Background:
The study aimed to assess the efficacy and safety of parasacral neuromodulation (PNS) versus tibial nerve stimulation (TNS) for patients with overactive bladder (OAB).
Methods:
Databases including PubMed, Embase, clinicalTrial.gov, and Cochrane Library Central Register of Controlled Trials were systematically searched from January 1, 1999 to September 9, 2022. The improvements in a 3-day voiding diary were set as the primary outcomes. Then, the scores of overactive bladder-validated 8-question awareness tool (OAB-V8), King’s health questionnaire (KHQ), and international consultation on incontinence questionnaire overactive bladder (ICIQ-OAB) were also evaluated.
Results:
Five articles (4 randomized controlled trials [RCTs] and 1 prospective study) including 255 OAB patients were enrolled. Two kinds of neuromodulations had similar performances in the micturition (mean difference [MD] = 0.26, 95% confidence interval [CI]: –0.51 to 1.04, P = .50), urgency episodes (MD = –0.16, 95% CI: –0.64 to 0.31, P = .50), incontinence episodes (MD = 0.09, 95% CI: –0.41 to 0.59, P = .72), as well as in the nocturia episodes (MD = 0.04, 95% CI: –0.45 to 0.52, P = .89). Furthermore, there was no difference regarding ICIQ-OAB scores (P = .83), KHQ (P = .91), and OAB-V8 scores (P = .83). Importantly, included studies reported no adverse events in the 2 groups.
Conclusion:
TNS and PNS had similar effectiveness for the treatment of OAB, moreover, without any identified adverse events in both groups. However, well-designed RCTs are stilled needed to verify our results.
Keywords: neuromodulation, overactive bladder, parasacral nerve stimulation, tibial nerve stimulation
1. Introduction
Patients with overactive bladder syndrome (OAB) usually present urinary urgency and increased daytime micturition and/or nocturia, with or without urinary incontinence.[1] Based on a real-word study, the prevalence of OAB is about 17% and which increases gradually with age.[2] OAB is not life-threatening, but it alters life styles and may have a significant impact on the life quality, sexual function, and social interaction of patients.[3–6] After failed conservative and behavioral therapies, antimuscarinics such as solifenacin are the mainstream treatments for OAB, but high costs and side effects reduce patient adherence to these drugs and ultimately limit their benefits to a wider range of patients with OAB.[2,7,8] Under this circumstance, patients tend to choose a more cost-effective and less invasive approach.
By modulating the sacral plexus and inhibiting detrusor muscle hyperactivity, physiotherapeutic treatment through electrostimulation of the tibial[9–11] and parasacral nerves[11–13] has proven an effective alternative to treat OAB symptoms in adult and infant patients. Both 2 neuromodulations target S2 to S4 nerves which correspond to the main bladder parasympathetic innervation, but the locations of electrodes in the 2 groups are different. With regard to tibial nerve stimulation (TNS), whose electrodes are usually located near the medial malleolus, covering the path of the tibial nerve to innervate S2 to S4 nerves.[14] Regarding parasacral nerve stimulation (PNS), electrodes are positioned over the parasacral region on the level of S3.[11] Although TNS and PNS have been proven effective and well-accepted,[11,13,14] it is unclear who has better effectiveness and safety profile for patients with OAB. Therefore, we conducted a meat-analysis to compare the safety and effectiveness of TNS versus PNS in treating patients with OAB and provide a better clinical reference for urologists when making a decision.
2. Materials and Methods
2.1. Study selection
The ethic approval of this study was not necessary because the included studies were open-sourced. The study was performed in line with the PRISMA guidelines.[15] Databases including PubMed, Embase, clinicalTrial.gov, and Cochrane Library Central Register of Controlled Trials were systematically searched from January 1, 1999 to September 9, 2022 to find the studies comparing the PNS and TNS for OAB. Each database was searched using the following formula: (Overactive bladder OR Overactive urinary bladder OR Overactive detrusor) AND (Tibial neuromodulation OR Tibial nerve stimulation OR Posterior tibial nerve stimulation) AND (Parasacral neuromodulation OR Parasacral nerve stimulation). Last, reference list of related studies was carefully checked for eligible articles.
2.2. Inclusion criteria and exclusion criteria
Study selection was conducted in line with the PICOS principle. Comparable studies (randomized controlled trial [RCT], retrospective study, and prospective study) evaluated the efficacy and safety of PNS versus TNS for patients with OAB were selected. There were no limitations regarding status and language. But a study should be excluded if other third-line treatment such as type A botulinum toxin injection was involved. Additionally, a study design of case report, protocol, comment, and an article without adequate data were also excluded.
2.3. Study selection and data extraction
First, we identified the eligible studies according to the established inclusion and exclusion criteria. Subsequently, the baseline information, treatment protocol, OAB symptom scores at last visit, and complications were collected to perform downstream analyses. Last, all authors double-checked included data. If there was a disagreement, a discussion was performed in our team to draw a conclusion.
2.4. Outcomes
The amount of micturition in 24 hour, the number of urgency episodes and incontinence episodes in 24 hour, and the average nocturia episodes were primary outcomes to assess the effectiveness of PNS versus TNS. Then, overactive bladder-validated 8-question awareness tool (OAB-V8), King’s health questionnaire (KHQ) (incontinence impact domain), and international consultation on incontinence questionnaire overactive bladder (ICIQ-OAB) scores were compared to evaluate patients’ life quality and OAB symptom improvements. Last, complications such as bleeding, discomfort, and pain over the treated area were recorded.
2.5. Quality assessment
The quality of RCTs and prospective studies was evaluated in line with the Cochrane handbook guideline.[16] The domains of risk of bias were judged as low, high, or unclear risk according to the scores.
2.6. Data analysis
All statistical analyses were performed using the Review Manager 5.3 (Cochrane Collaboration, Oxford, UK). All included data were continuous parameters, and their mean differences (MDs) with 95% confidence intervals (CIs) were calculated. I2 test was performed to identify heterogeneity among studies. IF I2 values <50%, the fixed-effect model was used, otherwise the random-effect method was used. Funnel plot was constructed to assess the publication bias of primary outcomes.
3. Results
3.1. Study characteristics
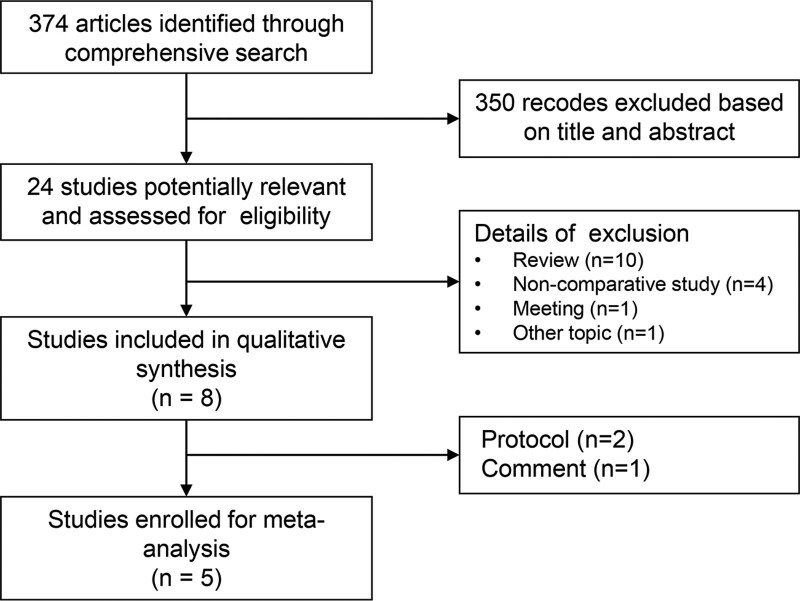
Following the study selection process in Figure 1, a total of 374 articles were initially identified, but 350 records were excluded according to the established inclusion and exclusion criteria. Subsequently, 8 articles were selected for qualitative synthesis after removal of noncomparative articles.[17–24] However, 2 study protocols[22,23] and 1 comment[24] with inadequate data were excluded. Eventually, a total of 5 trials (4 RCTs and 1 prospective study)[17–21] with 255 patients were enrolled. The characteristics of each study included were presented in Table 1. Notably, the study by Barroso et al[17] compared the efficacy and safety of 2 kinds of neuromodulations in children, but others 4 studies focused on adults. Table 2 showed the treatment protocol in each study. It should be noted that the treatment protocols in each study were not consistent. Importantly, the quality assessment showed a low risk in all studies (Fig. S1, Supplemental Digital Content http://links.lww.com/MD/H628).
Figure 1.
PRISMA flowchart of study selection.
Table 1.
The baseline information of included studies.
| Study | Design | Group | N (F/M) | Age (yrs) | Follow-up |
|---|---|---|---|---|---|
| Barroso (2013) | P | Tibial | 22 (15/7) | 8.4 ± 3.8 | 3 mon |
| Parasacral | 37 (25/12) | 7.5 ± 2.8 | |||
| Devi (2014) | RCT | Tibial | 15 (9/6) | 42.8 ± 8.12 | 4 wks |
| Parasacral | 15 (10/5) | 43.6 ± 7.56 | |||
| Jacomo (2019) | RCT | Tibial | 25 (25/0) | 66 (65–73) | 1 mon |
| Parasacral | 25 (25/0) | 66.5 (62.5–75.75) | |||
| Mallmann (2020) | RCT | Tibial | 25 (25/0) | 63.28 ± 9.80 | 6 wks |
| Parasacral | 25 (25/0) | 59.68 ± 10.27 | |||
| Padilha (2021) | RCT | Tibial | 33 (33/0) | 41.5 ± 13.8 | 6 wks |
| Parasacral | 33 (33/0) | 42.0 ± 17.1 |
P = prospective, RCT = randomized controlled trail.
Table 2.
The treatment protocol in each included study.
| Study | Group | Protocol | Current and pulse width | Type | Location | Stimulator |
|---|---|---|---|---|---|---|
| Barroso (2013) | Tibial | Once wkly, 30 min/session | 20 Hz, 400 µs | Needle electrodes | 2 fingers cephalad to the medial malleolus | 608E electrical current stimulator (NKL Electronic Products, Brazil) |
| Parasacral | 3 times wkly, 20 min/session | 10 Hz, 700 µs | Superficial electrodes | Parasacral region cover S2 and S3 nerves | Dualpex 961 Uro, Quark® Medical Products | |
| Devi (2014) | Tibial | 6 times wkly, 20 min/session | 10 Hz, 200 µs | Superficial electrodes | Proximal to the medial malleolus | – |
| Parasacral | 6 times wkly, 20 minutes/session | 10 Hz, 200 µs | Superficial electrodes | Parasacral region cover S2 and S3 nerves | – | |
| Jacomo (2019) | Tibial | Twice a wk, 30 min/session | 10 Hz, 200 µs | Superficial electrodes | Below the left medial malleolus | DUALPEX 961s (Quark, Brazil) |
| Parasacral | Twice a wk, 30 min/session | 10 Hz, 700 µs | Superficial electrodes | Parasacral region cover S2 and S3 nerves | DUALPEX 961s (Quark, Brazil) | |
| Mallmann (2020) | Tibial | 3 times per wk, 20 min/session | 20 Hz, 300 µs | Silver spike point electrodes | The medial region of the right ankle | – |
| Parasacral | 3 times per wk, 20 minutes/session | 20 Hz, 300 µs | Superficial electrodes | Bilteral sacral roots (parasacral region) | – | |
| Padilha (2021) | Tibial | Twice a wk, 20 min/session | 10 Hz, 200 µs | Superficial electrodes | One electrode positioned immediately posterior to the medial malleolus and another approximately 10 cm superior to it | TENS Vif 993 (Quark Medical) |
| Parasacral | Twice a wk, 20 min/session | 10 Hz, 200 µs | Superficial electrodes | Electrodes positioned side by side symmetrically, approximately 4 cm apart, at the S3 level | TENS Vif 993 (Quark Medical) |
3.2. Evaluation of effectiveness and safety profile
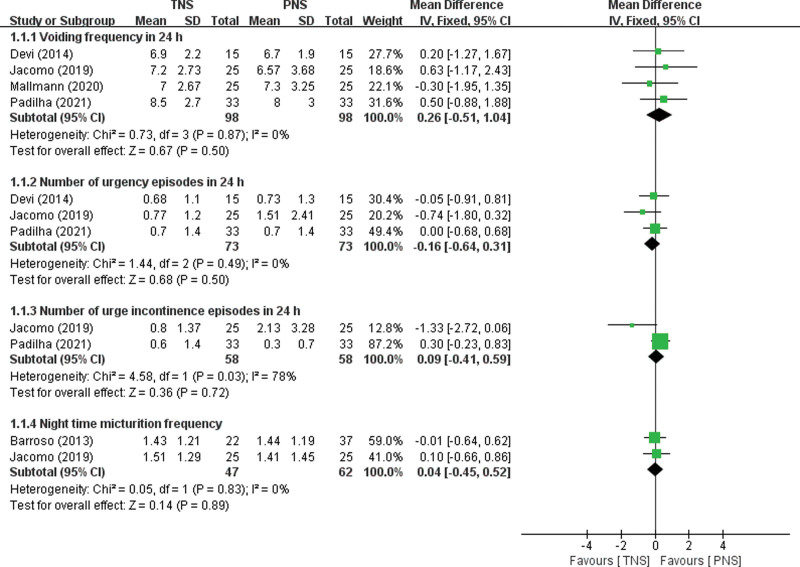
The amount of micturition in 24 hour was provided in 4 studies,[18–21] and the number of urgency episodes was presented in 3 studies.[18,20,21] But only 2 studies had data regarding the number of incontinence episodes in 24 hour and nocturia episodes.[17,18] No statistical differences were noted in the micturition (MD = 0.26, 95% CI: –0.51 to 1.04, P = .50), urgency episodes (MD = –0.16, 95% CI: –0.64 to 0.31, P = .50), incontinence episodes (MD = 0.09, 95% CI: –0.41 to 0.59, P = .72), as well as in the nocturia episodes (MD = 0.04, 95% CI: –0.45 to 0.52, P = .89) in the 2 groups (Fig. 2). Moreover, none of publication bias regarding primary outcomes was identified (Fig. S2, Supplemental Digital Content http://links.lww.com/MD/H629).
Figure 2.
Forest plot for the changes of primary outcomes. PNS = parasacral nerve stimulation, TNS = tibial nerve stimulation.
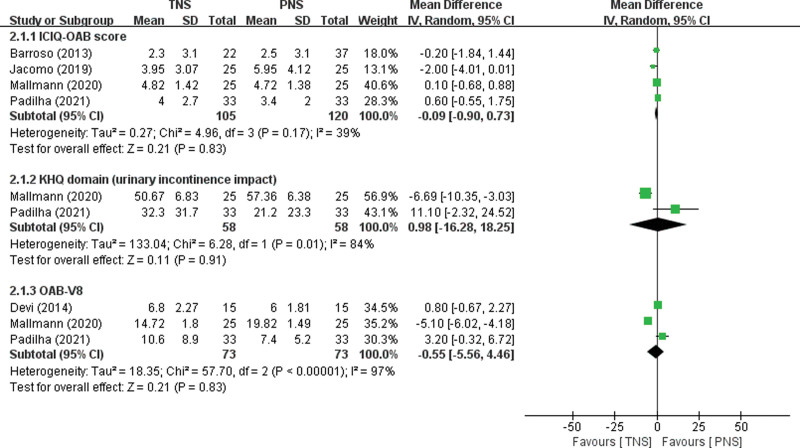
With regard to patients’ life quality, 4 articles[17–20] contained the data on ICIQ-OAB scores, 2 studies[19,20] presented the data on KHQ scores, and 3 articles[19–21] assessed OAB-V8 scores. Comparable pooled results were observed in terms of ICIQ-OAB scores (MD = –0.09, 95% CI: –0.90 to 0.73, P = .83), KHQ scores (MD = 0.98, 95% CI: –16.28 to 18.25, P = .91), and OAB-V8 scores (MD = –0.55, 95% CI: –5.56 to 4.46, P = .83) in the TNS and PNS groups (Fig. 3).
Figure 3.
Forest plot for life quality scores. Tibial nerve stimulation, ICIQ-OAB = International consultation on incontinence questionnaire overactive bladder, KHQ = King’s health questionnaire, OAB-V8 = overactive bladder-validated 8-question awareness tool, PNS = parasacral nerve stimulation, TNS = tibial nerve stimulation.
Regarding the safety profile, no complications were identified or reported in the included studies.
4. Discussion
Although the PNS and TNS are well accepted, the priority of 2 kinks of neuromodulations remains unclear. Therefore, the first meta-analysis was performed to shed some light on the topic. Based on the current data, TNS and PNS presented comparable efficacy regarding micturition (P = .50), urgency episodes (P = .50), incontinence episodes (P = .72), as well as in the nocturia episodes (P = .89). Furthermore, both 2 kinds of neuromodulations significantly improved the patients’ life quality. Importantly, good safety profile of 2 types of neuromodulations was found.
In the field of urology, neuromodulation was applied to target and modulate the innervation system that controls lower urinary tract. Tibial nerve (TN), a distal branch of the sciatic nerve, that originates from the pelvis (L5–S3 spinal roots) and descends towards the lower limbs.[25] Modulation of the TN provides retrograde stimulation to the sacral plexus, which drives bladder relaxing and contraction, and improves bladder rhythm.[25] Previous comparative studies have proved TNS an effective, acceptable, and noninvasive approach for OAB in both adults and children.[26–28] The results found that the patients in TNS group presented a higher response rate and had better improvement regarding frequency, nocturnal voiding, urgency, and urge incontinence. Additionally, Iyer et al reported that TNS provided continuous therapeutic effects in a 9-year follow-up.[29] Furthermore, a review showed that TNS was helpful in sexual function.[30] But it should be mentioned that the major complications of TNS (pain and infections at the puncture site) should be concerned and managed carefully despite with a low incidence. In regard to PNS, due to its noninvasive nature, it is more popular in children with OAB. Superficial electrodes of PNS were generally positioned at parasacral region to modulate S2 to S3 nerves.[23] Veiga et al reported that patients underwent twice-weekly sessions or three times weekly of PNS had the same improvements of OAB symptoms.[31] Many studies have proven PNS an effective approach for OAB,[11,31–33] which was in line with our results, but it should be kept in mind that PNS had limited effects on enuresis and constipation.[33] More studies are needed to further investigate this topic. Based on the results of the current study, electrical stimulation including PNS and TNS could be considered as home treatments due to its simplicity, practicability of operation, and low risk and incidence of adverse effects. Several studies have proposed that the benefits of neuromodulation would diminish after the treatment period, necessitating the use of continuous application for better clinical outcomes.[19,20] Therefore, home-based neuromodulation may be preferable to a large number of medical appointments.
Unfortunately, limited data were established on the adult sexual function after PNS. Moreover, a pooled result regarding evident cost-effectiveness can’t be performed due to insufficient data between 2 groups. At present, there is no evidence that longer stimulation durations produce better results and the optimal intervention protocol or schedule for both types of neuromodulations has not been determined.[34] More studies are needed to investigate these topics.
The study had several limitations. First, only 5 articles could be eventually selected, and the final number of patients was 255. Second, only 1 study focused on children, and it was difficult to perform subgroup analyses regarding gender and age. Therefore, prospective studies with a larger sample size should be considered in the future to verify the current findings.
5. Conclusion
The current pooled results supported that TNS is as effective as PNS for the treatment of OAB, moreover, without any reported adverse events in both groups. However, prospective studies with a larger sample size should be conducted to verify our findings.
Author contributions
Conceptualization: Zhi-Hong Wang, Zhi-Hong Liu.
Data curation: Zhi-Hong Wang, Zhi-Hong Liu.
Formal analysis: Zhi-Hong Wang, Zhi-Hong Liu.
Investigation: Zhi-Hong Wang, Zhi-Hong Liu.
Methodology: Zhi-Hong Wang, Zhi-Hong Liu.
Project administration: Zhi-Hong Wang, Zhi-Hong Liu.
Resources: Zhi-Hong Wang.
Software: Zhi-Hong Wang, Zhi-Hong Liu.
Supervision: Zhi-Hong Wang, Zhi-Hong Liu.
Validation: Zhi-Hong Wang.
Visualization: Zhi-Hong Wang.
Writing – original draft: Zhi-Hong Wang, Zhi-Hong Liu.
Writing – review & editing: Zhi-Hong Wang, Zhi-Hong Liu.
Supplementary Material
Abbreviations:
- ICIQ-OAB =
- international consultation on incontinence questionnaire overactive bladder
- KHQ =
- King’s health questionnaire
- OAB =
- overactive bladder
- OAB-V8 =
- overactive bladder-validated 8-question awareness tool
- PNS =
- Parasacral nerve stimulation
- TNS =
- tibial nerve stimulation
All data generated or analyzed during this study are included in this published article [and its supplementary information files]; The datasets generated during and/or analyzed during the current study are publicly available.The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
How to cite this article: Wang ZH, Liu ZH. Treatment for overactive bladder: A meta-analysis of tibial versus parasacral neuromodulation. Medicine 2022;101:41(e31165).
References
- [1].D’Ancona C, Haylen B, Oelke M, et al. The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn. 2019;38:433–77. [DOI] [PubMed] [Google Scholar]
- [2].Monteiro S, Riccetto C, Araújo A, et al. Efficacy of pelvic floor muscle training in women with overactive bladder syndrome: a systematic review. Int Urogynecol J. 2018;29:1565–73. [DOI] [PubMed] [Google Scholar]
- [3].Kinsey D, Pretorius S, Glover L, et al. The psychological impact of overactive bladder: a systematic review. J Health Psychol. 2016;21:69–81. [DOI] [PubMed] [Google Scholar]
- [4].Vaughan CP, Johnson TM, 2nd, Ala-Lipasti MA, et al. The prevalence of clinically meaningful overactive bladder: bother and quality of life results from the population-based FINNO study. Eur Urol. 2011;59:629–36. [DOI] [PubMed] [Google Scholar]
- [5].Coyne KS, Sexton CC, Irwin DE, et al. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101:1388–95. [DOI] [PubMed] [Google Scholar]
- [6].Balzarro M, Rubilotta E, Mancini V, et al. Impact of overactive bladder-wet syndrome on female sexual function: a systematic review and meta-analysis. Sexual Med Rev. 2019;7:565–74. [DOI] [PubMed] [Google Scholar]
- [7].Peng L, Zeng X, Shen H, et al. Efficacy and safety of combinations of mirabegron and solifenacin in patients with overactive bladder: a systematic review and meta-analysis. Int J Clin Exp Med. 2019;12:1355–65. [Google Scholar]
- [8].Wu JP, Peng L, Zeng X, Li H, Shen H, Luo DY. Is imidafenacin an alternative to current antimuscarinic drugs for patients with overactive bladder syndrome? Int Urogynecol J. 2020;32:1117–27. [DOI] [PubMed] [Google Scholar]
- [9].Schneider MP, Gross T, Bachmann LM, et al. Tibial nerve stimulation for treating neurogenic lower urinary tract dysfunction: a systematic review. Eur Urol. 2015;68:859–67. [DOI] [PubMed] [Google Scholar]
- [10].Ghavidel-Sardsahra A, Ghojazadeh M, Rahnama IM, et al. Efficacy of percutaneous and transcutaneous posterior tibial nerve stimulation on idiopathic overactive bladder and interstitial cystitis/painful bladder syndrome: A systematic review and meta-analysis. Neurourol Urodyn. 2022;41:539–51. [DOI] [PubMed] [Google Scholar]
- [11].Barroso U, Jr, Lordêlo P. Electrical nerve stimulation for overactive bladder in children. Nat Rev Urol. 2011;8:402–7. [DOI] [PubMed] [Google Scholar]
- [12].Hoffmann A, Sampaio C, Nascimento AA, et al. Predictors of outcome in children and adolescents with overactive bladder treated with parasacral transcutaneous electrical nerve stimulation. J Pediatr Urol. 2018;14:54.e1–6. [DOI] [PubMed] [Google Scholar]
- [13].de Paula L, de Oliveira LF, Cruz BP, et al. Parasacral transcutaneous electrical neural stimulation (PTENS) once a week for the treatment of overactive bladder in children: A randomized controlled trial. J Pediatr Urol. 2017;13:263.e1–63.e6. [DOI] [PubMed] [Google Scholar]
- [14].Al-Danakh A, Safi M, Alradhi M, et al. Posterior tibial nerve stimulation for overactive bladder: mechanism, classification, and management outlines. Parkinson’s Dis. 2022;2022:2700227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical Research ed). 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical Research ed). 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Barroso U, Jr, Viterbo W, Bittencourt J, et al. Posterior tibial nerve stimulation vs parasacral transcutaneous neuromodulation for overactive bladder in children. J Urol. 2013;190:673–7. [DOI] [PubMed] [Google Scholar]
- [18].Jacomo RH, Alves AT, Lucio A, et al. Transcutaneous tibial nerve stimulation versus parasacral stimulation in the treatment of overactive bladder in elderly people: a triple-blinded randomized controlled trial. Clinics (Sao Paulo, Brazil). 2020;75:e1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Mallmann S, Ferla L, Rodrigues MP, et al. Comparison of parasacral transcutaneous electrical stimulation and transcutaneous posterior tibial nerve stimulation in women with overactive bladder syndrome: a randomized clinical trial. Eur J Obstet Gynecol Reprod Biol. 2020;250:203–8. [DOI] [PubMed] [Google Scholar]
- [20].Falcão PJ, Arias AM, Driusso P. Parasacral versus tibial transcutaneous electrical stimulation to treat urinary urgency in adult women: randomized controlled clinical trial. Eur J Obstet Gynecol Reprod Biol. 2021;267:167–73. [DOI] [PubMed] [Google Scholar]
- [21].Devi LS, Khuman R, Vasveliya M, et al. Neuromodulation for overactive bladder with transcutaneous electrical nerve stimulation in adults – a randomized clinical study. International Journal of Pharma & Bio Sciences. 2014;5:671–79. [Google Scholar]
- [22].Candido TA, Ribeiro BM, de Araújo CRC, et al. Effects of tibial and parasacral nerve electrostimulation techniques on women with poststroke overactive bladder: study protocol for a randomized controlled trial. Trials. 2020;21:936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Padilha JF, Avila MA, Seidel EJ, et al. Different electrode positioning for transcutaneous electrical nerve stimulation in the treatment of urgency in women: a study protocol for a randomized controlled clinical trial. Trials. 2020;21:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Srivastav A, Sharma N, Srivastav AK. Comments on “Transcutaneous tibial nerve stimulation versus parasacral stimulation in the treatment of overactive bladder in elderly people: A triple-blinded randomized controlled trial”. Clinics (Sao Paulo, Brazil). 2020;75:e2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bhide AA, Tailor V, Fernando R, et al. Posterior tibial nerve stimulation for overactive bladder-techniques and efficacy. Int Urogynecol J. 2020;31:865–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Peters KM, Carrico DJ, Perez-Marrero RA, et al. Randomized trial of percutaneous tibial nerve stimulation versus Sham efficacy in the treatment of overactive bladder syndrome: results from the SUmiT trial. J Urol. 2010;183:1438–43. [DOI] [PubMed] [Google Scholar]
- [27].Finazzi-Agrò E, Petta F, Sciobica F, et al. Percutaneous tibial nerve stimulation effects on detrusor overactivity incontinence are not due to a placebo effect: a randomized, double-blind, placebo controlled trial. J Urol. 2010;184:2001–6. [DOI] [PubMed] [Google Scholar]
- [28].Cui H, Yao Y, Xu Z, et al. Role of transcutaneous electrical nerve stimulation in treating children with overactive bladder from pooled analysis of 8 randomized controlled trials. Int Neurourol J. 2020;24:84–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Iyer S, Laus K, Rugino A, et al. Subjective and objective responses to PTNS and predictors for success: a retrospective cohort study of percutaneous tibial nerve stimulation for overactive bladder. Int Urogynecol J. 2019;30:1253–9. [DOI] [PubMed] [Google Scholar]
- [30].Kershaw V, Khunda A, McCormick C, et al. The effect of percutaneous tibial nerve stimulation (PTNS) on sexual function: a systematic review and meta-analysis. Int Urogynecol J. 2019;30:1619–27. [DOI] [PubMed] [Google Scholar]
- [31].Veiga ML, Oliveira K, Batista V, et al. Parasacral transcutaneous electrical nerve stimulation in children with overactive bladder: comparison between sessions administered two and three times weekly. Int Braz J Urol. 2021;47:787–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Lordêlo P, Soares PV, Maciel I, et al. Prospective study of transcutaneous parasacral electrical stimulation for overactive bladder in children: long-term results. J Urol. 2009;182:2900–4. [DOI] [PubMed] [Google Scholar]
- [33].Veiga ML, Costa EV, Portella I, et al. Parasacral transcutaneous electrical nerve stimulation for overactive bladder in constipated children: the role of constipation. J Pediatr Urol. 2016;12:396.e1–96.e6. [DOI] [PubMed] [Google Scholar]
- [34].Chermansky C, Schurch B, Rahnama’i MS, et al. How can we better manage drug-resistant OAB/DO? ICI-RS 2018. Neurourol Urodyn. 2019;38(Suppl 5):S46–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.