Abstract
An estimated one-third of US adults use herbal supplements, often without reporting that use to their physicians. These supplements can potentially alter bleeding and coagulation during surgery and when used concomitantly with anticoagulants. Our objective was to provide a comprehensive review of the evidence of bleeding risks of the most popular herbal and dietary supplements. A PubMed search and review of the literature was performed. We found that garlic and hawthorn supplementation is strongly associated with surgical bleeding independent of anticoagulants. Cordyceps sinensis, echinacea, and aloe vera are loosely associated with surgical bleeding independent of anticoagulants. In patients on anticoagulants, ginkgo biloba, chondroitin-glucosamine, melatonin, turmeric, bilberry, chamomile, fenugreek, milk thistle, and peppermint are associated with bleeding risk. No evidence was found for bleeding with these supplements independent of anticoagulants. Fish oil, ginseng, and saw palmetto are not associated with bleeding. Evidence for overall bleeding risk associated with St. John’s wort, ginger, ginkgo biloba, or cranberry supplementation is conflicting. In conclusion, physicians must be aware of the potential anticoagulant effects of these supplements. It is imperative to report dietary and herbal supplement usage to physicians and is best to discontinue nonessential supplement use 2 weeks prior to surgery.
Keywords: Anticoagulants, bleeding, dietary supplements, herbal supplements, surgical bleeding
CME
Target audience: All physicians.
Learning objectives: After completing the article, the learner should be able to
1. Review with the patient a current list of herbal supplements the patient may not have disclosed, especially before procedures and when patients are on anticoagulants.
2. Differentiate between those dietary supplements for which there is high-level evidence of a bleeding risk and those supplements that should be approached with caution due to lack of substantial literature.
Faculty credentials/disclosure: Jess Hatfield is a medical student at Texas A&M University College of Medicine in Temple, Texas. Saadeddine Saad, MD, is a practicing dermatologist in Temple, Texas. Chad Housewright, MD, is director of dermatologic surgery at Baylor Scott & White Medical Center in Temple, Texas. The authors and planner for this educational activity have no relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, re-selling, or distributing health care products used by or on patients.
Accreditation: The A. Webb Roberts Center for Continuing Medical Education is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
Designation: The A. Webb Roberts Center for Continuing Medical Education of Baylor Scott & White Health designates this journal CME activity for a maximum of 1.0 AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
ABIM MOC: The successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
The A. Webb Roberts Center for Continuing Medical Education of Baylor Scott & White Health will submit participant completion information to the ACCME, which will be transferred to the ABIM for MOC credits claimed. By entering your ABIM Diplomate number into your profile and completing the credit claim process for this activity, you are giving permission for the transfer of your information to take place.
Process: To complete this CME activity, read the entire article and then go to https://ce.bswhealth.com/Proceedings2020. You will register for the course, pay any relevant fee, take the quiz, complete the evaluation, and claim your CME credit. For more information about CME credit, email ce@bswhealth.org.
Expiration date: November 1, 2024.
In practice, physicians must anticipate the bleeding potential of patients who are on anticoagulants. In addition, proceduralists must anticipate bleeding potential of patients to properly obtain intraoperative hemostasis and to reduce postoperative bleeding complications. Physicians are aware of when their patients are on medications that alter platelet function, which are often continued through procedures to minimize adverse cardiovascular events.1 However, the literature is less clear on the topic of dietary and herbal supplements with regard to bleeding risk. Approximately 33% of adults in the United States use herbal supplements.2 Supplements are generally considered safe, but they are not regulated as strictly as pharmaceuticals and can also lead to adverse outcomes.3 Thus, in this review, we sought to gather data on the most current popular dietary supplements and the effects they may have on bleeding.
METHODS
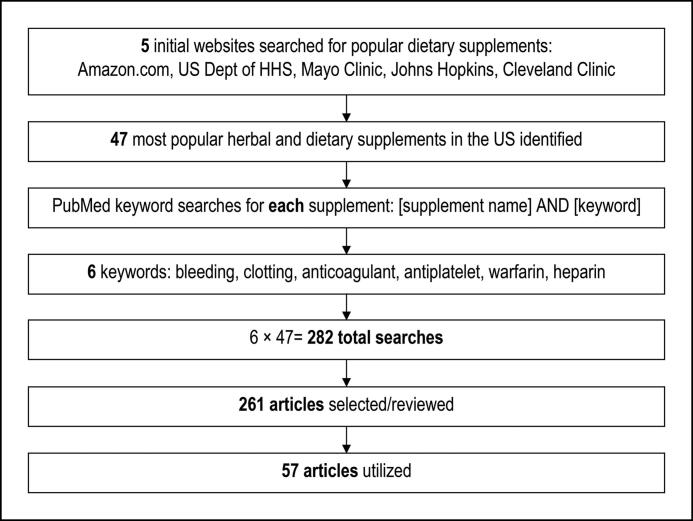
The search strategy is outlined in Figure 1. Forty-seven of the most popular herbal and dietary supplements in the United States were identified using five sources: the top 50 best-selling “herbal supplements” on Amazon.com, the US Department of Health and Human Services website,4 and the Mayo Clinic, Johns Hopkins, and Cleveland Clinic websites. Multiple vitamins and minerals were excluded to isolate specific supplements.
Figure 1.
Search strategy.
Next, a search of PubMed was conducted using the following search terms: “[supplement] AND (“bleeding” OR “clotting” OR “anticoagulant” OR “antiplatelet” OR “warfarin” OR “heparin”). All articles that these searches yielded were reviewed by title or abstract. Reference lists of relevant articles were also examined. Using these search strategies, a total of 261 articles were selected and reviewed: 63 randomized controlled trials (RCTs), 3 cohort studies, 1 case crossover study, 2 chart or database analyses, 82 case series or case reports, and 110 bench research studies. Ratings of 1 to 5 from the Center for Evidence-Based Medicine were initially used to rate each article.5 Of these 261 articles, the 57 most clinically relevant were chosen for direct reference in this review.6–63
FINDINGS
The 47 individual supplements in this results section are divided into nine categories (Table 1) and are reviewed in that order.
Table 1.
Categorization of the 47 identified supplements based on their association with bleeding outcomes and level of evidence to support the association
| Category | Supplements included |
|---|---|
| Surgical bleeding (5) | Garlic; hawthorn; Cordyceps sinensis; echinacea; aloe vera |
| Anticoagulant-related bleeding (11) | Ginkgo biloba; chondroitin-glucosamine; melatonin; turmeric; bilberry; chamomile; fenugreek; milk thistle; peppermint; cinnamon; ginger |
| Platelet aggregation affected in humans (3) | Melatonin; flaxseed; grape seed extract |
| No effect on platelet aggregation (3) | Fenugreek; turmeric; spirulina |
| Bench research supporting bleeding potential (8) | Ashwagandha; black pepper; dandelion; evening primrose; feverfew; honey; lavender; lion’s mane |
| No clinical association with bleeding (3) | Fish oil; ginseng; saw palmetto |
| Unclear evidence (4) | St. John’s wort; ginger; ginkgo biloba; cranberry |
| Procoagulant properties (8) | Black cohosh; chlorella vulgaris; green tea; menthol; propolis; red yeast rice; honey; isoflavones |
| No evidence (8) | Acidophilus; apple cider vinegar; beet; elderberry; goldenseal; horny goat weed; tea tree oil; valerian |
There is convincing evidence associating garlic supplementation and hawthorn supplementation with surgical bleeding (Table 2). Garlic has been associated with surgical bleeding in many case reports,6,7 and multiple RCTs show that garlic decreases platelet aggregation. A recent systematic review concluded that, based on the aggregated evidence, garlic does predispose to surgical bleeding.8 Hawthorn extract consumption has been shown in a cohort study to increase the risk of bleeding during cardiac surgery.9
Table 2.
Supplements associated with surgical bleeding (independent of anticoagulants)
| Supplement | Highest-level evidence |
|---|---|
| Garlic | Review of RCTs |
| Hawthorn | Cohort study |
| Cordyceps sinensis, echinacea, aloe vera | One case report |
RCT indicates randomized controlled trials.
Cordyceps sinensis, echinacea, and aloe vera are loosely associated with surgical bleeding (Table 2). A 2018 case report described excessive surgical bleeding in a patient using Cordyceps sinensis daily as a tonic.10 Another case report described surgical bleeding associated with echinacea,11 but an RCT showed no increase in bleeding or international normalized ratio (INR) increase associated with echinacea.12 Finally, aloe vera was associated with surgical bleeding in a case report, in which a patient consuming excess aloe vera had an adverse bleeding reaction with sevoflurane.13
There is convincing evidence associating ginkgo biloba supplementation and chondroitin-glucosamine supplementation with bleeding in patients on warfarin (Table 3). A large chart review (n = 807,399) revealed that taking ginkgo biloba with warfarin is associated with increased risk for major bleeding events compared to warfarin alone.14 In addition, two case reports described chondroitin-glucosamine use associated with an increased INR in patients on warfarin.15,16 As of 2011, over 40 cases of glucosamine-warfarin interactions had been reported by various drug-monitoring agencies.17
Table 3.
Supplements associated with anticoagulant-related bleeding, with no evidence for bleeding independent of anticoagulants
| Supplement | Highest-level evidence |
|---|---|
| Ginkgo biloba | Large-scale chart review |
| Chondroitin-glucosamine | Case series, government reporting bodies |
| Melatonin | Six case reports |
| Turmeric | Two case reports |
| Bilberry, chamomile, fenugreek, milk thistle, peppermint, cinnamon, ginger | One case report |
While there is no higher level evidence available, case reports have associated melatonin,18 turmeric,19,20 bilberry,21 chamomile,22 fenugreek,23 milk thistle,24 and peppermint25 with increased INR or bleeding in patients on warfarin (Table 3). Another case report described fatal gastrointestinal bleeding in a patient taking dabigatran along with cinnamon and ginger.26
Many supplements are notable due to their effect on platelet aggregation in humans. Melatonin, flaxseed, and grape seed extract affect platelet aggregation activity and/or blood coagulation activity in humans in RCTs.27 RCTs have additionally shown that flaxseed oil decreases platelet aggregation,28 and grape seed extract increases platelet closure time in humans.29
Conversely, some supplements that are clinically linked to bleeding through low-level evidence show no effect on platelet aggregation in humans. Previously described case studies associated fenugreek and turmeric with increased INR in patients on warfarin.19,20,23 However, RCTs showed that fenugreek does not affect platelet aggregation,30 and turmeric does not increase platelet inhibition, prothrombin time/activated partial thromboplastin time, or thrombin generation in humans.31 Additionally, subjective observations by those in an RCT treating patients with spirulina included multiple reports of bleeding, but the same RCT reported that thrombin clotting time and activated partial thromboplastin time were not changed.32
Some supplements showed anticoagulant or antiplatelet properties through level 5 evidence (bench research), but we could find no clinical evidence for or against bleeding in these supplements. These supplements include ashwagandha,33 black pepper,34 dandelion,35 evening primrose,36 feverfew,36 honey,37 lavender,38 and lion’s mane.39
Fish oil, ginseng, and saw palmetto were thought to be associated with bleeding, by bench research or low-level clinical evidence, but have since been shown in RCTs to have no association with bleeding. There are many case reports of fish oil associated with bleeding, and multiple RCTs have shown that fish oil has antiplatelet effects40; however, multiple RCTs have shown that these antiplatelet effects do not translate to increased bleeding.40 Additionally, a retrospective cohort study of 573 patients showed no interaction between fish oil and warfarin.41 Finally, a large RCT involving 25,871 participants showed no excess risks of bleeding associated with fish oil.42 As with fish oil, there are many case reports of the various types of ginseng associated with bleeding events and procoagulation events.7,43–45 However, RCTs have shown that ginseng does not affect31 or decreases46 warfarin’s anticoagulant effect, and a case-crossover study showed no association between ginseng and bleeding.47 Similarly to fish oil and ginseng, many case reports have also associated saw palmetto with increased bleeding6; however, two RCTs showed that saw palmetto does not increase perioperative bleeding in prostate resection surgery.48,49
St. John’s wort, ginger, ginkgo biloba, and cranberry are all heavily studied supplements, but the literature is unclear on their effect on bleeding. One RCT showed St. John’s wort to have the procoagulant effect of increasing warfarin clearance.50 In contrast, a World Health Organization database analysis showed a positive correlation between St. John’s wort and hemorrhage events.51 There are many case reports of ginger associated with bleeding, often due to interaction with anticoagulants.6,44,45 Four RCTs reported that ginger reduces platelet aggregation, while four RCTs reported no effect of ginger on platelet aggregation.52 Similar to ginger, there are many case reports of ginkgo biloba associated with bleeding—mostly cerebral or orbital bleeding.44,45 Despite these reports, a systematic review and meta-analysis including 18 RCTs found no bleeding risk associated with ginkgo biloba.53 Interestingly, as previously discussed, ginkgo biloba did increase bleeding in patients on warfarin in a large chart review.14 Finally, there are many case reports of cranberry-related bleeding, typically with patients on warfarin.6,36,44,45 An RCT of 12 participants showed that cranberry capsules coadministered with warfarin significantly increased INR, but did not cause major bleeding.12 In contrast, three RCTs concluded that there is no significant interaction between cranberry juice and warfarin at 240 to 480 mL per day.54–56
Many of the supplements investigated have a procoagulant effect, at varying levels of evidence. These include black cohosh,57 chlorella vulgaris,58 green tea,59 menthol,44 propolis,60 red yeast rice,61 honey,62 and isoflavones.45
The remaining supplements investigated had no evidence associating them with bleeding: acidophilus, apple cider vinegar, beet, elderberry, goldenseal, horny goat weed, tea tree oil, and valerian.
DISCUSSION
This review outlines a list of popular supplements that may be associated with bleeding, corroborated by varying levels of evidence. These supplements alter bleeding through (1) direct antiplatelet or anticoagulant effects, and/or (2) interaction with anticoagulant drugs, often through cytochrome P450 enzymes. Notably, warfarin is metabolized by cytochrome P450 enzymes; supplements that alter these enzymes often affect the coagulation status of patients on warfarin.6
It is imperative that physicians have a current list of their patients’ herbal supplements, especially before surgery and when patients are on drugs that affect coagulation. Though an estimated one-third of adults take herbal supplements,2 many patients do not report supplements they are taking to their physicians.3 In fact, a 2002 survey showed that while 4.8% (131/2723) of patients presenting for surgery were taking herbal supplements, only two of these instances were recorded in their charts.63 Due to the potential for adverse events, it is our conclusion that surgeons should encourage discontinuation of dietary supplements 2 weeks before surgery. This has been encouraged unless otherwise indicated on a case-by-case basis.64
While some supplements have clear contraindications, the evidence associating many of the supplements discussed in this review with bleeding is sparse or conflicting. For clinical ease, we have summarized relative bleeding risk of all the supplements discussed in Table 4. Due to high-level evidence, garlic and hawthorn should be discontinued prior to surgery. Additionally, there is strong evidence that ginkgo biloba and chondroitin-glucosamine should not be coadministered with warfarin. Many of the other supplements discussed have associations with bleeding in the form of case studies, platelet aggregation studies, and bench research and should be discontinued prior to surgery. However, low-level evidence can be misleading; it was previously thought that fish oil should be discontinued prior to surgery, but level 1 prospective studies have now shown it can be continued.64 Additionally, a limitation of our review is that much of the data is from specific surgical and medical fields and may not be directly applicable to all fields. Thus, larger prospective randomized trials and large-scale chart reviews will assist in guiding further recommendations for many of these supplements.
Table 4.
Approximation of overall bleeding risk for each supplement, based on the highest level of evidence for each
| Bleeding risk* | Supplement |
|---|---|
| High (4) | Garlic; hawthorn; ginkgo biloba; chondroitin-glucosamine |
| Moderate (25) |
|
| Low (15) |
|
| None (3) | Fish oil; ginseng; saw palmetto |
Inclusion in the “high risk” group is supported by high-level evidence in the clinical setting: systematic reviews, cohort studies, randomized controlled trials, and large case series. Supplements in the “moderate risk” group are supported by case reports (a, b), platelet aggregation studies (c), basic science research (d), or unclear/conflicting evidence (e). Supplements in the “low risk” group have no reported bleeding risk in the literature (a) or procoagulant properties (b). Supplements in the “no risk” group have strong evidence that suggests no clinical association with bleeding. The data include both surgical bleeding and anticoagulant-related bleeding risk.
References
- 1.Kirkorian AY, Moore BL, Siskind J, Marmur ES.. Perioperative management of anticoagulant therapy during cutaneous surgery: 2005 survey of Mohs surgeons. Dermatol Surg. 2007;33(10):1189–1197. doi: 10.1111/j.1524-4725.2007.33253.x. [DOI] [PubMed] [Google Scholar]
- 2.Rashrash M, Schommer JC, Brown LM.. Prevalence and predictors of herbal medicine use among adults in the United States. J Patient Exp. 2017;4(3):108–113. doi: 10.1177/2374373517706612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ronis MJJ, Pedersen KB, Watt J.. Adverse effects of nutraceuticals and dietary supplements. Annu Rev Pharmacol Toxicol. 2018;58:583–601. doi: 10.1146/annurev-pharmtox-010617-052844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnes PM, Bloom B, Nahin RL.. Complementary and alternative medicine use among adults and children: United States. Natl Health Stat Rep. 2007;2008(12):1–23. [PubMed] [Google Scholar]
- 5.Burns PB, Rohrich RJ, Chung KC.. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128(1):305–310. doi: 10.1097/PRS.0b013e318219c171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ge B, Zhang Z, Zuo Z.. Updates on the clinical evidenced herb-warfarin interactions. Evid Based Complement Alternat Med. 2014;2014:957362. doi: 10.1155/2014/957362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong WW, Gabriel A, Maxwell GP, Gupta SC.. Bleeding risks of herbal, homeopathic, and dietary supplements: a hidden nightmare for plastic surgeons? Aesthet Surg J. 2012;32(3):332–346. doi: 10.1177/1090820X12438913. [DOI] [PubMed] [Google Scholar]
- 8.Malhotra U, Hasday M, Romanos GE, Javed F.. Assessment of routine diet (garlic consumption) as a pre- and postoperative protocol in oral and maxillofacial surgical interventions: an evidence-based literature review. Nutr Health. 2020;26(2):135–139. doi: 10.1177/0260106020912940. [DOI] [PubMed] [Google Scholar]
- 9.Rababa’h AM, Altarabsheh SE, Haddad O, Deo SV, Obeidat Y, Al-Azzam S.. Hawthorn herb increases the risk of bleeding after cardiac surgery: an evidence-based approach. Heart Surg Forum. 2016;19(4):E175–179. doi: 10.1532/hsf.1570. [DOI] [PubMed] [Google Scholar]
- 10.Hatton MN, Desai K, Le D, Vu A.. Excessive postextraction bleeding associated with Cordyceps sinensis: a case report and review of select traditional medicines used by Vietnamese people living in the United States. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;126(6):494–500. doi: 10.1016/j.oooo.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Ananthanarayan C, Urbach G.. Herbals—beware bleeding. Can J Anaesth. 2000;47(10):1046. doi: 10.1007/BF03024882. [DOI] [PubMed] [Google Scholar]
- 12.Abdul MIM, Jiang X, Williams KM, et al. Pharmacokinetic and pharmacodynamic interactions of Echinacea and policosanol with warfarin in healthy subjects. Br J Clin Pharmacol. 2010;69(5):508–515. doi: 10.1111/j.1365-2125.2010.03620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee A, Chui PT, Aun CS, Gin T, Lau AS.. Possible interaction between sevoflurane and aloe vera. Ann Pharmacother. 2004;38(10):1651–1654. doi: 10.1345/aph.1E098. [DOI] [PubMed] [Google Scholar]
- 14.Stoddard GJ, Archer M, Shane-McWhorter L, et al. Ginkgo and warfarin interaction in a large Veterans Administration population. AMIA Annu Symp Proc. 2015;2015:1174–1183. [PMC free article] [PubMed] [Google Scholar]
- 15.Knudsen JF, Sokol GH.. Potential glucosamine-warfarin interaction resulting in increased international normalized ratio: case report and review of the literature and MedWatch database. Pharmacotherapy. 2008;28(4):540–548. doi: 10.1592/phco.28.4.540. [DOI] [PubMed] [Google Scholar]
- 16.Rozenfeld V, Crain JL, Callahan AK.. Possible augmentation of warfarin effect by glucosamine-chondroitin. Am J Health Syst Pharm. 2004;61(3):306–307. doi: 10.1093/ajhp/61.3.306. [DOI] [PubMed] [Google Scholar]
- 17.EFSA Panel on Dietetic Products Nutrition and Allergies . Statement on the safety of glucosamine for patients receiving coumarin anticoagulants. EFSA J. 2011;9(12):2473. [Google Scholar]
- 18.Herxheimer A, Petrie KJ.. Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev. 2002;2:CD001520. doi: 10.1002/14651858.CD001520. [DOI] [PubMed] [Google Scholar]
- 19.Medsafe . Monitoring Communication: Beware Tumeric/Curcumin Containing Product Can Interact with Warfarin. New Zealand Medicines and Medical Devices Safety Authority; 2018. https://medsafe.govt.nz/safety/EWS/2018/Turmeric.asp. [Google Scholar]
- 20.Daveluy A, Géniaux H, Thibaud L, Mallaret M, Miremont-Salamé G, Haramburu F.. Probable interaction between an oral vitamin K antagonist and turmeric (Curcuma longa). Therapie. 2014;69(6):519–520. doi: 10.2515/therapie/2014062. [DOI] [PubMed] [Google Scholar]
- 21.Aktas C, Senkal V, Sarikaya S, Karti S.. Bilberry potentiates warfarin effect? Turkish J Geriatr. 2011;14(1):79–81. [Google Scholar]
- 22.Segal R, Pilote L.. Warfarin interaction with matricaria chamomilla. CMAJ. 2006;174(9):1281–1282. doi: 10.1503/cmaj.051191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambert JP, Cormier J.. Potential interaction between warfarin and boldo-fenugreek. Pharmacotherapy. 2001;21(4):509–512. doi: 10.1592/phco.21.5.509.34492. [DOI] [PubMed] [Google Scholar]
- 24.Lash DB, Ward S.. CYP2C9-mediated warfarin and milk thistle interaction. J Clin Pharm Ther. 2020;45(2):368–369. doi: 10.1111/jcpt.13064. [DOI] [PubMed] [Google Scholar]
- 25.Moeinipour A, Abbassi Teshnizi M, Manafi B, Yavari H, Moeinipour Y, Hoseinikhah H.. Possible interaction of warfarin with peppermint herbal tea: a case report. Rev Clin Med. 2017;4(2):83–86. [Google Scholar]
- 26.Maadarani O, Bitar Z, Mohsen M.. Adding herbal products to direct-acting oral anticoagulants can be fatal. Eur J Case Rep Intern Med. 2019;6(8):001190. doi: 10.12890/2019_001190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wirtz PH, Spillmann M, Bartschi C, Ehlert U, von Kanel R.. Oral melatonin reduces blood coagulation activity: a placebo-controlled study in healthy young men. J Pineal Res. 2008;44(2):127–133. doi: 10.1111/j.1600-079X.2007.00499.x. [DOI] [PubMed] [Google Scholar]
- 28.Allman MA, Pena MM, Pang D.. Supplementation with flaxseed oil versus sunflower seed oil in healthy young men consuming a low fat diet: effects on platelet composition and function. Eur J Clin Nutr. 1995;49(3):169–178. [PubMed] [Google Scholar]
- 29.Shenoy SF, Keen CL, Kalgaonkar S, Polagruto JA.. Effects of grape seed extract consumption on platelet function in postmenopausal women. Thromb Res. 2007;121(3):431–432. doi: 10.1016/j.thromres.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 30.Bordia A, Verma SK, Srivastava KC.. Effect of ginger (Zingiber officinale Rosc.) and fenugreek (Trigonella foenumgraecum L.) on blood lipids, blood sugar and platelet aggregation in patients with coronary artery disease. Prostaglandins Leukot Essent Fatty Acids. 1997;56(5):379–384. doi: 10.1016/s0952-3278(97)90587-1. [DOI] [PubMed] [Google Scholar]
- 31.Fung FY, Wong WH, Ang SK, et al. A randomized, double-blind, placebo-controlled study on the anti-haemostatic effects of curcuma longa, angelica sinensis and Panax ginseng. Phytomedicine. 2017;32:88–96. doi: 10.1016/j.phymed.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 32.Jensen GS, Drapeau C, Lenninger M, Benson KF.. Clinical safety of a high dose of phycocyanin-enriched aqueous extract from Arthrospira (spirulina) platensis: results from a randomized, double-blind, placebo-controlled study with a focus on anticoagulant activity and platelet activation. J Med Food. 2016;19(7):645–653. doi: 10.1089/jmf.2015.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ku SK, Bae JS.. Antiplatelet, anticoagulant, and profibrinolytic activities of withaferin A. Vascul Pharmacol. 2014;60(3):120–126. doi: 10.1016/j.vph.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 34.Park BS, Son DJ, Park YH, Kim TW, Lee SE.. Antiplatelet effects of acidamides isolated from the fruits of Piper longum l. Phytomedicine. 2007;14(12):853–855. doi: 10.1016/j.phymed.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 35.Chua YT, Ang XL, Zhong XM, Khoo KS.. Interaction between warfarin and Chinese herbal medicines. Singapore Med J. 2015;56(1):11–18. doi: 10.11622/smedj.2015004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abebe W. Review of herbal medications with the potential to cause bleeding: dental implications, and risk prediction and prevention avenues. EPMA J. 2019;10(1):51–64. doi: 10.1007/s13167-018-0158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martina SJ, Ramar LAP, Silaban MRI, Luthfi M, Govindan PAP.. Antiplatelet effectivity between aspirin with honey on cardiovascular disease based on bleeding time taken on mice. Open Access Maced J Med Sci. 2019;7(20):3416–3420. doi: 10.3889/oamjms.2019.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ballabeni V, Tognolini M, Chiavarini M, et al. Novel antiplatelet and antithrombotic activities of essential oil from Lavandula hybrida Reverchon “grosso”. Phytomedicine. 2004;11(7-8):596–601. doi: 10.1016/j.phymed.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 39.Poniedziałek B, Siwulski M, Wiater A, et al. The effect of mushroom extracts on human platelet and blood coagulation: in vitro screening of eight edible species. Nutrients. 2019;11(12):3040. doi: 10.3390/nu11123040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Begtrup KM, Krag AE, Hvas AM.. No impact of fish oil supplements on bleeding risk: a systematic review. Dan Med J. 2017;64(5):A5366. [PubMed] [Google Scholar]
- 41.Pryce R, Bernaitis N, Davey AK, Badrick T, Anoopkumar-Dukie S.. The use of fish oil with warfarin does not significantly affect either the international normalised ratio or incidence of adverse events in patients with atrial fibrillation and deep vein thrombosis: a retrospective study. Nutrients. 2016;8(9):578. doi: 10.3390/nu8090578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manson JE, Cook NR, Lee IM, et al. Marine n-3 fatty acids and prevention of cardiovascular disease and cancer. N Engl J Med. 2019;380(1):23–32. doi: 10.1056/NEJMoa1811403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abebe W. Herbal medication: potential for adverse interactions with analgesic drugs. J Clin Pharm Ther. 2002;27(6):391–401. doi: 10.1046/j.1365-2710.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- 44.Tan CSS, Lee SWH.. Warfarin and food, herbal or dietary supplement interactions: a systematic review. Br J Clin Pharmacol. 2021;87(2):352–374. doi: 10.1111/bcp.14404. [DOI] [PubMed] [Google Scholar]
- 45.Nutescu EA, Shapiro NL, Ibrahim S, West P.. Warfarin and its interactions with foods, herbs and other dietary supplements. Expert Opin Drug Saf. 2006;5(3):433–451. doi: 10.1517/14740338.5.3.433. [DOI] [PubMed] [Google Scholar]
- 46.Yuan CS, Wei G, Dey L, et al. Brief communication: American ginseng reduces warfarin’s effect in healthy patients: a randomized, controlled trial. Ann Intern Med. 2004;141(1):23–27. doi: 10.7326/0003-4819-141-1-200407060-00011. [DOI] [PubMed] [Google Scholar]
- 47.Tsai HH, Lin HW, Tsai CL, Yam FK, Lin SS.. Uncertain associations of major bleeding and concurrent use of antiplatelet agents and Chinese medications: a nested case-crossover study. Evid Based Complement Alternat Med. 2017;2017:9417186. doi: 10.1155/2017/9417186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tuncel A, Ener K, Han O, et al. Effects of short-term dutasteride and Serenoa repens on perioperative bleeding and microvessel density in patients undergoing transurethral resection of the prostate. Scand J Urol Nephrol. 2009;43(5):377–382. doi: 10.3109/00365590903164498. [DOI] [PubMed] [Google Scholar]
- 49.Pecoraro S, Annecchiarico A, Gambardella MC, Sepe G.. Efficacy of pretreatment with serenoa repens on bleeding associated with transurethral resection of prostate. Minerva Urol Nefrol. 2004;56(1):73–78. [PubMed] [Google Scholar]
- 50.Jiang X, Williams KM, Liauw WS, et al. Effect of St John’s wort and ginseng on the pharmacokinetics and pharmacodynamics of warfarin in healthy subjects. Br J Clin Pharmacol. 2004;57(5):592–599. doi: 10.1111/j.1365-2125.2003.02051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gahr M, Zeiss R, Lang D, et al. Risk of bleeding related to selective and non-selective serotonergic antidepressants: a case/non-case approach using data from two pharmacovigilance databases. Pharmacopsychiatry. 2015;48(1):19–24. [DOI] [PubMed] [Google Scholar]
- 52.Marx W, McKavanagh D, McCarthy AL, et al. The effect of ginger (Zingiber officinale) on platelet aggregation: a systematic literature review. PLoS One. 2015;10(10):e0141119. doi: 10.1371/journal.pone.0141119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kellermann AJ, Kloft C.. Is there a risk of bleeding associated with standardized ginkgo biloba extract therapy? A systematic review and meta-analysis. Pharmacotherapy. 2011;31(5):490–502. doi: 10.1592/phco.31.5.490. [DOI] [PubMed] [Google Scholar]
- 54.Mellen CK, Ford M, Rindone JP.. Effect of high-dose cranberry juice on the pharmacodynamics of warfarin in patients. Br J Clin Pharmacol. 2010;70(1):139–142. doi: 10.1111/j.1365-2125.2010.03674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li Z, Seeram NP, Carpenter CL, Thames G, Minutti C, Bowerman S.. Cranberry does not affect prothrombin time in male subjects on warfarin. J Am Diet Assoc. 2006;106(12):2057–2061. doi: 10.1016/j.jada.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 56.Ansell J, McDonough M, Zhao Y, Harmatz JS, Greenblatt DJ.. The absence of an interaction between warfarin and cranberry juice: a randomized, double-blind trial. J Clin Pharmacol. 2009;49(7):824–830. doi: 10.1177/0091270009337510. [DOI] [PubMed] [Google Scholar]
- 57.Zimmermann R, Witte A, Voll RE, Strobel J, Frieser M.. Coagulation activation and fluid retention associated with the use of black cohosh: a case study. Climacteric. 2010;13(2):187–191. doi: 10.3109/13697130902939921. [DOI] [PubMed] [Google Scholar]
- 58.Ohkawa S, Yoneda Y, Ohsumi Y, Tabuchi M.. Warfarin therapy and chlorella. Rinsho Shinkeigaku. 1995;35(7):806–807. [PubMed] [Google Scholar]
- 59.Soltani R, Haghighat A, Fanaei M, Asghari G.. Evaluation of the effect of green tea extract on the prevention of gingival bleeding after posterior mandibular teeth extraction: a randomized controlled trial. Evid Based Complement Alternat Med. 2014;2014:857651. doi: 10.1155/2014/857651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moon JH, Lee MY, Chung YJ, Rhee CK, Lee SJ.. Effect of topical propolis on wound healing process after tonsillectomy: randomized controlled study. Clin Exp Otorhinolaryngol. 2018;11(2):146–150. doi: 10.21053/ceo.2017.00647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen TL, Yeh CC, Lin CS, Shih CC, Liao CC.. Effects of red yeast rice prescription (LipoCol Forte) on adverse outcomes of surgery. QJM. 2019;112(4):253–259. doi: 10.1093/qjmed/hcy278. [DOI] [PubMed] [Google Scholar]
- 62.Geißler K, Schulze M, Inhestern J, Meißner W, Guntinas-Lichius O.. The effect of adjuvant oral application of honey in the management of postoperative pain after tonsillectomy in adults: a pilot study. PLoS One. 2020;15(2):e0228481. doi: 10.1371/journal.pone.0228481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Skinner CM, Rangasami J.. Preoperative use of herbal medicines: a patient survey. Br J Anaesth. 2002;89(5):792–795. doi: 10.1093/bja/89.5.792. [DOI] [PubMed] [Google Scholar]
- 64.Cummings KC, Keshock M, Ganesh R, et al. Preoperative management of surgical patients using dietary supplements: Society for Perioperative Assessment and Quality Improvement (SPAQI) consensus statement. Mayo Clin Proc. 2021;96(5):1342–1355. doi: 10.1016/j.mayocp.2020.08.016. [DOI] [PubMed] [Google Scholar]