Abstract
Background:
Life expectancy in the US has declined since 2014, but characterization of disparities within and across metropolitan areas of the country is lacking.
Methods:
Using census tract-level life expectancy from the 2010–2015 US Small-area Life Expectancy Estimates Project, we calculate ten measures of total and income-based disparities in life expectancy at birth, age 25, and age 65 within and across 377 Metropolitan Statistical Areas (MSAs) of the US.
Results:
We found wide heterogeneity in disparities in life expectancy at birth across MSAs and regions: MSAs in the West show the narrowest disparities (absolute disparity: 8.7 years, relative disparity: 1.1), while MSAs in the South (absolute disparity:9.1 years, relative disparity: 1.1) and Midwest (absolute disparity: 9.8 years, relative disparity: 1.1) have the widest life expectancy disparities. We also observed greater variability in life expectancy across MSAs for lower income census tracts (coefficient of variation [CoV] 3.7 for first vs tenth decile of income) than for higher income census tracts (CoV 2.3). Finally, we found that a series of MSA-level variables, including larger MSAs and greater proportion college graduates, predicted wider life expectancy disparities for all age groups.
Conclusions:
Sociodemographic and policy factors likely help explain variation in life expectancy disparities within and across metro areas.
Keywords: social inequalities, health disparities, urban health, life expectancy, US
Introduction
Life expectancy in the United States has declined since 2014, after several decades of continuous increases(1). Disparities in mortality between non-Hispanic whites and non-Hispanic Blacks have increased across the country(2, 3), despite decreasing life expectancy disparities the previous two decades(4). These racial disparities in mortality, as well as disparities by socioeconomic status and geography(4, 5), are a persistent feature of the US epidemiologic map. Even in the years of overall increasing life expectancy (1969 to 2013), the average improvements(6) obscured substantial heterogeneity in life expectancy and mortality between states(7), counties(8–10) cities(11–15), racial-ethnic groups(4), occupations(16), and education(16–18). These unequal, and unjust, short life spans are produced by the inequitable distribution of resources due to income inequality, structural racism, environmental injustice, differential access to health care, and state and local policies(19, 20).
There is also evidence of substantial spatial heterogeneity in health. Studies have found disparities in life expectancy, when measured at the region, state, county, city, or neighborhood level, or when measuring multiple levels of geography simultaneously(11–13, 21–24). Boing et al., found a 13-year difference in life expectancy between the 5th and 95th percentile U.S. census tracts(22), while Purtle et al. found that mean life expectancy was 4.8 (Standard Deviation (SD)=1.3) years longer in census tracts in the top household income (MHI) quartile compared to those in the bottom quartile in 745 US cities(11). Some paradigmatic examples of within-city inequalities include the 2 miles and 8 life expectancy years that separate the Upper West Side and East Harlem in NYC; in Chicago the life expectancy gap in neighboring Hyde Park and Washington Park is 13 years(25); neighborhoods separated by one subway stop in London on the Jubilee subway line have a 10-year disparity in life expectancy(26); and sub-city units in Santiago de Chile and Panama have up to 15 years difference in life expectancy(23).
However, to our knowledge, there is no characterization of how disparities in life expectancy vary across all metropolitan areas of the US since 2000, or factors associated with larger or smaller disparities within metropolitan areas. Metropolitan statistical areas (MSAs) represent metropolitan core and adjacent areas with substantial economic and social integration and are useful aggregations of areas within and across states. While prior research has examined life expectancy disparities at the city-level(11–13), MSAs include suburban areas, and increasing poverty and racial diversity in the suburbs(27) have substantially shifted patterns of residential racial and economic segregation between urban and suburban areas in the past 30 years, impacting population health and potentially life expectancy disparities(28, 29).
The primary objectives of this study were to: 1) characterize disparities in life expectancy within metropolitan areas in the US in 2010–2015, a period of increasing disparities after decades of decline, using publicly available data, and 2) measure the association between metropolitan area-level features and the magnitude of disparities. Quantifying the various measures of life expectancy disparities improves our understanding of place effects on health, illuminates patterns of disparities in a period of shifting life expectancy disparities, and lends itself to further research identifying policies, practices, and population characteristics that impact these disparities.
Methods
Study Setting and Outcome
We obtained life expectancy data for 2010–2015 from the US Small-area Life Expectancy Estimates Project (USALEEP)(30) and income and population data from the American Community Survey (ACS) 2011–2015 5-year estimates (Table S1901 and B01001). We used data on all census tracts in the US contiguous states with available life expectancy and that belonged to a core-based statistical area (CBSA) of the metropolitan type, usually called Metropolitan Statistical Areas (MSAs). MSAs are geographically defined labor markets based on core population agglomerations, and a geographic approximation of urban areas. We use census tracts as proxies for neighborhoods.
Outcome
The primary outcome of this study was life expectancy at birth, defined as the average years a person born today is expected to live if current mortality patterns hold constant. We also include life-expectancy estimates at ages 25 and 65. We divide life expectancy estimates into these groups because previous literature has shown that life-expectancy disparities can vary across the age distribution and that life expectancy at birth is highly sensitive to infant mortality(31); these age groups also allow us to estimate life expectancy conditional on surviving to working age and to older ages(32). Life expectancy point estimates and standard errors were calculated by the USALEEP project using abridged period life tables for the 48 contiguous US states. Age-specific mortality rates were estimated using a combination of geocoding, ACS, and census-data linkage, and standard demographic techniques and statistical modeling. Further details are available elsewhere(30).
Predictors
We obtained data on census tract-level median household income from the 2011–2015 ACS. We categorized census tracts by deciles of median household income within each MSA, similar to the approach by Chetty et al(33). We standardize median household income within MSA because of substantial variation in income by MSA, but also include an alternative specification that does not standardize within MSAs. We also categorized MSAs according to the census region where most of the MSA population resides; we include region because life expectancy varies dramatically by region(34).
We additionally include data on several potential MSA-level predictors of MSA-level disparities from the 2011–2015 ACS: median household income, population size, percent non-Hispanic Black, percent Hispanic, percent foreign born, percent population aged 25 plus with a college education, percent aged less than 65 without insurance, percent poverty, percent housing burdened (spend >30% of income on rent or mortgage), and two versions of the dissimilarity index comparing 1) non-Hispanic Black to non-Hispanic white populations and 2) Hispanic to non-Hispanic white populations. Last, we calculated the percent unemployed between 2010 and 2015 using data from the Bureau of Labor Statistics.
Statistical Analysis
For each MSA, we computed several measures of disparities. Different disparity (or inequality) measures can often lead to different interpretations of the same data, and selection between measures carries several value-laden decisions(35). To provide a comprehensive picture of disparities, we computed a total of 10 measures of disparity(36). First, five measures of total disparity that evaluate the overall distribution of census-tract level life expectancy without regard to income: difference and ratio between top and bottom deciles, coefficient of variation (CoV), Gini, and mean log deviation. Second, five measures of social group disparities that use census tract median household income to calculate income-based life expectancy inequities: top-bottom gaps and ratios(36), between-group variance, slope index of inequality, and relative index of inequality (37). A full list of computed measures, how to calculate the measure, and key attributes of the measures can be found in Appendix eTable 1.
In this report we focus on two measures of absolute and relative disparities: the difference or ratio of life expectancy between the 90th and 10th population-weighted percentiles of census tract life expectancy in each MSA. Decisions to incorporate the size of groups also involve ethical decisions about how much weight to give to individuals within subpopulations or social groups(37). We weight the 90/10 difference and ratio disparity measures by population to account for differences in census tract and MSA population sizes(37), which allows us to count individuals within census tracts and MSAs equally. We selected the top vs bottom decile differences and ratios from the possible 10 measures for two reasons: 1) inferences did not differ substantially by measure (see Pearson correlations between measures, Appendix eFigure 1) so presenting all measures in the main article would be redundant, and 2) these two measures are most intuitive and easy to understand and widely used in disparities analysis(35). Presenting these simpler measures is preferred, if more complex measures do not substantially improve or change inferences about the disparity. We present both absolute and relative disparities because measures in different scales provide complementary information on the magnitude of a disparity, particularly when monitoring disparities over time or across spatial units(35, 37). To provide full visibility into the various measures, we also include results using the other eight measures in the online interactive dashboard (38) We also calculated the absolute and relative disparity and CoV for each census region, by pooling all MSAs in the same region.
To account for the uncertainty in each life expectancy estimate, we propagated the uncertainty by resampling the estimates 100 times based on their mean and standard error, assuming a normal distribution. Then, for each iteration and MSA, we estimated the life expectancy disparity measures, and then found the median, 2.5 percentile and 97.5 percentile estimate for each disparity measure. We present the median estimates in all figures and include the 2.5 and 97.5 percentile estimates in the Table (and online dashboard).
Table:
Univariable analysis of MSA characteristics and differences in the size of the absolute disparity in life expectancy at birth
| Predictor | Standard Deviation | Change in Mean Total Life Expectancy Disparity (95% CI) N=377 |
R-Squared |
|---|---|---|---|
| Population Sizea | NA | 0.32 (0.15;0.5) | 4.4% |
| Median Household Incomea | NA | 0.51 (−0.68;1.7) | 0.3% |
| Percent housing burdened | 5.3% | −0.06 (−0.26;0.14) | 0.2% |
| Percent college graduate | 8.1% | 0.28 (0.06;0.49) | 2.9% |
| Percent uninsured | 5.1% | −0.13 (−0.33;0.07) | 0.7% |
| Percent poverty | 4.1% | 0.01 (−0.2;0.22) | 0.1% |
| Percent unemployed | 2.3% | −0.14 (−0.36;0.08) | 0.9% |
| Percent foreign-born | 6.6% | 0.03 (−0.16;0.22) | 0.1% |
| Percent Hispanic | 16.% | −0.09 (−0.29;0.1) | 0.4% |
| Percent non-Hispanic Black | 11% | 0.28 (0.08;0.48) | 2.9% |
| Dissimilarity: Hispanic and NH-White | 0.09 | 0.22 (0.03;0.42) | 1.9% |
| Dissimilarity: NH-Black and NH White | 0.10 | 0.35 (0.15;0.55) | 4.5% |
| Region | - | 5.1% | |
| West | 0 (Ref) | ||
| Midwest | NA | 1.0 (0.42;1.6) | |
| South | NA | 0.33 (−0.18;0.85) | |
| Northeast | NA | 0.24 (−0.43;0.92) |
Footnote: N=377. Disparity calculated as absolute disparity: difference between 90th and 10th population-weighted percentiles of life expectancy for each city. Each variable was entered in a separate model.
Log of population and median household income.
Coefficient interpretation: a 10% larger population is associated with a 0.32*log(1.1)=0.032 years wider absolute disparity between tracts at the 90th and 10th percentile of life expectancy. West is reference group for region.
MSA=Metropolitan Statistical Area.
To explore associations between MSA-level characteristics and the magnitude of disparities, we ran MSA-level linear regression models with the P90-P10 difference (absolute disparity) as the outcome and the following MSA-level predictors (each in a separate model): population, MHI, non-Hispanic Black, percent Hispanic (log transformed), foreign born, college education, uninsurance, poverty, housing burdened, unemployed, non-Hispanic Black compared to non-Hispanic white dissimilarity index, Hispanic compared to non-Hispanic white dissimilarity index, and region (West as reference). We log-transformed total population and MHI and standardized all other continuous predictors. To propagate uncertainty around the estimation of life expectancy, we ran regressions separately for each sampled set of life expectancies, resulting in 100 slope estimates per model, which we pooled using Rubin’s formula.
We conducted all analyses in R v4.0.2 (39). All code and data are available here: https://github.com/usamabilal/LE_Income_Inequalities_City. A dashboard with interactive results is available here: https://drexel-uhc.shinyapps.io/LE_Income_Inequalities_City/.
Results
We included data from 55,306 census tracts and 377 MSAs in four census regions, where nearly 76% of the US population lives; 36% of the population was in the South, 24% in the West, 20% in the Midwest, and 20% in the Northeast. eFigure 1 shows the correlation between life expectancy disparity indicators for all MSAs. Total disparity measures were all highly correlated with each other (ρ> 0.80 in all cases). Total disparity measures were moderately correlated with social group disparities (ρ ranging from 0.57 to 0.77). Appendix eFigures 2 and 3 show the spatial distribution of absolute and relative disparities across all MSAs, and the dashboard includes the additional disparity measures. MSAs with the widest disparities were clustered in the South and Midwest, while very few of the MSAs with the largest disparities were in the West. eTable 2 shows the absolute and relative disparities (and their respective uncertainty bands) in life expectancy, for MSAs with >1 million people, sorted by the rank across absolute and relative disparities. Limiting our main analysis to MSAs with >1 million people allows for closer investigation of the largest MSAs in the country, though the interactive dashboard (Dashboard Table 1) includes the additional measures of disparities. The 10 MSAs with the widest disparities, except for one (Philadelphia), were in the South (4) or Midwest (5). While rank differed slightly by absolute or relative disparity, the top and bottom 10 MSAs were nearly the same using both metrics.
We found substantial variation in life expectancy within and between MSAs across the country (see Figure 1). We also found substantial variation in life expectancy within regions; across both absolute and relative measures of disparity, the region with the largest disparities was the Midwest (median absolute disparity: 9.8 years, relative disparity: 1.1), followed by the South (absolute disparity: 9.1 years, relative disparity: 1.1), then the Northeast (absolute disparity: 8.8 years, relative disparity: 1.1) and finally the West (absolute disparity:8.7 years, relative disparity: 1.1). While disparities were largest in the Midwest, the CoV of disparities was smallest in the Midwest for absolute disparities (12.9%), indicating limited variation in disparities between MSAs despite large disparities within MSAs. Appendix eFigure 4 repeats Figure 1 using top/bottom differences and ratios as well as the slope index of inequality and relative index of inequality (the additional measures are included in Dashboard Figure 1). Patterns are similar, with the widest disparities in the Midwest and narrowest in the West. Though the magnitudes of disparities differed slightly, with wider CVs and SDs using the social group disparity measures than the total disparity measures. Patterns did not differ substantively for other disparity measures and are available in the interactive dashboard. Appendix eFigure 5 repeats Figure 1 using life expectancy at ages 25 and 65. At age 25, relative life expectancy disparities were similar to disparities at birth. For life expectancy at age 65 compared to birth, absolute disparities were narrower than disparities at birth, while relative disparities were wider than at birth. The rank of disparities by region at age 65 also differed from the rank at birth; at age 65 the West had the widest absolute disparities, and second widest relative disparities, versus the lowest disparities at birth, and there was more limited variation between regions.
Figure 1:
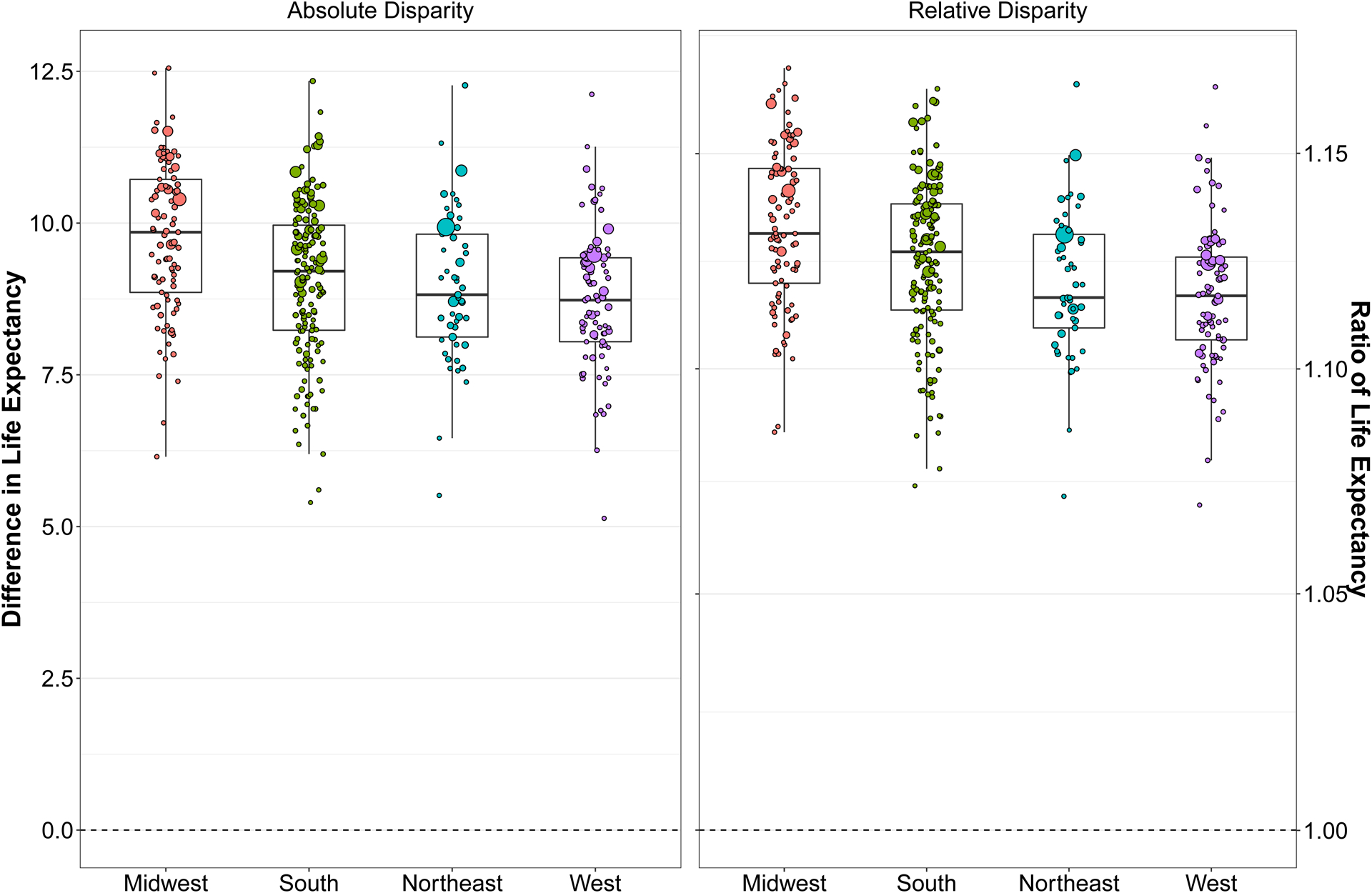
Absolute and Relative Life Expectancy Disparities in US MSAs
Footnote: Absolute Disparity: Difference between 90th and 10th population-weighted percentiles of life expectancy for each MSA; Relative Disparity: Ratio between the 90th vs 10th population-weighted percentiles of life expectancy for each MSA. Marker size is proportional to MSA population size.
Figure 2 characterizes differences in disparities by income, and shows mean, CoV, and standard deviation of life expectancy plotted against decile of census tract median household income, for all MSA’s (interactive figure available in Dashboard Figure 2). First, across all regions, life expectancy was higher in census tracts with higher median household income, with a disparity in life expectancy between the top vs bottom decile of income of 7.1 years. Second, variability across MSAs in life expectancy for census tracts at the lower end of the census tract income distribution contributed to the differences across MSAs in disparities in life expectancy between high- and low-income census tracts. Specifically, the overall variability in life expectancy in the first decile of census tract income was wider than at the tenth decile (standard deviation=2.7 and 1.8, and CoV=3.7 and 2.3 for first vs tenth decile of income, respectively). Third, disparities in life expectancy by census tract income varied by region, with the disparity in life expectancy between the top vs bottom decile of median household income varying from 5.7 years in the West, 6.9 in the Northeast, 7.3 in the South, and 7.9 in the Midwest. Appendix eFigure 6 repeats Figure 2 using median household income standardized across all MSAs rather than within MSAs, and shows similar patterns, though slightly narrower differences between regions. Appendix eFigure 7 repeats Figure 2 with life expectancy at ages 25 and 65; mean life expectancy remained higher in census tracts with higher median household income for life expectancy at ages 25 and 65, and regional patterns of variation remained consistent. The patterns of variability were similar at age 25 compared to at birth, with narrower standard deviations by median household income decile for age 65. On the other hand, we found a wider CoV for life expectancy at age 65 than at 25 or birth. The Table shows associations of MSA-level characteristics with disparities in life expectancy at birth. Several factors were associated with wider disparities: larger MSAs (mean difference in absolute disparity per 10% increase in population=0.032; CI: 0.015, 0.05), greater proportion college graduates (B per 1 SD increase=0.28; CI: 0.06; 0.49), and Non-Hispanic Black population (B=0.28, CI: 0.08, 0.48), and higher levels of Hispanic/White (B=0.22, CI:0.03, 0.42) and Non-Hispanic Black/White (B=0.35, CI: 0.15, 0.55) segregation. Disparities were narrower in the West than in the Midwest (Midwest: 1.02, CI: 0.42, 1.6), but similar to other regions. MSA-level disparities did not show an association with MSA-level median household income (B=0.51; CI: −0.68, 1.7), or proportion uninsured, in poverty, unemployed, housing burdened, foreign-born, or Hispanic. In Appendix eTable 2 we repeat the univariable analyses for life expectancy at age 25 and 65. Associations were similar for age 25. For age 65, we found that a greater number of variables explained a larger proportion of the variability in disparities compared to life expectancy at birth or age 25. For example, higher median household income explained 6% of the variability in disparities, proportion of college graduates 9%, and proportion of foreign-born individuals explained 7%.
Figure 2:
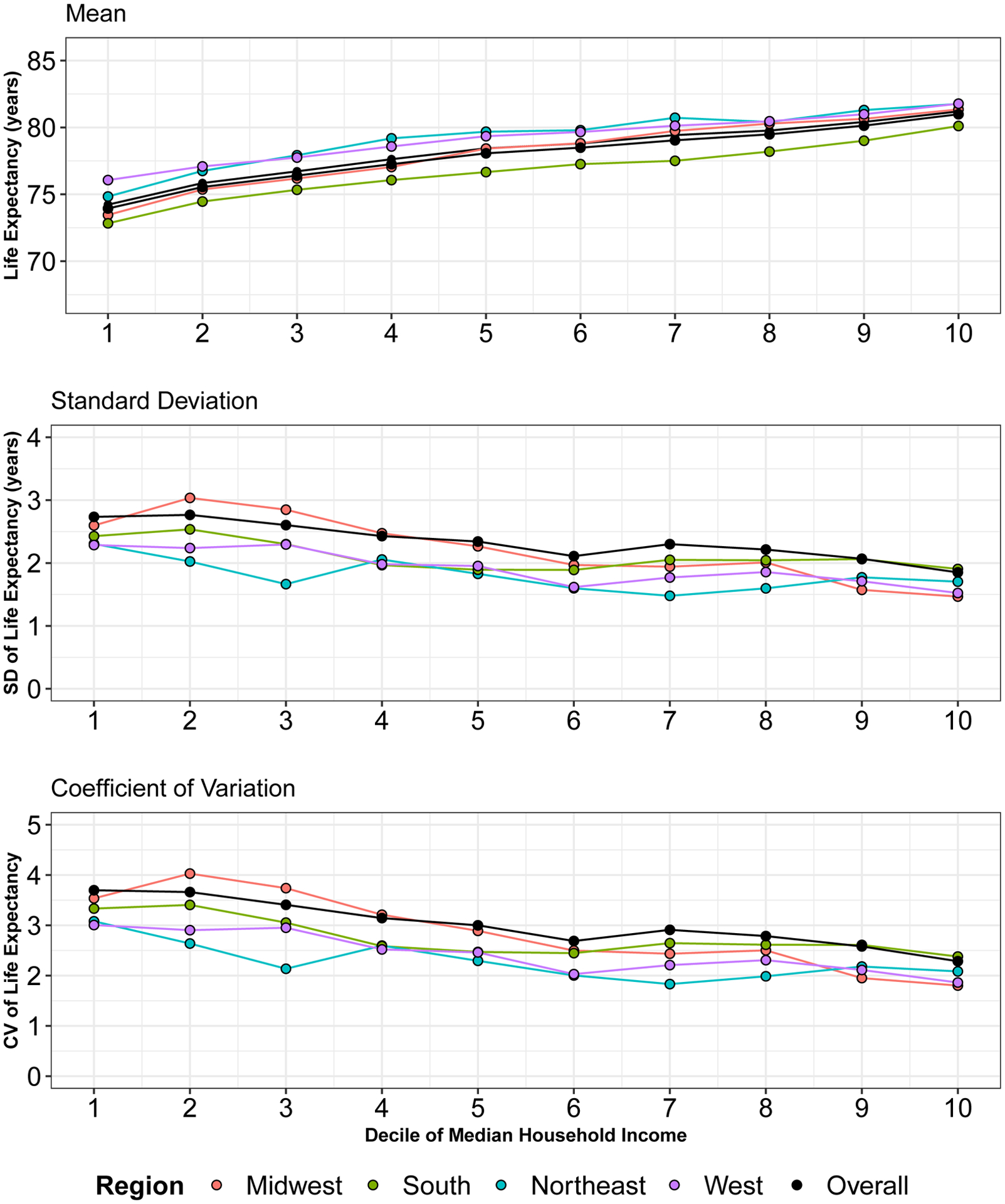
Mean, Standard Deviation, and Coefficient of Variation (CV) for life expectancy by tract median household income decile for each US MSA by region
Footnote: Median household income standardized within MSA.
Discussion
Our study examining life expectancy disparities across and within MSAs has four key findings. First, we found heterogeneity in disparities in life expectancy across MSAs and regions. Metropolitan areas in the Midwest had the widest life expectancy disparities while those in the West had the narrowest. In the Midwest and West, there were 9.8 and 8.7-year gaps in life expectancy, in the 90th versus 10th percentile census tracts. Second, we found a range of disparities between MSAs. While mean life expectancy monotonically increased with tract MHI across all regions, we observed greater variability across MSAs at lower income census tracts as compared to higher income ones. Third, MSA-level larger population size and higher proportion of college graduates were associated with wider disparities for life expectancy at birth, 25, and 65, while associations differed by age for other MSA-level factors. Fourth, patterns of life expectancy disparities at age 25 largely mirrored those at birth but differed for life expectancy at age 65 compared to life expectancy at birth: absolute disparities were narrower while relative disparities were wider, and there was more limited variation between regions.
Our finding of heterogeneous disparities across MSAs and regions is likely driven by a combination of the contextual features of places, the sociodemographic composition of residents of these areas, and the interaction between these contextual and sociodemographic characteristics(40). Populations in MSAs and regions differ by socioeconomic, demographic, and behavioral characteristics in ways that impact overall life expectancy and disparities in life expectancy, as suggested by other analysis(33), and our examination of various MSA-level factors. For example, we found wider life expectancy disparities in places with larger proportions of college graduates. Differences in contextual factors such as environmental exposures(41), deindustrialization(42), health care access(43), residential segregation(44), incarceration rates(42), differences in government expenditures(45), and social policies(19) are all associated with disparities in health and likely help explain MSA and regional differences in life expectancy. And finally, the interaction between sociodemographic and contextual characteristics of places likely help explain our findings(40). For example, economic decline and changing economic opportunities may create the context for both changing composition (declining middle class) and changing behaviors (greater substance dependence), which both may impact life expectancy(46).
We found clear patterns of wider disparities, for life expectancy at birth and at age 25, in MSAs in the South and Midwest compared to the Northeast and West, which may reflect regional- and state-level contextual differences in policies. MSAs represent both core areas and adjacent areas with substantial economic and social integration with the core, so are useful aggregations of areas within and across states. However, the political authority of metropolitan areas is limited, as they represent statistical aggregates of other units (counties and, if not consolidated, their respective cities). Therefore, there are few policies enacted directly at the MSA level (for example, minimum wage laws are enacted at the city or state level, and most medical insurance policy, such as Medicaid expansion or 1115 waivers, is enacted at the state level). However, designated market areas, also known as media markets, generally coincide or overlap with MSAs, and may impact exposure to health(47), which can impact life expectancy disparities. Additionally, metropolitan planning organizations, which are required for urban areas with more than 50,000 residents, enact policies at the metropolitan level. However, to our knowledge, the implications for health equity of metropolitan planning organizations policies have not been researched(48). Impacts of MSA level policy exposures on life expectancy disparities and disparities in other health outcomes warrant further attention.
In absence of MSA specific policies, we discuss how differences between regions may help explain the variability in disparities observed in our study. The South and Midwest, where we found lower average life expectancy and wider disparities in MSAs, respectively, and particularly in lower income census tracts, have increasingly enacted conservative policies that limit the social safety-net, while states and local governments in the West and Northeast have enacted policies targeting advancing equity and reducing disparities. States that implemented more conservative policies were more likely to experience declining life expectancy(19), while states controlled by Republican state legislatures(49) and states that spent less on social services(45) experienced higher infant mortality rates (potentially the most important determinant of lower life expectancy). Democrats are more likely to vote to support public health policies(50), and more progressive state and local governments have enacted social policies that benefit life expectancy, such as expanding Medicaid(51), or increasing the minimum wage(52), while more conservative governments have deregulated industry(19), and enacted policies limiting union power(53). These policies may be more impactful for life expectancy at birth and age 25, contributing to wider variation in disparities by region, versus at age 65 where policies tend to be set at the federal level (e.g. Medicare, Social Security)
Our finding of wider disparities in the Midwest is also consistent with other findings on racial–ethnic disparities. For example, Black infant mortality rates are also highest in the Midwest (54), while several midwestern states have a disproportionate contribution to the national Black–white life expectancy gap, especially due to injury-related mortality (55). Infant mortality is a key contributor to life expectancy at birth while injury-related deaths are more common in young adults, likely contributing to our observed wide disparities in life expectancy at birth and age 25, but not at age 65, in the Midwest. Larger per capita state budgets for maternal and child health (MCH) are associated with lower Black infant mortality rates, and the Midwest spends the least per capita on MCH (52). Cities and MSAs in conservative states have attempted to enact progressive policies, but state governments have used government preemption to increasingly limit local government’s ability to enact social policies which benefit health, particularly among low-income populations, and likely help explain regional disparities in mortality. Further research should investigate the role of specific state, MSA, and city-level social policies, as well as interactions between policies at these levels, in explaining life expectancy disparities, for example policies related to structural racism(56), or housing policy(57).
We found a consistent monotonic decrease in life expectancy with decreasing census tract level median household income. Lower census tract income may shape resident’s life expectancy via greater exposure to deleterious neighborhood conditions, including excess access to unhealthy foods and beverages(58), limited physical activity facilities or opportunities(59), greater exposure to air pollution(60), poor housing quality(61), and residential segregation(44). These disadvantageous neighborhood characteristics concentrate in low-income and racially segregated areas, creating a syndemic context, whereby multiple harmful exposures co-occur and enhance each other in neighborhoods and create multiple co-occurring health risks(62), ultimately impacting life-expectancy. Conversely the benefits of city living, such as proximate access to the most advanced health care(63) and low crime, may be only concentrated in high income(64) and majority white neighborhoods. Further, health related neighborhood selection may impact life expectancy by neighborhood median household income, where individuals with worse health may migrate (or be segregated) to lower-income neighborhoods(65), or individuals with better health may migrate to higher income neighborhoods(66), concentrating health by neighborhood income. Together, these features likely drive large disparities between low-and high-income areas within MSAs.
Our finding of greater variation between MSAs at low-income census tracts has been studied less frequently, though agrees with Chetty et al.(33), which showed wider variability by commuting zone in the life expectancy of individuals in lower-income households, but little variability in higher income households. Chetty et al found that life expectancy among low-income individuals was positively associated with proportion of immigrants (r = 0.72, P < .001), college graduates (r = 0.42, P < .001), and government expenditures (r = 0.57, P < .001). In this way, differences between MSAs at low-income levels may reflect differences in the composition of low-income census tracts by MSA. The wider variation at the 10th compared to the 90th decile of income, also may reflect the more limited possible variation at the upper limits of life expectancy, rather than contextual or compositional explanations. Variations in lifespan are usually driven by changes in earlier mortality(67). Alternatively, the differences may reflect differences in who is included in the lower income deciles, as there are differences in income distributions across MSAs. Another possible explanation is that variation in neighborhood features or neighborhood interventions may drive differences in life expectancy among low-income census tracts by MSA(68).
Life expectancy variability at birth and age 25 was wider in the Midwest in low-income neighborhoods, but shrank in higher-income areas, while in the South this variability persisted across income levels. The wide variability at low-income levels and lower average life expectancy in these two geographies, compared with the West and East coast, may be explained by policy differences as outlined above. The lack of variability at high income levels in the Midwest, but persistence of variability across income levels in the South, may be explained by compositional differences compared to the South; the South has a much larger Black population than the Midwest, and policies may have differential impacts by race and income, and we found wider disparities in MSAs with larger non-Hispanic Black populations. Racial disparities persist across socioeconomic status levels(69) and, for example, policies related to structural racism, including those that restrict the safety net(56), may adversely impact life expectancy among low-income white populations(70) but may impact Black Americans at all income levels. Future research should examine the differential mortality impacts of policies and laws that are explicitly or implicitly related to structural racism(56), by race and income.
Our findings regarding factors that are associated with disparities suggest that larger metro areas have larger life expectancy gaps. Larger cities have wider income inequality(64) (though income inequality does not fully explain life expectancy disparities(33)), likely because high-income jobs, earners, and the highest housing costs agglomerate in the largest cities(71), while also concentrating large proportions of low-income residents(72). Residents of large cities benefit from higher levels of innovation and productivity(71), higher mean earnings than smaller cities(64), greater availability of healthcare(73), and lower rates of noncommunicable disease(73). However, these benefits are distributed unequally, as the benefits of living in a city may be concentrated for high income residents(64) while the adverse impacts are concentrated for low-income residents and communities of color(74). We also found that MSAs with a higher proportion of non-Hispanic Black individuals and greater levels of racial–ethnic segregation have wider life expectancy disparities at birth, reinforcing these racialized patterns of inequity. Together these features of large MSAs predict longer life expectancy for high income and white residents(75), without commensurate life-expectancy benefits for low-income earners and communities of color, ultimately driving larger disparities in larger MSAs.
Strengths and Limitations
Our study has several strengths. To our knowledge, no previous studies have examined life expectancy disparities within and between MSAs across the United States. Our analysis reveals important variation in disparities that should spark further investigation into the causal factors producing variation in life expectancy between and within MSAs. Such analysis can help to identify effective interventions and policies to promote health and health equity. The disparities we examine occurred during a period in which racial disparities in life expectancy began increasing (2, 3), a reversal of decades of progress against disparities(4), and such disparities have been further exacerbated during the COVID-19 pandemic(76, 77), emphasizing the urgency of understanding and addressing these shifts in life expectancy disparities. Existing research points to differences in the composition of places as well as economic investment and implementation of social policies as important factors in reducing place-based disparities, but further research is needed to identify effective interventions and policies to promote health and health equity.
We also acknowledge some limitations. First, we leveraged a publicly available detailed census tract-level dataset to explore local-level variation in life expectancy between 2010–2015. The methodology employed by the NCHS improves upon prior approaches to calculating life expectancy for small areas, namely challenges due to small population sizes and missing age-specific death counts. However, because of lack of census population counts during the 2010–2015 period, the methodology uses population estimates from census-tract level ACS data, which may introduce additional bias(30). Moreover, as with other model-based small area estimates(78), we lack the ability to estimate the impact of policies on census tract life expectancy. Second, measures of disparities can differ substantially in magnitude, direction, and rate of change, producing drastically different insights about whether and how a disparity has changed over time(35, 36). However, we found consistent patterns of disparities across measures. Third, our measure of life expectancy was purely cross-sectional, aggregated across a five-year period, so we could not measure changes in disparities. Fourth, we conduct univariable analysis to describe differences in life expectancy disparities by MSA, but these associations should not be interpreted as causal. Future research could leverage longitudinal data to examine potential causal determinants of disparities by MSA. Fifth, our analysis uses only one geographic definition (core based statistical areas, specifically MSAs). There are numerous alternative definitions and measures of urban and metropolitan areas, including census designated places, commuting zones, combined statistical areas, or even just counties. These definitions have implications, as they may include or exclude suburbs and exurbs. Given geographic differences in contextual (e.g. access to care (28)) and compositional factors (e.g. racial–ethnic demographics and income levels(79)) between suburban and urban areas, life expectancy disparities likely differ by city definition. Future research should consider repeating this analysis using alternative geographic definitions. If disaggregated census tract level life-expectancy data becomes available, this research should also be repeated with separate analysis for men and women, given sex differences in mortality, and by race–ethnicity, given large racial and ethnic mortality disparities by place(4). Additionally, the COVID-19 pandemic has aggravated patterns of already decreasing life expectancy, with larger decreases for racial and ethnic minorities(76), suggesting our analysis should be repeated once census tract life expectancy data is made available for 2020 and 2021.
Conclusion
In this study of census tract-level life expectancy estimates within and across metropolitan areas in the US in 2010–2015, we found wide variation in the magnitude of disparities in life expectancy, both total and income-related. Metropolitan areas in the South and Midwest had the largest disparities at birth and age 25, mostly driven by large differences between cities in life expectancy in low-income census tracts. Differences in local context and composition, and their reciprocal relationships, may be behind these disparities. Further political and economic investment in social policies at the local and regional level may help to reduce inequities in life expectancy.
Supplementary Material
Funding:
UB, PM, and ASM were supported by the Office of the Director of the National Institutes of Health under award number DP5OD26429, UB was supported by a Pilot Award from the Urban Health Collaborative, ASM was supported by the National Institute of Allergy and Infectious Diseases under award number K01AI168579-01, and PM was supported by the Cotswold Postdoctoral Fellowship, award number 284134. The funding agencies had no involvement in the study design; in the data collection, analyses or interpretation of data; in the writing of this work; or in the decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest: None
Data:
All code and data are available here: https://github.com/usamabilal/LE_Income_Inequalities_City
References
- 1.Harper S, Riddell CA, King NB. Declining life expectancy in the United States: missing the trees for the forest. Annual Review of Public Health. 2021; 42:381–403. [DOI] [PubMed] [Google Scholar]
- 2.Bilal U, Diez-Roux AV. Troubling trends in health disparities. New England Journal of Medicine. 2018; 378:1557–8. [DOI] [PubMed] [Google Scholar]
- 3.Arias E, Tejada-Vera B, Ahmad F. Provisional life expectancy estimates for January through June, 2020: National Vital Statistics System. February 2021.
- 4.Harper S, MacLehose RF, Kaufman JS. Trends in the black-white life expectancy gap among US states, 1990–2009. Health Affairs. 2014; 33:1375–82. [DOI] [PubMed] [Google Scholar]
- 5.Bosworth B Increasing disparities in mortality by socioeconomic status. Annual Review of Public Health. 2018; 39:237–51. [DOI] [PubMed] [Google Scholar]
- 6.Kim D The associations between US state and local social spending, income inequality, and individual all-cause and cause-specific mortality: the National Longitudinal Mortality Study. Preventive Medicine. 2016; 84:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boscoe FP. Persistent and extreme outliers in causes of death by state, 1999–2013. PeerJ. 2015; 3:e1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Mackenbach JP, van Lenthe FJ, et al. Inequalities in life expectancy among US counties, 1980 to 2014: temporal trends and key drivers. JAMA Internal Medicine. 2017; 177:1003–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray CJL, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Medicine. 2006; 3:e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wami W, Walsh D, Hennig BD, McCartney G, Dorling D, Galea S, et al. Spatial and temporal inequalities in mortality in the USA, 1968–2016. Health & Place. 2021; 70:102586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Purtle J, Joshi R, Lê-Scherban F, Henson RM, Diez Roux AV. Linking Data on Constituent Health with Elected Officials’ Opinions: Associations Between Urban Health Disparities and Mayoral Officials’ Beliefs About Health Disparities in Their Cities. The Milbank Quarterly. 2021; 99:794–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fenelon A, Boudreaux M. Life and death in the American City: men’s life expectancy in 25 major American cities from 1990 to 2015. Demography. 2019; 56:2349–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benjamins MR, Silva A, Saiyed NS, De Maio FG. Comparison of all-cause mortality rates and inequities between black and white populations across the 30 most populous US cities. JAMA Network Open. 2021; 4:e2032086–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benjamins MR, Saiyed N, Bunting S, Lorenz P, Hunt B, Glick N, et al. HIV mortality across the 30 largest US cities: assessing overall trends and racial inequities. AIDS care. 2021:1–10. [DOI] [PubMed] [Google Scholar]
- 15.Schober DJ, Hunt BR, Benjamins MR, Saiyed NS, Silva A, De Maio FG, et al. Homicide mortality inequities in the 30 biggest cities in the US. American Journal of Preventive Medicine. 2021; 60:327–34. [DOI] [PubMed] [Google Scholar]
- 16.Singh GK, Lee H. Marked disparities in life expectancy by education, poverty level, occupation, and housing tenure in the United States, 1997–2014. International Journal of Maternal and Child Health and AIDS. 2021; 10:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Affairs. 2012; 31:1803–13. [DOI] [PubMed] [Google Scholar]
- 18.Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Affairs. 2008; 27:350–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montez JK, Beckfield J, Cooney JK, Grumbach JM, Hayward MD, Koytak HZ, et al. US state policies, politics, and life expectancy. The Milbank Quarterly. 2020; 98:668–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017; 389:1453–63. [DOI] [PubMed] [Google Scholar]
- 21.Kim R, Subramanian S. What’s wrong with understanding variation using a single-geographic scale? A multilevel geographic assessment of life expectancy in the United States. Procedia Environmental Sciences. 2016; 36:4–11. [Google Scholar]
- 22.Boing AF, Boing AC, Cordes J, Kim R, Subramanian S. Quantifying and explaining variation in life expectancy at census tract, county, and state levels in the United States. Proceedings of the National Academy of Sciences. 2020; 117:17688–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bilal U, Alazraqui M, Caiaffa WT, Lopez-Olmedo N, Martinez-Folgar K, Miranda JJ, et al. Inequalities in life expectancy in six large Latin American cities from the SALURBAL study: an ecological analysis. The Lancet Planetary Health. 2019; 3:e503–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bilal U, Hessel P, Perez-Ferrer C, Michael YL, Alfaro T, Tenorio-Mucha J, et al. Life expectancy and mortality in 363 cities of Latin America. Nature Medicine. 2021; 27:463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tavernise S, Sun A. Same city, but very different life spans. New York Times. 2015. [Google Scholar]
- 26.Cheshire J Featured graphic. Lives on the line: mapping life expectancy along the London Tube network. Environment and Planning A. 2012; 44:1525–8. [Google Scholar]
- 27.Allard SW. Places in Need: The Changing Geography of Poverty: Russell Sage Foundation; 2017.
- 28.Schnake-Mahl AS, Sommers BD. Health Care In The Suburbs: An Analysis Of Suburban Poverty And Health Care Access. Health Affairs. 2017; 36:1777–85. [DOI] [PubMed] [Google Scholar]
- 29.Schnake-Mahl AS, Jahn JL, Subramanian S, Waters MC, Arcaya M. Gentrification, neighborhood change, and population health: a systematic review. Journal of Urban Health. 2020; 97:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arias E, Escobedo LA, Kennedy J, Fu C, Cisewski JA. US small-area life expectancy estimates project: methodology and results summary. Vital Health Statistics 2. 2018; 181:1–40. [PubMed] [Google Scholar]
- 31.Anderson NW, Zimmerman FJ. Trends in health equity in mortality in the United States, 1969–2019. SSM-Population Health. 2021; 16:100966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crimmins EM, Zhang YS. Aging populations, mortality, and life expectancy. Annual Review of Sociology. 2019; 45:69–89. [Google Scholar]
- 33.Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA : the Journal of the American Medical Association. 2016; 315:1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farina MP, Zajacova A, Montez JK, Hayward MD. US state disparities in life expectancy, disability-free life expectancy, and disabled life expectancy among adults aged 25 to 89 years. American Journal of Public Health. 2021; 111:708–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harper S, King NB, Meersman SC, Reichman ME, Breen N, Lynch J. Implicit value judgments in the measurement of health inequalities. The Milbank Quarterly. 2010; 88:4–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harper S, Lynch J. Methods for measuring cancer disparities: using data relevant to healthy people 2010 cancer-related objectives. Bethesda, MD: National Cancer Institute 2005 Contract No.: NIH Publication No. 05–5777. [Google Scholar]
- 37.Harper S, Lynch J. Health inequalities: measurement and decomposition. In: Oakes JM, JS K, editors. Methods in social epidemiology. Second Edition ed. San Francisco: Josey-Bass; 2006. p. 91–131. [Google Scholar]
- 38.Schnake-Mahl AS, Mullachery PH, Purtle J, Li R, Diez Roux AV, Bilal U. Online Interactive Dashboard. 2022; Available from: https://drexel-uhc.shinyapps.io/LE_Income_Inequalities_City/.
- 39.Team RC. R: A lnaguage and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Australia, 2021. [Google Scholar]
- 40.Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing ‘place’in health research: a relational approach. Social Science & Medicine. 2007; 65:1825–38. [DOI] [PubMed] [Google Scholar]
- 41.Correia AW, Pope III CA, Dockery DW, Wang Y, Ezzati M, Dominici F. The effect of air pollution control on life expectancy in the United States: an analysis of 545 US counties for the period 2000 to 2007. Epidemiology (Cambridge, Mass). 2013; 24:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nosrati E, Ash M, Marmot M, McKee M, King LP. The association between income and life expectancy revisited: deindustrialization, incarceration and the widening health gap. International Journal of Epidemiology. 2018; 47:720–30. [DOI] [PubMed] [Google Scholar]
- 43.Bhatt CB, Beck-Sagué CM. Medicaid expansion and infant mortality in the United States. American Journal of Public Health. 2018; 108:565–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001; 116:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goldstein ND, Palumbo AJ, Bellamy SL, Purtle J, Locke R. State and local government expenditures and infant mortality in the United States. Pediatrics. 2020; 146:e20201134. [DOI] [PubMed] [Google Scholar]
- 46.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences. 2015; 112:15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim E, Shepherd ME, Clinton JD. The effect of big-city news on rural America during the COVID-19 pandemic. Proceedings of the National Academy of Sciences. 2020; 117:22009–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nelson AC, Sanchez TW, Wolf JF, Beth Farquhar M. Metropolitan planning organization voting structure and transit investment bias: Preliminary analysis with social equity implications. Transportation Research Record. 2004; 1895:1–7. [Google Scholar]
- 49.Rodriguez JM, Geronimus AT, Bound J, Wen R, Kinane CM. Partisan Control of US State Governments: Politics as a Social Determinant of Infant Health. American Journal of Preventive Medicine. 2021; 62:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Purtle J, Goldstein ND, Edson E, Hand A. Who votes for public health? US senator characteristics associated with voting in concordance with public health policy recommendations (1998–2013). Social Science & Medicine- Population Health. 2017; 3:136–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Miller S, Johnson N, Wherry LR. Medicaid and mortality: new evidence from linked survey and administrative data. The Quarterly Journal of Economics. 2021; 136:1783–829. [Google Scholar]
- 52.Van Dyke ME, Komro KA, Shah MP, Livingston MD, Kramer MR. State-level minimum wage and heart disease death rates in the United States, 1980–2015: A novel application of marginal structural modeling. Preventive Medicine. 2018; 112:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eisenberg‐Guyot J, Mooney SJ, Hagopian A, Barrington WE, Hajat A. Solidarity and disparity: declining labor union density and changing racial and educational mortality inequities in the United States. American Journal of Industrial Medicine. 2020; 63:218–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kandasamy V, Hirai AH, Kaufman JS, James AR, Kotelchuck M. Regional variation in Black infant mortality: The contribution of contextual factors. Plos One. 2020; 15:e0237314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Riddell CA, Morrison KT, Kaufman JS, Harper S. Trends in the contribution of major causes of death to the black-white life expectancy gap by US state. Health & Place. 2018; 52:85–100. [DOI] [PubMed] [Google Scholar]
- 56.Agénor M, Perkins C, Stamoulis C, Hall RD, Samnaliev M, Berland S, et al. Developing a Database of Structural Racism–Related State Laws for Health Equity Research and Practice in the United States. Public Health Reports. 2021:0033354920984168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Purtle J, Gebrekristos LT, Keene D, Schlesinger P, Niccolai L, Blankenship KM. Quantifying the restrictiveness of local housing authority policies toward people with criminal justice histories: United States, 2009–2018. American Journal of Public Health. 2020; 110:S137–S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Larson NI, Story MT, Nelson MC. Neighborhood Environments Disparities in Access to Healthy Foods in the US. American Journal of Preventive Medicine. 2009; 36:74–81. [DOI] [PubMed] [Google Scholar]
- 59.Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: a national study. American Journal of Public Health. 2006; 96:1676–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hajat A, Diez-Roux AV, Adar SD, Auchincloss AH, Lovasi GS, O’Neill MS, et al. Air pollution and individual and neighborhood socioeconomic status: evidence from the Multi-Ethnic Study of Atherosclerosis (MESA). Environmental Health Perspectives. 2013; 121:1325–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ellen IG, Glied S. Housing, Neighborhoods, and Children’s Health. The Future of Children. 2015:135–53. [Google Scholar]
- 62.Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- 63.Arcaya MC, Schnake-Mahl A. Health in the Segregated City. The Dream Revisited: Columbia University Press; 2019. p. 165–8. [Google Scholar]
- 64.Heinrich Mora E, Heine C, Jackson JJ, West GB, Yang VC, Kempes CP. Scaling of urban income inequality in the USA. Journal of the Royal Society Interface. 2021; 18:20210223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arcaya MC, Subramanian S, Rhodes JE, Waters MC. Role of health in predicting moves to poor neighborhoods among Hurricane Katrina survivors. Proceedings of the National Academy of Sciences. 2014; 111:16246–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Green MA, Subramanian S, Vickers D, Dorling D. Internal migration, area effects and health: Does where you move to impact upon your health? Social Science & Medicine. 2015; 136:27–34. [DOI] [PubMed] [Google Scholar]
- 67.Aburto JM, Villavicencio F, Basellini U, Kjærgaard S, Vaupel JW. Dynamics of life expectancy and life span equality. Proceedings of the National Academy of Sciences. 2020; 117:5250–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Garvin EC, Cannuscio CC, Branas CC. Greening vacant lots to reduce violent crime: a randomised controlled trial. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. 2013; 19:198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychology. 2016; 35:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Metzl JM. Dying of whiteness: How the politics of racial resentment is killing America’s heartland: Hachette UK; 2019. [Google Scholar]
- 71.Glaeser EL, Gottlieb JD. The wealth of cities: Agglomeration economies and spatial equilibrium in the United States. Journal of Economic Literature. 2009; 47:983–1028. [Google Scholar]
- 72.Kneebone E The growth and spread of concentrated poverty, 2000 to 2008–2012. Washington DC: The Brookings Institution, 2014. [Google Scholar]
- 73.Rocha LE, Thorson AE, Lambiotte R. The non-linear health consequences of living in larger cities. Journal of Urban Health. 2015; 92:785–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Massey DS, Gross AB, Eggers ML. Segregation, the concentration of poverty, and the life chances of individuals. Social Science Research. 1991; 20:397–420. [Google Scholar]
- 75.Singh GK, Siahpush M. Widening rural–urban disparities in life expectancy, US, 1969–2009. American Journal of Preventive Medicine. 2014; 46:e19–e29. [DOI] [PubMed] [Google Scholar]
- 76.Woolf SH, Masters RK, Aron LY. Effect of the covid-19 pandemic in 2020 on life expectancy across populations in the USA and other high income countries: simulations of provisional mortality data. BMJ (Clinical research ed). 2021; 373:n1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Arias E, Tejada-Vera B, Ahmad F, Kochanek KD. Provisional Life Expectancy Estimates for 2020. Hyattsville, MD: National Center for Health Statistics, July 2021. [Google Scholar]
- 78.Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the behavioral risk factor surveillance system. American Journal of Epidemiology. 2015; 182:127–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Parker K, Horowitz JM, Brown A, Fry R, Cohn D, Igielnik R. What unites and divides urban, suburban and rural communities. Wshington, DC: Pew Research Center, May 22, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All code and data are available here: https://github.com/usamabilal/LE_Income_Inequalities_City


