Abstract
Since human health greatly depends on a healthy and risk-free social environment, it is very important to have a concept to focus on improving epidemiology capacity and potential along with economic perspectives as a very influential factor in the future of societies. Through responsible behavior during an epidemic crisis, the health system units can be utilized as a suitable platform for sustainable development. This study employs the Best-Worst Method (BWM) in order to develop a system for identifying and ranking health system units with understanding the nature of the epidemic to help the World Health Organization (WHO) in recognizing the capabilities of resilient health system units. The purpose of this study is to identify and prioritize the resilient health system units for dealing with Coronavirus. The statistical population includes 215 health system units in the world and the opinions of twenty medical experts are also utilized as an informative sample to localize the conceptual model of the study and answer the research questionnaires. The resilient health system units of the world are identified and prioritized based on the statistics of “Total Cases”, “Total Recovered”, “Total Deaths”, “Active Cases”, “Serious”, “Total Tests” and “Day of Infection”. The present descriptive cross-sectional study is conducted on Worldometer data of COVID-19 during the period of 17 July 2020 at 8:33 GMT. According to the results, the factors of “Total Cases”, “Total Deaths”, “Serious”, “Active Cases”, “Total Recovered”, “Total Tests” and “Day of Infection” are among the most effective ones, respectively, in order to have a successful and optimal performance during a crisis. The attention of health system units to the identified important factors can improve the performance of epidemiology system. The WHO should pay more attention to low-resilience health system units in terms of promoting the health culture in crisis management of common viruses. Considering the importance of providing health services as well as their significant effect on the efficiency of the world health system, especially in critical situations, resilience analysis with the possibility of comparison and ranking can be an important step to continuously improve the performance of health system units.
Keywords: Multi-criteria decision-making, Health system unit, Resilience, COVID-19 pandemic, Best-worst method
1. Introduction
Large epidemics or pandemics lead that the patients' referrals to emergencies and hospital intensive care units exceed form their capacity, which result in a shortage of personnel, space, supplies, and poor health outcomes for patients [1]. The COVID-19 disease is a new infection with serious clinical symptoms involving death, which puts a lot of pressure on the infrastructure of the health system and greatly increases the demand for services [2]. The increasing number of people with similar symptoms along with healthy worried people imposes a serious shock on the health system. Lack of resources not only puts patients at risk but also delays treatment for patients with emergency needs [3]. In such situations of increased uninterrupted referrals, the resistance of the health system in functions and disruption of the service supply chain is an important necessity that is known as the resilience of the health system.
Health systems resilience means the capacity to prepare and respond effectively to crises while maintaining the key tasks of the health system before, during and after the crisis [4]. The concept of resilience is a goal and a means to improve a health system that is able to continue providing services at times of acute or chronic crisis [5]. Resilience is the ability to adapt and evolve a system that allows it to adapt or change its features or activities to facilitate shocks [6]. Epidemic prevention and outbreak control depend on coordinated response in key areas of the health system including monitoring, identifying cases, tracking and limiting contacts, clinical management, and accurate infection control. This coordinated response requires intra-organizational governance including the provision of infrastructure, trained personnel, essential medicines, and delivery to the target population and the ability to coordinate this response is a key sign of health system resilience [7,8].
Resilience needs to strengthen the health system. Public health coverage can also decrease the effect of crises and increase resilience [9,10]. The problems of non-resilient health systems include weakness of disease outbreak assessment teams, incoherence against epidemics and insufficient preparedness to deal with crises caused by infectious diseases. Weak laws and regulations and a lack of intra-organizational and cross-organizational coordination have been introduced as the most important challenges to the infectious disease monitoring system. The shortage of hospital beds and specialist physicians in some units as well as crisis and financial problems has created challenges for the health system to perform necessary interventions.
The process of learning from health system shocks is a necessity, especially in understanding how health systems have responded to crises [11,12]. Here, there are several questions to be answered: i. Have the responses been satisfactory? ii. Have the lessons learned been identified? and iii. What are the main steps to take to respond to crises considering the resilience?
It is also necessary to design a model and a tool that can measure the conceptual structures of health system performance in order to know the status of health system resilience against disease and to overcome shortages. Resiliency requires an organization to have the potential to provide resilient performance. In this regard, the organization must have the capacity to work with special methods and under certain situations. In fact, resiliency in health units is defined as the compatibility capacity to cope with various challenges and changes at different system levels to retain high-quality supervision [13].
[14] presented that outbreak and crisis communication concepts and tools have long been on the agenda of public health officials. There is still a need to clarify and integrate risk communication concepts into more standardized practices and improve risk communication and health, particularly among disadvantaged populations. To address these challenges, the European Center for Disease Prevention and Control (ECDC) convened a group of risk communication experts to review and integrate existing approaches and emerging concepts in the development of a training curriculum. This curriculum articulates a new approach to risk communication moving beyond information conveyance to knowledge- and relationship-building. In pilot training, this approach was reflected both in the topics addressed and in the applied methods. This article introduced a new conceptual approach to risk communication capacity building that emerged from this process, presents the pilot training approach developed and shares the results of the course evaluation.
[15] studied the MERS-CoV infection status of clinical nurses to evaluate perception for infection control. They analyzed the perception for infection control of 121 nurses of the three MERS intensive therapeutic hospitals in July 2015. The obtained results showed that 1–6 nurses per hospital in total 8 health care facilities were infected with MERS-CoV. They mainly had short clinical careers and were unaware of infection possibilities. The personal and organizational infection control levels that nurses perceive were low and the relationship between the two levels was statistically significant. It is necessary to prepare an institutional system for controlling infectious diseases for promoting health protection and infectious disease management competency of nurses [16]. presented a Data Envelopment Analysis (DEA) model to provide the corresponding development measures for medical subjects in hospitals. The evaluation index system of medical subjects was obtained based on the analysis of medical subjects at Peking University People's Hospital. The output-oriented DEA was selected and applied in the performance evaluation. The findings indicated the DEA ratio of every medical subject with the established method. Moreover, the method based on DEA can reflect the performance of medical subjects, and the analysis of the evaluation results can provide the management department of a hospital with shreds of evidence and references for policy-making of medical subjects' development.
[17] developed an integrated simulation and risk analysis in the sterilization service to take into account the effects of risks in the evaluation of the system performance. It consisted of creating an operating model of the sterilization service in order to describe the characteristics of the system. This system was subject to a multitude of risks, which can disrupt its operation. To take these risks into account, an analysis was carried out. The proposed model was simulated by a SIM. JS library using a JavaScript programming language. This simulation made it possible to evaluate the system performance in its different behavior modes (normal mode, degraded, reconfigured) [18]. introduced the domestic and overseas studies on the effectiveness of TCP for chronic diseases, and explored the key action links from three aspects, including functional training of multiple-joint guided by consciousness, relieving psychological risk factors, improving respiratory and digestive function, blood and lymph circulation through respiratory training, and regulation of nerve, metabolic, and immune system. Finally, the authors discussed how to integrate TCP into chronic disease management, and recommended that the practice methods and evaluation standards should be assessed academically.
[19] analyzed the technical foundation supporting the standardized healthcare system interoperability that will allow moving forward to e-health. They also reviewed the current usage of those foundational standards and advocate for their uptake by all infectious disease-related actors. Semantic data interoperability is one of the technical building blocks that support emerging digital medicine, e-health, and P4-medicine (predictive, preventive, personalized, and participatory). In a world where infectious diseases are on a trend to become hard-to-treat threats due to antimicrobial resistance, semantic data interoperability is part of the toolbox to fight more efficiently against those threats [20]. revealed that hand-washing with Povidone Iodine (PVP–I) based antiseptics is effective for the decontamination of skin, while PVP-I mouthwashes and gargles significantly reduce viral load in the oral cavity and the oropharynx. The importance of PVP-I was emphasized by its inclusion in the World Health Organization (WHO) list of essential medicines, and high potency for viral activity was observed against viruses of significant global concern, including hepatitis A and influenza, as well as the Middle-East respiratory syndrome and sudden acute respiratory syndrome coronaviruses. Together with its diverse applications in antimicrobial control, broad accessibility across the globe, and outstanding safety and tolerability profile, PVP-I offers an affordable, potent, and widely available antiseptic option.
[21] studied a comprehensive multi-criteria group decision-making model for hospital performance evaluation under uncertain conditions. The group BWM and fuzzy preference programming method have combined to create an applicable framework for group decision-making in which members of a decision making group have different expertise. The advantages of the proposed method addressed the integration of the group decision-making process in the form of a single model so that there is no need to calculate the consistency of the team decisions, separately. Finally, a case study was conducted on 5 hospitals in Tehran to demonstrate the applicability and effectiveness of the proposed approach [22]. evaluated the performance of the world health systems dealing with Coronavirus based on parametric and nonparametric statistical techniques according to “Population”, “GPD Per Capita”, “Total Recovered”, “Total Cases”, and “Total Deaths”. This descriptive cross-sectional study is performed on the World Population Review, Worldometer, and WHO data of the COVID-19 pandemic between 1 March, and 11 April 2020. Based on the obtained results, the efficient and inefficient health system units were identified. Moreover, they realized that 52 medical centers have not worked efficiently. The average efficiency of inefficient units was calculated at 0.30 whereas most of the studied countries did not operate efficiently due to the lack of optimal use of resources. Ineffective health system units call for greater attention from WHO in promoting health culture during the crisis management of common viruses. Therefore, there is a capacity to improve efficiency by 70%.
An intuitionistic fuzzy DEMATEL analysis was carried out by Ref. [23] in order to model the lockdown relaxation protocols during the COVID-19 pandemic in Philippines. According to the results, compliance with minimum public health standards, prohibition of mass gatherings, limited movement of persons, non-operation of category IV industries, non-operation of hotels or similar establishments and suspension of physical classes were found as the most critical protocols. Recently [24], performed a comparative study of three Multi-Criteria Decision-Making (MCDM) methods (i.e., VIKOR, COPRAS and TOPSIS) in order to evaluate the COVID-19 regional safety. They extracted the required data from Deep Knowledge Group (DKG) consortium and compared their findings with the ranking results presented in the DKG report. Finally, it was revealed that the proposed COPRAS yields the closest results to the results of the report.
[25] evaluated government strategies against the COVID-19 pandemic using q-rung orthopair fuzzy TOPSIS method. In this study, this decision process was considered as an MCDM problem which takes into account uncertainty. For this purpose, q-rung orthopair fuzzy sets were utilized to allow decision-makers to do their assessments in a wider space and efficiently deal with ambiguous information [26]. performed detection-based prioritization as a framework of multi-laboratory characteristics for asymptomatic COVID-19 carriers based on integrated Entropy–TOPSIS methods. Prioritization is a popular topic and a complex issue for patients with COVID-19, especially for asymptomatic carriers due to multi-laboratory criteria, criterion importance, and trade-off amongst these criteria. This study applied a new integrated decision-making framework to handle the prioritization of patients with COVID-19 and detect the health conditions of asymptomatic carriers. An additive utility assumption-based approach was studied by Ref. [27] to provide a multi-criterion decision support system for an accurate prediction of identified risk factors on certain well-defined input parameters. The methodology was validated empirically using the standard SEIR model (Susceptible, Exposed, Infected and Recovered). A comparative analysis with existing approaches was made to illustrate the potential of the proposed methodology including several parameters such as precision, recall, and F-score.
Recently [28], presented an extensive Multi-Criteria Group Decision-Making (MCGDM) method with psychological factors and a two-way influence relationship for selecting emergency medical providers. It was concluded that the proposed method is a good aid in emergency decision-making and can be extended and applied to other MCGDM problems [29]. investigated the impact of COVID-19 prevention policies on several aspects of supply chains under uncertainty. Supply chain operations are disrupted due to natural disasters or epidemics, and recently, supply chains have been suffering from obstacles and major challenges due to the spread of the COVID-19 epidemic around the world. In this work, an integrated framework based on BWM and TOPSIS was proposed to evaluate the impact of various policies on three main aspects of the supply chain; i.e., supply, demand, and logistics. Plithogenic sets were also utilized to provide a more accurate evaluation against uncertainty. Food industry, electronics industry, pharmaceutical industry, and textile industry were taken into account as the targets [30]. offered an integrated assessment methodology based on the distance-based Pythagorean fuzzy MCDM, TOPSIS, and Fuzzy Inference System (FIS) for the measurement of health care service quality. To validate the efficiency of the proposed method, a real case study problem was investigated by comparing 10 clinics of a private hospital. Five dimensions of Service Quality (SERVQUAL); i.e., tangibility, reliability, responsiveness, assurance, and empathy were addressed as the main criteria for evaluating the service quality levels of the clinics, and multiple sub-criteria were determined for each dimension to conduct a detailed analysis.
In line with and to continue the above-reviewed research works, the main objective of this research is to develop a model for analyzing the resilience of health system units against the COVID-19 crisis. However, the resiliency study has not been yet addressed in the previous studies. Therefore, the proposed framework is based on the application Best-Worst Method (BWM) with the aim of evaluating and ranking the resilient health system units for the management of the Coronavirus crisis in 2020. The BWM is one of the recently-developed MCDM techniques and a good alternative to the paired comparison-based methods. This technique provides more accurate solutions for models with more than 3 criteria and the possibility of multiple optimal solutions through converting the nonlinear programming model to a linear programming model [31]. The BWM is a simple and strong tool that can be utilized to tackle MCDM problems as well as determine the weight of each criterion [32]. Within well-known MCDM methods, BWM has been ranked as an approach yielding reliable results for optimal decision-making. For example, BWM resolved the shortcoming of Analytical Hierarchy Process (AHP) regarding too many pairwise comparisons among criteria [33].
The remaining sections of the study are organized as follows. Section 2 describes the proposed methodology. Section 3 elaborates on the findings of the research. The concluding remarks and recommendations are discussed in Section 4. Finally, Section 5 represents the limitations and outlook of the study.
2. Methodology
Our research study is descriptive-analytical and cross-sectional which has been carried out in 2020 to identify and rank the units of the resilient health system for dealing with Coronavirus using one of the novel MCDM techniques; i.e., BWM. The statistical population contains the health system units of the countries presented in the Worldometer report [34]. The required data were collected on 17 July 2020 at 8:33 GMT involving 215 countries, which are presented in Table A1. The two countries of Caribbean Netherlands and St. Barth were neglected due to the failure to record the start date of COVID-19. The best-worst technique is an algebraic method of decision-making on a relative scale. In this technique, different indicators and multiple criteria are used within a system to rank or determine the importance of different options in a decision-making process. MCDM methods are based on paired or binary comparisons of alternatives and decision-making criteria.
Evaluation criteria differ in different studies evaluating the performance of the health system units. Criterion selection plays an important role in the success of research analysis. Most researchers have utilized the common criteria of “Total Recovered”, “Total Deaths”, “Total Cases”, “Day of Infection”, “Active Cases” and “Serious” in evaluating the performance of health system units [[35], [36], [37]]. The importance of “Population” criterion has been also emphasized in valid documents [38,39].
The criterion is positive when its best value is higher and it is negative when its worst value is higher. In the other words, the best ideal positive solution or the worst negative solution are considered for the criterion. The criteria of “Total Recovered” and “Total Tests” have been considered positive and other criteria considered negative. The “Total Recovered” criterion has been positive because health is the center of social, economic, political and cultural development of all human societies and has special importance in the development of infrastructure of different sectors of society. The criterion of “Total Tests” has been considered positive because it is very important to perform COVID-19 tests in accordance with the guidelines announced by WHO in order to separate patients from healthy people to control the disease.
To extract the mechanisms of evaluation indicators, the BWM questionnaire was distributed among 20 expert members of the medical council. In the BWM technique, the compatibility rate is used to evaluate the questionnaire reliability. The most and the least resilient health system units are identified using BWM. The best-worst technique involves five main steps [40]:
-
•
First step: a set of decision criteria {C 1, C 2, …, C n} are determined and used to achieve the target decision.
-
•
Second step: decision makers choose the best and worst criteria according to the related issue and views. The best criterion indicates the most desirable or important criterion for decision-making, and the worst criterion has the least desirability and importance for decision-making.
-
•
Third step: paired comparisons are made between the best criterion and other criteria. The preference of the best criterion over other indicators is determined using numbers 1 to 9 (the number 9 means completely important and the number 1 means the same importance) and Best-to-Others (BTO) matrix is formed. The purpose of this step is to determine the priority and importance of the best criterion over other criteria. The vector (a Bj) indicates the superiority of the best criterion B over criterion . Hence, a BB = 1 and we have:
| AB= (aB1,aB2, …,aBn). | (1) |
-
•
Fourth step: paired comparisons are made between other criteria and the worst criterion. In the step, the priority and importance of other criteria over the worst criterion are determined using numbers 1 to 9 and Others-to-Worst (OTW) matrix is formed. The vector (a jW) indicates the superiority of criterion over the worst criterion . Therefore, a WW = 1 and we have:
| AW = (a1W, a2W, …, anW)T. | (2) |
-
•
Fifth step: the optimal values of weights (, …, ) are determined in this step. The optimal weight of criteria must be established for each of the pairs of Equation (3).
| (3) |
To establish these conditions for all , a solution should be found in which the maximum absolute difference is and () is the minimum. Model (4) is obtained by considering the positive values and conditions of the total weights:
| (4) |
Model (4) can be converted into Model (5) as follow:
| (5) |
where ξ* is used to determine the compatibility ratio. Whatever the amount of ξ* is higher, the value of the compatibility ratio is increased and the reliability of comparisons is decreased. The comparisons are fully consistent when the relation a Bj × a jW = a BW is established. In the equation, (a Bj), (a jW) and (a BW) represent the priorities of the best criterion over criterion , criterion over the worst criterion and priority of the best criterion over the worst criterion, respectively.
According to various researchers, the evaluation process consists of several phases, which are common in identifying evaluation criteria and decreasing the number of criteria. In the following and after reviewing various studies, a summary of performance measurement and resilience criteria of health system units were extracted and presented in Table A1 based on the data of Worldometer database.
MCDM problems require evaluation and determination of the functional value of understudy subjects and phenomena, which needs screening, identification and selection of key and important evaluation indicators. Screening problems commonly involve the participation of several people in the decision-making process in addition to having the feature of minimal information. After consensus of the experts' opinions, the evaluation indicators of this study were screened using the Content Validity Ratio (CVR) technique suggested by Ref. [41] according to Table 2. For more information, please see Ref. [42].
Table 2.
Identifying the final criteria through the Lawshe technique.
| No. | Symbol | Criteria | Definitions | CVR | Accepted |
|---|---|---|---|---|---|
| 1 | C1 | Total Deaths | Cumulative number of deaths among detected cases | 0.91 | ✓ |
| 2 | C2 | Total Cases | Total cumulative count of detected and laboratory-confirmed positive | 1 | ✓ |
| 3 | C3 | Serious | Number of patients currently being treated in the Intensive Care Unit (ICU) | 0.91 | ✓ |
| 4 | C4 | Active Cases | Current number of people detected and confirmed to be infected with the virus | 0.91 | ✓ |
| 5 | C5 | Day of Infection | Period from the first evident manifestation of an infectious disease to the final host reaction | 0.62 | ✓ |
| 6 | C6 | Total Recovered | Number of infected people making a recovery and get healed | 0.91 | ✓ |
| 7 | C7 | Total Tests | Total COVID-19 PCR tests | 0.91 | ✓ |
| 8 | C8 | Population | Total number of people or inhabitants in a country or region | 0.38 | × |
3. Findings
3.1. Criteria definition
Identifying the effective criteria is the most important step of selection and prioritization. In this study, the effective criteria for evaluating the resilience of health system units were identified and extracted through similar studies and available data. In this step, the content validity analysis questionnaire was distributed among medical experts with expertise and experience in the relevant field to screen and decrease the number of indicators (cf. Table A2). The quantitative technique of Lawshe was used to decline the uncertainty. The results of the data analysis are given in Table 2. According to the findings, the final criteria of "Total Cases”, “Total Recovered”, “Total Deaths”, “Active Cases”, “Serious”, “Total Tests” and “Day of Infection” are identified.
To proceed with the evaluations, Equation (6a), (6b) denotes how to compute CVR:
| (6a) |
where stands for the number of experts who chose the required dimension. Moreover, denotes the total number of experts. The validity for 20 experts must be at least 0.42 [43]. Table 1 represents the demographic information about the experts.
Table 1.
Demographic information of research experts.
| Gender | Women: 8 (4%) |
|---|---|
| Men: 12 (6%) | |
| Place of work | University of medical sciences: 10 (50%) |
| Health ministry: 7 (35%) | |
| Science ministry: 3 (15%) | |
| Position | Head of the pulmonology subspecialty hospital (1) |
| Deputy of training of nephrology and pulmonology research specialty (1) | |
| Infection control officer (3) | |
| Patient safety officer (3) | |
| Hospital matron (2) | |
| Senior supervisor (2) | |
| Emergency head nurse (2) | |
| ICU head nurse (2) | |
| Emergency doctors (2) | |
| ICU resident doctors (2) |
3.2. Determining the most and least important criteria
Given the wide range of susceptibility and different features of epidemic diseases, the criteria of "Total Cases" and "Day of Infection" were identified by the decision-making team as the most and least important criteria, respectively.
3.3. Identifying the preference of best criterion over other criteria
In this step, experts evaluated the preference number of the best criterion over other criteria through a 9-point Likert scale. Likert scaling is a bipolar scaling method, measuring either a positive or negative response to a statement. Since the psychologist Rensis Likert invented the Likert scale in 1932, scholars have been trying to optimize the number of scale points. Scales from anywhere between just two points up to a whopping 101 points were suggested at one time or another. Table 3 represents the BTO matrix, which has been formed based on experts' opinions. To form the matrix, it is necessary to calculate the preference number of the best criterion over other criteria through optimal weight obtained from the arithmetic mean of the experts' opinions.
Table 3.
Paired comparisons between the most important criteria and other criteria.
| Criteria | C1 | C2 | C3 | C4 | C5 | C6 | C7 | j |
|---|---|---|---|---|---|---|---|---|
| Best criterion = C2 = Total Cases | 3 | 1 | 5 | 4 | 9 | 6 | 4 | aBj |
3.4. Identifying the preference of other criteria over the worst criterion
The preference number of other criteria over the worst criterion was also determined by experts. The OTW matrix is shown in Table 4 based on the experts' opinions. To form an OTW matrix, it is necessary to calculate the preference number of other criteria over the worst criterion through optimal weight obtained from the arithmetic mean of the experts' opinions.
Table 4.
Paired comparisons between other criteria and the least important criterion.
| Criteria | Worst Criterion = Day of Infection = C5 |
|---|---|
| C1 | 3 |
| C2 | 9 |
| C3 | 2 |
| C4 | 3 |
| C5 | 1 |
| C6 | 2 |
| C7 | 3 |
| j | ajW |
3.5. Calculating the optimal weight of criteria
According to the opinions of experts, the optimal weight of criteria was calculated by solving the BWM optimization model in Lingo 12.0 Software. The results of calculations and the optimal weights of evaluation criteria are shown in Table 5 .
Table 5.
Optimal weight of evaluation criteria for the resilience of health system units based on the BWM.
| Symbol | Criteria | wj* |
|---|---|---|
| C1 | Total Deaths | 0.140 |
| C2 | Total Cases | 0.421 |
| C3 | Total Recovered | 0.084 |
| C4 | Serious | 0.117 |
| C5 | Day of Infection | 0.045 |
| C6 | Total Tests | 0.076 |
| C7 | Active Cases | 0.117 |
| ξ* | 0.394 | |
| ConsistencyIndex | 5.23 | |
| ConsistencyRatio | 0.075 | |
Matrix compatibility was almost confirmed with the relation a Bj × a jW ≈ 9. According to the results of Table A3, the compatibility rate was calculated at 0.075, indicating a good compatibility and stability of comparisons. The results of criteria prioritization by experts are displayed in Table 5 and Fig. 1 . The criteria of “Total Cases”, “Total Deaths”, “Serious”, “Active Cases”, “Total Recovered”, “Total Tests” and “Day of Infection” were identified as the most important effective criteria in evaluating the resilience of health system units, respectively.
Fig. 1.
Diagram of prioritizing the evaluation criteria for the resilience of health system units.
3.6. Calculating the resilience score of the world's health system units
By applying the optimal weights in the standard score of each supplier (represented by ), the final score of the health system units would be calculated according to Equation (6a), (6b).
| (6b) |
The tangible results of the evaluation framework for health system units' resilience are given in Table A3. The numbers obtained for each unit of the health system indicate the status or performance of that unit of the health system in the desired criterion and period. Equation (6a), (6b) of all indicators shows the overall performance of the health system unit.
According to the findings, ten countries of China, USA, Rwanda, UK, India, Germany, Italy, Spain, UAE, and Australia were identified as the best models for worldwide resilience benchmarking, respectively. The BWM provides a framework for the health system units and identifies the activities of the best health system units that distinguishing the differences between available health system units with the best health system unit can indicate how to bridge the existing gaps. In fact, modeling is a tool for continuous improvement and can be used by various types of health system units. The resilience of model health system units was selected and introduced based on the following cases. Health systems can vary significantly from country to country. Health systems around the world can be comprised based on the criteria of health distribution in populations and accountability and equitable provision of health services. Then, the resilience score of health system units has been evaluated by the separation of each continent. The goals of health systems are public health and meeting the expectations of the population, which have a significant effect on the quality of life. Quality of life is one of the most important and effective factors that includes an efficient and accessible health system and health care [44].
3.6.1. Calculating the resilience score of Europe's health system units
Europe is one of the five continents of the world in the Northern Hemisphere and the second smallest continent in the world after Oceania, which is known as the Green Continent. Despite its relatively small area, Europe is the second most populous continent in the world after Asia. European countries have a better economic situation compared to many other countries. On the other hand, their medical and pharmaceutical history is much longer compared to other countries. However, European countries faced serious problems in dealing with COVID-19 in the terms of medical care and hospital and pharmaceutical facilities. The outbreak of Coronavirus is an important benchmark for countries. The resilience evaluation framework was calculated for the health system units in Europe. The numbers obtained for each health system unit indicate the performance of the health system unit. The dispersion diagram of resilience evaluation for the health system units of European countries is shown in Fig. 2 . According to the findings, ten countries of Romania, UK, Germany, Italy, Spain, Poland, France, Denmark, Portugal, and Belgium were identified as the best models for European resilience benchmarking, respectively. According to the results, it is recommended to model the resilience of “Romania” health system unit.
Fig. 2.
Dispersion diagram of resilience evaluation of health system units in Europe.
3.6.2. Calculating the resilience score of America's health system units
3.6.2.1. North America
North America is the northern part of the American continent and has been divided into three countries of Canada, the United States and Mexico. The resilience evaluation framework was calculated for the health system units in North America. The numbers obtained for each health system unit indicate the performance of the health system unit. The dispersion diagram of resilience evaluation for the health system units of North American countries is depicted in Fig. 3 .
Fig. 3.
Dispersion diagram of resilience evaluation of health system units in North America.
According to the findings, ten countries of USA, Canada, Cuba, El Salvador, Cayman Islands, Jamaica, Bermuda, Guadeloupe, Barbados and Grenada in North America were identified as the best models for resilience benchmarking, respectively. According to the results, it is recommended to model the resilience of “USA” health system unit.
3.6.2.2. South America
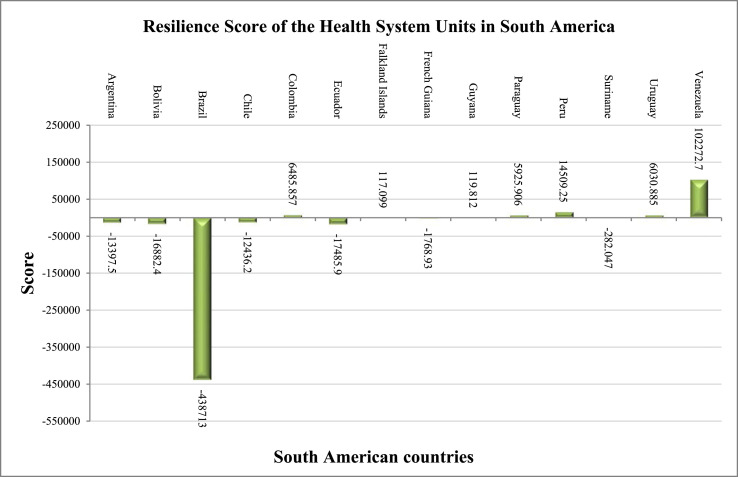
South America is the southern part of the Americas. South America is sometimes considered a separate continent. South America is located in the western hemisphere and most of its area is in the southern hemisphere. South America is bounded by the Pacific Ocean on the west and by the Atlantic Ocean on the north and east. The resilience evaluation framework was calculated for the health system units in South America. The numbers obtained for each health system unit indicate the performance of the health system unit. The dispersion diagram of resilience evaluation for the health system units of South American countries is represented in Fig. 4 .
Fig. 4.
Dispersion diagram of resilience evaluation of health system units in South America.
According to the findings, ten countries of Venezuela, Peru, Colombia, Uruguay, Paraguay, Guyana, Falkland Islands, Suriname, French Guiana and Chile in South America were identified as the best models for resilience benchmarking, respectively. According to the results, it is recommended to model the resilience of “Venezuela “health system unit.
3.6.3. Calculating the resilience score of Asian health system units
Asia is the largest continent in the world with an almost triangular shape and has many peninsulas. There is a significant difference between developed and developing nations in terms of access to public health and healthcare innovations. In the developing world (Asia, Africa and Latin America), public health infrastructure is still evolving. It is the shortage possibility of well-trained health workforce and sufficient financial resources to provide medical care and disease prevention, even at a basic level.
The resilience evaluation framework was calculated for the health system units in Asia. The numbers obtained for each health system unit indicate the performance of the health system unit. The dispersion diagram of resilience evaluation for the health system units of Asian countries is shown in Fig. 5 . According to the results, the countries of China, India, UAE, Turkey, S. Korea, Kazakhstan, Uzbekistan, Saudi Arabia, Israel, Malaysia, Singapore and Iran in Asia were identified as the best models for resilience benchmarking, respectively. According to the results, it is recommended to model the resilience of “China” health system unit.
Fig. 5.
Dispersion diagram of resilience evaluation of health system units in Asia.
3.6.4. Calculating the resilience score of African health system units
Africa is the second largest continent in the world after Asia. Africa is located on both sides of the equator and covers different climatic regions. In general, the health system in African countries is weak. The resilience evaluation framework was calculated for the health system units in Africa. The numbers obtained for each health system unit indicate the performance of the health system unit. The dispersion diagram of resilience evaluation for the health system units of African countries is shown in Fig. 6 .
Fig. 6.
Dispersion diagram of resilience evaluation of health system units in Africa.
According to the results, the countries of Morocco, Réunion, South Africa, Uganda, Ghana, Ethiopia, Mauritius, Kenya, Zimbabwe and Tunisia in Africa were identified as the best models for resilience benchmarking, respectively. According to the results, it is recommended to model the resilience of “Morocco” health system unit.
3.6.5. Calculating the resilience score of Oceanic health system units
Oceania is one of the continents of the world that includes various groups of Pacific islands. It is the smallest continent in the world. The resilience evaluation framework was calculated for the health system units in Oceania. The numbers obtained for each health system unit indicate the performance of the health system unit. The dispersion diagram of resilience evaluation for the health system units of Oceanic countries is shown in Fig. 7 .
Fig. 7.
Dispersion diagram of resilience evaluation of health system units in Oceania.
According to the results, the countries of Australia, New Zealand, New Caledonia, Papua New Guinea, French Polynesia and Fiji in Oceania were identified as the best models for resilience benchmarking, respectively. According to the results, it is recommended to model the resilience of “Australia” health system unit.
4. Discussion, conclusion and recommendations
The units of the health system are affected by many factors because they are in a complex political, economic, social and environmental structure and operate at the local, national and international levels. The shocks in health sectors can be sudden and extremely unexpected. In such conditions, the official services should be well planned and coordinated by the units of the health system so that the provision of health services to the people is not stopped. Health system units with the ability to provide health services will rapidly face an increase in demand for health services. Therefore, it is necessary to provide the facilities needed for serving the services in these units. Managers and personnel of health system units should receive the necessary training in the terms of providing emergency services to a large number of patients, patient prioritization and how to deal with patients. Most health system units may not have the specialized and required personnel and equipment for this type of sudden event [45]. Therefore, a network of specialized health system units should be established in this field. Presenting a model of health system units for providing necessary training and conducting specialized research can strengthen the balanced capacity of all health system units in that country to deal with the effects of such disasters. Health system units must be highly resilient to deal with these crises. Resilience helps to counteract unexpected shocks, and overcome crises without serious damage. Resilience reflects the health system unit's ability to counteract, adapt and change when faced with a shock so that it can maintain its structure and perform its current activities. The health system unit is resilient when it can provide health services during and after crises and disasters and save human lives. The resilient health system unit requires government support, adoption of related laws and policies, careful planning, needs assessments, and the provision of resources and facilities. A resilient health system unit needs a sufficient number of manpower, equipment and supplies and medicines, a strong health information system, sufficient financial resources and a capable management and leadership system to be able to provide high-quality and equitable services in the event of disasters and crises.
Given the high mortality rate of Coronavirus infection, this issue should be considered as a serious global health problem. Therefore, it is necessary for the WHO to develop appropriate intervention programs in order to prevent and minimize the incidence of the virus and periodic evaluation of prevention programs in the world. It is recommended to develop a comprehensive protocol by an international observer such as WHO. Developing protocols at the time of crisis can improve the performance of health care centers. For example, limiting the daily movement of individuals, operation of hotels or similar organizations, suspension of face-to-face classes, and finally, interdiction of mass gatherings are highly recommended to be included among the main protocols based on the practical experience of resilient countries. In this regard, the resilience study of different countries helps WHO enact an organized policy using efficient protocols. This study tried to address these requirements by evaluating and ranking the worldwide resilient health system units for the management of the COVID-19 pandemic based on real data collected in 2020. Using CVR calculations, the main criteria were identified, and then, resilience scores of different countries were calculated with the help of BWM as one of the most efficient MCDM tools.
In fact, it is possible to improve the performance of all units of the world health system through the proposed model by improving the performance and eliminating the risks of COVID-19 damages. Resilience of performance in each unit of the health system can lead to the resilience of all units of the health system. The proposed model aimed to develop the performance sustainability of all units of the world health system by creating interaction and communication between each unit of the health system. According to the measurements, the following results are discussable:
-
i.
Ten countries of China, USA, Rwanda, UK, India, Germany, Italy, Spain, UAE and Australia were identified as the best models for worldwide resilience benchmarking, respectively. Successful treatment of patients depends on a wide range of factors including timely diagnosis, quality of care, modern and advanced equipment, training and upgrading of medical staff, medical center budget and medical center self-government of the health system unit in addition to the competence of medical staff professionals.
-
ii.
According to the findings of this study, 10 countries of Romania, UK, Germany, Italy, Spain, Poland, France, Denmark, Portugal, and Belgium in Europe were identified as the best models for resilience benchmarking.
-
iii.
The countries of USA, Canada, Cuba, El Salvador, Cayman Islands, Jamaica, Bermuda, Guadeloupe, Barbados and Grenada were identified as the best models for resilience benchmarking in North America. The countries of Venezuela, Peru, Colombia, Uruguay, Paraguay, Guyana, Falkland Islands, Suriname, French Guiana, and Chile were also identified as the best models for resilience benchmarking in South America.
-
iv.
The countries of China, India, UAE, Turkey, S. Korea, Kazakhstan, Uzbekistan, Saudi Arabia, Israel, Malaysia, Singapore, and Iran were identified as the best models for resilience benchmarking in Asia, respectively.
-
v.
The countries of Morocco, Réunion, South Africa, Uganda, Ghana, Ethiopia, Mauritius, Kenya, Zimbabwe and Tunisia were identified as the best models for resilience benchmarking in Africa.
-
vi.
In Oceania, the countries of Australia, New Zealand, New Caledonia, Papua New Guinea, French Polynesia, and Fiji were identified as the best models for resilience benchmarking, respectively.
-
vii.
Death rate can be a reflection of the social and economic conditions of society and the extent to which individuals enjoy health and living standards. On the other hand, death rate depends on the age pyramid of a country's population, underlying diseases as well as geographical location and environmental and climatic conditions.
-
viii.
Health system units with lower ranks can improve the gap between health system units by adopting appropriate policies for improving the indicators with higher weights. The matter can increase the productivity of medical resources and increase community satisfaction and health.
-
ix.
Considering the obtained importance of indicators in health system units, it is necessary to prioritize and allocate resources based on the obtained results.
Finally, we can conclude that by conducting this research, in addition to the delineation of functional patterns to the top health managers, it is also possible to plan more accurately to optimally develop the capacity of health care services and save resources.
5. Limitations and outlook
As well as each research study, there are two main limitations in this work which can be tackled considering the following future research directions:
-
I.
While pharmaceuticals and essential medical equipment are immune from economic sanctions, the sanctions' direct and indirect consequences have harmed the economic system, resulting in significant commerce, manufacturing, insurance, and investment limitations. In the short term, sanctions may not cause substantial mortality and morbidity, but their chronic and long-term impacts may be more significant than their acute ones. The current analysis makes no allowance for the limits of sanctions in the healthcare system of a country.
-
II.
The COVID-19 crisis has left governments at all levels in a precarious situation. The regional and local impacts of COVID-19 are highly heterogeneous and have significant implications for crisis management and political responses. The effects of this pandemic can be seen in various health, economic, social and financial dimensions, which can be further studied [46].
-
III.
Since this study has been performed based on the primary data on the peak of Coronavirus disease on 17 July 2020 and arrived at its conclusions by relying on the accuracy and authenticity of data released by countries, there might be some difference between the obtained results and the actual status. In this regard, improved data policies provide a more accurate evaluation of the impacts of containment measures and better decision-making by public health authorities [47]. Therefore, the suggested methodology can be re-implemented according to the more accurate and updated data and also compared to the current status,
-
IV.
There are also other alternatives to conduct the identification and prioritization steps and to be compared with the suggested BWM, especially in uncertain environments. For example, please see fuzzy MCDM methods [[48], [49], [50]], neutrosophic-based MCDM methods [51], regression analysis to model the relationships between different criteria and variables [[52], [53], [54], [55]].
Author statement
Nazila Adabavazeh: Writing - Original Draft, Conceptualization, Methodology and Software. Mehrdad Nikbakht: Reviewing and Editing, Data curation and Validation. Erfan Babaee Tirkolaee: Reviewing and Editing, Supervision, Visualization and Investigation.
Biographies

Nazila Adabavazeh
PhD Candidate in Industrial Engineering, Islamic Azad University, Najafabad, IRAN
M.Sc. in Industrial Engineering, Islamic Azad University, Najafabad, IRAN
B.Sc. in Software Engineering, Islamic Azad University, Najafabad, IRAN
Honors and Awards
o The Best National Young Manager, House of Industry, Mine and trade of Isfahan Youth
o The Best Young Technology Manager, House of Industry, Mine and trade of Iranian Youth
Research Interests: Supply Chain, Management, Maintenance and Artificial Intelligence

Dr. Mehrdad Nikbakht
Record of Academic Accomplishments:
Ph.D. - Industrial Engineering, University Putra Malaysia, Serdang, Malaysia, 2008-12
M.Sc. - Industrial Engineering - Industrial Engineering (System Management & Productivity), Tehran, Iran, 2002-04
B.Sc. - Mechanical Engineering - Solid Design, Esfahan,Iran,1994-98
Work Experiences:
• Head Of The Post Graduate Department Of Industrial Engineering, Islamic Azad University Of Najafabad – Iran, (May/2019 – May/2021).
• Head Of The Department Of Industrial Engineering, Islamic Azad University Of Najafabad – Iran, (September/2016 - September/2017).
• Assistant Professor Of Industrial Engineering, Islamic Azad University Of Najafabad – Iran, (October/2014 - Now).
Research Interests: Supply Chain, Maintenance, Production, Planning, Modeling and Optimization.

Erfan Babaee Tirkolaee obtained a BSc. (2012) and MSc. (2014) in Industrial Engineering from Isfahan University of Technology in Isfahan, Iran. Then, he received a Ph.D. degree (2019) in Industrial Engineering from Mazandaran University of Science and Technology in Babol, Iran. Dr. Erfan Babaee Tirkolaee is currently an assistant professor in the Department of Industrial Engineering at Istinye University in Istanbul, Turkey. Meanwhile, he worked as a Quality Assurance consultant and Training manager in some automotive industries in Iran, and could go through different relevant courses like ISO 9001: 2015 and IATF 16949-2016. He has been verified as a scientific elite by the Young Researchers and Elite Club in 2017 and Iran's National Elites Foundation in 2018. He has published more than 80 papers in high-quality journals, including IEEE Transactions on Fuzzy Systems, Expert Systems with Applications, Waste Management, Journal of Cleaner Production, Computers & Industrial Engineering, Annals of Operations Research, etc. His eleven papers have been selected as ESI Highly Cited Papers. He has been serving as a chair/organizing & committe member/keynote speaker in several prestigious international conferences, and as a reviewer in many reputed WoS journals such that he has been recognized as a Top Peer Reviewer in 2 of the Essential Science Indicators research areas by Clarivate WoS. Dr. Erfan Babaee Tirkolaee is currently an Associate Editor of Expert Systems with Application (Elsevier) and an Editorial Advisory Board member of Management Decision (Emerald). Moreover, he has been serving on the guest editorial board in several journals such as Renewable and Sustainable Energy Reviews (Elsevier), Annals of Operations Research (Springer) and Environmental Science and Pollution Research (Springer). Recently, he has been featured among the "World’s Top 2% Researchers/Scientists in 2021" list identified by Elsevier BV, Stanford University.
His research interests mainly include Waste Management, Supply Chain Management and Transportation/Routing Problems, Operations Research, Fuzzy Systems, Solution Algorithms, Artificial Intelligence.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.seps.2022.101452.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- 1.Hick J.L., Hanfling D., Wynia M.K., Pavia A.T. Nam Perspectives; 2020. Duty to plan: health care, crisis standards of care, and novel coronavirus SARS-CoV-2; pp. 2578–6865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A.…Phillips J.P. Fair allocation of scarce medical resources in the time of Covid-19. The New. England Journal of Medicine. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 3.Gostin L.O., Friedman E.A., Wetter S.A. Responding to COVID-19: how to navigate a public health emergency legally and ethically. Hastings Cent Rep. 2020;50(2):8–12. doi: 10.1002/hast.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nuzzo J.B., Meyer D., Snyder M., Ravi S.J., Lapascu A., Souleles J.…Bishai D. What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Publ Health. 2019;19(1):1–9. doi: 10.1186/s12889-019-7707-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fleming Billy. The resilience dividend: being strong in a world where things go wrong, by judith rodin; and the social roots of risk: producing disasters, promoting resilience, by kathleen tierney. J Am Plann Assoc. 2015;81(4):316–317. [Google Scholar]
- 6.Fridell M., Edwin S., Von Schreeb J., Saulnier D.D. Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Pol Manag. 2020;9:6–16. doi: 10.15171/ijhpm.2019.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKenzie A., Abdulwahab A., Sokpo E., W Mecaskey J. Building a resilient health system: lessons from northern Nigeria. London. 2015. http://www.ids.ac.uk/files/dmfile/IDSOpenDocsStandardTermsOfUse.pdf Report No: 1781182299 Contract No: 454.
- 8.Huang C., Wang M., Rafaqat W., Shabbir S., Lian L., Zhang J.…Song W. Socio-Economic Planning Sciences; 2021. Data-driven test strategy for COVID-19 using machine learning: a study in lahore, Pakistan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abimbola S., Topp S.M. Adaptation with robustness: the case for clarity on the use of ‘resilience’in health systems and global health. BMJ global health. 2018;3 doi: 10.1136/bmjgh-2018-000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yao H., Liu W., Wu C.H., Yuan Y.H. Socio-Economic Planning Sciences; 2021. The imprinting effect of SARS experience on the fear of COVID-19: the role of AI and big data. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kruk M.E., Myers M., Varpilah S.T., Dahn B.T. What is a resilient health system? Lessons from Ebola. Lancet. 2015;385(9980):1910–1912. doi: 10.1016/S0140-6736(15)60755-3. [DOI] [PubMed] [Google Scholar]
- 12.Witter S., Hunter B. Resilience of health systems during and after crises-what does it mean and how can it be enhanced? Health systems during and after crisis: evidence for better policy and practice-brief. 2017;1 [Google Scholar]
- 13.Bjurling‐Sjöberg P., Göras C., Lohela-Karlsson M., Nordgren L., Källberg A.S., Castegren M.…Ekstedt M. Resilient performance in healthcare during the COVID-19 pandemic (ResCOV): study protocol for a multilevel grounded theory study on adaptations, working conditions, ethics and patient safety. BMJ Open. 2021;11(12) doi: 10.1136/bmjopen-2021-051928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dickmann P., Abraham T., Sarkar S., Wysocki P., Cecconi S., Apfel F., Nurm Ü.K. Risk communication as a core public health competence in infectious disease management: development of the ECDC training curriculum and programme. Euro Surveill. 2016;21(14) doi: 10.2807/1560-7917.ES.2016.21.14.30188. [DOI] [PubMed] [Google Scholar]
- 15.June K.J., Choi E. Infection control of hospital nurses: cases of middle east respiratory syndrome. Korean Journal of Occupational Health Nursing. 2016;25(1):1–8. [Google Scholar]
- 16.Liang G., Wang D., Wang B., Yuan L., Zhang H., Tao X.U. Evaluation of the research performance based on DEA and discussion of corresponding measures of medical subjects in hospital. Chinese Journal of Medical Science Research Management. 2017;30(3):177–180. [Google Scholar]
- 17.Di Mascolo M., Flaus J.M., Daadaa M. 9ème Conférence Francophone en gestion et ingénierie des systems hospitaliers, GISEH 2018. 2018. A new integrated approach for risk analysis and performance evaluation of a hospital sterilization service. [Google Scholar]
- 18.Wang N., Guo Y. Traditional Chinese practice, a promising integrative intervention for chronic non-infectious disease management. Chin J Integr Med. 2018;24(12):886–890. doi: 10.1007/s11655-018-2572-7. [DOI] [PubMed] [Google Scholar]
- 19.Gansel X., Mary M., van Belkum A. Semantic data interoperability, digital medicine, and e-health in infectious disease management: a review. Eur J Clin Microbiol Infect Dis. 2019;38(6):1023–1034. doi: 10.1007/s10096-019-03501-6. [DOI] [PubMed] [Google Scholar]
- 20.Eggers M. Infectious disease management and control with povidone iodine. Infect Dis Ther. 2019;8(4):581–593. doi: 10.1007/s40121-019-00260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amiri M., Hashemi-Tabatabaei M., Ghahremanloo M., Keshavarz-Ghorabaee M., Zavadskas E.K., Antucheviciene J. A new fuzzy approach based on BWM and fuzzy preference programming for hospital performance evaluation: a case study. Appl Soft Comput. 2020;92 [Google Scholar]
- 22.Adabavazeh N., Nikbakht M., Amirteimoori A. Envelopment analysis for global response to novel 2019 coronavirus-SARS-COV-2 (COVID-19) Journal of Industrial Engineering and Management Studies. 2020;7(2):1–35. [Google Scholar]
- 23.Ocampo L., Yamagishi K. Modeling the lockdown relaxation protocols of the Philippine government in response to the COVID-19 pandemic: an intuitionistic fuzzy DEMATEL analysis. Soc Econ Plann Sci. 2020;72 doi: 10.1016/j.seps.2020.100911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hezer S., Gelmez E., Özceylan E. Comparative analysis of TOPSIS, VIKOR and COPRAS methods for the COVID-19 regional safety assessment. Journal of Infection and Public Health. 2021;14(6):775–786. doi: 10.1016/j.jiph.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alkan N., Kahraman C. Evaluation of government strategies against COVID-19 pandemic using q-rung orthopair fuzzy TOPSIS method. Appl Soft Comput. 2021;110 doi: 10.1016/j.asoc.2021.107653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Albahri A.S., Hamid R.A., Albahri O.S., Zaidan A.A. Detection-based prioritisation: framework of multi-laboratory characteristics for asymptomatic COVID-19 carriers based on integrated Entropy-TOPSIS methods. Artif Intell Med. 2021;111 doi: 10.1016/j.artmed.2020.101983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aggarwal L., Goswami P., Sachdeva S. Multi-criterion intelligent decision support system for COVID-19. Appl Soft Comput. 2021;101 doi: 10.1016/j.asoc.2020.107056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu S., He X., Chan F.T., Wang Z. An extended multi-criteria group decision-making method with psychological factors and bidirectional influence relation for emergency medical supplier selection. Expert Syst Appl. 2022;202 doi: 10.1016/j.eswa.2022.117414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sotoudeh-Anvari A. Applied Soft Computing; 2022. The applications of MCDM methods in COVID-19 pandemic: a state of the art review; p. 109238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karasan A., Erdogan M., Cinar M. Socio-Economic Planning Sciences; 2022. Healthcare service quality evaluation: an integrated decision-making methodology and a case study; p. 101234. [Google Scholar]
- 31.Rezaei J., Kothadiya O., Tavasszy L., Kroesen M. Quality assessment of airline baggage handling systems using SERVQUAL and BWM. Tourism Manag. 2018;66:85–93. [Google Scholar]
- 32.Pamučar D., Ecer F., Cirovic G., Arlasheedi M.A. Application of improved best worst method (BWM) in real-world problems. Mathematics. 2020;8(8):1342. [Google Scholar]
- 33.Bafail O.A., Abdulaal R.M. 2022 the 3rd international conference on industrial Engineering and industrial management. 2022, January. A combined BWM-TOPSIS approach versus AHP-TOPSIS approach: an application to Solid Waste management; pp. 27–33. [Google Scholar]
- 34.Worldometer Country, total Cases,Total deaths, total recovered, active cases, serious, total tests, population. 2020. https://www.worldometers.info/coronavirus Retrieved from: 10:13 GMT]
- 35.Mohammadkarim B., Jamil S., Pejman H., Seyyed M.H., Mostafa N. Combining multiple indicators to assess hospital performance in Iran using the Pabon Lasso Model. Australas Med J. 2011;4(4):175. doi: 10.4066/AMJ.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garcia-Lacalle J., Martin E. Rural vs urban hospital performance in a ‘competitive’public health service. Soc Sci Med. 2010;71(6):1131–1140. doi: 10.1016/j.socscimed.2010.05.043. [DOI] [PubMed] [Google Scholar]
- 37.Tavakoli N., Kasnaviyeh M.H., Yasinzadeh M., Amini M., Nejad M.M. Evaluation of appropriate and inappropriate admission and hospitalization days according to appropriateness evaluation protocol (AEP) Arch Iran Med. 2015;18(7) [PubMed] [Google Scholar]
- 38.See K.F., Yen S.H. Does happiness matter to health system efficiency? A performance analysis. Health Economics Review. 2018;8(1):1–10. doi: 10.1186/s13561-018-0214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ECDPC Death rate. 2020. https://www.ecdc.europa.eu/en/current-risk-assessment-novel-coronavirus-situation Retrieved from:
- 40.Rezaei J. Best-worst multi-criteria decision-making method. Omega. 2015;53:49–57. [Google Scholar]
- 41.Lawshe C.H. A quantitative approach to content validity. Person Psychol. 1975;28(4):563–575. [Google Scholar]
- 42.Gilbert G.E., Prion S. Making sense of methods and measurement: lawshe's content validity index. Clinical Simulation in Nursing. 2016;12(12):530–531. [Google Scholar]
- 43.Adabavazaeh N., Nikbakht M. 2019 15th Iran international industrial engineering conference (IIIEC) IEEE; 2019. Interpretive structural modeling analysis of reverse supply chain critical success factors in air industry; pp. 99–105. [Google Scholar]
- 44.Tamornpark R., Utsaha S., Apidechkul T., Panklang D., Yeemard F., Srichan P. Quality of life and factors associated with a good quality of life among diabetes mellitus patients in northern Thailand. Health Qual Life Outcome. 2022;20(1):1–11. doi: 10.1186/s12955-022-01986-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.WHO Toolkit for assessing health-system capacity for crisis management. 2012. https://www.euro.who.int/__data/assets/pdf_file/0008/157886/e96187.pdf Preuzeto sa:
- 46.Allain-Dupré D., Chatry I., Michalun V., Moisio A. The territorial impact of COVID-19: managing the crisis across levels of government. OECD Policy Responses to Coronavirus (COVID-19) 2020;10:1620846020–1909698535. [Google Scholar]
- 47.Starnini M., Aleta A., Tizzoni M., Moreno Y. Impact of data accuracy on the evaluation of COVID-19 mitigation policies. Data and Policy. 2021;3 [Google Scholar]
- 48.Janaki D.M., Mirzazadeh A., Janaki M.M. Reducing barriers to the implementation of strategic management by providing improved strategies: using fuzzy QFD applied to Petropars Company. Int J Ind Syst Eng. 2019;31(4):535–557. [Google Scholar]
- 49.Bhaumik A., Roy S.K., Weber G.W. Hesitant interval-valued intuitionistic fuzzy-linguistic term set approach in Prisoners' dilemma game theory using TOPSIS: a case study on Human-trafficking. Cent Eur J Oper Res. 2020;28(2):797–816. [Google Scholar]
- 50.Tirkolaee E.B., Mardani A., Dashtian Z., Soltani M., Weber G.W. A novel hybrid method using fuzzy decision making and multi-objective programming for sustainable-reliable supplier selection in two-echelon supply chain design. J Clean Prod. 2020;250 [Google Scholar]
- 51.Bhaumik A., Roy S.K., Weber G.W. Multi-objective linguistic-neutrosophic matrix game and its applications to tourism management. J Dynam Game. 2021;8(2):101. [Google Scholar]
- 52.Weber G.W., Batmaz I., Köksal G., Taylan P., Yerlikaya-Ӧzkurt F. CMARS: a new contribution to nonparametric regression with multivariate adaptive regression splines supported by continuous optimization. Inverse Problems in Science and Engineering. 2012;20(3):371–400. [Google Scholar]
- 53.Özmen A., Batmaz İ., Weber G.W. Precipitation modeling by polyhedral RCMARS and comparison with MARS and CMARS. Environ Model Assess. 2014;19(5):425–435. [Google Scholar]
- 54.Çevik A., Weber G.W., Eyüboğlu B.M., Oğuz K.K. Voxel-MARS: a method for early detection of Alzheimer's disease by classification of structural brain MRI. Ann Oper Res. 2017;258(1):31–57. [Google Scholar]
- 55.Onak O.N., Serinagaoglu Dogrusoz Y., Weber G.W. Effects of a priori parameter selection in minimum relative entropy method on inverse electrocardiography problem. Inverse Problems in Science and Engineering. 2018;26(6):877–897. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.