Abstract
Telerehabilitation for pain management uses communication technology to minimize geographic barriers. Access to such technology has proven critically important during the coronavirus disease-2019 pandemic and has been useful for patients with chronic pain disorders unable to travel. The evaluation and treatment of such disorders requires a whole health approach that individualizes treatment options and delivers care through a biopsychosocial approach. The goals of care are unchanged from an in-person patient-provider experience. Telerehabilitation can be successfully implemented in pain management with appropriate consideration for staging an evaluation, a structured approach to the visit, and application of standard clinical metrics.
Keywords: Telerehabilitation, Telehealth, Telemedicine, Chronic pain, Pain management, Opioids, Whole health approach, Patient-centered care
Key points
-
•
Telerehabilitation for pain management decreases the burden of geographic, economic, and physical barriers for patients with chronic pain disorders.
-
•
The successful implementation of telerehabilitation for pain should include a structured set-up, interview, and examination to reduce errors and variability in patient outcomes.
-
•
The coronavirus disease-2019 public health emergency, along with changes to the Ryan Haight Act, and reimbursement schedule has increased access to telerehabilitation for pain management.
-
•
A whole health approach to pain management engages patients in self-care, emphasizes partnerships in a team-based approach, and supports general health and well-being.
Introduction
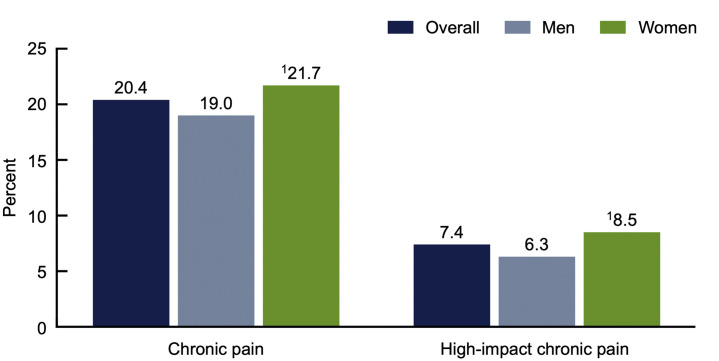
Timely access to medical care helps prevent and mitigate the impact chronic pain has on patients, their environment, and the health care system. In the United States, 20.4% of adults experience chronic pain and 7.4% experience high impact chronic pain, with women, non-Hispanic whites, and those older than 65 years most affected (Fig. 1 ).1 These patients often require effective coordination of services between their medical providers to ensure communication and establish an interdisciplinary platform of care. Despite these efforts, barriers may still exist that make in-person medical care impractical, inconvenient, or unsafe. Such obstacles include the hardship of securing transportation for an appointment, which affects an estimated 3.6 million Americans each year who cannot obtain medical care owing to a lack of transportation. These individuals demonstrate a higher prevalence of medical comorbidities, including pain-related disorders.2 To ensure access to timely care, especially in circumstances such as the coronavirus disease-2019 pandemic, virtual visits may provide the safest avenue to medical services.
Fig. 1.
Percentage of adults aged 18 and over with chronic pain and high-impact chronic pain in the past 3 months, overall and by sex, United States, 2019.
(From Centers for Disease Control and Prevention (CDC). Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high-impact chronic pain among U.S. adults, 2019. NCHS Data Brief, no 390. Hyattsville, MD: National Center for Health Statistics. 2020.)
Telemedicine was formally identified in the 1970s but has played a role in medical care for more than 100 years.3 The term literally means “healing at a distance” though more recently has been defined by the World Health Organization as:
The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.4
Telemedicine uses many of the technologies already in use by the general population for routine communication, with modifications made for the purpose of health care delivery. Telerehabilitation for pain management provides a method for the prompt delivery of pain care to a vulnerable population when there is no alternative, or to improve on conventional approaches.5 To develop the necessary skills, medical providers should review relevant evidence-based principles and practice a structured patient-centered approach. Regulations and guidance can vary during a given time period, with medical, legal, and financial implications. For example, paying close attention to the evolving telehealth guidelines for opioid prescribing and risk mitigation strategies can prevent serious health-related consequences, maintain compliance with governmental requirements, and ensure proper billing practices for medical encounters. This article outlines telerehabilitation strategies to deliver patient-centered care with a whole health approach to pain disorders.
Overview
As technological innovations have fostered development in the field of telerehabilitation, the coronavirus pandemic has spurred rapid transformation in health care. Before understanding how to best implement telerehabilitation for the purposes of pain management, it is useful to revisit the general principles of telemedicine. The roles and capabilities of telemedicine are dynamic, and the World Health Organization has identified 4 central pillars:
-
1.
“To provide clinical support
-
2.
To overcome geographic barriers
-
3.
The utilization of various types of information and communication technologies
-
4.
To improve health outcomes.”6
Adapting these principles to the telerehabilitation of pain is particularly challenging given the sheer number and complexity of chronic pain syndromes. The nature of this complexity is captured by the newly revised definition of pain by the International Association for the Study of Pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”7
The International Association for the Study of Pain attempts to provide a contextual basis for this definition by laying out several important reflections. Fundamentally, pain is a separate phenomenon from nociception, meaning that the experience of pain cannot be ascribed to sensory neuron depolarizations alone. Beyond this elementary biological basis, pain is also impacted by both psychological and social factors. Furthermore, the conceptualization of pain as an experience is one that is learned from and shaped by a culmination of life experiences. Last, and perhaps most important from the perspective of a provider, a patient’s pain should be respected regardless of whether or not objective findings are present.7
Managing pain through telerehabilitation has many challenges and, despite advancements in technology, such as video teleconferencing, has several drawbacks. These limitations include interpreting nonverbal cues, rapport building, and performing an in-depth physical examination, all of which are necessary components for pain management. Therefore, approaching the diagnosis of pain etiologies by telemedicine requires a systematic approach, including a focused pain history, physical observation, and a mental health assessment. Combining these elements with a knowledge of pain physiology can assist in identifying the pain generator and assist in designing a therapeutic blueprint. The treatment of pain should also be met systematically. Therapeutic measures should concentrate on evidence-based approaches that minimize risk, provide holistic and integrated care, and enrich function and quality of life.
A general approach to the telediagnosis of chronic pain
A virtual evaluation will likely be a new experience for most patients. To improve a patient’s response to this format, a few general considerations should be taken into account before and during a visit. The office space of the telehealth provider should be professional, use appropriate lighting, and be equipped with a high-quality camera and microphone to best imitate a face-to-face evaluation. Additionally, from an individual standpoint, the telehealth provider should look into the camera rather than at their computer screen to better facilitate eye contact. The provider should also pay close attention to delay in terms of audio and video input and output to allow patients to fully express their thoughts without interruption. Physicians rely on their skills of observation on a daily basis, but it may be even more important when transitioning to a virtual environment. Subtle changes in language, tone, sound, facial expression, and movement can all be windows into the thoughts and feelings of a patient. Last, an expression of compassion toward the patient comes as second nature in an in-person evaluation; however, much of this nuance may be lost in a video format. It is, therefore, important for the telehealth provider be attentive and convey empathy during the session.
Evaluation
Clinical History
Similar to a traditional in-person evaluation, the initial telemedicine evaluation for a chronic pain complaint begins with the clinical history (Box 1 ). The clinical history not only localizes the pain, but also distinguishes whether the pain is somatic, visceral, neuropathic, or mixed in etiology. The history also provides invaluable information in terms of what measures have previously been attempted in alleviating the pain complaints and can, therefore, guide consideration for future therapies. Qualitative tools should also be used to augment the clinical history by assessing the impact of pain on the patient’s physical, emotional, and social functioning. Last, a thorough assessment will include a consideration of the patient’s cultural background, personality, and psychological status. Within the context of telemedicine, patients can be sent a battery of validated assessment tools gauging pain and psychosocial factors before their visit.
Box 1. Pain clinical history prompts.
-
•
What is the intensity of pain or discomfort on a 0 to 10 scale?
-
•
When did the pain start?
-
•
Was there any preceding injury or surgery before the onset of pain?
-
•
Where is the pain located?
-
•
Does the pain radiate or change with activity?
-
•
What is the quality of pain (sharp, dull, throbbing, aching, tingling, numbness, burning, shooting)?
-
•
What activity or posture provokes the pain?
-
•
What alleviates the pain?
-
•
What medications have you tried, and did they help?
-
•
What therapies have you tried?
-
•
What additional modalities have you tried?
-
•
How does the pain affect your day-to-day activities?
As mentioned elsewhere in this article, pain is a highly subjective experience and requires the identification of a metric that can be monitored over time and serve as a measure for response to treatment. There are many tests available that assess a patient’s pain intensity and include single metric questions and comprehensive surveys. The tools discussed in this article can be provided to a patient before their scheduled appointment and reviewed at the time of the visit.
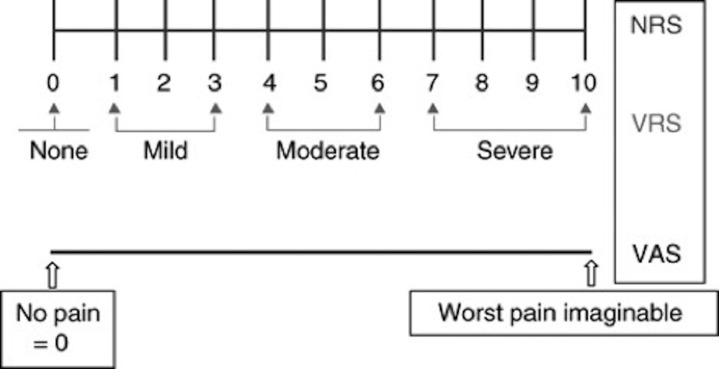
Unidimensional Self-Report Scales
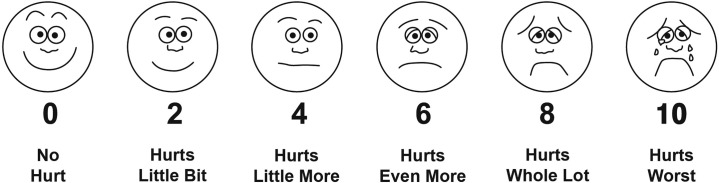
Unidimensional self-report scales typically operate on a “0 to 10” scale or in a derivative fashion. These scales are simple, valid, and reliable in both clinical and research settings.8 Examples include the Numeric Rating Scale, Verbal Rating Scale, visual analogue scale, and Wong-Baker FACES pain rating scale (Figs. 2 and 3 ).
Fig. 2.
Numeric rating scale (NRS), verbal rating scale (VRS), and visual analog scale (VAS).
(From Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. British Journal of Anaesthesia. 2008;101(1):17-24. https://doi.org/10.1093/bja/aen103.)
Fig. 3.
Wong-Baker FACES Pain Rating Scale. Explain to the person that each face represents a person who has no pain (hurt), or some, or a lot of pain. Face 0 doesn’t hurt at all. Face 2 hurts just a little bit. Face 4 hurts a little bit more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much as you can imagine, although you don’t have to be crying to have this worst pain. Ask the person to choose the face that best depicts the pain they are experiencing.
(From Wong-Baker FACES Foundation (2020). Wong-Baker FACES® Pain Rating Scale. Retrieved [11/7/20] with permission from http://www.WongBakerFACES.org.)
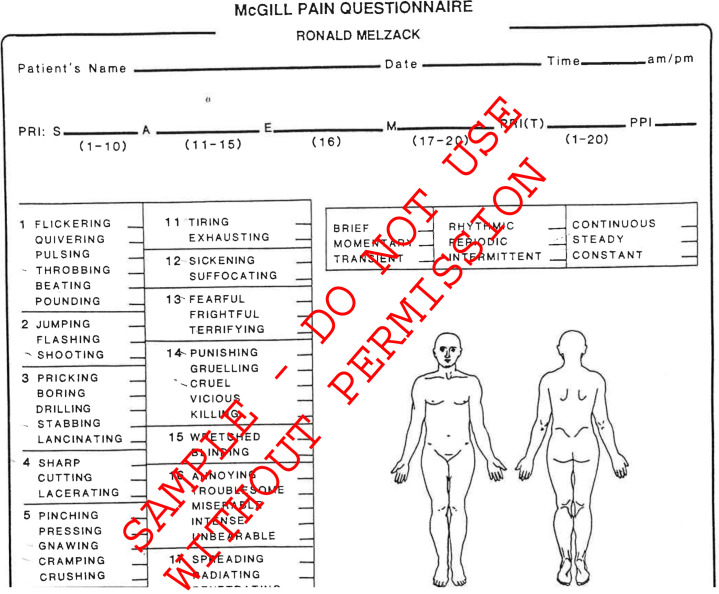
Multiple Dimension Instruments
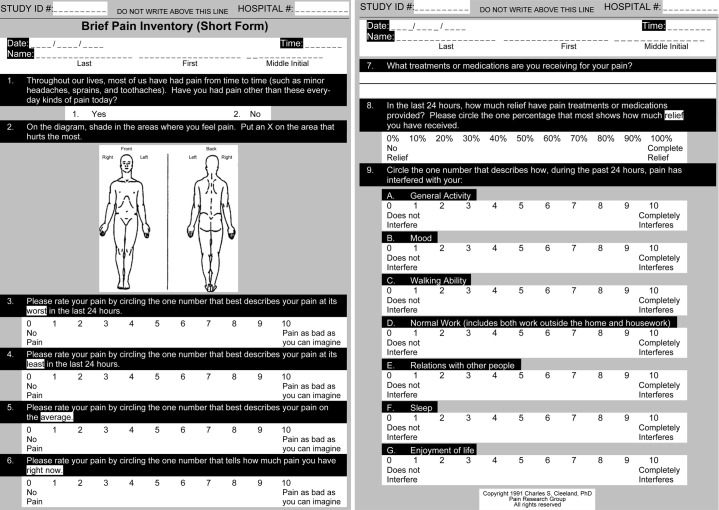
These tools provide a more comprehensive evaluation of a patient’s subjective pain experience oftentimes by taking in account the impact of pain on quality of life and function. Examples include the commonly used McGill Pain Questionnaire (Fig. 4 ) and Brief pain inventory (Fig. 5 ), which incorporates the impact of chronic pain on day to day functioning.
Fig. 4.
McGill pain questionnaire.
(From Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1975; 1:277-99; Mapi Research Trust, Lyon, France, https://eprovide.mapi-trust.org, with permission.)
Fig. 5.
Brief pain inventory.
(Copyright ©2009. MD Anderson Cancer Center. Reproduced from Cleeland CS. The Brief Pain Inventory User Guide. Available from: https://www.mdanderson.org/documents/Departments-and-Divisions/Symptom-Research/BPI_UserGuide.pdf.)
Physical Examination
Perhaps the most obvious limitation of a telehealth visit is the inability to perform a direct physical examination. For pain conditions, a thorough physical examination is integral to making an accurate diagnosis. It is, therefore, imperative to understand the strengths and limitations of the virtual examination. In general, the virtual examination for a pain visit follows a standard in-person examination. The telehealth provider should localize the presenting symptoms to the appropriate anatomic body part by history and proceed with inspection, palpation, range of motion, and special testing.
Inspection
Valuable information can be gleaned from simple observation. To facilitate observation via camera, the patient should be instructed to wear a short-sleeved shirt and shorts for the virtual examination. Next, correct laterality should be determined because the video feed may be mirrored. Therefore, before beginning any virtual examination, the patient should be asked to indicate which side is right and which side is left. Once the logistics are established, the inspection can begin.
The provider should initiate the observation portion of the examination by assessing general appearance. Hygiene, grooming, and affect are all characteristics that can be adequately assessed by the virtual examination and may provide significant insight into a patient’s mood and state of mind. After assessing general appearance, the provider should locate the anatomic region of interest as determined by the clinical history. Any obvious asymmetry from right to left, atrophy, hypertonicity, anatomic deformity, discoloration, or presence of swelling should be noted.
Palpation
The difference between pain as a subjectively reported symptom versus tenderness, which is objectively inferred by a health care provider, often relies upon palpation. Within a virtual examination, the provider must rely on the patient to report the findings of palpation. Palpation as a means to obtain objective data is therefore limited in a virtual examination because it is difficult to determine how much pressure is being applied by the patient or assistant during palpation. Despite this limitation, palpation is useful in determining the focal point of a patient’s pain; the provider can instruct a patient or family member toward anatomic landmarks. Palpation is also useful in the assessment of abnormal findings to gauge temperature, which may be increased with inflammation. Swelling can be palpated to determine underlying mobility, edema, or induration. Areas of erythema can be palpated to determine blanching; last, areas of asymmetry can be palpated to determine whether soft tissue laxity or osseous reducibility exists.
Range of motion
Before assessing for range of motion, patients should be instructed to position themselves or the camera to allow for a full body view. Additionally, providers should assess whether there exists enough space for the patient to safely move without restriction such that all planes of motion can be captured. Unfortunately, for the virtual physical examination, only active range of motion can be assessed. Passive range of motion can, however, be assessed with the assistance of a family member, friend, or assistant.
For any given joint, all planes of motion should be tested to their fullest extent. Careful attention should be paid to the smoothness of action and any restrictions to the degree of expected motion. Any deviations from full range of motion should be assessed for a limitation owing to pain or to an intrinsic defect of the joint itself. It is important to keep in mind that any patient that can actively resist gravity with respect to a particular joint movement is displaying at least a grade 3/5 motor strength for that muscle.
Special testing
Last, in the absence of a nonclinician assistant, consideration must be placed for a patient’s functional level when deciding upon which special tests to perform. There are several special tests that can be performed by the patient alone with adequate instruction and guidance from the telehealth provider. In general, the smaller the joint under consideration, the greater the feasibility of a nonassisted special test. For example, special testing of the hands including Phalen’s test, Tinel’s sign, Finkelstein test, and the CMC grind can generally be easily imitated by the patient. Special testing of the larger joints such as the lumbar spine or the hips requires an assistant, but can be achieved with guidance.9
Telehealth provider considerations
Throughout the virtual examination, it is critical to the success of a telehealth visit that the provider constantly be attuned to the subtle changes of a patient. Changes in facial expression, grimaces, and breathing patterns all provide insight into what a patient may be feeling without the need for verbal expression. The subtle reactions of a patient to any active or special testing maneuvers can not only guide the clinician, but also solidify the diagnosis.
Mental Health Assessment
A chronic pain evaluation is not complete without, at a minimum, a psychosocial screen. The simultaneous treatment of comorbid mental health disorders has been demonstrated to improve chronic pain symptoms.10 , 11 Additionally, the psychosocial factors of any individual experiencing chronic pain cannot be understated and are predictive of morbidity.12 Therefore, validated screening tools for mental health disorders, patterns in cognition, and alcohol or substance use disorder is an absolute necessity. The surveys described in this article can be combined in a single packet with the aforementioned unidimensional and multidimensional instruments for pain and delivered to the patient before evaluation by the telehealth provider.
Mental Health Screening Tools
Depression: Patients Health Questionnaire-9
Anxiety: General Anxiety Disorder-7
Post-traumatic stress disorder: Primary Care PTSD for DSM-V
Bipolar disorder: Mood Disorder Questionnaire
Pain catastrophizing scale
Alcohol or substance use screening tools
CAGE Adapted to Include Drugs
Treatment
Pharmacologic
Pharmacologic treatments for pain and rehabilitation in telemedicine are selected in a similar fashion to in-person visits. According to the diagnosis, treatments may be chosen for somatic, visceral, neuropathic, and mixed pain etiologies. Common medications that are used in pain and rehabilitation include nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, acetaminophen, and medications for muscle spasm and neuropathic pain. NSAIDs provide analgesic and anti-inflammatory properties by preventing the creation of proinflammatory prostaglandins.13 NSAIDs also bind and block the cyclo-oxygenase-2 enzyme to decrease prostanoid production and relieve pain. Table 1 includes common NSAID medications and dosing. Opioids produce pain relief by binding mu, kappa, and delta opioid receptors in the central nervous system to block the release of neurotransmitters that propagate pain signals. Table 2 provides a summary of common oral opioids.14 Of note, the Centers for Disease Control and Prevention and the Veterans Administration/Department of Defense do not recommend long-term opioid treatment for most patients with chronic pain.15 , 16 If opioids are used, proper safety precautions should be in place, including long-term opioid consents, naloxone kit prescribing, prescription drug monitoring program review, and urine toxicology screening. Urine toxicology screening may be performed at an appropriate health care facility or laboratory to ensure confirmation screening, urine specific gravity, and the presence of adulterants.
Table 1.
Common NSAID dosing
| Medication | Starting Dose | Usual Dosing Range | Other |
|---|---|---|---|
| Aspirin | 325 mg 3 times a day | 325–650 mg 4 times a day | Doses of 3600 mg/d are needed for anti-inflammatory activity |
| Celecoxib | 100 mg/d | 100 mg twice daily or 200 mg/d | |
| Diclofenac XR Diclofenac IR |
100 mg/d 50 mg twice a day |
100–200 mg/d 50–75 mg twice a day |
|
| Etodolac | 300 mg twice a day | 400–500 mg twice a day | |
| Ibuprofen | 200 mg 3 times a day | 1200–3200 mg/d in 3 to 4 divided doses | Available OTC and Rx |
| Indomethacin Indomethacin SR |
25 mg twice a day 75 mg SR once daily |
Titrate dose by 25–50 mg/d until pain controlled or maximum dose of 50 mg 3 times a day Can titrate to 75 mg SR twice daily if needed |
|
| Ketoprofen | 50 mg 3 times a day | 50–75 mg 3 to 4 times a day | |
| Meloxicam | 7.5 mg/d | 15 mg/d | |
| Naproxen | 250 mg twice a day | 500 mg twice a day | Available OTC and Rx |
| Naproxen sodium Naproxen sodium CR |
220 mg twice a day | 220–550 mg twice a day 375–750 mg twice a day |
|
| Salsalate | 500 mg twice a day | 500–1000 mg 2 to 3 times a day |
Abbreviations: CR, controlled release; IR, immediate release; OTC, over-the-counter; Rx, prescription; SR, sustained release; XR, extended release.
Data from Buys LM, Wiedenfeld SA. Osteoarthritis. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 10e. McGraw-Hill; Accessed October 06, 2020. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=133893029.
Table 2.
Common opioid dosing
| Medication | Usual Dosing Range | Other |
|---|---|---|
| Morphine | PO 5–30 mg every 4 h SR 15–30 mg every 12 h (may need to be every 8 h in some patients) |
Drug of choice in severe pain, use with caution in renally compromised patients |
| Hydromorphone | PO 2–4 mg every 4–6 h | Use in severe pain |
| Codeine | PO 15–60 mg every 4–6 h | Use in mild to moderate pain |
| Hydrocodone | PO 5–10 mg every 4–6 h | Use in moderate/severe pain |
| Oxycodone | PO 5–15 mg every 4–6 h CR 10–20 mg every 12 h |
Use in moderate/severe pain |
| Fentanyl | Transdermal 25 μg/h every 72 h Transmucosal, intranasal, and sublingual dosing based off of individual product |
Do not use transdermal patch in acute pain Follow product-specific initiation and titration dosing recommendations |
| Methadone | PO 2.5–10 mg every 8–12 h | Effective in severe chronic pain Equianalgesic dose of methadone when compared with other opioids will decrease progressively the higher the previous opioid dose. Methadone prescribed for maintenance or detoxification treatment and must be dispensed under a Substance Abuse and Mental Health Services administration–certified opioid treatment program |
| Buprenorphine | Transdermal delivery systems 5, 7.5, 10, 15, 20 μg/h every 7 d Buccal film 75 μg every 12 h to 900 μg every 12 h |
Second-line agent for moderate-to-severe pain May precipitate withdrawal in opiate-dependent patients Detailed manufacturer dosing conversion recommendations exist Buprenorphine products that contain naloxone (Suboxone) should be considered in patients with OUD). The prescribers of buprenorphine/naloxone products for OUD require a Drug Enforcement Agency waiver |
| Tramadol | PO 50–100 mg every 4–6 h ER PO 100 mg every 24 h |
Maximum dose for nonextended release, 400 mg/24 h; maximum for extended release, 300 mg/24 h Decrease dose in patient with renal impairment and in the elderly |
Abbreviations: CR, controlled release; ER, extended release; OUD, opioid use disorder; PO, oral; SR, sustained release.
Data from Herndon CM, Strickland JM, Ray JB. Pain Management. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 10e. McGraw-Hill; Accessed October 06, 2020.2020. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=146063604.
Medication monitoring will need to be planned before prescribing pharmacologic treatments. Table 3 includes common adverse drug reactions and monitoring parameters. For example, if laboratory monitoring is not feasible, alternative treatments should be chosen. Many pharmacies can also mail prescriptions to patient’s residences and provide telephonic medication counseling.
Table 3.
Adverse drug reactions and monitoring parameters
| Medication | Adverse Drug Reactions | Monitoring Parameters | Comments |
|---|---|---|---|
| Acetaminophen | Hepatotoxicity | Total daily dose limits | Use caution with multiple acetaminophen-containing products—total 4 g per 24-h limit |
| Opioids | Sedation, constipation, nausea, dry mouth, hormonal changes | Periodic assessment of renal (serum creatinine, eGFR) and hepatic (LFTs) function If methadone is used, EKG should be obtained before initiating treatment, at 30-d follow-up, and at least annually thereafter |
Risks of addiction, dependence, and drug diversion |
| NSAIDs | Dyspepsia, cardiovascular events, GI bleeding, renal impairment | BUN/creatinine, hemoglobin/hematocrit, blood pressure | Risks higher in those older than 75 y of age |
Abbreviations: BUN, blood urea nitrogen; eGFR, estimated glomerular filtration rate; EKG, electrocardiogram; GI, gastrointestinal; LFT, liver function test.
Data from Buys LM, Wiedenfeld SA. Osteoarthritis. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 10e. McGraw-Hill; Accessed October 06, 2020. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=133893029.
Pharmacologic treatments can be provided by remote prescribing only after a patient–provider interaction. The Ryan Haight Online Pharmacy Consumer Protection Act of 2008 requires an in-person patient examination before delivering, distributing, or dispensing controlled substances. The Ryan Haight Act was drafted in response to Internet pharmacies that were dispensing controlled substances online without prescribers seeing and evaluating the patient.17
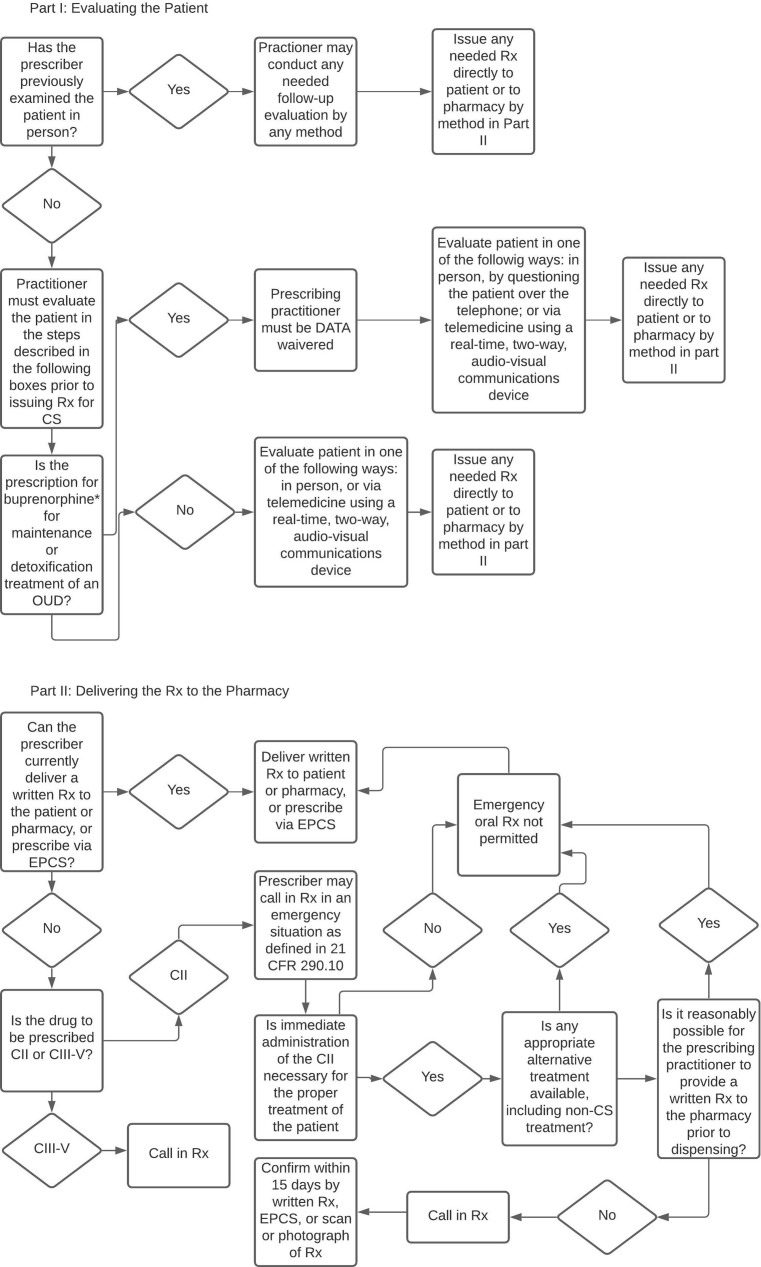
In March of 2020, the Drug Enforcement Agency (DEA) detailed exceptions to the Ryan Haight Act to allow controlled substance prescribing via telehealth without a prior in-person visit and examination.18 The designation of a Department of Health and Human Services public health emergency allows DEA-registered practitioners to issue controlled substances without a prior in-person evaluation if the following conditions are met: (1) the prescription is issued for a legitimate medical purpose in the normal course of the professional practice, (2) the telehealth platform uses audio-visual, real-time, 2-way communication, and (3) the practitioner is acting in accordance with applicable federal and state laws. The public health emergency exception applies to all schedule II through V controlled substances in all areas of the United States. The exemption rules remain in effect for as long as the public health emergency is in place. The designation of a public health emergency may also activate Section 1135 Waiver of the Social Security Act, which, for example, may waive or modify Medicare, Medicaid, Children’s Health Insurance Program, and Health Insurance Portability and Accountability Act requirements to allow health care services to meet individuals’ needs.19 Fig. 6 outlines the process of providing controlled substances to patients via telehealth as per DEA regulations. For additional information, the DEA has also published a coronavirus disease-2019 related informational webpage at www.deadiversion.usdoj.gov/coronavirus.html.20
Fig. 6.
DEA-compliant prescribing of controlled substances via telehealth. C, schedule; CS, controlled substance; DATA, Drug Addiction Treatment Act of 2000; EPCS, electronic prescriptions for controlled substances; OUD, opioid use disorder; Rx, prescription. Note: aMethadone cannot be prescribed for maintenance or detoxification treatment and must be administered or dispensed directly to the patient for that purpose. 21 CFR 1306.07(a).
(From How To Prescribe Substances To Patients During The COVID-19 Public Health Emergency. Drug Enforcement Agency: 2020. https://www.deadiversion.usdoj.gov/GDP/(DEA-DC-023)(DEA075)Decision_Tree_(Final)_33120_2007.pdf. Accessed November 12, 2020.)
Nonpharmacologic
The management of chronic pain frequently requires a multidisciplinary approach that takes advantage of pharmacologic and nonpharmacologic modalities. The nonpharmacologic modalities are well-suited for a telerehabilitation approach. Evidence-based, nonpharmacologic therapies for the management of pain are generally encompassed within 3 broad categories: psychological and behavioral therapies, exercise and movement therapies, and manual therapies. Of these 3 categories, the psychological and behavioral therapies have an advantage in terms of evidence as well as ease of delivery. Although the exercise and movement therapies contain several therapies such as Tai Chi and yoga that are beneficial for chronic pain, there currently is insufficient evidence supporting its use via telemedicine.21 , 22 Last, the manual therapies require a hands-on approach by a licensed provider and therefore fall out of the scope of telerehabilitation.
The overall philosophy of the psychological and behavioral therapies are similar in that they are all biopsychosocial interventions. As a result, their delivery to patients also follow similar schemata.23 These therapies are time-limited protocols that are delivered by a trained expert in a standardized format and rely on goal-oriented lessons, active participation, and the tracking of progress by objective metrics.24 Three well-known psychological and behavioral therapies that have found sufficient evidence in the treatment of chronic pain via telemedicine are cognitive behavioral therapy (CBT), acceptance and commitment therapy (ACT), and mindfulness-based stress reduction.
Cognitive behavioral therapy
CBT is a form of active psychotherapy that uses the interconnected nature of thoughts, behaviors, and feelings as a model to effect change. Within the context of pain management, the goal of CBT is to diminish both the maladaptive patterns of thoughts and behaviors that drive feelings of pain.25 In a 2012 Cochrane review of randomized clinical trials addressing chronic pain with CBT versus usual treatment or wait-listed controls, CBT was found to have small effects on decreasing pain and disability, as well as moderate effects on easing catastrophizing thoughts.26
CBT with the use of video chat can easily be practiced within the comfort of a patient’s home. The application of CBT through technological innovations has also shown to be beneficial in the management of chronic pain through randomized clinical trials. In the 2017 Cooperative Pain Education and Self-management (COPES) trial, interactive voice response CBT was found to be noninferior to in-person CBT in the management of chronic back pain. Patients randomized to the interactive voice response CBT arm were provided a self-help manual as well as weekly pre-recorded feedback from their therapist based on their outcome metrics. At the conclusion of the 3-month trial, the primary outcome of average pain measured by the Numeric Rating Scale was −0.77 for the interactive voice response CBT arm and −0.80 for the in-person CBT arm with a mean difference between groups of 0.07 (95% confidence interval, −0.67 to –0.80). Interestingly, patients in the virtual arm of the study also participated in more sessions than the in-person arm (mean difference, 2.3; P<.001).27
Acceptance and commitment therapy
ACT is a subset of CBT and is a relatively newer form of behavioral psychotherapy. The major aim of ACT is to promote psychological flexibility, examining thoughts as they come and go rather than wrestling with negative feelings. In contrast, CBT attempts to change fundamental beliefs. In this way, ACT can be thought of as a more passive engagement as compared with CBT.28 In a 2017 systematic review and metanalyses of 11 randomized controlled trials with a total sample size of 863, participation in ACT compared with control conditions was found to have medium to large effect sizes on pain acceptance and psychological flexibility, as well as small to medium effect sizes on improved functioning, anxiety, and depression.29
A 2017 randomized noninferiority trial of 129 veterans demonstrated that ACT delivered by a video teleconferencing platform was as effective as in-person therapy in terms of the primary outcome of pain interference. This study also supported noninferiority of video teleconferencing delivery in regard to several secondary outcomes including mental and physical health quality of life.30 Given the benefits of ACT for managing chronic pain as well as improving function and overall quality of life, transitioning toward a video-based platform is an option in situations of poor access to therapy.
Mindfulness-based stress reduction
Mindfulness-based stress reduction seeks to reframe a patient’s relationship to pain through detached self-observation.31 Mindfulness-based interventions have the benefit of being simple to use and least reliant on technology. Instructions and protocols can be delivered to patients through a variety of mediums, including written instructions, telephone, video conferencing, and smartphone applications. Compared with CBT and ACT, there is less evidence supporting the use of mindfulness-based stress reduction for chronic pain. There are, however, meta-analyses demonstrating that mindfulness interventions for chronic pain do have small beneficial effects on pain symptoms as well as mental and physical health quality of life metrics.32 , 33 Tele-mindfulness interventions have also demonstrated significant improvements in key aspects of chronic pain syndromes, including pain catastrophizing, suffering levels, and mental health.34
Exercise therapies
Exercise-based therapy and physical therapy oftentimes form the foundation for conservative treatment of musculoskeletal pain. Moreover, regular physical activity is widely accepted to be essential for overall quality of life, mood, and function. A 2017 Cochrane review examining physical activity and exercise-based interventions for chronic pain suggests that exercise interventions yield improved pain severity, physical function, and quality of life, albeit with a low level of evidence. Importantly, these findings were also in the setting of minimal adverse events.35 Similar findings were found in a telemedicine approach. A 2017 systematic review with a total sample size of 3575 concluded that compared with no intervention, telemedicine-based exercise intervention was beneficial for reducing pain in patients experiencing chronic pain.36 Although there is a lack of strong evidence for the treatment of chronic pain with an exercise-based intervention, patients should be encouraged to maintain mobility through appropriate exercise and activity. Last, we defer the discussion of any specific physical therapies or exercises, because the musculoskeletal pain conditions that would benefit from physical medicine typically require a highly individualized movement regimen.
Summary
Telerehabilitation for pain management uses communication technology to minimize barriers posed by geographic separation. Access to such technology has proven critically important during the coronavirus disease-2019 pandemic, but has also been useful in patients with chronic pain disorders who are unable to travel because of physical limitations. The evaluation and treatment of such disorders requires a whole health approach that individualizes treatment options and delivers care through a biopsychosocial approach. Although circumstances surrounding the need for telerehabilitation use may vary, including lack of reliable transportation to a medical facility, physical limitation precluding transport, or mitigation of person-to-person transmission of an illness, the goals of care are unchanged from an in-person patient–provider experience. Telerehabilitation can be successfully implemented in pain management with appropriate consideration for staging an evaluation, a structured approach to the visit, the use of standard clinical metrics, and the appropriate application of pharmacologic and nonpharmacologic treatments.
Clinics care points
-
•
During the coronavirus disease-2019 pandemic, there have been temporary policy changes for telehealth to allow Health Insurance Portability and Accountability Act flexibility, expansion of covered services, and reimbursement equivalent to in-person visits.
-
•
Telerehabitation for pain management can be offered in conjunction with, or in lieu of, in-person interaction. For example, a hybrid model may include an initial in-person consultation with options for virtual and/or in-person follow up visits.
-
•
Confirm the patient’s location, telephone number, emergency contact, and proximity to others during the initial stages of the visit in case communication becomes compromised or emergency medical services need to be rendered.
-
•
If the patient lacks access to a secure environment, options should be provided to them to ensure their comfort, privacy, and safety.
-
•
Avoid clothing with stripes or patterns because they can cause video distortion.
-
•
When available, a designated individual may accompany the patient to assist with camera operation during the physical examination.
Acknowledgments
Disclosure
The authors have nothing to disclose.
References
- 1.Zelaya C.E., Dahlhamer J.M., Lucas J.W., et al. National Center for Health Statistics; Hyattsville (MD): 2020. Chronic pain and high-impact chronic pain among U.S. adults, 2019. NCHS Data Brief, no 390. [PubMed] [Google Scholar]
- 2.Wallace R., Hughes-Cromwick P., Mull H., et al. Access to health care and nonemergency medical transportation: two missing links. Transportation Res Rec. 2005;1924:76–84. [Google Scholar]
- 3.Strehle E.M., Shabde N. One hundred years of telemedicine: does this new technology have a place in Paediatrics? Arch Dis Child. 2006;91(12):956–959. doi: 10.1136/adc.2006.099622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO . World Health Organization; Geneva: 1998. A health telematics policy in support of WHO’s Health-For-All strategy for global health development: report of the WHO group consultation on health telematics, 11–16 December, Geneva, 1997. [Google Scholar]
- 5.Craig J., Patterson V. Introduction to the practice of telemedicine. J Telemed Telecare. 2005;11(1):3–9. doi: 10.1177/1357633X0501100102. [DOI] [PubMed] [Google Scholar]
- 6.Ryu S. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2) Healthc Inform Res. 2012;18(2):153–155. [Google Scholar]
- 7.Raja S.N., Carr D.B., Cohen M., et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020 doi: 10.1097/j.pain.0000000000001939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDowell I. 3rd edition. Oxford University Press; New York: 2006. Measuring health: a guide to rating scales and questionnaires. [Google Scholar]
- 9.Verduzco-Gutierrez M., Bean A.C., Tenforde A.S., et al. How to Conduct an Outpatient Telemedicine Rehabilitation or Prehabilitation Visit. J Inj Funct Rehabil. 2020;12:714–720. doi: 10.1002/pmrj.12380. [DOI] [PubMed] [Google Scholar]
- 10.Howe C.Q., Sullivan M.D. The missing ‘P’ in pain management: how the current opioid epidemic highlights the need for psychiatric services in chronic pain care. Gen Hosp Psychiatry. 2014;36:99–104. doi: 10.1016/j.genhosppsych.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Cherkin D.C., Sherman K.J., Balderson B.H., et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA. 2016;315(12):1240–1249. doi: 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jensen M.P., Moore M.R., Bockow T.B., et al. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. Arch Phys Med Rehabil. 2011;92(1):146–160. doi: 10.1016/j.apmr.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buys L.M., Wiedenfeld S.A. Osteoarthritis. In: DiPiro JT, Talbert RL, Yee GC, et al. eds Pharmacotherapy: a pathophysiologic approach, 10th edition. McGraw-Hill. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=133893029 Available at: Accessed October 06, 2020.
- 14.Herndon C.M., Strickland J.M., Ray J.B. In: Pharmacotherapy: a pathophysiologic approach. 10th edition. DiPiro J.T., Talbert R.L., Yee G.C., et al., editors. McGraw-Hill; 2020. Pain Management.https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=146063604 Available at: Accessed October 06, 2020. [Google Scholar]
- 15.Dowell D., Haegerich T.M., Chou R. CDC guideline for prescribing opioids for chronic pain — United States, 2016. MMWR Recomm Rep. 2016;65(No. RR-1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Department of Veterans Affairs. VA/DoD clinical practice guideline for opioid therapy for chronic pain. February 2017. Available at: https://www.healthquality.va.gov/guidelines/Pain/cot/VADoDOTCPG022717.pdf#.
- 17.RYAN HAIGHT ONLINE PHARMACY CONSUMER PROTECTION ACT OF 2008. Vol. 154. Congressional Record; 2008. 110th Congress Public Law 425. Available at https://www.congress.gov/bill/110th-congress/house-bill/6353/text.
- 18.COVID-19 Information Page. 2020. Deadiversion.usdoj.govhttps://www.deadiversion.usdoj.gov/coronavirus.html Available at: Accessed October 30, 2020.
- 19.1135 Waivers. cms.gov. 2017. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertEmergPrep/1135-Waivers Available at: Accessed October 4, 2020.
- 20.COVID-19 Information Page. 2020. Deadiversion.usdoj.govhttps://www.deadiversion.usdoj.gov/coronavirus.html Available at: Accessed November 6, 2020.
- 21.Kligler B., Bair M.J., Banerjea R., et al. Clinical policy recommendations from the VHA state-of-the-art conference on non-pharmacological approaches to chronic musculoskeletal pain. J Gen Intern Med. 2018;33(Suppl 1):16–23. doi: 10.1007/s11606-018-4323-z. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5902342/ Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathersul D.C., Mahoney L.A., Bayley P.J. Tele-yoga for chronic pain: current status and future directions. Glob Adv Health Med. 2018;7 doi: 10.1177/2164956118766011. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5888810/ 2164956118766011 Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Day M.A., Thorn B.E., Burns J.W. The continuing evolution of biopsychosocial interventions for chronic pain. J Cogn Psychotherapy. 2012;26(2):114–129. doi: 10.1891/0889-8391.26.2.114%2020https://connect.springerpub.com/content/sgrjcp%203A%203A%203A26%203A%203A%203A2%203A%203A%203A114.full.pdf?implicit-login=true&sigma-token=IFGBw5_6ykj4YFVlxRCRXtkax-NoIGd18uqn0xjlgE4. [DOI] [Google Scholar]
- 24.Murphy JL, McKellar JD, Raffa SD, et al. Cognitive behavioral therapy for chronic pain among veterans: therapist manual. Washington, DC: U.S. Department of Veterans Affairs; 2014.
- 25.Hylands-White N., Duarte R.V., Raphael J.H. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2017;37(1):29–42. doi: 10.1007/s00296-016-3481-8. https://pubmed.ncbi.nlm.nih.gov/27107994/ Available at: [DOI] [PubMed] [Google Scholar]
- 26.Williams A.C., Eccleston C., Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11(11) doi: 10.1002/14651858.CD007407.pub3. https://pubmed.ncbi.nlm.nih.gov/23152245/ CD007407. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heapy A.A., Higgins D.M., Goulet J.L., et al. Interactive voice response-based self-management for chronic back pain: the COPES noninferiority randomized trial. JAMA Intern Med. 2017;177(6):765–773. doi: 10.1001/jamainternmed.2017.0223. https://pubmed.ncbi.nlm.nih.gov/28384682/ Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Graham C.D., Gouick J., Krahé C., et al. A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev. 2016;46:46–58. doi: 10.1016/j.cpr.2016.04.009. https://www.sciencedirect.com/science/article/pii/S0272735815301124?via%3Dihub Available at: [DOI] [PubMed] [Google Scholar]
- 29.Hughes L.S., Clark J., Colclough J.A., et al. Acceptance and commitment therapy (ACT) for chronic pain: a systematic review and meta-analyses. Clin J Pain. 2017;33(6):552–568. doi: 10.1097/AJP.0000000000000425. https://pubmed.ncbi.nlm.nih.gov/27479642/ Available at: [DOI] [PubMed] [Google Scholar]
- 30.Herbert M.S., Afari N., Liu L., et al. Telehealth versus in-person acceptance and commitment therapy for chronic pain: a randomized noninferiority trial. J Pain. 2017;18(2):200–211. doi: 10.1016/j.jpain.2016.10.014. https://pubmed.ncbi.nlm.nih.gov/27838498/ Available at: [DOI] [PubMed] [Google Scholar]
- 31.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3. https://pubmed.ncbi.nlm.nih.gov/7042457/ Available at: [DOI] [PubMed] [Google Scholar]
- 32.Hilton L., Hempel S., Ewing B.A., et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199–213. doi: 10.1007/s12160-016-9844-2. https://pubmed.ncbi.nlm.nih.gov/27658913/ Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chiesa A., Serretti A. Mindfulness-based interventions for chronic pain: a systematic review of the evidence. J Altern Complement Med. 2011;17(1):83–93. doi: 10.1089/acm.2009.0546. https://pubmed.ncbi.nlm.nih.gov/21265650/ Available at: [DOI] [PubMed] [Google Scholar]
- 34.Gardner-Nix J., Barbati J., Grummitt J., et al. Exploring the effectiveness of a mindfulness-based chronic pain management course delivered simultaneously to on-site and off-site patients using telemedicine. Mindfulness. 2014;5:223–231. https://link.springer.com/article/10.1007/s12671-012-0169-3#citeas Available at: [Google Scholar]
- 35.Geneen L.J., Moore R.A., Clarke C., et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4(4) doi: 10.1002/14651858.CD011279.pub3. https://pubmed.ncbi.nlm.nih.gov/28436583/ CD011279. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adamse C., Dekker-Van Weering M.G., van Etten-Jamaludin F.S., et al. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. J Telemed Telecare. 2018;24(8):511–526. doi: 10.1177/1357633X17716576. https://pubmed.ncbi.nlm.nih.gov/28696152/ Available at: [DOI] [PubMed] [Google Scholar]