Abstract
Background and Objectives
Improved measures capable of capturing the influence of person-centered caregiving by staff in formal care settings on people living with dementia beyond deficit-oriented outcomes such as absence or reduction of symptoms are important for measuring progress toward improvements in well-being. This exploratory ethnographic study aimed to identify verbal and nonverbal expressions evidenced by people living with dementia surrounding person-centered caregiving approaches and to consider their use in informing temporally specific observational measures.
Research Design and Methods
This study adopted a microethnographic approach through secondary analysis of 5.3 h of audiovisual observations of people living with dementia (N = 9) in nursing home settings at mealtimes. We observed expressions surrounding person-centered caregiving approaches. A systematic review of audiovisual observations generated codes (observable indicators) of expressions that were characterized at their most discrete and unambiguous level.
Results
Drawing from 82 observable verbal and nonverbal expressions by people living with dementia, 14 discrete observable indicators were identified, broadly evidencing shifts in engagement and communication. We found that people living with dementia’s expressions served both responsive and initiatory communicative purposes.
Discussion and Implications
Efforts to expand positive outcome measurement for people living with dementia should extend beyond characterizing them as passive respondents toward active participants in their lived experiences. Identified observable indicators can inform efforts to refine and validate measures of expressions among people living with dementia. Further research can extend this inquiry into different contexts and engage input from people living with dementia and caregivers.
Keywords: Dementia, Outcome measurement, Person-centered care, Personhood
Background and Objectives
Dementia is a major global health priority due to the rate of growth in cases, lack of effective disease-modifying treatment, and significant impacts of associated individual and societal challenges (Olivari et al., 2020; World Health Organization, 2017). Initiatives to improve outcomes for people living with dementia focus on maintaining well-being and quality of life (Olivari et al., 2020; Øksnebjerg et al., 2018; World Health Organization, 2017). At the core of this goal is an ethical commitment to protect the inalienable dignity and personhood of people living with dementia (McCormack, 2004; McGilton, 2004; Smebye & Kirkevold, 2013).
The concept of person-centered care has its origins in Carl Rogers’ work on approaches to humanistic psychotherapy, which emphasized the central role of understanding individuals as multidimensional beings as a basis for living and therapeutic intervention (Rogers, 1957, 1995). Building on this conceptualization, Thomas Kitwood applied the concept of person-centered care to help understand and explain differences in progression and experiences with dementia and to outline an approach to care intended to maintain or uphold personhood (Kitwood, 1997; Kitwood & Bredin, 1992). Personhood is defined as the quality of being worthy of respect and dignity and addresses the unique breadth of personal traits, values, and strengths that foster one’s sense of self (Kitwood, 1997; Manthorpe & Samsi, 2016; Smebye & Kirkevold, 2013). In that regard, one’s selfhood is manifested beyond one’s cognitive abilities (Fuchs, 2020; Sabat & Collins, 1999; Sabat & Harré, 1992). Personhood is inherently realized through relationship with dimensions of selfhood often expressed and experienced in social and relational contexts (Edvardsson et al., 2010; Harré, 1998; Ryan et al., 2009; Sabat & Harré, 1992).
Studies suggest that relationships support maintenance of social identity that promotes healthy aging, longevity, and life satisfaction and buffers against stressors threatening well-being, including changes in cognitive abilities (Gleibs et al., 2011; Hampson & Morris, 2016; Jetten et al., 2010). For people with dementia, social identity is established in part through social connection that recognizes the inherent value of ones’ unique self (Birt et al., 2020; Harris et al., 2021; Ryan et al., 2009). As people with dementia experience cognitive loss, maintenance of social identity through social connection promotes well-being and may modulate cognitive decline (Harris et al., 2021; Jetten et al., 2010; Lyreskog, 2021).
Person-centered caregiving is a holistic approach to care that prioritizes the person’s values, preferences, strengths, sense of self or autonomy, social identity, and right to meaningful relationships above care tasks (Edvardsson et al., 2008; McCormack, 2004). In nursing home contexts, person-centered caregiving is often realized through staff–resident interactions, including but not limited to recognizing a person’s whole self and story, and their preferences. For example, person-centered care may include connecting with an individuals’ social identities or values, offering choice, and adapting the pace of care to one’s abilities (Fazio et al., 2018). While there are various approaches to operationalizing the principles of person-centered care in practice (Edvardsson & Innes, 2010), a common approach is to compare care approaches demonstrating person-centeredness to approaches that are more task-centered in nature. Task-centered approaches are characterized as, intentionally or not, placing an emphasis on controlling the person and negatively characterized symptomatology to accomplish or expedite necessary care tasks (Barbosa et al., 2015; Lann-Wolcott et al., 2011; Savundranayagam, 2012). Prior studies suggest that person-centered caregiving approaches may alleviate or mitigate certain behavioral expressions (BEs)—actions, words, and gestures exhibited by the person living with dementia, which are understood as communication of unmet needs (Cohen-Mansfield et al., 2015; Gilmore-Bykovskyi et al., 2015; Kim & Park, 2017; Li & Porock, 2014). Conversely, task-centered caregiving approaches appear to increase or intensify BEs (Cohen-Mansfield et al., 2015; Gilmore-Bykovskyi et al., 2015). Often labeled as behavioral and psychological symptoms of dementia, BEs include symptoms referred to as agitation, aggression, wandering, and withdrawal (Cerejeira et al., 2012; Kales et al., 2015). While mechanisms driving these associations are not well understood, person-centered caregiving approaches may facilitate better recognition and responses by caregivers to unmet needs and thus reductions in BE (Kim & Park, 2017; Li & Porock, 2014).
While extant literature has focused on “negative” symptomatology as outcomes, emerging positive outcomes have captured constructs such as quality of life, well-being, and life satisfaction as well as social outcomes, including feeling valued and feeling safe (Csipke et al., 2021; Martyr et al., 2018; Reilly et al., 2020; Stansfeld et al., 2017). These outcomes have largely been applied to the evaluation of psychosocial interventions and highlight efforts toward the capture of the lived experiences of people living with dementia and those of their caregivers (Advisory Council on Alzheimer’s Research, 2020; Csipke et al., 2021; Gitlin, 2020; Reilly et al., 2020; Stansfeld et al., 2017).
Exploration of the interrelationships between person-centered caregiving approaches and broader outcomes among people living with dementia will require consideration of the dynamic, multidirectional interplay between caregivers and people living with dementia. While important progress is underway to expand both dimensions of and approaches to evaluating positive outcomes among people living with dementia, there has been limited progress in developing observational measures that can be both temporally and contextually situated (Gilmore-Bykovskyi et al., 2015). Temporally and contextually situated measures enable discernment of subtle communicative or BEs as well as their approximation temporally to other events, such as person-centered caregiving approaches or other salient situational or contextual features of the environment of care (Ellis & Astell, 2017; Perugia et al., 2018). Strong observational methods are particularly important for assessment of persons in advanced stages of dementia due to their limited verbal communication. These methods can detect subtle bodily shifts in response to social stimuli, which could indicate self-expressive actions (Ellis & Astell, 2017; Kontos, 2005).
We aimed to identify and describe observable verbal and nonverbal expressions evidenced by people living with dementia surrounding person-centered caregiving approaches and to consider their utility in informing future observational measures beyond the dominant paradigm of negative symptomology. This is a secondary analysis of audiovisual observation data from a study examining interactions between people living with dementia and professional caregiver staff interactions in nursing home settings (Gilmore-Bykovskyi et al., 2015).
Research Design and Methods
Design
This present study adopted an exploratory microethnographic approach through a secondary analysis of audiovisual observations of mealtime interactions between caregivers and people living with dementia in a nursing home environment (Gilmore-Bykovskyi et al., 2015). A microethnographic approach, sometimes referred to as “video-based ethnography,” examines dynamic social interactions and systems by engaging a microanalytic focus to delineate highly detailed communicative behaviors. Detailed communicative behaviors include specifications such as location, orientation, and movement toward others and things in the environment, as well as the situational and environmental contexts within which expressions occur (Bromley et al., 2012; LeBaron, 2008). The parent study collected naturalistic and nondirective video observations of people living with dementia in the context of mealtime in a nursing home environment (Gilmore-Bykovskyi et al., 2015).
Participants and Setting
Participants in the audiovisual observations included both residents with dementia and staff recruited from memory care units in two nursing homes in Wisconsin (Gilmore-Bykovskyi et al., 2015). Eligible nursing home residents had a documented diagnosis of dementia, presence of an activated power of attorney for health care, and required moderate to significant mealtime assistance that necessitated the provision of 1:1 care during mealtimes. Requiring significant mealtime assistance is one of the late-loss activities of daily living associated with moderate to severe dementia (Watson et al., 2017). As decisional incapacity was inherent in the inclusion criterion in the parent study for participants with dementia, the authorized legal representative for resident participants provided informed consent prior to participation, with assent obtained from participants with dementia. Eligible nursing home staff included nursing staff (certified nursing assistants and nurses) working primarily on the memory care unit and agreeable to audiovisual observation during their mealtime care for participating residents. Informed consent was completed with all participating nursing staff. The study received review and approval from the University of Wisconsin–Madison Institutional Review Board.
Data Sources and Measurement
Trained observers with a background in nursing reviewed audiovisual data to identify and characterize defining features and representative attributes of observable expressions. We defined observable expressions as the raw observations of verbal or nonverbal actions exhibited by people living with dementia. These observable expressions were derived from a secondary review of a total of 5.3 h of audiovisual observations of mealtime cares provided by six nursing assistants to nine nursing home residents with dementia requiring moderate to significant assistance.
Data Analysis
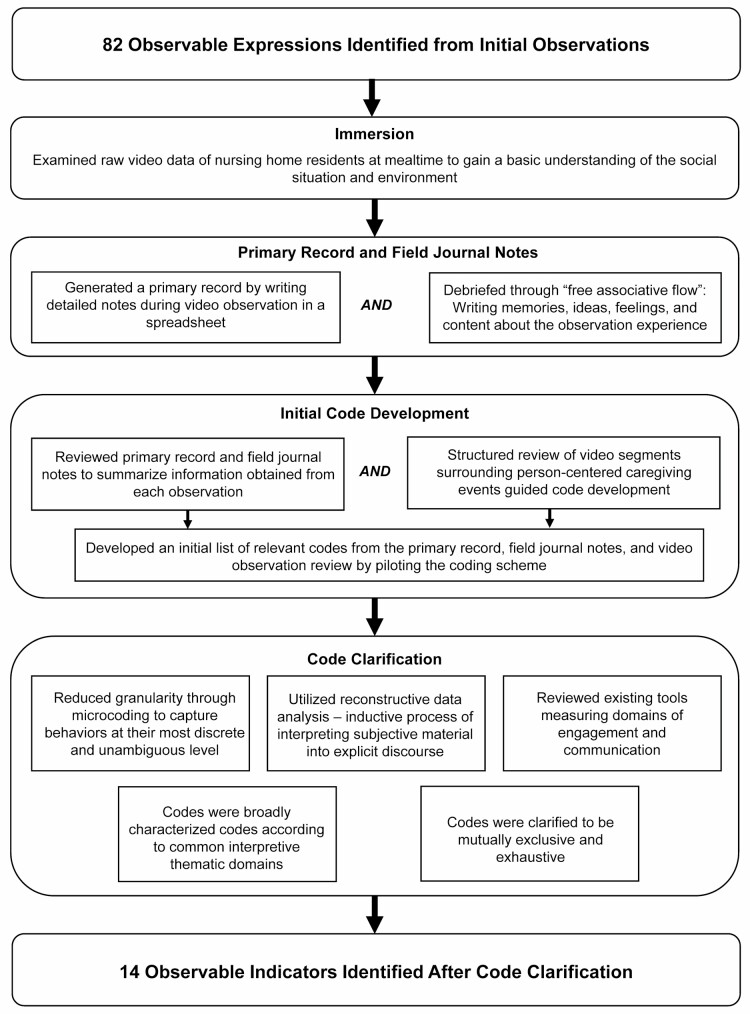
The analytic approach broadly followed analysis stages outlined by Pane and Rocco (2009) and methodological guidance outlined by Chorney et al. (2015) for developing observable indicators provided the overarching analytic goal of informing observational measurement opportunities (Chorney et al., 2015; Pane & Rocco, 2009). Observable indicators refer to the codes that captured the individual expressions evidenced by people living with dementia and their observable attributes. This approach consisted of a systematic review of audiovisual data guided by techniques for microethnographic analysis and behavioral observation coding scheme development. The approach progressed sequentially through stages of immersion, primary record and field journal notes, initial code development, and code clarification (Chorney et al., 2015; Pane & Rocco, 2009). Figure 1 outlines the steps of the analytical process.
Figure 1.
Flowchart of the analytical process.
Immersion
Members of the research team who were responsible for data analysis examined the raw video data. Through engagement with each observation, the reviewers began to immerse themselves in the data, gaining naturalistic insight into the context of the mealtime interactions and how people living with dementia manifested communicative expressions (Jones & Smith, 2017). In doing so, a basic understanding of the social situation and environment, the frequency and nature of person-centered approaches, and the degree to which people living with dementia contributed their expressions underpinned the analysis of observations.
Primary record and field journal notes
Following Pane and Rocco’s guidance on data collection for the primary record, we generated a primary record through field journal notes, writing detailed notes during video observation in a spreadsheet (Pane & Rocco, 2009). These notes or memos accounted for all salient and observable speech acts of the people living with dementia and the caregiver in verbatim form. Notes also included observations of body movements and posture, and other contextual information including event timing, event sequencing, and relevant environmental context, changes, or stimuli. While the provision of these general domains served to guide the observer, memoing was unstructured to ensure that relevant observations were not prematurely constrained provided the exploratory nature of the study aims. We also engaged in self-debriefing of the observation experience through “free associative flow,” or writing memories, ideas, feelings, and content about the experience (Pane & Rocco, 2009).
Code development, clarification, and assessment of utility
First, to guide initial code development, we reviewed the primary record and field journal notes to summarize information obtained from each observation. Code development involved a structured review of time points within each observation surrounding person-centered caregiving actions. Previous identification of person-centered caregiving approaches and application of timed-stamped codes occurred within the parent study, which applied a timed-event computer-assisted coding scheme that identified discrete behavior frequency and duration, derived from the Person-Centered Behavior Inventory observational tool (Gilmore-Bykovskyi et al., 2015; Lann-Wolcott et al., 2011). We recognized discrete person-centered caregiving events through actions such as orientation, showing interest, giving choices, adjusting to resident’s pace, and assessing comfort (Gilmore-Bykovskyi et al., 2015; Lann-Wolcott et al., 2011). Person-centered caregiving events were also identified through the absence of task-centered caregiving actions such as verbal interrupting statements, ignoring, physical control, and inappropriate touch. All behaviors were coded in Noldus Observer XT using timed-event coding that denoted the timing and duration of discrete actions (Gilmore-Bykovskyi et al., 2015).
Following guidance from Chorney, we developed an initial list of relevant codes from the primary record, field journal notes, and video observation review by piloting the coding scheme (Chorney et al., 2015). From the initial code development, we further clarified codes to capture what the research team observed from the people living with dementia, without inferring a purpose behind their observable expressions. In this clarification of the initial list of relevant codes, we used microcoding to capture behaviors at their most discrete and unambiguous level (Chorney et al., 2015). Discrete and unambiguous refers to the codes being applied in a mutually exclusive and exhaustive manner. Mutually exclusive codes required that each behavior was assigned to only one code. Exhaustive coding required applying a code for every behavior. We utilized reconstructive data analysis, or the inductive process of interpreting subjective material into explicit discourse to generate the primary list of relevant codes, to broadly characterize these codes according to common interpretive thematic domains (Pane & Rocco, 2009).
Code clarification also facilitated assessment of the potential utility of observable indicators in future timed-event observational measures and coding systems. Throughout the clarification stage, we utilized a team-based approach to reflect on the potential utility of observable indicators in future observational measurement by defining shared temporal and contextual attributes that enabled their reliable capture. Dialogue among team members involved critical reflection regarding the feasibility of reliable capture based on the clarity, cohesion, and internal consistency of each indicators’ description, and the degree of subjective interpretation required to identify each expression.
Rigor and Trustworthiness
We employed several strategies to enhance rigor and trustworthiness of our analysis, including deep and ongoing engagement with the data by multiple members of the research team, iterative interaction with the data across analytic stages, and incorporation of memoing. The research team held routine discussions of positionality toward the data, defined as the researchers’ philosophical, personal, and/or theoretical belief lens through which they view the research process. Active reflection (reflexivity) also occurred within the research team regarding procedures throughout all phases (Lincoln & Guba, 1986; Maher et al., 2018; Rowe, 2014). These discussions clarified the role of the researcher in identifying observable expressions of people living with dementia to reduce inference of the meaning of behavior.
Successive review of the observations ensured the reviewers were familiar with the data and thus more fully engaged in immersion (Webster & Rice, 2019). Two authors independently coded observable expressions, with disagreements resolved by a third reviewer. The three authors met routinely to discuss coding. In this process, we organized the expressions into indicators defined according to their observable features to enhance clarity and improve trustworthiness.
Results
Observers analyzed 33 video observations (5.3 h) of recorded mealtime care interactions (average mealtime duration 24.5 min) between the residents (N = 9) and their caregivers. Observers identified 82 observable expressions across 49 discrete events documenting person-centered caregiver approaches. Observable expressions encompassed both verbal behaviors (humming, babbling, muttering, coherent language, or incoherent language) and nonverbal behaviors (any behavior not classified as verbal).
Observable expressions occurred in response to person-centered caregiving approaches and as initiation of a new sequence of communicative interactions. Observation of expressions evidenced by people living with dementia surrounding person-centered care events enabled the capture of these initiatory expressions. In the following illustrative observation, the person living with dementia’s comment about the meal initiates a new sequence of conversation with the caregiver.
Person living with dementia’s expression: “This is pretty good.”
Caregiver: “It is, isn’t it?”
Person living with dementia’s expression: Resident laughs out loud, “I thought that, too,” smiles, sits up.
This illustrative observation demonstrates the person living with dementia contributing both initiatory and responsive conversation to the communicative interaction with the caregiver surrounding an interaction characterized by person-centered caregiving actions.
Identified Observable Indicators
Drawing from the 82 observable expressions, we identified 14 observable indicators. Indicators represented codes for the observable expressions—the raw observations of nonverbal and verbal actions demonstrated by people living with dementia—surrounding person-centered caregiving approaches. Observable indicators included mutual eye contact, gazing, touching, adjusting body position, arm or hand outreach, follow-through, initiating conversation, responding, responsive utterances, nods head, laughter, humming, singing, and facial expressions. Observable indicators were broadly characterized into thematic domains that could be understood as constituting a shift in degree of engagement or a shift in communicative expressions. These categorizations are not intended to confer meaning onto the discrete expressions manifested by people living with dementia but to communicate common characteristics across discrete expressive events.
The nomenclature chosen for observable indicators reflected their role in characterizing observable expressions in terms of unambiguous observable actions associated with each expressive event. For some observable indicators, nomenclature aligned word for word with the observable expressions they represented, as depicted in the illustrative observation below.
Person living with dementia’s expression: [Nods head]
Observable indicator: Nods head
As seen with a comparable illustrative observation, some observable indicators reframed the observable expressions into a representative domain:
Person living with dementia’s expression: [Smiles]
Observable indicator: Facial expression
Shift in degree of engagement with caregiver or environment
We characterized six observable indicators as indicating a shift in degree of engagement: mutual eye contact, gazing, touching, adjusting body position, arm or hand outreach, and follow-through. These indicators described observable expressions that demonstrated increased engagement with the caregiver or sometimes with other stimuli in the immediate environment, such as the food that was central in this observation context.
We defined follow-through as the behavior in which a person living with dementia responded to caregiver actions, such as the person opening their mouth to eat after a caregiver asks if they would like another bite of food. Gazing and adjusting body position involved the person living with dementia turning their head or their torso, respectively, toward a stimulus, such as the caregiver’s voice. We defined mutual eye contact, touching, and arm or hand outreach accordingly; see Table 1 for more details.
Table 1.
Descriptions of Observable Indicators With Illustrative Observations
| Thematic domain | Observable indicators | Description | Illustrative observation |
|---|---|---|---|
| Shift in degree of engagement with caregiver or environment | Mutual eye contact | Resident and caregiver look into each other’s eyes | Resident remains attentive, returns eye contact |
| Gazing | Resident’s head turns to face caregiver or object | Opens eyes, becomes more responsive | |
| Touching | Resident’s arms/hands reach out to touch the caregiver or object | Resident grabs hand | |
| Adjusting body position | Resident adjusts posture or leans in toward caregiver or object | Resident verbally responds, leans in | |
| Reaching | Resident reaches for object or person with arm or hand | Verbal response “later,” reaches out | |
| Follow-through | Resident behaves in the way requested by caregiver | Resident verbally responds “okay,” smiles, eats | |
| Shift in communication | Initiating conversation | Resident makes a comment about surroundings, personal life or asks a question | “This is pretty good” |
| Responding | Resident is responding in conversation | Eye contact, verbal response “yes” | |
| Responsive utterance | Resident produces a linguistically accepted nonword temporally after a conversational element, such as “mhmm” | Verbally expresses likeness of food “mhmm” | |
| Nods head | Resident nods head | Nods head, “mhmm” | |
| Laughter | Resident laughs when making a statement or responding to a statement by caregiver | Resident laughs out loud, “I thought that too,” smiles, sits up | |
| Humming | Resident hums along with caregiver or individually | Resident widens eyes, continues humming | |
| Singing | Resident sings along with caregiver or individually with or without lyrics | Resident sings | |
| Facial expression | Resident smiles, frowns, widens eyes, or exhibits another distinct facial expression | Resident widens eyes, nods head |
Note: Bolded text highlights the nonverbal or verbal expression demonstrated by the person living with dementia that is captured by the observable indicator, within the context of other nonbolded expressions present during the illustrative observation.
In the following illustrative observation, an observable expression surrounding a person-centered approach indicated a shift in engagement.
Caregiver: *Asks question, leans in*
Person living with dementia’s expression: [responds, mutual eye contact]
Observable indicator (denoting shift in degree of engagement): mutual eye contact
We interpret the person living with dementia making eye contact with the caregiver as an indicator of increased engagement in the conversation or interaction.
Shift in communication
We characterized eight observable indicators as indicating a shift in communication: initiating conversation, responding, responsive utterances, nods head, laughter, humming, singing, and facial expressions. These indicators described observable expressions where people living with dementia demonstrated self-expression through conversational elements or responses—commonly displaying an emotion, preference, or need.
Observable communicative indicators of initiating conversation and responding captured participants’ verbal commentary, including questioning, raising observations about the surroundings, requesting something or expressing a need or desire, or answering a prompt. Responsive utterances included socially routine use of nonword units of speech, such as “mhmm” and “mmm.” See Table 1 for descriptions of additional communicative indicators.
In the following illustrative observation, communicative observable indicators worked synergistically to represent the person living with dementia’s expressions surrounding the person-centered caregiving approach.
Caregiver: *Assesses taste of food* “Good, huh?”
Person living with dementia’s expression: [Nods head, “mhmm”]
Observable indicators (denoting shift in communication): Nods head, responsive utterance
We interpret the person living with dementia’s head nod and responsive utterance as representing a communicative interaction. The responsive utterance of “mhmm” answered the caregiver’s prompt, indicating its role in the conversation taking place. Nodding clarified the interpretation of “mhmm” by signaling agreement.
Coding Utility of Observable Indicators
The research team considered the potential utility of observational indicators in future observational measures through the extent to which observable indicators can be reliably identified, mutual exclusivity among indicators, and temporal and contextual attributes that shape measurement capacity.
Observable indicators represent temporal or state events
Quantifying observable indicators depends on whether the indicator represents a temporal event, which occurs for a variable amount of time, or a state event, which either occurs or does not occur. Observable indicators represented state events in this study, as we noted whether or not they occurred in the data and did not time stamp for their duration. However, the potential to associate all 14 observable indicators with timed-event onset and duration across a sequence of interactions exists, enabling the potential for their inclusion into multidimensional, temporally structured data.
Observable indicators are unambiguous and discrete
We derived unambiguous indicators of observable expressions, drawing on the clarity provided by each indicator description in representing discrete events. This means that, in observational measurement, the indicators are theoretically mutually exclusive. Discreteness guarantees each indicator definition is independent of other indicators and contributes to the goal of producing standardized measures. It is important to note that absent corroboration from the person living with dementia or those familiar with them, capturing any meaning associated with people living with dementia’s expressions, is inherently subjective to some degree.
Observable indicators are context-shaped
Most observable indicators were naturally context-shaped, meaning that their onset, frequency, and duration were interwoven with other aspects of the physical and social environment. For example, the onset and duration of the person living with dementia’s mutual eye contact likely depended on factors such as duration of caregiver’s commentary, duration of caregiver eye contact, and the onset of other environmental stimuli. Context-shaped observable expressions may encompass several actions exhibited by the person living with dementia. Thus, complete representation of observable expressions requires a synergy of multiple observable indicators. For example, a responsive utterance on its own may be communicative in nature; however, when paired with gazing, the responsive utterance may better indicate a shift in degree of engagement.
Discussion and Implications
While exploratory in nature, findings from this secondary descriptive ethnography introduce important findings regarding observable verbal and nonverbal expressions exhibited by people living with dementia surrounding person-centered caregiving events. Observable expressions may serve important communicative and engagement purposes, including initiating or responding to the caregiver or environment. Drawing from the identified observable expressions, observable indicators generated in the present study provide preliminary evidence for the development of observational measures that can capture and characterize nonverbal and verbal expressions among people living with dementia surrounding person-centered caregiving approaches.
This study contributes to the growing shift toward maintaining a broad perspective that is considerate of our external position as researchers looking in on the experiences of people living with dementia and their caregivers. This study also presents the opportunity to increase positive engagement of people living with dementia in alignment with research and advocacy work (Gove et al., 2018; Morbey et al., 2019; Reed et al., 2017). This emphasizes the importance of continual reflection on who can infer meaning over whom in order to promote ethical and agentic representation of people living with dementia and their lived experiences (Reed et al., 2017). Categorizing identified indicators into broader thematic domains related to engagement and communication is meant to provide probable distinction between subsets of behaviors; at this stage, it is not intended to infer meaning of the actions of people living with dementia (Øksnebjerg et al., 2018).
Indicators contribute to developing new observational measures, because they are unambiguous and discrete, temporal or state in nature, and context-shaped. They include place, time of day, and the presence of other persons and stimuli and are analyzed within the sequential nature of initiative and responsive communication (Heath et al., 2010). Indicators from this study captured expressions with respect to contextual factors and their temporal situation within person-centered caregiving events. Such findings suggest that the potential to time-stamp indicators in future measurement could enable the discrete study of expressions within care interactions and provide insight on the effects of personhood conferring care (Gilmore-Bykovskyi, 2015; Gilmore-Bykovskyi et al., 2015).
Measurement tools examining engagement and communication specific to people living with dementia exist, evincing the potential for reliable capture of observable expressions that point to a shift in degree of engagement and communication. These include the Observational Measurement of Engagement (Cohen-Mansfield et al., 2009), the Ethnographic and Laban-Inspired Coding System of Engagement, and the Evidence-Based Model of Engagement-Related Behavior (Perugia et al., 2018), which are designed to measure engagement, and the Roter Interaction Analysis System (Roter & Larson, 2002), which is designed to measure communication in terms of verbal responses. While these measurement tools individually address some key indicators of engagement and communication and can serve as models for innovative measurement development, they are limited in contextual applicability and full capture of expressions among people living with dementia. This includes insensitivity to contextual factors, such as caregiver presence, heightened focus on select indicators of engagement or communication that may discount other prevalent expressions among people living with dementia, and confined applicability to people living with mild to moderate dementia (Hackett et al., 2019; Han et al., 2016; Hennings & Froggatt, 2019). Expansion of current measurement tools is essential in capturing people living with dementia as active social beings in their lived experiences (Birt et al., 2020; Øksnebjerg et al., 2018). Further research focused on these expressions/indicators may also prove useful in research on people living with dementia’s social identity.
Socially sensitive measures identified in the present study captured people living with dementia’s expressions in terms of both initiatory and responsive events, where the caregiver does not simply “influence” outcomes, but the person living with dementia is present and contributes to the interaction as an active participant (Reed et al., 2017). This supports findings on the agentic role people living with dementia take in establishing social connections to support their social identity and personhood through a meaningful relationship with caregivers (Birt et al., 2020; Smebye & Kirkevold, 2013). Initiatory events may manifest as subtle expressions, such as eye or head movement, that could otherwise be overlooked in the absence of appropriate measures. This finding, while expanding beyond the objective of this study, is crucial in countering the stigmatized orientation of people living with dementia as solely passive beings (Low & Purwaningrum, 2020). Moreover, attention to initiatory expressions enhances identification of embodied responses, further evidencing continued attempts among people living with dementia to express their selfhood, engage with their surroundings, and support personhood through relationship (Fuchs, 2020; Kontos, 2005; Smebye & Kirkevold, 2013).
Limitations
The small sample size in this study limited the results. While ethnographic analyses such as those applied in this study do not typically intend for findings to be generalizable, it is important to address the context of observations as limited to mealtimes and the limited number of situations sampled. Considering participant inclusion criteria, findings are limited to persons living with dementia who require moderate to significant mealtime assistance. Therefore, proposed indicators may not capture the full range of expressions demonstrated at other stages in the dementia journey. Additionally, this study focused specifically on contributions of the person living with dementia during person-centered caregiving events; however, people living with dementia express themselves and contribute to interactions that cross a spectrum of person-centeredness. Broadening our understanding of expressions of people living with dementia outside of person-centered caregiving events is critical. Broader sampling and data collection are likely to yield greater clarity regarding proposed indicators, thereby enhancing efforts toward standardization.
Importantly, the utility of identified observable indicators was determined through discussion by the research team and did not include external review. Although our methodology incorporated multiple strategies to enhance trustworthiness and rigor, including routine discussions of positionality toward the data and active reflection within the research team regarding procedures, the substance and identified value of observable indicators did not benefit from external review. Specifically, due to the nature of the study, we were unable to triangulate our findings with the views and ideas of the participants. The use of triangulation would improve the trustworthiness of the results by minimizing the subjectivity of the findings and ensuring that the interpretation of the data is based on participants’ original data and views (Lincoln & Guba, 1986).
Future Research
Future research is needed to develop a standardized measurement system of observation that captures the dynamics of interactions, including both initiatory and responsive expressions. This requires expanding attention to subtle expressions that surround the event of interest, such as interactions among people living with dementia and their caregivers. In doing so, people living with dementia’s expressions to interactions within their environment would be better represented as they naturally exist, appropriately situating people living with dementia as social beings. Additionally, beyond capture of occurrence and duration of expressions, observable indicators could be derived to measure valence and intensity of people living with dementia’s expressions. External review would strengthen evaluation of the utility and validity of expanded observable indicators.
This study did not objectively measure dementia severity of the people living with dementia, but instead measured the level of mealtime care required of the people living with dementia as an indicator of severe disease. All people living with dementia required moderate to significant mealtime assistance that necessitated the provision of 1:1 care during mealtimes. Additionally, all participants had an activated alternative decision maker in place. Because disease severity modifies communicative abilities, assessment of disease stage and functional communication abilities will be important in future studies aimed at further developing measurement for expressive responses to person-centered caregiving.
Future measure development requires the triangulation of data from key informants, such as people living with dementia and their caregivers from a wide range of experiences, and across different contexts and points in care (Beuscher & Grando, 2009; Webb et al., 2020). Future research incorporating the voices of people living with dementia and their caregivers will enhance capture of what is meaningful to people living with dementia. This will also strengthen identification of the dynamics surrounding social interaction and meaningful shifts in communication or engagement (Webb et al., 2020). These efforts may involve guiding nomenclature of the indicators and terminology such as “observable expression” and “observable indicator” in order to shape a collaborative approach to measure development that empowers people living with dementia. Furthermore, triangulated data may be of use in expanding other already defined social constructs, such as engagement and affect. These constructs are inherently challenging to study given the natural space between a researcher’s external observation and the individual’s inner manifestation of their expressions, especially those related to affect.
Conclusion
The present study is a first step in addressing methodological gaps in developing nondeficit-oriented, observable measures for evaluating the impact of person-centered caregiving approaches among persons living with dementia. Capture of subtle expressions is particularly important for the study of persons living with advanced dementia, wherein novel attention can be given to subtle head or eye movement that may signal people living with dementia’s attempts to create connection and meaning within their lived experiences. Advancements in prioritizing the dignity, well-being, and life satisfaction of people living with dementia necessitate novel frameworks incorporating abilities-focused expressions that represent people living with dementia as active participants in their care experiences, thereby challenging ableist, stigmatized views of people living with dementia as solely respondents (Ihara et al., 2019). This study highlights the opportunity for ethnographic approaches and video observation to guide in development of such frameworks and measurement of positive outcome measure domains, including well-being, engagement, and responsiveness related to the lived experiences of dementia.
Contributor Information
Maya Staehler, University of Wisconsin–Madison School of Nursing, Madison, Wisconsin, USA.
Clark Benson, University of Wisconsin–Madison School of Nursing, Madison, Wisconsin, USA.
Laura Block, University of Wisconsin–Madison School of Nursing, Madison, Wisconsin, USA.
Tonya Roberts, University of Wisconsin–Madison School of Nursing, Madison, Wisconsin, USA.
Andrea Gilmore-Bykovskyi, University of Wisconsin–Madison School of Nursing, Madison, Wisconsin, USA; Division of Geriatrics, Department of Medicine, University of Wisconsin–Madison School of Medicine and Public Health, Madison, Wisconsin, USA.
Funding
This work was supported by the National Institute on Aging of the National Institutes of Health under award number (K76AG060005 to A. Gilmore-Bykovskyi). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
None declared.
References
- Advisory Council on Alzheimer’s Research, Care, and Services. (2020). Public members of the advisory council on Alzheimer’s research, care, and services: 2020 recommendations. https://aspe.hhs.gov/system/files/pdf/263911/2020PubMemRec.pdf
- Barbosa, A., Sousa, L., Nolan, M., & Figueiredo, D. (2015). Effects of person-centered care approaches to dementia care on staff: A systematic review. American Journal of Alzheimer’s Disease and Other Dementias, 30(8), 713–22. doi: 10.1177/1533317513520213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beuscher, L., & Grando, V. T. (2009). Challenges in conducting qualitative research with individuals with dementia. Research in Gerontological Nursing, 2(1), 6–11. doi: 10.3928/19404921-20090101-04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birt, L., Griffiths, R., Charlesworth, G., Higgs, P., Orrell, M., Leung, P., & Poland, F. (2020). Maintaining social connections in dementia: A qualitative synthesis. Qualitative Health Research, 30(1), 23–42. doi: 10.1177/1049732319874782 [DOI] [PubMed] [Google Scholar]
- Bromley, E., Adams, G. F., & Brekke, J. S. (2012). A video ethnography approach for linking naturalistic behaviors to research constructs of neurocognition in schizophrenia. Journal of Neuropsychiatry and Clinical Neurosciences, 24(2), 125–140. doi: 10.1176/appi.neuropsych.11080201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerejeira, J., Lagarto, L., & Mukaetova-Ladinska, E. B. (2012). Behavioral and psychological symptoms of dementia. Frontiers in Neurology, 3, 73. doi: 10.3389/fneur.2012.00073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorney, J. M., McMurtry, C. M., Chambers, C. T., & Bakeman, R. (2015). Developing and modifying behavioral coding schemes in pediatric psychology: A practical guide. Journal of Pediatric Psychology, 40(1), 154–164. doi: 10.1093/jpepsy/jsu099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield, J., Dakheel-Ali, M., & Marx, M. S. (2009). Engagement in persons with dementia: The concept and its measurement. American Journal of Geriatric Psychiatry, 17(4), 299–307. doi: 10.1097/JGP.0b013e31818f3a52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield, J., Dakheel-Ali, M., Marx, M. S., Thein, K., & Regier, N. G. (2015). Which unmet needs contribute to behavior problems in persons with advanced dementia? Psychiatry Research, 228(1), 59–64. doi: 10.1016/j.psychres.2015.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csipke, E., Shafayat, A., Sprange, K., Bradshaw, L., Montgomery, A. A., Ogollah, R., Moniz-Cook, E., & Orrell, M. (2021). Promoting independence in dementia (PRIDE): A feasibility randomized controlled trial. Clinical Interventions in Aging, 16, 363–378. doi: 10.2147/cia.s281139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edvardsson, D., Fetherstonhaugh, D., & Nay, R. (2010). Promoting a continuation of self and normality: Person-centred care as described by people with dementia, their family members and aged care staff. Journal of Clinical Nursing, 19(17–18), 2611–2618. doi: 10.1111/j.1365-2702.2009.03143.x [DOI] [PubMed] [Google Scholar]
- Edvardsson, D., & Innes, A. (2010). Measuring person-centered care: A critical comparative review of published tools. The Gerontologist, 50(6), 834–846. doi: 10.1093/geront/gnq047 [DOI] [PubMed] [Google Scholar]
- Edvardsson, D., Winblad, B., & Sandman, P.-O. (2008). Person-centred care of people with severe Alzheimer’s disease: Current status and ways forward. Lancet Neurology, 7, 362–367. doi: 10.1016/S1474-4422(08)70063-2 [DOI] [PubMed] [Google Scholar]
- Ellis, M., & Astell, A. (2017). Communicating with people living with dementia who are nonverbal: The creation of adaptive interaction. PLoS One, 12(8), e0180395. doi: 10.1371/journal.pone.0180395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazio, S., Pace, D., Flinner, J., & Kallmyer, B. (2018). The fundamentals of person-centered care for individuals with dementia. The Gerontologist, 58(Suppl. 1), S10–S19. doi: 10.1093/geront/gnx122 [DOI] [PubMed] [Google Scholar]
- Fuchs, T. (2020). Embodiment and personal identity in dementia. Medicine, Health Care, and Philosophy, 23, 665–676. doi: 10.1007/s11019-020-09973-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore-Bykovskyi, A. L. (2015). Caregiver person-centeredness and behavioral symptoms during mealtime interactions: Development and feasibility of a coding scheme. Geriatric Nursing, 36(2 Suppl), S10–S15. doi: 10.1016/j.gerinurse.2015.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore-Bykovskyi, A. L., Roberts, T. J., Bowers, B. J., & Brown, R. L. (2015). Caregiver person-centeredness and behavioral symptoms in nursing home residents with dementia: A timed-event sequential analysis. The Gerontologist, 55(Suppl. 1), S61–S66. doi: 10.1093/geront/gnu164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin, L. N. (2020). 2020 National research summit on care, services, and supports for people living with dementia and their caregivers: Progress to date. Presentation at the 2020 National Research Summit on care, services, and supports for people living with dementia and their caregivers. https://www.nia.nih.gov/sites/default/files/2020-07/Summit%20July%2010%20Opening%20remarks%20508-compliant.pdf [DOI] [PubMed]
- Gleibs, I. H., Haslam, C., Jones, J. M., Haslam, S. A., McNeill, J., & Connolly, H. (2011). No country for old men? The role of a ‘Gentlemen’s Club’ in promoting social engagement and psychological well-being in residential care. Aging & Mental Health, 15(4), 456–466. doi: 10.1080/13607863.2010.536137 [DOI] [PubMed] [Google Scholar]
- Gove, D., Diaz-Ponce, A., Georges, J., Moniz-Cook, E., Mountain, G., Chattat, R., & Øksnebjerg, L.; European Working Group of People with Dementia . (2018). Alzheimer Europe’s position on involving people with dementia in research through PPI (patient and public involvement). Aging & Mental Health, 22(6), 723–729. doi: 10.1080/13607863.2017.13173344 [DOI] [PubMed] [Google Scholar]
- Hackett, R. A., Steptoe, A., Cadar, D., & Fancourt, D. (2019). Social engagement before and after dementia diagnosis in the English Longitudinal Study of Ageing. PLoS One, 14(8), e0220195. doi: 10.1371/journal.pone.0220195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson, C., & Morris, K. (2016). Dementia: Sustaining self in the face of cognitive decline. Geriatrics (Basel, Switzerland), 1(4), 25. doi: 10.3390/geriatrics1040025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, A., Radel, J., McDowd, J. M., & Sabata, D. (2016). Perspectives of people with dementia about meaningful activities: A synthesis. American Journal of Alzheimer’s Disease & Other Dementias, 31(2), 115–123. doi: 10.1177/1533317515598857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harré, R. (1998). The singular self: An introduction to the psychology of personhood. Sage Publications, Inc. [Google Scholar]
- Harris, S. A., Baird, A., Matthews, S., Kennett, J., Gelding, R., & Harris, C. B. (2021). The impact of dementia on the self: Do we consider ourselves the same as others? Neuroethics, 14, 281–294. doi: 10.1007/s12152-021-09472-w [DOI] [Google Scholar]
- Heath, C., Hindmarsh, J., & Luff, P. (2010). Video in qualitative research. Sage Publications. doi: 10.4135/9781526435385 [DOI] [Google Scholar]
- Hennings, J., & Froggatt, K. (2019). The experiences of family caregivers of people with advanced dementia living in nursing homes, with a specific focus on spouses: A narrative literature review. Dementia, 18(1), 303–322. doi: 10.1177/1471301216671418 [DOI] [PubMed] [Google Scholar]
- Ihara, E. S., Tompkins, C. J., Inoue, M., & Sonneman, S. (2019). Results from a person-centered music intervention for individuals living with dementia. Geriatrics & Gerontology International, 19(1), 30–34. doi: 10.1111/ggi.13563 [DOI] [PubMed] [Google Scholar]
- Jetten, J., Haslam, C., Pugliese, C., Tonks, J., & Haslam, S. A. (2010). Declining autobiographical memory and the loss of identity: Effects on well-being. Journal of Clinical and Experimental Neuropsychology, 32(4), 408–416. doi: 10.1080/13803390903140603 [DOI] [PubMed] [Google Scholar]
- Jones, J., & Smith, J. (2017). Ethnography: Challenges and opportunities. Evidence-Based Nursing, 20, 98–100. doi: 10.1136/eb-2017-102786 [DOI] [PubMed] [Google Scholar]
- Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ, 350, h369–h369. doi: 10.1136/bmj.h369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. K., & Park, M. (2017). Effectiveness of person-centered care on people with dementia: A systematic review and meta-analysis. Clinical Interventions in Aging, 12, 381–397. doi: 10.2147/cia.s117637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitwood, T. (1997). The experience of dementia. Aging & Mental Health, 1(1), 13–22. doi: 10.1080/13607869757344 [DOI] [Google Scholar]
- Kitwood, T., & Bredin, K. (1992). Towards a theory of dementia care: Personhood and well-being. Ageing and Society, 12, 269–287. doi: 10.1017/s0144686x0000502x [DOI] [PubMed] [Google Scholar]
- Kontos, P. (2005). Embodied selfhood in Alzheimer’s disease: Rethinking person-centred care. Dementia, 4(4), 553–570. doi: 10.1177/1471301205058311 [DOI] [Google Scholar]
- Lann-Wolcott, H., Medvene, L. J., & Williams, K. (2011). Measuring the person-centeredness of caregivers working with nursing home residents with dementia. Behavior Therapy, 42(1), 89–99. doi: 10.1016/j.beth.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBaron, C. D. (2008). Microethnography. In W. Donsbach (Ed.), The International Encyclopedia of Communication. doi: 10.1002/9781405186407.wbiecm082 [DOI] [Google Scholar]
- Li, J., & Porock, D. (2014). Resident outcomes of person-centered care in long-term care: A narrative review of interventional research. International Journal of Nursing Studies, 51(10), 1395–415. doi: 10.1016/j.ijnurstu.2014.04.003 [DOI] [PubMed] [Google Scholar]
- Lincoln, Y. S., & Guba, E. G. (1986). But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Directions for Program Evaluation, 1986(30), 73–84. doi: 10.1002/ev.1427 [DOI] [Google Scholar]
- Low, L. F., & Purwaningrum, F. (2020). Negative stereotypes, fear and social distance: A systematic review of depictions of dementia in popular culture in the context of stigma. BMC Geriatrics, 20, 477. doi: 10.1186/s12877-020-01754-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyreskog, D. M. (2021). Withering Minds: towards a unified embodied mind theory of personal identity for understanding dementia. Journal of Medical Ethics. Advance online publication. doi: 10.1136/medethics-2021-107381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher, C., Hadfield, M., Hutchings, M., & de Eyto, A. (2018). Ensuring rigor in qualitative data analysis: A design research approach to coding combining NVivo with traditional material methods. International Journal of Qualitative Methods, 17(1), 1–13. doi: 10.1177/1609406918786362 [DOI] [Google Scholar]
- Manthorpe, J., & Samsi, K. (2016). Person-centered dementia care: Current perspectives. Clinical Interventions in Aging, 11, 1733–1740. doi: 10.2147/CIA.S104618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martyr, A., Nelis, S. M., Quinn, C., Wu, Y. T., Lamont, R. A., Henderson, C., Clarke, R., Hindle, J. V., Thom, J. M., Jones, I. R., Morris, R. G., Rusted, J. M., Victor, C. R., & Clare, L. (2018). Living well with dementia: A systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychological Medicine, 48(13), 2130–2139. doi: 10.1017/s0033291718000405 [DOI] [PubMed] [Google Scholar]
- McCormack, B. (2004). Person-centredness in gerontological nursing: An overview of the literature. Journal of Clinical Nursing, 13(s1), 31–38. doi: 10.1111/j.1365-2702.2004.00924.x [DOI] [PubMed] [Google Scholar]
- McGilton, K. (2004). Relating well to persons with dementia: A variable influencing staffing and quality of care outcomes. Alzheimer’s Care Today, 5(1), 71–80. [Google Scholar]
- Morbey, H., Harding, A., Swarbrick, C., Ahmed, F., Elvish, R., Keady, J., Williamson, P. R., & Reilly, S. T. (2019). Involving people living with dementia in research: An accessible modified Delphi survey for core outcome set development. Trials, 20(1), 12. doi: 10.1186/s13063-018-3069-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Øksnebjerg, L., Diaz-Ponce, A., Gove, D., Moniz-Cook, E., Mountain, G., Chattat, R., & Woods, B. (2018). Towards capturing meaningful outcomes for people with dementia in psychosocial intervention research: A pan-European consultation. Health Expectations, 21(6), 1056–1065. doi: 10.1111/hex.12799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivari, B. S., French, M. E., & McGuire, L. C. (2020). The public health road map to respond to the growing dementia crisis. Innovation in Aging, 4(1), igz043. doi: 10.1093/geroni/igz043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pane, D. M., & Rocco, T. S. (2009). Critical microethnography: The search for emancipatory methods. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research, 10(2). doi: 10.17169/fqs-10.2.442 [DOI] [Google Scholar]
- Perugia, G., van Berkel, R., Díaz-Boladeras, M., Català-Mallofré, A., Rauterberg, M., & Barakova, E. (2018). Understanding engagement in dementia through behavior. The ethographic and Laban-inspired coding system of engagement (ELICSE) and the evidence-based model of engagement-related behavior (EMODEB). Frontiers in Psychology, 9, 690. doi: 10.3389/fpsyg.2018.00690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed, P., Carson, J., & Gibb, Z. (2017). Transcending the tragedy discourse of dementia: An ethical imperative for promoting selfhood, meaningful relationships, and well-being. AMA Journal of Ethics, 19(7), 693–703. doi: 10.1001/journalofethics.2017.19.7.msoc1-1707 [DOI] [PubMed] [Google Scholar]
- Reilly, S., Harding, A., Morbey, H., Ahmed, F., Williamson, P., Swarbrick, C., Leroi, I., Davies, L., Reeves, D., Holland, F., Hann, M., & Keady, J. (2020). What is important to people with dementia living at home? A set of core outcome items for use in the evaluation of non-pharmacological community-based health and social care interventions. Age and Ageing, 49(4), 1–8. doi: 10.1093/ageing/afaa015 [DOI] [Google Scholar]
- Rogers, C. R. (1957). The necessary and sufficient conditions of therapeutic personality change. Journal of Consulting Psychology, 21(2), 95–103. doi: 10.1037/h0045357 [DOI] [PubMed] [Google Scholar]
- Rogers, C. R. (1995). Way of being. Houghton Mifflin. [Google Scholar]
- Roter, D., & Larson, S. (2002). The Roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Education and Counseling, 46(4), 243–51. doi: 10.1016/s0738-3991(02)00012-5 [DOI] [PubMed] [Google Scholar]
- Rowe, W. (2014). Positionality. In Coghlan D. & Brydon-Miller M. (Eds.), The SAGE encyclopedia of action research. SAGE Publications Ltd. doi: 10.4135/9781446294406 [DOI] [Google Scholar]
- Ryan, E. B., Bannister, K. A., & Anas, A. P. (2009). The dementia narrative: Writing to reclaim social identity. Journal of Aging Studies, 23(3), 145–157. doi: 10.1016/j.jaging.2007.12.018 [DOI] [Google Scholar]
- Sabat, S. R., & Collins, M. (1999). Intact social, cognitive ability, and selfhood: A case study of Alzheimer’s disease. American Journal of Alzheimer’s Disease, 14(1), 11–19. doi: 10.1177/153331759901400108 [DOI] [Google Scholar]
- Sabat, S. R., & Harré, R. (1992). The construction and deconstruction of self in Alzheimer’s disease. Ageing and Society, 12, 443–461. doi: 10.1017/S0144686X00005262 [DOI] [Google Scholar]
- Savundranayagam, M. Y. (2012). Person-centered care: Measurement, implementation, and outcomes. Clinical Gerontologist, 35(5), 357–359. doi: 10.1080/07317115.2012.702646 [DOI] [Google Scholar]
- Smebye, K. L., & Kirkevold, M. (2013). The influence of relationships on personhood in dementia care: A qualitative, hermeneutic study. BMC Nursing, 12(1), 29. doi: 10.1186/1472-6955-12-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stansfeld, J., Stoner, C. R., Wenborn, J., Vernooij-Dassen, M., Moniz-Cook, E., & Orrell, M. (2017). Positive psychology outcome measures for family caregivers of people living with dementia: A systematic review. International Psychogeriatrics, 29(8), 1281–1296. doi: 10.1017/s1041610217000655 [DOI] [PubMed] [Google Scholar]
- Watson, R., Palese, A., Zuttion, R., Ferrario, B., Ponta, S., & Hayter, M. (2017). Identifying longitudinal sustainable hierarchies in activities of daily living. Archives of Gerontology and Geriatrics, 71, 122–128. doi: 10.1016/j.archger.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Webb, J., Williams, V., Gall, M., & Dowling, S. (2020). Misfitting the research process: Shaping qualitative research “in the field” to fit people living with dementia. International Journal of Qualitative Methods. doi: 10.1177/1609406919895926 [DOI] [Google Scholar]
- Webster, F., & Rice, K. (2019). Conducting ethnography in primary care. Family Practice, 36, 523–525. doi: 10.1093/fampra/cmz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global action plan on the public health response to dementia 2017–2025. (2017). doi: 10.1080/13607863.2018.1544213. https://apps.who.int/iris/bitstream/handle/10665/259615/9789241513487-eng.pdf?sequence=1 World Health Organization. [DOI] [PubMed] [Google Scholar]