Abstract
Objective
(1) To evaluate the effects of surgery and conservative treatments for cervical spondylotic radiculopathy and (2) provide reference for choosing the time and method of treatment.
Methods
A literature search was performed using PubMed, EMbase, The Cochrane Library, Web of Science, and ClinicalTrials from inception to September 2021. Randomized controlled trials (RCTs) on the use of surgery or conservative Treatments in Cervical Spondylotic Radiculopathy (CSR) were selected. The primary outcomes were the neck and arm visual analog scale (VAS) and Neck Disability Index (NDI). Secondary outcomes included active range of cervical motion (ROM) and Mental Health. Two reviewers proceeded study selection and quality assessment.
Results
A total of 6 studies, which comprised a total of 464 participants were included in the final meta-analysis. Compared with conservative treatment, surgical treatment was more effective in lowering Neck-VAS (<3 m: MD = −29.44, 95% CI = (–41.62,–17.27), P < .00001; 3–6 M: MD = −20.97, 95% CI = (–26.36,–15.57), P < .00001; 6 M: MD = −13.40, 95% CI = (–19.39, −7.41), P<.0001; 12 M: MD=−15.53, 95% CI=(-28.38, −2.68), P=.02), Arm-VAS(<3 m: MD = −33.52, 95% CI = (–39.89, −27.16), P < .00001; 3-6 M: MD = −20.97, 95% CI = (–26.36, −15.57), P < .00001; 6 M: MD = −17.52, 95% CI=(–23.94, −11.11), P < .0001; 12 M: MD = −21.91, 95% CI=(–27.09, −16.72), P < .00001) and NDI (<3 m: MD = −8.89, 95% CI = (–11.17, −6.61), P < .00001; 6 M: MD = −5.14, 95% CI = (–7.60, −2.69), P < .0001). No significant difference was observed in NDI at 12-month time point (MD = −5.17, 95% CI = (–12.33, 2.00), P = .16), ROM(MD = 2.91, 95% CI = (–4.51, 10.33), P = .77) and Mental Health (MD = .05, 95% CI=(–.24, .33), P = .74).
Conclusion
The 6 included studies that had low risk of bias, providing high-quality evidence for the surgical efficacy of CSR. The evidence indicates that surgical treatment is better than conservative treatment in terms of VAS score and NDI score, and superior to conservative treatment in less than one year. There was no evidence of a difference between surgical and conservative care in ROM and mental health. A small sample study with a follow-up of 5 to 8 years showed that surgical treatment was still better than conservative treatment, but the sample size was small and the results should be carefully interpreted.
Compared with conservative treatment, surgical treatment had a faster onset of response, especially in pain relief, but did not have a significant advantage in range of motion or NDI. This seems to mean that for patients with severe or even unbearable pain, the benefits of surgery as soon as possible will be significant. Although it is not clear whether the short-term risks of surgery are outweighed by the long-term benefits, rapid pain relief is necessary. Conservative treatment (including medical exercise therapy, mechanical cervical tractions, transcutaneous electrical nerve stimulation, pain management education, and cervical collar) once or twice a week for 3 months is beneficial in the long term and avoids the risks of surgery. In consideration of the good natural history of CSR and the relatively good outcome of conservative treatment (although symptom relief is slow), we think that surgery is not necessary for patients who do not need rapid pain relief.
Keywords: Surgery, Conservative Treatments, Cervical Spondylotic Radiculopathy, Systematic review
Introduction
Cervical spondylosis is a very common disease, cervical spondylotic radiculopathy (CSR) is the most common type, accounting for about 60–70% of all cervical spondylosis. It is a clinical syndrome caused by cervical disc degeneration, hyperosteogeny, cervical joint and ligament loosening, and dislocation stimulation or compression of cervical nerve roots.1-6 The prevalence of cervical radiculopathy has been noted as 3.5 per 1000 population, with a peak incidence in the sixth decade of life. 7 The incidence of CSR tends to increase year by year due to population aging, lifestyle changes, and work or life stress. Its clinical manifestations focus on pain and numbness of the neck and arm as well as restricted movement of the neck, which greatly affects people’s lives and work. 8 In the Netherlands, with a population of 17 million, on average 2000 patients yearly receive surgery for a cervical herniated disc, resulting in direct costs of about €30 million per year. 9
Treatment of spondylitic cervical radiculopathy can range from conservative management to surgery. 14 Surgical treatment of CSR has been proven to be effective, but studies have shown that similar improvements can be achieved with conservative treatment and that conservative treatment is often the preferred option because it avoids the risks of surgical treatment.15-18 A study of perioperative management of cervical spine surgery showed that 44% of neurosurgeons chose surgical procedures regardless of the pathologic process, and the procedures chosen varied widely from center to center. In some studies, conservative treatment continued for months or even years, while in others surgery was performed after the first consultation. 19 Some literature suggests that surgery should be considered only when pain is severe, conservative treatment fails, or muscle weakness or atrophy is evident, 20 but many of the clinical practice guidelines suggested that there is a lack of conclusive evidence to define the indications and timing of CSR.21-23 The classification of CSR focuses on the description of the degree of intervertebral disc degeneration and protrusion, which has little guiding significance for the selection of treatment plan. In addition, it is not clear which surgical approach is best for CSR. ACDF is the most commonly used surgical approach, but studies have shown that neither anterior approach nor posterior approach has an overall advantage and there is conflicting evidence about the efficacy of anterior cervical foraminotomy, with success rates reported at 52–99%, but recurrent symptoms up to 30%. 19 Minimally invasive techniques have also developed rapidly in the past decade. Some clinical guidelines suggest that ACDF procedures can be performed under endoscopy with great safety and good results. 24
The natural history of CSR is favorable as most (83%) patients with symptomatic radiculopathy recover within 24–36 months and substantial improvements usually occur 4–6 months post onset.10-12 A study of 563 patients who visited the Mayo Clinic between 1976 and 1990 also showed that 90% had mild or no symptoms after 4 to 5 years of follow-up. 13 It is not clear whether the short-term risks of surgical treatment are offset by the long-term benefits. Previous studies included very few randomized controlled trials and were very old. Considering that indications, timing, techniques, and duration of efficacy of surgical and conservative care are not well defined, systematic evaluation of surgical and nonsurgical treatment for CSR is necessary. Which surgery is better will be the subject of another study.
Method
Inclusion Criteria
1. Study eligibility: Randomized controlled trials (RCTs) and pilot studies that applied a randomized controlled design. Non-English language studies were not included.
2. Types of participants: Patients clinically diagnosed with CSR (pain distributed along the skin of one or more cervical roots, sometimes accompanied by weakness and hyporeflexia). Patients with other mental illnesses and those taking other anti-depression and anxiety drugs were excluded.
3. Types of interventions: Patients in the experimental group were treated with surgery (including minimally invasive interventional surgery and open surgery, with or without fusion, designed to alleviate the root compression) and patients in the control group were given conservative treatment (including physiotherapy and cervical collar). OR experimental group received surgery combined with conservative treatment, and the control group received the same conservative treatment.
4. Types of outcome measures: Main outcomes: ① Neck and arm visual analog scale (VAS); ②Neck Disability Index (NDI); Secondary outcomes: ①Active range of cervical motion (ROM); and ②Mental Health included Mood Adjective Check List (MACL) or scoring of the mental health dimension of the SF-36 questionnaire.
Search Methods
We searched the following electronic databases from inception to September 2021: PubMed, EMbase, The Cochrane Library, Web of Science, and ClinicalTrials, and the combination of keyword and free word retrieval is adopted. The search terms include “Radiculopathy,” “Cervical Radiculopathies,” “Surgery,” “Conservative,” and “randomized controlled trial.” The complete PubMed search strategy is summarized in Table 1, this search strategy will be modified as required for other electronic databases. Eligible studies were selected and checked independently by two authors (HLY and YXX).
Table 1.
Search strategy used in PubMed database.
| Number | Search terms |
|---|---|
| 1 | Radiculopathy. Mesh. |
| 2 | Radiculopathies. ti, ab. |
| 3 | Radiculopathy, Cervical. ti, ab |
| 4 | Cervical Radiculopathies. ti, ab. |
| 5 | Cervical Radiculopathy. ti, ab. |
| 6 | Radiculopathies, Cervical. ti, ab. |
| 7 | Nerve Root Disorder. ti, ab. |
| 8 | Radicultis. ti, ab. |
| 9 | Nerve Root Inflammation. ti, ab. |
| 10 | Inflammation, Nerve Root. ti, ab |
| 11 | Nerve Root Inflammations. ti, ab. |
| 12 | Nerve Root Avulsion. ti, ab |
| 13 | Avulsion, Nerve Root. ti, ab |
| 14 | Avulsions, Nerve Root. ti, ab |
| 15 | Nerve Root Avulsions, ti, ab. |
| 16 | Nerve Root Compression. ti, ab. |
| 17 | Compression, Nerve Root. ti, ab. |
| 18 | Compressions, Nerve Root. ti, ab. |
| 19 | Nerve Root Compressions. ti, ab. |
| 20 | 1 or 2 or 3 or…or 18 or 19 |
| 21 | General Surgery. Mesh. |
| 22 | Surgery, General. ti, ab. |
| 23 | Surgery. ti, ab. |
| 24 | 21 or 22 or 23 |
| 25 | Conservative Treatments. Mesh. |
| 26 | Treatment, Conservative. ti, ab. |
| 27 | Treatments, Conservative. ti, ab. |
| 28 | Conservative Management. ti, ab. |
| 29 | Conservative Managements. ti, ab. |
| 30 | Management, Conservative. ti, ab. |
| 31 | Managements, Conservative. ti, ab. |
| 32 | Conservative Therapy. ti, ab. |
| 33 | Conservative Therapies. ti, ab. |
| 34 | Therapies, Conservative. ti, ab. |
| 35 | Therapy, Conservative. ti, ab. |
| 36 | 25 or 26 or 27 or … or 34 or 35 |
| 37 | randomized controlled trial. PT. |
| 38 | nonrandomized. ti, ab. |
| 39 | placebo. ti, ab. |
| 40 | 37 or 38 or 39 |
| 41 | 20 and 24 and 36 and 40 |
Data Extraction
Two researchers (HLY and YXX) independently extracted data from the included trials using standardized data extraction tables, including year, author, country, sample size, patient baseline characteristics, treatment duration, interventions, and outcomes. Any differences were resolved through discussion. Disagreement was resolved by discussion and reached consensus through a third party (WP or LYD). If additional data was needed, we contacted the study authors in time.
Risk of Bias Assessment
The risk of bias in the included studies was assessed by two researchers (HLY and FTX) using the Cochrane Collaboration Risk of Bias Tool, for risk assessment of bias in RCT. Seven items were included: generation of random order, concealment of random scheme allocation, blind method for research objects and intervention implementors, blind method for outcome evaluators, integrity of outcome indicator data, possibility of selective reporting of research results, and other sources of bias. The evaluator should make a low bias risk, high bias risk, and unclear judgment for each project.
Statistical Analysis
RevMan 5.3 software was used for meta-analysis of the data. First, the X2 test was used to test the heterogeneity between literature results. If the test results were P > .1 and I2 < 50%, the fixed-effect model was used for meta-analysis. If P < .1, I2 ≥ 50%, and no clinical heterogeneity was determined, the random effect model was used for meta-analysis. Subgroup analyses were performed on the studies to dissipate any heterogeneity. If the source of heterogeneity could not be determined, descriptive studies were used. For continuous data, if the results obtained by the same measuring tool are adopted, the difference in mean (MD) is used as the effect analysis statistics. If different measurement tools are used for the same variable, standardized mean difference (SMD) is used as the effect analysis statistic. The results of data analysis are presented using forest plots. Sensitivity analysis was performed by removing each study individually to assess the consistency and quality of the results.
Strength of Evidence
We applied the GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) approach to evaluate the overall quality of the evidence. 42 Five basic factors could decrease the quality of evidence: (1) Limitations in study design and/or execution; (2) inconsistency of results; (3) indirectness of evidence; (4) imprecision of results; and (5) publication bias. There were also three factors for upgrading. 43 Two independent reviewers (HLY and YXX) assessed the quality of evidence. The quality of the evidence was downgraded by one level when one of the factors described above was met.
The following grading of quality of evidence and definitions were used: (1) High quality: Further research is very unlikely to change our confidence in the estimate of effect; (2) Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; (3) Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; and (4) Very low quality: Any estimate of effect is very uncertain.
Results
Study Selection and Inclusion Process
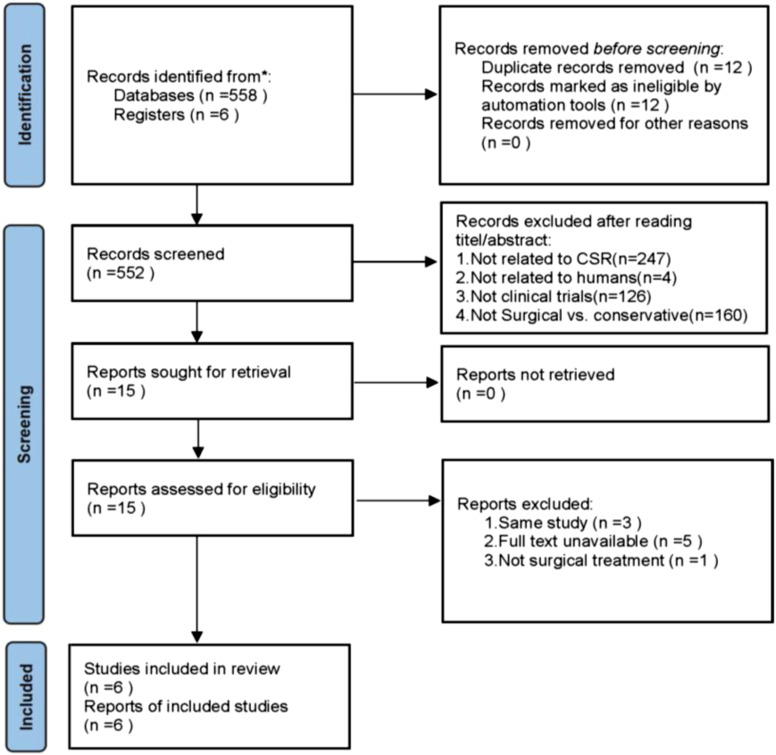
Through database search, a total of 564 potentially relevant studies were identified. Of those, 12 articles were duplicated. Of the remaining 552 articles, 537 were excluded by reading the title and abstract filters. In the remaining 15 articles, through searching and reading the full text, excluding non-randomized controls and research data to obtain fruitless clinical trials, 6 articles25-30 were finally included. These 6 articles included a total of 464 patients. Details of the selection process are illustrated in Figure 1.
Figure 1.
PRISMA 2020 flow diagram.
Study Characteristics
The included studies were published from 1996 through 2017. The major publishing countries are Sweden (n = 4), and Italy (n = 2). The studies contained a total of 464 patients, of whom 206 were treated with surgery and 258 patients were treated with conservative therapy. The primary outcomes included the neck and arm visual analog scale (VAS), Neck Disability Index (NDI). Secondary outcomes included active range of cervical motion (ROM) and Mental Health included Mood Adjective Check List (MACL) or scoring of the mental health dimension of the SF-36 questionnaire. Characteristics of included studies are summarized in Table 2.
Table 2.
Characteristics of the included studies.
| Study | Country | Study Design | No. Patients | Gender (M/F) | Age | Intervention Measure | Evaluating Indicator | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Sur | Con | Sur | Con | Sur | Con | |||||
| Alessandro 2010 | Italy | Prospective randomized study | 62 | 58 | 53/67 | 45.03 ± 10.72 | 47.43 ± 11.49 | PDD | Received an array of conservative care therapies, depending on the patient’s condition. Included transcutaneous electrical nerve stimulation (TENS), progressive neck mobilization accompanied by a gradual reduction in collar usage, postural rehabilitation of the Mezieres technique, analgesics and/or NSAIDs. | VAS,NDI,SF-36 |
| Engquist 2013 | Sweden | Prospective randomized study | 31 | 32 | 33/30 | 49 ± 8 | 44 ± 9 | ACDF with Physiotherapy (3 months after surgery, same as nonsurgical group) | Step 1 consisted of neck-specific exercises and procedures for pain relief. Step 2 involved general exercises, and step 3 involved pain coping, increasing self-efficacy, and stress management strategies | VAS,NDI |
| Anneli 2013 | Sweden | Prospective randomized study | 24 | 25 | 34/29 | 46 ± 8.9 | 46 ± 8.9 | ACDF with Physiotherapy (3 months after surgery, same as hysiotherapy group) | Medical exercise therapy (performed twice a week for 14 weeks); education in pain management (once a week during the first 14 weeks); neck-specific exercises (after 14 weeks) | ROM |
| Jacopo 2017 | Italy | Prospective randomized study | 40 | 40 | 46/34 | 46.1 ± 12.52 | 45.02 ± 12.87 | PCTF (after steroids and NSAIDs for 6 weeks) | Mechanical cervical tractions (after steroids and NSAIDs for 6 weeks. Patients were positioned supine and mechanical traction equipment was adjusted manually. A pulling force was applied equal to 10% of patient’s weight for 10 seconds followed by 5 seconds rest for a total of 15 minutes. The force was applied parallel to the cervical spine. The sessions were repeated biweekly for 5 weeks before the first pain and disability assessment.) | VAS,NDI |
| Liselott 1996 | Sweden | Prospective randomized study | 22 | 49 | 41/30 | 46 ± 8 | 48 ± 8 | ACDF | Physiotherapy (The choice of physiotherapeutic methods used was made by the physiotherapists according to their individual preferences and the patient’s symptoms.The treatments were given on 15 occasions, each 30 to 45 minutes long, over a 3-month period. Including ergonomic instructions, postural correction, heat, cryotherapy, massage, transcutaneous nerve stimulation, resting and relaxation exercises); cervical collar (over 3 months, during daytime only) | VAS,ROM |
| Liselott 2001 | Sweden | Prospective randomized study | 27 | 54 | 44/37 | 45 (47) | 46 (−) | ACD | Physiotherapy (over 3 months and was individual and divided into 15 sessions, with 1-2 sessions per week, each 30-45 minutes long. Including transcutaneous electrical nerve stimulation, heat (moist pack, ultrasound) or cold and massage, manual traction and gentle mobilization combined with heat therapy or relaxation exercises, active exercises, ergonomic instructions, postural corrections and co-ordination exercises); cervical collar (rigid collar during daytime and soft collar during night, over 3 months) | VAS,MACL |
Remarks. ACD: anterior cervical discectomy; ACDF: anterior cervical decompression and fusion; PCTF: posterior cervical transfacet fusion with facetal spacer; PDD:Plasma disc decompression.
Risk of Bias Assessment
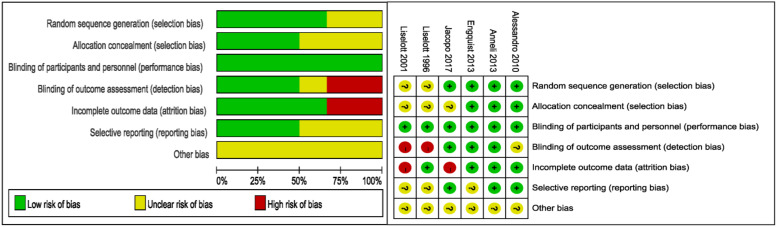
Each study reported that patients were randomly divided into surgery and conservative groups, four studies provided details of the randomization process.25,28-30 Three of the studies reported allocation concealment.28-30 Due to the particularity of the study protocol (surgical treatment or conservative treatment, no drug treatment), subjects and researchers cannot be blinded, but we judge that the results will not be affected. Three studies blinded outcome evaluators.25,28,29 With regard to selective reporting bias, we judged that expected outcomes were stated in all trials. The bias risks of the included studies are shown in Figure 2. (green circles indicate a low risk of bias, yellow circles indicate an unclear risk of bias, and red circles indicate a high risk of bias).
Figure 2.
Risk of bias summary. Remarks. Green circles indicate a low risk of bias, yellow circles indicate an unclear risk of bias and red circles indicate a high risk of bias.
Efficacy Analysis
VAS Score
Neck VAS
Five articles (419 patients) reported VAS scores as outcome measurements. Two articles26,27 did not separate the neck and arm VAS scores, and the reviewers regarded the neck VAS scores as the same as the arm VAS scores. Results of the heterogeneity test were (P < .00001, I2 = 76%), Meta-analysis using the random effect model. Overall, surgery group reduce the patient’s neck VAS score better than the conservative group, with statistically significant differences [MD = −17.90, 95% CI (−23.54, −12.26), P < .00001]. Since these studies provide different follow-up periods, subgroup analysis was used for different periods. In the test for subgroup differences, available evidence indicates that patients in the surgery group had lower VAS scores than those in the conservative treatment group at follow-up of less than 3 months to 1 year (Figure 3). Four studies25,27,28,30 provided long-term follow-up data over a period of one year, with high heterogeneity (I2 = 85%). Sensitivity analysis showed that the pooled result was unstable at one year follow-up without study, 30 and there was no significant change when studies25,27,28 were removed.
Figure 3.
Forest plot for Neck VAS.
Arm VAS
Five articles (419 patients) reported VAS scores as outcome measurements. Two articles26,27 did not separate the neck and arm VAS scores, and the reviewers regarded the neck VAS scores as the same as the arm VAS scores. The heterogeneity test results were (P = .0005, I2 = 76%). Heterogeneity exists between studies, excluding clinical heterogeneity. Meta-analysis using a random effects model showed that surgery group reduce the patient’s neck VAS score better than the conservative group, with a significant difference (MD = −23.13, 95% CI (−26.01, −20.25), P < .00001) (Figure 4). In the test for subgroup differences, all available evidence indicates that patients in the surgery group had lower VAS scores than those in the conservative treatment group at both long-term and short-term follow-up (Figure 4). Four studies25,27,28,30 provided long-term follow-up data over a period of one year, with high heterogeneity (I2 = 79%). Sensitivity analysis showed that the pooled result was unstable at one year follow-up without study, 30 and there was no significant change when studies25,27,28 were removed.
Figure 4.
Forest plot for Arm VAS.
Neck Disability Index (NDI)
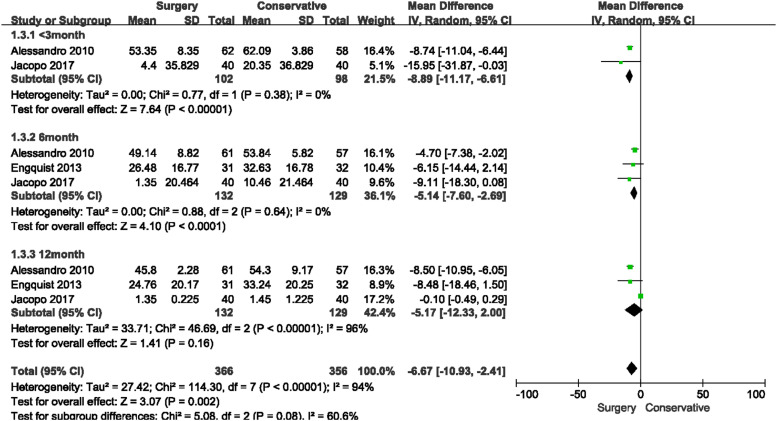
Three articles25,28,30(263 patients) reported Neck Disability Index as outcome indicator. The heterogeneity test results were (P < .0001, I2 = 94%). Heterogeneity exists between studies, meta-analysis using the random effect model. Overall, surgical treatment was more effective in improving disability than conservative treatment, with a significant difference (MD = −6.67, 95% CI (−10.93, −2.41), P = .002). In the test for subgroup differences, surgical treatment was observed to be more effective than conservative treatments in the 3 months and 6 months, but there was no difference in NDI improvement between surgical and conservative treatment at 12-month time point (MD = −5.17, 95% CI (−12.33, 2.00), P = .16). The significance of the results did not change when the studies were removed one by one at 3 and 6 months. At 1 year, sensitivity analysis showed that the pooled result was unstable without study 25 (Figure 5).
Figure 5.
Forest plot for Oswestry Disability Index (NDI).
Active Range of Cervical motion(ROM)
Two articles26,29 (120 patients)reported active range of cervical motion. One article 26 did not provide post-treatment cervical motion data, only reported that no significant difference between pre-treatment and post-treatment. Based on the literature, the reviewers used pre-treatment data as data for quantitative analysis. The heterogeneity test results were (P = .30, I2 = 5%). Meta-analysis using the fixed-effect model showed that there was no difference in ROM improvement between surgical and conservative group (MD = 2.91, 95% CI (−4.51,10.33), P = .44) (Figure 6).
Figure 6.
Forest plot for Active range of cervical motion.
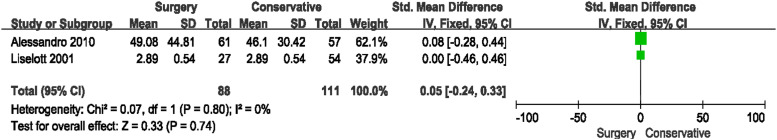
Mental Health
Two articles27,30 (196 patients) reported Mental Health. Alessandro Cesaroni 30 used the SF-36 scale as an evaluation indicator and reported score data on the mental health dimension before and after treatment. Liselott Persson 6 used Mood Adjective Check List (MACL) to measure emotional state and mental well-being quantitatively. The two studies used different scales so the results were combined using a standardized mean difference (SMD). The heterogeneity test results were (P = .80, I2 = 0%). Meta-analysis using the fixed-effect model showed that there was no difference in ROM improvement between surgical and conservative group (SMD = .05, 95% CI (−.24, 0.33), P = .74) (Figure 7).
Figure 7.
Forest plot for Mental Health.
Discussion
The efficacy of surgical and conservative treatment for radicular cervical spondylopathy has long been a subject of debate. The indications, timing, techniques, and duration of efficacy of surgical and conservative care are not well defined. The most recent cochrane systematic review 18 was published in 2010, when only one randomized controlled study of 81 patients of CSR with a short follow-up was available for analysis. More than 10 years have passed, minimally invasive surgical techniques and conservative treatment methods are developing rapidly, and many clinical studies have not been integrated and analyzed, so systematic evaluation of surgical and nonsurgical treatment for CSR is necessary.
This study included randomized controlled studies comparing surgical and conservative treatment of cervical spondylotic radiculopathy from 1996 to 2017, the randomized controlled studies previously analyzed by Nikolaidis l18 were also included for quantitative analysis. Open surgery and minimally invasive surgery were included. We performed short-and long-term subgroup analyses, taking into account the different duration of follow-up for each study. Overall, available evidence suggests that surgical treatment has superior Neck-VAS(MD = −17.90, 95% CI (−23.54, −12.26), P < .00001), Arm-VAS(MD = −23.13, 95% CI (−26.01, −20.25), P < .00001), and NDI scores (MD = −6.67, 95% CI (−10.93, −2.41), P = .002) in both short-term and long-term follow-up. As in Nikolaidis I et al.’s 2010 system review, 18 surgery resulted in faster pain relief. Most of the literature included in this study had a longer follow-up period, and we found that the long-term benefits (within 1 year) of surgical treatment exist. Markus Engquist 31 followed previous study 28 for 5 to 8 years and found that the surgery group was better than the non-surgery group in neck and arm pain and NDI scores, both better than baseline data, although this result may in part be attributable to the natural course of the disease, indicating that early treatment outcome can be expected to persist after more than 5 years. However, the number of studies followed for more than 5 years is very small, and the results may be affected by the small sample size, so the results need to be interpreted with caution.
In the subgroup analysis, VAS score and NDI in the operation group were better than those in the conservative group, heterogeneity was low in all follow-up studies with Neck-VAS and NDI score less than one year, but heterogeneity was high in several studies at one year, and sensitivity analysis revealed the combined results were unstable when the literature25,30 was removed. Alessandro’s study 30 used Plasma disc decompression (PDD) as surgical treatment, we speculated that heterogeneity may be caused by the different technical principles of PDD and ACDF. PDD is effective for inclusive herniation and small herniation. Therefore, in terms of indications, Anderson excluded patients with focal herniation of more than one-third of the spinal canal or with intervertebral foraminal stenosis caused by hyperosteogenesis. It is not the focus of this study to discuss whether PDD or ACDF has better long-term benefits in treating CSR, which should be further studied. Jacopo’s study 25 comparing the efficacy of PCTF and mechanical traction in CSR showed that the NDI scores of the surgical group were better than those of the conservative group at 1 month and 6 months, but there was no significant difference between the two groups at 12-month time point. It is not clear what causes the heterogeneity, and this result provides poor evidence for the paper. Existing evidence indicates that both PDD and open surgery are better than conservative treatment in reducing VAS score and NDI, and have advantages in at least one year. However, the therapeutic benefit of surgical treatment in NDI gradually decreases with the extension of the follow-up time, which is a changing process. The short-term (within 6 months) efficacy of surgical treatment is better than that of conservative treatment in terms of NDI, but the long-term benefits are not significantly different from that of conservative treatment.
Two studies26,29 involving 120 patients provided ROM data, and two studies27,30 involving 199 patients provided mental health data. Statistical results indicate that available data are insufficient to justify a difference between surgical and conservative treatment in ROM(MD = 2.91, 95% CI (−4.51,10.33), P = .44) and mental health (SMD = .05, 95% CI (−.24,0.33), P = .74). From the results of this study, conservative treatment seems to be more appropriate for patients with less significant pain because it can avoid the risks of surgery, and the natural course of CSR is also long-term improvement. 32 The included studies used different conservative approaches. Patients in study 30 received a series of conservative treatments including transcutaneous electrical nerve stimulation, progressive cervical movement, gradual reduction of cervical collar use, and postural rehabilitation by Mezieres technique, analgesics, and/or non-steroidal anti-inflammatory drugs, but did not say how often or how long the treatment would last. Patients in study 25 received steroids and NSAIDs for 6 weeks and mechanical traction in supine position at 10% of their body weight, parallel to the cervical spine, twice a week for 5 weeks. In the end, 18 patients (45%) decided to have surgical treatment before 12 months, all of whom were younger than 50 years old, and the elderly were treated with mechanical traction until the end of the study. Patients with severe pain and a desire to return to work as soon as possible seemed to have a higher benefit from surgery. The other 4 studies26-29 used conservative treatment options including transcutaneous electrical nerve stimulation, heat (moist pack, ultrasound) or cold and massage, manual traction and gentle mobilization combined with heat therapy or relaxation exercises, active exercises, ergonomic instructions, postural corrections, co-ordination exercises, pain management education, and cervical collar. These treatments lasted for at least 3 months, 1–2 times a week (wearing cervical collar alone also lasted for 3 months, but needed to be worn every day). The range of conservative treatment options received by patients is not detailed in the literature because the choice of methods is determined by the physical therapist’s individual will and the patient’s situation. Current evidence suggests that conservative treatment as mentioned above at a frequency of 1–2 times a week for at least 3 months is effective in providing long-term benefits. However, the role of each physical therapy technique in the treatment process remains unclear. Questions such as whether the combination of several technologies will bring superposition of curative effect and which conservative treatment is the most effective have not been clearly answered at present, and further research is needed.
It is important to consider the complications of any treatment, especially open surgery, as some complications can be permanent or even fatal. Although the overall long-term outcome is favorable, there have been some reports of complications in the short and long term after surgery.33-36 Postoperative complications may include dysphagia, wound hematoma, recurrent laryngeal nerve palsy, esophageal or pharyngeal perforation, and sometimes dural tearing. 33 In the long-term follow-up after ACDF, there were reports of adjacent segment degeneration (ASD),37,38 stent failure, and graft extrusion. 39 Only three of the six studies included in this study reported complications.25,28,30 In study, 25 one patient had persistent pain due to implant compression due to improper placement. The implant was repositioned in an open procedure and no other discomfort was observed for 6 months. No complications were recorded in the traction group. The other two studies28,30 reported no complications, and three of them26,27,29 had unclear postoperative complications. Currently available data suggest that long-term benefits of surgical treatment exist, but the extent of postoperative complications at long-term follow-up is unclear, which adds a discreditable element to the results and requires further study. There were reassuringly few complications reported in the included literature. Some new minimally invasive surgical techniques, such as dorsal foraminotomy, percutaneous endoscopic cervical discectomy (PECD), and anterior uncal microforaminotomy, are progressing, and clinical studies need to be followed up.40,41
Limitations
The strength of any meta-analysis to a certain extent depends on the homogeneity and quality of the studies included. A number of factors limit our reviews ability to draw strong conclusions for surgical or conservative treatment to CSR. First, in this study, only published English literature were retrieved, which may lead to publication bias due to incomplete literature collection. Second, the surgical methods and conservative treatment methods were not exactly the same between each of the included studies, and the follow-up time was also different, we did not perform a subgroup analyses for the different types of surgical treatment because of the amount of related study. Although the subgroup analysis was conducted to reduce the bias caused by the difference in follow-up time, time consistency could not be achieved, and only a larger period of time could be compared, which may have a certain impact on the outcome of the merger and generate a certain risk of bias. Few studies with follow-up of more than one year did not conduct quantitative analysis, but only described the results, and the sample size was small, resulting in low credibility of evidence on long-term benefits. Third, some of the included studies showed poor methodological quality based on the Cochrane Collaboration risk bias tool. To some extent, the credibility of the research results was affected; suggests that future researchers should strictly ensure the quality of clinical trial methodology, pay attention to the implementation of the scheme of hidden especially blinded, and avoid to produce selection and measurement bias. Fourth, the patients could not be blinded for the comparison in the surgical vs conservative group, which generated potential performance and response biases. Finally, several outcomes such as 36-item Short-Form Health Survey were and Mood Adjective Check List examined in only a small number of studies, which could have let to the overestimation of the effect sizes.
Conclusion
This study provides high-quality evidence for surgical and conservative treatment of cervical spondylotic radiculopathy. The evidence indicates that surgical treatment is better than conservative treatment in terms of VAS score and NDI score, and superior to conservative treatment in less than one year. There was no evidence of a difference between surgical and conservative care in ROM and mental health.
Compared with conservative treatment, surgical treatment had a faster onset of response, especially in pain relief, but did not have a significant advantage in range of motion or NDI. This seems to mean that for patients with severe or even unbearable pain, the benefits of surgery as soon as possible will be significant. Although it is not clear whether the short-term risks of surgery are outweighed by the long-term benefits, rapid pain relief is necessary. Conservative treatment (including medical exercise therapy, mechanical cervical tractions, transcutaneous electrical nerve stimulation, pain management education, and cervical collar) once or twice a week for 3 months is beneficial in the long term and avoids the risks of surgery. In consideration of the good natural history of CSR and the relatively good outcome of conservative treatment (although symptom relief is slow), we think that surgery is not necessary for patients who do not need rapid pain relief.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was partially supported by the Scientific research project of Tianjin Education Commission [no. 2019KJ064].
ORCID iD
Luyao Huo https://orcid.org/0000-0002-4208-1887
References
- 1.Zhu LG, Yu J. Research progress of non-operative treatment for cervical spondylotic radiculopathy. Chin J Trad Med Traum Orthop. 2011; 19(4): 66-69. [Google Scholar]
- 2.Wang YG, Guo XQ, Zhang Q, et al. A systematic review on the treatment of nerve root cervical disease by manipulation. Chin J Trad Chin Med Phar. 2013; 28(2): 499-503. [Google Scholar]
- 3.Zhu GM, Sun WQ, Shen GQ, et al. Mechanisms of spinal micro-adjustment manipulations in treating cervical spondylotic radiculopathy. J Acupuncture Chiropractic Tuina Sci. 2007; 5: 68-70. [Google Scholar]
- 4.Mayfield FH. Cervical spondylotic and myelopathy. Adv Neurol. 1985; 22: 307-321. [PubMed] [Google Scholar]
- 5.Epstein JA, Lavine LS, Aronson HA, Epstein BS. Cervical spondylotic radiculopathy. Clin Orthop Relat Res. 1965; 40: 113-122. [PubMed] [Google Scholar]
- 6.Zhu LG. Clinical observation on improvement of motion range of cervical spine of patients with cervical spondylotic treated with rotation-traction manipulation and neck pain particles and cervical neck pain rehabilitation exercises [in Chinese]. Zhong Guo Gu Shang. 2010; 23: 750-753. [PubMed] [Google Scholar]
- 7.Salemi G, Savettieri G, Meneghini F, et al. Prevalence of cervical spondylotic radiculopathy: A door-to-door survey in a Sicilian municipality. Acta Neurol Scand. 1996; 93: 184-188. [DOI] [PubMed] [Google Scholar]
- 8.Yang F, Li WX, Liu Z, Liu L. Balance chiropractic therapy for cervical spondylotic radiculopathy: Study protocol for a randomized controlled trial. Trials. 2016. Oct 22; 17(1): 513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thoomes E, Thoomes-de Graaf M, Cleland J, Gallina A, Falla D. Timing of evidence-based non-surgical interventions as part of multimodal treatment guidelines for the management of cervical radiculopathy: A Delphi study protocol. BMJ Open. 2021. Mar 16; 11(3): e043021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong JJ, Côté P, Quesnele JJ, Stern PJ, Mior SA. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: A systematic review of the literature. Spine J. 2014; 14: 1781-1789. [DOI] [PubMed] [Google Scholar]
- 11.Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994; 117(pt 2): 325-335. [DOI] [PubMed] [Google Scholar]
- 12.Kuijper B, Tans JT, Schimsheimer RJ, et al. Degenerative cervical radiculopathy: Diagnosis and conservative treatment. A review. Eur Neurol. 2009; 16: 15-20. [DOI] [PubMed] [Google Scholar]
- 13.Radhakrishan K, Litchy WJ, O’Fallon WM, et al. Epidemiology of cervical radiculopathy: A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994; 117: 325-335. [DOI] [PubMed] [Google Scholar]
- 14.Costello MMT. Treatment of a patient with cervical radiculopathy using thoracic Spine thrust manipulation, soft tissue mobilization, and exercise. J Man Manip Ther. 2008; 16: 129-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bono CM, Ghiselli G, Gilbert TJ, et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011; 11: 64-72. [DOI] [PubMed] [Google Scholar]
- 16.Salt E, Wright C, Kelly S, et al. A systematic literature review on the effectiveness of non-invasive therapy for cervicobrachial pain. Man Ther. 2011; 16: 53-65. [DOI] [PubMed] [Google Scholar]
- 17.Thoomes EJ, Scholten-Peeters W, Koes B, Falla D, Verhagen AP. The effectiveness of conservative treatment for patients with cervical radiculopathy. Clin J Pain. 2013; 29: 1073-1086. [DOI] [PubMed] [Google Scholar]
- 18.Nikolaidis I, Fouyas IP, Sandercock PA, Statham PF. Surgery for cervical radiculopathy or myelopathy. Cochrane Database Syst Rev. 2010; 24: Cd001466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braakman R. Management of cervical spondylotic myelopathy and radiculopathy. J Neurol Neurosurg Psychiatry. 1994; 57(3): 257-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu YL, Woo E, Huang CY. Cervical spondylotic myelopathy and radiculopathy. Acta Neurol Scand. 1987; 75(6): 367-373. [DOI] [PubMed] [Google Scholar]
- 21.Fehlings MG, Arvin B. Surgical management of cervical degenerative disease: The evidence related to indications, impact, and outcome. J Neurosurg Spine. 2009; 11(2): 97-100. [DOI] [PubMed] [Google Scholar]
- 22.Matz PG, Holly LT, Groff MW, et al. Indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine. 2009; 11(2): 174-182. [DOI] [PubMed] [Google Scholar]
- 23.Matz PG, Ryken TC, Groff MW, et al. Techniques for anterior cervical decompression for radiculopathy. J Neurosurg Spine. 2009; 11(2): 183-197. [DOI] [PubMed] [Google Scholar]
- 24.Tan J, Zheng Y, Gong L, Liu X, Li J, Du W. Anterior cervical discectomy and interbody fusion by endoscopic approach: A preliminary report. J Neurosurg Spine. 2008; 8(1): 17-21. [DOI] [PubMed] [Google Scholar]
- 25.Lenzi J, Nardone A, Passacantilli E, Caporlingua A, Lapadula G, Caporlingua F. Posterior cervical transfacet fusion with facetal spacer for the treatment of single-level cervical radiculopathy: A randomized, controlled prospective study. World Neurosurg. 2017. Apr; 100: 7-14. [DOI] [PubMed] [Google Scholar]
- 26.Persson L, Karlberg M, Magnusson M. Effects of different treatments on postural performance in patients with cervical root compression1. J Vestib Res. 1996. Nov-Dec; 6(6): 439-453. [PubMed] [Google Scholar]
- 27.Persson LC, Lilja A. Pain, coping, emotional state and physical function in patients with chronic radicular neck pain. A comparison between patients treated with surgery, physiotherapy or neck collar - a blinded, prospective randomized study. Disabil Rehabil. 2001. May 20; 23(8): 325-335. [DOI] [PubMed] [Google Scholar]
- 28.Engquist M, Löfgren H, Öberg B, et al. Surgery versus nonsurgical treatment of cervical radiculopathy: A prospective, randomized study comparing surgery plus physiotherapy with physiotherapy alone with a 2-year follow-up. Spine. 2013. Sep 15; 38(20): 1715-1722. [DOI] [PubMed] [Google Scholar]
- 29.Peolsson A, Söderlund A, Engquist M, et al. Physical function outcome in cervical radiculopathy patients after physiotherapy alone compared with anterior surgery followed by physiotherapy: a prospective randomized study with a 2-year follow-up. Spine. 2013. Feb 15; 38(4): 300-307. [DOI] [PubMed] [Google Scholar]
- 30.Cesaroni A, Nardi PV. Plasma disc decompression for contained cervical disc herniation: A randomized, controlled trial. Eur Spine J. 2010. Mar; 19(3): 477-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Engquist M, Löfgren H, Öberg B, et al. A 5- to 8-year randomized study on the treatment of cervical radiculopathy: Anterior cervical decompression and fusion plus physiotherapy versus physiotherapy alone. J Neurosurg Spine. 2017. Jan; 26(1): 19-27. [DOI] [PubMed] [Google Scholar]
- 32.Bier JD, Scholten- Peeters WGM, Staal JB, et al. Clinical practice guideline for physical therapy assessment and treatment in patients with nonspecific neck pain. Phys Ther. 2018; 98: 162-171. [DOI] [PubMed] [Google Scholar]
- 33.Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine. 2007; 32: 2310-2317. [DOI] [PubMed] [Google Scholar]
- 34.Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004; 4: 624-628. [DOI] [PubMed] [Google Scholar]
- 35.Kast E, Derakhshani S, Bothmann M, Oberle J. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev. 2009; 32: 207-214. [DOI] [PubMed] [Google Scholar]
- 36.Jagannathan J, Shaff rey CI, Oskouian RJ, et al. Radiographic and clinical outcomes following single level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine. 2008; 8: 420-428. [DOI] [PubMed] [Google Scholar]
- 37.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis*. J Bone Joint Surg [Am]. 1999; 81: 519-528. [DOI] [PubMed] [Google Scholar]
- 38.Elsawaf A, Mastronardi L, Roperto R, Bozzao A, Caroli M, Ferrante L. Effect of cervical dynamics on adjacent segment degeneration after anterior cervical fusion with cages. Neurosurg Rev. 2009; 32: 215-224. [DOI] [PubMed] [Google Scholar]
- 39.Fujibayashi S, Neo M, Nakamura T. Stand alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: Sequential changes in cage subsidence. J Clin Neurosci. 2008; 15: 1017-1022. [DOI] [PubMed] [Google Scholar]
- 40.Lee SH, Lee JH, Choi WC, Jung B, Mehta R. Anterior minimally invasive approaches for the cervical spine. Orthop Clin N Am. 2007; 38: 327-v. [DOI] [PubMed] [Google Scholar]
- 41.Choi G, Arbatti NJ, Modi HN, et al. Transcorporeal tunnel approach for unilateral cervical radiculopathy: A 2-year follow-up review and results. Minim Invasive Neurosurg. 2010. Jun; 53(3): 127-131. [DOI] [PubMed] [Google Scholar]
- 42.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008; 336: 924-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ. What is "quality of evidence" and why is it important to clinicians? BMJ. 2008; 336: 995-998. [DOI] [PMC free article] [PubMed] [Google Scholar]