Abstract
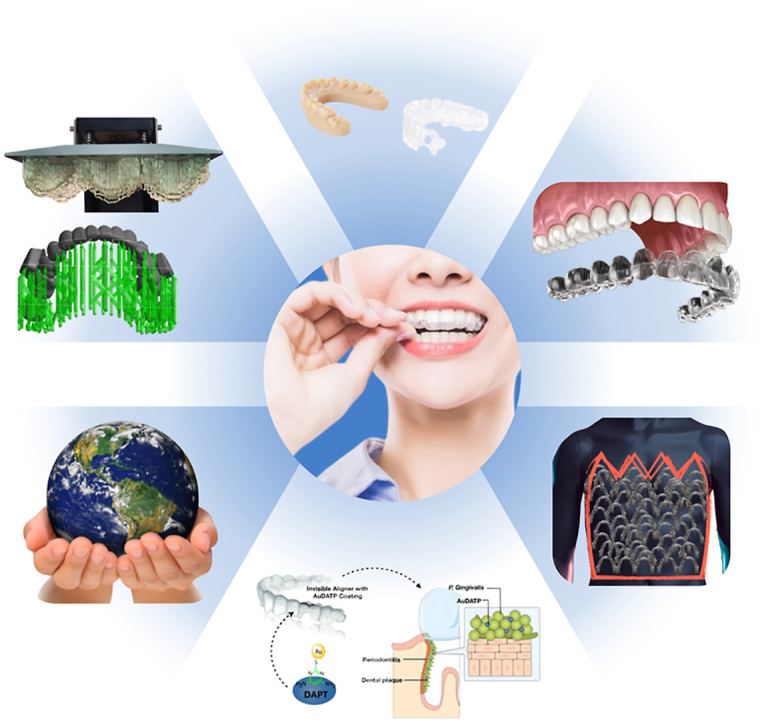
Rapid technological improvements in biomaterials, computer-aided design (CAD) and manufacturing (CAM) have endorsed clear aligner therapy (CAT) as a mainstay of orthodontic treatment, and the materials employed for aligner fabrication play an all-important role in determining the clinical performance of clear aligners. This narrative review has attempted to comprehensively encompass the entire gamut of materials currently used for the fabrication of clear aligners and elucidate their characteristics that are crucial in determining their performance in an oral environment. Historical developments and current protocols in aligner fabrication, features of contemporary bioactive materials, and emerging trends related to CAT are discussed. Advances in aligner material chemistry and engineering possess the potential to bring about radical transformations in the therapeutic applications of CAT; in the absence of which, clear aligners would continue to underperform clinically, due to their inherent biomechanical constraints. Finally, while innovations in aligner materials such as shape memory polymers, direct three-dimensional (3D) printed clear aligners and bioactive materials combined with clear aligner materials are essential to further advance the applications of CAT; increased awareness of environmental responsibilities among aligner manufacturers, aligner prescribing clinicians and aligner users is essential for better alignment of our climate change goals towards a sustainable planet.
Keywords: Clear aligners, Bioactive materials, Shape memory polymers, Direct 3D printing, Environment, Review
Graphical abstract
Highlights
-
•
Clear aligner fabrication material primary determinant of its clinical performance.
-
•
Present-day materials, characteristics, current fabrication protocols presented.
-
•
Shape memory polymers and direct 3D printed clear aligners highlighted.
-
•
Features of contemporary bioactive materials and emerging trends discussed.
-
•
Heightened environmental awareness due to increased plastic aligner use essential.
Abbreviations
- CAD/CAM
computer-aided design/manufacturing
- CAT
clear aligner therapy
- 3D
three-dimensional
- FA
fixed appliances
- PU
polyurethane
- PVS
polyvinyl siloxane
- CT
computed tomography
- FFF
fused filament fabrication
- SLS
selective laser sintering
- SLM
selective laser melting
- SLA
steriolithography apparatus
- KFDA
Korea Food and Drug Administration
- EC
European Commission
- FDA
Food and Drug Administration
- PET
polyethylene terephthalate
- PETG
polyethylene terephthalate glycol
- Tg
glass-transition temperature
- TPU
thermoplastic polyurethane
- PU
polyurethane
- PC
polycarbonate
- PP
polypropylene
- ISO
international standards organization
- HGFs
human gingival fibroblasts
- SMPs
shape memory polymers
- PRG
pre-reacted glass-ionmer
- S. mutans
streptococcus mutans
- P.gingivalis
porphyromonas gingivalis
- RCT
rondomized clinical trial
- NPs
nanoparticles
- AuDAPT
4,6-diamino-2- pyrimidinethiol-modified Au nanoparticles
- 3DPIN
3D printed in-house
- HM
Martens hardness
- EIT
indentation modulus
- ηIT
elastic index
- RIT
indentation relaxation
1. Introduction
With the rapid technological improvements in biomaterials, computer-aided design (CAD) and manufacturing (CAM), clear aligner therapy (CAT) has emerged as a promising alternative to conventional fixed appliances (FAs) in orthodontics. The demand for CAT has increased significantly over the last decade, presumably due to aggressive marketing strategies by commercial clear aligner companies that employ direct-to-consumer advertising as well as widespread utilization of various social media channels, thereby generating heightened public awareness for esthetic orthodontic treatment alternatives, especially for the adult patients [1]. The global clear aligners market size was projected to increase from USD 3.1 billion in 2021 to USD 11.6 billion in 2027 with a compound annual growth rate (CAGR) of 13% [2]. A recent survey carried out across North America also indicated that more orthodontists in the younger generations believe that clear aligners will be the main technique to treat malocclusions [3].
CAT typically comprises a series of clear plastic trays covering the dentition with a snug fit, that is to be used by the patient at all times except eating and brushing and generally changed sequentially every one to two weeks to accomplish planned orthodontic tooth movements. Although multiple commercial clear aligner systems are available today globally, the use of clear thermoformed plastic materials for clear aligner fabrication remains a common feature [4].
Although the clinical efficacy of clear aligners can be affected by a multitude of factors [[5], [6], [7], [8], [9]], the properties of materials used for their fabrication remain one of the most essential aspects in determining their mechanical and clinical features [10]. This review endeavours to comprehensively cover the advances in biomaterials used for clear aligner fabrication. Historical developments, current protocols, properties, and clinical performances of various clear aligner materials, features of contemporary bioactive materials as well as emerging trends are discussed in this narrative review of the literature.
2. Historical perspective
2.1. Origin and evolution
Harold D. Kesling in 1945, first advocated the use of rubber-based tooth positioners, fabricated from wax setups of patient's dentition, and demonstrated that these appliances not only helped in detailing orthodontically treated cases but could also sequentially reposition misaligned teeth, thereby pioneering the fundamental concepts of modern CAT with the possibility of performing significant orthodontic tooth movements with thermoplastic materials [11]. Kesling foresaw that more ambitious tooth movements could be realized with a series of aligners while recognizing the limitations of the technology available to him at that time: ‘Major tooth movements could be accomplished with a series of positioners by changing the teeth on the set-up slightly as treatment progresses. At present, this type of treatment does not seem to be practical. It remains a possibility, however, and the technique for its practical application might be developed in the future [12].
Henry Nahoum in 1964 [13], then refined Kesling's technique by developing a vacuum-based appliance that displayed firm adaptation to a patient's cast. This technique involved the fabrication of a plaster cast on which rotated anterior teeth were sectioned from the cast using a fissure bur or a goldsmith's saw and the sectioned teeth were then re-arranged with wax on the cast as per the desired outcome. A variety of thermoplastic materials, including acetates, vinyl, styrene, polyethylene, and butyrate sheets could then be vacuum formed over the designed cast to fabricate a dental contour appliance that could move teeth.
In 1971, Ponitz utilized Biocryl (polymethyl methacrylate), which was made out of cellulose acetate butyrate, polyurethane (PU), polyvinyl acetate-polyethylene polymer, polycarbonate-cycolac, and latex, to introduce an ‘Invisible retainer’. This vacuum-formed clear plastic appliance was initially fabricated for finishing and retention of orthodontic cases using base plate wax on the prepositioned cast and could obtain limited orthodontic tooth movements, chiefly by tipping crowns and could be used for subsequent retention [14].
In 1985, McNamara [15] modified Ponitz's technique and used 1 mm thick Biocryl™ polymers with a Biostar vacuum forming machine to fabricate invisible retainers for retention and final detailing. The difference between the Biostar machine and the previous vacuum former was that it used positive air pressure to adapt the thermoplastic Biocryl™ to the surface of the model rather than the vacuum pressure. However, the author admitted that the long-term durability of this clear removable retainer was not comparable to the conventional acrylic or bonded retainers.
Finally, Jack Sheridan 1993 further modified the process of fabricating clear appliances, utilizing polypropylene, a 0.030″ sheet of thermoplastic copolyester from Raintree Products, and coined the word ‘Essix appliance’ to describe an esthetic method for the alignment of anterior teeth by combining clear appliances with interproximal teeth reduction. He also recommended using a positive air pressure method for the thermoforming process like McNamara's to decrease the thickness of the sheet almost by half after fabrication [16].
However, throughout these advances, the basic principle of producing minor tooth movements with individual clear appliances did not change. Fabricating appliances by making impressions, pouring casts, sectioning individual teeth, re-arranging them into proper alignment to obtain a final cast and repeating this process at every clinical appointment was an extremely laborious and time-consuming process. The solution to which arrived in the form of a clear aligner system named Invisalign, which involved a series of removable polyurethane aligners created digitally by two Stanford graduates – Zia Chishti and Kelsey Wirth, launched in 1998 by Align Technology (Santa Clara, CA). This was the first orthodontic appliance to be fabricated using transparent and thermoplastic polymeric materials, with the aid of modern CAD/CAM technology [17]. This system involved a multiple-step process, beginning with the three-dimensional (3D) reconstruction of patients’ dentition, obtained either from an intra-oral scan or digital scanning of the study models, followed by segmentation of the individual crown with the help of a computer algorithm, and the development of treatment plans presented visually as a sequence of incremental tooth movement by a predetermined amount using the software. The next step comprised manufacturing the physical models for each stage of tooth movement using the rapid prototyping technique [18,19]. Finally, the bespoke aligners were produced using a thermoforming process and trimmed to the final configurations.
2.2. Generations of clear aligners
Clear aligners have undergone multiple transformations over the years in the quest for improved clinical efficiency to treat various malocclusions more aesthetically, comfortably, and effectively. These transformations of clear aligners in general and Invisalign in particular, are highly representative and have been summarized and reviewed as eight generations of clear aligners by Hennessy and Al-Awadhi [20], Ganta [21], Moshiri [22], and Wajekar [23] as follows.
2.2.1. First-generation aligners
The earliest forms of clear aligner systems were solely reliant on the thermoformed plastic aligner material to achieve intended results without any auxiliary elements being incorporated into the aligner system. The first case report was published in 2000 using 1st generation Invisalign to treat mild crowding and space closure cases [24]. The material used to fabricate Invisalign aligners before September 2001 was a polymer mixture and the brand name was Proceed30 (PC 30), which failed to meet all the physical, chemical, and clinical requirements for orthodontic tooth movement [25]. Clinicians encountered some difficulties and limitations with the usage of these clear aligners [26,27].
2.2.2. Second-generation aligners
With advances in aligner systems, manufacturers incorporated the use of attachments to provide better control of planned tooth movement. Clinicians could also request for composite buttons to be bonded on the teeth and utilize inter-maxillary elastics. Other features, including SmartForce™ attachments, Power Ridge™, Velocity Optimization, and interproximal reduction (IPR) became universal in the Invisalign system. A single layered polymer material Exceed30 (EX 30), an implantable medical-grade polymer made of polyurethane methylene diphenyl diisocyanate 1.6-hexanediol, tested for safety and biocompatibility by the United States Pharmacopeia, Class IV [28], was used to fabricate the aligners. The EX30 material provided 1.5 times greater elasticity and 4 times more adaptability than PC 30 and facilitated easier insertion and removal of the trays for the patient [29].
2.2.3. Third-generation aligners
In 2010, the third-generation aligners included SmartForce™ features, such as optimized attachments, designed and placed automatically by commercial software as well as indentations in the polyurethane plastic that placed increased pressure on specified points on the crown to produce a moment of a couple and root torque (Power Ridge). Further, the clinician could also prescribe non-precision attachments to be placed on the teeth wherever needed, to improve movements such as derotation and extrusion. New precision cuts were introduced to help with Class II and Class III interarch elastics [30].
2.2.4. Fourth-generation aligners
In 2011, G4 attachments were released to facilitate the clinical outcomes in open bite cases with improved optimized extrusion attachments on multiple teeth. New multi-plane movement features were available for upper laterals to enhance extrusion along with rotation and/or crown tipping. Optimized root control attachments were introduced for better mesiodistal root control of canines and central incisors [31].
Since 2013, EX 30 has been replaced by a new multi-layer aromatic thermoplastic polyurethane/co-polyester material, called SmartTrack™ (LD30). This new material provides better performance, such as a gentle and more constant force, more long-term action and improved adhesion, which eases the use for patients. Compared with EX30, LD30 has greater consistency of application of orthodontic forces, greater elasticity, chemical stability and an even more precise and comfortable aligner fit [32,33].
2.2.5. Fifth-generation aligners
In late 2013, fifth-generation enhancement improved the predictability of deep bite correction by introducing pressure areas on the lingual of the upper and lower anterior teeth, precision bite ramps on the lingual of the upper incisors, and bevelled dome-shaped retention attachments on the premolars [34]. However, a recent study by Blundell et al. found that the use of precision bite ramps does not appear to significantly improve the ability of SmartTrack™ material to predictably open the bite compared with EX30 materials [35].
2.2.6. Sixth-generation aligners
In late 2014, sixth-generation clinical innovation for orthodontic treatment of first premolar extractions was introduced using new SmartStage™ technology and SmartForce™ features to provide vertical control and root parallelism that optimize the progression of tooth movements for extraction treatment planned for maximum anchorage [36].
2.2.7. Seventh-generation aligners
Invisalign G7, a set of features designed to deliver greater control of tooth movements and improved treatment outcomes was released in 2016, particularly for teenage patients. It aimed to deliver better upper lateral incisor control, and improve root control and features to address the prevention of posterior open bites [37].
2.2.8. Eighth-generation aligners
Around late 2020, the eighth-generation enhancements were announced aiming to further improve the predictability of deep-bite correction with SmartForce™ aligner activation for anterior intrusion and improvements in the ClinCheck virtual proprietary software setup to level the Curve of Spee. G8 also minimizes unwanted crown tipping during posterior arch expansion with optimized expansion support and rotation attachments to reduce the potential for buccal crown tipping [22,38].
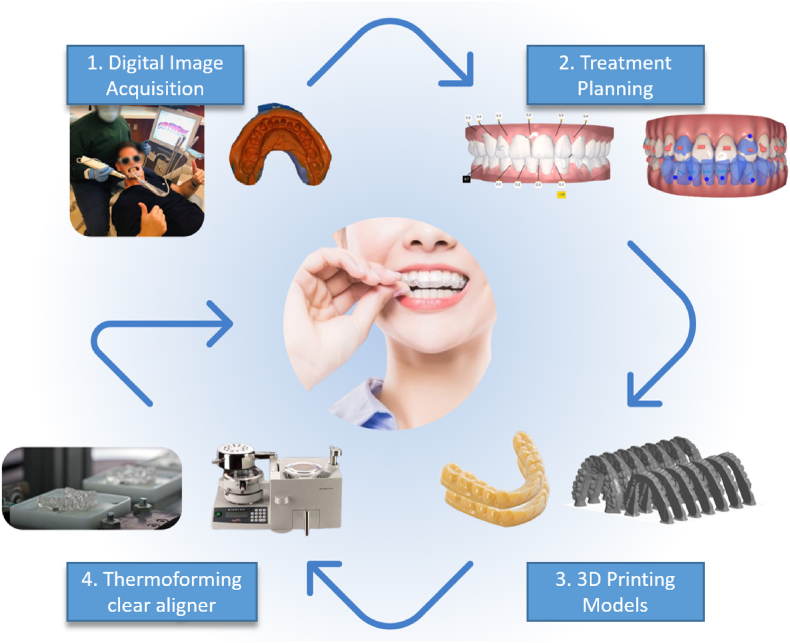
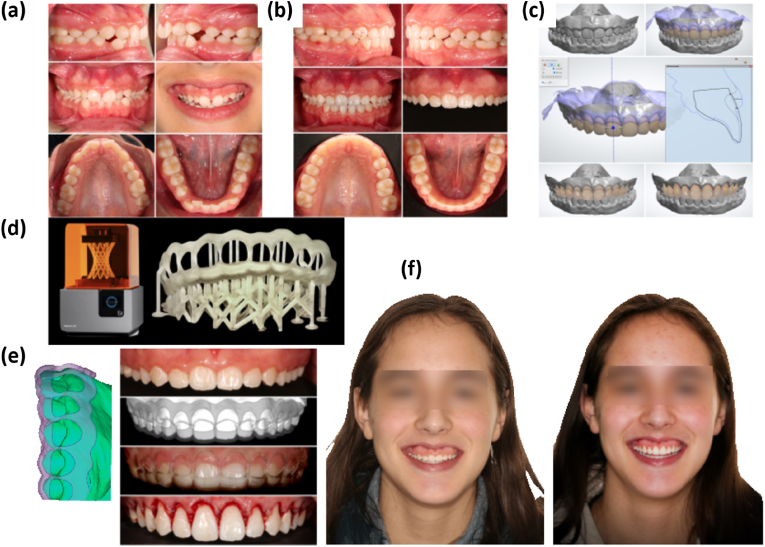
2.3. Aligner fabrication process
The pioneering methods involving the manual fabrication of clear aligners, are no longer used for commercial aligner fabrication, and the current digital fabrication method employs CAD/CAM technology and digital workflow protocol (Fig. 1). A digital image acquisition is obtained via either a direct approach (images from an intraoral scanner) or an indirect approach (high-quality polyvinyl siloxane (PVS) putty impressions that are then digitally scanned), eventually providing a digital representation of the patient's dentition that constitutes the basic framework for virtual planning of tooth movements desired with CAT [4]. Virtual treatment planning and tooth movement manipulations are then performed using CAD platforms. Computer algorithms segment the individual clinical crowns of the digitized 3D model. Additional visualization of the tooth roots is now possible by importing and overlaying computerized tomography (CT) scan data. The position of teeth is manipulated through sequential movements towards the finally desired positions, resulting in the generation of sequential virtual models with teeth in positions planned for each stage [4]. 3D model printing of each of these virtual setup models generates serial physical models via CAM technology, incorporating either subtractive (milling) or additive manufacturing (3D printing) techniques. Three-dimensional printing is currently the mainstream technology used for orthodontic model fabrication. The corresponding series of clear aligners are then thermoformed on the physical copies and finally trimmed and polished The process of 3D printing of serial digital models and the thermoforming process itself is time-consuming, labour-intensive, and costly depending on the malocclusion type, aligner changing protocol and the number of refinements. Concerns over the plastic burden on the environment have been raised and warrant research to investigate the environmental impact of clear aligner production [4].
Fig. 1.
Workflow of fabrication of clear aligners by the thermoforming process.
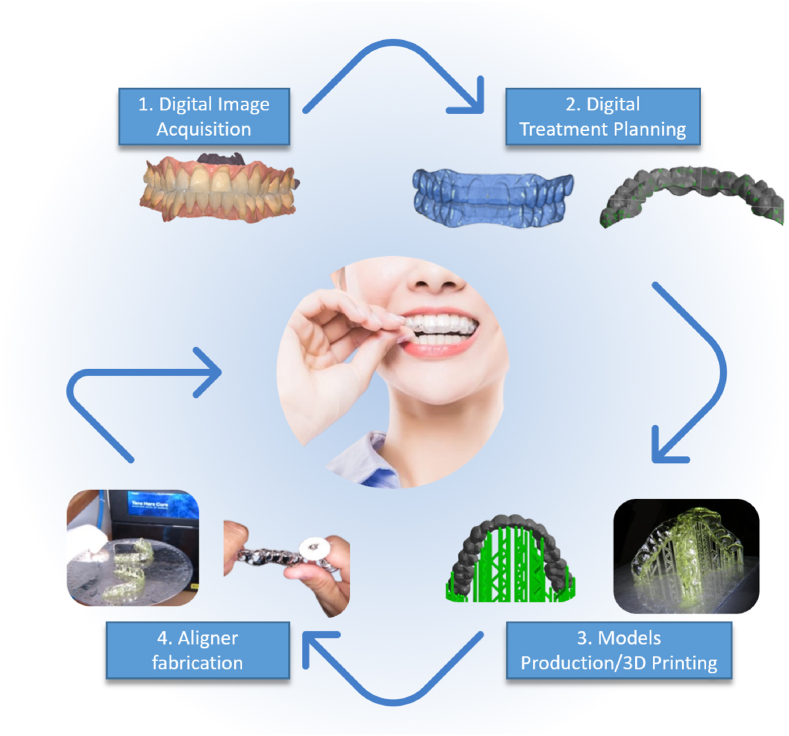
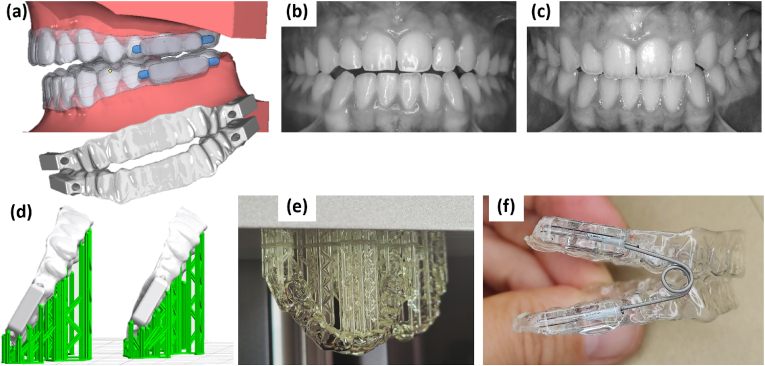
With technological advancements, the next paradigm shift would likely involve direct 3D printing of aligners from digital designs [39,40] and Nasef has been credited with the first novel attempt at 3D direct printing of retainers [41]. Current materials used for 3D printing in orthodontics include acrylonitrile-butadiene-styrene plastic, stereolithography materials (epoxy resins), polylactic acid, polyamide (nylon), glass-filled polyamide, silver, steel, titanium, photopolymers, wax, and polycarbonate. The advantages of using a clear aligner that is 3D printed are not just limited to the reduction of the cumulative errors introduced from the analog impression, intraoral scan, 3D printed physical model, and the subsequent thermoplastic process [42]. In addition to improved accuracy, 3D printing can shorten the supply chains, lower costs, and lead to a more sustainable process by generating less waste [43]. Theoretically, 3D direct printing allows the fabrication of clear aligners with customized thickness and spatial control of aligner thickness across the arch. The thickness of the aligner and the material chosen influence not only the magnitude of force delivered to teeth but also the mechanical properties of the aligners as well [40]. Although various 3D printing methods may be used for direct printing aligners, such as fused filament fabrication (FFF), selective laser sintering (SLS) or melting (SLM), stereolithography apparatus (SLA), multi-jet photocured polymer process, HP multiJet fusion technology or continuous liquid interface production technology, and powder binder printing [44]; 3D printing by photo-polymerization from clear resins seems to be a promising option, as the specific characteristics and requirements of the material properties are more appropriate [[45], [46], [47]]. Fig. 2 outlines the stepwise fabrication process of 3D direct printed clear aligners.
Fig. 2.
Stepwise fabrication process of 3D direct printed clear aligners.
3. Materials used for clear aligners
The composition of the material utilized for the fabrication of a clear aligner influences the clinical performance of the aligners [48,49] and this composition in turn is influenced by the actual manufacturing process that can basically be divided into two categories: the conventional method of vacuum thermoforming with thermoplastic material moulding on physical models and the other category of direct 3D printing without intermediary physical models [47,50]. Currently, the first fabrication process is widely adopted both commercially and clinically, including for the in-house production of aligners [51]. While, for the direct 3D printing process, with the exception of Tera Harz TC-85 (Graphy, Seoul, South Korea), which has been approved by the Korea Food and Drug Administration (KFDA), European Commission (EC) and Food and Drug Administration (FDA) as per the company website [52], there is no other 3D printable material currently available commercially that meets the standard of biocompatibility, translucency, and appropriate mechanical properties [39,40,42].
3.1. Thermoplastic polymers
Thermoplastic polymers can be classified as amorphous and semicrystalline polymers based on their inherent molecular structure. Amorphous polymers comprise irregularly arranged molecular structures characterized by a low degree of molecular packing. Semicrystalline polymers, on the other hand, comprise both areas of uniformly and tightly packed chains (crystalline domains) and irregularly arranged areas (amorphous regions). The role of crystalline domains in thermoplastic polymers can be likened to that of fillers in composite materials, which confer hardness and rigidity to the thermoplastic material. Generally, amorphous polymers are softer, transparent, exhibit low shrinkage, and possess better impact resistance. Contrastingly, semicrystalline polymers are hard, opaque, or translucent, possess good chemical resistance and exhibit a sharp melting point [50,53,54]. The polymers (either individual or blended) most commonly utilized for the manufacture of commercial clear plastic orthodontic aligners are polyester, polyurethane or co-polyester, polypropylene, polycarbonate, ethylene vinyl acetate, and polyvinyl chloride among others [4,48,54].
Clear aligner materials have evolved from single-layered or monophasic plastic to second-generation polyurethane materials, to the currently used third-generation multilayered materials that often comprise hard and soft layers. While the soft layer imparts the property of elastic deformation allowing smooth seating of the aligner, the hard layer ensures strength and durability [55].
Among polyesters, polyethylene terephthalate (PET) and polyethylene terephthalate glycol (PETG)- a non-crystallizing amorphous copolymer of PET, are extensively employed in the production of clear aligners primarily due to their excellent mechanical and optical properties [56]. Polyethylene terephthalate (PET) combines ethylene glycol with terephthalic acid and exists in both amorphous and crystalline forms, and the form type influences the material properties [57]. PET can be drawn into tapes, films, or fibres and is frequently used as a substitute for grafts and the fabrication of vascular prostheses. The amorphous structure of PET is transparent and demonstrates superior ductility, whereas the crystalline structure is opaque and white and exhibits hardness, stiffness and good strength [58]. PET can be rigid or semi-rigid depending upon the processing methods employed and displays excellent mechanical properties, toughness, and resistance against various solvents [21].
PETG is a non-crystalline co-polyester, comprised of 1,4-cyclohexane two methanol (CHDM), ethylene glycol (EG) and terephthalic acid (TPA) [59]. PETG shows excellent transparency, adequate flow property, and resistance against various solvents and can either be punched, die-cut, printed or hot stamped. PETG materials are exceptionally durable, have high impact strength, are resistant to chemical changes and are materials of choice for the fabrication of complex and intricate designs. PETG is an altered form of PET that transforms PET from a semicrystalline to an amorphous state, enabling the material to be more transparent and esthetic. The glass-transition temperature (Tg) of the material is around 80°C, allowing better handling of the material with features that resemble glass [60]. The improved transparency, mechanical, and optical properties make PETG a suitable material for the fabrication of clear aligners.
Thermoplastic polyurethane (TPU), primarily composed of di- and tri-isocyanates, and polyols [61] is another extremely versatile polymer that exhibits multiple favourable properties such as excellent mechanical and elastomeric characteristics, chemical and abrasion resistance, adhesion properties as well as simplicity of machining [48,62]. When subjected to load, TPU changes its shape but can recover its original shape when the load is removed and is able to elongate and recover due to the material's flexibility. The material also exhibits high tear resistance and a wide range of resiliency [59]. As stated previously, in 2013 Invisalign aligners transitioned from a single-layer of polyurethane, Exceed-30 (EX30) to a new polymer, SmartTrack™ (LD30)- a multilayer aromatic thermoplastic polyurethane/copolyester [5]. According to Aligntech, the new material should provide the aligners with more elasticity and produce more constant forces, thereby improving their clinical efficacy [49,54]. However, both materials show structural modifications that resulted in increased sample hardness and hyper-plasticity [25]. In terms of clinical outcomes presented by Peer Assessment Rating (PAR) score reduction, there were no significant differences between the two types of aligners [63].
3.2. Polymer blends
Thermoplastic orthodontic clear aligners should ideally exert continuous and controlled forces to produce intended tooth movements [48]. The mechanical properties of the polymers can be improved by mixing different types of polymers such as polyester, polyurethane, and polypropylene. Polymer blends of these three polymers are commonly employed in the commercial manufacturing of clear aligners [48,54]. Multiple studies on thermoplastic polymer blending have shown that polymer blends demonstrate improved mechanical and chemical properties, eventually enhancing the clinical performances of clear aligners [48,[64], [65], [66], [67], [68]].
The ratio employed for blending polymers significantly influences the features of the polymer blend. For instance, blending PETG/polycarbonate (PC)/TPU at a ratio of 70/10/20 resulted in better mechanical properties in comparison to other blending ratios, and was shown to exhibit sufficient and sustainable orthodontic forces than other commercialized products [48]. Similarly, PETG/PC2858 blended at a 70/30 ratio, expressed the best combination of tensile strength, impact strength and elongation at break [67].
3.3. 3D printed aligner materials
The potential advantages and the materials employed for 3D printed aligners were discussed previously. Direct 3D printing can avoid adverse effects of thermoforming processes, such as alteration of mechanical, dimensional and esthetic characteristics of the material [69], offering better geometric accuracy and precision, better fit, higher efficacy and mechanical resistance and reproducibility [45,70]. Materials utilized for 3D printing in orthodontics include acrylonitrile-butadiene-styrene plastic, stereolithography materials (epoxy resins), polylactic acid, polyamide (nylon), glass-filled polyamide, silver, steel, titanium, photopolymers, wax, and polycarbonates [71]. Various studies have investigated the mechanical and biological properties of resins suitable for 3D printing clear aligners [70,72]. Tera Harz TC-85 is a photopolymer material introduced by Graphy to overcome the current limitation of thermoforming sheet type aligners and the Tera Harz direct aligner can be 3D printed directly with a 3D printer. Tera Harz TC-85 is bio-compatible photopolymer material and is available in two colours as clear and white. TC-85DAC (clear) is fully transparent, whereas TC-85DAW (white) provides durability and aesthetics. In addition, Graphy Inc, claims that it can supply customized colours to meet specific needs [73].
3.4. Bioactive materials used with clear aligners
Microbial accumulation is a common problem during orthodontic treatment and studies have demonstrated elevated levels of presence of major oral pathogens, such as S. (streptococcus) mutants and P. (porphyromonas) gingivalis, during orthodontic treatment. Various attempts have been made to increase the antimicrobial properties of orthodontic appliances, and subsequent research on the application of nano-antibacterial materials in orthodontics is also increasing [74].
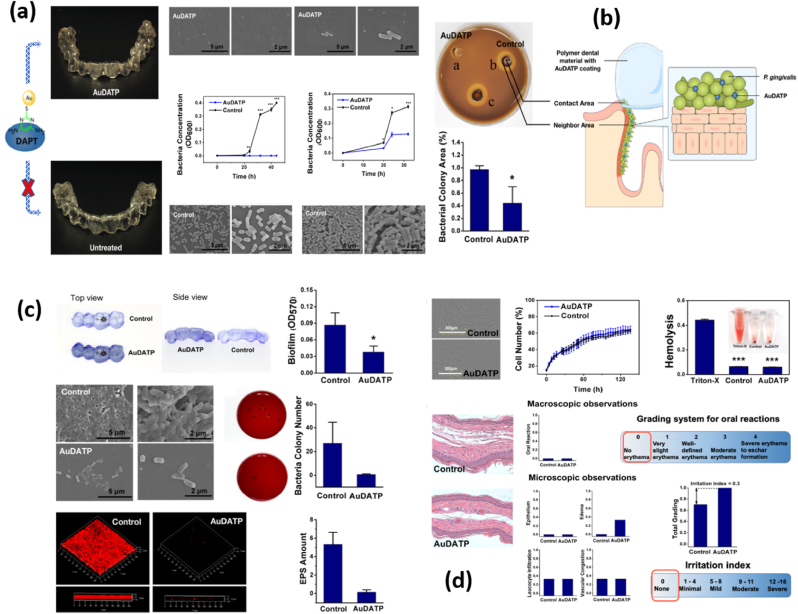
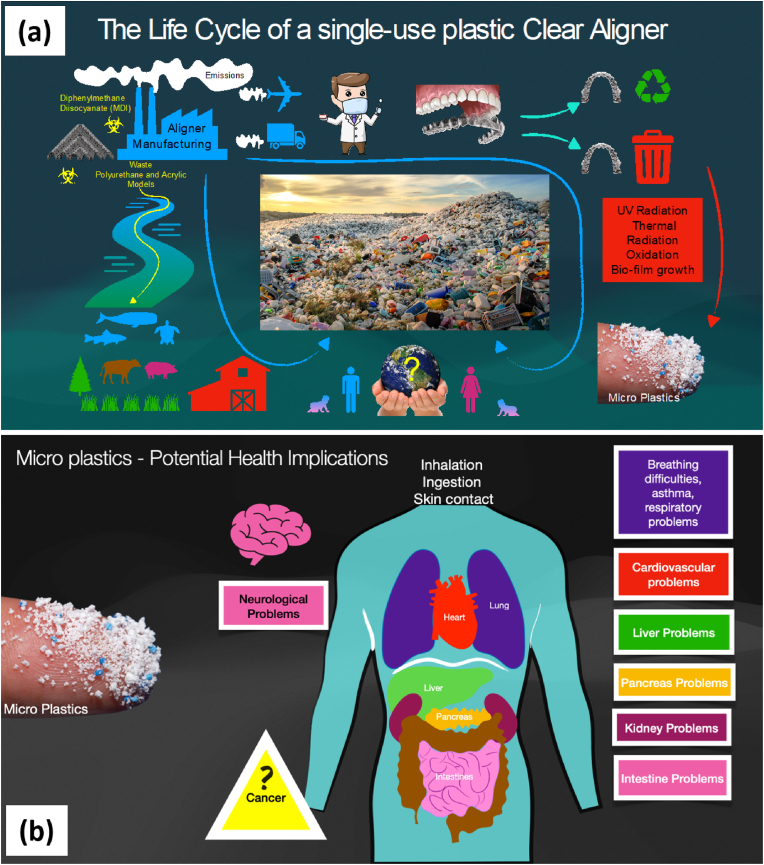
Despite the claims of proponents of clear aligner therapy, who extol aligners as a more hygienic alternative over FA due to the likelihood of facilitating better oral hygiene, the fact that patients’ teeth and gingiva are fully covered with aligners nearly the entire day, (with patients being typically instructed to use aligners 20–22 h a day except for a short removal period for food and cleaning) might increase the risk of bacterial growth and subsequent damage to the teeth and adjacent periodontal tissues. A randomized clinical trial (RCT) [75] that attempted to answer the question-of which orthodontic appliance is best for oral hygiene, clear aligners, self-ligated brackets, or conventional brackets; found no difference among the three treatment groups in terms of short-term (9 months) and long-term (18 months) oral hygiene levels. However, with proper modification, clear aligners may be used as a long-term drug delivery system for patients with P. gingivalis infection [76]. In their pilot study, Zhang et al. coated 4,6-diamino-2- pyrimidinethiol-modified gold nanoparticles (NPs) (AuDAPT) over clear aligners which presented antibacterial effects on a suspension of P. gingivalis, affecting the neighbouring area of the materials, slowing biofilm formation and showing favourable biocompatibility (Fig. 3). The antibacterial action of gold NPs has broadened a new research terrain, while other mechanical, physical, and biological properties of NP-coated aligners still warrant further investigations [77].
Fig. 3.
Gold nanoparticle-modified dental aligner can prevent porphyromonas gingivalis biofilm formation: (a) SEM images of bacterial cells accumulated on the coated AuDAPTs sample surface compared to uncoated control when immersed into bacterial suspension of different density of bacterial suspension (104 CFU/ml and 105 CFU/ml). (b) Comparison of the bacterial growth area ratio of the AuDAPT-coated samples and untreated samples. (c) CV staining images, SEM images, and confocal images of biofilms formed on AuDAPTs and control sample surface. (d) Biocompatibility of AuDAPT-coated aligners compared with control [76].
Worreth et al. have introduced a cellulose-based clear aligner material loaded with essential oils, such as cinnamaldehyde, and the tested material demonstrated antimicrobial properties against Staphylococcus epidermidis as well as S. mutans and S. mitis clinical isolates [78]. A lesser amount of biofilm was noted to be formed at the interface between the growth medium and the coating. In addition to its antimicrobial effect, cinnamaldehyde has been proven to increase the hydrophobicity of some materials, thus potentially decreasing the early adhesion of the biofilm formers and delaying the formation of a mature biofilm.
Due to the limited number of resins available for SLA, attempts to develop acrylic-based potocrosslinkable resins with different compositions and characterization in terms of mechanical, thermal and biological behaviour have been taken [79]. However, current nanomaterials have not yet achieved the perfect balance of antimicrobial effect and biocompatibility. Studies focusing on the application of nano-antibacterial materials in orthodontic aligners are few and should be given more attention [76].
Thermoplastic polymers and polymer blends continue to dominate the commercial clear aligner market and the Invisalign clear aligner system continues to be the most widely used commercial clear aligner system. However, after the expiry of its patent, several clear aligner systems have been introduced. Table 1 has attempted to organize the data from commercial aligner manufacturer websites, material safety data sheets and previously published studies to summarize the material composition, aligner thickness and commercial claims of multiple, globally popular clear aligner brands.
Table 1.
Aligner material specifications, properties and commercial claims.
| No | Clear Aligner Brand Name | Commercial Manufacturer | Aligner Material Composition | Aligner Material Thickness | Aligner Material Properties and Commercial Claims | Associated Software |
|---|---|---|---|---|---|---|
| 1. | Invisalign https://www.aligntech.com/solutions |
Align Technology Inc, San Jose, USA |
SmartTrack™ Material: LD30 A multi-layer aromatic thermoplastic polyurethane from methylene diphenyl diisocyanate and 1,6-hexanediol plus additives |
Aligner thickness stated by the manufacturer after thermoforming is 0.75 mm. |
SmartTrack™ material: applies gentle, constant force to improve control of tooth movement Comfortable and fits snugly around the teeth In comparison to EX30 used previously, LD30 exhibits a more amorphous structure and a greater elastic recovery SmartForce™: customized attachments, bite ramps and power ridges SmartStage™ technology: programs sequential tooth movement to straighten teeth more predictably |
ClinCheck Global cloud-based treatment visualization |
| 2. | Clarity https://www.3m.com/3M/en_US/orthodontics-us/featured-products/clarity-eos/clear-aligners/ |
3 M ESPE Maplewood, USA | 3 M™ Clarity™ Aligners Flex Flexible 5-layer material 3 M™ Clarity™ Aligners Force: Rigid material Proprietary 5-layer copolymer blend |
Flex: 0.625 mm Force: 0.75 mm |
Clarity Aligners Flex indicated a wire-sequencing approach Recommended for correction of rotation and proclination, when used in two-material Clarity Aligners Force indicated for a segmental mechanical approach Recommended for expansion, torque, sequential bodily movement, and segmental intrusion, when used in two-material treatment designs Outer layers resist staining and scratching, inner layers provide flexibility and resilience Overall structure provides durability even with reduced thickness |
Tx Design (TxD) Oral Care portal |
| 3. | Clear Correct https://www.straumann.com/clearcorrect/en/patients/about-the-aligners.html |
Institut Straumann AG, Basel, Switzerland |
ClearQuartz Material: Zendura Polyurethane Tri-layer proprietary material |
0.75 mm | ClearQuartz material features an elastomeric layer between two resilient, low-porosity shells The outer layers allow the aligner to be tough and stain-resistant owing to its low porosity The shells also help grip the teeth firmly The inner layer is engineered to provide consistent and continual force due to its enhanced elasticity and enhances patient comfort ClearQuartz retains 10x more of its initial force than other aligners and retains its shape throughout the wear time of the aligner |
Clear Pilot ClearComm portal |
| 4. | Spark https://ormco.com/spark/ |
Ormco Corporation, Brea, USA |
TruGEN™ and TruGEN XR Material: | 0.75 mm | More sustained force retention Better surface contact area with the tooth More efficient and effective tooth movement Clearer, more comfortable and stains less |
Approver |
| 5. | SureSmile https://www.dentsplysirona.com/en-us/categories/orthodontics/suresmile-aligner.html |
Dentsply Sirona, York, USA |
Essix Plastics: Plus, C plus Polypropylene/ethylene copolymer (>95%), stabilizers (<5%) |
Plus: 0.035 and 0.040 C plus: 0.040 inches/1 mm |
Essix Plus Plastic combines clarity with durability It is effortlessly removed from models and trims with ease Essix C plus: When making retainers and aligners for bruxers, a more flexible plastic provides additional strength to help withstand mastication pressure |
SureSmile Aligner |
| 6. | Argen Clear Aligners https://argen.com-clear-aligners |
Argen Corporation, San Diego, USA |
Argen Clear Aligners are made from premium thermoformed plastic material consisting of elastomeric layer encased in a dual shell construction |
Unspecified | Engineered for a precise fit, ongoing force retention, and exceptional durability Premium Material – a continual force for faster treatment and greater comfort for patients Improved Stain Resistance – starts clear, stays clear The consistent pressure produced by the dual-shell construction accurately moves teeth over the prescribed period of time |
Unspecified |
| 7. | Reveal https://www.henryschein.com/us-en/dental/supplies/reveal.aspx |
Henry Schein, Melville, USA |
Proprietary ClearWear™ material | Unspecified | Provides ultimate in aesthetics with precise force levels for speed of treatment Superior clarity compared to other aligners Guaranteed not to stain or cloud Zero to minimal unsightly attachments |
DDX SLX Approver portal |
| 8. | Nuvola https://www.nuvolaworld.com/nuvola-clear-aligners |
GEO Srl Rome, Italy |
Polyethylene terephthalate glycol (PET-G) | 0.75 mm | Tough and elastic Resistant to the aggressive chemical agent Proof against wear and tear Precisely designed to fit firmly Easy to wear and maintain Fidelity to their original conformation Long-lasting transparency and hygiene |
Unspecified |
| 9. | F22 https://www.f22aligner.com/en/ |
Sweden and Martina Company, Padua, Italy |
F22 Polyurethane: Evoflex: |
0.75 mm | An innovative polymer that ensures up to 17% greater transparency than other aligners on the market | Unspecified |
4. Properties of clear aligner materials
Thermoplastic materials employed for the fabrication of clear orthodontic aligners are primarily polymers that demonstrate differing characteristics and which respond varyingly to the multiple types of stress associated with the oral cavity, such as the mechanical stress associated with functional and parafunctional movements, thermal stress associated with the aligner thermoforming process and with exposure to oral temperature changes and the chemical stress created by exposure to saliva as well as and consumption of various beverages [67,80].
An ideal aligner material should exhibit high resilience, low hardness, sufficient elasticity, adequate resistance to varied stress and distortion, excellent transparency, low cytotoxicity, and high biocompatibility [67]. This paper investigated scholarly literature to comprehensively review how the properties of an ideal aligner material can influence the clinical performance of clear aligners for orthodontic treatment.
4.1. Mechanical properties, stress relaxation phenomenon and the physical performance of clear aligner materials
Thermoplastic materials in general follow Hooke's law when subjected to forces of short duration, indicating that within the elastic limit of the stress-strain curve, when the stress is proportional to strain; the material exhibits an elastic behaviour with a return to its original size and shape on the removal of applied stress [81]. The yield strength of a material can be described as the stress beyond which the strain is no longer proportional to stress and the material will no longer be elastic and instead behave as plastic. The ultimate tensile strength is indicated by the stress at which the material ruptures and the toughness of the material is defined as the energy absorbed by the material before it ruptures, which can be calculated by the area under the stress-strain curve. Thermoplastic materials with higher yield strength, higher ultimate tensile strength and higher toughness are desirable for the fabrication of clear aligners.
The modulus of elasticity or Young's modulus is a measure of the stiffness of a material and can be defined as the ratio between stress and corresponding strain. An aligner material should ideally possess adequate stiffness to exert the forces and moments needed to achieve the planned tooth movement. If the material used for aligner fabrication exhibits a very high modulus of elasticity (or high stiffness), then the resultant aligner would be very stiff leading to difficulty in aligner placement and removal for the patient. Likewise, a material with low stiffness will not be able to generate adequate forces required to move teeth [81].
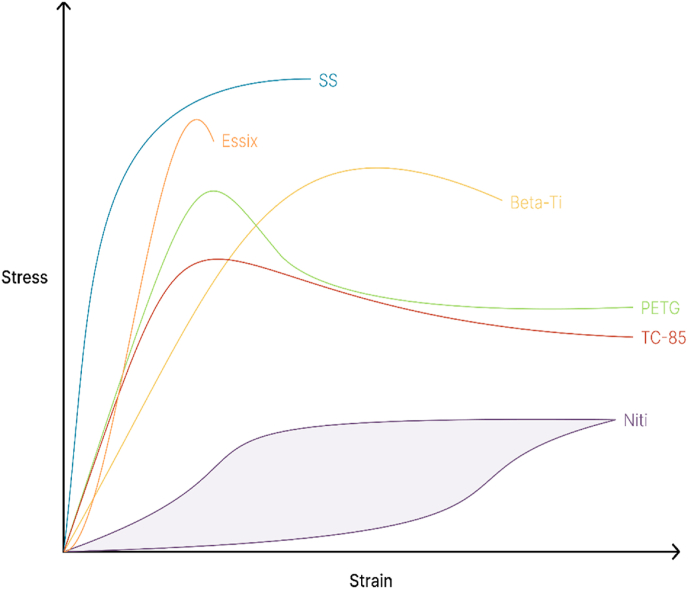
A material that can be easily deformed with minimal force can be described to possess low resiliency, which is the ability of a material to absorb energy when it is elastically “loaded” or deformed, and release that energy when “unloaded,” without causing permanent deformation of the material. The measure of resiliency is the point beyond which the material undergoes some amount of permanent deformation. Unloading can be described as the measure of the force exerted by a material to move teeth [82]. Aligners absorb less energy since they deform permanently under moderate-to-heavy loads [83] and exhibit considerably less resiliency as compared to metal archwires [84]. Clinically, dental crowding that can be resolved by a single nickel-titanium archwire, requires multiple aligners to correct the same. Metal archwires are good at storing energy (loading) and transferring (unloading) this energy to teeth over a period of time while undergoing minimal fatigue. Fig. 4 illustrates a relative comparison of the stress-strain curves of different orthodontic materials [52,81,85,86].
Fig. 4.
An illustration of the relative comparison of the stress-strain curves of different orthodontic materials does not reflect absolute values. It is based on the reference data from the literature [52,81,85,86]. SS, stainless steel. Beta-Ti, Beta titanuim. Niti, Nickel titanium. Essix, clear retainer material. PETG, polyethylene terephthalate glycol (thermoplastic aligner material). TC-85, photocurable resin (3D-printed aligner material).
When thermoplastic materials are subjected to long-term forces, they do not follow Hooke's law, and instead, exhibit ‘viscoelastic’ properties showing a time-dependent relationship between stress and strain [81]. Clear aligner materials are ‘viscoelastic’ in nature, with their properties constituting the middle ground between the properties of purely viscous and purely elastic materials. The behaviour of viscoelastic materials can vary significantly over time when subjected to a load such as the initial placement of an aligner onto the dentition and even before any of the planned tooth movement has been initiated [50]. The little energy that aligners absorb, is then mostly dissipated as heat with a relatively small amount being actually transferred to the dentition. Viscoelastic materials can absorb shock, vibrations, and force [49] and this nature allows the aligner to deform and stretch and generate forces required for the programmed tooth movement when the aligner is fitted onto the dentition.
The deflection of viscoelastic materials increases over time when subjected to constant loads, whereas constant deflection occurs if the load decreases and this phenomenon is termed stress-relaxation [49]. Stress relaxation results in a reduction of the forces exerted by the aligner when placed onto the teeth, maintaining a constant deflection rate before tooth movement begins, and this relaxation depends on the characteristics of the material of aligners and the magnitude of the applied force.
Stress relaxation, a time-dependent decrease in stress under a constant strain, is presumably the most crucial factor in determining the efficiency of clear aligners and can be observed by applying a fixed amount of deformation to material and measuring the load required to maintain it, as a function of time [87]. Stress relaxation is basically a measure of the constancy of force delivered over a period of time [87] and although maintaining a constant force is desirable in orthodontics [88], aligner materials do not seem to provide this admirably. The reduction in force noted with clear aligners is not linear with time, but quite exponential, translating to a dramatic force drop in the first few hours of aligner use, indicative of material fatigue [49]. In comparison, a nickel-titanium archwire at similar or greater stress levels remains active for weeks [89] and this force drop should be taken into consideration while planning treatment with aligners [90,91].
Lombardo and co-authors [49] examined the mechanical characteristics and investigated the stress relaxation of four different types of aligner materials, two single-layer materials based on PETG and polyurethane and two multilayer materials. All the samples were subjected to a constant load for 24 h in a humid environment and at a constant temperature after an initial resistance test. Study results showed that while monolayered materials exhibited significant resistance to absolute stress and stress relaxation speed; the multi-layered ones demonstrated a constant stress relaxation and an absolute stress resistance that was four times lower than that of the monolayered ones. Further, all four materials demonstrated significant relaxation to rapid stress in the first 8 h, which tended to plateau for some materials and decreased for others at a 24-h point. The polyurethane-based monolayer material produced higher initial stress values and a high decay rate, whereas monolayer PETG material showed the most significant stress relaxation rate during the 24 h. Multilayered materials generally displayed lower stress relaxation rates and lower initial stress values than monolayered materials.
In clinical situations, aligners are subjected to both short-term and long-term forces in the oral cavity. When an aligner is fitted onto the dentition, the aligner material is loaded with short-term forces, after the immediate fit-in. On the other hand, when the aligner is worn by the patient for a significant duration, it experiences long-term forces due to the displacement caused by the planned tooth movement and the reactionary forces generated by the musculoskeletal system [92].
With time, the force generated by the aligner material for the same deformation, decreases, due to its viscoelastic nature. This stress relaxation process is affected by the actual composition of the thermoplastic material, the temperature of the oral cavity, the magnitude of the force to which a specific part of the aligner is subjected to as well as the thickness of the material used for the fabrication of the aligner [80]. Further, the forces that aligners apply must be within the biological limitations of what human teeth can tolerate. These stress values can also help with the selection of the thickness of the aligner sheet.
Polyether compounds have been found to be tougher than polyester urethanes and have greater moisture resistance and dynamic characteristics. They also perform better at low temperatures. On the other hand, polyether materials have the lower abrasion resistance and are more likely to tear [93].
The factors highlighted above provide a fundamental understanding of the key features of clear aligners in terms of force delivery, magnitude, constancy, and decay. Aligners can be summarized to display the following characteristics: (i) apply low forces; (ii) perform better with lesser activations; (iii) exhibit low flexibility; and (iv) undergo rapid force decay [42].
4.2. Thermal properties and the influence of the thermoforming process on clear aligner behaviour
Thermoplastic materials are linear or slightly branched polymers with strong intramolecular covalent bonds and weak intermolecular Van der Waal's forces. These bonds melt and the polymers overflow at elevated temperatures and the molecular chains subsequently solidify into new shapes when cooled. Thermoplastic materials do not undergo further chemical changes at altered temperatures, hence the process of softening with heating and hardening with cooling may be repeated. In solid-state, the thermoplastic materials used for making clear aligners are semi-crystalline with amorphous strands of polymers dispersed in between. The crystalline polymers are more transparent with well-defined melting points and glass transition temperature [49]. The ability of the aligner material to adapt or conform to the models during the thermoforming process is an important requirement of an aligner material. At a defined temperature of around 110 °C, the adaptation ability of polyurethane material has been found to be superior to that of other materials [94,95].
Multiple studies have elucidated that the transparency, hardness, and thickness of aligner material, exhibit changes after being subjected to the thermoforming process during clear aligner fabrication [69, 96]. Ryu et al. [69] investigated the thickness and the transparency of aligner materials before and after the thermoforming process and demonstrated changes in four different types of clear aligner materials (two of which were copolyester-based: Essix A+ and Essix ACE, and the other two, PETG-based: Duran and ECligner). Study results revealed that thermoforming reduced the transparency of thermoplastic materials. Post-thermoforming, the transparency of the eCligner samples of 0.5 and 0.75 mm thickness respectively, was remarkably reduced compared to that of Duran and Essix A+ samples of the same thickness. The 0.75 mm thick Essix ACE sample, exhibited a significant reduction in its transparency as compared to the Ecligner material of 0.75 mm thickness. Similarly, the transparency of Duran and Essix A+ samples were found to be significantly lower after the thermoforming process. The study results also showed that the hardness of all four materials did not show a significant difference compared to their pre-thermoforming values. A significant increase in solubility in water was noted for Duran, Essix A+ and Essix ACE samples, unlike the eCligner sample, and the hardness of Essix A+ and Essix Ace samples was also noted to be lesser than that of the eCligner sample after thermoforming. Finally, Essix A+ and Essix ACE samples showed higher surface hardness post the thermoforming process.
Another study by Bucci and co-authors [96] in 2019, investigated two types of aligners, a passive and another active PETG material of 0.75 mm thickness, and found that the thermoforming process altered the thickness of clear aligners. After the thermoforming procedure, variable thicknesses were noted throughout the occlusal surface of the clear aligner ranging from a minimum value of 0.38 mm to a maximum of 0.69 mm and these values were lower than the 0.75 mm thickness of the original PETG sheets before being thermoformed. However, the authors mentioned that the variation in thickness does not seem to adversely affect the clinical performance of clear aligners.
An in vitro study by Dalaie and co-authors [97] investigated the changes in the thermomechanical properties of two PETG aligner sheets of two different thicknesses, 1 and 0.8 mm, after the thermoforming process; and concluded that the hardness of the material decreases by about 7.6% after thermoforming, for both types of material.
Thermoplastic polymers exhibit a Tg at which their rigid state transforms into a rubbery state. When the thermal properties of three commercial clear aligners (Invisalign [Align Technology, Inc., Santa Clara, CA, USA), Simpli5 [Allesee Orthodontic Appliances, Sturtevant, WI, USA], and ClearCorrect [ClearCorrect, Round Rock, TX, USA]) were compared, all three aligner systems were found to have a Tg above the accepted oral maximum temperature, with no significant differences observed before and after their clinical usage [98].
4.3. Optical properties, colour stability and clear aligner transparency
Aligner materials should exhibit good light transmittance and should ideally be able to transmit at least 80% of visible light for optimal clarity. Amorphous thermoplastic polymers exhibit high translucency and are thus preferred as clear aligner materials over crystalline polymers that are highly opaque and unaesthetic. Polyurethane, polyester, polyvinylchloride, polysulfone and polycarbonate are some of the polymers that demonstrate optical properties well suited for commercial aligner fabrication [99].
Aesthetics has played a vital role in the increased acceptance of clear orthodontic appliances and the transparency of a clear aligner is expected to remain consistent over a period of at least one to two weeks of intra-oral usage prior to an aligner change [33]. However, the transparency and colour stability of clear aligners are known to be affected by the consumption of coloured beverages, exposure to ultraviolet radiation, and use of mouthwashes [100].
Although clinicians recommend that patients remove their aligners to eat or drink (except water) to avoid pigment adsorption by the thermoplastic material, studies have demonstrated that often, many patients ignore these recommendations and consume food and/or beverages with the aligners in place, thereby undermining their transparency and consequentially their esthetics [100]. At least one study revealed that almost 50% of patients did not remove their aligners for eating and drinking [33].
Multiple studies have investigated the colour stability and transparency of clear aligners when exposed to colouring agents and saliva [33,97] evaluating various clear aligner materials such as multi-layered thermoplastic polyurethane with integrated elastomer (SmartTrack™), PETG material (Erkodur), co-polyester material (Essix ACE), two PET-based materials (Essix Plastic and Ghost aligner) and resin-based polyurethane material (Zendura). Visual inspection results on colour stability indicated that all the types of materials showed no colour change after 12 h of contact with colouring agents such as wine, coffee, black tea, cola and nicotine, except for SmartTrack™ material that displayed colour changes when subjected to coffee and red wine [33,97].
When the exposure time was increased to 7 days to different colouring agents, all the aligners showed only slight colour changes, however, immersion in coffee and black tea solution created a significant colour change for all the materials. Erkodur and SmartTrack™ samples displayed marked colour changes to coffee and black tea solution and SmartTrack™ also exhibit a substantial colour change after 7-day immersion in red wine. Immersion in a nicotine solution for 14 days, resulted in only minor colour changes for all the samples, whereas immersion in red wine for 14 days revealed enhanced colour variation, especially for Zendura and Essix P [33,97].
The colour change values of polyurethane-based Invisalign aligners have been found to be much higher than those noted for polycarboxylate and PETG-based aligners. Various studies have concluded that polyurethane is more susceptible to pigment adsorption and does not provide adequate colour stability. A clearer aligner was rated as more attractive, and a lower level of appliance display has been mentioned as necessary for societal acceptance [94,95].
4.4. Chemical resistance properties, the influence of the oral environment and clear aligner aging
Clear aligners are constantly exposed to saliva and its various enzymes apart from the temperature variations in the oral cavity and they are also sporadically exposed to beverages apart from water, all of which can adversely affect the chemical composition of their constituent thermoplastic polymers, thereby altering the aligner shape and/or its mechanical properties over time. Certain polyesters such as polycarbonates and polyamides may exhibit irreversible hydrolysis that may lead to the eventual degradation of their polymer structure, hence it is desirable that the polymers used for clear aligner fabrication are resistant to hydrolysis and water degradation [81].
An aligner is also subjected to continuous and intermittent forces associated with normal oral functions such as chewing, speaking, swallowing and parafunctional activities such as teeth clenching and grinding. An aligner material should be durable when exposed to the oral environment and possess high wear resistance to withstand masticatory and associated stresses to avoid distortion that can compromise its clinical performance [81].
Microcracks, delaminated areas, calcified biofilm deposits, and loss of aligner transparency have all been reported in Invisalign aligners that were used for 2 weeks [28,101]. An alteration in the fit of the aligner and a change in the resultant orthodontic forces exerted by the aligner can occur can as a result of intraoral hygroscopic expansion. Water absorption of thermoplastic materials has been shown to increase with time, with Invisalign aligner material showing the highest absorption values followed by PETG [102].
The temperature of the oral cavity can rise to 57 °C after the consumption of a hot beverage and it may take several minutes for it to return to its original temperature. These temperature changes have also been shown to affect the mechanical properties of thermoplastic materials [61], as evidenced by multiple in vivo and in vitro studies [61,96,97,102].
An in vitro study [102] compared eight different types of most commonly used thermoplastic materials (PETG (Duran), PC (polycarbonate, Imprelon”S″), PP (polypropylene, Hardcast), PUR (polyurethane, Invisalign), A+ (Copolyester, Essix A+), C+ (polypropylene/ethylene copolymer, Essix C+), PE (polyethylene, Copyplast), and EVA (ethylene-vinyl acetate copolymer, Bioplast)) from multiple commercial manufacturers and immersed them in a solution created to simulate the oral environment to assess the influence of oral environment on thermoplastic materials. The authors found that the elastic modulus of PETG, PC, and Essix A+ exhibited significant increases compared to the original samples on exposure to the intraoral environment, contrarily, the elastic modulus of PP, Essix C+, PE and EVA exhibited a significant reduction as compared to the original samples. No significant changes were observed in the PUR material. The same study also found an increase in the overall thickness of all thermoplastic materials due to water absorption.
The resistance of the thermoplastic material to surface cracking, when exposed to an oral environment comprising of cyclic stress is of paramount importance. Dalaie and co-authors simulated the temperature variations that occur in the oral environment through intermittent thermal cyclers for 22 h per day for 14 days and studied how the hardness, thickness and flexural modulus of two aligners (in PETG foil with thicknesses of 1 mm and 0.8 mm) vary in contact of the oral environment. Significant variations in hardness were noted only in the 0.8 mm thick PET-G sheet; not in the 1 mm ones This variation was attributed to changes in the crystalline and amorphous structures of the polymers or the release of plasticizers due to exposure to intermittent thermal cycling [97].
Another study [61] evaluated three thermoplastic materials- PETG (Duran), PP (Hardcast), and PU polymers (PU1, PU2, PU3) with different Tg and different crystalline structures and noted that the mechanical properties of each material were significantly reduced after 2500 thermal cycles. A significant decrease was observed for Hardcast material (crystal plastic) which had the highest Tg (155.5°) and PU1 (crystalline or semicrystalline plastic) with the lowest Tg (29.6 °C). Duran (73.3°), PU2 (56.5°) and PU3 (80.7°), with intermediate Tgs, exhibited more stable mechanical properties. The authors concluded that the mechanical properties of all thermoplastic materials decreased with the gradual temperature changes and that polyurethane polymers exhibited excellent shape memory throughout the range of intraoral temperature variations.
An in vivo study conducted by Bucci et al., in 2019 [96] considered the temperature variations in the oral cavity along with normal oral functions and parafunctional habits to which clear aligners are subjected. A series of passive and active aligners formed from PETG sheets were utilized in this study. Patients were instructed to wear these aligners for 22 h per day for 10 days and the study evaluated changes in aligner thickness over time. The authors found small reductions in the thickness of the aligners after 10 days but stated that these were not significant enough to affect the clinical performance of the clear aligners and opined that PETG demonstrated adequate stability in the oral environment.
4.5. Biocompatibility and cytotoxicity of clear aligners materials
As an intra-oral appliance material, thermoplastic polymers are expected not to leach out any potential toxins that may produce adverse local or systemic reactions, not be carcinogenic in nature and not produce any developmental defects [61].
The paucity of evidence-based literature due to few controlled trials with clear aligners and contradictory results mentioned in published literature continues to fuel the debate about the possibility of potentially toxic effects associated with the use of invisible aligners. Furthermore, the ever-burgeoning influx of multiple commercial aligner systems necessitates the continued need to test the cytotoxicity of orthodontic clear aligners produced by various manufacturers [50].
Allareddy and co-authors have summarized the adverse clinical events reported during the use of Invisalign aligners according to a retrospective analysis by the FDA. The most frequently reported adverse events associated with aligners, during a ten-year observation period included difficulty in breathing, sore throat, swollen throat, swollen tongue, hives, itchiness, and anaphylaxis [103].
Some in vitro studies have evaluated the potential cytotoxicity of thermoplastic materials used for the fabrication of various commercial clear aligner brands. The International Standards Organization (ISO) recommends the in vitro use of Human Gingival Fibroblasts (HGFs) cell lines to verify the biocompatibility of dental materials [104], as these cells are the primary cell lines present in the intra-oral tissues and are the most exposed to any toxic effects of the dental materials such as when the plastic aligners are in intimate contact with the periodontal tissues during patient use.
Ahrari and co-authors [105] investigated the cytotoxicity of four aligner materials- Duran (Germany), Biolon (Germany), Zendura (United States), and SmartTrack™ (United States) and found that Biolon showed the highest toxic effects on HGFs, followed by Zendura and SmartTrack™. Duran exhibited the lowest levels of toxicity. Table 2 shows that all the materials tested in the study exhibited low in vitro toxicity on the tested cells [104,[106], [107], [108]].
Table 2.
A summary of cell viability (cytotoxicity) at each time point (7 or 14 days) or solution concentrations (5%, 10%, and 20% vol/vol) of different clear aligner materials.
| Brand | Category | Composition | Cell viability (%) | Days or final solution concentration (% v/v) | Cytotoxicity |
|---|---|---|---|---|---|
| Duran [104] (Scheu-Dental GmbH, Iserlohn, Germany) |
Thermoformed | Polyethylen terephthalate glycol (PETG) |
84.6 ± 4.02 | 14 days | Slight |
| Biolon (Dreve Dentamid GmbH, Unna, Germany) |
Thermoformed | Polyethylene terephthalate glycol (PETG) |
64.6 ± 3.31 | 14 days | Slight |
| Zendura (Bay Materials LLC, Fremont, CA, USA) |
Thermoformed | Polyurethane resin (PU) |
74.4 ± 2.34 | 14 days | Slight |
| SmartTrack™ (Align Tech, San Jose, CA, USA) |
Thermoformed | Multilayer aromatic thermoplastic polyurethane/copolyester | 78.8 ± 6.35 | 14 days | Slight |
| E-Guard [106] (EnvisionTEC, Rockhill, SC, USA) |
3D printed | Photopolymer | 75.06 ± 8.98 | 7 days | Slight |
| Dental LT (Formlabsinc) |
3D printed | Photopolymer | 77.74 ± 3.22 | 7 days | Slight |
| SmartTrack™ (Align Tech, San Jose, CA, USA) |
Thermoformed | Multilayer aromatic thermoplastic polyurethane/copolyester | 94.07 ± 3.00 | 7 days | No |
| TC85A [107] (Graphy, Seoul, South Korea) |
3D printed | Photopolymerizable polyurethane | 97.6 ± 14.6 98.3 ± 15.9 92.0 ± 13.0 |
5% 4 10% 8 20% h |
No No No |
| SmartTrack™ [108] (Align Tech, San Jose, CA, USA) |
Thermoformed | Polyurethane | 82.6 ± 13.6 60.3 ± 8.8 54.5 ± 23.1 |
5% 7 10% 2 20% h |
Slight Slight Moderate |
| Eon (Eon Holding, Amman, JO) |
Thermoformed | Polyurethane resin (PU) |
85.1 ± 18.3 54.8 ± 16.8 60.4 ± 20.7 |
5% 10% 20% |
Slight Moderate Slight |
| Suresmile (Dentsply-Sirona, Charlotte, NC, USA) |
Thermoformed | Polyurethane resin (PU) |
85.4 ± 16.4 70.7 ± 15.8 56.8 ± 11.3 |
5% 10% 20% |
Slight Slight Moderate |
| Clarity (3 M, St Paul, MN, USA) |
Thermoformed | Polyurethane resin (PU) |
89.3 ± 15.0 72.9 ± 21.1 71.8 ± 15.4 |
5% 10% 20% |
Slight Slight Slight |
Cytotoxicity: No, cell viability more than 90%; Slight, cell viability 60%–90%; Moderate, cell viability 30%–59%; Severe, cell viability less than 30%.
Eliades et al. [109] evaluated the potential release of Bisphenol-A (BPA) from the thermoplastic material used for the fabrication of Invisalign aligners and demonstrated the non-existence of any estrogenic and toxic effects of aligner material on HGFs, which was in contrast to the slight toxicity levels documented by the previously mentioned study by Ahrari et al. [105].
Alexandropoulos and co-authors [110] have mentioned that the chemical composition of thermoplastic materials does not include elements necessary for the release of BPA and it is Isocyanate and not BPA, which is the component that could cause potential adverse effects. Another study found that tissue exposure to isocyanate release from Invisalign aligners can trigger deleterious oral health effects such as allergic contact reactions. On contacting oral tissues, isocyanates react by rapidly binding to cellular proteins and biomolecules, creating an immunogenic event that leads to a sensitization reaction in humans. Experiments have shown that the contact of the gingival epithelial cells with the thermoplastic material in a saline-based environment provoked an interruption of the membrane integrity, reduced cellular metabolism and reduced cell-cell contact capacity. However, these reactions did not occur in artificial saliva. Such studies provide valuable inputs in evaluating and controlling the cytotoxic effects of thermoplastic materials used for clear aligner fabrication [111]. A systematic review of the biological effects of 3D resins used in clear aligners or retainers also reveals that the evidence of the release of bisphenol A and other monomers, either in vitro or clinical studies, remains ambiguous due to few robust results in the current literature. There is an absolute need for further studies in these domains, especially given the possible implications for the fertility of young patients [112].
5. Emerging trends
5.1. Shape memory polymers
The efficacy of conventional aligner materials is restricted by the rate-limiting staging of the amount of tooth movement planned and built into an individual aligner [80,[113], [114], [115]] and material manufacturers aim to continually improve material type and resultant properties, thereby creating novel materials that can play an active role in the fabrication of orthodontic appliances [116]. Materials that can respond appropriately to various types of external stimuli such as electrical, thermal, or magnetic impulses among others, and generate a predictable and repeatable response are known as smart materials or stimuli-responsive materials [117].
Shape memory materials constitute a subset of smart materials that can display an alteration in their macroscopic shape upon the application of an appropriate stimulus; retain this temporary shape stably and recover back to their original shape on the re-application of another stimulus [118,119]. Shape memory polymers (SMPs), alternatively known as actively moving polymers, in turn, constitute a sub-category of shape memory materials [119,120]. The shape memory mechanism of SMPs relies on two crucial traits-the presence of a stable polymer network that determines the original shape of the material and a reversible polymer network that allows the material to transform to an altered or a temporary shape [121,122].
SMPs can display low density, considerable elastic deformation and high chemical stability; can be programmed to display adjustable physical properties and are relatively transparent, thus making them well suited to function as a novel clear aligner material, with the resultant aligner exhibiting a potential ability for significant self-shape recovery [116,123]. The shape memory effect in SMPs relies on the presence of a two-domain system that possesses two different glass transition temperatures; wherein one of the two domains is hard/elastic at room temperature and the other one is soft/ductile [124]. The shape memory mechanism in SMPs responsive to thermal stimuli relies on a reversible activation and deactivation of a polymer-chain motion in the switching segments respectively above and below a specified temperature termed as the transition temperature - that could either be their glass transition temperature or their melting temperature [116,122,125]. On reaching the transition temperature, the deformed shape memory material displays an elastic property to recover back to its original shape and this shape recovery in turn can generate forces that are able to produce orthodontic tooth movement [126].
SMPs could display more than one temporary shape, due to an extended shape recovery temperature range and a much higher recoverable strain level [121,127]. Shape memory polyurethane resins comprise polar and non-polar molecules that can distinguish into microdomains of hard and soft segments, the combination of which allows the material to achieve both high strength (from the hard segments) and high toughness (from the soft segments), facilitating the fabrication of durable orthodontic aligners that can move teeth over extended periods of time [128,129]. Further, the polyurethane resin is resistant to stain depositions enabling the aligner to stay clear in the intra-oral environment for a greater duration.
Elshazly and co-authors [130] conducted a preliminary, in vitro investigation of a clear aligner fabricated from thermal-responsive SMPs, to overcome the rate-limiting staging restriction of conventional aligner materials and demonstrate the possibility of using a single shape-memory aligner instead of three successive conventional aligners to achieve planned orthodontic tooth movement. This study involved the creation of a custom-made aligned typodont model with a movable upper central incisor and the generation of resin models utilizing orthodontic software and a 3D printer. Aligners were then fabricated by thermoforming ClearX sheets (0.76 mm thick, shape memory sheet material, supplied by Kline-Europe GmbH, Düsseldorf, Germany) on the resin aligned model and each aligner was tested for repositioning of the movable central incisor on the typodont model.
ClearX system sheets are fabricated from a thermo-responsive, shape memory, polyurethane-based thermoplastic material, which the manufacturers claim, possesses the ability to recover to its original thermoformed shape after a reforming step of thermal activation at a certain temperature for a pre-defined time duration. Initiation of the shape memory recovery was achieved by subjecting the aligner to an activation cycle by placing it in an activation device known as ClearX aligner booster (v. 2.1, Kline-Europe GmbH, Düsseldorf, Germany), a programmed electric device, that can be wirelessly connected and controlled by a mobile application (ClearX Mobil App. v. 1.1.4, Kline Europe GmbH, Düsseldorf, Germany), developed to create the needful medium required for the shape memory aligner to regain its original shape. The activation was achieved by immersing the aligner in hot water at 67C for 10 min within the container of the ClearX booster device. Models were scanned after each step and the corrective movement was measured through the superimposition of scans. Study results showed that the total correction efficiency of the aligner fabricated from the SMP material was approximately 93% (1.76 mm), with a corrective movement of 0.94 ± 0.04 mm after the reforming step, 0.66 ± 0.07 mm after the first activation step, and 0.15 ± 0.10 mm after the second activation step [130].
The authors [130] mentioned that although the results were promising, this study could only be considered as a proof of concept, due to the multiple limitations of an in vitro, typodont-based investigation. The study postulated that shape memory polymer materials could increasingly be used for the fabrication of orthodontic aligners and could enable the fabrication of a single shape-changing aligner that may be able to replace up to three successive conventional aligners. Consequently, the number of aligners used per orthodontic treatment could be reduced, reducing overall fabrication costs and the duration required for the correction of complex malocclusions [[131], [132], [133]] along with a reduction in the consumption of plastic. The study concluded that aligners made of SMPs could thus be a promising future choice for orthodontic clear aligner therapy.
5.2. 3D printed clear aligners
The current workflow for fabricating a series of clear aligners from a model either obtained from an impression, or a direct 3D intraoral scan, is cumbersome, labour intensive, and expensive [19,134,135]. Furthermore, studies have shown that the thermoplastic process employed for the fabrication of clear aligners can have several deleterious effects on the properties of the aligner material [44,69,96]. This has propelled the need for a more viable alternative to the conventional, thermoplastic, aligner fabrication process, which is currently being tested in the form of 3D direct printed clear aligners [44] using suitable resins.
3D printing, alternatively termed additive manufacturing, was conceptualized in the 1980s and now finds several applications in multiple disciplines of dentistry that enable dentists to custom design and print dentures, orthodontic appliances, maxillofacial prostheses and orthognathic surgical guides [49]. Fig. 5 & Fig. 6 demonstrate clinical applications of 3D printing of a surgical guide and the use of 3D printed stent in orthodontically treated multidisciplinary cases, respectively.
Fig. 5.
A multidisciplinary case treated with orthodontic appliance and 3D direct printed stent aided periodontal surgery. (a) Intra-oral photos before treatment. (b) Intra-oral photos after treatment. (c) 3D design simulates the amount of crown lengthening procedure. (d) 3D printer and 3D direct printed stent. (e) Frontal close-up view of before, during, and after the procedure. (f) Frontal smiling photos before and after orthodontic-periodontal combined treatment.
Fig. 6.
A multidisciplinary case treated with orthodontic appliance and 3D Digital Smile Design, digital wax-up and direct printed periodontal crown lengthening guide, and restorative stent for injection moulded composite restoration.
3D printing permits a layer-by-layer production of pieces, rather than relying on machining, moulding, and other subtractive methods [136]. An application of 3D printing during the production of thermoformed clear aligners is the 3D printing of the dental model on which an actual clear aligner is later thermoformed; this process led to a reduction in geometric inaccuracies and other errors associated with manual impression making [42]. Just as digital impressions and 3D printing of models proved superior to manual impressions and plaster models, clear aligners that are 3D printed directly may eliminate the cumulative errors resulting from analog impressions and the subsequent thermoplastic workflow [42]. Direct 3D printing shows promise for greater accuracy, shorter supply chains, significantly shorter lead times, and lower costs apart from being a more sustainable process that generates significantly less waste than subtractive and thermoforming processes [43]. 3D printed aligners are supposed to have better fitting accuracy compared with thermoforming clear aligners since some studies have reported significant changes in material properties due to the thermoforming process, which will decrease the force and regular thickness and affect the fitting accuracy of the aligners [45,69,134]. While a study examining the accuracy of 3D printed retainers compared with conventional vacuum-formed and commercially available vacuum-formed retainers has shown that average differences of the conventional vacuum-formed retainers ranged from 0.10 to 0.20 mm. The commercially available and 3D-printed retainers had ranges of 0.10–0.30 mm and 0.10–0.40 mm, respectively. The 3D printed retainers showed the greatest deviation although it is accepted to be clinically sufficient [137]. Despite the advances in different 3D printing technologies, there is a dearth of suitable materials for such printing for clinical use and consequently, literature on the materials and their properties is scarce as well.
Jindal and co-authors [42], successfully 3D printed a 0.75 mm thick clear aligner utilizing Dental LT (Long Term) clear resin (FormLabs, Somerville, MA, USA) and found the direct-printed aligner to be geometrically more accurate, display greater resistance to maximum load with low displacement, deform elastically with reversibility for lower displacements as compared to conventional thermoformed clear aligners fabricated from Duran foils. The authors also reported that LT clear resin performs comparably to thermoplastic materials when subjected to mechanical stress of non-linear compressive forces equivalent to human bite cycles [42], making it a suitable clinical alternative. Dental LT resin is an approved Class IIa biocompatible material with high resistance to breakage and is ideally suited for the fabrication of gnathological splints, orthodontic retainers, and other rigid direct-printed orthodontic appliances as functional appliances. However current studies do not provide clinical data for evaluating the performance of Dental LT resin as a clear aligner material in the oral environment [70].
Several preliminary studies are now evaluating various aspects of 3D printed clear aligners. The thickness of a thermoformed aligner influences the magnitude of force it delivers to generate optimal tooth movement and performance and 3D printing represents a complex method in controlling the thickness of dental aligners and subsequently the exerted force. Edelmann et al. reported an increase in overall aligner thickness than the corresponding design file, especially with LT clear resins [40]. The results obtained in the study showed that the 3D printing workflow did not precisely realize the designed thickness with clear material and it may produce deleterious effects on the clinical utility of aligners. Cole et al. have set the thickness of the 3D printed retainer to be 0.75 mm with a 0.25 mm offset to allow full seating in their pilot study [137]. What will be the ideal amount of compensation for the increase in thickness in 3D printed aligners might be different in terms of materials and protocols and need further investigation.
Deviation in the dimensional accuracy of the printed aligners can result in undesired tooth movement. One of the factors responsible for the adaptation between the aligner and the teeth is the print orientation and the post-print curing duration. Jindal et al. evaluated the effects of post-curing conditions on the mechanical characteristics of printed aligners and demonstrated that time and temperature are extremely important in the compression load resistance of the printed resin [42]. The correct post-curing process is essential to provide sufficient strength and biocompatibility for the final 3D printed product. Allowing for extra cross-linking of the polymer, ultimately enhances the mechanical properties of the printed material and reduces any residual stress.
3D printed materials are highly toxic before 3D printing, and the toxicity gradually decreases post-polymerization. Post curing and processing are vital for eliminating the toxicity levels as recommended by the manufacture of 3D printing material [106]. A study compared the cytotoxicity of direct 3D printed clear aligners to Invisalign aligners [138] and found that the Invisalign aligner material was the least cytotoxic, followed by Dental LT clear resin (Form Labs, Somerville, MA, USA) and Accura 60 SLA (3D Systems, Rockhill, SC, USA) and the latter two materials are not approved for direct printed clear aligners as yet. A recent, in-vitro study of cell viability by Ahamed et al. similarly showed that Invisalign material was found to be more biocompatible than directly printed aligner materials [106]. Cytotoxicity for direct 3D printed aligner materials was found to be more on the first day and then found to decrease gradually. These results suggest future studies are essential to evaluate 3D printed aligners clinically to determine their properties in an intra-oral environment (Table 2).
In September 2021, South Korean manufacturer Graphy showcased the world's first direct 3D-printed aligner, produced from the company's own 3D printing resin, which claimed to be equipped with a shape memory function, that according to Graphy, is the only one available on the current market. The company further mentioned that Graphy's aligners can be produced using any 3D printer. Owing to the direct production process, no printing models or vacuum forms are needed, resulting in time and cost savings. Moreover, this printing process reduces carbon emissions and produces less refuse because no cutting is needed, which benefits the environment [52].
Another benefit claimed by Graphy aligners is the opportunity for thorough disinfection. “Most companies do not recommend brushing their aligners because, if they get scratched, bacteria might enter, and this makes additional cleaning agents necessary,“. Graphy recommends brushing its aligners. The material is able to stay in hot water of up to 100 °C for 1–2 min, and this also helps with disinfection. Another feature claimed by the manufacturer includes the ability of the aligner to rotate teeth by up to 35°, which other aligners struggle to achieve. Although the product has CE certification, 510k clearance from the US Food and Drug Administration is pending [52,73].
With the rapid emergence of new direct 3D printing aligner materials and the increasing cost of commercial clear aligners, dental practitioners have become more interested in 3D printed in-house (3DPIN) aligners. 3DPIN aligners do have potential strengths, however, any commercially introduced resin must be tested extensively to demonstrate the practical effectiveness of its 3D printed aligner in a clinical environment. The different processes must be utilized to create customizable thicknesses and attachments; and the mechanical properties of these customizable aligners with regards to their materials, thickness, and auxiliary elements should be investigated by parametric modelling and finite element analysis among others [139]. Fig. 7 shows a clinical case treated with 3DPIN aligners. Can et al. [140] have attempted to investigate alterations in the mechanical properties (Martens hardness (HM), indentation modulus (EIT), elastic index (ηIT), and indentation relaxation (RIT)) of orthodontic 3DPIN aligners after intraoral aging and found that after 1 week in service period the mechanical properties were not affected. While the current state of published literature about directly printed clear aligners shows that such a process is technically possible, no commercially approved material marketed for this purpose exists and consequentially clinical studies on these aligners are yet to be published in current literature. Based on these premises, further in vitro and in vivo studies are needed to test these new technologies and materials. Special care must be taken concerning the cytotoxicity of printable resins and clinical performances of direct clear aligners must be evaluated to compare the obtained data with those of thermoformed aligners.
Fig. 7.
A relapsed anterior open bite case treated with modified 3DIH aligners (Graphy, Seoul, South Korea) with biting springs. (a) Digitally designed modified clear aligner with OnyxCeph3™ (Ghemnitx, Germany). (b) Frontal view after relapse. (c) Frontal view after retreatment, anterior open bite is closed. (d) Preview of the virtually designed model with the inclusion of supporting structures to facilitate printing. (e) Aligners printed with TC-85 (Graphy) on the build platform of a stereolithography 3D printer (SprintRay Pro, SprintRay, Los Angeles, CA, USA). (f) The final modified 3DIH aligners including 0.036″ TMA wires.
5.3. Bioactive aligner materials
Besides the application of nanoparticles in clear aligner materials for microbial inhibition described previously [76], rapid development in the synthesis of novel bioactive materials that have a wider range of applications has also been mentioned in the literature [[141], [142], [143]]. The most noticeable examples of bioactive materials are glass ionomers and composite resins modified with hydroxyapatite, bioactive glass, and other compounds [[143], [144], [145], [146]]. These biocompatible products are constructed to release various kinds of ions, such as fluoride, calcium, and phosphorus when used intra-orally. These ions are capable of initiating the remineralization and restoration process and inhibiting demineralization. In particular, fluoride ions can act as effective anticaries agents, and various dental materials have been modified to prolong the fluoride-releasing action of resins by adding fluoride salts and incorporating NPs of calcium fluoride, F-PRG, and S-PRG [147].
Raszewski et al. [148] created novel dental materials for 3D printed orthodontic splints enriched with novel bioactive glass fillers of different compositions and assessed their physical properties, cytotoxicity effects, solubility, capacity to release fluoride ions, elution of nanpolymerized components, and their influence on cell cultures. The experiment results showed that modification of methacrylate resin, used in 3D printing technology, with bioactive glasses can produce novel dental materials that possess desirable bioactive properties. However, the modified materials are characterized by a moderate decrease in physical properties and mild cytotoxicity on direct contact with human fibroblasts. Leaching of nonpolymerized components was also detected. Such indictive attempts may direct future studies on synthesizing unique bioactive 3D-printed aligner materials.
5.4. Plastic aligners and the environment
Any discussion on plastic waste dumped into the ocean and climate change typically begins with a stifled yawn and concludes with a self-consolation that everything somehow will eventually work out by itself. Advances in PET-G production resulted in a boom in the sale of plastic bottles in the 1980s and since then there has been an explosion in plastic use owing to its low cost, ease of production, and uncomplicated transportation. As a gross estimate, only 14% of the plastic ever produced, typically gets collected, less than 20% of this can be recycled, and only 9% of that eventually does get recycled, with the remaining 91% ending up in landfills, oceans, or incineration. The Economic World Forum estimates that an entire truckload of plastic trash is dumped into the ocean every single minute [149].
Clear aligners are now an increasingly sought-after form of orthodontic treatment owing to their superior esthetics and comfort as compared to fixed braces, apart from aggressive marketing by commercial manufacturers. Patients are typically provided multiple plastic aligners, each of which is worn for a week or two and all of these aligners, generally end up as trash with no hope of recycling. The plastic burden on the environment related to clear aligners has become a major concern [150]. Fig. 8 illustrates the relationship between plastic aligners and the environment. Clear plastic aligners are mostly composed of PET, PETG or TPU apart from other petroleum-based polymers that release a wide variety of nanoplastics. These plastics can not only influence the health of the oceans, marine life and eventually climate change; but also our overall health [149].
Fig. 8.
Schematic diagrams illustrate the relationship between the clear aligner and the environment. (a) Recycling process and the threat of plastic to the environment. (b) Micro-plastic hazards to human bodies.
The above context simply addresses the physical problem of plastic dumping; in addition, the deleterious health effects of plastics due to their presence in the ocean and subsequently in our food are further frightening. Studies estimate that there were between 93,000 and 236,000 tons of microplastics in the world's oceans, with traces of microplastics in the majority of the seafood that we consume. Similarly, the food or drink served in plastic containers may contain traces of micro or nanoplastics that directly enter our gut. These nanoplastics possess the potential to penetrate cell membranes and cause cell destruction or mutation [149]. The risk of possible cross-infection dissemination should also be considered since they were used intra-orally and disposed of in the common trash without any extra care [151].
Possible solutions to curb the use of plastics would include steps to minimize the very use of plastics and consequentially reduce their production and increase the recycling possibilities. The current orthodontic market does not seem to point towards a reduction in the use of clear aligners and for aligner companies, finding alternatives for plastic for clear aligner fabrication doesn't seem plausible [149]. The attitude and environmental awareness of all the three parties involved in clear aligner therapy-the aligner manufacturer, the clinician, and the patient will be instrumental in driving this change. The majority of clear aligner companies generally do not provide guidelines to the clinician or the patient about ways to recycle used aligners, nor do they strive to reduce the eventual plastic waste. Several companies, on the contrary, offer as many aligners as the patient wishes to opt for a period of multiple years, allowing clinicians to continue ordering additional aligners till patients are satisfied with the treatment results. Similarly, the majority of the clinicians do not offer the patient advice on the disposal or recycling of used aligners and consequently, the majority of patients do end up disposing of their aligners as trash [149].
Some of the clinics in the US and Europe have now started making patients aware of proper aligner disposal and recycling methods. Europe-based orthodontic clinic ‘Impress’ recently launched an aligner recycling initiative, to promote sustainability and hope that all patients will recycle their aligners and encourage their competitors to do the same. Impress has placed containers in all its flagship clinics so that patients can deposit their aligners and do their part to preserve the planet. All of these collected aligners will then be recycled to be used later as fuel or source of generating energy, or the aligner may be incinerated and the resulting energy could be used to generate heat or electricity, or the recycled plastic could be utilized as a material for other industries, such as the automotive sector; to be used in bumpers, acoustic insulation plates, interior door panels, floors and trunks. Finally, recycled aligners can be used to create fertilizers or soil conditioners to benefit agriculture and ecological development. Patients who wish to recycle their retainers are invited by the clinic to deposit their aligners in one of their clinics or send them by mail to the Impress laboratory [152]. Similarly, Spotlight Oral Care in the US has launched the Spotlight Oral Care Aligner Free Recycling Program that accepts and encourages patients to deposit clear aligner packaging material, clear aligners, as well as aligner cases from all clear aligner brands. Patients can find a participating dentist's office near then drop off their aligner trash, which in turn would be sent over to TerraCycle-a global organization working towards eliminating the idea of waste, for it to be recycled [153].
However, merely recycling a few of the plastic aligners at limited locations, is far from being an adequate solution, due to the large quantities of aligner waste generated globally. Furthermore, the time frame we are realistically staring at to curb drastic environmental consequences is extremely short, necessitating the need to curb the use of plastic and find alternatives [149].
Elshazly et al. [130] hope that shape memory polymers could enable the fabrication of a single shape-changing aligner that may be able to replace up to three successive conventional aligners. Consequently, the number of aligners used per orthodontic treatment could be reduced, reducing overall fabrication costs along with a reduction in the consumption of plastic. Similarly, Tartaglia et al. [45] have highlighted the fact that the environmental impact of printable resins used for 3D models generated during the thermoplastic process is not well documented and energy consumption, waste material generation, and environmental pollution remain of high concern. The authors hope that one solution to this problem could be the incorporation of the use of recycled materials in 3D printers to increase the sustainability of 3D printing technology.
Patients wear plastic aligners almost for 20 h every day. Fluctuating temperatures in the oral cavity, salivary composition and flow, oral microbiota, and masticatory or parafunctional stresses can all severely test and impact the aligner plastic. Is it worthwhile contemplating whether patients who wear clear aligners for significantly extended periods of time may show nanoplastic traces in their bodies and whether this in turn can impact their overall health? These are unanswered questions, with no studies conducted to evaluate nanoplastic concentration in blood or stool before, during or after aligner treatment. Or do we simply shrug this off as a conflict of interest? Overall, all pointers indicate that the economic costs of climate change are significant and will only increase over time, and it is essential that we educate ourselves and our patients before we increasingly recommend clear aligners to them as an orthodontic alternative and eventually end up throwing plastic aligners into the ocean or landfills [149]. Another strategy to tackle this environmental issue might rely on the advancement of bioactive materials. Biodegradable materials have been extensively investigated in tissue engineering and regenerative medicine [154,155] and have also shown a conceivable potential in waste management [156]. Even though biodegradable plastics are deemed as only a part of the solution to ease the environmental burden [157], it is still worth trying to explore the practical application of the bioactive surface coating on biodegradable thermoplastic materials or direct 3D printing materials in treating the malocclusions.
6. Conclusion
Clear aligner therapy is now an accepted mainstay of orthodontic treatment and among the multiple parameters that affect the clinical performance of clear aligners, the material employed for the aligner fabrication plays an all-important role.
This narrative review has attempted to comprehensively encompass the entire gamut of materials currently used for the fabrication of clear aligners and elucidate their mechanical, chemical, thermal, optical, and biological characteristics that are crucial in determining the clinical performance of clear aligners in an oral environment.
The present paper has also endeavoured to highlight the limitations of the biomechanics of clear aligners, specifically linked to the properties of the aligner material itself. Advances in aligner material chemistry, possess the potential to bring about radical transformations in the therapeutic applications of CAT; in the absence of which, CAT will be significantly limited due to its inherent biomechanical constraints and clear aligners would continue to underperform clinically, especially in comparison to conventional fixed orthodontic appliances.
Finally, while innovations in aligner materials such as shape memory polymers, direct 3D printed clear aligners and bioactive materials combined with clear aligner materials are essential to further advance the applications and predictability of CAT; increased awareness of environmental responsibilities among aligner manufacturers, aligner prescribing clinicians and aligner users is essential for a better alignment to our climate change goals towards a sustainable planet. From a technological development point of view, biodegradable thermoplastic or 3D direct printing materials might also be a promising solution.
Ethics approval and consent to participate
No ethical approvals or consent forms are needed.
CRediT authorship contribution statement
Yashodhan M. Bichu: Conceptualization, review, Writing – original draft. Abdulraheem Alwafi: Writing – review & editing. Xiaomo Liu: providing graphic materials, Writing – review & editing. James Andrews: Conceptualization, providing materials, writing-edit. Björn Ludwig: Writing – review & editing, providing graphic materials. Aditi Y. Bichu: Review, Writing – original draft. Bingshuang Zou: Conceptualization, Supervision, Writing – review & editing.
Footnotes
Peer review under responsibility of KeAi Communications Co., Ltd.
References
- 1.Iliadi A., Koletsi D., Papageorgious S.N., Eliades T. Safety considerations for thermoplastic-type appliances used as orthodontic aligners or retainers. A systematic review and meta-analysis of clinical and in-vitro research. Materials. 2020;13(8):1843. doi: 10.3390/ma13081843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee R. Invisible orthodontics market: North American market remains solid, Chinese market grows rapidly. 3D Printing—Int. Mag. Dent. Print. Technol. 2022;2(1):46–47. [Google Scholar]
- 3.Hussain S.R., Jiang S.S., Bosio J.A. Generational perspectives of orthodontists in the U.S. and Canada: a survey study. Am. J. Orthod. Dentofacial Orthop. 2022 doi: 10.1016/j.ajodo.2021.07.020. In press. [DOI] [PubMed] [Google Scholar]
- 4.Hartshorne J., Wertheimer M.B. Emerging insights and new developments in clear aligner therapy: a review of the literature. Am. J. Orthod. Dentofacial Orthop. Clin. Companion. 2022;2(4):311–324. [Google Scholar]
- 5.Rossini G., Parrini S., Castroflorio T., Deregibus A., Debernardi C.L. Efficacy of clear aligners in controlling orthodontic tooth movement. A systematic review. Angle Orthod. 2015;85(5):881–889. doi: 10.2319/061614-436.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kravitz N.D., Kusnoto B., BeGole E., Obrez A., Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofacial Orthop. 2009;135(1):27–35. doi: 10.1016/j.ajodo.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 7.Haouili N., Kravitz N.D., Vaid N.R., Ferguson D.J., Makki L. Has Invisalign improved? A prospective follow-up study on the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofacial Orthop. 2020;158(3):420–425. doi: 10.1016/j.ajodo.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Al-Nadawi M., Kravitz N.D., Hansa I., Makki L., Ferguson D.j., Vaid N.R. Effect of clear aligner wear protocol on the efficacy of tooth movement: a randomized clinical trial. Angle Orthod. 2021;91(2):157–163. doi: 10.2319/071520-630.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karras T., Singh M., Karkazis E., Liu D., Nimeri G., Ahuja B. Efficacy of Invisalign attachments: a retrospective study. Am. J. Orthod. Dentofacial Orthop. 2021;160(2):250–258. doi: 10.1016/j.ajodo.2020.04.028. [DOI] [PubMed] [Google Scholar]
- 10.Tamburrino F., D'Anto V., Bucci R., Alessandri-Bonetti G., Barone S., Razionale A.V. Mechanical properties of thermoplastic polymers for aligner manufacturing: in vitro study. Dent. J. 2020;8(2):47. doi: 10.3390/dj8020047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kesling H.D. The philosophy of the tooth positioning appliance. Am. J. Orthod. Oral Surg. 1945;31(6):297–304. [Google Scholar]
- 12.H.D. Kesling. Coordinating the predetermined pattern and tooth positioner with conventional treatment. Am. J. Orthod. Oral Surg. 32 (6) 1946 285-293.. [DOI] [PubMed]
- 13.Nahoum H.I. The vacuum formed dental contour appliance. NY State Dent. J. 1964;30(9):385–390. [Google Scholar]
- 14.Ponitz R.J. Invisible retainers. Am. J. Orthod. 1971;59(3):266–272. doi: 10.1016/0002-9416(71)90099-6. [DOI] [PubMed] [Google Scholar]
- 15.McNamara J.A., Kramer K.L. J.P. Juenker. Invisible retainers. J. Clin. Orthod. 1985;19(8):570–578. [PubMed] [Google Scholar]
- 16.Sheridan J., LeDoux W., McMinn R. Essix retainers: fabrication and supervision for permanent retention. J. Clin. Orthod. 1993;27(1):37–45. [PubMed] [Google Scholar]
- 17.Boyd R.L., Waskalic V. Three-dimensional diagnosis and orthodontic treatment of complex malocclusions with the invisalign appliance. Semin. Orthod. 2001;7(4):274–293. [Google Scholar]
- 18.Beers A.C., Choi W., Pavlovskaia E. Computer-assisted treatment planning and analysis. Orthod. Craniofac. Res. 2003;6(suppl 1):117–125. doi: 10.1034/j.1600-0544.2003.224.x. [DOI] [PubMed] [Google Scholar]
- 19.Martorelli M., Gerbino S., Giudice M., Ausiello P. A comparison between customized clear and removable orthodontic appliances manufactured using RP and CNC techniques. Dent. Mater. 2013;29(2):e1–e10. doi: 10.1016/j.dental.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Hennessy J., Al-Awadhi E.A. Clear aligners generation and orthodontic tooth movement. J. Orthod. 2016;43:68–76. doi: 10.1179/1465313315Y.0000000004. [DOI] [PubMed] [Google Scholar]
- 21.Ganta G.K., Cheruvu K., Ravi R.K., Reddy R.P. Clear aligners, the aesthetic solution: a review. Int. J. Dent. Materia. 2021;3(3):90–95. [Google Scholar]
- 22.Moshiri M., Kravitz N.D., Nicozisis J., Miller S. Invisalign eighth-generation features for deep-bite correction and posterior arch expansion. Semin. Orthod. 2021;27(3):175–178. [Google Scholar]
- 23.Wajekar N., Pathak S., Mani S. Rise & review of invisalign clear aligner system. IP Indian. J. Orthod. Dentofacial Res. 2022;8(1):7–11. [Google Scholar]
- 24.Boyd R., Miller R.J., Vlaskalic V. The Invisalign system in adult orthodontics: mild crowing and space closure cases. J. Clin. Orthod. 2000;34(4):203–212. [Google Scholar]
- 25.Condo R., Pazzini L., Cerroni L., Pasquantonio G., Lagana G., Pecora A., Mussi V., Rinaldi A., Mecheri B., Licoccia S., Maiolo L. Mechanical properties of “two generations” of teeth aligners: change analysis during oral permanence. Dent. Mater. J. 2018;37(5):835–842. doi: 10.4012/dmj.2017-323. [DOI] [PubMed] [Google Scholar]
- 26.Lagravere M.O., Flores-Mir C. The treatment effects of Invisalign orthodontic aligners: a systematic review. J. Am. Dent. Assoc. 2005;136(12):1724–1729. doi: 10.14219/jada.archive.2005.0117. [DOI] [PubMed] [Google Scholar]
- 27.Phan X., Ling P.H. Clinical limitations of invisalign. J. Can. Dent. Assoc. 2007;136(3):263–266. [PubMed] [Google Scholar]
- 28.Schuster S., Eliades G., Zinelis S., Eliades T., Bradley T.G. Structural conformation and leaching from in vitro aged and retrieved Invisalign appliances. Am. J. Orthod. Dentofacial Orthop. 2004;126(6):725–728. doi: 10.1016/j.ajodo.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 29.Eliades T., Bourauel C. Intraoral aging of orthodontic materials: the picture we miss and its clinical relevance. Am. J. Orthod. Dentofacial Orthop. 2005;127(4):403–412. doi: 10.1016/j.ajodo.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 30.2010. https://investor.aligntech.com/news-releases/news-release-details/align-technology-introduces-invisalign-g3 Available from:
- 31.2011. https://investor.aligntech.com/news-releases/news-release-details/align-technology-introduces-invisalign-g4 Available from:
- 32.Bräscher A.K., Zuran D., Jr Feldmann R.E., Benrath J. Patient survey on Invisalign® treatment compare the SmartTrack® material to the previous aligner material. J. Orofac. Orthop. 2016;77(6):432–438. doi: 10.1007/s00056-016-0051-3. [DOI] [PubMed] [Google Scholar]
- 33.Liu C.L., Sun W.T., Liao W., Lu W.X., Li Q.W., Jeong Y., et al. Colour stabilities of three types of orthodontic clear aligners exposed to staining agents. Int. J. Oral Sci. 2016;8(4):246–253. doi: 10.1038/ijos.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.2013. https://investor.aligntech.com/news-releases/news-release-details/align-technology-announces-invisalign-g5-innovations-treatment Available from:
- 35.Blundell H.L., Weir T., Byrne G. Predictability of overbite control with the Invisalign appliance comparing SmartTrack with precision bite ramps to EX30. Am. J. Orthod. Dentofacial Orthop. 2022;162(2):e71–e81. doi: 10.1016/j.ajodo.2022.05.012. [DOI] [PubMed] [Google Scholar]
- 36.2014. https://investor.aligntech.com/news-releases/news-release-details/align-technology-announces-invisalign-g6-clinical-innovations Available from:
- 37.2016. https://investor.aligntech.com/news-releases/news-release-details/align-technology-announces-next-series-innovation-invisalignr-g7 [Available from:
- 38.2020. https://investor.aligntech.com/news-releases/news-release-details/align-technology-announces-invisalign-g8-new-smartforce Available from:
- 39.Kasper F.K. In: Embracing Novel Technologies in Dentistry and Orthodontics. Bayirli B., Kim-Berman H., Puntillo A., Bielawski D., editors. vol. 56. The University of Michigan; Ann Arbor: 2020. 3D printing applications in clear aligner fabrication; pp. 7–21. [Google Scholar]
- 40.Edelmann A., English J.D., Chen S.J., Kasper F.K. Analysis of the thickness of 3-dimensional-printed orthodontic aligners. Am. J. Orthod. Dentofacial Orthop. 2020;158(5):e91–e98. doi: 10.1016/j.ajodo.2020.07.029. [DOI] [PubMed] [Google Scholar]
- 41.Nasef A.A., El-Beialy A.R., Mostafa Y.A. Virtual techniques for designing and fabricating a retainer. Am. J. Orthod. Dentofacial Orthop. 2014;146(3):394–398. doi: 10.1016/j.ajodo.2014.01.025. [DOI] [PubMed] [Google Scholar]
- 42.Jindal P., Juneja M., Siena F.L., Bajaj D., Breedon P. Mechanical and geometric properties of thermoformed and 3D printed clear aligners. Am. J. Orthod. Dentofacial Orthop. 2019;156(5):694–701. doi: 10.1016/j.ajodo.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 43.Peeters B., Kiratli N., Semeijn J. A barrier analysis for distributed recycling of 3D printing waste: taking the maker movement perspective. J. Clean. Prod. 2019;241 [Google Scholar]
- 44.P. Shivapuja, D. Shah, N. Shah, S. Shah, Direct 3D-printed orthodontic aligners with torque, rotation, and full control anchors, U.S. Patent No. 10,179,035 (15 January 2019).
- 45.Tartaglia G.M., Mapelli A., Maspero C., Santaniello T., Serafin M., Farronato M., et al. Direct 3D printing of clear orthodontic aligners: current state and future possibilities. Materials. 2021;14:1799. doi: 10.3390/ma14071799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Quan H., Zhang T., Xu H., Luo S., Nie J., Zhu X. Photo-curing 3D printing technique and its challenges. Bioact. Mater. 2020;5(1):110–115. doi: 10.1016/j.bioactmat.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khorsandi D., Fahimipour A., Abasian P., Saber S.S., Seyedi M., Ghanavati S., et al. 3D and 4D printing in dentistry and maxillofacial surgery: printing techniques, materials, and applications. Acta Biomater. 2021;122:26–49. doi: 10.1016/j.actbio.2020.12.044. [DOI] [PubMed] [Google Scholar]
- 48.Zhang N., Bai Y., Ding X., Zhang Y. Preparation and characterization of thermoplastic materials for invisible orthodontics. Dent. Mater. J. 2011;30(6) doi: 10.4012/dmj.2011-120. 964-959. [DOI] [PubMed] [Google Scholar]
- 49.Lombardo L., Marines E., Mazzanti V., Arreghini A., Molica F., Siciliani G. Stress relaxation properties of four orthodontic aligner materials: a 24-hour in vitro study. Angle Orthod. 2017;87(1):11–18. doi: 10.2319/113015-813.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Macri M., Murmura G., Varvara G., Traini T., Festa F. Clinical performances and biological features of clear aligners materials in orthodontics. Front. Mater. 2022;9 [Google Scholar]
- 51.Riolo C.S., Bayirli B. In: Embracing Novel Technologies in Dentistry and Orthodontics. Bayirli B., Kim-Berman H., Puntillo A., Bielawski D., editors. The University of Michigan; Ann Arbor: 2020. In-house orthodontic workflow using 3D printing; pp. 22–35. 56. [Google Scholar]
- 52.Lee S.Y., Kim H., Kim H.J., Chung C.J., Choi Y.J., J Kim S., et al. Thermo-mechanical properties of 3D printed photocurable shape memory resin for clear aligners. Sci. Rep. 2022;12:6246. doi: 10.1038/s41598-022-09831-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chalmers J.M., Meier R.J. Elsevier; Amsterdam: 2008. Molecular Characterization and Analysis of Polymers; pp. 329–335. [Google Scholar]
- 54.Condò R., Mampieri G., Giancotti A., Cerroni L., Pasquantonio G., Divizia A., et al. SEM Characterization and ageing analysis on two generations of Invisible aligners. BMC Oral Health. 2021;21(1):316. doi: 10.1186/s12903-021-01676-z. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kundal S., Aligners T. Shokeen. The science of clear orthodontics. Int. J. Dent. Medical. Specialty. 2020;7(1):38–42. [Google Scholar]
- 56.Dupaix R.B., Boyce M.C. Finite strain behavior of poly(ethylene terephthalate) (PET) and poly(ethylene terephthalate)-glycol (PETG) Polymer. 2005;46(13):4827–4838. [Google Scholar]
- 57.McKeen L.W. In: In Plastics Design Library, Permeability Properties of Plastics and Plastomers. fourth ed. McKeen L.W., editor. William Andrew Publishing; USA: 2017. 6 - polyester plastics; pp. 95–114. [Google Scholar]
- 58.Lanaro M., Booth L., Powell S.K., Woodruff M.A. Electrofluidodynamic Technologies (EFDTs) for Biomaterials and Medical Devices. Woodhead Publishing.; 2018. Electrofluidodynamic technologies for biomaterials and medical devices: melt electrospinning; pp. 37–69. [Google Scholar]
- 59.Latko-Durałek P., Dydek K., Boczkowska A. Thermal, rheological and mechanical properties of PETG/rPETG blends. J. Polym. Environ. 2019;27(11):2600–2606. [Google Scholar]
- 60.Hassan M.H., Omar A.M., Daskalakis E., Hou Y., Huang B., Strashnov I., et al. The potential of polyethylene terephthalate glycol as biomaterial for bone tissue engineering. Polymers. 2020;12(12):3045. doi: 10.3390/polym12123045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Iijima M., Kohda N., Kawaguchi K., Muguruma T., Ohta M., Naganishi A., et al. Effects of temperature changes and stress loading on the mechanical and shape memory properties of thermoplastic materials with different glass transition behaviors and crystal structures. Eur. J. Orthod. 2015;37(6):665–670. doi: 10.1093/ejo/cjv013. [DOI] [PubMed] [Google Scholar]
- 62.Frick A., Rochman A. Characterization of TPU-elastomers by thermal analysis (DSC) Polym. Test. 2004;23(4):413–417. [Google Scholar]
- 63.Griffith M., Fields H.W., Ni A., Guo X.H., Lee D.J., Deguchi T. Comparison of 2 invisalign tray generations using the peer assessment rating index. Am. J. Orthod. Dentofacial Orthop. 2021;160(5):718–724. doi: 10.1016/j.ajodo.2020.05.028. [DOI] [PubMed] [Google Scholar]
- 64.Medellín-Rodríguez F.J., Phillips P.J., Lin J.S., Avila-Orta C.A. Triple melting behavior of poly(ethylene terephthalate Co-1,4-cyclohexylene dimethylene terephthalate) random copolyesters. J. Polym. Sci., Part B: Polym. Phys. 1998;36(5):763–781. [Google Scholar]
- 65.Hwang S.H., Jeong K.S., Jung J.C. Thermal and mechanical properties of amorphous copolyester (PETG)/LCP blends. Eur. Polym. J. 1999;35(8):1439–1443. [Google Scholar]
- 66.Poomali S., Sureshac B., Lee J.H. Mechanical and three-body abrasive wear behavior of PMMA/TPU blends. Mater. Sci. Eng., A. 2008;492(1–2):486–490. [Google Scholar]
- 67.Ma Y.S., Fang D.Y., Zhang N., Ding X.J., Zhang K.Y., Bai Y.X. Mechanical properties of orthodontic thermoplastics PETG/PC2858 after blending. Chin. J. Dent. Res. 2016;19(1):43–48. doi: 10.3290/j.cjdr.a35696. [DOI] [PubMed] [Google Scholar]
- 68.Seeger P., Ratfisch R., Moneke M., Burkhart T. Addition of thermo-plastic polyurethane (TPU) to poly(methyl pethacrylate) (PMMA) to improve its impact strength and to change its scratch behavior. Wear. 2018;(406–407):68–74. [Google Scholar]
- 69.Ryu J.H., Kwon J.S., Jiang H.B., Cha J.Y., Kim K.M. Effects of thermoforming on the physical and mechanical properties of thermoplastic materials for transparent orthodontic aligners. Korean J. Orthod. 2018;48(5):316–325. doi: 10.4041/kjod.2018.48.5.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Maspero C., Tartaglia G.M. 3D printing of clear orthodontic aligners: where we are and where we are Going. Materials. 2020;13:5204. doi: 10.3390/ma13225204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Prasad S., Kader N.A., Sujath G., Raj T. 3D printing in dentistry. J. 3D Print. Med. 2018;2(3):89–91. [Google Scholar]
- 72.Nakano H., Kato R., Kakami C., Okamoto H., Mamada K., Maki K. Development of biocompatible resins for 3D printing of direct aligners. J. Photopolym. Sci. Technol. 2019;32(2):209–216. [Google Scholar]
- 73.2022. http://itgraphy.com/wp/material/dental/ Available from:
- 74.Zhang Y., Du Q., Fei W., Li X. Application of antibacterial nanoparticles in orthodontic materials. Nano Rev. 2022;11:2433–2450. [Google Scholar]
- 75.Chhibber A., Agarwal S., Yadav S., Kuo C.L., Upadhyay M. Which orthodontic appliance is best for oral hygiene? A randomized clinical trial. Am. J. Orthod. Dentofacial Orthop. 2018;153(2):175–183. doi: 10.1016/j.ajodo.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 76.Zhang M., Liu X., Xie Y., Zhang Q., Zhang W., Jiang X., Lin J.X. Biological safe gold nanoparticle-modified dental aligner prevents the porphyromonas gingivalis biofilm formation. ACS Omega. 2020;5(30):18685–18692. doi: 10.1021/acsomega.0c01532. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang S., Zhou H., Kong N., Wang Z., Fu H., Zhang Y., Xiao Y., Yang W., Yan F. l-cysteine-modified chiral gold nanoparticles promote periodontal tissue regeneration. Bioact. Mater. 2021;6(10):3288–3299. doi: 10.1016/j.bioactmat.2021.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Worreth S., Bieger V., Rohr N., Astasov-Frauenhoffer M., Töpper T., Osmani B., et al. Cinnamaldehyde as antimicrobial in cellulose-based dental appliances. J. Appl. Microbiol. 2022;132(2):1018–1024. doi: 10.1111/jam.15283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ronca A., Maiullari F., Milan M., Pace V., Gloria A., Rizzi R., De Santis R., Ambrosio L. Surface functionalization of acrylic based photocrosslinkable resin for 3D printing applications. Bioact. Mater. 2017;2(3):131–137. doi: 10.1016/j.bioactmat.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lombardo L., Arreghini A., Maccarrone R., Bianchi A., Scalia S., Siciliani G. Optical properties of orthodontic aligners--spectrophotometry analysis of three types before and after aging. Prog. Orthod. 2015;16(1):41. doi: 10.1186/s40510-015-0111-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gold B.P., Siva S., Duraisamy S., Idaayath A., Kannan R. Properties of orthodontic clear aligner materials - a review. J. Evolution Med. Dent. Sci. 2021;10(37):3288–3294. [Google Scholar]
- 82.Kusy R.P. Orthodontic biomaterials: from the past to the present. Angle Orthod. 2002;72(6):501–512. doi: 10.1043/0003-3219(2002)072<0501:OBFTPT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 83.Abdallah M.N., et al. Advanced Dental Biomaterials. Elsevier; Philadelphia: 2019. Biomaterials used in orthodontics: brackets, archwires, and clear aligners; pp. 541–579. [Google Scholar]
- 84.Kwon J.S., Lee Y.K., Lim B.S., Lim Y.K. Force delivery properties of thermoplastic orthodontic materials. Am. J. Orthod. Dentofacial Orthop. 2008;133(2):228–234. doi: 10.1016/j.ajodo.2006.03.034. [DOI] [PubMed] [Google Scholar]
- 85.Duong T., Kuo E. Finishing with invisalign. Prog. Orthod. 2006;7(1):44–55. [PubMed] [Google Scholar]
- 86.Upadhyay M., Arqub S.A. Biomechanics of clear aligners: hidden truth & first principles. J. World. Fed. Orthod. 2022;11(1):12–21. doi: 10.1016/j.ejwf.2021.11.002. [DOI] [PubMed] [Google Scholar]
- 87.Carniel E.L., Fontanella C.G., Stefanini C., Natali A.N. A procedure for the computational investigation of stress-relaxation phenomena. Mech. Time-Dependent Mater. 2013;17(1):25–38. [Google Scholar]
- 88.Owman-Moll P., Kurol J., Lundgren D. Continuous versus interrupted continuous orthodontic force related to early tooth movement and root resorption. Angle Orthod. 1995;65(6):395–401. doi: 10.1043/0003-3219(1995)065<0395:CVICOF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 89.Berger J., Waram T. Force levels of nickel titanium initial archwires. J. Clin. Orthod. 2007;41(5):286–292. [PubMed] [Google Scholar]
- 90.Simon M., Keilig L., Scwarze J., Jung B.A., Bourauel C. Forces and moments generated by removable thermoplastic aligners: incisor torque, premolar derotation, and molar distalization. Am. J. Orthod. Dentofacial Orthop. 2014;145(6):728–736. doi: 10.1016/j.ajodo.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 91.Chisari J.R., McGorray S.P., Nair M., Wheeler T.T. Variables affecting orthodontic tooth movement with clear aligners. Am. J. Orthod. Dentofacial Orthop. 2014;145(4) doi: 10.1016/j.ajodo.2013.10.022. S82–S91. [DOI] [PubMed] [Google Scholar]
- 92.Fang D., Zhang N., Chen H., et al. Dynamic stress relaxation of orthodontic thermoplastic materials in a simulated oral environment. Dent. Mater. J. 2013;32(6):946–951. doi: 10.4012/dmj.2013-131. [DOI] [PubMed] [Google Scholar]
- 93.Kohda N., Iijima M., Muguruma T., Brantley W.A., Ahluwalia K.S., Mizoguchi I. Effects of mechanical properties of thermoplastic materials on the initial force of thermoplastic appliances. Angle Orthod. 2013;83(3):476–483. doi: 10.2319/052512-432.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zafeiriadis A.A., Karamouzos A., Athanasiou A.E., Eliades T., Palaghias G. An in vivo spectrophotometric evaluation of Vivera and Essix clear thermoplastic retainer discoloration. Aust. Orthod. J. 2018;34(1):3–10. [PubMed] [Google Scholar]
- 95.Talic N.F., Almudhi A.A. The effect of dietary pigmentation on the esthetic appearance of clear orthodontic elastomeric modules. J. Orthod. Sci. 2016;5(2):70–73. doi: 10.4103/2278-0203.179418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bucci R., Rongo R., Levatè C., Michelotti A., Barone S., Razionale A.V., et al. Thickness of orthodontic clear aligners after thermoforming and after 10 days of intraoral exposure: a prospective clinical study. Prog. Orthod. 2019;20(1):36. doi: 10.1186/s40510-019-0289-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dalaie K., Fatemi S.M., Ghaffari S. Dynamic mechanical and thermal properties of clear aligners after thermoforming and aging. Prog. Orthod. 2021;22(1):15. doi: 10.1186/s40510-021-00362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Louis W. Master’s Thesis; 2009. Thermal Properties of Commonly Used Clear Aligner Systems As-Received and after Clinical Use. [Google Scholar]
- 99.Liu C.L., Sun W.T., Liao W., Lu W.X., Li Q.W., Jeong Y., et al. Color stabilities of three types of orthodontic clear aligners exposed to staining agents. Int. J. Oral Sci. 2016;8(4):246–253. doi: 10.1038/ijos.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bernard G.P., Rompré, Tavares J.R., Montpetit A. Colorimetric and spectrophotometric measurements of orthodontic thermoplastic aligners exposed to various staining sources and cleaning methods. Head Face Med. 2020;16(1):2. doi: 10.1186/s13005-020-00218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gracco A., Mazzoli A., Favoni O., Conti C., Ferraris P., Tosi G., et al. Short-term chemical and physical changes in Invisalign appliances. Aust. Orthod. J. 2009;25(1):34–40. [PubMed] [Google Scholar]
- 102.Ryokawa H., Miyazaki Y., Fujishima A., Miyazaki T., Maki K. The mechanical properties of dental thermoplastic materials in a simulated intraoral environment. Orthod. Waves. 2006;65(2):64–72. [Google Scholar]
- 103.Allareddy V., Nalliah R., Lee M.K., Rampa S., Allareddy V. Adverse clinical events reported during Invisalign treatment: analysis of the MAUDE database. Am. J. Orthod. Dentofacial Orthop. 2017;152(5):706–710. doi: 10.1016/j.ajodo.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 104.Martina S., Rongo R., Bucci R., Razionale A.V., Valletta R., D'Antò V. In Vitro cytotoxicity of different thermoplastic materials for clear aligners. Angle Orthod. 2019;89(6):942–945. doi: 10.2319/091718-674.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ahrari F., Afshari J.T., Poosti M., Brook A. A. Cytotoxicity of orthodontic bonding adhesive resins on human oral fibroblasts. Eur. J. Orthod. 2010;32(6):688–692. doi: 10.1093/ejo/cjq019. [DOI] [PubMed] [Google Scholar]
- 106.Ahamed S.F., Kumar S.M., Kumar R.K.V., Kanna A.S.A., Dharshini K.I. Cytotoxic evaluation of directly 3D printed aligners and Invisalign. Eur. J. Molecular & Clin. Med. 2020;7(5):1129–1140. [Google Scholar]
- 107.Pratsinis H., Papageorgiou S.N., Panayi N., Iliadi N., Eliades T., Kletsas D. Cytotoxicity and estrogenicity of a novel 3-dimensional printed orthodontic aligner. Am. J. Orthod. Dentofacial Orthop. 2022;162(3):e116–e122. doi: 10.1016/j.ajodo.2022.06.014. [DOI] [PubMed] [Google Scholar]
- 108.Alhendi A., Khounganian R., Almudhi A. Cytotoxicity assessment of different clear aligner systems: an in vitro study. Angle Orthod. 2022;92(5):655–660. doi: 10.2319/121621-919.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Eliades T., Pratsinis H., Athanasiou A.E., Eliades G., Kletsas D. Cytotoxicity and estrogenicity of Invisalign appliances. Am. J. Orthod. Dentofacial Orthop. 2009;136(1):100–103. doi: 10.1016/j.ajodo.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 110.Alexandropoulos A., Al Jabbari Y.S., Zinelis S., Eliades T. Chemical and mechanical characteristics of contemporary thermoplastic orthodontic materials. Aust. Orthod. J. 2015;31(2):165–170. [PubMed] [Google Scholar]
- 111.Premaraj T., Simet S., Beatty M., Premaraj S. Oral epithelial cell reaction after exposure to Invisalign plastic material. Am. J. Orthod. Dentofacial Orthop. 2014;145(1):64–71. doi: 10.1016/j.ajodo.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 112.Francisco I., Paula A.B., Ribeiro M., Marques F., Travassos R., Nunes C., et al. The biological effects of 3D resins used in orthodontics: a systematic review. Bioengineering. 2022;9(1):15. doi: 10.3390/bioengineering9010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Thukral R., Gupta A. Invisalign: invisible orthodontic treatment - a review. J. Adv. Med. Dent. Sci. Res. 2015;3(5):S42–S44. [Google Scholar]
- 114.Elkholy F., Schmidt F., Jäger R., Lapatki B.G. Forces and moments delivered by novel, thinner PET-G aligners during labiopalata bodily movement of a maxillary central incisor: an in vitro study. Angle Orthod. 2016;86(6):883–890. doi: 10.2319/011316-37R.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zheng M., Liu R., Ni Z., Yu Z. Efficiency, effectiveness and treatment stability of clear aligners: a systematic review and meta-analysis. Orthod. Craniofac. Res. 2017;20(3):127–133. doi: 10.1111/ocr.12177. [DOI] [PubMed] [Google Scholar]
- 116.Bruni A., Serra F.G., Deregibus A., Castroflorio T. Shape-memory polymers in dentistry: systematic review and patent landscape report. Materials. 2019;12:2216. doi: 10.3390/ma12142216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lendlein A., Kelch S. Shape-memory polymers. Angew. Chem. Int. Ed. 2002;41(12):2034–2057. [PubMed] [Google Scholar]
- 118.Sun L., Huang W., Ding Z., Zhao Y., Wang C., Purnawali H., et al. Stimulus responsive shape memory materials: a review. Mater. Des. 2012;33(1):577–640. [Google Scholar]
- 119.Lendlein A. Progress in actively moving polymers. J. Mater. Chem. 2010;20(17):3332–3334. [Google Scholar]
- 120.Meng H., Li G. A review of stimuli-responsive shape memory polymer composites. Polymer. 2013;54(9):2199–2221. [Google Scholar]
- 121.Huang W., Ding Z., Wang C., Wei J., Zhao Y., Purnawali H. Shape memory materials. Mater. Today. 2010;13(7–8):54–61. [Google Scholar]
- 122.Voit W., Ware T., Dasari R.R., Smith P., Danz L., Simon D., et al. High-strain shape-memory polymers. Adv. Funct. Mater. 2010;20(1):162–171. [Google Scholar]
- 123.Jung Y.C., Cho J.W. Application of shape memory polyurethane in orthodontics. J. Mater. Sci. Mater. Med. 2010;21(10):2881–2886. doi: 10.1007/s10856-008-3538-7. [DOI] [PubMed] [Google Scholar]
- 124.Behl M., Lendlein A. Shape-memory polymers. Mater. Today. 2007;10(4):20–28. [Google Scholar]
- 125.Liu C., Qin H., Mather P.T. Review of progress in shape-memory polymers. J. Mater. Chem. 2007;17(16):1543–1558. [Google Scholar]
- 126.Nakasima A., Hu J.R., Ichinose M., Shimada H. Potential application of shape memory plastic as elastic material in clinical orthodontics. Eur. J. Orthod. 1991;13(3):179–186. doi: 10.1093/ejo/13.3.179. [DOI] [PubMed] [Google Scholar]
- 127.Xie T. Tunable polymer multi-shape memory effect. Nature. 2010;464:267–270. doi: 10.1038/nature08863. [DOI] [PubMed] [Google Scholar]
- 128.Li F., Zhang X., Hou J., Xu M., Luo X., Ma D., et al. Studies on thermally stimulated shape memory effect of segmented polyurethanes. J. Appl. Polym. Sci. 1997;64(8):1511–1516. [Google Scholar]
- 129.Jeong H.M., Lee S.Y., Kim B.K. Shape memory polyurethane containing amorphous reversible phase. J. Mater. Sci. 2000;35(7):1579–1583. [Google Scholar]
- 130.Elshazly T.M., Keilig L., Alkabani Y., Ghoneima A., Abuzayda M., Talaat S., et al. Primary evaluation of shape recovery of orthodontic aligners fabricated from shape memory polymer (A typodont study) Dent. J. 2021;9(3):31. doi: 10.3390/dj9030031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Caruso S., Nota A., Ehsani S., Maddalone E., Ojima K., Tecco S. Impact of molar teeth distalization with clear aligners on occlusal vertical dimension: a retrospective study. BMC Oral Health. 2019;19(1):1–5. doi: 10.1186/s12903-019-0880-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Caruso S., Darvizeh A., Zema S., Gatto R., Nota A. Management of a facilitated aesthetic orthodontic treatment with clear aligners and minimally invasive corticotomy. Dent. J. 2020;8(1):19. doi: 10.3390/dj8010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Harris K., Ojima K., Dan C., Upadhyay M., AlShehri A., Kuo C.L., et al. Evaluation of open bite closure using clear aligners: a retrospective study. Prog. Orthod. 2020;21(1):23. doi: 10.1186/s40510-020-00325-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Weir T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017;62(Suppl. 1):58–62. doi: 10.1111/adj.12480. [DOI] [PubMed] [Google Scholar]
- 135.Martorelli M., Gerbino S., Giudice M., Ausiello P. A comparison between customized clear and removable orthodontic appliances manufactured using RP and CNC techniques. Dent. Mater. 2013;29(2):e1–e10. doi: 10.1016/j.dental.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 136.Dawood A., Marti M.B., Sauret-Jackson V., Darwood A. 3D printing in dentistry. Br. Dent. J. 2015;219(11):521–529. doi: 10.1038/sj.bdj.2015.914. [DOI] [PubMed] [Google Scholar]
- 137.Cole D., Bencharit S., Carrico C.K., Arias A., Tüfekçi E. Evaluation of fit for 3D-printed retainers compared with thermoform retainers. Am. J. Orthod. Dentofacial Orthop. 2019;155(4):592–599. doi: 10.1016/j.ajodo.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 138.Kumar S.M. 2019. Cytotoxicity of 3D Printed Materials: an in Vitro Study. Master's Thesis, Sri Ramakrishna Dental College and Hospital. Coimbatore. [Google Scholar]
- 139.Barone S., Paoli A., Razionale A.V., Savignano R. Computational design and engineering of polymeric orthodontic aligners. Int. J. Numer. Method Biomed. Eng. 2017;33(8):e2839. doi: 10.1002/cnm.2839. [DOI] [PubMed] [Google Scholar]
- 140.Can E., Panayi N., Polychronis G., Papageorgiou S.N., Zinelis S., Eliades G., et al. In-house 3D-printed aligners: effect of in vivo aging on mechanical properties. Eur. J. Orthod. 2022;44(1):51–55. doi: 10.1093/ejo/cjab022. [DOI] [PubMed] [Google Scholar]
- 141.Karatepe U.Y., Ozdemir T. Improving mechanical and antibacterial properties of PMMA via polyblend electrospinning with silk fibroin and polyethyleneimine towards dental applications. Bioact. Mater. 2020;5(3):510–515. doi: 10.1016/j.bioactmat.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Liu H., Lu J., Jiang Q., Haapasalo M., Qian J., Tay F.R., Shen Y. Biomaterial scaffolds for clinical procedures in endodontic regeneration. Bioact. Mater. 2021;12:257–277. doi: 10.1016/j.bioactmat.2021.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.C. Yu, L. Li, S. Wang, Y. Xu, L. Wang, Y. Huang, et al. Advances in nanomaterials for the diagnosis and treatment of head and neck cancers: a review. Bioact. Mater. Available online 2 September 2022. In press. [DOI] [PMC free article] [PubMed]
- 144.De Caluwé T., Vercruysse C.W.J., Ladik I., Convents R., Declerc H., Marten L.C., et al. Addition of bioactive glass to glass ionomer cements: effect on the physico-chemical properties and biocompatibility. Dent. Mater. 2017;33(4) doi: 10.1016/j.dental.2017.01.007. e180–e203. [DOI] [PubMed] [Google Scholar]
- 145.Naguib G.H., Nassar H.M., Hamed M.T. Antimicrobial properties of dental cements modified with zein-coated magnesium oxide nanoparticles. Bioact. Mater. 2021;8(1):49–56. doi: 10.1016/j.bioactmat.2021.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stuart B.W., Stan G.E., Popa A.C., Carrington M.J., Zgura I., Necsulescu M., Grant D.M. New solutions for combatting implant bacterial infection based on silver nano-dispersed and gallium incorporated phosphate bioactive glass sputtered films: a preliminary study. Bioact. Mater. 2022;8:325–340. doi: 10.1016/j.bioactmat.2021.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Raszewski Z., Nowakowska D., Wieckiewicz W., Nowakowska-Toporowska A. Release and recharge of fluoride Ions from acrylic resin modified with bioactive glass. Polymers. 2021;13(7):1054. doi: 10.3390/polym13071054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Raszewski Z., Kulbacka J., Nowakowska-Toporowska A. Mechanical properties, cytotoxicity, and fluoride ion release capacity of bioactive glass-modified methacrylate resin used in three-dimensional printing technology. Materials. 2022;15(3):1133. doi: 10.3390/ma15031133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Available from: clear aligners: a plastic economic bubble. April 29, 2019. https://www.kline-europe.com/post/zahnschienen-eine-wirtschaftsblase-aus-plastik updated Jun 16, 2021.
- 150.Peter E., Monisha J., George S.A. Are clear aligners environment friendly? Am. J. Orthod. Dentofacial Orthop. 2022;161(5):619–620. doi: 10.1016/j.ajodo.2021.12.012. [DOI] [PubMed] [Google Scholar]
- 151.Freitas M.P.M., Aligners M.P.M. Environmental contamination, and the role of orthodontics. Angle Orthod. 2022;92(1):148–149. doi: 10.2319/1945-7103-92.1.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Leading the way with recyclable aligners. Br. Dent. J. 2022;232:414. [Google Scholar]
- 153.Spotlight oral care aligners free recycling program. Available from: www.terracycle.com. [accessed Aug 26, 2022].
- 154.Xu C., Hong Y Y. Rational design of biodegradable thermoplastic polyurethanes for tissue repair. Bioact. Mater. 2021;15:250–271. doi: 10.1016/j.bioactmat.2021.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Singh N., Batra U., Kumar K., Ahuja N., Mahapatro A. Progress in bioactive surface coatings on biodegradable Mg alloys: a critical review towards clinical translation. Bioact. Mater. 2022;19:717–757. doi: 10.1016/j.bioactmat.2022.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ab Rahman M.R., Rusli A., Misman M.A., Rashid A.A. Biodegradable gloves for waste management post-Covid-19 outbreak: a shelf-life prediction. ACS Omega. 2020;5(46):30329–30335. doi: 10.1021/acsomega.0c04964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Shen M., Song B., Zeng G., Zhang Y., Huang W., Wen X., Tang W. Are biodegradable plastics a promising solution to solve the global plastic pollution? Environ. Pollut. 2020;263(Pt A) doi: 10.1016/j.envpol.2020.114469. [DOI] [PubMed] [Google Scholar]