Abstract
The article presents the results of neuropsychological remote and face-to-face testing of 25 children aged 12 to 17 years in the nearest (during and 1-2 weeks after the treatment) and later period (2-12 months) after COVID-19 infection with predominant respiratory tract infection, organized in Ekaterinburg in the State Autonomous Institution "Children's Hospital № 8". Indication of family contact with patients with a new coronavirus infection was found in all patients, a positive nasopharyngeal swab for SARS-CoV-2 RNA by PCR was found in 58%, non-focal neurological complaints were found in 54% of children. The control group consisted of 25 pupils of Moscow comprehensive schools (14 girls and 11 boys) aged between 12 and 16 years who were examined before the pandemic. The methods included: investigation of the kinesthetic, spatial, dynamic, graphic praxis; auditory-motor coordination; visual, object-constructive gnosis; auditory-speech, visual memory; voluntary attention; thinking. Significant differences with the results of neuropsychological tests performed in children in the control group were found, allowing us to assert impairment of memory, attention, visual gnosis, visual-spatial function, kinesthetic and dynamic praxis, verbal and non-verbal component of thinking. According to A.R. Luria's theory, the topic of the disorders involves the temporo-parieto-occipital, mediobasal, frontotemporal parts of the brain, the reticular formation and limbic structures. This necessitates the development of corrective educational programs and an in-depth diagnostic algorithm that determines the morphological substrate of cognitive disorders in children, who have undergone COVID-19.
Key Words: Childhood neuropsychology, long-term effects of COVID-19, neurocognitive tests, cognitive functions
Ethical Publication Statement
We confirm that we have read the journal’s position on ethical issues involved in publication and affirm that this report is consistent with those guidelines.
With development of the COVID-19 pandemic, research is increasingly aimed at addressing its long-term effects. This complex of disorders, together with other effects of the new coronavirus infection, are grouped under the term "post-COVID syndrome" or Long Covid. Post-COVID syndrome is identified when signs and symptoms that develop during or after an infection that correspond to COVID-19 persist for more than 12 weeks and cannot be attributed to alternative diagnoses.1,2 Patients with Post-COVID-19 syndrome are divided into "acute" (e.g. thromboembolic complications) and "chronic" - with a nonspecific clinical picture, often characterized by fatigue and shortness of breath.3 Patients with COVID-19 and CNS damage demonstrate behavioral changes, mental and cognitive disorders, retardation, feelings of 'stupefaction', reduced concentration.4 Many authors report long-term persistent symptoms after COVID-19 in individuals with a mild course of the disease, including asymptomatic/low-symptomatic children. In a recent study Buonsenso D. et al. (2021)5 reported persistence of symptoms 120 days after COVID-19 in more than half of the children previously diagnosed with COVID-19, in 42.6% of whom these disorders limited daily activities.5 Fatigue, muscle and joint pain, headache, insomnia, breathing difficulties and heart palpitations were particularly common. Cognitive disorders have been reported in 34.3% of patients who had COVID-19.6 The authors emphasize the need to monitor children for several months after hospitalization in order to preserve their mental health. In their opinion inclusion of a psychological evaluation in the diagnosis of children with Long Covid is a practical necessity. Neuropsychological symptoms reflect subtle functional changes in brain tissue. Today, cognitive and emotional studies in psychiatry and neurology, based on neuropsychological methods, are firmly embedded in the scientific and research practice of medical professionals and psychologists. New studies in these areas are relevant to clinical psychology (primarily neuropsychology), pediatrics, psychiatry and neurology.
As part of a multidisciplinary approach to analysis, a study of higher mental functions in children in the immediate and long-term period after a new coronavirus infection was conducted at the premises of the autonomous public health care institution "Children's Hospital No. 8" in Ekaterinburg.
Aims of the study were development of a comprehensive psychological evaluation of the cognitive and emotional state of children with Post-COVID-19 syndrome based on structural and functional features of the brain by: i). analyzing psychological content of the processes that ensure the cognitive activity of children with Post-COVID-19 syndrome - mnemastic, speech, visual-spatial gnosis and praxis and ii) characterizing the state of higher mental functions in children with COVID-19 using a special set of neuropsychological methods developed by A.R. Luria and his school.7-9
Materials and Methods
Neuropsychological testing of children was organized online in a 24-hour in-patient unit, at home in the immediate (1-2 weeks) period following the treatment, and face-to-face in the day hospital of Ekaterinburg Children's Hospital No. 8 for children in the long-term period following the COVID-19 infection. The adaptation of the existing neuropsychological tests to study children remotely using digital technology was carried out as part of the research work of 4th year students at the Department of Medical and Preventive Medicine of Ural State Medical University of Ministry of Health of the Russian Federation.
The main study group consisted of 25 children (9 girls and 16 boys) aged between 12 and 17, who were admitted to the hospital with moderate severity of acute respiratory infections and reported family contact with COVID 19 patients (9 individuals) and children who had had mild COVID-19 within the preceding 12 months (16 individuals), including 8 children (50%) in the preceding 4 months and 8 (50%) in the preceding 6-12 months.
The control group consisted of 25 Moscow secondary school students (14 girls and 11 boys) aged between 12 and 16. Studies in the control group of children were conducted before the start of the pandemic.
The study protocol, prepared and executed in accordance with the Declaration of Helsinki. To participate in the study all patients or their patrons were preliminarly informed and signed an informed consent.
Block of techniques
Praxis: kinesthetic, spatial, dynamic, graphic; auditory-motor coordination.
Gnosis: visual, object-constructive, arithmetic problem solving.
Fig 1.
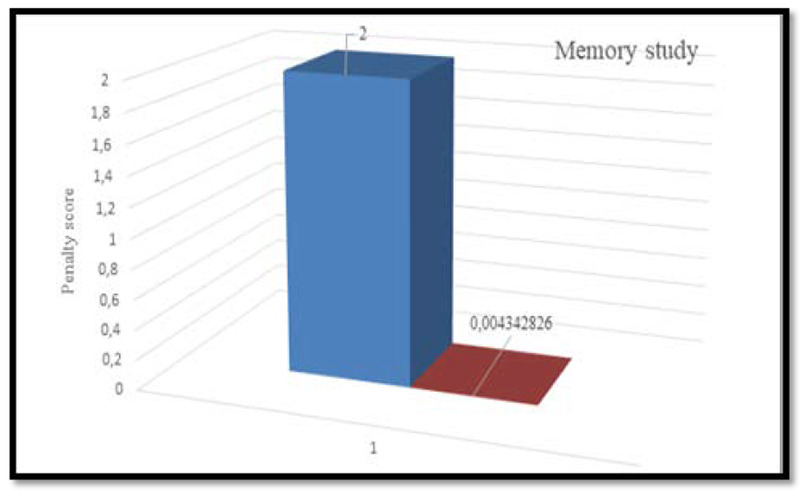
The results of the attention study in children of the main (blue color) and control (red color) groups.
Fig 2.
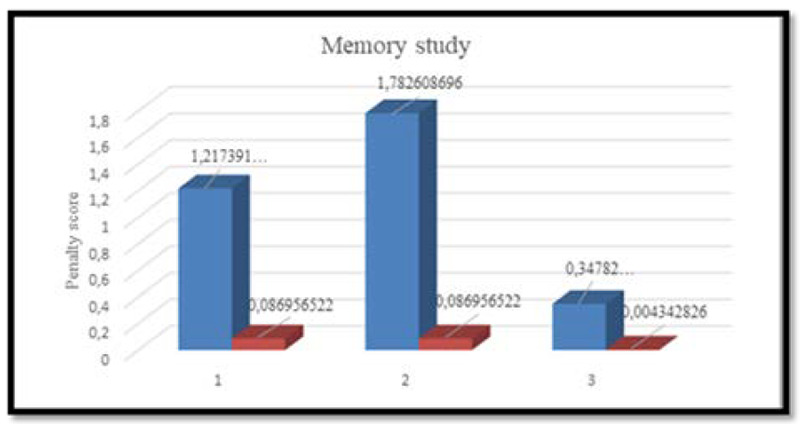
Auditory verbal direct memorization (1), two-phrase memorization (2) and visual memorization (3) of children in the main (blue color) and control (red color) groups.
Fig 3.
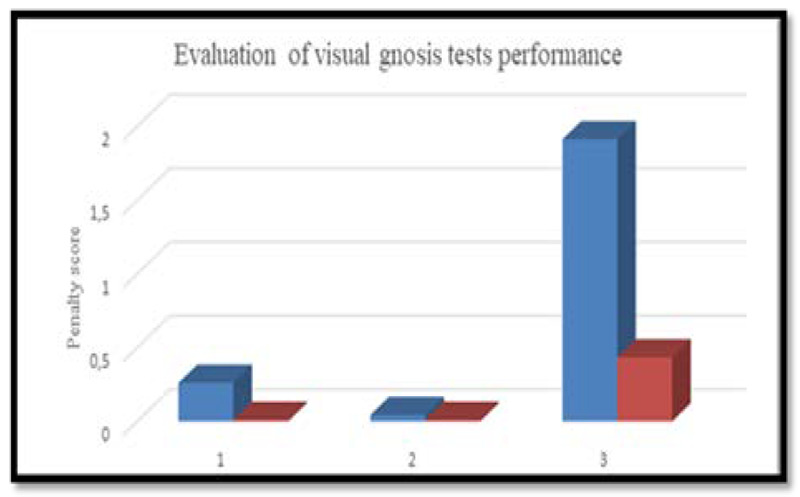
Results of visual gnosis study in children of the main (blue color) and control (red color) groups.
Fig 4.
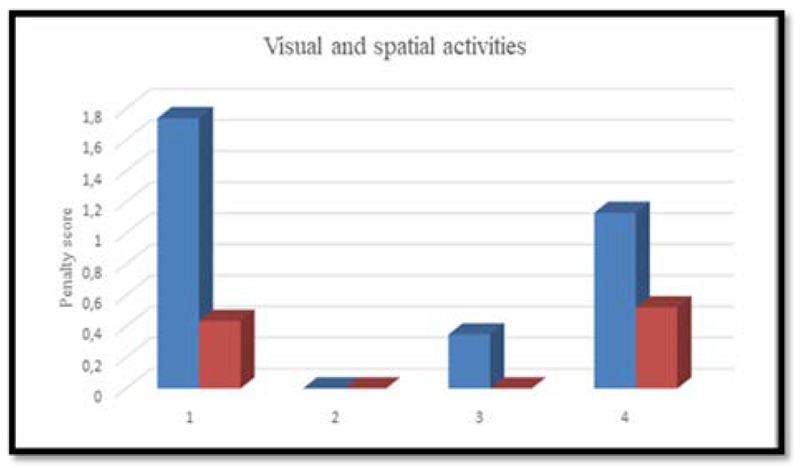
Evaluation of the results the visual and spatial function study in children of the main(blue color) and control (red color) group.
Memory: auditory-verbal, visual.
Motor attention ("Schulte tables" technique).
Thinking.
The methodological basis for the analysis of cognitive functions are: modern ideas of domestic psychology about higher mental functions as complex self-organizing processes, social in origin, intermediate in structure and conscious, arbitrary in the way of implementation;7,8 theory of systemic dynamic localization of higher mental functions;8 position of child neuropsychology and other neurosciences on the high functional specialization of various brain structures and their plasticity in childhood.9,10
Results and Discussion
The main group included children with a predominant infection of the respiratory organs: pneumonia (3 patients, 12%); acute bronchitis (2 patients, 8 %); ARVI with pulmonary syndrome (20 patients, 80%). A period of fever from 4 to 7 days (t 38.2-39.6 ° C) was observed in 84% of children, normal body temperature in 16%. An indication of family contact with patients with a new coronavirus infection was in all patients, a positive analysis of swab from the nasopharynx for SARS-CoV-2 RNA by PCR was present in 58% of children. Peripheral oxygen saturation SpO2 92-94% (25%) of children. Severe concomitant pathology in state of compensation before an acute illness was observed in 1 child of 13 years of age (bronchial asthma, condition after liver transplantation due to congenital atresia of the biliary tract, chronic hepatitis B, subcompensation stage). 44% of patients had no complaints related to the CNS. 54% of children independently noted that after suffering a coronavirus infection, they had the following complaints from the nervous system: impaired taste and smell: 32%; headaches: 12%; myalgia; 8%; hand numbness, hand tremor: 8%; sweating of the hands:8%; dizziness, "darkened vision” when bending:12%; weakness, fatigue, decreased exercise tolerance: 20%; memory impairment, academic performance decline: 28%; mood swings, irritability: 8%, meteorological dependence: 8%, dyssomnia, weakness in the legs, attention deficit, hyperkinesis: 4% each. A 17-year-old girl developed a persistent tremor in one hand. One patient reported short-term amnesia. For the first time, a neurologist diagnosed after an infection in 5 children, including cerebroasthenic syndrome: 2 patients; autonomic dystonia syndrome: 1 patient; attention deficit disorder: 1 patient; radiculopathy: 1 patient.
Fig 5.
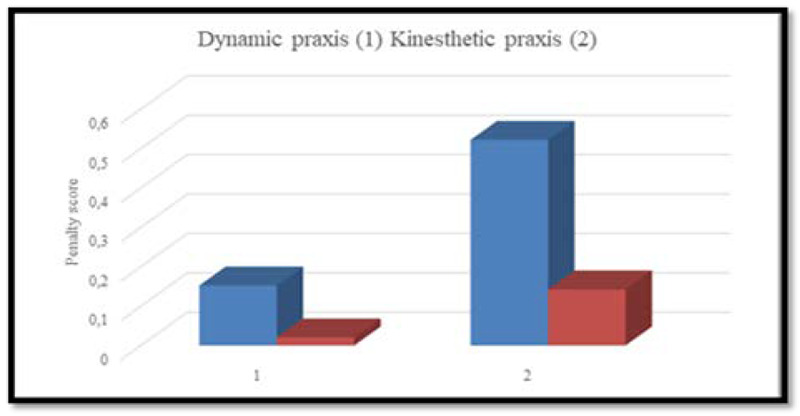
Evaluation of the results the visual and s Level of expression of dynamic (1) and kinesthetic (2) praxis impairments in children in the main (blue color) and control (red color) groups.
Fig 6.
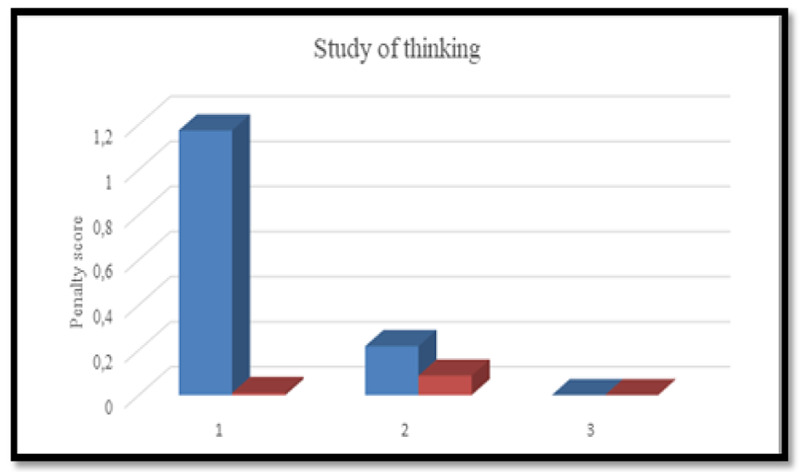
Evaluation of a study on thinking in children in the main (blue color) and control (red color) groups
Results of neuropsychological diagnostics.
When evaluating and analyzing the results obtained, age standards for implementation of samples were taken into account. The degree of manifestation of the identified violations was determined by a scoring system from 0 (no violations) to 3 points (presence of a pronounced defect). The level of complexity of the methods included in the complex of neuropsychological examination was determined by the possibility of independent and correct performance of diagnostic tests by the majority (> 75%) of adolescents in the control group of the corresponding age.11,12
Attention failure in children of the main group.
The analysis showed a significant degree of severity of attention disorders in patients of the main group compared with children in the control group (U-Mann-Whitney = 39.0; p-level = 0.00), according to the number of errors when performing tests in the method of "Schulte Tables" (Figure 1).
In the children of the main group were observed: a slow pace of the task, rapid exhaustion, distractibility, impaired concentration. This indicates the insufficiency of the neurodynamic component of activity, or 1 block of the brain according to Luria A.R. (energy, activation), with a topic of disorders in the brainstem, mediobasal frontotemporal parts of the brain, reticular formation and limbic structures.8
When performing a test for auditory direct memorization of 10 words in the main group, the following was found: an increase in the latent period, especially when reproducing from the first or second time; verbal paraphasia; speech perseveration; lack of regulation and control. The test “Memorizing two phrases” (semantic memorization) was performed incompletely by the children of the main group due to the influence of heterogeneous interference, a decrease in volume and a violation of the order of reproduction, a change in the grammatical structure of speech (by gender, number, case). Significant statistical differences were revealed with the children of the control group in the test for auditory-speech direct memorization (1) (U-Mann-Whitney = 104.0; p-level = 0.00027), and "Memorization of two phrases" (2) (U-Mann - Whitney=30.0; p-level=0.00). When performing a visual memory test, statistical differences between the main and control groups were not significant (3) (U-Mann-Whitney=206.0; p-level=0.2) (Figure 2).
The mechanism of such disorders is based on the insufficiency of the neurodynamic component of activity; the topic of the lesion is the mediobasal frontotemporal parts of the brain with the formation of the leading temporal neuropsychological syndrome (Т2).
Study of visual gnosis.
When performing these tests, the children of the experimental group experienced the greatest difficulties in recognizing unfinished images. A test for the identification of unfinished images, which requires the actualization of a holistic image, allows you to assess the formation of a holistic information processing strategy. Simultaneous agnosia, which is part of the neuropsychological TPO syndrome (temporo-parieto-occipital regions of the brain), was found. The success of this significantly differed in the main and control groups in the recognition of unfinished images (U-Mann-Whitney = 74.0; p-level=0.000009). Figure 3: 1 - identification of crossed out images, 2 - identification of superimposed images; 3- recognition of unfinished images.
Study of visuospatial function.
To study visual-spatial gnosis and praxis, a battery of neuropsychological methods was used: copying (houses, figures with superencipherment), telling the time by “blind” clock, a test for understanding logical and grammatical relationships, recognizing time by “blind” clock. The children of the main group made the following types of errors: topological (changes in the general scheme of the figure), metric (errors in estimating distances, angles and proportions), coordinate errors in the location of parts of the object (top-bottom and right-left). Figure 4: 1 – understanding of logical constructions (U-Mann-Whitney=104.0; p-level=0.00027); 2 – understanding of grammatical constructions (U-Mann-Whitney=230.0; p-level=0.458); 3 – copying the figure with half turn (180º) (U- Mann-Whitney =215,5; p-level =0,315); 4 – copying a perspective drawing (house) (U-Mann-Whitney=185.0; p-level=0.08) (differences are not significant). Violation of visual-spatial perception indicates the insufficiency of the TPO zone (temporal-parietal-occipital regions of the brain), which can present difficulties for children when learning geometry and stereometry.
Study of motor functions (kinesthetic and dynamic praxis
To study kinesthetic praxis, two-handed tests with visual control were used, dynamic praxis - the “fist-rib-palm” technique. The analysis of the performance of this test by children was conducted in accordance with the following parameters: serial organization of movements, retention and assimilation of the motor program, the presence of perseverations and errors in the serial organization of movements. The level of expression of impairments in dynamic praxis (U-Mann-Whitney=236.0; p-level=0.542) and kinesthetic praxis (U-Mann-Whitney=255.0; p-level=0.845) in children in the main group exceeded that in the control group, but the differences were not significant (Figure 5).
Impaired dynamic praxis is part of the premotor syndrome, and arbitrary regulation of motor functions relates to the syndrome of regulatory apraxia. Kinesthetic apraxia is a manifestation of inferior parietal syndrome.
A study into the structure of thinking (verbal and non-verbal components)
The following methods were used to assess the thinking function: problem solving, drawing up a story based on plot pictures, and “Fourth is a crowd”). The results of the study showed that difficulties in performing visual-imagery operations in children in the main group were due to impaired simultaneous analysis and synthesis. At the same time, some of the patients were "bogged down" in numerous details and required additional questions to understand the meaning of the image. Only 26.1% of the children in the main group performed the task correctly, which indicates insufficiency of the prefrontal parts of the brain. When solving tasks, 91.3% of children in the control group completed the task correctly and independently, while in the main group only 65.22% of test takers completely coped with the test, which is a sign of insufficiency of the TPO zone. Figure 6: 1 - understanding the meaning of a story picture (U-Mann-Whitney=104.0; p-level=0.00027); 2 - solving arithmetic problems (U-Mann-Whitney=230.0; p-level=0.46); 3 - "Fourth is a crowd" (U-Mann-Whitney=264.5; p-level=0.8).
The findings are consistent with international studies that have identified the effects of direct damaging effects of the virus, systemic inflammatory response and cerebral hypoxia on cognitive brain functions, structures such as the hippocampus and basal ganglia, which contain more enzymes involved in inflammatory responses than other areas, thus determining an increased risk for neurocognitive deficits affecting memory, attention and emotions.6 However, application of a neuropsychological diagnostic package, based on Luria A.R.'s theory of systemic dynamic localization of higher mental functions,8 made it possible to identify significant cognitive dysfunctions in children associated with COVID-19 compared to children examined before the pandemic. The topic of the disorders involves the temporo-parieto-occipital, mediobasal, frontotemporal, reticular formation, and limbic structures of the brain.
In conclusion, our report shows that: i) Comprehensive psychological diagnosis helps to identify the individual psychological characteristics, the nature of the defect and the degree of functional abilities of children with post-COVID-19 syndrome; ii) the findings indicate profound cognitive impairments occurring in initially unaffected children in the immediate and distant period after a non-serious new coronavirus infection with predominantly respiratory disease; iii) significant differences with the results of neuropsychological tests performed by the children in the control group before the pandemic suggest impairments in memory, attention, visual gnosis, visual-spatial function, kinesthetic and dynamic praxis, and verbal and non-verbal components of thinking; iv) drawing on A. R. Luria's concept, we can assume that the cognitive profile and pattern of neurological complaints of children in the main group indicate that the topic of the disorders involves the temporo-parieto-occipital, mediobasal frontotemporal regions of the brain, the reticular formation and the limbic structures; v) of particular importance is to developm remedial education programmes and an in-depth diagnostic algorithm that may identify the morphological substrate of cognitive disorders in children after COVID-19.
Acknowledgments
The authors thank the patients who volunteered for the study
List of acronyms
- CNS
Central nervous system
- TPO
Overlapping areas of the temporal, parietal and occipital cortex
Funding Statement
Funding: The study was funded by Pirogov Russian National Research Medical University of the Ministry of Health of the Russian Federation, Moscow.
Contributor Information
Lubov A. Troitskaya, Email: t-luba@mail.ru.
Inga A. Plotnikova, Email: inga63@bk.ru.
Georgy G. Avakyan, Email: avakyan_georgy@mail.ru.
Vera A. Erokhina, Email: verayerokhina@rambler.ru.
Oganes L. Badalyan, Email: epileptolog@mail.ru.
Antonina V. Muraveva, Email: homosaltans@yandex.ru.
Vera L. Zelentsova, Email: vera-zelentsova@mail.ru.
Oksana K. Khodko, Email: dgb8-ok@yandex.ru.
Sabina T. Safarova, Email: safarovasabina@bk.ru.
Evgenia I. Shirokova, Email: eugenias2000@mail.ru.
Ekaterina A. Rusina, Email: Erusina82@yandex.ru.
Natalia P. Sanina, Email: nataliasanina2@yandex.ru.
Andrey P. Rachin, Email: RachinAP@nmicrk.ru.
References
- 1.Shah W, Hillman T, Playford ED, Hishmeh L. Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ. 2021. Jan 22;372:n136. doi: 10.1136/bmj.n136. [DOI] [PubMed] [Google Scholar]
- 2.Khoreva MA. Postcovid syndrome — a new reality. Zhurnal Nevrologii i Psikhiatrii imeni S.S. Korsakova. 2021;121(10):131-137. (In Russ.). doi: 10.17116/jnevro2021121101131. [DOI] [PubMed] [Google Scholar]
- 3.Kabi A, Mohanty A, Mohanty AP, Kumar S. Post-COVID-19 Syndrome: A LiteratureReview. Journal of Advances in Medicine and Medical Research. 2020. Vol.32, No. 24. Р.289–295. doi: 10.9734/JAMMR/2020/v32i2430781. [Google Scholar]
- 4.Stefano GB, Ptacek R, Ptackova H, Martin A, Kream RM. Selective Neuronal Mitochondrial Targeting in SARS-CoV-2 Infection Affects Cognitive Processes to Induce 'Brain Fog' and Results in Behavioral Changes that Favor Viral Survival. Med Sci Monit. 2021. Jan 25;27:e930886. doi: 10.12659/MSM.930886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buonsenso D, Munblit D, De Rose C, Sinatti D, Ricchiuto A, Carfi A, Valentini P. Preliminary evidence on long COVID in children. Acta Paediatr. 2021. Jul;110(7):2208-2211. doi: 10.1111/apa.15870. Epub 2021 Apr 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Almeria M, Cejudo JC, Sotoca J, Deus J, Krupinski J. Cognitive profile following COVID-19 infection: Clinical predictors leading to neuropsychological impairment. Brain Behav Immun Health. 2020. Dec;9:100163. doi: 10.1016/j.bbih.2020.100163. Epub 2020 Oct 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adrianov OS. On the principles of structural and functional organization of the brain. Selected works. Moscow-Leningrad: Nauka, 1999;280. Russian. [Google Scholar]
- 8.Luria A.R. Human higher cortical functions and their disorders in local brain lesions. A.R. Luria. St. Petersburg: “Piter”, 2008. (In Russ.). [Google Scholar]
- 9.Chomskaya ED. Neuropsychology: 4th edition. ED. Chomskaya. St. Petersburg: “Piter”, 2005;496. Russian. [Google Scholar]
- 10.Akhutina TV, Polonskaya NN, Yablokova LV. Neuropsychological analysis of individual differences in children: evaluation parameters Neuropsychology and psychophysiology of individual differences. Moscow-Orenburg, 2017;132-152. Russian. [Google Scholar]
- 11.Balashova EY, Kovyazina MS. Neuropsychological diagnostics. Classical stimulus materials. 5th ed. Genesis. 2015;70. Russian. [Google Scholar]
- 12.Glozman JM. Quantification of neuropsychological examination data. JM Glozman. 2019;25. (In Russ.). [Google Scholar]


