Abstract
Pancreatic ductal adenocarcinoma (PDAC) is a highly desmoplastic, aggressive cancer that frequently progresses and spreads by metastasis to the liver1. Cancer-associated fibroblasts, the extracellular matrix and type I collagen (Col I) support2,3 or restrain the progression of PDAC and may impede blood supply and nutrient availability4. The dichotomous role of the stroma in PDAC, and the mechanisms through which it influences patient survival and enables desmoplastic cancers to escape nutrient limitation, remain poorly understood. Here we show that matrix-metalloprotease-cleaved Col I (cCol I) and intact Col I (iCol I) exert opposing effects on PDAC bioenergetics, macropinocytosis, tumour growth and metastasis. Whereas cCol I activates discoidin domain receptor 1 (DDR1)–NF-κB–p62–NRF2 signalling to promote the growth of PDAC, iCol I triggers the degradation of DDR1 and restrains the growth of PDAC. Patients whose tumours are enriched for iCol I and express low levels of DDR1 and NRF2 have improved median survival compared to those whose tumours have high levels of cCol I, DDR1 and NRF2. Inhibition of the DDR1-stimulated expression of NF-κB or mitochondrial biogenesis blocks tumorigenesis in wild-type mice, but not in mice that express MMP-resistant Col I. The diverse effects of the tumour stroma on the growth and metastasis of PDAC and on the survival of patients are mediated through the Col I–DDR1–NF-κB–NRF2 mitochondrial biogenesis pathway, and targeting components of this pathway could provide therapeutic opportunities.
Subject terms: Cancer metabolism, Cancer microenvironment, Cancer metabolism, Nutrient signalling
Cleaved and intact type I collagen have different effects on pancreatic ductal adenocarcinoma (PDAC), and remodelling of type I collagen—mediated through DDR1 signalling—is a prognostic indicator for the survival of patients with PDAC.
Main
Retrospective clinical studies suggest that patients with PDAC whose tumours have a fibrogenic but inert stroma (defined by extensive extracellular matrix (ECM) deposition, low expression of the myofibroblast marker α-SMA and low levels of matrix metalloprotease (MMP) activity) have improved progression-free survival compared to patients whose tumours are populated by a fibrolytic stroma (defined by a low content of collagen fibres, high expression of α-SMA and high levels of MMP activity)5. How the stromal state affects clinical outcome is unknown. Moreover, previous investigations of the influence of the stroma on the growth and progression of PDAC have yielded conflicting results, assigning stroma and cancer-associated fibroblasts (CAFs) as either tumour-supportive6 or tumour-restrictive4. It is likely that the failure of stromal-targeted PDAC therapies7 is due, in part, to unrecognized pathways that result in tumour-promoting or tumour-suppressive stromal subgroups; successful treatments may thus require precision medicine rather than one-size-fits-all approaches.
cCol I and iCol I differentially affect PDAC growth
To investigate how the fibrolytic stroma affects PDAC outcome, we compared survival between patients with high and low collagenolysis, using a panel of collagen-cleaving MMPs (MMP1, MMP2, MMP8, MMP9, MMP13 and MMP14), and found that high mRNA expression of MMPs correlated with poor survival (Extended Data Fig. 1a). Single-cell RNA sequencing (scRNA-seq) revealed that MMP1, MMP14 and MMP2 mRNAs were the most abundant MMP family members, and were expressed in epithelial-tumour cells, M2-like macrophages and fibroblastic cells (Extended Data Fig. 1b). The main target of MMPs in desmoplastic tumours is Col I, the prevalent ECM protein. Using antibodies that distinguish iCol I from cCol I (3/4 Col I; Fig. 1a), we stratified a cohort of 106 patients with PDAC whose tumours had been resected (see below), and correlated the tumour Col I state with survival data. These results also pointed to Col I remodelling as a strong prognostic factor, as patients whose tumours were enriched for cCol I had poorer median survival (Fig. 1b). To understand the basis for these results and mimic a cCol Ilow inert tumour stroma, we used mice expressing either wild-type Col1a1+/+ (Col IWT), or a MMP-resistant version of Col I generated by two amino acid substitutions in the 1α1 subunit that block the cleavage of Col I by MMPs8, Col1a1r/r (Col Ir/r). Col Ir/r mice develop more-extensive hepatic fibrosis than Col IWT mice, but despite the hepatocellular carcinoma (HCC)-supportive functions of hepatic fibrosis9, they poorly accommodate HCC growth, through unknown mechanisms10. Col IWT and Col Ir/r mice were either orthotopically or intrasplenically (to model liver metastasis) transplanted with mouse PDAC KPC960 (KPC) or KC6141 (KC) cells. Col Ir/r mice poorly supported the growth of primary pancreatic tumours or hepatic metastases, even though their pancreata were more fibrotic than Col IWT pancreata. These differences persisted in mice that were pretreated with the pancreatitis inducer caerulein (CAE), which stimulated liver metastasis in Col IWT pancreata (Fig. 1c,d and Extended Data Fig. 1c–f). After intrasplenic transplantation, KPC or KC tumours in Col IWT livers were larger in mice pretreated with CCl4 to induce liver fibrosis, whereas the number and size of tumours were lower in Col Ir/r livers, regardless of CCl4 pretreatment (Fig. 1e,f and Extended Data Fig. 1g). As expected, Col Ir/r livers were more fibrotic than Col IWT livers, regardless of CCl4 pretreatment (Extended Data Fig. 1h). Primary PDAC and liver metastases were confirmed by staining with ductal (CK19), progenitor (SOX9) or proliferation (Ki67) markers (Extended Data Fig. 1e,f,i). Enhanced tumour growth in CAE- or CCl4-pretreated Col IWT mice suggested that tumour suppression in Col Ir/r mice was not simply due to a space limitation imposed by a build-up of Col I. To determine how Col I remodelling affects human PDAC, we subcutaneously co-transplanted wild-type and R/R fibroblasts with a patient-derived xenograft cell line (1305) into immunocompromised Nu/Nu mice. Wild-type fibroblasts enhanced tumour growth, whereas R/R fibroblasts inhibited tumour growth but lost their inhibitory activity after ablation of Col1a1 (Fig. 1g) whose loss did not affect the stimulatory activity of wild-type fibroblasts, suggesting a specific inhibitory function of noncleaved Col I.
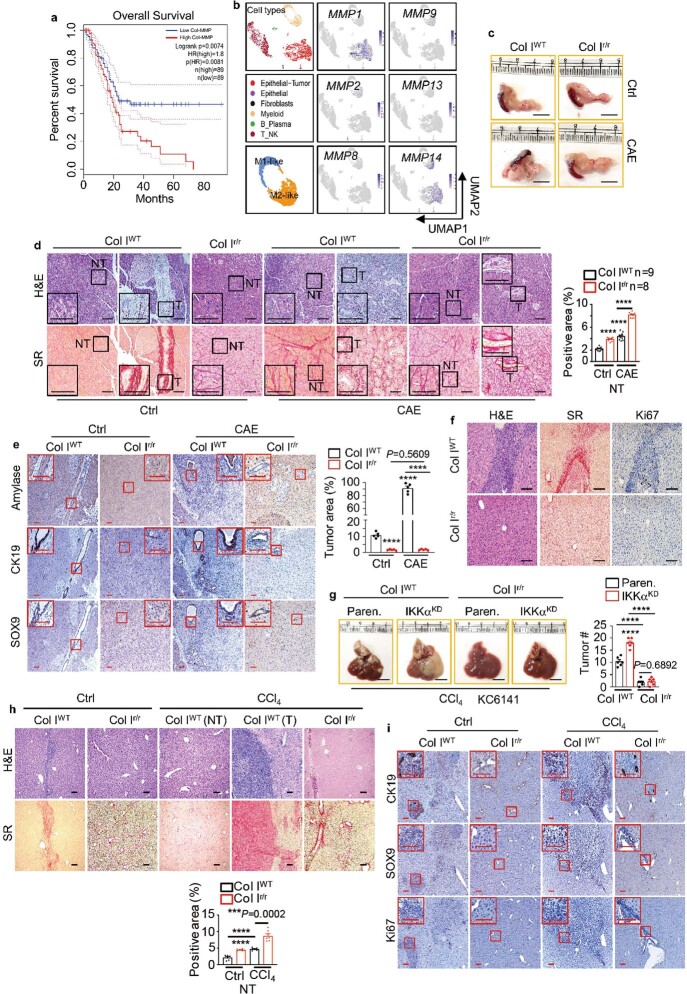
Extended Data Fig. 1. Col I cleavage stimulates PDAC growth.
a, Overall survival of patients with PDAC from TCGA with high and low collagen-cleaving MMP signature (MMP1, 2, 8, 9, 13, 14). Significance was analysed by log-rank test. b, UMAPs showing scRNA-seq data from 5 primary PDACs, displaying cell types and expression of the most abundant MMP mRNAs. c, Pancreas morphology 4 wk after orthotopic KPC cell transplantation into Col IWT or Col Ir/r mice −/+ CAE pretreatment. d, H&E and sirius red (SR) staining of pancreatic sections from above mice. Boxed areas were further magnified. Quantification of SR positivity in nontumor (NT) areas is shown to the right. e, IHC of pancreatic sections from above mice. Quantification of tumour areas is shown to the right. f, H&E, SR, Ki67 staining of liver sections from above CAE-pretreated mice. g, Liver gross morphology and tumour numbers (#) 2 wk after i.s. transplantation of Paren. or IKKα knockdown (KD) KC cells into CCl4 pretreated Col IWT or Col Ir/r mice. h, H&E and SR staining of liver sections 2 wk after i.s. transplantation of KPC cells into Col IWT and Col Ir/r mice −/+ CCl4 pretreatment. Quantification of SR positivity in NT areas is shown at the bottom. i, IHC of liver sections from above mice. Boxed areas show higher magnification. Results in (e) (n = 5 fields), (g), (h) (n = 6 mice) and (d) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. ***P < 0.001, ****P < 0.0001. Scale bars in (d–f, and h,i), 100 μm, (c,g), 1 cm.
Fig. 1. Col I cleavage controls PDAC growth.
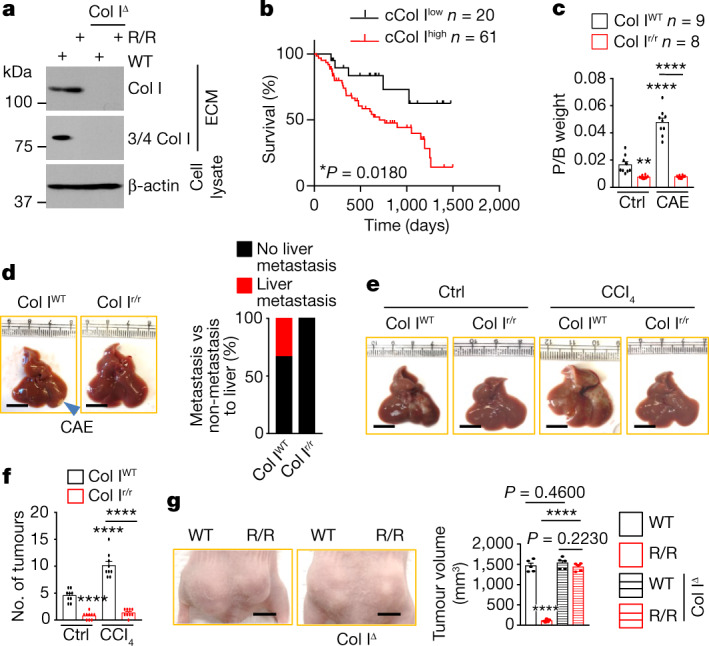
a, Immunoblot showing the specificity of antibodies to iCol I and cCol I (3/4 Col I) in ECM produced by the indicatedfibroblasts. Col IΔ, Col I knockout; WT, wild type. b, Overall survival of patients with resected PDAC stratified according to cCol I expression (shown in Fig. 5a). Significance was determined by log-rank test. c, Pancreas weight relative to body weight (P/B weight) four weeks after orthotopic KPC cell transplantation into Col IWTor Col Ir/rmice that were pretreated with CAE or without CAE. Ctrl, control. d, Liver morphology in CAE-treated mice. Liver metastases were detected in 33% of Col IWTmice. e,f, Liver gross morphology (e) and tumour numbers (f) two weeks after intrasplenic transplantation of KPC cells into Col IWTor Col Ir/rmice with or without CCl4 pretreatment. g, Representative images and sizes of subcutaneous tumours formed by human 1305 cells co-transplanted with WT, R/R or Col IΔ WT or R/R fibroblasts into Nu/Nu mice. Data in f (n = 9 mice), g (n = 5 mice) and c are mean ± s.e.m. Statistical significance determined by two-tailed t-test. Exact P values in c,f are shown in the Source Data. ****P < 0.0001. Scale bars (d,e,g), 1 cm.
The Col I state controls PDAC metabolism
To determine the basis for reduced tumorigenesis in Col Ir/r mice, we plated KPC cells on ECM deposited by wild-type and R/R fibroblasts, incubated them in low-glucose (LG) medium (to model nutrient restriction) and performed RNA sequencing (RNA-seq). Bioinformatic analysis revealed marked differences between cells cultured on wild-type and cells cultured on R/R ECM, with the former showing an upregulation of signatures related to sulfur amino acid metabolism, mammary gland morphogenesis, telomere maintenance and RNA processing, and the latter showing an upregulation of mRNAs related to innate immunity and inflammation (Extended Data Fig. 2a). The most notable differences were in nuclear and mitochondrial genes that encode components of the mitochondrial electron transfer chain (ETC) and ribosome subunits, and macropinocytosis-related genes, which were upregulated by wild-type and suppressed by R/R ECM (Fig. 2a–c). Consistent with the upregulation of macropinocytosis-related genes by wild-type ECM, IKKα-deficient KC cells, which have high macropinocytosis activity11, grew better than parental cells in Col IWT livers, but grew as poorly as parental KC cells in Col Ir/r livers (Extended Data Fig. 1g).
Extended Data Fig. 2. The Col I state controls PDAC gene expression and metabolism.
a, Dataset enrichment of RNA-seq data (n = 3) from KPC cells plated on wild-type (WT) (blue) or R/R (red) ECM and incubated in LG for 24 h. b, KPC cells grown on [3H]-proline-labelled WT, R/R, Col IΔ R/R or Col IΔ R/R + Col IWT ECM were incubated in LG −/+ EIPA for 24 h. [3H] uptake is presented relative to vehicle treated WT ECM-plated KPC cells. IB analysis of iCol I and 3/4 Col I in ECM produced by indicated fibroblasts. c, Indicated KPC cells were plated on [3H]-proline-labelled ECM and incubated in LG for 24 h. [3H] uptake is presented relative to Paren. uptake. KD efficiency is demonstrated. d, KPC cells were plated on [3H]-proline-labelled ECM and incubated in LG −/+ indicated reagents for 24 h. [3H] uptake is presented as above. e, [3H] uptake by KC cells treated as above. f, AA content of ECM-plated KPC cells incubated in LG −/+ indicated reagents for 24 h. Cell number normalized data are presented relative to untreated WT ECM-plated cells. g, KC cells were plated −/+ WT or R/R ECM and incubated in complete (CM) or LG media −/+ indicated reagents for 24 h. Cellular ATP content is presented relative to untreated plastic-plated cells. h, KPC cells were plated as in (b) and incubated in LG −/+ EIPA for 24 h. Cellular ATP content is presented relative to untreated WT ECM-plated cells. i, Total AA in KC cells plated on ECM and incubated in LG −/+ indicated reagents for 24 h. Data are presented as above. j, Total AA in KPC cells treated as in (h). Results in (b,d–j) (n = 3 independent experiments), (c) (n = 4 independent experiments) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. **P < 0.01, ***P < 0.001, ****P < 0.0001. Exact P values in (b–j) are shown in Source Data.
Fig. 2. Col I cleavage controls PDAC metabolism.

a–c, Genes differentially expressed between KPC cells grown on wild-type or R/R ECM in LG (0.5 mM) medium for 24 h. Blue, replicates with low expression (z-score = −2); red, replicates with high expression (z-score = 2). Mitochondrial ETC genes (a), mitochondrial ribosome subunit genes (b) and macropinocytosis-related and NRF2-target genes (c). d,e, Fractional labelling (mole per cent enrichment) of TCA cycle intermediates (d) and intracellular amino acids (e) in KPC cells incubated for 24 h in LG medium after plating on [U-13C]-glutamine-labelled wild-type or R/R ECM. α-KG-, α-ketoglutarate. f, KPC cells plated on wild-type or R/R ECM or plastic were incubated in CM or LG medium with or without EIPA, MBQ-167 (MBQ), MRT68921 (MRT), EIPA + MRT or MBQ + MRT for 24 h. Total cellular ATP is presented relative to untreated plastic-plated cells. CM, complete medium. Data in d,e (n = 3 per condition) and f (n = 3 independent experiments) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. Exact P values are shown in the Source Data. ***P < 0.001; ****P < 0.0001.
To assess the effects of Col I on metabolism, we labelled wild-type and R/R fibroblasts with [3H]-proline or [U-13C]-glutamine for five days, during which period the cells coated the plates with Col I-containing ECM. After decellularization, KPC or KC cells and variants thereof were plated and cultured for 24 h in LG medium. The uptake of [3H] in cells plated on wild-type ECM was dependent on macropinocytosis, as indicated by sensitivity to macropinocytosis inhibitors (EIPA (an NHE1 inhibitor), IPI549 (a PI3Kγ inhibitor) or MBQ-167 (a CDC42 and RAC inhibitor)) and to the knockdown of NHE1 or SDC1, and enhancement by the ULK1 inhibitor MRT68921 (MRT)11. By contrast, cells plated on R/R ECM showed a negligible uptake of [3H] that was unaffected by the inhibition of macropinocytosis (Extended Data Fig. 2b–e). Notably, ablation of Col1a1 or overexpression of cleavable Col I in ECM-laying R/R fibroblasts restored [3H] uptake (Extended Data Fig. 2b). Cells that were cultured on 13C-glutamine-labelled wild-type ECM took up glutamine and metabolized it, but cells that were plated on 13C-glutamine-labelled R/R ECM exhibited minimal glutamine uptake and metabolism (Fig. 2d,e). Congruently, cells that were cultured on wild-type ECM had higher levels of ATP and a higher amino acid content than cells that were cultured on R/R ECM, and this effect was further increased by treatment with MRT and reduced by blockade of macropinocytosis; by contrast, cells that were cultured on R/R ECM had low levels of ATP and amino acids, which were barely affected by the inhibition of macropinocytosis (Fig. 2f and Extended Data Fig. 2f–j). Ablation of Col I or overexpression of wild-type Col I prevented the decline in ATP and amino acids (Extended Data Fig. 2h,j), suggesting that cCol I is a key signalling molecule that stimulates PDAC metabolism and energy generation.
cCol I to iCol I ratio controls DDR1–NRF2 signalling
KPC or human MIA PaCa-2 cells plated on wild-type ECM or co-cultured with wild-type fibroblasts in LG or low-glutamine (LQ) medium exhibited high rates of macropinocytosis, as measured by their uptake of tetramethylrhodamine-labelled high-molecular-mass dextran (TMR-DEX), whereas cells plated on R/R ECM or co-cultured with R/R fibroblasts exhibited low rates of macropinocytosis (Fig. 3a and Extended Data Fig. 3a). Furthermore, KPC cells cultured on wild-type ECM showed a marked upregulation of macropinocytosis-related proteins and NRF2 relative to plastic-cultured cells, but culturing on R/R ECM had the opposite effect (Fig. 3b). Similar differences in macropinocytosis activity, NRF2 and macropinocytosis-related mRNAs and proteins were shown by KPC tumours in Col IWT or Col Ir/r pancreata or livers (Extended Data Fig. 3b–d). Mitochondria are important for cancer growth in that they generate energy for macromolecular synthesis12. Consistent with the RNA-seq data, mitochondria and ETC proteins were decreased in PDAC cells grown on R/R ECM or in Col Ir/r pancreata (Fig. 3c,d and Extended Data Fig. 3e).
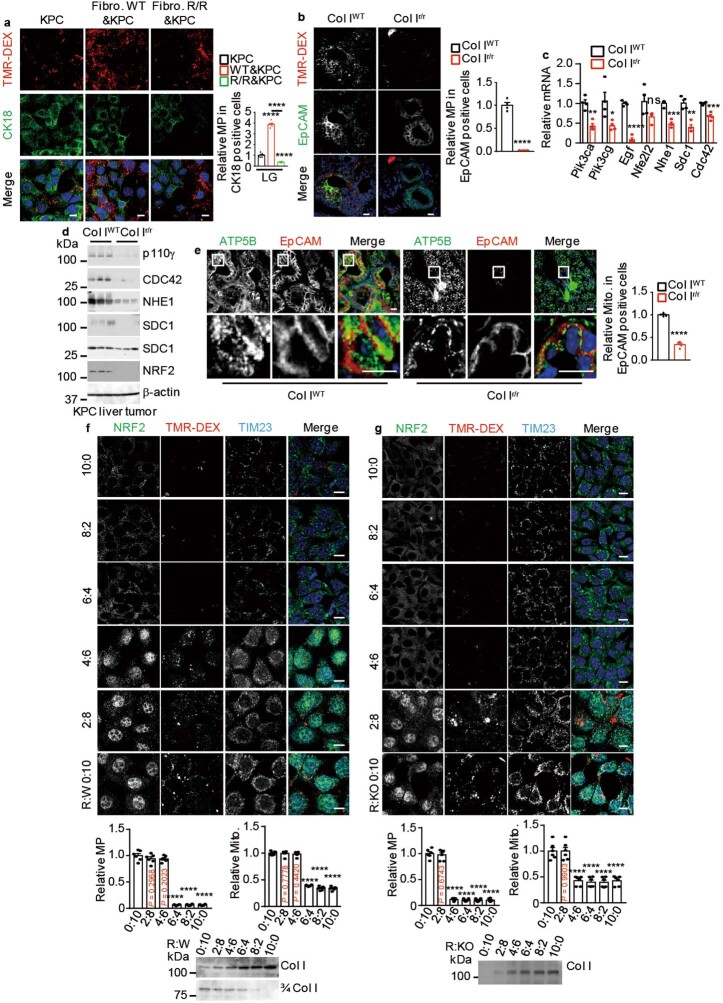
Fig. 3. Col I cleavage controls macropinocytosis and the number of mitochondria in PDAC.

a, Representative images and rates of macropinocytosis (MP) in TMR-DEX-incubated KPC and MIA PaCa-2 cells grown on plates with or without wild-type or R/R ECM and incubated in LQ or LG medium for 24 h. b, Immunoblot analysis of the indicated proteins in KPC cells treated as in a. c, Representative images of mitochondria (TIM23) in KPC cells grown on plates with or without wild-type or R/R ECM and incubated in LG medium for 24 h. Bottom left, quantification of the number of mitochondria. d, Immunoblot analysis of the indicated proteins in KPC cells treated as in c. Results in a,c (n = 6 fields) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. ****P < 0.0001. Scale bars (a,c), 10 μm.
Extended Data Fig. 3. The cleaved to intact Col I ratio controls macropinocytosis and mitochondrial biogenesis.
a, Macropinocytosis (MP) visualization and quantification using TMR-DEX in KPC cells co-cultured with WT or R/R fibroblasts and incubated in LG medium for 24 h. KPC cells were marked by cytokeratin 18 (CK18, green). b, Representative images, and MP quantification in TMR-DEX-injected pancreatic tissue from Col IWT or Col Ir/r mice 4 wk after orthotopic KPC cell transplantation. Carcinoma cells are marked by EpCAM staining (green). Quantification is on the right. c, qRT-PCR analysis of MP-related mRNAs in liver tumours 2 wk after i.s. KPC cell transplantation into CCl4 pretreated ColWT or Colr/r mice. Exact P values are shown in Source Data. d, IB analysis of MP-related proteins in above liver tumours. e, Representative images, and quantification of Mito. (ATP5B, green) in pancreatic tissue from indicated mice analysed as in (b). Carcinoma cells are marked by EpCAM staining (red). Quantification is on the right. f,g, Representative images, and quantification of Mito. (TIM23) and MP in TMR-DEX-incubated KPC cells grown on mixed ECM produced by R/R and WT (R:W) (f) or R/R and Col IΔ R/R (R:KO) (g) fibroblasts in the indicated ratios and incubated in LG medium for 24 h. IB analysis of iCol I or cCol I (3/4 Col I) in above ECM preparations is shown at the bottom. Results in (a,f,g) (n = 6 fields), (b,c,e) (n = 4 mice) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Scale bars, 10 μm.
The human PDAC stroma consists of intact and cleaved collagens. To recapitulate this setting and determine how the balance of iCol I to cCol I affects PDAC metabolism, we mixed R/R fibroblasts with wild-type (R:W) or Col IΔ (knockout) (R:KO) fibroblasts to generate ECM with different amounts of iCol I and cCol I, and confirmed this with isoform-specific antibodies. KPC cells were plated on the ECM preparations and kept in LG medium for 24 h, and their rates of macropinocytosis, numbers of mitochondria and levels of nuclear NRF2 were evaluated. Nondegradable Col I at 6:4 (R:W) or 4:6 (R:KO) ratios and higher ratios inhibited macropinocytosis and reduced mitochondria numbers and nuclear NRF2 (Extended Data Fig. 3f,g). We conclude that iCol I inhibits macropinocytosis and mitochondrial biogenesis, which are stimulated by different cleaved collagens, not just cCol I.
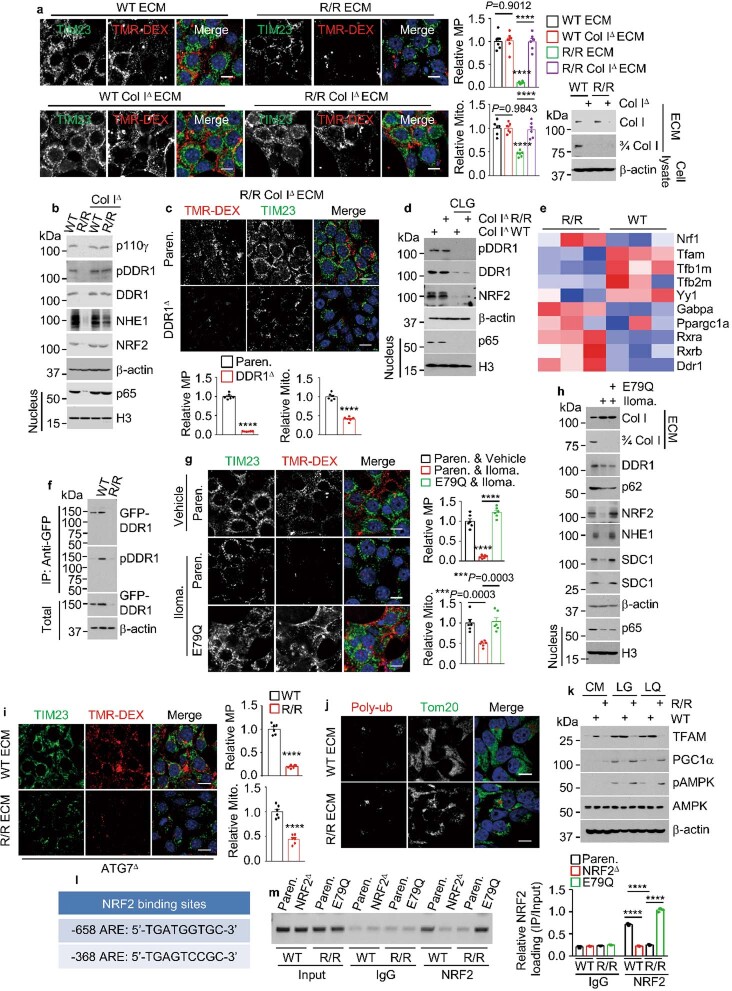
To investigate how Col I regulates macropinocytosis and mitochondrial biogenesis, we systematically ablated (Extended Data Fig. 4a) all known collagen receptors expressed by KPC cells—MRC2, DDR1, LAIR1 and β1 integrin (ITGB1). The only receptor whose ablation inhibited macropinocytosis activity and mitochondrial biogenesis (Fig. 4a) was DDR1, a collagen-activated receptor tyrosine kinase (RTK)13, which scRNA-seq showed was highly expressed in primary and liver-metastatic human PDAC epithelial-tumour cells, marked by the mRNA expression of EPCAM and KRT19 (Extended Data Fig. 4b). Other collagen receptor mRNAs were either not expressed in PDAC (LAIR1 and MRC2) or had a broad distribution (ITGB1). Whereas wild-type ECM stimulated the expression and phosphorylation of DDR1, R/R ECM strongly downregulated DDR1 and its downstream effector NF-κB14, as well as p62 (Fig. 4b), an NF-κB target15. The inhibitory effect of iCol I was not observed in previous DDR1 signalling studies, which used artificially fragmented acid-solubilized collagens as ligands16. Consistent with the induction of p62, wild-type ECM decreased KEAP1 and upregulated NRF2, whereas R/R collagen had the opposite effect (Fig. 4b). We wondered whether cCol I affects macropinocytosis and mitochondrial biogenesis through the DDR1–NF-κB–p62–NRF2 cascade. Indeed, R/R ECM and inhibition or ablation of NRF2, DDR1 or IKKβ decreased macropinocytosis activity, 3/4 Col I fragment uptake, NRF2 nuclear localization, mitochondria number and expression of macropinocytosis-related and mitochondrial ETC proteins (Fig. 4c,d and Extended Data Figs. 4c–g and 5a–e). Overexpression of an activated NRF2(E79Q) variant reversed the inhibitory effects of R/R ECM, DDR1 inhibition or IKKβ inhibition but did not restore or affect DDR1 expression or phosphorylation and p65 nuclear localization. Consistent with these data, pancreatic and liver tumours from Col Ir/r mice showed more-extensive expression of iCol I but no cCol I and lower levels of DDR1, p65, p62, NRF2, NHE1 and SDHB (a mitochondrial marker), as compared to tumours from Col IWT mice (Fig. 4e and Extended Data Fig. 5f,g). These results suggest that Col I controls macropinocytosis and mitochondrial biogenesis through the DDR1–NF-κB–p62–NRF2 axis. As myofibroblast-specific ablation of Col I enhances intrahepatic PDAC growth17, we examined how Col IΔ ECM affects macropinocytosis and DDR1 signalling. Notably, Col IΔ ECM behaved like wild-type ECM, stimulating macropinocytosis, mitochondrial biogenesis and DDR1 phosphorylation, which were blocked by the ablation of DDR1 (Extended Data Fig. 6a–c). However, collagen-free ECM generated by Col IΔ fibroblasts and treatment with bacterial collagenase no longer activated DDR1 and its downstream effectors (Extended Data Fig. 6d). These results are consistent with DDR1 being a general collagen receptor13, with other collagens in Col IΔ fibroblasts acting as ligands.
Extended Data Fig. 4. Col I controls macropinocytosis and mitochondrial content through DDR1–NRF2 signalling.
a, IB analysis of KPC cells ablated for indicated collagen receptors. b, UMAPs showing scRNA-seq data from 5 primary PDAC (upper row) and 1 PDAC liver metastasis (lower row), displaying the identified cell populations and expression of the indicated mRNAs. c, Representative images, and quantification of Mito. and MP in TMR-DEX-incubated Paren. and NRF2Δ (ΚΟ) KPC cells plated on WT or R/R ECM and incubated in LG for 24 h. NRF2 IB analysis is shown on the right. d, MP and NRF2 localization in Paren. and NRF2KD MIA cells plated −/+ WT or R/R ECM and incubated in LG for 24 h. MP quantification is shown on the right. e, 3/4 Col I and MP imaging and quantification in KPC cells treated as above. Although NRF2E79Q (E79Q) stimulates MP, cCol I uptake is detected only in cells plated on WT ECM. f, Representative images, and quantification of MP and nuclear NRF2 in 1305 cells plated on WT ECM and incubated in LG for 24 h. IB analysis of DDR1 and Flag-tagged E79Q is shown on the right. g, MP imaging and quantification in Paren. and E79Q MIA cells plated on WT or R/R ECM and incubated in LG for 24 h. Results in (c-g) (n = 6 fields) are mean ± s.e.m. Statistical significance was determined by two-tailed t-test. ****P < 0.0001. Scale bars, 10 μm.
Fig. 4. The Col I–DDR1–NRF2 axis controls macropinocytosis and mitochondrial biogenesis.
a, Representative images and quantification of mitochondria and macropinocytosis in TMR-DEX-incubated parental and variant KPC cells grown on wild-type ECM. b, Immunoblot analysis of the indicated proteins in KPC cells grown on plastic or wild-type or R/R ECM and incubated in LG or LQ medium for 24 h. The effects of wild-type and R/R ECM on DDR1 signalling are summarized on the right. mito., mitochondria; pDDR1, phosphorylated DDR1. c, Representative images and quantification of mitochondria and macropinocytosis in TMR-DEX-incubated parental and NRF2E79Q (E79Q) KPC cells plated on wild-type or R/R ECM in LG medium with or without 7rh or ML120B for 24 h. d, Immunoblot analysis of the indicated proteins in parental, E79Q, DDR1Δ and E79Q/DDR1Δ KPC cells plated with or without wild-type or R/R ECM and incubated in LG medium for 24 h. e, Representative IHC of the indicated proteins in Col IWT and Col Ir/r pancreata four weeks after KPC cell transplantation. Boxed areas are further magnified. Scale bars, 100 μm. f, Immunoblot analysis of the indicated proteins in KPC cells plated on wild-type or R/R ECM and incubated in LG medium with or without + MG132 or chloroquine (CQ) for 24 h. g, Representative images showing GFP–DDR1 and polyubiquitin (polyub) colocalization in GFP–DDR1-expressing 1305 cells co-cultured with wild-type or R/R fibroblasts in LG medium for 24 h. Boxed areas are further magnified. Data in a,c (n = 6 fields) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. Exact P values are shown in the Source Data. ****P < 0.0001; NS, not significant. Scale bars (a,c,g), 10 μm.
Extended Data Fig. 5. cCol I–DDR1–NRF2 signalling controls macropinocytosis and mitochondrial protein expression.
a, IB analysis of ETC complexes I-V (CI-CV) in Paren. and E79Q KPC cells plated on WT or R/R ECM and incubated in LG for 24 h. b, IB analysis of indicated KPC cells −/+ ectopic p62 or E79Q plated on WT ECM and incubated in LG for 24 h. c, IB of ETC proteins in Paren., DDR1Δ, or E79Q/DDR1Δ KPC cells plated on WT ECM and incubated in LG for 24 h. d,e, IB of indicated proteins in Paren. or E79Q KPC cells plated on WT ECM and incubated in LG medium −/+ML120B for 24 h. f, Staining intensity of the indicated proteins in tumour areas depicted Fig. 4e determined with Image J. g, IHC of liver sections prepared 2 wk after i.s. transplantation of KPC cells into CCl4 pretreated Col IWT and Col Ir/r mice. Scale bars, 100 μm. Image J determined staining intensity of indicated proteins in tumour areas is shown at the bottom. Results in (f,g) (n = 6 fields) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. ****P < 0.0001.
Extended Data Fig. 6. Inhibition of Col I cleavage shuts down NRF2-driven macropinocytosis and mitochondrial biogenesis.
a, MP and mitochondria in KPC cells plated on indicated ECM and incubated in LG for 24 h. Col I IB in indicated ECM preparations is shown on the right. b, IB of indicated proteins in above cells. c, MP and mitochondria in indicated KPC cells plated on R/R Col IΔ ECM and incubated in LG for 24 h. d, IB of indicated proteins in 1305 cells plated on ECM produced by bacterial collagenase (CLG, 50 μg/ml) treated or untreated fibroblasts and incubated in LG medium −/+ CLG for 24 h. e, Genes differentially expressed between KPC cells plated on indicated ECM. Blue: replicates with low expression (z-score = −2); red: replicates with high expression (z-score = +2). f, Immunoprecipitation (IP) of GFP–DDR1 from 1305 cells plated −/+ indicated ECM. g, MP and mitochondria in Paren. or E79Q KPC cells plated on ECM produced by Ilomastat (Iloma.) treated or untreated WT fibroblasts and incubated in LG medium −/+ Iloma. for 24 h. h, IB of indicated proteins in above cells. i, MP and mitochondria in ATG7Δ MIA PaCa-2 cells plated on indicated ECM and incubated in LG for 24 h. j, Imaging of 1305 cells plated on indicated ECM showing rare poly-Ub and Mito. (Tom20) colocalization. k, IB analysis of KPC cells plated −/+ indicated ECM and incubated in indicated media for 24 h. l, Locations of putative NRF2-binding sites (AREs) relative to the transcriptional start site (TSS, +1) of the mouse Tfam gene. m, Chromatin IP probing NRF2 recruitment to the Tfam promoter in KPC cells plated on WT or R/R ECM and incubated in LG for 24 h. The image shows PCR-amplified ARE-containing promoter DNA fragments. Quantitation on the right. Results in (a,c,g,i) (n = 6 fields), (m) (n = 3 independent experiments) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. ***P < 0.001, ****P < 0.0001. Scale bars, 10 μm.
iCol I triggers DDR1 proteasomal degradation
The expression and function of DDR1 vary in different cancer stages and types18–21. Levels of mouse Ddr1 mRNA were increased by culturing KPC cells on R/R ECM (Extended Data Fig. 6e), implying that the diminished expression of DDR1 protein in these cultures is post-transcriptional. Indeed, MG132, a proteasome inhibitor, but not the lysosomal inhibitor chloroquine, rescued DDR1 expression but not autophosphorylation (Fig. 4f). Notably, GFP–DDR1 showed cell-surface localization and little polyubiquitin colocalization in human 1305 cells that were co-cultured with wild-type fibroblasts, but was cytoplasmic and colocalized with polyubiquitin in R/R fibroblast cocultures (Fig. 4g). Unlike DDR1 in triple-negative breast cancer (TNBC)20, no shedding of the DDR1 extracellular domain was detected (Extended Data Fig. 6f). Our results therefore reveal a new mode of DDR1 regulation in PDAC and probably in other desmoplastic cancers.
NRF2 controls mitochondrial biogenesis
ECM from fibroblasts treated with the FDA-approved MMP inhibitor Ilomastat behaved like R/R ECM (Extended Data Fig. 6g,h), indicating that the results were not unique to the Col IR variant. R/R ECM also decreased the number of mitochondria in autophagy-deficient PDAC cells (Extended Data Fig. 6i), which suggests that the reduced mitochondrial content is not mediated by mitophagy. Moreover, colocalization of mitochondria and polyubiquitin, which marks mitophagy, was rarely observed (Extended Data Fig. 6j). Expression of TFAM, a key activator of mitochondrial DNA transcription, replication and biogenesis22, was downregulated in PDAC cells cultured in R/R ECM, but Nrf1 (unrelated to NRF2) mRNA, PGC1α protein and AMPK activity, which also stimulate mitochondrial biogenesis23, were upregulated (Extended Data Fig. 6e,k). The latter results match the low ATP content of R/R-ECM-cultured cells. In silico analysis revealed putative NRF2-binding sites in the Tfam promoter region, to which NRF2 was recruited in cells plated on wild-type ECM or in NRF2(E79Q)-expressing cells (Extended Data Fig. 6l,m), confirming that NRF2 mediates cCol I-stimulated macropinocytosis and mitochondrial biogenesis.
Higher levels of iCol I correlate with improved survival
Immunohistochemistry (IHC) of surgically resected human PDAC showed that most tumours (77/106) contained high amounts of 3/4 Col I and most of them exhibited higher levels of staining for DDR1 (58/77), NF-κB p65 (55/77), NRF2 (60/77), SDC1 (53/77), CDC42 (52/77), SDHB (62/77), α-SMA (56/77) and MMP1 (52/77) than did cCol Ilow tumours (Fig. 5a and Extended Data Fig. 7a,b), suggesting that PDAC tumours with fibrolytic stroma have higher macropinocytosis activity and mitochondrial content than do tumours with inert stroma. Moreover, DDR1 and p65, DDR1 and NRF2, p65 and NRF2, NRF2 and macropinocytosis proteins (NHE1, SDC1 or CDC42), and NRF2 and SDHB showed strong positive correlations (Extended Data Fig. 7b), suggesting that the fibrolytic stroma stimulates macropinocytosis and mitochondrial biogenesis through the DDR1–NF-κB–NRF2 axis in human PDAC. Increased levels of cCol I also correlated with high expression of inflammatory markers (Extended Data Fig. 7c), supporting the notion that inflammation may drive Col I remodelling. Notably, patients with cCol Ihigh and DDR1high, cCol Ihigh and NRF2high or DDR1high and NRF2high tumours had a considerably worse median survival than did patients with low expression of these markers (Fig. 5b). These results are consistent with those obtained in our preclinical PDAC models, suggesting that the fibrolytic stroma may drive the recurrence of human PDAC through NRF2-mediated macropinocytosis and mitochondrial biogenesis.
Fig. 5. Col I cleavage and increased DDR1–NRF2 signalling predict poor patient survival.

a, Representative IHC of 106 resected human PDAC tissues. H&E, haematoxylin and eosin. Boxed areas are further magnified. Scale bars, 100 μm. b, Comparisons of overall survival between patients stratified according to cCol I, DDR1 and NRF2 expression. Significance was determined by log-rank test.
Extended Data Fig. 7. Correlation between Col I–DDR1–NRF2 signalling components and inflammation in human PDAC.

a, Numbers and percentages of human PDAC specimens (n = 106 specimens) positive for the indicated proteins (arbitrarily indicated as low and high). b, Correlation between indicated proteins in above specimens was analysed by a two-tailed Chi-square test. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. cCol I (3/4 Col I). c, Representative IHC and quantification of the indicated markers in cCol Ihigh (#43) and cCol Ilow (#54) human PDAC specimens from Fig. 5a. Mean ± s.e.m. (n = 16 specimens). Statistical significance determined by two-tailed t-test. ***P = 0.0001. *P = 0.0145, *P = 0.0388. Scale bars, 100 μm.
Targeting the DDR1–NF-κB–NRF2 cascade
Increasing iCol I in the ECM inhibited cellular DNA synthesis (Extended Data Fig. 8a). Parental, NRF2E79Q or IKKα-knockdown (IKKαKD) PDAC cells were plated on wild-type or R/R ECM, incubated in LG medium and treated with inhibitors of DDR1 (7rh), IKKβ (ML120B), NRF2 (ML385) or macropinocytosis (NHE1KD or EIPA, IPI549 or MBQ-167). Whereas wild-type ECM increased and R/R ECM decreased parental PDAC cell growth, inhibition of macropinocytosis, DDR1, IKKβ or NRF2 decreased growth on wild-type ECM (Fig. 6a and Extended Data Fig. 8b–f). NRF2(E79Q)-expressing cells grew faster than parental cells and were resistant to R/R ECM, DDR1 inhibition or IKKβ inhibition but not NRF2 inhibition. IKKαKD cells with high rates of macropinocytosis and high levels of nuclear NRF2 also grew faster than parental cells on wild-type ECM but were more sensitive to R/R ECM and macropinocytosis inhibitors (Extended Data Fig. 8b,c). Inhibition of macropinocytosis, DDR1, IKKβ or NRF2 did not decrease the low growth of parental cells on R/R ECM (Fig. 6a and Extended Data Fig. 8b–f). Moreover, parental KPC or 1305 cells that were plated on wild-type ECM were more sensitive to the mitochondrial protein synthesis inhibitor tigecycline than cells plated on R/R ECM or DDR1KD cells grown on wild-type ECM (Extended Data Fig. 8g). NRF2E79Q cells showed higher rates of oxygen consumption and mitochondrial ATP production than did parental cells; these rates were diminished by R/R ECM but only in the parental cells (Fig. 6b and Extended Data Fig. 8h). Thus, the fibrolytic stroma may support PDAC cell growth through Col I-stimulated macropinocytosis and mitochondrial biogenesis. R/R fibroblasts inhibited human PDAC (MIA PaCa-2) tumour growth, but wild-type fibroblasts were stimulatory. NHE1 ablation or EIPA inhibited tumour growth with or without co-transplanted wild-type fibroblasts or in wild-type livers, but had little effect on tumours growing with R/R fibroblasts or in Col Ir/r livers (Fig. 6c and Extended Data Fig. 8i). Tumours growing with wild-type fibroblasts were more fibrotic than tumours without added fibroblasts, and small tumours growing with R/R fibroblasts had the highest collagen content (Extended Data Fig. 8j), indicating that deposition of Col I enhances the growth of PDAC only when Col I is cleaved by MMPs. NRF2E79Q cells in Col Ir/r hosts exhibited similar growth, NRF2, NHE1 and SDHB expression and liver metastases to cells growing in Col IWT hosts, despite low expression of DDR1 and p65 (Fig. 6d–f and Extended Data Fig. 9a).
Extended Data Fig. 8. Effect of macropinocytosis and mitochondria on Col I-controlled PDAC cell growth.
a, Bromodeoxyuridine (BrdU) incorporation into KPC cells plated on ECM mixtures produced by R/R and WT fibroblasts (R:W). Scale bars, 10 μm. b,c, Paren. and IKKαKD KPC (b) or KC (c) cells were plated −/+ WT or R/R ECM and incubated in LG −/+ indicated reagents. Viable cells were measured after 3 days and depicted relative to untreated plastic-plated Paren. cells. (c). IKKα KD efficiency is shown on the right (b). d,e, Viable 1305 (d) or MIA PaCa-2 (e) cells plated as above and incubated in LG −/+ EIPA. f, Viable Paren. and E79Q KPC cells plated, treated, and presented as above. g, Paren. and DDR1KD 1305 or KPC cells plated on indicated ECM preparations and incubated in LG medium −/+ indicated tigecycline concentrations for 24 h. Total viable cells were measured as above and are presented relative to the untreated cells. h, Mitochondrial ATP production calculated from Fig. 6b. i, Liver morphology and tumour numbers (#) 2 wk after i.s. transplantation of Paren. or NHE1KD KPC cells into CCl4-pretreated Col IWT and Col Ir/r mice −/+ EIPA. NHE1 IB is shown on bottom left. ****P < 0.0001. j, H&E and SR staining of s.c. tumours from Fig. 6c. Quantification of the SR positive area is shown on the left. Scale bars, 100 µm. Results in (a) (n = 6 fields), (b–g) (n = 3 independent experiments), (h) (n = 3 per condition), (j) (n = 5 mice) and (i) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. Exact P values in (a−c,f,h) are shown in Source Data.
Fig. 6. Therapeutic targeting of the DDR1–NF-κB–NRF2 axis inhibits PDAC growth and metabolism.
a, Parental and E79Q KPC cells plated on wild-type or R/R ECM were incubated in LG medium with or without 7rh, ML120B or ML385. Total viable cells are presented relative to parental cells that were treated with vehicle and plated on wild-type ECM. b, Oxygen consumption rate (OCR) of parental and E79Q KPC cells plated on wild-type or R/R ECM and incubated in LG medium for 24 h before and after treatment with oligomycin (Omy), FCCP or rotenone/antimycin A. c, Representative images and sizes of parental and NHE1KD MIA tumours grown with or without wild-type or R/R fibroblasts in nude mice. Right, immunoblot analysis of NHE1 in MIA cells. d,e, Liver and pancreas morphology (d) and weight (e) four weeks after orthotopic transplantation of KPC E79Q cells into CAE-pretreated Col IWT and Col Ir/r mice. f, IHC of pancreatic sections from the mice in d,e. Boxed areas are further magnified. Scale bars, 100 μm. g, P/B weight four weeks after orthotopic transplantation of the indicated KPC cells into Col IWT and Col Ir/r mice pretreated with or without CAE. Right, immunoblot analysis of DDR1 and Flag-tagged E79Q in the indicated KPC cells plated on wild-type ECM in LG medium for 24 h. h, Representative images and sizes of MIA tumours grown with wild-type or R/R fibroblasts in nude mice with or without ML120B or tigecycline. Data in a (n = 3 independent experiments), c,g,h (n = 5 mice) and e (n = 9 mice) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. ***P < 0.001, ****P < 0.0001; NS, not significant. Exact P values in a,c,g are shown in the Source Data. Scale bars (c,d,h), 1 cm.
Extended Data Fig. 9. The cCol I–DDR1–NRF2 axis controls PDAC growth but not collagen fibre alignment.
a, H&E, SR and cytokeratin 19 (CK19) and SOX9 staining of pancreatic and liver sections from CAE-pretreated Col IWT and Col Ir/r mice 4 wk after orthotopic KPC NRF2E79Q cell transplantation. Scale bars, 100 µm. b, Tumours formed by orthotopically transplanted Paren. or DDR1KD KPC cells in Col IWT and Col Ir/r mice analysed by SHG and collagen fibre individualization. BF-bright field. c, IHC of indicated markers in pancreatic sections of Col IWT and Col Ir/r mice orthotopically transplanted with KPC cells. Quantification of staining positivity in tumour areas is shown below. Left to right: ****P < 0.0001, **P = 0.0013, P = 0.5351. d, Pancreas morphology 4 wk after orthotopic transplantation of Paren., DDR1KD, E79Q/DDR1KD KPC cells into Col IWT and Col Ir/r mice pretreated −/+ CAE. Scale bars, 1 cm. e, H&E staining and IHC analysis of pancreatic sections from above mice. Quantification of tumour area by Image J is shown below. Left to right: ****P < 0.0001, P = 0.5748, P = 0.3606. Results in (c,e) (n = 5 fields) are mean ± s.e.m. Statistical significance determined by two-tailed t-test. Scale bars, 100 µm.
In TNBC, DDR1 aligns collagen fibres to exclude immune cells20. By measuring second-harmonic generation (SHG), we observed no change in collagen fibre alignment and CD8+ T cell content between tumours from Col IWT and Col Ir/r pancreata or between parental and DDR1KD tumours, although CD45-, F4/80- or CD4-expressing cells were reduced in tumours from Col Ir/r pancreata (Extended Data Fig. 9b,c). Accordingly, ablation of DDR1 inhibited tumour growth, p65, p62, NRF2, NHE1 and SDHB expression in Col IWT pancreata but did not reduce it further in Col Ir/r pancreata (Fig. 6g and Extended Data Figs. 9d,e and 10a). NRF2(E79Q) rescued tumour growth and the expression of NHE1 and SDHB—but not p65 or p62—in DDR1KD cells, regardless of Col I status. Similar results were observed in immunodeficient mice (Extended Data Fig. 10b), indicating that the effects of Col I–DDR1 interaction differ between PDAC and TNBC. Notably, inhibition of IKKβ, mitochondrial protein synthesis, TFAM or NRF2 decreased the growth of tumours that were co-transplanted with wild-type fibroblasts or grown in Col IWT pancreata, but had no effect on tumours that were co-transplanted with R/R fibroblasts or grown in Col Ir/r pancreata (Fig. 6h and Extended Data Fig. 10c,d), illustrating different ways of targeting PDAC with fibrolytic stroma.
Extended Data Fig. 10. cCol I stimulates PDAC growth, macropinocytosis and mitochondrial biogenesis through the DDR1–NRF2 axis.
a, IHC of pancreatic sections of CAE-pretreated Col IWT or Col Ir/r mice 4 wk after orthotopic transplantation of Paren., DDR1KD and E79Q/DDR1KD KPC cells. Boxed areas were further magnified. Scale bars, 100 µm. b, Representative images and sizes of s.c. tumours generated by Paren., DDR1KD (KD) and E79Q/KD 1305 cells transplanted −/+ WT or R/R fibroblasts into Nu/Nu mice. Scale bars, 1 cm. c, Pancreas weight relative to body weight (P/B) of Col IWT or Col Ir/r mice 4 wk after orthotopic transplantation of Paren., NRF2KD and TFAMKD KPC cells. NRF2 and TFAM KD efficiency is shown below. d, H&E staining and CK19 IHC of above pancreata. Image J quantification of tumour area is shown on the left. Scale bars, 100 µm. Results in (b,c) (n = 5 mice), (d) (n = 5 fields) are mean ± s.e.m. Statistical significance was determined by a two-tailed t-test. ****P < 0.0001.
Discussion
We show here that Col I remodelling is a prognostic indicator for the survival of patients with PDAC. In preclinical models, Col I remodelling modulated tumour growth and metabolism through a DDR1–NF-κB–p62–NRF2 cascade that is activated by cCol I and inhibited by iCol I. The activation of DDR1 by collagens and downstream activation of NF-κB have been described before14,16. However, it was previously unknown—to our knowledge—that iCol I triggers the polyubiquitylation and proteasomal degradation of DDR1. This indicates that DDR1 distinguishes cleaved from intact collagens, and that the latter are capable of restraining the metabolism and growth of tumours. Although inhibition of DDR1 reduces the growth of mouse PDAC24, the ability of DDR1 to control tumour metabolism by stimulating macropinocytosis and mitochondrial biogenesis was unknown. It is unclear, however, why DDR1—a rather weak RTK13—exerts such profound metabolic effects on PDAC cells that express more potent RTKs, such as EGFR and MET. Perhaps this is due to high concentrations of cCol I in the PDAC tumour microenvironment and the stronger NF-κB-activating capacity of DDR1 relative to other RTKs. Indeed, IKKβ inhibition was as effective as the blockade of mitochondrial protein synthesis in curtailing the growth of PDAC with fibrolytic stroma. The differential effects of fibrolytic and inert tumour stroma on PDAC growth and metabolism explain much of the controversy that surrounds the effects of CAFs and Col I on the progression of PDAC in mice6,17. Most notably, our findings extend to humans and suggest that Col I remodelling is linked to tumour inflammation. We thus propose that treatments that target DDR1–IKKβ–NF-κB–NRF2 signalling and mitochondrial biogenesis should be evaluated in prospective clinical trials that include stromal state—an important modifier of tumour growth—as an integral biomarker. Given that three Col I-cleaving MMPs were highly expressed in the human PDAC samples we analysed, and that this situation may differ from patient to patient25, specific MMP inhibitors are additional candidates for precision therapy. A deeper understanding of whether stromal state is affected by neoadjuvant chemotherapy and how it affects metastasis is another area of priority for further investigation. Although our results do not apply to TNBC, they provide mechanistic insight into SPARC-mediated PDAC progression26, 27, and may be applicable to other desmoplastic and fibrolytic cancers.
Methods
Cell culture
All cells were incubated at 37 °C in a humidified chamber with 5% CO2. MIA PaCa-2 (MIA), UN-KPC-960 (KPC) and UN-KC-6141 (KC) cells, wild-type and R/R fibroblasts were maintained in Dulbecco’s modified Eagle’ s medium (DMEM) (Invitrogen) supplemented with 10% fetal bovine serum (FBS) (Gibco). MIA cells were purchased from ATCC. KPC and KC cells were generated at the laboratory of S. K. Batra28. Wild-type and R/R fibroblasts were generated at the laboratory of D.B.10. The 1305 primary human PDAC cells were generated by the A.M.L. laboratory from a human PDAC patient-derived xenograft11 and were maintained in RPMI (Gibco) supplemented with 20% FBS and 1 mM sodium pyruvate (Corning). All media were supplemented with penicillin (100 mg ml−1) and streptomycin (100 mg ml−1). All cells were partially authenticated by visual morphology. Wild-type and R/R fibroblasts were partially authenticated by ECM production and collagen type I alpha 1 cleavage. KPC and KC cells were partially authenticated by orthotopic tumour formation in mouse pancreas. MIA and 1305 cells were partially authenticated by subcutaneous tumour formation in nude mice. Cells were not further authenticated. Cell lines were tested for mycoplasma contamination. LG medium: glucose-free DMEM medium was supplemented with 0.5 mM glucose in the presence of 10% dialysed FBS and 25 mM HEPES. LQ medium: glutamine-free DMEM medium was supplemented with 0.2 mM glutamine in the presence of 10% dialysed FBS and 25 mM HEPES.
Plasmids
For gene ablations, the target cDNA sequences (Supplementary Table 1) of mouse Ddr1, Mrc2, Itgb1, Lair1, Nrf2, Col1a1 and human DDR1 were cloned into a lentiCRISPR v2-Blast vector or lentiCRISPR v2-puro vector, respectively using BsmBI. For gene knockdowns, pLKO.1-puro-Ddr1 (TRCN0000023369), pLKO.1-puro-DDR1 (TRCN0000121163), pLKO.1-puro-Sdc1 (TRCN0000302270), pLKO.1-puro-Nrf2 (TRCN0000054658) and pLKO.1-puro-Tfam (TRCN0000086064) were ordered from Sigma. pCDH-CMV-MCS-EF1-puro-Col1α1-6XHis and pLVX-IRES-Puro-NRF2E79Q-Flag were made by Sangon Biotech (Shanghai, China). pLKO.1-blast-Ikkα, pLKO.1-puro-Nhe1, pLKO.1-puro-NHE1, pLKO.1-puro-NRF2, and lentiCRISPR v2-Puro-p62/Sqstm1 have been described previously11. LentiCRISPR v2-Blast-ATG7 (ref. 29) was a gift from S. Ghaemmaghami.
Stable cell line construction
Lentiviral particles were generated as before30. MIA, 1305, KPC or KC cells and fibroblasts were transduced by combining 1 ml of viral particle-containing medium with 8 μg ml−1 polybrene. The cells were fed 8 h later with fresh medium and selection was initiated 48 h after transduction using 1.25 μg ml−1 puromycin or 10 μg ml−1 blasticidin. IKKαKD KC, NRF2KD MIA and ATG7Δ MIA cells have been described previously11.
Mice
Female homozygous Nu/Nu nude mice and C57BL/6 mice were obtained at six weeks of age from Charles River Laboratories and The Jackson Laboratory, respectively. Col1a1+/+ (Col IWT) or Col1a1r/r (Col Ir/r) mice on a C57BL/6 background were obtained from D.B. at UCSD and were previously described8,31. Mice matched for age, gender and equal average tumour volumes were randomly allocated to different experimental groups on the basis of their genotypes. No sample size pre-estimation was performed but as many mice per group as possible were used to minimize type Ι/II errors. Both male and female mice were used unless otherwise stated. Blinding of mice was not performed except for IHC analysis. All mice were maintained in filter-topped cages on autoclaved food and water at constant temperature and humidity and in a pathogen-free controlled environment (23 °C ± 2 °C, 50–60%) with a standard 12-h light–12-h dark cycle. Experiments were performed in accordance with UCSD Institutional Animal Care and Use Committee and NIH guidelines and regulations. Animal protocol S00218 (M.K.) was approved by the UCSD Institutional Animal Care and Use Committee. The number of mice per experiment is indicated in the figure legends and their age is indicated in Methods.
Orthotopic PDAC cell implantation
Col IWT or Col Ir/r mice were pretreated with or without 50 μg kg−1 CAE by intraperitoneal injections every hour, six times daily on the first, fourth and seventh days. On day 11, parental, NRF2E79Q, DDR1KD, DDR1KD + NRF2E79Q, NRF2KD or TFAMKD KPC or KC cells were orthotopically injected into three-month-old Col IWT or Col Ir/r mice as described11. After surgery, mice were given buprenorphine subcutaneously at a dose of 0.05–0.1 mg kg−1 every 4–6 h for 12 h and then every 6–8 h for 3 additional days. Mice were analysed after four weeks.
Intrasplenic PDAC cell implantation
Three-month-old Col IWT or Col Ir/r mice were treated with or without an oral gavage of 25% CCl4 in corn oil twice a week for two weeks. After two weeks of recovery, parental, NHE1KD or IKKαKD KPC or KC cells (106 cells in 50 μl phosphate-buffered saline; PBS) were adoptively transferred into the livers of Col IWT or Col Ir/r mice by intrasplenic injection, followed by immediate splenectomy10. Mice were analysed 14 days after treatment with or without 10 mg kg−1 EIPA (Sigma) by intraperitoneal injection every other day.
Subcutaneous PDAC cell implantation
Homozygous BALB/c Nu/Nu female mice were injected subcutaneously in a single flank or in both flanks at 7 weeks of age with 5 × 105 parental, NHE1KD, DDR1KD or DDR1KD + NRF2E79Q MIA cells or 1305 cells mixed with or without 5 × 105 wild-type, R/R, Col IΔ wild-type or Col IΔ R/R fibroblasts diluted 1:1 with BD Matrigel (BD Biosciences) in a total volume of 100 μl. Tumours were collected after four weeks. To evaluate the effect of IKKβ or mitochondrial protein synthesis inhibition on tumour growth, mice were treated with vehicle (dimethyl sulfoxide in PBS), ML120B (60 mg kg−1) twice daily through oral gavage or tigecycline (50 mg kg−1) twice daily through intraperitoneal injection for three weeks. Therapy was started one week after tumour implantation. Volumes (1/2 × (width2 × length)) of subcutaneous tumours were calculated on the basis of digital caliper measurements. Mice were euthanized to avoid discomfort if the tumour diameter reached 2 cm.
Samples of human PDAC
Survival analysis of patients expressing high and low levels of Col I–MMP was performed using The Cancer Genome Atlas (TCGA) data and the GEPIA2 platform. The collagen-cleaving signature consisted of MMP1, MMP2, MMP8, MMP9, MMP13 and MMP14. Overall survival was determined in the TCGA cohort of 178 patients with PDAC using a median cut-off.
A total of 106 specimens of human PDAC were acquired from patients who were diagnosed with PDAC between January 2017 and May 2021 at The Affiliated Drum Tower Hospital of Nanjing University Medical School. All patients received standard surgical resection and did not receive chemotherapy before surgery. Paraffin-embedded tissues were processed by a pathologist after surgical resection and confirmed as PDAC before further investigation. Overall survival duration was defined as the time from the date of diagnosis to that of death or last known follow-up examination. Survival information was available for 81 of the 106 patients. The study was approved by the Institutional Ethics Committee of The Affiliated Drum Tower Hospital with IRB 2021-608-01. Informed consent for tissue analysis was obtained before surgery. All research was performed in compliance with government policies and the Helsinki declaration.
IHC
Pancreata or liver were dissected and fixed in 4% paraformaldehyde in PBS and embedded in paraffin. Five-micrometre sections were prepared and stained with H&E or sirius red. IHC was performed as before11. Slides were photographed on an upright light/fluorescent Imager A2 microscope with AxioVision Rel. 4.5 software (Zeiss). Antibody information is shown in Supplementary Table 2.
IHC scoring
IHC scoring was performed as before11. Negative and weak staining was viewed as a low expression level and intermediate and strong staining was viewed as a high expression level. For cases with tumours with two satisfactory cores, the results were averaged; for cases with tumours with one poor-quality core, results were based on the interpretable core. On the basis of this evaluation system, a chi-squared test was used to estimate the association between the staining intensities of Col I–DDR1–NRF2 signalling proteins. The number of evaluated cases for each different staining in PDAC tissues and the scoring summary are indicated in Extended Data Fig. 7a.
ECM preparation
Wild-type or R/R fibroblasts were seeded on 6, 12 or 96-well plates. One day after plating, cells were switched into DMEM (with pyruvate) with 10% dialysed FBS supplemented with or without 500 μM [3H]-proline or [U-13C]-glutamine and 100 μM vitamin C. Cells were cultured for five days with renewal of the medium every 24 h. Then fibroblasts were removed by washing in 1 ml or 500 μl or 100 μl per well PBS with 0.5% (v/v) Triton X-100 and 20 mM NH4OH. The ECM was washed five times with PBS before cancer cell plating. The following day, cancer cells were switched into the indicated medium for 24 or 72 h.
Cell imaging
Cells were cultured on coverslips coated with or without ECM and fixed in 4% paraformaldehyde for 10 min at room temperature or methanol for 10 min at −20 °C. Macropinosome visualization in cell and tissue and immunostaining were performed as previously described11. Images were captured and analysed using a TCS SPE Leica confocal microscope with Leica Application Suite AF 2.6.0.7266 software (Leica). Antibody information is shown in Supplementary Table 2.
SHG
Mouse pancreatic tumour tissue was fixed in 4% paraformaldehyde in PBS and embedded in paraffin. Five-micrometre sections were prepared and deparaffinized in xylene, rehydrated in graded ethanol series as described32, mounted using an aqueous mounting medium and sealed with a coverslip. All samples were imaged using a Leica TCS SP5 multiphoton confocal microscope and an HC APO LC 20× 1.00W was used throughout the experiment. The excitation wavelength was tuned to 840 nm, and a 420 ± 5-nm narrow bandpass emission controlled by a prism was used for detecting the SHG signal of collagen. SHG signal is generated when two photons of incident light interact with the non-centrosymmetric structure of collagen fibres, which leads to the resulting photons being half the wavelength of the incident photons. SHG measurements were performed using CT-Fire software (v.2.0 beta) (https://loci.wisc.edu/software/ctfire). The tumour area was confirmed by H&E staining.
Immunoblotting and immunoprecipitation
Preparation of protein samples from cells and tissues, immunoblotting and immunoprecipitation were performed as before10,30. Immunoreactive bands were detected by an automatic X-ray film processor or a KwikQuant Imager. Antibody information is shown in Supplementary Table 2.
Chromatin immunoprecipitation
Cells were cross-linked with 1% formaldehyde for 10 min and the reaction was stopped with 0.125 M glycine for 5 min. The chromatin immunoprecipitation assay was performed as described11. Cells were lysed and sonicated on ice to generate DNA fragments with an average length of 200–800 bp. After pre-clearing, 1% of each sample was saved as the input fraction. Immunoprecipitation was performed using antibodies that specifically recognize NRF2 (CST, 12721). DNA was eluted and purified from complexes, followed by PCR amplification of the target promoters or genomic loci using primers for mouse Tfam: 5′-GAGGCAGGGTCTCATG-3′ and 5′-CAAGCTGAGTTCTATC-3′; 5′- TCTGGGCCATCTTGGG-3′ and 5′- CCATGGGCCTGGGCTG-3′.
Quantitative PCR analysis
Total RNA and DNA were extracted using the All Prep DNA/RNA Mini Kit (Qiagen). RNA was reverse-transcribed using a Superscript VILO cDNA synthesis kit (Invitrogen). Quantitative (q)PCR was performed as described11. Primers obtained from the NIH Primer-BLAST (https://www.ncbi.nlm.nih.gov/tools/primer-blast/index.cgi?LINK_LOC=BlastHome) are shown in Supplementary Table 3.
RNA-seq library preparation, processing and analysis
Total RNA was isolated as described above from KPC samples grown on wild-type (n = 3) or R/R (n = 3) ECM as indicated. RNA purity was assessed by an Agilent 2100 Bioanalyzer. Five hundred nanograms of total RNA was enriched for poly-A-tailed RNA transcripts by double incubation with Oligo d(T) Magnetic Beads (NEB, S1419S) and fragmented for 9 min at 94 °C in 2× Superscript III first-strand buffer containing 10 mM DTT (Invitrogen, P2325). The reverse-transcription reaction was performed at 25 °C for 10 min followed by 50 °C for 50 min. The reverse-transcription product was purified with RNAClean XP (Beckman Coulter, A63987). Libraries were ligated with dual unique dual index (UDI) (IDT) or single UDI (Bioo Scientific), PCR-amplified for 11–13 cycles, size-selected using one-sided 0.8× AMPure clean-up beads, quantified using the Qubit dsDNA HS Assay Kit (Thermo Fisher Scientific) and sequenced on a HiSeq 4000 or NextSeq 500 (Illumina).
RNA-seq reads were aligned to the mouse genome (GRCm38/mm10) using STAR. Biological and technical replicates were used in all experiments. Quantification of transcripts was performed using HOMER (v.4.11). Principal component analysis (PCA) was obtained on the basis of transcripts per kilobase million (TPM) on all genes from all samples. Expression value for each transcript was calculated using the analyzeRepeats.pl tool of HOMER. Differential expression analysis was calculated using getDiffExpression.pl tool of HOMER. Pathway analyses were performed using the Molecular Signature Database of GSEA.
scRNA-seq analysis
Samples from five primary tumours from patients with PDAC and one PDAC liver metastasis were obtained33 and analysed separately to better identify cell heterogeneity and clusters. The datasets were processed in R (v.4.0.2) and Seurat34 (v.4.0.5) and cells with at least 200 genes and genes expressed in at least 3 cells were retained for further quality control analysis for the percentage of mitochondrial genes expressed, total genes expressed and unique molecular identifier (UMI) counts. The gene–cell barcode matrix obtained after quality control analysis was log-normalized and 3,000 variable genes were identified and scaled to perform PCA. The five PDAC primary patient samples were then batch-corrected and integrated using a reciprocal PCA (RPCA) pipeline in Seurat using ‘FindIntegrationAnchors’ and ‘IntegrateData’ functions. The ‘integrated’ assay was again scaled to perform PCA. The top significant principal components of PCA were identified using ‘ElbowPlot’ in each dataset. To cluster and visualize the cells, ‘FindNeighbours’, ‘FindClusters’ and ‘RunUMAP’ functions were used on the top identified principal components in each dataset.
The cell types were identified by manual annotation of well-known makers33, namely: epithelial-tumour cells (EPCAM and KRT8), pancreatic epithelial cells (CPA1 and CTRB1), T cells (CD3D and IL7R), myeloid cells (CD14, CD68, FCGR3A and LYZ), NK cells (NKG7 and GNLY), B cells (CD79A and MS4A1), dendritic cells (FCGR1A and CPA3), endothelial cells (PECAM1, KDR and CDH5), fibroblasts (ACTA2, COL1A1, COLEC11 and DCN), vascular smooth muscle cells (MYH11 and ACTA2), hepatocytes (ALB, APOE and CPS1), cholangiocytes (ANXA4, KRT7 and SOX9), plasma cells (JCHAIN and IGKC) and cycling cells (TOP2A and MKI67).
M1/M2 macrophages were designated as described35: M1-like macrophages (AZIN1, CD38, CXCL10, CXCL9, FPR2, IL18, IL1B, IRF5, NIFKBIZ, TLR4, TNF and CD80) and M2-like macrophages (ALOX5, ARG1, CHIL3, CD163, IL10, IL10RA, IL10RB, IRF4, KIF4, MRC1, MYC, SOCS2 and TGM2). The mean expression score for the M1 and M2 signatures were computed for each macrophage subcluster using ‘AddModuleScore’ function and clusters with a higher M1 or M2 signature score were assigned M1-like or M2-like annotation, respectively.
Metabolite extraction and analysis
Cells grown on a 12-well plate coated with or without ECM. Metabolite extraction and analysis were performed as before11. Gas chromatography-mass spectrometry (GC-MS) analysis was performed using an Agilent 6890 gas chromatograph equipped with a 30-m DB-35MS capillary column connected to an Agilent 5975B mass spectrometer operating under electron impact ionization at 70 eV. For measurement of amino acids, the gas chromatograph oven temperature was held at 100 °C for 3 min and increased to 300 °C at 3.5 °C per min. The mass spectrometer source and quadrupole were held at 23 °C and 150 °C, respectively, and the detector was run in scanning mode, recording ion abundance in the range of 100–605 m/z. Mole per cent enrichments of stable isotopes in metabolite pools were determined by integrating the appropriate ion fragments and correcting for natural isotope abundance as previously described36.
Cell viability assay
Cells were plated in 96-well plates coated with or without ECM at a density of 3,000 cells (MIA, 1305) or 1,500 cells (KPC or KC) per well and incubated overnight before treatment. 7rh (500 nM), ML120B (10 μM), EIPA (10.5 μM), IPI549 (600 nM), MBQ-167 (500 nM), MRT68921 (600 nM) or ML385 (10 μM), or their combinations, were added to the wells in the presence of complete medium (CM), LG medium or LQ medium for 72 h. Cell viability was determined with a Cell Counting Kit-8 assay (Glpbio). Optical density was read at 450 nm and analysed using a microplate reader with SoftMax 6.5 software (FilterMax F5, Molecular Devices). For all experiments, the medium was replaced every 24 h.
Luminescence ATP detection assay
KPC or KC cells were grown on 96-well plates coated with or without the indicated ECM in the presence of 100 μl CM or LG medium with or without EIPA (10.5 μM), MBQ-167 (500 nM), MRT68921 (600 nM) or their combinations for 24 h. Then the cell number was measured. Intracellular ATP was determined with a luminescence ATP detection assay system (PerkinElmer) according to the manufacturer’s protocol. Finally, luminescence was measured and normalized to cell number.
l-amino acid assay
KPC or KC cells were grown on six-well plates coated with or without the indicated ECM in the presence of 100 μl LG medium with or without EIPA (10.5 μM), MRT68921 (600 nM) or their combinations for 24 h. Total amounts of free l-amino acids (except for glycine) were measured using an L-Amino Acid Assay Kit (Colorimetric, antibodies) according to the manufacturer’s protocol. The concentration of l-amino acids was calculated within samples by comparing the sample optical density to the standard curve and normalized to cell number.
Statistics and reproducibility
Macropinosomes or mitochondria were quantified by using the ‘Analyze Particles’ feature in Image J (NIH). Macropinocytotic uptake index37 or mitochondria number was computed by the macropinosome or mitochondria area in relation to the total cell area for each field and then by determining the average across all the fields (six fields). Tumour area (%) was quantified by using the ‘Polygon’ and ‘Measure’ feature in Fiji Image J and was computed by tumour area in relation to total area for each field and then by determining the average across all the fields (five fields). Positive area of protein expression in tumour (%) was quantified by using ‘Colour Deconvolution’, ‘H DAB’, and ‘Analyze Particles’ feature in Fiji Image J and was computed by the protein-positive area in relation to the tumour area for each field and then by determining the average across all the fields (5–6 fields). These measurements were done on randomly selected fields of view. A two-tailed unpaired Student’s t-test was performed for statistical analysis using GraphPad Prism software. Data are presented as mean ± s.e.m. Kaplan–Meier survival curves were analysed by log-rank test. Statistical correlation between Col I–DDR1–NRF2 signalling proteins in human PDAC specimens was determined by two-tailed chi-squared test. (****P < 0.0001, ***P < 0.001, **P < 0.01 and *P < 0.05). All experiments except the IHC analysis of 106 human specimens were repeated at least 3 times.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Online content
Any methods, additional references, Nature Research reporting summaries, source data, extended data, supplementary information, acknowledgements, peer review information; details of author contributions and competing interests; and statements of data and code availability are available at 10.1038/s41586-022-05169-z.
Supplementary information
This file contains Supplementary Tables 1–3 and Supplementary Fig. 1
Source data
Acknowledgements
We thank members of the M.K. laboratory for discussions; Cell Signaling Technologies, Santa Cruz Technologies, Thermo Fisher Scientific, Promega and MedChemExpress for gifts of antibodies and reagents; and UCSD Tissue Technology Shared Resources (TTSR) and J. Santini at the UCSD School of Medicine Microscopy Core for histology and microscopy services. Research was supported by grants from Padres Pedal the Cause/C3 (PPTC2018 to M.K. and A.M.L.); the Youth Program of the National Natural Science Foundation of China (81802757 to H.S. and 82002931 to F.Y.); the NIH (R01CA211794, R37AI043477, P01DK098108 and U01AA027681 to M.K., U01CA274295 to M.K., R.F.S. and A.M.L., R01CA155630 to A.M.L. and R01CA234245 and R01CA218254 to C.M.M.); the National Key Research and Development Program of China (2016YFC0905900 to B.S.); the National Cancer Institute Cancer Center Support Grant (CCSG) (P30CA23100 to TTSR); and the UCSD School of Medicine Microscopy Core (NINDS P30-NS047101). Additional support was provided by Ride the Point (M.K. and A.M.L.); the Research for a Cure of Pancreatic Cancer Fund and the Alexandrina M. McAfee Trust Foundation (A.M.L.); and the UC Pancreatic Cancer Consortium to A.M.L., who is the Homer T. Hirst III Professor of Oncology in Pathology, and M.K., who is the Ben and Wanda Hillyard Chair for Mitochondrial and Metabolic Diseases.
Extended data figures and tables
Author contributions
M.K. and H.S. conceived the project. H.S. designed the study and H.S. and F.Y. performed most experiments. F.Y., H.S. and R.F. performed IHC analysis of human and mouse PDAC. H.S., F.Y., B.T., J. Siruno., M.L., Y.L. and N. Sinchai performed immunoblotting and qPCR analysis. C.M.M. and A.K. performed the 13C-tracing experiments. A.M., N. Sun. and S.D. performed Seahorse experiments. J.L. performed several orthotopic PDAC cell implantations. J.B. performed several intrasplenic PDAC implantations. R.F.S., A.N. and A.F. performed scRNA-seq analysis. S.B.R. performed RNA-seq analysis. J. Santini detected SHG signal of collagen. D.A.B. provided Col Ir/r mice. A.M.L. provided human PDAC 1305 cells. B.S. collected human PDAC tissue and supervised and supported F.Y. and R.F. M.K. and H.S. wrote the manuscript, with all authors contributing and providing feedback and advice.
Peer review
Peer review information
Nature thanks Rolf Brekken and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Data availability
RNA-seq data are available at the Gene Expression Omnibus (GEO) under accession number GSE206218. scRNA-seq data were obtained from a published GEO dataset (GSE156405). Graph data and raw images of immunoblot and DNA gels are provided within the Source Data. All raw image data including immunostaining, immunoblotting, DNA gels, IHC, H&E and sirius red staining were uploaded to Mendeley Data (10.17632/9v2hyb4j7n.1). Source data are provided with this paper.
Code availability
Custom computer code used in the scRNA-seq analysis is available at https://github.com/ajynair/Collagen_DDR1_PDACmets.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hua Su, Fei Yang
Change history
3/7/2023
A Correction to this paper has been published: 10.1038/s41586-023-05920-0
Change history
6/18/2025
A Correction to this paper has been published: 10.1038/s41586-025-09285-4
Contributor Information
Beicheng Sun, Email: sunbc@nju.edu.cn.
Michael Karin, Email: karinoffice@health.ucsd.edu.
Extended data
is available for this paper at 10.1038/s41586-022-05169-z.
Supplementary information
The online version contains supplementary material available at 10.1038/s41586-022-05169-z.
References
- 1.Makohon-Moore, A. & Iacobuzio-Donahue, C. A. Pancreatic cancer biology and genetics from an evolutionary perspective. Nat. Rev. Cancer16, 553–565 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grzesiak, J. J. & Bouvet, M. The α2β1 integrin mediates the malignant phenotype on type I collagen in pancreatic cancer cell lines. Br. J. Cancer94, 1311–1319 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beatty, G. L. et al. CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science331, 1612–1616 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhim, A. D. et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell25, 735–747 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erkan, M. et al. The activated stroma index is a novel and independent prognostic marker in pancreatic ductal adenocarcinoma. Clin. Gastroenterol. Hepatol.6, 1155–1161 (2008). [DOI] [PubMed] [Google Scholar]
- 6.Armstrong, T. et al. Type I collagen promotes the malignant phenotype of pancreatic ductal adenocarcinoma. Clin. Cancer Res.10, 7427–7437 (2004). [DOI] [PubMed] [Google Scholar]
- 7.Ramanathan, R. K. et al. Phase IB/II randomized study of FOLFIRINOX plus pegylated recombinant human hyaluronidase versus FOLFIRINOX alone in patients with metastatic pancreatic adenocarcinoma: SWOG S1313. J. Clin. Oncol.37, 1062–1069 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu, H. et al. Generation of collagenase-resistant collagen by site-directed mutagenesis of murine pro alpha 1(I) collagen gene. Proc. Natl Acad. Sci. USA 87, 5888–5892 (1990). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang, D. Y. & Friedman, S. L. Fibrosis-dependent mechanisms of hepatocarcinogenesis. Hepatol.56, 769–775 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baglieri, J. et al. Nondegradable collagen increases liver fibrosis but not hepatocellular carcinoma in mice. Am. J. Pathol.191, 1564–1579 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Su, H. et al. Cancer cells escape autophagy inhibition via NRF2-induced macropinocytosis. Cancer Cell39, 678–693 (2021). [DOI] [PMC free article] [PubMed]
- 12.Criscuolo, D., Avolio, R., Matassa, D. S. & Esposito, F. Targeting mitochondrial protein expression as a future approach for cancer therapy. Front. Oncol.11, 797265 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogel, W., Gish, G. D., Alves, F. & Pawson, T. The discoidin domain receptor tyrosine kinases are activated by collagen. Mol. Cell1, 13–23 (1997). [DOI] [PubMed] [Google Scholar]
- 14.Das, S. et al. Discoidin domain receptor 1 receptor tyrosine kinase induces cyclooxygenase-2 and promotes chemoresistance through nuclear factor-kappaB pathway activation. Cancer Res.66, 8123–8130 (2006). [DOI] [PubMed] [Google Scholar]
- 15.Zhong, Z. et al. NF-κB restricts inflammasome activation via elimination of damaged mitochondria. Cell164, 896–910 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Juskaite, V., Corcoran, D. S. & Leitinger, B. Collagen induces activation of DDR1 through lateral dimer association and phosphorylation between dimers. eLife6, e25716 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhattacharjee, S. et al. Tumor restriction by type I collagen opposes tumor-promoting effects of cancer-associated fibroblasts. J. Clin. Invest.131, 146987 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang, S. H. et al. Discoidin domain receptor 1 is associated with poor prognosis of non-small cell lung carcinomas. Oncol. Rep.24, 311–319 (2010). [DOI] [PubMed] [Google Scholar]
- 19.Turashvili, G. et al. Novel markers for differentiation of lobular and ductal invasive breast carcinomas by laser microdissection and microarray analysis. BMC Cancer7, 55 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun, X. et al. Tumour DDR1 promotes collagen fibre alignment to instigate immune exclusion. Nature599, 673–678 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Martino, J. S. et al. A tumor-derived type III collagen-rich ECM niche regulates tumor cell dormancy. Nat. Cancer3, 90–107 (2022). [DOI] [PMC free article] [PubMed]
- 22.Picca, A. & Lezza, A. M. S. Regulation of mitochondrial biogenesis through TFAM-mitochondrial DNA interactions: useful insights from aging and calorie restriction studies. Mitochondrion25, 67–75 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Scarpulla, R. C., Vega, R. B. & Kelly, D. P. Transcriptional integration of mitochondrial biogenesis. Trends Endocrinol. Metab.23, 459–466 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aguilera, K. Y. et al. Inhibition of discoidin domain receptor 1 reduces collagen-mediated tumorigenicity in pancreatic ductal adenocarcinoma. Mol. Cancer Ther.16, 2473–2485 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Slapak, E. J., Duitman, J., Tekin, C., Bijlsma, M. F. & Spek, C. A. Matrix metalloproteases in pancreatic ductal adenocarcinoma: key drivers of disease progression? Biology9, E80 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aguilera, K. Y. et al. Collagen signaling enhances tumor progression after anti-VEGF therapy in a murine model of pancreatic ductal adenocarcinoma. Cancer Res.74, 1032–1044 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng, J. et al. DDR1-induced neutrophil extracellular traps drive pancreatic cancer metastasis. JCI Insight6, 146133 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Torres, M. P. et al. Novel pancreatic cancer cell lines derived from genetically engineered mouse models of spontaneous pancreatic adenocarcinoma: applications in diagnosis and therapy. PLoS ONE 8, e80580 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang, T., Shen, S., Qu, J. & Ghaemmaghami, S. Global analysis of cellular protein flux quantifies the selectivity of basal autophagy. Cell Rep.14, 2426–2439 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Su, H. et al. VPS34 acetylation controls its lipid kinase activity and the initiation of canonical and non-canonical autophagy. Mol. Cell67, 907–921 (2017). [DOI] [PubMed] [Google Scholar]
- 31.Liu, X. et al. A targeted mutation at the known collagenase cleavage site in mouse type I collagen impairs tissue remodeling. J. Cell Biol.130, 227–237 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Monaghan, M. G., Kroll, S., Brucker, S. Y. & Schenke-Layland, K. Enabling multiphoton and second harmonic generation imaging in paraffin-embedded and histologically stained sections. Tissue Eng. Part C Methods22, 517–523 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee, J. J. et al. Elucidation of tumor-stromal heterogeneity and the ligand–receptor interactome by single-cell transcriptomics in real-world pancreatic cancer biopsies. Clin. Cancer Res.27, 5912–5921 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell184, 3573–3587 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li, S. et al. Metabolism drives macrophage heterogeneity in the tumor microenvironment. Cell Rep.39, 110609 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar, A., Mitchener, J., King, Z. A. & Metallo, C. M. Escher-Trace: a web application for pathway-based visualization of stable isotope tracing data. BMC Bioinformatics21, 297 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Commisso, C., Flinn, R. J. & Bar-Sagi, D. Determining the macropinocytic index of cells through a quantitative image-based assay. Nat. Protoc.9, 182–192 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This file contains Supplementary Tables 1–3 and Supplementary Fig. 1
Data Availability Statement
RNA-seq data are available at the Gene Expression Omnibus (GEO) under accession number GSE206218. scRNA-seq data were obtained from a published GEO dataset (GSE156405). Graph data and raw images of immunoblot and DNA gels are provided within the Source Data. All raw image data including immunostaining, immunoblotting, DNA gels, IHC, H&E and sirius red staining were uploaded to Mendeley Data (10.17632/9v2hyb4j7n.1). Source data are provided with this paper.
Custom computer code used in the scRNA-seq analysis is available at https://github.com/ajynair/Collagen_DDR1_PDACmets.