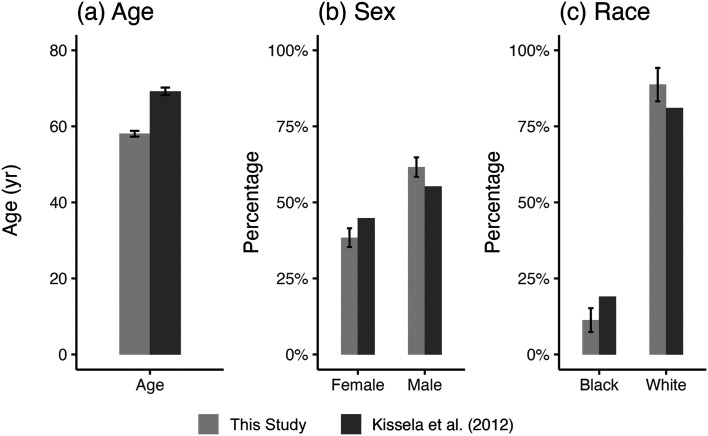
Regarding Question 2, of the studies that reported age, the mean age was 58.04 years. Of the studies that reported sex, 61.6% of participants were men and 38.4% were women. Of the studies that reported race/ethnicity, 86.5% of participants were White, 11.0% were Black, 2.0% were Hispanic/Latino, and 0.5% were Asian or other racial categories.
Regarding our Question 3, Figure 3 compares these rates with existing stroke demographic data from Kissela et al. (2012). All three comparisons were statistically significant, as follows. Age: β = −11.15, t = −28.65 (778), p < .001. Sex: x 2 = (1, 955) = 108.57, p < .001. Race: x 2 = (1, 195) = 7.05, p = .008.
Figure 3.
Mean age, sex, and race as reported from Kissela et al. (2012) and this study. Error bars indicate 95% confidence intervals. No variance was reported by Kissela et al. for sex or race.
Discussion
Given the importance of establishing demographic representation in clinical research, the goals of this scoping review were to characterize the reporting rates (Question 1) and participant demographics (Question 2) of age, sex, and race/ethnicity in recent U.S.-based aphasia treatment research and compare reported demographics from these research studies to estimated demographics of current U.S. stroke survivors (Question 3).
Demographics in Recent U.S.-Based Aphasia Treatment Research
Reporting rates for age and sex in U.S.-based aphasia treatment research published between 2009 and 2019 were high (> 97%), consistent with previous reviews of the literature (Brookshire, 1983; Roberts et al., 2003). However, reporting rates for race/ethnicity in our data remain low (< 30%). This is despite the fact that researchers are required to collect and report data on these factors and to describe plans to ensure that women and minorities are appropriately represented in federally funded research (Rockey, 2013) and that Ellis (2009) highlighted this as an unaddressed issue in the field over 10 years ago.
The reasons for these continued low reporting rates for race and ethnicity are unclear. One possibility is that researchers may be seeking to avoid undue focus on race due to personal discomfort or misplaced concerns of potential bias (Apfelbaum et al., 2008). Another is that researchers may be choosing to report as little demographic information as possible to maintain participant confidentiality, as even a small set of factors reported together (e.g., age, sex, race, stroke status, and general geographic region) may make some participants identifiable (Sweeney, 2000). Maximizing participant privacy is an important ethical consideration, but the costs and benefits should be carefully weighed. The lack of demographic reporting, especially for race and ethnicity, makes it difficult to accurately characterize representation in our literature. Without this characterization it is more difficult to improve representation in our field (see study limitations below).
Comparisons With Estimated Demographics of Current U.S. Stroke Survivors
Compared with stroke survivor estimates from Kissela et al. (2012), participants from recent aphasia treatment research were significantly younger and more men. Regarding race, participants from recent aphasia treatment research were significantly more White and less Black, with Black research participants enrolled at approximately half the proportion as would be expected based on Kissela et al. This underrepresentation likely has negative consequences in terms of ecological validity, given well-documented racial disparities and the fact that stroke prevalence is disproportionately high for Black Americans (Howard et al., 2011).
While our data and those from Kissela et al. (2012) precluded statistical comparison for other race/ethnic categories, these groups do appear to be underrepresented compared with general U.S. census data. For example, recent census data (United States Census Bureau, 2019a) estimate that together, Asian, American Indian/Alaskan Native, and Native Hawaiian/Pacific Islander make up 7.4% of the U.S. population, compared with only 1.0% of participants reported in the “Asian or other races” category from our scoping review. Similarly, the census data put Hispanic/Latinos at 18.5% of the U.S. population, compared with only 2.0% of research participants reported in this category from our scoping review. In the event that stroke survivor demographics are similar to this recent census data, these preliminary findings suggest that underrepresentation in aphasia treatment research may be of considerable concern for these groups (Ellis & Jacobs, 2021).
These data suggest that these demographic groups (women, older individuals, and minorities) are underrepresented in aphasia treatment research. This disparity has the potential to negatively affect the translation and implementation of aphasia treatments to diverse clinical practice settings because the evidence based may not address the diverse needs and characteristics of all individuals with aphasia. To address these issues, researchers should consistently report participant demographics, especially regarding race/ethnicity, following the National Institutes of Health (NIH) minimal standard guidelines for reporting race (Rockey, 2013). Researchers should also seek to improve the representation of participants in clinical studies (Flanagin et al., 2021). Potential methods for improving representation in research include (a) fostering relationships with the community (e.g., building trust with community groups, accommodating transportation for potential participants, providing flexible hours, highlighting the need for representation in research, showing appreciation for participation, and emphasizing available support to answer questions; Clark et al., 2019), (b) increasing education in cultural issues for research staff (e.g., training and regular check-ins regarding cultural competence available at https://www.asha.org/practice/multicultural/self/), (c) guaranteeing safety for members of minority communities with different immigration status (e.g., assuring potential participants that immigration status will not be collected as part of the study), (d) creating culturally sensitive campaigns for recruitment (Gardener et al., 2020), (e) supporting training of and research from researchers and clinicians from culturally and linguistically diverse backgrounds, and (f) allocating research funding which specifically targets communication disorders in underrepresented individuals.
Future Directions
While this study focuses on age-, sex-, and race-related disparities, additional dimensions of representation warrant close examination. One of these dimensions is cultural and linguistic diversity. Worldwide, about 85% of international aphasia treatment research has focused on English-speaking individuals (Beveridge & Bak, 2011). In the United States, the U.S. census reports that 21.6% of the population speaks a language other than English at home (United States Census Bureau, 2019b). These percentages highlight a pressing need to adapt and develop aphasia treatments for a linguistic and culturally diverse global population. Furthermore, such adaptations need to account for multilingualism: In our sample, only 14 of 139 studies reported having at least one participant who spoke more than one language. Of these 14 studies, eight reported treating participants only in English. Future research should therefore aim to (a) report information about languages spoken by stroke survivors with aphasia, (b) increase the number of studies addressing multiple languages spoken by stroke survivors with aphasia (i.e., bilingual aphasia), and (c) adapt and implement research in culturally and linguistically diverse populations with aphasia.
Study Limitations
There are a number of limitations in this study. In our sample of U.S.-based studies, only 28.1% of studies reported race/ethnicity, which increases the possibility of biased estimates of race/ethnicity representation. For example, researchers who prioritize demographic representation in their study recruitment and enrollment efforts may also be more likely to report these demographics. Additionally, Kissela et al. (2012) provide demographic estimates for stroke survivors in general and without reporting aphasia status. While the cohort in Kissela et al. (2012) was carefully chosen to be representative of the United States at the time of the study, it is not a national sample concurrent with the time period of aphasia studies. We considered using the prevailing national data source on stroke incidence reported by the Centers for Disease Control and Prevention (2007; Mozaffarian et al., 2016) but ultimately elected not to use this data, as it (a) stemmed from a national phone survey that has published concerns related to nonresponse bias (Crouch et al., 2018; Gettens et al., 2015; Schneider et al., 2012) and (b) does not permit proxy reporting, which is therefore likely to exclude stroke survivors with communication disorders such as aphasia. To our knowledge, there are no comprehensive demographic estimates of stroke survivors living in the United States, which also report the presence or absence of aphasia, which is an important topic for future aphasia research in its own right.
Acknowledgments
This research was supported by the University of Pittsburgh School of Health and Rehabilitation Sciences 2020 McMurtry Family Undergraduate Research Award, the University of Pittsburgh School of Health and Rehabilitation Sciences Development Fund, and the National Center for Advancing Translational Sciences of the NIH under Award TL1TR001858. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding Statement
This research was supported by the University of Pittsburgh School of Health and Rehabilitation Sciences 2020 McMurtry Family Undergraduate Research Award, the University of Pittsburgh School of Health and Rehabilitation Sciences Development Fund, and the National Center for Advancing Translational Sciences of the NIH under Award TL1TR001858. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- Apfelbaum, E. P. , Sommers, S. R. , & Norton, M. I. (2008). Seeing race and seeming racist? Evaluating strategic colorblindness in social interaction. Journal of Personality and Social Psychology, 95(4), 918–932. https://doi.org/10.1037/a0011990 [DOI] [PubMed] [Google Scholar]
- Arksey, H. , & O'Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616 [Google Scholar]
- Beveridge, M. E. L. , & Bak, T. H. (2011). The languages of aphasia research: Bias and diversity. Aphasiology, 25(12), 1451–1468. https://doi.org/10.1080/02687038.2011.624165 [Google Scholar]
- Brookshire, R. H. (1983). Subject description and generality of results in experiments with aphasic adults. Journal of Speech and Hearing Disorders, 48(4), 342–346. https://doi.org/10.1044/jshd.4804.342 [DOI] [PubMed] [Google Scholar]
- Cavanaugh, R. , Kravetz, C. , Jarold, L. , Quique, Y. , Turner, R. , & Evans, W. S. (2021). Is there a research–practice dosage gap in aphasia rehabilitation. American Journal of Speech-Language Pathology, 30(5), 2115–2129. https://doi.org/10.1044/2021_AJSLP-20-00257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2007). Prevalence of stroke–United States, 2005. MMWR, 56(19), 469–474. [PubMed] [Google Scholar]
- Clark, L. T. , Watkins, L. , Piña, I. L. , Elmer, M. , Akinboboye, O. , Gorham, M. , Jamerson, B. , McCullough, C. , Pierre, C. , Polis, A. B. , Puckrein, G. , & Regnante, J. M. (2019). Increasing diversity in clinical trials: Overcoming critical barriers. Current Problems in Cardiology, 44(5), 148–172. https://doi.org/10.1016/j.cpcardiol.2018.11.002 [DOI] [PubMed] [Google Scholar]
- Crouch, E. , Radcliff, E. , Strompolis, M. , & Hartley, S. N. (2018). Behavioral risk factor surveillance system state survey on exposure to adverse childhood experiences (ACEs): Who declines to respond. Children and Youth Services Review, 91, 259–262. https://doi.org/10.1016/j.childyouth.2018.06.024 [Google Scholar]
- Ellis, C. (2009). Does race/ethnicity really matter in adult neurogenics. American Journal of Speech-Language Pathology, 18(4), 310–314. https://doi.org/10.1044/1058-0360(2009/08-0039) [DOI] [PubMed] [Google Scholar]
- Ellis, C. , & Jacobs, M. (2021). The complexity of health disparities: More than just Black–White differences. Perspectives of the ASHA Special Interest Groups, 6(1), 112–121. https://doi.org/10.1044/2020_PERSP-20-00199 [Google Scholar]
- Etikan, I. , Musa, S. A. , & Alkassim, R. S. (2016). Comparison of convenience sampling and purposive sampling. American Journal of Theoretical and Applied Statistics, 5(1), 1–4. https://doi.org/10.11648/j.ajtas.20160501.11 [Google Scholar]
- Flanagin, A. , Frey, T. , Christiansen, S. L. , & Bauchner, H. (2021). The reporting of race and ethnicity in medical and science journals: Comments invited. JAMA, 325(11), 1049–1052. https://doi.org/10.1001/jama.2021.2104 [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson, E. , Nuru-Jeter, A. , Minkler, M. , & Guralnik, J. M. (2009). Black—White disparities in disability among older Americans: Further untangling the role of race and socioeconomic status. Journal of Aging and Health, 21(5), 677–698. https://doi.org/10.1177/0898264309338296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardener, H. , Sacco, R. L. , Rundek, T. , Battistella, V. , Cheung, Y. K. , & Elkind, M. S. (2020). Race and ethnic disparities in stroke incidence in the Northern Manhattan study. Stroke, 51(4), 1064–1069. https://doi.org/10.1161/STROKEAHA.119.028806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gettens, J. , Lei, P.-P. , & Henry, A. D. (2015). Using American Community Survey disability data to improve the behavioral risk factor surveillance system accuracy (DRC Brief 2015-05). Disability Research Consortium. [Google Scholar]
- Harrison, T. (2009). Health disparities among Latinas aging with disabilities. Family & Community Health, 32(1), S36–S45. https://doi.org/10.1097/01.FCH.0000342838.05607.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard, V. J. , Kleindorfer, D. O. , Judd, S. E. , McClure, L. A. , Safford, M. M. , Rhodes, J. D. , Cushman, M. , Moy, C. S. , Soliman, E. Z. , Kissela, B. M. , & Howard, G. (2011). Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of Neurology, 69(4), 619–627. https://doi.org/10.1002/ana.22385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joo, J. Y. , & Liu, M. F. (2020). Effectiveness of culturally tailored interventions for chronic illnesses among ethnic minorities. Western Journal of Nursing Research, 43(1), 73–84. https://doi.org/10.1177/0193945920918334 [DOI] [PubMed] [Google Scholar]
- Kelley-Moore, J. A. , & Ferraro, K. F. (2004). The black/white disability gap: Persistent inequality in later life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 59(1), S34–S43. https://doi.org/10.1093/geronb/59.1.S34 [DOI] [PubMed] [Google Scholar]
- Kissela, B. M. , Khoury, J. C. , Alwell, K. , Moomaw, C. J. , Woo, D. , Adeoye, O. , Flaherty, M. L. , Khatri, P. , Ferioli, S. , De Los Rosa, F. , Broderick, J. P. , & Kleindorfer, D. O. (2012). Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology, 79(17), 1781–1787. https://doi.org/10.1212/WNL.0b013e318270401d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleindorfer, D. O. , Khoury, J. , Moomaw, C. J. , Alwell, K. , Woo, D. , Flaherty, M. L. , Khatri, P. , Adeoye, O. , Ferioli, S. , Broderick, J. P. , & Kissela, B. M. (2010). Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater Cincinnati/Northern Kentucky stroke study. Stroke, 41(7), 1326–1331. https://doi.org/10.1161/STROKEAHA.109.575043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, S.-F. , Beck, A. N. , & Finch, B. K. (2014). Black–White disparity in disability among U.S. older adults: Age, period, and cohort trends. The Journals of Gerontology. Series B: Psychological Sciences and Social Sciences, 69(5), 784–797. https://doi.org/10.1093/geronb/gbu010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian, D. , Benjamin, E. J. , Go, A. S. , Arnett, D. K. , Blaha, M. J. , Cushman, M. , Das, S. R. , De Ferranti, S. , Després, J.-P. , Fullerton, H. J. , Howard, V. J. , Huffman, M. D. , Isasi, C. R. , Jiménez, M. C. , Judd, S. E. , Kissela, B. M. , Lichtman, J. H. , Lisabeth, L. D. , Liu, S. , … Stroke Statistics Subcommittee. (2016). Executive summary: Heart disease and stroke statistics—2016 update: A report from the American Heart Association. Circulation, 133(4), 447–454. https://doi.org/10.1161/CIR.0000000000000366 [DOI] [PubMed] [Google Scholar]
- Pannucci, C. J. , & Wilkins, E. G. (2010). Identifying and avoiding bias in research. Plastic and Reconstructive Surgery, 126(2), 619–625. https://doi.org/10.1097/PRS.0b013e3181de24bc [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2020). R: A language and environment for statistical computing (4.0.3). R Foundation for Statistical Computing. https://www.r-project.org/ [Google Scholar]
- Roberts, P. , Code, C. , & McNeil, M. (2003). Describing participants in aphasia research: Part 1. Audit of current practice. Aphasiology, 17(10), 911–932. https://doi.org/10.1080/02687030344000328 [Google Scholar]
- Rockey, S. (2013). Reporting to NIH on race and ethnicity of clinical research participants. National Institutes of Health Office of Extramural Research. https://nexus.od.nih.gov/all/2013/08/21/reporting-to-nih-on-race-and-ethnicity-of-clinical-research-participants/ [Google Scholar]
- Schneider, K. L. , Clark, M. A. , Rakowski, W. , & Lapane, K. L. (2012). Evaluating the impact of non-response bias in the Behavioral Risk Factor Surveillance System (BRFSS). Journal of Epidemiology and Community Health, 66(4), 290–295. https://doi.org/10.1136/jech.2009.103861 [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie, N. (2018). Aphasia in North America. Aphasia Access. [Google Scholar]
- Smith, J. , & Noble, H. (2014). Bias in research: Table 1. Evidence-Based Nursing, 17(4), 100–101. https://doi.org/10.1136/eb-2014-101946 [DOI] [PubMed] [Google Scholar]
- Sweeney, L. (2000). Simple demographics often identify people uniquely. Health (San Francisco), 671(2000), 1–34. [Google Scholar]
- Torres-Ruiz, M. , Robinson-Ector, K. , Attinson, D. , Trotter, J. , Anise, A. , & Clauser, S. (2018). A portfolio analysis of culturally tailored trials to address health and healthcare disparities. International Journal of Environmental Research and Public Health, 15(9), 1859. https://doi.org/10.3390/ijerph15091859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2019a). QuickFacts: United States. Census.Gov. https://www.census.gov/quickfacts/fact/table/US/PST045219
- United States Census Bureau. (2019b). Selected Social Characteristics in the United States. Language spoken at home. Census.Gov. https://data.census.gov/cedsci/table?tid=ACSDP5Y2019.DP02&hidePreview=true
- Warner, D. F. , & Brown, T. H. (2011). Understanding how race/ethnicity and gender define age-trajectories of disability: An intersectionality approach. Social Science & Medicine, 72(8), 1236–1248. https://doi.org/10.1016/j.socscimed.2011.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]