Abstract
Traditional risk factors for obesity and the metabolic syndrome, such as excess energy intake and lack of physical activity, cannot fully explain the high prevalence of these conditions. Insufficient sleep and circadian misalignment predispose individuals to poor metabolic health and promote weight gain and have received increased research attention in the past 10 years. Insufficient sleep is defined as sleeping less than recommended for health benefits, whereas circadian misalignment is defined as wakefulness and food intake occurring when the internal circadian system is promoting sleep. This Review discusses the impact of insufficient sleep and circadian misalignment in humans on appetite hormones (focusing on ghrelin, leptin and peptide-YY), energy expenditure, food intake and choice, and risk of obesity. Some potential strategies to reduce the adverse effects of sleep disruption on metabolic health are provided and future research priorities are highlighted. Millions of individuals worldwide do not obtain sufficient sleep for healthy metabolic functions. Furthermore, modern working patterns, lifestyles and technologies are often not conducive to adequate sleep at times when the internal physiological clock is promoting it (for example, late-night screen time, shift work and nocturnal social activities). Efforts are needed to highlight the importance of optimal sleep and circadian health in the maintenance of metabolic health and body weight regulation.
Subject terms: Obesity, Metabolism
Insufficient sleep and circadian misalignment contribute to obesity risk. This Review discusses how modern society disrupts sleep, it considers evidence from human studies on how sleep disruption affects energy expenditure, appetite hormones and food intake, and discusses some potential strategies to reduce the adverse effects of sleep disruption.
Key points
Insufficient sleep and circadian misalignment are common in modern society.
Insufficient sleep and circadian misalignment are important metabolic stressors and are associated with weight gain and obesity.
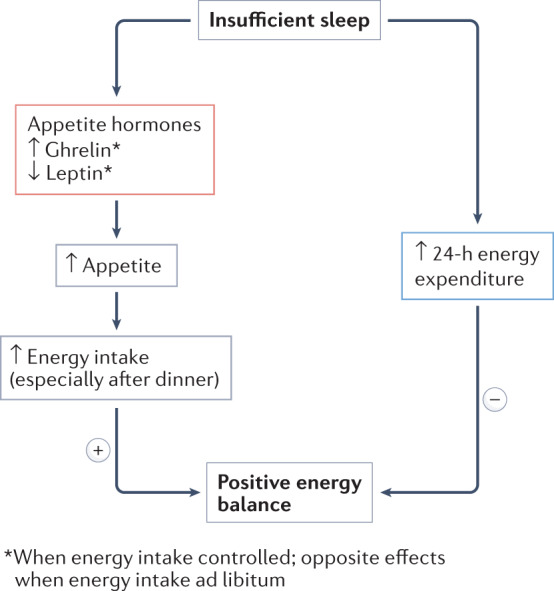
Insufficient sleep increases energy expenditure by ~100 kcal per day but also increases energy intake by >250 kcal per day, resulting in a positive energy balance and weight gain.
Sleep restriction increases the drive to eat, and excess food intake resulting from not sleeping enough is more related to cognitive control and reward mechanisms than to appetite hormones.
Circadian misalignment reduces 24-h energy expenditure by ~3% (~55 kcal per day), alters the levels of appetite hormones and promotes unhealthier food choices than conditions of adequate sleep.
Introduction
Obesity is a major public health issue worldwide caused by a complex interplay of multiple factors1. Efforts to counter the obesity pandemic and its associated metabolic dysregulations (for example, type 2 diabetes mellitus (T2DM) and non-alcoholic fatty liver disease) have largely focused on traditional risk factors, such as excess energy intake and insufficient physical activity. However, traditional risk factors cannot fully explain the increase in obesity rates that have occurred in the past few decades. Over the past 20 years, many novel contributors to obesity and the risk of associated metabolic disease have been identified2,3, including insufficient sleep and circadian misalignment4,5.
Sleep is a foundational pillar of health (Box 1). Unfortunately, the prevalence of insufficient sleep is high in modern society, such that one-third or more of adults in the Americas, Europe and Asia sleep less than the 7 h per night recommended by public health authorities for health maintenance6–10. Furthermore, modern society is active 24 h a day, 7 days a week, which is conducive to circadian misalignment. For example, shift-work schedules require people to work during the biological night (when circadian clocks promote sleep) and sleep during the biological day (when circadian clocks promote activity)11–13. Moreover, access to electric light can delay the timing of the central circadian clock, which can result in delayed sleep schedules that are not conducive to early school and work start times11.
Both insufficient sleep and circadian misalignment (Box 2) are stressors to metabolic health and are associated with adverse health outcomes, including an increased risk for the development of obesity14,15. For example, short sleep duration (defined in most of the cited studies as less than 5 or 6 h per day) is associated with a 38% absolute increase in the incidence of obesity compared with normal sleep duration in a meta-analysis of prospective cohort studies among adults14. Other adverse metabolic health outcomes commonly associated with insufficient sleep and/or circadian misalignment include T2DM, cardiovascular disease, hypertension and dyslipidaemia14.
In this Review, we highlight the role of insufficient sleep and circadian misalignment in obesity and associated metabolic dysregulation, focusing on human studies. We overview common sleep disruptors and discuss the effects of insufficient sleep and circadian misalignment on appetite hormones, energy expenditure, food intake and choice, and obesity risk. We also consider the impact of obesity on sleep. Finally, some potential strategies to reduce the adverse effects of sleep and circadian disruption on metabolic health as well as future research directions are discussed. Of note, this Review focuses on the adult population (mainly young adult workers) because this population is where most of the mechanistic evidence lies in experimental studies.
Box 1 What is sleep and what purpose does it serve?
Sleep (see IOMC: Sleep quality and pain) is the opposite of wakefulness and has been defined as “a naturally recurring state of mind and body, characterized by altered consciousness, relatively inhibited sensory activity, reduced muscle activity and inhibition of nearly all voluntary muscle during rapid eye movement [REM] sleep, and reduced interactions with surroundings”203.
During sleep, the brain alternates between non-REM (NREM) sleep and REM sleep, with a complete NREM–REM cycle occurring approximately every 90 min. NREM sleep is divided into light sleep and deep sleep (also called slow-wave sleep). During sleep, NREM sleep occurs first and decreases in duration throughout the night; therefore, NREM sleep occurs more in the first half of the night. During this phase, breathing and heart rate are regular and slow, the brain uses less energy and thoughts can occur. REM sleep occurs next and increases in duration throughout the night; therefore, REM sleep occurs more in the second half of the night. This phase of sleep is associated with irregular and faster breathing and heart rates than NREM sleep, REMs, loss of muscle tone and a temporary suspension of homeostasis, the brain uses more energy, and bizarre and fantastic dreams occur204.
Sleep has many functions, including energy conservation and the repartitioning of energy to sleep-dependent or sleep-optimal functions that cost energy such as protein and hormone synthesis. In addition, sleep reduces oxidative stress, enhances the removal of metabolic waste products from the brain, promotes immune function, and facilitates synaptic homeostasis and memory consolidation. Most of the systems of the body are in an anabolic state during sleep, which helps to restore the nervous, immune, skeletal and muscular systems. These processes are vital for the maintenance of memory, cognitive function and mood as well as for endocrine and immune functions205. Although the diverse mechanisms and purposes of sleep are still under investigation, sleep has been a highly conserved behaviour throughout evolution206.
Box 2 Definitions of insufficient sleep and circadian misalignment.
Insufficient sleep
Insufficient sleep occurs when sleep does not support adequate alertness, performance and health. These effects arise either owing to reduced total sleep time (short sleep duration or decreased quantity) or fragmentation of sleep (poor sleep quality). In epidemiology, insufficient sleep is generally defined as sleeping less than recommended by public health authorities for health benefits14. For example, adults that report sleeping fewer than 7 h per night are considered to have insufficient sleep in most epidemiological studies14.
Circadian misalignment
Circadian misalignment describes a variety of circumstances, such as inappropriately timed sleep–wakefulness and fasting–energy intake cycles relative to the internal circadian and/or environmental time, or misaligned timing of central and peripheral rhythms. For example, night-shift workers have a mismatch between environmental time and the body’s internal circadian time, as wakefulness activities, such as physical activity and energy intake, occur when the circadian rhythm is promoting sleep and fasting. Thus, night-shift workers are an ideal population in which to study circadian misalignment.
Sleep disruption in modern society
Behaviours and events that disrupt sleep have been described in religious scriptures that were written thousands of years ago16. Since then, humanity has gone through several breakthroughs and cultural and societal changes. As such, sleep patterns have changed and sleep disruptors or ‘sleep stealers’ have grown in number and complexity17,18.
Historical sleeping patterns
Pre-industrial societies had a distinct pattern of sleep from modern societies, possibly reflecting the lifestyle of humanity before the availability of electricity. Societies of hunter-gatherers and/or hunter-horticulturalists did not have access to artificial light or heating and cooling systems; thus, their sleeping patterns often varied according to sunlight exposure and temperature19. As such, sleep has been shown to be influenced by natural events outside of the control of individuals. For example, in pre-industrial society, sleep was longer in winter than in summer, as low temperatures during the night favour sleep in equatorial regions. Furthermore, napping occurred more during summer than winter, possibly under shade to avoid temperatures above thermoneutral conditions during the afternoons. In addition, the duration of nightly sleep was more strongly determined by the time of sleep onset (which typically occurred 3.3 h after sunset) than sleep offset (which occurred typically before sunrise)19. Of note, nightly sleep duration in these pre-industrial societies has been shown to be shorter than that observed and recommended in modern societies19.
Different sleep patterns, such as biphasic sleep or multiphasic sleep, were also reported historically. These patterns were typically characterized by a first sleep, occurring somewhere between 9 pm and 1 am, and a second sleep, from the end of the first sleep until somewhere around sunrise20. The time between the first and second sleep periods was reportedly used for various tasks, from meditating to house chores. The night-to-night consistency in the reported biphasic sleep pattern and the average duration of wakefulness between sleeps are unknown, as is whether this pattern was seen in different age groups and segments of the population. Other segments of sleep might have been more common than biphasic sleep, such as naps in the early afternoon, which are still common in ‘siesta’ cultures in Spain and Italy20. These different sleep patterns were substantially changed in the early 1900s, with the development of electric power grids enabling widespread access to electric lights, technologies to control temperatures and industrial work schedules. The following sections highlight some common ‘sleep stealers’ that have become prevalent in modern society.
Modern working patterns
The growth, development and diversification of work in the global economy have increased the necessity of workers across different settings to maintain high productivity, often at the expense of sleep21. This effect has been evident since the Fourth Industrial Revolution, when workers began to report burnout, increasingly complex tasks, social disconnection and other problems that were not as present previously22. To keep up with these demands, workers consistently use substances to reduce sleepiness such as coffee and energy drinks that contain caffeine. These substances can increase wakefulness and productivity but, in turn, might contribute to insufficient sleep and circadian misalignment, which results in an increased need for substances to manage fatigue that feeds back into a vicious cycle. This cycle is common in shift workers23 and in workers with uncertain schedules24, who are prone to chronic circadian misalignment and its many associated adverse effects25. For example, working atypical shifts (for example, before 8 am, after 6 pm or during the night) is associated with trouble sleeping, excessive sleepiness, fatigue, and poor physical and mental health — effects that eventually lead to reduced quality of life25.
Screen time
In addition to work schedules, many recreational activities of the modern and globalized society have been shown to affect sleep18. The use of screen-based devices is now widespread, even in low-income and middle-income countries; these include televisions, game consoles, computers and portable devices such as tablets, smartphones and smartwatches26. In fact, among young adults and adolescents, total screen time adds up to more than a third of the day27,28. Young people use mobile phones for several hours a day29 and, among adults, text messages, phone calls and night-time device notifications have been shown to negatively affect sleep30–32. Evidence published in 2019 showed that portable electronic devices, rather than stationary devices, are a main driver of sleep disturbances33. Using portable electronic devices is associated with shorter sleep duration than using non-portable electronic screens33. Many modern jobs also require a substantial amount of screen time that can potentially affect the sleep of individuals worldwide.
The negative effects of screen time on sleep can be partly explained by exposure to bright light at night, especially blue–green light, which reduces circulating levels of melatonin34. Light is also arousing to the brain and thus light exposure at night increases alertness. Increased screen time might also be associated with reduced time spent outside and therefore with reduced exposure to bright sunlight, which might affect sleep and circadian alignment35. Furthermore, the content of screen time activities might be engaging and alerting to the brain and can increase wakefulness. This fact could help explain the link between screen time-related issues (for example, internet addiction36, problematic social media use37 and problematic gaming38) and poor sleep outcomes39,40.
Sleep-disrupting substances
To help fulfil either occupational or leisure objectives, voluntary sleep restriction and the use of sleep-disrupting substances are becoming popular. Trends in caffeine intake have shown substantial increases in many parts of the world41, not only in the form of coffee but also as cola drinks and energy drinks among young people42. Caffeine can affect the onset of sleep and reduce sleep time (especially slow-wave sleep; Box 1), sleep efficiency and satisfaction levels43.
Cigarette smoking has become less prevalent globally but is still present. Of note, nicotine, one of the main substances in cigarettes, is a common sleep disruptor17,42. Nicotine is also a stimulant and is associated with increased insomnia severity and shortened sleep duration, particularly if intake occurs at night44. In adolescents, nicotine use through vaping has been increasing, which can negatively affect sleep45–47.
Alcoholic beverages are commonly used as sleep aids owing to their ability to reduce sleep onset latency. These beverages are popular among adults48 and adolescents, despite their consumption actually resulting in disturbed sleep17,42. People who drink alcohol before bed often experience disruptions late in their sleep cycle as their liver enzymes metabolize the alcohol; this disruption can lead to excessive daytime sleepiness the following day. Finally, recreational and medical drugs, such as marijuana and opiates, have also been shown to disrupt sleep49,50.
Modern emotional stressors and sleep
Many health problems and conditions can affect sleep, including diabetes mellitus, heart disease, cancer, pain, medication use and substance abuse. However, there is no doubt that sleep is intrinsically related to mental health, with chronic sleep problems being highly comorbid with depression, anxiety and other mental health conditions. The relationship between sleep and mental health is so strong that sleep problems, such as insomnia, are simultaneously causes and consequences of mental health problems51–53. Consequently, the worsening of sleep observed in the past few decades cannot be dissociated from the increase in mental health problems observed over the same period54. Furthermore, this decrease in sleep amount and quality cannot be dissociated from the rising rates of the aforementioned sleep-disrupting lifestyle behaviours. This change is reflected in the shift from life stressors commonly reported a century ago (for example, physical stressors) to new, non-physical work-related stressors linked to burnout and emotional exhaustion55 or stress due to major societal events such as the COVID-19 pandemic56 or negative emotions about climate change57 and even global conflicts. Even the stress caused by sleep loss itself can be a disruptor of sleep58. In conclusion, although the marvels of modernization and technology have improved life at several levels, achieving a healthy balance with these technologies is still a challenge that keeps many people awake at night.
Temporal variation in human physiology
Human physiology varies across the 24-h day at every level of physiological organization — from cellular59,60, transcriptomic61–64, proteomic65, metabolomic66–68, tissue and organ systems69,70, to physiological and behavioural systems71–73. Such 24-h variation is controlled by circadian and sleep–wakefulness-dependent processes. Sleep–wake cycles and circadian rhythms are fundamentally involved in energy metabolism and related behaviours such as eating and activity74. Over the 24-h day, human physiology is organized by the central circadian clock and peripheral circadian clocks, such that wakefulness, energy intake, nutrient processing and activity occur during the biological daytime (when levels of melatonin are low). By contrast, sleep, fasting, inactivity and restorative processes occur during the biological night-time (when levels of melatonin are high). Additionally, the central circadian clock, along with external cues (for example, light, energy intake and activity), can entrain peripheral clocks located throughout the body.
Energy metabolism
Multiple components of energy metabolism are influenced by circadian and sleep–wakefulness processes, including energy expenditure75–77 and metabolic and appetite hormones78–83 (Figs. 1,2 and 3). For example, circulating levels of growth hormone are largely sleep dependent, with pulses of secretion that predominately occur during slow-wave sleep82. By contrast, levels of cortisol are largely dependent on the circadian rhythm, with a peak in the early morning hours82. Circulating levels of the appetite-regulating hormone ghrelin are dependent on both sleep–wakefulness and energy intake76,84,85. Finally, energy expenditure is highest during wakefulness and lowest during sleep75. Many of these parameters (such as ghrelin80 and energy expenditure70) also display circadian rhythms that are independent of the sleep–wakefulness cycle; therefore, it is no surprise that, when sleep and circadian rhythms are disrupted, energy expenditure and hormone profiles are subsequently altered.
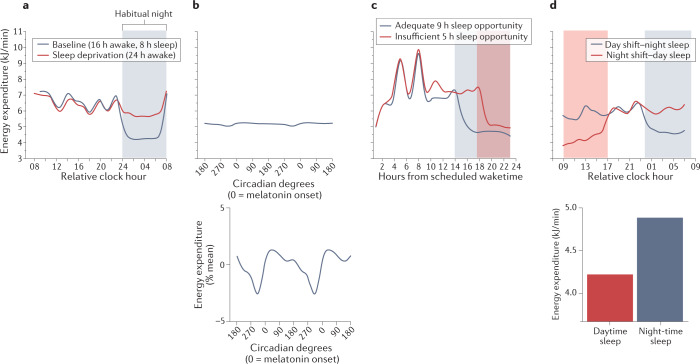
Fig. 1. Energy expenditure in healthy adults is influenced by both sleep and circadian processes.
a | Hourly 24-h energy expenditure with diet controlled for energy balance during a typical day with adequate sleep and one night of total sleep deprivation. b | The circadian rhythm of energy expenditure during a constant routine protocol; bottom graph shows percentage change for the circadian variation in energy expenditure (0° = melatonin onset, 360° = 24 hours after melatonin onset, where each 1 hour increment = 15°). Energy expenditure follows a circadian rhythm, with decreases in energy expenditure levels across the biological daytime, when levels of the hormone melatonin are low, and a trough in energy expenditure during early evening hours. During biological night-time, increases in energy expenditure occur when levels of melatonin are high (that is, 0 to ~180 circadian degrees), with a peak near the end of the biological night. c | Hourly 24-h energy expenditure during adequate sleep and insufficient sleep regardless of controlled or ad libitum diet. During sleep, energy is conserved, whereas energy expenditure during sleep deprivation (part a) and sleep restriction (part c) are similar to that of typical waking energy expenditure. d | Hourly 24-h energy expenditure during circadian misalignment with diet controlled for a typical day with adequate sleep; bottom graph shows the percentage change for sleeping energy expenditure during daytime and night-time sleep. If sleep is initiated during the daytime, energy expenditure is lower than during sleep under conditions of circadian alignment, resulting in an overall decreased 24-h energy expenditure. Figures show mean data with b-spline creating smooth curve fits. Note that energy expenditure plotted in parts a, b and d were assessed under bed rest conditions controlling for posture and activity, whereas energy expenditure in part c was assessed under ambulatory conditions in the whole-room calorimeter with two scheduled stair-stepping sessions each day. Grey panels show control sleep patterns and red panels show experimentally disrupted sleep patterns. Part a adapted with permission from ref.75, Wiley. Data for parts b–d from refs.75,76,80,100,139.
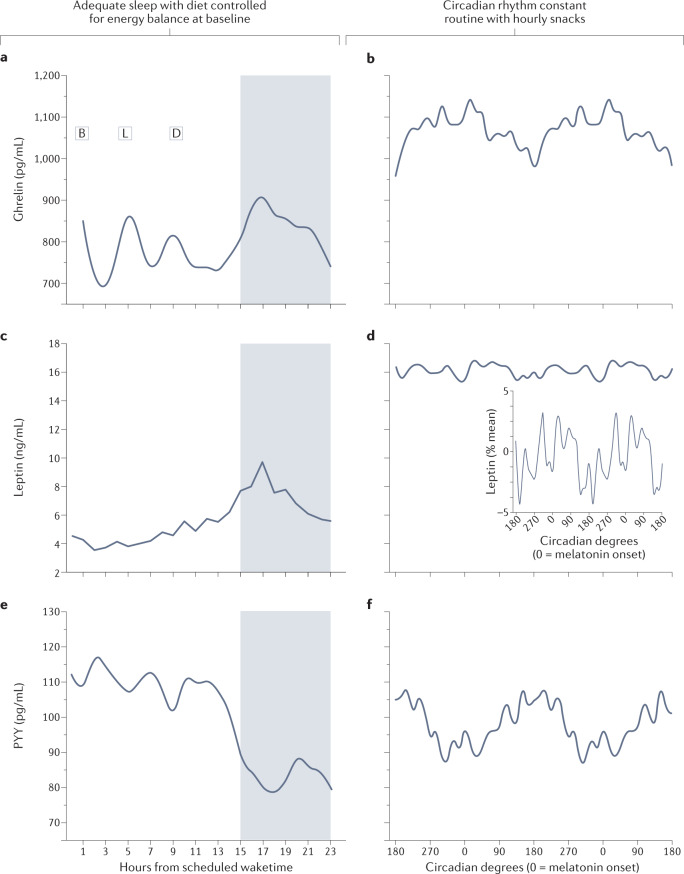
Fig. 2. The appetite-stimulating hormone ghrelin and the satiety hormones leptin and PYY are affected by energy intake, sleep and circadian rhythm in healthy adults.
The figure shows blood hormonal profiles during adequate sleep with diet controlled for energy balance at baseline as well as the circadian rhythm of these hormones during a constant routine protocol with hourly snacks. During conditions of habitual sleep timing with adequate sleep and an energy-balanced diet, levels of ghrelin peak near the beginning of sleep and decrease across the sleep episode (part a). From a circadian perspective, levels of ghrelin increase across the biological day and decrease across the biological night (part b). During conditions of habitual sleep timing with adequate sleep and an energy-balanced diet, levels of leptin are higher during sleep than during wakefulness, peak near the beginning of sleep and decrease thereafter (parts c), while levels of peptide-YY (PYY) are higher during wakefulness than during sleep (parts e). From a circadian perspective, levels of leptin decrease across the biological night and increase across the biological day; inset shows the percentage change for the circadian variation in leptin (part d). By contrast, levels of PYY increase across the biological night and decrease across the biological day (part f). Graphs show mean data with b-spline creating smooth curve fits. For comparison purposes, data for each hormone are plotted on the same scale. Parts a, c and e: Adequate sleep with diet controlled for energy balance at baseline. Parts b, d and f: circadian rhythm constant routine with hourly snacks. B, breakfast timing; D, dinner timing; L, lunch timing. Data from refs.76,80.
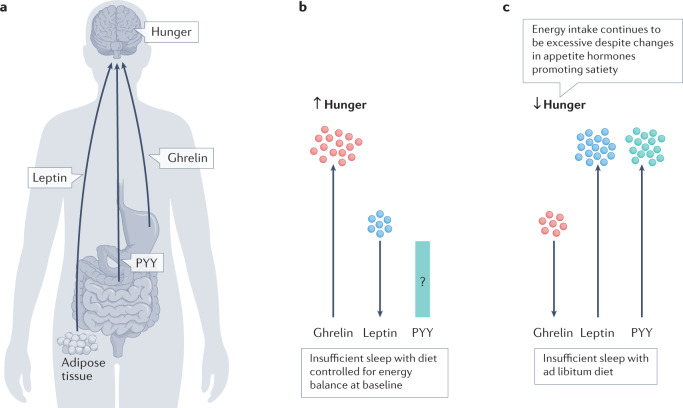
Fig. 3. Model of changes in appetite hormones, hunger and energy intake in response to insufficient sleep.
The peripheral appetite-stimulating hormone ghrelin and the satiety hormones leptin and peptide-YY (PYY) feed back to the brain to influence appetite and hunger. When sleep is restricted but diet is controlled for the energy balance needed for a typical day with adequate sleep, the appetite-stimulating hormone ghrelin is increased and the satiety hormone leptin is decreased, resulting in increased hunger levels. By contrast, ghrelin is decreased and leptin and PYY are increased under an ad libitum diet during restricted sleep, reducing hunger levels. Changes in appetite hormones during ad libitum diets are probably due to increased energy intake during sleep restriction. However, energy intake remains excessive despite reductions in hunger, which suggests that other factors promote food intake. It is unknown how PYY might change during sleep restriction under a diet controlled for energy balance for a typical day with adequate sleep.
The constant routine
A physiological or behavioural outcome might demonstrate a diurnal rhythm that is driven by external factors (for example, ambient temperature or sleep–wake cycles) rather than the endogenous clock. The gold standard protocol for assessing the circadian contribution to a physiological or behavioural outcome is the constant routine. The constant routine protocol controls for factors that might affect the outcome of interest by eliminating, holding constant or equally distributing such factors across at least one 24-h circadian cycle. In this protocol, participants are maintained in constant environmental conditions of dim light and thermoneutral ambient temperature. Wakefulness, activity and posture are controlled by maintaining wakefulness in bed rest conditions with the head raised for at least 24 h. Energy intake can be equally distributed in small hourly snacks or constantly maintained using a continuous infusion. Canonical circadian markers of biological time, such as melatonin, cortisol or core body temperature, are typically measured to facilitate the interpretation of findings; that is, how outcomes of interest vary relative to central circadian rhythms. Circadian rhythms in the outcomes of interest can then be compared with patterns observed in other non-constant conditions, for example, whether they are influenced by factors such as wakefulness–sleep, energy intake–fasting, activity–inactivity or light–dark cycles. Understanding the distinct contributions of circadian versus diurnal rhythms in the regulation of physiological processes could inform how these mechanisms are dysregulated as well as how they can be targeted for obesity prevention and treatment67,86,87.
Energy expenditure and appetite hormones
To examine the role of sleep and circadian disruption in obesity development, this section primarily focuses on findings from studies that examined 24-h patterns in energy expenditure and the appetite-regulating hormones ghrelin, leptin and peptide-YY (PYY) that feed back to energy intake regulatory centres in the hypothalamus88–90. Compared with fasting values, 24-h patterns in these parameters are more relevant to understanding weight gain and metabolic dysregulation and have been repeatedly studied under conditions of insufficient sleep and circadian misalignment (Box 2). We also briefly examine the limited existing data on the effect of insufficient sleep and circadian misalignment on the 24-h or daytime patterns in the gut hormones glucagon-like peptide 1 (GLP1) and pancreatic polypeptide. Other potentially relevant hormones, such as gastric inhibitory polypeptide, cholecystokinin and amylin, are not discussed here as data are not currently available.
24-h variation
Energy expenditure
The 24-h pattern of energy expenditure has been measured under controlled energy intake, controlled activity and bed rest conditions (Fig. 1). Increases in energy expenditure occur in response to meals (referred to as the thermic effect of food or diet-induced thermogenesis) and sleep induces a decrease in energy expenditure that is absent when wakefulness is maintained. Staying awake for a single night results in a physiologically relevant ~7% increase in 24-h energy expenditure in healthy young adults75. If activity or diet-induced energy expenditure occurred overnight, the 24-h increase in energy expenditure during sleep deprivation would probably be even larger than 7%. Under constant routine conditions, the circadian variation in energy expenditure decreases across the biological day and increases across the biological night (Fig. 1b). However, the circadian rhythm in energy expenditure is of much smaller magnitude than the sleep–wake modulation of energy expenditure. In addition, wakefulness–sleep, energy intake–fasting and circadian rhythms are observed in the thermic effects of energy intake and in levels of hunger in healthy young adults and healthy middle-aged (aged 38–69 years) adults77,80,91.
Appetite hormones
Sleep and circadian rhythms influence the levels of appetite hormones (Figs. 2 and 3). Ghrelin is produced by P/D1 cells in the stomach and is a hormone that increases appetite. In healthy adults, a 24-h pattern occurs in circulating levels of ghrelin under conditions of energy balance, such that ghrelin levels increase between meals, decrease after meals, increase before and during the first few hours of sleep, and decrease during the second half of the sleep episode76,84 (Fig. 2a). Under constant routine conditions, the circadian rhythm of ghrelin increases across the biological daytime and decreases across the biological night80 (Fig. 2b). Of note, prolonged fasting (72 h) is not associated with elevated levels of ghrelin, thereby suggesting that the meal-related pattern observed in plasma concentrations of ghrelin in the aforementioned studies76,80,84 might be driven more by the postprandial reduction rather than by preprandial increases in circulating levels of ghrelin92. Furthermore, hypocaloric diets that induce moderate weight loss are not necessarily associated with elevated ghrelin93. Together, these reports suggest that increased levels of ghrelin are not required to increase appetite.
Leptin is produced by white adipocytes and is a hormone that decreases appetite. Circulating levels of leptin are positively associated with adiposity and are considered representative of energy storage. In healthy adults, a 24-h pattern of levels of leptin can be observed under conditions of energy balance, with relatively lower levels most of the waking day and higher levels at night76,94 (Fig. 2c). Like ghrelin, leptin levels peak in the first few hours of the habitual sleep episode and decrease across the remainder of the sleep episode. Under constant routine conditions, a very small amplitude circadian rhythm occurs in leptin, which increases across the biological daytime and decreases across the biological night80 (Fig. 2d).
PYY is produced by L cells of the small intestine and is a hormone that decreases appetite. In healthy adults, the 24-h pattern of circulating levels of PYY under conditions of energy balance shows higher levels during the daytime and lower levels at night76 (Fig. 2e). Under constant routine conditions, the circadian rhythm of PYY shows decreased levels across the biological daytime and increased levels across the biological night80 (Fig. 2f). Thus, 24-h patterns of the appetite hormones ghrelin, leptin and PYY are modulated by circadian rhythms and by wakefulness–sleep, activity–inactivity and energy intake–fasting processes.
GLP1 is produced by L cells of the intestine and is a hormone that reduces appetite. In healthy adults, the 24-h pattern of GLP1 shows that higher levels of GLP1 are observed in the afternoon after food intake than at other times95. Whether a circadian rhythm of GLP1 occurs is unknown. Whether this diurnal rhythm is circadian and/or influenced by sleep is also unknown and requires follow-up studies with more frequent sampling.
Pancreatic polypeptide is produced by PP cells of the pancreas and is a hormone that reduces appetite96. In healthy adults, the 24-h pattern of circulating levels of pancreatic polypeptide shows higher levels during the daytime with food intake and lower levels at night97–99. Whether a circadian rhythm of pancreatic polypeptide occurs is unknown. Under a 24-h fast in healthy adults, a diurnal rhythm was observed, with highest levels occurring during the early evening and night and low levels in the second half of the night98. Whether the potential diurnal rhythm observed during this fast is circadian and/or sleep influenced is unknown and requires follow-up studies.
Impact of insufficient sleep
Increased energy expenditure
Similar to total sleep deprivation, insufficient night-time sleep increases 24-h energy expenditure, in this case by 4–5% (~100 kcal per day) of total daily energy expenditure in healthy young populations75,76,100–102, when assessed using rigorous and sensitive whole-room calorimeter techniques. Such increases in 24-h energy expenditure occur regardless of whether energy intake is maintained at levels that are sufficient for energy balance during adequate sleep conditions or whether energy intake is permitted ad libitum. Furthermore, increased energy expenditure during insufficient sleep occurs rapidly and is sustained across many days in both healthy young men and women100. In lean individuals, measuring energy expenditure using doubly labelled water (a less sensitive and more variable technique than whole-room calorimeter techniques) does not detect these small but physiologically meaningful changes in response to insufficient sleep103,104. However, the doubly labelled water technique can be more readily employed in free-living studies and when large changes in energy balance are predicted.
Controlled energy intake
When energy intake is controlled during insufficient sleep and not increased to account for the increased energy expenditure, a negative energy balance occurs. This negative energy balance and changes in the levels of appetite hormones (namely increased ghrelin and reduced leptin) are associated with increased hunger ratings across days of insufficient sleep in healthy populations94,105–107; however, not all appetite hormones (for example, T3, T4 or adiponectin) were altered in these studies. Furthermore, PYY has not been assessed under insufficient sleep with controlled energy intake conditions. Energy intake during adequate habitual sleep in healthy lean adults was isocaloric; thus, the 24-h pattern of leptin, ghrelin and PYY during adequate sleep was under assumed conditions of energy balance76,100. By contrast, during insufficient sleep in healthy lean adults, if energy intake is not increased to meet the increased energy expenditure during insufficient sleep, the 24-h pattern of these same appetite hormones can be assumed to reflect conditions of negative energy balance (Fig. 2).
Findings on the effect of insufficient sleep on the 24-h pattern in gut hormones associated with satiety, such as GLP1 and pancreatic polypeptide, are mixed and potentially dependent on sex or context. For example, afternoon blood levels of GLP1 were reduced during experimental sleep restriction under conditions of controlled energy intake (negative energy balance) in young women (compared with adequate sleep), whereas circulating levels of GLP1 across the 24-h day did not notably change under the same conditions in young men108. However, afternoon levels of GLP1 were decreased during sleep fragmentation in young men tested under energy balance conditions109. Of note, in young men, circulating levels of pancreatic polypeptide across the 24-h day during experimental sleep restriction did not notably change but after-dinner levels were reduced compared with adequate sleep conditions107.
Uncontrolled energy intake
When energy intake is uncontrolled in lean adults during periods of insufficient sleep, an increase in energy intake occurs that is larger than the increase in energy expenditure, which results in a positive 24-h energy balance and weight gain76 (Fig. 4). Meta-analyses of sleep restriction interventions in both lean adults and adults with overweight or obesity have reported respective average increases in energy intake by 253 kcal per day5 and 385 kcal per day110 following sleep restriction compared with recommended sleep duration. Importantly, this excess in 24-h energy intake in healthy adults occurs5,103,104,111 even with changes in appetite hormones that should reduce levels of hunger (reduced ghrelin, increased leptin and increased PYY)76,112. Although changes in ghrelin, leptin and PYY might initially promote energy intake during acute sleep restriction, mechanisms other than changes in these appetite hormones are probably involved in the continued excess energy intake and obesogenic effects of chronic insufficient sleep76,112.
Fig. 4. Insufficient sleep affects energy intake and energy expenditure, which leads to a positive energy balance and the risk of weight gain.
During experimental conditions of insufficient sleep in healthy adults, when energy intake is designed to meet the energy balance demands for a typical day with adequate sleep at baseline, there is an increase in energy expenditure due to the increased wakefulness and a negative energy balance (that is, energy expended is greater than energy consumed). Concurrently, hunger will increase owing to changes in appetite hormones. However, if sleep is restricted and food is provided ad libitum, participants will eat far more calories than expended during the additional wakefulness despite changes in appetite hormones that would promote satiety. These extra calories put participants into a positive energy balance and weight gain if maintained over time. Moreover, the increase in calories occurs predominately in after-dinner snacks, a time in which the energetic response to energy intake is decreased, further promoting a positive energy balance and weight gain. +, Positive energy balance; –, negative energy balance.
Mechanisms beyond appetite hormones
Potential explanations for increased energy intake during sleep restriction beyond appetite hormones include increased energy expenditure that does not seem to adapt to continued insufficient sleep113 and the activation of brain regions associated with changes in hunger and food choices. For example, healthy volunteers underwent restricted sleep in a laboratory setting under conditions of either controlled energy intake or ad libitum energy intake. Both conditions resulted in increased activation of areas of the brain associated with an increased desire for energy intake when the volunteers were shown pictures of food items114,115, particularly foods with high caloric content that could be deemed ‘unhealthy’ options116,117. Brain areas associated with reward following sleep restriction include the putamen, nucleus accumbens, thalamus, insula and prefrontal cortex.
Behavioural observations support these brain imaging findings as insufficient sleep is associated with poor dietary choices and altered dietary patterns118. Specifically, insufficient sleep was reported to increase the consumption of high-carbohydrate foods, fats, sugar-sweetened beverages and alcohol103,119–121, in addition to inducing an increased drive for hedonic eating. One potential mechanism for an elevated drive for hedonic eating during insufficient sleep is increased activation of the endocannabinoid system122, an important part of the hedonic food pathway123,124.
Large inter-individual and sex differences are observed in the amount of increased energy intake and energy expenditure occurring during insufficient sleep100,125–129. In general, inter-individual differences are consistent and robust100. Furthermore, men consistently show higher energy intake, energy expenditure and larger positive energy balance than women during insufficient sleep76,111. However, in epidemiological work, the notable association between short sleep and obesity and/or body composition is most consistently found in women130–133. Such inter-individual differences contribute to inconsistencies in some findings. For example, in highly controlled crossover research designs, where each participant serves as their own control, robust and meaningful differences in energy intake and expenditure are seen between conditions of insufficient sleep and of adequate sleep76. However, inter-individual designs are limited by large variability between individuals100.
Another important consideration in studies of insufficient sleep is the timing of food intake as when we eat has been demonstrated as an important determinant of metabolic health and disease risk134–137. In many individuals, insufficient sleep changes the biological timing of food intake. For example, insufficient sleep increases food intake later in the day76,103,121 and later timing of food intake (closer to the biological night) is associated with a reduced thermic effect of food (the energetic response to a meal)138,139 and with weight gain and obesity140. Of note, people who consume a larger proportion of their food intake later in the day show reduced weight loss during caloric restriction compared with those who eat a larger proportion of their food intake earlier in the day137. In adults with overweight, weight loss in response to caloric restriction under conditions of insufficient sleep leads to loss of muscle mass in lieu of adipose tissue mass compared with caloric restriction under conditions of adequate sleep141. Importantly, under experimental insufficient sleep conditions, switching to an adequate sleep schedule reduces food intake in lean adults75,76,100 and leads to weight loss over time in adults with obesity142.
Whether insufficient sleep reduces physical activity — an effect that would further contribute to a positive energy balance and weight gain — is unclear. Some individuals who are sleep restricted move less than those who have adequate sleep owing to increased tiredness, whereas others do not change their activity behaviours, thereby reflecting large inter-individual variability14. Decreased sleep duration in middle-aged adults was associated with increased sedentary activity (such as screen time143,144), including next-day sedentary activity144. Such increased sedentary time could contribute to reduced energy expenditure and increased risk for obesity and metabolic dysfunction.
Impact of circadian misalignment
Many aspects of 24-h energy metabolism are influenced by circadian processes. Circadian misalignment, from a metabolic perspective, is defined as energy intake, activity and wakefulness occurring during the biological night73,139,145,146 (Box 2). Circadian misalignment also disturbs sleep and thus insufficient sleep probably contributes to the alterations in metabolism observed during circadian misalignment. Furthermore, sleeping during the biological daytime probably also contributes to alterations in 24-h rhythms of metabolites and proteins65,67. Moreover, internal circadian desynchrony can occur between the central circadian clock and peripheral clocks when animals (such as mice) are awake, active and consuming energy during their inactive phase147, although data for such internal circadian desynchrony in humans is limited.
Energy expenditure
In contrast to findings regarding insufficient night-time sleep, simulated shift work (sleeping during the daytime and eating at night) reduced 24-h energy expenditure by ~3% (~55 kcal per day) and sleep energy expenditure by 12–16% (200–250 kcal per day) in healthy lean adults139. Examination of the human proteome during a simulated shift-work protocol in healthy lean individuals has provided some initial mechanistic insight into these changes. For example, decreased levels of fibroblast growth factor 19 (a protein that increases energy expenditure) were found to be associated with a reduction in energy expenditure65. Working during the biological night is also associated with increased rates of obesity and related metabolic diseases140,148. However, findings regarding energy intake during circadian misalignment induced by shift work are mixed. For example, a meta-analysis published in 2016 found no difference in energy intake between shift workers and non-shift workers149.
Food intake, physical activity and food timing
Another mechanism by which circadian misalignment could increase obesity risk is by alterations in food intake. For example, food choices made during circadian misalignment might be less healthy than those made during day work conditions (for example, less vegetables and more sweets and saturated fats); this effect has been observed in both lean individuals and individuals with overweight or obesity who are shift workers150,151. Circadian misalignment could also contribute to weight gain by inducing a reduction in physical activity in lean men and women152.
If sustained, reduced 24-h energy expenditure during circadian misalignment, even without a change in energy intake, could result in weight gain over time. Indeed, when food intake is restricted to the time of day typically reserved for sleep, mice show higher weight gain than when their food intake is restricted to the time of typical wakefulness. This finding occurs despite similar amounts of caloric intake and activity levels134,153. In conjunction with a circadian variation in the thermic effect of food in humans, these findings indicate that a calorie is not a calorie per se and that the timing of calorie intake has importance for metabolic health.
Appetite hormones
Under conditions of controlled energy intake or energy balance in healthy adults, circadian misalignment has been reported to have minimal influence on total circulating levels of ghrelin139. However, under these same conditions, circadian misalignment increases postprandial levels of active (acylated) ghrelin154 and reduces levels of leptin139,155,156 and PYY139 (Fig. 2), which should promote energy intake. Findings for hunger during circadian misalignment are mixed, with overall decreases139 or postprandial increases154. Moreover, there is a paucity of evidence for changes in 24-h patterns of other gut satiety hormones (for example, GLP1 or pancreatic polypeptide) in humans during circadian misalignment.
Other factors in addition to appetite hormones might contribute to hunger during circadian misalignment (for example, reduced 24-h energy expenditure139 and reduced circadian drive for hunger; mechanisms are summarized in ref.91 and Fig. 5). Additional research is needed to determine whether energy intake is promoted under conditions of circadian misalignment and ad libitum feeding. Additionally, whether repeated exposures to circadian misalignment (for example, during night-shift work) and alignment (days off) chronically alter appetite hormones and energy intake remains to be determined. Finally, inter-individual differences during circadian misalignment that might be sex dependent should be examined152.
Fig. 5. Circadian misalignment affects energy intake and appetite hormones, which potentially leads to a positive energy balance and the risk of weight gain.
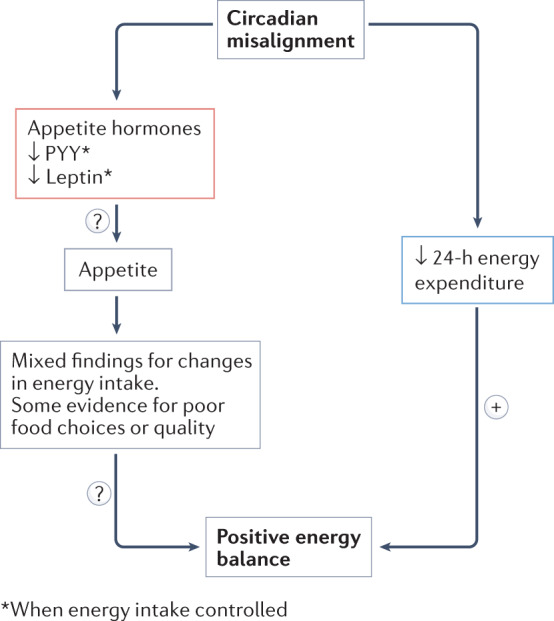
During experimental conditions of circadian misalignment in healthy adults, when energy intake is designed to meet energy balance demands for a typical day with adequate night-time sleep at baseline, there is a decrease in 24-h energy expenditure predominantly due to decreased sleeping energy expenditure. Hunger might increase owing to changes in appetite hormones, but hunger might also decrease owing to the circadian variation in hunger that shows lower hunger levels during the biological night-time than during the biological daytime. Alternations in food choices and eating during the biological night might also contribute to weight gain. Pathways with limited evidence are indicated with ‘?’. +, positive energy balance; PYY, peptide-YY.
Combined effects
The combined effects of circadian misalignment and insufficient sleep can be assessed using a modified forced desynchrony protocol, which permits assessment of circadian and sleep–wakefulness-driven processes. Under presumed negative energy balance conditions in older and younger adults, combined circadian misalignment and insufficient sleep increased blood levels of ghrelin and decreased blood levels of leptin, which should promote energy intake157. However, decreased levels of PYY were also found, which should reduce energy intake157. Experimental studies with ad libitum food intake in humans are needed to determine the influence of circadian misalignment on energy intake under these conditions. Notably, when sleep restriction and circadian misalignment are combined and energy intake is controlled in healthy young adults in a fasted state, circadian timing seems to be more influential on appetite hormone fluctuations than sleep restriction81.
Circadian misalignment and obesity risk
To date, the scientific literature on circadian misalignment and obesity risk has primarily focused on fairly large challenges to the circadian system (for example, night-shift work or a 12-h inverted shift in behaviours). Smaller degrees of misalignment, such as staying up late on weekends (social jetlag; commonly found in teenagers), travel across a few time zones, early work start times (for example, early morning shift work) and insufficient sleep (which can lead to morning misalignment or energy intake at night) occur more frequently than large degrees of misalignment, and are also associated with adverse metabolic health158,159. For example, every hour a person must shift their internal clock to match the wakefulness period between weekends and weekdays resulted in an increased odds ratio of 1.3 of having metabolic syndrome in the general population160. Likewise, social jetlag score (a higher score is indicative of a greater change in sleep timing between weekdays and weekends) is positively associated with obesity in the general population161.
Observations between social jetlag and health have predominately been conducted in cross-sectional designs, which limit the ability to identify mechanisms for observed associations. However, individuals with an obesity-related chronic illness with a higher social jetlag consume more calorie-dense foods than those with a lower score162. This finding could be driven by higher circulating levels of ghrelin, as observed in lean adults with social jetlag in free-living conditions163. Insufficient sleep also leads to morning circadian misalignment (melatonin levels are still high in the morning) or to energy intake during the biological night. Such morning circadian misalignment contributes to metabolic dysregulation (for example, in blood levels of insulin and glucose) in humans76,113,145,164,165.
Obesity and its effect on sleep
People with obesity typically report reductions in both sleep duration and quality, although research has largely focused on sleep disorders14,166. Although there is no discounting the importance of sleep disorders in this population, little is known about the independent effects of obesity on sleep itself. In addition, most investigations into the association between obesity and sleep rely on self-reported sleep and cross-sectional study designs. Such research might not adequately control for confounders and is unable to determine the directionality of the association14,166. Although limited, evidence suggests that adults with obesity are more likely to report either short or long sleep durations compared with adults without obesity, who reported sleep of between 7 and 8 h per night14,166. However, whether poor sleep quality is a factor in this U-shaped association is unclear as sleep fragmentation might not be accounted for in these studies and can be one reason for a longer sleep duration (in addition to other underlying comorbidities). Adults with obesity are also more likely to report sleep problems than people without any comorbidities167. Excessive daytime sleepiness has also been reported in adults with severe obesity but without obstructive sleep apnoea168.
A variety of physiological factors could affect sleep in a population with obesity. For example, the location of adipose tissue has a role in the risk of certain sleep disorders. For instance, abdominal obesity and large neck circumference are risk factors for obstructive sleep apnoea169. Visceral adipose tissue is also well established as a key adipose depot associated with cardiovascular disease risk and T2DM. Other factors, such as inflammatory markers170 and gut microbiome171, should also be considered for their effects on sleep. Additionally, behavioural factors, such as poor diet and lack of physical activity, are likely to have an impact on sleep. More research is needed to elucidate the causal mechanisms that link sleep and circadian disruption in order to define the directionality of these associations.
Potential strategies to improve sleep
This section briefly discusses some potential strategies that might help individuals to mitigate the adverse effects of sleep and circadian disruption on metabolic health. These strategies do not currently differ much from traditional sleep hygiene strategies and a detailed discussion of sleep hygiene falls outside the scope of this paper. Further information can be found at the National Sleep Foundation.
Physical activity
Increased levels of physical activity are well known to be related to decreased levels of metabolic syndrome172–174. Furthermore, a synergistic health effect has been documented of physical inactivity and poor sleep on the development of metabolic syndrome and increased mortality175,176. Findings also suggest that evening physical activity should be discouraged owing to a disturbance of night-time sleep; however, any effect here is likely to be small177. Of note, whether being physically active helps to prevent or reduce the metabolic health consequences of insufficient sleep and circadian misalignment is unknown.
Eat well and avoid eating at night
Healthy eating patterns have been reported to be associated with a decreased risk of developing metabolic syndrome178,179. Healthful diets, especially dietary patterns similar to the Mediterranean diet, have been associated with improved sleep quality in various populations180. Increased food intake in the evening is associated with weight gain and obesity140 and reduces the effectiveness of weight loss programmes137. A 2022 study showed that early time-restricted feeding in healthy adults (food intake restricted to the early part of the day) provides greater benefits for insulin resistance and related metabolic parameters than mid-day time-restricted feeding181.
Have brighter days and dimmer nights
Bright daytime and dim evening light exposure is important for circadian alignment and could benefit metabolic function182–184. Further studies are needed to examine whether increasing bright light exposure during the day (by going outside more often) can improve metabolic health by improving sleep and circadian health11. In addition, research is needed to determine whether bright light exposure during evening physical activity could affect sleep. Previous research has shown that a reduction of exposure to blue light at night promotes better sleep quality185–187. This strategy might also decrease the risk of developing metabolic syndrome by improving fasting plasma levels of glucose and insulin resistance; however, more research in this area is needed186.
Avoid caffeine late in the day
Observational studies report that people who drink coffee seem to have a lower risk of obesity, metabolic syndrome and T2DM than people who do not drink coffee188–190. However, caffeine consumed later in the day is well known to disrupt sleep. For example, in healthy adults, 400 mg of caffeine taken 6 h before bedtime was found to reduce sleep by more than 1 h (ref.191). Caffeine might also contribute to late sleep and circadian timing. Furthermore, consumption of a caffeine dose equivalent to that in a double espresso 3 h before habitual bedtime in healthy adults induced a ~40-min phase delay of the circadian melatonin rhythm192. The magnitude of that delay was nearly half the size of the delay induced by evening exposure to bright light. Further research is needed to determine whether earlier versus later time of day caffeine consumption has benefits for sleep, circadian alignment and metabolic health.
Have a nap
A dose–response meta-analysis on napping found a J-shaped relationship between the length of nap time and the risk of T2DM and metabolic syndrome193. Napping up to about 40 min per day had no effect, followed by a sharp increase in the risk at longer nap times. Short naps (10–20 min) have been associated with a wide range of health benefits in healthy young adults, including improved cognitive functions and a reduction in daytime sleepiness and fatigue194. A short nap when night-time sleep is insufficient could potentially help reduce the adverse effects of a lack of night-time sleep on metabolic health but research in this area is needed.
Limit alcohol consumption and do not smoke
Alcohol consumption in adults has been found to interact with reduced sleep duration to increase the risk of dysglycaemia195. Evidence also suggests that smoking is associated with the development of metabolic syndrome whereas smoking cessation seems to reduce this risk196. People who smoke, particularly at night-time, have longer sleep latency, more awakenings, poorer sleep quality and shorter sleep duration than people who do not smoke44,197,198. Not smoking and limiting alcohol consumption, especially near bedtime, are recommended for healthy sleep and optimal metabolic regulation.
Get treatment
Effective treatment strategies are available for sleep problems and sleep and circadian disorders. As noted, sleep and circadian disorders are often comorbid with mental health and obesity. Treating sleep and circadian problems and any related health conditions concurrently is generally associated with better health outcomes compared with treating these disorders alone199,200. Addressing modern emotional stresses and mental health issues is also important given that they are prominent risk factors for insufficient sleep and obesity.
Conclusions
Growing evidence indicates that both insufficient sleep and circadian misalignment contribute to adverse metabolic health and obesity by altering multiple components of energy metabolism and behaviour. Insufficient sleep increases 24 h energy expenditure and, under controlled energy intake conditions, changes in appetite hormones occur that promote hunger and energy intake75,76,80,84. Importantly, during insufficient sleep and ad libitum food intake, 24 h energy intake is higher than the increase in 24 h energy expenditure, which leads to a positive energy balance5,76,110. Furthermore, energy intake tends to occur later in the day (for example, after dinner) despite appetite-reducing changes in the levels of appetite hormones. Later timing of food intake is associated with lower thermic effects of food than earlier timing of intake and obesity76,103,121,138–140. The timing of food intake is emerging as an important factor in weight regulation. Food choices during conditions of insufficient sleep might also be less healthy than during adequate sleep103,118–121.
Circadian misalignment increases the risk of obesity by reducing 24 h energy expenditure. Furthermore, changes in appetite hormones occur that promote hunger and energy intake139,154–156. Energy intake does not seem to be higher in shift workers experiencing circadian misalignment than in non-shift workers; however, food choices might be less healthy and obesity rates are higher149–152. Findings from rodent models indicate that the consumption of calories during the circadian time typically reserved for sleep leads to more weight gain than consumption of the same number of calories during the circadian time typically reserved for wakefulness134,153. These findings highlight that, even without changes in energy intake, weight gain could ensue when energy is consumed at inappropriate circadian times.
Knowledge in this field has substantially increased over the past 10 years and the importance of sleep is increasingly recognized in public health strategies and clinical practice201,202. However, key knowledge gaps remain and future studies are needed to address these gaps and move the agenda forward (Box 3).
Although nutrition and physical activity are key health pillars, it is important that we pay more attention to sleep and circadian health in today’s society. Sleep and circadian rhythms are critical for optimal metabolic and weight regulation and directly influence eating and activity behaviours to impact health. Future efforts should aim to quantify the global burden of disease associated with poor sleep health and circadian health (for example, health-care and productivity costs) and test the cost-effectiveness of interventions at the population level. Sleep and circadian health are important pillars of health and are part of an overall healthy lifestyle along with a healthy diet and physical activity.
Box 3 Research priorities in relation to sleep disruption and metabolic health and obesity.
Large trials with long follow-ups are needed to determine whether the short-term effects of sleep restriction and circadian disruption on metabolic health and obesity last over time. Furthermore, studies are needed to determine whether there are differences between acute and chronic insufficient sleep and circadian disruption. Research in this area is limited by safety concerns; thus, designs are mostly limited to observational studies.
Longitudinal studies are needed that follow people across their lifespan in order to determine whether the associations between insufficient sleep and/or misaligned sleep, metabolic outcomes, and obesity are affected by age.
The interaction between sleep, circadian clocks and gut hormones and how these factors modulate appetite and metabolism as well as their clinical relevance for the efficacy of novel pharmacotherapies for obesity should be examined.
More studies should examine the potential risks and benefits of ‘catch-up sleep’ on metabolic health and weight regulation.
The timing of food intake as it relates to the sleep schedule and circadian timing as well as its influence on altering metabolic health and obesity should be examined.
Studies are needed to examine how the different sleep health characteristics, combined and individually, affect metabolic health and obesity.
Research is needed to determine whether energy intake is promoted under conditions of circadian misalignment and ad libitum food intake.
Studies are needed to examine the most effective circadian times for exercising and how much exercise is needed for shift workers to maintain their metabolic health.
Sleep extension and/or improvement interventions are needed that are aimed at improving metabolic health as well as an examination of their effects on metabolic health outcomes and weight.
Studies should examine whether obesity, independent of sleep disorders, causes poor sleep and should identify the underlying mechanisms.
Additional investigations are needed into how diet content and quality affect circadian rhythmicity and sleep health.
Acknowledgements
The authors acknowledge the support of the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number T32HL149646 and K01HL146992. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Glossary
- Central circadian clock
Residing in the suprachiasmatic nucleus of the hypothalamus (master oscillator in humans), the central circadian clock receives light cues and drives circadian rhythms.
- The Fourth Industrial Revolution
This time period in the twenty-first century entailed rapid changes to technology, industries, societal patterns and processes due to increasing interconnectivity and smart automation.
- Caffeine
This central nervous system stimulant has a mean half-life in the plasma of healthy individuals of about 5 h.
- Melatonin
This important circadian hormone is predominantly produced in the pineal gland and induces physiological changes to help prepare the body and brain for sleep and increase sleepiness.
- Sleep onset latency
The length of time it takes to fall asleep.
- Peripheral circadian clocks
Clocks located in cells, tissues or organs outside the suprachiasmatic nucleus.
- Hedonic eating
Eating for pleasure and not hunger.
- Mediterranean diet
A diet characterized by plant-based foods such as whole grains, vegetables, legumes, fruits, nuts, seeds, herbs and spices.
Author contributions
All authors researched data for the article, contributed to discussion of the content, wrote the article, and reviewed and/or edited the manuscript before submission.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Satchidananda Panda, who reviewed the manuscript with Laura Van Rosmalen; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interests
K.P.W. reports research support and donated materials from DuPont Nutrition & Biosciences, Grain Processing Corporation and Friesland Campina Innovation Centre. K.P.W. also reports financial relationships, including consulting with or without receiving fees and/or serving on the advisory boards for Circadian Therapeutics, LTD., Circadian Biotherapies, Inc., Philips Respironics, and the U.S. Army Medical Research and Materiel Command–Walter Reed Army Institute of Research. The other authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
IOMC: sleep quality and pain: https://www.iomcworld.org/medical-journals/sleep-quality-and-pain-52349.html
National Sleep Foundation: https://www.thensf.org/
References
- 1.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keith SW, et al. Putative contributors to the secular increase in obesity: exploring the roads less traveled. Int. J. Obes. 2006;30:1585–1594. doi: 10.1038/sj.ijo.0803326. [DOI] [PubMed] [Google Scholar]
- 3.McHill AW, Wright KP. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes. Rev. 2017;18:15–24. doi: 10.1111/obr.12503. [DOI] [PubMed] [Google Scholar]
- 4.Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018;84:56–66. doi: 10.1016/j.metabol.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Zhu B, Shi C, Park CG, Zhao X, Reutrakul S. Effects of sleep restriction on metabolism-related parameters in healthy adults: a comprehensive review and meta-analysis of randomized controlled trials. Sleep Med. Rev. 2019;45:18–30. doi: 10.1016/j.smrv.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Liu Y, et al. Prevalence of healthy sleep duration among adults–United States, 2014. Morb. Mortal. Wkly. Rep. 2016;65:137–141. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 7.Chaput J-P, Wong SL, Michaud I. Duration and quality of sleep among Canadians aged 18 to 79. Health Rep. 2017;28:28–33. [PubMed] [Google Scholar]
- 8.Zhu G, et al. Objective sleep assessment in >80,000 UK mid-life adults: associations with sociodemographic characteristics, physical activity and caffeine. PLoS ONE. 2019;14:e0226220. doi: 10.1371/journal.pone.0226220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morita Y, Sasai-Sakuma T, Asaoka S, Inoue Y. Prevalence and correlates of insufficient sleep syndrome in Japanese young adults: a web-based cross-sectional study. J. Clin. Sleep Med. 2015;11:1163–1169. doi: 10.5664/jcsm.5092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan CMH, et al. Prevalence of insufficient sleep and its associated factors among working adults in Malaysia. Nat. Sci. Sleep. 2021;13:1109–1116. doi: 10.2147/NSS.S295537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wright KP, et al. Entrainment of the human circadian clock to the natural light-dark cycle. Curr. Biol. 2013;23:1554–1558. doi: 10.1016/j.cub.2013.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Su F, Huang D, Wang H, Yang Z. Associations of shift work and night work with risk of all-cause, cardiovascular and cancer mortality: a meta-analysis of cohort studies. Sleep Med. 2021;86:90–98. doi: 10.1016/j.sleep.2021.08.017. [DOI] [PubMed] [Google Scholar]
- 13.IARC Working Group on the Identification of Carcinogenic Hazards to Humans. Night Shift Work. IARC Monographs on the Identification of Carcinogenic Hazards to Humanshttps://publications.iarc.fr/Book-And-Report-Series/Iarc-Monographs-On-The-Identification-Of-Carcinogenic-Hazards-To-Humans/Night-Shift-Work-2020 (2020).
- 14.Chaput J-P, et al. Sleep duration and health in adults: an overview of systematic reviews. Appl. Physiol. Nutr. Metab. 2020;45(10 Suppl. 2):S218–S231. doi: 10.1139/apnm-2020-0034. [DOI] [PubMed] [Google Scholar]
- 15.Boege HL, Bhatti MZ, St-Onge M-P. Circadian rhythms and meal timing: impact on energy balance and body weight. Curr. Opin. Biotechnol. 2021;70:1–6. doi: 10.1016/j.copbio.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ancoli-Israel S. ‘Sleep is not tangible’ or what the Hebrew tradition has to say about sleep. Psychosom. Med. 2001;63:778–787. doi: 10.1097/00006842-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Shochat T. Impact of lifestyle and technology developments on sleep. Nat. Sci. Sleep. 2012;4:19–31. doi: 10.2147/NSS.S18891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Owens J. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134:e921–e932. doi: 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yetish G, et al. Natural sleep and its seasonal variations in three pre-industrial societies. Curr. Biol. 2015;25:2862–2868. doi: 10.1016/j.cub.2015.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ekirch AR. The modernization of western sleep: or, does insomnia have a history? Past Present. 2015;226:149–192. doi: 10.1093/pastj/gtu040. [DOI] [Google Scholar]
- 21.Gangwisch JE. Work-life balance. Sleep. 2014;37:1159–1160. doi: 10.5665/sleep.3826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Min J, et al. The fourth industrial revolution and its impact on occupational health and safety, worker’s compensation and labor conditions. Saf. Health Work. 2019;10:400–408. doi: 10.1016/j.shaw.2019.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shriane AE, Ferguson SA, Jay SM, Vincent GE. Sleep hygiene in shift workers: a systematic literature review. Sleep Med. Rev. 2020;53:101336. doi: 10.1016/j.smrv.2020.101336. [DOI] [PubMed] [Google Scholar]
- 24.Harknett K, Schneider D, Irwin V. Improving health and economic security by reducing work schedule uncertainty. Proc. Natl Acad. Sci. USA. 2021;118:e2107828118. doi: 10.1073/pnas.2107828118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jehan S, et al. Shift work and sleep: medical implications and management. Sleep Med. Disord. Int. J. 2017;1:00008. [PMC free article] [PubMed] [Google Scholar]
- 26.Lund L, Sølvhøj IN, Danielsen D, Andersen S. Electronic media use and sleep in children and adolescents in western countries: a systematic review. BMC Public Health. 2021;21:1598. doi: 10.1186/s12889-021-11640-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Castro O, Bennie J, Vergeer I, Bosselut G, Biddle SJH. How sedentary are university students? A systematic review and meta-analysis. Prev. Sci. 2020;21:332–343. doi: 10.1007/s11121-020-01093-8. [DOI] [PubMed] [Google Scholar]
- 28.LeBlanc AG, et al. Correlates of total sedentary time and screen time in 9–11 year-old children around the world: the international study of childhood obesity, lifestyle and the environment. PLoS ONE. 2015;10:e0129622. doi: 10.1371/journal.pone.0129622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haug S, et al. Smartphone use and smartphone addiction among young people in Switzerland. J. Behav. Addict. 2015;4:299–307. doi: 10.1556/2006.4.2015.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murdock KK, Adams SK, Crichlow-Ball C, Horissian M, Roberts M. Nighttime notifications and compulsivity illuminate the link between emerging adults’ cellphone use and sleep-related problems. Psychol. Pop. Media Cult. 2019;8:12–21. doi: 10.1037/ppm0000156. [DOI] [Google Scholar]
- 31.Murdock KK, Horissian M, Crichlow-Ball C. Emerging adults’ text message use and sleep characteristics: a multimethod, naturalistic study. Behav. Sleep Med. 2017;15:228–241. doi: 10.1080/15402002.2015.1120203. [DOI] [PubMed] [Google Scholar]
- 32.Thomée S, Härenstam A, Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults — a prospective cohort study. BMC Public Health. 2011;11:66. doi: 10.1186/1471-2458-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Twenge JM, Hisler GC, Krizan Z. Associations between screen time and sleep duration are primarily driven by portable electronic devices: evidence from a population-based study of U.S. children ages 0–17. Sleep Med. 2019;56:211–218. doi: 10.1016/j.sleep.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Tähkämö L, Partonen T, Pesonen A-K. Systematic review of light exposure impact on human circadian rhythm. Chronobiol. Int. 2019;36:151–170. doi: 10.1080/07420528.2018.1527773. [DOI] [PubMed] [Google Scholar]
- 35.Wams EJ, et al. Linking light exposure and subsequent sleep: a field polysomnography study in humans. Sleep. 2017;40:zsx165. doi: 10.1093/sleep/zsx165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alimoradi Z, et al. Internet addiction and sleep problems: a systematic review and meta-analysis. Sleep Med. Rev. 2019;47:51–61. doi: 10.1016/j.smrv.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Tandon A, Kaur P, Dhir A, Mäntymäki M. Sleepless due to social media? Investigating problematic sleep due to social media and social media sleep hygiene. Comput. Hum. Behav. 2020;113:106487. doi: 10.1016/j.chb.2020.106487. [DOI] [Google Scholar]
- 38.Kristensen JH, Pallesen S, King DL, Hysing M, Erevik EK. Problematic gaming and sleep: a systematic review and meta-analysis. Front. Psychiatry. 2021;12:830. doi: 10.3389/fpsyt.2021.675237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peracchia S, Curcio G. Exposure to video games: effects on sleep and on post-sleep cognitive abilities. A sistematic review of experimental evidences. Sleep Sci. 2018;11:302–314. doi: 10.5935/1984-0063.20180046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higuchi S, Motohashi Y, Liu Y, Maeda A. Effects of playing a computer game using a bright display on presleep physiological variables, sleep latency, slow wave sleep and REM sleep. J. Sleep Res. 2005;14:267–273. doi: 10.1111/j.1365-2869.2005.00463.x. [DOI] [PubMed] [Google Scholar]
- 41.Fulgoni VL, Keast DR, Lieberman HR. Trends in intake and sources of caffeine in the diets of US adults: 2001–2010. Am. J. Clin. Nutr. 2015;101:1081–1087. doi: 10.3945/ajcn.113.080077. [DOI] [PubMed] [Google Scholar]
- 42.James JE, Kristjánsson AL, Sigfúsdóttir ID. Adolescent substance use, sleep, and academic achievement: evidence of harm due to caffeine. J. Adolesc. 2011;34:665–673. doi: 10.1016/j.adolescence.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 43.Clark I, Landolt HP. Coffee, caffeine, and sleep: a systematic review of epidemiological studies and randomized controlled trials. Sleep Med. Rev. 2017;31:70–78. doi: 10.1016/j.smrv.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 44.Nuñez A, et al. Smoke at night and sleep worse? The associations between cigarette smoking with insomnia severity and sleep duration. Sleep Health. 2021;7:177–182. doi: 10.1016/j.sleh.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 45.Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME. Trends in adolescent vaping, 2017–2019. N. Engl. J. Med. 2019;381:1490–1491. doi: 10.1056/NEJMc1910739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamberger ES, Halpern-Felsher B. Vaping in adolescents: epidemiology and respiratory harm. Curr. Opin. Pediatr. 2020;32:378–383. doi: 10.1097/MOP.0000000000000896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kianersi S, Zhang Y, Rosenberg M, Macy JT. Association between e-cigarette use and sleep deprivation in U.S. Young adults: results from the 2017 and 2018 behavioral risk factor surveillance system. Addict. Behav. 2021;112:106646. doi: 10.1016/j.addbeh.2020.106646. [DOI] [PubMed] [Google Scholar]
- 48.Grucza RA, et al. Trends in adult alcohol use and binge drinking in the early 21st-century united states: a meta-analysis of 6 national survey series. Alcohol. Clin. Exp. Res. 2018;42:1939–1950. doi: 10.1111/acer.13859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eacret D, Veasey SC, Blendy JA. Bidirectional relationship between opioids and disrupted sleep: putative mechanisms. Mol. Pharmacol. 2020;98:445–453. doi: 10.1124/mol.119.119107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Edwards D, Filbey FM. Are sweet dreams made of these? Understanding the relationship between sleep and cannabis use. Cannabis Cannabinoid Res. 2021;6:462–473. doi: 10.1089/can.2020.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baglioni C, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 52.Baglioni C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol. Bull. 2016;142:969–990. doi: 10.1037/bul0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gregory AM, Rijsdijk FV, Lau JYF, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep. 2009;32:189. doi: 10.1093/sleep/32.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Olfson M, Wang S, Wall M, Marcus SC, Blanco C. Trends in serious psychological distress and outpatient mental health care of US adults. JAMA Psychiatry. 2019;76:152–161. doi: 10.1001/jamapsychiatry.2018.3550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bliese PD, Edwards JR, Sonnentag S. Stress and well-being at work: a century of empirical trends reflecting theoretical and societal influences. J. Appl. Psychol. 2017;102:389–402. doi: 10.1037/apl0000109. [DOI] [PubMed] [Google Scholar]
- 56.Tsang S, Avery AR, Seto EYW, Duncan GE. Is COVID-19 keeping us up at night? Stress, anxiety, and sleep among adult twins. Front. Neurosci. 2021;15:479. doi: 10.3389/fnins.2021.665777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ogunbode CA, et al. Negative emotions about climate change are related to insomnia symptoms and mental health: Cross-sectional evidence from 25 countries. Curr. Psychol. 2021 doi: 10.1007/s12144-021-01385-4. [DOI] [Google Scholar]
- 58.Nollet M, Wisden W, Franks NP. Sleep deprivation and stress: a reciprocal relationship. Interface Focus. 2020;10:20190092. doi: 10.1098/rsfs.2019.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cuesta M, Cermakian N, Boivin DB. Glucocorticoids entrain molecular clock components in human peripheral cells. FASEB J. 2015;29:1360–1370. doi: 10.1096/fj.14-265686. [DOI] [PubMed] [Google Scholar]
- 60.O’Neill JS, Reddy AB. Circadian clocks in human red blood cells. Nature. 2011;469:498–503. doi: 10.1038/nature09702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Archer SN, et al. Mistimed sleep disrupts circadian regulation of the human transcriptome. Proc. Natl Acad. Sci. USA. 2014;111:E682–E691. doi: 10.1073/pnas.1316335111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Christou S, et al. Circadian regulation in human white adipose tissue revealed by transcriptome and metabolic network analysis. Sci. Rep. 2019;9:2641. doi: 10.1038/s41598-019-39668-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ruben MD, et al. A database of tissue-specific rhythmically expressed human genes has potential applications in circadian medicine. Sci. Transl Med. 2018;10:eaat8806. doi: 10.1126/scitranslmed.aat8806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kervezee L, Cuesta M, Cermakian N, Boivin DB. Simulated night shift work induces circadian misalignment of the human peripheral blood mononuclear cell transcriptome. Proc. Natl Acad. Sci. USA. 2018;115:5540–5545. doi: 10.1073/pnas.1720719115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Depner CM, Melanson EL, McHill AW, Wright KP. Mistimed food intake and sleep alters 24-hour time-of-day patterns of the human plasma proteome. Proc. Natl Acad. Sci. USA. 2018;115:E5390–E5399. doi: 10.1073/pnas.1714813115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dallmann R, Viola AU, Tarokh L, Cajochen C, Brown SA. The human circadian metabolome. Proc. Natl Acad. Sci. USA. 2012;109:2625–2629. doi: 10.1073/pnas.1114410109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Skene DJ, et al. Separation of circadian-and behavior-driven metabolite rhythms in humans provides a window on peripheral oscillators and metabolism. Proc. Natl Acad. Sci. USA. 2018;115:7825–7830. doi: 10.1073/pnas.1801183115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chua EC-P, et al. Extensive diversity in circadian regulation of plasma lipids and evidence for different circadian metabolic phenotypes in humans. Proc. Natl Acad. Sci. USA. 2013;110:14468–14473. doi: 10.1073/pnas.1222647110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wu G, et al. Population-level rhythms in human skin with implications for circadian medicine. Proc. Natl Acad. Sci. USA. 2018;115:12313–12318. doi: 10.1073/pnas.1809442115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Anafi RC, Francey LJ, Hogenesch JB, Kim J. CYCLOPS reveals human transcriptional rhythms in health and disease. Proc. Natl Acad. Sci. USA. 2017;114:5312–5317. doi: 10.1073/pnas.1619320114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Imeri L, Opp MR. How (and why) the immune system makes us sleep. Nat. Rev. Neurosci. 2009;10:199–210. doi: 10.1038/nrn2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Morris CJ, Purvis TE, Hu K, Scheer FA. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc. Natl Acad. Sci. USA. 2016;113:E1402–E1411. doi: 10.1073/pnas.1516953113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Morris CJ, et al. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc. Natl Acad. Sci. USA. 2015;112:E2225–E2234. doi: 10.1073/pnas.1418955112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Arble DM, et al. Impact of sleep and circadian disruption on energy balance and diabetes: a summary of workshop discussions. Sleep. 2015;38:1849–1860. doi: 10.5665/sleep.5226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jung CM, et al. Energy expenditure during sleep, sleep deprivation and sleep following sleep deprivation in adult humans. J. Physiol. 2011;589:235–244. doi: 10.1113/jphysiol.2010.197517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Markwald RR, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc. Natl Acad. Sci. USA. 2013;110:5695–5700. doi: 10.1073/pnas.1216951110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zitting K-M, et al. Human resting energy expenditure varies with circadian phase. Curr. Biol. 2018;28:3685–3690. doi: 10.1016/j.cub.2018.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Morgan L, et al. Effects of the endogenous clock and sleep time on melatonin, insulin, glucose and lipid metabolism. J. Endocrinol. 1998;157:443–452. doi: 10.1677/joe.0.1570443. [DOI] [PubMed] [Google Scholar]
- 79.Shea SA, Hilton MF, Orlova C, Ayers RT, Mantzoros CS. Independent circadian and sleep/wake regulation of adipokines and glucose in humans. J. Clin. Endocrinol. Metab. 2005;90:2537–2544. doi: 10.1210/jc.2004-2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rynders CA, Morton SJ, Bessesen DH, Wright KP, Jr, Broussard JL. Circadian rhythm of substrate oxidation and hormonal regulators of energy balance. Obesity. 2020;28(Suppl. 1):S104–S113. doi: 10.1002/oby.22816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McHill AW, Hull JT, McMullan CJ, Klerman EB. Chronic insufficient sleep has a limited impact on circadian rhythmicity of subjective hunger and awakening fasted metabolic hormones. Front. Endocrinol. 2018;9:319. doi: 10.3389/fendo.2018.00319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Czeisler CA, Klerman EB. Circadian and sleep-dependent regulation of hormone release in humans. Recent. Prog. Horm. Res. 1999;54:97–130. [PubMed] [Google Scholar]
- 83.Simon C, Gronfier C, Schlienger JL, Brandenberger G. Circadian and ultradian variations of leptin in normal man under continuous enteral nutrition: relationship to sleep and body temperature. J. Clin. Endocrinol. Metab. 1998;83:1893–1899. doi: 10.1210/jcem.83.6.4864. [DOI] [PubMed] [Google Scholar]
- 84.Cummings DE, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N. Engl. J. Med. 2002;346:1623–1630. doi: 10.1056/NEJMoa012908. [DOI] [PubMed] [Google Scholar]
- 85.Spiegel K, Tasali E, Leproult R, Scherberg N, Van Cauter E. Twenty-four-hour profiles of acylated and total ghrelin: relationship with glucose levels and impact of time of day and sleep. J. Clin. Endocrinol. Metab. 2011;96:486–493. doi: 10.1210/jc.2010-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mason, I., McHill, A. W., Wright, K. P. Jr. & Scheer, F. A. J. L. in Principles and Practice of Sleep Medicine 7th Edn (eds Kryger, M. H., Roth, T. & Goldstein, C. A.) 423–432 (Elsevier, 2021).
- 87.Broussard, J. L. et al. in Biological Timekeeping: Clocks, Rhythms and Behaviour (ed. Kumar, V.) 279–295 (Springer, 2017).
- 88.Nakazato M, et al. A role for ghrelin in the central regulation of feeding. Nature. 2001;409:194–198. doi: 10.1038/35051587. [DOI] [PubMed] [Google Scholar]
- 89.Morris A. Mapping leptin-responsive neurons in the hypothalamus. Nat. Rev. Endocrinol. 2019;15:376–377. doi: 10.1038/s41574-019-0209-3. [DOI] [PubMed] [Google Scholar]
- 90.Batterham RL, et al. Gut hormone PYY3-36 physiologically inhibits food intake. Nature. 2002;418:650–654. doi: 10.1038/nature00887. [DOI] [PubMed] [Google Scholar]
- 91.Scheer FAJL, Morris CJ, Shea SA. The internal Circadian clock increases hunger and appetite in the evening independent of food intake and other behaviors. Obesity. 2013;21:421. doi: 10.1002/oby.20351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chan JL, Bullen J, Lee JH, Yiannakouris N, Mantzoros CS. Ghrelin levels are not regulated by recombinant leptin administration and/or three days of fasting in healthy subjects. J. Clin. Endocrinol. Metab. 2004;89:335–343. doi: 10.1210/jc.2003-031412. [DOI] [PubMed] [Google Scholar]
- 93.Weigle DS, et al. Roles of leptin and ghrelin in the loss of body weight caused by a low fat, high carbohydrate diet. J. Clin. Endocrinol. Metab. 2003;88:1577–1586. doi: 10.1210/jc.2002-021262. [DOI] [PubMed] [Google Scholar]
- 94.Spiegel K, et al. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J. Clin. Endocrinol. Metab. 2004;89:5762–5771. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- 95.Galindo Muñoz JS, Jiménez Rodríguez D, Hernández Morante JJ. Diurnal rhythms of plasma GLP-1 levels in normal and overweight/obese subjects: lack of effect of weight loss. J. Physiol. Biochem. 2015;71:17–28. doi: 10.1007/s13105-014-0375-7. [DOI] [PubMed] [Google Scholar]
- 96.Batterham RL, et al. Pancreatic polypeptide reduces appetite and food intake in humans. J. Clin. Endocrinol. Metab. 2003;88:3989–3992. doi: 10.1210/jc.2003-030630. [DOI] [PubMed] [Google Scholar]
- 97.Jorde R, Burhol PG. Fasting and diurnal plasma PP, and the effect of fasting and somatostatin on postprandial plasma PP. Acta Physiol. Scand. 1982;115:421–425. doi: 10.1111/j.1748-1716.1982.tb07100.x. [DOI] [PubMed] [Google Scholar]
- 98.Track NS, McLeod RS, Mee AV. Human pancreatic polypeptide: studies of fasting and postprandial plasma concentrations. Can. J. Physiol. Pharmacol. 1980;58:1484–1489. doi: 10.1139/y80-223. [DOI] [PubMed] [Google Scholar]
- 99.Johns CE, Newton JL, Westley BR, May FEB. Human pancreatic polypeptide has a marked diurnal rhythm that is affected by ageing and is associated with the gastric TFF2 circadian rhythm. Peptides. 2006;27:1341–1348. doi: 10.1016/j.peptides.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 100.Depner CM, et al. Effects of ad libitum food intake, insufficient sleep and weekend recovery sleep on energy balance. Sleep. 2021;44:zsab136. doi: 10.1093/sleep/zsab136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shechter A, Rising R, Albu JB, St-Onge M-P. Experimental sleep curtailment causes wake-dependent increases in 24-h energy expenditure as measured by whole-room indirect calorimetry. Am. J. Clin. Nutr. 2013;98:1433–1439. doi: 10.3945/ajcn.113.069427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Klingenberg L, et al. Sleep restriction is not associated with a positive energy balance in adolescent boys. Am. J. Clin. Nutr. 2012;96:240–248. doi: 10.3945/ajcn.112.038638. [DOI] [PubMed] [Google Scholar]
- 103.Nedeltcheva AV, et al. Sleep curtailment is accompanied by increased intake of calories from snacks. Am. J. Clin. Nutr. 2009;89:126–133. doi: 10.3945/ajcn.2008.26574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.St-Onge M-P, et al. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Am. J. Clin. Nutr. 2011;94:410–416. doi: 10.3945/ajcn.111.013904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann. Intern. Med. 2004;141:846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 106.Hibi M, et al. Effect of shortened sleep on energy expenditure, core body temperature, and appetite: a human randomised crossover trial. Sci. Rep. 2017;7:39640. doi: 10.1038/srep39640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Broussard JL, et al. Elevated ghrelin predicts food intake during experimental sleep restriction. Obesity. 2016;24:132–138. doi: 10.1002/oby.21321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.St-Onge M-P, O’Keeffe M, Roberts AL, RoyChoudhury A, Laferrère B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep. 2012;35:1503–1510. doi: 10.5665/sleep.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gonnissen HKJ, Hursel R, Rutters F, Martens EAP, Westerterp-Plantenga MS. Effects of sleep fragmentation on appetite and related hormone concentrations over 24 h in healthy men. Br. J. Nutr. 2013;109:748–756. doi: 10.1017/S0007114512001894. [DOI] [PubMed] [Google Scholar]
- 110.Al Khatib HK, Harding SV, Darzi J, Pot GK. The effects of partial sleep deprivation on energy balance: a systematic review and meta-analysis. Eur. J. Clin. Nutr. 2017;71:614–624. doi: 10.1038/ejcn.2016.201. [DOI] [PubMed] [Google Scholar]
- 111.Spaeth AM, Dinges DF, Goel N. Sex and race differences in caloric intake during sleep restriction in healthy adults. Am. J. Clin. Nutr. 2014;100:559–566. doi: 10.3945/ajcn.114.086579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chaput J-P, St-Onge M-P. Increased food intake by insufficient sleep in humans: are we jumping the gun on the hormonal explanation? Front. Endocrinol. 2014;5:116. doi: 10.3389/fendo.2014.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Depner CM, et al. Ad libitum weekend recovery sleep fails to prevent metabolic dysregulation during a repeating pattern of insufficient sleep and weekend recovery sleep. Curr. Biol. 2019;29:957–967. doi: 10.1016/j.cub.2019.01.069. [DOI] [PubMed] [Google Scholar]
- 114.St-Onge M-P, et al. Sleep restriction leads to increased activation of brain regions sensitive to food stimuli. Am. J. Clin. Nutr. 2012;95:818–824. doi: 10.3945/ajcn.111.027383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Benedict C, et al. Acute sleep deprivation enhances the brain’s response to hedonic food stimuli: an fMRI study. J. Clin. Endocrinol. Metab. 2012;97:E443–E447. doi: 10.1210/jc.2011-2759. [DOI] [PubMed] [Google Scholar]
- 116.Greer SM, Goldstein AN, Walker MP. The impact of sleep deprivation on food desire in the human brain. Nat. Commun. 2013;4:2259. doi: 10.1038/ncomms3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.St-Onge M-P, Wolfe S, Sy M, Shechter A, Hirsch J. Sleep restriction increases the neuronal response to unhealthy food in normal-weight individuals. Int. J. Obes. 2014;38:411–416. doi: 10.1038/ijo.2013.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Dashti HS, Scheer FA, Jacques PF, Lamon-Fava S, Ordovás JM. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv. Nutr. 2015;6:648–659. doi: 10.3945/an.115.008623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chaput J-P, McNeil J, Després J-P, Bouchard C, Tremblay A. Short sleep duration is associated with greater alcohol consumption in adults. Appetite. 2012;59:650–655. doi: 10.1016/j.appet.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 120.Sampasa-Kanyinga H, Hamilton HA, Chaput J-P. Sleep duration and consumption of sugar-sweetened beverages and energy drinks among adolescents. Nutrition. 2018;48:77–81. doi: 10.1016/j.nut.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 121.Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36:981–990. doi: 10.5665/sleep.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hanlon EC, et al. Sleep restriction enhances the daily rhythm of circulating levels of endocannabinoid 2-arachidonoylglycerol. Sleep. 2016;39:653–664. doi: 10.5665/sleep.5546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.De Luca MA, Solinas M, Bimpisidis Z, Goldberg SR, Di Chiara G. Cannabinoid facilitation of behavioral and biochemical hedonic taste responses. Neuropharmacology. 2012;63:161–168. doi: 10.1016/j.neuropharm.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kirkham TC, Williams CM, Fezza F, Marzo VD. Endocannabinoid levels in rat limbic forebrain and hypothalamus in relation to fasting, feeding and satiation: stimulation of eating by 2-arachidonoyl glycerol. Br. J. Pharmacol. 2002;136:550–557. doi: 10.1038/sj.bjp.0704767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Melanson EL, et al. Daytime bright light exposure, metabolism, and individual differences in wake and sleep energy expenditure during circadian entrainment and misalignment. Neurobiol. Sleep Circadian Rhythm. 2018;4:49–56. doi: 10.1016/j.nbscr.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Spaeth AM, Dinges DF, Goel N. Phenotypic vulnerability of energy balance responses to sleep loss in healthy adults. Sci. Rep. 2015;5:14920. doi: 10.1038/srep14920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.McNeil J, St-Onge M-P. Increased energy intake following sleep restriction in men and women: a one-size-fits-all conclusion? Obesity. 2017;25:989–992. doi: 10.1002/oby.21831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dennis LE, Spaeth AM, Goel N. Phenotypic stability of energy balance responses to experimental total sleep deprivation and sleep restriction in healthy adults. Nutrients. 2016;8:E823. doi: 10.3390/nu8120823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.St-Onge M-P. The role of sleep duration in the regulation of energy balance: effects on energy intakes and expenditure. J. Clin. Sleep Med. 2013;9:73–80. doi: 10.5664/jcsm.2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.St-Onge M-P, et al. Gender differences in the association between sleep duration and body composition: the Cardia Study. Int. J. Endocrinol. 2010;2010:726071. doi: 10.1155/2010/726071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yeom H-E, Lee J. Sex differences in the influence of sleep on body mass index and risk of metabolic syndrome in middle-aged adults. Healthcare. 2020;8:E561. doi: 10.3390/healthcare8040561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Fan Y, et al. Gender differences in the association between sleep duration and body mass index, percentage of body fat and visceral fat area among chinese adults: a cross-sectional study. BMC Endocr. Disord. 2021;21:247. doi: 10.1186/s12902-021-00913-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mercy UC, et al. Sex differences in the association between short sleep duration and obesity among US adults: findings from NHANES, 2015-2020. Sleep Med. 2022;92:59–63. doi: 10.1016/j.sleep.2022.03.004. [DOI] [PubMed] [Google Scholar]
- 134.Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW. Circadian timing of food intake contributes to weight gain. Obesity. 2009;17:2100. doi: 10.1038/oby.2009.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22:789–798. doi: 10.1016/j.cmet.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Baron KG, Reid KJ, Horn LV, Zee PC. Contribution of evening macronutrient intake to total caloric intake and body mass index. Appetite. 2013;60:246–251. doi: 10.1016/j.appet.2012.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Garaulet M, et al. Timing of food intake predicts weight loss effectiveness. Int. J. Obes. 2013;37:604–611. doi: 10.1038/ijo.2012.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Morris CJ, et al. The human circadian system has a dominating role in causing the morning/evening difference in early diet-induced thermogenesis. Obesity. 2015;23:2053. doi: 10.1002/oby.21189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.McHill AW, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc. Natl Acad. Sci. USA. 2014;111:17302–17307. doi: 10.1073/pnas.1412021111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.McHill AW, et al. Later circadian timing of food intake is associated with increased body fat. Am. J. Clin. Nutr. 2017;106:1213–1219. doi: 10.3945/ajcn.117.161588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Nedeltcheva AV, Kilkus JM, Imperial J, Schoeller DA, Penev PD. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann. Intern. Med. 2010;153:435–441. doi: 10.7326/0003-4819-153-7-201010050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chaput J-P, Bouchard C, Tremblay A. Change in sleep duration and visceral fat accumulation over 6 years in adults. Obesity. 2014;22:E9–E12. doi: 10.1002/oby.20701. [DOI] [PubMed] [Google Scholar]
- 143.Creasy SA, et al. Higher amounts of sedentary time are associated with short sleep duration and poor sleep quality in postmenopausal women. Sleep. 2019;42:zsz093. doi: 10.1093/sleep/zsz093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Thosar SS, et al. Shorter sleep predicts longer subsequent day sedentary duration in healthy midlife adults, but not in those with sleep apnea. Nat. Sci. Sleep. 2021;13:1411–1418. doi: 10.2147/NSS.S322459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Eckel RH, et al. Morning Circadian misalignment during short sleep duration impacts insulin sensitivity. Curr. Biol. 2015;25:3004–3010. doi: 10.1016/j.cub.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 146.Markwald, R. R. & Wright, K. P. Jr in Sleep Loss and Obesity: Intersecting Epidemics (eds Shiromani, P., Horvath, T., Redline, S. & Cauter, E. V.) 101–118 (Springer, 2012).
- 147.Damiola F, et al. Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes Dev. 2000;14:2950–2961. doi: 10.1101/gad.183500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zimberg IZ, et al. Short sleep duration and obesity: mechanisms and future perspectives. Cell Biochem. Funct. 2012;30:524–529. doi: 10.1002/cbf.2832. [DOI] [PubMed] [Google Scholar]
- 149.Bonham MP, Bonnell EK, Huggins CE. Energy intake of shift workers compared to fixed day workers: a systematic review and meta-analysis. Chronobiol. Int. 2016;33:1086–1100. doi: 10.1080/07420528.2016.1192188. [DOI] [PubMed] [Google Scholar]
- 150.Balieiro LCT, et al. Nutritional status and eating habits of bus drivers during the day and night. Chronobiol. Int. 2014;31:1123–1129. doi: 10.3109/07420528.2014.957299. [DOI] [PubMed] [Google Scholar]
- 151.Mota MC, et al. Dietary patterns, metabolic markers and subjective sleep measures in resident physicians. Chronobiol. Int. 2013;30:1032–1041. doi: 10.3109/07420528.2013.796966. [DOI] [PubMed] [Google Scholar]
- 152.Qian J, et al. Sex differences in the circadian misalignment effects on energy regulation. Proc. Natl Acad. Sci. USA. 2019;116:23806–23812. doi: 10.1073/pnas.1914003116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hatori M, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15:848–860. doi: 10.1016/j.cmet.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Qian J, Morris CJ, Caputo R, Garaulet M, Scheer FAJL. Ghrelin is impacted by the endogenous circadian system and by circadian misalignment in humans. Int. J. Obes. 2019;43:1644–1649. doi: 10.1038/s41366-018-0208-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Nguyen J, Wright KP., Jr Influence of weeks of circadian misalignment on leptin levels. Nat. Sci. Sleep. 2010;2:9. doi: 10.2147/NSS.S7624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Scheer FAJL, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc. Natl Acad. Sci. USA. 2009;106:4453–4458. doi: 10.1073/pnas.0808180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Buxton OM, et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci. Transl Med. 2012;4:129ra43. doi: 10.1126/scitranslmed.3003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Crispim CA, et al. Adipokine levels are altered by shiftwork: a preliminary study. Chronobiol. Int. 2012;29:587–594. doi: 10.3109/07420528.2012.675847. [DOI] [PubMed] [Google Scholar]
- 159.Padilha HG, et al. Metabolic responses on the early shift. Chronobiol. Int. 2010;27:1080–1092. doi: 10.3109/07420528.2010.489883. [DOI] [PubMed] [Google Scholar]
- 160.Parsons MJ, et al. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int. J. Obes. 2015;39:842–848. doi: 10.1038/ijo.2014.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr. Biol. 2012;22:939–943. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 162.Mota MC, et al. Association between social jetlag food consumption and meal times in patients with obesity-related chronic diseases. PLoS ONE. 2019;14:e0212126. doi: 10.1371/journal.pone.0212126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Rusu A, et al. Chronic disruption of circadian rhythm with mistimed sleep and appetite — an exploratory research. Chronobiol. Int. 2021;38:807–816. doi: 10.1080/07420528.2021.1895196. [DOI] [PubMed] [Google Scholar]
- 164.Simon SL, et al. Too late and not enough: school year sleep duration, timing, and circadian misalignment are associated with reduced insulin sensitivity in adolescents with overweight/obesity. J. Pediatr. 2019;205:257–264. doi: 10.1016/j.jpeds.2018.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Simon SL, et al. Morning Circadian misalignment is associated with insulin resistance in girls with obesity and polycystic ovarian syndrome. J. Clin. Endocrinol. Metab. 2019;104:3525–3534. doi: 10.1210/jc.2018-02385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Jean-Louis G, et al. Associations between inadequate sleep and obesity in the US adult population. BMC Public Health. 2014;14:290. doi: 10.1186/1471-2458-14-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: analysis of the 2002 National Health Interview Survey Data. Arch. Intern. Med. 2006;166:1775–1782. doi: 10.1001/archinte.166.16.1775. [DOI] [PubMed] [Google Scholar]
- 168.Dixon JB, Dixon ME, Anderson ML, Schachter L, O’Brien PE. Daytime sleepiness in the obese: Not as simple as obstructive sleep apnea. Obesity. 2007;15:2504–2511. doi: 10.1038/oby.2007.297. [DOI] [PubMed] [Google Scholar]
- 169.Meurling IJ, Shea DO, Garvey JF. Obesity and sleep: a growing concern. Curr. Opin. Pulm. Med. 2019;25:602–608. doi: 10.1097/MCP.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 170.Huang Y, Jiang Y, Zhu M. The relationship between global sleep score and inflammatory markers in obese adults from the United States. Nat. Sci. Sleep. 2019;11:317–324. doi: 10.2147/NSS.S220436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Withrow D, et al. Sleep and circadian disruption and the gut microbiome-possible links to dysregulated metabolism. Curr. Opin. Endocr. Metab. Res. 2021;17:26–37. doi: 10.1016/j.coemr.2020.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.He D, et al. Association between leisure time physical activity and metabolic syndrome: a meta-analysis of prospective cohort studies. Endocrine. 2014;46:231–240. doi: 10.1007/s12020-013-0110-0. [DOI] [PubMed] [Google Scholar]
- 173.Petersen CB, Nielsen AJ, Bauman A, Tolstrup JS. Joint association of physical activity in leisure and total sitting time with metabolic syndrome amongst 15,235 Danish adults: a cross-sectional study. Prev. Med. 2014;69:5–7. doi: 10.1016/j.ypmed.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 174.Rennie KL, McCarthy N, Yazdgerdi S, Marmot M, Brunner E. Association of the metabolic syndrome with both vigorous and moderate physical activity. Int. J. Epidemiol. 2003;32:600–606. doi: 10.1093/ije/dyg179. [DOI] [PubMed] [Google Scholar]
- 175.Huang B-H, et al. Sleep and physical activity in relation to all-cause, cardiovascular disease and cancer mortality risk. Br. J. Sports Med. 2022;56:718–724. doi: 10.1136/bjsports-2021-104046. [DOI] [PubMed] [Google Scholar]
- 176.Zuo H, et al. Interaction between physical activity and sleep duration in relation to insulin resistance among non-diabetic Chinese adults. BMC Public Health. 2012;12:247. doi: 10.1186/1471-2458-12-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kahn M, et al. Is it time we stop discouraging evening physical activity? New real-world evidence from 150,000 nights. Front. Public Health. 2021;9:772376. doi: 10.3389/fpubh.2021.772376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Baik I, Lee M, Jun N-R, Lee J-Y, Shin C. A healthy dietary pattern consisting of a variety of food choices is inversely associated with the development of metabolic syndrome. Nutr. Res. Pract. 2013;7:233. doi: 10.4162/nrp.2013.7.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Tortosa A, et al. Mediterranean diet inversely associated with the incidence of metabolic syndrome: the SUN prospective cohort. Diabetes Care. 2007;30:2957–2959. doi: 10.2337/dc07-1231. [DOI] [PubMed] [Google Scholar]
- 180.Zuraikat FM, Wood RA, Barragán R, St-Onge M-P. Sleep and diet: mounting evidence of a cyclical relationship. Annu. Rev. Nutr. 2021;41:309–332. doi: 10.1146/annurev-nutr-120420-021719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Xie Z, et al. Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Nat. Commun. 2022;13:1003. doi: 10.1038/s41467-022-28662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Bilu C, Einat H, Zimmet P, Vishnevskia-Dai V, Kronfeld-Schor N. Beneficial effects of daytime high-intensity light exposure on daily rhythms, metabolic state and affect. Sci. Rep. 2020;10:19782. doi: 10.1038/s41598-020-76636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Brown TM, et al. Recommendations for daytime, evening, and nighttime indoor light exposure to best support physiology, sleep, and wakefulness in healthy adults. PLoS Biol. 2022;20:e3001571. doi: 10.1371/journal.pbio.3001571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Harmsen J-F, et al. The influence of bright and dim light on substrate metabolism, energy expenditure and thermoregulation in insulin-resistant individuals depends on time of day. Diabetologia. 2022;65:721–732. doi: 10.1007/s00125-021-05643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Ayaki M, et al. Protective effect of blue-light shield eyewear for adults against light pollution from self-luminous devices used at night. Chronobiol. Int. 2016;33:134–139. doi: 10.3109/07420528.2015.1119158. [DOI] [PubMed] [Google Scholar]
- 186.Nagai N, et al. Suppression of blue light at night ameliorates metabolic abnormalities by controlling Circadian rhythms. Invest. Ophthalmol. Vis. Sci. 2019;60:3786–3793. doi: 10.1167/iovs.19-27195. [DOI] [PubMed] [Google Scholar]
- 187.Chinoy ED, Duffy JF, Czeisler CA. Unrestricted evening use of light-emitting tablet computers delays self-selected bedtime and disrupts circadian timing and alertness. Physiol. Rep. 2018;6:e13692. doi: 10.14814/phy2.13692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Nordestgaard AT, Thomsen M, Nordestgaard BG. Coffee intake and risk of obesity, metabolic syndrome and type 2 diabetes: a Mendelian randomization study. Int. J. Epidemiol. 2015;44:551–565. doi: 10.1093/ije/dyv083. [DOI] [PubMed] [Google Scholar]
- 189.Ding M, Bhupathiraju SN, Chen M, van Dam RM, Hu FB. Caffeinated and decaffeinated coffee consumption and risk of type 2 diabetes: a systematic review and a dose-response meta-analysis. Diabetes Care. 2014;37:569–586. doi: 10.2337/dc13-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Hino A, et al. Habitual coffee but not green tea consumption is inversely associated with metabolic syndrome: an epidemiological study in a general Japanese population. Diabetes Res. Clin. Pract. 2007;76:383–389. doi: 10.1016/j.diabres.2006.09.033. [DOI] [PubMed] [Google Scholar]
- 191.Drake C, Roehrs T, Shambroom J, Roth T. Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. J. Clin. Sleep Med. 2013;9:1195–1200. doi: 10.5664/jcsm.3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Burke TM, et al. Effects of caffeine on the human circadian clock in vivo and in vitro. Sci. Transl Med. 2015;7:305ra146. doi: 10.1126/scitranslmed.aac5125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Yamada T, Nobuhiro S, Takashi K. Daytime napping, daytime sleepiness and the risk of metabolic diseases: dose-response meta-analysis using restricted cubic spline model. J. Am. Coll. Cardiol. 2016;67:1951. doi: 10.1016/S0735-1097(16)31952-0. [DOI] [Google Scholar]
- 194.Milner CE, Cote KA. Benefits of napping in healthy adults: impact of nap length, time of day, age, and experience with napping. J. Sleep Res. 2009;18:272–281. doi: 10.1111/j.1365-2869.2008.00718.x. [DOI] [PubMed] [Google Scholar]
- 195.Kadono M, et al. Joint effect of alcohol and usual sleep duration on the risk of dysglycemia. Sleep. 2007;30:1341–1347. doi: 10.1093/sleep/30.10.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Sun K, Liu J, Ning G. Active smoking and risk of metabolic syndrome: a meta-analysis of prospective studies. PLoS ONE. 2012;7:e47791. doi: 10.1371/journal.pone.0047791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wetter DW, Young TB. The relation between cigarette smoking and sleep disturbance. Prev. Med. 1994;23:328–334. doi: 10.1006/pmed.1994.1046. [DOI] [PubMed] [Google Scholar]
- 198.Patterson F, et al. Sleep as a target for optimized response to smoking cessation treatment. Nicotine Tob. Res. 2019;21:139. doi: 10.1093/ntr/ntx236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Manber R, et al. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Chirinos JA, et al. CPAP, weight loss, or both for obstructive sleep apnea. N. Engl. J. Med. 2014;370:2265–2275. doi: 10.1056/NEJMoa1306187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Chaput J-P. The integration of pediatric sleep health into public health in Canada. Sleep Med. 2019;56:4–8. doi: 10.1016/j.sleep.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 202.Chaput J-P, Carrier J. First sleep health guidelines for Canadian adults: implications for clinicians. Sleep Med. 2021;79:117–118. doi: 10.1016/j.sleep.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 203.Ferri R, et al. A quantitative statistical analysis of the submentalis muscle EMG amplitude during sleep in normal controls and patients with REM sleep behavior disorder. J. Sleep Res. 2008;17:89–100. doi: 10.1111/j.1365-2869.2008.00631.x. [DOI] [PubMed] [Google Scholar]
- 204.McCarley RW. Neurobiology of REM and NREM sleep. Sleep Med. 2007;8:302–330. doi: 10.1016/j.sleep.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 205.Krueger JM, Frank MG, Wisor JP, Roy S. Sleep function: toward elucidating an enigma. Sleep Med. Rev. 2016;28:46–54. doi: 10.1016/j.smrv.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Joiner WJ. Unraveling the evolutionary determinants of sleep. Curr. Biol. 2016;26:R1073–R1087. doi: 10.1016/j.cub.2016.08.068. [DOI] [PMC free article] [PubMed] [Google Scholar]