Abstract
Human papillomavirus (HPV), the most prevalent sexually transmitted disease worldwide, is the causative agent for several genital and oropharyngeal cancers and a suspected agent for many malignancies. HPV is associated with several adverse health outcomes during pregnancy. Infants are also at risk of HPV infection via different transmission routes: vertically from an infected mother and horizontally through sexual or non-sexual contact with infected individuals. Several HPV manifestations have been identified during childhood, ranging from common skin infections to severe complications such as juvenile recurrent respiratory papillomatosis. This review aims to provide a comprehensive overview of the epidemiology, manifestations, and treatment strategies of HPV infection during pregnancy and childhood. Moreover, we underline the role of vaccination in preventing complications.
Keywords: HPV, gestation, newborn infants, children, pregnancy complications, neoplasms, retinoblastoma
1. Introduction
As the most frequent sexually transmitted disease (STD) worldwide, human papillomavirus (HPV) has posed a substantial burden to healthcare [1]. In addition to the established causation between HPV and some genital and oropharyngeal cancers, HPV is a suspected agent for lung and esophageal cancers [2]. While over 120 types of HPV have been isolated [3], according to their oncogenic activity, HPV types are divided into high- (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, and 82) and low-risk (6, 11, 40, 42, 43, 44, 53, 54, 61, 72, and 81) types [2,3]. The low-risk HPV types usually cause benign lesions such as warts [4].
The prevalence of HPV among pregnant women in different sampling sites, including the cervix, serum, placenta, urine, or amniotic fluid, was determined in a recent meta-analysis [5]. The study indicated that HPV is more prevalent among pregnant women in less developed countries and pregnant women with certain disorders [5]. Unfavorable pregnancy outcomes such as the preterm premature rupture of membranes and preterm births were also significantly associated with HPV infection [6]. Several studies have investigated the transmission rate of HPV based on the delivery mode [7,8,9] and HPV-related disorders during infancy and childhood [10,11]. In the present review study, we aimed to provide a comprehensive review of HPV infection and its consequences in pregnancy, the possible relationship between HPV and adverse pregnancy outcomes, routes of maternal–fetal HPV transmission, and possible and definite manifestations of HPV in childhood.
2. HPV Transmission Routes
While HPV infection is generally considered an STD, the presence of this virus in individuals who never had sexual contact, neonates, or pediatrics implies the presence of other transmission routes [12]. HPV infection is transmitted from mother to infant (i.e., vertical transmission), which could occur either peri-conceptually, prenatally, or perinatally [6,13]. Moreover, HPV infection in infants may be caused via horizontal transmission from peers, parents, and relatives [12]. Therefore, infants are at risk of infection from three main routes [12]: vertical, non-sexual horizontal, and sexual abuse transmissions.
2.1. Vertical Transmission
2.1.1. Peri-Conceptual Transmission
Vertical transmission of HPV could happen from either parent to their descendants [14]. Vertical transmission from the father may occur around fertilization, either pre-implantation or during implantation, typically known as peri-conceptual transmission [15]. Previous studies have detected HPV in semen that could infect spermatozoon [16]. In a systematic review assessing the prevalence of HPV infections among men, HPV DNA was found in 11.4% of semen samples in the general population and in 20.4% of men referred to infertility clinics [16]. Mechanistic studies have implied that HPV DNA is placed in the head of a spermatozoon [17,18]. Moreover, an infected spermatozoon could serve as a vector to transfer the virus and its genes (i.e., E6/E7 genes) into the oocyte, where these genes are further expressed [17,18]. However, this situation is associated with a high risk for a spontaneous abortion [19]. The vas deferens of healthy men who underwent a vasectomy have also contained HPV DNA [20].
Mothers can also be a source of peri-conceptual transmission [21]. To date, no studies have been conducted to detect HPV DNA in the oocytes; however, studies have reported the presence of HPV in the upper genital tracts, including the endometrium, mucosa of the fallopian tubes, ovarian epithelium, and germinal epithelial inclusions in patients with invasive cervical cancers who had undergone a hysterectomy and salpingo-oophorectomy [22,23]. In a systematic review and meta-analysis of a total of 2280 patients with ovarian cancer, the pooled prevalence of HPV detection was estimated at 15.9% (95% confidence interval (CI): 11–22%) [24]. As the significance of the results is debatable, further studies are required, mainly to discover the presence of the HPV genome within oocytes.
2.1.2. Intrauterine Transmission
Intrauterine transmission of HPV, also known as prenatal transmission, is among the proposed HPV transmission routes in a fetus [25]. HPV DNA has been detected in placental samples [5,26,27], amniotic fluid [5,9,28], and fetal membranes [29]. In these cases, the fetus could be infected through micro-abrasions in the membranes or through the placenta, from its tissue or the cord blood. In a cohort study on pregnant women, cervicovaginal samples and maternal and fetal placental tissues were obtained. The results showed that about 14 percent of samples tested positive for HPV, and viral particles were found on both sides of the placenta [27]. Furthermore, in most cases, the genotype was concordant with the isolated genotype from cervicovaginal specimens taken from pregnant mothers [27]. In a study by Rombaldi et al. [26], HPV was detected in 24.5% (12 out of 49) of placental samples of women with positive cervicovaginal HPV tests. Concordance between samples from placental tissues and the genital areas of the mothers was observed in 11 pairs. While HPV tests were positive in seven genital/placental/newborn samples, suggesting an intrauterine transmission of HPV. Inoculation of the placenta with HPV could occur as a complication of an ascending infection from the cervicovaginal areas [30]. Discordance in genotypes of HPV DNA could result from the presence of various genotypes of HPV, inadequate sampling, or improper sampling techniques [27].
Hematogenous spread from the mother to the fetus via cord blood has also been postulated as a possible HPV transmission route; however, the transmission possibility is relatively low [31]. Viremia has been reported to have no effect on the viral replication cycle of HPV [32]. There is limited evidence regarding HPV transmission through blood. The blood from infected animals has been injected intravenously into two naïve animal models: mouse and rabbit [33]. In this experiment, papillomavirus infections were observed in the tissues of these naïve animals [33]. HPV DNA has been identified in the lymphocytes of peripheral blood samples [34]; however, the potential for activation, replication, or infection warrants further investigations.
2.1.3. Perinatal Transmission
During the delivery, direct contact of the fetus with the HPV-infected cells of the genital tract of the mother, mainly the vagina and the cervix, could result in perinatal transmission. The presence of genital warts and positive HPV tests from cervicovaginal samples of the mothers coupled with positive tests from conjunctival, buccal, pharyngeal, and genital swabs of the neonates suggest perinatal HPV transmission [8]. Concordance between the HPV types of maternal and fetal samples lends credence to the vertical transmission theory [35].
In a systematic review and meta-analysis by Chatzistamatiou et al., eight studies containing information on 446 mother–infant pairs were analyzed [8]. This study assessed the type-concordant transmission of HPV, and the pooled perinatal transmission rate was estimated at 25% (95% CI: 20 to 29%). Furthermore, there was a significantly lower relative risk of HPV transmission in participants who had cesarean section than those who delivered vaginally. However, cesarean delivery did not outweigh the risk of neonatal laryngeal papillomatosis [36]. The persistence of infection in an afflicted infant through perinatal transmission has been controversial, as it may be due to contamination or involvement of the top layers of skin, which normally could be shed during the first days of life [37]. In a longitudinal study by Castellsagué et al., neonates with positive HPV DNA tests at birth were followed up with, and the test was repeatedly performed on multiple visits [38]. In more than 80% of neonates, the subsequent HPV tests performed on their 6th week were negative, implying that the cesarean delivery route would not provide complete prevention, negating the routine use of cesarean section in pregnant women with positive HPV tests [39]. A cesarean section may benefit a selected group of mothers with bulky or friable HPV lesions in their genital tract [36]. Table 1 presents the studies that addressed the possibility of vertical transmissions.
Table 1.
Studies regarding maternal–fetal transmission of HPV.
| Author, Year, Country | Features of the Participants of the Studies | Number of Pregnant Women Tested/Number of Positive Pregnant Women | Number of Newborns Tested/Number of Positive Newborns | Time and Sample for HPV Detection in Neonate | Type of HPV Screened (DNA PCR) | Positive Neonates/Positive Mother of Total Vaginal Delivery | Positive Neonates/Positive Mother of Total Cesarean Section |
|---|---|---|---|---|---|---|---|
| Trottier et al., 2016, Canada [27] | Pregnant women in the first trimester | 167/75 | 67/7 | At birth/3-month visits, conjunctival, oral, pharyngeal and genital areas | 6, 11, 16, 18, 26, 31, 33, 34, 35, 39, 40, 42, 44, 45, 51, 52, 53, 54, 56, 58, 59, 61, 62, 66, 67, 68, 69, 70, 71, 72, 73, 81, 82, 83, 84, 89 | -/- of 136 | -/- of 31 |
| Sánchez-Torices et al., 2015, Spain [40] | HPV-positive pregnant women | 91/91 | 92/53 | Immediately after delivery, cord blood and oropharynx | 6, 11, 16, 18, 31, 33, 35, 38, 52 | 53/91 of 92 | None |
| SkoczyNski et al., 2015, Poland [41] | Healthy pregnant women prior to delivery with a singleton pregnancy | 152/29 | 152/16 | Immediately after delivery, oral area | 33 different HPV genotypes including 16 and 18 | NM | NM |
| Hahn et al., 2015, South Korea [42] | Pregnant women over 36 weeks of gestation | 469/72 | 469/15 | Immediately after delivery, oral area and secretions | 6, 11, 16, 18, 30, 31, 32, 33, 35, 39, 40, 42, 43, 44, 45, 51, 52, 53, 54, 55, 56, 58, 59, 62, 66, 67, 68, 68a, 69, 70, 72, 81, 82, 84, 90, 91 | 14/51 of 300 | 1/21 of 169 |
| Lee et al., 2013, South Korea [14] | Healthy women with a singleton pregnancy | 153/37 | 153/8 | Immediately after delivery, cord blood and nasopharyngeal aspirate | 6, 11, 16, 18, 26, 30–35, 39, 40, 42–45, 51–56, 58, 59, 61, 62, 66–70, 72, 73, 81–84, 90, 91 | 3/- of 108 | 5/- of 45 |
| Hong et al., 2013, China [43] | HPV-positive pregnant women at delivery | 3139/422 | 233/35 | <24 h after birth, exfoliated oral and genital cells | 6, 11, 16, 18, 33, 43, 56, 58 | 19/136 of 136 | 16/97 of 97 |
| Park et al., 2012, South Korea [44] | Pregnant women over 36 weeks of gestation | 291/55 | 291/10 | Immediately after delivery, oral area | 24 different HPV genotype including 6, 11, 16, 18, 31, 33, 35, 39, 40, 44, 45, 51, 53, 56, 58, 66, 68, 70 | 10/- of 193 | None/- of 98 |
| Koskimaa et al., 2012, Finland [35] | Pregnant women in third trimester of pregnancy | 329/NM | 331/59 | At birth and till 2 months, oral area | 6, 11, 16, 18, 26, 31, 33, 35, 39, 42, 43, 44, 45, 51, 52, 53, 56, 58, 59, 66, 68, 70, 73, 82 | NM | NM |
| Smith et al., 2010, USA [45] | Healthy women with a singleton pregnancy | 333/99 | 333/5 | At a median of 42 h after birth, oral and genital areas, and cord blood | 6, 11, 16, 18, 31, 33, 39, 51, 53, 54, 56, 58, 59, 61, 69, 66, 70, 83, 84 | 3/86 of 295 | 2/13 of 38 |
| Castellsagué et al., 2009, Spain [38] | Pregnant women with potential risk of HPV exposure | 143/66 | 143/26 | From birth till 24 months of age, oral and genital areas | 6, 11, 16, 18, 31, 33, 39 | 22/- of 124 | 4/- of 19 |
| Rombaldi et al., 2008, Brazil [26] | HPV-positive pregnant women at delivery with prior history of HPV infection, abnormal smear, or genital warts | 49/49 | 49/11 | Immediately after delivery, oral, body, nasopharyngeal aspirates and cord blood | 6, 11, 16, 18, 31, 33, 42, 52, 58 | 5/24 of 24 | 6/25 of 25 |
| Gajewska et al., 2005, Poland [46] | Pregnant women with and without pregestational insulin-dependent diabetes mellitus | 45/12 | 45/9 | 48 h after birth, oral area, cord blood | 6, 11, 16 | NM | NM |
| Rintala et al., 2005, Finland [47] | Pregnant women in the third trimester | 76/57 | 77/56 | At birth till 2 years, oral and genital areas | 16, 18, 31, 33, 35, 39, 45, 51, 52, 54, 56, 58 | -/- of 63 | -/- of 13 |
| Worda et al., 2005, Austria [48] | Pregnant women underwent cesarean section between 37 and 40 weeks of pregnancy | 153/56 | NM | NM | 6, 11, 16, 18, 31, 33, 35, 39, 42, 43, 44, 45, 51, 52, 56, 58, 59, 68 | None | -/56 of 153 |
| Deng et al., 2005, China [49] | Pregnant women without condylomata acuminata in the genital tract | 116/42 | 116/10 | 4 h after birth, cord blood, oropharyngeal secretions, amniotic fluid | 6, 11, 16, 18, 31, 33 | NM | NM |
| Bandyopadhyay et al., 2003, India [50] | Term pregnant women without a history of abnormal smears or genital warts | 135/38 | 135/14 | After birth, oral areas | 6, 11, 16, 18, 31, 33 | 3/11 of 59 | 11/27 of 76 |
| Peng et al., 2000, China [51] | Pregnant women in third trimester of pregnancy | 31/23 | 31/13 | Immediately after delivery, nasopharyngeal aspirates | 6, 11, 16, 18 | NM | NM |
| Tenti et al., 1999, Italy [52] | Pregnant women with negative Papanicolaou smear at first trimester | 711/37 | 711/11 | Immediately after delivery, nasopharyngeal aspirates | 6, 11, 16, 18, 33 | 11/29 of 557 | 0/8 of 154 |
| Wang et al., 1998, China [29] | Pregnant women on third trimester of pregnancy | 73/26 | 73/11 | Immediately after delivery, nasopharyngeal aspirates and amniotic fluid | 16, 18, 35 | 7/14 of 49 | 4/12 of 24 |
| Tseng et al., 1998, Taiwan [53] | Healthy women with a singleton pregnancy | 301/68 | 68/27 | At least 3 days after delivery, oral and genital area | 16, 18 | 18/35 of 160 | 9/33 of 141 |
| Xu et al., 1998, China [54] | Pregnant women on third trimester of pregnancy | 30/16 | 30/14 | 12–48 h after birth, pharyngeal secretions | 6, 11, 16, 18, 31, 33, 35, 38 | - of 17 | - of 13 |
| Watts et al., 1998, USA [55] | Pregnant women before 20 weeks of gestation | 151/112 | 151/8 | At birth and till 3 years, oral, genital and anal areas, nasopharyngeal aspirates | 6, 11, 16, 18, 31, 33, 35, 39, 45 | 6/- of - | 2/- of - |
| Puranen et al., 1997, Finland [56] | Pregnant women | 105/41 | 106/39 | Immediately after delivery, nasopharyngeal aspirates | 2, 6, 7, 11, 16, 18, 30, 31, 33, 53, 66 | 30/30 of 78 | 9/11 of 27 |
| Alberico et al., 1995, Italy [57] | Pregnant women in the first trimester | 170/53 | 170/37 | Immediately after delivery, oropharyngeal secretions | 6, 11, 16, 18, 31, 33, 52 | NM | NM |
| Cason et al., 1995, United Kingdom [58] | Pregnant women, some of them had history of abnormal smears and genital warts | 61/45 | 62/33 | After birth, oral and genital areas, nasopharyngeal aspirates | 16, 18 | NM | NM |
| Parkarin et al., 1994, United Kingdom [59] | Pregnant women, some with a history of abnormal smears or of previous genital warts | 31/20 | 32/12 | 24 h after birth, oral and genital areas | 16, 18, 31, 33 | NM | NM |
Abbreviations: DNA: deoxyribonucleic acid; NM: not mentioned; PCR: polymerase chain reaction.
2.2. Non-Sexual Horizontal Transmission
A body of literature also shows non-sexual skin-to-skin or skin-to-mucosa HPV transmissions [60]. Non-sexual transmission can occur by heteroinoculation, autoinoculation, inanimate objects, or fomites [61].
Heteroinoculation is mainly seen among family members, and transmission can occur by kissing and other non-sexual contacts such as changing diapers, bathing, or fondling [61]. Viral persistence in the oral cavity is quite long [62,63]; therefore, oral and (to a lesser degree) hand warts are hypothesized to impact the transmission. In addition to the cutaneous and low-risk HPV types, high-risk HPV types such as types 16 and 18 can be inoculated in this transmission mode [64]. Condyloma acuminatum can occasionally be found on the nipple and areola [65,66]. This may give rise to horizontal HPV transmission from mothers to infants during breastfeeding and can develop between sexual partners without penetrative sex.
Autoinoculation is the transmission of a virus from one body site to another [13]. For example, scratching the genitalia with an HPV-infected finger or chewing the viral lesion can result in genital and oral HPV, respectively [13,67].
Fomites can also be assumed as a possible way for horizontal HPV transmission [60]. HPV is a stable and heat-resistant virus that remains on the surfaces for a long time and can survive outside living organisms [68]. To date, there has been no definite evidence of HPV infection following the use of an object, but the possibility cannot be ignored. Gynecological equipment has high contamination risks when used to examine a woman with viral shedding [69]. Besides, there is a chance of micro-trauma or micro-abrasions of the genital areas during the examination with the equipment, making the mucosa vulnerable to HPV entry. In a study by Gallay et al., the presence of HPV on non-disposable gynecological equipment such as boxes of gloves, lubricant tubes, colposcope handles, and lamp handles was examined. They found that 18% of the samples were contaminated with HPV [69]. HPV can also be found on surfaces such as common shower rooms, bathroom surfaces, or underwear [67,70,71,72]. De Martino et al. found that foreskins of 6 out of 50 boys without a history of sexual relations tested positive for high-risk types of HPV and suggested shared towels or other objects as possible sources of transmission [73]. However, positive tests for HPV in those objects do not necessarily indicate infection but a detectable level of viral particles.
2.3. Sexual Abuse
Pediatric sexual abuse is a neglected health concern, especially when the child has mental or physical disabilities to express the issue properly [74,75]. The presence of abnormal or changed behavior and inconsistent or illogical statements by parents or caregivers raise suspicions of child abuse for the physician; however, in many cases, there are no physical findings or associated injuries [76,77]. In these cases, HPV might be transmitted by oral-to-genital, oral-to-anal, genital-to-anal, or genital-to-genital contacts [77]. Unger et al. conducted a multicenter study on 537 children without having a history of consensual sexual contact referred for an evaluation of child sexual abuse [76]. The samples were taken from the urine and external genitalia of both genders for HPV tests. Among all individuals with any evidence of sexual abuse (possible, probable, or definite), the rate of positive HPV tests was 13.7%, while the rate was higher among those with a higher certainty of abuse (possible: 8.4%, probable: 15.6%, and definite: 14.5%); however, genital warts were only observed in 14 children [76]. Other studies have reported an almost similar prevalence of anogenital warts among children who were sexually abused: 1.8% and 1.3% in studies by Ingram et al. and Muram et al., respectively [78,79].
A positive test for an STD, such as HPV infection in an infant, should raise suspicion towards sexual abuse, especially if vertical transmission can be ruled out [80]. However, even in children with no evidence of prenatal HPV transmission, interpreting HPV detection in the anogenital areas as sexual abuse is still subject to debate. This might be due to the lack of substantial evidence on the epidemiology of genital warts and positive HPV tests in infants [80]. Infants need high care from their parents or caregivers, particularly in the diaper sites and anogenital areas, resulting in frequent skin-to-skin contact between infants with their caregivers. Besides, moisture and lacerations or fissures can increase the risk of heteroinoculation, especially with cutaneous types of HPV [81,82]. Therefore, detailed history taking, with a particular focus on perinatal history and performing a meticulous physical examination on the infants and the caregivers, could be beneficial for determining the transmission route.
3. Pregnancy-Related Complications
The prevalence of HPV among pregnant women is higher than in non-pregnant counterparts [5]. According to a recent analysis, the global prevalence ratio of HPV infection in pregnant women with human immunodeficiency virus (HIV) and pregnant women with pregnancy-related disorders were respectively 3.31 and 2.35 compared to healthy pregnant women [5]. Given that pregnancy is a state of mild immunosuppression [83], the manifestations of HPV may be more severe in pregnant women [84]. Genital warts may become larger and require treatment after the first trimester [85]. For small warts, treatment is usually not required. In the case of annoying symptoms or large lesions, cryotherapy should be performed as the first-line treatment, and laser remains the second-line therapy [85]. Routine treatment options such as 5-fluorouracil, podophyllin, and interferon should not be used during pregnancy [86]. The Centers for Disease Control and Prevention (CDC) does not recommend HPV vaccination during pregnancy [87]. A prelicensure trial among 172 women vaccinated within 30 days of the estimated conception date found a higher rate of spontaneous abortion after 9-valent HPV vaccine exposures (20%) compared with 4-valent HPV vaccine exposures (9.2%) [88]. However, numerous studies have indicated no association between HPV vaccination and adverse pregnancy outcomes [89,90,91,92,93]. Still, the current guidelines are against HPV vaccination during pregnancy, and further investigations are ongoing [87].
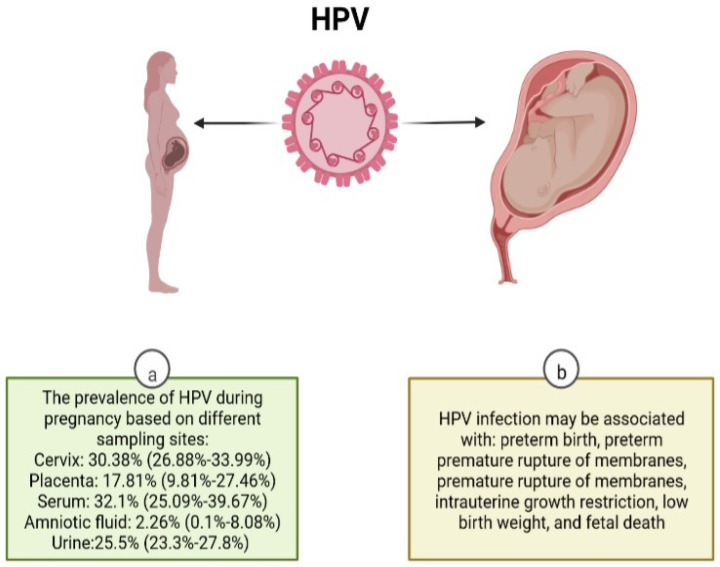
Another conflicting entity about HPV infection during pregnancy is the possible relationship of HPV with adverse pregnancy outcomes [6,94,95]. The global prevalence of HPV in placental samples is estimated to be as high as 32.1% (95% CI: 25.09–39.67%), whereas the prevalence of HPV in amniotic fluid samples is estimated to be as low as 2.26% (95% CI: 0.1–8.08%) [5]. A recent comprehensive meta-analysis [6] based on 36 studies has concluded that HPV infection during pregnancy is associated with preterm birth (adjusted for age odds ratio [aOR]: 1.50; 95% CI: 1.19–1.88), preterm premature rupture of membranes (aOR: 1.96; 95% CI: 1.11–3.45), and premature rupture of membranes (aOR: 1.42; 95% CI: 1.08–1.86). Moreover, fetal death (aOR: 2.23; 95% CI: 1.14–4.37), low birth weight (aOR: 1.91; 95% CI: 1.33–2.76), and intrauterine growth restriction (aOR: 1.17; 95% CI, 1.01–1.37) were significantly associated with HPV infection during pregnancy. However, given the suboptimal bias control, the results should be interpreted cautiously. The mechanisms through which HPV infection influences pregnancy outcomes have been suggested to be through alterations in cervical competence, changing the vaginal microbiota, placental infection, amniotic fluid infection, secondary to cervical manipulations (for the treatment of HPV during the pregnancy) and semen infection [5,6,95,96,97,98]. Figure 1 summarizes the prevalence of HPV in different specimens of pregnant women and related complications with HPV infection in pregnant women.
Figure 1.
Manifestations of HPV in pregnancy. (a) Information adapted from Ardekani et al. [5]. (b) Information adapted from Niyibizy et al. [6]. Created with BioRender.com, accessed on 6 July 2022.
4. HPV in Childhood
As screening for HPV among children is not a routine practice, the HPV data in infancy and childhood are inadequate for epidemiological inferences. A well-designed longitudinal study from Finland indicated that the percentage of offspring born to HPV-seronegative mothers and seroconverted to HPV-positive results was 21%, 38%, and 21% at 12, 24, and 36 months of follow-up. This indicates that they acquired HPV infection during their lifetime [99]. For HPV-seropositive mothers, seropositivity in the offspring ranged from 9–25%, 8–38%, and 0–33% based on different HPV serotypes at 12, 24, and 36 months of follow-up, respectively [99]. The seroprevalence of HPV among children of various ages was 15–44% in a review study [100]. In addition, the presence of HPV in the foreskins of asymptomatic children was 17.3% (95% CI: 0.8 to 46.3%) [101]. To our knowledge, there is no global estimate of HPV prevalence in children; however, the current reports indicate a relatively high prevalence of HPV in infancy and childhood, calling for immediate preventive measures. A wide range of definite and possible manifestations in infancy and childhood have been reported for HPV infection (Figure 2) as following:
Figure 2.
Manifestations of HPV in childhood. Created with BioRender.com, accessed on 6 July 2022.
4.1. Skin Lesions
One of the most common presentations of HPV is verruca vulgaris, also known as the common wart [102]. Wart is usually a solitary rough-surfaced papule that commonly occurs on the back of hands, fingers, or knees but can occur on any part of the body, including the oral cavity and genitalia [103,104]. The common wart is predominant in school-age children [105].
Condyloma acuminata are the warts of the anogenital region [61] that usually present as hyper-pigmented plaques or papules, occasionally with a cauliflower-shaped appearance. They are usually in the anogenital region but may less commonly occur in the oral cavity [106]. Due to the long incubation period of HPV (three weeks to eight months) [107], determining the transmission route is difficult. However, the older the child becomes, the less likely vertical transmission is. Thus, screening for sexual abuse should be considered in all cases of anogenital and oral warts, first presenting in children older than three to four years [106]. In addition, differential diagnoses should be considered in case of similar presentations, such as molluscum contagiosum, benign nevi, infantile perianal pyramidal protrusion, and syphilis condylomata [108,109,110,111]. A study reported that six out of eight children who did not receive treatments experienced spontaneous resolution of condylomas [112]. Given the self-resolution of the lesion in most cases, a “Watch-and-Wait” treatment strategy has been suggested, especially for lesions that appeared for less than two years. Several interventional (e.g., laser, cryotherapy, cauterization, and surgical removal) and non-interventional (e.g., Podophyllotoxin, Imiquimod) options are available. However, children are normally less cooperative with interventional therapies, so the non-interventional choices are the first-line treatment [113].
Skin cancers are rare in children, and even rarer are HPV-related carcinomas of the skin in children [114]. Bowen’s disease, a type of squamous cell carcinoma (SCC) in situ, has been associated with HPV in immunodeficient children [114].
4.2. Mucosal Lesions
Oral squamous papilloma is the most common benign oral lesion associated with HPV in children and adults [115]. They are exophytic projections which may appear red, pink, or white depending on the degree of keratinization [116]. HPV DNA was detected in up to 68% of oral squamous papillomas [117]. Heck’s disease, also known as Focal Epithelial Hyperplasia (FEH), is an uncommon, benign oral disorder associated with infection with HPV types 13, 32, or both [103,118]. It is clinically manifested by multiple small papules and white-to-pinkish (mucosa-colored) plaques in the oral cavity, with a preference for the lower lip. It is most common in children and young adults and has a racial predominance in Eskimo and Native American populations [103,118].
Malignant mucosal lesions are uncommon in children, as the occurrence may take about 5 years (in immunodeficient individuals) up to 30 years following HPV infection [119]. While there is no report of HPV-related neoplasms of the cervix of children, cervical dysplasia, preneoplastic, and perhaps even neoplastic lesions can occur more commonly in immunodeficient children or adolescents [120]. In general, oropharyngeal cancers in children are sporadic; however, several cases of HPV-associated SCC in the oral cavity and oropharynx of children have been reported [121,122,123].
4.3. Juvenile Recurrent Respiratory Papillomatosis
Juvenile onset recurrent respiratory papillomatosis (JRRP) is a rare disease mainly caused by HPV 6 and 11 [124]. The disease presents as the recurrent growth of papillomas in the upper respiratory tract, usually in children 2 to 6 years old [125]. Patients with JRRP may exhibit hoarseness (most common presentation), a weak cry, choking episodes, and a failure to thrive [126]. Visible external genital warts in the mother have been strongly associated with JRRP [127,128]. A majority of children with JRRP were those who delivered to young mothers through the vaginal canal, firstborn children, and those who delivered to unvaccinated mothers [129]. Not all infected with HPV 6 and 11 develop JRRP, and the prevalence of JRRP is much lower than the reported prevalence for HPV 6 and 11 [5,130]. This raises the hypothesis of immunosuppression or genetic susceptibility in patients with respiratory papillomatosis. Certain human leukocyte antigens (HLA), namely, HLA- DQB1*0201, DQB1*0202, and DRB1*0301, are associated with severe recurrent respiratory papillomatosis, proposing a regulatory role for these alleles [131]. In addition, killer cell immunoglobulin-like receptors (KIR) regulate the natural killer (NK) cell response against viral infection. Individuals with more severe recurrent respiratory papillomatosis typically lack activating KIR genes 3DS1 and 2DS1 [132].
Owing to the changing nature of the disease, its management depends on a case-by-case basis. Some children exhibit modest symptoms with spontaneous remission, while others need several interventions due to rapid disease development [125]. A possibility of lung involvement exists in 3.3% of recurrent respiratory papillomatosis cases [133], which can adversely affect the patients’ quality of life [134]. The repeated surgical removal of papillomas is a widely accepted approach for treatment in symptomatic cases [135] to debulk the papilloma while preserving intact laryngeal tissue. In addition, a number of adjuvant therapies have been proposed to increase the symptom-free intervals [136], such as indole-3 carbinol [137], HPV vaccination [138], bevacizumab [139,140], interferon-α [141], cidofovir [142], programmed cell death protein 1 (PD-1) inhibitors [143], celecoxib along with erlotinib [144,145], and antivirals [146,147].
4.4. Retinoblastoma
Retinoblastoma (RB) is the most prevalent intraocular malignancy in children [148]. Previous efforts have identified possible etiologies for sporadic RB [149]. It is hypothesized that due to the higher prevalence of sporadic RB in less developed areas with poorer socioeconomic status, infections may be a possible culprit for the sporadic form of the malignancy [150]. HPV has been notorious for its oncogenic properties and is linked to several malignancies [151]. The E7 protein produced by the high-risk HPV types 16 and 18 bind more avidly to the RB protein than those encoded by low-risk types [152]. The binding, interaction, and subsequent inhibition of the RB protein by E7 is the suggested theory for the carcinogenesis of high-risk HPV types [153]. As RB tumor suppressor gene inactivation has been linked to a range of malignancies, including RB, the hypothesis of the possible role of HPV in RB development has strengthened. Therefore, several studies have evaluated the prevalence of HPV in the intraocular samples of patients with RB [150,153,154,155]. HPV has been detected in RB samples from 0% to 82% of the study participants in different investigations [150,153]. This wide range of positivity for HPV has raised suspicions about its effect on RB development. While some studies support the relationship between HPV and RB progression [155,156,157,158], other studies, especially those in which the HPV prevalence in cases was less than the normal population or controls, refute the hypothesis of possible association [153,154,159]. One possible explanation for the significant variations among the studies is the method used for virus detection. Polymerase chain reaction (PCR) is the most widely used technique among the studies, with the highest sensitivity for HPV DNA detection; however, in-situ hybridization (ISH) and immunohistochemistry (IHC) have also been used. Another reason for the high heterogeneity across studies is the ophthalmic tissues used to detect HPV DNA, as the prevalence of HPV DNA detection is higher in fresh tissues than in formalin-fixed paraffin-embedded (FFPE) tissues [160]. The higher rate of DNA degradation in FFPE tissues might be the reason for the variations. The prevention of sporadic RB due to HPV is similar to the prevention of HPV and other STDs. Barrier contraception and vaccination can avoid HPV and HPV-related malignancies, including RB [157].
4.5. Conjunctival Papilloma
Conjunctival papilloma is a slowly progressive benign tumor of the conjunctiva and is known to be responsible for 1–10% of the conjunctival lesions in children and adolescents [161]. However, its prevalence is higher in sexually active adults aged 20–40 [161]. The transmission route in infants is mainly through vaginal delivery; however, direct autoinoculation and sexually transmission are the predominant transmission routes in older children and adolescents [161,162]. Furthermore, low-risk HPV 6 and 11 were mostly detected in positive samples from conjunctival papilloma, while high-risk HPV 16 and 18 were the most common reported types in RB samples. The number of conjunctival papillomas in each eye is more likely higher in children and adolescents than adults [163]. Contrary to the controversial association between HPV and RB, HPV is a known risk factor for conjunctival papilloma development [161]. The oncogenic properties of HPV might be responsible for the changes that occur during conjunctival papilloma development [161]. Similar to the interaction of E7 and RB, E6 is the other encoded HPV protein and is associated with impairing the function of another tumor suppressor gene, p53 [162]. According to the “Two-hit” theory, both copies of the p53 gene should be impaired to allow for the progression of the tumor [162]. It is thought that the UV radiation is responsible for the first hit, and the HPV-associated oncogenesis is accountable for the second hit [162]. Histopathologic evaluation of the tumor revealed a fibrovascular core covered by papillary projections [161,163]. Sessile and pedunculated papilloma are more likely to be observed in adults and pediatrics, respectively [161]. The clinical implication of this observation is the lower probability of pedunculated papilloma to develop epithelial dysplasia [163]. It should be noted that patients with conjunctival papilloma are more likely to develop laryngeal papilloma [164,165]. Different treatments have been suggested for conjunctival papilloma, which are categorized into sole and combination therapies. Sole therapies are oral cimetidine (300–400 mg 3 times a day), photodynamic therapy, cryotherapy, and topical interferon alfa-2b (1 MU 3 times a day). The combination therapies are excisional biopsy and cryotherapy, excisional biopsy and cryotherapy and oral cimetidine, and excisional biopsy and cryotherapy and interferon alfa-2b [161].
5. Conclusions
HPV infection could lead to severe complications in mothers and their children. The worldwide prevalence of HPV among pregnant women is high, affecting mothers and their children in the short- and long-term. HPV positivity and certain adverse pregnancy outcomes are significantly associated with each other. A wide range of manifestations for children, from infancy to childhood, have been reported to be related to maternal HPV infections. However, as a curative treatment is not yet discovered for this infection, vaccination is the most feasible way of prevention.
Acknowledgments
The authors would like to thank Seyed AmirAli Tavangar for his help in preparing the figures.
Author Contributions
Conceptualization, A.A. and A.R. (Amirhossein Roshanshad); methodology, A.A., E.T. and A.R. (Amirhossein Roshanshad); software, A.A. and E.H.; validation, A.A., A.M., S.R., M.R. (Mahroo Rezaeinejad), M.F.-M., M.R. (Maryam Razavi) and A.R. (Ali Rostami); investigation, E.H. and R.F.; resources, E.H. and R.F.; data curation, A.A., E.T., E.H., A.R. (Amirhossein Roshanshad) and R.F.; writing—original draft preparation, A.A., E.T., E.H., A.R. (Amirhossein Roshanshad) and R.F.; writing—review and editing, A.M., S.R., M.R. (Mahroo Rezaeinejad), M.F.-M., M.R. (Maryam Razavi) and A.R. (Ali Rostami); visualization, A.M., S.R., M.R. (Mahroo Rezaeinejad), M.F.-M., M.R. (Mahroo Rezaeinejad) and A.R. (Ali Rostami); supervision, A.A. and A.R. (Ali Rostami); project administration, A.A. and A.R. (Ali Rostami). All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Forman D., de Martel C., Lacey C.J., Soerjomataram I., Lortet-Tieulent J., Bruni L., Vignat J., Ferlay J., Bray F., Plummer M., et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012;30((Suppl. S5)):F12–F23. doi: 10.1016/j.vaccine.2012.07.055. [DOI] [PubMed] [Google Scholar]
- 2.Zandberg D.P., Bhargava R., Badin S., Cullen K.J. The role of human papillomavirus in nongenital cancers. CA A Cancer J. Clin. 2013;63:57–81. doi: 10.3322/caac.21167. [DOI] [PubMed] [Google Scholar]
- 3.Steben M., Duarte-Franco E. Human papillomavirus infection: Epidemiology and pathophysiology. Gynecol. Oncol. 2007;107:S2–S5. doi: 10.1016/j.ygyno.2007.07.067. [DOI] [PubMed] [Google Scholar]
- 4.Dunne E.F., Park I.U. HPV and HPV-Associated Diseases. Infect. Dis. Clin. 2013;27:765–778. doi: 10.1016/j.idc.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Ardekani A., Sepidarkish M., Mollalo A., Afradiasbagharani P., Rouholamin S., Rezaeinejad M., Farid-Mojtahedi M., Mahjour S., Almukhtar M., Nourollahpour Shiadeh M., et al. Worldwide prevalence of human papillomavirus among pregnant women: A systematic review and meta-analysis. Rev. Med. Virol. 2022:e2374. doi: 10.1002/rmv.2374. [DOI] [PubMed] [Google Scholar]
- 6.Niyibizi J., Zanré N., Mayrand M.-H., Trottier H. Association between Maternal Human Papillomavirus Infection and Adverse Pregnancy Outcomes: Systematic Review and Meta-Analysis. J. Infect. Dis. 2020;221:1925–1937. doi: 10.1093/infdis/jiaa054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medeiros L.R., Ethur A.B., Hilgert J.B., Zanini R.R., Berwanger O., Bozzetti M.C., Mylius L.C. Vertical transmission of the human papillomavirus: A systematic quantitative review. Cad. Saude Publica. 2005;21:1006–1015. doi: 10.1590/S0102-311X2005000400003. [DOI] [PubMed] [Google Scholar]
- 8.Chatzistamatiou K., Sotiriadis A., Agorastos T. Effect of mode of delivery on vertical human papillomavirus transmission—A meta-analysis. J. Obstet. Gynaecol. 2016;36:10–14. doi: 10.3109/01443615.2015.1030606. [DOI] [PubMed] [Google Scholar]
- 9.Zouridis A., Kalampokas T., Panoulis K., Salakos N., Deligeoroglou E. Intrauterine HPV transmission: A systematic review of the literature. Arch. Gynecol. Obstet. 2018;298:35–44. doi: 10.1007/s00404-018-4787-4. [DOI] [PubMed] [Google Scholar]
- 10.LaCour D.E., Trimble C. Human papillomavirus in infants: Transmission, prevalence, and persistence. J. Pediatr. Adolesc. Gynecol. 2012;25:93–97. doi: 10.1016/j.jpag.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mammas I.N., Sourvinos G., Spandidos D.A. Human papilloma virus (HPV) infection in children and adolescents. Eur. J. Pediatr. 2009;168:267–273. doi: 10.1007/s00431-008-0882-z. [DOI] [PubMed] [Google Scholar]
- 12.Sabeena S., Bhat P., Kamath V., Arunkumar G. Possible non-sexual modes of transmission of human papilloma virus. J. Obstet. Gynaecol. Res. 2017;43:429–435. doi: 10.1111/jog.13248. [DOI] [PubMed] [Google Scholar]
- 13.Syrjanen S., Puranen M. Human Papillomavirus Infections in Children: The Potential Role of Maternal Transmission. Crit. Rev. Oral Biol. Med. 2000;11:259–274. doi: 10.1177/10454411000110020801. [DOI] [PubMed] [Google Scholar]
- 14.Lee S.M., Park J.S., Norwitz E.R., Koo J.N., Oh I.H., Park J.W., Kim S.M., Kim Y.H., Park C.-W., Song Y.S. Risk of Vertical Transmission of Human Papillomavirus throughout Pregnancy: A Prospective Study. PLoS ONE. 2013;8:e66368. doi: 10.1371/journal.pone.0066368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zgura A.F., Bratila E., Vladareanu S. Transplacental Transmission of Human Papillomavirus. Maedica. 2015;10:159–162. [PMC free article] [PubMed] [Google Scholar]
- 16.Lyu Z., Feng X., Li N., Zhao W., Wei L., Chen Y., Yang W., Ma H., Yao B., Zhang K., et al. Human papillomavirus in semen and the risk for male infertility: A systematic review and meta-analysis. BMC Infect. Dis. 2017;17:714. doi: 10.1186/s12879-017-2812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foresta C., Garolla A., Zuccarello D., Pizzol D., Moretti A., Barzon L., Palù G. Human papillomavirus found in sperm head of young adult males affects the progressive motility. Fertil. Steril. 2010;93:802–806. doi: 10.1016/j.fertnstert.2008.10.050. [DOI] [PubMed] [Google Scholar]
- 18.Foresta C., Patassini C., Bertoldo A., Menegazzo M., Francavilla F., Barzon L., Ferlin A. Mechanism of human papillomavirus binding to human spermatozoa and fertilizing ability of infected spermatozoa. PLoS ONE. 2011;6:e15036. doi: 10.1371/journal.pone.0015036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pereira N., Kucharczyk K.M., Estes J.L., Gerber R.S., Lekovich J.P., Elias R.T., Spandorfer S.D. Human Papillomavirus Infection, Infertility, and Assisted Reproductive Outcomes. J. Pathog. 2015;2015:578423. doi: 10.1155/2015/578423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rintala M.A.M., Pöllänen P.P., Nikkanen V.P., Grénman S.E., Syrjänen S.M. Human Papillomavirus DNA Is Found in the Vas Deferens. J. Infect. Dis. 2002;185:1664–1667. doi: 10.1086/340421. [DOI] [PubMed] [Google Scholar]
- 21.SyrjÄNen S. Current concepts on human papillomavirus infections in children. APMIS. 2010;118:494–509. doi: 10.1111/j.1600-0463.2010.02620.x. [DOI] [PubMed] [Google Scholar]
- 22.Giordano G., D’Adda T., Gnetti L., Froio E., Merisio C., Melpignano M. Detection of human papillomavirus in organs of upper genital tract in women with cervical cancer. Int. J. Gynecol. Cancer. 2006;16:1601–1607. doi: 10.1111/j.1525-1438.2006.00633.x. [DOI] [PubMed] [Google Scholar]
- 23.Ip S., Wong L., Xu C., Cheung A., Tsang P., Ngan H. Detection of human papillomavirus DNA in malignant lesions from Chinese women with carcinomas of the upper genital tract. Gynecol. Oncol. 2002;87:104–111. doi: 10.1006/gyno.2002.6784. [DOI] [PubMed] [Google Scholar]
- 24.Cherif S., Amine A., Thies S., Taube E.T., Braicu E.I., Sehouli J., Kaufmann A.M. Prevalence of human papillomavirus detection in ovarian cancer: A meta-analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2021;40:1791–1802. doi: 10.1007/s10096-021-04282-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freitas A.C., Mariz F.C., Silva M.A.R., Jesus A.L.S. Human Papillomavirus Vertical Transmission: Review of Current Data. Clin. Infect. Dis. 2013;56:1451–1456. doi: 10.1093/cid/cit066. [DOI] [PubMed] [Google Scholar]
- 26.Rombaldi R.L., Serafini E.P., Mandelli J., Zimmermann E., Losquiavo K.P. Transplacental transmission of Human Papillomavirus. Virol. J. 2008;5:106. doi: 10.1186/1743-422X-5-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trottier H., Mayrand M.H., Coutlée F., Monnier P., Laporte L., Niyibizi J., Carceller A.M., Fraser W.D., Brassard P., Lacroix J., et al. Human papillomavirus (HPV) perinatal transmission and risk of HPV persistence among children: Design, methods and preliminary results of the HERITAGE study. Papillomavirus Res. 2016;2:145–152. doi: 10.1016/j.pvr.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Armbruster-Moraes E., Ioshimoto L.M., Leão E., Zugaib M. Presence of human papillomavirus DNA in amniotic fluids of pregnant women with cervical lesions. Gynecol. Oncol. 1994;54:152–158. doi: 10.1006/gyno.1994.1185. [DOI] [PubMed] [Google Scholar]
- 29.Wang X., Zhu Q., Rao H. Maternal-fetal transmission of human papillomavirus. Chin. Med. J. 1998;111:726–727. [PubMed] [Google Scholar]
- 30.Weyn C., Thomas D., Jani J., Guizani M., Donner C., Van Rysselberge M., Hans C., Bossens M., Englert Y., Fontaine V. Evidence of human papillomavirus in the placenta. J. Infect. Dis. 2011;203:341–343. doi: 10.1093/infdis/jiq056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sarkola M.E., Grénman S.E., Rintala M.A., Syrjänen K.J., Syrjänen S.M. Human papillomavirus in the placenta and umbilical cord blood. Acta Obstet. Gynecol. Scand. 2008;87:1181–1188. doi: 10.1080/00016340802468308. [DOI] [PubMed] [Google Scholar]
- 32.Brown D.R., Ermel A. Human Papillomavirus Infections. In: Jameson J.L., Fauci A.S., Kasper D.L., Hauser S.L., Longo D.L., Loscalzo J., editors. Harrison’s Principles of Internal Medicine. 20th ed. McGraw-Hill Education; New York, NY, USA: 2018. [Google Scholar]
- 33.Cladel N.M., Jiang P., Li J.J., Peng X., Cooper T.K., Majerciak V., Balogh K.K., Meyer T.J., Brendle S.A., Budgeon L.R., et al. Papillomavirus can be transmitted through the blood and produce infections in blood recipients: Evidence from two animal models. Emerg. Microbes Infect. 2019;8:1108–1121. doi: 10.1080/22221751.2019.1637072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pao C.C., Lin S.S., Lin C.Y., Maa J.S., Lai C.H., Hsieh T.T. Identification of human papillomavirus DNA sequences in peripheral blood mononuclear cells. Am. J. Clin. Pathol. 1991;95:540–546. doi: 10.1093/ajcp/95.4.540. [DOI] [PubMed] [Google Scholar]
- 35.Koskimaa H.M., Waterboer T., Pawlita M., Grénman S., Syrjänen K., Syrjänen S. Human papillomavirus genotypes present in the oral mucosa of newborns and their concordance with maternal cervical human papillomavirus genotypes. J. Pediatr. 2012;160:837–843. doi: 10.1016/j.jpeds.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 36.Cunningham F.G., Leveno K.J., Bloom S.L., Dashe J.S., Hoffman B.L., Casey B.M., Spong C.Y. Williams Obstetrics. 25th ed. McGraw-Hill Education; New York, NY, USA: 2018. Neoplastic Disorders. [Google Scholar]
- 37.Society C.P. Skin care for your baby. Paediatr. Child. Health. 2007;12:245–251. doi: 10.1093/pch/12.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Castellsagué X., Drudis T., Cañadas M.P., Goncé A., Ros R., Pérez J.M., Quintana M.J., Muñoz J., Albero G., de Sanjosé S., et al. Human Papillomavirus (HPV) infection in pregnant women and mother-to-child transmission of genital HPV genotypes: A prospective study in Spain. BMC Infect. Dis. 2009;9:74. doi: 10.1186/1471-2334-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Workowski K.A., Bolan G.A. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm. Rep. 2015;64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 40.Sánchez-Torices M.S., Corrales-Millan R., Hijona-Elosegui J.J. Colonización orofaríngea perinatal por el virus del papiloma humano. Acta Otorrinolaringológica Española. 2016;67:135–141. doi: 10.1016/j.otorri.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 41.Skoczyński M., Goździcka-Józefiak A., Kwaśniewska A. The Prevalence of Human Papillomavirus between the Neonates and Their Mothers. Biomed. Res. Int. 2015;2015:126417. doi: 10.1155/2015/126417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hahn H.S., Kee M.K., Kim H.J., Kim M.Y., Kang Y.S., Park J.S., Kim T.J. Distribution of maternal and infant human papillomavirus: Risk factors associated with vertical transmission. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013;169:202–206. doi: 10.1016/j.ejogrb.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 43.Hong Y., Li S.Q., Hu Y.L., Wang Z.Q. Survey of human papillomavirus types and their vertical transmission in pregnant women. BMC Infect. Dis. 2013;13:109. doi: 10.1186/1471-2334-13-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park H., Lee S.W., Lee I.H., Ryu H.M., Cho A.R., Kang Y.S., Hong S.R., Kim S.S., Seong S.J., Shin S.M., et al. Rate of vertical transmission of human papillomavirus from mothers to infants: Relationship between infection rate and mode of delivery. Virol. J. 2012;9:80. doi: 10.1186/1743-422X-9-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith E.M., Parker M.A., Rubenstein L.M., Haugen T.H., Hamsikova E., Turek L.P. Evidence for vertical transmission of HPV from mothers to infants. Infect. Dis. Obstet. Gynecol. 2010;2010:326369. doi: 10.1155/2010/326369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gajewska M., Marianowski L., Wielgos M., Malejczyk M., Majewski S. The occurrence of genital types of human papillomavirus in normal pregnancy and in pregnant women with pregestational insulin dependent diabetes mellitus. Neuro Endocrinol. Lett. 2005;26:766–770. [PubMed] [Google Scholar]
- 47.Rintala M.A., Grénman S.E., Puranen M.H., Isolauri E., Ekblad U., Kero P.O., Syrjänen S.M. Transmission of high-risk human papillomavirus (HPV) between parents and infant: A prospective study of HPV in families in Finland. J. Clin. Microbiol. 2005;43:376–381. doi: 10.1128/JCM.43.1.376-381.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Worda C., Huber A., Hudelist G., Schatten C., Leipold H., Czerwenka K., Eppel W. Prevalence of cervical and intrauterine human papillomavirus infection in the third trimester in asymptomatic women. J. Soc. Gynecol. Investig. 2005;12:440–444. doi: 10.1016/j.jsgi.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 49.Deng D., Wen L., Chen W., Ling X. Asymptomatic genital infection of human papillomavirus in pregnant women and the vertical transmission route. J. Huazhong Univ. Sci. Technolog. Med. Sci. 2005;25:343–345. doi: 10.1007/bf02828162. [DOI] [PubMed] [Google Scholar]
- 50.Bandyopadhyay S., Sen S., Majumdar L., Chatterjee R. Human papillomavirus infection among Indian mothers and their infants. Asian Pac. J. Cancer Prev. 2003;4:179–184. [PubMed] [Google Scholar]
- 51.Peng P., Weng X., Gu Z. Detection of the asymptomatic infection by human papillomavirus in pregnant women and neonates. Zhonghua Fu Chan Ke Za Zhi. 2000;35:523–526. [PubMed] [Google Scholar]
- 52.Tenti P., Zappatore R., Migliora P., Spinillo A., Belloni C., Carnevali L. Perinatal transmission of human papillomavirus from gravidas with latent infections. Obstet. Gynecol. 1999;93:475–479. doi: 10.1016/s0029-7844(98)00459-1. [DOI] [PubMed] [Google Scholar]
- 53.Tseng C.J., Liang C.C., Soong Y.K., Pao C.C. Perinatal transmission of human papillomavirus in infants: Relationship between infection rate and mode of delivery. Obstet. Gynecol. 1998;91:92–96. doi: 10.1016/S0029-7844(97)00593-0. [DOI] [PubMed] [Google Scholar]
- 54.Xu S., Liu L., Lu S., Ren S. Clinical observation on vertical transmission of human papillomavirus. Chin. Med. Sci. J. Chung-Kuo I Hsueh K’o Hsueh Tsa Chih. 1998;13:29–31. [PubMed] [Google Scholar]
- 55.Watts D.H., Koutsky L.A., Holmes K.K., Goldman D., Kuypers J., Kiviat N.B., Galloway D.A. Low risk of perinatal transmission of human papillomavirus: Results from a prospective cohort study. Am. J. Obstet. Gynecol. 1998;178:365–373. doi: 10.1016/S0002-9378(98)80027-6. [DOI] [PubMed] [Google Scholar]
- 56.Puranen M.H., Yliskoski M.H., Saarikoski S.V., Syrjänen K.J., Syrjänen S.M. Exposure of an infant to cervical human papillomavirus infection of the mother is common. Am. J. Obstet. Gynecol. 1997;176:1039–1045. doi: 10.1016/S0002-9378(97)70399-5. [DOI] [PubMed] [Google Scholar]
- 57.Alberico S., Pinzano R., Comar M., Toffoletti F., Maso G., Ricci G., Guaschino S. Maternal-fetal transmission of human papillomavirus. Minerva Ginecol. 1996;48:199–204. [PubMed] [Google Scholar]
- 58.Cason J., Kaye J.N., Jewers R.J., Kambo P.K., Bible J.M., Kell B., Shergill B., Pakarian F., Raju K.S., Best J.M. Perinatal infection and persistence of human papillomavirus types 16 and 18 in infants. J. Med. Virol. 1995;47:209–218. doi: 10.1002/jmv.1890470305. [DOI] [PubMed] [Google Scholar]
- 59.Pakarian F., Kaye J., Cason J., Kell B., Jewers R., Derias N.W., Raju K.S., Best J.M. Cancer associated human papillomaviruses: Perinatal transmission and persistence. Br. J. Obstet. Gynaecol. 1994;101:514–517. doi: 10.1111/j.1471-0528.1994.tb13153.x. [DOI] [PubMed] [Google Scholar]
- 60.Petca A., Borislavschi A., Zvanca M.E., Petca R.C., Sandru F., Dumitrascu M.C. Non-sexual HPV transmission and role of vaccination for a better future (Review) Exp. Ther. Med. 2020;20:186. doi: 10.3892/etm.2020.9316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Benjamin L.T., Levy M., Ofori A. Condylomata Acuminata (Anogenital Warts) in Children. UpToDate; Waltham, MA, USA: 2014. [Google Scholar]
- 62.Campbell C.M.P., Kreimer A.R., Lin H.Y., Fulp W., O’Keefe M.T., Ingles D.J., Abrahamsen M., Villa L.L., Lazcano-Ponce E., Giuliano A.R. Long-term persistence of oral human papillomavirus type 16: The HPV Infection in Men (HIM) study. Cancer Prev. Res. 2015;8:190–196. doi: 10.1158/1940-6207.CAPR-14-0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rautava J., Willberg J., Louvanto K., Wideman L., Syrjänen K., Grénman S., Syrjänen S. Prevalence, Genotype Distribution and Persistence of Human Papillomavirus in Oral Mucosa of Women: A Six-Year Follow-Up Study. PLoS ONE. 2012;7:e42171. doi: 10.1371/journal.pone.0042171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cason J., Rice P., Best J.M. Transmission of cervical cancer-associated human papilloma viruses from mother to child. Intervirology. 1998;41:213–218. doi: 10.1159/000024939. [DOI] [PubMed] [Google Scholar]
- 65.Zhang L.-W., Wang W.-J., Li C.-H., Xu L., Liu X.-Y., Zheng L., Liu D.-X. A Case of Condyloma Acuminatum on the Nipple Detected via Dermoscopy. Int. J. Dermatol. Venereol. 2020;3:125–126. doi: 10.1097/01.JD9.0000563564.57133.50. [DOI] [Google Scholar]
- 66.Saeki Y., Sato S., Okajima K., Ando N., Saeki H., Kawase M., Ito K., Nakagawa H., Ohtsuki M. Condyloma acuminatum of the nipple and areola. Int. J. Dermatol. 2014;53:e171–e172. doi: 10.1111/j.1365-4632.2012.05727.x. [DOI] [PubMed] [Google Scholar]
- 67.Sonnex C., Strauss S., Gray J.J. Detection of human papillomavirus DNA on the fingers of patients with genital warts. Sex. Transm. Infect. 1999;75:317–319. doi: 10.1136/sti.75.5.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ryndock E.J., Meyers C. A risk for non-sexual transmission of human papillomavirus? Expert Rev. Anti-Infect. Ther. 2014;12:1165–1170. doi: 10.1586/14787210.2014.959497. [DOI] [PubMed] [Google Scholar]
- 69.Gallay C., Miranda E., Schaefer S., Catarino R., Jacot-Guillarmod M., Menoud P.A., Guerry F., Achtari C., Sahli R., Vassilakos P., et al. Human papillomavirus (HPV) contamination of gynaecological equipment. Sex. Transm. Infect. 2016;92:19–23. doi: 10.1136/sextrans-2014-051977. [DOI] [PubMed] [Google Scholar]
- 70.Strauss S., Sastry P., Sonnex C., Edwards S., Gray J. Contamination of environmental surfaces by genital human papillomaviruses. Sex. Transm. Infect. 2002;78:135–138. doi: 10.1136/sti.78.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Johnson L.W. Communal showers and the risk of plantar warts. J Fam Pract. 1995;40:136–138. [PubMed] [Google Scholar]
- 72.Houlihan C.F., Baisley K., Bravo I.G., Pavón M.A., Changalucha J., Kapiga S., De Sanjosé S., Ross D.A., Hayes R.J., Watson-Jones D. Human papillomavirus DNA detected in fingertip, oral and bathroom samples from unvaccinated adolescent girls in Tanzania. Sex. Transm. Infect. 2019;95:374–379. doi: 10.1136/sextrans-2018-053756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.de Martino M., Haitel A., Wrba F., Schatzl G., Klatte T., Waldert M. High-risk human papilloma virus infection of the foreskin in asymptomatic boys. Urology. 2013;81:869–872. doi: 10.1016/j.urology.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 74.Liel C., Ulrich S.M., Lorenz S., Eickhorst A., Fluke J., Walper S. Risk factors for child abuse, neglect and exposure to intimate partner violence in early childhood: Findings in a representative cross-sectional sample in Germany. Child Abuse. Negl. 2020;106:104487. doi: 10.1016/j.chiabu.2020.104487. [DOI] [PubMed] [Google Scholar]
- 75.Mulder T.M., Kuiper K.C., van der Put C.E., Stams G.J.M., Assink M. Risk factors for child neglect: A meta-analytic review. Child Abuse. Negl. 2018;77:198–210. doi: 10.1016/j.chiabu.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 76.Unger E.R., Fajman N.N., Maloney E.M., Onyekwuluje J., Swan D.C., Howard L., Beck-Sague C.M., Sawyer M.K., Girardet R.G., Sautter R.L., et al. Anogenital Human Papillomavirus in Sexually Abused and Nonabused Children: A Multicenter Study. Pediatrics. 2011;128:e658–e665. doi: 10.1542/peds.2010-2247. [DOI] [PubMed] [Google Scholar]
- 77.Hornor G. Ano-genital warts in children: Sexual abuse or not? J. Pediatr. Health Care. 2004;18:165–170. doi: 10.1016/S0891-5245(04)00018-5. [DOI] [PubMed] [Google Scholar]
- 78.Ingram D.L., Everett V.D., Lyna P.R., White S.T., Rockwell L.A. Epidemiology of adult sexually transmitted disease agents in children being evaluated for sexual abuse. Pediatr. Infect. Dis. J. 1992;11:945–950. doi: 10.1097/00006454-199211110-00008. [DOI] [PubMed] [Google Scholar]
- 79.Muram D. Anal and perianal abnormalities in prepubertal victims of sexual abuse. Am. J. Obstet. Gynecol. 1989;161:278–281. doi: 10.1016/0002-9378(89)90498-5. [DOI] [PubMed] [Google Scholar]
- 80.Awasthi S., Ornelas J., Armstrong A., Johnson J.A., Eisen D.B. Anogenital warts and relationship to child sexual abuse: Systematic review and meta-analysis. Pediatric Dermatol. 2021;38:842–850. doi: 10.1111/pde.14650. [DOI] [PubMed] [Google Scholar]
- 81.Bussen S., Sütterlin M., Schmidt U., Bussen D. Anogenital Warts in Childhood—Always a Marker for Sexual Abuse? Geburtshilfe Frauenheilkd. 2012;72:43–48. doi: 10.1055/s-0031-1280417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Obalek S., Jablonska S., Favre M., Walczak L., Orth G. Condylomata acuminata in children: Frequent association with human papillomaviruses responsible for cutaneous warts. J. Am. Acad. Dermatol. 1990;23:205–213. doi: 10.1016/0190-9622(90)70200-2. [DOI] [PubMed] [Google Scholar]
- 83.Abu-Raya B., Michalski C., Sadarangani M., Lavoie P.M. Maternal Immunological Adaptation during Normal Pregnancy. Front. Immunol. 2020;11:575197. doi: 10.3389/fimmu.2020.575197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Akhavan S., Mousavi A., Modaresgilani M., Alibakhshi A. Genital Warts. J. Obstet. Gynecol. Cancer Res. 2017;2:e11440. [Google Scholar]
- 85.Sugai S., Nishijima K., Enomoto T. Management of Condyloma Acuminata in Pregnancy: A Review. Sex. Transm. Dis. 2021;48:403–409. doi: 10.1097/OLQ.0000000000001322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shehata H.A., Nelson-Piercy C. Drugs to avoid. Best Pract. Res. Clin. Obstet. Gynaecol. 2001;15:971–986. doi: 10.1053/beog.2001.0241. [DOI] [PubMed] [Google Scholar]
- 87.Centers for Disease Control and Prevention (CDC) HPV Vaccination Recommendations. [(accessed on 23 July 2022)]; Available online: https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html.
- 88.Moreira E.D., Jr., Block S.L., Ferris D., Giuliano A.R., Iversen O.E., Joura E.A., Kosalaraksa P., Schilling A., Van Damme P., Bornstein J., et al. Safety Profile of the 9-Valent HPV Vaccine: A Combined Analysis of 7 Phase III Clinical Trials. Pediatrics. 2016;138:e20154387. doi: 10.1542/peds.2015-4387. [DOI] [PubMed] [Google Scholar]
- 89.Kharbanda E.O., Vazquez-Benitez G., DeSilva M.B., Naleway A.L., Klein N.P., Hechter R.C., Glanz J.M., Donahue J.G., Jackson L.A., Sheth S.S., et al. Association of Inadvertent 9-Valent Human Papillomavirus Vaccine in Pregnancy with Spontaneous Abortion and Adverse Birth Outcomes. JAMA Netw. Open. 2021;4:e214340. doi: 10.1001/jamanetworkopen.2021.4340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kharbanda E.O., Vazquez-Benitez G., Lipkind H.S., Sheth S.S., Zhu J., Naleway A.L., Klein N.P., Hechter R., Daley M.F., Donahue J.G., et al. Risk of Spontaneous Abortion after Inadvertent Human Papillomavirus Vaccination in Pregnancy. Obstet. Gynecol. 2018;132:35–44. doi: 10.1097/AOG.0000000000002694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lipkind H.S., Vazquez-Benitez G., Nordin J.D., Romitti P.A., Naleway A.L., Klein N.P., Hechter R.C., Jackson M.L., Hambidge S.J., Lee G.M., et al. Maternal and Infant Outcomes After Human Papillomavirus Vaccination in the Periconceptional Period or during Pregnancy. Obstet. Gynecol. 2017;130:599–608. doi: 10.1097/AOG.0000000000002191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Faber M.T., Duun-Henriksen A.K., Dehlendorff C., Tatla M.K., Munk C., Kjaer S.K. Adverse pregnancy outcomes and infant mortality after quadrivalent HPV vaccination during pregnancy. Vaccine. 2019;37:265–271. doi: 10.1016/j.vaccine.2018.11.030. [DOI] [PubMed] [Google Scholar]
- 93.Sy L.S., Meyer K.I., Klein N.P., Chao C., Velicer C., Cheetham T.C., Ackerson B.K., Slezak J.M., Takhar H.S., Hansen J., et al. Postlicensure safety surveillance of congenital anomaly and miscarriage among pregnancies exposed to quadrivalent human papillomavirus vaccine. Hum. Vaccines Immunother. 2018;14:412–419. doi: 10.1080/21645515.2017.1403702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Condrat C.E., Filip L., Gherghe M., Cretoiu D., Suciu N. Maternal HPV Infection: Effects on Pregnancy Outcome. Viruses. 2021;13:2455. doi: 10.3390/v13122455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Popescu S.D., Boiangiu A.G., Sima R.M., Bilteanu L., Vladareanu S., Vladareanu R. Maternal HPV Infection and the Estimated Risks for Adverse Pregnancy Outcomes-A Systematic Review. Diagnostics. 2022;12:1471. doi: 10.3390/diagnostics12061471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nimrodi M., Kleitman V., Wainstock T., Gemer O., Meirovitz M., Maymon E., Benshalom-Tirosh N., Erez O. The association between cervical inflammation and histologic evidence of HPV in PAP smears and adverse pregnancy outcome in low risk population. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018;225:160–165. doi: 10.1016/j.ejogrb.2018.04.023. [DOI] [PubMed] [Google Scholar]
- 97.Capra G., Schillaci R., Bosco L., Roccheri M.C., Perino A., Ragusa M.A. HPV infection in semen: Results from a new molecular approach. Epidemiol. Infect. 2019;147:e177. doi: 10.1017/S0950268819000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gudnadottir U., Debelius J.W., Du J., Hugerth L.W., Danielsson H., Schuppe-Koistinen I., Fransson E., Brusselaers N. The vaginal microbiome and the risk of preterm birth: A systematic review and network meta-analysis. Sci. Rep. 2022;12:7926. doi: 10.1038/s41598-022-12007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Syrjänen S., Waterboer T., Rintala M., Pawlita M., Syrjänen K., Louvanto K., Grenman S. Maternal HPV-antibodies and seroconversion to HPV in children during the first 3 years of life. Sci. Rep. 2022;12:2227. doi: 10.1038/s41598-022-06343-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cason J., Mant C.A. High-risk mucosal human papillomavirus infections during infancy & childhood. J. Clin. Virol. 2005;32((Suppl. S1)):S52–S58. doi: 10.1016/j.jcv.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 101.Lee B., Lee S.W., Kim D.I., Kim J.H. HPV prevalence in the foreskins of asymptomatic healthy infants and children: Systematic review and meta-analysis. Sci. Rep. 2017;7:7050. doi: 10.1038/s41598-017-07506-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Juckett G., Hartman-Adams H. Human papillomavirus: Clinical manifestations and prevention. Am. Fam. Physician. 2010;82:1209–1213. [PubMed] [Google Scholar]
- 103.Leto M., Santos Júnior G.F., Porro A.M., Tomimori J. Human papillomavirus infection: Etiopathogenesis, molecular biology and clinical manifestations. An. Bras. Dermatol. 2011;86:306–317. doi: 10.1590/S0365-05962011000200014. [DOI] [PubMed] [Google Scholar]
- 104.Aguilera-Barrantes I., Magro C., Nuovo G.J. Verruca Vulgaris of the Vulva in Children and Adults: A Nonvenereal Type of Vulvar Wart. Am. J. Surg. Pathol. 2007;31:529–535. doi: 10.1097/01.pas.0000213409.41182.56. [DOI] [PubMed] [Google Scholar]
- 105.Van Haalen F.M., Bruggink S.C., Gussekloo J., Assendelft W.J.J., Eekhof J.A.H. Warts in primary schoolchildren: Prevalence and relation with environmental factors. Br. J. Dermatol. 2009;161:148–152. doi: 10.1111/j.1365-2133.2009.09160.x. [DOI] [PubMed] [Google Scholar]
- 106.Costa-Silva M., Fernandes I., Rodrigues A.G., Lisboa C. Anogenital warts in pediatric population. An. Bras. Dermatol. 2017;92:675–681. doi: 10.1590/abd1806-4841.201756411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jayasinghe Y., Garland S.M. Genital warts in children: What do they mean? Arch. Dis. Child. 2006;91:696–700. doi: 10.1136/adc.2005.092080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wiley D.J., Douglas J., Beutner K., Cox T., Fife K., Moscicki A.-B., Fukumoto L. External Genital Warts: Diagnosis, Treatment, and Prevention. Clin. Infect. Dis. 2002;35:S210–S224. doi: 10.1086/342109. [DOI] [PubMed] [Google Scholar]
- 109.Zavras N., Christianakis E., Tsamoudaki S., Velaoras K. Infantile perianal pyramidal protrusion: A report of 8 new cases and a review of the literature. Case Rep. Dermatol. 2012;4:202–206. doi: 10.1159/000342954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Berbegal-DeGracia L., Betlloch-Mas I., DeLeon-Marrero F.J., Martinez-Miravete M.T., Miralles-Botella J. Neonatal Molluscum contagiosum: Five new cases and a literature review. Australas. J. Dermatol. 2015;56:e35–e38. doi: 10.1111/ajd.12127. [DOI] [PubMed] [Google Scholar]
- 111.Pourang A., Fung M.A., Tartar D., Brassard A. Condyloma lata in secondary syphilis. JAAD Case Rep. 2021;10:18–21. doi: 10.1016/j.jdcr.2021.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Allen A.L., Siegfried E.C. The natural history of condyloma in children. J. Am. Acad. Dermatol. 1998;39:951–955. doi: 10.1016/S0190-9622(98)70268-3. [DOI] [PubMed] [Google Scholar]
- 113.Boull C., Groth D. Update: Treatment of Cutaneous Viral Warts in Children. Pediatr. Dermatol. 2011;28:217–229. doi: 10.1111/j.1525-1470.2010.01378.x. [DOI] [PubMed] [Google Scholar]
- 114.Carroll K.A., Pierce J., Kovarik C.L. Perianal Bowen disease in a child with human immunodeficiency virus. Pediatr. Dermatol. 2010;27:166–169. doi: 10.1111/j.1525-1470.2010.01103.x. [DOI] [PubMed] [Google Scholar]
- 115.Betz S.J. HPV-Related Papillary Lesions of the Oral Mucosa: A Review. Head Neck Pathol. 2019;13:80–90. doi: 10.1007/s12105-019-01003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Frigerio M., Martinelli-Kläy C.P., Lombardi T. Clinical, histopathological and immunohistochemical study of oral squamous papillomas. Acta Odontol. Scand. 2015;73:508–515. doi: 10.3109/00016357.2014.996186. [DOI] [PubMed] [Google Scholar]
- 117.Ward K.A., Napier S.S., Winter P.C., Maw R.D., Dinsmore W.W. Detection of human papilloma virus DNA sequences in oral squamous cell papillomas by the polymerase chain reaction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995;80:63–66. doi: 10.1016/S1079-2104(95)80017-4. [DOI] [PubMed] [Google Scholar]
- 118.Bennett L.K., Hinshaw M. Heck’s Disease: Diagnosis and Susceptibility. Pediatr. Dermatol. 2009;26:87–89. doi: 10.1111/j.1525-1470.2008.00830.x. [DOI] [PubMed] [Google Scholar]
- 119.Word Health Organization Cervical Cancer. 2022. [(accessed on 15 August 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer.
- 120.Balarezo F.S., Joshi V.V. Proliferative and neoplastic disorders in children with acquired immunodeficiency syndrome. Adv. Anat. Pathol. 2002;9:360–370. doi: 10.1097/00125480-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 121.Lee N.V., Kang E.T.B., Senger C., Poh C.F. Oral cancer in a 5-year-old boy: A rare case report and review of literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020;130:e10–e19. doi: 10.1016/j.oooo.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 122.Joos B., Joos N., Bumpous J., Burns C., French C.A., Farghaly H. Laryngeal Squamous Cell Carcinoma in a 13 Year-Old Child Associated with Human Papillomaviruses 16 and 18: A Case Report and Review of the Literature. Head Neck Pathol. 2008;3:37. doi: 10.1007/s12105-008-0093-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chow C.W., Tabrizi S.N., Tiedemann K., Waters K.D. Squamous cell carcinomas in children and young adults: A new wave of a very rare tumor? J. Pediatric Surg. 2007;42:2035–2039. doi: 10.1016/j.jpedsurg.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 124.Donne A.J., Hampson L., Homer J.J., Hampson I.N. The role of HPV type in Recurrent Respiratory Papillomatosis. Int. J. Pediatr. Otorhinolaryngol. 2010;74:7–14. doi: 10.1016/j.ijporl.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 125.Seedat R.Y. Juvenile-Onset Recurrent Respiratory Papillomatosis Diagnosis and Management—A Developing Country Review. Pediatr. Health Med. Ther. 2020;11:39–46. doi: 10.2147/PHMT.S200186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Scadding G.K., Bull P.D., Graham J.M., editors. Pediatric ENT. Springer; Berlin/Heidelberg, Germany: 2007. Recurrent Respiratory Papillomatosis; pp. 255–265. [DOI] [Google Scholar]
- 127.Quick C.A., Watts S.L., Krzyzek R.A., Faras A.J. Relationship between condylomata and laryngeal papillomata. Clinical and molecular virological evidence. Ann. Otol Rhinol. Laryngol. 1980;89:467–471. doi: 10.1177/000348948008900521. [DOI] [PubMed] [Google Scholar]
- 128.Silverberg M.J., Thorsen P., Lindeberg H., Grant L.A., Shah K.V. Condyloma in pregnancy is strongly predictive of juvenile-onset recurrent respiratory papillomatosis. Obstet. Gynecol. 2003;101:645–652. doi: 10.1016/s0029-7844(02)03081-8. [DOI] [PubMed] [Google Scholar]
- 129.Amiling R., Meites E., Querec T.D., Stone L., Singh V., Unger E.R., Derkay C.S., Markowitz L.E. Juvenile-Onset Recurrent Respiratory Papillomatosis in the United States, Epidemiology and HPV Types—2015–2020. J. Pediatric Infect. Dis. Soc. 2021;10:774–781. doi: 10.1093/jpids/piab016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lépine C., Voron T., Berrebi D., Mandavit M., Nervo M., Outh-Gauer S., Péré H., Tournier L., Teissier N., Tartour E., et al. Juvenile-Onset Recurrent Respiratory Papillomatosis Aggressiveness: In Situ Study of the Level of Transcription of HPV E6 and E7. Cancers. 2020;12:2836. doi: 10.3390/cancers12102836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bonagura V.R., Vambutas A., DeVoti J.A., Rosenthal D.W., Steinberg B.M., Abramson A.L., Shikowitz M.J., Gjertson D.W., Reed E.F. HLA alleles, IFN-gamma responses to HPV-11 E6, and disease severity in patients with recurrent respiratory papillomatosis. Hum. Immunol. 2004;65:773–782. doi: 10.1016/j.humimm.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 132.Bonagura V.R., Du Z., Ashouri E., Luo L., Hatam L.J., DeVoti J.A., Rosenthal D.W., Steinberg B.M., Abramson A.L., Gjertson D.W., et al. Activating killer cell immunoglobulin-like receptors 3DS1 and 2DS1 protect against developing the severe form of recurrent respiratory papillomatosis. Hum. Immunol. 2010;71:212–219. doi: 10.1016/j.humimm.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gélinas J.F., Manoukian J., Côté A. Lung involvement in juvenile onset recurrent respiratory papillomatosis: A systematic review of the literature. Int. J. Pediatr. Otorhinolaryngol. 2008;72:433–452. doi: 10.1016/j.ijporl.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 134.Montaño-Velázquez B.B., Nolasco-Renero J., Parada-Bañuelos J.E., Garcia-Vázquez F., Flores-Medina S., García-Romero C.S., Jáuregui-Renaud K. Quality of life of young patients with recurrent respiratory papillomatosis. J. Laryngol. Otol. 2017;131:425–428. doi: 10.1017/S0022215117000354. [DOI] [PubMed] [Google Scholar]
- 135.Ivancic R., Iqbal H., deSilva B., Pan Q., Matrka L. Current and future management of recurrent respiratory papillomatosis. Laryngoscope Investig. Otolaryngol. 2018;3:22–34. doi: 10.1002/lio2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ouda A.M., Elsabagh A.A., Elmakaty I.M., Gupta I., Vranic S., Al-Thawadi H., Al Moustafa A.E. HPV and Recurrent Respiratory Papillomatosis: A Brief Review. Life. 2021;11:1279. doi: 10.3390/life11111279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rosen C.A., Bryson P.C. Indole-3-carbinol for recurrent respiratory papillomatosis: Long-term results. J. Voice. 2004;18:248–253. doi: 10.1016/j.jvoice.2003.05.005. [DOI] [PubMed] [Google Scholar]
- 138.Rosenberg T., Philipsen B.B., Mehlum C.S., Dyrvig A.K., Wehberg S., Chirilǎ M., Godballe C. Therapeutic Use of the Human Papillomavirus Vaccine on Recurrent Respiratory Papillomatosis: A Systematic Review and Meta-Analysis. J. Infect. Dis. 2019;219:1016–1025. doi: 10.1093/infdis/jiy616. [DOI] [PubMed] [Google Scholar]
- 139.Best S.R., Mohr M., Zur K.B. Systemic bevacizumab for recurrent respiratory papillomatosis: A national survey. Laryngoscope. 2017;127:2225–2229. doi: 10.1002/lary.26662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Evers G., Schliemann C., Beule A., Schmidt L.-H., Schulze A.B., Kessler C., Hoffmann T.K., Wiewrodt R., Groll A.H., Bleckmann A., et al. Long-Term Follow-Up on Systemic Bevacizumab Treatment in Recurrent Respiratory Papillomatosis. Laryngoscope. 2021;131:E1926–E1933. doi: 10.1002/lary.29351. [DOI] [PubMed] [Google Scholar]
- 141.Gerein V., Rastorguev E., Gerein J., Jecker P., Pfister H. Use of interferon-alpha in recurrent respiratory papillomatosis: 20-year follow-up. Ann. Otol. Rhinol. Laryngol. 2005;114:463–471. doi: 10.1177/000348940511400608. [DOI] [PubMed] [Google Scholar]
- 142.Broekema F.I., Dikkers F.G. Side-effects of cidofovir in the treatment of recurrent respiratory papillomatosis. Eur. Arch. Otorhinolaryngol. 2008;265:871–879. doi: 10.1007/s00405-008-0658-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Allen C.T., Lee S., Norberg S.M., Kovalovsky D., Ye H., Clavijo P.E., Hu-Lieskovan S., Schlegel R., Schlom J., Strauss J., et al. Safety and clinical activity of PD-L1 blockade in patients with aggressive recurrent respiratory papillomatosis. J. ImmunoTherapy Cancer. 2019;7:119. doi: 10.1186/s40425-019-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Limsukon A., Susanto I., Soo Hoo G.W., Dubinett S.M., Batra R.K. Regression of recurrent respiratory papillomatosis with celecoxib and erlotinib combination therapy. Chest. 2009;136:924–926. doi: 10.1378/chest.08-2639. [DOI] [PubMed] [Google Scholar]
- 145.Rojas-Lechuga M.J., Remacha J., González-Sánchez N., Grau J.J., Castillo P., Haag O., Vilaseca I. Juvenile recurrent respiratory papillomatosis treated with combined erlotinib and celecoxib: Initial report. Int. J. Pediatr. Otorhinolaryngol. 2020;137:110194. doi: 10.1016/j.ijporl.2020.110194. [DOI] [PubMed] [Google Scholar]
- 146.Mitra S., Das A., Ghosh D., Sengupta A. Postoperative Systemic Acyclovir in Juvenile-Onset Recurrent Respiratory Papillomatosis: The Outcome. Ear Nose Throat J. 2019;98:28–31. doi: 10.1177/0145561318823311. [DOI] [PubMed] [Google Scholar]
- 147.Morrison G.A.J., Kotecha B., Evans J.N.G. Ribavirin treatment for juvenile respiratory papillomatosis. J. Laryngol. Otol. 1993;107:423–426. doi: 10.1017/S0022215100123321. [DOI] [PubMed] [Google Scholar]
- 148.Rao R., Honavar S.G. Retinoblastoma. Indian J. Pediatrics. 2017;84:937–944. doi: 10.1007/s12098-017-2395-0. [DOI] [PubMed] [Google Scholar]
- 149.Dimaras H., Kimani K., Dimba E.A.O., Gronsdahl P., White A., Chan H.S.L., Gallie B.L. Retinoblastoma. Lancet. 2012;379:1436–1446. doi: 10.1016/S0140-6736(11)61137-9. [DOI] [PubMed] [Google Scholar]
- 150.Chauhan S., Sen S., Singh N., Sharma A., Chawla B., Kashyap S. Human papillomavirus detection strategies in retinoblastoma. Pathol. Oncol. Res. 2020;26:1341–1344. doi: 10.1007/s12253-018-00577-x. [DOI] [PubMed] [Google Scholar]
- 151.Antoneli C.B., Ribeiro K.B., Sredni S.T., Arias V.E., Andreoli M.A., De Camargo B., Sobrinho J.S., Prado J.C., Soares F.A., Villa L.L. Low prevalence of HPV in Brazilian children with retinoblastoma. J. Med. Virol. 2011;83:115–118. doi: 10.1002/jmv.21925. [DOI] [PubMed] [Google Scholar]
- 152.Yim E.-K., Park J.-S. The role of HPV E6 and E7 oncoproteins in HPV-associated cervical carcinogenesis. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2005;37:319–324. doi: 10.4143/crt.2005.37.6.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Soltani S., Tabibzadeh A., Yousefi P., Zandi M., Zakeri A., Akhavan Rezayat S., Ramezani A., Esghaei M., Farahani A. HPV infections in retinoblastoma: A systematic review. J. Clin. Lab. Anal. 2021;35:e23981. doi: 10.1002/jcla.23981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ryoo N.-K., Kim J.-E., Choung H.-K., Kim N., Lee M.-J., Khwarg S.-I. Human papilloma virus in retinoblastoma tissues from Korean patients. Korean J. Ophthalmol. 2013;27:368–371. doi: 10.3341/kjo.2013.27.5.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Shetty O.A., Naresh K.N., Banavali S.D., Shet T., Joshi R., Qureshi S., Mulherkar R., Borges A., Desai S.B. Evidence for the presence of high risk human papillomavirus in retinoblastoma tissue from nonfamilial retinoblastoma in developing countries. Pediatr. Blood Cancer. 2012;58:185–190. doi: 10.1002/pbc.23346. [DOI] [PubMed] [Google Scholar]
- 156.Bhuvaneswari A., Pallavi V., Jayshree R., Kumar R.V. Maternal transmission of human papillomavirus in retinoblastoma: A possible route of transfer. Indian J. Med. Paediatr. Oncol. 2012;33:210–215. doi: 10.4103/0971-5851.107080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Heck J.E., Lombardi C.A., Meyers T.J., Cockburn M., Wilhelm M., Ritz B. Perinatal characteristics and retinoblastoma. Cancer Causes Control. 2012;23:1567–1575. doi: 10.1007/s10552-012-0034-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Javanmard D., Moein M., Esghaei M., Naseripour M., Monavari S.H., Bokharaei-Salim F., Sadeghipour A. Molecular evidence of human papillomaviruses in the retinoblastoma tumor. Virusdisease. 2019;30:360–366. doi: 10.1007/s13337-019-00540-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gillison M.L., Chen R., Goshu E., Rushlow D., Chen N., Banister C., Creek K.E., Gallie B.L. Human retinoblastoma is not caused by known pRb-inactivating human DNA tumor viruses. Int. J. Cancer. 2007;120:1482–1490. doi: 10.1002/ijc.22516. [DOI] [PubMed] [Google Scholar]
- 160.Anand B., Ramesh C., Appaji L., Kumari B.A., Shenoy A., Jayshree R., Kumar R.V. Prevalence of high-risk human papillomavirus genotypes in retinoblastoma. Br. J. Ophthalmol. 2011;95:1014–1018. doi: 10.1136/bjo.2010.199802. [DOI] [PubMed] [Google Scholar]
- 161.Theotoka D., Morkin M.I., Galor A., Karp C.L. Update on diagnosis and management of conjunctival papilloma. Eye Vis. 2019;6:18. doi: 10.1186/s40662-019-0142-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Mammas I.N., Dalianis T., Doukas S.G., Zaravinos A., Achtsidis V., Thiagarajan P., Theodoridou M., Spandidos D.A. Paediatric virology and human papillomaviruses: An update. Exp. Ther. Med. 2019;17:4337–4343. doi: 10.3892/etm.2019.7516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kaliki S., Arepalli S., Shields C.L., Klein K., Sun H., Hysenj E., Lally S.E., Shields J.A. Conjunctival papilloma: Features and outcomes based on age at initial examination. JAMA Ophthalmol. 2013;131:585–593. doi: 10.1001/jamaophthalmol.2013.83. [DOI] [PubMed] [Google Scholar]
- 164.Li Y., Witte D., Myer C., Gluckman J., Pavelic Z., Pavelic L., Stambrook P. Involvement of episomal hpv31 in a laryngeal carcinoma-persistent episomal maintenance of hpv DNA after passage through nude-mice. Int. J. Oncol. 1994;4:1377–1382. doi: 10.3892/ijo.4.6.1377. [DOI] [PubMed] [Google Scholar]
- 165.Egbert J.E., Kersten R.C. Female genital tract papillomavirus in conjunctival papillomas of infancy. Am. J. Ophthalmol. 1997;123:551–552. doi: 10.1016/S0002-9394(14)70184-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.