Abstract
This study aims to estimating the prevalence of type 2 diabetes and prediabetes among adult from 30 to 69 years old and assess the association of risk factor with the conditions. A total of 5244 aged 30 to 69 years old were participated in this cross-sectional study, using nationally representative sampling frame. All participants were taking blood sample to measure fasting blood glucose level and 2-hour postload oral glucose tolerance test by National Hospital of Endocrinology, Vietnam. Multinomial logistic regressions with baseline-category logit models were conducted to identify factors associated with diabetes and prediabetes among respondents. The prediabetes prevalence was in 17.9% and diabetes in 7.3%. Patients who were male (reference group vs female OR = 0.79; 95% CI: 0.64, 0.97), in the 50 to 59 years old group (OR = 1.60; 95% CI: 1.28, 2.00), have hypertension and WHR risk have higher prevalence to have prediabetes (OR = 1.31; 95% CI: 1.12, 1.53; OR = 1.37; 95% CI: 1.11, 1.70, respectively). Male patients (reference group vs female OR = 0.62; 95% CI: 0.45, 0.84), patients who were in 40 to 49; 50 to 59; 60 to 69 years old, those who were housewife (OR = 2.17; 95% CI: 1.43, 3.28; OR = 2.85; 95% CI: 1.91, 4.27; OR = 3.12; 95% CI: 2.08, 4.69; OR = 1.71; 95% CI: 1.22, 2.40, respectively). Diabetes have significant associated with participants have hypertension (OR = 1.19; 95% CI: 1.72, 2.70). The common factor directly related to prediabetes and diabetes in both genders is age. Other factors directly associated with prediabetes and diabetes include BMI, WHR, hypertension, educational level, and job.
Keywords: associated factor, prediabetes, risk factor, type 2 diabetes
1. Introduction
Diabetes mellitus has become a major public health problem. Type-2 diabetes mellitus (T2DM) is a chronic disease characterized by high levels of sugar in the blood and used to start almost always in the middle- and late-adulthood. T2DM is the most prevalent form of diabetes, accounting for an estimated 95% of the global diabetic population.[1] There were 425 million people diagnosed with T2DM around the world in 2017.[1] It is predicted that the number of adults with T2DM will increase to 629 million by 2045.[1] T2DM causes approximately 12% of the economic burden from diabetes treatment and its complications.[2] Moreover, T2DM is also a major risk factor for cardiovascular diseases, which increases morbidity and mortality rates.[2]
In Vietnam, the prevalence of T2DM increased double in 10 years, from 2.7% in 2002 to 5.4% in 2012.[3] The national survey on the risk factors of non-communicable diseases (STEPS) Vietnam in 2015 reported there was a high increase in the rate of impaired fasting glucose (3.6%), and raised blood glucose (4.1%).[4] According to the International Diabetes Federation, the estimated number of Vietnamese people aged 20 to 79 with diabetes in 2019 was 3,779,600 cases.[5]
T2DM is affected by lifestyle that includes many risk factors. The consequences of diabetes can be reduced by determining and controlling the modifiable risk factors. A study in Pakistan in 2016 to 2017 showed that older age, family history of diabetes, hypertension, obesity, and dyslipidemia were associated with T2DM.[6] The National Health and Nutrition Examination Survey in Korea from 2005 to 2015 also showed similar results.[7] In addition, according to the 2019 American Association of Diabetes, there are several risk factors for type 2 diabetes, including body mass index (BMI) score, waist-hip ratio, and high blood pressure.[8]
The last comprehensive national survey to evaluate the prevalence of T2DM in Vietnam among people from 30 to 69 years old was implemented in 2012 by the National Hospital of Endocrinology of Vietnam in 6 ecological regions of Vietnam, which is too old.[4] The lack of such update information might lead to outdated and ineffective public health strategies to prevent diabetes. Therefore, we conducted this study to explore the T2DM prevalence and associated factors with T2DM in 2020/2021. The result will help evaluate the change and the trend of increasing T2DM in Vietnam. Moreover, the study finding also provides evidence for the Ministry of Health to operate policy and intervention plans to prevent T2DM in Vietnam.
2. Materials and Methods
2.1. Design and setting
This cross-sectional study was conducted in six areas (Red River Delta, Northwest – Northeast, North Central – South Central Coast, Central Highlands, Southeast, Mekong River Delta) and two major cities of Vietnam (Hanoi and Ho Chi Minh City), which cover national representative for Vietnamese population. All the participants will be randomly selected by local authorities from representative ward of each city/provinces.
2.2. Sampling and data collection
An equal number of participants was selected using the basic equation in random sampling: type I error rate = 0.05; P = 4.1% (Rate of fasting hyperglycemia according to the 2015 STEPS survey); relative marginal error ε = 20% and design effect = 2. Under these conditions, the minimum number of participants was 4494. Assuming the non-response rate of 15%, the final sample size needed was 5376. Among 5376 participants recruited, there were 132 peoples who were reject to participate. In final, our study had 5244 participants met the selection criteria and completed the entire questionnaire. The sample was collected stratified by gender and age groups (30–39, 40–49, 50–59, and 60–49 years old).
The inclusion criteria of this study were Vietnamese people from 30 to 69 years old, having the ability to answer the questionnaire verbally.
2.3. Variables
2.3.1. Outcome.
The primary outcome of this study was diabetes and pre-diabetes.
Participants visited the National Hospital of Endocrinology will attend the morning examination session for measurement of fasting plasma glucose (FPG) levels after fasting for at least 8 hours. Immediately after taking blood for the first fasting blood glucose test, the patient was given 75g of glucose (pure) mixed with 250 to 300 mL of purify water, the participants were asked to drink it all within 5 minutes. After exactly 120 minutes, the participants had a second blood glucose test by the medical staff to give the test results of 2-hour postload oral glucose tolerance test (OGTT). Diabetes was determined as FPG ≥ 7.0 mmol/L or OGTT ≥ 11.1 mmol/L. Prediabetes was defined as FPG of 5.6 to 6.9 mmol/L or a OGTT level of 7.8 to 11.1 mmol/L.[9]
2.3.2. Independent variables.
The independent variables included hypertension, waist circumference (WC), waist hip ratio (WHR), and BMI. Blood pressure measurements were performed with a standardized sphygmomanometer in the sitting position after 10 minutes of rest. Participant’s hypertension status also grouped into yes (blood pressure ≥ 140/90 mm Hg); and no.[10] WC was measured using a wire gauge at the midpoint between the lowest rib and the anterior iliac crest in the standing position. Large WC was grouped to yes (male ≥ 0.9 m and female ≥ 0.8 m); and no.[11] Hip circumference measurement was taken around the abdomen at the level of the umbilicus (belly button). WHR was categorized to yes; and no, with the cutoff for males was above 0.95 and females was above 0.8.[11]
Bodyweight was measured using a digital weight scale with participants wearing only underwear beneath the examination gown. Standing height was measured using a stadiometer with a fixed vertical backboard and adjustable headpiece. BMI was calculated as participant weight in kilograms divided by the square of height in meters. BMI was classified into 3 categories following the WHO criteria of BMI cutoff points for Asia-Pacific peoples: underweight (<18.5), normal (18.5–24.9), and overweight-obese (>25.0).[12]
2.3.3. Other covariates.
The survey was conducted in face-to-face interviews using a designed questionnaire. The questionnaire sought ‘participants’ information on their demographic, knowledge about diabetes, and hypertension history. The covariates included demographic information collected from the participants included: age, sex, residential area, education, and job.
2.4. Data analysis
Descriptive statistics were used to summarize the data, with frequencies and percentages for categorical variables and means with standard deviations (SD) or median with inter-quartile ranges (IQR) for quantitative variables. Multinomial logistic regressions with baseline-category logit models were conducted to identify factors associated with diabetes and prediabetes among respondents. A significant level of P < .05 was used for all statistical tests. All analyses were carried out using Stata v16 (Stata Corp, College Station, TX).
2.5. Ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethical Committee in Biomedical Research at the National Hospital of Endocrinology, No.308/QD-BVNTTW. All participants provided signed informed consent.
3. Results
A total of 5244 participants enrolled in the study, among them 17.9% have prediabetes and 7.3% have diabetes. Participant’s demographic characteristics are shown in Table 1. The mean age of participants was 49.62 ± 0.15 years. More than half of participants were female (52.0%) and finished secondary to high school. About 36.1% of male participants were farmers, and this prevalence among female was 37.7%. There were 23.7% overweight-obese and 6.6% underweight among male group, which is higher than the female group (19.9% overweight-obese and 5.0% underweight). WHR risk of male participants was lower than that of female participants was (20.2% vs 88.4%). The hypertension prevalence among male participant was 38.5% and among female were 26.8%. The proportions of male and female participants with prediabetes and diabetes were 7.2% and 6.4%, 6.2%, and 4.5%, respectively.
Table 1.
General information of participants by gender, data from a national survey on type 2 diabetes and prediabetes mellitus in Vietnam 2021.
| Factor | Male | Female |
|---|---|---|
| Total | n = 2514 | n = 2730 |
| Age groups | ||
| 30–39 | 590 (23.5) | 686 (25.1) |
| 40–49 | 612 (24.3) | 660 (24.2) |
| 50–59 | 646 (25.7) | 692 (25.3) |
| 60–69 | 666 (26.5) | 692 (25.3) |
| Location | ||
| Red River Delta | 377 (15.0) | 402 (14.7) |
| Northwest – Northeast | 342 (13.6) | 351 (12.9) |
| North Central – South Central Coast | 518 (20.6) | 569 (20.8) |
| Central Highlands | 158 (6.3) | 159 (5.8) |
| Southeast | 235 (9.3) | 253 (9.3) |
| Mekong River Delta | 446 (17.7) | 507 (18.6) |
| Hanoi – Ho Chi Minh City | 438 (17.4) | 489 (17.9) |
| Education | ||
| Primary school | 482 (19.2) | 685 (25.1) |
| Secondary – high school | 1519 (60.4) | 1555 (57.0) |
| University/college and higher | 513 (20.4) | 490 (17.9) |
| Jobs | ||
| Farmer | 907 (36.1) | 1028 (37.7) |
| Worker | 346 (13.8) | 160 (5.9) |
| Trade | 228 (9.1) | 367 (13.4) |
| Officer | 460 (18.3) | 418 (15.3) |
| Housewife | 103 (4.1) | 538 (19.7) |
| Unemployment | 38 (1.5) | 8 (0.3) |
| Others | 432 (17.2) | 211 (7.7) |
| History of family member have diabetes | 350 (13.9%) | 403 (14.8%) |
| BMI | ||
| Underweight | 167 (6.6) | 137 (5.0) |
| Normal | 1751 (69.6) | 2049 (75.1) |
| Overweight—obese | 596 (23.7) | 544 (19.9) |
| Waist circumference | ||
| No | 2024 (80.5) | 1614 (59.1) |
| Yes | 490 (19.5) | 1116 (40.9) |
| Waist hip ratio risk (Male > 0.95; Female > 0.8) | ||
| No | 2007 (79.8) | 318 (11.6) |
| Yes | 507 (20.2) | 2412 (88.4) |
| Hypertension | ||
| No | 1546 (61.5) | 1997 (73.2) |
| Yes | 968 (38.5) | 733 (26.8) |
| Blood glucose level | ||
| Normal | 1845 (73.4%) | 2080 (76.2%) |
| Prediabetes | 456 (18.1%) | 481 (17.6%) |
| Diabetes | 213 (8.5%) | 169 (6.2%) |
BMI = body mass index.
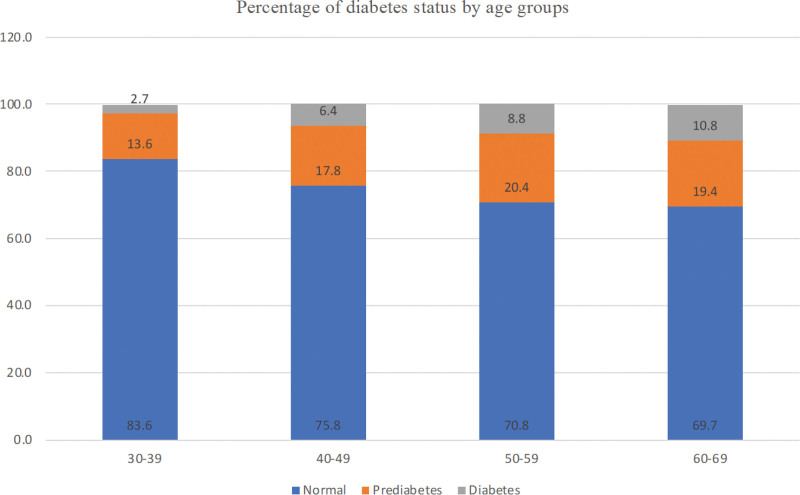
Figure 1 shows percentage of diabetes status among participants by age groups. The highest proportion of diabetes was in 60 to 69 age groups (10.8%), followed by 50 to 59 age groups (8.8%), 40 to 49 age groups (6.4%) and the lowest was in 30 to 39 (2.7%).
Figure 1.
Percentage of prediabetes and diabetes status by age groups, data from a national survey on type 2 diabetes and prediabetes mellitus in Vietnam 2021.
The association between several risk factors to diabetes status are summerized in Table 2. When analyze the BMI factor, among patients who have diabetes, there were 66% underweight, 5% normal and 29.1% overweight-obese; 56.5% have WHR risk (WHR > 0.95 in male and WHR > 0.8 in female); 53.7% have hypertension. Among patients who have pre-diabetes, 70.1% were underweight, 4.9% normal and 25% overweight-obese; 59.6% have WHR risk; 37.6% have hypertension.
Table 2.
Risk factors of prediabetes and diabetes, data from a national survey on type 2 diabetes and prediabetes mellitus in Vietnam 2021.
| Factor | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| Total | 3925 | 937 | 382 |
| Jobs | |||
| Farmer | 1474 (37.6) | 343 (36.6) | 118 (30.9) |
| Worker | 404 (10.3) | 74 (7.9) | 28 (7.3) |
| Trade | 468 (11.9) | 93 (9.9) | 34 (8.9) |
| Civil servants/office workers | 677 (17.2) | 156 (16.6) | 45 (11.8) |
| Housewife | 453 (11.5) | 120 (12.8) | 68 (17.8) |
| Unemployment | 32 (0.8) | 9 (1.0) | 5 (1.3) |
| Others | 417 (10.6) | 142 (15.2) | 84 (22.0) |
| History of family member have diabetes | 522 (13.3) | 144 (15.4) | 87 (22.8) |
| BMI | |||
| Underweight | 2891 (73.7) | 657 (70.1) | 252 (66.0) |
| Normal | 239 (6.1) | 46 (4.9) | 19 (5.0) |
| Overweight – obese | 795 (20.3) | 234 (25.0) | 111 (29.1) |
| Waist circumference | |||
| No | 2803 (71.4) | 609 (65.0) | 226 (59.2) |
| Yes | 1122 (28.6) | 328 (35.0) | 156 (40.8) |
| Waist hip ratio | |||
| No | 1780 (45.4) | 379 (40.4) | 166 (43.5) |
| Yes | 2145 (54.6) | 558 (59.6) | 216 (56.5) |
| Hypertension | |||
| No | 2781 (70.9) | 585 (62.4) | 177 (46.3) |
| Yes | 1144 (29.1) | 352 (37.6) | 205 (53.7) |
BMI = body mass index.
The multinomial logistic of factors that related to diabetes and prediabetes showed in Table 3. Participants who were male (reference group vs female OR = 0.79; 95% CI: 0.64, 0.97), in the 50 to 59 years old group (OR = 1.60; 95% CI: 1.28, 2.00) have higher odds of having prediabetes as compared to normal. Besides, prediabetes also correlated with patients who have hypertension and WHR risk (OR = 1.31; 95% CI: 1.12, 1.53; OR = 1.37; 95% CI: 1.11, 1.70, respectively).
Table 3.
Multinomial logistic of factors related to diabetes and prediabetes, data from a national survey on type 2 diabetes and prediabetes mellitus in Vietnam 2021.
| Factors | Prediabetes vs Normal | Diabetes vs Normal | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age groups | ||||||
| 30–39 | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| 40–49 | 1.36* | [1.09, 1.70] | .007 | 2.17** | [1.43, 3.28] | .000 |
| 50–59 | 1.60** | [1.28, 2.00] | .000 | 2.85** | [1.91, 4.27] | .000 |
| 60–69 | 1.47* | [1.17, 1.85] | .001 | 3.12** | [2.08, 4.69] | .000 |
| Gender | ||||||
| Male | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Female | 0.79* | [0.64, 0.97] | .025 | 0.62* | [0.45, 0.84] | .002 |
| Education (primary school) | ||||||
| Primary school | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Secondary – high school | 1.04 | [0.87, 1.25] | .666 | 0.83 | [0.65, 1.08] | .164 |
| University/college and higher | 0.86 | [0.64, 1.17] | .332 | 0.67 | [0.43, 1.04] | .076 |
| Jobs | ||||||
| Farmer | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Worker | 0.86 | [0.65, 1.14] | .290 | 1.03 | [0.66, 1.60] | .911 |
| Trade | 0.89 | [0.69, 1.15] | .385 | 1.05 | [0.70, 1.59] | .802 |
| Civil servants/office workers | 1.28 | [0.96, 1.72] | .096 | 1.36 | [0.85, 2.17] | .204 |
| Housewife | 1.06 | [0.83, 1.35] | .646 | 1.71* | [1.22, 2.40] | .002 |
| Unemployment | 1.14 | [0.53, 2.43] | .741 | 1.48 | [0.55, 3.97] | .437 |
| Others | 1.47* | [1.16, 1.85] | .001 | 2.43** | [1.77, 3.35] | .000 |
| History of family member have diabetes | ||||||
| No | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Yes | 1.19 | [0.97, 1.46] | .089 | 1.99** | [1.52, 2.60] | .000 |
| BMI | ||||||
| Normal | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Underweight | 0.90 | [0.64, 1.25] | .517 | 0.96 | [0.58, 1.59] | .871 |
| Overweight – obese | 1.15 | [0.95, 1.40] | .162 | 1.19 | [0.89, 1.58] | .235 |
| Hypertension risk | ||||||
| No | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Yes | 1.31** | [1.12, 1.53] | .001 | 2.16** | [1.72, 2.70] | .000 |
| Waist circumference risk | ||||||
| No | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Yes | 1.09 | [0.90, 1.32] | .360 | 1.28 | [0.96, 1.70] | .094 |
| Waist hip ratio risk | ||||||
| No | 1.00 | [1.00, 1.00] | 1.00 | [1.00, 1.00] | ||
| Yes | 1.37* | [1.11, 1.70] | .003 | 1.26 | [0.91, 1.72] | .159 |
Exponentiated coefficients; 95% confidence intervals in brackets.
BMI = body mass index.
P <.05
P <.001.
Similarly, higher odds of diabetes as compared to normal were found in male patients (reference group vs female OR = 0.62; 95% CI: 0.45, 0.84), patients who were in 40 to 49; 50 to 59; 60 to 69 years old, those who were housewife (OR = 2.17; 95% CI: 1.43, 3.28; OR = 2.85; 95% CI: 1.91, 4.27; OR = 3.12; 95% CI: 2.08, 4.69; OR = 1.71; 95% CI: 1.22, 2.40, respectively). Diabetes have significant associated with participants have hypertension (OR = 1.19; 95% CI: 1.72, 2.70).
4. Discussion
In this study, 17.9% of participants have prediabetes, and 7.3% have diabetes. The prevalence of diabetes tended to increase compared to the number in 2012 was 5.4%.[3] Our results showed diabetes in Vietnam was lower than in India (8.0% from a national study from 2013–2019),[13] higher than Laos (5.7% in 2016).[14] This difference could occur due to the difference in population in each country. Moreover, our findings showed the growing trend of T2DM prevalence in Vietnam’s population from 30 to 69 years old, similar to results from studies in several Asian countries, such as China,[15] India,[16] Sri Lanka, and Bangladesh.[17]
Our results show that age is the common factor directly related to prediabetes and diabetes in both genders. Other factors directly associated with prediabetes and diabetes include BMI, WHR, hypertension, educational level, and job.
Regarding the non-modifiable risk factors of T2DM, including age, gender, and genetic factors, our findings show that diabetic patients were more likely to be male and have a family history of diabetes. Contrary to our finding, results from research in China on adults aged 45 to 75 years and Iran on adults aged 15 and 64 years reported that diabetes was predominant in female.[18,19] However, our findings are similar to those of other authors who also reported diabetes to be more frequent in male.[20–22] This contrast could be due to the different ethnic backgrounds (Vietnam population) to other countries, and the insulin resistance among non-diabetic males was generally higher than females.[23]
In the current study, BMI is the most influential modifiable factor directly associated with diabetes. This could be explained by the obesity status leading to enhanced insulin resistance. Similar to our findings, previous studies showed a direct relationship between BMI and diabetes.[24,25] Moreover, BMI has been proven as a risk factor that has a significant association with prediabetes.[26] On the contrary, some studies show BMI only affects male patients with type 2 diabetes, such as the Roche et al study reported that being overweight-obese is the dominant risk factor for developing diabetes only in men.[27] In addition, results from Njølstad et al[29] study in Norway also showed BMI is only positively correlated with diabetes in men.
Besides BMI, WC, and Waist-Hip Ratio (WHR) are also predictors of the risk of developing T2DM. In the present study, WC risk is found to be higher in male and all female participants have normal WC. However, our result showed that WC risk have positively associated with prediabetes and diabetes status, which similar with study at Nepal in 2009.[29] We conduct multinomial logistics in this study, and the results show the correlation of WHR with prediabetes and diabetes, respectively. High WHR means a higher risk to develop diabetes, which is consistent with the study of A Shah et al[29] in Nepal and the study of Dalton et al[11] in Australia. The increasing diabetes prevalence has been linked to overweight-obese status in Vietnam, which is a consequence of lifestyle change during urbanization. The promotion of fast food consumption and the change in diet and lack of physical activity caused weight gain, high BMI, and high WHR. In order to control the rising incidence of T2DM, we propose weight reduction, weight gain prevention, increased active physical activity. It is essential due to adult-onset diabetes not only linked to high BMI score, high WHR score but also associated with the duration of weight gain.[30]
Moreover, the prevalence of T2DM also increases with age, as seen in the present study, which is consistent with other study in Vietnam, New South Wales and Germany.[31–33]
In our current study, hypertension has a higher prevalence among prediabetes and diabetes patients. Previous medical literature also mentioned that hypertension is present in more than 50% of patients with diabetes mellitus, and having one of the two conditions increases the risk of developing the other by 1.5 to 2.0 times.[34,35] Similarly, our multinomial logistic analysis reported that hypertension increases nearly 1.4 times the chance patients will have prediabetes and increases two times the odds of developing diabetes. However, the causal relationship between hypertension and T2DM is unclear and needs more future studies to identify.
Despite the advantage of the study’s large sample size, our research still has several limitations. First, as a cross-sectional survey, the results will limit interpreting any causal inference. Second, our research has not been able to collect information about the lifestyle of people with diabetes. Further studies in Vietnam are needed to explore the associated factor and detect modifiable factors with T2DM to thoroughly increase the quality of life among T2DM patients.
5. Conclusions
This study provides the national prevalence and association with type 2 diabetes and prediabetes risk factors among adults aged 30 to 69 years old in Vietnam. Type 2 diabetes has associated with other conditions such as hypertension, obesity, WC, and WHR. We suggested that further study explore the association with these risk factors to prevent and decrease the rising prevalence of diabetes among the population.
Acknowledgments
This study was financially supported by the National Hospital of Endocrinology of Vietnam.
Author contributions
Conceptualization: Duong Huong Phan, Trang Thu Vu, Minh Van Hoang.
Data curation: Duong Huong Phan, Vu Tuan Doan, Toan Quang Le, Thanh Duc Nguyen.
Formal analysis: Duong Huong Phan, Trang Thu Vu, Vu Tuan Doan.
Funding acquisition: Duong Huong Phan.
Investigation: Duong Huong Phan, Trang Thu Vu, Vu Tuan Doan, Toan Quang Le, Thanh Duc Nguyen, Minh Van Hoang.
Methodology: Duong Huong Phan, Trang Thu Vu, Minh Van Hoang.
Project administration: Duong Huong Phan, Toan Quang Le.
Supervision: Duong Huong Phan, Minh Van Hoang.
Validation: Duong Huong Phan, Thanh Duc Nguyen, Minh Van Hoang.
Writing – original draft: Duong Huong Phan, Trang Thu Vu.
Writing – review & editing: Duong Huong Phan, Trang Thu Vu, Vu Tuan Doan, Toan Quang Le, Thanh Duc Nguyen, Minh Van Hoang.
Abbreviations:
- BMI =
- body mass index
- FPG =
- fasting plasma glucose
- OGTT =
- oral glucose tolerance test
- T2DM =
- type 2 diabetes mellitus
- WC =
- waist circumference
- WHR =
- waist hip ratio
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Phan DH, Vu TT, Doan VT, Le TQ, Nguyen TD, Hoang MV. Assessment of the risk factors associated with type 2 diabetes and prediabetes mellitus: A national survey in Vietnam. Medicine 2022;101:41(e31149).
Contributor Information
Duong Huong Phan, Email: phanhuongduong@gmail.com.
Vu Tuan Doan, Email: tuanvu138@gmail.com.
Toan Quang Le, Email: letoan.endo@gmail.com.
Thanh Duc Nguyen, Email: ducthanhytcc@gmail.com.
Minh Van Hoang, Email: hvm@huph.edu.vn.
References
- [1].East M, Africa N. IDF diabetes atlas. Diabetes. 2017;20:79. [Google Scholar]
- [2].Beckman JA, Paneni F, Cosentino F, et al. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Eur Heart J. 2013;34:2444–52. [DOI] [PubMed] [Google Scholar]
- [3].Nguyen CT, Pham NM, Lee AH, et al. Prevalence of and risk factors for type 2 diabetes mellitus in Vietnam: a systematic review. Asia Pac J Public Health. 2015;27:588–600. [DOI] [PubMed] [Google Scholar]
- [4].Ministry of Health, Vietnam. The National Survey on the Risk Factors of Noncommunicable, Diseases (STEPS) Viet Nam in 2015. World Health Organization. 2015. [Google Scholar]
- [5].International Diabetes Federation. IDF Diabetes Atlas. 9th ed. International Diabetes Federation, 2019. [Google Scholar]
- [6].Basit A, Fawwad A, Qureshi H, et al. Prevalence of diabetes, pre-diabetes and associated risk factors: second national diabetes survey of Pakistan (NDSP), 2016-2017. BMJ Open. 2018;8:e020961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cho EH, Shin D, Cho KH, et al. Prevalences and management of diabetes and pre-diabetes among korean teenagers and young adults: results from the Korea national health and nutrition examination survey 2005-2014. J Korean Med Sci. 2017;32:1984–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].American Diabetes Association. Standards of medical care in diabetes—2018 abridged for primary care providers. Clin Diabetes. 2018;36:14–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].American Diabetes Association. Standards of medical care in diabetes‐2019 abridged for primary care providers. Clin Diabetes. 2019;37:11–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chalmers J, MacMahon S, Mancia G, et al. 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin Exp Hypertens. 1999;21:1009–60. [DOI] [PubMed] [Google Scholar]
- [11].Dalton M, Cameron A, Zimmet PZ, et al. Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med. 2003;254:555–63. [DOI] [PubMed] [Google Scholar]
- [12].Erdembileg A, Shiwaku K, Nogi A, et al. The New BMI criteria for Asians by the regional office for the Western Pacific Region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health. 2003;45:335–43. [DOI] [PubMed] [Google Scholar]
- [13].Rajendra Prasad Center for Ophthalmic Sciences and AIIMS, New Delhi. National Diabetes and Diabetic Retinopathy Survey India 2015–2019 – A Summary Report. New Delhi: Ministry of Health & Family Welfare GoI, 2019. [Google Scholar]
- [14].World Health Organization. Diabetes Lao People's Democratic Republic 2016 Country Profile. World Health Organization, 2016. [Google Scholar]
- [15].Zuo H, Shi Z, Hussain A. Prevalence, trends and risk factors for the diabetes epidemic in China: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2014;104:63–72. [DOI] [PubMed] [Google Scholar]
- [16].Ramachandran A, Snehalatha C, Shetty AS, et al. Trends in prevalence of diabetes in Asian countries. World J Diabetes. 2012;3:110–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ramachandran A, Wan Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375:408–18. [DOI] [PubMed] [Google Scholar]
- [18].Qin X, Li J, Zhang Y, et al. Prevalence and associated factors of diabetes and impaired fasting glucose in Chinese hypertensive adults aged 45 to 75 years. PLoS One. 2012;7:e42538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Azimi-Nezhad M, Ghayour-Mobarhan M, Parizadeh MR, et al. Prevalence of type 2 diabetes mellitus in Iran and its relationship with gender, urbanisation, education, marital status and occupation. Singapore Med J. 2008;49:571–6. [PubMed] [Google Scholar]
- [20].Lipscombe LL, Hux JE. Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995-2005: a population-based study. Lancet. 2007;369:750–6. [DOI] [PubMed] [Google Scholar]
- [21].Choi YJ, Kim HC, Kim HM, et al. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009;32:2016–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Logue J, Walker JJ, Colhoun HM, et al. Do men develop type 2 diabetes at lower body mass indices than women? Diabetologia. 2011;54:3003–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Geer E, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6(Suppl 1):60–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bays HE, Chapman RH, Grandy S, et al. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. Int J Clin Pract. 2007;61:737–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bakhotmah B. Prevalence of obesity among type 2 diabetic patients: non-smokers housewives are the most affected in Jeddah, Saudi Arabia. Open J Endocr Metab Dis. 2013;03:25–30. [Google Scholar]
- [26].Amiri P, Jalali-Farahani S, Karimi M, et al. Factors associated with pre-diabetes in Tehranian men and women: a structural equations modeling. PLoS One. 2017;12:e0188898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Roche MM, Wang PP. Factors associated with a diabetes diagnosis and late diabetes diagnosis for males and females. J Clin Transl Endocrinol. 2014;1:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Njølstad I, Amesen E, Lund-Larsen PG. Sex differences in risk factors for clinical diabetes mellitus in a general population: a 12-year follow-up of the Finnmark study. Am J Epidemiol. 1998;147:49–58. [DOI] [PubMed] [Google Scholar]
- [29].Shah A, Bhandary S, Malik SL, et al. Waist circumference and waist-hip ratio as predictors of type 2 diabetes mellitus in the Nepalese population of Kavre District. Nepal Med Coll J. 2009;11:261–7. [PubMed] [Google Scholar]
- [30].Will JC, Williamson DF, Ford ES, et al. Intentional weight loss and 13-year diabetes incidence in overweight adults. Am J Public Health. 2002;92:1245–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Son L, Kusama K, Hung N, et al. Prevalence and risk factors for Diabetes in Ho Chi Minh City, Vietnam. Diabetic Med. 2004;21:371–6. [DOI] [PubMed] [Google Scholar]
- [32].Irvine K, Eyeson-Annan M. Continuous NSW health survey: quarterly report on health status, health behaviours, and risk factors. NSW Public Health Bulletin. 2004;15:112–4. [PubMed] [Google Scholar]
- [33].Schulze MB, Heidemann C, Schienkiewitz A, et al. Comparison of anthropometric characteristics in predicting the incidence of type 2 diabetes in the EPIC-Potsdam study. Diabetes Care. 2006;29:1921–3. [DOI] [PubMed] [Google Scholar]
- [34].Lastra G, Syed S, Kurukulasuriya LR, et al. Type 2 diabetes mellitus and hypertension: an update. Endocrinol Metab Clin North Am. 2014;43:103–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Roth GA, Huffman MD, Moran AE, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132:1667–78. [DOI] [PubMed] [Google Scholar]