Abstract
Poor diet quality exacerbates risks for acute and chronic conditions. People experiencing food insecurity have an increased likelihood of lower diet quality; however, this has not been investigated in the Australian context. The aim of this cross-sectional study was to examine whether the diet quality of Australian adults differed according to their household food security status. Data were analysed from a nationally representative sample (≥19 years; n = 9115) collected as part of the National Nutrition and Physical Activity Survey 2011-12. Household food security status and socio-demographic and health characteristics were assessed using data from an 18-module health interview. A 24 h dietary recall was used to estimate food and nutrient intakes and to calculate the Dietary Guidelines Index (DGI). DGI is a food-based score (0 to 130) that assesses adherence to the 2013 Australian Dietary Guidelines. Survey-weighted linear regression models, adjusted for age and sex, were used to examine diet quality (total DGI and component scores), and total energy and nutrient intake by food security status. Adults from food-insecure households had a mean total DGI score 3.5 points lower (95% CI −5.57, −1.46) than food-secure adults (p = 0.001). Adults from households experiencing food insecurity, when compared to those who were food-secure, had several lower DGI component scores including for dietary variety (1.6 vs. 2.3, p = 0.009), fruit (3.8 vs. 5.0, p = 0.001) and vegetables (3.7 vs. 4.4, p = 0.010). Adults from food-insecure households consumed on average more carbohydrates (45.6 vs. 43.3, p = 0.004) and total sugar (21.8 vs. 19.0, p = 0.003) as a percentage of daily energy and less protein (18.5 vs. 17.2, p = 0.004), mono-unsaturated fats (11.2 vs. 11.8, p = 0.026) as a percentage of daily energy, and fibre (20.1 vs. 23.0, p = 0.003), than food-secure adults. Sub-optimal diet may be one of the contributing factors to, or outcomes of, poorer health in food-insecure populations. Food security interventions are required to better address nutrition in food-insecure households and should be tailored to the health and socio-demographic characteristics of this population.
Keywords: food security, diet quality, nutrition inequities, adults, nationally representative survey
1. Introduction
Due to the impact of the COVID-19 pandemic, the prevalence of household food insecurity is globally on the rise, including in developed economies [1]. This health and social problem that affects households can be both a precursor to, and a consequence of, economic marginalisation and poor health. Food insecurity occurs when there is inadequate access to safe, culturally appropriate, and nutritious food [2]. According to the 2017–2019 estimates by the Food and Agriculture Organization (FAO), the average prevalence of food insecurity across high-income countries was 7.5% and 13.5% in Australia [3], with these rates likely to have risen since then.
Evidence suggests that the diet quality of people experiencing food insecurity can be sub-optimal. A systematic review of 26 diet quality studies from the United States (US) (published 1997–2012) [4] found that adults experiencing food insecurity consumed fewer vegetables, fruit, and dairy products and had lower intake of vitamins A and B-6, zinc, calcium and magnesium when compared to food-secure adults. However, associations between food security status and other aspects of dietary intake (e.g., macronutrients, grains, iron) were not substantiated. In 2014, a nationally representative cross-sectional analysis from the U.S. found that, compared with food-secure adults, food-insecure adults reported a 2-unit lower Healthy Eating Index score [5] and low-income food-insecure adults had a higher consumption of high-fat dairy products, salty snacks, sugar-sweetened beverages, processed meat and consumed fewer vegetables than low-income food-secure adults [6]. Similarly older Americans (aged > 60 years) experiencing food insecurity, when compared to their food-secure peers, have a lower mean total Healthy Eating Index score [7]. A nationally representative study from France [8] found that people experiencing food insecurity consumed less fruit, vegetables and fish than those who were food-secure. In Australia, a study using the National Nutrition and Physical Activity Survey (NNPAS) 2011-12 found that, when compared with the least socio-economically disadvantaged group, the most disadvantaged group had a 2.5–4.5 units lower Dietary Guidelines Index score. Considering that socio-economically disadvantaged populations are more likely to experience food insecurity, an examination of food security status and diet quality in an Australian setting may further highlight priority populations for public health intervention.
The aim of this cross-sectional study was to examine the diet quality of Australian adults according to household food security status using the nationally representative NNPAS 2011-12. A secondary aim was to investigate the health and socio-demographic characteristics of Australian adults according to food security status.
2. Materials and Methods
2.1. Study Design and Participants
This manuscript describes a cross-sectional observational study using data from the most recent nationally representative Australian nutrition survey, the NNPAS 2011-12 component of the Australian Health Survey [9]. This survey [10,11] was administered by the Australian Bureau of Statistics (ABS) and sampled households across all states and territories. The NNPAS did not include participants who are Indigenous, as these respondents participated in the National Aboriginal and Torres Strait Islander Nutrition and Physical Activity Survey 2012-13 [12]. Full details of the Australian Health Survey study design are published elsewhere, including in a number of previously published nutrition studies [10,11].
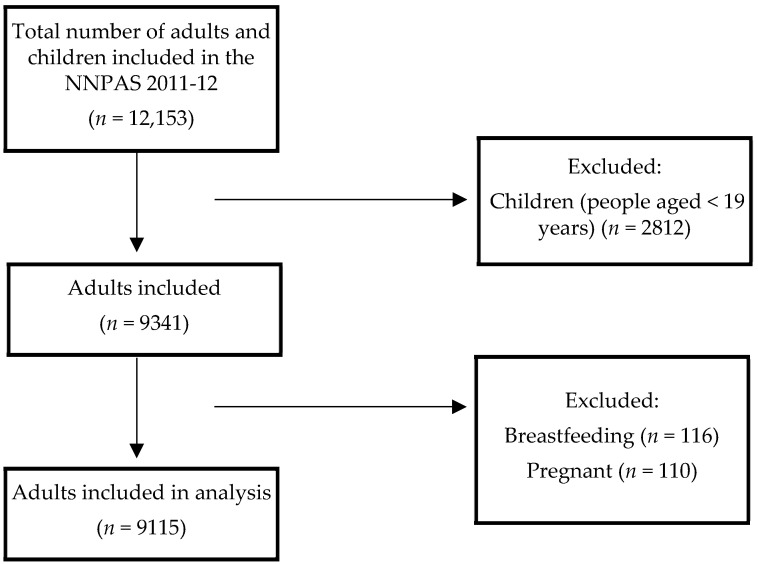
A total of 14,363 private dwellings were initially selected to participate in the survey, of which 9519 households responded to the NNPAS interview component (77% response rate; n = 12,153 adults and children). The interview included 18 modules, on a range of demographic, nutrition, physical activity and health questions. A total of 9341 adults (≥19 years) completed the food security questions in the interview and one 24 h dietary recall (see Figure 1). After excluding pregnant and breastfeeding adults, 9115 adults were ultimately included in the analysis.
Figure 1.
Flow diagram of participants included in the analysis of the National Nutrition and Physical Activity Survey 2011-12.
2.2. Procedures
2.2.1. Food Security
Household food security status was established using a standard single-item measure common in national ABS surveys [9]: asking respondents if they (or any member of the household) had run out of food in the last 12 months and could not afford to buy more (binary variable; yes, no). Affirmative responses were considered ‘food insecure’.
2.2.2. Dietary Intake
Information on consumed food and beverages was collected using a 24 h dietary recall based on the United States Department of Agriculture’s Automated Multiple-Pass Method (adapted to the Australian context) and facilitated by face-to-face trained interviewers. Energy and nutrient intakes (total energy—KJ), percentage energy from total fat, saturated fat, trans fat, mono-unsaturated fat, poly-unsaturated fat, carbohydrates, total sugars and protein, and fibre density and sodium density(g/MJ) were estimated from the recall using the Australian Food and Nutrient Database 2011–2013 [13]. Brief questionnaires were used to report on the usual daily use of salt (both at the table and during cooking, with response options: “not used”, “rarely”, “occasionally” or “very often”) [9].
2.2.3. Diet Quality
Diet quality was assessed by the Dietary Guideline Index (DGI) (see Supplemental Table S1). The DGI is a food-based score that assesses compliance with age- and sex-specific recommendations outlined in the current (2013) Australian Dietary Guidelines [14]. Dietary intakes were scored according to recommended dietary components (food variety, fruit, vegetables, cereals, meat and alternatives, dairy and alternatives, and fluid intake in terms of total consumed beverages and proportion of these that are water) and adverse dietary components (discretionary foods, saturated fat, unsaturated fat, added salt, added sugars, and alcohol). Each component was scored out of 10, with proportionate scoring used to score intakes that fell between the maximum and minimum scoring criteria. For example, if a participant consumed 1 serving of fruit per day, they received a score of 5 out of 10. The total DGI scores range between 0 and 130. A higher score indicates a better diet quality.
2.2.4. Sociodemographic and Health Characteristics
Collected information on sociodemographic and health characteristics included age (discrete; years), sex (binary; male, female), household income based on the gross weekly combined equivalised income of all household members aged ≥15 years (categorised into deciles), educational obtainment assessed on highest level completed (categorised into low—incomplete high school or less; medium—completed high school or incomplete high school and/or certificate/diploma; or high—tertiary qualification), location (determined by using the Australian Statistical Geography Standard Remoteness areas [9] and categorised into major cities of Australia, inner regional Australia and a combined outer regional Australia, remote Australia and very remote Australia), country of birth (categorised into Australia; English-speaking country outside of Australia; non-English speaking countries outside of Australia), marital status (binary; married, not married) and smoking status (categorised into current; ex-smoker; never smoked). Weight (kg) and height (m) were measured by trained interviewers using digital scales to measure weight and a stadiometer to measure height. BMI was calculated from weight and height and categorized into underweight (BMI ≤ 20 kg/m2), normal weight (BMI ≤ 24.9 kg/m2), overweight (BMI ≥ 25 kg/m2 and < 30 kg/m2) and obese (BMI ≥ 30 kg/m2) [9].
2.3. Analysis
Statistical analysis was performed using Stata [15] applying survey weightings to account for the survey design and for the probability of selection. p-values < 0.05 were considered statistically significant. As there were no participants with substantive missing data for outcomes or covariates (i.e., no participant had more than 2 variables missing), no exclusions were made on this basis. Multiple imputation by chained equations (50 imputations), with all study variables used in the imputation models, was used for handling missing data, as 7176 adults had complete data for study variables, 1033 were missing BMI, 602 were missing income, and 304 were missing both BMI and income.
Descriptive statistics (means and proportions with 95% CIs) were used to report the distribution of socio-demographic and health characteristics and diet quality according to food security status. Survey-weighted, multiple imputation linear regression models were fitted to test differences in diet quality (DGI total score and component scores; continuous dependent variables), total energy and nutrient intakes (continuous dependent variables) according to food security status (binary independent variable). Confounders were established a priori based on the previous literature [6,16,17]. Data were analysed using the following two covariate models: model 1 (minimally adjusted), included age (continuous) and sex (binary) as covariates; model 2 provided a sensitivity analysis (see supplement 2) and was adjusted for model 1 covariates (age, sex), as well as equivalised household income (categorical), educational obtainment (categorical), country of birth (categorical), marital status (categorical) and smoking status (categorical).
2.4. General Procedure
This project (number 2021-357) was declared exempt from ethical review by the Deakin University Human Research Ethics Committee. The STROBE-nut checklist [18] was used to design and report the findings.
3. Results
3.1. Socio-Demographic and Health Characteristics of Australian Adults by Food Security Status
The survey-weighted estimates indicate most adult participants (95.6%) were assessed as living in households that were food-secure, and 4.4% lived in households experiencing food insecurity. Survey-weighted participant demographic and health characteristics according to food security status are described in Table 1. Adults in food-insecure households were younger (mean age 39.9 vs. 46.9 years) with a higher proportion of being female (61.6% vs. 48.9%) and living below the poverty line (44.7% vs. 18.1%), compared to adults not experiencing food insecurity. Half of those who were food-insecure were employed; 9.4% were unemployed; and 40.9% were not in the labour force, compared with 67.7%, 2.3% and 30.0%, respectively, for food-secure adults. Higher proportions of food-secure adults were married (60.1% vs. 33.8%), and adults experiencing food insecurity reported higher rates of current smoking (50.3% vs. 16.8%). More than one-third (37.9%) of those experiencing food insecurity reported low educational attainment (25.4% of food-secure), and 14.2% had obtained a tertiary qualification (25.5% of food-secure). There were no significant differences according to food security status in terms of country of birth, location or BMI category.
Table 1.
Survey-weighted socio-demographic and health characteristics of Australian adults by food security status using the NNPAS 2011-12.
| Characteristic | Food-Secure (95.6%) |
Food-Insecure (4.4%) |
p Value ^ | |
|---|---|---|---|---|
| Age, mean | Years | 46.9 (46.8, 47.1) |
39.9 (38.8, 41.6) |
<0.001 |
| Sex, % | Male Female |
51.1 (50.7, 51.5) 48.9 (48.5, 49.3) |
38.4 (32.5, 44.8) 61.6 (55.2, 67.5) |
<0.001 |
| Equivilised household income, % # | Below the poverty line Above the poverty line |
18.1 (17.0, 19.2) 81.9 (80.8, 83.0) |
44.7 (37.7, 51.7) 55.3 (48.3, 62.3) |
<0.001 |
| Country of birth, % * | Australia English speaking Non-English speaking |
68.6 (66.9, 70.3) 11.7 (10.8, 12.6) 19.7 (18.1, 21.4) |
74.4 (67.7, 80.2) 10.0 (5.7, 17.0) 15.6 (10.5, 22.5) |
0.33 |
| Location, % ± | Major city Inner regional Outer regional/remote |
71.7 (70.5, 73.0) 19.0 (17.3, 20.8) 9.3 (7.8, 11.0) |
66.0 (59.6, 71.7) 24.0 (18.6, 30.3) 10.1 (6.8, 14.6) |
0.11 |
| Labour status, % | Employed Unemployed Not in labour force |
67.7 (66.3, 69.1) 2.3 (1.9, 2.9) 30.0 (28.8, 31.2) |
49.7 (42.7, 56.7) 9.4 (5.5, 15.6) 40.9 (34.4, 47.8) |
<0.001 |
| Marital status, % | Married Not married |
60.1 (58.9, 61.3) 39.9 (38.7, 41.1) |
33.8 (27.0) 66.2 (58.7, 73.0) |
<0.001 |
| Educational obtainment, % ^^ | Low Medium High | 25.4 (24.2, 26.5) 49.2 (47.6, 50.8) 25.5 (24.1, 26.9) |
37.9 (31.0, 45.4) 47.9 (40.3, 55.6) 14.2 (9.5, 20.7) |
<0.001 |
| Body Mass Index, % ## | Underweight Normal weight Overweight Obese |
2.2 (1.7, 2.7) 34.0 (32.6, 35.4) 36.6 (35.1, 38.1) 27.2 (25.9, 28.6) |
2.9 (0.4, 5.4) 35.6 (28.8, 42.4) 27.5 (21.0, 33.9) 33.9 (27.5, 40.4) |
0.06 |
| Smoking status, % ** | Current smoker Ex-smoker Never smoked |
16.8 (15.7, 17.9) 31.4 (30.1, 32.8) 51.8 (50.3, 53.2) |
50.3 (42.6, 58.0) 23.8 (18.2, 30.5) 25.9 (20.8, 31.8) |
<0.001 |
Values represent mean and in brackets, 95% confidence intervals after applying survey weighting, rounded to 1 decimal place. ^ Unadjusted survey-weighted regression models were used to compare characteristics between food-secure and food-insecure populations. # Below poverty line—income decile 1 and 2 ≤ AUD 398/weekly; above poverty line—income decile 3–10. * English Speaking—Canada, Repub. of Ireland, New Zealand, South Africa, UK and USA. We considered anglophone countries to have some similarities in terms of food cultures and diets, and hence they were grouped together. ± Outer regional/remote—outer regional Australia, remote Australia and very remote Australia, ^^ Low—incomplete high school or less; medium—completed high school or incomplete high school and/or certificate/diploma; high—tertiary qualification. ## Body mass Index (BMI). Underweight is BMI less than 18.5 kg/m2, normal BMI is 18.5 to < 25 kg/m2, overweight BMI is 25.0 to <30 kg/m2, Obese BMI is 30.0 kg/m2 or higher ** Current—daily, at least once a week and less than weekly.
3.2. Diet Quality Assessment Using the Dietary Guidelines Index (DGI)
The total DGI mean score for adults in food-secure households was 76.8 (95% CI 76.3, 77.3), and it was 72.8 (95% CI 70.5, 75.2) for those experiencing food insecurity. After adjustment for age and sex (model 1), adults in food-insecure households had a 3.52 (−5.57, −1.46) lower mean DGI score than food-secure adults (p = 0.001) (Table 2). In the fully adjusted model, (model 2) the difference between the groups was no longer statistically significant and was closer to half a point (B = - 0.45; 95% CI −2.48, 1.58, see Supplement Table S2). Food variety scores were significantly different (in both models 1 and 2) between the groups, with adults in food-secure households achieving a mean score of 2.3 and food-insecure achieving 1.6. In terms of fruit, vegetables, cereals (including wholegrains), and meat and alternatives, adults in food-insecure households had lower mean scores compared to food-secure adults, with significant differences for model 1 (but not model 2). The mean scores were comparable for dairy and fluid intake. In terms of mean scores for adverse dietary components (discretionary foods, saturated fat, unsaturated fat, added salt, added sugar, and alcohol), the groups were comparable on most scores except moderating unsaturated fat intake, where food-insecure adults obtained higher scores (8.7 vs. 8.2) and, limiting added salt at the table, where food-insecure adults obtained lower scores (2.8 vs. 3.3).
Table 2.
DGI total and component scores by food security status.
| DGI Component Mean Scores * | Food-Secure | Food-Insecure | Model 1—Group Differences (Minimally Adjusted) a |
|
|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | B (95% CI) | p Value | |
| 1. Food variety | 2.3 (2.3, 2.3) | 1.6 (1.5, 1.8) | −0.54 (−0.72, −0.36) | <0.005 |
| 2. Fruit | 5.0 (4.9, 5.1) | 3.8 (3.1, 4.5) | −1.06 (−1.69, −0.43) | 0.001 |
| 3. Vegetables | 4.4 (4.3, 4.5) | 3.7 (3.2, 4.2) | −0.62 (−1.09, −0.15) | 0.010 |
| 4. Cereal (total) serves per day | 2.8 (2.8, 2.9) | 2.4 (2.2, 2.7) | −0.26 (−0.50, −0.03) | 0.026 |
| mostly wholegrain | 1.5 (1.4, 1.5) | 1.0 (0.8, 1.2) | −0.31 (−0.57, −0.05) | 0.021 |
| 5. Meat and alternatives (total) serves per day | 3.0 (2.9, 3.0) | 2.6 (2.3, 2.9) | −0.28 (−0.55, −0.01) | 0.045 |
| mostly lean | 4.5 (4.4, 4.5) | 4.5 (4.3, 4.6) | 0.01 (−0.18, 0.19) | 0.95 |
| 6. Dairy and alternatives (total) | 4.7 (4.6, 4.8) | 4.6 (4.1, 5.1) | −0.32 (−0.80, 0.16) | 0.19 |
| 7. Fluid intake (total) serves per day | 3.8 (3.7, 3.8) | 3.9 (3.6, 4.1) | −0.02 (−0.21, 0.18) | 0.87 |
| mostly water | 4.3 (4.3, 4.4) | 4.4 (4.2, 4.6) | −0.01 (−0.20, 0.17) | 0.90 |
| 8. Limit discretionary foods | 3.3 (3.1, 3.4) | 3.5 (2.8, 4.2) | 0.21 (−0.42, 0.84) | 0.51 |
| 9. Limit saturated fat mostly trimmed meat | 4.4 (4.4, 4.5) | 4.2 (3.9, 4.5) | −0.22 (−0.47, 0.03) | 0.08 |
| mostly low-fat milk | 3.8 (3.7, 3.9) | 3.7 (3.4, 4.0) | −0.02 (−0.33, 0.29) | 0.91 |
| 10. Moderate unsaturated fat | 8.2 (8.0, 8.3) | 8.7 (8.1, 9.3) | 0.60 (0.10, 1.09) | 0.018 |
| 11. Limit added salt during cooking | 2.6 (2.5, 2.6) | 2.5 (2.1, 2.8) | −0.02 (−0.34, 0.29) | 0.88 |
| at the table | 3.3 (3.2, 3.4) | 2.8 (2.5, 3.2) | −0.58 (−0.89, −0.27) | <0.001 |
| 12. Limit extra sugars | 6.6 (6.4, 6.7) | 6.5 (5.9, 7.0) | 0.13 (−0.49, 0.76) | 0.68 |
| 13. Limit alcohol | 8.5 (8.4, 8.6) | 8.5 (8.1, 9.0) | −0.20 (−0.71, 0.31) | 0.45 |
| TOTAL DGI SCORE | 76.8 (76.3, 77.3) | 72.8 (70.5, 75.2) | −3.52 (−5.57, −1.46) | 0.001 |
Values represent unadjusted means and in brackets, 95% confidence intervals after applying survey weighting * See Supplement Table S1 for how scores are calculated. a Mean difference between food-secure and food-insecure groups, adjusted for age and sex, estimated using survey-weighted multiple imputation linear regression models.
3.3. Energy and Nutrient Intakes by Food Security Status
As shown in Table 3, adults in food-insecure households had lower overall energy intake (8147 kJ/day; food-secure 8694 kJ/day, p = 0.048), protein intake (17.2% E/day; food-secure 18.5% E/day, p = 0.004), mono-unsaturated fat intake (11.2%E/day; food-secure 11.8%E/day, p = 0.026), and fibre intake (20.1 g/MJ; food-secure 23.0 g/MJ, p = 0.003). Conversely, they had a higher carbohydrate intake (45.6% E/day; food-secure 43.3% E/day, p = 0.004) and total sugar intake (21.8% E/day; food-secure 19.0% E/day, p = 0.003) than those in food-secure households. After adjusting for age, sex, and additional co-variates equivalised household income, education, country of birth, marital status and smoking status (model 2), significant differences remained between adults in food-secure and -insecure households in terms of protein, mono-unsaturated fat, carbohydrates and total sugar intake (Supplement Table S3).
Table 3.
Total energy and nutrient intakes of adults by food security status.
| Energy/Nutrient Mean | Food-Secure | Food-Insecure | Model 1—Group Differences (Minimally Adjusted) a | |
|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | B (95% CI) | p Value | |
| Energy intake (kJ/day) | 8694 (8589, 8800) | 8147 (7622, 8672) | −474.2 (−943.3, −5.1) | 0.048 |
| Protein intake (%E/day) | 18.5 (18.3, 18.6) | 17.2 (16.3, 18.1) | −1.24 (−2.09, −0.39) | 0.004 |
| Total fat (%E/day) | 30.9 (30.6, 31.1) | 30.0 (28.5, 31.4) | −1.13 (−2.42, 0.17) | 0.09 |
| Saturated fat intake (%E/day) | 12.1 (11.9, 12.2) | 12.1 (11.4, 12.8) | −0.01 (−0.74, 0.72) | 0.97 |
| Trans fat intake (%E/day) | 0.5 (0.6, 0.6) | 0.6 (0.5, 0.6) | 0.01 (−0.05, 0.07) | 0.81 |
| Mono-unsaturated fat intake (%E/day) | 11.8 (11.7, 12.0) | 11.2 (10.5, 11.9) | −0.73 (−1.37, −0.09) | 0.026 |
| Poly-unsaturated fat intake (%E/day) | 4.8 (4.7, 4.9) | 4.6 (4.2, 5.0) | −0.29 (−0.66, 0.08) | 0.13 |
| Carbohydrate intake (%E/day) | 43.3 (43.0, 43.6) | 45.6 (44.0, 47.2) | 2.03 (0.65, 3.41) | 0.004 |
| Total sugars intake (%E/day) | 19.0 (18.8, 19.3) | 21.8 (19.8, 23.8) | 2.55 (0.90, 4.21) | 0.003 |
| Fibre intake (g/MJ) | 23.0 (22.6, 23.4) | 20.1 (18.3, 21.8) | −2.29 (−3.81, −0.77) | 0.003 |
| Sodium intake (mg/MJ) | 2443 (2407, 2479) | 2321 (2152, 2490) | −136.7 (−321.6, 48.2) | 0.15 |
Values represent unadjusted means and in brackets, 95% confidence intervals after applying survey weighting. a Mean difference between food-secure and food-insecure groups, adjusted for age and sex, estimated using survey weighted multiple imputation linear regression models.
4. Discussion
This is the first study to examine diet quality according to household food security status in Australia. The results suggest differences in the quality of diets and the demographic and health characteristics between Australian adults living in households experiencing food insecurity and those from food-secure households. Adjusted for age and sex, food-insecure adults had more than a three-point lower average total DGI score than their food-secure peers; lower fruit, vegetable, and cereal intake; and lower total energy, protein, fibre, and mono-unsaturated fat intake. Half of the adults in food-insecure households were employed, and one-third had not completed high school (categorised as low educational attainment). Adults in food-insecure households were younger, with a higher proportion of those who were female, unmarried, and living below the poverty line, compared to food-secure adults. In terms of health status, BMI was similar between the two groups, and a larger proportion of adults living in food-insecure households reported being current smokers.
This investigation reports similar findings to national and international research regarding the diet quality of adults residing in food-insecure households. Whilst the diet quality measures have similar components but different scales (in the US, scores range from 0 to 100; in Australia, they range from 0 to 130), a 2014 US investigation [5] found an average of 2 units lower for adults in food-insecure households versus food-secure households, similar to our finding of a 3.5 units difference in the total DGI score. The difference in the Australian scores is equivalent to daily food intakes of one less serving of vegetables or more frequent salt use. These differences, if sustained, could adversely impact diet-related chronic disease risk, such as cardiovascular disease, for food-insecure populations [19].
Higher carbohydrate, lower dietary diversity score, and lower meat (or alternative) intakes are consistent with the literature describing the coping strategies of people who experience food insecurity. Australian qualitative research examining the experience of people on low incomes or in poverty identifies coping strategies aiming to bulk out diets by adding cheaper (often less nutritious) and filling foods, such as low-cost cereals in the daily-food practices of adults reliant on charitable food [20,21]. Both meat and dairy have also been identified in research as more expensive components of a diet that are sometimes forgone by single mothers [22], urban households [23], and households impacted by the COVID-19 pandemic [24]. Consistent with our findings, adults living in food-insecure households in Australia and other high-income countries eat less than their recommended amount of fruit and vegetables and less than their food-secure peers [4,8]. Furthermore, a lower food variety score and higher carbohydrate intake in food-insecure households remained following the adjustment for model 2, suggesting these dietary practices persist independent of strong and inter-connected predictors of food security.
Non-dietary risk factors for chronic disease, such as smoking and high-BMI may be compounded by food insecurity in households. In this study, differences in BMI were not significant overall, although greater proportions of adults who were food-insecure were underweight or obese. There is growing global evidence to suggest there is a paradoxical association between food insecurity and obesity [25]. In our study, the increased likelihood of food-insecure adults currently smoking is also reported in US studies [26]. This further underscores the complex potential syndemic of health, social, and economic factors faced by adults residing in food-insecure households. Reducing household food insecurity could be an effective way to prevent chronic disease, and clinicians are increasingly urged to consider and screen adults [25] and children [27] for food insecurity.
There are several potential research, policy, and practice implications of this study. To our knowledge, this research is a first in Australia and the only study to include detailed dietary data from non-Indigenous adults living in food-insecure households. It provides a methodology that can be repeated and improved upon in the forthcoming ABS nutrition and physical activity survey (planned for 2023) and for ongoing monitoring.
In terms of policy, Australians experiencing food insecurity are more likely to be in receipt of social assistance payments than the general population [28]. Increasing social protection incomes to a level that at least meets the minimum costs of living [28] and ensures the affordability of a nutritious diet is included in those calculations, would help to address some of the concerning dietary intake identified in this study. For Australians experiencing food insecurity whilst in paid employment (49.7% of our sample), the adequacy of wages is important. This study found that the dietary intake of several recommended food groups was sub-optimal in food-insecure adults and that particular sub-populations might be at an increased risk, for example women, people out of the workforce, people who are single, and/or people living below the poverty line. The Government should consider the potential impact of fiscal policies, such as the good and services tax (GST), on these groups, and single-parent households (for example) are more likely to experience food stress with proposed changes to the GST [29,30]. This research supports the calls for a national integrated food and nutrition policy and monitoring and surveillance system that includes a focus on equity, household food security, and priority populations at increased risk of diet-related diseases [31,32].
Practitioners and programmes supporting food-insecure households could sensibly prioritize fruit, vegetables, wholegrains, increased variety, and foods high in mono-unsaturated fats and fibre to improve diet quality. Interventions should seek to target populations identified as at higher risk (e.g., women, single people, and people living below the poverty line). The current findings also emphasize the importance of nutrition and food security interventions for people who smoke.
There are several design strengths and limitations of this study. The ABS 2011-12 NNPAS is a nationally representative study, which is a strength. However, this is the latest national dietary survey that is a decade old, and dietary practices are likely to have changed over that time. The single-item food insecurity measure used is known to under-report [33] and the prevalence among the Australian population may be closer to 10–13% [3], and higher still in Aboriginal and Torres Strait Islander populations [12], and especially since the COVID-19 pandemic [1]. This would suggest that the dietary implications demonstrated by this current study are likely to be reaching further into society. The sample for this analysis was limited to 399 non-Indigenous adults, and despite the sampling strategy to recruit a nationally representative participant group and the use of survey-weighting in the statistical analysis, it is unlikely to represent the diets, health, and demographics of all food-insecure Australian adults and it excludes first-nation people who are disproportionally affected by food insecurity. Unlike the measures used elsewhere [34], the Australian food and nutrition monitoring system does not allow for the assessment of the severity of food insecurity or impact on households with children [35]. Furthermore, in order to maximise the sample size, only one day of dietary recall was used, rather than two days. While this has limitations in terms of assessing the usual intake of individuals, it is appropriate for population monitoring and surveillance [36]. Self-reported dietary assessment is known to be subject to under-reporting; however, 24 h recalls are shown to be the least impacted by measurement error compared to other approaches. The food frequency questionnaire and the tool used in Australia was based on the standardised Automated Multiple Pass method [36,37]. Due to the cross-sectional design, we were unable to infer any temporal relationships between diet and food security status.
5. Conclusions
This cross-sectional study examined whether the diet quality of Australian adults differed according to their household food security status. Adults residing in households experiencing food insecurity were found to have a mean total DGI score 3.5 points lower than those in food-secure households. In addition, adults experiencing food insecurity, when compared to those who were food-secure, had lower scores for dietary variety, fruit, and vegetables and consumed more carbohydrates and total sugars and less protein, mono-unsaturated fat, and fibre. If these dietary patterns persist, Australians from food-insecure households are at increased risk of diet-related chronic disease, and thus should be a priority population for public health interventions.
Acknowledgments
R.L. wishes to acknowledge Priscila Machado for her assistance with Stata software and data analysis.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu14194133/s1, Table S1. Components and scoring methods of the Dietary Guideline Index (DGI-2013). Table S2. DGI score by food security status, Table S3. Total energy and nutrient intakes of adults by food security status.
Author Contributions
Conceptualization, R.L., K.M.L. and S.A.M.; methodology and data analysis plan, R.L., S.A.M., G.A., C.M.P., A.L.Y. and K.M.L.; software, R.L., K.M.L. and G.A.; data analysis, R.L, K.M.L. and G.A.; data curation, R.L. and K.M.L.; writing—original draft preparation, R.L.; writing—review and editing, all authors; supervision, S.A.M.; project administration, R.L.; funding acquisition, R.L. and S.A.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to the study requiring only the use of pre-existing collections of non-identifiable data about human beings. This is in accordance with the Australian ‘National Statement on Ethical Conduct in Human Research (2007, updated 2018)’.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the National Nutrition and Physical Activity survey, as described by the Australian Bureau of Statistics here: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4363.0.55.001Chapter2152011-13 (accessed on 1 September 2022).
Data Availability Statement
Data are available from the Australian Bureau of Statistics.
Conflicts of Interest
Authors have no conflicts of interest to declare.
Funding Statement
This research received no external funding and was made possible through a Dean’s Postdoctoral Research Fellowship, Deakin University. KML is supported by a National Health and Medical Research Council Emerging Leadership Fellowship (APP1173803).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.High Level Panel of Experts (HLPE) Impacts of COVID-19 on Food Security and Nutrition: Developing Effective Policy Responses to Address the Hunger and Malnutrition Pandemic Rome. 2020. [(accessed on 3 August 2021)]. Available online: http://www.fao.org/3/cb1000en/cb1000en.pdf.
- 2.Food and Agriculture Organziation (FAO) The State of Food Insecurity in the World 2001 Rome: United Nations. 2001. [(accessed on 15 August 2022)]. Available online: https://www.fao.org/3/y1500e/y1500e00.htm.
- 3.Food and Agriculture Organization (FAO) State of Food Security and Nutrition in the World—Table A1.1 Geneva: United Nations 2020. [(accessed on 2 March 2022)]. Available online: https://www.fao.org/3/ca9692en/online/ca9692en.html#chapter-a1_1.
- 4.Hanson K.L., Connor L.M. Food insecurity and dietary quality in US adults and children: A systematic review. Am. J. Clin. Nutr. 2014;100:684–692. doi: 10.3945/ajcn.114.084525. [DOI] [PubMed] [Google Scholar]
- 5.Leung C.W., Tester J.M. The Association between Food Insecurity and Diet Quality Varies by Race/Ethnicity: An Analysis of National Health and Nutrition Examination Survey 2011–2014 Results. J. Acad. Nutr. Diet. 2019;119:1676–1686. doi: 10.1016/j.jand.2018.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leung C.W., Epel E.S., Ritchie L.D., Crawford P.B., Laraia B.A. Food Insecurity Is Inversely Associated with Diet Quality of Lower-Income Adults. J. Acad. Nutr. Diet. 2014;114:1943–1953.e2. doi: 10.1016/j.jand.2014.06.353. [DOI] [PubMed] [Google Scholar]
- 7.Vaudin A., Moshfegh A., Sahyoun N. Measuring Food Insecurity in Older Adults Using both Physical and Economic Food Access, NHANES 2013-18. J. Nutr. 2022;152:1953–1962. doi: 10.1093/jn/nxac058. [DOI] [PubMed] [Google Scholar]
- 8.Bocquier A., Vieux F., Lioret S., Dubuisson C., Caillavet F., Darmon N. Socio-economic characteristics, living conditions and diet quality are associated with food insecurity in France. Public Health Nutr. 2015;18:2952–2961. doi: 10.1017/S1368980014002912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Australian Bureau of Statistics (ABS) 4363.0.55.001—Australian Health Survey: Users’ Guide, 2011–2013. Australian Bureau of Statistics (ABS); Canberra, Australia: 2015. [Google Scholar]
- 10.Machado P.P., Steele E.M., Levy R.B., Sui Z., Rangan A., Woods J., Gill T., Scrinis G., Monteiro C.A. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: Evidence from a nationally representative cross-sectional study. BMJ Open. 2019;9:e029544. doi: 10.1136/bmjopen-2019-029544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchese L., Livingstone K.M., Woods J.L., Wingrove K., Machado P. Ultra-processed food consumption, socio-demographics and diet quality in Australian adults. Public Health Nutr. 2022;25:94–104. doi: 10.1017/S1368980021003967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Australian Bureau of Statistics (ABS) 4727.0.55.005—Australian Aboriginal and Torres Strait Islander Health Survey: Nutrition Results—Food and Nutrients, 2012–2013. Australian Bureau of Statistics (ABS); Canberra, Australia: 2015. [(accessed on 24 May 2022)]. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/PrimaryMainFeatures/4727.0.55.005?OpenDocument. [Google Scholar]
- 13.Food Standards Australia New Zealand (FSANZ) AUSNUT 2011–2013 Food Composition Database. FSANZ; Canberra, Australia: 2014. [(accessed on 24 May 2022)]. Available online: https://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/Pages/default.aspx. [Google Scholar]
- 14.Thorpe M.G., Milte C.M., Crawford D., McNaughton S.A. A Revised Australian Dietary Guideline Index and Its Association with Key Sociodemographic Factors, Health Behaviors and Body Mass Index in Peri-Retirement Aged Adults. Nutrients. 2016;8:160. doi: 10.3390/nu8030160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.StataCorp . Stata Statistical Software: Release 16 College Station. StataCorp LLC; College Station, TX, USA: 2019. [(accessed on 5 July 2022)]. Available online: https://www.stata.com. [Google Scholar]
- 16.Gamba R., Leung C.W., Guendelman S., Lahiff M., Laraia B.A. Household Food Insecurity Is Not Associated with Overall Diet Quality Among Pregnant Women in NHANES 1999–2008. Matern. Child Health J. 2016;20:2348–2356. doi: 10.1007/s10995-016-2058-1. [DOI] [PubMed] [Google Scholar]
- 17.Jia J., Fung V., Meigs J.B., Thorndike A.N. Food Insecurity, Dietary Quality, and Health Care Utilization in Lower-Income Adults: A Cross-Sectional Study. J. Acad. Nutr. Diet. 2021;121:2177–2186. doi: 10.1016/j.jand.2021.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Lachat C., Hawwash D., Ocké M.C., Berg C., Forsum E., Hörnell A., Larsson C.L., Sonestedt E., Wirfält E., Åkesson A., et al. Strengthening the Reporting of Observational Studies in Epidemiology-Nutritional Epidemiology (STROBE-nut): An Extension of the STROBE Statement. PLoS Med. 2016;13:e1002036. doi: 10.1371/journal.pmed.1002036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Australian Bureau of Statistics (ABS) Australian Burden of Disease Study 2015: Dietary Risk Factors. ABS; Canberra, Australia: 2020. [(accessed on 20 July 2022)]. Available online: https://www.aihw.gov.au/reports/burden-of-disease/interactive-data-risk-factor-burden/contents/dietary-risk-factors. [Google Scholar]
- 20.Booth S., Begley A., Mackintosh B., Kerr D.A., Jancey J., Caraher M., Whelan J., Pollard C.M. Gratitude, resignation and the desire for dignity: Lived experience of food charity recipients and their recommendations for improvement, Perth, Western Australia. Public Health Nutr. 2018;21:2831–2841. doi: 10.1017/S1368980018001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lindberg R., Lawrence M., Caraher M. Kitchens and pantries—Helping or hindering? The perspectives of emergency food users in Victoria, Australia. J. Hunger. Environ. Nutr. 2017;12:26–45. doi: 10.1080/19320248.2016.1175397. [DOI] [Google Scholar]
- 22.McKenzie H.J., McKay F.H. Food as a discretionary item: The impact of welfare payment changes on low-income single mother’s food choices and strategies. J. Poverty Soc. Justice. 2017;25:35–48. doi: 10.1332/175982716X14822521840954. [DOI] [Google Scholar]
- 23.Ramsey R., Giskes K., Turrell G., Gallegos D. Food insecurity among adults residing in disadvantaged urban areas: Potential health and dietary consequences. Public Health Nutr. 2012;15:227–237. doi: 10.1017/S1368980011001996. [DOI] [PubMed] [Google Scholar]
- 24.Elsahoryi N., Al-Sayyed H., Odeh M., McGrattan A., Hammad F. Effect of COVID-19 on food security: A cross-sectional survey. Clin. Nutr. ESPEN. 2020;40:171–178. doi: 10.1016/j.clnesp.2020.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thomas M.K., Lammert L.J., Beverly E.A. Food Insecurity and its Impact on Body Weight, Type 2 Diabetes, Cardiovascular Disease, and Mental Health. Curr. Cardiovasc. Risk Rep. 2021;15:15. doi: 10.1007/s12170-021-00679-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vercammen K.A., Moran A.J., McClain A.C., Thorndike A.N., Fulay A.P., Rimm E.B. Food Security and 10-Year Cardiovascular Disease Risk Among U.S. Adults. Am. J. Prev. Med. 2019;56:689–697. doi: 10.1016/j.amepre.2018.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Browne N.T., Cuda S.E. Nutritional and activity recommendations for the child with normal weight, overweight, and obesity with consideration of food insecurity: An Obesity Medical Association (OMA) Clinical Practice Statement 2022. Obes. Pillars. 2022;2:100012. doi: 10.1016/j.obpill.2022.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Temple J.B., Booth S., Pollard C.M. Social Assistance Payments and Food Insecurity inAustralia: Evidence from the HouseholdExpenditure Survey. Int. J. Environ. Res. Public Health. 2019;16:455. doi: 10.3390/ijerph16030455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Landrigan T.J., Kerr D.A., Dhaliwal S.S., Savage V., Pollard C.M. Removing the Australian tax exemption on healthy food adds food stress to families vulnerable to poor nutrition. Aust. N. Z. J. Public Health. 2017;41:591–597. doi: 10.1111/1753-6405.12714. [DOI] [PubMed] [Google Scholar]
- 30.Lee A.J., Kane S., Ramsey R., Good E., Dick M. Testing the price and affordability of healthy and current (unhealthy) diets and the potential impacts of policy change in Australia. BMC Public Health. 2016;16:315. doi: 10.1186/s12889-016-2996-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carey R., Caraher M., Lawrence M., Friel S. Opportunities and challenges in developing a whole-of-government national food and nutrition policy: Lessons from Australia’s National Food Plan. Public Health Nutr. 2016;19:3–14. doi: 10.1017/S1368980015001834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Public Health Association of Australia, Heart Foundation, Dietitians Australia, Red Cross, Indigenous Allied Health Australia, Victorian Aboriginal Community Controlled Health Organisation Joint Policy Statement on: Food Security for Aboriginal & Torres Strait Islander Peoples. 2019. [(accessed on 10 September 2022)]. Canberra. Available online: https://www.phaa.net.au/documents/item/3824.
- 33.McKechnie R., Turrell G., Giskes K., Gallegos D. Single-item measure of food insecurity used in the National Health Survey may underestimate prevalence in Australia. Aust. N. Z. J. Public Health. 2018;42:389–395. doi: 10.1111/1753-6405.12812. [DOI] [PubMed] [Google Scholar]
- 34.Beacom E., Furey S., Hollywood L., Humphreys P. Investigating food insecurity measurement globally to inform practice locally: A rapid evidence review. Crit. Rev. Food Sci. Nutr. 2021;61:3319–3339. doi: 10.1080/10408398.2020.1798347. [DOI] [PubMed] [Google Scholar]
- 35.Bastian A., Parks C., McKay F.H., van der Pligt P., Yaroch A., McNaughton S.A., Lindberg R. Development of a Comprehensive Household Food Security Tool for Families with Young Children and/or Pregnant Women in High Income Countries. Int. J. Environ. Res. Public Health. 2022;19:10543. doi: 10.3390/ijerph191710543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Subar A.F., Freedman L.S., Tooze J.A., Kirkpatrick S.I., Boushey C., Neuhouser M.L., Thompson F.E., Potischman N., Guenther P.M., Tarasuk V., et al. Addressing Current Criticism Regarding the Value of Self-Report Dietary Data. J Nutr. 2015;145:2639–2645. doi: 10.3945/jn.115.219634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Freedman L.S., Commins J.M., Moler J.E., Willett W., Tinker L.F., Subar A.F., Spiegelman D., Rhodes D., Potischman N., Neuhouser M.L., et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake. Am. J. Epidemiol. 2015;181:473–487. doi: 10.1093/aje/kwu325. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available from the Australian Bureau of Statistics.