Abstract
Medical waste has increased in the past 3 years as a result of the coronavirus disease 2019 (COVID-19) pandemic. This condition is expected to exacerbate due to the growing healthcare markets and aging population, posing health threats to the public via environmental footprints. To alleviate these impacts, there is an urgent need for medical waste management. This article highlights the drawbacks of current disposal methods and the potential of medical waste reuse and recycling, emphasizing the processes, materials, and chemistry involved in each practice. Further discussion is provided on the chemical and mechanical recycling of plastics as the dominating material in biomedical applications, and possible strategies and challenges in recycling and reusing biomedical materials are explored in this review.
Keywords: Recycling, Reuse, Waste management, Medical waste, Biomaterials, Circular economy
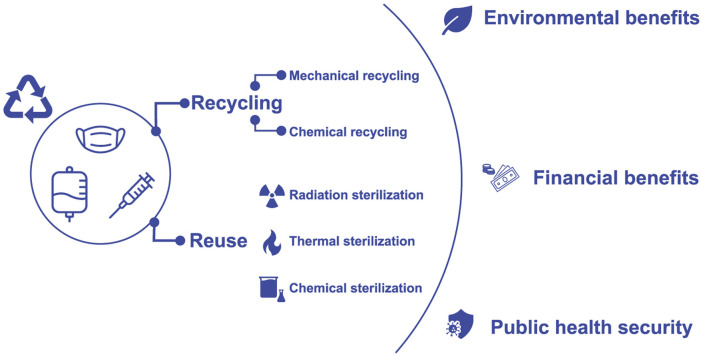
Graphical abstract
For complete overview of the section, please refer the article collection - Recycling and Reuse within a Circular Economy (2023)
Introduction
Healthcare waste is defined as the waste generated via medical procedures at healthcare or research facilities and laboratories [1,2]. Medical waste is divided into two categories: (i) hazardous waste, involving biological, chemical, radioactive, and/or physical footprints, and (ii) non-hazardous waste, constituting about 85% of waste generated from healthcare activities that are similar to domestic waste [3]. Improper medical waste handling and disposal may impose health risks on healthcare workers and the public [4]. This mainly occurs through the transmission of infectious or drug-resistant microorganisms, toxic exposure to chemical and pharmaceutical waste, and the release of air pollutants [3,4]. Soaring medical waste production as a result of the COVID-19 pandemic [5,6] is expected to be perpetuated by the projected growth of emerging healthcare sectors and the aging population, posing environmental hazards and causing illnesses in a significant number of people [7].
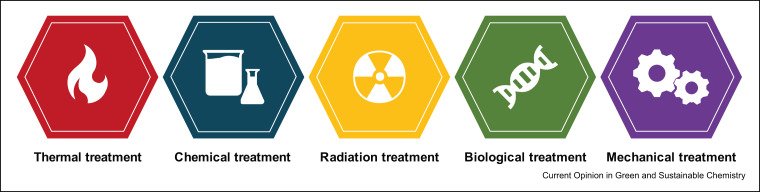
Figure 1 shows the current medical waste treatment methods, including thermal, chemical, radiation, biological, and mechanical treatments, where the thermal treatment is the most common technology worldwide [1]. The two most common thermal treatment methods to dispose of hazardous waste are incineration and autoclaving [4,8]. Undesirable emissions, such as dioxins, furans, and heavy metals, occur during incineration [9,10]. Also, some organic solvents used in the pharmaceutical industry, such as 2,2,2-trifluoroethanol, cause corrosion in incinerators [11]. With autoclaves, aside from the difficulties of handling mixed clinical waste or large and bulky materials [1,4,8], additional treatments may be required because of the untreated appearance of autoclaved waste, involving financial costs and adverse environmental impacts [4].
Figure 1.
Current medical waste treatment strategies [1].
Overall, the environmental impacts and health risks associated with medical waste, as well as the shortcomings of current disposal approaches have increased the demand for recycling and reuse strategies as part of waste management. In addition, other factors such as reducing the reliance on natural resources, improving the accessibility of medical products, and increasing the financial gain for the health sectors motivate the utilization of these approaches [12]. In this article, we will review the recent advances in recycling and reusing biomedical materials, discuss challenges associated with each practice, and outline prospects for future research.
Reprocessing and reusing biomedical materials
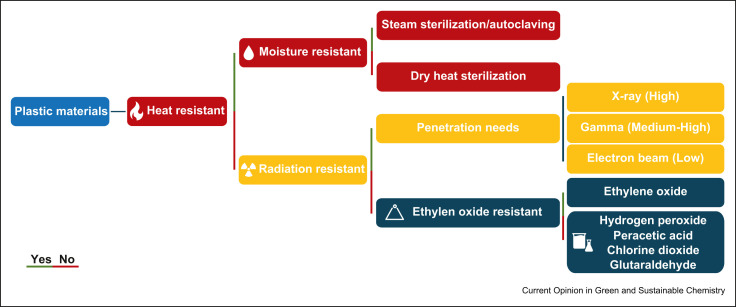
Reprocessing and reusing medical materials and devices are common waste management approaches to increase economic and environmental benefits [7,13]. There are protocols and guidelines specifically designed for reprocessing and sterilizing multiuse medical devices, whereby health risks merely ensue in case these protocols are not rigorously followed [14]. Likewise, with strict considerations, the reprocessing of single-use medical devices (SUMDs) has been established and supported in various countries, including Germany and the USA [15]. The ability of a target biomedical material to withstand cleaning, disinfection, and sterilization without undergoing any property change plays a significant role in selecting appropriate methods for reprocessing and reusing. Figure 2 demonstrates suitable sterilization approaches based on plastic material properties. The growing use of disposable devices has led to a shift from other biomedical materials, such as glass, metals, and ceramics, to plastics [16].
Figure 2.
Decision tree for plastic material sterilization method selection—Reproduced from the study by Sastri et al. [16], Copyright 2022, with permission from Elsevier.
Sterilization can be divided into three categories: (i) thermal, (ii) radiation, and (iii) chemical sterilization [17]. Steam sterilization (autoclaving, limited to moisture-resistant materials) and dry heat sterilization are among the thermal treatments that are used for heat-resistant materials [16]. Autoclaving can cause corrosion in surgical alloys or rust in instruments [17]. Moreover, it has been reported that the repeated autoclaving of polyvinyl chloride (PVC), used in blood bags, causes plasticizer loss, molecular weight reduction, and increase in tensile modulus and yield strength [18].
In low-temperature sterilization methods, medical devices are radiated at varying wavelengths and penetration power. Electron beam, gamma, and X-ray radiations are used for low, medium to high, and high penetration needs, respectively [16]. Typically, plastics used in medical devices are susceptible to structural changes, including degradation, discoloration, and crosslinking during radiation sterilization [16,18]. This includes the gamma irradiation of PVC/polystyrene blends [19], polypropylene (PP) [20], polymethyl methacrylate [21], and polyethylene terephthalate fibers [22], as well as the electron beam sterilization of polylactic acid [23].
For radiation- and heat-sensitive materials, chemical agents, such as chlorine compounds, aldehydes (formaldehyde and glutaraldehyde), hydrogen peroxide, peracetic acid, and ethylene oxide (EO), are used as chemical treatments for disinfection and sterilization [16]. In this type of treatment, disinfection is typically conducted instead of sterilization [1]. It should be noted that different chemical treatments may affect the tensile strength of materials used in SUMDs, such as polyurethane (PU), latex, nylon, or polyethylene (PE) [24]. It has been shown that using EO as a low-temperature sterilization method renders PU catheters toxic, which requires a long aeration time to remove toxic residues [25]. Sterilization of PU electrophysiology catheters via the concurrent use of plasma and oxidative sterilants, such as vaporized hydrogen peroxide or peracetic acid, resulted in additive (antioxidant Irganox 1076) degradation or difference in coloration [25]. Moreover, antimicrobial nanostructured zinc-based coating in personal protective equipment (PPE) may improve disinfection, enabling the extended reuse of PPE via self-sterilization [26].
Overall, these studies show that reprocessing and reusing biomedical materials should be material specific. Moreover, after each sterilization or disinfection cycle, validation tests are needed to ensure that medical devices maintain functionality, and the risk of disease transmission by microorganisms is eliminated.
Recycling and recovery of biomedical materials
Recycling is conducted by converting a product to its materials and turning them into a new product, wherein the process suitability depends on the product components [7]. Most medical instruments are made from plastics, as they are cost-effective, durable, and flexible compared with steel, ceramics, and glass [27∗]. It is therefore essential to recycle plastic-based materials, while a variety of non-plastic wastes have also been reported to be recyclable, such as stainless steel used in surgical instruments [28∗], medical implants and dental prosthetics collected from the cremation industry [29], mercury from dental amalgams [30], and aluminum from waste pharmaceutical blister [31, 32, 33, 34]. At least 12 United Nations Sustainable Development Goals are impacted directly or indirectly by plastic and microplastic pollution [35], which attests to the urgency of recycling plastic-based materials.
Several programs have been developed worldwide for plastic-based medical waste recycling. A recycling pilot was developed in the UK to downcycle PVC-based materials such as anesthesia masks, oxygen masks, and tubing into horticultural items [36]. Another PVC recycling program in hospitals is conducted by the Vinyl Council of Australia to remanufacture valuable items, including industrial hoses, from recycled PVC medical waste, such as oxygen masks and tubing, intravenous fluid bags, and suction tubing [37].
In general, plastic waste is recycled using primary, secondary, tertiary, or quaternary pathways. Primary recycling (also known as re-extrusion and closed-loop recycling) is limited to almost pristine waste and is generally exploited in the processing line, because the recycled products must have a similar quality to the original plastic [38,39]. Consequently, applying primary recycling to medical wastes may not be feasible. In secondary (mechanical) recycling, mechanical processes are used to recover plastic wastes. These processes, involving the sorting, washing, and extrusion of plastic waste, generally lead to the degradation of polymers [38]. Tertiary (chemical) recycling refers to the use of chemical processes to recover the petrochemical components of plastic wastes [38]. During quaternary recycling (or energy recovery), energy is recovered by waste incineration, and harmful emissions are inevitably produced [38], which is unsuitable for recycling medical waste. Effective energy recovery is not attainable in healthcare waste incinerators due to their small sizes [1]; however, by reusing incineration products, the environmental impacts of incineration may be reduced. For instance, replacing fine aggregates in concrete with incinerated biomedical waste ash results in improved strength and reduced permeability, while eliminating the necessity of landfilling the ash [40]. Considering the limitations of primary and quaternary recycling, mechanical and chemical treatments may be primarily considered for the recycling and recovery of biomedical materials.
Mechanical recycling of plastic-based biomedical materials
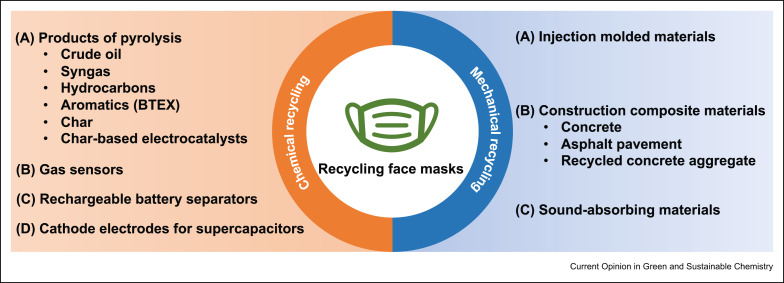
Mechanical recycling of medical waste has been the focus of several studies. Blue wrapping papers, made from PP used to wrap surgical instruments, are injection-molded into new medical devices without using additives. The mechanical properties of materials recycled through the injection molding of molten wrapping paper waste did not significantly change at varying melting temperatures, and the products withstood up to 10 disinfection cycles with preserved properties [12]. With the extensive consumption of PPE, such as surgical face masks during the COVID-19 pandemic, there has been an increasing interest in PPE recycling [41∗] via mechanical and chemical recycling pathways to yield products for various applications (Figure 3 ). This includes developing sound-absorbing porous materials from PP-based face masks with comparable performance to commercial counterparts [42∗], as well as the immense potential of using recycled face masks in construction applications [43,44]. Adding shredded face masks (SFM) to concrete resulted in negligible changes in compressive (about 5% increase) and tensile (about 3% decrease) strengths, with preserved material stability under spalling and frost resistance tests [43]. Incorporating 1.5% of SFM into hot mix asphalt ameliorated the rutting resistance of asphalt pavement, resulting in 69% decrease in the rutting depth [45]. In another study, using 1% of SFM in recycled concrete aggregate (RCA) increased the unconfined compressive strength (by 17%) and resilient modulus (by about 4%), as the PP fibers reinforced RCA particles, rendering the final blend suitable for pavements base and subbase applications [44].
Figure 3.
Recycling face masks via chemical or mechanical methods to yield a variety of products.
Chemical recycling of plastic-based biomedical materials
Tertiary recycling enables the treatment of contaminated and heterogenous plastics with minimal pretreatment [39]. Pyrolysis is a promising thermochemical treatment of medical waste, as it provides environmental advantages [46], including lower pollution and carbon footprint compared with other thermal treatments, and there is no requirement for the earlier separation of different waste plastics prior to pyrolysis [47]. This process has been applied to different types of medical waste to produce value-added materials [47, 48, 49∗, 50, 51]. Waste syringes made from PP were recycled via pyrolysis in a semi batch reactor, where the pyrolysis oil contained alkanes, alkenes, and aromatic rings, and the physical properties of it were close to the diesel fuel and petrol blend [48]. Syngas and C1-2 hydrocarbons were yielded from the catalytic conversion of disposable masks made from PP, PE, and nylon-6 over nickel/sulfur dioxide (Ni/SO2) catalysts in a carbon dioxide (CO2) reaction medium. In this thermochemical process, the conversion of long-chain hydrocarbons to methane and hydrogen on the Ni/SO2 catalyst was significant, and the carbon monoxide (CO) formation was increased in the CO2 medium [49∗]. The catalytic fast pyrolysis of disposable masks has been used to produce high-value aromatics, including benzene, toluene, ethylbenzene, and xylene (BTEX) [50]. Without catalysts, branched hydrocarbons were yielded, whereas zeolite catalysts enabled the production of aromatic compounds, and higher BTEX selectivity was obtained in the catalysts containing larger pore sizes [50]. Also, activating and functionalizing char, as a product of face mask pyrolysis, with iron (Fe)-phthalocyanine and Ni-phthalocyanine has yielded electrocatalysts for oxygen reduction and hydrogen evolution reactions, respectively [51].
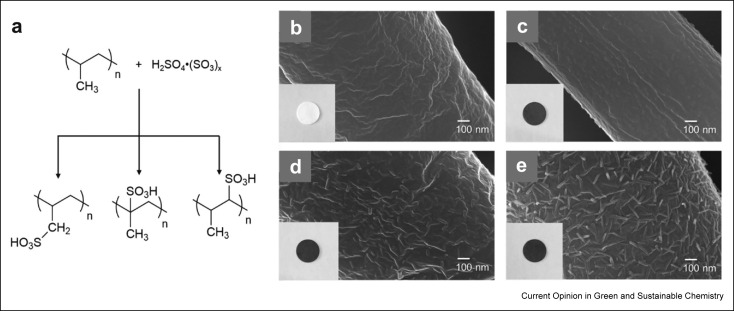
Other chemical processes may also enable tertiary biomedical material recycling. Recently, a process has been developed, whereby a simple chemical treatment on face masks resulted in a highly efficient separator for aqueous rechargeable batteries [52∗]. In this process (Figure 4 a), the middle filter layer of disposable masks made from PP-based nonwoven fabrics (Figure 4b) was treated with fuming sulfuric acid (FSA) for 2–6 min, changing the color to light brown and increasing the surface toughness (Figure 4c–e). During this reaction, the hydrophobic surface of middle filter was rendered hydrophilic with copious hydroxyl (-OH) and sulfonic acid (-SO3H) groups, and the final separator improved the electrochemical performance compared with conventional glass-fiber based separators [52∗]. In another study, a hydrothermal process was used to load zinc sulfide (ZnS) nanoparticles in a sensing substrate made from waste mask fibers, where the resulting composite was used as a gas sensor [53]. Compared with ZnS-loaded ceramic substrates, this gas sensor demonstrated 8.4–35.2 times higher sensitivity to different analytes, including formaldehyde, ammonia, hydrogen peroxide, and relative humidity (85%). This is attributed to the complete exposure of nanoparticles to target gases because mask fibers are highly permeable [53]. It has been shown that waste PP masks could be recycled into sulfur-doped porous carbon via sulfonation and carbonization methods, which is used as a cathode for supercapacitors [54].
Figure 4.
(a) Expected pathway for FSA-mediated PP chemical modification. Optical and scanning electron microscopy (SEM) images of (b) a mask filter, and sulfonated mask filters treated with FSA for (c) 2 min, (D) 4 min, and (e) 6 min—Reproduced from the study by Kim et al. [52∗], Copyright 2021, with permission from Elsevier.
Recycling PVC, as the primarily utilized plastic in terms of volume in medical devices [27,55], is challenging and imposes adverse environmental impacts, especially in the forms of air pollutants and chlorine, which contaminates recycling products and causes equipment corrosion [38]. These problems are addressed by introducing catalysts, hydrogen chloride inhibitors, or pretreatment processes to increase the efficiency of recycling procedures [38]. Promising techniques such as near-critical methanol (NCM) for PVC-medical waste treatment may be implemented, wherein efficient additive recovery and dechlorination efficiency of >90% have been obtained at 250 °C [56]. Aluminum has also been completely recovered from PVC plastic in waste pharmaceutical blisters via a hydrometallurgical method, wherein the waste is leached with hydrochloric acid [57].
Challenges and outlook in recycling and reusing medical waste
Medical waste recycling faces several challenges, including unstandardized sorting as well as health concerns regarding recycling infectious waste. Most hospital wastes are not infectious, rendering them suitable for recycling programs [58]. However, unstandardized medical waste sorting has led to the erroneous disposal of items as infectious waste [59], imposing unnecessary costs associated with infectious waste treatment [4]. This challenge might be addressed using machine learning algorithms, as they have been utilized to sort and classify wastes for different industrial applications, such as plastic waste, bottle, and municipal solid waste recycling, with >90% accuracy [60]. Training healthcare workers on waste management may improve their practices in biomedical waste handling and disposal [61,62]. Furthermore, social and ethical concerns stemming from the health risks of infectious medical waste recycling should be addressed by raising public awareness and implementing strict protocols for medical waste recycling [27∗]. In addition, economically feasible processes should be developed for plastic recycling, and the design of plastic-based materials should satisfy the feasibility of efficient recycling by following healthy design practices [27∗]. Using bio-based plastics in medical applications is another alternative that may lower environmental impacts [63] and, with further exploration, might lessen recycling costs associated with the petroleum-based counterparts [64].
Conclusions
Environmental and public health concerns regarding the rapid increase in medical waste generation and the drawbacks of current disposal methods may be addressed by practicing recycling and reuse programs. Compared with current disposal methods, reprocessing and reusing medical devices are environmentally and financially beneficial. Still, established protocols should be strictly followed to eliminate the risk of contamination. Also, preserving the functionality and original properties of materials needs to be considered in selecting reuse methods. Recycling and recovery are other approaches that may enable the efficient management of biomedical material waste. Nevertheless, challenges associated with sorting, designing, and sterilization are ahead of recycling programs. In summary, efforts should be devoted to allocating financial and technological resources, enabling sustainable waste management programs in healthcare sectors through recycling and reusing biomedical materials.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
Acknowledgments
Amir Sheikhi would like to acknowledge the startup fund provided by Penn State.
This review comes from a themed issue on Recycling and Reuse within a Circular Economy (2023)
Edited by Vijay Kumar Thakur and Stefan Ioan Voicu
Available online 06 September 2022
References
- 1.Chartier Y. World Health Organization; 2014. Safe management of wastes from health-care activities. [Google Scholar]
- 2.United States Environmental Protection Agency (EPA) Medical waste. https://www.epa.gov/rcra/medical-waste (n.d.)
- 3.World Health Organization (WHO) Health-care waste. https://www.who.int/news-room/fact-sheets/detail/health-care-waste/ (n.d.)
- 4.Windfeld E.S., Brooks M.S.-L. Medical waste management – a review. J Environ Manag. 2015;163:98–108. doi: 10.1016/j.jenvman.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Haque Md.S., Uddin S., Sayem S.Md., Mohib K.M. Coronavirus disease 2019 (COVID-19) induced waste scenario: a short overview. J Environ Chem Eng. 2021;9 doi: 10.1016/j.jece.2020.104660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patrício Silva A.L., Prata J.C., Walker T.R., Duarte A.C., Ouyang W., Barcelò D., Rocha-Santos T. Increased plastic pollution due to COVID-19 pandemic: challenges and recommendations. Chem Eng J. 2021;405 doi: 10.1016/j.cej.2020.126683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kane G.M., Bakker C.A., Balkenende A.R. Towards design strategies for circular medical products. Resour Conserv Recycl. 2018;135:38–47. doi: 10.1016/j.resconrec.2017.07.030. [DOI] [Google Scholar]
- 8.Khadem Ghasemi M., Mohd Yusuff R. Advantages and disadvantages of healthcare waste treatment and disposal alternatives: Malaysian scenario. Pol J Environ Stud. 2016;25:17–25. doi: 10.15244/pjoes/59322. [DOI] [Google Scholar]
- 9.Insa E., Zamorano M., López R. Critical review of medical waste legislation in Spain. Resour Conserv Recycl. 2010;54:1048–1059. doi: 10.1016/j.resconrec.2010.06.005. [DOI] [Google Scholar]
- 10.Verma R., Vinoda K.S., Papireddy M., Gowda A.N.S. Toxic pollutants from plastic waste- A review. Procedia Environ Sci. 2016;35:701–708. doi: 10.1016/j.proenv.2016.07.069. [DOI] [Google Scholar]
- 11.Becker J., Manske C., Randl S. Green chemistry and sustainability metrics in the pharmaceutical manufacturing sector. Curr Opin Green Sustain Chem. 2022;33 doi: 10.1016/j.cogsc.2021.100562. [DOI] [Google Scholar]
- 12.van Straten B., van der Heiden D.R., Robertson D., Riekwel C., Jansen F.W., van der Elst M., Horeman T. Surgical waste reprocessing: injection molding using recycled blue wrapping paper from the operating room. J Clean Prod. 2021;322:129121. doi: 10.1016/j.jclepro.2021.129121. [DOI] [Google Scholar]
- 13.Voudrias E.A. Healthcare waste management from the point of view of circular economy. Waste Manag. 2018;75:1–2. doi: 10.1016/j.wasman.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 14.Shuman E.K., Chenoweth C.E. Reuse of medical devices: implications for infection control. Infect Dis Clin North Am. 2012;26:165–172. doi: 10.1016/j.idc.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 15.de Sousa Martins B., Queiroz e Melo J., Logarinho Monteiro J., Rente G., Teixeira Bastos P. Reprocessing of single-use medical devices: clinical and financial results. Portuguese J Public Health. 2018;36:150–156. doi: 10.1159/000496299. [DOI] [Google Scholar]
- 16.Sastri V.R. Elsevier; 2022. Plastics in medical devices. [DOI] [Google Scholar]
- 17.McKeen L.W. Elsevier; 2018. The effect of sterilization methods on plastics and elastomers. [DOI] [Google Scholar]
- 18.Jayabalan M. Sterilization and reprocessing of materials and medical devices—reusability. J Biomater Appl. 1995;10:97–112. doi: 10.1177/088532829501000105. [DOI] [PubMed] [Google Scholar]
- 19.Vinhas G.M., Souto-Maior R.M., de Almeida Y.M.B., Neto B.B. Radiolytic degradation of poly(vinyl chloride) systems. Polym Degrad Stabil. 2004;86:431–436. doi: 10.1016/j.polymdegradstab.2004.05.013. [DOI] [Google Scholar]
- 20.Jayabalan M., Nair P.D., Sreenivasan K. Ageing of radiation-sterilized polypropylene: changes in semicrystallinity. Biomaterials. 1989;10:33–37. doi: 10.1016/0142-9612(89)90006-9. [DOI] [PubMed] [Google Scholar]
- 21.Cehreli M.C., Sahin S., Ergunay K., Ustacelebi S., Sevil U.A. Cytotoxicity of eluates from a gamma-ray-polymerized poly(methyl methacrylate) J Biomater Appl. 2004;18:223–231. doi: 10.1177/0885328204039832. [DOI] [PubMed] [Google Scholar]
- 22.Nair P.D., Sreenivasan K., Jayabalan M. Multiple gamma radiation sterilization of polyester fibres. Biomaterials. 1988;9:335–338. doi: 10.1016/0142-9612(88)90029-4. [DOI] [PubMed] [Google Scholar]
- 23.McKeen L.W. Handbook of Polymer Applications in Medicine and Medical Devices. Elsevier; 2014. Plastics used in medical devices; pp. 21–53. [DOI] [Google Scholar]
- 24.Brown S.A., Merritt K., Woods T.O., McNamee S.G., Hitchins V.M. Effects of different disinfection and sterilization methods on tensile strength of materials used for single-use devices. Biomed Instrum Technol. 2002;36:23–27. doi: 10.2345/0899-8205(2002)36[23:eoddas]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 25.Lerouge S., Guignot C., Tabrizian M., Ferrier D., Yagoubi N., Yahia L. Plasma-based sterilization: effect on surface and bulk properties and hydrolytic stability of reprocessed polyurethane electrophysiology catheters. J Biomed Mater Res. 2000;52:774–782. doi: 10.1002/1097-4636(20001215)52:4<774::AID-JBM23>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 26.Gutiérrez Rodelo C., Salinas R.A., Armenta Jaime E., Armenta S., Galdámez-Martínez A., Castillo-Blum S.E., Astudillo-de la Vega H., Nirmala Grace A., Aguilar-Salinas C.A., Gutiérrez Rodelo J., Christie G., Alsanie W.F., Santana G., Thakur V.K., Dutt A. Zinc associated nanomaterials and their intervention in emerging respiratory viruses: journey to the field of biomedicine and biomaterials. Coord Chem Rev. 2022;457 doi: 10.1016/j.ccr.2021.214402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph B., James J., Kalarikkal N., Thomas S. Recycling of medical plastics. Adv Ind Eng Polym Res. 2021;4:199–208. doi: 10.1016/j.aiepr.2021.06.003. [DOI] [Google Scholar]; This review paper provides a comprehensive overview of the recycling potential of plastics-based medical waste. It also highlights the challenges associated with plastic waste recycling and provides suggestions for addressing them.
- van Straten B., Dankelman J., van der Eijk A., Horeman T. A Circular Healthcare Economy; a feasibility study to reduce surgical stainless steel waste. Sustain Prod Consum. 2021;27:169–175. doi: 10.1016/j.spc.2020.10.030. [DOI] [Google Scholar]; This paper provides a feasibility study on recycling and reuse strategies for medical devices made from stainless steel and their potential to move towards circular economy. The results suggest that environmental and financial benefits are associated with these approaches.
- 29.Lidgren L., Raina D.B., Tägil M., Tanner K.E. Recycling implants: a sustainable solution for musculoskeletal research. Acta Orthop. 2020;91:125. doi: 10.1080/17453674.2019.1706301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iano F.G., dos Santos Sobrinho O., da Silva T.L., Pereira M.A., Figueiredo P.J.M., Alberguini L.B.A., Granjeiro J.M. Optimizing the procedure for mercury recovery from dental amalgam. Braz Oral Res. 2008;22:119–124. doi: 10.1590/S1806-83242008000200005. [DOI] [PubMed] [Google Scholar]
- 31.Shukla S., Halli P., Khalid M.K., Lundström M. Waste pharmaceutical blister packages as a source of secondary aluminum. J Miner Met Mater Soc. 2022;74:612–621. doi: 10.1007/s11837-021-05038-6. [DOI] [Google Scholar]
- 32.Nieminen J., Anugwom I., Kallioinen M., Mänttäri M. Green solvents in recovery of aluminium and plastic from waste pharmaceutical blister packaging. Waste Manag. 2020;107:20–27. doi: 10.1016/j.wasman.2020.03.014. [DOI] [PubMed] [Google Scholar]
- 33.Yousef S., Mumladze T., Tatariants M., Kriūkienė R., Makarevicius V., Bendikiene R., Denafas G. Cleaner and profitable industrial technology for full recovery of metallic and non-metallic fraction of waste pharmaceutical blisters using switchable hydrophilicity solvents. J Clean Prod. 2018;197:379–392. doi: 10.1016/j.jclepro.2018.06.154. [DOI] [Google Scholar]
- 34.Agarwal V., Halli P., Helin S., Tesfaye F., Lundström M. Electrohydraulic fragmentation of aluminum and polymer fractions from waste pharmaceutical blisters. ACS Sustainable Chem Eng. 2020;8:4137–4145. doi: 10.1021/acssuschemeng.9b06810. [DOI] [Google Scholar]
- 35.Walker T.R. (Micro)plastics and the UN sustainable development Goals. Curr Opin Green Sustain Chem. 2021;30 doi: 10.1016/j.cogsc.2021.100497. [DOI] [Google Scholar]
- 36.Royal College of Physicians Less waste, more health: a health professional's guide to reducing waste. https://www.rcplondon.ac.uk/projects/outputs/less-waste-more-health-health-professionals-guide-reducing-waste/ (n.d.)
- 37.Vinyl Council Australia A guide to recycling PVC medical product waste. https://www.vinyl.org.au/images/vinyl/Sustainability/PVCRecoveryInHospitals.pdf (n.d.)
- 38.Rahimi A.R., Garciá J.M. Chemical recycling of waste plastics for new materials production. Nat Rev Chem. 2017;1 doi: 10.1038/s41570-017-0046. [DOI] [Google Scholar]
- 39.Al-Salem S.M., Lettieri P., Baeyens J. Recycling and recovery routes of plastic solid waste (PSW): a review. Waste Manag. 2009;29:2625–2643. doi: 10.1016/j.wasman.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 40.Kaur H., Siddique R., Rajor A. Influence of incinerated biomedical waste ash on the properties of concrete. Construct Build Mater. 2019;226:428–441. doi: 10.1016/j.conbuildmat.2019.07.239. [DOI] [Google Scholar]
- Siwal S.S., Chaudhary G., Saini A.K., Kaur H., Saini V., Mokhta S.K., Chand R., Chandel U.K., Christie G., Thakur V.K. Key ingredients and recycling strategy of personal protective equipment (PPE): towards sustainable solution for the COVID-19 like pandemics. J Environ Chem Eng. 2021;9 doi: 10.1016/j.jece.2021.106284. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors discussed recycling pathways for producing value-added products from PPE in this comprehensive review. Furthermore, PPE kits, raw components used in them, and chemicals and apparatus utilized in the recycling processes are reviewed in this paper.
- Maderuelo-Sanz R., Acedo-Fuentes P., García-Cobos F.J., Sánchez-Delgado F.J., Mota-López M.I., Meneses-Rodríguez J.M. Vol. 786. Sci Total Environ; 2021. The recycling of surgical face masks as sound porous absorbers: preliminary evaluation. [DOI] [PMC free article] [PubMed] [Google Scholar]; This work demonstrates the potential of using recycled disposable face masks as sound porous absorbers, where the polypropylene fibers recycled from face masks had better sound absorption performance than commercial fibrous absorbers.
- 43.Koniorczyk M., Bednarska D., Masek A., Cichosz S. Performance of concrete containing recycled masks used for personal protection during coronavirus pandemic. Construct Build Mater. 2022;324 doi: 10.1016/j.conbuildmat.2022.126712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saberian M., Li J., Kilmartin-Lynch S., Boroujeni M. Repurposing of COVID-19 single-use face masks for pavements base/subbase. Sci Total Environ. 2021:769. doi: 10.1016/j.scitotenv.2021.145527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang G., Li J., Saberian M., Rahat M.H.H., Massarra C., Buckhalter C., Farrington J., Collins T., Johnson J. Use of COVID-19 single-use face masks to improve the rutting resistance of asphalt pavement. Sci Total Environ. 2022:826. doi: 10.1016/j.scitotenv.2022.154118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li C., Yuan X., Sun Z., Suvarna M., Hu X., Wang X., Ok Y.S. Pyrolysis of waste surgical masks into liquid fuel and its life-cycle assessment. Bioresour Technol. 2022;346 doi: 10.1016/j.biortech.2021.126582. [DOI] [PubMed] [Google Scholar]
- 47.Aragaw T.A., Mekonnen B.A. Current plastics pollution threats due to COVID-19 and its possible mitigation techniques: a waste-to-energy conversion via Pyrolysis. Environ Syst Res. 2021;10 doi: 10.1186/s40068-020-00217-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dash A., Kumar S., Singh R.K. Thermolysis of medical waste (Waste syringe) to liquid fuel using semi batch reactor. Waste and Biomass Valorization. 2015;6:507–514. doi: 10.1007/s12649-015-9382-3. [DOI] [Google Scholar]
- Jung S., Lee S., Dou X., Kwon E.E. Valorization of disposable COVID-19 mask through the thermo-chemical process. Chem Eng J. 2021;405 doi: 10.1016/j.cej.2020.126658. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper developed an environmentally benign thermochemical process, wherein the conversion of disposable face masks and CO2 over Ni/SO2 catalysts led to the generation of value-added materials, while CO2 emission was reduced by counterbalancing fossil fuel production.
- 50.Lee S.B., Lee J., Tsang Y.F., Kim Y.M., Jae J., Jung S.C., Park Y.K. Production of value-added aromatics from wasted COVID-19 mask via catalytic pyrolysis. Environ Pollut. 2021;283 doi: 10.1016/j.envpol.2021.117060. [DOI] [PubMed] [Google Scholar]
- 51.Muhyuddin M., Filippi J., Zoia L., Bonizzoni S., Lorenzi R., Berretti E., Capozzoli L., Bellini M., Ferrara C., Lavacchi A., Santoro C. Waste face surgical mask transformation into crude oil and nanostructured electrocatalysts for fuel cells and electrolyzers. ChemSusChem. 2022;15 doi: 10.1002/cssc.202102351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S., Yang X., Yang K., Guo H., Cho M., Kim Y.J., Lee Y. Recycling respirator masks to a high-value product: from COVID-19 prevention to highly efficient battery separator. Chem Eng J. 2022;430 doi: 10.1016/j.cej.2021.132723. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this paper, the authors developed a straightforward and simple reaction, wherein the face masks were converted to battery separators with outstanding electrochemical performance. This technology is very promising and can be used to address challenges associated with discarded face masks.
- 53.Wang Q.Y., Wu Z.F., Zhang M., Qin Z.J., Wang L., Zhong F.R., Duan H.M. Gas-sensing properties and preparation of waste mask fibers/ZnS composites. J Electron Mater. 2022 doi: 10.1007/s11664-022-09644-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hu X., Lin Z. Transforming waste polypropylene face masks into S-doped porous carbon as the cathode electrode for supercapacitors. Ionics. 2021;27:2169–2179. doi: 10.1007/s11581-021-03949-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jiang D.-H., Satoh T., Tung S.H., Kuo C.-C. Sustainable alternatives to nondegradable medical plastics. ACS Sustainable Chem Eng. 2022;10:4792–4806. doi: 10.1021/acssuschemeng.2c00160. [DOI] [Google Scholar]
- 56.Qi Y., He J., Li Y., Yu X., Xiu F.R., Deng Y., Gao X. A novel treatment method of PVC-medical waste by near-critical methanol: dechlorination and additives recovery. Waste Manag. 2018;80:1–9. doi: 10.1016/j.wasman.2018.08.052. [DOI] [PubMed] [Google Scholar]
- 57.Wang C., Wang H., Liu Y. Separation of aluminum and plastic by metallurgy method for recycling waste pharmaceutical blisters. J Clean Prod. 2015;102:378–383. doi: 10.1016/j.jclepro.2015.04.067. [DOI] [Google Scholar]
- 58.Garcia R. Effective cost-reduction strategies in the management of regulated medical waste. Am J Infect Control. 1999;27:165–175. doi: 10.1016/S0196-6553(99)70093-3. [DOI] [PubMed] [Google Scholar]
- 59.Almuneef M., Memish Z.A. Effective medical waste management: it can be done. Am J Infect Control. 2003;31:188–192. doi: 10.1067/mic.2003.43. [DOI] [PubMed] [Google Scholar]
- 60.Erkinay Ozdemir M., Ali Z., Subeshan B., Asmatulu E. Applying machine learning approach in recycling. J Mater Cycles Waste Manag. 2021;23:855–871. doi: 10.1007/s10163-021-01182-y. [DOI] [Google Scholar]
- 61.Wafula S.T., Musiime J., Oporia F. Health care waste management among health workers and associated factors in primary health care facilities in Kampala City, Uganda: a cross-sectional study. BMC Publ Health. 2019;19:203. doi: 10.1186/s12889-019-6528-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Letho Z., Yangdon T., Lhamo C., Limbu C.B., Yoezer S., Jamtsho T., Chhetri P., Tshering D. Awareness and practice of medical waste management among healthcare providers in National Referral Hospital. PLoS One. 2021;16 doi: 10.1371/journal.pone.0243817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thakur S., Verma A., Sharma B., Chaudhary J., Tamulevicius S., Thakur V.K. Recent developments in recycling of polystyrene based plastics. Curr Opin Green Sustain Chem. 2018;13:32–38. doi: 10.1016/j.cogsc.2018.03.011. [DOI] [Google Scholar]
- 64.Thakur S., Chaudhary J., Sharma B., Verma A., Tamulevicius S., Thakur V.K. Sustainability of bioplastics: opportunities and challenges. Curr Opin Green Sustain Chem. 2018;13:68–75. doi: 10.1016/j.cogsc.2018.04.013. [DOI] [Google Scholar]