Abstract
Background:
We sought to examine the effectiveness of the Enhancing the Quality of Prescribing Practices for Older Adults Discharged from the Emergency Department (EQUiPPED) medication safety program in three emergency departments (EDs) within the largest health system in Rhode Island (RI) with funding through a quality incentive payment by a private insurance partner.
Methods:
This study utilized a quasi-experimental interrupted time series design to implement EQUiPPED, a three-prong intervention aimed at reducing potentially inappropriate medication (PIM) prescriptions to 5% or less per month. We included clinicians who prescribed medications to older ED patients during the pre- and post-intervention periods from July 2018 to January 2021. We determined the monthly rate of PIM prescribing among older adults discharged from the ED, according to the American Geriatrics Society Beers Criteria, using Poisson regression.
Results
247 ED clinicians (48% attendings (n=119), 27% residents (n=67), 25% advanced practice providers (n=61)) were included in EQUiPPED, of which 92% prescribed a PIM during the study period. In the pre-implementation period (July 2018 – July 2019) the average monthly rate of PIM prescribing was 9.30% (95% CI: 8.82%, 9.78%). In the post-implementation period (October 2019 – January 2021) the PIM prescribing rate decreased significantly to 8.62% (95% CI: 8.14%, 9.10%, p <0.01). During pre-implementation, 1,325 of the 14,193 prescribed medications were considered inappropriate, while only 1,108 of the 13,213 prescribed medications in post-implementation were considered inappropriate. The greatest reduction was observed among antihistamines, skeletal muscle relaxants, and benzodiazepines.
Conclusions:
EQUiPPED contributed to a modest improvement in PIM prescribing to older adults amongst clinicians in these RI EDs even in the midst of the COVID-19 pandemic. The quality incentive funding model demonstrates a successful strategy for implementation and, with greater replication, could shape national policy regarding health care delivery and quality of care for older adults.
Keywords: Emergency department, older adults, inappropriate medications, polypharmacy
INTRODUCTION
Polypharmacy, or regular use of at least five medications,1 is a growing concern among the older adult population, which is projected to nearly double by 2060 in the United States (US).2 Specifically, four in ten older adults ages 65 and older in the US take more than five medications and two in ten take more than ten medications, making excessive medication use among this population a nationwide problem.3 Older adults who have polypharmacy are at increased risk for adverse drug events,4–6 which cost an estimated $3.8 billion each year to payors,3, 4, 7 primarily Medicare. While older adults often have multiple comorbidities justifying the need for complex pharmaceutical regiments, 34% of these patients are prescribed potentially inappropriate medications (PIM).8 Deprescribing, or stopping medications, is a potential solution and a complementary approach. However, an alternative approach, which we focus on in this study, is to avoid starting medications that are potentially harmful.
Approximately 40% of older Americans receive a prescription upon emergency department (ED) discharge,9 and even a short course of a PIM increases the risk of adverse drug events,10 including delirium, falls, and organ dysfunction. Adverse drug events can be associated with ED recidivism, hospitalization, and death.11–13 The Enhancing the Quality of Prescribing Practices for Older Adults Discharged from the Emergency Department (EQUiPPED) intervention14–18 which uses a three-prong approach – geriatric education, academic detailing, and electronic health record (EHR) clinical decision support – to assist prescribers in choosing safer medications for older adults, is an evidence-based approach to addressing this problem. Although this quality initiative has already been successful in multiple academic and Veterans Affairs (VA) hospitals throughout the country,14, 19, 20 the cost of implementing the program has been primarily funded through grants, limiting the scalability. Health plans, however, can contribute to clinical research by directly funding projects and in turn, disseminating findings to physicians and patients.21 We present an alternative funding source to public grant coverage, a private payor quality initiative through Blue Cross & Blue Shield of Rhode Island (BCBSRI), thus highlighting the potential for other funding mechanisms to continue this work.
In this paper, we discuss a novel partnership with a private payor to support the implementation of EQUiPPED as a quality initiative in the largest health system in the state, encompassing three acute care hospitals. We hypothesized that EQUiPPED could be successful in reducing the rate of PIM prescribing among older adult patients being discharged from the ED.
STUDY DATA AND METHODS
This is a quality improvement study using a quasi-experimental interrupted time series design with a staggered intervention at three hospitals within the same health system. Data were extracted electronically each month from the health system’s clinical data warehouse. We followed SQUIRE (Standards for Quality Improvement Reporting Excellence) 2.0 reporting guidelines, which aim to improve the reporting of quality improvement work, in the creation of this manuscript.22 This study was approved by the hospital’s institutional review board.
Study Setting
The EQUiPPED intervention was instituted in three acute care hospitals comprising the largest health system in Rhode Island:
Rhode Island Hospital, an urban academic hospital, and the only level I trauma and tertiary referral center in the state, which receives 100,000 annual ED visits.
The Miriam Hospital, an urban academic hospital with 80,000 ED visits, which cares for predominantly older individuals.
Newport Hospital, a community hospital with 27,000 annual ED visits.
In addition to the three hospitals in this study, grand rounds lectures were also provided at others throughout the state to educate prescribers in various specialties about the EQUiPPED model. These other hospitals, however, were not part of this study; and other components of the EQUiPPED intervention were not implemented nor were outcome data collected at these sites.
All three study sites share the same EHR and are staffed by one emergency medicine clinician group. Most clinicians work at all or two of the three study sites and the same approach was used to implement EQUiPPED across all three sites, thus data on prescribing was aggregated under the clinician and not the site where they worked that particular day. Thus, we did not aim to look at performance differences across the three hospitals.
Procedures
Intervention material and components
EQUiPPED, an intervention which aims to reduce PIMs prescribed among older adults discharged from the ED, takes place in three-prongs: 1) medication order sets, 2) academic detailing and clinician feedback, and 3) geriatric education. The EQUiPPED intervention has previously been described in greater detail.23
-
Medication order sets
The principal investigator (PI)(EG) worked in collaboration with an EQUiPPED mentor (CV), a geriatrician, to obtain a list of medications deemed potentially inappropriate based on the American Geriatrics Society Beers Criteria,15 as well as the order set templates used during prior implementation studies at the VA hospital (using the Computerized Patient Record System EHR) and non-VA hospital (using Epic EHR) sites.
-
Academic detailing and clinician feedback
The medication order sets were used to develop monthly prescribing reports sent to clinicians (academic detailing) which showed them their personal rate of inappropriate prescribing in that month and overall, since the intervention started compared to their peers across the health system. Additionally, they were used to generate the EHR clinical decision support (reminders that pop up during clinical care).
-
Geriatric education
To perform the geriatric teaching, the study team obtained educational material to present during grand rounds, including several PowerPoint presentations on geriatric prescribing principles, as well as EQUiPPED laminated reminder cards which listed the top five PIMs. Reminder cards were affixed to the prescriber workstations in all three hospitals at the beginning of the intervention period.
Funding acquisition
The PI presented the EQUiPPED model at BCBSRI Medical Expense Trend Summit. The purpose of this summit was for community clinicians to present cost and quality improvement initiatives to providers within the insurers’ network that could improve the Triple Aim24 – quality, cost, and patient experience – of BCBSRI’s enrollees. As a winner of the summit competition, the PI met several times with representatives of the insurance company which resulted in a quality incentive payment to perform EQUiPPED within the health system and to promote and assist with implementation of the program at other sites within the state.25 Representatives from BCBSRI played no role in the design, data analysis, interpretation, or reporting of results.
The implementation of EQUiPPED was funded through a lump sum quality payment to the emergency medicine physician group that staffs the three EDs where the study was implemented. Deliverables in the contract included providing Continuing Medical Education or grand round lectures to clinicians at the study sites and to other clinicians across the state and providing information on how to implement EQUiPPED to quality staff and directors at other EDs in the state. Additionally, the funding supported the time and effort of the PI, information technology staff, and a fidelity visit by the study’s EQUiPPED mentor (CV), who traveled from Georgia to Rhode Island to hold a grand rounds lecture on EQUiPPED and meet with local study staff. Payments were not used to reimburse individual clinicians for their prescribing changes.
Modifications to intervention components to adapt to local practices
After obtaining funding, the PI shared the order set templates with the Director of Antibiotic Stewardship, an infectious disease physician (CC), at the health system, who worked with the infectious disease specialist pharmacist to make recommendations to modify the order set based on the local resistance patterns. Emphasis was placed on recommending effective antimicrobial therapy with low C.difficile and low resistance potential,26, 27 and listing appropriate dosing based on renal function. Antibiotics with low risk of side effects were also preferentially selected to minimize adverse events.
In addition, a geriatrician (NM) reviewed and modified the order set to align it with the current evidence-base and to ensure consistency with nationwide best practices. For instance, for some medications doses were decreased; trazodone changed from 50mg to 25mg when used for insomnia. Quetiapine 12.5 mg was added as an alternative to haloperidol for agitation in patients with Parkinson’s disease. First generation antipsychotics, like haloperidol, have high rates of extrapyramidal side effects such as acute dystonia and tardive dyskinesia due to dopamine receptor blockade, and should be avoided in Parkinson’s disease.28 Additionally, the stool softener senna with docusate was added because it is safe and more efficacious than docusate alone in geriatric populations.29, 30 Thereafter, the order set was approved and validated by the health system’s pharmacy & therapeutics committee.
Electronic health record integration
To make the order set accessible to prescribers in the ED, the PI worked together with the EPIC design team to create a new disposition order set within the discharge workflow. Specifically, when ED prescribers opened the disposition screen for the patient they were planning to discharge, they could select the “ED Geriatric Order Set.” This order set enabled them to click on the indication (e.g., “urinary tract infection”), and several antibiotics deemed appropriate for the local antibiogram, and the patient’s renal function, could be selected. Other indications that prescribers could select from included cardiology, dermatology, diabetes mellitus, gastroenterology, neurology, pain, and pulmonary. All prescription information including dosage and length of days were preprogrammed to improve efficiency and safety. For some medications, additional guidance relating to use in geriatric patients was included (e.g., under urticaria, prescribers were advised to avoid diphenhydramine due to anticholinergic effects).
Once the intervention started, the discharge order set could be accessed during an ED shift by clinicians as they were discharging a patient from the ED. After completion of the discharge order set build, the PI presented the new order set and the EQUiPPED program to the ED attendings, fellows, residents, and advanced practice providers (APPs). These meetings were held at all three sites during the intervention period. Boosters were held at faculty meetings, clinical site meetings, resident orientation, and APP educational meetings in subsequent months.
Implementation
The PI also met with the ED informatics specialists to plan collection and analysis of the prescribing data prior to and after the intervention. Each month after the initial presentation about EQUiPPED, every ED attending, fellow, resident, and APP received a monthly e-mail report showing them their personal rate of inappropriate prescribing in that month and overall, since the intervention started, compared to their peers across the health system. The prescriber also received a list of the PIMs they prescribed in that month and overall. The PI audited the monthly results, contacting prescribers with the highest monthly PIM rates and responding to inquiries from individual prescribers desiring to improve their practices or discuss a specific patient encounter. When trends emerged in the prescribing habits (e.g., meclizine and benzodiazepines were commonly prescribed for vertigo), targeted lectures and evidence-based material were delivered to inform clinicians of alternative treatment options to prescribing PIMs. During the COVID-19 pandemic, in person meetings with prescribers were avoided and most communication was via email or telephone. It was at the clinician’s discretion whether to read the monthly reports, use the discharge order set, or attend geriatric teaching sessions. Continuing medical education and resident conference credits were provided as incentives to engage with the content.
Emergency medicine clinicians
In response to concerns from attendings that high PIM prescribing rates were affected by the prescribing practices of supervised fellows, resident physicians, or APPs rather than by personal prescribing habits, the study team changed the monthly reports to disaggregate trainees from the supervising attendings and subsequently all prescribers received individual reports.
Statistical Analysis
Descriptive analyses were performed to describe the prescribers and medication use. We performed Poisson regression to compare the rate of PIMs prescribed in the 13 months before the EQUiPPED intervention with the 16 months of data after the intervention period. The natural log of the total number of prescriptions served as the offset term in the model, and a piecewise, non-linear regression model was used to evaluate the pattern of PIMs prescribed over time. The primary outcome, monthly rate of PIMs, was calculated from all PIMs prescribed to older patients (aged 65 and older) being discharged from the ED in each month (numerator) divided by the total number of medications prescribed to older patients in each month (denominator). The use of aggregate monthly rate of PIMs addressed the potential for overdispersion. Statistical analysis was conducted using SAS (version 9.4, Cary, NC).
RESULTS
247 ED clinicians (48.2% were attending physicians (n=119), 27.1% were resident physicians (n=67), 24.7% were APPs (n=61) were included in EQUiPPED (Table 1) across all three hospital sites, of which 92.3% (n=228) prescribed a PIM during the study period. See Figure 1. for a pictogram which highlights the different stages of the study. Among clinicians prescribing a PIM during the study period, 184 (80.7%) in the pre-implementation and 187 (82%) in the post-implementation period provided a prescription to older adults in one of the three hospitals.
Table 1.
Characteristics of clinicians (n=247)
| Characteristic | n (%) |
|---|---|
| Credentials | |
| Attending physician | 119 (48.2%) |
| Resident physician | 67 (27.1%) |
| Advanced Practice Provider | 61 (24.7%) |
| Participated in intervention | |
| Yes | 224 (90.7%) |
| No | 23 (9.3%) |
| Clinician prescribed at least one PIM | |
| Yes | 228 (92.3%) |
| No | 19 (7.7%) |
| PIM by study period among clinicians prescribing at least one PIM | |
| Pre-implementation | 184 (80.7%) |
| Post-implementation | 187 (82.0%) |
NOTE: PIM= Potentially Inappropriate Medication
Figure 1:
Pictogram of Study
NOTE: This figure was created by the authors of this paper and has not been reused.
Change in prescribing over time
In the pre-implementation period (July 2018 – July 2019), the average monthly rate of PIM prescribing to older adults was 9.30% (95% CI: 8.82% – 9.78%). In the post-implementation period (October 2019 to January 2021), the PIM prescribing rate decreased significantly to 8.62% (95% CI: 8.14% – 9.10%, p <0.01) (Figure 2, Table 2). In the pre-implementation period 1,325 of the 14,193 prescribed medications were considered inappropriate, while only 1,108 of the 13,213 prescribed medications in the post-implementation period were considered inappropriate (Supplementary Table S1).
Figure 2:
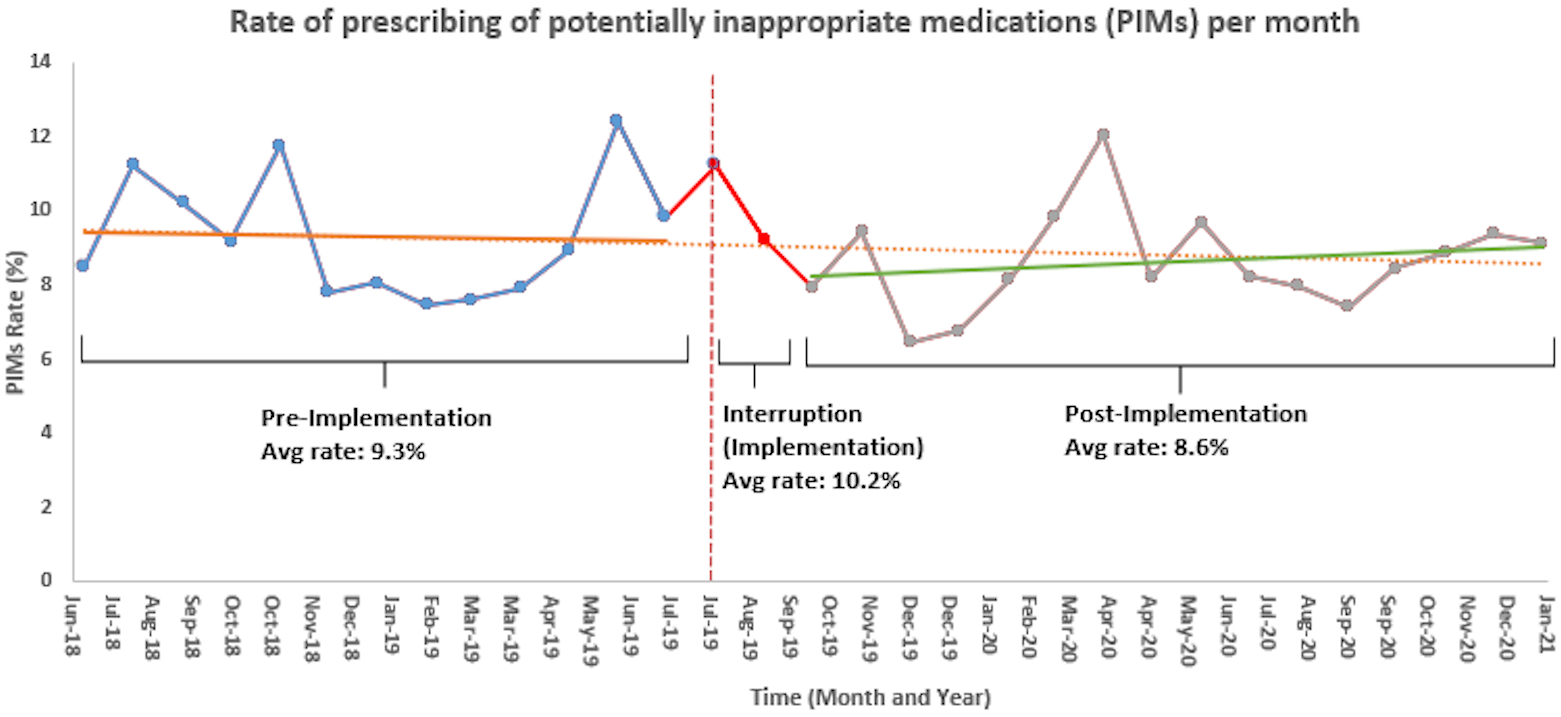
Rate of prescribing of potentially inappropriate medications (PIMs) per month
NOTE: The pre-implementation period data points are denoted by the blue dots and a solid orange line for the slope. The interruption (implementation period) is denoted by the red dots and the interruption point is depicted with a vertical dotted red line. The post implementation period is denoted by grey dots and a solid green line for the slope. The counterfactual slope is depicted with the dotted orange horizontal line, which was generated using the forecast function in excel based on data from the pre-implementation period.
NOTE: This figure was created by the authors of this paper and has not been reused.
Table 2.
Poisson regression assessing the effect of time on monthly PIMs rates
| Effect | Estimate (95% CI) |
|---|---|
| Intercept | 0.084 (0.079–0.089) *** |
| Pre-Implementationa vs. Post-Implementationb | 1.11 (1.03–1.21) ** |
| Pre-implementation slope | −0.0011 (−0.015–0.013 |
| Post implementation slope | 0.0081 (−0.0043–0.02) |
NOTE: PIM= Potentially Inappropriate Medication
NOTE: CI = Confidence Interval
p < .05;
p < .01;
p < .001
Log likelihood: 8399.43; AIC: 245.10; BIC: 247.83
Pre-implementation period covers medication prescribing behaviors during the 13-months before program implementation
Post-implementation period covers medication prescribing behaviors during the 16-months after program implementation
The results of the piecewise, non-linear regression model evaluating the pattern of PIMs prescribed over time are shown in Table 2. The incidence rate ratios comparing the difference in PIMs at various study time points were statistically significant. PIMs at the pre-implementation compared to the post-implementation time periods had a rate 1.11 times greater (95% CI: 1.03–1.21, p < .01). The pre-implementation slope had an estimate of −0.0011 (95% CI: −0.015–0.013), p = 0.88 and post-implementation slope had an estimate of 0.0081 (95% CI: −0.0043–0.02), p = 0.20. Both pre-implementation and post-implementation slopes were not significantly different suggesting that the pre- to post-implementation change in PIMs represents a significant change in level with no significant change in slope. The change in level indicates a change in the intercept, i.e., there is a significant change in the mean following the intervention. The slope pre-intervention is non-significant, indicating an overall consistency in the intercept, on average, and the post-intervention slope is non-significant indicating that the rate of change in the intercept does not significantly change over the months of observation. PIMs at the implementation compared to the post-implementation period (results not shown) had a rate 1.23 times greater (95% CI: 1.07–1.41). We conducted a sensitivity analysis excluding the pandemic period (March 2020 – January 2021) from the post-implementation period, and the original results held. In the modified analysis excluding “COVID months” had an odds ratio estimate of 1.21 (95% CI: 1.09–1.36). The modified analysis excluding “COVID months” had a slope of −0.031 (95% CI: −0.1005 – 0.0389).
What drug classes were most impacted by EQUiPPED intervention?
The change in PIM rate by drug class can be seen in Figure 3. The greatest change from pre-implementation to post-implementation was in antihistamines (3.36% to 3.01%; Δ = −0.35%; 95% CI: −0.42% – −0.28%), skeletal muscle relaxants (3.08% to 2.36%; Δ = −0.72%; 95% CI: −0.82% – −0.62%) and benzodiazepines (1.91% to 1.30%; Δ = −0.61%; 95% CI: −0.70% – −0.62%). Antispasmodic (0.32% to 0.25%; Δ = −0.07%; 95% CI: −0.10% – −0.04%) and NSAID (0.32% to 0.26%; Δ = −0.06%; 95% CI: −0.09% – −0.03%) prescribing also improved, though less so. A full list of medications and their relative changes can be viewed in Supplementary Figure S1.
Figure 3:
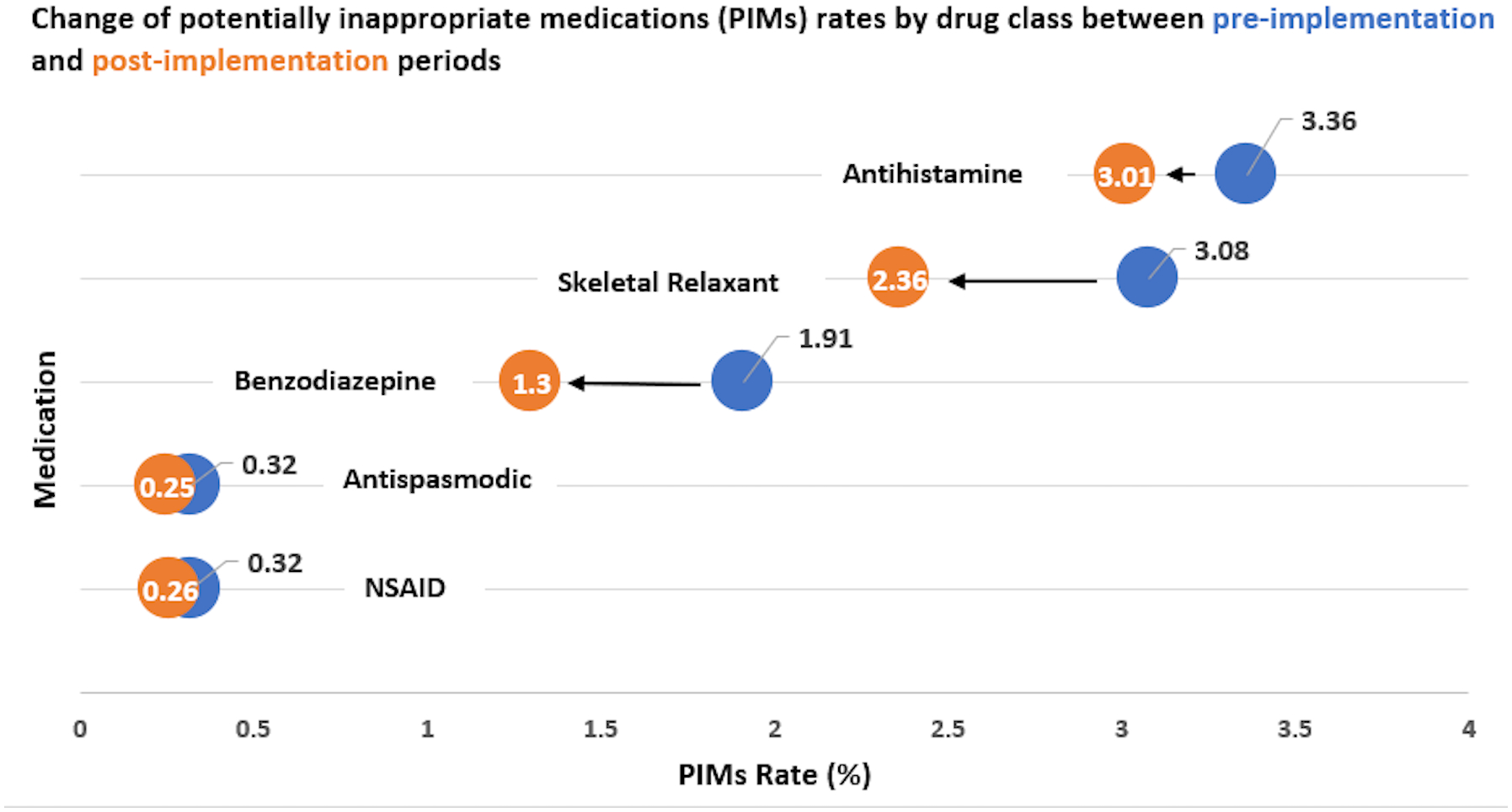
Change of potentially inappropriate medications (PIMs) rate by drug class between pre-implementation (blue) and post-implementation (orange) periods
NOTE: This figure was created by the authors of this paper and has not been reused.
DISCUSSION
In this quality improvement project among 247 prescribers in the largest health system in Rhode Island, we found the EQUiPPED intervention modestly contributed to a reduction in PIM prescribing to older adults discharged from the ED. Our results are similar to those seen in other VA and academic health systems;14, 19 however, our implementation was unique as it was conducted among the largest number of clinicians of any EQUiPPED implementation site, supported by a payor through a quality incentive program, included attendings, trainees, and APPs (vs. attendings only), and occurred during a pandemic.
Prior studies of EQUiPPED instituted in VA hospitals demonstrated a significant reduction in PIM prescribing from 9.4 +/− 1.5% before the intervention to 4.6 +/− 1.0% after initiation of EQUiPPED (p<0.001)23 and that these improvements were sustained for months after the completion of the intervention. Our study showed comparable directionality of prescribing rates prior to and after the intervention, but the magnitude of change, while significant, was much lower in our study (0.7% v. 4.8%). When EQUiPPED was first implemented outside of the VA at academic medical centers, only one of the three implementation sites demonstrated significant reduction in PIMs,31 which was thought to be due to lower baseline PIM proportions when compared to the VA (5.6%−7.3% vs. 7.4%−11.9%). There may be other factors at academic medical centers that yield less significant reductions, such as a large amount of prescribing being initiated by rotating trainees. Additionally, COVID cause marked disruption of clinical care in the ED and could have affected the potential for behavior change among clinicians. It is important to note, however, that existing findings in the literature, including this study, must be interpreted with caution, due to the usage of observational study designs. Future work could employ a randomized controlled trial (RCT) to better account for potential unmeasured confounders, but this design could be difficult to implement given that a different EHR build would be necessary for the intervention and control arm.
A critique of the EQUiPPED intervention includes that Beers medication may only account for a small percent of medications that cause adverse drug events.32 In a study by Shehab et al.7 Beers criteria medications were implicated in only 1.8% (95% CI, 1.5%−2.1%) of ED visits for adverse drug events, but other analyses have shown that medications on the Beers list are associated with significant adverse drug events.33, 34 We may have seen a less pronounced reduction in PIMs prescribing due to several factors: 1) the large number of rotating trainees in any given month in the ED that did not have full exposure to the intervention (e.g., only had access to the order sets), and 2) the COVID-19 pandemic significantly decreased ED volume system-wide, increased severity of illness, and may have made clinicians less responsive to quality initiatives.
While EQUiPPED focuses on reducing the prescribing of new PIMs at the point of ED discharge, there are several other ways to improve medication safety among older adult ED patients. For instance, a recent analysis of 168 non-cognitively impaired older ED patients (mean age = 65), revealed that only 23% could recall their medications accurately as compared to pharmacy-dispense records.35 Using multiple sources for recall (e.g., lists and caregiver help) improved recall, but emergency clinicians should be aware that recall errors are common in this population and could lead to prolonged harmful medication use. Additionally, medication not disclosed could be the inciting reasons for the ED visit or could interact with newly prescribed medication. ED-embedded pharmacists are becoming more prevalent in large health systems and could improve medication reconciliation, the identification of adverse drug events, and prevent future medication-related health events, such as falls.36, 37
Clinical and policy implications of this work include that working together with payors in a quality incentive program may reduce the need for longer timelines of funding acquisition and enhance the willingness of clinical departments to agree to large-scale changes in clinical practice.21 These projects are often burdensome and led by researchers that may have fewer interactions with clinical personnel, but receiving funding from a payor allows for more buy-in from department leadership and medical directors, and therefore could ease implementation.
Limitations
Although findings may not necessarily be generalizable outside of Rhode Island, this study was conducted among the largest number of clinicians of any EQUiPPED implementation site and included attendings, trainees, and APPs (vs. attendings only), expanding the scope of previous work. Additionally, the absolute change in our findings was small, likely correlated with the effects of COVID-19 which included a significant decrease in health system wide ED volume, potentially more patients requiring hospice/palliative care, and yet unclear impacts on prescribing practices. However, we estimate that COVID-19 would make quality initiatives more challenging and yet we were able to achieve a modest reduction in the rate of PIM prescribing. Thus, without COVID-19 we suspect a greater rate of decline would have been observed.
CONCLUSIONS
Implementation of EQUiPPED through a payor supported quality incentive program in the largest health system in Rhode Island contributed to an improvement in PIM prescribing amongst clinicians in the ED. Payment models like these should be considered in other states and could shape national policy.
Supplementary Material
Supplementary Table S1: Changes in PIMS between intervention time points by drug class.
Supplementary Figure S1: Change of potentially inappropriate medications (PIMs) rates by drug class between pre-implementation (blue) and post-implementation (orange) periods
NOTE: This figure was created by the authors of this paper and has not been reused.
Key points:
EQUiPPED contributed to a modest reduction in the PIM prescribing rate at three acute care hospitals comprising the largest health system in Rhode Island.
This project was funded through a private payor quality initiative, highlighting to utility of alternative payment methods to support quality improvement work.
Why Does this Paper Matter?
Our findings demonstrate that the EQUiPPED intervention can contribute to reducing PIM prescribing to older adults being discharged from the ED; greater replication of this intervention and outsourcing for other means of funding, such as the private payor initiative described here, to support this project can influence national policy regarding quality of care for older adults.
ACKNOWLEDGEMENTS
Special thanks to Lynn McNicoll, MD, Diane Parente, PharmD, Kim Rodrigues and Lori Connors (Epic team), John Brister and Dennis Ferrante (IT team) for their contributions.
This work was supported by Blue Cross & Blue Shield of Rhode Island. This research was also supported by the National Institute of Health’s National Institute on Aging (NIA), grant K76 AG059983.
FUNDING
This work was supported by Blue Cross & Blue Shield of Rhode Island. The funder met with the principal investigator to discuss the implementation of the study and ensure study progress. However, the funder played no role in the design, data analysis, interpretation or reporting of results. This research was also supported by the National Institute of Health’s National Institute on Aging (NIA), grant K76 AG059983. The NIA played no role in the study design, collection, analysis, and interpretation of the data, in the writing of the report or the decision to submit the paper for publication.
SPONSOR’S ROLE
The sponsors were not involved in any aspect of study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, or preparation of manuscript.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
- 1.Halli-Tierney AD, Scarbrough C, Carroll D. Polypharmacy: Evaluating Risks and Deprescribing. Am Fam Physician 2019;100(1):32–38. [PubMed] [Google Scholar]
- 2.Mather MSP, Kilduff L. Fact Sheet: Aging in the United States. Population Reference Bureau; 2019. (online). Available at: https://www.prb.org/resources/fact-sheet-aging-in-the-united-states/. Accessed November 20, 2021. [Google Scholar]
- 3.Garber J, Brownlee S. Medication Overload: America’s Other Drug Problem. Brookline, MA: The Lown Institute, 2019. (online). Available at: 10.46241/LI.WOUK3548. Accessed November 20, 2021. [DOI] [Google Scholar]
- 4.Bourgeois FT, Shannon MW, Valim C, Mandl KD. Adverse drug events in the outpatient setting: an 11-year national analysis. Pharmacoepidemiol Drug Saf 2010;19(9):901–10. DOI: 10.1002/pds.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanlon JT, Pieper CF, Hajjar ER et al. Incidence and predictors of all and preventable adverse drug reactions in frail elderly persons after hospital stay. J Gerontol A Biol Sci Med Sci 2006;61(5):511–5. DOI: 10.1093/gerona/61.5.511. [DOI] [PubMed] [Google Scholar]
- 6.Gandhi TK, Weingart SN, Borus J et al. Adverse drug events in ambulatory care. N Engl J Med 2003;348(16):1556–64. DOI: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 7.Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US Emergency Department Visits for Outpatient Adverse Drug Events, 2013–2014. Jama 2016;316(20):2115–2125. DOI: 10.1001/jama.2016.16201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clark CM, Shaver AL, Aurelio LA et al. Potentially Inappropriate Medications Are Associated with Increased Healthcare Utilization and Costs. J Am Geriatr Soc 2020;68(11):2542–2550. DOI: 10.1111/jgs.16743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hastings SN, Schmader KE, Sloane RJ et al. Quality of Pharmacotherapy and Outcomes for Older Veterans Discharged from the Emergency Department. J Am Geriatr Soc 2008;56(5):875–880. DOI: 10.1111/j.1532-5415.2008.01648.x. [DOI] [PubMed] [Google Scholar]
- 10.Brown JD, Hutchison LC, Li C, Painter JT, Martin BC. Predictive Validity of the Beers and Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions (STOPP) Criteria to Detect Adverse Drug Events, Hospitalizations, and Emergency Department Visits in the United States. J Am Geriatr Soc 2016;64(1):22–30. DOI: 10.1111/jgs.13884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang P, Wang Q, Li F, Bian M, Yang K. Relationship Between Potentially Inappropriate Medications And The Risk Of Hospital Readmission And Death In Hospitalized Older Patients. Clin Interv Aging 2019;14:1871–1878. DOI: 10.2147/cia.S218849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cross AJ, George J, Woodward MC et al. Potentially Inappropriate Medication, Anticholinergic Burden, and Mortality in People Attending Memory Clinics. J Alzheimers Dis 2017;60(2):349–358. DOI: 10.3233/jad-170265. [DOI] [PubMed] [Google Scholar]
- 13.Jeon HL, Park J, Han E, Kim DS. Potentially inappropriate medication and hospitalization/emergency department visits among the elderly in Korea. Int J Qual Health Care 2018;30(1):50–56. DOI: 10.1093/intqhc/mzx171. [DOI] [PubMed] [Google Scholar]
- 14.Stevens M, Hastings SN, Markland AD et al. Enhancing Quality of Provider Practices for Older Adults in the Emergency Department (EQUiPPED). J Am Geriatr Soc 2017;65(7):1609–1614. DOI: 10.1111/jgs.14890. [DOI] [PubMed] [Google Scholar]
- 15.Panel BtAGSBCUE. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 2019;67(4):674–694. DOI: 10.1111/jgs.15767. [DOI] [PubMed] [Google Scholar]
- 16.Vandenberg AE, Stevens M, Echt KV et al. Implementing the EQUiPPED Medication Management Program at 5 VA Emergency Departments. Fed Pract 2016;33(4):29–33. [PMC free article] [PubMed] [Google Scholar]
- 17.Vandenberg AE, Vaughan CP, Stevens M et al. Improving geriatric prescribing in the ED: a qualitative study of facilitators and barriers to clinical decision support tool use. Int J Qual Health Care 2017;29(1):117–123. DOI: 10.1093/intqhc/mzw129. [DOI] [PubMed] [Google Scholar]
- 18.Burningham Z, Jackson GL, Kelleher J et al. The Enhancing Quality of Prescribing Practices for Older Veterans Discharged From the Emergency Department (EQUIPPED) Potentially Inappropriate Medication Dashboard: A Suitable Alternative to the In-person Academic Detailing and Standardized Feedback Reports of Traditional EQUIPPED? Clin Ther 2020;42(4): 573–582. DOI: 10.1016/j.clinthera.2020.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Vandenberg AE, Stevens M, Echt KV et al. Implementing the EQUiPPED Medication Management Program at 5 VA Emergency Departments. Fed Pract 2016;33(4):29–33. [PMC free article] [PubMed] [Google Scholar]
- 20.Moss JM, Bryan WE III, Wilkerson LM et al. Impact of Clinical Pharmacy Specialists on the Design and Implementation of a Quality Improvement Initiative to Decrease Inappropriate Medications in a Veterans Affairs Emergency Department. J Manag Care Spec Pharm 2016;22(1):74–80. DOI: 10.18553/jmcp.2016.22.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tunis SKA, Ommaya A. The Role of Purchasers and Payers in the Clinical Research Enterprise: Workshop Summary. Institute of Medicine (US) Clinical Research Roundtable. Washington (DC): National Academies Press (US); 2002. [PubMed] [Google Scholar]
- 22.SQUIRE. Revised Standards for Quality Improvement Reporting Excellence. 2020. (online). Available at: http://squire-statement.org/index.cfm?fuseaction=Page.ViewPage&PageID=471. Accessed November 20, 2021.
- 23.Stevens MB, Hastings SN, Powers J et al. Enhancing the Quality of Prescribing Practices for Older Veterans Discharged from the Emergency Department (EQUiPPED): Preliminary Results from Enhancing Quality of Prescribing Practices for Older Veterans Discharged from the Emergency Department, a Novel Multicomponent Interdisciplinary Quality Improvement Initiative. J Am Geriatr Soc 2015;63(5):1025–9. DOI: 10.1111/jgs.13404. [DOI] [PubMed] [Google Scholar]
- 24.Institute for Healthcare Improvement. Triple Aim for Populations. 2022. (online). Available at: http://www.ihi.org/Topics/TripleAim/Pages/Overview.aspx. Accessed November 20, 2021.
- 25.Minemyer P Blue Cross & Blue Shield of Rhode Island, Brown launch initiative to reduce adverse drug events. Fierce Healthcare 2019. (online). Available at: https://www.fiercehealthcare.com/payer/blue-cross-blue-shield-rhode-island-brown-launch-initiative-to-reduce-adverse-drug-events. Accessed November 20, 2021.
- 26.Cunha CB, Opal SM. Antibiotic Stewardship: Strategies to Minimize Antibiotic Resistance While Maximizing Antibiotic Effectiveness. Med Clin North Am 2018;102(5):831–843. DOI: 10.1016/j.mcna.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 27.Cunha BA, Hage JE, Schoch PE, Cunha CB, Bottone EJ, DC T . Overview of Antimicrobial Therapy, 17th Ed. New Delhi: Jaypee Brothers Medical Publishers Ltd, 2020. [Google Scholar]
- 28.Kennedy M, Koehl J, Shenvi CL et al. The agitated older adult in the emergency department: a narrative review of common causes and management strategies. J Am Coll Emerg Physicians Open 2020;1(5):812–823. DOI: 10.1002/emp2.12110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Izzy M, Malieckal A, Little E, Anand S. Review of efficacy and safety of laxatives use in geriatrics. World J Gastrointest Pharmacol Ther 2016;7(2):334–342. DOI: 10.4292/wjgpt.v7.i2.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pasay D, Guirguis M, Shkrobot R, Slobodan J, Bresee L. Association of Dissemination of an Educational Communication Tool With Docusate Administration. JAMA Intern Med 2017;177(10):1433–1436. DOI: 10.1001/jamainternmed.2017.3605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vaughan CP, Hwang U, Vandenberg AE et al. Early prescribing outcomes after exporting the EQUIPPED medication safety improvement programme. BMJ Open Qual 2021;10(4):e001369. DOI: 10.1136/bmjoq-2021-001369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Budnitz DS, Shehab N, Kegler SR, Richards CL. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med 2007;147(11):755–65. DOI: 10.7326/0003-4819-147-11-200712040-00006. [DOI] [PubMed] [Google Scholar]
- 33.Lund BC, Steinman MA, Chrischilles EA, Kaboli PJ. Beers Criteria as a Proxy for Inappropriate Prescribing of Other Medications Among Older Adults. Ann Pharmacother 2011;45(11):1363–1370. DOI: 10.1345/aph.1Q361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Arch Intern Med 2005;165(1):68–74. DOI: 10.1001/archinte.165.1.68. [DOI] [PubMed] [Google Scholar]
- 35.Goldberg EM, Marks SJ, Merchant RC, Nagy JL, Aquilante JA Jr, Beaudoin FL. How accurately do older adult emergency department patients recall their medications? Acad Emerg Med 2021;28(2):248–252. DOI: 10.1111/acem.14032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldberg EM, Marks SJ, Ilegbusi A, Resnik L, Strauss DH, Merchant RC. GAPcare: The Geriatric Acute and Post-Acute Fall Prevention Intervention in the Emergency Department: Preliminary Data. J Am Geriatr Soc 2020;68(1):198–206. DOI: 10.1111/jgs.16210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goldberg EM, Marks SJ, Resnik LJ, Long S, Mellott H, Merchant RC. Can an Emergency Department-Initiated Intervention Prevent Subsequent Falls and Health Care Use in Older Adults? A Randomized Controlled Trial. Ann Emerg Med 2020;76(6):739–750. DOI: 10.1016/j.annemergmed.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Changes in PIMS between intervention time points by drug class.
Supplementary Figure S1: Change of potentially inappropriate medications (PIMs) rates by drug class between pre-implementation (blue) and post-implementation (orange) periods
NOTE: This figure was created by the authors of this paper and has not been reused.


